CMS-10310.Mockup 4_Imaging Measures_REV_1_15
CMS-10310.Mockup 4_Imaging Measures_REV_1_15.doc
Consumer Research on Public Reporting of Hospital Outpatient Measures (CMS-10310)
CMS-10310.Mockup 4_Imaging Measures_REV_1_15
OMB: 0938-1081
Imaging Measures - Tables, Graphs and Explanatory Text
Your Selected Hospitals |
EDGEFIELD HOSPITAL |
MITCHELL HOSPITAL
|
RIVER VIEW HOSPITAL |
|
Appropriate Use of Medical Imaging (tests like Mammograms, MRIs, and CT scans) These measures tell how well hospitals are following standards for the safe and appropriate use of medical imaging tests for outpatients. These standards are based on medical research and include things such as:
The information shown here is limited to medical imaging facilities that are part of a hospital or associated with a hospital. These facilities can be inside or near the hospital, or in a different location. This information only includes medical imaging done on outpatients. Medical imaging tests done for patients who have been admitted to the hospital as inpatients aren’t included. |
||||
Your Selected Hospitals |
EDGEFIELD HOSPITAL |
MITCHELL HOSPITAL
|
RIVER VIEW HOSPITAL |
|
T |
||||
|
Select All |
|||
|
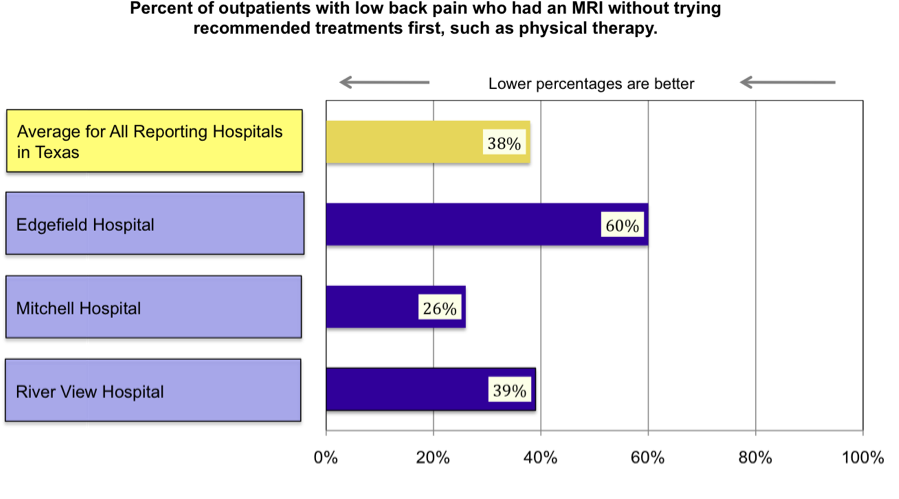
Percent of outpatients with low back pain who had an MRI without trying recommended treatments first, such as physical therapy. (If a percent is high, it may mean the facility is doing too many unnecessary MRIs for low back pain.) |
60% |
26% |
39% |
|
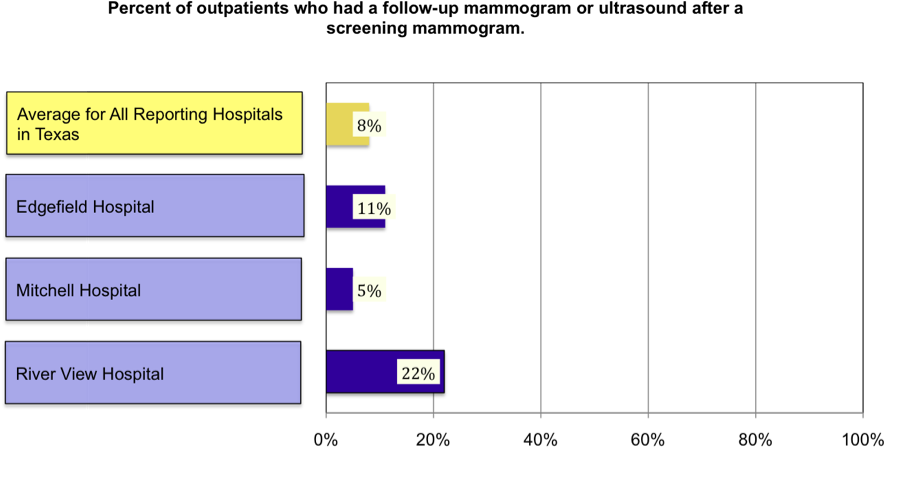
Percent of outpatients who had a follow-up mammogram or ultrasound after a screening mammogram. (A percent close to 0% may mean there’s not enough follow-up. A percent much higher than 14% may mean there’s too much unnecessary follow-up.) |
11% |
5% |
22% |
|
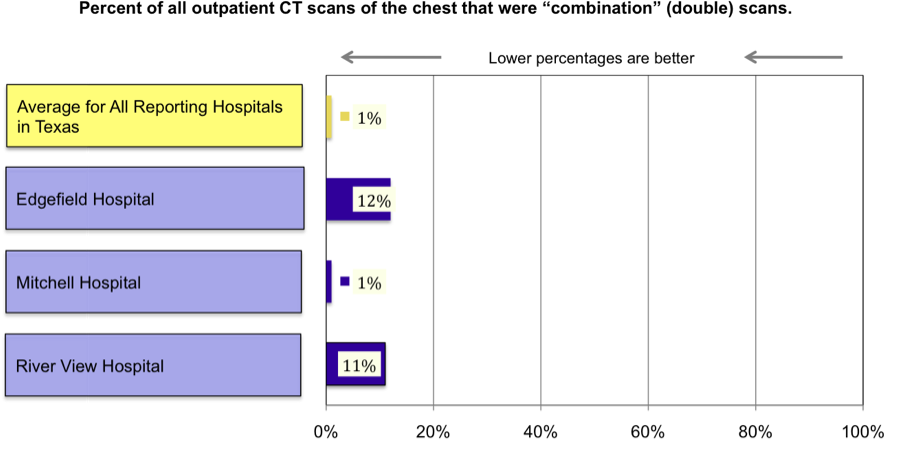
Percent of all outpatient CT scans of the chest that were “combination” (double) scans. (If a percent is very high, it may mean that too many patients are being given a double scan when a single scan is all they need.) |
