Supporting Statement A-B 12 31 07
Supporting Statement A-B 12 31 07.doc
Survey of 911 Emergency Treatment for Heart Disease and Stroke
OMB: 0920-0782
Survey of 911 Emergency Treatment for Heart Disease and Stroke
Supporting Statement
Part A
December 26, 2007
Contact:
Ishmael Williams
Telephone: (770) 488-8060
Fax: (770) 488-8151
Email: [email protected]
Division for Heart Disease and Stroke Prevention
National Center for Chronic Disease Prevention and Health Promotion
Centers for Disease Control and Prevention
Koger Center, MS K-47
Atlanta, Georgia 30341
TABLE OF CONTENTS
A. JUSTIFICATION
A.1. Circumstances Making the Information Collection Necessary
A.2. Purpose and Use of Information Collection
A.3. Use of Improved Information Technology and Burden Reduction
A.4. Efforts to Identify Duplication and Use of Similar Information
A.5. Impact on Small Businesses or Other Small Entities
A.6. Consequences of Collecting the Information Less Frequently
A.7. Special Circumstances Relating to the Guidelines of 5 CFR 1320.5
A.8. Comments in Response to the Federal Register Notice and Efforts to Consult Outside the Agency
A.9. Explanation of Any Payment or Gift to Respondents
A.10. Assurance of Confidentiality Provided to Respondents
A.11. Justification for Sensitive Questions
A.12. Estimates of Annualized Burden hours and costs
A.13. Estimates of Other Total Annual Cost to Respondents and Recordkeepers
A.14. Annualized Cost to the Federal Government
A.15. Explanation for Program Changes or Adjustments
A.16 Plans for Tabulation and Publication and Project Time Schedule
A.17 Reason(s) Display of OMB Expiration Date is Inappropriate
A.18. Exceptions to Certification for Paperwork Reduction Act Submissions
LIST OF TABLES – SECTION A
Table A.12-1 Estimated Burden in Hours
Table A.12-2 Estimated Cost to Respondents
Table A.14-1 Estimated Cost to the Federal Government
Table A.16-1 EMS Provider Organization Survey Variables
Table A.16-2 Description of State Profiles in Terms of Pre-hospital Local EMS System Characteristics; and, Comparisons of Local EMS System Characteristics Between States
Table A.16-3 Comparison of Local EMS Provider Profiles by State EMS Context – Type of EMS Administrative Structure
Table A.16-4 Likelihood of Selected Local EMS Provider Characteristic, by Type of State Context
Table A.16-5 Degree of Adoption of Leading Edge Practices, by Selected Characteristic of Local EMS Provider Organization – All States
Table A.16-6 Depth of Local EMS Provider Organization Capability, by Selected Characteristic of Local EMS Service Area – State A
Table A.16-7 Depth of Local EMS Provider Organization Capability, by Selected Characteristic of Local EMS Service Area 3
Table A.16-8 Map of Arkansas—Spatial Distribution Example
Table A.16-9 Project Activity Time Schedule
LIST OF ATTACHMENTS
Attachment A: Authorizing Legislation, Public Health Service Act (PHSA)
Attachment B: Copy of Federal Register 60-Day Notice (February 5, 2007)
Attachment C Screening Script to Identify Supervisor for Interview: Local EMS Provider Survey – Computer Assisted Telephone Interview
Attachment D Local EMS Provider Survey – Computer Assisted Telephone Interview
Attachment D-1 Script for Informed Consent: Local EMS Provider Survey – Computer Assisted Telephone Interview
Attachment E-1 Follow-up Message to the Request for Interview: Sub-State EMS Region Respondent
Attachment E-2 Informed Consent Script: Sub-State EMS Region Respondent
Attachment F Topic Outline for Semi-Structured Telephone Interview: Sub-State EMS Region Respondent
Attachment G Battelle IRB Review Report. Current Implementation Approval – Entire Project
A. JUSTIFICATION
A.1 Circumstances Making the Information Collection Necessary
Cardiac-related deaths and stroke-related deaths are, respectively, the highest and third highest causes of mortality in the United States. Approximately two-thirds of cardiac-related deaths and half of stroke-related deaths occur before the patients arrive at a hospital. This high percentage of “out of hospital” deaths for these health crises in the United States underscores the important role of pre-hospital emergency medical care in our nation’s overall heart disease and stroke outcomes, along with disease prevention programs and policies and hospital emergency department care.
The Division for Heart Disease and Stroke Prevention (DHDSP) of the Centers for Disease Control and Prevention (CDC) National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP) is committed to providing public health leadership and technical assistance so that state and local health and medical programs have the capacity and resources to carry out a comprehensive heart disease and stroke prevention program. All the links in the chain from an individual’s recognition of symptoms to specialized hospital care need to be characterized in order to develop a comprehensive strategy for improving the acute outcomes for heart disease and stroke patients. Pre-hospital EMS care is one of several intervention points for reducing death and disability from an acute coronary or cardiovascular episode. This data collection effort provides valuable information for this segment of the “chain of survival” for heart attack and stroke victims.
As part of achieving its own public health objectives, CDC/DHDSP seeks with this research to: gain a better understanding of pre-hospital EMS capabilities, administration, and oversight; identify important stakeholders for partnering and cooperation; and, characterize the pre-hospital EMS heart attack and stroke emergency treatment protocols in use. This project will help to enhance CDC’s understanding of the contribution of pre-hospital heart attack and stroke emergency medical care as an important component of overall pre-hospital EMS services.
Further, national health surveillance data and other preliminary studies suggest that 911-initiated emergency medical services (EMS) are an important link in our nation’s healthcare delivery system. With improvements, pre-hospital EMS can contribute to decreased rates of mortality and disability related to heart disease and stroke and to a reduction in geographic-based health and health care disparities. Preliminary surveys indicate that the nation’s local 911 emergency medical services often struggle to meet care objectives due to funding constraints for staffing, competing resource needs in fire, police, and emergency management, lack of EMS medical oversight, unmet training and technical support needs, and lack of consensus on treatment protocols for cardiac and stroke emergency care.
The most recent EMS status report to raise the alarm is the 2006 study by the Institute of Medicine of the National Academies (IOM) The Future of Emergency Care in the United States Health System1 which declared the nation’s emergency healthcare system to be in crisis. The report identified a number of problems including inadequate funding and reimbursement to cover costs, inefficiencies brought on by fragmentation of care, overcrowding, ambulance diversions, and staff shortages. The IOM report and the testimony of the authors before Congress called for creation of a well funded, highly coordinated, regionalized, accountable system for emergency care that manages patient flow without ambulance diversion to other hospitals and without lengthy “boarding” of patients in hospital emergency departments awaiting care. The committee recommended enhanced emergency care research to improve systems of care, develop consistent workforce standards, and other improvements. The report also called for consolidation of lead functions for EMS under the Department of Health and Human Services (DHHS).
In 2007, in response to calls for better coordination and support for EMS at the national level, a coordinating committee of federal agencies – the Federal Interagency Committee on Emergency Medical Services (FICEMS) was reauthorized by Congress2 to coordinate efforts of various federal agencies on these critical EMS issues (including the Department of Transportation, Department of Homeland Security, Department of Defense, Federal Communications Commission, and Department of Health and Human Services). CDC has a representative on the FICEMS committee and the Division for Heart Disease and Stroke Prevention (DHDSP) in CDC/NCCDPHP has been chosen to serve on the Technical Working Group in support of FICEMS. Specifically, the Technical Working Group has been tasked to research and implement the IOM recommendations, design a national EMS assessment strategy, and coordinate EMS activities across federal agencies.
With this new and increased national responsibility and authority for CDC over EMS, the data collection described here is anticipated to be an important component of DHDSP’s response to the Congressionally-mandated FICEMS request for coordinated national solutions to the crisis in emergency care. CDC’s response is due to FICEMS at the end of 2008.
The collection of information through a survey of local EMS provider organizations is the centerpiece of the overall study. The study is designed to provide detailed information by collecting information on EMS systems in nine states across the nation. The survey of EMS provider organizations in each of nine states will cover typical depth of capability in various types of EMS organizations, access to expert medical care facilities, the scope of pre-hospital EMS practice for heart attack and stroke, extent of medical direction, and the EMS field practice protocols. This information will characterize these aspects in a wide variety of: community contexts from urban to rural; staffing configurations of career and volunteer emergency medical technicians (EMT) and paramedics; and, the various public and private auspices under which they provide services (e.g., fire departments, stand alone EMS organizations, hospitals).
Also, in some but not all states, counties have been grouped into EMS regions which may provide a degree of similarity in administration within each region, but not necessarily between them. Little is said in the national reports on EMS about the role or impact of this sub-state organizational variation from state to state. Besides the quantitative survey of local EMS provider organizations, this request for information collection also includes interviews with officials that serve as administrators or directors of sub-state EMS regions. With respect to the role of EMS administrators for sub-state regions, five of the states selected for the local EMS provider survey have delineated sub-state EMS regions. These sub-state administrators will be asked to provide insights into the relationship between state-funded EMS oversight agencies, health care alternatives, and local EMS systems managed under local auspices. The sub-state administrators may serve as an important pivot point between state-level program objectives and the enhancement of local EMS systems, by playing a role in the amplification of state level efforts for EMS improvement within a state. A limited number of informal consultations with state level regulatory and medical authorities also will take place, and will complement the local and sub-state region descriptions.
This information collection is being requested for a period of one year. The authorizing legislation for this study is the Public Health Service Act (PHSA) which is included in the United States Code, Title 42, Public Health and Welfare, Chapter 6A. Under the auspices of the U.S. Department of Health and Human Services (DHHS), the CDC is authorized to conduct studies relating to the control and prevention of physical impairments of man. The PHSA, Sec. 241 describes in general terms the powers and duties of the Secretary with respect to research and investigations. These powers include conducting or assisting with research, and entering into contracts for research. Attachment A displays the Authorizing Legislation (PHSA) for this study.
