Supporting_Statment_B_HIV_China_7_2014_V_9.0
Supporting_Statment_B_HIV_China_7_2014_V_9.0.docx
HIV Study in Blood Donors from Five Chinese Regions (NHLBI)
OMB: 0925-0596
HIV Risk Factors Study in Blood Donors from Five Chinese Regions
OMB Number: 0925-0596
July 2014
Supporting Statement B
Sponsored by:
The National Heart, Lung, and Blood Institute
Transfusion Medicine and Cellular Therapeutics Branch
National Institutes of Health
Project Officer/ICD Contact:
Simone Glynn, MD
Transfusion Medicine and Cellular Therapeutics Branch
Division of Blood Diseases and Resources
National Heart, Lung, and Blood Institute
Two Rockledge Center
Suite 9142
6701 Rockledge Drive
Bethesda, MD 20892
Phone: (301) 435-0065
Fax: (301) 480-0868
Email: [email protected]
TABLE OF CONTENTS
Page
B. Collection of Information Employing Statistical Methods 1
B.1 Respondent Universe and Sampling Methods 1
B.2 Procedure for the Collection of Information 4
B.2.1 Questionnaire 4
B.2.2 Donor Enrollment and Questionnaire Administration 4
B.2.3 Variables to be Collected and Data Analysis 6
B.3 Methods to Maximize Response Rates and Deal with Non-response 7
B.4 Test of Procedures 7
B.5 Individuals Consulted on Statistical Aspects and Individuals Collecting and/or
Analyzing Data 8
B. Collection of Information Employing Statistical Methods
B.1. Respondent Universe and Sampling Methods
HIV prevalence and incidence data from Chinese blood donors will be collected and analyzed which will complement similar information collected from the general Chinese population and high risk populations thus providing a comprehensive evaluation of the HIV epidemic in China. This information will also contribute to the global HIV surveillance and prevention. Accurate and up-to-date epidemiological information including the prevalence and incidence rates and residual risk of HIV transmission by transfusions in Chinese blood donors is badly needed and will be valuable in guiding the development of new blood safety initiatives in China. Information on donor demographic correlates of HIV risk will support policy discussions over strategies to recruit the low risk donors in China. Since many infected donors are likely to have been recently infected, analyzing their viral genotype profile will allow for characterization of circulating strains of viruses thus enabling early detection of rare variants and longitudinal tracking of changes in genotype frequency of actively transmitted strains. This information will also be helpful in guiding future anti-viral and vaccine research. Meanwhile, findings from the HIV risk factor study will help identify new and major risk factors among blood donors and help develop more effective donor behavioral screening policies to prevent window period (not detected by the routine donor screening tests) infections from threatening the safety of blood supply.
B1.1. Study population and sampling methods
The HIV Study in Blood Donors from five Chinese Regions includes three components: 1) estimation of HIV prevalence and incidence in blood donors by demographics; 2) an evaluation of the genetic characteristics of HIV infections in blood donors; and 3) an evaluation of the relative prevalence of risk factors in HIV-positive blood donors.
General demographic information, routine donor testing results as well as confirmatory test results for all donors and their donations are collected for operational purposes and retrospectively compiled in a database by each of the five blood centers participating in REDS-III. This database can be used to estimate HIV prevalence and incidence overall and by demographics..
Four blood samples from each donation with a reactive HIV antibody screening result will be labeled with a REDS-III study ID and stored by participating centers and Guangxi Center for Disease Control (CDC) at -200C, preferably at -700C. The plasma (or serum) specimens’ minimal acceptable volume will be 1.0 ml. Screening reactive samples will be shipped in batches to the Institute of Blood Transfusion (IBT) by each blood center on dry ice every month. IBT is REDS-III China Program’s in-country coordinating center and has a Chinese Ministry of Health licensed HIV Confirmatory Laboratory.. IBT will perform genotype and drug resistance testing on confirmed positive samples.