12% |
1% |
11% |
|
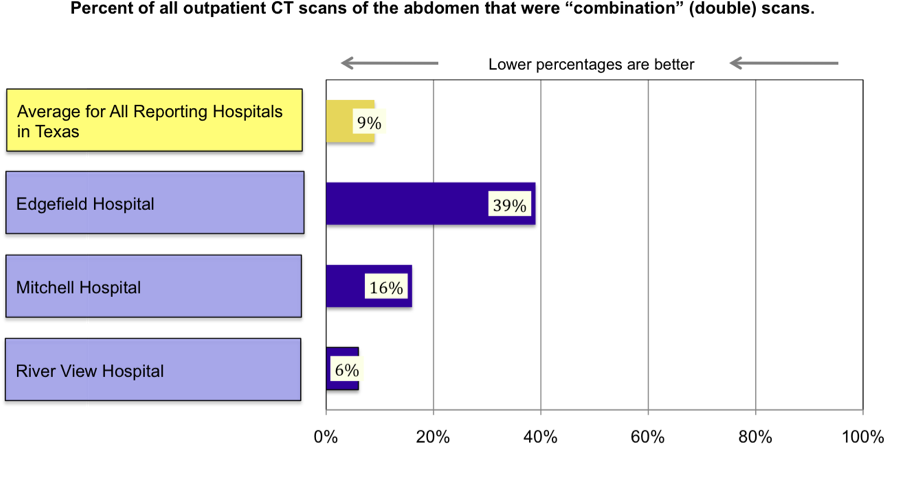
Percent of all outpatient CT scans of the abdomen that were “combination” (double) scans. (If a percent is very high, it may mean that too many patients are being given a double scan when a single scan is all they need.) |
39% |
16% |
6% |
|
Select All |
Appropriate Use of Medical Imaging (tests like Mammograms, MRIs, and CT scans)
Measures based on standards of care |
Compare the hospitals to this: |
EDGEFIELD HOSPITAL |
MITCHELL HOSPITAL |
RIVER VIEW HOSPITAL |
TEXAS AVERAGE |
||||
Percent of outpatients with low back pain who had an MRI without trying recommended treatments first, such as physical therapy. (If a percent is high, it may mean the facility is doing too many unnecessary MRIs for low back pain.) |
38% |
60% of 25 patients |
26% of 570 patients |
39% of 309 patients |
Percent of outpatients who had a follow-up mammogram or ultrasound after a screening mammogram. (A percent close to 0% may mean there’s not enough follow-up. A percent much higher than 14% may mean there’s too much unnecessary follow-up.) |
8% |
11% of 136 patients |
5% of 3126 patients |
22% of 4365 patients |
Percent of all outpatient CT scans of the chest that were “combination” (double) scans. (If a percent is very high, it may mean that too many patients are being given a double scan when a single scan is all they need.) |
1% |
12% of 37 CT scans |
1% of 976 CT scans |
11% of 678 CT scans |
Percent of all outpatient CT scans of the abdomen that were “combination” (a double) scans. (If a percent is very high, it may mean that too many patients are being given a double scan when a single scan is all they need.) |
9% |
39% of 70 CT scans |
16% of 1145 CT scans |
6% of 1442 CT scans |
Percent of outpatients with low back pain who had an MRI without trying recommended treatments first, such as physical therapy.