A.2 Purpose and Use of Information Collection
The purpose of the information collected is to obtain a specific set of general purpose statistics for Government use. More specifically, the purpose of the information collection is to conduct in-depth exploratory research on the array of organizational configurations for providing pre-hospital emergency care in order to move perceptions and understanding beyond the anecdotal level. In addition, the research will lend itself to identifying relationships among selected variables as a means of suggesting hypotheses for more detailed research and program planning for pre-hospital EMS.
The information provided by this data collection effort has several practical uses related to the initiatives of the CDC/DHDSP heart disease and stroke program agendas and to the pre-hospital EMS assessment requested by FICEMS, as indicated in the following list:
1) CDC/DHDSP will use the detailed information on the array of pre-hospital EMS provider profiles provided by the local EMS provider survey in its contribution to the FICEMS Technical Working Group, of which it is a member. This working group is tasked with designing a national EMS assessment strategy and improvement plan. CDC’s contribution is due to FICEMS at the end of 2008.
2) State regulatory EMS officials and EMS medical directors can obtain insights from the local EMS provider survey about important EMS issues that need to be addressed in their regulatory, training, and technical assistance programs for local EMS providers.
3) The Heart Disease and Stroke Prevention Programs that exist in many states will use the information to obtain insight into pre-hospital EMS practices and gaps in service levels that can be addressed in their state program plans.
4) The EMS professional community will use the information from the local EMS provider survey -- which is major empirical validation of the scope of practice as it is applied in different states -- as it formulates agendas for research and actions needed to enhance pre-hospital EMS capabilities and consistency across the nation for heart attack and stroke care. No other data set of this nature exists.
5) The DHDSP will use the data set from the local EMS provider survey for examining spatial correlations of heart disease and stroke prevalence, practice levels of local EMS providers, and local infrastructure of greatest concern for improving pre-hospital care and linking it to specialty centers for cardiac and stroke emergencies.
6) The DHDSP and the state heart disease and stroke programs will use the hypotheses suggested by the data set for the design of detailed studies of specific issues important for improvement of local pre-hospital EMS services.
7) Other states not included in this study will use the data collection instrument for the local EMS provider survey for the collection of similar information, thereby extending the reach of the nine-state data set from this study.
A.3 Use of Improved Information Technology and Burden Reduction
The data from the local EMS provider organizations will be collected utilizing Computer Assisted Telephone Interview (CATI) technology for the Local EMS Provider Survey instrument (Attachment D) that is administered to the manager or supervisor of the local EMS organization’s personnel and operations. The CATI technology was selected over the use of a self-administered electronic questionnaire accessed through the internet because the central consideration is to acquire a high quality data set for characterizing these organizations and examining relationships among variables. There are several advantages to the use of the CATI technology including: a) a far higher response rate than is typically achieved for a voluntary self-administered questionnaire, electronic or otherwise; b) higher quality information because the respondent can request clarification if needed; and, c) all EMS organizations have telephone technology, but the smaller and more rural organizations will not necessarily have adequate technology for completing an on-line questionnaire. The CATI technology, compared to the use of a self-administered paper questionnaire, offers the same advantage as a well-programmed internet questionnaire in that the electronic data set is built as responses are entered for each question. Also with a telephone interviewer the respondent is less able to skip questions, which minimizes missing data.
A.4 Efforts to Identify Duplication and Use of Similar Information
A review of major reports (i.e., EMS enhancement Agendas funded by the National Highway Traffic Safety Administration [NHTSA] ) on the state of EMS systems and services did not indicate any data collection effort focused on creating a large, multi-state data set about pre-hospital EMS capabilities specifically focused on the pre-hospital care of cardiac-related crises and strokes. These EMS Agenda documents also indicate that the lack of carefully collected empirical data on pre-hospital EMS services is a major issue for the stakeholders and policy-makers regarding the design and funding of emergency medical systems. The regulation and oversight of local 911 EMS systems is conducted on a state by state basis (and in some instances on a sub-state level), with no national set of guidelines. A major development effort was recently completed (referred to as NEMSIS: National EMS Information System) for the purpose of developing a nomenclature that would enable the creation of comparable data sets on patient encounters and the demographic characteristics of EMS providers. The use of this nomenclature will be voluntary. While almost all states have agreed to its use, it will take several years for it to be widely implemented at either the state or local agency levels.
A large percentage of state level EMS regulatory agencies have web sites. These were examined for the purpose of finding state reports on EMS capabilities or performance, and in particular with respect to cardiac and stroke emergencies. This investigation yielded evidence of relatively minimal data collected by the states examined (including the states selected for this study); few state EMS web sites indicate any systematic data collection from the EMS agencies that they license. When they do, state agencies more typically collect information on EMS trauma response, but not on heart attack and stroke response needs. Some states produce an occasional report on an aspect of training levels or EMS performance, or from an EMS needs assessment conducted at the state level, typically focused on training or equipment needs.
A publication for the EMT/paramedic profession, Journal of EMS (JEMS), in recent years has prepared an annual report based on responses to a questionnaire sent to EMS agencies in the 200 largest cities. The information is collected by JEMS, using a voluntary, self-administered questionnaire. In 2003 the report included information on the response rate, which was 17%, suggesting the need for caution in the use of the information. The response rate has been improving but as of 2005 was still below 40%. The JEMS survey is focused on the service in general, without calling out specific information on pre-hospital EMS care for cardiac and stroke emergencies. Its focus on EMS only in large cities leaves a large gap in information on EMS in medium sized cities and in rural and frontier (largely unpopulated) areas.
With the use of an internet search engine a few reports were found that addressed EMS topics. One type of survey data found is that in which individual EMTs and paramedics were asked to provide information about the nature of their EMS job and their satisfaction with certain elements of it, in order to better understand what would contribute to the retention of EMTs. Two recent surveys report data aggregated at the national level. The “2003 National Survey,” funded in part by the Human Resources Services Administration (HRSA) of DHHS, collected information from state and territorial EMS offices about the structure and function of state EMS offices. This survey updated similar information from earlier national studies, the most recent of which was in 1992. Through special efforts and technology to promote response, the 111 question survey achieved a 100% response rate. The 2006 “National Report Card on the State of Emergency Medicine,” under the auspices of the American College of Emergency Physicians, focused on the state of services in hospital emergency departments. A recent report funded by NHTSA puts forth the “Emergency Medical Services Workforce Agenda for the 21st Century” for which anecdotal information about EMS workforce issues and concerns, especially in relation to rural and volunteer services, was collected through interviews with key informants.
Queries also were made to practitioners and leaders in the field to try to identify recent or existing data collection similar to that for CDC’s study. These include the following contacts.
1. The CDC Principal Investigator attended the annual national meeting of State EMS Directors in 2005. He observed that there were no presentations on the topic of pre-hospital cardiac and stroke care; however, conversations with other attendees indicated there is interest on the part of these national leaders in having data of this nature collected.
2. The CDC Principal Investigator obtained information at the above meeting on the activities being carried out or planned by the Emergency Medical Services Division of NHTSA, none of which are data collection efforts similar to CDC’s planned survey. The CDC principal investigator also spoke with the Chief of the Division, Drew Dawson, about CDC’s planned effort. NHTSA was the lead federal agency on EMS issues and worked cooperatively with other state and federal agencies. Another contact was made with Mr. Dawson in May 2006 to again inquire about NHTSA sponsored surveys, at which time he indicated that CDC’s planned survey does not overlap with NHTSA activities. He also mentioned a long-term survey on EMS career paths (see #5 below).
3. The CDC Principal Investigator talked with other federal-level public health program staff within CDC at the time the data collection contract was let. These staff indicated no such data existed but would be useful.
4. The director of the Minnesota health department’s Stroke Committee was contacted (May 2006) because of information that he was preparing to collect data on the state’s EMS provider agency services for stroke. The Stroke Committee was preparing to develop a stroke training curriculum for pre-hospital EMS but had decided, prior to actually developing and implementing training curricula, an assessment of current practices and knowledge was needed. The survey was conducted as a mail survey with two follow-up letters to all ground-based emergency ambulance companies and achieved a 77% return. A summary report of the findings was released in December 2006. The survey is focused on pre-hospital EMS protocols and care decision making related to patients with symptoms of stroke. Minnesota is not one of the states proposed for the CDC EMS provider study.
5. Conversation with Dr. Ron Pirello (May 2006), chairperson of a committee that oversees the Longitudinal EMT Attributes and Demographic Study (LEADS). He described this as a long-term survey activity to collect information from individual EMTs about the course of their EMS career and as such is not similar to CDC’s planned survey of organizations. The LEADS is done under the auspices of the National Registry of Emergency Medical Technicians (NREMT).
A.5 Impact on Small Businesses or Other Small Entities
The pre-hospital EMS provider organizations to be surveyed for this study range from organizations with only one or two EMTs or paramedics and an ambulance on call for a given shift, to entities in the largest cities that have more than 100 EMTs and paramedics and several emergency transport vehicles. Although many small ambulance companies will be asked to respond to the survey, the impact on theses small entities is not significant for the following reasons. Only one person, representing a supervisory role, from each entity will be asked to provide the information about the entity. The questionnaire is designed as a telephone interview to be completed in about 15 minutes, and this 15-minute data collection is a one-time occurrence. Keeping the interview to 15 minutes limits the number of questions that can be used, including ones that would provide useful detail about specific topics of interest for the overall study. CDC feels this is a necessary trade-off for limiting the time burden to the respondents, in order to not interfere with their other activities.
