Final In person interview
The Effect of Reducing Falls on Acute and Long -Term Care Expenses
0990-0308 Appendix C
Final In person interview
OMB: 0990-0308
APPENDIX C
IN-PERSON ASSESSMENT INSTRUMENT
(FOR USE AS BOTH INITIAL AND FINAL ASSESSMENT)
Form Approved
OMB No. 0990-0308
Exp. Date XX/XX/20XX
R
Participant Name:
Address:
Phone Number:
Independent Living and
Mobility Program
In-Person Interview
Assessor – Print your name with credentials and the date that the interview was completed.
Name and credentials:
Date of interview:
Was more than one person in this household interviewed? No Yes
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is 0990-0308. The time required to complete this information collection is estimated to average 1.25 hours per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. If you have comments concerning the accuracy of the time estimate(s) or suggestions for improving this form, please write to: U.S. Department of Health & Human Services, OS/OCIO/PRA, 200 Independence Ave., S.W., Suite 336-E, Washington D.C. 20201, Attention: PRA Reports Clearance Officer



Instructions
Please read this paragraph to the participant before beginning the interview.
My name is ______________, and I will be interviewing you and taking your height, weight and blood pressure readings as part of the Independent Living and Mobility Program.
The interview takes approximately one hour. I will be asking questions about your health and daily activities and will perform a brief home safety evaluation.
I will be asking you questions on a number of different topics. Some of these questions may or may not be applicable to you; but it is important that we ask all participants the same questions.
If this is the initial in-person assessment add:
The information from this interview will be sent to the home office where a report will be created that highlights things you can do to improve your safety and reduce the chance of falling in your home. This report will then be sent to you. Along with the summary, a Health Promotion and Independent Living and Mobility Tool kit will be sent to you that contains
Health and Home Safety Handout,
Wipe-Off Medication Management Planner,
Exercise video,
Exercise Progress Chart,
Falls Journal in which you can record any falls or near falls that may occur and
Pedometer.
Additionally, you will be receiving a quarterly follow-up phone call shortly after this interview. In the interim, if you have any questions regarding the Independent Living and Mobility Program, please contact XXXXXXXX at XXX-XXX-XXXX.
If this is the final in-person assessment add:
This is the final interview that we will be conducting, thank you for participating in this important national program over the past 2 years.
For all assessments finish the introduction with:
Do you have any questions regarding the interview before we begin?
Please document any questions the participant has.
General Questions
Do you have any visual deficits? (If “Yes,” explain below) No Yes
Do you have any hearing deficits? (If “Yes,” explain below) No Yes
Condition |
Date of Diagnosis (month/year) |
Dr. Name |
Treatment |
Current Status |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Are you having any difficulty understanding me? (If “Yes,” explain below) No Yes
Reason for difficulty:
What can be done to compensate for this problem?
Assessor: compensate as best you can and then ask:
Now can you understand me? (If “No,” terminate interview) No Yes
Hospital/Emergency Visits and Surgery
Since your recent phone interview have you had any Hospital Admissions, Emergency Room visits or Surgery? No Yes
If Yes, indicate number of times: _________
Reason for Hospital Admission/ Emergency Room visit/ Surgery |
Date (month/year) |
Type of Surgery &/or Treatment received |
Current Status |
|
|
|
|
|
|
|
|
|
|
|
|
Primary Care Physician
Do you have a primary care physician? No Yes
Physician’s name: Phone number:
City: State Street address:
Specialty:
Falls History
Since your recent phone interview have you had one or more episodes of fainting, falling or dropping to the ground, passing out or have you lost your balance, slipped or tripped over something that resulted in falling or dropping to the ground? No Yes
If Yes, How many times did this happen?
Regarding your most recent fall, what time of day did it happen? Day Eve
Morn/Day 5:01AM-9:00AM 9:01AM-12:00PM 12:01PM-4:00PM
Eve/Noc 5:01PM-7:00PM 7:01PM-10:00AM 10:01AM-5:00AM
Did you get hurt or injure yourself? No Yes
Did you require Medical Attention? No Yes
Emergency Room Visit Hospital Admission Doctor Visit
What were you doing when you fell?
