ATTACHMENT M_CHIPRA ELE Evaluation Final Design and Work Plan Part 1
11. ATTACHMENT M_CHIPRA ELE Evaluation Final Design and Work Plan Part 1.docx
CHIPRA-Children's Health Insurance Program Reauthorization Act of 2009 -ELE
ATTACHMENT M_CHIPRA ELE Evaluation Final Design and Work Plan Part 1
OMB: 0990-0400
Attachment m
CHIPRA ELE EVALUATION DESIGN REPORT
CHIPRA Express Lane Eligibility Evaluation
Final Design Report and Work Plan
Volume I: Evaluation Design
January 13, 2012
Mathematica Policy Research Marian Wrobel Sheila Hoag Margaret Colby Sloane Frost Cara Orfield Sean Orzol Adam Swinburn Kristina Rall
|
Urban Institute Fiona Adams Sarah Benatar Frederic Blavin Brigette Courtot Stan Dorn Ian Hill Genevieve Kenney Health Management Associates Jennifer Edwards Rebecca Kellenberg Eileen Ellis Sharon Silow-Carroll Esther Reagan Diana Rodin
|

This page has been left blank for double-sided copying.
This page has been left blank for double-sided copying.
CONTENTS
I. introduction 1
A. ELE as a Policy Tool for Expanding Coverage 1
1. The Potential of ELE to Raise Enrollment 2
2. Other Potential Benefits of ELE 2
3. Current State Implementation of ELE 4
B. Alternate Approaches to Expanding Coverage and Simplifying Enrollment and Retention 7
C. The Congressionally Mandated Evaluation of ELE 8
II. overview of the evaluation design 11
III. The Technical Advisory Group and its role in the evaluation 19
A. Purpose of the TAG 19
B. TAG Member Selection and Recruitment 19
C. Methods 20
D. Initial TAG Meeting 20
E. Next Steps 21
IV. Study 1: Ongoing Assessment of the State Policy Context 23
A. Baseline Information Review 23
B. State Tracking and Monitoring 24
1. Selecting the 30 States 24
2. Selecting Key Informants 25
3. Key Informant Interviews 25
4. Quarterly Reports 26
C. 51-State Survey 26
V. Study 2: Analysis of ELE Impacts on Enrollment (Using SEDS) 29
A. Data Sources 29
B. Analysis 32
C. Challenges 34
VI. Study 3: Case Studies of States Adopting ELE and Other Approaches to Simplifying Enrollment and/or Retention 37
A. ELE Program Case Studies 37
1. Review of State Documents, Evaluation Reports, and Other Background Material 38
2. Site Visits 38
3. Focus Groups 41
B. Case Studies in Non-ELE States 38
1. Selecting Non-ELE States 38
2. Focus Groups in Non-ELE States 39
C. Analysis and Reporting 38
D. Challenges and Limitations 38
vii. DESCRIPTIVE STUDY OF COSTS, ENROLLMENT, AND UTILIZATION IN CASE STUDY STATES 40
A. ELE States 41
1. Acquisition of Data 41
B. Cost Analysis 43
1. Motivation 43
2. Administrative Cost Data and Analysis—First Year 44
3. Administrative Cost Data and Analysis—Second Year 61
4. Challenges 61
C. Enrollment Analysis 62
1. Motivation 62
2. Enrollment Data and Analysis – First Year 62
3. Enrollment Data and Analysis—Second Year 64
4. Challenges 65
D. Utilization Analysis 65
1. Motivation 65
2. Utilization Data and Analysis 66
3. Challenges 67
E. Reporting 67
Chapter VII (Continued)
F. Non-ELE Program Cost and Enrollment Study 68
1. Acquisition of Data 68
2. Motivation 68
3. Cost and Enrollment Data and Analysis 68
4. Challenges 68
5. Coordination 69
6. Reporting 69
VIII. Evaluation Reports and related briefings 71
A. Recommendations on ELE Improvements 71
B. Reports to Congress 72
C. Study Briefings 73
IX. Developing and Obtaining Approval for Data Collection Instruments 75
A. OMB Clearance 75
B. IRB Approval 76
REFERENCES 77
APPENDIX A: Example of memorandum of understanding for study of costs enrollment, and utilization 81
APPENDIX B: example of table shells for study of costs, enrollment, and utlization 86
This page has been left blank for double-sided copying.
TABLES
I.1 States with Approved State Plan Amendments for CHIPRA Express Lane Eligibility (ELE) Prepared November 14, 2011 5
I.2 Mapping of RFP Tasks to the Evaluation’s Four Studies and Chapters of the Design Report 10
II.1 Evaluation Goals, Research Questions, and the Main Studies and Data Sources for Addressing Them 14
II.2 Key Characteristics of Evaluation Studies and Data Sources 15
III.1 TAG Members 19
VI.1 ELE Site Visit Interview Protocol Potential Topics and Questions 43
VI.2 Potential ELE State Focus Group Moderators’ Guide 37
VI.3 Proposed Non-ELE States Focus Group Moderator’s Guide 41
VII.1. Key Research Questions Addressed Through Program Cost, Enrollment, and Utilization Study 40
VII.2 Summary of Analyses Completed Under Program Cost, Enrollment, and Utilization Study 41
VII.3 Draft Discussion Guide for ELE States Cost Study 45
VIII.1 Content and Sources of Data for Interim and Final Reporting to ASPE 72
IX.1 Schedules for OMB Submission 75
This page has been left blank for double-sided copying.
FIGURES
V.1 Snapshot of the 2010 Form 21E Quarterly (SEDS) Enrollment Report 31
This page has been left blank for double-sided copying.
I. introduction
As part of the Children’s Health Insurance Program Reauthorization Act of 2009 (CHIPRA), Congress gave states the option to implement a new policy known as Express Lane Eligibility (ELE). With ELE, a state’s Medicaid and/or Children’s Health Insurance Program (CHIP) can rely on another agency’s eligibility findings to qualify children for health coverage, despite its different methods of assessing income or otherwise determining eligibility. ELE thus gives states another way to try to enroll and retain children who are eligible for Medicaid and CHIP but remain uninsured, including children who have traditionally been most difficult to reach.
CHIPRA authorized an extensive, rigorous evaluation of ELE, creating an exceptional opportunity to document ELE implementation across states and to assess the changes to coverage or administrative costs that might have resulted. The evaluation also provides an opportunity to understand other methods of simplified or streamlined enrollment that states have pursued and to assess the benefits and potential costs of these methods compared with those of ELE. The evaluation, to be conducted on behalf of the Office of the Assistant Secretary for Planning and Evaluation (ASPE) within the U.S. Department of Health and Human Services (HHS), will yield two major Reports to Congress: an interim report, due by September 30, 2012, and a final report, due by September 30, 2013.
This report presents the design for the congressionally mandated evaluation of ELE. The evaluation will be led by Mathematica Policy Research, with the assistance of the Urban Institute and Health Management Associates (HMA). The design presented here has benefited from multiple discussions with ASPE as well as a day-long meeting with our technical advisory group (TAG), discussed in Chapter III.
A. ELE as a Policy Tool for Expanding Coverage
ELE is best described as an open-ended authorization of a broad range of state efforts to incorporate findings from other public agencies into the eligibility determinations of Medicaid and CHIP programs. As the Centers for Medicare & Medicaid Services (CMS) explained, “There is no one way to implement the Express Lane option” (Centers for Medicaid and State Operations 2010).
This breadth in the definition of ELE distinguishes it from other strategies to improve enrollment and retention (such as continuous eligibility, elimination of asset requirements, elimination of in-person interview requirements, and joint Medicaid/CHIP applications), which have similar basic structural features in most implementing states. In contrast, with ELE, a state can choose from among 13 named agencies with which to partner, or even select an unlisted program that fits the statute’s broad definition of an “Express Lane Agency.”1 Other features can vary. For example, ELE can apply to enrollment, retention, or both; ELE can either include or exclude an automatic enrollment option; ELE can apply to CHIP, Medicaid, or both; states can use traditional approaches to CHIP screen-and-enroll requirements or choose from among two alternative approaches specified in CHIPRA; and states may choose the element or elements of Medicaid or CHIP eligibility (except citizenship) to borrow from the findings of other agencies. Thus, many facets of the evaluation treat ELE as consisting of multiple differing initiatives in different states, not as one single initiative carried out in multiple states.
1. The Potential of ELE to Raise Enrollment
ELE has the potential to raise the enrollment of eligible children in public health insurance, both by raising families’ awareness of their eligibility and by reducing barriers to enrollment. With roughly two-thirds of the nation’s uninsured children eligible for Medicaid or CHIP but not enrolled (Kenney et al. 2010), significant progress in expanding coverage might depend on the kind of flexible strategy that ELE permits states to follow. As a tool for increasing eligible children’s coverage through Medicaid and CHIP, the promise of ELE has been well identified. For example, using ELE to qualify children for health coverage based on their participation in the Supplemental Nutrition Assistance Program (SNAP), Kenney et al. (2010) estimate that ELE could reach 15.4 percent of eligible, uninsured children. Using ELE to qualify children for health coverage based on state income tax records could reach even more children. An estimated 89 percent of uninsured children who qualify for Medicaid or CHIP live in families who file federal income tax returns (Dorn et al. 2009). Presumably, a large proportion of these families file state returns as well, particularly in states that supplement the federal Earned Income Tax Credit. ELE might also hold the potential to reach many adults beginning in 2014.
Insights from behavioral economics further underscore the potential of ELE as a way to expand coverage. Behavioral economists have reminded us of inertia’s remarkable power to shape enrollment into public or private benefits. For example, with the by-now-classic example of 401(k) retirement savings accounts, if new employees must complete applications to enroll, roughly a third participate; but if they are automatically enrolled unless they complete a form opting out, 90 percent join (Laibson 2005). ELE was intended to greatly minimize the need to complete applications for health coverage, because eligibility determination could be based on the findings of other agencies to which the families of uninsured children had already demonstrated low income or other facts relevant to eligibility for Medicaid and CHIP.
2. Other Potential Benefits of ELE
ELE also has other potential benefits beyond the potential increases in enrollment. Families that would otherwise have enrolled in public health insurance via traditional pathways also benefit when enrollment is made more automatic and less difficult. When systems function smoothly, states might enjoy lower per-application costs due to a streamlined process.
In addition, investments in the name of ELE can offer diverse benefits beyond increased enrollment and reduced burden. We discuss these briefly next.
ELE embodies an innovative approach to the broad problem of siloed public benefits. Low-income families seeking several forms of assistance must typically provide the same information to more than one program, each of which pays its staff to process that information. This creates needless red tape for families, administrative costs for government agencies, and more demanding application procedures that ultimately reduce participation levels. One reason for such redundancy involves technical differences between program eligibility rules. For example, SNAP generally limits benefits to households with net income at or below 100 percent of the federal poverty level (FPL). One might think that SNAP-recipient children are thus necessarily income-eligible for Medicaid and that, when families seek Medicaid on their behalf, they could be relieved of the need to document income. However, SNAP determines net income by applying excess shelter cost deductions that Medicaid does not use. SNAP and Medicaid also use different definitions of the household members whose needs and earnings count in determining income. Therefore, SNAP eligibility determinations typically cannot qualify children for Medicaid without families providing additional information or Medicaid staff meticulously “cross-walking” information from SNAP records into the categories established by Medicaid eligibility rules.
A traditional approach to breaking down these silos involves modifying different programs’ rules and procedures so they align. Although this approach has considerable merit, it is difficult to change the rules of multiple programs. ELE takes a different approach that can, under some circumstances, be easier to implement. In this approach, each program continues to apply its own eligibility methodologies, but one agency uses the other agency’s findings to qualify people for subsidies, despite their methodological differences.
ELE provides a new way to address the challenges created by delinking Medicaid and cash assistance. Before the Personal Responsibility and Work Opportunity Reconciliation Act (PRWORA) passed in 1996, the typical route to Medicaid ran through applications for cash assistance, which represented a higher priority than health coverage for many low-income families. With ELE, a state can once again hitch health coverage to other benefits, such as SNAP, that many families perceive as a higher priority.
It is true that public benefit programs have long offered application forms that permit families to simultaneously seek SNAP, Medicaid, cash assistance, and sometimes other benefits (such as energy assistance). However, such forms request the information needed by all these programs, a burden that defeats many applicants. To help families avoid long forms, some states have encouraged families to file SNAP-only applications or Medicaid/CHIP-only applications. ELE offers states a way to reduce the burden of multiprogram enrollment: a family filing a SNAP-only application can receive Medicaid or CHIP as well.
ELE substitutes data matches for the manual processing of forms in determining eligibility. This helps states do more with less. In much of the country, the worst state budget crises in decades have led to staff cutbacks and hiring freezes, shrinking the staff that take applications and determine eligibility, even as the ongoing economic downturn continues an elevated demand for services. Strategies such as ELE, which can lower administrative costs of enrollment and renewal, are particularly appealing to state officials with limited administrative resources.
ELE can help states comply with the Affordable Care Act. The Affordable Care Act requires states to transition to data-based eligibility methods that will qualify people for Medicaid, CHIP, and subsidies in the Affordable Insurance Exchanges, a step that ELE states have made progress to implement. Because of the central role of modified adjusted gross income and tax return information under the Affordable Care Act, this progress is particularly meaningful for states that use ELE to grant eligibility based on data matches with tax agencies. In addition, SNAP linkages might be useful for states seeking to reduce their administrative burdens by prequalifying low-income adults who will be newly eligible for Medicaid in 2014. More fundamentally, the Affordable Care Act requires that, whenever possible, eligibility for Medicaid, CHIP, and subsidies in the Affordable Insurance Exchanges must be established, verified, and renewed based on matches with reliable data sources. With ELE, states can begin making the challenging shift from traditional, manual methods to data-based routines for processing applications and renewals.
3. Current State Implementation of ELE
Despite the substantial promise of ELE as a way to achieve progress across a range of state priorities, only a handful of states have implemented it so far. As Table I.1 shows, only eight states—Alabama, Georgia, Iowa, Louisiana, Maryland, New Jersey, Oregon, and South Carolina—currently have approved plan amendments. Moreover, several of these amendments (Georgia, Iowa, Maryland, Oregon, and South Carolina) were approved only in the past 18 months. Even among this small group of states, however, the variation in the ELE model is striking and reflects the flexibility that the CHIPRA authorization afforded. For example, their matching agencies range from those administering a collection of different benefits—such as school lunch (New Jersey, just approved), SNAP (Alabama, Iowa, Louisiana, and South Carolina), Temporary Assistance for Needy Families (TANF) (Alabama and South Carolina), and WIC (Georgia)—to those responsible for aspects of state revenue, including the Division of Taxation (New Jersey) and the Office of the Comptroller (Maryland).
Results from the models are beginning to emerge and often reflect self-reported descriptive data or qualitative information. These results suggest that the benefits of ELE vary, depending on the models implemented, though a more formal evaluation is clearly needed to draw credible conclusions within and across these states. Current data indicate that variation exists in enrollment using the ELE mechanism across the states (Table I.1). The ELE evaluation will build upon this base to fully characterize existing programs, to understand their impacts and implications, and to determine which programs have best practices that other states should model.
With only eight approved and implemented ELE programs, several factors have likely contributed to the modest uptake of ELE. The first is the economy: even in states with longstanding commitments to reaching all eligible children, serious fiscal woes have created strong resistance to the cost effects of increasing the number of children receiving Medicaid and CHIP. The second is the level of effort that might be required. This includes addressing challenging operational issues (such as linkages with sibling agencies that run different programs) and the intensive retraining and monitoring of social services staff unaccustomed to the approach. Finally, like any new, simplified enrollment method, ELE requires leadership and creative energy to pursue. Management staff have been reduced in many state agencies, and ELE implementation must compete for attention with top priorities, such as managing severe cutbacks and preparing for Affordable Care Act implementation.
Including ELE as one of the eight best practices for enrollment and retention, of which a state must implement at least five to qualify for performance bonuses under CHIPRA, likely has been a countervailing force and encouraged take-up of ELE among states.
Table I.1. States with Approved State Plan Amendments for CHIPRA Express Lane Eligibility (ELE) Prepared November 14, 2011
State and Program Type(s) using ELEa |
Matching Agencies, Eligibility Level for Ages 0-18, Effective Dates |
ELE Activities |
Results |
Alabamab
Medicaid
|
SNAP & TANF, 300% FPL, 4/1/2010 (SNAP) 10/1/2009 (TANF) |
Approved state plan amendment to conduct Medicaid eligibility and renewal using net income, family size, and income disregards from TANF and SNAP. Also deployed technology that allows online enrollment for multiple public programs and, on the back end, supports cross-agency data retrieval, verification, and processing. |
Three months after enactment, Alabama had renewed eligibility for more than 3,600 children. By the end of August 2010, 28,927 children had been processed. Alabama attributes its early success to good collaboration among Medicaid, TANF, and SNAP agencies. |
Georgia
Medicaid & CHIP |
WIC, 235% FPL, 1/1/2011 (Medicaid) 4/1/2011 (CHIP) |
Approved state plan amendment to use income information from WIC to establish CHIP eligibility. WIC agents check a system indicator field that enables them to share the information with the Department of Community Health (DCH). A data file from WIC is uploaded to PeachCare’s system nightly. DCH uses the income, age, residency, and identity portions of the WIC file, but must request additional information on household members, Social Security number (SSN), and citizenship status. |
Georgia has approved about 1,000 individuals for coverage between the two programs since April.
Although approved for enrollment and renewal, although in practice only the enrollment process is in place (ELE is not yet being used for redeterminations). |
Iowa
Medicaid & CHIP |
SNAP & Medicaid, 300% FPL, 6/1/2010 |
Approved state plan amendment to conduct automatic enrollment without a Medicaid application, using SNAP findings/data for all eligibility elements except citizen/alien status. |
As of June 30, 2011, the ELE form was sent to 15,549 families, and 1,396 children had been approved through the ELE option; 1,623 applications were in process. ELE must be requested by returning an opt-in form. ELE was not requested by 12,365 children. |
Louisiana
Medicaid |
SNAP & NSLP, 250% FPL, 10/10/2009 |
Approved state plan amendment to conduct Medicaid eligibility and renewal using SNAP and school lunch agency findings as to SSN (from SNAP), income, age, residency, and identity. Allows for the use of automatic enrollment. This process was implemented after years of conducting ex parte renewal through the Food Stamp and TANF programs. |
10,545 children were enrolled in the first month of ELE-enabled automatic eligibility. As of April 30, 2010, 3,391 children had already obtained medical services. Another 6,000 children needed further review due to minor errors in dates or names that prevented data-matching. After the initial wave of enrollment, child enrollment grew at 2.8% (the national average is 5.3%). |
Maryland Medicaid |
Office of the Comptroller 200% FPL, 4/1/2010 |
Approved state plan amendment to use information from state income tax records to make an initial Medicaid determination, using state residency information. Notices were sent to taxpayers with a dependent child who met income eligibility standards in tax year 2007. 2008 tax forms asked taxpayers to report health insurance coverage status for each dependent child. Medicaid/CHIP applications and enrollment instructions were then sent to all potentially eligible families. Maryland provides accelerated enrollment to Medicaid and CHIP applicants who already have an active case with Maryland’s Department of Social Services. Those children are eligible for up to three months pending a final determination. |
In 2007, approximately 450,000 families received the eligibility letter—180,000 families under 116% of the FPL and the rest between 116 and 300% of the FPL. One year after the comptroller sent the first wave of notices to taxpayers, more than 30,000 of Maryland’s uninsured children were enrolled in public coverage. The extent to which the notices were responsible for Maryland’s enrollment is unknown.
|
New Jersey Medicaid & CHIP |
Div. Taxation National School Lunch Program (NSLP), 350% FPL, 5/1/2009 |
Approved state plan amendment to use state tax records to establish income, budget unit, health insurance, citizenship (through SSN), and identity, for initial enrollment and renewal into Medicaid. Families have an opportunity to indicate they have uninsured dependents on their tax forms. These families are sent a form on which they authorize the use of the tax agency’s income finding to make an income-eligibility determination for Medicaid and CHIP and provide minimal additional information for a full eligibility picture. Also, New Jersey recently approved the use of data from the school lunch agency. |
The Department of Human Services mailed New Jersey FamilyCare Express Lane applications to each household identified as uninsured and below the eligibility threshold. It had a response rate of 5.7 percent, receiving only 16,504 completed applications. Of those, only 3,834 children were enrolled in FamilyCare. Initial feedback is that not many families have enrolled due to the two-step process. |
Oregon
Medicaid & CHIP |
SNAP & NSLP, 184% FPL, 8/1/2010 |
Approved state plan amendment to use SNAP and school lunch agency findings to make an initial Medicaid determination as to income, group size/household composition, SSN, and residency. Allows for the use of automatic enrollment. |
The state reports investing heavily in outreach and streamlining applications across programs. Internal culture has changed to work across programs for a common purpose. No data available. |
South Carolina
Medicaid
|
SNAP & TANF, 200% FPL, 4/1/2011 |
Approved state plan amendment allows South Carolina Medicaid to process redeterminations for children in families with incomes less than 200% of FPL in partnership with SNAP and TANF. |
The state expects to enroll 70,000 children and save $1 million in administrative costs as a result of this electronic collaboration. |
Sources: CHIP and Medicaid State Plan Amendments. Centers for Medicare & Medicaid Services web site. Accessed August 2, 2011.
The Children’s Partnership. “Express Lane Activities: States on the Move.” January 2011. Accessed August 2, 2011. http://www.childrenspartnership.org/AM/Template.cfm?Section=State_Activity_Report&Template=/CM/ContentDisplay.cfm&ContentID=13347
The Children’s Partnership ELE Program Examples web page. Accessed August 2, 2011. http://www.childrenspartnership.org/AM/Template.cfm?Section=State_Activity_Report&Template=/TaggedPage/TaggedPageDisplay.cfm&TPLID=153&ContentID=12200
The Children’s Partnership. “Express Lane Eligibility: Louisiana Moves Forward.” Updated April 2010. Accessed August 2, 2011. http://www.childrenspartnership.org/AM/Template.cfm?Section=Express_Lane_Toolkit&Template=/CM/ContentDisplay.cfm&ContentID=14527
Families USA. “Express Lane Eligibility: Early State Experiences and Lessons for Health Reform.” January 2011. Accessed August 2, 2011. http://www.familiesusa.org/assets/pdfs/chipra/Express-Lane-Eligibility-State-Experiences.pdf
Interviews with state officials conducted by HMA. July 2011.
Kaiser Family Foundation’s State Health Facts web page. Accessed August 2, 2011. http://www.statehealthfacts.org/comparemaptable.jsp?ind=898&cat=4&sub=195&rgnhl=2
Robert Wood Johnson and State Health Access Data Center. “Reaching Uninsured Children: Iowa’s Income Tax Return and CHIP Project.” August 2010. Accessed August 2, 2011. http://www.childrenspartnership.org/AM/Template.cfm? Section=State_Activity_Report&TEMPLATE=/CM/ContentDisplay.cfm&CONTENTID=14979
Robert Wood Johnson[Foundation?] and State Health Access Data Center. “Using Information from Income Tax Forms to Target Medicaid and CHIP Outreach: Preliminary Results of the Maryland Kids First Act.” September 2009. Accessed August 2, 2011. http://www.childrenspartnership.org/AM/Template.cfm?Section=State_Activity_Report&TEMPLATE=/CM/ContentDisplay.cfm&CONTENTID=13839
Adcox, Seanna. “Good News: S.C. Medicaid May Add 70,000 Kids to Program.” South Carolina Health Care Voices, October 25, 2011. Available at http://schealthcarevoices.org/2011/10/25/good-news-s-c-medicaid-may-add-70000-kids-to-program/. Accessed 2011.
a Program Type shows the program(s) that allow(s) ELE matching, according to the RFP. Program Type does not reflect the programs states reported utilizing in 2010 CHIP Annual Reporting Template System (CARTS) or the CMS CHIP map
(https://www.cms.gov/LowCostHealthInsFamChild/downloads/CHIPMapofStatePlanActivity.pdf. Accessed August 2, 2011).
b Alabama submitted two ELE state plan amendments. The first covered redetermination and was approved on November 2, 2009; the second covered both initial determination and redetermination and was approved on June 7, 2010.