Personnel from both small and large EMS provider entities are not continuously engaged in emergency runs. The notifications for beginning an emergency run typically come from a separate dispatch communications center so the organization’s regular telephone line is available. Therefore contacting EMS organizations via telephone is feasible, especially since EMS organizations have personnel standing by 24 hours a day. In the smaller entities it may be necessary for the person answering the questions to go on an emergency call, in which case the interviewer will call again later to complete the interview.
All organizations will be asked the same set of questions, since size of the organization may well be a predictor of certain capabilities and of the level of cardiac and stroke care that the organization can provide. The questionnaire is not designed in such a way that the smaller organizations will be asked fewer questions than the larger organizations. While some questions will not be applicable to all organizations so will be skipped, this is not necessarily related to the size of the EMS organization. At the same time, size is a variable expected to be related to other characteristics, necessitating inclusion of the full range of sizes.
For the information collection on the administration of sub-state EMS regions, the staff of the EMS sub-state regions that are to be contacted for an interview are small. An examination of the web-sites indicates that sub-state regions most typically have a board of directors or council that represents the provider organizations in the counties in that region. There will be an executive director or coordinator (i.e., administrator) and maybe some office staff as clerical support or to handle some specific activity (e.g., scheduling training) that is part of the region’s function. In Massachusetts for example, the coordinating activities of each region are handled by a non-profit corporation with a small staff. In the more rural states the administrator for the regional council may only work part time. The interviewer will engage this executive director or administrative coordinator for approximately 45 minutes for a one time data collection using the Topic Guide for Semi-Structured Telephone Interview: Sub-State EMS Region Respondent (Attachment F). Since it is the responsibility of this person to engage in communications related to the region as part of his or her role, the 45-minute interview is likely to be seen as an expected aspect of the position. The interview can be done at whatever is the most convenient time proposed by the respondent.
A.6 Consequences of collecting the information less frequently
This is a one-time data collection effort. Reducing frequency would negate data collection at all. Each organization to be called will only be asked to provide a complete interview once for this study. The set of elements to be covered has been carefully considered in order to balance the need to cover many different pre-hospital EMS organizational and operating variables while not burdening the respondents with an excessively long interview. The survey instrument is designed to take about 15 minutes to complete during a telephone interview. Decreasing the length of the interview further would result in a reduction of the scope of information available to CDC for determining their future research agenda. There are no legal obstacles to reduce the burden. The same is true for the interviews with each of the sub-state regions. Without this one time interview this information about the potential contributions of the sub-regions to local EMS practice, such information will not be available for the analysis. There are no legal obstacles to reduce the burden.
Without these surveys, the CDC’s newly established Division for Heart Disease and Stroke Prevention (DHDSP) will be missing information about one of the several interventions that make up the “chain of survival” for heart attack and stroke sufferers. The information from this survey of pre-hospital EMS capabilities and practices is one piece of the overall process to reduce mortality and prevent disability for people dealing with heart disease and stroke conditions and acute episodes. An understanding of the degree to which pre-hospital capabilities for cardiac and stroke care vary, which capabilities are in the scarcest supply geographically, and how the pre-hospital EMS capacity can be presented geographically in the states selected for the survey are important to the Division as it establishes its agenda for the next few years. The survey instrument’s series of questions that cover the staffing profile and other general characteristics of the unit’s activities are directly applicable to CDC’s development of recommendations to FICEMS on the design of a national EMS assessment in future years (c.f., Section A-1). The data from the study is critical to the ability of DHDSP to provide evidence-based information of this type to the FICEMS Technical Working Group in time for its use in the report due at the end of 2008.
A.7 Special Circumstances Relating to the Guidelines of 5 CFR 1320.5
There is one special circumstance, as described in the Guidelines of 5 CFR 1320.5, related to this data collection. CDC intends to use RUCA codes (Rural Urban Commuting Areas) for classifying each local EMS organization with respect to the characteristics of its service area along a continuum from very rural to very urban. RUCA codes are based on the same theoretical concepts used by the OMB to define county-level metropolitan and micropolitan areas.3 The use of census tracts instead of counties as building blocks for RUCA codes provides a more detailed geographic pattern of settlement classification. A ZIP code approximation of the RUCA codes is also available, so the data set includes the ZIP code for each EMS organization as an indicator of the general geographic location of the service area. The ZIP code approximation, according to its developers, is based on an overlay of ZIP code areas on census tracts and not on a separate analysis of population and commuting data unique to the ZIP code geographic unit.4 There is a strong tendency for EMS service areas to be quite large when the population density is very low, and small where it is quite dense, as in cities with multi-story residential buildings. Thus, EMS response time and time to hospital is expected to be related to the settlement pattern. Also, the size of the population base of an EMS service area tends to affect resources available to support a high level of capability. A more detailed and accurate measure of the rural/urban distinction will be useful for cross-tabulations of various variables.
A.8 Comments in Response to the Federal Register Notice and Efforts to
Consult Outside the Agency
A.8.a Federal Register Notice
A Federal Register 60-Day Notice about the data collection was published in the Federal Register on February 5, 2007, Vol. 72, No. 23, p.5297 (see Attachment B). No public comments were received.
A.8.b. Efforts to Consult Outside the Agency
CDC’s contractor for the data collection talked with various EMS practitioners about the availability of EMS data in general, and the types of data available.
The following EMS practitioners were contacted by phone. Their e-mail addresses have been included, where available.
(a) Mickey Eisenberg, MD, Ph.D., 206-296-4553, Medical Program Director of the King County, Washington, Emergency Medical Services Division. Dr. Eisenberg serves as a paid subject matter expert consultant to CDC’s study. The contractor project team met intermittently with Dr. Eisenberg while designing the survey instrument, provides all research documents to him, and will involve him in the development of recommendations from the findings. E-mail: [email protected]
(b) June, 2004. Richard Benjamin, (509) 826-2835. Washington State Department of Health, Emergency Medicine and Trauma Division. E-mail: [email protected]
(c) June, 2004. Steve Bowman. (360) 236-2873. Washington State Department of Health, Emergency Medicine and Trauma Division, Trauma Registry. [No longer there.]
(e) June, 2004. Shawn Rogers. (405) 271-4027. State EMS Director, State of Oklahoma.
E-mail: [email protected]
(f) June 2004. Dan Manz. (802) 863-7310, Chief, Office of EMS and Injury Prevention. State of Vermont. Leader of project to develop a National EMS Scope of Practice Model. Past President of National Association of State EMS Directors.
E-mail: [email protected]
(g) June 2004. Dr. Greg Mears. (919) 843-0201, Principal Investigator. National EMS Information System (NEMSIS). Project to develop a standardized data collection system for EMS data. University of North Carolina-Chapel Hill, EMS Performance Improvement Center. E-mail: [email protected]
(h) February, 2005. John Rigg. Part-time paramedic. Project Manager for a state wide survey titled Washington Regional Cardiac Arrest Data (WACAD), supported jointly by King County EMS Division. [E-mail not available]
(i) May 2006. Dr. Robert Bass (410-706-5974), an emergency physician serving as president of the National Association of State EMS Organizations (NASEMSO—previously titled NASEMSD, for Association of State EMS Directors), and past president of the National Association of EMS Physicians (NAEMSP), and Maryland State EMS Director. He was asked to review the list of EMS therapies included in the questionnaire for the purpose of identifying the scope of practice in each of the respondent EMS organizations. E-mail: [email protected]
(j) May 2006. Dr. Bob O’Conner (302) 733-4176), past president and current board member of the NAEMSP active in the revision of emergency cardiac care guidelines. Now an Emergency Medicine Professor at the University of Virginia Health System. He was asked to review the list of EMS therapies included in the questionnaire for the purpose of identifying the scope of practice in each of the respondent EMS organizations. E-mail: [email protected]
A.9 Explanation of any Payment or Gift to Respondents
None of the respondents will be provided payment or a gift in exchange for their participation in an interview.
A.10 Assurance of Confidentiality Provided to Respondents
CDC Privacy staff have reviewed this information collection request and determined that the Privacy Act does not apply. For the Local EMS Provider Survey Computer-Assisted Telephone Interview (CATI) the name of the organization is kept but the name of the person who provides the information about the organization and its service area resources is not retained as part of the data file (see Script for Informed Consent. Attachment D-1). The Local EMS Provider Survey CATI uses the “Screening Script to Identify Respondent for Interview” (Attachment C) to identify the appropriate EMS operations supervisory person to provide the information. For all questions, the respondents are asked to provide information on the basis of their role in an EMS organization; no personal information about the respondent is collected. The responses to the survey questions are recorded electronically as the interview is conducted by a trained telephone interviewer in the survey operations center of the Battelle Centers for Public Health Research and Evaluation, the data collection contractor. All electronic project data files will be password protected and access to the files will be limited to authorized project staff. CDC will receive an analysis data set. This data set will be provided in two separate files, one of which will contain the data records identified by the ID codes for each respondent organization. The other file will contain a cross-walk of the respondent organization ID code and the organization name and address.
