111208_SupportStatement_SectionB_Barriers
111208_SupportStatement_SectionB_Barriers.docx
Barriers to Occupational Injury Reporting by Workers: A NEISS Telephone Interview Survey
OMB: 0920-0939
Barriers to occupational injury reporting by workers:
A NEISS Telephone Interview Survey
Request for Office of Management and Budget Review and
Approval for Federally Sponsored Data Collection
Section B
Project officer: Larry L. Jackson, Chief, Injury Surveillance Team
National Institute for Occupational Safety and Health
Division of Safety Research
1095 Willowdale Road, MS H1808
Morgantown, WV 26505
Phone: 304-285-5980
Fax: 304-285-5774
E-mail: [email protected]
November 2011
Table of Contents
B.1 Respondent Universe and Sampling Methods 3
B.2 Procedures for the Collection of Information 6
B.2.1 Stratification and Sample Selection 6
B.2.2 Collection of Telephone Interview Data 11
B.3 Methods to Maximize Response Rates and Deal with Nonresponse 12
B.4 Test of Procedures or Methods to be Undertaken 13
B.4.1. Interview Questionnaire. 13
B.5 Individuals Consulted on Statistical Aspects and Individuals Collecting and/or Analyzing Data 15
B.1 Respondent Universe and Sampling Methods
Study Population
Potential participants will be identified by the Consumer Product Safety Commission (CPSC) from the occupational injury supplement to the National Electronic Injury Surveillance System (NEISS-Work) and the NEISS-All Injury program (NEISS-AIP) surveillance databases. The NEISS-Work and the NEISS-AIP, collected by the CPSC, capture people who were treated in the emergency department (ED) for work-related injuries and illnesses and non-work-related injuries, respectively. To participate in this study, subjects:
(1) Must be between 20 and 64 years old;
(2) Must speak English;
(3) Must NOT be employed on a farm or a ranch;
(4) Must NOT be self-employed or an independent contractor or a day laborer;
(5) Must have experienced an acute physical injury (chronic, repetitive motion injuries and illnesses will be excluded);
(6) Must have felt well enough to return work in three days or less from the time of injury; and
(7) Must have been employed during the time period that the injury occurred.
As this is intended, in part, to be a pilot project, we have limited the respondent population to those ages who are most likely to be employed. In addition, because of variations in the age of majority across states and the added complication of obtaining parental or guardian consent for a very small number of cases, respondents are required to be between the ages of 20 and 64. We have also limited the sample population with respect to type of health complaint (injuries only), job type of respondent (e.g., self-employed workers and those who work on a farm or ranch are excluded), and severity of injury in order to ensure that results will be reportable given NIOSH reporting guidelines. NIOSH has three criteria for determining reportability of NEISS-Work data results that are intended to ensure reasonable and reliable data quality and appropriate interpretation and use of these data1:
1. Number of cases treated within the hospital sample must exceed a specified value;
2. The extrapolated national estimates must exceed a specified value; and
3. The coefficient of variation must be less than or equal to 33%.
Potential respondents will be identified from the routine NEISS-Work and NEISS-AIP surveillance case data on an ongoing basis over the period of one year. Selection of cases will be restricted to NEISS-Work hospitals among the small, medium, large, and very large hospital stratum (cases treated in a Children’s Hospital will be excluded). CPSC will pre-screen cases selected from the NEISS-Work and the NEISS-AIP databases so that they likely meet the age, employment, and diagnostic criteria. Additional screening questions for these criteria will be asked during the survey interview.
NEISS-Work and NEISS-AIP
Routinely collected NEISS-Work and NEISS-AIP data are captured from a national stratified probability sample created in 1997 of 67 of the approximately 5,400 rural and urban hospitals in the U.S. and its territories. These 67 hospitals were divided into strata by hospital size, based on the number of ED visits annually. The 1997 NEISS-Work stratified sample consisted of 32 small, 9 medium, 6 large, 15 very large sized, and 5 children’s hospitals. Four small hospitals within the sample have closed since 1997 resulting in 63 reporting hospitals. At each of these hospitals, a coder employed by CPSC abstracts standardized information from the ED record. According to the NEISS coder training manuals, cases should be captured if they are a first visit to that hospital’s ED for (a) an injury, regardless of product involvement and regardless of intent; or (b) an illness causally linked to a civilian work activity. For the purposes of NEISS-AIP, an injury is defined as a medical condition resulting from contact with an external force, including chemicals or poisons, temperature extremes, or self harm, and typically involves a single, instantaneous event (e.g., sprain or fracture).
