Hospitals and Health Care Complex Cost Report (CMS-2552-10)
Hospitals and Health Care Complex Cost Report
CMS-2552-10_COST REPORT INSTRUCTIONS
Hospitals and Health Care Complex Cost Report (CMS-2552-10)
OMB: 0938-0050
CHAPTER 40
HOSPITAL AND HOSPITAL
HEALTH CARE COMPLEX COST REPORT
FORM CMS-2552-10
Section
General 4000
Rounding Standards for Fractional Computations 4000.1
Acronyms and Abbreviations 4000.2
Recommended Sequence for Completing Form CMS-2552-10 4001
Sequence of Assembly for Hospital and Hospital Health Care Complex Providers Participating in Medicare 4002.1
Worksheet S - Hospital and Hospital Health Care Complex Cost Report Certification and Settlement Summary 4003
Part I - Cost Report Status 4003.1
Part II - Certification by Officer or Administrator of Provider(s) 4003.2
Part III - Settlement Summary 4003.3
Worksheet S-2 - Hospital and Hospital Health Care Complex Identification Data 4004
Part I - Hospital and Hospital Health Care Complex Identification Data 4004.1
Part II - Hospital and Hospital Heath Care Complex Reimbursement Questionnaire 4004.2
Worksheet S-3 - Hospital and Hospital Health Care Complex Statistical Data and Hospital Wage Index Information 4005
Part I - Hospital and Hospital Health Care Complex Statistical Data 4005.1
Part II - Hospital Wage Index Information 4005.2
Part III - Hospital Wage Index Summary......................................... 4005.3
Part IV - Hospital Wage Related Cost 4005.4
Part V - Hospital and Health Care Complex Contract Labor and Benefit Cost 4005.5
Worksheet S-4 - Hospital-Based Home Health Agency Statistical Data 4006
Worksheet S-5 - Hospital Renal Dialysis Department Statistical Data 4007
Worksheet S-6 - Hospital-Based Outpatient Rehabilitation Provider Data 4008
Worksheet S-7 - Statistical Data and Prospective Payment for Skilled Nursing Facilities .................................................... 4009
Worksheet S-8 - Hospital-Based RHC/FQHC Statistical Data 4010
Worksheet S-11 - Hospital-Based FQHC Identification Data 4010.1
Part I - Hospital-Based FQHC Identification Data 4010.2
Part II - Hospital-Based FQHC Consolidated Cost Report Participant Identification Data 4010.3
Part III - Hospital-Based FQHC Statistical Data 4010.4
Worksheet S-9 - Hospital-Based Hospice Identification Data 4011
Part I - Enrollment Days for Cost Reporting Periods Beginning Before October 1, 2015 4011.1
Part II - Census Data for Cost Reporting Periods Beginning Before October 1, 2015 4011.2
Part III - Enrollment Days for Cost Reporting Periods Beginning On or After October 1, 2015 4011.3
Part IV - Contracted Statistical Data for Cost Reporting Periods Beginning On or After October 1, 2015 4011.4
Worksheet S-10 - Hospital Uncompensated Care Data 4012
Rev. 40-1
CHAPTER 40
Section
Worksheet A - Reclassification and Adjustment of Trial Balance of Expenses............... 4013
Worksheet A-6 - Reclassifications.....................................................................................4014
Worksheet A-7 - Analysis of Capital Assets...................................................................... 4015
Part I - Analysis of Changes in Capital Asset Balances 4015.1
Part II - Reconciliation of Capital Cost Centers 4015.2
Part III - Reconciliation of Amounts from Worksheet A, Column 2, Lines 1 and 2 4015.3
Worksheet A-8 - Adjustments to Expenses........................................................................ 4016
Worksheet A-8-1 - Statement of Costs of Services from Related Organizations and Home Office Costs 4017
Worksheet A-8-2 - Provider-Based Physician Adjustments.............................................. 4018
Worksheet A-8-3 - Reasonable Cost Determination for Therapy Services Furnished by Outside Suppliers for Cost-Based Providers 4019
Part I - General Information 4019.1
Part II - Salary Equivalency Computation 4019.2
Part III - Standard Travel Allowance and Standard Travel Expense Computation - Provider Site 4019.3
Part IV - Standard Travel Allowance and Standard Travel Expense - Off‑Site Services 4019.4
Part V - Overtime Computation 4019.5
Part VI - Computation of Therapy Limitation and Excess Cost Adjustment 4019.6
Worksheet B, Part I - Cost Allocation - General Service Cost and Worksheet B-1 - Cost Allocation - Statistical Basis 4020
Worksheet B, Part II - Allocation of Capital-Related Costs and Worksheet B.................. 4021
Worksheet B-2 - Post Stepdown Adjustments................................................................... 4022
Worksheet C - Computation of Ratio of Cost to Charges and Outpatient Capital Reduction 4023
Part I - Computation of Ratio of Costs to Charges 4023.1
Part II - Computation of Ratio of Outpatient Service Cost to Charge Ratios Net of reductions 4023.2
Worksheet D - Cost Apportionment…............................................................................... 4024
Part I - Apportionment of Inpatient Routine Service Capital Costs 4024.1
Part II - Apportionment of Inpatient Ancillary Service Capital Costs 4024.2
Part III - Apportionment of Inpatient Routine Service Other Pass Through Costs 4024.3
Part IV - Apportionment of Inpatient Ancillary Service Other Pass Through Costs 4024.4
Part V - Apportionment of Medical and Other Health Services Costs 4024.5
40-2 Rev.
CHAPTER 40
Section
Worksheet D-1 - Computation of Inpatient Operating Cost 4025
Part I - All Provider Components 4025.1
Part II - Hospital and Subproviders Only 4025.2
Part III - Skilled Nursing Facility and Other Nursing Facility Only 4025.3
Part IV - Computation of Observation Bed Cost 4025.4
Worksheet D-2 - Apportionment of Cost of Services Rendered by Interns and Residents 4026
Part I - Not in Approved Teaching Program 4026.1
Part II - In Approved Teaching Program (Title XVIII, Part B Inpatient Routine Costs Only) 4026.2
Part III - Summary for Title XVIII 4026.3
Worksheet D-3 - Inpatient Ancillary Service Cost Apportionment 4027
Worksheet D-4 - Computation of Organ Acquisition Costs and Charges for Hospitals Which Are Certified Transplant Centers 4028
Part I - Computation of Organ Acquisition Costs (Inpatient Routine and Ancillary Services) 4028.1
Part II - Computation of Organ Acquisition Costs (Other Than Inpatients Routine and Ancillary Service Costs) 4028.2
Part III - Summary of Costs and Charges 4028.3
Part IV - Statistics 4028.4
Worksheet D-5 - Apportionment of Cost for Physicians’ Services in a Teaching Hospital 4029
Part I - Reasonable Compensation Equivalent Computation for Cost Reporting Periods Ending Before June 30, 2014 4029.1
Part II - Apportionment of Cost for Physicians’ Services in a Teaching Hospital for Cost Reporting Periods Ending Before June 30, 2014 4029.2
Part III - Reasonable Compensation Equivalent Computation for Cost Reporting Periods Ending On or After June 30, 2014 4029.3
Part IV - Apportionment of Cost for Physicians’ Services in a Teaching Hospital for Cost Reporting Periods Ending On or After June 30, 2014 4029.4
Worksheet E - Calculation of Reimbursement Settlement 4030
Part A - Inpatient Hospital Services Under PPS 4030.1
Part B - Medical and Other Health Services 4030.2
Worksheet E-1 - Analysis of Payments to Providers for Services Rendered 4031
Part I - Analysis of Payments to Providers for Services Rendered 4031.1
Part II - Calculation of reimbursement Settlement for Health Information Technology 4031.2
Worksheet E-2 - Calculation of Reimbursement Settlement - Swing Beds 4032
Worksheet E-3 - Calculation of Reimbursement Settlement…….……………….……… 4033
Part I - Calculation of Medicare Reimbursement Settlement Under 4033.1
Part II - Calculation of Reimbursement Settlement for Medicare Part A IPF PPS Services 4033.2
Part III - Calculation of Reimbursement Settlement All Other Health Services - IRF PPS 4033.3
Part IV - Calculation of Reimbursement Settlement All Other Health Services - LTCH PPS 4033.4
Part V - Calculation of Reimbursement Settlement for Medicare Part A Services - Cost Reimbursement 4033.5
Part VI - Calculation of Reimbursement Settlement - Title XVIII Part A PPS SNF Services 4033.6
Part VII - Calculation of Reimbursement Settlement for Title V & XIX 4033.7
Worksheet E-4 - Direct Graduate Medical Education and ESRD Outpatient Direct Medical Education Costs 4034
Rev. 40-3
CHAPTER 40
Section
Financial Statements Worksheets 4040
Worksheet G - Balance Sheet 4040.1
Worksheet G-1- Statement of Changes in Fund Balances 4040.2
Worksheet G-2, Parts I and II - Statement of Patient Revenues and Operating Expenses 4040.3
Worksheet G-3 - Statement of Revenues and Expenses 4040.4
Worksheet H - Analysis of Hospital-Based Home Health Agency Costs 4041
Worksheet H-1 - Cost Allocation HHA Statistical Basis 4042
Worksheet H-2 - Allocation of General Service Costs to HHA Cost Centers 4043
Part I - Allocation of General Service Costs to HHA Cost Centers 4043.1
Part II - Allocation of General Service Cost to HHA Cost Centers – Statistical Basis 4043.2
Worksheet H-3 - Apportionment of Patient Service Costs 4044
Part I - Computation of Lesser of Aggregate Medicare Cost Aggregate Medicare Limitation Cost, or Per Beneficiary Cost Limitation 4044.1
Part II - Apportionment of Cost of HHA Services Furnished by Shared Hospital Departments 4044.2
Worksheet H-4 - Calculation of HHA Reimbursement 4045
Part I - Computation of Lesser of Reasonable Cost or Customary Charges 4045.1
Part II - Computation of HHA Reimbursement Settlement 4045.2
Worksheet H-5 - Analysis of Payments to Hospital-Based HHAs for Services Rendered to Program Beneficiaries 4046
Worksheet I - Analysis of Renal Dialysis Department Costs 4047
Worksheet I-1 - Analysis of Renal Dialysis Department Costs 4048
Worksheet I-2 - Allocation of Renal Department Costs to Treatment Modalities 4049
Worksheet I-3 - Direct and Indirect Renal Dialysis Cost Allocation - Statistical Basis 4050
Worksheet I-4 - Computation of Average Cost Per Treatment for Outpatient Renal Dialysis 4051
Worksheet I-5 - Calculation of Reimbursable Bad Debts - Title XVIII, Part B 4052
40-4 Rev.
CHAPTER 40
Section
Worksheet J-1 - Allocation of General Service Costs to CMHC Cost Centers…….…… 4053
Part I - Allocation of General Service Costs to CMHC Cost Centers 4053.1
Part II - Allocation of General Service Costs to CMHC
Cost Centers -Statistical Basis…….……………….…………………………….. 4053.2
Worksheet J-2 - Computation of CMHC Provider Costs…….……………….…………. 4054
Part I - Apportionment of CMHC Cost Centers…….……………….…………….. 4054.1
Part II - Apportionment of Cost of CMHC Provider Services Furnished
by Shared Hospital Departments…….……………….………………………… 4054.2
Worksheet J-3 - Calculation of Reimbursement Settlement -
CMHC Provider Services…….……………….……………………………….. 4055
Worksheet J-4 - Analysis of Payments to Hospital-Based CMHC
for Services Rendered to Program Beneficiaries…….……………….……….. 4056
Worksheet K - Analysis of Hospital-Based Hospice Costs…….……………….………. 4057
Worksheet K-1 - Compensation Analysis - Salaries and Wage…….……………….….. 4058
Worksheet K-2 - Compensation Analysis - Employee Benefits (Payroll Related) …….. 4059
Worksheet K-3 - Compensation Analysis - Contracted Services/Purchased Services….. 4060
Worksheet K-4 - Part I - Cost Allocation - General Service Costs and
Part II - Cost Allocation - Statistical Basis…….……………….………………. 4061
Worksheet K-5 - Allocation of General Service Costs to Hospice Cost Centers…….….. 4062
Part I - Allocation of General Service Costs to Hospice Cost Centers…….………. 4062.1
Part II - Allocation of General Service Costs to Hospice
Cost Centers - Statistical Basis…….……………….…………………………... 4062.2
Part III - Computation of the Total Hospice Shared Costs…….……………….….. 4062.3
Worksheet K-6 - Calculation of Per Diem Cost…….……………….………………….. 4063
Rev. 40-5
CHAPTER 40
Section
Worksheet L - Calculation of Capital Payment 4064
Part I - Fully Prospective Method 4064.1
Part II - Payment Under Reasonable Cost 4064.2
Part III - Computation of Exception Payments 4064.3
Worksheet L-1 4065
Part I - Allocation of Allowable Capital Costs for Extraordinary Circumstances 4065.1
Part II - Computation of Program Inpatient Ancillary Service Capital Costs for Extraordinary Circumstances 4065.2
Part II - Computation of Program Inpatient Routine Service Capital Costs for Extraordinary Circumstances 4065.3
Worksheet M-1 - Analysis of Hospital-Based RHC/FQHC Costs 4066
Worksheet M-2 - Allocation of Overhead to Hospital-Based RHC/FQHC Services 4067
Worksheet M-3 - Calculation of Reimbursement Settlement for Hospital-Based
RHC/FQHC Services 4068
Worksheet M-4 - Computation of Hospital-Based RHC/FQHC Pneumococcal
and Influenza Vaccine Cost 4069
Worksheet M-5 - Analysis of Payments to Hospital-Based RHC/FQHC Services Rendered to Program Beneficiaries 4070
Worksheet N-1 - Reclassification and Adjustment of Trial Balance of Expenses For Hospital-Based FQHC 4071
Worksheet N-2 - Calculation of Hospital-Based FQHC Cost Per Visit 4071.1
Worksheet N- 3 - Computation of Hospital-Based FQHC Pneumococcal and Influenza Vaccine Cost 4071.2
Worksheet N-4 - Calculation of Hospital-Based FQHC Reimbursement Settlement 4071.3
Worksheet N-5 - Analysis of Payments to Hospital-Based FQHC for Services Rendered 4071.4
Worksheet O - Analysis of Hospital-Based Hospice Costs 4072
Worksheets O-1, O-2, O-3, and O-4 - Analysis of Hospital-Based Hospice Costs 4072.1
Worksheet O-1 - Analysis of Hospital-Based Hospice Costs Hospice Continuous Home Care
Worksheet O-2 - Analysis of Hospital-Based Hospice Costs Hospice Routine Home Care
Worksheet O-3 - Analysis of Hospital-Based Hospice Costs Hospice Inpatient Respite Care
Worksheet O-4 - Analysis of Hospital-Based Hospice Costs Hospice General Inpatient Care
Worksheet O-5 - Determination of Hospital-Based Hospice Net Expenses for Allocation 4072.2
Worksheet O-6 - Part I - Cost Allocation - Hospital-Based Hospice General Service Costs 4072.3
Worksheet O-6 - Part II - Cost Allocation - Hospital-Based Hospice General Service Costs Statistical Basis 4072.3
Worksheet O-7 - Apportionment of Hospital-Based Hospice Shared Service Costs by Level of Care 4072.4
Worksheet O-8 - Calculation of Hospital-Based Hospice Per Diem Cost 4072.5
Exhibit 1 - Form CMS-2552-10 Worksheets 4090
Exhibit 2 - Electronic Reporting Specifications for Form CMS-2552-10 4095
40-6 Rev.
03-14 FORM CMS-2552-10 4000
4000. GENERAL
The Paperwork Reduction Act of 1995 requires that you be informed why information is collected and what the information is used for by the government. Section 1886(f)(1) of the Social Security Act (the Act) requires the Secretary to maintain a system of cost reporting for hospitals receiving payment computed under subsection (d), which includes a standardized electronic format. In accordance with §§1815(a), 1833(e), and 1861(v)(1)(A) of the Act, and 42 CFR 413.20(b), providers of service participating in the Medicare program are required to submit annual information to achieve settlement of costs for health care services rendered to Medicare beneficiaries. In accordance with these provisions, all hospital and hospital health care complexes must complete Form-CMS-2552-10 with a valid Office of Management and Budget (OMB) control number in order to determine program payment. In addition to determining program payment, the data submitted on the cost report support management of the federal programs, e.g., data extraction in developing cost limits, data extraction in developing and updating various prospective payment systems. The information reported on Form CMS‑2552‑10 must conform to the requirements and principles set forth in 42 CFR 412, 42 CFR 413, and in the Provider Reimbursement Manual, Part 1 (CMS Pub. 15‑1). The filing of the cost report is mandatory, and failure to do so results in all payments being deemed overpayments and a withhold up to 100 percent until the cost report is received. (See Provider Reimbursement Manual, Part 2 (CMS Pub. 15-2), chapter 1, §100.) The Medicare cost report information is considered public record under the freedom of information act 45 CFR Part 5. The Form CMS-2552-10 is effective for hospitals and hospital health care complexes with cost reporting periods beginning on or after May 1, 2010.
Worksheets are provided on an as needed basis dependent on the needs of the hospital. Not all worksheets are needed by all hospitals. The following are a few examples of conditions for which worksheets are needed:
Reimbursement is claimed for hospital swing beds;
Reimbursement is claimed for a hospital-based inpatient rehabilitation facility (IRF) or inpatient psychiatric facility (IPF);
Reimbursement is claimed for a hospital-based community mental health center (CMHC);
The hospital has physical therapy services furnished by outside suppliers (applicable for cost reimbursement and Tax Equity and Fiscal responsibility Act of 1982 (PL97248) (TEFRA providers, not PPS); or
The hospital is a certified transplant center (CTC).
NOTE: Public reporting burden for this collection of information is estimated to average 108 hours per response, and record keeping burden is estimated to average 565 hours per response. This includes time for reviewing instructions, searching existing data sources, gathering and maintaining data needed, and completing and reviewing the collection of information. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing the burden, to:
o Center for Medicare and Medicaid Services
Attn: PRA Report Clearance Officer
7500 Security Boulevard
Mail Stop C4-26-05
Baltimore, MD 21244-1855
o The Office of Information and Regulatory Affairs
Office of Management and Budget
Washington, DC 20503
Rev. 40-7
4000 (Cont.) FORM CMS-2552-10 03-14
Section 4007(b) of the Omnibus Budget Reconciliation Act (OBRA 1987) states that effective with cost reporting periods beginning on or after October 1, 1989, you are required to submit your cost report electronically unless you receive an exemption from CMS. The legislation allows CMS to delay or waiver implementation if the electronic submission results in financial hardship (in particular for providers with only a small percentage of Medicare volume). Exemptions are granted on a case-by-case basis (see 42 CFR 413.24(h)).
In addition to Medicare reimbursement, these forms also provide for the computation of reimbursement applicable to titles V and XIX to the extent required by individual State programs. Generally, the worksheets and portions of worksheets applicable to titles V and XIX are completed only to the extent these forms are required by the State program. However, Worksheets S-3 and D-1 must always be completed with title XIX data.
Each electronic system provides for the step down method of cost finding. This method provides for allocating the cost of services rendered by each general service cost center to other cost centers, which utilize the services. Once the costs of a general service cost center have been allocated, that cost center is considered closed. Once closed, it does not receive any of the costs subsequently allocated from the remaining general service cost centers. After all costs of the general service cost centers have been allocated to the remaining cost centers, the total costs of these remaining cost centers are further distributed to the departmental classification to which they pertain, e.g., hospital general inpatient routine, subprovider.
This cost report is designed to accommodate a hospital health care complex with multiple entities. If a hospital health care complex has more than one entity reporting (except skilled nursing facilities and nursing facilities which cannot exceed more than one hospital-based facility), add additional lines for each entity by subscripting the appropriate line designation.
In completing the worksheets, show reductions in expenses in parentheses ( ) unless otherwise indicated.
4000.1 Rounding Standards for Fractional Computations.--Throughout the Medicare cost report, required computations result in fractions. The following rounding standards must be employed for such computations. When performing multiple calculations, round after each calculation. However,
1. Round to 2 decimal places:
a. Percentages
b. Averages, standard work week, payment rates, and cost limits
c. Full time equivalent employees
Per diems, hourly rates
Round to 3 decimal places:
Payment to cost ratio
3. Round to 4 decimal places:
Wage adjustment factor
Medicare SSI ratio
Disproportionate patient percentage
40-8 Rev.