Were you at home when you fell? No Yes
If Yes, Where? Bathroom Kitchen Entryway
Stairs Other:
If No, Where? Store/Business Parking Lot/Street Relative/Friend House
Dr. Office Walkway/Pathway Other
What was the cause of your fall? Tripped Slipped Dizziness Seizure
Loss of Balance Fainted/Blacked out Other:
Were any of the following conditions present when you fell? (read all)
Ground conditions |
|
Wet Ground |
No Yes |
Icy/snowy Ground |
No Yes |
Uneven Ground |
No Yes |
Stepping up onto/down from a Curb |
No Yes |
Climbing up/going down stairs |
No Yes |
Object in walkway/path |
No Yes |
Behaviors For each Yes, answer additional question |
Additional Question |
|
Wearing shoes that did not fit properly |
No Yes |
Have you changed this behavior?..................No Yes |
Wearing clothes that did not fit properly |
No Yes |
Have you changed this behavior?..................No Yes |
Not using necessary visual aid/glasses |
No Yes |
Have you changed this behavior?..................No Yes |
Not using necessary equipment |
No Yes |
Have you changed this behavior?..................No Yes |
(cane, walker, shower seat, grab bars) |
No Yes |
|
|
|
|
Have you been anxious or worried or afraid you might fall? No Yes
Do you ever limit your activities, for example, what you do or where you go because you are afraid of falling? No Yes
If Yes, Which activities and why?
How often? All of the time Some of the time Rarely Doesn’t know
Medications
Please tell me the names and dosages of all the medications you currently take including non-prescription medications, eye drops and inhalers. (Assessor - Please obtain details for all medications)
|
Medication Name |
Dosage |
Frequency |
If PRN, indicate how often used |
Reason for taking |
Do you take this as prescribed by your doctor? |
If NO, Why Not? Too Expensive, Side Effects; “I don’t need them”, ”They don’t work”, Ran out of Rx, Forgets, Other: |
1 |
|
|
|
|
|
Yes No |
|
2 |
|
|
|
|
|
Yes No |
|
3 |
|
|
|
|
|
Yes No |
|
4 |
|
|
|
|
|
Yes No |
|
5 |
|
|
|
|
|
Yes No |
|
6 |
|
|
|
|
|
Yes No |
|
7 |
|
|
|
|
|
Yes No |
|
8 |
|
|
|
|
|
Yes No |
|
9 |
|
|
|
|
|
Yes No |
|
10 |
|
|
|
|
|
Yes No |
|
11 |
|
|
|
|
|
Yes No |
|
12 |
|
|
|
|
|
Yes No |
|
13 |
|
|
|
|
|
Yes No |
|
14 |
|
|
|
|
|
Yes No |
|
15 |
|
|
|
|
|
Yes No |
|
16 |
|
|
|
|
|
Yes No |
|
17 |
|
|
|
|
|
Yes No |
|
18 |
|
|
|
|
|
Yes No |
|
19 |
|
|
|
|
|
Yes No |
|
20 |
|
|
|
|
|
Yes No |
|
Medical Conditions and Symptoms
Do you have a history of any of the following conditions? (if any answer is “Yes,” explain below)
Irregular Heart Beat/A-fib/Arrhythmia |
No |
Yes |
Sciatica, Back pain or swelling |
No |
Yes |
High Blood Pressure |
No |
Yes |
Foot Disorders |
No |
Yes |
Low Blood Pressure |
No |
Yes |
Ankle, Knee or Hip replacement |
No |
Yes |
Congestive Heart Failure |
No |
Yes |
Ankle, Knee or Hip pain, swelling or redness |
No |
Yes |
Heart Attack |
No |
Yes |
Amputation of Leg, Foot or Toe |
No |
Yes |
Any other heart problem(s) |
No |
Yes |
Cancer, Leukemia, Lymphoma |
No |
Yes |
Vitamin B12 Deficiency or Anemia |
No |
Yes |
Diabetes |
No |
Yes |
Other blood disorder? |
No |
Yes |
Numbness (where?) |
No |
Yes |
Circulatory Problems |
No |
Yes |
Weakness (where?) |
No |
Yes |
Stroke, TIA or “Mini-Stroke” |
No |
Yes |
Fatigue |
No |
Yes |
Paralysis (where?) |
No |
Yes |
Tremors (where?) |
No |
Yes |
Peripheral Neuropathy |
No |
Yes |
Seizures, convulsions (date of last) |
No |
Yes |
Multiple Sclerosis |
No |
Yes |
Neurological Problems |
No |
Yes |
Parkinson’s Disease |
No |
Yes |
Unsteadiness/Imbalance |
No |
Yes |
Alzheimer’s Disease/Dementia |
No |
Yes |
Psychiatric Disorders |
No |
Yes |
Shortness of breath/Difficulty Breathing |
No |
Yes |
Depression |
No |
Yes |
Asthma, Emphysema, COPD, Chronic Cough |
No |
Yes |
Anxiety |
No |
Yes |
Arthritis (Type? Location?) |
No |
Yes |
Alcoholism/Drug Addiction |
No |
Yes |
Osteoporosis |
No |
Yes |
Dizziness/Vertigo |
No |
Yes |
Bone Fractures (where? why?) |
No |
Yes |
Insomnia/difficulty sleeping |
No |
Yes |
If any condition is answered “Yes,” gather details in the grid below
