Form CMS-10416 Exchange Blueprint Revised
Blueprint for Approval of Affordable State-based and State Partnership Insurance Exchanges
CMS-10416 Exchangeblueprint_081312
Exchange Blueprint
OMB: 0938-1172
Draft Blueprint for Approval of Affordable State-based and State Partnership Insurance Exchanges
Introduction
The Affordable Care Act establishes Affordable Insurance Exchanges (Exchanges) to provide individuals and small business employees with access to health insurance coverage beginning January 1, 2014.1 An Exchange is an entity that both facilitates the purchase of Qualified Health Plans (QHP) by qualified individuals and provides for the establishment of a Small Business Health Options Program (SHOP), consistent with Affordable Care Act 1311(b) and 45 CFR 155.20. Exchanges will provide competitive marketplaces for individuals and small employers to directly compare and purchase private health insurance options based on price, quality, and other factors. Exchanges are integral to the Affordable Care Act’s goal of prohibiting discrimination against people with pre-existing conditions and insuring all Americans.
The Affordable Care Act provides States with significant flexibility in the design and operation of their Exchange to best meet the unique needs of their citizens and their marketplace. States can choose to operate as a State-based Exchange, or the Secretary of the Department of Health & Human Services (HHS) will establish and operate a Federally-facilitated Exchange in any State that does not elect to operate a State-based Exchange. In a Federally-facilitated Exchange, the State may pursue a State Partnership Exchange, where a State may administer and operate Exchange activities associated with plan management and/or consumer assistance. States that elect to participate in a State Partnership Exchange will administer these functions in both the individual and the small group market.
Regulations implementing the Affordable Care Act require HHS to Approve or Conditionally Approve State-based Exchanges no later than January 1, 2013, for operation in 2014. In addition, the Affordable Care Act 1321(c)(1) (B)(ii)(I) directs the Secretary to make a determination regarding whether the State will operate reinsurance and/or risk adjustment programs or will use Federal government services for these activities. To receive HHS Approval or Conditional Approval for a State-based Exchange or a State Partnership Exchange, as well as reinsurance and risk adjustment programs2, a State must complete and submit an Exchange Blueprint that documents how its Exchange meets or will meet all legal and operational requirements associated with the model it chooses to pursue. As part of its Exchange Blueprint, a State will also demonstrate operational readiness to execute Exchange activities.3
Flexible Exchange Options for States
In an effort to provide States with significant flexibility in the development of Exchanges to meet the needs of their citizens, HHS has developed a program that offers multiple Exchange models as well as a number of design alternatives within each model. A State also has the flexibility to transition between models annually (see page 4 for details). See Figure 1 for a representation of the Exchange models and flexibility within those models.
Figure 1: Flexible Exchange Options for States
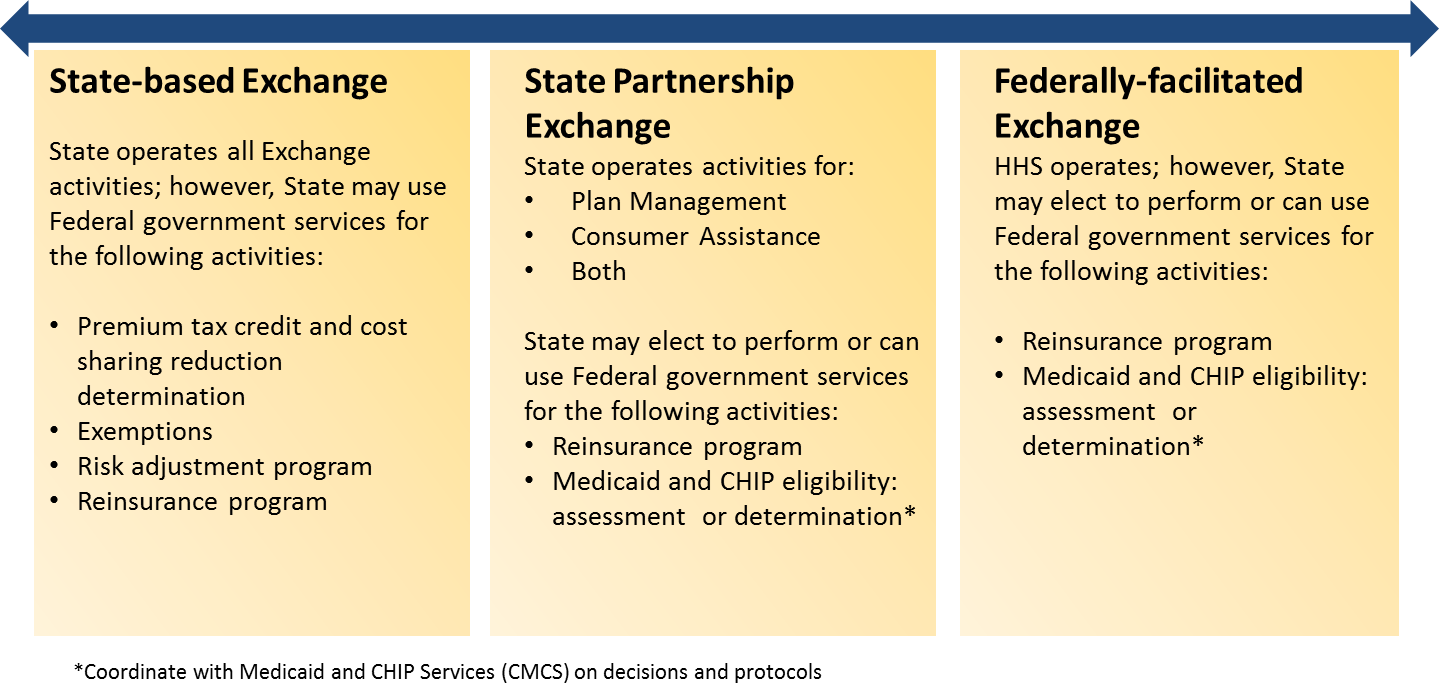
Exchanges will operate either as a State-based Exchange or a Federally-facilitated Exchange. A State may also operate in partnership with HHS as a State Partnership Exchange, which provides States with the option to administer and operate Exchange activities associated with plan management activities, some consumer assistance activities, or both. HHS, as the party responsible for Exchange implementation, will provide as much flexibility as possible; however, HHS will need to ratify inherently governmental decisions made by the State Partner.