DRAFT FORM CMS-2552-10 4000.2
4. Round to 5 decimal places:
a. Payment reduction (e.g., capital reduction, outpatient cost reduction)
5. Round to 6 decimal places:
a. Ratios (e.g., unit cost multipliers, cost/charge ratios, days to days)
6. Round to 9 decimal places:
a. Uncompensated care factor 3
Where a difference exists within a column as a result of computing costs using a fraction or decimal, and the sum of the parts do not equal the whole, the highest amount in that column must either be increased or decreased by the difference. If there are two high numbers equaling the same amount, adjust the first high number from the top of the worksheet for which it applies.
4000.2 Acronyms and Abbreviations.--Throughout the Medicare cost report and instructions, a number of acronyms and abbreviations are used. For your convenience, commonly used acronyms and abbreviations are summarized below.
ACA - Affordable Care Act
A&G - Administrative and General
AHSEA - Adjusted Hourly Salary Equivalency Amount
ARRA - American Recovery and Reinvestment Act of 2009
ASC - Ambulatory Surgical Center
BBA - Balanced Budget Act
BBRA - Balanced Budget Reform Act
BIPA - Benefits Improvement and Protection Act
CAH - Critical Access Hospitals
CAPD - Continuous Ambulatory Peritoneal Dialysis
CAP-REL - Capital-Related
CBSA - Core Based Statistical Areas
CCN - CMS Certification Number
CCPD - Continuous Cycling Peritoneal Dialysis
CCU - Coronary Care Unit
CFR - Code of Federal Regulations
CMHC - Community Mental Health Center
CMS - Centers for Medicare & Medicaid Services
CNA - Certified Nursing Assistant
COL - Column
CORF - Comprehensive Outpatient Rehabilitation Facility
CRNA - Certified Registered Nurse Anesthetist
CT - Computer Tomography
CTC - Certified Transplant Center
DEFRA - Deficit Reduction Act of 1984
DRA - Deficit Reduction Act of 2005
DRG - Diagnostic Related Group
DSH - Disproportionate Share
EACH - Essential Access Community Hospital
ECR - Electronic Cost Report
EHR - Electronic Health Records
ESRD - End Stage Renal Disease
FFY - Federal Fiscal Year
FQHC - Federally Qualified Health Center
Rev. 40-9
4000.2 (Cont.) FORM CMS-2552-10 DRAFT
FR - Federal Register
FTE - Full Time Equivalent
GME - Graduate Medical Education
HCERA - Health Care and Education Reconciliation Act of 2010
HCHC - Hospice Continuous Home Care
HCPCS - Healthcare Common Procedure Coding System
HCRIS - Healthcare Cost Report Information System
HFS - Health Financial Systems
HGIP - Hospice General Inpatient Care
HIRC - Hospice Inpatient Respite Care
HRHC - Hospice Routine Home Care
HRSA - Health Resources and Services Administration
HHA - Home Health Agency
HIT - Health Information Technology
HMO - Health Maintenance Organization
HSR - Hospital Specific Rate
I & Rs - Interns and Residents
ICF/IID - Intermediate Care Facility for Individuals with Intellectual Disabilities
ICU - Intensive Care Unit
IME - Indirect Medical Education
INPT - Inpatient
IOM - Internet Only Manual
IPF - Inpatient Psychiatric Facility
IPPS - Inpatient Prospective Payment System
IRF - Inpatient Rehabilitation Facility
KPMG - Klynveld, Peat, Marwick, & Goerdeler
LCC - Lesser of Reasonable Cost or Customary Charges
LDP - Labor, Delivery and Postpartum
LIP - Low Income Patient
LOC - Level of Care
LOS - Length of Stay
LPN - Licensed Practical Nurse
LTCH - Long Term Care Hospital
LVN - Licensed Vocational Nurse
MA - Medicare Advantage (previously known as M+C)
M+C - Medicare + Choice (also known as Medicare Part C, Medicare Advantage and Medicare HMO)
MCP - Monthly Capitation Payment
MDH - Medicare Dependent Hospital
MED-ED - Medical Education
MIPPA - Medicare Improvements for Patients and Providers Act of 2008
MMA - Medicare Prescription Drug Improvement and Modernization Act of 2003
MMEA - Medicare and Medicaid Extenders Act of 2010
MRI - Magnetic Resonance Imaging
MS-DRG - Medicare Severity Diagnosis-Related Group
MSP - Medicare Secondary Payer
NF - Nursing Facility
NPI - National Provider Identifier
NPR - Notice of Program Reimbursement
OBRA - Omnibus Budget Reconciliation Act
OLTC - Other Long Term Care
OOT - Outpatient Occupational Therapy
OPD - Outpatient Department
OPO - Organ Procurement Organization
OPPS - Outpatient Prospective Payment System
40-10 Rev.
DRAFT FORM CMS-2552-10 4000.3
OPT - Outpatient Physical Therapy
OSP - Outpatient Speech Pathology
ORF - Outpatient Rehabilitation Facility
PCR - Payment to Cost Ratio
PCRE - Primary Care Residency Expansion Program
PBP - Provider-Based Physician
PPS - Prospective Payment System
PRM - Provider Reimbursement Manual
PRA - Per Resident Amount
PS&R - Provider Statistical and Reimbursement Report (or System)
PT - Physical Therapy
PTO - Paid Time Off
RCE - Reasonable Compensation Equivalent
RHC - Rural Health Clinic
RN - Registered Nurse
RPCH - Rural Primary Care Hospitals
RT - Respiratory Therapy
RUG - Resource Utilization Group
SCH - Sole Community Hospitals
SCHIP - State Children’s Health Insurance Program
SNF - Skilled Nursing Facility
SSI - Supplemental Security Income
TEFRA - Tax Equity and Fiscal Responsibility Act of 1982
THC - Teaching Health Center
TOPPS - Transitional Corridor Payment for Outpatient Prospective Payment System
UPIN - Unique Physician Identification Number
WKST - Worksheet
NOTE: In this chapter, TEFRA refers to §1886(b) of the Act and not to the entire Tax Equity and Fiscal Responsibility Act.
4000.3 Instructional, Regulatory and Statutory Effective Dates.--Throughout the Medicare cost report instructions, various effective dates implementing instructions, regulations and/or statutes are utilized.
Where applicable, at the end of select paragraphs and/or sentences the effective date(s) is indicated in parentheses ( ) for cost reporting periods ending on or after that date, i.e., (12/31/2010). Dates followed by a “b” are effective for cost reporting periods beginning on or after the specified date, i.e., (9/30/2010b). Dates followed by an “s” are effective for services rendered on or after the specified date, i.e., (4/1/2010s). Instructions not followed by an effective date are effective retroactive back to cost reporting periods beginning on or after 5/1/2010 (transmittal 1).
Rev. 40-11
4001 FORM CMS-2552-10 DRAFT
4001. RECOMMENDED SEQUENCE FOR COMPLETING FORM CMS-2552-10
Part I - Statistics, Departmental Cost Adjustments and Cost Allocations
Step Worksheet Instructions
 1 S-2,
Parts I & II Read §4004.1-4004.2. Complete entire
worksheet.
1 S-2,
Parts I & II Read §4004.1-4004.2. Complete entire
worksheet.
2 S-3, Parts I - V Read §4005-4005.5. Complete entire worksheets.
3 S-4 Read §4006. Complete entire worksheet, if applicable.
4 S-5 Read §4007. Complete entire worksheet, if applicable.
5 S-6 Read §4008. Complete entire worksheet, if applicable.
6 S-7 Read §4009. Complete entire worksheet, if applicable.
7 S-8 Read §4010. Complete entire worksheet, if applicable.
8 S-9 Read §4011. Complete portions of worksheet, as applicable.
9 S-11, Parts I - III Read §§4010.1-4010.4. Complete entire worksheet, if applicable.
10 A Read §4013. Complete columns 1through 3, lines 1 through 200.
11 A-6 Read §4014. Complete, if applicable.
12 A Read §4013. Complete columns 4 and 5, lines 1 through 200.
13 A-7, Parts I - III Read §4015. Complete entire worksheet.
14 A-8-1 Read §4017. Complete Parts A and B.
 15 A-8-2 Read
§4018. Complete, if applicable.
15 A-8-2 Read
§4018. Complete, if applicable.
 16 A-8-3,
Parts I - VI Read §§4019-4019.6. Complete, if applicable.
16 A-8-3,
Parts I - VI Read §§4019-4019.6. Complete, if applicable.
40-12 Rev.
DRAFT FORM CMS-2552-10 4001 (Cont.)
Step Worksheet Instructions
 17 A-8 Read
§4016. Complete entire worksheet.
17 A-8 Read
§4016. Complete entire worksheet.
 18 A Read
§4013. Complete columns 6 and 7, lines 1
through 200.
18 A Read
§4013. Complete columns 6 and 7, lines 1
through 200.
19 B, Part I & B-1 Read §4020. Complete all columns through column 26.
20 B, Part II Read §4021. Complete entire worksheet.
21 B-2 Read §4022. Complete, if applicable.
22 L-1, Part I Read §§4065-4065.1. Complete, if applicable.
Rev. 40-13
4001 (Cont.) FORM CMS-2552-10 DRAFT
Part II - Departmental Cost Distribution and Cost Apportionment
Step Worksheet Instructions
 1 C Read
§§4023-4023.1.
Complete entire worksheet, except for line 92.
1 C Read
§§4023-4023.1.
Complete entire worksheet, except for line 92.
2 D, Part I Read §§4024-4024.1. Complete entire worksheet.
3 D, Part III Read §§4024 and 4024.3. Complete entire worksheet.
4 L-1, Part II Read §4065.2. Complete, if applicable.
5 D-1, Parts I & IV Read §§4025, 4025.1 and 4025.4. Complete both parts.
 6 C Read
§4023.1. Complete line 92.
6 C Read
§4023.1. Complete line 92.
7 D, Part II Read §§4024 and 4024.2. Complete entire worksheet. A separate worksheet must be completed for each applicable healthcare program for each hospital and subprovider subject to PPS or TEFRA provisions.
 8 D,
Part IV Read §§4024 and 4024.4. Complete entire
worksheet. A separate worksheet must be completed for each
applicable health care program for each hospital and subprovider
subject to PPS or TEFRA provisions.
8 D,
Part IV Read §§4024 and 4024.4. Complete entire
worksheet. A separate worksheet must be completed for each
applicable health care program for each hospital and subprovider
subject to PPS or TEFRA provisions.
 9 L-1,
Part III Read §4065.3. Complete, if applicable.
9 L-1,
Part III Read §4065.3. Complete, if applicable.
10 D, Part V Read §§4024 and 4024.5. Complete entire worksheet. A separate worksheet must be completed for each applicable health care program for each applicable provider component.
11 D-3 Read §4027. Complete entire worksheet. A separate copy of this worksheet must be completed for each applicable health care program for each applicable provider component.
12 D-1, Parts I & II Read §§4025, 4025.1 and 4025.2. All providers must complete Part I. The hospital and subprovider(s) must complete Part II, lines 38 through 49 and lines 64 through 69.
40-14 Rev.
DRAFT FORM CMS-2552-10 4001 (Cont.)
Step Worksheet Instructions
12 D-1, Parts III & IV Read §§4025, 4025.3 and 4025.4. Only the hospital-based SNF and hospital-based NF must complete Part III, lines 70 through 86. All providers must complete Part IV.
13 D-2, Parts I through III Read §§4026-4026.3. Complete only those parts that are applicable. Do not complete Part III unless both Parts I and II are completed.
14 L, Parts I through III Read §4064. Complete applicable parts.
15 D-5, Parts I and II, or Read §§4029-4029.4. Complete applicable parts.
Parts III and IV
16 D-4, Parts I through IV Read §§4028-4028.4. Complete only if hospital is a certified transplant center.
17 E-4 Read §§4034. Complete entire worksheet, if applicable.
Rev. 40-15
4001 (Cont.) FORM CMS-2552-10 DRAFT
Part III - Calculation and Apportionment of Hospital-Based Facilities
A. Title XVIII - For SNF Only Reimbursed Under PPS.--
Step Worksheet Instructions
1 E-3, Part VI Read §4033.6. If applicable, complete lines 1 through 15 for title XVIII SNF PPS services.
2 E-1, Part I Read §4031.1. Complete this worksheet for title XVIII services corresponding to Worksheet E-3, Part VI.
3 E-3, Part VI Complete the remainder of this worksheet, lines 16 through 19.
B. Titles V and XIX - For Hospital, Subprovider(s), NF and ICF/IIDs.--
Step Worksheet Instructions
4 E-3, Part VII Read §4033.7. If applicable, complete entire worksheet for titles V and XIX services. Use a separate worksheet for each title.
C. Title XVIII - For Swing Bed-SNF and Titles V and XIX - For Swing Bed-NF.--
Step Worksheet Instructions
5 E-2 Read §4032. Complete a separate copy of this worksheet (lines 1 through 19) for each applicable health care program for each applicable provider component. Only entries applicable to title XVIII are made in column 2. Complete lines 9, 13, and 17 of column 1 for titles V and XIX, and columns 1 and 2 for title XVIII.
6 E-1, Part I Read §4031.1. Complete this worksheet for title XVIII services corresponding to Worksheet E-2 title XVIII swing bed-SNF only.
7 E-2 Complete the remainder of this worksheet, lines 20 through 23.
40-16 Rev.
DRAFT FORM CMS-2552-10 4001 (Cont.)
D. Title XVIII Only - For Home Health Agency.--
Step Worksheet Instructions
8 H Read §4041. Complete entire worksheet, if applicable.
9 H-1, Parts I and II Read §4042. Complete entire worksheet, if applicable.
10 H-2, Parts I and II Read §§4043-4043.2. Complete entire worksheet, if applicable.
11 H-3, Parts I and II Read §§4044-4044.2. Complete entire worksheet, if applicable.
12 H-4, Parts I and II Read §§4045-4045.2. Complete entire worksheet, if applicable.
13 H-5 Read §4046. Complete entire worksheet, if applicable.
E. Title XVIII- For ESRD.--
Step Worksheet Instructions
14 I-1 Read §§4047-4048. Complete a separate worksheet for renal dialysis department(s) and a separate worksheet for home program dialysis department(s), if applicable.
15 I-2 Read §4049. Complete a separate worksheet for renal dialysis department(s) and a separate worksheet for home program dialysis department(s), if applicable.
16 I-3 Read §4050. Complete a separate worksheet for renal dialysis department(s) and a separate worksheet for home program dialysis department(s), if applicable.
17 I-4 Read §§4051. Complete a separate worksheet for renal dialysis department(s) and a separate worksheet for home program dialysis department(s), if applicable.
18 I-5 Read §4052. Complete only one worksheet combining all renal dialysis departments and home program dialysis departments, if applicable.
Rev. 40-17
4001 (Cont.) FORM CMS-2552-10 DRAFT
F. Title XVIII - For CMHC.--
Step Worksheet Instructions
19 J-1, Parts I and II Read §§4053-4053.2. Complete entire worksheet, if applicable.
20 J-2, Part I Read §§4054-4054.1. Complete entire worksheet, if applicable.
21 J-2, Part II Read §4054.2. Complete entire worksheet, if applicable.
22 J-3 Read §4055. Complete entire worksheet, if applicable.
23 J-4 Read §4056. Complete lines 1 through 4 for title XVIII only.
G. Titles XVIII and XIX - For Provider Based-Hospice.--
Step Worksheet Instructions
24 K-1 Read §4058. Complete entire worksheet, if applicable.
25 K-2 Read §4059. Complete entire worksheet, if applicable.
26 K-3 Read §4060. Complete entire worksheet, if applicable.
27 K Read §4057. Complete entire worksheet, if applicable.
28 K-4, Parts I and II Read §4061. Complete both worksheets, if applicable.
29 K-5, Parts I, II & III Read §§4062-4062.3. Complete all worksheets, if applicable.
30 K-6 Read §4063. Complete entire worksheet, if applicable.
40-18 Rev.
DRAFT FORM CMS-2552-10 4001 (Cont.)

 H.
Titles V, XVIII, and XIX - For
Hospital-Based
RHC/FQHC.--
H.
Titles V, XVIII, and XIX - For
Hospital-Based
RHC/FQHC.--
Step Worksheet Instructions


 31 M-1 Read
§4066. Complete entire worksheet, if applicable.
31 M-1 Read
§4066. Complete entire worksheet, if applicable.


 32 M-2 Read
§4067. Complete entire worksheet, if applicable.
32 M-2 Read
§4067. Complete entire worksheet, if applicable.

 33 M-3 Read
§4068. Complete entire worksheet, if applicable.
33 M-3 Read
§4068. Complete entire worksheet, if applicable.

 34 M-4 Read
§4069. Complete entire worksheet, if applicable.
34 M-4 Read
§4069. Complete entire worksheet, if applicable.


 35 M-5 Read
§4070. Complete entire worksheet, if applicable, for title
XVIII only.
35 M-5 Read
§4070. Complete entire worksheet, if applicable, for title
XVIII only.

 I.
Titles V, XVIII, and XIX -
For Hospital-Based FQHC.--
I.
Titles V, XVIII, and XIX -
For Hospital-Based FQHC.--
 Step Worksheet Instructions
Step Worksheet Instructions


 36 N-1 Read
§4071. Complete entire worksheet, if applicable.
36 N-1 Read
§4071. Complete entire worksheet, if applicable.


 37 N-2 Read
§4071.1. Complete entire worksheet, if applicable.
37 N-2 Read
§4071.1. Complete entire worksheet, if applicable.

 38 N-3 Read
§4071.2. Complete entire worksheet, if applicable.
38 N-3 Read
§4071.2. Complete entire worksheet, if applicable.

 39 N-4 Read
§4071.3. Complete entire worksheet, if applicable.
39 N-4 Read
§4071.3. Complete entire worksheet, if applicable.


 40 N-5 Read
§4071.4. Complete entire worksheet, if applicable, for title
XVIII only.
40 N-5 Read
§4071.4. Complete entire worksheet, if applicable, for title
XVIII only.

 J.
Titles V, XVIII, and XIX -
For Hospital-Based
Hospice.--
J.
Titles V, XVIII, and XIX -
For Hospital-Based
Hospice.--
 Step Worksheet Instructions
Step Worksheet Instructions
41 O-1, O-2, O-3, O-4 Read §4072.1. Complete entire worksheet, if applicable.
42 O Read §4072. Complete entire worksheet, if applicable.
43 O-5 Read §4072.2. Complete entire worksheet, if applicable.
44 O-6, Parts I and II Read §4072.3. Complete both worksheets in entirety, if applicable.
45 O-7 Read §4072.4. Complete entire worksheet, if applicable.
46 O-8 Read §4072.5. Complete entire worksheet, if applicable.
Rev. 40-19
4001 (Cont.) FORM CMS-2552-10 DRAFT
Part IV - Calculation of Reimbursement Settlement
Step Worksheet Instructions
1 E, Part A Read §§4030-4030.1. Complete lines 1 through 71 for title XVIII for each applicable provider component subject to IPPS.
2 E-1, Part I Read §4031.1. Complete this worksheet for title XVIII services corresponding to Worksheet E, Part A.
3 E, Part A Complete the remainder of this worksheet, lines 72 through 75.
4 E, Part B Read §4030.2. Complete lines 1 through 40 for title XVIII for each applicable provider component.
5 E-1, Part I Read §4031.1. Complete this worksheet for title XVIII services corresponding to Worksheet E, Part B.
6 E, Part B Complete the remainder of this worksheet, lines 41 through 44.
7 E-3, Part I Read §§4033-4033.1. If applicable, complete lines 1 through 18 for title XVIII for each applicable provider component subject to TEFRA.
8 E-1, Part I Read §4031.1. Complete this worksheet for title XVIII services corresponding to Worksheet E-3, Part I.
9 E-3, Part I Complete the remainder of this worksheet, lines 19 through 22.
10 E-3, Part II Read §4033.2. If applicable, complete lines 1 through 31 for title XVIII IPF PPS.
11 E-1, Part I Read §4031.1. Complete this worksheet for title XVIII services corresponding to Worksheet E-3, Part II.
12 E-3, Part II Complete the remainder of this worksheet, lines 32 through 35.
40-20 Rev.
DRAFT FORM CMS-2552-10 4001 (Cont.)
Step Worksheet Instructions
13 E-3, Part III Read §4033.3. If applicable, complete lines 1 through 32 for title XVIII IRF PPS.
14 E-1, Part I Read §4031.1. Complete this worksheet for title XVIII services corresponding to Worksheet E-3, Part III.
15 E-3, Part III Complete the remainder of this worksheet, lines 33 through 36.
16 E-3, Part IV Read §4033.4. If applicable, complete lines 1 through 22 for title XVIII LTCH PPS.
17 E-1, Part I Read §4031.1. Complete this worksheet for title XVIII services corresponding to Worksheet E-3, Part IV.
18 E-3, Part IV Complete the remainder of this worksheet, lines 23 through 26.
19 E-3, Part V Read §4033.5. If applicable, complete lines 1 through 30 for title XVIII reasonable cost reimbursed providers.