|
Condition |
Date of Diagnosis/ 1st Symptom |
Date of most recent Symptom |
Is Condition treated by a doctor? |
Is Condition Controlled/ Stable? |
Treatment |
1 |
|
|
|
No Yes |
No Yes |
|
2 |
|
|
|
No Yes |
No Yes |
|
3 |
|
|
|
No Yes |
No Yes |
|
4 |
|
|
|
No Yes |
No Yes |
|
5 |
|
|
|
No Yes |
No Yes |
|
6 |
|
|
|
No Yes |
No Yes |
|
7 |
|
|
|
No Yes |
No Yes |
|
8 |
|
|
|
No Yes |
No Yes |
|
9 |
|
|
|
No Yes |
No Yes |
|
Physical Measurements
Some falls occur when people stand up from a lying position because their blood pressure drops. Therefore, I would like to take your blood pressure from two positions – one when you are lying down, then one after you stand up from a lying position. Please lie down on a couch for the first blood pressure and pulse.
A. Supine BP: _____ / _____ Exact Time: ____: _____ (wait no more than 1 minute before taking standing BP)
& Heart rate:_____ What does your blood pressure usually run? _____ / _____ or Unknown
Now please stand up and I will take your blood pressure and pulse again.
B. Standing BP: _____ / _____ Exact Time: ____: _____
& Heart rate:_____
C. Height: ____ft._____ in. Have you had any loss of height? No Yes
How much? Reason:
D. Weight: _________ lbs.
Activities of Daily Living & Physical Performance Measurements
The next questions concern your current ability to perform daily activities. I will first ask if you have any difficulty doing the activity, then if you receive any assistance or use any equipment and then I will ask you to demonstrate the motions that are required to complete the activities. I will also be asking to do a safety evaluation in your kitchen, bedroom, the bathroom that you use most often and the rooms in which you spend most of your time. Assessor: As you view each room, look to see that flooring is securely attached (including area rugs), walkways are well lit and clear of obstructions, thresholds are only ½ inch high, furniture is sturdy and note any nightlights that are used regularly.
Transferring:
Do have difficulty when transferring in or out of a bed or chair without assistance from another person? No Yes
If Yes, Describe why completion of this activity is difficult for you:
Does anyone help you transfer in and out of a bed or chair? No Yes
Do you use equipment when transferring from a bed or chair? No Yes
If Yes identify type: hoyer lift chair lift walker cane other___________
Please stand up then sit back down for me.
Assessor: Did the participant have any difficulty completing this task? No Yes
If Yes, choose one and explain: Difficulty noted Not completed, safety issue
Based on the information above and using your clinical judgment, choose the level of assistance from another person most often required for the insured to complete this activity: (Choose only one)
No physical assistance from another person required
Stand-by assistance from another person required – within arm’s reach for safety
Hands-on assistance from another person required – physical assist
Mobility Outside:
Do have difficulty when walking outside your home (within walking distance) including negotiating uneven surfaces (curbs, ramps, sidewalks, uneven ground etc…) without assistance from another person? No Yes
If Yes, Describe why completion of this activity is difficult for you:
Does anyone help you when you walk outside your home? No Yes
Do you require equipment when walking outside your home? No Yes
If yes, identify type: scooter wheelchair walker cane other_________
Based on the information above and using your clinical judgment, choose the level of assistance from another person most often required for the insured to complete this activity: (Choose only one)
No physical assistance from another person required
Stand-by assistance from another person required – within arm’s reach for safety
Hands-on assistance from another person required – physical assist
Chair stands
Baseline Chair Stand
These next exercises measure the strength in your legs. Please sit in a chair that is at a comfortable height.