Technical Assistance and Establishment Grant funding under Section 1311(a) of the Affordable Care Act continues to be available to States through 2014 for State-based Exchanges, State Partnership Exchanges, and States that are building linkages to the Federally-facilitated Exchange.4
State-based Exchange
The Exchange final rule outlines the activities required to operate a State-based Exchange. Within the required activities, a State-based Exchange has additional operational flexibility. It may choose to use Federal government services for the following activities:
Determination of advance premium tax credit (APTC) and cost sharing reduction (CSR)
Individual responsibility requirement and payment exemption as defined in future rulemaking and guidance
Reinsurance
Risk adjustment
State Partnership Exchange
States have the option to operate as a State Partnership with HHS to administer and operate select Exchange activities. Specifically, a State Partnership Exchange may assume primary responsibility for activities including:
Plan Management. In a Plan Management Partnership, a State will conduct all analyses and reviews necessary to support QHP certification, collect and transmit necessary data to HHS, and manage certified QHPs.
Consumer Assistance. In a Consumer Assistance Partnership, a State will provide in-person application and other assistance to consumers. In-person assistance may include supporting consumers in filing an application, obtaining an eligibility determination or reporting a change in status, comparing coverage options, and selecting and enrolling in a QHP.
Both Plan Management and Consumer Assistance. In a Plan Management and Consumer Assistance Partnership, a State will perform all of the Partnership activities described above.
In addition to Plan Management and Consumer Assistance Partnership activities, Partnership States may elect to perform the following Exchange activities:
Reinsurance
Medicaid and CHIP eligibility: A State may coordinate with the Center for Medicaid and CHIP Services (CMCS) on decisions and protocols for either an assessment or determination model for eligibility in the Exchange
Federally-facilitated Exchange without Partnership
For States that do not seek to operate a State-based Exchange or a Partnership with the Federally-facilitated Exchange, HHS will establish and operate a Federally-facilitated Exchange. In such instances, a State may elect to run reinsurance and may elect to coordinate with CMCS on decisions and protocols for either an eligibility assessment or eligibility determination model in the Federally-facilitated Exchange.
Regardless of a State’s Exchange model, HHS intends to work in collaboration with States, where appropriate, to ensure the best, most effective experience for the State and its residents.
Overview of Exchange Approval Requirements
HHS may approve States that seek to operate a State-based Exchange or participate in a State Partnership Exchange based upon a State’s submission of its Blueprint. A Blueprint is made up of two components:
Declaration Letter (Section 1)
Exchange Application (Section 2)
States seeking to operate a State-based Exchange or electing to participate in a State Partnership Exchange must submit a complete Exchange Blueprint no later than 30 business days prior to the required approval date of January 1 (November 16, 2012, for plan year 2014).