20 E-1, Part I Read §4031.1. Complete this worksheet for title XVIII services corresponding to Worksheet E-3, Part V.
21 E-3, Part V Complete the remainder of this worksheet, lines 31 through 34.
19 E-3, Part VI Read §4033.6. If applicable, complete lines 1 through 15 for title XVIII reasonable cost reimbursed providers.
20 E-1, Part I Read §4031.1. Complete this worksheet for title XVIII services corresponding to Worksheet E-3, Part VI.
21 E-3, Part VI Complete the remainder of this worksheet, lines 16 through 19.
22 E-3, Part VII Read §4033.7. If applicable, complete the entire worksheet for titles V and XIX providers.
Rev. 40-21
4001 (Cont.) FORM CMS-2552-10 DRAFT
Part V - Additional Data
Step Worksheet Instructions
1 G Read §4040. All providers maintaining fund type accounting records must complete this worksheet. Nonproprietary providers which do not maintain fund type records complete the General Fund column only.
2 G-1 Read §4040.1. Complete entire worksheet.
3 G-2, Parts I & II Read §4040.2. Complete entire worksheet.
4 G-3 Read §4040.3. Complete entire worksheet.
5 S-10 Read §4012. Acute care hospitals and CAHs complete this worksheet.
6 E-1, Part II Read §4031.2 Acute care hospitals and CAHs complete this worksheet.
7 S, Parts I, II, and III Read §§4003.1-4003.3. Complete Part III, then complete Parts I and II.
40-22 Rev.
DRAFT FORM CMS-2552-10 4002.1
4002. SEQUENCE OF ASSEMBLY
The following examples of assembly of worksheets are provided so all providers are consistent in the order of submission of their annual cost report. All providers using Form CMS-2552-10 must adhere to this sequence. If worksheets are not completed because they are not applicable, do not include blank worksheets in the assembly of the cost report.
4002.1 Sequence of Assembly for Hospital and Hospital Health Care Complex Providers Participating in Medicare.--Cost report worksheets are assembled in alpha-numeric sequence starting with the "S" series, followed by A, B, C, etcetera.
Work- Health Care
Form CMS sheet Part Program (Title) Component
2552-10 S I - III
2552-10 S-2 I & II
2552-10 S-3 I - V
2552-10 S-4 Hospital-Based HHA
2552-10 S-5 Renal Dialysis Department
2552-10 S-6 Hospital-Based CMHC
 2552-10 S-7 Hospital-Based
SNF
2552-10 S-7 Hospital-Based
SNF
 2552-10 S-8 Hospital-Based
RHC/FQHC
2552-10 S-8 Hospital-Based
RHC/FQHC
2552-10 S-9 Hospital-Based Hospice
2552-10 S-10 Hospital & CAH
2552-10 S-11 I - III Hospital-Based FQHC
2552-10 A
2552-10 A-6
2552-10 A-7 I - III
2552-10 A-8
2552-10 A-8-1
2552-10 A-8-2
2552-10 A-8-3 I - VI
2552-10 B I
2552-10 B II
2552-10 B-1
2552-10 B-2
2552-10 C I Hospital
2552-10 C II V Hospital
2552-10 C II XIX Hospital
2552-10 D I V Hospital
2552-10 D II V Hospital
2552-10 D III V Hospital
2552-10 D IV V Hospital
2552-10 D V V Hospital
2552-10 D II V Subprovider
2552-10 D V V Subprovider
2552-10 D I XVIII Hospital
2552-10 D II XVIII Hospital
2552-10 D III XVIII Hospital
2552-10 D IV XVIII Hospital
2552-10 D V XVIII Hospital
2552-10 D II XVIII Subprovider
2552-10 D III XVIII Subprovider
Rev. 40-23
4002.1 (Cont.) FORM CMS-2552-10 DRAFT
Work- Health Care
Form CMS sheet Part Program (Title) Component
2552-10 D V XVIII Subprovider
2552-10 D III XVIII Swing Bed SNF
2552-10 D III XVIII SNF
2552-10 D I XIX Hospital
2552-10 D II XIX Hospital
2552-10 D III XIX Hospital
2552-10 D IV XIX Hospital
2552-10 D V XIX Hospital
2552-10 D II XIX Subprovider
2552-10 D V XIX Subprovider
2552-10 D-1 I, II, & IV V Hospital
2552-10 D-1 I, II, & IV V Subprovider
2552-10 D-1 I & III V SNF
 2552-10 D-1 I
& III V NF, ICF/IID
2552-10 D-1 I
& III V NF, ICF/IID
2552-10 D-1 I, II, & IV XVIII Hospital
2552-10 D-1 I, II, & IV XVIII Subprovider
2552-10 D-1 I & III XVIII SNF
2552-10 D-1 I, II, & IV XIX Hospital
2552-10 D-1 I, II, & IV XIX Subprovider
2552-10 D-1 I & III XIX SNF
 2552-10 D-1 I
& III XIX NF, ICF/IID
2552-10 D-1 I
& III XIX NF, ICF/IID
2552-10 D-2 I V, XVIII, & XIX
2552-10 D-2 II XVIII
2552-10 D-2 III XVIII
2552-10 D-3 V Hospital
2552-10 D-3 V Subprovider
2552-10 D-3 V Swing Bed SNF
2552-10 D-3 V Swing Bed NF
2552-10 D-3 V SNF
2552-10 D-3 V NF, ICF/IID
2552-10 D-3 XVIII Hospital
2552-10 D-3 XVIII Subprovider
2552-10 D-3 XVIII Swing Bed SNF
2552-10 D-3 XIX Hospital
2552-10 D-3 XIX Subprovider
2552-10 D-3 XIX Swing Bed SNF
2552-10 D-3 XIX Swing Bed NF
2552-10 D-3 XIX SNF
2552-10 D-3 XIX NF, ICF/IID
2552-10 D-4 I - IV XVIII
2552-10 D-5 I V, XVIII, & XIX
2552-10 D-5 II V, XVIII, & XIX Hospital
2552-10 D-5 II V, XVIII, & XIX Subprovider
2552-10 E A XVIII Hospital
2552-10 E B XVIII Hospital
2552-10 E-1 Part I XVIII Hospital
2552-10 E-1 Part I XVIII IPF-Subprovider
2552-10 E-1 Part I XVIII IRF-Subprovider
2552-10 E-1 Part I XVIII Subprovider
2552-10 E-1 Part I XVIII Swing Bed SNF
2552-10 E-1 Part I XVIII SNF
40-24 Rev.
DRAFT FORM CMS-2552-10 4002.1 (Cont.)
Work- Health Care
Form CMS sheet Part Program (Title) Component
2552-10 E-1 II HIT Hospital and CAH
2552-10 E-2 V Swing Bed SNF
2552-10 E-2 V Swing Bed NF
2552-10 E-2 XVIII Swing Bed SNF
2552-10 E-2 XIX Swing Bed SNF
2552-10 E-2 XIX Swing Bed NF
2552-10 E-3 I - V XVIII Hospital
2552-10 E-3 II & III XVIII Subprovider
2552-10 E-3 IV XVIII LTCH
2552-10 E-3 VI XVIII SNF
2552-10 E-3 VII V & XIX Hospital
2552-10 E-3 VII V & XIX NF, ICF/IID
2552-10 E-3 VII V & XIX SNF
2552-10 G
2552-10 G-1
2552-10 G-2
2552-10 G-3
2552-10 H Hospital-based HHA
2552-10 H-1 I & II Hospital-based HHA
2552-10 H-2 I & II Hospital-based HHA
2552-10 H-3 I & II V, XVIII, & XIX Hospital-based HHA
2552-10 H-4 I & II V, XVIII, & XIX Hospital-based HHA
2552-10 H-5 XVIII Hospital-based HHA
2552-10 I-1 - I-5 Renal Dialysis
2552-10 I-1 - I-5 Home Program Dialysis
2552-10 J-1 - J-2 I & II CMHC
2552-10 J-3 V, XVIII, & XIX CMHC
2552-10 J-4 XVIII CMHC
2552-10 K Hospital-based Hospice
2552-10 K-1 Hospital-based Hospice
2552-10 K-2 Hospital-based Hospice
2552-10 K-3 Hospital-based Hospice
2552-10 K-4 I & II Hospital-based Hospice
2552-10 K-5 I - III Hospital-based Hospice
2552-10 K-6 XVIII, XIX Hospital-based Hospice
2552-10 L I - III V, XVIII, & XIX Hospital
2552-10 L I - III V, XVIII, & XIX Subprovider
2552-10 L-1 I Hospital
2552-10 L-1 II V, XVIII, & XIX Hospital
2552-10 L-1 III V, XVIII, & XIX Hospital
2552-10 L-1 III V, XVIII, & XIX Subprovider
2552-10 M-1 Hospital-based RHC/FQHC
2552-10 M-2 Hospital-based RHC/FQHC
2552-10 M-3 V, XVIII, & XIX Hospital-based RHC/FQHC
2552-10 M-4 V, XVIII, & XIX Hospital-based RHC/FQHC
2552-10 M-5 XVIII Hospital-based RHC/FQHC
2552-10 N-1 Hospital-based FQHC
2552-10 N-2 XVIII Hospital-based FQHC
2552-10 N-3 XVIII Hospital-based FQHC
2552-10 N-4 XVIII Hospital-based FQHC
2552-10 N-5 XVIII Hospital-based FQHC
2552-10 O Hospital-based Hospice
2552-10 O-1 Hospital-based Hospice
2552-10 O-2 Hospital-based Hospice
Rev. 40-25
4002.1 (Cont.) FORM CMS-2552-10 DRAFT
Work- Health Care
Form CMS sheet Part Program (Title) Component
2552-10 O-3 Hospital-based Hospice
2552-10 O-4 Hospital-based Hospice
2552-10 O-5 Hospital-based Hospice
2552-10 O-6 I & II Hospital-based Hospice
2552-10 O-7 Hospital-based Hospice
2552-10 O-8 Hospital-based Hospice
40-25.1 Rev.
DRAFT FORM CMS-2552-10 4002.1 (Cont.)
This page is reserved for future use.
Rev. 40-25.2
4003 FORM CMS-2552-10 DRAFT
4003. WORKSHEET S - HOSPITAL AND HOSPITAL HEALTH CARE COMPLEX COST REPORT CERTIFICATION AND SETTLEMENT SUMMARY
4003.1 Part I - Cost Report Status.--This section is to be completed by the provider and contractor as indicated on the worksheet.
Lines 1 through 3, column 1--The provider must check the appropriate box to indicate on line 1 or 2, whether this cost report is being filed electronically or manually. For manually submitted cost reports, line 2 is only completed by providers filing low utilization cost reports in accordance with CMS Pub. 15-2, chapter 1, §110, or providers demonstrating financial hardship in accordance with §133. For electronic submitted cost reports, indicate on line 1, the date and time corresponding to the creation of the electronic file. This date and time remain identifiers for the file by the contractor and are archived accordingly. This file is your original submission and is not to be modified. If this is an amended cost report, enter on line 3 the number of times the cost report has been amended.
Line 4, column 1--The provider must enter an “F” if this is a full cost report or an “L” for a low Medicare utilization (requires prior contractor approval, see CMS Pub. 15-2, chapter 1, §110).
Line 5, column 1--The contractor enters the Healthcare Cost Report Information System (HCRIS) cost report status code on line 5, column 1 that corresponds to the filing status of the cost report: 1=As submitted; 2=Settled without audit; 3=Settled with audit; 4=Reopened; or 5=Amended.
Line 6, column 2--The contractor enters the date (mm/dd/yyyy) an accepted cost report was received from the provider.
Line 7, column 2--The contractor enters the 5 position contractor number.
Lines 8 and 9, column 2--If this is an initial cost report, enter “Y” for yes in the box on line 8. If this is a final cost report, enter “Y” for yes in the box on line 9. If neither, enter “N”.
An initial report is the very first cost report for a particular provider CCN. A final cost report is a terminating cost report for a particular provider CCN.
If the cost report is both initial and terminating in the same year (for example, the provider started Medicare and decided to leave the program in the same year), and the cost report is a full Medicare utilization report, the contractor must submit to HCRIS an as submitted and a final settled report. The as submitted extract is the initial report, and the final settled is the final report.
If the cost report is both initial and terminating in the same year, and the cost report is a No or Low Medicare utilization, the contractor must only submit to HCRIS a final settled with or without audit report. This is the only situation in which a HCRIS extract would be both initial and final.
Line 10, column 3--The contractor enters the Notice of Program Reimbursement (NPR) date (mm/dd/yyyy). The NPR date must be present if the cost report status code is 2 or 3.
Line 11, column 3--Enter software vendor code of the cost report software used by the contractor to process this HCRIS cost report file. Use “4” for HFS or “3” for KPMG.
Line 12, column 3--If this is a reopened cost report (response to line 5, column 1 is “4”), the contractor enters the number of times the cost report has been reopened.
4003.2 Part II - Certification.--This certification is read, prepared, and signed by an officer or administrator of the provider after the cost report has been completed in its entirety.
40-26 Rev.
DRAFT FORM CMS-2552-10 4003.3 (Cont.)
4003.3 Part III - Settlement Summary.--Enter the balance due to or due from the applicable program for each applicable component of the hospital or hospital healthcare complex. Transfer settlement amounts as follows:
FROM
Hospital/ Title XVIII Title XVIII
Hospital Component Title V Part A Part B HIT Title XIX
Hospital Wkst. E-3, Wkst. E, Wkst. E, Wkst. E-1, Wkst. E-3, Part VII, Part A, Part B, Part II, Part VII,
line 42 line 74 line 43 line 32 line 42
or Wkst. E-3,
Part I,
line 21
or
Wkst. E-3,
Part II,
line 34
or
Wkst. E-3,
Part III,
line 35
or
Wkst. E-3,
Part IV,
line 25
or
Wkst. E-3,
Part V,
line 33
Subprovider-IPF Wkst. E-3, Wkst. E-3, Wkst. E Wkst. E-3,
Part VII, Part II, Part B, Part VII,
line 42 line 34 line 43 line 42
Subprovider-IRF Wkst. E-3 Wkst. E-3, Wkst. E Wkst E-3,
Part VII, Part III, Part B, Part VII
line 42 line 35 line 43 line 42
Subprovider-Other
Swing Bed - SNF Wkst. E-2, Wkst. E-2, Wkst. E-2, Wkst. E-2,
col. 1, col. 1, col. 2, col. 1,
line 22 line 22 line 22 line 22
Swing Bed - NF Wkst. E-2, N/A N/A Wkst. E-2
col. 1, col. 1,
line 22 line 22
SNF Wkst. E-3, Wkst. E-3, Wkst. E, Wkst. E-3,
Part VII, Part VI, Part B, Part VII,
line 42 line 18 line 43 line 42
NF, ICF/IID Wkst. E-3, N/A N/A Wkst. E-3,
Part VII, Part VII
line 42 line 42
Rev. 40-27
DRAFT FORM CMS-2552-10 4003.3 (Cont.)
FROM
Hospital/ Title XVIII Title XVIII
Hospital Component Title V Part A Part B Title XIX
Home Health Wkst. H-4, Wkst. H-4, Wkst. H-4, Wkst. H-4,
Agency Part II, Part II, Part II, Part II, sum of cols. col. 1, col. 2, sum of cols. 1&2, line 34 line 34 line 34 1 & 2, line 34
Outpatient Wkst. N/A Wkst. Wkst.
Rehabilitation J-3, J-3, J-3,
Providers line 29 line 29 line 29
Hospital-Based Wkst. N/A Wkst. Wkst.
RHC/FQHC* M-3, M-3, M-3,
line 29 line 29 line 29
Hospital-based Wkst. Wkst. Wkst.
FQHC** N-4, N-4, N-4,
line 19 line 19 line 19
*For hospital-based FQHCs for cost reporting periods beginning prior to October 1, 2014.
**For hospital-based FQHCs for cost reporting periods beginning on and after October 1, 2014.
40-28 Rev.
DRAFT FORM CMS-2552-10 4004.1
4004. WORKSHEET S-2 - HOSPITAL AND HOSPITAL HEALTH CARE COMPLEX
IDENTIFICATION DATA
This worksheet consists of two parts:
Part I - Hospital and Hospital Health Care Complex Identification Data
Part II - Hospital and Hospital Health Care Complex Reimbursement Questionnaire
4004.1 Part I - Hospital and Hospital Health Care Complex Identification Data.--The information required on this worksheet is needed to properly identify the provider. The responses to all lines are Yes or No unless otherwise indicated.
Line descriptions
Lines 1 and 2--Enter the street address, post office box (if applicable), the city, state, ZIP code, and county of the hospital.
Lines 3 through 17--Enter on the appropriate lines and columns the component names, CMS certification numbers (CCN), core based statistical area (CBSA) codes (non-CBSA (rural) codes are assembled by placing the digits “999” in front of the two digit state code, e.g., for the State of Maryland the non-CBSA code is 99921), provider type, and certification dates of the hospital and its various components, if any. Indicate for each health care program (titles V, XVIII, or XIX), the payment system applicable to the hospital and its various components by entering P, T, O, or N in the appropriate column to designate PPS, TEFRA, OTHER, or NOT APPLICABLE, respectively. The “OTHER” payment system includes critical access hospitals (CAHs) and cost reimbursed providers such as new TEFRA providers exempt from the rate of increase limits.
Column 4--Indicate, as applicable, the number listed below which best corresponds with the type of services provided.
1 = General Short Term 6 = Religious Non-Medical Health Care Institution
2 = General Long Term 7 = Children
3 = Cancer 8 = Alcohol and Drug
4 = Psychiatric 9 = Other
5 = Rehabilitation
If your hospital services various types of patients, indicate "General - Short Term" or "General - Long Term," as appropriate.
NOTE: Long term care hospitals are hospitals organized to provide long term treatment programs with average lengths of stay greater than 25 days. Some hospitals may be certified as other than long term care hospitals, but also have average lengths of stay greater than 25 days.
If your hospital cares for only a special type of patient (such as cancer patients), indicate the special group served. If you are not one of the hospital types described in items 1 through 8 above, indicate 9 for "Other".
Line 3--This is an institution which meets the requirements of §1861(e) or §1861(mm)(1) of the Act and participates in the Medicare program or is a federally controlled institution approved by CMS.
Line 4--The distinct part inpatient psychiatric facility (IPF) is a portion of a general hospital which has been issued a subprovider CCN because it offers a clearly different type of service from the remainder of the hospital with such services reimbursed under inpatient psychiatric PPS. (See 42 CFR 412.25)
Rev. 40-29
4004.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 5--The distinct part inpatient rehabilitation facility (IRF) is a portion of a general hospital which has been issued a subprovider CCN because it offers a clearly different type of service from the remainder of the hospital with such services reimbursed under inpatient rehabilitation PPS. (See 42 CFR 412.25)
Line 6--This is a portion of a general hospital defined as non-Medicare certified and not included in lines 4 through 18, which offers a clearly different type of service from the remainder of the hospital.
Line 7--Medicare swing-bed services are paid under the SNF PPS system (indicate payment system as “P”). CAHs are reimbursed on a cost basis for swing-bed services and should indicate “O” as the payment system. Rural hospitals with fewer than 100 beds may be approved by CMS to use these beds interchangeably as hospital and skilled nursing facility beds with payment based on the specific care provided, as authorized by §1883 of the Act. (See CMS Pub. 15-1, chapter 22, §§2230-2230.6.)
Line 8--Swing bed-NF services are not payable under the Medicare program but are payable under State Medicaid programs if included in the Medicaid State plan. Rural hospitals with fewer than 100 beds that have a Medicare swing bed agreement approved by CMS and that are approved by the State Medicaid agency to use these beds interchangeably as hospital and other nursing facility beds, with payment based on the specific level of care provided, as authorized by §1913 of the Act.
Line 9--This is a distinct part skilled nursing facility that has been issued an SNF identification number and which meets the requirements of §1819 of the Act. For cost reporting periods beginning on or after October 1, 1996, a complex cannot contain more than one hospital-based SNF or hospital-based NF.
Line 10--This is a distinct part nursing facility which has been issued a separate identification number and which meets the requirements of §1905 of the Act. (See 42 CFR 441.400 for standards for other nursing facilities, for other than facilities for individuals with intellectual disabilities, and for facilities for individuals with intellectual disabilities.) If your State recognizes only one level of care, i.e., skilled, do not complete any lines designated as NF and report all activity on the SNF line for all programs. The NF line is used by facilities having two levels of care, i.e., either 100 bed facility all certified for NF and partially certified for SNF or 50 beds certified for SNF only and 50 beds certified for NF only. The contractor will reject a cost report attempting to report more than one nursing facility.