For the HIV risk factor case-control study, all donors whose sero-reactive samples are confirmed HIV positive by the Western blot from the local CDC will be recruited for participation in the study as cases. Controls will be those whose sero-reactive samples confirmed negative for HIV. Details about subject enrollment and data collection for this study are presented in Section 4.7 of Attachment 6.1.
Statistical Considerations for Sampling Process
Research Triangle Institute (RTI), the REDS-III data coordinating center, will conduct the statistical analysis for the study. Statistical analysis for the first two components of the study are detailed in section 4.7 of Attachment 6.1 Statistical analysis for the first two components of the study are detailed in sections 4.5 and 4.6 of Attachment 6.1. This section focuses on the case-control risk factor study where donors (HIV-positive or negative) will be asked to complete a questionnaire to evaluate their risk factors.
In this case-control study, we want to understand risk factors for HIV infection in Chinese blood donors. In addition to investigating the association between HIV infection and exposure to some well-established risk factors, such as injection drug use, history of previous whole blood or plasma donation, and blood transfusion history, we also want to investigate some potential risk factors among Chinese blood donors such as having multiple sex partners, involvement in commercial sex, male to male sex, therapeutic acupuncture, and test-seeking behavior. According to the REDS-II China study (“An Analysis of Risk Factors for HIV Infection among Chinese Blood Donors”, by Jingxing Wang et al., Transfusion 2013; 53 Suppl 3:2431-40), the odds ratios of HIV infection and risk factors among Chinese blood donors ranged between 2-5 (OR=2.7 for test-seeking tendency, OR=1.8 for medical-related risks, and OR=5.1for high-risk sexual behaviors). The prevalence of the risk factors among controls (i.e. general population) ranged between 0.2% and 23% (11% test-seeking tendency, 3% having had blood transfusion, 23% injection in the past 12 months,7% endoscopy, 4% having a tattoo, 15% having two or more sexual partners, 4% paying or receiving money for sex, and 0.2% being MSM).
Here in Table 1, we present two sample size estimates based on 50% and 33% response rates, within the study period of January 2015 to June 2017 (30 months).
. Table 1. Sample size estimates for HIV risk factor study
Response Rate |
Primary Sites |
Peripheral Sites |
50%
|
Assuming 50 screen reactive samples per month, 14 confirmed positive (28% CT rate):
Cases: N = (14*30 months)*50% = 210 Control : N = (36*30 months)*50% = 540
Total = 210+540 = 750 |
Assuming 40 screen reactive samples per month, and 12 confirmed positive (30% CT rate):
Cases: N = (12*30 months)*50% = 180 Control: N = (28*30 months)*50% = 420
Total =180+420 =600 |
33%
|
Cases: N = (14*30 months)*33% = 138 Control 1: N = (36*30 months)*33% = 356
Total = 138+356=494 |
Cases: N = (12*30 months)*33% = 118 Control: N = (28*30 months)*33% = 277
Total = 118+277= 395 |
Thus, assuming a 50% response rate and a 28% or 30% HIV Western blot confirmatory rate respectively, we expect to have 210 HIV positive donors from primary REDS-III blood centers and 180 from peripheral blood centers. Meanwhile, 540 and 420 false positive donors will be recruited as controls from primary and peripheral sites respectively. We therefore will have a total of (210+180) = 390 HIV positive donors and (540+420) = 960 controls at 50% response rate. At a slightly higher than 1:2 case:control ratio, such sample sizes will allow us to detect an odds ratio of 3 with greater than 80% power, when the prevalence of a risk behavior is about 4% in the case group and 2% in the control group. The test statistic used is the two-sided Z test with pooled variance. The significance level of the test was targeted at 0.0500.
Currently available REDS-III confirmatory testing results suggest an about 1% Western blot indeterminate rate among screened-reactive samples (3.75% in REDS-II study period). Exclusion of these Western Blot indeterminate donors may result in the loss of a small number of donors in the control group. Given the slightly higher than 1:2 case to control ratio for this study, the power and sample size would remain intact by the exclusion of indeterminate donors.