For NEISS-Work, emergency department records are abstracted regardless of age, type of employer or industry, or employer size. Work-relatedness is determined by the hospital abstractor based on the information provided in the ED chart at the time of treatment. “Work” is defined as performing an activity for pay or other compensation, volunteering for an organized group such as an EMS squad or fire department, or unremunerated work on a family farm or business. Indication or filing of a Workers’ Compensation claim is not required. NEISS-Work guidelines for defining a work-related injury or illness generally follow the Occupational Safety and Health Administration’s (OSHA) requirements for recordable injuries and illnesses (e.g., all incidents resulting in a loss of consciousness and heart attacks that occur at work are included). Commuting to or from work and non-professional sports or recreational-related injuries are normally excluded. However, because emergency responders may respond to urgent situations in personal vehicles, these cases are included. Because emergency responder jobs often have physical fitness requirements, cases involving injury during fitness activities are also included. Common illnesses are not reportable within NEISS-Work unless a causal link to work activities can be established (e.g., TB exposure at work). Routine visits for drug and alcohol screening or treatment are also not reportable within NEISS-Work.
The NEISS-Work data are the property of NIOSH and are used for a variety of projects. They are maintained on password-protected computers and in secure files in locked NIOSH offices. NEISS-AIP records used for this project will be maintained in the same manner. NEISS data will be archived on a secure network drive accessible only by those persons who have completed required annual confidentiality training. The archived NEISS files will be maintained for a minimum of 20 years after the study is completed or becomes inactive in accordance with the CDC Records Control Schedule.
Sample Design
A nonprobability sampling scheme will be used to select potential participants from the NEISS-Work and NEISS-AIP databases. Two sample selection pools will be used: cases with a work-related injury (NEISS-Work) and cases with a non-work-related injury (NEISS-AIP). The sample design uses methodology to (1) minimize the variance within hospital strata by using balanced designs in lieu of simple random sampling; (2) apply an appropriate statistical weight to each interview, taking into account potential respondent biases when respondent characteristics are compared to NEISS-Work and NEISS-AIP case characteristics as a whole; and (3) optimize the ability for this project to attain reportable, stable, and valid data results that meet NIOSH confidentiality requirements.
The goal when setting the sampling rates was to minimize variation in final patient weights, obtain the required total initial sample size from both the work-related and non-work-related injury groups (n=300 to 600 for each group), and acquire enough cases to make subgroup estimates. The sampling rate for eligible patients in each hospital/patient-type stratum (i.e., sampling rates are initially uniform across hospital strata by data source (NEISS-Work or NEISS-AIP)) was calculated by first solving for the rate that gives an overall constant weight for the remaining patients across all 58 hospitals (63 hospitals minus the five children’s hospitals, which will not be sampled for this project). The rates were then “rounded” to integer rates for ease of sampling, and adjusted slightly if necessary to produce the total desired initial sample size.
The hospital sampling rates can be adjusted periodically to account for variation in response rates across hospitals and patient group to prevent sample size shortfalls. The patient sampling will be done in batches on a flow basis. The frequency of sampling will depend on the volume of work-related injuries at the hospital ED. However, sampling will occur throughout the entire 12 month period to avoid seasonal effects bias. Every eligible case will be given one (and only one) chance of selection. Prior to sampling cases, if possible, the list of patients will be sorted by demographic characteristics such as race/ethnicity, occupation type, sex, and age.
Each hospital is assigned two within-hospital sampling rates based on its hospital stratum—one sampling rate for cases from NEISS-Work and a second sampling rate for cases from NEISS-AIP. The same sampling rates will initially be assigned to all hospitals in the stratum, based on the rates needed to minimize variation in the final patient weights and obtain the total required sample sizes. The initial total sample sizes will be inflated to allow for loss due to noncontact and nonresponse. An overall completion rate of 40 percent for sampled ED patients in both groups has been assumed. In reality, response rates will differ by patient characteristics and by hospital. Thus, a sample tracking system will be implemented to review the sample yields as the study progresses. The rates for some hospitals and/or patient groups may need to be adjusted periodically to keep the sample yields on target should the response rates and contact assumptions prove to be inaccurate. The sample tracking system will also store the sampling rates used for each batch of sampled cases for use in calculating patient weights for analysis. As the interviewing begins, interview response rates and number of completed interviews will also be monitored. If the response rates are lower than expected, the sampling rates will need to be increased.