If the facility operates an Intermediate Care Facility for Individuals with Intellectual Disabilities (ICF/IID) subscript line 10 to 10.01 and enter the data on that line. Note: Subscripting is allowed only for the purpose of reporting an ICF/IID.
Line 11--This is any other hospital-based facility not listed above. The beds in this unit are not certified for titles V, XVIII, or XIX.
Line 12--This is a distinct part HHA that has been issued an HHA identification number and which meets the requirements of §§1861(o) and 1891 of the Act. If you have more than one hospital-based HHA, subscript this line, and report the required information for each HHA.
Line 13--This is a distinct entity that operates exclusively for the purpose of providing surgical services to patients not requiring hospitalization and which meets the conditions for coverage in 42 CFR 416, Subpart B. The ASC operated by a hospital must be a separately identifiable entity which is physically, administratively, and financially independent and distinct from other operations of the hospital. (See 42 CFR 416.30(f).) Under this restriction, hospital outpatient departments providing ambulatory surgery (among other services) are not eligible. (See 42 CFR 416.120(a).)
40-30 Rev.
DRAFT FORM CMS-2552-10 4004.1 (Cont.)
Line 14--This is a distinct part hospice and separately certified component of a hospital which meets the requirements of §1861(dd) of the Act. No payment designation is required in columns 6, 7, and 8.
Lines 15 and 16--Enter the applicable information for hospital-based rural health clinics (RHCs) on line 15 and for hospital-based federally qualified health centers (FQHCs) on line 16. These lines are used by hospital-based RHCs and/or FQHCs which have been issued a CCN and meet the requirements of §1861(aa) of the Act. If you have more than one hospital-based RHC, report them on subscripts of line 15. If you have more than one hospital-based FQHC, report them on subscripts of line 16. Report the required information in the appropriate column for each. Hospital-based RHCs and FQHCs may elect to file a consolidated cost report pursuant to CMS Pub. 100-04 (Medicare Claims Processing Manual), chapter 9, §30.8. Do not subscript this line if you elect to file under the consolidated cost reporting method. See §§4010 and 4010.1 for further instructions.
Line 17--This line is used by hospital-based community mental health centers (CMHCs). Subscript this line as necessary to accommodate multiple CMHCs (lines 17.00-17.09). Also subscript this line to accommodate CORFs (lines 17.10-17.19), OPTs (lines 17.20-17.29), OOTs (lines 17.30-17.39) and OSPs (lines 17.40-17.49). (See §4095, Exhibit 2, Table 4, Part III.)
Line 18--If this facility operates a renal dialysis facility (CCN 2300-2499), a renal dialysis satellite (CCN 3500-3699), and/or a special purpose renal dialysis facility (CCN 3700-3799), enter in column 2 the applicable CCN. Subscript this line as applicable.
Line 19--For any component type not identified on lines 3 through 18, enter the required information in the appropriate column.
Line 20--Enter the inclusive dates covered by this cost report. In accordance with 42 CFR 413.24(f), you are required to submit periodic reports of your operations which generally cover a consecutive 12 month period of your operations. (See CMS Pub. 15-2, chapter 1, §§102.1‑102.3, for situations where you may file a short period cost report.)
Line 21--Indicate the type of control under which the hospital operates:
1 = Voluntary Nonprofit, Church 8 = Governmental, City-County
2 = Voluntary Nonprofit, Other 9 = Governmental, County
3 = Proprietary, Individual 10 = Governmental, State
4 = Proprietary, Corporation 11 = Governmental, Hospital District
5 = Proprietary, Partnership 12 = Governmental, City
6 = Proprietary, Other 13 = Governmental, Other
7 = Governmental, Federal
Line 22--Does your facility qualify and is it currently receiving payments for disproportionate share hospital adjustment, in accordance with 42 CFR 412.106? Enter in column 1, “Y” for yes or “N” for no. Is this facility subject to the provisions of 42 CFR 412.106(c)(2) (Pickle Amendment hospitals)? Enter in column 2, “Y” for yes or “N” for no.
Line 22.01--For cost reporting periods that overlap or begin on or after October 1, 2013, did this hospital receive interim uncompensated care payments? Enter in column 1, “Y” for yes or “N” for no, for the portion of the cost reporting period prior to October 1. Enter in column 2, “Y” for yes or “N” for no, for the portion of the cost reporting period beginning on or after October 1. For cost reporting periods that begin on October 1, complete only column 2 (i.e., enter “N” for no in column 1 or leave column 1 blank). The responses to Worksheet S-2, columns 1 and 2, correspond to Worksheet E, Part A, columns 1 and 2, respectively, for lines 35 through 35.02.
Line 23--Indicate in column 1 the method used to capture Medicaid (title XIX) days reported on lines 24 and/or 25 of this worksheet during the cost reporting period by entering a “1” if days are based on the date of admission, “2” if days are based on census days (also referred to as the day count), or “3” if days are based on the date of discharge. Is the method of identifying the days in
Rev. 40-31
4004.1 (Cont.) FORM CMS-2552-10 DRAFT
the current cost reporting period different from the method used in the prior cost reporting period? Enter in column 2 “Y” for yes or “N” for no.
NOTE: For lines 24 and 25, columns 1 through 6 are mutually exclusive. For example, if patient days are entered in column 1, those days may not be entered in any other columns.
Line 24--If line 23, column 1, is “3” and this is an IPPS provider, enter the in-state Medicaid paid days in column 1 (report these days on Worksheet S-3, Part I, column 7, line 1, and lines 8 through 13, as applicable), the in-state Medicaid eligible but unpaid days in column 2 (report these days on Worksheet S-3, Part I, column 7, line 2, for adult and pediatric patients, and line 13, for nursery patients, as applicable), the out-of-state Medicaid paid days in column 3 (report these days on Worksheet S-3, Part I, column 7, line 2, for adult and pediatric patients and line 13, for nursery patients, as applicable), the out-of-state Medicaid eligible but unpaid days in column 4 (report these days on Worksheet S-3, Part I, column 7, line 2, for adult and pediatric patients, and line 13, for nursery patients, as applicable), the Medicaid HMO paid and eligible but unpaid days in column 5 (report these days on Worksheet S-3, Part I, column 7, line 2 for adult and pediatric patients and line 13 for nursery patients, as applicable). Enter only labor and delivery days (reported on Worksheet S-3, Part 1, column 7, line 32) as “Other Medicaid days” in column 6. If line 23, column 1, is “1” or “2”, enter the Medicaid days based on each column description; however, these days may not equal the Medicaid days reported by discharge on Worksheet S-3, Part I. Do not include swing-bed, observation or hospice days in any columns on this line. See 42 CFR 412.106(a)(1)(ii) and 412.106(b)(4).
Line 25--If line 23, column 1, is “3” and this provider is an IRF or contains an IRF unit, enter the in-state Medicaid paid days in column 1, (report IRF days on Worksheet S-3, Part I, column 7, line 1, or IRF unit days on Worksheet S-3, Part I, column 7, line 17), the in-state Medicaid eligible but unpaid days in column 2 (report IRF days on Worksheet S-3, Part I, column 7, line 2, or IRF unit days on Worksheet S-3, Part I, column 7, line 4), the out-of-state Medicaid paid days in column 3 (report IRF days on Worksheet S-3, Part I, column 7, line 2, or IRF unit days on Worksheet S-3, Part I, column 7, line 4), the out-of-state Medicaid eligible but unpaid days in column 4 (report IRF days on Worksheet S-3, Part I, column 7, line 2, or IRF unit days on Worksheet S-3, Part I, column 7, line 4), the Medicaid HMO paid and eligible but unpaid days in column 5 (report IRF days on Worksheet S-3, Part I, column 7, line 2, or IRF unit days on Worksheet S-3, Part I, column 7, line 4). Do not enter any days in column 6 for cost reporting periods beginning on or after October 1, 2012. If line 23, column 1, is “1” or “2”, enter the Medicaid days based on each column description; however, these days may not equal the Medicaid days reported by discharge on Worksheet S-3, Part I. Do not include swing-bed, observation or hospice days in any columns on this line.
Line 26--For the Standard geographic classification (not wage), what is your status at the beginning of the cost reporting period. Enter “1” for urban or “2” for rural.
Line 27--For the Standard geographic classification (not wage), what is your status at the end of the cost reporting period. Enter “1” for urban or “2” for rural. If applicable, enter the effective date of the geographic reclassification in column 2.
Lines 28 through 34--Reserved for future use.
Line 35--If this is a sole community hospital (SCH), enter the number of periods (0, 1 or 2) within this cost reporting period that SCH status was in effect.
Line 36--Enter the beginning and ending dates of SCH status during this cost reporting period. Subscript line 36 if more than one period is identified for this cost reporting period and enter multiple dates. Multiple dates are created where there is a break in the date between SCH status, i.e., for calendar year provider SCH status dates are 1/1/2010 through 6/30/2010 and 9/1/2010 through 12/31/2010.
Line 37--If this is a Medicare dependent hospital (MDH), enter the number of periods within this
40-32 Rev.
DRAFT FORM CMS-2552-10 4004.1 (Cont.)
cost reporting period that MDH status was in effect.
Line 38--Enter the beginning and ending dates of MDH status during this cost reporting period. Subscript line 38 if more than one period is identified for this cost reporting period and enter multiple dates.
Line 39--For cost reporting periods that overlap or begin on or after October 1, 2010, does the hospital qualify for the inpatient hospital adjustment for low volume hospitals for a portion of the cost reporting period? Enter in column 1, “Y” for yes or “N” for no. If column 1 is “Y”, does the facility meet the mileage requirements in accordance with 42 CFR 412.101(b)(2)(ii)? Enter in column 2, “Y” for yes or “N” for no. Hospitals are required to request low-volume status in writing to their contractor and provide documentation that they meet the mileage criteria.
The response to these questions determines the completion of the low-volume calculation adjustment.
NOTE: 42 CFR 412.101(c)(2) provides for a temporary change in the low-volume adjustment for qualifying hospitals for federal fiscal year (FFYs) 2011 through March 31, 2015 as follows:
•Those hospitals with 200 or fewer Medicare discharges will receive an adjustment of an additional 25 percent for each Medicare discharge; and,
•Those with more than 200 and fewer than 1,600 Medicare discharges will receive an adjustment of an additional percentage for each Medicare discharge. This adjustment is calculated using the formula [(4/14) - (Medicare discharges/5600)].
To qualify as a low-volume hospital, the hospital must meet both of the following criteria:
•Be more than 15 road miles from the nearest subsection (d) hospital; and,
•Have fewer than 1,600 Medicare discharges based on the latest available Medicare Provider Analysis and Review (MedPAR) data as determined by CMS.
Lines 40 through 44--Reserved for future use.
Line 45--Does your facility qualify and receive capital payments for disproportionate share in accordance with 42 CFR 412.320? Enter "Y" for yes and "N" for no.
Line 46--Are you eligible for the exception payment for extraordinary circumstances pursuant to 42 CFR 412.348(f)? Enter “Y” for yes or “N” for no. If yes, complete Worksheets L, Part III, and L-1.
Line 47--Is this a new hospital under 42 CFR 412.300(b) (PPS capital)? Enter “Y” for yes or “N” for no for the respective programs.
Line 48--If line 47 is yes, do you elect full federal capital payment. Enter “Y” for yes or “N” for no for the respective programs.
Lines 49 through 55--Reserved for future use.
NOTE: CAHs complete question 107 in lieu of question 57.
Line 56--Is this a hospital involved in training residents in approved GME programs? Enter “Y” for yes or “N” for no.
Line 57--If line 56 is yes, is this the first cost reporting period in which you are training residents in approved programs? Enter “Y” for yes or “N” for no in column 1. If column 1 is yes, were residents training during the first month of the cost reporting period? Enter “Y” for yes or “N” for no in column 2. If column 2 is yes, complete Worksheet E-4. If column 2 is “N”, complete Worksheets D, Parts III and IV, and D-2, Part II, if applicable.
Rev. 40-33
4004.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 58--As a teaching hospital, did you elect cost reimbursement for teaching physicians as defined in CMS Pub. 15-1, chapter 21, §2148? Enter “Y” for yes or “N” for no. If yes, complete Worksheet D-5.
Line 59--Are you claiming costs of intern & resident in unapproved programs on Worksheet A, column 7, line 100? Enter “Y” for yes or “N” for no. If yes, complete Worksheet D-2, Part I.
Line 60--Are you claiming nursing school and/or allied health costs for a program that meets the provider-operated criteria under 42 CFR 413.85? Enter “Y” for yes or “N” for no. If yes, you must identify such costs in the applicable column(s) of Worksheet D, Parts III and IV, to separately identify nursing and allied health (paramedical education) from all other medical education costs.
Requirements During Five Year Period Following Implementation of Increases to Hospitals’ FTE Resident Caps Under Section 5503 of the Affordable Care Act (ACA), Lines 61 and Subscripts--Section 5503 of the ACA states that a hospital that receives an increase to its FTE resident cap under section 5503 shall ensure, during the 5-year period beginning on July 1, 2011, that:
(I) The number of FTE primary care residents is not less than the average number of FTE primary care residents during the three most recent cost reporting periods ending prior to the date of enactment of section 5503; and,
(II) Not less than 75 percent of the positions attributable to such increase are in a primary care or general surgery residency.
Failure to comply with either of these two requirements, known as the 3-year primary care average requirement (I) and the 75 percent test (II), means permanent removal of all section 5503 slots from the earliest applicable cost reporting period under the regulations at 42 CFR 413.79(n)(2).
Line 61--Did your hospital receive FTE slots under section 5503 of the ACA? Enter “Y” for yes or “N” for no in column 1. If “Y”, enter the number of IME section 5503 slots awarded in column 4 and direct GME section 5503 slots awarded in column 5. The number of IME and/or direct GME slots entered here should be the amounts on the award letter from CMS. Complete the subscripts of line 61. If “N” for no, do not complete columns 4 or 5 and subscripts of line 61.
NOTE: Effective for portions of cost reporting periods occurring on or after July 1, 2011, do not complete line 61, columns 2 and 3. This information is now reported on line 61.01, columns 2 and 3.
Line 61.01--Effective for portions of cost reporting periods occurring on or after July 1, 2011, enter the average unweighted number of primary care FTE residents from the hospital’s three most recent cost reports ending and submitted to the contractor before March 23, 2010. See 42 CFR 413.75(b) for the definition of “primary care resident”. Enter the 3-year primary care average for IME in column 2. The source of the primary care IME FTE residents is the rotation schedules submitted by the provider to support its cost reports for the three most recent cost reports ending and submitted to the contractors prior to March 23, 2010. Any audit adjustments to these IME primary care FTE residents must be taken into account in computing the 3-year average. Exclude OB/GYN and general surgery FTE residents. This primary care average is based on the hospital’s total primary care FTE count that would otherwise be allowable if not for the FTE resident cap for each year in the 3-year period. If any of the three cost reports is not a 12-month cost report, enter the 12-month equivalent FTE count.
Enter the average unweighted number of primary care FTE residents for direct GME in column 3. This primary care average is based on the hospital’s total unweighted primary care FTE count that would otherwise be allowable if not for the FTE resident cap for each year in the 3-year period. If the hospital did not train any OB/GYN residents in its three most recent cost
40-33.1 Rev.
DRAFT FORM CMS-2552-10 4004.1 (Cont.)
reports ending and submitted prior to March 23, 2010, convert the weighted primary care FTE counts from line 3.19 of Worksheet E-3, Part IV, of Form CMS-2552-96, to unweighted FTE counts, compute a 3-year average, and report the average in column 3. If the hospital did train OB/GYN FTE residents in its three most recent cost reports ending and submitted prior to March 23, 2010, subtract the OB/GYN FTE counts from line 3.19 of Worksheet E-3, Part IV, of Form CMS-2552-96, convert the remaining primary care FTE counts to unweighted FTE counts, compute a 3-year average, and report the average in column 3. Exclude general surgery FTE residents. If any of the three cost reports is not a 12-month cost report, enter the 12-month equivalent FTE count.
Line 61.02--Enter the current cost reporting period total unweighted primary care FTE count (excluding obstetrics and gynecology and general surgery), which is used to determine compliance with the 3-year primary care average requirement. In accordance with section 5503 of the ACA, which states that the 3-year primary care average requirement must be met by “excluding any additional positions” added as a result of the section 5503 FTE cap increase, also exclude from this unweighted primary care FTE count any primary care FTEs added in the current cost reporting period specific to new or expanded programs under section 5503 (see 75 FR 72198-72199 dated November 24, 2010). Enter the unweighted IME FTE count in column 2 and the direct GME FTE count in column 3. If the current cost report is not a 12‑month cost report, enter the 12-month equivalent FTE count. These current cost reporting period unweighted primary care FTE counts are compared to the 3-year primary care average amounts in line 61.01.
Line 61.03--Enter the baseline FTE count for primary care and/or general surgery residents, that is used for determining compliance with the 75 percent requirement. These primary care and/or general surgery FTEs would be a part of the unweighted allopathic and osteopathic FTE count from the hospital’s 12-month (or prorated equivalent) cost report that immediately precedes the cost report that includes July 1, 2011. Report the IME primary care and/or general surgery baseline FTE count in column 2 and the direct GME baseline primary care and/or general surgery FTE count in column 3. (For example, the baseline cost report for June 30 providers would be July 1, 2010 through June 30, 2011; for December 31 providers, this would be January 1, 2010 through December 31, 2010; for September 30 providers, this would be October 1, 2009 through September 30, 2010). (On the Form CMS-2552-96, the baseline FTE primary care and/or general surgery count is included and commingled in the allopathic and osteopathic FTEs reported on line 3.08 of Worksheet E, Part A, and on line 3.05 of Worksheet E‑3, Part IV. On the Form CMS-2552-10, the baseline primary care and/or general surgery FTE count is included and commingled in the allopathic and osteopathic FTEs reported on line 10 of Worksheet E, Part A, and on line 6 of Worksheet E‑4). Use the rotation schedules from the hospital’s 12-month (or prorated equivalent) cost report that immediately precedes the cost report that includes July 1, 2011, as the source for the primary care and/or general surgery FTEs.
Line 61.04--Enter the total number of unweighted primary care and/or general surgery allopathic and/or osteopathic FTEs in the current cost reporting period. If the cost report is not a 12-month cost report, enter the 12-month equivalent FTE count. Exclude OB/GYN FTEs. (These FTEs are part of the current year FTE count, and are included on Form CMS-2552-10, line 10 of Worksheet E, Part A, and line 6 of Worksheet E-4). Report the unweighted IME FTE count in column 2 and the direct GME FTE count in column 3.
Line 61.05--Determination of Compliance with 75 Percent Requirement--Enter the difference between the baseline primary care and/or general surgery FTE counts and the current year primary care and/or general surgery FTE counts (line 61.04 minus line 61.03). Report the IME FTE count difference in column 2 and the direct GME FTE count difference in column 3. (If the difference is less than or equal to zero, enter a zero).
The section 5503 FTE cap slots reported on Worksheet E, Part A, line 8.01 (for IME), and Worksheet E-4, line 4.01 (direct GME), are dependent upon this difference on line 61.05, because of the requirement that 75 percent of the section 5503 FTE cap award be used for primary care and/or general surgery FTEs in new or expanded programs. If the difference on line 61.05 is greater than zero, then it must be at least 75 percent of the section 5503 FTE cap
Rev. 40-33.2
4004.1 (Cont.) FORM CMS-2552-10 DRAFT
award to be reported on Worksheet E, Part A, line 8.01 (for IME) and Worksheet E-4, line 4.01 (for direct GME). For example, if a hospital was awarded a total of 10 slots, but the difference reported on line 61.05 is 5, then the section 5503 FTE slots reported on Worksheet E, Part A, line 8.01 (for IME), and Worksheet E-4, line 4.01 (for direct GME), cannot be more than 6.67 (that is, 5 divided by 75 percent). Therefore, determine that the difference on line 61.05 is at least 75 percent of the section 5503 award amount that is reported on Worksheet E, Part A, line 8.01 (for IME), and Worksheet E-4, line 4.01 (for direct GME).
Line 61.06--Enter the amount of the ACA section 5503 award FTEs that are being used for cap relief, if any, and/or that are nonprimary care or non-general surgery FTEs. Report the IME amount in column 2 and the direct GME amount in column 3. The amount reported on this line can be no more than 25 percent of the section 5503 FTE cap slots reported on Worksheet E, Part A, line 8.01 (for IME), and Worksheet E-4, line 4.01 (for direct GME). If the amount on line 61.05, columns 2 or 3, is greater than or equal to the section 5503 cap award reported on line 61, columns 4 or 5, respectively, report zero on this line.