A State may submit its Declaration Letter at any time prior to this deadline. If a State’s Declaration Letter is received more than 20 business days prior to the submission of its Blueprint, the State may request an Exchange Application consultation with CMS regarding preparation of its Application for Approval as a State-based Exchange or State Partnership Exchange.
States that plan to operate in the Federally-facilitated Exchange without Partnership that intend to operate their own reinsurance programs should submit a declaration letter addressing how they meet or will meet the requirements of Section 5.2: reinsurance and are invited to submit a Declaration Letter otherwise but do not need to complete the Exchange Application.
In particular, HHS strongly encourages States that are considering operating a State-based Exchange or a Plan Management Partnership to submit the Declaration Letter as soon as possible and to seek technical assistance and consultation with HHS to ensure State readiness to operate Plan Management activities in time for operational implementation.
States that seek HHS Approval to operate a State-based Exchange or State Partnership Exchange for coverage years beginning after January 1, 2014 (e.g., January 1, 2015, January 1, 2016) should submit an Exchange Blueprint in accordance with the same process and timeframe specified for those States seeking to operate an Exchange on January 1, 2014, for the applicable year (e.g., November 18, 2013, for plan year 2015, November 18, 2014, for plan year 2016)
Initial Exchange Approval Determinations
HHS will approve a State-based Exchange once the State has demonstrated the ability to satisfactorily perform all required Exchange activities.
HHS recognizes that States depend on HHS and other Federal Agencies for guidance associated with their Exchange establishment. In this regard, particularly in the first year of the program (plan year 2014), approval of State-based Exchanges will take into account timelines for guidance and infrastructure development (e.g., Data Services Hub). Similarly, HHS expects that States will be in various stages of the Exchange development lifecycle when Blueprints are submitted. Many State Exchange development activities are likely to occur in 2013. HHS will utilize Conditional Approval for State-based Exchanges and Partnership States whose Exchange establishment is not complete at the time of Blueprint submission.
Conditional Approval will be granted for State-based Exchanges and Partnership Exchanges that do not meet all Exchange Approval requirements on January 1, 2013, but are making significant progress toward these requirements and will be operationally ready for the initial open enrollment period beginning October 1, 2013. HHS will work with each State that receives Conditional Approval to develop a comprehensive agreement that sets out expected future milestones and dates for operational readiness reviews. This will allow HHS and the State to work jointly to ensure that the Exchange continues to develop at a pace on track for operation during the initial open enrollment period beginning on October 1, 2013.
Conditional Approval will continue as long as a State continues to meet expected progress milestones and until a State successfully demonstrates its ability to perform all required Exchange activities. Provided that the State is meeting the milestones outlined in its Conditional Approval determination, a State Exchange can maintain Conditional Approval. In this capacity, an Exchange must be able to:
Provide consumer support for coverage decisions
Facilitate eligibility determinations for individuals
Provide for enrollment in QHPs
Certify health plans as QHPs
Operate a SHOP
The technical assistance and grant funding available to States prior to Approval or Conditional Approval will continue to be available under the terms and requirements of those programs.
Questions Regarding the Exchange Blueprint & Technical Assistance
States should contact their CMS Center for Consumer Information and Insurance Oversight (CCIIO) State Officer for specific questions regarding their Exchange Blueprints. In addition, all States are encouraged to contact CCIIO’s State Exchange Group for information regarding technical assistance consultations, available resources, and funding opportunities available to States for Exchange build activities. General questions may be directed to [email protected].
Disclosure: According to the Paperwork Reduction Act (PRA), no persons are required to respond to a collection of information unless it displays a valid Office of Management and Budget (OMB) control number. The valid OMB control number for this information collection is 0938-XXXX. The estimated time required to complete this information collection will average 211 hours per response including the time to review instructions, search existing data resources and gather the data needed, and complete and review the information collection. If you have any comments concerning the accuracy of the time estimate or suggestions for improving this form, please write to: CMS, Office of Strategic Operations and Regulatory Affairs, Division of Regulations Development, Attention: Document ID: CMS-10416, Room C4-26-06, 7500 Security Boulevard, Baltimore, Maryland 21244-1850.