Do you think it would be safe for you to try to stand up from a chair without using your arms? No Yes
If Yes: Demonstrate chair stand for participant as you explain and record results below
First fold your arms across your chest and sit so that your feet are on the floor, then try to stand up, keeping your arms folded across your chest.
Gets up easily on first try (continue with #2 below)
Gets up on first try but has difficulty (continue with #2 below)
Requires more than one attempt (continue with #2 below)
Can rise but not without using arms (skip to next page)
Cannot rise without assistance from another person (skip to next page)
Refused to participate (indicate reason and skip to next page)
Fear of falling Physically unable Other:
If No: Record reason and skip to next page
Cannot rise without assistance from another person (skip to next page)
Refused to participate (indicate reason and skip to next page)
Fear of falling Physically unable Other:
Timed Chair Stands (do not complete if participant indicates it is unsafe to stand without using arms)
Assessor: use a STOP WATCH or WATCH WITH A SECOND HAND for this section.
OK, now I am going to ask you to stand up a few more times. Please keep your arms folded across your chest and stand up straight as many times as you can until I tell you to stop. After standing up each time, sit down and then stand up again. Keep your arms folded across your chest. I will be timing you for 30 seconds. OK, are you ready? Stand. Assessor: Start timing and Count out loud how many times the participant rises from the chair during the 30 seconds. Record results below. Stop timing if there is a safety concern.
Timed for 30 seconds – Indicate the number of times participant stood from chair during 30 seconds: chair stands
Time stopped due to safety concern at: seconds. Number of chair stands during that time: chair stands
Time stopped due to participant’s inability to complete any chair stands with arms folded on chest.
Mobility Inside & timed get up and go:
Do you have difficulty when walking from one room to another inside your home without assistance from another person? No Yes
If Yes, Describe why completion of this activity is difficult for you:
Does anyone help you walk from one room to another inside your home? No Yes
Do you require equipment when performing this activity? No Yes
If yes, identify type: stair lift wheelchair walker cane other_________
Do you think it would be safe for you to stand up from a chair walk 8 feet and back then sit back down? No Yes
If Yes: Use Measuring Tape to measure out 8 feet. Stand 8 feet from participant and say:
OK, I am going to time how long it takes you to stand up, walk to here (8 feet from where participant is seated), turn around, walk back and sit down on that seat again. Are you ready?
OK, Go. (START TIMING and Describe below)
Time taken for participant to rise from chair, walk 8 feet, turn, walk back and sit down again: seconds
Posture: (e.g. : erect, kyphotic)
Balance: (e.g. : steady, imbalanced)
Pace: (e.g. : fast, medium, slow)
Stride length: (e.g. : short, medium, long)
Step height: (e.g. : shuffle, exaggerated, natural)
Gait: (e.g. : smooth, choppy , stiff)
Arm movement: (e.g. : pendulum swing, stiff, bent elbows)
Ability to turn: (e.g. natural, small steps, unbalanced)
Physical Abnormalities/Deformities/Equipment:
If No, Why would it not be safe?
Assessor: Did the participant have any difficulty completing this task? No Yes
If Yes, choose one and explain: Difficulty noted Not completed, safety issue
Based on the information above and using your clinical judgment, choose the level of assistance from another person most often required for the insured to complete this activity: (Choose only one)
No physical assistance from another person required
Stand-by assistance from another person required – within arm’s reach for safety
Hands-on assistance from another person required – physical assist
Four-test balance scale
DO NOT DO this test if participant cannot stand without the assistance of a person/assistive device or if s/he feels it is unsafe. Use a STOP WATCH or a WATCH WITH A SECOND HAND for this section. No practices are allowed for these exercises and they should be carried out in bare feet or stocking feet. You may help the person in to each position, but the person must hold the position unaided. Each position must be held for 10 seconds before progressing to the next position.