If the amount on line 61.05 is less than the section 5503 cap award, and the hospital either is training FTE residents over its existing FTE cap or has added nonprimary care and non-general surgery FTEs in the current cost reporting period, report on this line the difference of the section 5503 cap slots on Worksheet E, Part A, line 8.01 (for IME), and Worksheet E-4, line 4.01 (for direct GME), and the amount reported on line 61.05. For example, if a hospital was awarded a total of 10 slots, and 5 is reported on line 61.05, and the section 5503 FTE slots reported on Worksheet E, Part A, line 8.01 (for IME), and Worksheet E-4, line 4.01 (for direct GME) is 6.67 FTEs, then the amount reported on line 61.06 cannot exceed 1.67 FTEs which is the difference between the amount on line 61.05, and the amount reported on Worksheet E, Part A, line 8.01 (for IME), and Worksheet E-4, line 4.01 (for direct GME). If 10 is reported on line 61.05, then report 0 (zero) on line 61.06. If 8 is reported on line 61.05 and the hospital added 2 or more nonprimary care FTEs in the current cost reporting period, then report 2 on this line.
Lines 61.07 - 61.09--Reserved for future use.
Line 61.10--Of the FTEs in line 61.05, specify each new primary care or general surgery program specialty, if any, and the number of FTE residents for each new program. Use subscripted lines 61.11 through 61.19 for each additional new program. Enter in column 1 the program name, enter in column 2 the program code, enter in column 3 the IME FTE unweighted count and enter in column 4 the direct GME FTE unweighted count.
Line 61.20--Of the additional FTEs in line 61.05, specify each expanded primary care or general surgery program specialty, if any, and the number of FTE residents for each program expansion. Use subscripted lines 61.21 through 61.29 for each additional program expansion. Enter in column 1 the program name, enter in column 2 the program code, enter in column 3 the IME FTE unweighted count and enter in column 4 the direct GME FTE unweighted count.
Lines 62 - 62.01--ACA Provisions Affecting the Health Resources and Services Administration (HRSA)--These provisions are effective for a five year period for the Health Resources and Services Administration (HRSA) Primary Care Residency Expansion (PCRE) program and the Teaching Health Center (THC) program.
Line 62--Effective for services rendered during September 30, 2010 through September 29, 2015, enter the number of FTE residents that your hospital trained in this cost reporting period for which your hospital received HRSA PCRE funding. (Sections 4002 and 5301 of the ACA.)
Line 62.01--Effective for services rendered during October 1, 2010, through September 30, 2015, enter the number of FTE residents that rotated from a THC into your hospital during this cost reporting period under the HRSA THC program. (Section 5508 of the ACA.)
40-33.3 Rev.
DRAFT FORM CMS-2552-10 4004.1 (Cont.)
Line 63--Has your facility trained residents in a non-provider setting during this cost reporting period? Enter “Y” for yes or “N” for no in column 1. (See 75 FR 72139-72140 (November 24, 2010)). If column 1 is “Y” for yes, complete lines 64 through 67 and applicable subscripts. If “N” for no, but your facility trained residents in a non-provider setting during the base year period (cost reporting period that begins on or after July 1, 2009 and before June 30, 2010), complete lines 64 and 65 and applicable subscripts effective for cost reporting periods beginning on or after July 1, 2010.
Lines 64 and 65--Section 5504 of the ACA Base Year FTE Residents in Nonprovider Settings--The base year is your cost reporting period that begins on or after July 1, 2009 and before June 30, 2010.
Line 64--If line 63 is yes or your facility trained residents in the base year period, enter in column 1, for cost reporting periods that begins on or after July 1, 2009, and before June 30, 2010, the number of unweighted nonprimary care FTE residents attributable to rotations that occurred in all nonprovider settings. Enter in column 2, the number of unweighted nonprimary care FTE residents that trained in your hospital. Include unweighted OB/GYN, dental and podiatry FTEs on this line. Enter in column 3, the ratio of column 1 divided by the sum of columns 1 and 2.
Line 65--If line 63 is yes or your facility trained residents in the base year period, enter from your cost reporting period that begins on or after July 1, 2009, and before June 30, 2010, the number of unweighted primary care FTE residents for each primary care specialty program in which you train residents. (See 42 CFR 413.75(b) for the definition of “primary care resident.”) Use subscripted lines 65.01 through 65.50 for each additional primary care program. Enter in column 1, the program name. Enter in column 2, the program code. Enter in column 3, the number of unweighted primary care FTE residents attributable to rotations that occurred in nonprovider settings for each applicable program. Enter in column 4, the number of unweighted primary care FTE residents in your hospital for each applicable program. Enter in column 5, the ratio of column 3 divided by the sum of columns 3 and 4. If you operated a primary care program that did not have FTE residents in a nonprovider setting, enter zero in column 3 and complete all other columns for each applicable program.
NOTE: The sum of the FTE counts on line 64, columns 1 and 2, and line 65, columns 3 and 4, should approximate the sum of the FTE counts on Form CMS-2552-96, Worksheet E-3, Part IV, lines 3.05 and 3.11, for your cost reporting period that begins on or after July 1, 2009 and before June 30, 2010.
Lines 66 and 67--Section 5504 of the ACA Current Year FTE Residents in Nonprovider Settings--Effective for cost reporting periods beginning on or after July 1, 2010.
Line 66--If line 63 is yes, enter in column 1, the unweighted number of nonprimary care FTE residents attributable to rotations occurring in all non-provider settings. Enter in column 2, the number of unweighted nonprimary care FTE residents in your hospital. Include unweighted OB/GYN, dental and podiatry FTEs on this line. Enter in column 3, the ratio of column 1 divided by the sum of columns 1 and 2.
Line 67--If line 63 is yes, then, for each primary care residency program in which you are training residents, enter in column 1, the program name. Enter in column 2, the program code. Enter in column 3, the number of unweighted primary care FTE residents attributable to rotations that occurred in nonprovider settings for each applicable program. Enter in column 4, the number of unweighted primary care FTE residents in your hospital for each applicable program. Enter in column 5, the ratio of column 3 divided by the sum of columns 3 and 4. Use subscripted lines 67.01 through 67.50 for each additional primary care program.
Rev. 40-33.4
4004.1 (Cont.) FORM CMS-2552-10 DRAFT
If you operated a primary care program that did not have FTE residents in a nonprovider setting, enter zero in column 3 and complete all other columns for each applicable program.
NOTE: The sum of the FTE counts on line 66, columns 1 and 2, and line 67, columns 3 and 4, should approximate the sum of the FTE counts on Worksheet E-4, lines 6 and 10 for this current cost reporting period.
Lines 68 through 69--Reserved for future use.
Line 70--Are you an IPF or do you contain an IPF subprovider? Enter in column 1 “Y” for yes or “N” for no.
Line 71--If this facility is an IPF or contains an IPF subprovider (response to line 70, column 1 is “Y” for yes), were residents training in this facility in the most recent cost report filed on or before November 15, 2004? Enter in column 1 “Y” for yes or “N” for no. Is the facility training residents in new teaching programs in accordance with 42 CFR 412.424(d)(1)(iii)(D)? Enter in column 2 “Y” for yes or “N” for no. (Note: questions 1 and 2 must have opposite answers, i.e., if column 1 is “Y”, then column 2 must be “N” and vice versa; columns 1 and 2 cannot be “Y” simultaneously, columns 1 and 2 can be “N” simultaneously.) If yes, enter a “1”, “2”, or “3”, respectively, in column 3 to correspond to the I&R academic year in the first 3 program years of the first new program’s existence that begins during the current cost reporting period. If the current cost reporting period covers the beginning of the fourth academic year of the first new teaching program’s existence, enter the number “4” in column 3. If the current cost reporting period covers the beginning of the fifth or subsequent academic years of the first new teaching program’s existence, enter the number “5” in column 3.
Lines 72 through 74--Reserved for future use.
Line 75--Are you an IRF or do you contain an IRF subprovider? Enter in column 1 “Y” for yes and “N” for no.
Line 76--If this facility is an IRF or contains an IRF subprovider (response to line 75, column 1 is “Y” for yes), did the facility train residents in teaching programs in the most recent cost reporting period ending on or before November 15, 2004? Enter in column 1 “Y” for yes or “N” for no. Is the facility training residents in new teaching programs in accordance with 70 FR 47929 (August 15, 2005)? Enter in column 2 “Y” for yes or “N” for no. (Note: Questions 1 and 2 must have opposite answers, i.e., if column 1 is “Y”, then column 2 must be “N”, and vice versa. Columns 1 and 2 cannot be “Y” simultaneously but columns 1 and 2 can be “N” simultaneously.) If yes, enter a “1”, “2”, or “3”, respectively, in column 3 to correspond to the I&R academic year in the first 3 program years of the first new program’s existence that begins during the current cost reporting period. If the current cost reporting period covers the beginning of the fourth academic year of the first new teaching program’s existence, enter the number “4” in column 3. If the current cost reporting period covers the beginning of the fifth or subsequent academic years of the first new teaching program’s existence, enter the number “5” in column 3.
Lines 77 through 79--Reserved for future use.
Line 80--Are you a freestanding long term care hospital (LTCH)? Enter in column 1 “Y” for yes and “N” for no. LTCHs can only exist as independent/freestanding facilities. To be considered as independent or a freestanding facility, a LTCH located within another hospital must meet the separateness (from the host/co-located provider) requirements identified in 42 CFR 412.22(e.)
Lines 81 through 84--Reserved for future use.
Line 85--Is this a new hospital under 42 CFR 413.40(f)(1)(i) (TEFRA)? Enter “Y” for yes or “N” for no in column 1.
40-34 Rev.
DRAFT FORM CMS-2552-10 4004.1 (Cont.)
Line 86--Have you established a new “Other” subprovider (excluded unit) under 42 CFR 413.40(f)(1)(ii)? Enter “Y” for yes or “N” for no in column 1. If there is more than one subprovider, subscript this line. Do not complete this line.
Lines 87 through 89--Reserved for future use.
Lines 90--Do you provide title V and/or XIX inpatient hospital services? Enter "Y" for yes or "N" for no in the applicable column.
Line 91--Is this hospital reimbursed for title V and/or XIX through the cost report in full or in part? Enter “Y” for yes or “N’ for no in the applicable column.
Line 92--If all of the nursing facility beds are certified for title XIX, and there are also title XVIII certified beds (dual certified), are any of the title XVIII beds occupied by title XIX patients? Enter “Y” for yes or “N” for no in the applicable column. You must complete a separate Worksheet D-1 for title XIX for each level of care.
Line 93--Do you operate an ICF/IID facility for purposes of title XIX? Enter “Y” for yes or “N” for no.
Line 94--Does title V and/or XIX reduce capital costs? Enter “Y” for yes or “N” for no in the applicable column.
Line 95--For each column, if line 94 is “Y” for yes, enter the percentage by which capital costs are reduced.
Line 96--Does title V and/or XIX reduce operating costs? Enter “Y” for yes or “N” for no in the applicable column.
Line 97--For each column, if line 96 is “Y” for yes, enter the percentage by which operating costs are reduced.
Lines 98 through 104--Reserved for future use.
Line 105--If this hospital qualifies as a CAH, enter “Y” for yes in column 1. Otherwise, enter “N” for no, and skip to line 108. (See 42 CFR 485.606ff.)
Line 106--If line 105 is yes, has this CAH elected the all-inclusive method of payment for outpatient services? Enter “Y” for yes or “N” for no. If yes, an adjustment for the professional component is still required on Worksheet A-8-2.
NOTE: If the facility elected the all-inclusive method for outpatient services, professional component amounts should be excluded from deductible and coinsurance amounts and should not be included on E-1.
Line 107--If line 105 is yes, is this CAH eligible for 101 percent reasonable cost reimbursement for I&R in approved training programs? Enter a “Y” for yes or an “N” for no in column 1. If yes, the GME elimination is not made on Worksheet B, Part I, column 25 and the program is cost reimbursed. If yes, complete Worksheet D-2, Part II.
Rev. 40-35
4004.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 108--Is this a rural hospital qualifying for an exception to the certified registered nurse anesthetist (CRNA) fee schedule? (See 42 CFR 412.113(c).) Enter “Y” for yes or “N” for no, in column 1.
Line 109--If this hospital qualifies as a critical access hospital (CAH) (response to line 105 is yes) or is a cost reimbursed provider, are therapy services provided by outside suppliers? Enter “Y” for yes or “N” for no under the corresponding physical, occupational, speech and/or respiratory therapy services as applicable.
Lines 110 through 114--Reserved for future use.
Line 115--Is this an all-inclusive rate provider (see instructions in CMS Pub. 15-1, chapter 22, §2208). Enter “Y” for yes or “N” for no in column 1. If yes, enter the applicable method (A, B, or E only) in column 2. If column 2 is “E”, enter the inpatient Medicare calculation percentage in column 3. Enter “93” for short-term hospitals where over 50 percent of all patients admitted stay less than 30 days or “98” for long-term hospitals where over 50 percent of all patients stay 30 days or more. (See CMS Pub. 15-1, chapter 22, §2208.1.E.)
Line 116--Are you classified as a referral center? Enter “Y” for yes or “N” for no. See 42 CFR 12.96.
Line 117--Are you legally required to carry malpractice insurance? Enter “Y” for yes or “N” for no. Malpractice insurance, sometimes referred to as professional liability insurance, is insurance purchased by physicians and hospitals to cover the cost of being sued for malpractice.
Line 118--Is the malpractice insurance a claims-made or occurrence policy? A claims-made insurance policy covers claims first made (reported or filed) during the year the policy is in force for any incidents that occur that year or during any previous period during which the insured was covered under a "claims-made" contract. The occurrence policy covers an incident occurring while the policy is in force regardless of when the claim arising out of that incident is filed. If the policy is claims-made, enter 1. If the policy is occurrence, enter 2.
Line 118.01--Enter the total amount of malpractice premiums paid in column 1, enter the total amount of paid losses in column 2, and enter the total amount of self-insurance paid in column 3.
Line 118.02--Indicate if malpractice premiums and paid losses are reported in a cost center other than the Administrative and General (A&G) cost center. If yes, provide a supporting schedule and list the amounts applicable to each cost center.
Malpractice insurance premiums are money paid by the provider to a commercial insurer to protect the provider against potential negligence claims made by their patients/clients. Malpractice paid losses is money paid by the healthcare provider to compensate a patient/client for professional negligence. Malpractice self-insurance is money paid by the provider where the healthcare provider acts as its own insurance company (either as a sole or part-owner) to financially protect itself against professional negligence. Often providers will manage their own funds or purchase a policy referred to as captive insurance, which protects providers for excess protection that may be unavailable or cost-prohibitive at the primary level.
Line 119--This question is eliminated and this line must not be used.
Line 120--If this is an SCH (or EACH), that qualifies for the outpatient hold harmless provision in accordance with ACA section 3121, enter “Y” for yes or “N” for no in column 1. If this is a rural hospital with 100 or fewer beds, that qualifies for the outpatient hold harmless provision in accordance with ACA section 3121, enter “Y” for yes or “N” for no in column 2. ACA section
40-36 Rev.
DRAFT FORM CMS-2552-10 4004.1 (Cont.)
3121, was amended by the Medicare and Medicaid Extenders Act (MMEA) of 2010, section 108; the Temporary Payroll Tax Cut Continuation Act of 2011, section 308; and the Middle Class Tax Relief and Job Creation Act of 2012, section 3002. Note that for SCHs and EACHs, the outpatient hold harmless provision is effective for services rendered from January 1, 2010 through February 29, 2012, regardless of bed size, and from March 1, 2012 through December 31, 2012, for SCHs and EACHs with 100 or fewer beds. Rural hospitals with 100 or fewer beds are also extended through December 31, 2012. These responses impact the TOPs calculation on Worksheet E, Part B, line 8.
Line 121--Did this facility incur and report costs (direct or indirect) in the “Implantable Devices Charged to Patients” (line 72) cost center as indicated in the 73 FR 48462 (August 19, 2008) bearing the revenue codes established by the National Uniform Billing Committee (NUBC) for high cost implantable devices. Enter “Y” for yes or “N” for no.
Lines 122 through 124--Reserved for future use.
Line 125--Does your facility operate a transplant center(s)? Enter “Y” for yes or “N” for no in column 1. If yes, enter the certification dates and termination dates, if applicable, on lines 126 through 133.
Line 126--If this is a Medicare certified kidney transplant center, enter the certification date in column 1 and termination date in column 2. Also complete Worksheet D-4.
Line 127--If this is a Medicare certified heart transplant center, enter the certification date in column 1 and termination date in column 2. Also complete Worksheet D-4.
Line 128--If this is a Medicare certified liver transplant center, enter the certification date in column 1 and termination date in column 2. Also complete Worksheet D-4.
Line 129--If this is a Medicare certified lung transplant center, enter the certification date in column 1 and termination date in column 2. Also, complete Worksheet D-4.
Line 130--If Medicare pancreas transplants are performed, enter the more recent date of July 1, 1999 (coverage of pancreas transplants) or the certification date for kidney transplants in column 1 and termination date in column 2. Also, complete Worksheet D-4.
Line 131--If this is a Medicare certified intestinal transplant center enter the certification date in column 1 and termination date in column 2. Also, complete Worksheet D-4.
Line 132--If this is a Medicare certified islet transplant center enter the certification date in column 1 and termination date in column 2. Also, complete Worksheet D-4.
Line 133--Use this line if your facility contains a Medicare certified transplant center not specifically identified on lines 126 through 132. Enter the certification date in column 1 and termination date in column 2, if applicable. Subscript this line as applicable; however, do not complete a separate Worksheet D-4 for each Medicare certified transplant center type. For organs identified on this line, enter the corresponding cost on Worksheet A, line 112, and subscripts as applicable.
Line 134--If this is an organ procurement organization (OPO), enter the OPO CCN number in column 1 and termination date, if applicable, in column 2.
Lines 135 through 139--Reserved for future use.
Line 140--Are there any related organization or home office costs claimed as defined in CMS Pub. 15-1, chapter 10? Enter “Y” for yes or “N” for no in column 1. If yes, complete Worksheet A-8-1. If this facility is part of a chain and you are claiming home office costs, enter
Rev 40-37
4004.1 (Cont.) FORM CMS-2552-10 DRAFT
in column 2 the home office chain number and complete lines 141 through 143. See CMS Pub. 15-1, chapter 21, §2150, for a definition of a chain organization.
Line 141--Enter the name of the chain home office in column 1, the home office contractor name in column 2, and the home office contractor number in column 3.
Line 142--Enter the street address and P. O. Box (if applicable) of the home office.
Line 143--Enter the city, State and ZIP code of the home office.
Line 144--Are provider based physicians' costs included in Worksheet A? Enter “Y” for yes or “N” for no. If yes, complete Worksheet A-8-2.
Line 145--If you are claiming costs for renal services on Worksheet A, line 74, are they inpatient services only? Enter “Y” for yes or “N” for no. If yes, do not complete Worksheet S-5 and the Worksheet I series.
Line 146--Have you changed your cost allocation methodology from the previously filed cost report? Enter “Y” for yes or “N” for no. If yes, enter the approval date in column 2.
Line 147--Was there a change in the statistical basis? Enter “Y” for yes or “N” for no.
Line 148--Was there a change in the order of allocation? Enter “Y” for yes or “N” for no.
Line 149--Was there a change to the simplified cost finding method? Enter “Y” for yes or “N” for no.
Lines 150 through 154--Reserved for future use.
Lines 155 through 161--If you are a hospital (public or non-public) that qualifies for an exemption from the application of the lower of cost or charges principle as provided in 42 CFR 413.13, indicate the component and/or services for titles V, XVIII and XIX that qualify for the exemption by entering in the corresponding box a “Y” for yes, if you qualify for the exemption, or an “N” for no, if you do not qualify for the exemption. Subscript as needed for additional components. For title XVIII providers, a response of “Y” does not subject the provider to the LCC principle.
Lines 162 through 164--Reserved for future use.
Line 165--Is the hospital part of a multi-campus hospital that has one or more campuses in different CBSAs? Enter “Y” for yes or “N” for no. (For purposes of this question, only answer yes if the main campus and the off-site campus(es) are classified as section 1886(d) hospitals, or they are located in Puerto Rico).
Line 166--If you responded “Y” for yes to question 165, enter information for each campus (including the main campus) as follows: name in column 0, county in column 1, State in column 2, ZIP code in column 3, geographic CBSA in column 4, and the FTE count for this campus in column 5. If additional campuses exist, subscript this line as necessary. Enter the information in columns 0 through 5 for the main campus first, and then enter the information in each column for the subordinate campuses, in any order. For example, for the main campus, enter on line 166 the name, county, state, ZIP code, geographic CBSA, and FTEs per campus. For the first subordinate campus, enter on line 166.01 the name, county, state, ZIP code, geographic CBSA, and FTEs per campus.