Section I: Declaration Letter
A State seeking to operate a State-based Exchange or participate in a State Partnership Exchange in plan year 2014 will declare the type of Exchange Model it intends to pursue through an Exchange Declaration Letter as part of its Exchange Blueprint. States that plan to operate in the Federally-facilitated Exchange without Partnership that intend to operate their own reinsurance programs should submit a declaration letter addressing how they meet the requirements of Section 5.2: reinsurance. To facilitate coordination, States seeking to participate in a Federally-facilitated Exchange without Partnership and not electing to operate reinsurance are also invited, at their option, to complete a Declaration Letter.
A State’s Declaration Letter must be signed by the State’s Governor5. As described below, the Letter’s contents should include basic information associated with its designated Exchange Model. The Letter should include a designation of the individual(s) (Designee (s) who should serve as the primary point of contact for HHS regarding the Exchange. The individual(s) should be authorized to bind the State regarding the State’s Exchange, as well as to complete and sign the Exchange Application. In the case of State-based Exchanges and State Partnership Exchanges, this should be the individual(s) authorized to electronically attest to the facts in the Exchange Application.
States are encouraged to submit their Exchange Declaration Letters early, but a Declaration Letter must be sent to the Centers for Medicare & Medicaid Services (CMS) Center for Consumer Information and Insurance Oversight (CCIIO) at least 30 business days prior to the required Approval date of January 1 (November 16, 2012, for plan year 2014). Declaration Letters may be sent to the CMS Center for Consumer Information and Insurance Oversight (CCIIO), 200 Independence Avenue SW, Suite 739H, Washington DC, 20201. In addition, please email a copy to the [email protected]. To support HHS’ goal of public transparency, States must post their Model Declaration Letter to the State (or other appropriate) website
Contents of Exchange Declaration Letters
A State’s Declaration Letter must include the following contents based on the Exchange Model that the State chooses to pursue.
State-based Exchange
Confirmation of the State’s intention to apply to operate a State-based Exchange
Indication of whether the State intends to administer a risk adjustment program in the first year of operations or if it will be using Federal government services. If yes,
What is the State’s risk adjustment entity?
Is the State planning to use the Federal risk adjustment methodology?
What is the proposed data model (i.e., intermediate or distributed)?
Indication of whether the State intends to administer its own reinsurance program by establishing or contracting with a nonprofit reinsurance entity. If yes, provide the name of the selected entity.
Indication of whether the State-based Exchange will perform its Advance Premium Tax Credit (APTC)/Cost-Sharing Reduction (CSR) eligibility determinations or if it will use Federal government services for this activity.
Designation of the individual(s) (Designee) authorized to act as primary point of contact and authorized to bind the State with HHS regarding the State’s Exchange, as well as to complete and sign the Exchange Application.
State Partnership Exchange
Confirmation of the State’s intention to participate in a State Partnership Exchange, including which Partnership the State intends to pursue:
Plan Management
Consumer Assistance
Plan Management and Consumer Assistance
Indication of whether the State intends to administer its own reinsurance program by establishing or contracting with a nonprofit reinsurance entity. If yes, provide the name of the selected entity.
Designation of the individual(s) (Designee) authorized to act as primary point of contact and authorized to bind the State with HHS regarding the State’s Exchange, as well as to complete and sign the Exchange Application. The State Medicaid Director will be assumed to be the primary contact on issues related to eligibility determination and coordination unless otherwise indicated by State Governor or the authorized personnel in the Declaration Letter. In States with separate CHIP programs, the State’s CHIP Director will be assumed to serve as the point of contact for CHIP-related eligibility issues unless otherwise indicated.
Federally-facilitated Exchange
Confirmation of the State’s intention to elect for the Secretary to establish and operate a Federally-facilitated Exchange.
Designation of the State agency or official who is authorized by the State to collaborate with HHS on issues related to Exchange issues in the Federally-facilitated Exchange in that State. The State Medicaid Director will be assumed to be the primary contact on issues related to eligibility determination and coordination unless otherwise indicated by State Governor or the authorized personnel in the Declaration Letter. In States with separate CHIP programs, the State’s CHIP Director will be assumed to serve as the point of contact for CHIP-related eligibility issues unless otherwise indicated.
Indication of whether the State intends to administer its own reinsurance program by establishing or contracting with a nonprofit reinsurance entity. If yes, indicate how the State meets or will meet the requirements of Section 5.2: reinsurance.