On the other hand, assuming a 33% response rate and a 28% or 30% HIV Western Blot confirmatory rate respectively, we will enroll 138 HIV positive donors from primary sites and 118 from peripheral blood centers, and 356 and 277 false positive controls respectively. We therefore will have a total of 256 HIV positive donors and 633 controls at 33% response rate. Again, at a slightly higher than 1:2 case:control ratio, such sample sizes will allow us to detect an odds ratio of 3 with greater than 80% power, when the prevalence of a risk behavior is about 6% in the case group and 3% in the control group, or an odds ratio of 4 with greater than 80% power, when the prevalence of a risk behavior is about between 1-2% in the control group. The test statistic used is the two-sided Z test with pooled variance. The significance level of the test was targeted at 0.0500. Figure 1 presents the power and sample size estimates for various odds ratios that can be detected at varying prevalence of risk factors in the control group for different sample sizes (Section 4.9 Statistical Considerations of Attachment 6.1 also presents discussion of unexpected occurrences and proposed solutions.)
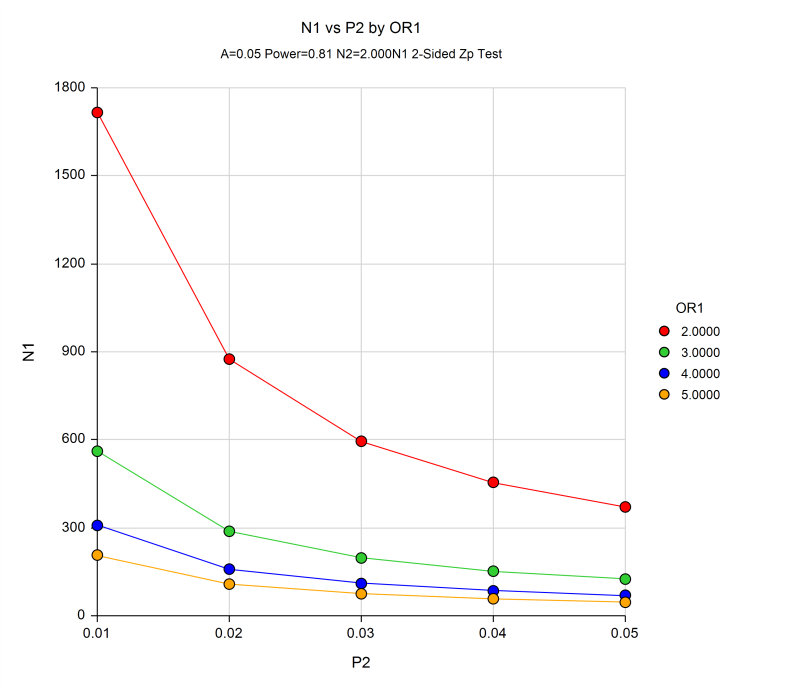
Figure 1. Two Independent Proportions (Null Case) Power Analysis (The sample size and power calculations were calculated using PASS 11 software (Hintze, J. 2011). PASS 11. NCSS, LLC. Kaysville, Utah, USA. www.ncss.com. N1 = Sample size for HIV cases; P2 = prevalence of risk factor in Controls; OR1 = Odds ratio for case and control groups)
Potential Nonresponse Bias
The exploratory data analysis stage will investigate the information provided in the data sets to determine, type of variable, valid values, level of missingness, and, if applicable, coding schemes. In addition, if there is any information available about relationships among variables, these relationships will be checked for logical consistency. Any data anomalies or logical inconsistencies identified during this stage of the analysis will be resolved. This will provide a relatively clean data set for the next stages of the data analysis.