The name and address of the local EMS provider organization is to be retained as part of the data set because the CDC unit for which data are being collected engages in small area analyses regarding the distribution of heart disease, stroke and relevant health-related services. Greater specificity in geo-coding is achieved when the name and address of a health care service (e.g. an EMS unit) is available, thereby enhancing the accuracy for examining issues related to access to care in which the data are examined in relation to other public use data (e.g., road networks, specialty care hospitals). The contractor, when preparing and displaying the tabulations of the data, does not intend to use the name or street address of the provider units. The data will be aggregated at the state level for tabulation. A separate pass-word protected electronic file will be created that links the name of the organization with the unique identifier in the data record for that organization. Given the number of provider organizations in each state, a particular organization should not be identifiable in frequencies for sub-sets of the state’s data used as variables. Where necessary, table cells can be left blank or categories adjusted to capture larger numbers of organizations. The respondents are advised of the inclusion of the agency’s name in the CDC data set when they are informed about the nature of the Local EMS Provider Survey and asked to indicate verbal consent (see Attachment D-1) to the telephone interview
The semi-structured telephone interview with the administrators of each of ten sub-state EMS regions results in a set of notes taken by the professional social scientist interviewer during the interview. The Topic Guide for the Semi-Structured Telephone Interview with each of the 10 Sub-State EMS Region Respondents (Attachment F) focuses on the function of the EMS region and the activities associated with their position and the EMS region in relation to local EMS providers and state EMS authorities. The responses sought are all role-based without personal information. Each interview and its corresponding file of the notes will have a unique identifier. A separate electronic file will be created that contains the list linking the unique identifier to the organization represented. Both files will be pass-word protected and access to the files will be limited to authorized project staff. The Follow-up Message to the Request for Interview (Attachment E-1) that reminds the respondent about the date and time of the interview includes the Informed Consent Script for the Sub-State EMS Region Respondents (Attachment E-2). This script advises the respondent that in the qualitative analysis of the responses the information they provide about the function and activities of their EMS region will be linked with the particular state, making it likely that it will be evident who provided the information for that region. Persons acting in a civil servant role are familiar with this aspect of their role.
It is the policy of the contractor’s Institutional Review Board (IRB) to review all primary data collection plans, independent of the unit of analysis. The project’s information collection design and procedures have been reviewed and assessed to be of minimal risk by the contractor’s IRB (see Attachment G, Battelle IRB Review Report. Current Implementation Approval).
A.11 Justification for Sensitive Questions
There are no sensitive personal questions in the Local EMS Provider Survey (Attachment D). The organization will be the unit of analysis and all questions in the survey relate to characteristics and practices of the organization. The person identified as appropriate to provide the information for the Local EMS Provider Survey- CATI will not be asked any questions about him/herself; all questions refer to the organization. The respondents for the sub-state EMS region semi-structured interviews will be asked to provide only role-based information. The respondents will be asked about which EMS credential they have and remainder of the topics focus on functions and issues related to the region and its relationship with the state EMS agency and the local provider units (see Attachment F, Topic Guide for Semi-Structured Telephone Interview: Sub-State EMS Region Respondent).
A.12. Estimates of Annualized Burden Hours and Costs
A.12.a Burden in Hours
OMB review and approval is requested for a telephone survey of 2,250 local EMS provider organizations and ten exploratory telephone interviews with two administrators in each of five sub-state EMS regions. The duration of the data collection and analysis is one year. The survey of local EMS provider organizations consists of a one-time interview with approximately 1,800 local EMS provider organizations. All 2,250 local EMS provider organizations contacted will participate in an estimated 2-minute set of questions that the interviewer will ask in order to ascertain the appropriate respondent for the survey (see Attachment C: Screening Script to Identify Supervisor for Interview). As shown in Table A.12.1, the estimated total burden in hours for the two minute screening call is 75. An estimated total of 1,800 respondents, which is 80% of the 2,250 organizations contacted, will agree to participate in the 15-minute telephone interview. As shown in Table A.12.1, the estimated total burden in hours for the 15-minute interview is 450.
The burden hour estimate for the Local EMS Provider Survey was derived from experience with developing questionnaires and a pretest of the instrument. The pre-test of the draft instrument, conducted by telephone with eight local EMS provider organizations verified that the reading of the Script for Informed Consent (Attachment D-1) and the interview questions and responses for the Local EMS Provider Survey – Computer Assisted Telephone Interview (Attachment D) take about 15 minutes to complete. The final instrument was tested through role playing by the contractor’s survey manager and a telephone interviewer to verify appropriate skip patterns for each type of organizational configuration; the approximately 15-minute length was validated.
The semi-structured interviews with administrators of selected sub-state EMS regions will consist of one-time telephone interviews with ten EMS region administrators. The estimated length of the interview is 45 minutes. A 100% response rate is expected. The estimated burden in hours of these interviews is 8. The estimated burden in hours is based on the researchers’ experience with interviews with public officials and the intent to hold the interview to 45 minutes. There are 12 topics in the Topic Guide for Semi-Structured Telephone Interview: Sub-State EMS Region Respondent (Attachment F). It is expected that some of the respondents’ responses will address more than one topic, so there will not be a need for a specific question to initiate each topic.
Table A.12-1 provides the burden hours for each of the two data collection efforts. The total estimated burden in hours for respondents in these information collection activities is 533 hours.
Table A.12-1 Estimated Burden in Hours
Type of Respondents |
Form Name |
No. of Respondents |
No. of Responses per Respondent |
Average Burden per Response (in hours) |
Total Burden (in hours)
|
Supervisor/ Manager of EMS Personnel |
Screening Script to Identify Supervisor for Interview |
2,250
|
1 |
2/60 |
75 |
Local EMS Provider Survey |
1,800 |
1 |
15/60 |
450 |
|
Administrator/ Director of Sub-state EMS Region |
Topic Guide for Semi-Structured Telephone Interview |
10 |
1 |
45/60 |
8 |
Total |
533 |
||||
The local EMS provider organizations and the sub-state EMS region organizations included in the study will include a mix of both private and public organizations. The organizations that respond to the two minute Screening Script to Identify Supervisor for Interview for the Local EMS Provider survey are estimated to include 1,687 public organizations and 563 private. The organizations that respond to the 15 minute Local EMS Provider Survey – Computer Assisted Telephone Interview are estimated to include 1,350 public organizations and 450 private.
The ten sub-state EMS region organizations included in the study will include a mix of both private and public organizations. The organizations that respond to the 45 minute Semi-Structured Telephone Interview for Sub-State EMS Region respondents are estimated include five public organizations and five private.
A.12.b. Cost to Respondents
The estimated cost to respondents for the Local EMS Provider Survey – Computer Assisted Telephone Interview is shown in Table A.12-2. The identification of the job category of the respondent, the corresponding estimated hourly wage, and its source is as follows:
Supervisor/Manager of EMS Personnel: The hourly rate for the supervisor or operations manager of a local-level EMS provider organization is based on a salary survey conducted in 2006 by Fitch & Associates, for the JEMS (Journal of Emergency Medical Services).5 The survey collects salary information for 15 different EMS personnel titles. The salary data for the category of “EMS Operations Manager/Chief” is used to calculate an estimated average hourly wage of $31.61 for a supervisor/operations manager of EMS personnel. Given the average starting salary ($54,310) and average maximum salary ($72,139) for an EMS Operations Manager/Chief, the estimated mean salary of Local EMS Provider organization supervisors is $63,224. The cost estimate assumes a 2080 hour work year (52 weeks of 40 paid hours), for an hourly wage of $30.40.
Table A.12-2, using an average hourly rate of $30.40 displays the costs to respondents of the two minute screening interviews and the 15 minute interview. The first row assumes that 2,250 local EMS provider organizations will be contacted by the telephone interviewer who will spend approximately two minutes with the contact asking the set of questions in the Screening Script (Attachment C) designed to identify the appropriate respondent for the local EMS Provider Survey. The second row assumes that approximately 80% of the 2,250 local EMS provider organizations contacted, or 1800, will complete the 15 minute Local EMS Provider Survey CATI (Attachment D). The total cost for the former is estimated to be $2,280, and for the latter, $13,680.6
Table A.12-2 also displays the estimated cost of $225 for the 45-minute semi-structured telephone interviews (see Attachment F) with ten Sub-State EMS Region respondents. The average hourly wage of $30.06 based on an estimated annual salary figure of $62,5337`for the job of executive director of a state government non-profit organization and the assumption of a 2080 hour work year (52 weeks of 40 paid hours). The cost to respondents assumes a 100% response rate for ten sub-state EMS regions for a total cost of $225. Table A.12-2 displays a total estimated cost to respondents of $16,185.
Table A.12-2. Estimated Cost to Respondents
Type of Respondent |
Form Name |
No. of Respondents |
No. of Responses per Respondent |
Average Burden per Response (in hours) |
Average Hourly Wage
|
Total Cost |
Supervisor/ Manager of EMS Personnel |
Screening Script to Identify Supervisor for Interview |
2,250
|
1 |
2/60 |
$30.40 |
$2,280 |
Local EMS Provider Survey |
1,800 |
1 |
15/60 |
$30.40 |
$13,680 |
|
Administrator/ Director of Sub-state EMS Region |
Topic Guide for Semi-Structured Telephone Interview |
10 |
1 |
45/60 |
$30.06 |
$225
|
Total |
$16,185 |
|||||
A.13 Estimates of other total annual cost to respondents and recordkeepers
There are neither (a) total capital and start-up costs, nor (b) operation, maintenance, or maintenance and purchase of services cost to respondents in either survey.
A.14 Annualized Cost to the Federal Government
The study is funded through the Centers for Disease Control and Prevention (CDC), NCCDPHP, Division of Heart Disease and Stroke Prevention (DHDSP). The contractor project cost of $411,186 to implement the survey of Local EMS provider organizations and the semi-structured telephone interviews with the administrators of sub-state EMS regions includes formative research, survey design, expert emergency medicine consultant, response to required reviews including the PRA, the CATI programming and interviewers, data analysis, a working group meeting with subject matter experts, report preparation, data set transfer to CDC, and project management. The cost of Federal government personnel is estimated to be $13,486 which includes one Federal employee at GS-13 who will be involved for approximately 10% of his time for the project to coordinate the planning and perform technical monitor duties. In addition, one Federal employee at GS-14 will be involved for approximately 5% of her time for the project serving as Principal Investigator. The cost to the government for Federal personnel is based on 10% of the mean salary for GS-13 and 5% of mean salary for a GS-14.
As shown in Table A.14.1, the cost to the Federal government is $424,672. This includes the salary cost ($13,486) of the Federal staff and the program funds to the contractor ($411,186).