If a Declaration Letter is not received 30 business days prior to January 1, 2013 (November 16, 2012), HHS will plan to implement a Federally-facilitated Exchange for the State. In the absence of a Declaration Letter, HHS will operate a Federally-facilitated Exchange for the State under the following assumptions:
The State will not administer its own reinsurance program;
The State’s small group and individual markets will be merged in the Federally-facilitated Exchange only if the current individual and small group markets are merged. If a State does not merge the individual and small group market risk pools, the SHOP will permit each qualified employee to enroll only in QHPs in the small group market; and
The State’s current definition of “small group” employer (i.e., up to 50, or up to 100 employees) will be followed, while the method of determining employer size will be based on full-time equivalent employees consistent with other Affordable Care Act policies.
Section II: Application for Approval of Affordable State-based and State Partnership Insurance Exchanges
Table of Contents
State Background Information for Application Submission 18
1.0 Legal Authority and Governance 19
2.0 Consumer and Stakeholder Engagement and Support 21
3.0 Eligibility and Enrollment 26
5.0 Risk Adjustment and Reinsurance 37
6.0 Small Business Health Options Program (SHOP) 38
7.0 Organization and Human Resources 40
11.0 Oversight and Monitoring 42
The Exchange Application must be completed online. Beginning September 14, 2012, the Exchange Application will be available for online completion and submission on CMS’ Center for Consumer Information and Insurance Oversight’s (CCIIO) State Exchange Resource and Virtual Information System (SERVIS) system https://servis.cms.gov.6 The online Exchange Application has been designed so only the questions relevant to the Exchange Model the State has selected will be presented to the applicant.
Application Instructions
Introduction
In addition to a Declaration Letter, a complete Exchange Blueprint requires submission of an Exchange Application. This Exchange Application is used to document a State’s completion, or progress towards completion, of all Exchange requirements, either as a State-based Exchange or State Partnership Exchange.
Exchange Application: Overview of Exchange Activities
The Exchange Application is comprised of a list of activities that a State-based Exchange or State Partnership Exchange must perform to comply with the Affordable Care Act and associated regulations. In some instances, a State may use Federal services to perform an Exchange activity. Table 1 outlines all of the Exchange activities that an Exchange must perform and can serve as a roadmap for Exchange development.
States that are seeking Approval of their State-based Exchange or State Partnership Exchange should use Table 1 to complete the Application accordingly. Required activities within an Exchange model are designated with an “X”. Select activities are also described as “if applicable,” “can use Federal government services,” “may elect to perform,” and “optional.” States may attest to activities being completed by the Exchange or a designee – through contract, agreement, or other arrangement; however, the Exchange is ultimately responsible for successful performance of the activity.
Approval requirements for a State Partnership Exchange will mirror State-based Exchange Approval requirements for those activities a State elects to perform within a Federally-facilitated Exchange. Therefore, all States that seek Approval of a State-based Exchange or a State Partnership Exchange can use this list of activities and common elements as part of the Exchange Approval process. The activities associated with the State Partnership Exchanges are similarly designated in Table 1 below.
States that are applying to be State-based Exchanges are also encouraged to complete the subset of activities associated with the Partnership models. By also completing the Partnership activities, a State can assure that if it receives Conditional Approval but is ultimately unable to achieve operational milestones in other areas it will be able to participate as aState Partnership Exchange in pan year 2014.
If you are interested in additional requirements associated with a Regional or Subsidiary Exchange, please contact your State Officer or email CCIIO at [email protected].