The adjustment for missing data stage will minimize the potential bias from missing data. Virtually all data collection efforts experience the challenge of missing data. Typically, the missing data are not missing completely at random. Consequently, failure to account for the missing data, e.g., available or complete case analysis, can potentially lead to bias in the estimates produced. To investigate the potential for bias from the nonresponse, we will conduct a nonresponse bias analysis. Given the results of this analysis, which usually indicates that there is the potential for bias, we will use multiple imputation to account for the missing values, and, therefore, minimize the potential bias.
Stratification or Randomization (if applicable)
N/A
B.2. Procedure for the Collection of Information
B.2.1. Questionnaire
We have developed a Risk Factor Questionnaire (RFQ) that will be used for assessing the risk factors for HIV infection. The questionnaire will collect general demographic and risk factor information pertinent to HIV infection. The questionnaire has been developed based on a thorough review of the current international and Chinese literature. Efforts have been made to ensure that our questionnaire is comprehensive and culturally appropriate. The questionnaire has been translated into Chinese and Uyghur languages. The Uyghur translation will be used for Uyghur donors in Urumqi, Xinjiang. A similar version of the questionnaire was used in a REDS-II survey, for which we conducted focus group discussions and cognitive testing to improve the potential reliability of responses. Attachment 2 presents the Donor Consent Form for all REDS-III blood donors and Attachment 1 presents the HIV Risk Factor Survey Questionnaire.
B.2.2. Donor Enrollment and Questionnaire Administration
This study will follow all policies and rules established by the Chinese government for protecting the privacy and other rights of HIV infected individuals.
At the REDS-III blood centers, blood donors who gave consent for their donation information (including donation screening test results) to be included in the REDS-III China Donation Database will be eligible for this study (See Attachment 2.1). At the time of donation, as part of the routine operational donation process at the participating blood centers, these donors will have already given consent for their samples and information to be used for blood safety research. Each donor will have also been assigned a REDS-III Study ID under which donor and donation information can be identified in the REDS-III China Donation Database. This database does not include any personally identifying information and consists of retrospective information collected as a part of the routine blood donation operational procedures at the blood centers.
Routinely, screening tests for HIV infection are done at the blood centers. Confirmatory testing is the responsibility of the local Chinese Center for Disease Control (C-CDC) laboratories. Local C-CDCs are also responsible for notifying, counseling, and follow-up care of donors with confirmed anti-HIV results. The Guangxi CDC receives all the screened-reactive samples and donor information from its peripheral blood centers. Consequently, we will follow exactly the same recruitment and enrollment procedures at the primary and peripheral sites. As soon as the C-CDC receives the screen reactive donor information through email or telephone, designated staff at the C-CDC will request trained peripheral blood center staff to contact screened-reactive donors and invite them to participate in the study. The same REDS-III Informed Consent Form that is completed at the primary REDS-III sites will be completed by these donors. Upon completion of these consent forms, peripheral blood center staff will extract donor information from their database and complete the Data Collection Form for Peripheral Blood Centers and email them to the Guangxi CDC (see Attachment 6.1). Screened-reactive samples may be received a couple of days later for Western blot confirmation. The required donor and sample information will be entered into the Specimen Tracking System developed for REDS-III and sent to FEi Systems and IBT on a monthly basis. FEi assists the REDS-III China program with data management. FEi and IBT will merge the data by site and will send the data to RTI after data QC is conducted.
Case/Control Selection.
For this study, all screening anti-HIV reactive samples from the REDS-III China blood centers and peripheral blood centers will be shipped to the HIV confirmatory testing laboratory at the Institute of Blood Transfusion (IBT, a Chinese Ministry of Health licensed HIV Confirmatory Laboratory and REDS-III China Program’s in-country coordinating center) as well as to the local CDC laboratories. At local CDC laboratories, all screened-reactive samples will undergo HIV Western Blot testing using an US FDA licensed kit. Cases are defined as donors with Western blot confirmed anti-HIV antibody reactivity who have either completed the risk factor survey or agreed to complete the survey before receiving CDC donor notification of their confirmatory status. Controls will be HIV false positive donors who had a screened-reactive test but confirmed negative by Western blot and have completed or agreed to complete the survey.