Table A.14-1. Estimated Cost to the Federal Government
Type of Cost |
Total Cost |
Federal Personnel |
$13,486 |
Program Funds to Contractor |
$411,186 |
Total |
$424,672 |
A.15 Explanation for Program Changes or Adjustments
This is new data collection.
A.16. Plans for tabulation and publication and project time schedule
A.16.a Tabulation and Analysis Plan
The major data collection effort is a survey of local EMS provider organizations. Information will be collected from all the provider organizations in each of nine purposively selected states, using computer assisted telephone interview (CATI) technology. The survey technology includes programming that tabulates the responses to each question as the interviewer enters them, providing a cumulative data set as the survey progresses. Even though the CATI technology helps to eliminate certain kinds of data entry errors, it still is necessary to examine and clean the data set before beginning the analysis. After conducting a preliminary analysis the contractor implementing the survey will provide the CDC with a raw data set and code book which CDC can use when working on publications. The raw data will be prepared for use with SPSS or SAS analysis software, depending on the CDC technical monitor’s preference. The contractor will carry out initial analysis on the data to prepare descriptive statistics for all the variables, by state, and cross-tabulations of selected variables to examine relationships, both of which can provide the basis for at least one journal article or conference presentation by CDC soon after the initial data analysis is completed. Both the EMS community and the chronic disease community have indicated an interest in the findings from the survey. The states selected for data collection represent a purposively selected array of regions, demographics, and state rates of heart disease and stroke mortality. The data patterns from each state can be compared with those of other states in the study and hypotheses proposed about the relationship between state EMS structures and scope of practice profiles for the local EMS provider organizations. However, the findings from one state are not generalizable to any other states. Findings from the aggregated data for each state can be compared to each other for similarities and differences with respect to context and services. They can also be used for hypothesis generation, and can be used for consideration of future research into topics of particular use for addressing the potential contributions of pre-hospital EMS care for heart and stroke emergencies. Particular elements of the data set will be selected and prepared for use by DHDSP as supporting evidence for recommendations about EMS assessments for FICEMS. The survey instrument, or parts of it, can be used by other states that wish to collect similar information and have a basis for comparison of their findings to those from the study states.
Attachment D provides the Local EMS Provider Survey – Computer Assisted Telephone Interview instrument. The survey instrument content can be summarized in terms of five conceptual variables (CV) as shown below in Table A.16-1. These will be used to provide a general description of the data analysis. The actual analysis will also include the use of the separate elements that make up the conceptual variables for preparing the profile of EMS organizations in each of the nine states, and for testing hypotheses about relationships among the individual variables.
Table A.16-1 EMS Provider Organization Variables
Conceptual Variables (CV) |
Constituent Elements |
CV-1. Degree of EMS organizations’ adoption of leading edge practices for pre-hospital cardiac and stroke care. [Percent local EMS provider organization use of newest therapies/techniques]
|
Determined from survey questions on permitted therapies and techniques. Specification of the leading edge therapies will be sought from subject matter experts in the stakeholder group closer to the time of the survey because consensus changes over time and place. |
CV-2. Scope of practice of organization’s EMT/paramedic staff [EMT-B/EMT-I/Paramedic use of each of the therapies/techniques listed]
|
Determined from survey questions on permitted therapies and techniques, by EMT certification level. |
CV-3. Degree of access to medical direction. [Percent of EMS provider organizations with each of the elements.] [High, medium, low access to medical direction] |
Elements from survey questions including: having local Medical Director; level of interaction with Medical Director; immediate on-line access to medical consultation during runs.) |
CV-4. Density of local care system elements for enhancing cardiac and stroke emergency care. [Percent of EMS service areas with each of the preferred care system elements] [Percent of EMS service areas with all/some/none of the preferred care system elements] |
Elements from survey questions including: local availability of primary stroke center; hospital with heart catheter lab; certification requirement and assist functions provided by call takers/dispatchers; implementation of Enhanced-911 system (i.e., provides address of phone used to call 911) |
CV-5. Depth of EMS organization capability [Percent of EMS provider organizations with specified configurations of each element] [Percent of EMS provider organizations with highest capability level profiles] |
Elements related to survey questions including configuration of ALS/BLS capability; total professional EMS staff; ratio of paramedics to EMTs; ratio of career staff to non-paid volunteer staff, scope of practice. |
CV-6. Settlement density of service area (population density of service area is related to response and transport times due to distance, and to opportunities to maintain skills through use) [Percent of EMS provider organizations serving frontier/rural/town/mixed/urban service areas] |
Approximate population density calculated from respondents’ estimate of square miles in service area and size of population; rural/urban character of the service area based on zip code-based RUCA code; and, subjective response of respondent to an ordinal scale of settlement density. |
The frequency distributions for all the variables, for each of the states, will be produced (see Table A.16-2). These quantitative data provide a descriptive profile of EMS provider organizations variable by variable, for each state. Because these represent all of the provider organizations, the frequency distributions of the state profiles can be compared directly to each other as percentages, without the use of inferential statistics.
Table A.16-2 Description of State Profiles in Terms of Pre-hospital Local
EMS System Characteristics; and, Local EMS System Characteristics, By State
Pre-Hospital Local EMS System Characteristic [see Table A.16-1 for explanation of Conceptual Variables(CV)] |
State 1 |
State 2 |
State 3 |
State 4 |
State n |
CV-1. Degree of EMS organizations’ adoption of leading edge practices for pre-hospital cardiac and stroke care, e.g.: [Percent local EMS provider organization use of newest therapies/techniques] |
% |
|
|
|
|
CV-2. Scope of practice of organization’s EMT/paramedic staff, e.g.: [EMT-B/EMT-I/Paramedic use of each of the therapies/techniques listed] |
|
|
|
|
|
CV-3. Degree of access to medical direction, e.g.: [Percent of EMS provider organizations with each of the elements.] [High, medium, low access to medical direction] |
|
|
|
|
|
CV-4. Density of local care system elements for enhancing cardiac and stroke emergency care, e.g.: [Percent of EMS service areas with each of the preferred care system elements] [Percent of EMS service areas with all/some/none of the preferred care system elements] |
|
|
|
|
|
CV-5. Depth of EMS organization capability, e.g.: [Percent of EMS provider organizations with specified configurations of each element] [Percent of EMS provider organizations with highest capability level profiles] |
|
|
|
|
|
CV-6. Settlement density of service area, e.g.: [Percent of EMS provider organizations serving frontier/rural/town/mixed/urban service areas] |
|
|
|
|
|
Differences in the State Profiles of EMS System Characteristics are hypothesized to be related to variation in the characteristics of the state and (where applicable) region EMS Context. This will be examined by comparing local EMS characteristics in states having one type of context or another. As an example, two possible types of state-level administrative structure, determined from other study data are centralized and regionalized. Table A.16-3 below demonstrates the comparison of the descriptive profiles of local EMS provider organizations in states with a centralized type of administrative structure to those in states with a regionalized type of administrative structure. The same comparison can be made with each of the Characteristics of the State EMS Context described in Table A.16-6 below. The analysis can identify contextual variables such as State EMS administrative structure and regulatory role, presence of a strong state EMS Medical Director, and the degree of support to local EMS organizations from the sub-state Region (where applicable). These can be used as variables for the local organizations and provide insights to the CDC about, for example, relationships observed between the nature of the state EMS agency’s regulatory responsibilities or between the EMS Region’s training responsibilities and the scope of practice of the EMTs and paramedics in the local provider organizations in the state.
Table A.16-3 Comparison of Local EMS Provider Profiles by State EMS Context--Type of EMS Administrative Structure
|
Type of EMS Administrative Structure |
||||||
|
Centralized |
|
Regionalized |
||||
Pre-Hospital Local EMS System Characteristics |
State A |
State B |
State C |
|
State D |
State C |
State n |
CV-1. Degree of EMS organizations’ adoption of leading edge practices for pre-hospital cardiac and stroke care. |
% |
|
|
|
|
|
|
CV-2. Scope of practice of organization’s EMT/paramedic staff |
|
|
|
|
|
|
|
CV-3. Degree of access to medical direction. |
|
|
|
|
|
|
|
CV-4. Density of local care system elements for enhancing cardiac and stroke emergency care. |
|
|
|
|
|
|
|
CV-5. Depth of EMS organization capability |
|
|
|
|
|
|
|
This study is considered exploratory in that it will provide patterns that suggest fertile areas for further, more precise research on the influence of some system variables on others, with practical implications. As an example of a hypothesis to test, states without a state medical director are less likely to have leading edge pre-hospital heart attack mitigation adopted at the local level. This type of analysis can be useful, for example, for defining types of technical assistance or policy development related to enhancing local EMS quality or funding training. Another approach to examining the effect of State Context is to code each Local EMS Provider Organization as being in one type of state or another and compare the expected distribution for a Local EMS variable with actual distribution found in the data (Table A.16-4).
Table A.16-4 Likelihood of Selected Local EMS Provider Characteristic, by Type of State Context
Local EMS Provider Organization Variable [see Table A.16-1 for explanation of Conceptual Variables(CV)] |
Local EMS Provider Organizations in State Type 1 (e.g., With State Medical Director) |
Local EMS Provider Organizations in State Type 2 (e.g., W/o State Medical Director) |
Total |
|
CV-1. Degree of EMS organizations’ adoption of leading edge practices for pre-hospital cardiac and stroke care, e.g.: capnography. |
High |
% |
% |
100% |
Low |
% |
% |
100% |
|
CV-2. Expanded scope of practice of organization’s paramedic staff. |
Yes |
% |
% |
100% |
No |
% |
% |
100% |
|
CV-3. Degree of access to local medical direction. |
High |
% |
% |
100% |
Low |
% |
% |
100% |
|
Hypothesis development also can be conducted from among the characteristics of Local Level EMS Provider Organizations, as illustrated in the following Tables A.16-5, A.16-6, and A.16-7.