Table 1: Roadmap for Completing the Exchange Application
Section of Exchange Blueprint |
Required Activities |
|||
Exchange
Activity |
State-based Exchange |
State Partnership Exchange– Plan Management |
State Partnership Exchange– Consumer Assistance |
|
|
||||
1.1 Enabling authority for Exchange and SHOP |
X |
|
|
|
1.2 Board and governance structure |
X |
|
|
|
|
||||
2.1 Stakeholder consultation plan |
X |
|
|
|
2.2 Tribal consultation plan |
X |
|
|
|
2.3 Outreach and education |
X |
|
|
|
2.4 Call center |
X |
|
|
|
2.5 Internet web site |
X |
|
|
|
2.6 Navigators |
X |
|
|
|
2.7 In-person assistance program |
X if applicable |
|
|
|
2.8 Agents/brokers |
X |
|
|
|
2.9 Web brokers |
X |
|
|
|
|
||||
3.1 Single streamlined application(s) for Exchange and SHOP |
X |
|
|
|
3.2 Coordination strategy with Insurance Affordability Programs and the SHOP |
X |
|
|
|
3.3 Application, updates, acceptance and processing, and responses to redeterminations |
X |
|
|
|
3.4 Notices, data matching, annual redeterminations and response processing |
X |
|
|
|
3.5 Verifications |
X
|
|
|
|
3.6 Document acceptance and processing |
X |
|
|
|
3.7 Eligibility determination |
X |
|
|
|
3.8 Eligibility determinations for APTC and CSR |
X |
|
|
|
3.9 Applicant and employer notification |
X |
|
|
|
3.10 Individual responsibility requirement and payment exemption determinations |
X |
|
|
|
3.11 Eligibility appeals |
X |
|
|
|
3.12 QHP selections and terminations, and APTC/advance CSR information processing |
X |
|
|
|
3.13 Electronically report results of eligibility assessments and determinations |
X |
|
|
|
3.14 . In accordance with section 155.345(i) of the Exchange Final Rule, the Exchange must follow procedures established in accordance with 45 CFR 152.45 related to the Pre-Existing Condition Insurance Plan (PCIP) transition |
X |
X (as applicable)
|
X (as applicable) |
|
|
||||
4.1 Appropriate authority to perform and oversee certification of QHPs |
X |
X |
|
|
4.2 QHP certification process |
X |
X |
|
|
4.3 Plan management system(s) or processes that support the collection of QHP issuer and plan data |
X |
X |
|
|
4.4 Ensure ongoing QHP compliance |
X |
X |
|
|
4.5 Support issuers and provide technical assistance |
X |
X |
|
|
4.6 Issuer recertification, decertification and appeals |
X |
X |
|
|
4.7 Timeline for QHP accreditation |
X |
X |
|
|
4.8 QHP quality reporting |
X |
X |
|
|
|
||||
5.1 Risk adjustment program |
X |
|
|
|
5.2 Reinsurance program |
X |
X or can use Federal service |
X may elect to perform or can use Federal service |
|
|
||||
6.1 SHOP compliance with 45 CFR 155 Subpart H
|
X |
|
|
|
6.2 SHOP premium aggregation |
X |
|
|
|
6.3 Electronically report results of eligibility assessments and determinations for SHOP |
X |
|
|
|
|
||||
7.1 Organizational structure and staffing resources to perform Exchange activities
|
X |
|
|
|
|
||||
8.1 Long-term operational cost, budget, and management plan |
X |
|
|
|
|
||||
9.1 Compliance with HHS IT Guidance |
X |
X |
|
|
9.2 Adequate technology infrastructure and bandwidth |
X |
X |
|
|
9.3 IV&V, quality management and test procedures |
X |
X |
|
|
|
||||
10.1 Privacy and Security standards policies and procedures |
X |
X |
X (if applicable) |
|
10.2 Safeguards based on HHS IT guidance |
X |
X |
|
|
10.3 Safeguard protections for Federal information |
X |
|
|
|
11.0 Oversight, Monitoring, & Reporting |
||||
11.1 Routine oversight and monitoring of the Exchange’s activities |
X |
X |
X (if applicable) |
|
11.2 Track/report performance and outcomes metrics related to Exchange activities |
X |
X |
X (if applicable) |
|
11.3 Uphold financial integrity provisions including accounting, reporting, and auditing procedures |
X |
X |
X (if applicable) |
|
12.0 Contracting, Outsourcing, and Agreements |
||||
12.1 Contracting and outsourcing agreements |
X |
X |
X (if applicable) |
|
13.0 State Partnership Exchange Activities |
||||
13.1 Plan Management |
Optional |
X |
|
|
13.2 Capacity to interface with the Federally-facilitated Exchange |
Optional |
X |
X |
|
13.3 Consumer Assistance |
Optional |
|
X |
|
Relationship between Exchange Application and the Establishment Grant Review Process
HHS has developed an Establishment Review Process to monitor and assist States that have received grant(s) through the Cooperative Agreements for Establishment of Exchanges under the Affordable Care Act 1311(a). While the Establishment Review Process is intended to support States as they work toward Exchange Approval, the Establishment Review Process is independent of the Exchange Approval process. However, to streamline data collection requirements, HHS has aligned requirements so that a State may utilize information submitted during the Establishment Review Process to complete a State’s Exchange Blueprint. If a State successfully completes a portion of an activity requirement during its Establishment Review, the State may waive out of re-submitting testing files or supporting documentation as part of the Exchange Application requirements. As referenced in the Exchange Application, a State may upload and submit a letter(s) from HHS confirming successful completion of documentation requirements instead of re-submitting documentation.