B. Alternate Approaches to Expanding Coverage and Simplifying Enrollment and Retention
At the same time that some states are introducing ELE, many states are developing and implementing other approaches to raising families’ awareness of the availability of public health insurance and streamlining the enrollment and renewal process. Similar to ELE, these approaches frequently involve partnering with other organizations that serve the same population or making use of electronic data collected for other purposes. These alternate approaches include the following:
Online applications, including universal online application for multiple programs (for example, Wisconsin and Massachusetts both use a single portal model to apply for many public benefit programs)
Community-based application assistance (for example, many community groups received CHIPRA outreach grants in 2010 and 2011 to focus on community application assistance)
Automatic conversion from Medicaid to CHIP and vice versa if a child’s age or income change is reported (as in Massachusetts and possibly other states)
Use of data obtained from other state sources (ex parte data); for example, 13 states currently use ex parte data for renewal in CHIP (Hoag et al., 2011)
Co-location of Medicaid/CHIP eligibility determination with other benefit offices (such as in Utah, Michigan, and Wisconsin, among others)
Presumptive eligibility, permitting providers, schools, or other community-based organizations (CBOs) to screen and enroll those who appear eligibility (offered in CHIP by 16 states as of federal fiscal year 2010) (Hoag et al., 2011)
Data matching, which might be viable for adult enrollment support in 2014 (similar to ELE states that use income tax data)
Outreach via other programs, such as schools (some of the CHIPRA outreach grants are to schools, and 29 states reported schools as key outreach partners in the most recent CHIP annual reports) (Hoag et al., 2011)
Like ELE, these alternate approaches have the potential to raise enrollment and/or to alter the enrollment pathway for families who would otherwise have enrolled via a traditional pathway. Moreover, most of the approaches have some long-term potential to reduce the burden on states, families, or both via efficient use of existing data or by capitalizing on a situation or relationship that leads a family to be particularly receptive to enrolling in insurance. Like ELE, these approaches can create partnerships among agencies, move state data systems forward, and help states lay a strong foundation for the Affordable Care Act.
In some cases, the line between ELE and non-ELE approaches is not clear. In a few states, including California, Hawaii, and Illinois, the states referred to the use of ELE in their 2010 CHIP annual reports, implying that they defined their approaches as ELE, but did not have CMS-approved state plan amendments for ELE.
C. The Congressionally Mandated Evaluation of ELE
As the first major federal project to study ELE, the congressionally mandated evaluation of ELE offers an outstanding opportunity to (1) document the current state of ELE policy development and implementation; (2) assess its progress and potential for expanding coverage, reducing administrative costs, and creating a more streamlined enrollment process for families; (3) examine alternative approaches to streamlining the enrollment process and relate the associated benefits and costs to those of ELE; and (4) identify and share recommendations, best practices, promising approaches, and areas for improvement.
Mathematica, the Urban Institute, and HMA have designed the evaluation to consist of four independent but related studies:
Study 1 – Ongoing Assessment of the State Policy Context, via document review, quarterly interviews with state officials, and an all-state survey
Study 2 – Analysis of ELE Impacts on Enrollment using SEDS data
Study 3 – Case Studies of States Adopting ELE and Other Approaches to Streamlining Enrollment, including key informant interviews and focus groups with families
Study 4 – Descriptive Study of Costs, Enrollment, and Utilization in Case Study States
Each of these studies will feature its own design and draw on its own data sources, many of which will be available only through the substantial assistance of state agencies and state-level program stakeholders. However, the design of these studies will be coordinated to ensure that they benefit from one another and can be brought together in the two reports to Congress and other integrated reporting of findings.
Chapter II offers an overview of the evaluation design; Chapters III describes the TAG, whose comments will inform the design and the analysis of findings. Chapters VI to VII present the four studies: Chapter IV, the assessment of the state policy context; Chapter V, the analysis of enrollment data from SEDS; Chapter VI, the ELE and non-ELE state case studies; and Chapter VII, the study of costs, enrollment, and utilization. Chapter VIII describes how we will report on study findings, and Chapter XI explains how we will attain the necessary clearance from the Office of Management and Budget (OMB) and the necessary approval of an institutional review board (IRB) approval.
The organization of this report differs from the task structure proposed in ASPE’s request for proposals (RFP) in order to reflect the intellectual and operational structure of the evaluation. For ASPE’s convenience, Table I.2 maps the evaluation tasks, as specified in the RFP, to the four studies that make up the evaluation and to the chapters of the design report. Table I.2 also indicates major changes to the evaluation design relative to the RFP. The remainder of the report will describe the current design without ongoing references to the RFP task structure or other aspects of the RFP.
A second volume presents our work plan, including the organizational chart of our proposed team and a detailed scheduled of the timing of tasks and project deliverables. We have designed our management plan to coordinate closely with ASPE to ensure that our team meets the CHIPRA requirements for the congressionally mandated evaluation of ELE. The work plan does follow the task structure defined in the RFP.
Table I.2. Mapping of RFP Tasks to the Evaluation’s Four Studies and Chapters of the Design Report
RFP Task Number |
RFP Task Description |
Evaluation Study |
Chapter of Design Reporta |
Major Changes to Design Relative to RFP |
1 |
Initial Meeting |
|
Volume II Only |
|
2 |
TAG |
|
Chapter 2 |
|
3 |
Work Plan |
|
Volume II is the work plan |
|
4 |
Analysis of the Statistical Enrollment Data System |
Study 2 |
Chapter 5 |
Add a second round of SEDS analysis in Year 1 |
5 |
Data Collection Instruments/OMB |
|
Chapter 9 |
|
6 |
ELE Program Cost and Enrollment Data Collection/Analysis |
Study 4 |
Chapter 7 |
Add
a second round of analysis of ELE states’ cost and
enrollment data in Year 2;. |
7 |
ELE Program Case Studies |
Study 3 |
Chapter 6 |
Reduce the number of ELE case studies from 10 to 8 |
8.1 |
Information Review |
Study 1 |
Chapter 4 |
|
8.2 |
State Tracking and Monitoring |
Study 1 |
Chapter 4 |
|
8.3 |
Case
Studies (in non-ELE states) |
Study 3 |
Chapter 6 |
Reduce
the number of ELE case studies from 10 to 6; |
8.3 |
Analysis of enrollment trends and collection of cost and enrollment data in Non-ELE States |
Study 4 |
Chapter 7 |
Design for non-ELE cost and enrollment analysis is in Chapter 7; add financial compensation for participating states (as in the ELE states) |
8.4 |
51 State Survey |
Study 1 |
Chapter 4 |
|
9 |
Recommendations |
|
Chapter 8 |
|
10 |
Reports to Congress |
|
Chapter 8 |
|
11 |
Study Briefings |
|
Chapter 8 |
|
12 |
Deliver Data and Programs |
|
Volume II only |
|
13 |
Progress Reports |
|
Volume II only |
|
a All tasks are discussed in the work plan, Volume II, of this report, which is organized according to ASPE’s task structure.
II. overview of the evaluation design
The goals and design of the evaluation aim to give Congress, the U.S. Department of Health and Human Services (HHS), and state policymakers the necessary basis for making decisions on the use, design, and implementation of Express Lane Eligibility (ELE) and other non-ELE efforts aimed at streamlining the enrollment and/or retention process for public health insurance. In addition, the evaluation develops broader implications, notably those that pertain to the Medicaid expansions authorized by the Affordable Care Act.
The evaluation is framed around two broad goals and, within each of these goals, the major research questions specified in the request for proposals (RFP):
Goal 1: Describe ELE implementation, evaluate its benefits, assess ELE best practices, and make recommendations. Focusing on the subset of states that have implemented ELE as of June 30, 2011, the evaluation will examine how states are adopting ELE and the extent to which it has expanded coverage and affected administrative costs. The evaluation will also examine the potential benefits of, and barriers to, ELE in states that have not yet adopted it; the extent to which specific models might be most effective; and how ELE approaches can be improved, through changes at the federal level and through state policy and practice. The upper panel of Table II.1 shows questions addressed as part of this first goal.
Goal 2: Describe the adoption of alternative (or complementary) approaches to ELE, evaluate and compare their potential benefits, and assess best practices. Drawing on the experience of several states that have pursued alternatives to ELE for simplifying or streamlining enrollment or otherwise reaching and enrolling eligible but uninsured children, the evaluation will document alternatives, how they have been implemented, and their relative success in expanding coverage and reducing administrative costs. The evaluation will emphasize alternative approaches to streamlining and automation, such as online applications or data-driven approaches. The lower panel of Table II.1 shows questions addressed as part of this second goal.
As mentioned earlier, to meet these goals and address the research questions, the evaluation will consist of four independent but related studies:
Study 1: Ongoing assessment of the state policy context. Together, the three components of this study catalog the various approaches that states are using for outreach, enrollment, and retention, as well as state officials’ and others’ assessments of the impacts of these strategies in terms of enrollment, administrative costs, burden on families and other factors. They create a foundation of knowledge, a point of departure for other studies, and assist in the interpretation of other studies’ findings. The first component of the study is a comprehensive review of publicly available information, conducted early in the study. The second component is quarterly tracking in 30 states (almost all of the states that are not part of case studies), consisting of both ongoing document review and quarterly interviews with well-informed state officials. This tracking will enable the evaluation team to understand and assess ongoing policy developments in many states and to fill in any gaps in knowledge left by the information review. The final component is an internet survey of Medicaid/ Children’s Health Insurance Program (CHIP) directors in all 50 states and the District of Columbia. This survey will produce data on program characteristics and perceived impacts that can be readily compared among all 51 states and can be used to quantify the prevalence of various program features among states as well as perceptions regarding program impacts. The 2012 Interim Report to Congress will include results from the information review and early results from the ongoing document review; the 2013 Final Report to Congress will contain all results.
Study 2: Analysis of ELE impacts on enrollment using data from the CMS Statistical Enrollment Data System (SEDS). This study draws upon quarterly state-level enrollment data from the Centers for Medicare & Medicaid Services (CMS) for all 50 states and the District of Columbia in order to estimate the effects of ELE on Medicaid and CHIP enrollment. It uses the differences-in-differences methodology in which trends in non-ELE states are used to simulate the counterfactual, defined as what would have occurred in ELE states absent ELE, and therefore to estimate program impacts. Other policy and economic variables are entered into the estimating equation as controls. An initial analysis will be conducted for the Interim Report to Congress, and an updated analysis will be part of the Final Report to Congress. If these results are consistent with other evaluation findings, then they will represent rigorous evidence of a critical intended outcome of ELE.
Study 3: Case studies of states adopting ELE and other approaches to streamlining enrollment and/or retention. The case studies in eight ELE states offer rich detail on the design and implementation of ELE programs, including the perspectives of multiple stakeholders. The case studies pursue all the steps in program implementation, the motivations and expectations of participants, the barriers, and the unexpected outcomes. The case studies include both interviews with state officials, ELE partners, and other stakeholders as well as focus groups with families that can speak to their side of the enrollment process. A parallel set of case studies in six non-ELE states, selected for their innovative approaches to streamlining enrollment, will offer comparable insights into other strategies deemed particularly important to the Assistant Secretary for Planning and Evaluation (ASPE) and other evaluation audiences. A case study report will be prepared for each of the 14 study states, and the case studies, collectively, will be summarized in the Final Report to Congress.
Study 4: Descriptive study of costs, enrollment, and utilization in case study states. In ELE states, the cost study invites one or more informed individuals to map out the ELE process, compare it to the traditional enrollment/renewal process, and identify the potential for long-term cost savings from offering families an alternate pathway. At the same time, this study inquires about the fixed and start-up costs involved in establishing an ELE program. In non-ELE case-study states, the cost study is structured similarly but focuses on other strategies of interest. Costs and administrative simplification are also intended outcomes of ELE and related initiatives.
The enrollment studies in ELE states collect aggregate or individual-level data on enrollment by pathway to analyze (1) the numbers of children reached by ELE, (2) their demographic characteristics, and 3) their long-term enrollment outcomes. In the second and third cases, data on ELE are compared with parallel data for traditional pathways. Aggregate data are obtained from the states, whereas individual-level data can be obtained either from the states or from other centralized sources, such as MaxEnroll or the Medicaid Statistical Information System (MSIS).2 The first analysis offers a critical consistency check on the findings from the Statistical Enrollment Data System (SEDS) analysis regarding net new enrollment and hints at the potential of ELE to displace families that would otherwise have enrolled via other pathways; the second analysis sheds light on whether ELE reaches specific demographic groups; the third assesses a critical outcome. Again, parallel studies in non-ELE case-study states assess comparable topics for strategies of interest.
Finally, the utilization studies, in ELE states only, analyze individual-level data, obtained from MSIS, on spending for families enrolled via ELE and traditional pathways. Observed differences reflect both baseline differences in medical need between those who are reached by ELE and traditional means as well as any impact the pathway might have on use. (For example, ELE enrollees might not understand that they have health insurance or how to use it.) Despite this conceptual ambiguity, evidence of spending is critical to assessing the effect of ELE on state budgets.
The 2012 Interim Report to Congress will include cost results for six ELE states, aggregate enrollment results for four ELE states, and enrollment results based on individual data for two ELE states; the Final Report to Congress will offer updated cost results for up to eight ELE states (currently six ELE states operational as of December 31, 2010 are funded for this portion of the study, although if the evaluation has leftover funds we will discuss with ASPE using those resources for cost and enrollment studies in the other two ELE states approved as of June 30, 2011) and six non-ELE states, aggregate enrollment results for two additional ELE states and six non-ELE states, and both enrollment results and utilization based on individual data for four ELE states.
Table II.2 summarizes key characteristics of the four studies side by side. As Table II.1 shows, although these studies are distinct, the questions they inform cut across multiple sources. For example, every single data source will contribute to our understanding of the enrollment effect of ELE and other streamlined pathways. The cross-cutting nature of these questions underscores the importance of coordinating and integrating the design and conduct of the four studies. Moreover, it underscores the critical need to synthesize findings across tasks in the reporting on the evaluation finding.
Table II.1. Evaluation Goals, Research Questions, and the Main Studies and Data Sources for Addressing Them
|
Study
1: |
Study
2: |
Study
3: |
Study
4: |
||||||||
Information Review |
Information Review |
Quarterly Interviews and Ongoing Document Review |
51-State Survey |
|
Interviews |
Focus Groups |
|
|||||
Describe ELE implementation, evaluate its benefits, and assess ELE best practices and lessons for improvement |
||||||||||||
Does ELE raise enrollment? |
x |
x |
x |
x |
x |
x |
x |
|||||
Has ELE adoption facilitated readiness for the upcoming Medicaid expansion? |
x |
x |
x |
|
x |
|
x |
|||||
What are the administrative costs or savings from ELE programs? How do these costs and savings related to those from other approaches or processes to streamline enrollment? |
x |
x |
x |
|
x |
|
x |
|||||
What are recommendations for legislative or administrative changes to improve ELE? |
x |
x |
x |
|
x |
x |
|
|||||
What ELE practices proved most effective in enrolling and retaining children in Medicaid and CHIP? |
x |
x |
x |
|
x |
x |
|
|||||
What barriers to enrollment and retention remain? |
x |
x |
x |
|
x |
x |
|
|||||
Describe alternative approaches to creating streamlined pathways, evaluate their benefits, and assess best practices |
||||||||||||
What other approaches or processes do states have in place for outreach and to streamline enrollment? |
x |
x |
x |
x |
x |
|
|
|||||
How do they compare to ELE? |
x |
x |
x |
|
x |
x |
x |
|||||
Enrollment? |
x |
x |
x |
|
x |
x |
x |
|||||
Facilitating readiness for expansions? |
x |
x |
x |
|
x |
|
|
|||||
Administrative costs and savings? |
x |
x |
x |
|
x |
|
x |
|||||
What are best practices for outreach and to streamline enrollment? |
x |
x |
x |
|
x |
x |
|
|||||
Table II.2. Key Characteristics of Evaluation Studies and Data Sources
Study and Data Source |
Mode |
States |
Topics Emphasized |
Study 1: Ongoing Assessment of the State Policy Context |
|||
Baseline Information Review |
Comprehensive review of publicly available information |
All states |
Baseline information on program design, implementation, and impact |
Ongoing Document Review |
Periodic document review focusing on state-specific sources and issues |
30 selected states |
Program design, implementation, and impact—emphasis on changes over time |
Quarterly Interviews |
Quarterly interviews with informed state officials |
30 selected states |
Program design, implementation, and impact—emphasis on changes over time as well as gaps in knowledge |
51-State Survey |
Internet survey with open- and closed-ended items answered by Medicaid/CHIP directors and their staff |
All states |
Comprehensive census of states’ approaches to enrollment and renewal as well as perspectives on other evaluation topics |
Study 2: Analysis of ELE Impacts on Enrollment Using SEDS Data |
|||
Data from CMS’ Statistical Enrollment Data Systems (SEDS) |
Administrative data on enrollment from CMS |
All states (repeated in Years 1 and 2) |
Net enrollment impact of ELE or other approaches or processes to simplify enrollment |
Study 3: Case Studies of States Adopting ELE and Other Approaches to Simplifying Enrollment and/or Retention |
|||
Key Informant Interviews |
Key informant interviews with state officials, program partners, and other stakeholders |
8 ELE 6 non-ELE |
In-depth information on program design, implementation, and impact |
Focus Groups |
Focus groups with parents of children enrolled via ELE in ELE states and with parents of children enrolled via other simplified pathways in non-ELE states |
2 groups in each of 8 ELE states 2 groups in each of 4 selected non-ELE case study states |
Families’ experience with ELE and traditional enrollment approaches, in ELE states Families’ experience with alternate and traditional enrollment approaches, in non-ELE case study states |
Study 4: Descriptive Study of Costs, Enrollment, and Utilization in Case Study States |
|||
Costs |
Guided discussion with knowledgeable officials using a recording form |
6 ELE states with programs as of December 2010 (Years 1 and 2) 2 additional ELE states (funds permitting) and 6 non-ELE case study states (Year 2) Total: 6 to 8 ELE states and 6 non-ELE case study states |
Total costs of ELE/non-ELE simplification program Per-application costs of ELE/non-ELE simplification versus traditional pathways |
Aggregate Enrollment |
Administrative data gathered directly from states or from centralized sources |
4 ELE states with programs as of December 2010 (Year 1) 2 additional ELE states (funds permitting) and 6 non-ELE case study states (Year 2) Total: 4 to 6 ELE states and 6 non-ELE case study states. |
Net enrollment impact of ELE/non-ELE (total and by demographic group) Numbers enrolled via ELE/non-ELE pathways Baseline characteristics of ELE/non-ELE simplification versus other enrollees |
Individual-Level Enrollment |
Administrative
data |
2 ELE states (MaxEnroll Year 1) 4 ELE states (MSIS Year 2) Total: 6 ELE states |
Same as aggregate enrollment Plus, enrollment outcomes of ELE/non-ELE simplification versus other enrollees |
Utilization |
Administrative data (MSIS) |
4 ELE states (MSIS) (Year 2) |
Baseline utilization of ELE versus other enrollees (ELE renewals only) First-year utilization of ELE versus other enrollees |
a Most primary data collection will touch on all evaluation topics. This column highlights the distinctive focus of each study.
In carrying out the evaluation, we will address several challenges that cut across studies. They include:
Attributing observed changes in enrollment or administrative costs. Even when enough data are available to measure changes in key outcomes such as enrollment and administrative costs, a further challenge arises in attributing these changes to ELE (or other approaches) with a high degree of confidence. Often, for example, the adoption of policies such as ELE can arise simultaneously with other important policies or procedures that, in turn, risk confounding any estimates of ELE effects. In addition, many external and perhaps unobserved changes, such as shifts in economic conditions or changes in the private insurance market may affect Medicaid/CHIP enrollment patterns and further confound estimates of ELE effects. Not all children enrolled via ELE represent new enrollment. Some of these children might have enrolled via another pathway had ELE not been in force.
We will address this challenge via triangulation of multiple data sources. For example, the finding that ELE increases net enrollment in a state will be most convincing if it is observed in both the SEDS and in other enrollment data; if net enrollment gains are concentrated in the populations most likely to use ELE; and if participants in case studies, interviews, and the survey report a consistent story. When findings from various sources are inconsistent, we will probe for answers via additional data analyses or follow-up questions to the extent possible.
Minimizing burden on states and other stakeholders. Central to Studies 1, 3, and 4 is large-scale data collection across multiple states, combining primary data (such as stakeholder interviews and focus groups) and secondary data (such as acquisition of enrollment and cost data). This effort will place a significant burden on the study states, particularly the states that will be part of the cost, enrollment, and utilization study, which requires access to detailed data. Recognizing this burden, we plan to make significant payments to each participating state and will be able to increase these payments if documented efforts exceed our intended payment amount. In addition, we will leverage existing data when possible and only request that states provide data when we cannot access it independently. Finally, as described next, we will ensure linkages across study activities to avoid duplicate requests or asking the same question twice. Still, the evaluation must be careful in all states to balance the study’s data collection needs with the demands they place on state personnel.
Ensuring coordination among studies. In the final reporting, findings from the different analyses must be linked to address research questions as rigorously and thoroughly as possible and to use ASPE and state resources efficiently. We will ensure this coordination in several ways. First, to the extent feasible, we will use a common topical structure across study protocols and interim reports. Such a structure tends to focus the evaluation and makes it easier to integrate findings. Second, we plan to feature key staff across multiple studies to maximize the consistency of our approach and facilitate the synthesis of lessons learned. For example, the task leader of the cost and enrollment study will also be part of the case study team in non-ELE states. Some staff will conduct both ELE and non-ELE case studies, which will improve our ability to compare and contrast ELE versus non-ELE experiences. Third, we will maintain an internal library of study documents (data collection instruments for case studies and interviews, recording forms, case study reports, and documents identified in the information review) catalogued by state. Researchers will review relevant documents before embarking on site visits, interviews, and other discussions with states.
This page has been left blank for double-sided copying.
III. The Technical Advisory Group and its role in the evaluation
Purpose of the TAG
The technical advisory group (TAG) was formed to help guide the design and execution of the congressionally mandated Express Lane Eligibility (ELE) evaluation. The TAG will meet four times over the course of the evaluation to help the research team develop an effective and rigorous design, focus attention on the central policy issues, and assist in interpreting the evaluation’s findings.
TAG Member Selection and Recruitment
To maximize the potential value to the evaluation, TAG members were selected to represent a broad range of stakeholders and to bring diverse ELE perspectives and experiences to the table. Using our knowledge of the relevant design issues to be addressed by the group, we developed and submitted a list of potential TAG members as part of the project proposal. We sought candidates who understood both the policy and operational issues related to ELE, such as enrollment systems, program simplifications, and Medicaid/Children’s Health Insurance program (CHIP) coordination. Potential TAG members were selected from four different strata: ELE state governments, non-ELE state governments, research/policy/advocacy organizations, and the federal government. We refined and expanded our original list with guidance and input from the project officers during the project kickoff meeting. The project officers helped us prioritize selections within each category and to identify potential back-up participants in case the original selection was unable to participate.
