Data Collection for the Nursing Home Value-Based Purchasing (NHVBP) Demonstration: ONGOING DATA (CMS-10240)
Data Collection for the Nursing Home Value-Based Purchasing (NHVBP) Demonstration
CMS-10240 pra-attachments
Data Collection for the Nursing Home Value-Based Purchasing (NHVBP) Demonstration: ONGOING DATA (CMS-10240)
OMB: 0938-1039
ATTACHMENTS
Nursing Home Application
NHVBP Survey Electronic Payroll Data Submission Guidelines
NHVBP Data Collection Form
Federal Register Notice
Statistical Methods
Attachment 1
Nursing Home Application
MEDICARE NURSING HOME VALUE-BASED PURCHASING DEMONSTRATION APPLICATION
Applicant Legal Name |
|
Date Submitted |
|
Address |
|
Date Received by CMS |
|
City |
County |
|
State ZIP Code |
Name, telephone number, address, fax number (if available) and email address (if available) of person to be contacted on matters involving the application: |
|||
Project Description: Nursing Homes that apply for the NHVBP demonstration must submit data according to the attached data collection protocol. Applicants will be assigned to either the demonstration group, the control group, or neither group. Nursing homes that are selected for the demonstration must agree to submit the data per the protocol and to participate in the 3-year demonstration in order to be eligible for awards under the demonstration. The submitted data will be included in the determination of each nursing home’s performance score. Nursing homes with superior performance or improvement will be eligible for an annual performance payment award. |
|||
Are 50 percent or more of applicant’s residents Medicare eligible? Yes No
Does the applicant use an electronic health record (EHR) that captures, maintains, and manages patient health information? Yes No
If applicant is part of a multi-facility organization, please specify chain name_____________________
Areas Affected by Project (city/county and state):
Applicant’s Medicare Provider Number(s) Applicant’s Employer Identification Number
Is The Applicant a Medicare Provider/Organization in Good Standing?
Yes No (If No, attach an explanation)
To the best of my knowledge and belief, all data in this application are true and correct, the document has been duly authorized by the governing body of the applicant and the applicant will comply with the terms and conditions of the award and applicable Federal requirements if awarded.
Write or Type Name and Title of Authorized Representative Telephone Number (include area code)
S ignature
of Authorized Representative Date Signed (mm/dd/yyyy)
ignature
of Authorized Representative Date Signed (mm/dd/yyyy)
Disclosure Statement According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is 0938-NEW. The time required to complete this information collection is estimated to average 15 minutes, including the time to review instructions, search existing data sources, gather the data needed, and complete and review the information collection. If you have any comments concerning the accuracy of the time estimates or suggestions for improving the form, please write to: CMS, 7500 Security Boulevard, Attn: PRA Reports Clearance Officer, Mail Stop C4-26-05, Baltimore, Maryland 21244-1850.
Attachment 2
NHVBP Survey Electronic Payroll Submission Guidelines
Submission of Payroll Data from Nursing Homes
This document outlines the specifications for payroll information to be electronically submitted by participants in the CMS Nursing Home Value Based Purchasing Demonstration.
Each quarterly electronic data submission will consist of an Excel or ASCII text file in three parts: a header record, a series of data records, and a trailer record. The header record will contain identification and contact information for your facility. The data records will consist of one record for each employee, and will include information on job category and hours worked in each pay period during the previous quarter. The trailer record will indicate the total number of data records to be submitted. The remainder of this document describes the information to be included in each data record in greater detail, including a sample data record for your guidance.
DATA ELEMENTS
One data record should be submitted electronically for each employee who worked at your facility in the previous quarter. The following four pieces of employee information should be included in columns in each data record: employee number or other unique identifier, pay period end date, employee job category, and number of hours worked. Each of these four data elements is described in greater detail below.
Medicare provider number (PROV_ID)
This a six-digit number where the first two digits identify the state (e.g., Colorado is 06) and the 3rd-6th digits uniquely identify the facility and range from 5000 to 6399 (the 3rd digit can be a U, W, Y, or Z, if the facility is a swing-bed unit in a hospital).
Facility name (FAC_NAME)
Employee number or other unique identifier (EMPLOYEE_ID)
A unique employee identifier must be submitted with each payroll record. The unique employee identification should not contain identifying information such as employee names or social security numbers. The same unique Employee ID must be used for an employee’s tenure within a nursing home. If the employee leaves the nursing home and returns to its employ at a later point in time the facility may choose to retain the original employee ID or assign a new employee ID. A new employee ID should not be assigned when an employee is promoted within a nursing home facility.
Employee Start Date (EMP_START_DATE)
The Employee Start Date is the date the employee began their employment at the nursing home. If the employee has left the nursing home for a period of time and returned as an employee the date provided should be the most recent start date.