Completion of the Exchange Application
In completing the Exchange Application, States are asked to submit the elements described below.
Attestations
The individual(s) designated in the Declaration Letter (the Designee(s)) must attest, on behalf of the State, to either completion or expected completion of an Exchange activity. Specifically, the State can attest to their Exchange’s current ability to meet specified Exchange requirements. Alternatively, if the State is unable to meet requirements by the time of the Exchange Application submission date, the State may attest to expected completion andits expected ability to meet the specified activity requirements by a future date.
As appropriate, for attestations related to expected completion, the State should provide a timeline and work plan that includes key milestones, including any vendor-related agreements, so that HHS understands the State’s expected ability to complete the activity by a future date. The State may choose to provide one comprehensive work plan that outlines all applicable activities or a set of work plans that logically bundle activities (e.g., a work plan for all Eligibility activities). However, the work plan(s) must clearly reference the specific activities required as part of the Exchange Application.
Supporting Documentation
For some activities, supporting documentation is required. States must upload requested documentation associated with the Exchange activity. Alternatively a State may submit a letter(s) from HHS confirming successful demonstration of the associated supporting document through the Establishment Review process. In such cases, the State does not need to provide documentation/descriptions, and HHS will confirm the State’s submitted documentation from the Establishment Review.
Testing Files
As part of a standard systems development process, States and their vendors will develop and implement testing and validation plans. For some activities, the Application requires submission of these files.
Three different types of testing files may be required:
Summary of results of State-developed testing: These summaries should document State-defined and executed system testing, including details of Exchange activities tested, the scope of testing activities conducted, and metrics detailing the results of that testing as it relates to each designated Exchange Application requirement.
Results of State execution of HHS-developed test scenarios: HHS, in collaboration with States, developed test scenarios to confirm implementation of those Exchange activities that require standardization across all State Exchanges. These scenarios will be released to a central Test Library on the Collaborative Application Lifecycle Tool (CALT)7. For CALT login and password assistance, please send a request to [email protected].
Summary of Independent Verification & Validation (IV&V) of applicable system components: A report by an independent third party which provides verification and validation that designated Exchange activities are built and operating as designed and in compliance with documented requirements.
Upload Relevant Files
Files are requested to be uploaded, as applicable. The files should be clearly labeled with the appropriate activity or activities). Activities requiring additional documentation in the form of uploaded files are specifically identified in the Exchange Application. Depending on the Exchange activity being tested, a given document or file may encompass multiple activities. In such cases, please note any file cross-referencing and clearly label the activities within the attachments. States do not need to upload the same file multiple times. Instead referencingwill allow HHS to identify files provided, as appropriate.
Supporting Documentation
Testing Files
Letter(s) from HHS allowing an applicant to waive out of any requirements successfully completed in an Establishment Review(s)
Expected Completion Work Plan
Operational Readiness Assessment and Additional Information Requests
In addition to reviewing the completed Exchange Application, HHS may conduct on-site or virtual Exchange assessments as part of its verification of an Exchange’s Operational Readiness. Operational Readiness entails HHS’ and its Federal agency partners’ assessment to determine the capacity of an Exchange to conduct Exchange business. The objective of the Operational Readiness assessment is to assure that an Exchange’s policies, procedures, operations, technology, and other administrative capacities have been implemented and scaled to meet the needs of the State’s Exchange population. HHS will use the information in a State’s Exchange Application, including results from a State’s Testing Files, to determine the need for, and timing of, an on-site or virtual Operational Readiness assessment.
In addition, the State may be asked to provide supplemental information after the Application has been submitted, as determined necessary by HHS and its Federal agency partners.
Public Transparency
The Affordable Care Act envisions a significant role for consumers and other stakeholders in the design, implementation and on-going operations of Exchanges. For example, an Exchange that is an independent State agency or a non-profit established by a State will include consumer representatives on its board and hold regular public governing board meetings. In addition, Exchanges will develop and implement a comprehensive stakeholder engagement plan that includes meaningful engagements with consumers, advocates, employers, and members of Federally-recognized Tribes (where applicable).