Since nucleic acid testing (NAT) is being gradually implemented at the participating REDS-III blood centers, we may have a small number of NAT yield cases (HIV NAT positive but anti-HIV antibody negative by screening) that are likely recently-acquired (incident) infections. We will perform confirmatory NAT testing and repeat serological testing on these samples. If confirmed as incident infections, we will try to enroll these donors as cases in the risk factor study. The protocol for laboratory testing is presented in Attachment 6.1.
All local C-CDC labs and IBT use the same Western blot kit for HIV confirmatory testing on seroreactive donations. Once confirmed as positive, the local CDC will inform the blood centers of the confirmatory test result and contact the confirmed positive donors for further testing, counseling, and follow up care.
Survey method.
For all five REDS-III blood centers, blood centers will mail a study enrollment packet to all donors selected as potential cases and controls. Telephone calls will be made before sending out packets to confirm the correspondence address. Cases and controls will receive the same packets which will include:
A Consent Form embedded in the HIV Risk Factor Survey questionnaire. Receipt of a completed paper or online survey will indicate a donor’s agreement for participation in the study. Donor’s signature will not be included on the paper form to safeguard patient privacy.
A Risk Factor Questionnaire (RFQ): The paper questionnaire will be sent to all participants along with instructions for completing the questionnaire online as an alternative way of participating. The RFQ will be labeled only with a REDS-III Study ID, i.e., no personal identifiers will be used.
The REDS-III Risk Factor Study online survey data collection tool will be developed and maintained by FEI. A similar data collection tool was used for the REDS-II study during which 16 questionnaires were completed online and all data were extracted appropriately. Attachment 1.2 presents the full set of screen shots for the online survey
A pre-stamped envelope for returning the completed questionnaire to the blood center. Survey completion will prompt local blood centers/Guangxi CDC to issue the incentive either in the form of cash to be picked up by individuals at the Guangxi CDC or local blood centers, coupons for phone charge through email, or a check or paper coupons in the mail of the same value.
Active follow up reminder
Follow up calls or text messages (no more than 5 times) will be made 4 days after sending out the questionnaire to inquire whether or not the donor has received the questionnaire. If the questionnaire has been received, the donor will be reminded to complete the questionnaire (online completion is optional). If the questionnaire is not received by the donor, the staff will mail the questionnaire again and remind the participant to complete the questionnaire (online completion is optional).
If the questionnaire is not mailed back to the blood center within 10 days (or if online completion of the questionnaire is not observed in 10 days), reminder telephone calls or text messages will be made. In order to increase the successful contact rate, the blood center will call during different time slots (morning, afternoon and evening on weekdays). Weekend calls will be made if necessary. A maximum of five calls or text messages will be made for non-responded donors. Additional calls will not be made if a donor refuses to participate. The interval between the first and last call/text message will be at least one week. Each telephone call and text message will be documented. After 5 reminder calls or text messages, the follow up process will end. Surveys not returned to the blood centers or Guangxi CDC after the 5th reminder will be defined as no responses.
B.2.3 Variables to be Collected and Data Analysis
Case/Control status will be the main outcome variable (e.g., HIV-positive vs. HIV-negative), whereas the various risk factors will be the independent variables of main interest. Other variables such as blood center, age, gender, ethnicity, education, occupation, and first-time/repeat status could be potential confounders or effect modifiers and will be evaluated.
We will first produce frequency tables and associated Chi-square tests (or Exact tests for small sample size) to review potential associations. We will calculate odds ratios (OR) with 95% CI using logistic regression analysis to compare the odds of HIV positive donors having a risk factor compared to HIV negative donors.