Table A.16-5 Degree Of Adoption Of Leading Edge Practices, By Selected Characteristic Of Local EMS Provider Organization – All States
Local EMS Provider Organization Characteristic [see Table A.16-1 for explanation of Conceptual Variables(CV)] |
CV-1. Degree of EMS organizations’ adoption of leading edge practices for pre-hospital cardiac and stroke care. |
|||
High |
Medium |
Low |
||
CV-3. Degree of access to medical direction |
High |
% |
% |
% |
Medium |
% |
% |
% |
|
Low |
% |
% |
% |
|
CV-4. Density of local care system elements for enhancing cardiac and stroke emergency care |
High |
% |
% |
% |
Medium |
% |
% |
% |
|
Low |
% |
% |
% |
|
CV-6. Settlement density of service area |
High |
% |
% |
% |
Medium |
% |
% |
% |
|
Low |
% |
% |
% |
|
|
|
|||
Table A.16-6 Depth of Local EMS Provider Organization Capability, by Selected Characteristic of Local EMS Service Area – State A
Local EMS Provider Organization Characteristic [see Table A.16-1 for explanation of Conceptual Variables(CV)] |
CV-5. Depth of EMS organization capability
|
|||
High |
Medium |
Low |
||
CV-6. Settlement density of service area |
High |
|
|
|
Medium |
|
|
|
|
Low |
|
|
|
|
CV-4. Density of local care system elements for enhancing cardiac and stroke emergency care. |
High |
|
|
|
Medium |
|
|
|
|
Low |
|
|
|
|
Table A.16-7 Depth of Local EMS Provider Organization Capability, by Selected Characteristic of Local EMS Service Area
Local EMS Provider Organization Characteristic [see Table A.16-1 for explanation of Conceptual Variables(CV)] |
CV-2 Local EMS Provider Organizations with Scope of Practice of [EMT-I] Expanded from Norm |
||
Yes |
No |
||
CV-6. Settlement density of service area |
High |
% |
% |
Medium |
% |
% |
|
Low |
% |
% |
|
CV-3. Degree of access to medical direction |
High |
% |
% |
Medium |
% |
% |
|
Low |
% |
% |
|
CV-5. Depth of EMS organization capability
|
High |
% |
% |
Medium |
% |
% |
|
Low |
% |
% |
|
Data will be collected from the total census of local EMS provider organizations in the selected states. In five of the states, the local EMS provider organizations are clustered into state EMS regions that may vary in the function and activities they perform for local EMS organizations. Graphic spatial representations of the distribution of local EMS provider organization capabilities can provide a visual comparison of the relationship between the geographic distribution of heart disease or stroke mortality and the depth of the pre-hospital EMS capability. Admittedly, this information will contain limitations based on the difficulty of accurately mapping 9-1-1 EMS service areas since the service areas of individual EMS agencies don’t necessarily correspond to the boundaries of counties, census tracts, or zip code areas. In the future it should be possible to make more precise analyses as an increasing percentage of service areas now have the geographic coordinates of their service area because of vehicle tracking systems. At the moment, this type of information is not as yet widely available so is not being collected in the local EMS provider survey.
Nonetheless, the local EMS provider survey with a total census of the local EMS organizations, provides the opportunity to show the actual extent of variation in distribution of local EMS provider organizations of selected characteristics or in relation to certain contextual variables. For example, the zip code of the EMS organization’s station can be assigned a value that represents whether or not the EMS organization can provide pre-hospital emergency care at the level of Advanced Life Safety (ALS). The zip code can then be cross-referenced to a census tract or county, which makes it possible to place it on a map as a point, or with skilled application of GIS data smoothing techniques, as an area. CDC’s NCCDPHP has highly skilled GIS analysts who work with this type of data.
Table A.16-8 is an example of the type of graphic display that has been developed to indicate the geographic distribution of the mortality of a disease or condition. For this map, the increasingly intense shading indicates the areas with higher rates.
Table A.16-8. Map of Arkansas Spatial Distribution Example
Example of geographic mapping of the distribution of the mortality rate of a specific disease or condition in the state of Arkansas, prepared by CDC, National Center for Chronic Disease Prevention and Health Prevention (NCCDPHP). Source: http://apps.nccd.cdc.gov/giscvh/(mis3ij554a2byv2c3a1lswzs)/default.aspx
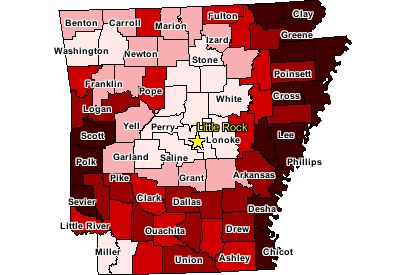
CDC can apply the data for each state in the EMS survey as described above. The survey data supply information to develop an approximate rendition of “Counties with Advanced Life Safety (ALS) EMS services,” as an approach for providing a graphic representation of the extent to which levels of EMS resources correspond to the distribution of rates of heart disease.
As another type of analysis, the CDC division collecting this data engages in small area analyses regarding the distribution of heart disease, stroke and the relevant health-related services. Greater specificity in geo-coding can be achieved with the name and address of a health care service (e.g. an EMS unit), thereby enhancing the accuracy for examining issues related to access to care in which the data are examined in relation to other public use data (e.g., road networks, specialty care hospitals). The maintenance of the local agencies’ name and addresses with the data set is important as information that can be matched with other information.
A-16.b Time Schedule
The time schedule for remaining project activities is presented in Table A.16-9.
Table A.16-9. Project Activity Time Schedule
-
Activity
Est. Schedule
(Months after OMB Approval for Surveys)
Finalize local EMS provider survey CATI programming and provide interviewer training.
Month 0-1
Obtain most recent list of licensed EMS provider organizations from each state EMS regulatory office.
Month 0-1
Conduct survey of EMS provider organizations in nine states, using a CATI.
Month 2 -3
Select and invite EMS subject matter experts and stakeholders to participate in a workshop scheduled for month 6 to review study findings
Month 2-3
Conduct quality assurance on the quantitative data set for the survey, examine initial frequency distributions, and begin populating table shells for the examination of frequencies, state comparisons, and variable relationships.
Month 4*
Conduct telephone semi-structured interviews with administrators of two sub-state EMS regions in each of five states and prepare interview notes for textual coding into themes for use in analysis.
Month 4
Complete quantitative data analysis of local EMS survey and prepare a draft document to present frequencies for each item and the most important cross-tabulations for the workshop. .
Month 4-5
CDC and contractor conduct stakeholder workshop to review study findings and formulate recommendations.
Month 6
Contractor complete draft report of study findings and revisions requested by CDC.
Month 7-8
Contractor submit EMS provider survey data set and documentation to CDC
Month 8
Finalize study report, prepare contributions to the FICEMS report, and submit for CDC clearance
Month 9-10
CDC prepare and submit journal article of selected survey findings
Month 11-12
A.16.c Publication Plan
A working group of stakeholders will be convened to review the initial findings from the analysis of the study data. This group is being selected to include subject matter experts and advocates from both the EMS community and the community working with heart attack and stroke care. The purpose of the workshop is to gain different perspectives on the interpretation of the findings and collect the working group’s insights about further practical uses of the information for their respective professional and practitioner communities. The CDC principal investigator will select and prepare findings and recommendations relevant to CDC’s contributions to the FICEMS report (c.f. Section A-1). The CDC principal investigator intends to prepare at least one article to disseminate the descriptive findings shortly following the finalization of the final report. CDC specialists will then begin working with the data that indicates the geographic location of special services to evaluate the feasibility of using it to do further analysis of spatial relationships of elements related to the distribution of heart disease and stroke, populations particularly vulnerable to acute episodes related to the diseases, and other public use data such as road networks or locations of special care hospitals that must be considered in conjunction with improvement in pre-hospital EMS.
A.17 Reason(s) Display of OMB Expiration Date is Inappropriate
We are not seeking approval to withhold display of the expiration date for OMB approval of the information collection.
A.18 Exceptions to Certification for Paperwork Reduction Act Submissions
There are no exceptions to the certification.
Survey of 911 Emergency Treatment for Heart Disease and Stroke
Supporting Statement
Part B
December 26, 2007
Contact:
Ishmael Williams
Telephone: (770) 488-8060
Fax: (770) 488-8151
Email: [email protected]
Division for Heart Disease and Stroke Prevention
National Center for Chronic Disease Prevention and Health Promotion
Centers for Disease Control and Prevention
Koger Center, MS K-47
Atlanta, Georgia 30341
TABLE OF CONTENTS
B. COLLECTION OF INFORMATION EMPLOYING STATISTICAL
METHODS
B.1. Respondent Universe and Sampling Methods
B.2. Procedures for the Collection of Information
B.3. Methods to Maximize Response Rates and Deal with Nonresponse
B.4. Test of Procedures or Methods to be Undertaken
B.5. Individuals Consulted on Statistical Aspects and Individuals
collecting and/or Analyzing Data
TABLE – SECTION B
Table B.1-1 Approximate Number of Ground-Based EMS Provider Units, by State
LIST OF ATTACHMENTS
Attachment A: Authorizing Legislation, Public Health Service Act (PHSA)
Attachment B: Copy of Federal Register 60-Day Notice (February 5, 2007)
Attachment C Screening Script to Identify Supervisor for Interview: Local EMS Provider Survey – Computer Assisted Telephone Interview
Attachment D Local EMS Provider Survey – Computer Assisted Telephone Interview
Attachment D-1 Script for Informed Consent: Local EMS Provider Survey – Computer Assisted Telephone Interview
Attachment E-1 Follow-up Message to the Request for Interview: Sub-State EMS Region Respondent
Attachment E-2 Informed Consent Script: Sub-State EMS Region Respondent
Attachment F Topic Outline for Semi-Structured Telephone Interview: Sub-State EMS Region Respondent
Attachment G Battelle IRB Review Report. Current Implementation Approval – Entire Project
B. COLLECTION OF INFORMATION EMPLOYING STATISTICAL METHODS
Statistical methods were not used to select respondents for any of the data collection used in this study. The 9-1-1 (pre-hospital) Emergency Medical Services (EMS) units to be studied were purposely selected. The unit of analysis is the organization being studied. These are Local EMS Provider organizations and Sub-State EMS Region administrative organizations. The following section describes respondent selection and data collection procedures.