Line 167--Is this hospital/campus a meaningful user of electronic health record (EHR) technology in accordance §1886(n) of the Social Security Act as amended by the section 4102 of the American Recovery and Reinvestment Act (ARRA) of 2009? Enter “Y” for yes or “N” for no.
40-38 Rev.
DRAFT FORM CMS-2552-10 4004.1 (Cont.)
Line 168--If this provider is a CAH (line 105 is “Y” for yes) and is also a meaningful EHR technology user (line 167 is “Y” for yes) enter, if applicable, the reasonable acquisition cost incurred for EHR assets either purchased or initially rented under a virtual purchase lease (see CMS Pub. 15-1, chapter 1, §110.B.1.b) in the current cost reporting period. If applicable, also enter the un-depreciated cost (i.e., net book value), as of the beginning of the current cost reporting period, for assets purchased or initially rented under a virtual purchase lease in prior cost reporting period(s) which were used for EHR purposes in the current cost reporting period. Do not enter on this line any cost for EHR assets which was already claimed for the same assets in previous cost reporting period(s). The reasonable acquisition cost incurred is for depreciable assets such as computers and associated hardware and software necessary to administer certified EHR technology. (See 75 FR 44461 (July 28, 2010) and 42 CFR 495.106(a) and (c)(2).)
Additionally, if the amount on this line is greater than zero, submit a listing of the EHR assets showing the following information for each asset: (1) nature of each asset and acquisition cost; (2) an annotation whether the asset was purchased or leased under a virtual purchase lease (42 CFR 413.130(b)(8)); (3) date of purchase or date the virtual purchase lease was initiated; (4) name(s) of original purchaser (e.g., CAH, CAH’s home office, group of unrelated providers); (5) information regarding the asset’s use (i.e., indication whether the asset (hardware of software) will be shared with CAH’s non-EHR systems); and (6) tag number and location (department unit).
Line 169--If this is a §1886(d) provider that responded “N” for no to question 105 and “Y” for yes to question 167, enter the transition factor to be used in the calculation of your HIT incentive payment.
See 75 FR 44458-44460 (July 28, 2010). The transition factor equals:
If a hospital first becomes a meaningful EHR user in fiscal year 2011, 2012 or 2013
The first year transition factor is 1.00
The second year transition factor is 0.75
The third year transition factor is 0.50
The fourth year transition factor is 0.25
Any succeeding transition year is 0
If a hospital first becomes a meaningful EHR user in fiscal year 2014
The first year transition factor is 0.75
The second year transition factor is 0.50
The third year transition factor is 0.25
Any succeeding transition year is 0
If a hospital first becomes a meaningful EHR user in fiscal year 2015
The first year transition factor is 0.50
The second year transition factor is 0.25
Any succeeding transition year is 0
Line 170--If line 167 is “Y”, enter the EHR reporting period. Enter in column 1 the reporting period beginning date and in column 2 the ending date in accordance with 42 CFR 495.4. The EHR reporting period may be a full federal fiscal year or if this is the first payment year, any continuous 90-day period within a federal fiscal year. If the EHR reporting period ending date is on or after April 1, 2013, the EHR incentive payment will be subject to the 2 percent sequestration adjustment. The response to this question impacts the sequestration calculation on Worksheet E-1, Part II, line 9.
Rev. 40-38.1
4004.1 (Cont.) FORM CMS-2552-10 DRAFT
This page is reserved for future use.
40-38.2 Rev.
DRAFT FORM CMS-2552-10 4004.2
4004.2 Part II - Hospital and Hospital Health Care Complex Reimbursement Questionnaire.-- The information required on Part II of this worksheet (formerly Form CMS-339) must be completed by all hospitals submitting cost reports to the Medicare contractor under title XVIII of the Act. Its purpose is to assist you in preparing an acceptable cost report, to minimize the need for direct contact between you and your contractor, and to expedite review and settlement of cost reports. It is designed to answer pertinent questions about key reimbursement concepts displayed in the cost reports and to gather information necessary to support certain financial and statistical entries on the cost report. The questionnaire is a tool used in arriving at a prompt and equitable settlement of your cost report.
Where the instructions for this worksheet direct you to submit documentation/information, mail or otherwise transmit to the contractor immediately after submission of the ECR. The contractor has the right under §§1815(a) and 1883(e) of the Act to request any missing documentation required to complete the desk review.
To the degree that the information in the questionnaire constitutes commercial or financial information which is confidential and/or is of a highly sensitive personal nature, the information will be protected from release under the Freedom of Information Act. If there is any question about releasing information, the contractor should consult with the CMS Regional Office.
NOTE: The responses on all lines are Yes or No unless otherwise indicated. If in accordance with the following instructions, you are requested to submit documentation, indicate the line number for each set of documents you submit.
Line Descriptions
Lines 1 through 21 are required to be completed by all hospitals.
Line 1--Indicate whether the hospital has changed ownership immediately prior to the beginning of the cost reporting period. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, enter the date the change of ownership occurred in column 2. Also, submit the name and address of the new owner and a copy of the sales agreement with the cost report.
Line 2--Indicate whether the hospital has terminated participation in the Medicare program. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, enter the date of termination in column 2, and “V” for voluntary or “I” for involuntary in column 3.
Line 3--Indicate whether the hospital is involved in business transactions, including management contracts, with individuals or entities (e.g., chain home offices, drug or medical supply companies) that are related to the provider or its officers, medical staff, management personnel, or members of the board of directors through ownership, control, or family and other similar relationships. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit a list of the individuals, the organizations involved, and a description of the transactions with the cost report.
Rev. |
40-39 |
4004.2 (Cont.) FORM CMS-2552-10 DRAFT
Note: A related party transaction occurs when services, facilities, or supplies are furnished to the provider by organizations related to the provider through common ownership or control. (See CMS Pub. 15-1, chapter 10, and 42 CFR 413.17.)
Line 4--Indicate whether the financial statements were prepared by a certified public accountant. Enter “Y” for yes or “N” for no in column 1. If you answer “Y” in column 1, enter “A” for audited, “C” for compiled, or “R” for reviewed in column 2. Submit a complete copy of the financial statements (i.e., the independent public accountant’s opinion, the statements themselves, and the footnotes) with the cost report. If the financial statements are not available for submission with the cost report enter the date they will be available in column 3.
If you answer no in column 1, submit a copy of the financial statements you prepared, and written statements of significant accounting policy and procedure changes affecting Medicare reimbursement which occurred during the cost reporting period. You may submit the changed accounting or administrative procedures manual in lieu of written statements.
Line 5--Indicate whether the total expenses and total revenues reported on the cost report differ from those on the filed financial statements. Enter “Y” for yes or “N” for no in column 1. If you answer “Y” in column 1, submit a reconciliation with the cost report.
Line 6--Indicate whether costs were claimed for Nursing School. Enter “Y” for yes or “N” for no in column 1. If you answer “Y” in column 1, enter “Y” for yes or “N” for no in column 2 to indicate whether the provider is the legal operator of the program .
Line 7--Indicate whether costs were claimed for Allied Health programs. Enter “Y” for yes or “N” for no in column 1. If you answer “Y” in column 1, submit a list of the program(s) with the cost report and annotate for each whether the provider is the legal operator of the program.
Note: For purposes of lines 6 and 7, the provider is the legal operator of a nursing school and/or allied health programs if it meets the criteria in 42 CFR 413.85(f)(1) or (f)(2).
Line 8--Indicate whether approvals and/or renewals were obtained during the cost reporting period for Nursing School and/or Allied Health programs. Enter “Y” for yes or “N” for no in column 1. If you answer “Y” in column 1, submit a list of the program(s), and copies of the approvals and/or renewals with the cost report.
Line 9--Indicate whether Intern-Resident costs were claimed on the current cost report. Enter “Y” for yes or “N” for no in column 1. If you answer “Y” in column 1, submit the current year Intern-Resident Information System (IRIS) on diskette with the cost report.
Line 10--Indicate whether Intern-Resident program(s) have been initiated or renewed during the cost reporting period. Enter “Y” for yes or “N” for no in column 1. If you answer “Y” in column 1, submit copies of the certification(s)/program approval(s) with the cost report. (See 42 CFR 413.79(l) for the definition of a new program.)
Line 11--Indicate whether Graduate Medical Education costs were directly assigned to cost centers other than the Intern-Resident Services in an Approved Teaching Program on Worksheet A. Enter “Y” for yes or “N” for no in column 1. If you answer “Y” in column 1, submit a listing of the cost centers and amounts with the cost report.
40-40 |
Rev. |
DRAFT FORM CMS-2552-10 4004.2 (Cont.)
Line 12--Indicate whether you are seeking reimbursement for bad debts resulting from Medicare deductible and coinsurance amounts which are uncollectible from Medicare beneficiaries. (See 42 CFR 413.89ff and CMS Pub. 15-1, chapter 3, §§306-324, for the criteria for an allowable bad debt.) Enter “Y” for yes or “N” for no in column 1. If you answer “Y” in column 1, submit a completed Exhibit 2 or internal schedules duplicating the documentation requested on Exhibit 2 to support the bad debts claimed. If you are claiming bad debts for inpatient and outpatient services, complete a separate Exhibit 2 or internal schedule for each category.
Exhibit 2 requires the following documentation:
Columns 1, 2, and 3 - Patient Names, Health Insurance Claim (HIC) Number, and Dates of Service (From - To)--The documentation required for these columns is derived from the beneficiary’s bill. Furnish the patient’s name, health insurance claim number and dates of service that correlate to the filed bad debt. (See CMS Pub. 15-1, chapter 3, §314, and 42 CFR 413.89.)
Column 4--Indigency/Welfare Recipient--If the patient included in column 1 has been deemed indigent, place a check in this column. If the patient in column 1 has a valid Medicaid number, also include this number in this column. See the criteria in CMS Pub. 15-1, chapter 3, §§312 and 322, and 42 CFR 413.89 for guidance on the billing requirements for indigent and welfare recipients.
Columns 5 & 6--Date First Bill Sent to Beneficiary & Date Collection Efforts Ceased--This information should be obtained from the provider’s files and should correlate with the beneficiary name, HIC number, and dates of service shown in columns 1, 2 and 3 of this exhibit. The dates in column 6 represents the date that the unpaid account is deemed worthless, whereby all collection efforts, both internal and by an outside entity, ceased and there is no likelihood of recovery of the unpaid account. (See CFR 413.89(f), and CMS Pub. 15-1, chapter 3, §§308, 310, and 314.)
Column 7--Remittance Advice Dates--Enter in this column the remittance advice dates that correlate with the beneficiary name, HIC No., and dates of service shown in columns 1, 2, and 3 of this exhibit.
Columns 8 & 9--Deductibles & Coinsurance--Record in these columns the beneficiary’s unpaid deductible and coinsurance amounts that relate to covered services.
Column 10--Total Medicare Bad Debts--Enter on each line of this column, the sum of the amounts in columns 8 and 9. Calculate the total bad debts by summing up the amounts on all lines of column 10. This “total” must agree with the bad debts claimed on the cost report. Attach additional supporting schedules, if necessary, for bad debt recoveries.
Line 13--Indicate whether your bad debt collection policy changed during the cost reporting period. Enter “Y” for yes or “N” for no in column 1. If you answer “Y” in column 1, submit a copy of the policy with the cost report.
Line 14--Indicate whether patient deductibles and/or coinsurance amounts are waived. Enter “Y” for yes or “N” for no in column 1. If you answer “Y” in column 1, ensure that they are not included on the bad debt listings (i.e., Exhibit 2 or your internal schedules) submitted with the cost report.
Rev. |
40-41 |
4004.2 (Cont.) FORM CMS-2552-10 DRAFT
Line 15--Indicate whether total available beds have changed from the prior cost reporting period. Enter “Y” for yes or “N” for no in column 1. If you answer “Y” in column 1, provide an analysis of available beds and explain any changes that occurred during the cost reporting period.
NOTE: For purposes of line 15, available beds are provider beds that are permanently maintained for lodging inpatients. They must be available for use and housed in patient rooms or wards (i.e., do not include beds in corridors or temporary beds). (See CMS Pub. 15-1, chapter 22, §2200.2.C., CMS Pub. 15-2, chapter 40, §4005.1, and CFR §412.105(b).)
Line 16--Indicate whether the cost report was prepared using the Provider Statistical & Reimbursement Report (PS&R) only. Use columns 1 and 2 for Part A and columns 3 and 4 for Part B. Enter “Y” for yes or “N” for no in columns 1 and 3. If either column 1 or 3 is “Y” enter the paid-through date of the PS&R in columns 2 and/or 4. Also, submit a crosswalk between revenue codes and charges found on the PS&R to the cost center groupings on the cost report. This crosswalk will reflect a cost center to revenue code match only.
Line 17--Indicate whether the cost report was prepared using the PS&R for totals and provider records for allocation. Use columns 1 and 2 for Part A and columns 3 and 4 for Part B. Enter “Y” for yes or “N” for no in columns 1 and 3. If either column 1 or 3 is “Y” enter the paid through date of the PS&R used to prepare this cost report in columns 2 and/or 4. Also, submit a detailed crosswalk between revenue codes, departments and charges on the PS&R to the cost center groupings on the cost report. This crosswalk must show dollars by cost center and include which revenue codes were allocated to each cost center. The total revenue on the cost report must match the total charges on the PS&R (as appropriately adjusted for unpaid claims, etcetera) to use this method. Supporting workpapers must accompany this crosswalk to provide sufficient documentation as to the accuracy of the provider records. If the contractor does not find the documentation sufficient, the PS&R will be used in its entirety.
Line 18--If you entered “Y” on either line 16 or 17, columns 1 and/or 3, indicate whether adjustments were made to the PS&R data for additional claims that have been billed but not included on the PS&R used to file this cost report. Enter “Y” for yes or “N” for no in columns 1 and 3. If either column 1 or 3 is “Y”, include a schedule which supports any claims not included on the PS&R. This schedule should include totals consistent with the breakdowns on the PS&R, and should reflect claims that are unprocessed or unpaid as of the cut-off date of the PS&R used to file the cost report.
Line 19--If you entered “Y” on either line 16 or 17, columns 1 and/or 3, indicate whether adjustments were made to the PS&R data for corrections of other PS&R information. Enter “Y” for yes or “N” for no in columns 1 and 3. If either column 1 or 3 is “Y”, submit a detailed explanation and documentation which provides an audit trail from the PS&R to the cost report.
Line 20--If you entered “Y” on either line 16 or 17, columns 1 and/or 3, indicate whether other adjustments were made to the PS&R data. Enter “Y” for yes or “N” for no in columns 1 and 3. If either column 1 or 3 is “Y”, include a description of the other adjustments and documentation which provides an audit trail from the PS&R to the cost report.
Line 21--Indicate whether the cost report was prepared using provider records only. Enter “Y” for yes or “N” for no in columns 1 and 3. If either column 1 or 3 is “Y”, submit detailed documentation of the system used to support the data reported on the cost report. If detail documentation was previously supplied, submit only necessary updated documentation with the cost report.
40-42 |
Rev. |
DRAFT FORM CMS-2552-10 4004.2 (Cont.)
The minimum requirements are:
Copies of input tables, calculations, or charts supporting data elements for PPS operating rate components, capital PPS rate components and other PRICER information covering the cost reporting period.
Internal records supporting program utilization statistics, charges, prevailing rates and payment information broken into each Medicare bill type in a manner consistent with the PS&R.
Reconciliation of remittance totals to the provider’s internal records.
Include the name of the system used and indicate how the system was maintained (vendor or provider). If the provider maintained the system, include date of last software update.
Note: Additional information may be supplied such as narrative documentation, internal flow charts, or outside vendor informational material to further describe and validate the reliability of your system.
Lines 22 through 40 are required to be completed by cost-reimbursed and TEFRA hospitals only.
Line 22--Indicate whether assets have been relifed for Medicare purposes. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit a detailed listing of these specific assets, by class, as shown in the Fixed Asset Register with the cost report.
Note: “Class” means those depreciable asset groupings you use (e.g., land improvements, moveable equipment, buildings, fixed equipment).
Line 23--Indicate whether changes occurred in the Medicare depreciation expense due to appraisals made during the cost reporting period. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit a copy of the Appraisal Report and Appraisal Summary by class of asset with the cost report.
Line 24--Indicate whether new leases and/or amendments to existing leases were entered into during the cost reporting period. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit a listing of the new leases and/or amendments to existing leases if the annual rental cost of each of these leases is $50,000 or greater with the cost report. The listing should include the following information:
Identify if the lease is new or a renewal.
Parties to the lease.
Period covered by the lease.
Description of the asset being leased.
Annual charge by the lessor.
NOTE: Providers are required to submit copies of the lease, or significant extracts, upon request from the contractor.
Rev. |
40-43 |
4004.2 (Cont.) FORM CMS-2552-10 DRAFT
Line 25--Indicate whether new capitalized leases were entered into during the cost reporting period. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit a list of the individual assets by class, the department assigned to, and respective dollar amounts if the annual rental cost of these leases is $50,000 or greater with the cost report.
Line 26--Indicate whether assets subject to §2314 of DEFRA were acquired during the cost reporting period. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit a computation of the basis with the cost report.
Line 27--Indicate whether your capitalization policy changed during the cost reporting period. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit a copy with the cost report.
Line 28--Indicate whether new loans, mortgage agreements, or letters of credit were entered into during the cost reporting period. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit copies of the debt documents and amortization schedules with the cost report. Also, state the purpose of the borrowing.
Line 29--Indicate whether you have a funded depreciation account and/or bond funds (Debt Service Reserve Fund) treated as a funded depreciation account. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit a detailed analysis of the funded depreciation account for the cost reporting period with the cost report. (See CMS Pub. 15-1, chapter 2, §226, and 42 CFR 413.153.)
Line 30--Indicate whether existing debt has been replaced prior to its scheduled maturity with new debt. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit a copy of the new debt document and a schedule calculating the allowable cost. (See CMS Pub. 15-1, chapter 2, §233.3, for description of allowable cost.)
Line 31--Indicate whether debt has been recalled before its scheduled maturity without the issuance of new debt. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit a detailed analysis supporting the debt cancellation costs and treatment of these expenses on the cost report. (See CMS Pub. 15-1, chapter 2, §215, for description and treatment of debt cancellation costs.)
Line 32--Indicate whether you have entered into new agreements or if changes occurred in patient care services furnished through contractual arrangements with suppliers of service. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit copies of the contracts in those instances where the cost of the individual’s services exceeds $25,000 per year with the cost report.
Where you do not have written agreements for purchased services, submit a description listing the following information:
Duration of the arrangement.
Description of services.
Financial arrangement.
Name(s) of parties to the agreement furnishing the services.
Line 33--If you answered “Y” on line 32, were the requirements of CMS Pub. 15-1, chapter 21, §2135.2, pertaining to competitive bidding applied? Enter “Y” for yes or “N” for no in column 1. If column 1 is “N”, submit an explanation with the cost report.
40-44 |
Rev. |
DRAFT FORM CMS-2552-10 4004.2 (Cont.)
Line 34--Indicate whether services are furnished at your facility under an arrangement with provider-based physicians. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit Exhibit 1, where applicable.
You may submit computer generated substitutes for these schedules provided they contain, at a minimum, the same information as in Exhibit 1. (This includes the signature on a substitute Exhibit 1.)
Allocation agreements (Exhibit 1) are required if physician compensation is attributable to both direct patient care and provider services. Allocation agreements are also required if all of the provider-based physician’s compensation is attributable to provider services (i.e., departmental supervision and administration, quality control activities, teaching and supervision of Interns-Residents and/or Allied Health Students, and in the case of teaching hospitals electing cost reimbursement for teaching physicians’ services, for compensation attributable to direct medical and surgical services furnished to individual patients, and the supervision of intern and residents furnishing direct medical and surgical services to individual patients. However, Exhibit 1 is not required if all of the provider-based physician’s compensation is attributable to direct medical and surgical services to individual patients.
Physicians’ compensation information is considered to be confidential, and therefore, qualifies for exemption from disclosure under the Freedom of Information Act, and specifically under 5 U.S.C. 552(b)(4). The compensation information also qualifies for exemption from disclosure under 5 U.S.C. 552(b)(6) which covers “personnel and medical files, the disclosure of which would constitute a clearly unwarranted invasion of personal privacy.” An individual’s compensation is a personal matter and its release would be an invasion of privacy. Accordingly, CMS will not release, or make available to the public, compensation information collected.