B.2 Procedures for the Collection of Information
B.2.1 Stratification and Sample Selection
NEISS, NEISS-Work, and NEISS-AIP sample selection
T
 he
hospital populations for NEISS-Work and NEISS-AIP data are based on
two-thirds of the CPSC NEISS sample. The NEISS sample design is
based on a stratified simple random sample of hospitals with an
emergency department (ED) in the U.S. and its territories. A
hospital is defined as a general or specialty care facility with a
minimum of six beds and a 24-hour ED. The requirement for a hospital
to have at least six beds conforms to the American Hospital
Association (AHA) registration requirements (AHA, 2006).
he
hospital populations for NEISS-Work and NEISS-AIP data are based on
two-thirds of the CPSC NEISS sample. The NEISS sample design is
based on a stratified simple random sample of hospitals with an
emergency department (ED) in the U.S. and its territories. A
hospital is defined as a general or specialty care facility with a
minimum of six beds and a 24-hour ED. The requirement for a hospital
to have at least six beds conforms to the American Hospital
Association (AHA) registration requirements (AHA, 2006).
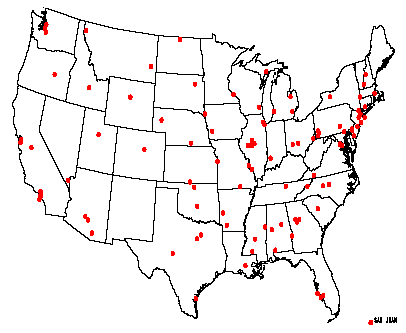
Figure B.2.1. U.S.
distribution of CPSC hospitals
NEISS hospital sample with four size-related strata and a children’s hospital stratum. In addition to stratification by hospital size, the NEISS sample is stratified geographically. Within each size stratum, a systematic hospital sample was drawn from a geographically-ordered SMG hospital list. The U.S. distribution of CPSC hospitals in the NEISS sample is shown in Figure B.2.1.
Since the initiation of the NEISS program in 1972, the CPSC hospital sample has been redesigned three times with implementation in 1978, 1990, and 1997. In addition to redesign changes, the number of hospitals in the sample has changed over time as CPSC has tried to enhance the data collection or reduce the system cost depending upon the vagaries of budgetary constraints. NIOSH has undergone similar expansions and contractions in its NEISS-Work data collection efforts. Currently, NIOSH collects data on all work-related injuries and illnesses treated in the ED at two thirds of the CPSC hospitals. The NEISS-Work data collection has been uniform and systematic since January 1, 1998, the last effective date of a break in series. NEISS-AIP data collection comes from the same hospital subset as that used by NEISS-Work.
For the purposes of NEISS-Work and NEISS-AIP methodology descriptions, the number of hospitals in the samples is defined as the number of hospitals in the sample at the time the current sample was initially selected. Both supplements use the same 1997 redesign hospital sample of 67 hospitals. When a hospital closes, the number of in-scope hospitals decreases because closures are not replaced in the sample. If a hospital simply withdraws from participating in NEISS, a new hospital is recruited and the original hospital is replaced, although there may be an extended lapse in reporting. The withdrawal of a hospital from NEISS or hospital non-response for a period of time does not result in a reduction of the number of in-scope hospitals (although it does influence the case weights for the period). The number of in-scope hospitals and reporting hospitals may change in any month of the year. Because four small hospitals have closed, there are currently only 63 in-scope hospitals. Also, one of the nine medium size hospitals stopped reporting and a replacement hospital is being sought. Case weights are adjusted to account for this nonresponse until the hospital is replaced.
The 1997 CPSC sample redesign is based on a 1995 SMG sample frame. The full sample had 102 hospitals (1.9% of qualifying hospital EDs), but by the time the sample was implemented one hospital had closed resulting in 101 in-scope hospitals. CPSC used a Keyfitz procedure for resampling a stratified simple random sample that maximized the probability of retaining hospitals from the former sample (i.e., participating hospitals in 1996). As a result, 75 hospitals were retained and 26 new hospitals were recruited. As a part of this redesign, the children’s hospital stratum became a probability based sample and no longer a simple convenience sample.