Stop timing if: (1) the person moves their feet from the proper position,
(2) you provide contact to prevent a fall or
(3) the person touches the wall or other support with their hand.
Many falls are caused by imbalance, so next I will check your balance. For this exercise, please take off your shoes. I will ask you to stand in 4 different positions for about 10 seconds each.
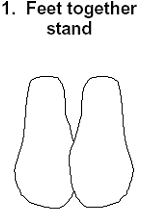
Feet Together Stand
First I would like you to try to stand with your feet together, side-by-side, for about 10 seconds (show picture). You may use your arms, bend your knees or move your body to maintain your balance, but try not to move your feet. Try to hold this position until I tell you to stop.
OK, Start. (Time for 10 seconds) Ok, Stop. (Record result below)
Held position successfully for 10 seconds
Held position successfully, but not for 10 seconds
Unable to hold position/did not do (indicate reason and skip to next page)
Fear of falling Physically unable Other: _________________
Semi-tandem stand
N

OK, Start. (Time for 10 seconds) Ok, Stop. (Record result below)
Held position successfully for 10 seconds
Held position successfully, but not for 10 seconds
Unable to hold position/did not do (indicate reason and skip to next page)
Fear of falling Physically unable Other: _________________
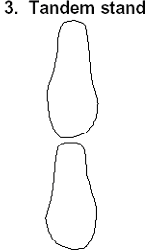
Tandem stand
Now, I want you to try to stand with the heel of one foot in front of and touching the toes of the other foot for about 10 seconds (show picture). You may put either foot in front, whichever is more comfortable for you. You may use your arms, bend your knees or move your body to maintain your balance, but try not to move your feet. Try to hold this position until I tell you to stop.
OK, Start. (Time for 10 seconds) Ok, Stop. (Record result below)
Held position successfully for 10 seconds
Held position successfully, but not for 10 seconds
Unable to hold position/did not do (indicate reason and skip to next page)
Fear of falling Physically unable Other: _________________
One leg stand
N

OK, Start. (Time for 10 seconds) Ok, Stop. (Record result below)
Held position successfully for 10 seconds
Held position successfully, but not for 10 seconds
Unable to hold position/did not do (indicate reason and skip to next page)
Fear of falling Physically unable Other: _________________
Eating (Note: Eating does not include meal preparation, cooking, cutting food, pouring liquids or buttering bread):
Do you have difficulty eating without assistance from another person? No Yes
If Yes, Describe why completion of this activity is difficult for you:
Does anyone help you eat? No Yes
Do you require equipment when eating? No Yes
If Yes identify type: Feeding tube TPN other:__________
Please demonstrate how you grasp a cup and then a fork or spoon. (Use pen if fork/spoon not available)
Assessor: Did the participant have any difficulty completing this task? No Yes
If Yes, choose one and explain: Difficulty noted Not completed, safety issue
Based on the information above and using your clinical judgment, choose the level of assistance from another person most often required for the insured to complete this activity: (Choose only one)
No physical assistance from another person required
Stand-by assistance from another person required – within arm’s reach for safety
Hands-on assistance from another person required – physical assist
Kitchen safety evaluation
Let’s go into the kitchen and I will evaluate the lighting, counter height and flooring.
Is lighting adequate (light bulbs greater than 60 watts) in this room? No Yes
If No: Explain:
Are counters and shelves at an appropriate height such that items can be easily reached? No Yes
If No: Explain:
Is a sturdy, non-skid step stool used to reach items outside participant’s reach?.....No Yes
Stairway Safety Evaluation
Next I would like to see any stairs that you use.
Are the stairs used to enter/exit well lit with sturdy railings on both sides? None No Yes
If No: Explain:
Are the stairs inside the home well lit with sturdy railings on both sides? None No Yes
If No: Explain:
Bedroom safety evaluation
Next I will ask you about dressing, let’s go into the bedroom and I will evaluate the lighting, mattress safety, flooring and pathway to the bathroom.