Instructions for completing Exhibit 1:
Exhibit 1, Allocation of Physician Compensation Hours:
Complete this exhibit in accordance with CMS Pub. 15-1, chapter 21, §2182.3. The data elements shown are physicians’ hours of service providing a breakdown between the professional and provider component.
Prepare a physician time allocation for each physician by department, who receives payment directly from you or a related organization for services rendered. This includes physicians paid through affiliated agreements. A weighted average for the entire department may be used where all physicians in the department are in the same specialty. Where a weighted average is submitted, individual time allocations need not be submitted. The physician or department head supplying this information must sign the schedule.
Line 35--If you answered “Y” on line 34, indicate whether new agreements or amendments to existing agreements were entered into during the cost reporting period. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit copies of the new agreements or the amendments to existing agreements with the cost report.
Rev. |
40-45 |
4004.2 (Cont.) FORM CMS-2552-10 DRAFT
Line 36--Indicate whether home office costs are claimed on the cost report. Enter “Y” for yes or “N” for no in column 1.
Line 37--If you answered “Y” on line 36, indicate whether a home office cost statement was prepared by the home office. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit a schedule displaying the entire chain’s direct, functional, and pooled costs as provided to the designated home office contractor as part of the home office cost statement.
Line 38--If you answered “Y” on line 36, indicate whether the fiscal year end of the home office is different from that of the provider. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, enter the fiscal year end of the home office in column 2.
Line 39--If you answered “Y” on line 36, indicate whether the provider renders services to other components of the chain. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit a schedule listing the names of the entities, the services provided, and cost incurred to provide these services with the cost report.
Line 40--If you answered “Y” on line 36, indicate whether the provider renders services to the home office. Enter “Y” for yes or “N” for no in column 1. If column 1 is “Y”, submit a schedule listing the services provided, and cost incurred to provide these services with the cost report.
Cost Report Preparer Contact Information:
Line 41--Enter the first name, last name and the title/position held by the cost report preparer in columns 1, 2, and 3, respectively.
Line 42--Enter the employer/company name of the cost report preparer.
Line 43--Enter the telephone number and email address of the cost report preparer.
NOTE: Exhibits 1 and 2 must be completed either manually (in hard copy) or via separate electronic/digital media as this information is not captured in the ECR file.
40-46 |
Rev. |
DRAFT FORM CMS-2552-10 4004.2 (Cont.)
EXHIBIT 1
Allocation of Physician Provider Name: ________________________________________
Compensation: Hours
CCN:____________________ Department: ___________________________
Physician Name: _______________________________________
______________________________________________________________________________________________________
Cost Reporting Year: Beginning___________________ Ending ___________________
___ ___ ___ ___
Basis of Allocation: Time Study /__/; Other /__/; Describe:______________________________
______________________________________________________________________________________________________
Services Total
Hours
______________________________________________________________________________________________________
1. Provider Services - Teaching and Supervision of I/R's and other GME Related Functions. _________
1A. Provider Services - Teaching and Supervision of Allied Health Students _________
1B. Provider Services - Non Teaching Reimbursable Activities such as Departmental Administration,
Supervision of Nursing, and Technical Staff, Utilization Review, etcetera. _________
1C. Provider Services - Emergency Room Physician Availability _________
(Do not include minimum guarantee arrangements for Emergency Room Physicians.)
1D. Sub-Total - Provider Administrative Services (Lines 1, 1A, 1B, 1C). _________
2. Physician Services: Medical and Surgical Services to Individual Patients _________
3. Non-Reimbursable Activities: Research, Teaching of I/R's in Non-Approved Programs, Teaching
and Supervision of Medical Students, Writing for Medical Journals, etcetera,. _________
4. Total Hours: (Lines 1D, 2, and 3) _________
5. Professional Component Percentage (Line 2 / Line 4) _________
6. Provider Component Percentage - (Line 1D / Line 4) _________
_________________________________________ ______________
Signature: Physician or Physician Department Head Date
Rev. |
40-47 |
4004.2 (Cont.) FORM CMS-2552-10 DRAFT
EXHIBIT 2
LISTING OF MEDICARE BAD DEBTS AND APPROPRIATE SUPPORTING DATA
PROVIDER NAME ____________________ PREPARED BY __________________________________
CCN ______________________ DATE PREPARED ________________________________
FYE _________________________ INPATIENT __________ OUTPATIENT ______________
(1) Patient Name |
(2) HIC. NO. |
(3) DATES OF SERVICE
|
(4) INDIGENCY & WEL. RECIP. (CK IF APPL) |
(5) DATE FIRST BILL SENT TO BENEFICIARY |
(6) DATE COLLECTION EFFORTS CEASED |
(7) MEDICARE REMITTANCE ADVICE DATES |
(8)* DEDUCT |
(9)* CO-INS |
(10) TOTAL |
||
FROM |
TO |
YES |
MEDICAID NUMBER |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
* THESE AMOUNTS MUST NOT BE CLAIMED UNLESS THE PROVIDER BILLS FOR THESE SERVICES WITH THE INTENTION OF PAYMENT.
SEE INSTRUCTIONS FOR COLUMN 4 - INDIGENCY/WELFARE RECIPIENT, FOR POSSIBLE EXCEPTION
40-48 Rev.
12-10 FORM CMS-2552-10 4004.2 (Cont.)
Page 49 reserved for future use.
Rev. |
40-49 |
4004.2 (Cont.) FORM CMS-2552-10 12-10
Pages 50 through 54 are reserved for future use.
40-50 |
Rev. |
DRAFT FORM CMS-2552-10 4005.1
4005. WORKSHEET S-3 - HOSPITAL AND HOSPITAL HEALTH CARE COMPLEX STATISTICAL DATA AND HOSPITAL WAGE INDEX INFORMATION
This worksheet consists of five parts:
Part I - Hospital and Hospital Health Care Complex Statistical Data
Part II - Hospital Wage Index Information
Part III - Hospital Wage Index Summary
Part IV - Hospital Wage Related Costs
Part V - Hospital Contract Labor and Benefit Costs
4005.1 Part I - Hospital and Hospital Health Care Complex Statistical Data.--This part collects statistical data regarding beds, days, FTEs, and discharges.
Column Descriptions
Column 1--Enter the Worksheet A line number that corresponds to the Worksheet S-3 component line description.
Column 2--Refer to 42 CFR 412.105(b) and 69 FR 49093-49098 (August 11, 2004) to determine the facility bed count. Indicate the number of beds available for use by patients at the end of the cost reporting period.
A bed means an adult bed, pediatric bed, portion of inpatient labor/delivery/postpartum (LDP) room (also referred to as birthing room) bed when used for services other than labor and delivery, or newborn ICU bed (excluding newborn bassinets) maintained in a patient care area for lodging patients in acute, long term, or domiciliary areas of the hospital. Beds in post‑anesthesia, post-operative recovery rooms, outpatient areas, emergency rooms, ancillary departments (however, see exception for labor and delivery department), nurses' and other staff residences, and other such areas that are regularly maintained and utilized for only a portion of the stay of patients (primarily for special procedures or not for inpatient lodging) are not termed a bed for these purposes. (See CMS Pub. 15-1, chapter 22, §2205.)
For cost reporting periods beginning prior to October 1, 2012, beds in distinct ancillary labor and delivery rooms and the proportion of LDP room (birthing room) beds used for labor and delivery services are not a bed for these purposes. (See 68 FR 45420 (August 1, 2003).)
For cost reporting periods beginning on or after October 1, 2012, in accordance with 77 FR 53411-53413 (August 31, 2012), beds in distinct labor and delivery rooms, when occupied by an inpatient receiving IPPS-level acute care hospital services or when unoccupied, are considered to be part of a hospital’s inpatient available bed count in accordance with 42 CFR 412.105(b) and are to be reported on line 32. Furthermore, the proportion of the inpatient LDP room (birthing room) beds used for ancillary labor and delivery services is considered part of the hospital’s available bed count.
Column 3--Enter the total bed days available. Bed days are computed by multiplying the number of beds available throughout the period in column 2 by the number of days in the reporting period. If there is an increase or decrease in the number of beds available during the period, multiply the number of beds available for each part of the cost reporting period by the number of days for which that number of beds was available.
Column 4--CAHs accumulate the aggregate number of hours all CAH patients spend in each category on lines 1 and 8 through 12. This data is for informational purposes only.
Columns 5 through 7--Enter the number of inpatient days or visits, where applicable, for each component by program. Do not include HMO days except where required (lines 2 through 4, columns 6 and 7; line 13, column 7), organ acquisition, or observation bed days in these
Rev. 40-55
4005.1 (Cont.) FORM CMS-2552-10 DRAFT
columns. Nursery days (all the days during which a newborn infant occupies a nursery) are reported on line 13, column 7, and include the in-state paid Medicaid days; in-state Medicaid eligible but unpaid days; out-of-state Medicaid paid days; out-of-state Medicaid eligible but unpaid days paid; and Medicaid HMO paid and eligible but unpaid days. Observation bed days are reported in columns 7 (title XIX) and 8 (total), line 28. For LTCH, enter in column 6, the applicable line, the number of covered Medicare days (from the PS&R) and enter in column 6, line 33, the number of non-covered days (from provider’s books and records) for Medicare patients.
Report the program days for PPS providers (acute care hospital, IPF, IRF, and LTCH) in the cost reporting period in which the discharge is reported. This also applies to providers under the TEFRA/PPS blend. TEFRA providers should report their program days in the reporting period in which they occur.
NOTE: Medicaid days for Medicaid recipients who are members of an HMO as well as out-of-state days, Medicaid secondary payer patient days, Medicaid eligible days for which no payment was received, and nursery days are reported on lines 2, 3, 4 or 13 in accordance with 42 CFR 412.106(b)(4)(ii). Therefore, Medicaid patient days reported on line 1, column 7 do not include days for Medicaid patients who are also members of an HMO, out of State Medicaid days, Medicaid secondary payer patient days, Medicaid eligible days for which no payment was received, and nursery days.
Column 8--Enter the number of inpatient days for all classes of patients for each component. Include organ acquisition and HMO days in this column. This amount will not equal the sum of columns 5 through 7 when the provider renders services to other than titles V, XVIII, or XIX patients.
Column 9--Enter the number of intern and resident full time equivalents (FTEs) in an approved program determined in accordance with 42 CFR 412.105(f) for the indirect medical education adjustment. The FTE residents reported by an IPF PPS facility or an IRF PPS facility (whether freestanding or a unit reported on line 16 or 17, respectively, of an IPPS hospital’s cost report) shall be determined in accordance with 42 CFR 412.424(d)(1)(iii) for IPFs and in accordance with the 70 FR 47929-79930 (August 15, 2005) for IRFs.
Columns 10 and 11--The average number of FTE employees for the period may be determined either on a quarterly or semiannual basis. When quarterly data are used, add the total number of hours worked by all employees on the first week of the first payroll period at the beginning of each quarter, and divide the sum by 160 (4 times 40). When semiannual data are used, add the total number of paid hours on the first week of the first payroll period of the first and seventh months of the period. Divide this sum by 80 (2 times 40). Enter the average number of paid employees in column 10 and the average number of nonpaid workers in column 11 for each component, as applicable.
Columns 12 through 14--Enter the number of discharges including deaths (excluding newborn and DOAs) for each component by program. A patient discharge, including death, is a formal release of a patient. (See 42 CFR 412.4.) Enter the title XVIII Medicare Advantage (MA) discharges in column 13, line 2. For cost reporting periods ending on or after June 30, 2014, enter the title XIX managed care discharges in column 14, line 2. For columns 13 and 14, line 2 is a subset of column 15, line 1.
Column 15--Enter the number of discharges including deaths (excluding newborn and DOAs) for all classes of patients for each component.
40-56 Rev.
DRAFT FORM CMS-2552-10 4005.1 (Cont.)
Line Descriptions
Line 1--For cost reporting periods beginning before October 1, 2012, exclude from column 2 the portion of LDP room (birthing room) beds used for ancillary labor and delivery services, but include on this line beds used for routine adult and pediatric services (postpartum). In accordance with the instructions in 68 FR 45420 (August 1, 2003), compute this proportion (off the cost report) by multiplying the total number of occupied and unoccupied available beds in the LDP room by the percentage of time these beds were used for ancillary labor and delivery services. An example of how to calculate the “percentage of time” would be for a hospital to determine the number of hours for the cost reporting period during which each LDP room maternity patient received labor and delivery services and divide the sum of those hours for all such patients by the sum of the total hours (for both, ancillary labor and delivery services and for routine postpartum services) that all maternity patients spent in the LDP room during that cost reporting period. Alternatively, a hospital could calculate an average percentage of time maternity patients received ancillary labor and delivery services in an LDP room during a typical month.
For cost reporting periods beginning on or after October 1, 2012, include all the available LDP room (birthing room) beds in the available bed count in column 2. (See 77 FR 53411-53413 (August 31, 2012).) The proportion of available LDP room beds related to the ancillary labor and delivery services must not be excluded from column 2 for those cost reporting periods.
In columns 5, 6, 7 and 8, enter the number of adult and pediatric hospital days excluding the SNF and NF swing bed, observation bed, and hospice days. In columns 6 and 7, also exclude HMO days. Do not include in column 6 Medicare Secondary Payer/Lesser of Reasonable Cost (MSP/LCC) days. Include these days only in column 8. However, do not include employee discount days in column 8.
Labor and delivery days (as defined in the instructions for Worksheet S-3, Part I, line 32) must not be included on this line.
Line 2--Enter in column 6, the title XVIII MA days and days for individuals enrolled in Medicare cost plans (§1876 of the Act). Enter in column 7 the title XIX Medicaid HMO days and other Medicaid eligible days not included on line 1, column 7.
Line 3--Enter in column 6, the title XVIII MA days and days for individuals enrolled in Medicare cost plans (§1876 of the Act) that pertain to IPF subprovider patients. Enter in column 7 the title XIX Medicaid HMO days and other Medicaid eligible days not included on line 16, column 7.
Line 4--Enter in column 6, the title XVIII MA days and days for individuals enrolled in Medicare cost plans (§1876 of the Act) that pertain to IRF subprovider patients. Enter in column 7 the title XIX Medicaid HMO days and other Medicaid eligible days not included on line 17, column 7.
Line 5--Enter the Medicare covered swing bed days (which are considered synonymous with SNF swing bed days) for all title XVIII programs where applicable. (See 42 CFR 413.53(a)(2).) Exclude all MA days from column 6, include the MA days in column 8.
Line 6--Enter the non-Medicare covered swing bed days (which are considered synonymous with NF swing bed days) for all programs where applicable. (See 42 CFR 413.53(a)(2).)
Line 7--Enter the sum of lines 1, 5, and 6.
Lines 8 through 13--Enter the appropriate statistic applicable to each discipline for all programs.
Line 14--Enter the sum of lines 7 through 13 for columns 2 through 8, and for columns 12 through 15, enter the amount from line 1. For columns 9 through 11, enter the total for each from your records.
Rev. 40-57
4005.1 (Cont.) FORM CMS-2552-10 DRAFT
Labor and delivery days (as defined in the instructions for Worksheet S-3, Part I, line 32) must not be included on this line.
Line 15--Enter the number of outpatient visits for CAHs by program and total. An outpatient CAH visit is defined in 42 CFR 413.70(b)(3)(iii).
Line 16--Enter the applicable data for the IPF subprovider.
Line 17--Enter the applicable data for the IRF subprovider.
Line 18--Enter the applicable data for other than IPF or IRF subproviders. If you have more than one subprovider, subscript this line.
Line 19--If your State recognizes one level of care, complete this line for titles V, XVIII, and XIX, however, do not complete line 20. If you answered yes to line 92 of Worksheet S-2, Part I, complete all columns.
Line 20--Enter nursing facility days if you have a separately certified nursing facility for title XIX or you answered yes to line 92 of Worksheet S-2, Part I. Make no entry if your State recognizes only SNF level of care. If you operate an ICF/IID, subscript this line to 20.01 and enter the ICF/IID days. Do not report any nursing facility data on line 20.01.
Line 21--Enter data for an other long term care facility.
Line 22--If you have more than one hospital-based HHA, subscript this line.
Line 23--Enter data for an ASC. If you have more than one ASC, subscript this line.
Line 24--Enter days applicable to hospice patients in a distinct part hospice.
Line 24.10--Effective for cost reporting periods beginning on or after October 1, 2011, enter in column 8, the days applicable to hospice patients currently under a valid hospice election who occupy general inpatient routine beds under a contractual arrangement between the hospital and hospice to provide general inpatient hospice and/or respite care services.
Line 25--CMHCs enter the number of partial hospitalization days as applicable. For reporting of multiple facilities follow the same format used on Worksheet S-2, Part I, line 17.
Line 26--Enter the number of outpatient visits for FQHC and RHC. If you have both or multiples of one, subscript the line. If the RHC/FQHC is approved to file a consolidated cost report all data is reported in aggregate as a single provider and must use either line 26 with no subscripting or must use a single subscript of line 26 representing the consolidated RHC/FQHC. If a consolidated RHC and FQHC cost reports exists, each consolidated cost report will use a separate line.
Line 28--Enter the total observation bed days in column 8. Divide the total number of observation bed hours by 24 and round up to the nearest whole day. These total hours should include the hours for observation of patients who are subsequently admitted as inpatients but only the hours up to the time of admission as well as the hours for observation of patients who are not subsequently admitted as inpatients but only the hours up to the time of discharge from the facility. Observation bed days only need to be computed if the observation bed patients are placed in a routine patient care area. The bed days are needed to calculate the cost of observation beds since it cannot be separately costed when the routine patient care area is used. If, however, you have a distinct observation bed area, it must be separately costed (as are all other outpatient cost centers), and this computation is not needed.
Line 29--Enter in column 6, the total number of ambulance trips, as defined by §4531(a)(1) of the BBA. Do not subscript this line.
40-58 Rev.
DRAFT FORM CMS-2552-10 4005.1 (Cont.)
Line 30--Enter in column 8, the employee discount days if applicable. These days are used on Worksheet E, Part A, line 31, in the calculation of the DSH adjustment and Worksheet E-3, Part III, line 3, in the calculation of the LIP adjustment.
Line 31--Enter in column 8, the employee discount days, if applicable, for IRF subproviders.
Line 32--Effective for cost reporting periods beginning on or after October 1, 2012, enter in column 2, the total number of available beds located in the distinct ancillary labor and delivery rooms. In accordance with 42 CFR 412.105(b) and 77 FR 53411-53413 (August 31, 2012), distinct ancillary labor and delivery room beds, when occupied by an inpatient receiving IPPS-level acute care hospital services or when unoccupied, are considered to be part of a hospital’s inpatient available bed count. These beds are not included in the inpatient routine beds reported on line 1. Note that the available bed days reported in column 3 are reduced on Worksheet E, Part A by the equivalent of outpatient labor and delivery days from line 32.01.
Effective for cost reporting periods beginning on or after October 1, 2013, enter in column 6 the number of labor/delivery inpatient days for title XVIII. (See 78 FR 50730-50733 (August 19, 2013).)
Effective for cost reporting periods beginning on or after October 1, 2009, enter in column 7 the number of labor/delivery inpatient days for title XIX and in column 8 the total number of labor/delivery inpatient days for the entire hospital. (See 74 FR 43899-43901 (August 27, 2009).)
For the purposes of reporting on this line, labor and delivery days are defined as days during which a maternity patient is in the labor/delivery room ancillary area at midnight at the time of census taking, and is not included in the census of the inpatient routine care area because the patient has not occupied an inpatient routine bed at some time before admission (see CMS Pub. 15-1, chapter 22, §2205.2). Maternity patients must be admitted to the hospital as an inpatient for their labor and delivery days to be included on line 32. These days must not be reported on Worksheet S-3, Part I, line 1 or line 14. In the case where the maternity patient is in a single multipurpose labor/delivery/postpartum (LDP) room (also referred to as a birthing room), hospitals must determine the proportion of each inpatient stay that is associated with ancillary services (labor and delivery) versus routine adult and pediatric services (postpartum) and report the days associated with the labor and delivery portion of the stay on this line. An example of this would be for a hospital to determine the percentage of each stay associated with labor/delivery services and apply that percentage to the stay to determine the number of labor and delivery days of the stay. Alternatively, a hospital could calculate an average percentage of time maternity patients receive ancillary services in an LDP room during a typical month, and apply that percentage through the rest of the year to determine the number of labor and delivery days to report on line 32.