After reaching consensus on the list of desired TAG members, we drafted and sent a letter inviting each person to participate in the TAG. The letter described the background of the project and the purpose of the TAG, outlining the commitment needed and remuneration for the member’s assistance. Most of our first-round invitees accepted the invitation to participate in the TAG. If an invitee was unable to participate, we invited our previously identified back-up candidate.3 The list of TAG members appears in Table III.1.
Table III.1. TAG Members
Name |
Affiliation |
State Government Officials |
|
Lesli Boudreaux |
LACHIP
Director |
Gretel Felton |
Director,
Certification Support Division |
Table II.1 (Continued)
Name |
Affiliation |
State Government Officials |
|
Becky Pasternik-Ikard |
Deputy
State Medicaid Director |
Anita Smith |
Bureau
Chief |
Thought Leaders from Private/Nonprofit Sector |
|
Tricia Brooks |
Senior
Fellow |
Anne Dunkelberg |
Associate
Director |
Beth Morrow |
Director
of Health IT Initiatives |
Federal Government Officials |
|
Anne Marie Costello |
Technical
Director, Division of Eligibility, Enrollment and
Outreach |
Vivian Lees |
Branch
Chief, State Systems Support Branch, Child Nutrition
Division |
Jennifer Ryan |
Deputy
Director, Children and Adults Health Programs Group |
Benjamin Sommers |
Senior
Advisor |
C. Methods
Participation in the TAG entails three one-day meetings and one conference call. The first one-day meeting was held at Mathematica’s offices in Washington, D.C., on Wednesday, November 30, 2011. The TAG will reconvene via conference call in May 2012 to review the preliminary findings from the ELE-state cost and enrollment data analysis. The next in-person meeting will occur in November 2012 (week 58) at which members will discuss the progress of the evaluation, including preliminary findings. The final in-person meeting will occur in June 2013, at which we will discuss recommendations coming out of the project and the final report.
D. Initial TAG Meeting
The main topics of discussion during the initial TAG meeting included (1) evaluation objectives, key audiences, and potential challenges; (2) case studies in 14 states; (3) cost and enrollment analysis; and (4) state monitoring, tracking, and selection. The TAG engaged in a lively discussion and provided the evaluation team with valuable feedback and new ideas for consideration. Many of the TAG’s suggestions have been incorporated into chapters throughout this design report.4
E. Next Steps
In general, the TAG’s comments confirmed the overall emphasis and direction of the evaluation. At the same time, the TAG made a number of useful suggestions regarding (1) topics for case studies, quarterly interviews, and 51-state surveys; (2) data fields for the cost and enrollment studies; (3) potential criteria for selecting states as well as states to consider; and (4) how to both raise the quality of data collected and reduce burden on states. The TAG also showed a strong interest in the implications of the ELE experience for federal and state decisions related to the Affordable Care Act. We thus plan to develop recommendations that address, not only federal and state policy options for ELE implementation, but also the lessons ELE holds for successful implementation of the Affordable Care Act. The evaluation team considered all of these discussions when preparing this design report, and insights from the TAG, both major and minor, have been incorporated in the evaluation design.
This page has been left blank for double-sided copying.
IV. Study 1: Ongoing Assessment of the State Policy Context
The first study will document states’ policy context and progress in enrolling and retaining children throughout the evaluation and will consist of three coordinated activities: a baseline information review, tracking and monitoring in 30 states not selected for case studies, and a 51 state survey. Collectively, these activities will build a foundation of knowledge regarding states’ outreach, enrollment, and retention strategies and serve as a point of departure for other study components; for example, the information review will inform the selection of states for non-Express Lane Eligibility (ELE) case studies, and the quarterly data and 51 state survey findings will help inform the interpretation of quantitative data from the Statistical Enrollment Data System (SEDS) analysis. They will complement the case study reports and give us the context to understand what observations from case studies might apply to other states. The remainder of the chapter discusses each of the three components of the study.
A. Baseline Information Review
At the outset of the project, we are reviewing and synthesizing available research, analysis, and descriptive information from states; published literature; and the grey literature (for example, policy organizations and think tanks) to understand states’ experiences in identifying, enrolling, and recertifying eligible children in Medicaid and the Children’s Health Insurance Program (CHIP). Two resources with particularly high value because they cover all 51 states are those collected by the Kaiser Family Foundation, including an annual survey of Medicaid and CHIP eligibility and enrollment practices, and the CHIP Annual Reporting Template System (CARTS) data that states submit to the Centers for Medicare & Medicaid Services (CMS). In addition, the Robert Wood Johnson Foundation’s Maximizing Enrollment for Kids program (MaxEnroll) has generated detailed information about innovative practices in eight grantee states.
To carry out our search efficiently, we will first turn to the reputable sources that we know have published articles on the relevant topics, particularly the research partners’ own work. Second, we will use key terms to search Medline and the Grey Literature database, such as “enrollment—Medicaid and CHIP,” “simplification,” “streamlining,” and “renewal—Medicaid and CHIP.” We will search explicitly for “ELE,” as well as other related terms such as “outreach,” “ex parte,” and “data matching.” We will review the products in light of the project’s goals and synthesize the most useful information.
We will prepare a memo with the following elements:
States’ activities pertaining to outreach, enrollment, and renewal for Medicaid and CHIP, as well as the key contextual factors, such as number of eligible but uninsured children,
Summary of the research pertaining to the effectiveness of current outreach, enrollment, and renewal strategies,
Summary of the eight ELE state plan amendments,
Key findings and states to watch, with implications for the other work to be conducted as part of this project, and
Appendices with 51-state tables.
Already, components of the information gathered have been used for the technical advisory group (TAG) meeting.
B. State Tracking and Monitoring
The information review might raise questions or leave gaps in knowledge that would best be resolved via an interview. In addition, over the two years of the project, states’ plans and policies related to outreach, enrollment, and renewal strategies could change in response to shifting priorities and local needs, and in preparation for health reform. We will enhance and maintain our knowledge base by following 30 states closely throughout the project period. In those 30 states, we will stay abreast of state news sources, reading any new articles and tracking states’ web sites to see how their outreach, enrollment, and renewal policies might change. We will also have quarterly calls with a key informant in those states who is likely to be aware of changing policy and progress toward implementing any changes.
1. Selecting the 30 States
The study team, in coordination with the project officers, will identify 30 states for monitoring and tracking of key activities related to identifying and enrolling children in Medicaid, CHIP, and other publicly subsidized health insurance programs. The states will be diverse along a variety of dimensions, such as number of simplifications adopted as well as demographic characteristics.
At the initial TAG meeting, discussed in Chapter III, we shared a table that arrayed states by various features tied to children’s enrollment and retention and asked advisors to identify any additional factors that should be taken into consideration in selecting states, such as innovations in enrollment or renewal not captured in existing documents. Using the table as a guide, the TAG broadly recommended that we select states that are both highly and less active in pursuing simplifications. The TAG also recommended we select a mix of states with high and low numbers of uninsured children. TAG members made some further, more specific recommendations on states to select, pointing to the value of using states already participating in other studies, which could facilitate low-cost access to data. These recommendations will be reflected in the list of states that we will submit to the project officers as the first milestone to this activity.
We also discussed with the TAG the value of including the case study states, both ELE and non-ELE, in the quarterly calls. Many TAG members agreed there would be value to having ongoing contact with these states (presumably selected because they are the states of greatest interest/the most to learn from their experiences). However, upon further consideration, we identified three reasons that the 30 states exclude all of the 14 case study states. First, we have an overarching concern about burden on participants. We are already asking all states to participate in an online survey; to ask a subset of 14 states to participate in an additional case study, a quarterly call focused on ELE and simplification issues, and the cost and enrollment study, seems burdensome and would pose a formidable hurdle for securing Office of Management and Budget (OMB) clearance. Second, we cannot envision a way that the case study protocols and the quarterly monitoring call protocols could be mutually exclusive and still gather the data necessary for understanding the pertinent issues. Thus in the case study states, the quarterly call would seem duplicative of the information we gather on site (and vice versa). Third, and perhaps most importantly, it expands the number of states on which we will gather information: by excluding the 14 case study states and focusing the quarterly calls on 30 separate states, our study will gather in-depth information on 44 states. We think this advantage—of gathering more on-the-ground data from more states—is beneficial in trying to understand the evolution of state policies regarding enrollment and retention simplification and the outcomes of related policy changes. Given this approach, identifying the 30 states for quarterly calls will, in some ways, become a process of identifying which 7 states we will not collect data on. This is likely to be an easier task, given some states have adopted few simplifications and are not considered innovators when it comes to CHIP enrollment and retention. However, the TAG did point out that the 30 states may “self-select,” as some among the 30 selected states may decline to participate, and so we may need to dig into those 7 remaining states as back-up states.
2. Selecting Key Informants
Because resources permit only a single respondent per state in the quarterly calls, we plan to focus these interviews on those who would be best informed and have the most accurate information about state policy decisions. Thus, our targets in states will be a government official with responsibility for developing and implementing enrollment and renewal policy. This might be the state Medicaid or CHIP administrator, eligibility policy director, or another high-level health policy official who has been directed to lead this work. We maintain a list of Medicaid and CHIP directors and will use this as a starting point for identifying our interviewees together with our knowledge of the states, the focal point of eligibility and enrollment activity, and recommendations from others in the state.
We appreciate the value in bellwether or alternate approaches, which might seek respondents with broader perspectives on health policy or individuals outside government; however, in our experience, these approaches work best when the resources exist to interview multiple respondents in a single state, enabling us to cover all topics with many respondents and to triangulate the information to be sure of what is factual and what is subjective. After discussion, ASPE officials agreed with this approach. However, should state officials be unavailable or unwilling to participate, we agree that individuals outside government, such as representatives of organizations in the State Fiscal Analysis Initiative, might be acceptable alternatives. If alternatives are needed, we can discuss these with ASPE on a case by case basis.
3. Key Informant Interviews
Upon OMB approval of the interview protocol, we will recruit a key informant within each of the 30 selected states. We will invite the key informant to participate in the study and confirm his or her availability for quarterly calls. Initially, the first call is likely to be lengthy (up to one hour), but we anticipate that subsequent calls will be much shorter (on average, about 15 minutes), particularly because state policies and processes usually change more slowly than every three months.
The study team will email a short list of questions based on the approved protocol to the key informants before each call. We will tailor follow-up questions to each state’s policy context and will design them to learn about progress toward planning, implementing, and operating activities that identify and enroll eligible children, as well as efforts to measure administrative efficiencies and impacts on Medicaid and CHIP enrollment trends. The quarterly key informant interviews will enable the study team to obtain the following information from the 30 states:
Plans for developing new activities and policies that will improve identification and enrollment of children in Medicaid, CHIP, and other publicly subsidized health insurance programs,
Updates on progress of implementation efforts currently under way, including the identification of administrative or policy barriers, efforts to overcome them, and states’ perceived outcomes,
Any newly available findings related to measuring the impact of identification and enrollment activities that are in operational phase, and
Findings will be organized by state and by theme using an in-house database developed for this purpose. We will work with the full evaluation team to identify key themes and be consistent across interviews and case study components in describing state activities related to these topics. In this way, we hope to maximize the connections among all the evaluation components.
4. Quarterly Reports
The study team will submit a quarterly report summarizing the latest developments in each of the 30 states. We also will use the quarterly reports to inform the interpretation of the enrollment data from SEDS, to provide more context for all of the case study reports, and as part of the final syntheses produced. Because the first quarterly report will be due in March 2012, before OMB approval of the protocol, we will use only publicly available information in it, relying heavily on findings from the information gathering.
C. 51-State Survey
We will conduct a survey of Medicaid and CHIP administrators in all 50 states and the District of Columbia, which will do the following:
Identify and catalog outreach strategies used by states and supplement existing knowledge of states’ enrollment and renewal practices, beyond information captured in existing surveys,
Gather findings from states’ own analyses of the effectiveness and efficiency of these approaches,
Understand states’ perspectives on the value of ELE and non-ELE approaches, including determining the ongoing barriers to enrollment in ELE states,
Determine states’ views of the implications of their enrollment and retention strategies on the upcoming Medicaid expansion populations, and
Identify ways that ELE effectiveness could be improved
We will conduct the survey electronically, using a custom-designed internet-based survey running on a Dataweb platform. The survey will include questions with multiple-choice response options; branched questions (for example, depending upon answers, the respondent will be directed to particular follow-up questions or skip others); and an opportunity for the respondent to provide additional information, including statistics, in a comment box for several questions. The breadth of information might necessitate completing the survey in multiple sessions or by multiple respondents within the state agency; therefore, we will structure the survey instrument so it can be saved and re-opened by the same or a different individual.
To optimize state participation, we will send a personalized letter to each state Medicaid and CHIP director by email, including an explanation of the purpose of the survey and the manner in which findings will be used. This email message will include the Internet link to the instrument and our contact information in case the respondent has questions regarding the instrument. We will monitor the response site regularly and will send at least two follow-up emails to non-responders during the field period. The survey instrument web site will be available for four weeks after the second email. It is possible, if we have to make reminder calls to respondents, that we will keep the site live for a slightly longer period to increase response rates. Our experience with similar surveys indicates that this is likely the case, and we have planned for this contingency.
The structural design of our survey in Dataweb will enable us to compile responses in a database. We will then review, clean, and analyze the data to determine themes and other findings relevant to key research questions. We will focus on key themes from other components of the study, including strengths and weaknesses of current approaches and considerations for new policies. We will compile and analyze the survey responses, looking for patterns and trends (for example, program-level trends, with certain responses more likely among CHIP than Medicaid directors or vice versa; policy trends that might vary along geographic or other lines; and so on), with a draft memo of findings submitted to the project officers. We will address feedback from the project officers and make revisions within one week of receiving the comments. We will use these findings to develop recommendations and to give input to the team. Findings will be incorporated into the Final Report to Congress.
We are mindful of the time frame requirements associated with this survey and of the need for OMB clearance, which could require 120 days or more. To maintain this schedule, we will provide a draft of the survey instrument and personalized letter template by January 20, 2012, as agreed at the initial meeting. Upon receipt of comments from the project officers, and other reviewers as appropriate, we will immediately revise the clearance package for ASPE’s submission to OMB. We will make additional revisions as necessary for final approval, based on comments received from both the general public and OMB during the clearance process.
This page has been left blank for double-sided copying.
V. Study 2: Analysis of ELE Impacts on Enrollment (Using SEDS)
The analysis of the Statistical Enrollment Data System (SEDS) offers a rigorous assessment of the effects of Express Lane Eligibility (ELE) on Medicaid and Children’s Health Insurance Program (CHIP) enrollment in time for the Interim Report, with an expanded and updated analysis to follow in the Final Report. Using Medicaid and CHIP enrollment data readily available for all states through the SEDS data system, the analysis will begin with a descriptive component comparing Medicaid and CHIP enrollment trends in ELE states with those of non-ELE states. This component will help identify any obvious spikes and changes in the enrollment before and after ELE in the adopting states, in addition to any similar change in non-ELE states. Building on this component, we will conduct a rigorous assessment of ELE’s impact, using the trends in the non-ELE states as a formal counterfactual against which to assess the gains in the ELE states and their causal links to ELE adoption. This causal assessment will rely on multivariate models to account for possible confounding policy changes or trends in ELE states that could be driving Medicaid/CHIP enrollment gains and might otherwise be incorrectly attributed to ELE adoption.
Through the descriptive and multivariate components, the analysis of SEDS will address three primary questions:
Does the implementation of ELE have a positive effect on Medicaid/CHIP enrollment? If so, how large are the enrollment gains? Are any positive enrollment impacts one-time increases, or are they sustained over time?
Are enrollment effects robust with respect to the type of ELE implemented?
Are differential effects found for Medicaid enrollment as opposed to CHIP enrollment?
In this chapter, we review the data sources for the study, our analysis plans, the key challenges to this work, and our plans for addressing those challenges.
Data Sources
SEDS data. SEDS is a web-based system maintained by the Centers for Medicare & Medicaid Services (CMS) to collect Medicaid and CHIP enrollment data from states on a quarterly basis since 2000. States must submit quarterly enrollment data within 30 days of the end of the quarter and aggregate annual data within 30 days of the end of the fourth quarter. This analysis will use quarterly and annual data from three of the SEDS reporting forms:
Form CMS-21E. This form collects data on children enrolled in separate child health programs.
Form CMS-64.21E. This form collects data on children enrolled in Medicaid expansion CHIPs—that is, Title XXI-funded Medicaid coverage.
Form CMS-64EC. This form collects data on children enrolled in the Medical Assistance Program—that is, Title XIX-funded Medicaid coverage or “traditional Medicaid.”
We will use the unduplicated counts of new enrollees during the quarter as the core enrollment measure for the SEDS analysis. New quarterly enrollees are defined as children who enrolled in the program at any time during the quarter and who were not enrolled in the program as of the last day of the previous quarter. We will also explore using, as a sensitivity test, the unduplicated number of children ever enrolled during the quarter or year.
Figure V.1 shows a snapshot of the 2010 Form 21E Quarterly Enrollment Report for children enrolled in separate child health programs only. States without separate CHIP programs, such as Maryland, have zero enrollment levels in this form. To create a combined CHIP enrollment variable, we will combine Form 21E data with Form 64.21E data. Some quality issues are evident in the SEDS data, including missing observations and likely reporting errors. For example, in Figure V.1, we see potential reporting error across quarters in states such as Connecticut, New Jersey, and Washington. In addition, the zeros in the table could indicate “not applicable” (for example, the state does not have a separate CHIP program) or a missing value within a given cell.
We will address these quality issues by imputing missing values and correcting reporting errors identified by examining growth rates in the quarterly and annual data and conducting outlier analyses. We will also consider following procedures that Mathematica has developed for working with these data (Ellwood et al. 2003). Based on an initial assessment of SEDS, it appears that reporting quality has increased; but that quality decreased the further the data were disaggregated. For example, states are unlikely to report a missing value for a single annual enrollment number, but are more likely to report at least one missing value for a quarterly enrollment number within a given year. For this reason, we will conduct both annual and quarterly analyses to determine the extent to which reporting error biases the results and will assess the sensitivity of estimates to the choice of initial data year.
Figure V.1. Snapshot of the 2010 Form 21E Quarterly (SEDS) Enrollment Report
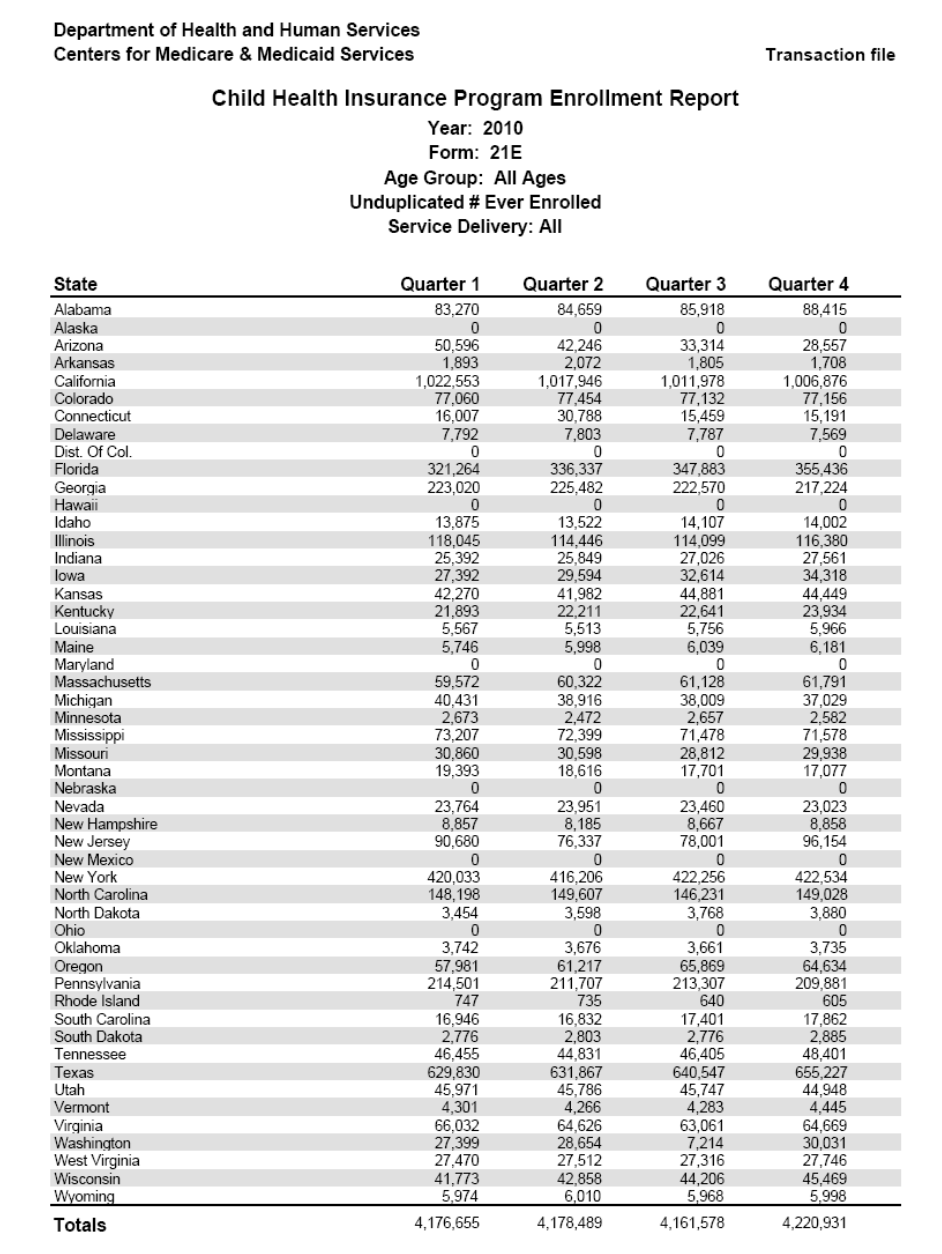
Additional data. The proposed multivariate (causal) analysis will account for many variables (such as changes in economic conditions or the adoption of various non-ELE policies) that might otherwise bias the estimates of ELE’s effects. To construct these variables, we will draw on a number of data sources:
State Medicaid eligibility rules for childless adults, parents, and children from the Urban Institute’s Medicaid eligibility simulation model and the Kaiser Family Foundation
State unemployment rate data from the Bureau of Labor Statistics
State demographic and population characteristics, such as income, from the U.S. Census Bureau and the Current Population Survey
Implementation dates of various state policies that influence the ease of new enrollment into Medicaid or CHIP (for example, presumptive eligibility, joint applications for Medicaid and CHIP, administrative verification of income, auto-renewal, and elimination of in-person interviews). We can obtain the year of implementation from publications from the Kaiser Commission on Medicaid and the Uninsured and the Georgetown Center for Children and Families. However, we will have to conduct additional analyses (which might involve additional document review) and follow up in particular states to determine the month or quarter of policy implementation. We will select the final policy covariates based on the number of program changes observed during the period of analysis to ensure sufficient degrees of freedom.
Analysis
At the start of the analysis, we will investigate the ELE policies that have been implemented to gain a sense of when they began to have a practical impact and to further understand how ELE alters Medicaid and CHIP enrollment patterns to help us model the ELE variable(s). This investigation will draw upon the project’s information review and might involve discussions with other experts on the team, outside government, and at ASPE.