Is the mattress firm and sag resistant and at a height that enables easy transfers? No Yes
If No: Explain:
Is there a clear path from where participant sleeps to the bathroom for easy navigation in the dark? No Yes
If No: Explain:
Are nightlights used so that the pathway to the bathroom is visible at night? No Yes
If No: Explain:
Dressing:
Do you have difficulty when dressing/undressing including getting your clothes from closets/drawers, putting them on and taking them off and doing buttons, hooks and zippers without assistance from another person? No Yes
If Yes, Describe why completion of this activity is difficult for the participant:
Does anyone help you dress or undress? No Yes
Do you require equipment when dressing or undressing? No Yes
If Yes identify type: ___________
Please show me the movements you use to get your clothes, put on a shirt, pants/skirt and shoes.
Assessor: Did the participant have any difficulty completing this task? No Yes
If Yes, choose one and explain: Difficulty noted Not completed, safety issue
Based on the information above and using your clinical judgment, choose the level of assistance from another person most often required for the insured to complete this activity: (Choose only one)
No physical assistance from another person required
Stand-by assistance from another person required – within arm’s reach for safety
Hands-on assistance from another person required – physical assist
Bathroom safety evaluation:
Next I will ask you about bathing and toileting, let’s go into the bathroom and I will evaluate the lighting and the flooring in the bathing area and toilet are as well as check if there are any grab bars.
Is lighting adequate (light bulbs greater than 60 watts) in the tub, toilet and shower areas? No Yes
If No: Explain:
Are grab bars securely fastened for use while bathing in the bathing area? None No Yes
If No: Explain:
Are grab bars/toilet safety frame securely fastened for use with getting on and off toilet? None No Yes
If No: Explain:
Is there a bath mat or non-skid flooring in tub/shower? No Yes
If No: Explain:
Are nightlights used so the bathroom is visible at night? No Yes
If No: Explain:
Many falls that occur in the home occur in the bathroom while people are transferring on and off the toilet and getting in and out of the shower or tub. Since these two actions are the most common cause of fall, I am going to ask you to demonstrate how you do these activities for me.
Bathing:
A. How do you usually bathe? Sponge Bath Whirlpool/Tub Shower in Tub Shower in Stall/Walk-in Shower
Do you have difficulty when bathing including getting to and from and in and out of the bathing area, washing and drying all parts of your body without assistance from another person? No Yes
If Yes, Describe why completion of this activity is difficult for you:
Does anyone help you bathe? No Yes
Do you require equipment when bathing? No Yes
If Yes identify type: bath bench/seat hand held shower grab bars other_____
Please show me how you get in and out of your bathing area and show me how you can wash your head, back and feet.
Assessor: Did the participant have any difficulty completing this task? No Yes
If Yes, choose one and explain: Difficulty noted Not completed, safety issue
Based on the information above and using your clinical judgment, choose the level of assistance from another person most often required for the insured to complete this activity: (Choose only one)
No physical assistance from another person required
Stand-by assistance from another person required – within arm’s reach for safety
Hands-on assistance from another person required – physical assist
TOILETING:
Do you have difficulty when toileting including getting to and from and on and off the toilet, cleaning yourself after elimination and adjusting your clothing without assistance from another person? No Yes
If Yes, Describe why completion of this activity is difficult for the participant:
Does anyone help you toilet at all? No Yes
Do you require equipment when performing this activity? No Yes
If Yes identify type: bedpan urinal commode raised toilet seat
walker cane wheelchair toilet safety frame other___________
Please show me how you get on and off of your toilet.
Assessor: Did the participant have any difficulty completing this task? No Yes
If Yes, choose one and explain: Difficulty noted Not completed, safety issue
Based on the information above and using your clinical judgment, choose the level of assistance from another person most often required for the insured to complete this activity: (Choose only one)
No physical assistance from another person required
Stand-by assistance from another person required – within arm’s reach for safety
Hands-on assistance from another person required – physical assist
BLADDER CONTINENCE:
Do you ever experience any loss of bladder control? No Yes
Do you use a urostomy or a catheter? No Yes
If No to both questions, skip to Bowel Continence question.