What does this measure tell you about appropriate use of MRIs for low back pain?
Although MRIs can be helpful for diagnosing low back pain, MRIs can be used too much.
Usually, low back pain improves or goes away within six weeks and an MRI is not needed.
Standards for care say that most patients with low back pain should start with treatment such as physical therapy or chiropractic care, and have an MRI only if the treatment doesn’t help.
Finding out whether treatment helps before having an MRI is better and safer for most patients because it avoids the stress, risk, and cost of doing MRIs that patients don’t need.
If a percent is high, it may mean that the facility is doing many MRIs for low back pain that are not necessary. (For some patients with certain conditions, getting an MRI right away is appropriate care. Patients with these conditions are not included in this measure.)
If you have low back pain, you, your doctor, and the medical imaging facility should all talk about the best time to do an MRI if you need one.
The rates in this graph are from data reported for outpatient medical imaging services from January 2008 through December 2008.
What is an MRI?
An MRI (magnetic resonance imaging) is a test that uses a powerful magnetic field and a computer to produce detailed pictures of the inside of the body (bones, organs, and other body parts).
What are the risks of having an MRI?
Since MRIs use magnets rather than x-rays, there is no radiation risk. However, because the magnets attract some kinds of metal, it’s important for the technician to know if there are any metal objects or implants inside the patient’s body, such as pacemakers, artificial joints, screws, stents, plates, or staples. Metal objects can pose serious risk to the patient and interfere with the test.
For some MRIs, a substance called “contrast” is injected before the test to make parts of the body stand out more clearly on the images. Risks of contrast include possible harm to the kidneys or allergic reactions. Contrast shouldn’t be used if it isn’t needed.
Having the test can be stressful to some people. Patients must hold still for about 15 to 45 minutes while lying on a table that moves inside a large scanning machine. While images are being taken, the machine makes loud noises.
Percent of outpatients who had a follow-up mammogram or ultrasound after a screening mammogram.
What does this measure tell you about appropriate follow-up for screening mammograms?
When a screening mammogram shows signs of possible breast cancer, the patient is asked to come back for a follow-up appointment. A follow-up means having more tests (mammograms, an ultrasound, or both.
Medical research shows that there may be a problem if a facility has either a very low percent or a very high percent of follow-up:
A percent that is very low (close to 0%) may mean there's not enough follow-up and possible signs of cancer are being missed.
A percent that is very high (much higher than 14%) may mean the facility is doing too much follow-up that’s not needed.
Reasons could include poor technique (blurry X-rays that need to be repeated) or a lack of skill or experience interpreting the screening mammograms.
Whatever the reason, unnecessary follow-up is stressful to patients and results in needless exposure to radiation. (There is no radiation exposure for ultrasounds because they don’t use x-rays.)
If you are going to have a screening mammogram, talk with your doctor about the results below and what a facility’s results mean for you and your care.
The rates in this graph are from data reported for outpatient medical imaging services from January 2008 through December 2008.
What is a “screening” mammogram?
A screening mammogram is an x-ray of the breast to check for possible breast cancer.