For the descriptive component, we propose using an extensive time series of SEDS data to analyze Medicaid and CHIP enrollment trends among the ELE states compared with the non-ELE states. We will explore using data as far back as 2000 to obtain a robust trend, but we will pay particular attention to the quarterly data from 2007 onward. The more recent data enable us to see any noticeable spikes in Medicaid or CHIP enrollment among the states that implemented ELE during this period. One-time spikes provide descriptive evidence that ELE affects the overall stock (for example, shift in the intercept) of Medicaid/CHIP enrollment, whereas a change in the trend offers descriptive evidence that ELE has a more lasting effect on enrollment (for example, change in the slope). We will also produce data tables and graphs to illustrate these spikes and trends and will explore conducting analyses disaggregated by income group, age group, and delivery system type to assess variation in impacts across subgroups. However, as discussed earlier, disaggregated SEDS data are more prone than the aggregated data to reporting error and high rates of missing values, a limitation that will be well documented in our tables and any related findings.
In combination with other components of this project (for example, case studies), the multivariate analysis will assess more formally whether or not there is a causal link between ELE and any enrollment gains observed in the descriptive component. Central to this component will be the estimation of the following linear model:
where
 is
the intercept term, i is an index for state, t is an
index for time period (either year or quarter, going as far back as
2000),
is
the intercept term, i is an index for state, t is an
index for time period (either year or quarter, going as far back as
2000),
 is
a set of state dummy variables (state fixed effects),
is
a set of state dummy variables (state fixed effects),
 is a set of time period dummy variables (we will also explore using
time and time-squared covariates), and
is a set of time period dummy variables (we will also explore using
time and time-squared covariates), and
 is a random error term. The dependent variable,
is a random error term. The dependent variable, ,
is the number of new Medicaid or CHIP enrollees in state i
during time period t. After we obtain the data, we will
conduct tests to determine the best functional form and explore
specifications of key variables.
,
is the number of new Medicaid or CHIP enrollees in state i
during time period t. After we obtain the data, we will
conduct tests to determine the best functional form and explore
specifications of key variables.
The key
independent variable of interest is
 ,
which is set to one when the observation is an ELE state and the
time period is during or after the ELE implementation date. This
variable measures the causal effects of ELE on the number of new
Medicaid or CHIP enrollees. By reaching out to Medicaid- or
CHIP-eligible but uninsured children who participate in other public
programs, we anticipate that new enrollee counts will be more
sensitive to ELE as opposed to total counts. In other words,
,
which is set to one when the observation is an ELE state and the
time period is during or after the ELE implementation date. This
variable measures the causal effects of ELE on the number of new
Medicaid or CHIP enrollees. By reaching out to Medicaid- or
CHIP-eligible but uninsured children who participate in other public
programs, we anticipate that new enrollee counts will be more
sensitive to ELE as opposed to total counts. In other words,
 >0
would provide evidence that ELE alters the flow of new enrollment
into Medicaid or CHIP. We will also interact the ELE variable with
the time period variables to test whether ELE has a one-time effect
or if the effect persists over multiple time periods after the
policy is introduced.
>0
would provide evidence that ELE alters the flow of new enrollment
into Medicaid or CHIP. We will also interact the ELE variable with
the time period variables to test whether ELE has a one-time effect
or if the effect persists over multiple time periods after the
policy is introduced.
We will also
test the effects of ELE on the overall number of Medicaid and CHIP
enrollees (not only new enrollees), estimate separate models for
Medicaid and CHIP enrollment, and explore functional forms for the
enrollment variable. To ensure accuracy of this variable, we will
determine if implementation lags or delays were associated with any
of the ELE implementation dates.
 is a series of variables that control for changes in state policy,
and
is a series of variables that control for changes in state policy,
and
 is a series of other state-level controls that vary over time and
that could influence Medicaid/CHIP enrollment levels (discussed
above).
is a series of other state-level controls that vary over time and
that could influence Medicaid/CHIP enrollment levels (discussed
above).
Compared with the simple descriptive comparisons, findings from this model offer far more rigorous evidence of the effects of ELE because they can control for many sources of potential confounding. First, and perhaps most importantly, the state fixed effects control for all time-invariant differences across states that may otherwise bias estimate ELE effects. This includes, for example, all differences that may exist in the policies/procedures or populations between the ELE and non-ELE states that remain largely stable over the time period of the study. In addition, it accounts for possible differences in how individual states may report their data into SEDS. For example, to the extent that some states include inter-program transfers in their new enrollment counts (while other may not), the state fixed effects can account for this difference, again to the extent that the transfers remains largely stable over time. Second, the time period fixed effects control for observable and unobservable differences across time periods and differences between pre- and post-ELE implementation time periods that again might otherwise bias estimated ELE effects. Third, by including indicators for other state policy changes and time-varying covariates, we can control for other factors that change over time that could also explain differences in aggregate Medicaid and CHIP enrollment numbers. As noted above, we anticipate drawing on a collection of sources to construct these covariates, including data from the Bureau of Labor Statistics and annual reports from the Kaiser Commission and the Georgetown Center for Children and Families that summarize the major application and renewal policies and procedures across all 50 states.
Challenges
As with any quasi-experimental impact analysis, unobservable factors might result in bias to our estimated ELE effects. Specifically, unless accounted for in our models, any factors correlated with the timing of ELE adoption that also affect enrollment might bias our estimates effects. For example, some states might have upgraded their information technology (IT) systems at the same time they implemented ELE, resulting in improved processing of applications and subsequent increases in enrollment. Barring any control for the adoption of this change, the estimated effect of ELE may be biased upward. In contrast, non-ELE states could be taking similar, but unobservable initiatives (to the researcher), that have a positive effect on Medicaid or CHIP enrollment. If this were the case, the estimated effect of ELE might be biased downward.
The threat of this bias underscores the importance of measuring well the other factors that might be driving enrollment in the state, particularly in states that have adopted ELE. This, in turn, underscores the value of revisiting the SEDS analysis later in the project, when we will have detailed case study data with which to identify such changes and control for them to the extent possible. We will also conduct a series of robustness checks to explore the consistency of the regression model’s parameter estimates. To the extent that these estimates display consistency, it strengthens the evidence provided by the original model specification and, thereby, the conclusions that can be drawn from the analysis.
One example of these checks will be to conduct statistical tests (for example, DFFITS or Cook’s Distance) to determine if any of the observations are outliers or if specific ELE states have a strong influence on the overall regression results.5 For instance, it is possible that some non-ELE states are not accurate counterfactuals to ELE states, as certain non-ELE states could experience time-varying economic or policy shocks that drastically alter Medicaid or CHIP enrollment. The outlier tests would detect which states experienced these shocks and when they occurred, helping the research team determine which event(s) could have altered enrollment. As a result, we might remove some non-ELE states from our model that do not serve as the best counterfactual to the ELE states. In addition, we will compare several model specifications to determine the robustness of the ELE parameter estimate. For example, we will compare the estimates from our fully specified model that includes all of our proposed control variables with estimates from a model that redefines key variables (for example, the current unemployment rate versus the unemployment rate lagged by one year versus the unemployment rate lagged by six months). We will assess whether or not the ELE parameter is robust across model specifications and to which specifications the results are sensitive.
Another major challenge for this analysis is the relatively short post-ELE period we will encounter at the time of the analysis. As indicated in the request for proposals (RFP), most of the ELE policies were approved in 2010 or later, and the final analysis for the SEDS data is due less than two years later, in spring 2012. We will rely on the quarterly SEDS data to obtain the longest possible window of post-ELE data over this period. However, as an extension to this year one analysis, we will update the SEDS analysis later in the second evaluation year and incorporate the findings into the final congressional report. By doing so, we can assess a much more substantial period of ELE performance in most states, enriching the statistical precision of the analysis and being far more able to detect effects of ELE, particularly those that might be modest in size or lagged. Components of the second year analysis are consistent with the year one work:
Imputing missing values and correcting reporting errors in the most recent SEDS data,
Using the updated SEDS file to analyze Medicaid and CHIP enrollment trends among the ELE states compared with the non-ELE states and updating data tables and graphs to illustrate spikes and trends in enrollment,
Updating the additional data (for example, state unemployment and demographic data) used to create covariates in the multivariate analysis,
Reestimating the multivariate regression models with updated data, and
Providing a summary of key findings from updated analyses.
Finally, any measured effects of ELE must be seen in the context of a policy that can vary widely in both its implementation and target population. This underscores the importance of assessing the effects of ELE within individual or small groups of states, as a way to best understand the models that are most effective. However, such an assessment can be difficult. For example, in our multivariate models, we can create multiple ELE policy variables, such as “ELE through the Supplemental Nutrition Assistance Program” and “ELE through other agency,” working with the project team to determine different and relevant ways to characterize the ELE policies. This analysis can provide separate estimates of the effects of various ELE models; however, there might not be enough statistical power and degrees of freedom to detect a difference between pre- and post-ELE enrollment levels for different types of ELE approaches. This limitation can be mitigated, however, through the analysis undertaken as part of the proposed extension to this analysis, which would include a longer time frame for ELE implementation and effects to be observed empirically. Although most policymakers expect ELE to have a positive effect on Medicaid or CHIP enrollment, it will be very challenging to detect significant changes given these statistical challenges.
This page has been left blank for double-sided copying.
VI. Study 3: Case Studies of States Adopting ELE and Other Approaches to Simplifying Enrollment and/or Retention
The case study component of this evaluation will provide contextual information critical to understanding the design and implementation of Express Lane Eligibility (ELE) programs and of other simplification initiatives in non-ELE states, as well as the persistent barriers or challenges to enrollment and retention across ELE and non-ELE states. This task hinges on our ability to collect information systematically and to organize information consistently within an analytical framework to develop an in-depth understanding of ELE and non-ELE program implementation, successes, and challenges. Case studies will be conducted in a total of eight ELE states and six non-ELE states.
The case study design has three primary data collection components: (1) document review, (2) key informant interviews, and (3) focus groups. During interviews and focus groups we will inquire about program design features that have and have not worked, persistent barriers states have faced, and opportunities upon which they have capitalized; we will also consider the implications of ELE programs for coverage expansions required under federal health reform. Such case study analysis will give policymakers a more nuanced understanding of state experiences with ELE implementation. Used in concert with the case study data collected in non-ELE states, these data will provide Congress with rich contextual information about the strengths, weaknesses, and effects of ELE and alternative state approaches to identifying, enrolling, and continuously covering children eligible for Medicaid and the Children’s Health Insurance Program (CHIP). The ELE and non-ELE case study teams will collaborate throughout to ensure the use of parallel approaches and consistency across the evaluation. We will conduct a training before the site visits with all ELE and non-ELE case study staff to ensure that all team members are familiar with the interview protocols and moderators’ guides and with the steps involved in planning and conducting the site visits.
In this section, we review (1) the design for the ELE case study states; (2) the design for the case studies in non-ELE states, focusing on the key ways in which the non-ELE case studies will differ from those in the ELE states; (3) the plans for analysis and reporting for both types of case studies; and (4) challenges and limitations to this work.
A. ELE Program Case Studies
Case studies and focus groups in ELE states will describe states’ eligibility and enrollment processes for Medicaid and CHIP, the factors that influence state policy choices in this area, and how ELE fits into overall strategies for identifying, enrolling and retaining eligible but uninsured children in coverage. By examining states’ experiences implementing diverse ELE programs and exploring whether and how ELE processes improve states’ ability to reach uninsured children, the case studies will generate unique findings that add richness and context to the interpretation of the evaluation’s quantitative findings. The three components of the ELE-state case studies include:
Review of documents, reports, and summary materials,
In-depth site visits in the eight ELE states, and
Focus groups in the same eight states with families of children whose eligibility was established or renewed through ELE methods.
1. Review of State Documents, Evaluation Reports, and Other Background Material
As a first step in our qualitative assessment we will draw on any documentation available on state ELE programs. These documents may include the following:
ELE state plan amendments
States’ annual reports to the Centers for Medicare & Medicaid Services (CMS) available through the CHIP Annual Reporting Template System (CARTS)
State correspondence with enrollees regarding Medicaid and CHIP eligibility, enrollment, and consent
Policy guidance materials and procedural manuals
Media releases (for example, news articles on receipt of CHIPRA performance bonuses)
In addition, we will draw on the institutional knowledge of the evaluation team members and their extensive experience with Medicaid and CHIP research. For example, highly relevant research projects that are currently underway include the congressionally mandated CHIP Reauthorization Act of 2009 (CHIPRA) evaluation of 10 States being conducted for Assistant Secretary for Planning and Evaluation (ASPE) by Mathematica and the Urban Institute; the Urban Institute’s evaluation of Louisiana’s ELE program conducted through the Robert Wood Johnson Foundation’s State Health Access Reform Evaluation (SHARE) program; the evaluation of CHIPRA Quality Demonstrations being conducted by Mathematica and the Urban Institute for the Agency for Healthcare Research and Quality and CMS; and the annual survey of state Medicaid directors on trends in Medicaid budgets, enrollment, and policy directions in eligibility, benefits, cost containment, reimbursement, and other issues, conducted by Health Management Associates (HMA) for the Kaiser Commission on Medicaid and the Uninsured.
Our review of state documents, evaluation reports, and background materials will enable the research team to develop an analytical framework of critical ELE design features, policy variations, and implementation issues. This framework will inform our preparation for conducting case studies and focus groups, solidify our understanding of states’ evolving program characteristics, and identify salient and emerging issues. The information gleaned from this review will also help us tailor our interview protocols to explore state-specific issues and ensure that we use valuable interview time efficiently.
2. Site Visits
We will conduct case studies in all eight states with ELE programs, obviating the need for a state selection process. We will develop a letter from ASPE for states that introduces the ELE evaluation, describes the case study component, and provides contact information for both ASPE staff and evaluation team members. We will provide the letter in draft form to our project officers, whose feedback will be incorporated into a final version. Upon approval from ASPE, the evaluation team will send the letters by email (a method that worked well in the ASPE-sponsored, congressionally mandated, 10-state CHIPRA evaluation currently underway) to all eight states, and follow this letter with a brief telephone call to state officials to introduce the study and secure state participation.
Protocol. The interview protocol is a critical tool for conducting high-quality evaluations within a case study framework. A carefully structured protocol permits discussion of a range of issues in a consistent and thorough manner across all interviews and sites while providing the flexibility to consider interesting issues as they arise. Potential topics and questions are listed in Table VI.1. We will develop a series of interview protocols tailored to each state’s environment and key informant type, organized into sections that correspond to the major topic areas for the evaluation, including the following:
Medicaid and CHIP program features
ELE policy development
ELE implementation
Outcomes of ELE program
Role of ELE in federal health reform coverage expansions
Lessons learned and best practices
Key informants. Key informant interviews represent the core activity of the site visit and will facilitate the gathering of in-depth information and insights from a broad range of system stakeholders at the state and local levels. As such, we plan to organize our time on site between each state’s capital and one local community (selected for driving proximity to the state capital and based upon recommendations from state officials of a locale with an eligibility determination office as well as advocacy groups and others we might interview about the program). We plan to interview the following types of key informants during our site visits, ensuring that all appropriate perspectives are represented:
At the state level, officials responsible for administering CHIP and Medicaid, including program directors, eligibility policy chiefs, and key staff involved with ELE design and implementation; Express Lane partner agency officials; key legislative staff, such as the chair of the state legislature’s health committee; and family and child advocates
At the local level, county social services administrators, frontline eligibility workers, local offices for Express Lane agencies, and community-based organizations involved with outreach and application assistance
Most interviews at the state capital will focus on ELE program design and implementation decisions and experiences. We expect to interview 15 key informants, on average, in each state. We will inquire about how programs and policies were established and implemented, challenges that were encountered, and innovations that were implemented to overcome these challenges. At the local level, our questions will focus on the actual implementation of the ELE processes, asking about the changes the program has introduced to consumers and in communities. Because a portion of the local-level interviews will occur in and around the state capital—for instance, at a community-based organization involved with outreach to the capital city’s residents—the state capital interviews will encompass both local- and state-level interviews. As requested in the request for proposals (RFP), we will submit the case study methodology and draft interview protocols to the federal project officer for review and approval as part of the project’s overall evaluation work plan; and all protocols will go through the Office of Management and Budget (OMB) clearance process.
Conducting the site visits. The site visit approach will follow a series of steps designed to ensure the systematic collection of information and data from a broad set of key informants. We will conduct the first site visit as a pilot to test the proposed case study methodology and interview protocols. Based on results from this site visit, we will make appropriate revisions to the methodology and implement them during the seven remaining site visits.
A team of two senior researchers and a junior analyst will conduct each three-day site visit: one senior team member will lead the site visit interviews, the other will lead the focus groups, and the analyst will take notes. On the pilot, the Urban Institute case study team will bring an additional senior researcher (from HMA) to observe and participate in the site visit. We have found this model advantageous on past site visits, as it enables a dedicated observer to hear the protocols delivered in person and to suggest refinements as needed. The two senior researchers/one junior analyst combination will conduct the remaining visits.
The specific steps we will follow to arrange and conduct our site visits follow:
Contact state officials. After emailing the letter from ASPE announcing the study, we will call key CHIP and Medicaid officials to discuss the goals and process of the case study, the types of organizations and individuals we would like to interview, potential communities to visit, and possible site visit dates. This task will secure the participation and support of key state officials.
Assemble state-specific background materials. As described previously, we will collect and review background materials pertinent to each state’s ELE program. Information and insights we garner will not only help us understand the program from the outset but also feed directly into our development of state-specific questions for our interview protocols (as opposed to the core questions, which we will develop and ask in all states).
Identify key informants and local sites. Working with state officials, we will identify the full complement of state agencies, policymakers, and child health advocates involved with Medicaid and CHIP program design, implementation, and monitoring. From this list we will select appropriate individuals and organizations to interview. We will also identify several local communities that might represent typical experiences in implementing ELE.
Establish site visit logistics. Working with state and local officials, we will schedule site visits lasting three days in each state, with roughly two-thirds of that time spent in the state capital (conducting interviews with state and local officials) and the remaining third spent in another local community. On each visit, we plan to conduct focus groups in the evenings (discussed later in this chapter).
Conduct interviews. We will conduct interviews with 15 to 20 respondents drawn from the above-mentioned groups (on average, we expect about 15 participants to be interviewed). The site visit team leader, a senior staff person, will have primary responsibility for asking questions and conducting necessary follow-ups to address evaluation goals; an accompanying junior analyst will have primary responsibility for note taking. (The third site visit team member will moderate the evening focus groups, allowing the team leader and analyst to observe and take notes.) Urban Institute will lead five of the ELE case studies, with HMA staffing the other three trips.
Compile notes. Upon completion of each site visit we will compile and clean the notes from each interview, in preparation for coding and analysis using Atlas.ti software. The consistent coding of notes will facilitate more systematic and rigorous analysis of the site visit notes.
3. Focus Groups
As part of the case studies, we will conduct two focus groups in each ELE state. We expect the focus group findings to enrich the other evaluation components in two key ways. First, they will bring the voices of parents and other family members into our evaluation reports to illustrate their experiences and enhance our understanding of concepts and issues identified through other components of the evaluation. Second, they will highlight particular focal areas for our analysis of the key informant findings. The specific steps we will follow to arrange and conduct our focus groups are described next.
a. Sample selection
We will hold two focus groups in each ELE state, one in the capital and one in the local site. Both focus groups will be held with parents of children who were enrolled or whose eligibility was renewed via ELE programs. Focus group participants’ comments will provide insights regarding how families learned of their child’s eligibility, how they consented to enrollment, what benefits they perceived coverage to offer, whether they were able to access services, and how they renewed their children’s eligibility.
We carefully considered alternative focus group designs—including those suggested by technical advisory group (TAG) members at their initial meeting—that would have involved parents of children enrolled or whose eligibility was renewed through another pathway (that is, parents without ELE experiences). However, because the primary aim of these groups is to understand families’ perspectives on ELE and to explore in depth a number of issues specific to this pathway, we decided that the best approach is one that maximizes the number of participants with ELE experiences. By holding two groups with parents of children who enrolled or renewed coverage via ELE, we have a greater assurance of sufficient input from these parents. On the other hand, if we limit groups with ELE experiences to just one per state, we run the risk of learning about ELE from only a handful of parents (for example, in the event that a group is more sparsely attended) and if we form a group of parents with mixed experiences (some with ELE, some without), we increase the potential for confusion among the participants and findings that are difficult to disentangle.
In recognition of the importance of understanding ELE as it relates to other enrollment pathways in each state, we will invite participants to compare the experience of ELE enrollment with any prior experiences they might have had enrolling in public programs (whether Medicaid or its ELE partner program) via traditional approaches or another pathway, if applicable. These within-person comparisons offer a useful way to assess, based on parents’ opinions, the relative strengths and weaknesses of ELE as an enrollment pathway. In addition, we will leverage information on non-ELE enrollment experiences collected via the 10-state CHIPRA evaluation project, which includes focus groups with parents of CHIP enrollees and disenrollees (some with Spanish-speaking parents).
There is always the possibility that states will have difficulty identifying children who enter via the ELE pathway, but given our experience conducting similar groups in Louisiana last year, as well as the initial investigative calls with six ELE states done for the cost and enrollment study, we are not anticipating this problem. Right now, the only state in which we are aware that this might be a problem is Maryland, which at least initially, has not been able to identify children who enter via the ELE pathway in the administrative data. However, Maryland also informed us that this is expected to change in 2012, when the Medicaid agency there will take over the mailings to those identified by the tax agency (currently, the state comptroller mails those applications and has not established a tracking system for them). Thus, even in Maryland, we expect this approach to work.
b. Moderator’s guides
As with key informant interview protocols, the focus group moderator’s guide is the critical tool for consistent and systematic information gathering. The guide will consist of a set of approximately 20 open-ended questions, organized and structured to address the research questions of interest. Each focus group will run up to 90 minutes (including time for gaining participants’ consent and reimbursing them for participation). Table VI.2 illustrates some of the critical issues that the guide will include, but each state’s guide will be tailored to the specifics of that state’s program. We will submit the focus group methodology and draft moderator’s guides to the federal project officer for review and approval as part of the project’s overall evaluation work plan, and the instruments will go through the OMB clearance process.
c. Recruitment
Groups of 8 to 10 participants are optimal for focus groups, but to ensure adequate participation (and account for likely no shows) we will recruit 12 people per group. Recruitment strategies will likely enlist the help of Medicaid, CHIP, and Express Lane agency staff to gain access to potential participants. We will ask Medicaid/CHIP program staff to generate two lists of children for focus group recruitment:
Children who enrolled or renewed in Medicaid or CHIP via ELE and reside in the state capital
Children who enrolled or renewed in Medicaid or CHIP via ELE and reside in the selected local community
We do not plan to screen participants based on whether the families understand that they were enrolled through ELE; we seek the perspectives both of those who know they were enrolled through this mechanism as well as those who do not know this. If we were to screen out those who did not know they were enrolled through ELE, we would potentially bias the results. There might be participants who do not know how they were enrolled, but know they were enrolled and are using services—indicating ELE is working seamlessly and leading to the desired outcomes. Likewise, it would be important to know if some enrolled through ELE do not know they are enrolled and are not using services. As discussed at the TAG, this is especially important to understand in states using a managed care delivery system, where the state or health plan pays a capitated amount regardless of service use.