Although not used for the NEISS sample frame, the American Hospital Association annual surveys illustrate the decrease in emergency departments in community hospitals (nonfederal, short-term general and other special hospitals), while ED visits have increased in number and rate (Figure B.2.2) (AHA, 2006). Whereas the NEISS sample includes Federal and non-federal hospitals with 5,388 EDs in 1995, the AHA sample of community hospitals with 4,923 EDs in 1995 is generally representative of U.S. hospital trends as a whole.
Figure B.2.2. (a) Number of ED visits and number of EDs in community hospitals; (b) rate of ED visits per 1,000 persons; 1991-2004 (AHA, 2006).
Source:
The Lewin Group analysis of American Hospital Association Annual
Survey data, 1991 – 2004, for community hospitals and US
Census Bureau: State and County QuickFacts, 2004 population
estimate data derived from Population Estimates, 2000 Census of
Population and Housing

In October 1997, NIOSH implemented the 1997 CPSC sample design. However, budgetary constraints prohibited using the full 102 hospital sample. To continue with a sample of approximately the same size (i.e., ~65 hospitals) NIOSH obtained a new sample of 67 hospitals that was approximately two-thirds of the CPSC sample for each stratum at that time. For the new NIOSH sample, 52 hospitals were retained from the prior sample and 15 new hospitals were added. Although adding a large number of new hospitals to the sample created some difficulties, work-related case reporting appeared stabilized by January 1998. When NEISS-AIP began in 2000, it used the NEISS-Work hospital sample created in the 1997 sample redesign.
Each NEISS-Work and NEISS-AIP case is assigned a statistical weight based on the inverse probability of selection. National estimates (i.e., the number of injuries and/or illnesses) are obtained by summing weights for all cases or particular cases of interest. The basic case weight is the inverse probability of selection for the hospitals in each stratum. The inverse probability of selection is the number of hospitals in the stratum universe divided by the number of hospitals in the NEISS sample for the stratum.
CPSC makes two types of routine weight adjustments to the basic case weights. First, weights are adjusted for non-participation if a hospital does not report fully during any given month or to account for hospital mergers, hospital closings or withdrawal from the NEISS-Work/NEISS-AIP sample. Secondly, CPSC makes an annual ratio adjustment to the case weights by comparing the most recent U.S. hospital sample frame (i.e., for the prior year) with the 1995 sampling frame (used in 1997 for the latest NEISS sample). This adjustment is designed to account for changes in ED usage and the number of hospitals with EDs over time to provide the best opportunity for trend analysis and to minimize the expense of frequent sample redesigns. Thus, final case weights for each hospital stratum by month and year are calculated from the basic weight with adjustments for non-reporting and changes in the sampling frame over time.
Barriers project sample selection
The goal when setting sampling rates was to minimize variation in final patient weights, obtain the required total initial sample sizes, and to acquire enough cases to make subgroup estimates. Using these criteria, two sampling rates were calculated for each hospital—one sampling rate for cases from NEISS-Work and a second sampling rate for cases from NEISS-AIP. All sampling rates have been “rounded” to integer rates for ease of sampling, and adjusted slightly if necessary to produce the total desired initial sample sizes. Initial sampling rates do not vary across hospitals within the same strata. For example, in the medium hospital stratum, all NEISS-Work cases will initially be sampled at the same rate. The same holds true for all NEISS-AIP cases within a particular stratum. However, within a single stratum, the initial NEISS-Work sampling rate does not equal the NEISS-AIP initial sampling rate. The initial within-hospital sampling rates for each subsample do not vary within a stratum since the hospital weights are the same within each stratum (with the exception of one hospital in the medium stratum). The sampling rates can be adjusted periodically to account for variation in response rates across hospitals to prevent a sample size shortfall. The rates have been set to produce 300 to 600 completed interviews per year in each subgroup. If sampling rates are modified over time to increase the yields, the overall patient weights may become more variable. The final patient weights will also become more variable when they are adjusted for interview nonresponse.