Pay Period Start Date (PAYROLL_START_DATE)
The Pay Period Start Date is the first day of the pay period being reported. The date cannot overlap with prior pay periods submitted for the same employee working at the same nursing home.
Pay Period End Date (PAYROLL_END_DATE)
The Pay Period End Date is the last day of the pay period being reported. The date cannot overlap with prior pay periods submitted for the same employee working at the same nursing home. The pay period length (number of days between pay period start and end dates) cannot exceed 15 days and must be equal to a 7-day, 14-day, or a bi-monthly (15-day) pay period.
Employee job category (JOB_CAT)
The data specification requires nursing home facilities to classify nursing staff into one of the four job categories described below. Staff should be assigned to the appropriate job category based on their job title on the first day of the pay period being reported.
Registered Nurse – Those persons licensed to practice as registered nurses in the State where the facility is located. This category includes RN/ADONs whose primary1 responsibilities involve direct patient care2.
Licensed Practical/Vocational Nurse – Those persons licensed to practice as licensed practical/vocational nurses in the State where the facility is located. This category includes LPNs/ADONs whose primary responsibilities involve direct patient care.
Certified Nurse Aide – Individuals who have completed a State approved training and competency evaluation program, or competency evaluation program approved by the State, or have been determined competent as provided in 483.150(a) and (3) and who are providing nursing or nursing-related services to residents. This category includes State certified Medication Aides and Restorative Aides. CNAs in training should not be included. If an individual works in two positions (e.g., CNA and housekeeping) all hours for this employee should be reported as CNA hours.
Director of Nursing – Professional registered nurse(s) administratively responsible for managing and supervising nursing services within the facility.
Number of hours worked (PROD_HOURS)
Number of hours worked includes the total number of hours worked during the pay period at the nursing home for the employee identified in the record. This number cannot include hours for vacation leave, sick leave, corrections to reconcile errors from previous pay periods, etc. This number does reflect hours worked in both direct and non-direct patient care. If an employee covers a shift at a facility within a nursing home corporation, the hours worked should be assigned to the respective facility and not allocated to a “home” or “primary” facility. If no productive hours were worked during a pay period the data element should be submitted with zero hours.
Nonproductive Hours (NON_PROD_HOURS)
Nonproductive Hours includes the total number of hours paid during the pay period for leave (sick, vacation, administrative), bonuses, employee payouts, etc. If no nonproductive hours were paid during the pay period the data element should be submitted with zero hours.
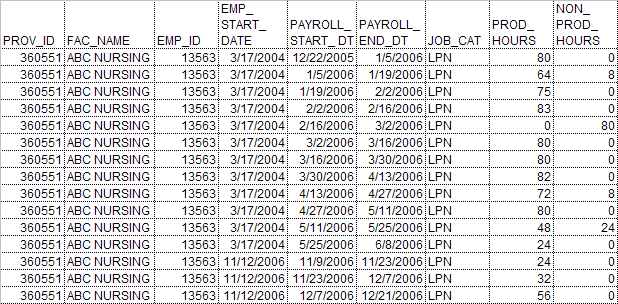
SAMPLE DATA RECORD
The following illustration shows a single data record for an individual employee at a facility with bi-weekly pay periods. This employee worked at this facility for two separate periods in 2006, January through early June, and mid-November through December.
This individual was employed as a Licensed Practical Nurse throughout their employment at the facility. If they had changed jobs, this should be reflected in the JOB_CAT filled.
This employee missed work due to vacation and sick days at several points during the year. The hours that the employee was paid for this time are recorded in the non-productive hours field (NON_PROD_HOURS), but not the productive hours (PROD_HOURS) field. Compare this to the period between early June and mid-November, during which this individual was not employed at the facility, and the pay periods were therefore not included in the data record.
In this example, the employee identification number was not re-assigned upon the employee’s return to the facility but their start date was reassigned; note that assigning a new employee identification and creating a separate data record for the employee’s second stint at the facility would also have been acceptable.
Attachment 3
NHVBP Data Collection Form
NHVBP Data Collection Form
General Instructions and Definitions
Section A: General Information
Name of Facility: Use the official name of the facility for business and mailing purposes.
Medicare Provider Number: Enter the facility’s assigned six-digit provider code.
Street Address: Street address refers to the physical location, not mailing address, if the two addresses differ.
City: The city in which the facility is located. Rural facilities should include the city of the nearest post office.
State: The state in which the facility is located.
Zip Code: The zip code of the facility. If available, report the “zip-plus-four” code.
Telephone Number: The main business phone number of the facility. Include the area code.
Section
B: Resident Census
Total Resident Days: The number of days that all patients spent in the facility by payor during the reporting period as counted at the census taking time each day. Patient days include the day of admission, but not the day of discharge.
Definitions of the payor categories follow:
Medicare - Enter the number of resident days for which Medicare was the primary payor.