If Yes to either question:
Do have difficulty when washing yourself, disposing of soiled items, changing or adjusting your clothing or caring for the medical device without assistance from another person? No Yes
If Yes, Describe why completion of this activity is difficult you:
Does anyone help you when you are incontinent? No Yes
Do you require equipment when because of your bladder incontinence? No Yes
If Yes identify type: pads briefs urostomy catheter other__________
Based on the information above and using your clinical judgment, choose the level of assistance from another person most often required for the insured to complete this activity: (Choose only one)
No physical assistance from another person required
Stand-by assistance from another person required – within arm’s reach for safety
Hands-on assistance from another person required – physical assist
BOWEL CONTINENCE:
Do you ever experience any loss of bowel control? No Yes
Do you use a colostomy or ileostomy? No Yes
If No to both questions, skip to next page.
If “Yes” to either question Do have difficulty when washing yourself, disposing of soiled items, changing or adjusting your clothing or caring for the medical device without assistance from another person? No Yes
If Yes, Describe why completion of this activity is difficult you:
Does anyone help you when you are incontinent? No Yes
Do you require equipment when because of your bladder incontinence? No Yes
If Yes identify type: pads briefs colostomy ileostomy other__________
Based on the information above and using your clinical judgment, choose the level of assistance from another person most often required for the insured to complete this activity: (Choose only one)
No physical assistance from another person required
Stand-by assistance from another person required – within arm’s reach for safety
Hands-on assistance from another person required – physical assist
Current Care
Do you receive personal care or assistance from any paid caregivers (including Medicare services)? No Yes
Assessor: Below please document any and all paid services provided to the participant.
Service Provider
(e.g. RN, CNA)
Service Provided
(e.g. skilled care, ADLs, supervision, etc.)
Frequency per Week and Hours per Day
(e.g., 2-3 hrs / day 7 days / wk)
Projected Duration
(e.g., Long term, 3 weeks, 3-6 weeks)
Start Date of Service
Hourly Rate/ monthly fee
Do you receive personal care or assistance from any unpaid caregivers (including family members/friends)? No Yes
Assessor: Below please document any and all services provided to the participant.
Unpaid Caregiver Name and relationship |
Service Provided (check all that apply) |
Frequency per Week and Hours per Day (e.g., 2-3 hrs/day 7 days/wk) |
Projected Duration (e.g., Long term, 3 weeks, 3-6 weeks) |
Start Date of assistance |
Does this person live with the participant? No Yes |
Bathing Dressing Transfers Eating Toileting Continence IADLs Companionship Supervision Med Administration Other____________ |
|
|
|
Does this person live with the participant? No Yes |
Bathing Dressing Transfers Eating Toileting Continence IADLs Companionship Supervision Med Administration Other____________ |
|
|
|
Does this person live with the participant? No Yes |
Bathing Dressing Transfers Eating Toileting Continence IADLs Companionship Supervision Med Administration Other____________ |
|
|
|
Summary of Home Safety Evaluation
Assessor: Take one last walk through any rooms that you viewed and answer the following questions about the areas where the participant spends most of his/her time. Please supply details for each “No” answer.
Is flooring non-skid and firmly attached to floor? No Yes
If No: in which rooms: Bathroom Bedroom Kitchen Other:
Explain:
Are walkways are well lit, visible and free of obstruction and clutter? No Yes
If No: in which rooms: Bathroom Bedroom Kitchen Other:
Explain:
Are thresholds at a height no greater than ½ inch? No Yes
If No: in which rooms: Bathroom Bedroom Kitchen Other:
Explain:
Are scatter rugs (throw rugs) securely fastened to the floor? None No Yes
If No: in which rooms: Bathroom Bedroom Kitchen Other:
Explain:
Are the electrical cords cleared from pathways? No Yes
If No: in which rooms: Bathroom Bedroom Kitchen Other:
Explain:
Are seats and chairs safe for transfers with sturdy footing and secure armrests? No Yes
If No: in which rooms: Bathroom Bedroom Kitchen Other:
Explain:
Are counters/furniture secure enough to provide support if leaned upon for mobility assistance? No Yes
If No: in which rooms: Bathroom Bedroom Kitchen Other:
Explain:
Other than was noted in the previous few pages, did the participant’s home appear to be hazard-free? No Yes
If No: Explain other safety hazards noted:



Wrap up
If this is the initial in-person assessment end with:
Thank you for your participation in the Independent Living and Mobility Prevention Program. A summary of this interview will be sent to you along with recommendations of how to maintain your independence over time and keep your home safer. Also we will be sending the Health Promotion and Fall Prevention Tool kit mentioned at the beginning of the interview. Additionally, a clinician will be calling you every 3 months or so to gather information from your Exercise Progress Chart and Falls Journal which are part of the Tool kit. As part of the program, you will be asked to document in your Exercise Progress Chart an on a weekly basis and in the Falls Journal every time you ever experience a fall or a near fall of some kind. Thank you again for your participation!