Percent of all outpatient CT scans of the chest that were “combination” (double) scans
What is a “combination” CT scan?
For some CT scans, a substance called “contrast” is put into the patient’s body before the scan begins, to help make parts of the body stand out more clearly on the x-rays. Contrast can be either swallowed or injected into a vein.
A “combination” CT scan means that the patient gets two CT scans – one scan without contrast followed by a second scan with contrast.
What does this measure tell you about appropriate use of CT scans of the chest?
Standards for quality care say that most patients who are getting a CT scan of the chest should be given a single CT scan rather than a “combination” CT scan. (Although a combination CT scan is appropriate for some parts of the body and some medical conditions, a combination scan is usually not appropriate for the chest.)
Depending on the patient’s medical condition, using contrast for the single scan might or might not be appropriate.
For this measure, if a percent is very high, it may mean that the facility is routinely giving patients a combination CT scan of the chest when a single scan is all they need.
Giving patients two scans when they only need one needlessly doubles their exposure to radiation:
Radiation exposure from a single CT scan of the chest is about 350 times higher than for an ordinary chest x-ray.
For a combination CT scan, radiation exposure is 700 times higher than for a chest x-ray because the patient is given two scans.
When contrast is used, there are risks that can include possible harm to the kidneys or allergic reactions (especially if the contrast is injected). To avoid unnecessary risk, contrast should be used only when it is needed. If you need to have a CT scan of the chest, talk with your doctor about what’s best for your medical condition:
Do you need a single scan - either with or without contrast - or is a combination scan necessary?
Is using contrast appropriate for your medical condition?
The information that follows can help you judge how well hospital imaging facilities are following standards for quality care when they do CT scans of the chest. Talk with your doctor about this information and how it applies to you.
The rates in this graph are from data reported for outpatient medical imaging services from January 2008 through December 2008.
Percent of all outpatient CT scans of the abdomen that were “combination” (double) scans
What is a “combination” CT scan?
For some CT scans, a substance called “contrast” is put into the patient’s body before the scan begins, to help make parts of the body stand out more clearly on the x-rays. Contrast can be either swallowed or injected into a vein.
A “combination” CT scan means that the patient gets two CT scans – one scan without contrast followed by a second scan with contrast.
What does this measure tell you about appropriate use of CT scans of the abdomen?
Standards for quality care say that most patients who are getting a CT scan of the abdomen should be given a single CT scan rather than a “combination” CT scan. (Although a combination CT scan is appropriate for some parts of the body and some medical conditions, a combination scan is usually not appropriate for the abdomen.)
Depending on the patient’s medical condition, using contrast for the single scan might or might not be appropriate.
For this measure, if a percent is very high, it may mean that the facility is routinely giving patients a combination CT scan of the abdomen when a single scan is all they need.
Giving patients two scans when they only need one needlessly doubles their exposure to radiation:
Radiation exposure from a single CT scan of the abdomen is about 11 times higher than for an ordinary x-ray of the abdomen.
For a combination CT scan, radiation exposure is 22 times higher than for an x-ray of the abdomen because the patient is given two scans.
Risks of injected contrast include possible harm to the kidneys or allergic reactions. Contrast shouldn’t be used if it isn’t needed.
If you need to have a CT scan of the chest, talk to your doctor about what’s best for your medical condition:
Do you need a single scan - either with or without contrast - or is a combination scan necessary?
Is using contrast appropriate for your medical condition?
The information that follows can help you judge how well facilities are following standards for quality care when they do CT scans of the abdomen. Talk to your doctor about this information and how it applies to you.
The rates in this graph are from data reported for outpatient medical imaging services from January 2008 through December 2008.
What is a “CT scan”?
A CT scan (also called a CAT scan) uses multiple x-rays to produce detailed pictures of the inside of the body (bones, organs, and other body parts).
| File Type | application/msword |
| File Title | Your Selected Hospitals |
| Author | Kelly Moriarty |
| Last Modified By | sally crelia |
| File Modified | 2010-01-15 |
| File Created | 2010-01-15 |
© 2026 OMB.report | Privacy Policy
 o
view more information, select the topic(s) below and click “View
Graphs”.
o
view more information, select the topic(s) below and click “View
Graphs”.