B.1 Respondent Universe and Sampling Methods
Local EMS Provider Survey: Computer Assisted Telephone Interview (CATI)
All fifty states have some type of state-level pre-hospital EMS regulatory body. The original design proposed for the study included a survey of a national sample of 1,200 EMS organizations (out of an estimated 25,000 to 30,000) and a mail survey of all 50 state EMS agencies. However, after in-depth examination of EMS issues from major reports and discussions with experts early in the study the research team feels it is important to acknowledge the considerable variability from state to state in the organizational configuration and scope of capabilities of local level EMS provider organizations as well as the uncertainty about the extent of within-state variability. This variability appears to be primarily due to local jurisdictional responsibility for funding and staffing of the EMS provider organizations, in lieu of national EMS system standards.
Several experts consulted noted that the dearth of systematic information about pre-hospital EMS provider organizations (many typically referred to as ambulance companies) lies in the difficulty in stratifying and sampling from a universe of such diverse organizations. The research team decided that the study needed to be more basic than initially proposed. Rather than sampling from all local EMS organizations in the United States, the study intends to document the configuration of selected capabilities of every pre-hospital EMS organization in each of nine states. First, the survey will provide comprehensive data about the scope of practice for pre-hospital EMS care for heart attack and stroke victims for the selected states. Secondly, the study as designed will provide a strong basis for sampling design in future studies, and a rich evidence base for determining aspects of pre-hospital EMS on which to focus for future assessments of pre-hospital EMS. This is important because CDC Division for Heart Disease and Stroke Prevention (DHDSP) serves on the newly reauthorized Federal Interagency Committee on Emergency Medical Services (FICEMS) Technical Working Group tasked to design a national EMS assessment strategy by the end of 2008.
The data from the local EMS provider telephone survey will provide a profile of the intra-state variation of local EMS provider services and practices in the nine states. This information will be matched with qualitative state-level contextual information for each of the survey states. For this project, the design will yield a data set to provide: a detailed look at the array of organizational configurations for EMS provider organizations useful for sampling design in future research; an exploratory examination of relationships among state regulatory and medical direction policy, the influence of the activities of EMS regions (in those states where they have been designated), and EMS provider scope of practice; and, an examination of the relationships between provider organization capacity, scope of practice, and the use of specific skills and medications for pre-hospital EMS care for symptoms of chest pain and stroke.
Local EMS Provider data is to be collected by the use of a computer assisted telephone interview (CATI) with every local EMS provider organizations in each of nine purposively selected states. An initial set of states was chosen for the study, based on the objectives of achieving regional representation for the U.S. and variation in rural/urban population distribution. This list was adjusted by examining chronic disease rates in each of those states to ensure some variation in state rates for heart disease and stroke. For the final selection of states, one that turned out to have almost 1000 EMS provider organizations was replaced with another less prolific in this aspect. This decision takes into account the likelihood that states with very high numbers of EMS provider organizations—some states have over a 1,000--would have a high proportion that were very similar with respect to staffing (very small staff and mainly volunteer), thereby greatly reducing the variance on those variables. The study objectives are focused on describing and comparing variations in organizational configurations and practices in different state contexts.
The study design does not support strict generalization of the findings to all states. However, the data set will permit verification of the type of variability in organizational configurations and whether it exists to the essentially anecdotal degree described by EMS practitioners and stakeholders. Also, collecting data from all local EMS provider organizations in the selected states will permit a test of the feasibility and utility of overlaying the geographical distribution of attributes of a state’s EMS provider systems with already existing CDC-developed maps of morbidity for heart disease and stroke for each state and by race and ethnic group8 or with other geo-coded information. This is particularly useful to the CDC’s Division for Heart Disease and Stroke Prevention.
The Local EMS Provider organization list will include only ground-based EMS provider organizations licensed (or the equivalent) in the nine states selected purposively to represent different parts of the country, variation in urban and rural population distribution, and variation in rates of heart disease and stroke. The number 2,250 is based on budget boundaries. For the states selected for the survey, an estimate of the number of respondents (i.e., local EMS provider organizations) in each state selected is provided in Table B.1-1. The response rate for the Local EMS Provider Survey is expected to be approximately 80% in each state.
Table: B.1-1. Approximate Number* of Ground-Based EMS Provider Units
|
AR |
FL |
KS |
MA |
MT |
NM |
OR |
WI |
SC |
Total (approx) |
1. Local Provider Units* |
195 |
270 |
170 |
300 |
260 |
290 |
130 |
420 |
215 |
2,250 |
*These numbers are based on state lists of EMS providers found on state EMS websites but are approximate because the number of licensed units changes over time. Also, state lists may contain service units that don’t meet the criteria for being included in the study (i.e., air transport; facility-to facility transport only). If the most current list of licensed organizations does not indicate the type of service unit, this information will be obtained during the screening questions asked of the respondent and the interview ended if the service unit is not eligible.
Semi-Structured Telephone Interviews with Sub-State EMS Region Administrators
Five of the nine states selected for the study have grouped counties into sub-state EMS regions, with the number of regions in these states varying from three to six. Semi-structured interviews conducted by a social scientist using a topic guide (see Attachment F) will be done for the purpose of exploring the functions of the regions and their influence on state or local initiatives for the improvement of local pre-hospital EMS practices and coverage. These interviews will be conducted by telephone. Little mention was found in the literature of the function of sub-state EMS regions. The interview is designed to be relatively exploratory in nature. A general topic guide is being used in order to avoid missing variation in the sub-state EMS regions across the five states, which could occur through the use of specific questions based on erroneous assumptions about the function of the EMS regions in different states. The interviewer will make a telephone call to set a date and time for an interview with the person who is responsible for the EMS region activities, such as an administrator or executive director. Two EMS regions in each of the five states will be selected for a sample of 10 -- the region with the highest average population density across the counties in the region and the region with the lowest average population density across the counties in the region. This will ensure that one of the interviews will be with an EMS region where challenges to urban EMS delivery and one with challenges to EMS in a highly rural or frontier part of the state.
B.2 Procedures for the Collection of Information
Local EMS Provider Survey: Computer Assisted Telephone Interview (CATI)
The Local EMS Provider Survey in the nine states will be conducted using the method of computer-assisted telephone interviews (CATI). The telephone interviewer reads from a computer display programmed to show each question and its response categories or metric. The computerized survey instrument is programmed to minimize errors as the interviewer enters the responses; for example, the programming will automatically execute “skip” instructions as appropriate to particular responses, or provide an alert if the interviewer enters an “out-of-range” response. The cumulative data set is built as the responses are entered by the interviewers, thereby eliminating a second manipulation of the responses for purposes of data entry which could introduce error.
The lists of all EMS provider organizations obtained from each state will be incorporated into a database for tracking the status of the interview for each respondent organization (e.g., call; call back at specific time; call back to complete; completed; refused). Each interviewer works from a segment of the status tracking list in order to maintain progress on the survey consistent with respondent’s time zone or timing request. The organizations to be interviewed will not receive advance notice of the interview from the research team. The telephone interviewer will use a script (Attachment C) for the purpose of identifying and contacting the appropriate respondent (EMS operations supervisor) once a local EMS organization is reached by telephone. When the appropriate respondent is available, the interviewer will read the Script for Informed Consent for the interview (Attachment D-1) and if the respondent agrees, will move on to the questions (Attachment D). If the respondent gets interrupted to participate on an emergency run, the interviewer will suspend the interview at that point and call back at a later time to cover the remaining questions.
The survey, using CATI, will be conducted by the study contractor’s in-house Survey Operations Center (SOC). The SOC provides the capability for the data to be collected by experienced telephone interviewers who have participated in a wide variety of studies for many different sponsors. The SOC Director will assign a Study Director who will coordinate all aspects of the survey including formatting of the survey instrument, oversight of the CATI programming, training of interviewers on the content and terminology of the survey instrument, and quality assurance for the data set. The Study Director will assign a Survey Manager who will supervise the day-to-day work of the telephone interviewers, including assigning shift supervisors for off-hours interviewing, to ensure consistent use of the survey instrument and provide assistance and quality assurance for the telephone interviewers. The Project Manager will assist with the substantive aspects of the training for the interviewers. The SOC Study Director will provide up to eight hours of training to the telephone interviewers, as appropriate, and any refresher training as needed. The training materials then serve as a handbook available to the telephone interviewers, shift Survey Manager, and SOC Study Director during the hours the survey is being conducted.
Semi-Structured Telephone Interviews with Sub-State EMS Region Administrators
The semi-structured interviews with ten EMS region administrators/directors will be conducted by a Ph.D.-level social scientist. For each EMS region to be included, contact information exists on the web site for the region, or if not, can be obtained from the State Regulatory EMS Director. The interviewer will contact the EMS region, request an interview with the administrator (or equivalent), schedule a time for the 45-minute interview, and send a follow-up e-mail message (Attachment E-1) as a written reminder of the interview date and time. The script for informed consent (Attachment E-2) will be sent to the respondent in advance, along with the follow-up message about the interview appointment. If the administrator provides the interview, that serves as the indication that the administrator has consented to the interview. The interviewer will conduct the interview using the Topic Guide for the Semi-Structured Interview (Attachment F) and take notes, either by hand or on a computer, during each interview. These interviewers will result in mainly qualitative data from each of the ten interviews.