Trained evaluation team members will telephone potential participants directly to solicit their interest in participating in our focus groups, following recruitment scripts that describe the purpose and process for the groups. Research staff will emphasize that participation is entirely voluntary. To help with recruitment, we will offer incentives (we have budgeted $50 per respondent as an incentive payment) and will provide light refreshments and child care during the groups. To avoid liability issues, we will contract with licensed child care providers in each state to provide the child care. Alternatively, to avoid liability altogether, we will consider using the budgeted amount for child care providers to instead offer a small stipend to participating parents for them to arrange their own child care in order to attend.
d. Conducting the focus groups
A senior member of the evaluation team skilled in leading focus groups will moderate the focus groups, which will last 1.5 to 2.0 hours. We will obtain written informed consent from all study participants before the focus groups begin. The moderator will be supported by the two other site visit team members, who will take extensive notes and digitally record the sessions. During the groups, we will discuss parents’ experiences with awareness and impact of outreach; enrollment experiences under ELE (such as how they found out their child was enrolled, given that they went through the ELE route); and if applicable, a comparison to enrollment experiences pre-ELE (if applicable), access-to-care issues, and parents’ impressions of the enrollment process. As described earlier, we will tailor the moderator’s guide to probe on specific issues related to each state’s unique ELE approach for the groups focused on ELE experiences.
We will analyze focus group notes (and code them into our Atlas.ti files) to support and further illustrate findings from the case studies and quantitative data analysis. We will refer to the digital recordings for quotes that illustrate a particular point; we will destroy all digital recordings at the end of the project.
Table VI.1. ELE Site Visit Interview Protocol Potential Topics and Questions
Potential Topic |
Potential Questions |
1. Medicaid and CHIP Program Features |
Please describe your state’s policies for CHIP and Medicaid related to eligibility criteria; outreach and marketing efforts; screening, enrollment, and renewal procedures; benefits and cost-sharing; service delivery and payment arrangements; and initiatives for special populations. |
2. ELE Policy Development |
|
3. ELE Implementation |
|
4. Outcomes of ELE Program |
|
5. Role of ELE in Federal Health Reform Coverage Expansions |
|
6. Lessons Learned and Best Practices |
|
Table VI.2. Potential ELE State Focus Group Moderators’ Guide
Potential Topic |
Potential Questions |
1. Outreach |
|
2. Enrollment |
|
3. Access to Care |
|
4. Affordable Care Act |
|
5. Lessons Learned |
|
B. Case Studies in Non-ELE States
Like the ELE case studies, non-ELE case studies offer additional nuanced information on program details and stakeholder experiences. The primary motivation for conducting the non-ELE case studies is to understand alternatives to ELE with similar potential to simplify the enrollment and/or retention processes. Most states have not pursued ELE, but many have implemented simplified approaches to try to enroll and retain children. Understanding these alternatives—and which show the most promise, in terms of cost and enrollment effects and potential for simplifying adults’ enrollment in 2014—is critical to helping guide policy recommendations about the best ways—ELE or other—states should proceed.
The six non-ELE case studies will follow the same general approach as the ELE cases studies (document review, in-depth case studies, and focus groups). However, the non-ELE case studies are distinct for three reasons: (1) because so many more states fall into the non-ELE category, we must develop a process for selecting six non-ELE states for intensive study; (2) we propose fewer focus groups in the non-ELE states than in ELE states, although we are proposing a consistent design as in the ELE states (that is, to select families who have entered through the pathway of interest in the non-ELE states); and (3) the non-ELE case studies involve collection of aggregate administrative cost and enrollment data, if it is available (in the ELE states, this data is collected outside the case studies; the design of the cost and enrollment study in both ELE and non-ELE states is reviewed in Chapter VII).
1. Selecting Non-ELE States
Given the project’s emphasis on best practices and on examining ELE in the context of other outreach and enrollment strategies, we will focus the non-ELE case studies on states that are thought to have adopted particular enrollment or retention simplifications and/or that are examples of outreach and enrollment strategies and approaches that are similar in nature to ELE but do not qualify as ELE programs, whether because the states have not applied for a state plan amendment or other reasons.6 In choosing states for the non-ELE case studies, we will seek examples of Medicaid or CHIP program simplifications that offer simplified enrollment or renewal for children. There are many types of approaches from which to choose; as discussed in the introduction, we have already identified many examples worthy of study, including online universal program applications, single portal models, community-based application assistance, and the use of administrative renewal processes (sometimes called ex parte renewal) in which the state uses information available to it from other databases to verify ongoing eligibility, among others. The U.S. Department of Health and Human Services (HHS), through its issuance of CHIPRA performance bonus criteria (focused on eight simplification policies) has also shown a preference for certain simplifications it views as important; although some of these are common among states (for example, eliminating the in-person interview, which 49 of 51 states have eliminated), we also will consider some of the less commonly implemented simplifications from among the eight, such as presumptive eligibility or auto-renewal procedures.7
We must be deliberate about selecting states with a particular intervention we can study, because we are trying to understand viable alternatives to ELE that help states enroll children and keep them enrolled. However, we also will seek to balance the sample across the other relevant dimensions. These will include some outcome variables, such as enrollment rates in public coverage, rates of uninsurance among low-income children, and whether the state received a 2011 CHIPRA bonus payment. Another indicators we will consider is whether the state considered, but did not apply for, an ELE state plan amendment (per the TAG’s advice that such states would help us garner important perspectives on ELE).
Another high-priority criterion for the study is selecting states that can identify children who entered through the particular pathway in their administrative data, both for the enrollment study and for focus group recruiting (discussed later). Thus, before submission of the state selection memo, we will investigate the expected quality of the state’s administrative data for use in a quantitative study of state approaches and for the focus groups. As discussed at the first TAG meeting, states with more recent systems improvements will have a better chance of being able to fulfill these requests.
We will summarize the list of the final selection criteria, how they were applied, and our final recommendations of non-ELE case study states in a memo to the project officers; this memo will also offer potential alternative states and the reasons to consider them in place of the proposed states. We will submit the final memo within one week after receiving comments from ASPE.
2. Focus Groups in Non-ELE States
In four of the six non-ELE case study states, we will also conduct two focus groups with families of children who have recently enrolled in public insurance through the non-ELE pathway of interest, for a total of eight focus groups in non-ELE states. Similar to the ELE states, we recommend that the non-ELE groups focus on families whose children have enrolled through the particular non-ELE pathway of interest being studied in each of the four states. After the six non-ELE states are selected, we will recommend four states in which the state selection evidence suggests the states employ outreach/enrollment interventions that might easily be replicated or that hold promise for easily enrolling large numbers of children (or adults beginning in 2014) and for which families can be identified in state records. After discussion with ASPE about the four recommended focus group states, we will finalize the recommended states and conduct the focus groups in those states.
Given the large number of possible alternatives to ELE we will have the opportunity to study across the non-ELE states, we expect to focus on a different alternative in each of the four states in which we will conduct focus groups. That means that we expect to conduct two focus groups in four states with four different approaches to simplification or outreach that we are trying to better understand. We have considered other approaches to the focus group design in the non-ELE states, such as conducting half of these focus groups with families whose children came in the pathway of interest and half with families whose children came in through any pathway. However, we decided against this approach because it dilutes our ability to say much about the particular pathway of interest with the resources available.8 Instead, we will use information gathered from focus groups being conducted as part of the congressionally mandated 10-state CHIP evaluation to understand other types of enrollment experiences in non-ELE states. That study, which includes 8 non-ELE states, is conducting focus groups with families with children (1) enrolled in CHIP or Medicaid, (2) disenrolled from CHIP or Medicaid, (3) eligible for CHIP or Medicaid but uninsured, and (4) covered under employer-sponsored insurance (ESI). Participants in those focus groups also will be asked about enrollment and outreach experiences; and the same teams are conducting the focus groups in both studies. We believe this represents a win-win situation for the ELE evaluation.
As in the ELE focus groups, recruitment strategies will enlist the help of Medicaid and CHIP agencies to gain access to potential participants. We will work with the state and its partners, as appropriate, to identify families to recruit; as noted, a key criterion for selecting the four states in which to conduct focus groups is that the state can identify participants who entered through the non-ELE pathway of interest. Given that we expect to study at least some states using technology-based simplifications—such as online applications or single-portal models or with particular outreach models in communities—we expect that states and outreach partners will be able to identify the clients of interest. It is possible that some states might not be able to identify such participants. If that is the case, we could discuss with ASPE an alternative design for consideration. For example, we could increase the number of focus groups in non-ELE states that can identify participants in their administrative data (conducting the non-ELE focus groups in fewer states but with the same total number of focus groups); conduct focus groups in the non-ELE states with those who entered through any pathway; or reallocate these focus group resources to the ELE states, to conduct additional focus groups in those states, among other possibilities.
For all groups, we will target families whose children were newly enrolled or renewed within the prior 6 to 10 months. This will provide relevant information about how families were identified for enrollment, why they enrolled, what benefits of coverage they perceived, whether they had accessed services, and if and how they renewed their children’s eligibility.
Table VI.3 provides a sample focus group moderator’s guide for the non-ELE states. The topics covered are the same as in the ELE states, but we have modified the questions as needed to address the differences in the issues in non-ELE states and in the target populations for these focus groups.
We will submit the focus group methodology and draft moderator’s guide to the project officers for review and approval as part of the project’s overall evaluation work plan; then the instrument will go through the OMB clearance process.
Table VI.3. Proposed Non-ELE States Focus Group Moderator’s Guide
Potential Topic |
Potential Questions |
1. Outreach |
|
2. Enrollment |
|
3. Access to Care |
|
|
|
4. Affordable Care Act |
|
5. Lessons Learned |
|
C. Analysis and Reporting
The case studies will draw on data from background materials, key informant interviews, and focus groups to construct a comprehensive assessment of each state’s ELE or non-ELE program. The analysis of case study data in preparation for report writing will involve a series of systematic steps to ensure our interpretation of findings is accurate and comprehensive.
We plan to use Atlas.ti, a software program designed to facilitate the analysis of qualitative data. The software helps to organize the large amount of qualitative information gathered from the different case study data sources so that we can identify and more readily analyze common themes and contrasting points of view. The primary structure for the coding scheme will build on the interview protocols for the site visits and on the moderator’s guide for the focus groups, along with the research questions the findings will inform. For the key informant interviews, the process will begin with a review of the clean version of the notes from the first two key informant interviews. A senior team member will construct a list of the topics and themes we want to capture with codes; other team members will review and add to this list as appropriate. In addition to coding topic areas and the content of responses, the coding scheme will include codes for different types of informants and different states. When the team comes to a consensus about the coding scheme, two trained analysts will code the key informant interview notes (that is, they will code the same notes from the first case study). A senior team member will review these two sets of coded notes for quality and consistency across the two coders. Inconsistencies in the coding will be discussed and resolved before the analysts code the notes for the remaining key informant interviews. The ELE and non-ELE site visit teams will share their coding schemes, with the understanding that the common issues identified in non-ELE states might differ from the findings in the ELE states. This will be an important step for developing the cross-state syntheses required for the Report to Congress.
We will use a similar process to code the notes from the focus groups, using the moderator’s guide as the basic structure for the coding scheme. We will create theme tables for each state, categorizing findings across the focus groups conducted in that state; this will enable us to compare and contrast results across the groups within each state. To ensure the coding is completed within the demanding time line for the case studies, and because the content of the key informant interview and focus group material will largely be distinct, we will have separate teams code the notes from the key informant interviews and the focus groups. When the coding process is complete, we will use Atlas.ti to sort and query the data by topic or theme so we can identify commonalities and differences across interview respondents.
This coding process will facilitate the analysis for individual case study reports and it will support the cross-cutting analysis for the final Report to Congress. Because of the diversity of ELE and non-ELE approaches and state Medicaid and CHIP programs, we will use Atlas.ti to facilitate key word and theme searches, which enables grouping portions of text for comparisons across states with different ELE approaches, among states that have adopted similar ELE approaches, and between ELE and non-ELE states using the data obtained through the non-ELE case studies. We will combine the ELE and non-ELE case study data and, using output reports generated from Atlas.ti, we will organize findings by theme and develop matrices that will help us synthesize and summarize evidence gathered from the key informant interviews and focus groups. This in turn will help in developing a cross-cutting report that illuminates commonalities and differences within the key research areas across states, program types, and types of informants.
The evaluation team will develop individual case study reports for each state, summarizing state-specific findings in a useful and readable manner. To facilitate later analysis, all state case study reports, including those for non-ELE states, will share a common outline. We will develop the outline as part of the design process, in conjunction with the protocols and analysis sheets, and in light of the design for the evaluation as a whole. We will then adapt the outline based on findings from the first ELE and non-ELE case studies. A member of the case study team will take primary responsibility for preparing each of these reports, with support from other team members and oversight by the principal investigators. This staffing strategy will enable the proposed research team to produce reports in a timely fashion. We will provide each report in draft form to our project officers on a rolling basis as we complete them and we will incorporate ASPE’s feedback into the final versions. We will also synthesize case study findings in a cross-cutting analysis that will be part of the evaluation’s final Report to Congress.
D. Challenges and Limitations
Qualitative methods of data collection provide textured and nuanced findings that other research methods are unable to capture; however, certain challenges are inherent to this method of inquiry. Most notably, sample size is a limitation that will affect the generalizability of the evidence gathered through interviews and focus groups. By their nature, key informant interviews and focus groups obtain information from a relatively small number of individuals and thus cannot be presumed to be representative of the entire population of interest. For key informant interviews, we will work closely with well-known contacts at the state and local levels to identify people and organizations that hold the greatest promise for providing us with exposure to a broad and representative group of stakeholders. Because we will be limited to conducting 15 to 20 interviews per state, we might inadvertently miss important individuals and/or perspectives. At the same time, this represents a total of 210 to 280 respondents across the ELE and non-ELE states, a large pool of respondents. Similarly, because we will speak with a relatively small number of parents in the focus groups, we must acknowledge that they might not be representative of families as a whole. The value of the qualitative data is that it provides context for ELE and non-ELE program design, implementation, and impacts on families across each state and in selected localities. Through cross-cutting analysis of these efforts, the research team will synthesize the data and identify common themes with regard to program implementation and perceived effects in as useful and generalizable a manner as possible.
vii. DESCRIPTIVE STUDY OF COSTS,
ENROLLMENT, AND UTILIZATION
IN CASE STUDY STATES
The cost, enrollment, and utilization study will include both Express Lane Eligibility (ELE) and non-ELE case study states and seeks to inform two broad policy issues: (1) the potential administrative efficiency of ELE and alternate approaches to simplifying enrollment relative to traditional processes and (2) the contributions of simplified approaches (ELE and non-ELE) to enrollment growth and to reaching eligible populations that have not been enrolled with existing methods. Within these two broad issues, the task will address a number of more focused research questions, as summarized in Table VII.1. Our approach to examining these questions will be largely descriptive, combining data from multiple states and for multiple measures to assess the potential contribution of simplified enrollment mechanisms to administrative efficiencies and to enrollment gains.
Table VII.1. Key Research Questions Addressed Through Program Cost, Enrollment, and Utilization Study
Analysis
of Costs and Cost Savings Under ELE and Alternate (Non-ELE)
Approaches |
|
What are the marginal and fixed costs of ELE and alternate non-ELE approaches to simplifying enrollment, relative to traditional processes? |
|
Analysis
of Enrollment and Retention Under ELE and Alternative (Non-ELE)
Approaches |
|
Have simplified approaches (ELE and non-ELE) to enrollment led to gains in Medicaid and CHIP enrollment? Is there evidence that simplified approaches (ELE and non-ELE) to enrollment attract a different group of families than traditional enrollment mechanisms? |
|
Do enrollees who enter through simplified approaches (ELE and non-ELE) to enrollment remain enrolled in Medicaid and/or CHIP? |
|
Analysis of Utilization Under ELE and Alternative (Non-ELE) Approaches to Simplifying Enrollment |
|
What types of services do children who enter through simplified approaches (ELE and non-ELE) to enrollment access?
|
|
The cost, enrollment, and utilization study will proceed in several phases, summarized in Table VII.2. The earliest phase will examine enrollment and program cost data for the six ELE states with programs effective as of December 2010 (Alabama, Iowa, Louisiana, Maryland, New Jersey, and Oregon), and the results will support the 2012 Interim Report to Congress. In the second year of the evaluation, we will update the cost analysis, conduct additional enrollment analyses using individual-level data, and when possible, examine the service utilization patterns of ELE enrollees. We will also conduct cost and enrollment analyses in the non-ELE states selected for case studies and, if sufficient funds remain, will extend the analysis to include Georgia and South Carolina, two states with recently approved ELE processes. The remainder of this section provides additional detail for each analysis, beginning with those planned for ELE states and then addressing non-ELE states. We have included our finalized data collection tools, which incorporate comments received from the Assistant Secretary of Planning and Evaluation (ASPE).
Table VII.2. Summary of Analyses Completed Under Program Cost, Enrollment, and Utilization Study
|
Study
Year 1 |
|
Study
Year 2 |
|
|
ELE States |
ELE States |
Non-ELE States |
|
Cost Analyses |
Six states with programs as of December 2010: Alabama, Iowa, Louisiana, Maryland, New Jersey, and Oregon |
|
Update in study Year 1 states and (if funds are available) new analyses in South Carolina and Georgia |
All six case study states |
Enrollment Analyses |
Iowa, Maryland, New Jersey, and Oregon: Demographics and retention outcomes analyzed at the aggregate level Alabama, Louisiana: Demographics and retention outcomes analyzed with individual-level data (MaxEnroll) |
|
Update in Study Year 1 states: Demographics and retention outcomes analyzed with individual-level data (Medicaid Statistical Information System [MSIS] or from states) South Carolina and Georgia (if funds are available): Demographics and retention outcomes analyzed at the aggregate level |
All six case study states: Demographics and retention outcomes analyzed at aggregate level |
Utilization Analyses |
|
|
Alabama, Louisiana, New Jersey, and Oregon: Utilization patterns analyzed with individual-level data (MSIS/Medicaid Analytic Extract [MAX]) |
|
A. ELE States
1. Acquisition of Data
To obtain the administrative cost and enrollment data for this task, we developed a letter from ASPE to the six ELE states involved during the first study year, which was signed by Sherry Glied and Cynthia Mann and sent via email to Medicaid and (as applicable) CHIP directors on November 21, 2011. The letter provided background on the evaluation, the analyses and tasks in which states would be asked to participate, contact information for Mathematica and ASPE staff, and a discussion of compensation for providing ELE cost and enrollment data for this evaluation. We followed this email with telephone contact the week of November 28, 2011, to ensure receipt of the letter, identify the appropriate state staff whom we should contact for the first year’s cost and enrollment study, and begin exploring limitations that states might face in providing the types of data we plan to request.
Following this initial contact, we will establish a memorandum of understanding (MOU) with each state to formalize participation in the evaluation. The MOU template, which we will customize for each state, is submitted with this work plan as Appendix A. The MOU contains our data needs, processes for communicating with state personnel, and payments for state data acquisition. It also includes a statement that states accepting payment for participation cannot request administrative funding under Medicaid or CHIP for the time and resources expended that are reimbursed through this evaluation. We will aim to submit all finalized and signed MOUs for the six ELE states to ASPE by March 16, 2012; however, we will begin the data collection and analysis efforts described here immediately after receiving ASPE’s feedback on the approaches and tools proposed in this work plan.
In conjunction with ASPE, we have determined that Alabama and Louisiana will each initially be offered $20,000 in compensation for the data they provide as part of the cost and enrollment study; Iowa, Maryland, New Jersey, and Oregon will receive $50,000 each. The amounts differ due to the differing level of effort we anticipate each state will need to invest to complete our enrollment analyses in the first year of the evaluation. In the cases of Alabama and Louisiana, we will amend data use agreements (DUAs) that were established with Mathematica for the MaxEnroll project in order to use existing enrollment data sets to address key research questions for this evaluation. We have begun the process of amending these DUAs and hope to obtain final signatures in January 2012. In the remaining four states, we will ask state staff to populate data tables with aggregate demographic and retention data on ELE enrollees and those entering through traditional pathways (see Section C). All six states will be asked to provide the same information (an update of their cost data and either MSIS or individual-level data) in the second year of the evaluation. Our MOU proposes dividing compensation to states so that they receive some reimbursement each year. We plan to disperse the same amount ($15,000) to all states in the second year of the evaluation, as all states will be presented with the same requests. If we determine that MSIS data are sufficient, we will not reduce this payment to states. However, our solicitation letter and MOU communicate that, in the event a state documents costs in excess of the agreed-upon total compensation levels, funds are available to reimburse some additional costs.
During the second year of the evaluation, we plan to follow similar procedures to secure the participation of Georgia and South Carolina if funds are leftover from the first states, coordinating closely with the case studies team to ensure consistent communications with the state and a clear point of contact within the evaluation team. If Georgia and South Carolina are included, we will jointly craft the solicitation letter and MOU with the case studies team and will discuss with ASPE the appropriate compensation level that should be offered. We anticipate Georgia and South Carolina would have the same level of effort in completing the cost and enrollment analyses as non-ELE states.
There are two possibilities we will consider for acquiring individual-level data to support the second year enrollment data analyses—requesting an individual-level data set directly from the state or obtaining data from MSIS. There are advantages and disadvantages to each approach. Requesting data directly from the state would introduce a significant reporting burden; however, the range of available data elements might be wider than those available through MSIS and the file might be timelier.
On the other hand, because states already report MSIS data to the Centers for Medicare & Medicaid Services (CMS), using these data would not introduce new reporting burdens on states. Rather, Mathematica would work with ASPE to obtain authorization to use MSIS data for the proposed project through an interagency DUA with CMS. However, data timeliness and the availability of all needed data elements could be limited in MSIS. Regarding timeliness, we anticipate that by January 2013 states would likely have submitted MSIS data through at least June 2012. Regarding available data elements, all states might not have created MSIS indicators to distinguish ELE from non-ELE enrollments. Anticipating that evaluating ELE would be a federal priority, Mathematica has worked with Louisiana to establish unique state eligibility group codes identifying ELE enrollees in MSIS data submissions, and we are working with additional states—including Alabama, New Jersey, and Oregon—to establish similar identifiers. However, our initial conversations with Iowa and Maryland indicate that these states might be unable to establish ELE identifiers in MSIS data within the time frame of this study, and we anticipate that we might have to obtain data directly from these two states. Finally, we note that reporting CHIP data into MSIS is voluntary and not all states do so. For example, Alabama does not report CHIP data into MSIS; however, Alabama’s ELE design does not extend to CHIP enrollees.
To determine which data sets to pursue in each state for the second year of the evaluation, we will consult with Mathematica’s MSIS team in August 2012 to update our assumptions concerning data element availability and submission timeliness for each of the six states. We will then prepare a decision memo for ASPE, submitted during the first week of September 2012, discussing the tradeoffs and our recommended approach(es). We anticipate that this schedule will still provide us time to obtain individual-level data directly from states, in the event that MSIS data are determined insufficient for the evaluation. We will execute the appropriate DUAs with CMS and/or individual states during fall 2012 and aim to acquire data by January 2013 so that we can complete these analyses by April 2013.
If Georgia and South Carolina are included in this analysis during the second year of the evaluation, we will request that the states populate the aggregate tables described in Section C. Again, we will carefully coordinate with the case study teams to ensure that we make this request at the appropriate time to minimize the state burden. We will also incorporate refinements to the table shells and accompanying guidance that reflect our experience gathering this data from Iowa, Maryland, New Jersey, and Oregon during the first year of the evaluation.