We also plan to explore risk factors associated with recent HIV infections vs. those associated with long term infection. Regional differences as represented by blood center variations in the association between certain risk factors and HIV infection status will be explored. Multiple logistic regression models will be constructed both unadjusted and adjusted for factors that may affect the association between the risk factor and the infection of interest. We will also determine what final set of independent risk factors appear to be associated with the infection of interest by building a multiple logistic regression model that includes as independent variables all risk factors that are independently associated with each infection.
We will use several automated variable selection methods, e.g., forward selection, backwards elimination and stepwise, to build the multiple logistic regression models and will examine interactions between independent variables, as appropriate. We hope to identify the risk factors that have the greatest impact on HIV infections among donors.
B.3. Methods to Maximize Response Rates and Deal with Non-response
The primary limitations of this study are those which are inherent with questionnaire surveys to ascertain specific risk factors. The data may be influenced by socially desirable responses, recall bias and sampling bias. We will attempt to maximize the reliability of the results by assuring the participants of the private nature of the study.
A detailed explanation will be given to each participant in the study package on the research objectives and his or her individual rights as a research subject. The REDS-III consent form that will be given to all donors will explain that all study information entered into the REDS-III China donation database, submitted to the REDS-III China Data Coordinating Center (FEI, Xian, China), and then submitted to the REDS-III Data Coordinating Center (RTI, USA) will be identified only with a study ID, i.e., without any of the donor’s personal information. The study ID is generated for the REDS-III China program using an irreversible process. A link between the Study ID and the donor personal information is only maintained by the Chinese blood center without any access of the other study personnel outside of the blood center. The consent form will include information on the potential of a follow-up investigation and a look-back study.
B.4. Test of Procedures
The questionnaire was developed based on a thorough review of the international and Chinese literature. Efforts have been made to ensure that our questionnaire is comprehensive and culturally appropriate. Many items included in the questionnaire were extracted from published survey studies and were validated in the sense that across many studies, the risk behavior items were reliably correlated with HIV infectious status in the literature. Each item was reviewed by the study group and various wording options were considered before finalization. Items belonging to the same category, such as demographics, donation or transfusion history, questions targeting major risk behaviors [e.g., having sex with multiple partners or male who has had sex with another male (MSM)], or less frequent risk behaviors (e.g., sharing a razor), were thoroughly examined. The questionnaire was tested in the study conducted in REDS-II for its eligibility and feasibility and a nearly identical version was previously approved by OMB (OMB CONTROL NUMBER: 0925-0596). Reliability and validity of the questionnaire are supported by statistical analyses using REDS-II data. Exploratory and confirmatory factor analyses were performed on REDS-II data to find those conceptually related items (e.g., behavior risks) having high factor loadings on the same factor (average factor loading =.67 for behavior risk items; .40 for medical risk items; and .81 for test-seeking behavior items) and high inter-item correlations. Bivariate analyses evaluated the relationship between each factor and HIV confirmatory status, results of which supported the construct validity of the questionnaire. Since many of the items in the questionnaire are rather private, there is no data on the reliability testing among the same respondents. However, the repeated use of the same questions in many studies across different countries and similar findings strongly indicate the reliability of the questionnaire.
B.5. Individuals Consulted on Statistical Aspects and Individuals Collecting and/or Analyzing Data
We have consulted biostatisticians on statistical aspects of the study design, the blood centers researchers responsible for enrollment, administering questionnaires and collection of samples as well as the Coordinating Center staff for protocol development, study monitoring, and data management. Data analysis will be performed by the analytic staff at the Coordinating Center that includes epidemiologists and biostatisticians, with assistance and oversight provided by the REDS-III International Advisory Committee (see Attachment 5.3 for a complete list of International Advisory Committee members). The REDS-III OSMB (Attachment 5.1) will monitor the study.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| File Title | HIV Risk Factors Study in Blood Donors from Five Chinese Regions |
| Author | thornburg |
| File Modified | 0000-00-00 |
| File Created | 2021-01-26 |
© 2026 OMB.report | Privacy Policy