B.3. Methods to Maximize Response Rates and Deal with Nonresponse
Local EMS Provider Survey: Computer Assisted Telephone Interview (CATI)
For the CATI survey, the response rate will be maximized through the repeated efforts of telephone interviewers to reach each organization on the call list and then to talk directly to the EMS operations supervisor or equivalent for that organization, to obtain his or her agreement to answer the interview questions. As emergency response organizations, the local EMS provider organizations typically are staffed and operate 24 hours a day, seven days a week. Notification for an emergency run comes from an emergency dispatch unit such as a community or agency 9-1-1 call dispatch center, so EMS organizations also have a non-emergency business phone number. This non-emergency number most likely is answered 24 hours a day in all but the smallest voluntary EMS organizations, but the interviewer will make the initial call during day-shift hours (by time zone). If the person answering the initial phone call is the appropriate person for the interview, the interview will be conducted at that time or an appointment time will be established for a call-back. If the initial contact person is not the appropriate person for the telephone interview, a time will be established for a call-back to reach the identified individual. If the organization’s contact prefers to have the appropriate person call back at his or her convenience, the interviewer can provide an 800 number to reach the Survey Operations Center. Calls to the 800 number for this survey are then relayed to one of the interviewers working on this EMS survey. Respondents who ask to talk to the Project Manager will be provided her phone number.
The achievable response rate is estimated to be 80% of all the provider organizations on the official list obtained from the state EMS web-site or contact person and that were reached at least once by telephone. This anticipated response rate is based on the expectation that most EMS organizations have someone available at all times to respond to the emergency calls and will generally also have someone available to answer the non-emergency telephone. We expect that the preferred respondent, unless called to an emergency, will consider 15 minutes an acceptable amount of time to spend with the interviewer since much of an EMT’s time is spent waiting to be called out to provide emergency service. The pre-test of the survey, albeit limited in size (n=8), indicated that once the appropriate contact person is reached, that person is likely to prefer to conduct the interview immediately, rather than at a later time, because of the unpredictability of the next emergency call-out. If the respondent must suspend the interview to go on an emergency run, the interviewer will call at a later time to complete the interview.
A few reports were found describing one-time mail surveys with EMS organizations, for which the response rates were generally less than 50%. This is not unusual for self-administered mail questionnaires, unless aggressive and repeated efforts are made or incentives provided to turn non-respondents into respondents. For this reason, the telephone survey has been selected as likely to be the most successful in obtaining a high response rate because of the capacity for making numerous call-backs and for making a personal request for the interview directly to the person with the information. One potential challenge that may be encountered in the larger, urban EMS organizations is that an administrative person who makes decisions about access to the operations supervisor acts as a gatekeeper. The trained telephone interviewers have experience and training to provide information designed to reassure the initial contact about the nature of the phone call and the purpose of the interview.
When a phone number provided for the organization has not been answered within three attempts at different times of the day, it will be considered “inoperable” and removed from the total count of organizations. The SOC Study Director will make an effort to obtain a functional alternative phone number for the named organization through telephone directory information or the state EMS licensing records and if successful, the organization will be included in the total count of organizations. Once the interviewer has made an initial telephone contact with the EMS organization, up to four attempts will be made to reach the person identified as the appropriate person to interview. If not successful, the organization will be categorized as a “Non-Respondent” organization.
Two types of failures to complete an interview with an organization on the official list of EMS organizations constitute a “non-response.” One type is the true refusal of the preferred respondent to complete the interview. The other type of non-response is when the preferred respondent has been identified but contact cannot be made with him or her within four attempts. This would include the situation where a gatekeeper has refused to provide access to the appropriate respondent. The total number of organizations on the official list, less those for which one of these failures was experienced, is the basis for the calculation of a response rate.
Semi-Structured Telephone Interviews with Sub-State EMS Region Administrators
Ten interviews, two for each of five states, will be requested with the most urban and most rural EMS regions in each state identified for the interview. The states in the study with sub-state EMS regions are Kansas, Massachusetts, Montana, New Mexico, and South Carolina. The interview will be done with the person who is responsible for the official activities of the EMS region, such as an Administrator or Executive Director. A 100% response rate is anticipated. The researchers’ experience with interviews with officials with a public service role is that refusals are rare, as long as the time window for scheduling is adequate in length to provide the respondent with many optional dates and times. If for some reason a sub-state EMS region is not staffed at the time of the interview, an alternate region will be selected that has the next highest population density or the next to lowest population density, depending on the region to be replaced.
B.4. Test of Procedures or Methods to be Undertaken
Local EMS Provider Survey: Computer Assisted Telephone Interview (CATI)
A pre-test of a draft version of the telephone survey instrument for the EMS provider organizations was conducted, including the script for identifying the appropriate respondent and for verbal consent. Eight EMS provider organization supervisors were contacted by phone, with four from each of two states (TN and AZ) not included among the states selected for the study. They were selected from the official list of licensed EMS provider organizations on each state’s EMS agency web site. The respondents were informed that the interview was for the purpose of pre-testing the interview questions. A paper copy of the instrument was used by the interviewer, because the programming for the CATI version is not done until the instrument is finalized. Using a cognitive interview approach, the pre-test interviewer went through each question on the draft survey instrument, and respondents were encouraged to indicate when they wanted further clarification of a question or had suggestions for changes in response categories or specific terms. Because of these pretest conversations, most interviews took longer than 15 but less than 30 minutes to complete. Two respondents who made only a few comments completed the interview in approximately 15 minutes. As a result of the pretest, the wording of several questions was modified in an effort to make them clearer for the respondents. Further consultation was sought on some of the items with other subject matter experts, in order to arrive at a question better suited to capture certain concepts. In addition, changes were made to response categories for a few questions. An emergency medicine physician active on several national-level committees working on EMS issues was asked to review the lists of specific therapies used by EMTs and paramedics to further clarify response categories for the segment of the instrument that asks about use of specific interventions. He concurred with most of the items and revised others to make them more generic, since EMS organizations might use a variety of terms or brand-names for equipment and procedures.
Semi-Structured Telephone Interviews with Sub-State EMS Region Administrators
No testing has been done of the semi-structured interview approach or of the Topic Guide for the interviews with Administrators of Sub-state EMS regions. The Topic Guide is designed to allow for flexibility to adjust a topic if necessary, to be more consistent with the actual function and activities of the EMS region. One of two researchers will be making the first contact, arranging the interview time, and conducting the telephone interview. Both researchers are Ph.D-level social scientists with extensive experience in many types of interviews, including semi-structured interviews, and with taking notes during an interview.
B.5. Individuals Consulted on Statistical Aspects and Individuals collecting and/or Analyzing Data
CDC personnel responsible for selecting the contractor and for receiving and approving contract deliverables are;
G. Ishmael Williams, MA. (Technical Monitor)
Division of Heart Disease and Stroke Prevention, NCCDPHP, CDC
770-488-8060
Michele Casper, Ph.D. (Principal Investigator)
Division of Heart Disease and Stroke Prevention, NCCDPHP, CDC
770-488-2571;
The contractor selected to collect and do preliminary analysis of the data is the
Battelle Centers for Public Health Research and Evaluation. Research personnel responsible for design, data collection, and analysis are as follows:
(1) Data collection design: Led by Patricia Bolton, Ph.D.
(2) Data Collection: Battelle Survey Operations Center, overseen by Davis Patterson, Ph.D.
(3) Data Analysis: Led by Davis Patterson, Ph.D.
Contractor Contact Information:
Patricia Bolton, Ph.D., Project Manager, (206) 528-3310; [email protected]
Davis Patterson, Ph.D., Deputy Project Manager, (206) 528-3029, [email protected]
1 Committee on the Future of Emergency Care in the United States Health System. Board on Health Care Services and Institute of Medicine. 2006. Hospital-Based Emergency Care: At the Breaking Point, and Emergency Medical Services: At the Crossroads. Washington DC: National Academies Press.
2 U.S. Department of Transportation, Reauthorization Legislation (P.L. 109-59). 2007. Safe, Accountable, Flexible, Efficient Transportation Equity Act: A Legacy for Users (SAFETEA-LU).
3 Measuring Rurality: Rural-Urban Commuting Area Codes, Economic Research Service, U.S. Department of Agriculture, 2005. http://www.ers.usda.gov/briefing/Rurality/RuralUrbanCommutingAreas/
4 WWAMI Rural Health Research Center. 2005. http://www.fammed.washington.edu/wwamirhrc/rucas/modifier.html
5 Williams, DM, Fitch and Associates, “2006 JEMS Salary and Workplace Survey,” pp. 38-49 in JEMS, Journal of Emergency Medical Services, Vol. 31 (10) October 2006, Figure 7: Salary by Region.. .
6 In Table A-12.1, Estimated Burden in Hours, the calculated burden hours of 7.5 for the sub-state EMS region respondents were rounded to 8 hours, which is the average burden per response used for Table A-12.2.
7 PayScale, Inc., “Salary Survey Report for Job: Executive Director, Non-Profit Organization,” November 2007, accessed at: www.payscale.com/research/US/job=Executive_Director%2c_Non-Profit_Organization/Salary/by_Employer_Type
8 Examples of mortality mapping by disease and race and ethnic group prepared for this Division of CDC, NCCDPHP are: Atlas of Stroke Mortality: Racial, Ethnic, and Geographic Disparities in the United States, 2003; and, Atlases of Racial and Ethnic Disparities in Mortality, for Men and for Women. These can be viewed on-line at www.cdc.gov/cvh/maps .
Page -
| File Type | application/msword |
| File Title | Application for OMB Clearance |
| Author | Battelle |
| Last Modified By | cww6 |
| File Modified | 2008-01-09 |
| File Created | 2007-12-31 |
© 2026 OMB.report | Privacy Policy