If this is the Final in-person assessment end with:
Thank you for your participation in the Independent Living and Mobility Program. This ends the 2 year study, we really appreciate the time you have invested in this important national program.
Clinical Summary
Assessor: Complete the Clinical Summary after you have left the Participant’s home. Please be sure to provide an answer for each question
Was there any indication that the participant is unsafe to be left alone? No Yes
If Yes, explain
Was there any indication that the participant is not taking reasonable care of his/her home environment in terms of cleanliness, neatness and minimizing clutter? No Yes
If Yes, explain
Was there any indication that the participant is not taking reasonable care of themselves in terms of appearance, hygiene, and grooming? No Yes
If Yes, explain
Was anyone other than the participant present during any part of the interview? No Yes
Who:
Relationship to participant:
Did anyone other than the participant answer any of the interview questions? No Yes
If Yes, explain
Does the participant appear to be in immediate danger due to an unsafe home environment? No Yes
If Yes, explain
Did you observe any non-reported safety issues (including skin breakdown, bruises, malnourishment etc…)? No Yes
If Yes, explain
Are there any other concerns or comments that you feel should be documented or explained? No Yes
If Yes, explain
Field Based Observations
Please use the information you gathered during the interview to identify unmet needs that should be addressed in the summary that will be sent to the participant.
Do you feel the insured has the appropriate equipment in his/her home? Yes No
Check all equipment/safety devices that the insured does not have, but would benefit from, to remain safely in his/ her present location: For each piece of equipment noted, indicate why it is needed below:
|
Straight Cane |
|
Hospital Bed |
|
Commode |
|
Multi-pronged Cane |
|
Tub rail (tub) |
|
Raised Toilet Seat |
|
Walker |
|
Bath/shower Stool |
|
Toilet Safety Frame1 |
|
Wheelchair |
|
Shower bench with back |
|
Medical Alert System |
|
Electric Scooter |
|
Hand Held Shower2 |
|
Stair Lift |
|
Electric Recliner |
|
Grab Bars in shower/tub |
|
Other: |
Type of Equipment |
Reason recommended |
|
|
|
|
|
|
|
|
|
|
|
|
Do you feel the insured has the appropriate level, intensity and duration of services? Yes No
If No, complete the table below. In the table below, check the type of care you would recommend for this insured and provide information on frequency and duration.
|
Recommended Service |
Recommended Frequency |
Recommended Duration |
|
Home Health Aide/Personal Care Attendant |
____hrs/day ____d/wk |
|
|
Homemaker/Companion |
____hrs/day ____d/wk |
|
|
Physical/Occupational/Speech Therapy |
____hrs/day ____d/wk |
|
|
Skilled Nurse |
____hrs/day ____d/wk |
|
|
Medical Social Worker |
____hrs/day ____d/wk |
|
|
Meals on Wheels/Nutritional Services |
____meals/wk |
|
|
Pharmaceutical Care |
|
|
|
Transportation |
|
|
|
Other_____________________ |
|
|
|
Other_____________________ |
|
|
Why are these services being recommended?
Assessor
signature: Date
of interview:
~ PLEASE FAX IMMEDIATELY TO ----------------- WHEN COMPLETED! THANK YOU ~
1 Minimum requirement: 3 inches between toilet and sink/tub and no shelves above toilet with legs going to floor
2 Due to liability, typically Hand Held Showers will not be installed by the Medical Equipment Vendors
The Effect of Reducing Falls on Long Term Care Expenses – Literature Review
| File Type | application/msword |
| File Title | APPENDIX A |
| Author | LifePlans |
| Last Modified By | DHHS |
| File Modified | 2013-06-28 |
| File Created | 2013-06-28 |
© 2026 OMB.report | Privacy Policy