B. Cost Analysis
1. Motivation
ELE and other alternate approaches have significant potential to increase administrative efficiencies, enabling states to enroll more eligible children at lower per capita costs by utilizing eligibility findings from partner agencies and thereby reducing, for example, the number of interactions required with state personnel or the number of data entry and verification steps. At the same time, automated data sharing is likely to carry initial implementation costs, both for Medicaid/CHIP agencies and the agencies with which they partner, as the information systems required to support simplified approaches (ELE and non-ELE) to enrollment are developed and built. Therefore, to carefully assess the costs of ELE and other alternate approaches, we will gather data on the marginal differences in costs that state Medicaid and CHIP agencies might experience versus traditional enrollment mechanisms, the fixed initial costs associated with the alternate approach, and, in ELE states, the costs newly incurred by the designated ELE agencies referring children to Medicaid and CHIP. Findings from the cost analyses are expected to be particularly relevant for state policymakers as they continue to consider strategies that facilitate enrollment expansion with limited operational budgets, a goal that became particularly salient during the recession as states faced dramatic budget shortfalls and implemented hiring freezes, employee furloughs, and layoffs, creating new administrative limitations (Kaiser Family Foundation 2011).
2. Administrative Cost Data and Analysis—First Year
The potential for differences in costs between ELE and traditional mechanisms will vary greatly based on each state’s particular arrangements. For example, a state that can omit steps in the enrollment process that are typically completed by a third-party vendor reimbursed on a per-application basis might realize immediate monetary savings by using the ELE route. However, in a state in which state employees perform most functions, ELE might save time in processing a given application without creating enough savings to reduce staffing. Similarly, initial implementation costs are likely to differ widely across states. States that formalized long-standing data sharing agreements with partner agencies might have very low implementation costs, whereas those that established new relationships that required modifications of the information technology infrastructure might have higher initial costs. In assessing the long-term value of ELE, we must also be careful to differentiate whether these initial costs—particularly those related to systems development—would be necessary to implement the provisions of the ACA. In these cases, ELE implementation might have simply accelerated administrative costs that would have accrued in later years.
To estimate the costs of ELE, we will begin by consulting with state staff, through one or two group discussions held by telephone, to gain a detailed understanding of the traditional enrollment process in each state; the steps that can be abbreviated, omitted, or added through the ELE process; the costs associated with each step of the traditional and ELE enrollment processes; the costs of initial implementation; and key contextual factors that might affect estimates of costs. To address these dimensions, we anticipate that we will likely have to solicit the input of policy, budget, human resources, and information systems staffs. These conversations, which we plan to conduct in January and February 2012, will follow the discussion guide in Table VII.3.
The guide begins by asking about the planning process for ELE and by building a flow chart of the current enrollment steps that occur under both traditional and ELE pathways. Because many states maintain these documents already, we will request any existing documentation during our initial contacts, so that we can use our time with state staff more efficiently. We will use the enrollment flow charts to understand the potential for cost differences between ELE and traditional enrollment mechanisms, and we have developed questions to probe more deeply about the staff time and contracted costs that could be affected. For example, we will ask about contractor reimbursement arrangements (that is, fixed contract price, cost-plus-fee, per application) for steps that are completed by a third party and about the number of state staff involved with processing ELE applications on a full- or part-time basis, as well as their salary ranges. In some states that have implemented ELE renewal processes (such as Alabama and Louisiana), we might explore both initial and renewal ELE processes, relative to the traditional processes.
We will next discuss the initial fixed costs of implementation. Specific domains that we will consider include modification of information management systems (which could reduce expenditures needed to prepare for implementation of the ACA) and staff training. We will also try to learn about costs newly incurred by other agencies to facilitate Medicaid and CHIP enrollment, and will request contact information at the partner agency for follow-up. Because these cost analyses will occur before the case studies, we have built into the discussion guide several key contextual questions so that we do not inappropriately attribute costs to ELE. For example, if a state implemented several enrollment process initiatives concurrently, we would not want to attribute all information systems costs associated with the initiatives as ELE costs. Similarly, we will have to understand prior data-sharing relationships with state partner agencies to interpret state comments on the relative cost and ease of formalizing ELE processes.
Table VII.3. Draft Discussion Guide for ELE States Cost Study
State Planning for ELE
Understanding State Enrollment Processes
Marginal Impacts on Contracted Costs and Staff Time
Implementation Costs
ELE Impacts on Partner Agencies
Overall Enrollment and Outreach Costs
Impacts for Beneficiaries
Concluding Thoughts
|
We plan to conclude by discussing overall costs for enrollment and outreach to provide some context for interpreting our data on ELE, and will gather state perspectives on the benefits to beneficiaries of the ELE enrollment mechanism. If ELE is particularly effective at enrolling children, overall enrollment costs might actually increase; however, the cost per child might have declined. By combining state estimates of the changes in overall administrative enrollment costs with changes in total enrollment (discussed later), we can evaluate whether the cost per child has changed under ELE. From another perspective, ELE might be considered as an alternative outreach strategy and its success might be measured alongside other marketing or community-based efforts. We will seek basic information about major state outreach strategies in order to compare investments in those approaches with investments in ELE. Finally, we will begin to gather input on the benefits that beneficiaries might enjoy under ELE, which should be considered alongside the state administrative costs or savings associated with ELE. Although beneficiary perspectives will be best gathered through the focus groups that are planned as part of our case studies, these first-year cost analyses will occur before the focus groups have begun. Gathering data on the beneficiary perspective from state staff will provide a balance to our cost findings in advance of more direct evidence from children and their parents.
After we have completed these discussions with the state, we will compile our notes for state review and verification. We will also create a spreadsheet for each state that captures all requested or obtained quantitative cost data. For example, we will note all steps that differed between the traditional and ELE enrollment processes, and the staff time (and salary estimate) or contractor costs associated with each step. We will separately note each initial start-up cost, and the global enrollment and outreach budgets reported by the state. When we share this spreadsheet with the state, we will request that it complete any blank fields in which data might have been unavailable at the time of our discussions and verify those fields that we have prepopulated. We will work flexibly with states to obtain data in the way they believe costs can be estimated most accurately. For example, in some cost domains, states might have fluctuating costs from month to month and believe that annual expenditures are most accurate. In other domains, such as application processing, the state might be able to estimate a per-application figure or cite the salary range of a staff member who handles a set of activities. In all cases, we will seek to obtain the total state and federal combined cost, or to adjust costs to account for the state Federal Medical Assistance Percentage (FMAP) rate if we receive data only on state expenditures.
After receiving data from the states, we will convert each of the reported cost elements into a cost-per-enrolled-child measure and will sum the costs from each step to estimate the ongoing difference in cost per new ELE enrollee versus an enrollee entering through traditional enrollment routes. We will aim to decompose the source of cost differences across major input categories, such as labor, third-party payments, and other expenditures. We will separately report the initial fixed costs required to implement ELE; as members of the TAG reported, states might consider these costs differently from the ongoing marginal costs of ELE due to the 90/10 federal matching rate available to support ACA-related infrastructure improvements. We will also construct an overall cost-per-enrolled-child measure, dividing total ELE and traditional enrollment expenditures by the total number of ELE and traditional enrollees, to understand whether global enrollment efficiency has changed with the introduction of ELE.
3. Administrative Cost Data and Analysis—Second Year
In the second year of the evaluation, we will complete an updated cost analysis in the six ELE states included in the first year and, if funds are available, will seek cost information from Georgia and South Carolina.
As ELE processes mature, the costs and savings that states accrue could change, so updating cost analyses for the first six ELE states could provide valuable insight. For example, the partner agencies might have developed a more efficient way of exchanging information that further reduces application processing times for ELE enrollments, or efficiencies could be realized in the traditional enrollment process that have implications for ELE enrollment. We will also explore whether any staff time costs or efficiencies documented in the initial analysis have been sufficiently large in scope to affect staffing requirements. For example, has the Medicaid program been able to increase enrollment without adding another enrollment staff member? Or did it need to recruit someone to specialize in ELE cases? We might also request data on new cost elements that we learn are relevant through the case study process. For example, by the second year of the evaluation, states will begin to have data on the renewal rate among children who first enrolled through ELE mechanisms. If we learn that ELE enrollees are particularly difficult to reenroll, the additional effort required to ensure continued coverage should be balanced against the low cost to initially enroll children through ELE.
From a procedural perspective, we will first revise our discussion guide, which will be available for ASPE review and comment in November 2012. We will then use that guide to facilitate a conversation with state staff around marginal administrative costs and any new fixed costs, and will complete a verification process with the states before converting cost estimates into cost-per-enrolled-child figures. We anticipate that this update will be complete by March 2013.
In Georgia and South Carolina, the two ELE states not included in the first year of analysis, we will use a slightly different strategy if funds remain to extend this study to include those states. Although our discussions would be rooted in the first-year discussion guide (shown in Table VII.3), to minimize the reporting burden for states, we will have to carefully coordinate with the case study teams who might be exploring some of the same issues. Also, some topics might be better addressed by the case study teams during their site visits as part of the natural flow of interviews. Depending on the timing of the case study visits and our own consultations, we will either abbreviate our discussion guide to focus on areas not already discussed during the case studies or will convey our findings to the case study teams along with requests for follow-up in any outstanding areas.
4. Challenges
We anticipate that it will be difficult to disentangle the costs that are uniquely associated with ELE from those that occurred due to concurrent policy changes. To address this concern, our discussion guide specifically probes several cost elements and explores potentially relevant contextual developments (such as concurrent process changes) to help prompt state staff. In addition, although we are optimistic that partner agency staff will participate in brief conversations regarding their cost experiences with ELE, we expect that in some states we might be limited to the Medicaid and/or CHIP agency perspective during the first year, if partner agency staff are not available within our time frame for analysis (completion by March 2012).
C. Enrollment Analysis
1. Motivation
The primary goal of ELE, besides making administrative efficiencies, is to increase enrollment among eligible children. In principle, ELE and alternate approaches to simplifying enrollment have two potential effects: (1) attracting new families into Medicaid and CHIP and (2) more efficiently enrolling families that would have been enrolled through traditional pathways (perhaps reducing the length of gaps in coverage that might have occurred). These effects are difficult to distinguish because we cannot observe the counterfactual. That is, we do not know what families who enrolled via simplified approaches (ELE and non-ELE) would have done if those pathways were not available.
Although we will not be able to calculate a definitive impact of ELE on enrollment, descriptive analyses using individual-level data that we will conduct as part of this task will improve our insights about the likely effects of ELE. First, we will examine the most basic question: How many children have entered through ELE and other simplified mechanisms? Findings from this analysis can be compared against those from the SEDS analysis to corroborate that study’s conclusions about net gains in enrollment. Second, to the extent that ELE reaches new families, those families are likely to differ from those that can be reached by other means in terms of knowledge of public health insurance, medical need, and other characteristics. Similarly, among families who would have enrolled in public insurance regardless of ELE’s availability, there are likely to be differences between families who do and do not take advantage of ELE when it is available. To shed light on whether ELE and alternate approaches to simplifying enrollment are reaching a unique group of beneficiaries, we will examine and compare demographic characteristics and prior public insurance coverage among children who enroll through alternative pathways and those who enroll through traditional processes. We will also consider whether children enrolled through simplified approaches (ELE and non-ELE) are more difficult to retain in the system at renewal. If so, the initial efficiencies of enrollment might be diminished by additional expenditures needed to retain them in coverage.
2. Enrollment Data and Analysis – First Year
In the first year of the evaluation, the enrollment data analysis will follow one of two approaches across the six ELE states. In two states—Alabama and Louisiana—we will have access to individual-level data to support detailed analyses. In the remaining four ELE states—Iowa, Maryland, New Jersey, and Oregon—we will request that states populate aggregate data tables that we specify. (These aggregate table shells are included as Appendix B. We have also developed a draft document providing guidance to the state in populating these tables.) We begin by discussing this latter approach.
At the most basic level, we plan to request aggregate monthly ELE enrollments and traditional enrollments for children who primarily qualify for Medicaid or CHIP on the basis of income (rather than disability, foster care status, and so on).9 We expect the highest number of ELE enrollments during the first month of operations, reflecting the stock of potential Medicaid/CHIP beneficiaries from the entire existing caseload of an ELE partner agency’s programs. Later months will likely have fewer ELE entrants, reflecting those new to the designated ELE agency and to Medicaid/CHIP. We will consider whether there are notable fluctuations in the flow of ELE enrollments that we might want to explore in more detail with states during the case studies.10 We will request one year of historical data before ELE implementation so that we can establish a baseline enrollment trend.
Next, the tables request enrollment counts disaggregated by several demographic characteristics. For example, we will request data on a child’s age, race/ethnicity, primary language, citizenship status, household income, and urban/rural status (we will provide states with a crosswalk to designate counties or zip codes). We will also request that states review past enrollment records to look for a period of prior public coverage in Medicaid or CHIP, to help address whether ELE enrollees are truly new to the system and how recently they might have had contact. Understanding the demographic and prior enrollment profile of ELE enrollees will address the questions of whether ELE is reaching a unique or distinct group of beneficiaries and whether some groups seem to particularly benefit from the availability of an ELE enrollment mechanism. These findings will help policymakers understand whether ELE brings unique value as an outreach or enrollment tool.
Finally, the tables request information on disenrollments and reenrollments, stratified by ELE status. For example, we will request data on the number of beneficiaries who remain enrolled 6, 12, 13, 18, and 24 months following initial enrollment (enrollment during month 13 would indicate successful renewal with no gaps in coverage), and among disenrollees, the number who reenrolled (via ELE or traditional routes) within 3, 6, or 12 months. These outcomes will help us understand whether ELE enrollees are any easier or more difficult to retain in Medicaid and CHIP, a finding that we will balance against the relative ease of initial enrollment via ELE in determining the overall effectiveness of this mechanism. We note that many of the retention and renewal time points might not be observable by December 2011, depending on when ELE was first implemented within a state, and we plan to update these statistics with individual-level data during the second year of the evaluation. Similarly, to simplify the data request and ensure that we are able to provide quality assurance (QA) by reviewing the spreadsheets for internal consistency, we have specifically avoided including many calculated statistics that might be of interest, such as the average length of continuous enrollment, average gap in enrollment, or churning rate. We plan to address those questions with individual-level data in the second year of the evaluation.
We will share the table shells with states in January 2012 and schedule an orientation call, including both policy staff and the information systems staff directly responsible for compiling the data request, to walk through the table shells and guidebook and to answer any immediate questions. We will remain available for further follow-up as needed, and will periodically reach out to states to assess progress and provide support until the populated tables have been submitted. We will request that states submit the tables by the end of February 2012 (using data through December 2011), recognizing that in practice, some states might need additional time to complete the work. We will conduct follow-up calls as needed to ensure that we understand the data that states have reported. After reviewing the submissions for emerging key themes, we will prepare summary tables and charts to highlight those findings. Because of differences in state administrative record keeping (see Section 4, Challenges, below), we anticipate that it will not be appropriate to aggregate data across states.
In Alabama and Louisiana, we will use a different technical strategy to address the same research questions and to generate comparable statistics to those requested through the aggregate tables. Rather than asking states to populate data tables, we will analyze individual-level data for 2005 through 2011 that Mathematica has already acquired or will acquire for the Robert Wood Johnson Foundation MaxEnroll project. Using these data, we will construct as many of the same descriptive measures as are feasible, as well as some calculated retention measures—such as the average length of continuous enrollment and the average gap in coverage among those who reenroll. We will also be able to conduct descriptive regression analyses to compare the likelihood of retention outcomes for ELE versus traditional enrollees within a state, after controlling for differences in observable characteristics across the groups. In this case, we are not employing regression analyses in order to conclude that ELE causes children to be more or less difficult to retain, as there are likely to be significant selection issues regarding the types of children and families that opt in to Medicaid and CHIP via ELE and traditional routes. Instead, we will use regressions to control observable characteristics that we expect can affect retention and that are likely to differ across groups, so that we can better estimate the differential between children enrolling via different mechanisms.
Regression models will follow the general model below, where the retention outcome for person p is a function of the enrollment pathway, a vector (DEMO) of demographic characteristics, and a vector of fixed effects for the initial enrollment month. ELE is a dummy variable (0/1) indicating whether a beneficiary enrolled through the ELE pathway or traditional application routes.
(2) Retention Outcomep = β0 + β1ELE + DEMOα +Enrollment Monthγ + εp
Again, because Alabama and Louisiana have unique ELE designs and might report data differently, we do not plan to pool data across states. In each state, β1 will indicate whether the differential retention patterns of ELE participants persist after controlling for observable personal characteristics. We anticipate reporting the results of this analysis as regression-adjusted retention rates, rather than focusing on the magnitude of β1 or attempting a causal interpretation.
3. Enrollment Data and Analysis—Second Year
During the second year of the evaluation, we will update the analyses conducted during the first year and will conduct descriptive multivariate analyses in all six ELE states (following the first-year model for Alabama and Louisiana), utilizing individual-level data. An updated analysis will enable us to observe long-run trends in new enrollments, renewals, and retention outcomes that were not possible given the relatively short observation period in the first evaluation year. For example, we might be able to examine whether ELE children who fail to renew enrollment eventually return to the Medicaid or CHIP programs, and their average length of gaps in coverage. In addition, the new enrollment analysis will be able to draw on data and findings from other major analytic tasks, most notably the case study work to be conducted in both ELE and non-ELE states. We anticipate that the rich contextual data gathered through the case studies will enable us to explore new hypotheses that emerge and refine our analytic approaches to reflect the timing of specific implementation milestones in each state. For example, if we learned that a state began aggressive renewal outreach to ELE children 18 months after first implementing ELE enrollment mechanisms, we might look for a change in renewal rates that coincided with that initiative. Finally, utilizing individual-level data in all six states will enable a more detailed evaluation of ELE, which we will be able to conduct only in Alabama and Louisiana during the first year of the evaluation.
4. Challenges
The most significant challenge for the enrollment analysis is data availability. Although ELE states are required to attest that they have flagged ELE enrollees in their administrative systems, we understand that CMS has not focused on this requirement, and we anticipate that some states might face technical limitations in producing the requested data tabulations separately for ELE and traditional enrollees.
We also anticipate that states might have implemented the requirement to flag ELE enrollees differently. For example, some states could have administratively flagged all children who first entered through the ELE pathway, regardless of whether they were ultimately deemed eligible under other criteria. Other states might have narrowed the ELE classification only to those children who completed the ELE processes as specifically outlined in the approved waiver from CMS. For these reasons, we plan to hold conversations with knowledgeable policy and data staff before interpreting the data that we receive from states. Also, we do not anticipate that it will be appropriate to combine data across states. To the extent that states are able to report some data separately for ELE enrollees, this challenge is primarily one of appropriately framing and communicating the results to external stakeholders, so that they are not misled by apparently different outcomes across states.
Finally, in the first year of the evaluation the enrollment study faces the challenge of an aggressive time line for completion. We have partially addressed that challenge by requesting aggregate data (with few calculated statistics) or using individual-level data that are already accessible to Mathematica through existing projects. However, we still anticipate that we might not be able to obtain all requested data by March 2012. For example, a state might be able to prepare month-by-month tabulations for demographic characteristics relatively easily, but it might not have the staff resources to extract historic data to look at prior public enrollment. In the event that states face major reporting limitations, or that reporting is significantly uneven across states, we will work with ASPE to identify the appropriate way to address these limitations in the Interim Report to Congress, understanding that we will have the opportunity to expand and update these analyses in the second year of the evaluation.
D. Utilization Analysis
1. Motivation
If we move forward with utilizing MSIS data for the second-year enrollment analyses, in four states (Alabama, Louisiana, New Jersey, and Oregon) we will be able to examine utilization patterns among ELE and traditional enrollees during the second year of the evaluation. For these four states, we could link individual-level enrollment records with claims and encounter data to examine the types of services most frequently used by ELE enrollees and whether those patterns differ from traditional enrollees.11 These analyses could address several important questions. For example, some ELE states use passive enrollment processes and ELE enrollees might not know that they are eligible to use services or how to access services. Examining utilization data will enable us to address several basic questions: Are ELE enrollees using services? If they use services, is there a longer gap between official enrollment and initial service receipt compared with traditional enrollees? (For this analysis, we will exclude those who enroll due to hospitalizations or other major medical events.) Does first-year service utilization differ between ELE and traditional enrollees?
Utilization data can also help to inform the question of whether ELE enrollees have different characteristics and might find different value in Medicaid/CHIP than traditional enrollees. For example, is there evidence that ELE enrollees use Medicaid/CHIP to provide wraparound eye, dental, or prescription drug coverage to supplement private insurance? Is there evidence that ELE enrollees are relatively low risk and use few services? This last question could be particularly relevant for states considering both ELE mechanisms and an expanded role for capitated managed care, as states would be responsible for the capitation payment, regardless of the actual service use of an enrollee.
Our findings on retention and service utilization have important implications for the administrative and overall costs that accrue to the state agencies implementing ELE and other simplified pathways. For example, evidence that ELE children are slower to use services might warrant additional state investigation—and potentially new outreach—to ensure that families enrolling through these pathways understand the scope of their benefits and how to access services. Lower service utilization might also be an indicator that children entering through simplified pathways are generally healthier and have fewer health care needs, an important budgetary factor for states to consider, particularly those states that must negotiate capitated payment rates with managed care providers.
2. Utilization Data and Analysis
Analyses conducted to address these questions might include producing both unadjusted and regression-adjusted descriptive tables that display the rate of service use by enrollment pathway. As with the analysis of retention outcomes, in this case regression analyses are used to control for observable characteristics that we expect could affect utilization and that are likely to differ across groups, so that we can better estimate the differential between children enrolling via ELE and traditional mechanisms. We will not interpret results to conclude that ELE has caused changes in utilization. Regression models will follow the general model below, where the utilization outcome for person p is a function of the enrollment pathway, a vector (DEMO) of demographic characteristics, and a vector of fixed effects for the initial enrollment month. ELE is a dummy variable (0/1) indicating whether a beneficiary enrolled through the ELE pathway or traditional application routes. We might also explore using first-year utilization measures as variables predicting retention outcomes if we find that retention and first-year utilization differ by enrollment pathway. As with the enrollment analyses, we do not plan to pool data across states. In each state, β1 will indicate whether the differential retention patterns of ELE participants persist after controlling for observable personal characteristics.
(3) Utilization Measure (that is, receipt of any physician visits within six months of enrollment)p = β0 + β1ELE +DEMOα +Enrollment Monthγ + εp
We could conduct these utilization analyses using either of two alternative federal data sources: MSIS or MAX data. Although MSIS data are timelier, MAX files incorporate corrections for retroactive claims and eligibility, making them easier to use for research. The current data production time line calls for calendar year 2010 MAX data to be available by January 2013. If these data are not considered timely, given the number of ELE enrollees that entered Medicaid and CHIP in 2010, we could access MSIS utilization records. Two states (Alabama and Louisiana) operate fee-for-service programs, so we can expect to obtain a clear picture of utilization through MSIS/MAX. In addition, New Jersey and Oregon, which rely primarily on managed care for children in Medicaid and CHIP, report reliable encounter data from their managed care organizations (Vivian Byrd, Mathematica Research Analyst, personal communication based on her project work on MSIS, September 9, 2011). We will consult with Mathematica’s MSIS and MAX teams in August 2012 to update our assumptions concerning data availability and submission timeliness for each of these four states, and will incorporate a discussion of utilization data in our September 2012 decision memo to ASPE. We anticipate that the utilization analyses will move forward in parallel with our updated individual-level enrollment analyses, with data acquisition by January 2013 and completed analyses by April 2013.