Based on the sample design requirements for final data collection, CPSC will select potential respondents weekly from incoming routine NEISS-Work and NEISS-AIP case data. Prescreening will be used to restrict the potential respondents to those individuals most likely to meet the respondent definition (e.g., ages <20 and >64 and self-employed will be excluded). CPSC will then contact the participating hospital and request patient contact information. Individuals identified with potentially viable contact information will be sent one letter notifying them of the interview study and giving them the opportunity to “Opt Out.” Contact information for individuals who do not opt out, or who fail to respond to the letter within ten days, will be provided to a third-party contractor who will conduct the interviews. Contact information will be provided by the CPSC approximately three weeks after the date of treatment. At no time will NIOSH have the individual identifiers or contact information for the potential respondents.
The patient sampling will be done in batches on a flow basis. The frequency of sampling will depend on the volume of work-related injuries and overall injuries at hospital EDs. However, sampling will occur throughout the entire 12-month period to avoid seasonal effects bias. Every eligible case will be given one (and only one) chance of selection. Prior to sampling cases, if possible, the list of patients will be sorted by demographic characteristics such as race/ethnicity, occupation type, sex, and age.
Each time sampling is done, the following information will be recorded in an electronic sample tracking sheet for each subgroup: hospital name and ID, date of sampling, total number reported, total number sampled, and the sampling rate used. Periodically, the total number sampled will be tallied to check sample yields against the targets. If the total number of a subgroup sampled is below the expected number given how far the field period has progressed, the sampling rate for that subgroup in the hospital will be increased. New sampling rates will be calculated as follows: 1) update the total number of eligible cases in that subgroup reported in each hospital over the first six months, 2) calculate the remainder sample size needed based on the cases obtained so far, and 3) calculate new sampling rates to obtain the remainder needed. As the interviews begin, interview response rates and number of completed interviews will also be monitored. If the response rates are lower than expected, the sampling rates will be increased.
B.2.2 Collection of Telephone Interview Data
Telephone interviewers are contracted through CPSC to complete the follow-back interviews. These interviewers are experienced interviewers and will receive additional training specific to the Barriers questionnaire to be used for this study.
Prior to being contacted by telephone, potential participants will receive a letter describing the study and their protections as a participant should they choose to participate (Appendix C). This letter also provides them with the opportunity to not participate in the study by calling a toll-free number. While the time for the telephone interview is not initially scheduled, participants have the option at the time of contact to indicate that it is not a good time and to schedule a more convenient time to complete the interview.
B.2.3 Data Quality Control
Quality control of the data will not involve any additional contact with participants. Throughout data collection, a data cleaner will review the CATI database for appropriate values and skip pattern consistency. Analyses that will be used for this review include:
One-way, labeled frequency distributions of database variables.
Cross-tabulations of database variables to check skip patterns and other relationships.
A query-by-identifier interactive report used to browse variable values by case.
A query-by-value report to identify every record or record group matching a value, condition, or pattern.
Interviewer comment file review – interviewers may enter comments about anything that was said or happened during an interview. The data cleaner will review this file and use it to resolve issues during data collection, such as an interviewer believing that the response did not fit any of the available categories or because it was outside a hard range.
Using all of these resources, the data cleaner may make changes to specific variables in specific interview records or a set of records. Any changes will be automatically captured in an edit log, which becomes part of the permanent documentation of the database. At this stage, the edit log contains any and all updates performed on a dataset during data collection, along with a brief note describing the reason for each edit. If an edit is performed, both the original coded value and the new updated value are documented in the log for each variable, for each affected case. As described below, this log is passed to the post-data collection data manager and maintained through all subsequent processing stages.
In addition to the CATI data cleaner’s ongoing review of data during data collection, a second, independent review will be performed by the project data manager on the stable survey database immediately following data collection. The data manager will use the CATI instrument specifications and develop an independent SAS program that tests the integrity of the data collected. Any skip patterns/coding inconsistencies or violations of hard range values will be reviewed and any edits/updates will be documented. It should also be noted that before any edits or updates are performed, a back-up copy of the original dataset, as collected, will always be stored separately to allow for recourse in rare instances when there are problems with manipulated or processed datasets.