In that spirit, as part of a State’s Approval or Conditional Approval decision, States should post the following sections (excluding test data) of a State’s Exchange Application on the appropriate State website within ten (10) business days of an Approval or Conditional Approval decision:
Section 1.2: Exchange board and governance structure
Section 2.1: Stakeholder consultation plan
Section 2.2: Tribal consultation policy
Section 2.3: Outreach and education plan
Section 2.6: Navigators
Section 2.7: Role of in-person assistance programs
Section 2.8: Role of agents and brokers
Section 2.9: Role of web agents and brokers
Section 3.1: State-developed single-streamlined application (if applicable)
Section 3.2: Coordination strategy
Section 3.14: PCIP transition Section 4.4: Integration between Exchange and other State entities with respect to QHP issuer oversight
Section 8.1: Long-term operational cost plan
If a
State is concerned that the publication of the above information may
jeopardize an active procurement process, it may contact their State
Officer or email CCIIO at [email protected]
to discuss the timing of the publication of this information.
Application Format and Availability
The Exchange Application will be electronically available for States to complete on HHS’ Center for Consumer Information and Insurance Oversight’s (CCIIO) State Exchange Resource and Virtual Information System (SERVIS) system https://servis.cms.gov beginning September 14, 2012.
Attestation
ON THIS DATE, I ATTEST THAT THE STATEMENTS AND INFORMATION CONTAINED IN THIS EXCHANGE BLUEPRINT AND DOCUMENTS SUBMITTED IN CONJUNCTION WITH THIS EXCHANGE BLUEPRINT ACCURATELY REPRESENT THE STATUS OF MY STATE’S INSURANCE EXCHANGE BEING DEVELOPED UNDER TITLE I OF THE PATIENT PROTECTION AND AFFORDABLE CARE ACT OF 2010 (Pub. L. 111-148), AS AMENDED BY THE HEALTH CARE AND EDUCATION RECONCILIATION ACT OF 2010 (Pub. L. 111-152), AND REFERRED TO COLLECTIVELY AS THE AFFORDABLE CARE ACT; AND REGULATIONS AT 45 CFR PARTS 153, 155 AND 156.
State: ___________________________________________________________
(Name of State)
________________________________________________________________________
(Signature of Governor Designee of the State, Date Signed)
State Background Information for Application Submission
|
NAME: TELEPHONE: EMAIL ADDRESS:
NAME: TELEPHONE: EMAIL ADDRESS:
|
__STATE-BASED EXCHANGE __STATE PARTNERSHIP EXCHANGE
__PLAN MANAGEMENT
__CONSUMER ASSISTANCE
|
__3.8 Eligibility determinations for APTC and CSR __3.10 Individual responsibility requirements and payment exemption determinations __5.1 Risk adjustment program __5.2 Reinsurance program
|
__5.2 Reinsurance program
|
L |
|
* Supporting Documentation and Testing Files eligible for waive out given an applicant’s successful completion of an Establishment Review(s) |
|
Relevant
File Uploads |
|
Testing Files |
|
Supporting Documentation |
|
Letter(s) from HHS allowing an applicant to waive out of any supporting documentation and/or testing file requirements given successful completion of an activity through Establishment Review(s) |
|
Expected Completion Work Plan and Timeframes
|
|
Please provide any additional comments related to completion of this Application |
|
1 Affordable Care Act 1311(b)(1)
2 Additional requirements for Risk Adjustment will be provided in the HHS Notice of Benefit and Payment Parameters.”
3 45 CFR 155.105, Establishment of Exchanges and Qualified Health Plans; Exchange Standards for Employers, 77 Fed. Reg. 18310, 18446 (Mar. 27, 2012)
4 http://www.grants.gov/search/search.do;jsessionid=0VqkQpTV3Z1fR74Z7rvnwjqf42vlsyw15Qp1FWKbqrQlJ8CQ7zJj!-1406353995?oppId=180734&mode=VIEW
5 CMS has been advised that in some States, the Governor does not have the authority to enter into a State Partnership Exchange. Please contact your CCIIO State Officer if the Governor of your State believes that another entity is the appropriate authority to sign the State’s Model Declaration Letter so that we can work with your State on an appropriate arrangement.
6 SERVIS and the Collaborative Application Lifecycle Tool (CALT) are password protected. To receive a CALT/SERVIS user ID and password please contact [email protected] or [email protected].
7 Test scenarios will be available on the Collaborative Application Lifecycle Tool (CALT) site (https://calt.hhs.gov); a more specific link to the site will be provided at a future date
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| File Title | Draft Blueprint for Approval of Affordable State-based and State Partnership Insurance Exchanges |
| Subject | Affordable Health Care Act |
| Author | Department of Health and Human Services |
| File Modified | 0000-00-00 |
| File Created | 2021-01-30 |
© 2026 OMB.report | Privacy Policy