3. Challenges
Like the enrollment analysis, the most significant challenge for the utilization analysis is data availability. The utilization analyses are particularly vulnerable to data availability, as they depend on our ability to use MSIS or MAX, and therefore state reporting of an ELE indicator into MSIS, which all ELE states do not currently do.
E. Reporting
For the first-year analyses in ELE states, we will draft and submit a brief memo in April 2012 summarizing the data, analyses, and findings from the cost and enrollment study, which can be shared before the scheduled TAG meeting (by telephone) in May 2012. The memo will present three or four key messages that we plan to communicate in the Interim Report to Congress, along with tables that support these messages and a brief methodological narrative. This memo will form the basis for sections of the 2012 Report to Congress, after incorporating additional observations from TAG members and ASPE.
For the second-year analyses in ELE states, we will produce several deliverables addressing cost, enrollment, and utilization separately. In February 2013 we will submit a memo to ASPE that discusses the findings from the cost analyses. The memo will incorporate and discuss the first-year findings and the extent to which the new analyses have changed or enhanced our findings. Similarly, in April 2013 we will submit a memo to ASPE that discusses the findings from both the first and second year enrollment analyses, and we will prepare a separate stand-alone memo presenting the utilization analyses. Collectively, these three memos will form the basis for sections of the Final Report to Congress, after incorporating any comments from ASPE and from the TAG members.
F. Non-ELE Program Cost and Enrollment Study
1. Acquisition of Data
Processes for data acquisition and analysis will be similar to those proposed for ELE states. First, we will develop a letter from ASPE to each state that provides background on the evaluation, the data collection tools and proposed data collection procedures, contact information for Mathematica and ASPE staff, and a discussion of the compensation (up to the specified limit of $100,000). This letter will serve as the solicitation notice for both the cost and enrollment study and the case studies. Soon after sending the letter, we will conduct telephone follow-up to address any questions or concerns the state might have, obtain the state’s preliminary (oral) agreement to provide the requested data and participate in case studies, and identify appropriate points of contact. Next, we will draft and submit to each state an MOU that formalizes the initial agreement. Contents of this MOU will include the specific data elements requested from the states, the exact time line for providing these data, the process by which the data will be submitted to Mathematica, and the compensation schedule and amount (determined in conjunction with ASPE). As with the ELE states, the MOU will clarify that states accepting payment for participation cannot request administrative funding under Medicaid or CHIP for the time and resources expended that were reimbursed through this evaluation.
2. Motivation
Studying the program costs and enrollment patterns for alternate approaches to simplifying enrollment will enable us to examine administrative costs per child, the demographics of children who enroll, and their retention outcomes separately for each non-ELE state, just as we have proposed doing in ELE states. However, the real value-added of this approach is to compare the findings for each of the non-ELE states with those documented in ELE states, providing a point of comparison regarding the relative costs and benefits of ELE versus alternate approaches to simplifying enrollment that a state might consider.
3. Cost and Enrollment Data and Analysis
As part of the case studies in six non-ELE states, we will seek administrative cost and enrollment data parallel to those acquired for ELE states during the first year of the evaluation, using tools that are modeled on the administrative cost discussion guide that we present in Table VII.3, and the aggregate data tables that we present as Appendix B. These tools will be modified to specifically focus on the non-ELE intervention of interest in each state. Because we cannot request that non-ELE states complete data collection forms or participate in interviews without OMB clearance, these activities will primarily occur in the second year of the evaluation, between September 2012 and March 2013. Because one criterion for selecting non-ELE states will be the existence of enrollment simplification strategies that are sufficiently well-established to obtain meaningful data on cost and enrollment effects by fall 2012, we anticipate that capturing a single point in time will provide an accurate snapshot of costs and enrollment in these states. We will confirm this assumption during our discussions with program staff.
4. Challenges
The most significant challenge that is unique to the non-ELE cost and enrollment analysis will be states’ ability to administratively distinguish children who enrolled through an alternate approach to simplifying enrollment from those who enrolled through a traditional route. Because CMS has not typically required states to establish new administrative flags for each enrollment route, states are likely to have pursued a variety of strategies for tracking the effects of these initiatives. In some cases aggregate data might be available (for example, enrollment reports submitted to the state by managed care organizations), but states might not have the ability to flag individuals in their own administrative systems to enable more sophisticated data analyses. In other states, we might be entirely unable to identify children who enrolled through an alternative approach to simplifying enrollment. However, if we are able to pinpoint the date of policy implementation, we could explore a descriptive analysis that looks at overall enrollment trends before and after the new simplified approach became available.
5. Coordination
We will be careful to coordinate with the non-ELE case study team to make the most efficient use of state staff time. For example, it might be most appropriate to incorporate the cost discussion guide as part of our scheduled interviews during the site visit, or we might determine that it would be advantageous to conduct these analyses first, identifying specific areas for follow-up with state staff during the case study period. As we finalize the non-ELE case study states and begin to gather background data on the simplified approach of interest, we will determine the most appropriate approach. Maggie Colby, the task leader for the cost, enrollment, and utilization study, will also be leading case studies in two non-ELE states, which will enhance our ability to coordinate across tasks.
6. Reporting
Findings from this comparative analysis of ELE and alternate approaches to simplifying enrollment will be communicated as part of the final Report to Congress.
This page has been left blank for double-sided copying.
VIII. Evaluation Reports and related briefings
As described in Chapter II, many research questions central to the evaluation will be best addressed by synthesizing findings from multiple analyses across the four studies. To communicate these integrated findings effectively, we plan three different reporting activities: (1) a stand-alone report on possible Express Lane Eligibility (ELE) improvements; (2) two Reports to Congress; and (3) briefings.
A. Recommendations on ELE Improvements
As specified in the request for proposals (RFP) for the evaluation, we will draft a brief report outlining recommendations on two topics central to maximizing ELE’s effectiveness: (1) administrative and legislative changes to improve ELE’s effectiveness and (2) best outreach and simplified enrollment practices for children under Medicaid and the Children’s Health Insurance Program (CHIP) (ELE and non-ELE). The audiences for these recommendations are federal policymakers with the authority to reshape ELE and federal and state officials seeking guidance on how best to enroll eligible-but-uninsured children into Medicaid/CHIP, whether through ELE or other strategies.
In addition to these two central topics, we will consider several other possible topics that could be of interest to the report’s target audiences. These topics, which would extend the focus of the reports’ lessons (pending approval of the Assistant Secretary for Planning and Evaluation [ASPE]), include the following:
ELE lessons for Affordable Care Act implementation. Given the current state and federal focus on effective implementation of the Affordable Care Act, we can identify Affordable Care Act-relevant lessons learned from ELE and other efforts to reach children who qualify for Medicaid and CHIP. These lessons can help federal and state policymakers as they work under the Affordable Care Act to increase enrollment of eligible-but-uninsured children, lower administrative costs, and prevent erroneous eligibility decisions. The technical advisory group (TAG) emphasized the potential value of distilling such lessons, including lessons that relate to enrolling additional adults.
ELE reauthorization issues. Findings from our evaluation could also offer guidance on the potential gains and risks of extending authorization of ELE as a state option beyond federal fiscal year 2013. In addition to examining the relative benefits of the policy, we can also examine the extent to which ELE might lead to erroneous enrollment decisions—a fear that some policymakers voiced as ELE was debated (Congressional Record 2009 [Grassley]; Leavitt 2007). Many members of the TAG echoed this issue, believing it was important to understand whether the data used in ELE were as accurate as those collected via other means and to understand which of the potential sources of ELE data were most accurate.
ELE as a means of program integration. As indicated earlier, ELE represents an innovative approach to breaking down silos between public benefit programs—a topic of interest to human services and health coverage programs. As a further extension to our report, we could explore this issue drawing on evaluation data from the case studies and other study activities. In conducting this exploration, we would place the research findings of this project in the context of published literature concerning similar efforts applied by other programs.
To the extent that the report makes specific recommendation regarding ELE implementation or the more specific topics raised here, we will be careful to characterize each recommendation in terms of the evidence and the strength of its evidentiary support. We will also note those topics or issues that the research does not definitively resolve.
B. Reports to Congress
We will compile and integrate all available analyses to support two comprehensive reports on ELE for delivery to Congress: an interim report in 2012 and a final evaluation report in 2013. Specifically, the Interim Report to Congress will synthesize available findings from the assessment of the state policy context, the analysis of ELE impacts on enrollment using data from Statistical Enrollment Data System (SEDS), and the cost and enrollment studies in ELE states. The Final Report to Congress will synthesize all findings from all studies, summarizing and incorporating themes that emerged across them. The sources of findings for the two evaluation reports are summarized in Table VIII.1.
Table VIII.1 Content and Sources of Data for Interim and Final Reporting to ASPE
Source of Analysis/Report |
2012 Interim Report |
2013 Final Evaluation Report |
Assessment of the State Policy Context |
|
|
Baseline and Ongoing Document Review |
X |
X |
Quarterly Interviews in 30 States |
|
X |
51-State Survey |
|
X |
Analysis of ELE Impacts on Enrollment Using SEDS Data |
X |
X |
Case Studies in ELE and Non-ELE States |
|
X |
Cost, Enrollment, and Utilization Study |
|
|
ELE States |
X |
X |
Non-ELE Case Study States |
|
X |
Recommendations for ELE Improvements |
|
X |
We expect that each report will contain the following features:
An executive summary will serve as a stand-alone, succinct summary of the ELE evaluation and key findings.
An introduction will provide an overview of the purpose and goals of the project, conceptual framework, and background regarding the evaluation.
A policy context chapter will describe the policy issues related to identifying and enrolling children in Medicaid and CHIP and the context in which ELE programs operate to set the stage for the remainder of the report.
A methodology chapter will describe the various methods used for data collection activities, including data collection objectives, content, and procedures; sample design and recruitment strategies; and methods used for the analysis; We might address some of the methodological issues in a technical appendix, to minimize the level of detail in the body of the report
A summary of key findings will draw from the multiple data sources used in the report and conclusions drawn from the findings. The report will include one chapter for each of the applicable studies as well as one chapter that draws findings together across studies, noting and analyzing areas of convergence or divergence.
Discussion of the findings will provide the audience with a clear understanding of what was learned through the evaluation; this chapter will also identify the limitations of the study and interpretation of the findings.
A chapter on policy implications and next steps will discuss recommendations for public policy and, in the interim report, will highlight the remaining research activities of the evaluation; the final report will discuss any further research needed to update and extend the knowledge gained from the evaluation.
An appendix will provide further technical information as appropriate, individual state case study reports, quarterly tracking and monitoring reports, and other information as needed.
The Final Report to Congress will include two additional chapters. The first will present the ELE error rates (the percentage of children erroneously enrolled in Medicaid or CHIP from a statistically valid sample) as computed by states in compliance with CMS guidelines; it will also describe how the rates were calculated.12 The second chapter will present and summarize recommendations and best practices, both for ELE programs and for other streamlined enrollment activities.
Although Congress will require detailed reports, we also appreciate that, in practice, individual members of Congress and their staffs have limited time to review and digest the depth of the findings presented. Accordingly, as noted earlier, we will produce for each report a concise, stand-alone executive summary. We will draw on the expertise of in-house editorial and communications staff to lay out each chapter for maximum clarity and usefulness. Examples include the use of brief chapter summaries as a means of communicating key messages concisely throughout the report, the use of simple but meaningful graphics to communicate key statistical information, and the use of text boxes and other techniques to improve the accessibility of the report and vary the flow of the text. We will write reports in an engaging tone, accessible to a wide audience, with consistent and clear visuals throughout. Both reports will also be compliant with Section 508 requirements.
C. Study Briefings
In addition to conveying the findings from this project clearly in writing, we will also conduct two separate in-person briefings with federal officials covering the respective findings in the Interim and Final Reports to Congress. The goals of these briefings will be to communicate central lessons from the evaluation and to characterize their policy implications, thereby supporting federal policymaking and program design efforts. Before each briefing, we will discuss with the ASPE task order officer (TOO) and other key ASPE staff the specific content and focus of the briefing, to ensure that briefings are responsive to the audience and the needs of the U.S. Department of Health and Human Services (HHS).
This page has been left blank for double-sided copying.
IX. Developing and Obtaining Approval for Data Collection Instruments
A. OMB Clearance
Overview. Obtaining clearance from the Office of Management and Budget (OMB) ensures the quality and utility of the data collected by a federal agency and minimizes the public burden incurred by the collection process. Using OMB guidelines from the U.S. Department of Health and Human Services (HHS), Mathematica will assist the Assistant Secretary for Planning and Evaluation (ASPE) in navigating the OMB process, preparing submissions, responding to public and OMB questions, and obtaining clearance for the data collection instruments or tools spanning the four studies described in the report. They include (1) an ELE case study protocol, including the site visit interview protocol, sample selection plan for focus groups, and the focus group moderators guide; (2) a non-ELE case study protocol, including the site visit interview protocol, sample selection plan for focus groups, and the focus group moderators guide; (3) a non-ELE administrative cost and extraction tool; (4) a non-ELE enrollment data collection form and extraction tool; (5) a quarterly monitoring protocol; and (6) a 51-state survey instrument. Table IX.1 outlines the schedule for the OMB submission and the following chapter discusses the content of the package.
Table IX.1. Schedules for OMB Submission
OMB Process |
Dates |
Submit the 60-day Federal Register Notice (FRN) for project officers’ review |
1/20/12 |
Project officers publish 60-day FRN |
~1/20/12 |
During 60-day public comment period, conduct pretest and submit pretest report, and revise instruments as needed |
1/20 - 3/23/12 |
Respond to public comment after 60 days and revise package |
3/23 – 4/20/12 |
Submit final OMB package to HHS |
4/20/12 |
Project officers publish 30-day FRN, submits final OMB package to OMB |
~4/20/12 |
OMB review usually takes about 60 days |
6/15/12 |
Assist project officers in responding to any OMB questions |
6/20/12 |
Receive final OMB clearance |
6/22/12 |
Starting the OMB process: 60-day FRN. For the OMB package, we will assist the project officers in preparing the 60-day FRN and developing a preliminary set of supporting documents in case the public wishes to review them at some time during the public comment period. The package will include the preliminary supporting statement and proceed to the specifics of all eight data collection instruments/tools discussed above.
Pretesting instruments in preparation for submitting the final packages to OMB. While waiting to receive public comments, we will be using the ELE data collection form and extraction tool in the six ELE states (which does not require OMB approval). This can also serve as the pre-test for the non-ELE enrollment data collection form and extraction tool, since that will be a similar instrument. The ELE case study and non-ELE case study protocols do not require pretesting. (However, as is standard procedure at Mathematica, we will use the first case study in each type of state [ELE and non-ELE] as a pretest of the protocols, making any adjustments that seem necessary after that first visit for use in the remaining states.) We will conduct pretests of the quarterly monitoring protocol and the 51-state survey instrument. We will prepare a short pretest report with recommendations for the project officers’ consideration before including them in the final OMB package.
30-day FRN. Mathematica will assist the project officers in preparing the 30-day FRN. Based on public comments and the pretest reports, we will prepare draft and final versions of the OMB package for submission to the project officers and internal review at ASPE. We will respond succinctly to OMB’s established Part A and Part B questions using HHS guidelines. The final OMB package will include copies of the federal authorizing legislation, the 60- and 30-day FRNs, pretest reports, public comments and responses from the 60-day FRN, and final versions of instruments and protocols.
Receiving clearance. After OMB receives the package, it can take 60 days or more before ASPE will learn the outcome of the review (approved, approved with change, or disapproved). If approved with change (a not uncommon occurrence), OMB will present questions to ASPE and Mathematica will assist the project officers in responding to them. When OMB issues a control number and expiration date, we can finalize the instruments and begin data collection.
B. IRB Approval
Federal and state regulations govern research on human subjects in order to protect these subjects’ rights and welfare, including their rights to privacy and confidentiality. The institutional review board (IRB) process applies these regulations as well as other institutional guidelines as they apply to individual research studies. Specifically, the IRB process focuses on ensuring that all survey materials are understandable by the target population, participation risks and benefits are stated clearly, confidentiality is assured, and respondents understand they may refuse to respond to the whole or any part of the survey.
OMB expects that IRB approval will be secured for all components of the evaluation. In obtaining this approval, Mathematica will use a single external IRB, Public and Private Ventures (or PP/V) in Philadelphia, Pennsylvania, to review survey instruments and materials seen by respondents, an approach that is more efficient than seeking approval from the different states. The PP/V IRB will normally specify a series of questions (focused on the topics listed earlier) to be answered and reviews the responses, questionnaires and all materials seen by respondents. The process usually takes two to three months. It is possible that an individual state participating in the study may expect that the evaluation submit to its state-specific IRB. If this arises, we will proceed with the state IRB following an approach likely to be similar to our PP/V submission. In completing its submission to all IRBs, the evaluation team will work closely with the project officers, sharing the drafted materials and working through any follow-up questions that might arise subsequent to the initial review.
REFERENCES
Adcox, Seanna, Associated Press. “Good News: S.C. Medicaid May Add 70,000 Kids to Program.” South Carolina Health Care Voices, October 25, 2011. Available at schealthcarevoices.org/2011/10/25/good-news-s-c-medicaid-may-add-70000-kids-to-program/. Accessed December 15, 2011.
Centers for Medicare & Medicaid Services. “CHIP and Medicaid State Plan Amendments.” Baltimore, MD: CMS, 2011. Available at www.cms.gov. Accessed August 2, 2011.
Center for Medicaid and State Operations. “Letter to State Health Officials re: Express Lane Eligibility Option.” Baltimore, MD: CMSO, CMS, February 4, 2010.
The Children’s Partnership. “Express Lane Activities: States on the Move.” Washington, DC: The Children’s Partnership, January 2011. Available online at www.childrenspartnership.org/AM/Template.cfm?Section=State_Activity_Report&Template=/CM/ContentDisplay.cfm&ContentID=13347. Accessed August 2, 2011.
The Children’s Partnership. “ELE Program Examples web page.” Washington, DC: The Children’s Partnership, 2011. Available online at www.childrenspartnership.org/AM/Template.cfm?Section=State_Activity_Report&Template=/TaggedPage/TaggedPageDisplay.cfm&TPLID=153&ContentID=12200. Accessed August 2, 2011.
The Children’s Partnership. “Express Lane Eligibility: Louisiana Moves Forward.” Updated April 2010. Washington, DC: The Children’s partnership, 2010. Available at www.childrenspartnership.org/AM/Template.cfm?Section=Express_Lane_Toolkit&Template=/CM/ContentDisplay.cfm&ContentID=14527/. Accessed August 2, 2011.
Congressional Record. “Proceedings and Debates of the 111th Congress.” Congressional Record, vol. 155, no. 18, January 29, 2009, p. S1045. Available at http://www.gpo.gov/fdsys/pkg/CREC-2009-01-29/pdf/CREC-2009-01-29-pt1-PgS1007-6.pdf#page=1. Accessed August 5, 2011.
Dorn, Stan. “Applying 21st-Century Eligibility and Enrollment Methods to National Health Care Reform.” Washington, DC: Urban Institute, December 2009. Available at www.urban.org/UploadedPDF/411985_national_health_care_reform.pdf. Accessed July 31, 2011.
Dorn, Stan, Bowen Garrett, Cynthia Perry, Lisa Clemans-Cope, and Aaron Lucas. “Nine in Ten: Using the Tax System to Enroll Eligible, Uninsured Children into Medicaid and SCHIP.” Washington, DC: Urban Institute, January 2009. Available at www.urban.org/UploadedPDF/411844_tax_system.pdf. Accessed July 31, 2011.
Ellwood, Marilyn, Angela Merrill, and Wendy Conroy. “SCHIP’s Steady Enrollment Growth Continues: Final Report.” Cambridge, MA: Mathematica Policy Research, May 2003.
Families USA. “Express Lane Eligibility: Early State Experiences and Lessons for Health Reform.” Washington, D.C., January 2011. Available at www.familiesusa.org/assets/pdfs/chipra/Express-Lane-Eligibility-State-Experiences.pdf. Accessed August 2, 2011.
Hoag, Sheila, Mary Harrington, Cara Orfield, Victoria Peebles, Kimberly Smith, Adam Swinburn, Matthew Hodges, Kenneth Finegold, Sean Orzol, and Wilma Robinson. “Children’s Health Insurance Program: An Evaluation (1997–2010). Interim Report to Congress.” Ann Arbor, MI: Mathematica Policy Research, December 21, 2011. Available at: http://aspe.hhs.gov/health/reports/2012/CHIPRA-IRTC/index.shtml. Accessed January 8, 2012.
Kaiser Family Foundation. “Medicaid’s Continuing Crunch in a Recession: A Mid-Year Update for State FY 2010 and Preview for FY 2011.” Washington, DC: Kaiser Family Foundation, February 2011. Available at www.kff.org/medicaid/upload/8049.pdf. Accessed December 8, 2011.
Kaiser Family Foundation. “State Health Facts Web Page.” Available online at www.statehealthfacts.org/comparemaptable.jsp?ind=898&cat=4&sub=195&rgnhl=2. Accessed August 2, 2011.
Kenney, Genevieve M., Victoria Lynch, Allison Cook, and Samantha Phong. “Who and Where Are the Children yet to Enroll in Medicaid and the Children’s Health Insurance Program?” Health Affairs, vol. 29, no. 10, October 2010, pp. 1920–1929.
Laibson, David. “Impatience and Savings.” NBER Reporter, Research Summary. Cambridge, MA: National Bureau of Economic Research, fall 2005. Available online at http://www.nber.org/reporter/fall05/laibson.html. Accessed July 31, 2011.
Leavitt, Mike. “Express Lane SCHIP.” In Secretary Mike Leavitt's Blog. October 31 2007. Available at http://archive.hhs.gov/secretarysblog/my_weblog/2007/10/express-lane-sc.html. Accessed July 31, 2011.
Robert Wood Johnson Foundation and State Health Access Data Center. “Reaching Uninsured Children: Iowa’s Income Tax Return and CHIP Project.” Minneapolis, MN: State Health Access Data Assistance Center, August 2010. Available online at www.childrenspartnership.org/AM/Template.cfm?Section=State_Activity_Report&TEMPLATE=/CM/ContentDisplay.cfm&CONTENTID=14979. Accessed August 2, 2011.
Robert Wood Johnson Foundation and State Health Access Data Center. “Using Information from Income Tax Forms to Target Medicaid and CHIP Outreach: Preliminary Results of the Maryland Kids First Act.” Minneapolis, MN: State Health Access Data Assistance Center, September 2009. Available online at www.childrenspartnership.org/AM/ Template.cfm?Section=State_Activity_Report&TEMPLATE=/CM/ContentDisplay.cfm&CONTENTID=13839. Accessed August 2, 2011.
APPENDIX A
Example of Memorandum of Understanding for Study of Costs, Enrollment, and Utilization
This page has been left blank for double-sided copying.
MEMORANDUM OF
UNDERSTANDING
CHIPRA
Express Lane eligibility evaluation
(MOU No. 06988SXXXXXXX)
This memorandum of understanding (MOU) outlines an agreement between the [state] [relevant department] (XYZ) and Mathematica Policy Research regarding XYZ’s participation in the 2011–2013 congressionally mandated evaluation of Express Lane Eligibility (ELE) being conducted by Mathematica and its partners, the Urban Institute and Health Management Associates (HMA), for the Office of the Assistant Secretary for Planning and Evaluation (ASPE) of the U.S. Department of Health and Human Services (HHS) under contract number HHSP23320095642WC/ HHSP23337026T. A description of the evaluation is provided in Attachment A. In this MOU, XYZ and Mathematica may be referred to individually as a Party or jointly as the Parties. Mathematica and its subcontractors are referred to collectively as the Research Team.