B.3 Methods to Maximize Response Rates and Deal with Nonresponse
We acknowledge that our projected response rate of 40%, based on the current CPSC reported 40-45% response rate is low. However, it must be noted that this rate of overall response includes cases identified in NEISS-Work and NEISS-AIP for which hospitals will not release contact information or correct contact information is unavailable. These insurmountable barriers drive the response rate down prior to us beginning to contact potential participants. In a recent study, this accounted for 35% of all potential cases.
Given a potentially low response rate, we plan to take several steps to help access potential participants and facilitate their willingness to participate. These steps include:
A letter describing the study will be sent to potential participants in advance of the initial phone call. This letter will alert and prepare potential participants for the phone call requesting their participation.
Telephone interviewers are required to make at least ten attempts to reach a potential respondent. The contact attempts are made at varying, but reasonable, hours of the day and on varying days of the week. When no personal contact is made after a number of attempts, the interview is set aside and contact attempts are made at a later date as time permits to maximize the response rate while minimizing recall bias issues. Interviewers are trained to be considerate of respondents and their families, leaving a minimal number of messages or speaking with the respondent or another individual of the residence to arrange a convenient interview time. Messages include a toll-free response number so that the respondent may call at their convenience. When no personal contact is made, no message system is available, or there is no indicator of an incorrect number, the interviewer typically spreads call attempts over a longer period and makes more than 10 contact attempts.
This project will use trained telephone interviewers who are experienced at conducting interviews. This will facilitate ease of survey participation for the respondent, increasing the likelihood that they will complete the survey in its entirety.
If the participant refuses the initial offer to participate in the study in a non-firm way, the interviewer will emphasize the importance of their participation and inquire as to whether they would be willing to participate at another time. The training and experience of the telephone interviewers will be key factors to understanding the reactions of potential participants and appropriately encouraging their participation in cases of refusal.
The questionnaire has been designed to be as easy and non-burdensome as possible. This includes ordering the questions in a logical sequence and asking only those questions that are needed for analysis purposes.
Despite a potentially low response rate, one of the benefits of this study is that we capture basic demographic and injury or illness information on all potential participants. Ultimately, we will compare the information we have on respondents and non-respondents using the NEISS-Work and NEISS-AIP datasets to provide insight on any potential response bias. At a minimum, the case weights are adjusted for non-response within each stratum and subgroup so that the completed interviews within each stratum-subgroup truly represent that population. If other factors are determined to influence answers, raking is performed so that the analysis weights for each variable of interest are equal to the corresponding national estimate.
B.4 Test of Procedures or Methods to be Undertaken
B.4.1. Interview Questionnaire.
To achieve the aims for this project, we will use a telephone interview questionnaire that has been developed by NIOSH, based on applicable existing research and related questionnaires. During development, the questionnaire was reviewed by experts and cognitively tested. This questionnaire will maximize our ability to identify the perceived barriers and incentives to reporting of an occupational injury and confirm the work- or non-work-relationship of the treated injury.
The interview will be about 30 minutes or less in length, including the introductory materials. The interview will begin with an explanation of the study purpose and provide the information needed for informed consent. The subsequent questionnaire will begin with a brief series of qualifying questions, followed by an opportunity for the respondent to give a free form narrative statement of the recent injury event. The remainder of the questionnaire will consist of separate modules that address workplace, personal, and injury characteristics; beliefs and reporting behaviors with respect to one’s employer and ED staff; and elements of the Theory of Planned Behavior in response to hypothetical vignettes. The specific modules included are: (1) qualifying section; (2) ED reporting; (3) reporting a work-related injury (this section is only given to those whose injury occurred or was made worse at work); (4) medical coverage and state of recovery; (5) occupational data; (6) Theory of Planned Behavior questions; (7) demographic and sensitive occupational information; and (8) debriefing/summary.
The initial draft questionnaire was developed by NIOSH staff in collaboration with outside experts in the field. NIOSH staff solicited comments from both experiential and topical experts. Experiential experts consisted of several workers (e.g., nurses and construction workers) who were asked to review the Theory of Planned Behavior questions and to provide feedback on ease of comprehension and relevance to their work situation. Topical experts reviewed and provided feedback on the questionnaire in its entirety. Revisions were made to the instrument to incorporate reviewers’ comments and to harmonize the questionnaire with another underreporting survey being conducted by NIOSH. The revised questionnaire was pilot tested on a small number of employees at the NIOSH Morgantown branch who used constructed scenarios in order to test the skip pattern, flow, understandability, and comprehensiveness of the questions and their answer choices. Subsequently, survey experts from Research Triangle Institute (RTI), an independent, nonprofit research institution with more than 45 years of experience in survey methodology, reviewed and commented on the questionnaire and conducted cognitive interviews on nine participants. Finally, NIOSH staff worked with RTI staff to revise the questionnaire (Appendix D) based on the results of cognitive testing.