Medicaid Dual Eligible - Enter the number of resident days for Medicare-eligible beneficiaries for which Medicaid was the primary payor.
Medicaid Only - Enter the number of resident days for non Medicare-eligible beneficiaries for which Medicaid was the primary payor.
Other Payers - Enter the number of resident days for which neither Medicare nor Medicaid was the primary payor.
Section C: Nursing Temporary Agency Staff
Staff Type:
Director of Nursing - Includes DON and Assistant Director of Nursing.
Registered Nurses - Includes Registered Nurses (RNs) employed in the performance of direct nursing care to patients. Includes geriatric nurse practitioners and clinical nurse specialists who primarily perform nursing-related tasks. (RNs functioning as supervisors should not be reported here.)
Licensed Nurses - Includes Licensed Vocational Nurses (LVNs) or Licensed Practical Nurses (LPNs) employed in the performance of direct nursing care to patients.
Nurse Aides - This classification includes non-technical personnel employed in the performance of direct nursing care to patients. Examples of job titles include Nurse Assistant, Certified Nurse Assistant/Aide (CNA), Orderly, and Medication Technicians/Assistants. Nurse Aides in training should not be included.
Section D: Staff
Influenza Immunizations
1. Number of Staff Employed - Report the number of staff in all departments employed at the facility as of this point in time. Count full, part-time and per diem (or on-call) staff. Count per diem staff if they worked four or more hours in the last 30 days.
2a. Number of staff immunized - Report the number of staff who received the recommended influenza vaccine for the 2006-2007 influenza season. Report staff who received the vaccine from the facility as well as those who report having received the vaccine from an outside source (clinic/physician).
2b. Number of staff not eligible for immunization - Report the number of staff who were not eligible to receive the vaccination due to contraindications.
2c. Number of staff not immunized - Report the number of staff who were eligible to receive the vaccination but did not receive it during the 2006 – 2007 influenza season.
2d. Insufficient supply - Check if there was an insufficient supply of influenza vaccine.
Section E: Use of
Resident Care Experience Surveys
1. Does your facility conduct any resident care experience survey? The survey must include feedback, for example, on domains such as dining, food quality, staff knowledge and responsiveness, activities, cleanliness and/or communication.
2. Is the survey conducted in-house or by an external vendor? Indicate if the survey is administered and analyzed by facility staff or by an outside vendor. A standardized tool developed by an outside vendor but administered by the facility staff should be reported as conducted by in-house staff.
3. What percentage of total residents were included in the survey sample? Report the number of residents (or families of residents) who were surveyed as a percent of the total resident census. Use the facility census as of the first day the survey was administered.
4. How is the survey information used? (Check all that apply). Check all of the following list that apply:
Informing quality improvement activities
As a measure of quality of care
Identifying strengths and weaknesses
Peer group comparison (i.e., benchmarking)
To identify service-related issues
Linked to financial incentives (e.g., bonuses)
Marketing purposes
Accreditation purposes
Other (please specify)
Attachment 4
Federal Register Notice
Attachment 5
Statistical Methods
STATISTICAL METHODS
Potential Respondent Universe and Sampling
We anticipate that approximately 1,000 nursing homes will apply to be included in the NHVBP Demonstration project. Nursing homes that indicate an interest in participating in the demonstration will be stratified and then randomly assigned to either the intervention or a comparison group. The intervention group is expected to include an average of 50 nursing homes per state in 4 or 5 States (a total of 200 to 250 nursing homes); an equal number of nursing homes will be assigned to the control group. Participation will be voluntary.
Estimation of Response Rates
CMS will require submission of baseline data for all applicants to the NHVBP Demonstration; we therefore anticipate a 100% response rate for nursing homes applying to the demonstration. We anticipate that nursing homes unwilling or unable to submit these data will elect not to apply to the demonstration.
CMS further anticipates that all demonstration group nursing homes will submit the required quarterly data over the course of the demonstration period; otherwise they will not be eligible for an incentive payment. Nursing homes assigned to the control group are not expected to submit data.
1 Primary refers to greater than 50% of time.
2 Involved in direct patient care is defined to mean that an individual is providing direct care to residents or is directly responsible for care provided to residents. Providing direct care means that an individual has responsibility for the residents’ total care or some aspect of the residents’ care. Resident contact is an intrinsic part of direct care. Directly involved in patient care includes, but is not limited to, such activities as assisting with activities of daily living (ADLs), performing gastro-intestinal feeds, giving medications, supervising the care given by CNAs, and performing nursing assessments to admit residents or notify physicians about a change in condition. [Final Rule – 42 CFR Part 483]
| File Type | application/msword |
| File Title | Draft OMB |
| Author | dstrouse |
| Last Modified By | CMS |
| File Modified | 2007-10-01 |
| File Created | 2007-10-01 |
© 2026 OMB.report | Privacy Policy