This MOU describes in general terms the types of data and access to program staff that XYZ agrees to provide to the Research Team, the time frames within which the data or access will be provided, and the payments that will be made to XYZ by Mathematica in compensation for the costs of data provision. The particular documents and data elements not described in this MOU that will be provided by XYZ, as well as procedures for securely transmitting the documents and data to the Research Team, will be specified by Mathematica in consultation with XYZ at a later date.
1. Cost and Enrollment Study
Program Enrollment Data [Version for Iowa, Maryland, New Jersey, and Oregon]
XYZ agrees to complete [Specified Tables], which request aggregate demographic characteristics and retention outcomes for [Children’s Health Insurance Program [CHIP], Medicaid, and Medicaid Expansion—select as appropriate] beneficiaries enrolling through ELE and non-ELE mechanisms, by [DATE]. The tables are provided and should be returned as Microsoft Excel files.
In addition, XYZ understands that the Research Team will need access to individual-level data to complete analyses planned for the second year of the evaluation. To minimize the burden on XYZ, the Research Team will first seek to acquire necessary data through the Medicaid Statistical Information System (MSIS). In the event the state does not report data into MSIS that would support the evaluation, or that MSIS data are not sufficiently timely, XYZ will provide individual-level claims and enrollment data to the Research Team by [DATE]. It is anticipated that the requested data elements will be similar to those needed to complete the aggregate data tables prepared during the first year of the evaluation. In the event the Research Team requires individual-level data from the state, XYZ will work with Mathematica to amend this MOU to specify the transfer and use of those data files.
Program Enrollment Data [Version for Alabama and Louisiana]
XYZ agrees to amend, by [DATE], the [data use agreement, data sharing agreement] used for the Maximizing Enrollment for Kids Evaluation (MaxEnroll), dated [insert date], between Mathematica Policy Research and XYZ. The amendment will have the effect of enabling Mathematica to use the data, as described in the MaxEnroll Agreement, for the CHIP Reauthorization Act of 2009 (CHIPRA) Express Lane Eligibility Evaluation. XYZ agrees to provide the Research Team access to the appropriate technical staff for assistance related to use of these data.
In addition, XYZ understands that the Research Team will need access to individual-level data to complete analyses planned for the second year of the evaluation. To minimize the burden on XYZ, the Research Team will first seek to acquire necessary data through the Medicaid Statistical Information System (MSIS). In the event the state does not report data into MSIS that would support the evaluation, or that MSIS data are not sufficiently timely, XYZ will provide individual-level claims and enrollment data to Mathematica by [DATE]. In the event the Research Team requires new, individual-level data from the state, XYZ will work with Mathematica to amend this MOU to specify the transfer and use of those data files.
Program Cost Information
XYZ agrees to participate, by [DATE], in consultations with the Research Team regarding standard enrollment processes; ELE enrollment processes; start-up costs associated with ELE; and the differences in time and direct expenditures associated with an ELE application compared with standard application processes. Staff whose input might be requested include those working in policy, eligibility, information technology, and human resources.
XYZ further agrees to review the Research Team’s summary of enrollment process changes and associated costs and savings, based on the above consultations, and to provide any comments and data that are otherwise missing from the summary. XYZ agrees to perform this review within two weeks of receiving the summary from the Research Team.
XYZ agrees to participate in additional consultations, between [DATES], to update program cost data gathered during the first year of the evaluation.
Access to XYZ Staff
XYZ agrees to give the Research Team access to [CHIP, Medicaid and Medicaid Expansion] program staff for telephone and email follow-up after data provision, as necessary between [DATES].
Data Confidentiality
The Research Team will protect the confidentiality of information provided by XYZ, or to which the Research Team obtains access by virtue of its performance under this MOU, that either has been identified as confidential by XYZ or by its nature warrants confidential treatment. The Research Team will use such information only for the purpose for which it was provided and will not disclose it to anyone except those of its employees who need to know the information. These nondisclosure obligations will not apply to information that is or becomes public through no breach of this MOU; that is received from a third party which the recipient believes had the right to disclose the information; or that is required by law, regulation, or subpoena to be disclosed.
In the event XYZ is asked to provide an individual-level data set to the Research Team for the second year of the evaluation, Mathematica will work with relevant state officials to amend this MOU to specify the transfer and use of claims and enrollment data files. Mathematica will ensure all information, records, data, and data elements pertaining to applicants and recipients of [CHIP, Medicaid, and Medicaid Expansion], or to providers, facilities, and associations, will be protected by Mathematica, its employees, its subcontractors, and their employees from unauthorized disclosure in accordance with XYZ policies established pursuant to 42 USC 1396(a)(7) and 42 CFR Part 431, Subpart F and section 457.1110.
Confidential information will be returned to XYZ upon written request. ASPE has required that all data collected during the course of the evaluation will be property of the Federal Government. The Research Team will provide ASPE the information used to generate tables and analysis in reports, all data collected under this contract, and all programs used to analyze the data, except data containing personally identifiable information, which will be will be disposed of at the conclusion of the project in accordance with instructions provided by XYZ.
Payment Schedule
Mathematica agrees to compensate XYZ a total of [insert amount] for the cost of providing data and other information as described in this section. In the event XYZ documents additional costs above this total amount, some additional funds are available to reimburse excess costs. XYZ understands that the state cannot request administrative funding under Medicaid or CHIP for the time and resources expended that were reimbursed through this evaluation.
Payment will be made to XYZ within one month of submitting complete versions of data required by this MOU, according to the following payment schedule.
Schedule for Iowa, Maryland, New Jersey, Oregon
Data Element |
Expected Date |
Payment Amount |
Aggregate Enrollment and Retention Data Tables and Program Cost Data |
[TBD] |
$35,000 |
Individual-Level Claims and Enrollment Data (if MSIS is unsuitable)* and Program Cost Data Update |
[TBD] |
$15,000 |
|
TOTAL |
$50,000 |
*In the event MSIS data are deemed sufficient for the evaluation, the state will still receive the $15,000 payment for providing the Program Cost Data update.
TBD = to be determined.
Schedule for Alabama and Louisiana
Data Element |
Expected Date |
Payment Amount |
Program Cost Data |
[TBD] |
$5,000 |
Individual-Level Claims and Enrollment Data (if MSIS is unsuitable)* and Program Cost Data Update |
[TBD] |
$15,000 |
|
TOTAL |
$20,000 |
*In the event MSIS data are deemed sufficient for the evaluation, the state will still receive the $15,000 payment for providing the Program Cost Data update.
TBD = to be determined.
2. Case Study
2.1 Access to XYZ Staff
XYZ agrees to give the Research Team access to [CHIP, Medicaid, and Medicaid Expansion] program staff for the following:
Assistance between [DATES] with identifying and accessing documents describing XYZ’s ELE program and aspects of ELE policy in [state name].
Assistance between [DATES] identifying key informants able and willing to participate in site visits at the state and local levels. State-level key informants will include those staff responsible for administering CHIP and Medicaid, including program directors, key ELE design and implementation staff, Express Lane Partner Agency officials, legislative staff, and family and child advocates. Local-level key informants will include county social services administrators, frontline eligibility workers, local Express Lane agency staff, and community-based outreach organizations.
In-person interviews with approximately 15 state- and local-level staff during a three-day site visit between [DATES]. State-level staff will be interviewed about topics including the establishment and implementation of ELE programs and policies, challenges encountered, and innovations implemented to overcome these challenges. Local-level staff will be interviewed about topics including their experiences concerning ELE implementation processes and the changes that ELE has introduced for consumers.
Assistance, between [DATES], in constructing sample frames for two focus groups with parents of [CHIP, Medicaid, and Medicaid Expansion] ELE enrollees. Each focus group will require 10 parents, each representing one family. One focus group will be for people residing in the state capital, the other for people residing outside the state capital, both at locations to be determined with assistance from XYZ. Topics for discussion at focus groups include parents’ experiences with outreach; ELE enrollment experiences; non-ELE enrollment experiences; and experiences before ELE implementation.
Telephone follow-up as necessary between [DATES].
Points of Contact.
Each Party hereby designates in writing one or more individuals within their own organization as their point of contact responsible for managing performance of the Parties’ necessary functions and responsibilities under this Memorandum of Understanding.
For “XYZ”: (name, title, phone number, email address)
For Mathematica: (name, title, phone number, email address)
Amendment.
This Memorandum of Understanding may be amended at any time by mutual consent of the Parties. All amendments will be in writing and signed by the authorized signatory of each Party.
Term.
This Memorandum of Understanding is effective as of the date last signed below and shall terminate on ___________________, unless amended in a writing signed by both Parties.
______________________________ _______________________________
Name and Date Name and Date
______________________________ _______________________________
Title Title
For XYZ For Mathematica Policy Research
ATTACHMENT A
DESCRIPTION OF THE CHIPRA-MANDATED EXPRESS LANE ELIGIBILITY EVALUATION
A research project of Mathematica Policy Research, the Urban Institute, and Health Management Associates
under contract to the Assistant Secretary for Planning and Evaluation (ASPE),
U.S. Department of Health and Human Services (HHS)
As part of the Children’s Health Insurance Program Reauthorization Act of 2009 (CHIPRA), Congress gave states the option to implement a new policy known as Express Lane Eligibility (ELE). With ELE, a state’s Medicaid and/or Children’s Health Insurance Program (CHIP) can rely on another agency’s eligibility findings to qualify children for health coverage, despite their different methods of assessing income or otherwise determining eligibility. ELE thus gives states another way to try to enroll and retain children who are eligible for Medicaid and CHIP but remain uninsured, including children who have traditionally been most difficult to reach.
CHIPRA authorized an extensive, rigorous evaluation of ELE. The Assistant Secretary for Planning and Evaluation (ASPE) of the U.S. Department of Health and Human Services (HHS) has contracted with Mathematica Policy Research and its subcontractors, the Urban Institute and Health Management Associates (HMA), to conduct an independent evaluation of ELE in Medicaid and CHIP programs. As the first major federal project to study ELE, this two-year evaluation will document the current implementation of ELE; assess its progress and potential for expanding coverage and reducing administrative costs; examine how its benefits and costs compare with those of other strategies states have used to simplify enrollment and enhance outreach; and identify and share lessons, best practices, promising approaches, and areas for improvement.
Key questions to be addressed by this evaluation. (1) To what extent does ELE increase enrollment of eligible, uninsured children? (2) Has ELE adoption facilitated readiness for the upcoming Medicaid expansion? (3) What are the administrative costs or savings from ELE-based enrollment? (4) What are recommendations for improving ELE effectiveness? (5) What ELE practices proved most effective in enrolling and retaining children? (6) What barriers to enrollment and retention remain in ELE states? (7) What streamlined enrollment approaches/processes are states pursuing other than ELE? (8) How do these alternative (non-ELE) approaches compare with ELE in terms of implementation, administrative complexity, and enrollment gains? (9) How do these alternative (non-ELE) approaches compare with ELE in terms of administrative cost savings? (10) What barriers to enrollment and retention remain in non-ELE states?
Evaluation overview. The project will draw information from a variety of sources, including an analysis of state administrative cost and enrollment data, quarterly monitoring and tracking of 30 states, a 50-state program administrators’ online survey, and 14 case studies. The case studies will include all eight states with approved and implemented ELE programs as well as six states with exceptionally strong or innovative (non-ELE) enrollment or retention programs. The evaluation will yield two major Reports to Congress that will synthesize findings from the data collection and analysis activities, summarize and incorporate themes that emerge across the different evaluation components, and offer insights on public policy implications and policy recommendations.
Key project staff. Sheila Hoag of Mathematica Policy Research is the project director. Other Mathematica staff include Marian Wrobel, Christopher Trenholm, Maggie Colby, Kristina Rall, Sean Orzol, Cara Orfield, Matt Hodges, Vivian Byrd, Adam Swinburn, and Sloane Frost. Urban Institute staff include Ian Hill, Genevieve Kenney, Stan Dorn, Fredric Blavin, Sarah Benatar, Fiona Adams, and Brigette Courtot. HMA staff include Jennifer Edwards, Rebecca Kellenberg, Eileen Ellis, Esther Reagan, and Sharon Silow-Carroll. Carrie Shelton and Rose Chu are the co-project officers at HHS/ASPE.
_____________________________________________________________________________________
HHS/ASPE Mathematica Policy Research Urban Institute Health Management Associates
200 Independence Avenue, SW 600 Alexander Park 2100 M Street, N.W. 1133 Avenue of the Americas, Suite 2810
Washington, DC 20201 Princeton, NJ 08540 Washington, DC 20037 New York, NY 10036
202.690.6870 609.799.3535 202.833.7200 212.575.5929
www.aspe.hhs.gov www.mathematica-mpr.com www.urban.org http://www.healthmanagement.com/
APPENDIX B
Example of Table Shells for Study of Costs, Enrollment, and Utilization
This page has been left blank for double-sided copying.
Table B.1. New [Medicaid/CHIP] Enrollees by Month, [Express Lane Eligibility/Non-ELE]
|
START |
|
ELE Implementation |
|
|
|
End |
|
Month 1 |
Month 2… |
…Month 13 |
Month 14 |
Month 15 |
Month
16+ |
Dec-11 |
Number of New Enrollees |
|
|
|
|
|
|
|
By Subgroup Demographic Characteristics |
|
|
|
|
|
|
|
Age of Child at Start of Month |
|
|
|
|
|
|
|
Younger than 1 |
|
|
|
|
|
|
|
1-5 |
|
|
|
|
|
|
|
6-12 |
|
|
|
|
|
|
|
13-18 |
|
|
|
|
|
|
|
19-21 |
|
|
|
|
|
|
|
Unknown |
|
|
|
|
|
|
|
Race/Ethnicity |
|
|
|
|
|
|
|
Hispanic NH American Indian and NH Alaska Native NH Asian, NH Native Hawaiian and Other Pacific Islander |
|
|
|
|
|
|
|
NH Black NH White |
|
|
|
|
|
|
|
Other |
|
|
|
|
|
|
|
Unknown |
|
|
|
|
|
|
|
Gender |
|
|
|
|
|
|
|
Female |
|
|
|
|
|
|
|
Male |
|
|
|
|
|
|
|
Unknown/ Other |
|
|
|
|
|
|
|
Primary Language |
|
|
|
|
|
|
|
English |
|
|
|
|
|
|
|
Spanish |
|
|
|
|
|
|
|
Other non-English |
|
|
|
|
|
|
|
Unknown |
|
|
|
|
|
|
|
U.S. Citizenship |
|
|
|
|
|
|
|
Citizen |
|
|
|
|
|
|
|
Qualified noncitizen |
|
|
|
|
|
|
|
Nonqualified noncitizen |
|
|
|
|
|
|
|
Awaiting confirmation |
|
|
|
|
|
|
|
Other |
|
|
|
|
|
|
|
Unknown |
|
|
|
|
|
|
|
Household Income by FPL |
|
|
|
|
|
|
|
< 100% |
|
|
|
|
|
|
|
100-< 133 |
|
|
|
|
|
|
|
133-< 185 |
|
|
|
|
|
|
|
185-< 200 |
|
|
|
|
|
|
|
200- < 300 |
|
|
|
|
|
|
|
300 + |
|
|
|
|
|
|
|
Unknown |
|
|
|
|
|
|
|
Residence |
|
|
|
|
|
|
|
Urban |
|
|
|
|
|
|
|
Rural |
|
|
|
|
|
|
|
Unknown |
|
|
|
|
|
|
|
Family Size |
|
|
|
|
|
|
|
2 |
|
|
|
|
|
|
|
3 |
|
|
|
|
|
|
|
4 |
|
|
|
|
|
|
|
5 |
|
|
|
|
|
|
|
6 or more |
|
|
|
|
|
|
|
Unknown |
|
|
|
|
|
|
|
Number of Children in Household |
|
|
|
|
|
|
|
1 |
|
|
|
|
|
|
|
2 |
|
|
|
|
|
|
|
3 |
|
|
|
|
|
|
|
4 or more |
|
|
|
|
|
|
|
Unknown |
|
|
|
|
|
|
|
Number with a TANF Flag |
|
|
|
|
|
|
|
Number with Parent/Caregiver Employment |
|
|
|
|
|
|
|
Private
Insurance Coverage |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Number with Coverage available from employer (if available) |
|
|
|
|
|
|
|
Number with recent loss of private coverage, (if available ) |
|
|
|
|
|
|
|
Prior Public Coverage |
|
|
|
|
|
|
|
Number with a previous spell of public coverage, past 3 month |
|
|
|
|
|
|
|
Number with a previous spell of public coverage, past 6 months |
|
|
|
|
|
|
|
Number with a previous spell of public coverage, past 12 months |
|
|
|
|
|
|
|
ELE = Express Lane Eligibility; FPL = federal poverty level; NH = Non-Hispanic; TANF = Temporary Assistance for Needy Families.
Table B.2. New [Medicaid/CHIP] Enrollees Retention Measures, [Express Lane Eligibility/Non-ELE]
|
START |
|
Month When ELE Is First Implemented |
|
|
|
|
End |
|
Month 1 |
Month 2… |
…Month 13 |
Month 14 |
… |
|
…Month
24+ |
Dec 11 |
Number of New Enrollees |
|
|
|
|
|
|
|
|
Likelihood of Retention |
|
|
|
|
|
|
|
|
Number still enrolled 6 months from enrollment |
|
|
|
|
|
|
|
|
Number still enrolled 12 months from enrollment |
|
|
|
|
|
|
|
|
Number still enrolled 13 months from enrollment |
|
|
|
|
|
|
|
|
Number still enrolled 18 months from enrollment |
|
|
|
|
|
|
|
|
Number still enrolled 24 months from enrollment |
|
|
|
|
|
|
|
|
Disenrollment/Reenrollment Measures |
|
|
|
|
|
|
|
|
Number disenrolled (within 6 months) |
|
|
|
|
|
|
|
|
Number disenrolled (within 12 months) |
|
|
|
|
|
|
|
|
Number disenrolled (within 13 months) |
|
|
|
|
|
|
|
|
Number disenrolled (within 18 months) |
|
|
|
|
|
|
|
|
Number disenrolled (within 24 months) |
|
|
|
|
|
|
|
|
Number of disenrollees that reenrolled within 3 months |
|
|
|
|
|
|
|
|
Number of disenrollees that reenrolled within 6 months |
|
|
|
|
|
|
|
|
Number of disenrollees that reenrolled within 12 months |
|
|
|
|
|
|
|
|
Number of disenrollees that reenrolled within 3 months via ELE |
|
|
|
|
|
|
|
|
Number of disenrollees that reenrolled within 6 months via ELE |
|
|
|
|
|
|
|
|
Number of disenrollees that reenrolled within 12 months via ELE |
|
|
|
|
|
|
|
|
Transfers |
|
|
|
|
|
|
|
|
Number of enrollees that transferred to [CHIP/ Medicaid] within 3 months |
|
|
|
|
|
|
|
|
Number of enrollees that transferred to [CHIP/ Medicaid] within 6 months |
|
|
|
|
|
|
|
|
Number of enrollees that transferred to [CHIP/ Medicaid] within 12 months |
|
|
|
|
|
|
|
|
Number of enrollees that transferred to [CHIP/ Medicaid] within 3 months via ELE |
|
|
|
|
|
|
|
|
Number of enrollees that transferred to [CHIP/ Medicaid] within 6 months via ELE |
|
|
|
|
|
|
|
|
Number of enrollees that transferred to CHIP with/in 12 months via ELE |
|
|
|
|
|
|
|
|
CHIP = Children’s Health Insurance Program; ELE = Express Lane Eligibility.
www.mathematica-mpr.com
Improving
public well-being by conducting high-quality, objective research and
surveys
Princeton,
NJ ■
Ann Arbor, MI ■
Cambridge, MA ■
Chicago, IL ■
Oakland, CA ■
Washington, DC
Mathematica®
is a registered trademark of Mathematica Policy Research
1 Express Lane agencies include those that determine eligibility for assistance for the following programs: Temporary Assistance for Needy Families; child support enforcement; Medicaid; CHIP; Supplemental Nutrition Assistance Program; school lunch programs; WIC (the health and nutrition program for Women, Infants, and Children; the United States Housing Act of 1937; Head Start; child care under the Child Care and Development Block Grant Act of 1990; the Native American Housing Assistance and Self-Determination Act of 1996; another state government agency that has fiscal liability or legal responsibility for the accuracy of the eligibility determination findings relied on by the state; a public agency that is subject to an interagency agreement limiting the disclosure and use of information disclosed for purposes of determining Medicaid or CHIP eligibility (public agency can include an agency administered by an Indian tribe recognized by the state or federal government that determines eligibility for any of the programs listed above); or a state can obtain and use information directly from state income tax records or returns (Centers for Medicaid and State Operations 2010).
2 See Chapter VII for a complete description of these sources.
3 Cathy Kaufmann, administrator of Oregon Healthy Kids, and Nicole Ravenell Edwards, chief executive officer/president of the Southern Institute on Children and Families, were invited and interested in participating in the TAG but unable to attend the initial meeting. Attendance at the initial meeting was a requirement for TAG participation. In order to capture their perspectives, we conducted separate one-hour interviews with both individuals. The interviews followed the same line of inquiry as the TAG meeting, and we incorporated the comments and ideas expressed during those interviews into the TAG memo and design report.
4 A more thorough description of the meeting was submitted to ASPE in a separate memo.
5 DFFITS (“difference in fit”) is a diagnostic meant to show how influential a point is in a statistical regression.
6 The alternatives would be to select a representative sample of non-ELE states, including states that are considered either strong or weak in this area, or to select a comparison state for each ELE state. We believe both approaches are unsuitable alternatives because this study seeks to examine costs and enrollment for a particular intervention that is an alternative to ELE; thus, selecting a weak outreach state will not help compare alternatives to ELE.
7 The eight program features considered for CHIPRA performance bonus awards are continuous eligibility; liberalization of asset requirements; elimination of in-person interview; use of a joint (same) application and renewal form; auto/administrative renewal; presumptive eligibility; ELE; and premium assistance subsidies.
8 Likewise, although we discussed at the first TAG meeting the use of blended groups, which would include those who came in through the pathway of interest as well as those who came in through other paths, after further thought we believe the disadvantages of blended groups include the potential for confusion in the group and, more importantly, unclear take-away messages about the value of the pathway being studied.
9 The tables are structured to collect Medicaid and CHIP data separately, recognizing that the data systems and availability of variables might differ across the two programs in some states. In states that operate only Medicaid ELE programs, we will request only Medicaid data.
10 TAG members also noted that we should separately consider ELE renewals from new enrollments. We concur with this suggestion; however, to our knowledge, the four states from which we will request aggregate data have not yet implemented renewal-related ELE pathways. In Alabama and Louisiana, states in which we will have access to individual-level data, ELE renewal has played a more prominent role and, subject to data quality constraints, we will examine renewals during the first study year. If we learn that another ELE state has begun ELE renewals, we will separately collect aggregate data for those beneficiaries.
11 We do not expect that MSIS data elements that would allow the identification of ELE enrollees will be available in Iowa and Maryland, and do not have the resources to pursue utilization analyses with claims or encounter data obtained directly from the states.
12 The ELE error rates will not be calculated under this evaluation contract; these will be provided to the evaluation team by CMS.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | Sheila Hoag |
| File Modified | 0000-00-00 |
| File Created | 2021-01-30 |
© 2026 OMB.report | Privacy Policy