B.4.2. Cognitive Testing.
RTI conducted cognitive testing of the questionnaire with nine potential respondents, five from NEISS-Work and four from NEISS-AIP, to insure clarity of questionnaire language and identify problems related to timing, skip patterns, and other complex conceptual issues that may not be readily obvious from simple reading of the questionnaire.
To identify the pool of participants for the cognitive interviews, CPSC selected potential respondents from incoming routine NEISS-Work and NEISS-AIP case data. Prescreening was used to restrict the potential respondents to those individuals who were most likely to meet the respondent definition (e.g., ages <20 and >64 and self-employed were excluded). CPSC contacted the participating hospital and requested patient contact information. Individuals identified with potentially viable contact information were sent a letter notifying them of the cognitive testing for the NIOSH interview study and giving them the opportunity to “Opt Out.” Contact information for individuals who did not opt out was provided to CPSC by the hospital approximately three weeks after the date of treatment. CPSC provided the contact information for potential respondents to NIOSH for transmission to RTI following NIOSH confidentiality protocols. In compliance with Office of Management and Budget (OMB) requirements, RTI interviewed no more than 9 individuals as a part of this cognitive testing.
B.5 Individuals Consulted on Statistical Aspects and Individuals Collecting and/or Analyzing Data
Individuals who were consulted on statistical aspects
David A. Marker, Ph.D.
Senior Statistician
Westat, Inc.
1650 Research Blvd.
Rockville, MD 20850-3195
Phone: 301-251-1500
Pam Broene, Ph.D.
Senior Statistician
Westat, Inc.
1650 Research Blvd.
Rockville, MD 20850-3195
Phone: 301-251-1500
Tom Schroeder, MS
Statistician, Director
Division of Hazard and Injury Data Systems
U.S. Consumer Product Safety Commission
Phone: 301-504-0539 x1179
E-mail: [email protected]
Individuals who will collect the data
CPSC staff and contracted interviewers under the direction of:
Tom Schroeder, MS
Statistician, Director
Division of Hazard and Injury Data Systems
U.S. Consumer Product Safety Commission
Phone: 301-504-0539 x1179
E-mail: [email protected]
Individuals who will analyze the data
Larry Jackson, PhD
Chief, Injury Surveillance Team
Division of Safety Research, NIOSH
Phone: 304-285-5980
E-mail: [email protected]
Susan Derk, MA
Epidemiologist, Injury Surveillance Team
Division of Safety Research, NIOSH
Phone: 304-285-6245
E-mail: [email protected]
Suzanne Marsh, MPA
Statistician, Injury Surveillance Team
Division of Safety Research, NIOSH
Phone: 304-285-6009
Email: [email protected]
Audrey Reichard, MPH, OTR
Epidemiologist, Injury Surveillance Team
Division of Safety Research, NIOSH
Phone: 304-285-6019
E-mail: [email protected]
Tom Schroeder, MS
Statistician, Director
Division of Hazard and Injury Data Systems
U.S. Consumer Product Safety Commission
Phone: 301-504-0539 x1179
E-mail: [email protected]
Selected Citations
AHA. Hospital Statistics, 2006 ed: Health Forum, Chicago, IL. 2006.
Marker, D.A., and Lo, A. (1996). Update of the NEISS sampling frame and sample, final report. Prepared by Westat for the Consumer Product Safety Commission, October 11, 1996.
1 Because of confidentiality restrictions, NIOSH does not publicly release the minimum sample case or national estimate requirements. Variance requirements are released.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| File Title | Occupational injuries and illnesses among emergency medical services (EMS) workers: A NEISS-Work telephone interview survey |
| Author | Audrey Reichard |
| File Modified | 0000-00-00 |
| File Created | 2021-01-31 |
© 2026 OMB.report | Privacy Policy