Line 32.01--Effective for cost reporting periods beginning on or after October 1, 2012, enter in column 8 the equivalent days for the entire hospital that are attributable to outpatient services provided in the distinct ancillary labor and delivery room. Calculate the number of days by dividing the total number of hours attributable to the outpatient services by 24, and round to the nearest whole day. These total outpatient hours include the hours for outpatients occupying the distinct ancillary labor and delivery room until they are admitted as inpatients or are discharged from the hospital. For example, one patient is admitted as an inpatient after first occupying the distinct ancillary labor and delivery room bed for 8 hours. Therefore, for this patient, 8 hours would be included in the sum of the total hours used to compute equivalent days to be entered on line 32.01. Another patient is admitted to the distinct ancillary labor and delivery room for monitoring of possible labor or for a sonogram, etcetera. After spending 6 hours in this department (room), this patient is discharged from the hospital without being admitted as an inpatient. Therefore, for this patient, 6 hours would be included in the sum of the total hours used to compute the equivalent days to be entered on line 32.01. These outpatient labor and delivery days are used on Worksheet E, Part A to reduce the available bed days reported on line 32 so that only those distinct ancillary labor and delivery room beds which are occupied by inpatients or are unoccupied are ultimately counted as “beds.”
Rev. 40-58.1
4005.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 33--See instructions for columns 5 through 7 of this worksheet.
4005.2 Part II - Hospital Wage Index Information.--This worksheet provides for the collection of hospital wage data which is needed to update the hospital wage index applied to the labor-related portion of the national average standardized amounts of the prospective payment system. It is important for hospitals to ensure that the data reported on Worksheet S-3, Parts II, III and IV, are accurate. Beginning October 1, 1993, the wage index must be updated annually. (See §1886(d)(3)(E) of the Act.) Congress also indicated that any revised wage index must exclude data for wages incurred in furnishing SNF services. Complete Worksheet S-3, Parts II, III, and IV, for IPPS hospitals (see §1886(d)), any hospital with an IPPS subprovider, or any hospital that would be subject to IPPS if not granted a waiver.
NOTE: Any line reference for Worksheets A and A-6 includes all subscripts of that line.
NOTE: Lines 4 and 22 apply to physician’s Part A administrative costs.
NOTE: Capital-related salaries, hours, and wage-related costs associated with lines 1 and 2 of Worksheet A must not be included on Worksheet S-3, Parts II and III.
Column 2
General instructions for completing column 2:
For each line item (except for wage-related costs on lines 17 through 25 or as otherwise indicated), report in column 2, the direct salaries and wages, including amounts for related paid vacation, holiday, sick leave, other paid-time-off (PTO), severance pay, and bonus pay for personnel associated with the line item.
Paid vacation, holiday, sick leave, other PTO, severance pay, and bonus pay must be reported in column 2, with related direct salaries and wages to be considered an allowable cost for the wage index.
Paid vacation, holiday, sick leave, other PTO, severance pay, and bonus pay must be reported in the same cost center as the related direct salaries and wages. For example, do NOT report the direct salaries and wages of an employee in one cost center and report the employee’s paid vacation in a different cost center.
To be considered an allowable salary cost (i.e., direct salaries and wages plus paid vacation, holiday, sick leave, other PTO, and severance pay), the associated hours must also be reported in column 5. (See exceptions in column 5 instructions for bonus pay and overtime pay. Also, for wage-related costs, there are no associated hours.)
Bonus pay includes award pay and vacation, holiday, and sick pay conversion (pay in lieu of time off).
NOTE: Methodology for including vacation/holiday/sick/other PTO accruals in the wage index:
PTO salary cost--The required source for costs on Worksheet A is the general ledger (see §4013 and 42 CFR 413.24(e)). Worksheet S-3, Part II, (wage index) data are derived from Worksheet A; therefore, the proper source for costs for the wage index is also the general ledger. A hospital’s current year general ledger includes both costs that are paid during the current year and costs that are expensed in the current year but paid in the subsequent year (current year accruals). Hospitals and contractors are to include on Worksheet S-3, Part II the current year PTO cost incurred as reflected on the general ledger; that is, both the current year PTO cost paid and the current year PTO accrual. (Costs that are expensed in the prior year but paid in the current year (prior year accruals) are not included on a hospital’s current year general ledger and should not be included on the hospital's current year Worksheet S-3, Part II.)
40-58.2 Rev.
DRAFT FORM CMS-2552-10 4005.2 (Cont.)
PTO hours--The source for PTO paid hours on Worksheet S-3, Part II, is the provider’s payroll report. Hours are included on the payroll report in the period in which the associated PTO expense is paid. Hospitals and contractors are to include on Worksheet S-3, Part II, the PTO hours that are reflected on the current year payroll report, which includes hours associated with PTO cost that was expensed in the prior year but paid in the current year. The time period must cover the weeks that best matches the provider’s cost reporting period. (Hours associated with PTO cost expensed in the current year but not paid until the subsequent year (current year PTO accrual) are not included on the current year payroll report and should not be included on the hospital’s current year Worksheet S-3, Part II.)
Although this methodology does not provide a perfect match between paid PTO cost and paid PTO hours for a given year, it should approximate an actual match between cost and hours.
Line 1--Enter from Worksheet A, column 1, line 200, the direct salaries and wages, including the amounts for related paid vacation, holiday, sick leave, other PTO, severance pay, and bonus pay, paid to hospital employees. See Worksheet A instructions (§4013).
Lines 2 through 10--The amounts to be reported must be adjusted for vacation, holiday, sick, other paid time off, severance, and bonus pay if not already included. Do not include in lines 2 through 8 the salaries for employees associated with excluded areas lines 9 and 10.
Line 2--Enter the salaries for directly-employed Part A non-physician anesthetist salaries (for rural hospitals that have been granted CRNA pass through) to the extent these salaries are included in line 1. Add to this amount the costs for CRNA Part A services furnished under contract to the extent hours can be accurately determined. Report only the personnel costs associated with these contracts. DO NOT include cost for equipment, supplies, travel expenses, and other miscellaneous or overhead items. DO NOT include costs applicable to excluded areas reported on lines 9 and 10. Additionally, contract CRNA cost must be included on line 11. Report in column 5, the hours that are associated with the costs in column 4 for directly employed and contract Part A CRNAs.
Do not include physician assistants, clinical nurse specialists, nurse practitioners, and nurse midwives.
Line 3--Enter the non-physician anesthetist salaries included in line 1, subject to the fee schedule and paid under Part B by the contractor. Do not include salary costs for physician assistants, clinical nurse specialists, nurse practitioners, and nurse midwives.
Line 4--Enter the physician Part A administrative salaries, (excluding teaching physician salaries), which are included in line 1. Also do not include intern and resident (I & R) salary on this line. Report I & R salary on line 7. Subscript this line and report salaries for Part A teaching physicians on line 4.01.
Lines 5 and 6--Enter the total physician, physician assistant, nurse practitioner and clinical nurse specialist salaries billed under Part B that are included in line 1. Under Medicare, these services are related to patient care and billed separately under Part B. Also include physician salaries for patient care services reported for rural health clinics (RHC) and federally qualified health centers (FQHC) included on Worksheet A, column 1, lines 88 and/or 89 as applicable. Report on line 6, the non-physician salaries reported for hospital-based RHC and FQHC services included on Worksheet A, column 1, lines 88 and/or 89, as applicable. Do not include on these lines amounts that are included on lines 9 and 10 for the SNF or excluded area salaries.
Rev. 40-58.3
4005.2 (Cont.) FORM CMS-2552-10 DRAFT
Line 7--Enter from Worksheet A the salaries reported in column 1, line 21, for interns and residents. Subscript this line and report salaries for contracted interns and residents in an approved program on line 7.01. Report only the personnel costs associated with these contracts. DO NOT include cost for equipment, supplies, travel expenses, and other miscellaneous or overhead items. DO NOT include costs applicable to excluded areas reported on lines 9 and 10. Additionally, contract intern and resident costs must be included on line 11. DO NOT include contract intern and residents costs on line 13. Report in column 5, the hours that are associated with the costs in column 4 for directly employed and contract interns and residents.
Line 8--If you are a member of a chain or other related organization as defined in CMS Pub. 15‑1, chapter 21, §2150, enter from your records, the wages and salaries for home office related organization personnel that are included in line 1.
Lines 9 and 10--Enter on line 9, the amount reported on Worksheet A, column 1, line 44, for the SNF. On line 10, enter from Worksheet A, column 1, the sum of lines 20, 23, 40 through 42, 45, 45.01, 46, 94, 95, 98 through 101, 105 through 112, 114, 115 through 117, and 190 through 194. DO NOT include on lines 9 and 10, any salaries for general service personnel (e.g., housekeeping) which, on Worksheet A, column 1, may have been included directly in the SNF and the other cost centers detailed in the instructions for line 10.
General Instructions for Contract Labor:
In general, for contract labor, the minimum requirement for supporting documentation is the contract itself. If the wage costs, hours, and non-labor costs are not clearly specified in the contract, then other documentation is necessary, such as a representative sample of invoices which specify the wage costs, hours, and non-labor costs or a signed declaration from the vendor in conjunction with a sample of invoices. Hospitals must be able to provide such documentation when requested by the contractor. A hospital’s failure to provide adequate supporting documentation may result in the cost being disallowed for the wage index. Report only personnel costs associated with the contract. DO NOT include cost for equipment, supplies, travel expenses, and other miscellaneous or overhead items (non-labor costs).
Workers who are contracted solely for the purpose of providing services on-call can only be included on Worksheet S-3 when they actually work the on-call schedule. That is, they are actually delivering patient care at the hospital, or are at the hospital so as to be available to deliver patient care. If either of these latter two scenarios occur, then both the wages and associated hours actually worked must be included in the appropriate contract labor line on Worksheet S-3.
40-58.4 Rev.
DRAFT FORM CMS-2552-10 4005.2 (Cont.)
Line 11--Enter the amount paid for services furnished under contract, rather than by employees, for direct patient care, as defined below. Do not include costs applicable to excluded areas reported on line 9 and 10. Include costs for contract CRNA and intern and resident services (these costs are also to be reported on lines 2 and 7.01, respectively). Include on this line contract pharmacy and laboratory wage costs as defined below.
Direct patient care services include nursing, diagnostic, therapeutic, and rehabilitative services. Report only personnel costs associated with these contracts. DO NOT apply the guidelines for contracted therapy services under §1861(v)(5) of the Act and 42 CFR 413.106. Direct patient care contracted labor, for purposes of this worksheet, DOES NOT include the following: services paid under Part B: (e.g., physician clinical services, physician assistant services), management and consultant contracts, billing services, legal and accounting services, clinical psychologist and clinical social worker services, housekeeping services, security personnel, planning contracts, independent financial audits, or any other service not directly related to patient care.
Contract pharmacy services are furnished under contract, rather than by employees. DO NOT include the following services paid under Part B (e.g., physician clinical services, physician assistant services), management and consultant contracts, clerical and billing services, legal and accounting services, housekeeping services, security personnel, planning contracts, independent financial audits, or any other service not directly related to patient care. Report only personnel costs associated with the contracts.
Contract laboratory services are furnished under contract, rather than by employees. DO NOT include the following services paid under Part B (e.g., physician clinical services, physician assistant services), management and consultant contracts, clerical and billing services, legal and accounting services, housekeeping services, security personnel, planning contracts, independent financial audits, or any other service not directly related to patient care. Report only personnel costs associated with the contracts.
If you have no contracts for direct patient care as defined above, enter a zero in column 2. If you are unable to accurately determine the number of hours associated with contracted labor, enter a zero in column 2.
Line 12--Enter the amount paid for contracted top level management services, and other contract management and administrative services furnished under contract, rather than by employees. Include on this line contract management and administrative services associated with cost centers other than those listed on lines 26 through 43 (and their subscripts) of this worksheet that are included in the wage index.
Rev. 40-59
4005.2 (Cont.) FORM CMS-2552-10 DRAFT
Contracted Top Level Management: Include the amount paid for top level management services, as defined below, furnished under contract rather than by employees. Contract management is limited to the personnel costs for those individuals who are working at the hospital facility in the capacity of chief executive officer, chief operating officer, chief financial officer, or nursing administrator. The titles given to these individuals may vary from the titles indicated above. However, the individual should be performing those duties customarily given these positions.
For purposes of this worksheet, contract top level management services DO NOT include the following: physician Part A services, consultative services, clerical and billing services, legal and accounting services, unmet physician guarantees, physician services, planning contracts, independent financial audits, or any services other than the top level management contracts listed above. Per instructions on Worksheet S-2, Part II, for top level management contracts, submit to your Medicare contractor the aggregate wages and hours.
Other Contract Management and Administrative Services: Examples of other contract management and administrative services that would be reported on line 12 include department directors, administrators, managers, ward clerks, and medical secretaries. Report only those personnel costs associated with the contract. DO NOT include on line 12 any contract labor costs associated with lines 26 through 43 and subscripts for these lines.
Line 13--Enter from your records the amount paid under contract (in accordance with the general instructions above for contract labor) for Part A physician services - administrative, excluding teaching physician services. DO NOT include contract I & R services (to be included on line 7). DO NOT include the costs for Part A physician services from the home office allocation and/or from related organizations (to be reported on line 15).
Line 14--Enter the salaries and wage-related costs (as defined on lines 17 and 18) paid to personnel who are affiliated with a home office and/or related organization, who provide services to the hospital, and whose salaries are not included on Worksheet A, column 1. In addition, add the home office/related organization salaries included on line 8 and the associated wage-related costs. This figure must be based on recognized methods of allocating an individual's home office/related organization salary to the hospital. If no home office/related organization exists or if you cannot accurately determine the hours associated with the home office/related organization salaries that are allocated to the hospital, then enter a zero in column 1. All costs for any related organization must be shown as the cost to the related organization.
NOTE: Do not include any costs for Part A physician services from the home office allocation and/or related organizations. These amounts are reported on line 15.
If a wage related cost associated with the home office is not “core” (as described in the Worksheet S-3, Part IV) and is not a category included in “other” wage related costs on line 18 (see Worksheet S-3, Part IV, and line 18 instructions below), the cost cannot be included on line 14. For example, if a hospital’s employee parking cost does not meet the criteria for inclusion as a wage-related cost on line 18, any parking cost associated with home office staff cannot be included on line 14.
Line 15--Enter from your records the salaries and wage-related costs for Part A physician services - administrative, excluding teaching physician Part A services from the home office allocation and/or related organizations.
40-60 Rev.
DRAFT FORM CMS-2552-10 4005.2 (Cont.)
Line 16--Enter from your records the salaries and wage-related costs for Part A teaching physicians’ from the home office allocation and/or related organizations. Also report on this line Part A teaching physicians’ salaries under contract.
Lines 17 through 25--In general, the amount reported for wage-related costs must meet the “reasonable cost” provisions of Medicare. For pension and executive deferred compensation costs see the instructions below in Part IV.
For those wage-related costs that are not covered by Medicare reasonable cost principles, a hospital shall use generally accepted accounting principles (GAAP). For example, for purposes of the wage index, disability insurance cost should be developed using GAAP. Hospitals are required to complete Worksheet S-3, Part IV, a reconciliation worksheet to aid hospitals and contractors in implementing GAAP when developing wage-related costs. Upon request by the contractor or CMS, hospitals must provide a copy of the GAAP pronouncement, or other documentation, showing that the reporting practice is widely accepted in the hospital industry and/or related field as support for the methodology used to develop the wage-related costs. If a hospital does not complete Worksheet S-3, Part IV, or, the hospital is unable, when requested, to provide a copy of the standard used in developing the wage-related costs, the contractor may remove the cost from the hospital’s Worksheet S-3 due to insufficient documentation to substantiate the wage-related cost relevant to GAAP.
NOTE: All costs for any related organization must be shown as the cost to the related organization. (For Medicare cost reporting principles, see CMS Pub. 15-1, chapter 10, §1000. For GAAP, see FASB 57.) If a hospital’s consolidation methodology is not in accordance with GAAP or if there are any amounts in the methodology that cannot be verified by the contractor, the contractor may apply the hospital’s cost to charge ratio to reduce the related party expenses to cost.
NOTE: All wage-related costs, including FICA, workers compensation, and unemployment compensation taxes, associated with physician services are to be allocated according to the services provided; that is, those taxes and other wage-related costs attributable to Part A administrative services must be placed on line 22, to Part A teaching services must be placed on line 22.01, and to Part B (patient care services) must be placed on line 23. Line 17 must not include wage-related costs that are associated with physician services.
Line 17--Enter the core wage-related costs from Worksheet S-3, Part IV, line 24. (See note below for costs that are not to be included on line 17). Only the wage-related costs reported on Worksheet S-3, Part IV, line 24, are reported on this line. (Wage-related costs are reported in column 2, not column 1, of Worksheet A.)
NOTE: Do not include wage-related costs applicable to the excluded areas reported on lines 9 and 10. Instead, these costs are reported on line 19. Also, do not include the wage‑related costs for physicians Parts A and B, non-physician anesthetists Parts A and B, interns and residents in approved programs, and home office personnel. (See lines 14, 15, and 20 through 25.)
Health Insurance and Health-Related Wage Related Costs:
The following are the allowable health insurance and health-related costs for the wage index.
1) Purchased Health Insurance:
• Premium costs.
• Costs paid to external organizations for plan administration.
Rev. 40-61
4005.2 (Cont.) FORM CMS-2552-10 DRAFT
2) Self (or Self-Funded) Health Insurance:
• Costs paid to external organizations for plan administration.
• Without a Third-Party Administrator (TPA).
• Costs the hospital incurs in providing services under the plan to its employees. (Domestic claim charges must be reduced to cost. Costs must also exclude any copayments and deductibles paid by employees.) Employee withholdings and contributions are employee costs, not hospital costs. Hospitals are not permitted to treat as hospital wage-related costs the amounts that their employees incur for their health insurance benefits.
• Hospital’s payment to unrelated health care providers for services rendered, under the plan, to hospital’s employees.
• With a TPA.
• Amount the TPA pays to the hospital or other health care providers for services rendered under the plan. (For domestic claims, the hospital must provide documentation from its TPA to demonstrate that payments for services rendered to employees are based on a discount from full charges. Also, the payments must be reasonable; that is, the costs included for domestic claims must not exceed the amount that commercial insurers pay the hospital for the same services rendered to nonemployees.) Employee withholdings and contributions are employee costs, not hospital costs. Hospitals are not permitted to treat as hospital wage-related costs the amounts that their employees incur for their health insurance benefits.
NOTE: Hospitals and contractors are not required to remove from domestic claims costs, the personnel costs that are associated with hospital staff who deliver the services to employees.
3) Health-Related Services: Inpatient and outpatient health services that are not covered under the hospital’s health insurance plan, but are provided to employees at no cost or at a discount, for example, employee physicals, flu shots, smoking cessation, and weight control programs, are to be included as a core wage-related cost. (Domestic claim charges must be reduced to cost. Costs must also exclude any copayments and deductibles paid by employees.)
NOTE: Hospitals and contractors are not required to remove from domestic claims costs, the personnel costs that are associated with hospital staff who deliver the services to employees.
Line 18--Enter the wage-related costs that are considered an exception to the core list. (See note below for costs that are not to be included on line 18.) In order for a wage-related cost to be considered an exception, it must meet all of the following tests:
a. The cost is not listed on Worksheet S-3, Part IV,
b. The wage-related cost has not been furnished for the convenience of the provider,
c. The wage-related cost is a fringe benefit as defined by the Internal Revenue Service and, where required, has been reported as wages to IRS (e.g., the unrecovered cost of employee meals, education costs, auto allowances), and
40-62 Rev.
DRAFT FORM CMS-2552-10 4005.2 (Cont.)
d. The total cost of the particular wage-related cost for employees whose services are paid under IPPS exceeds 1 percent of total salaries after the direct excluded salaries are removed (Worksheet S-3, Part III, column 4, line 3). Wage-related cost exceptions to the core list are not to include those wage-related costs that are required to be reported to the Internal Revenue Service as salary or wages (i.e., loan forgiveness, sick pay accruals). Include these costs in total salaries reported on line 1 of this worksheet.
NOTE: Do not include wage-related costs applicable to the excluded areas reported on lines 9 and 10. Instead, these costs are reported on line 19. Also, do not include the wage-related costs for physician Parts A and B, non-physician anesthetists Parts A and B, interns and residents in approved programs, and home office personnel.
Line 19--Enter the total (core and other) wage-related costs applicable to the excluded areas reported on lines 9 and 10.
Lines 20 through 25--Enter from your records the wage-related costs for each category of employee listed. The costs are the core wage related costs plus the other wage-related costs. Do not include wage-related costs for excluded areas reported on line 19. Subscript line 22, and report the wage related costs for Part A teaching physicians reported on line 4.01, on line 22.01. On line 23, do not include wage-related costs related to non-physician salaries reported for hospital-based RHCs and FQHCs services included on Worksheet A, column 1, lines 88 and/or 89, as applicable. These wage-related costs are reported separately on line 24.
Lines 26 through 43--Enter the direct salary and wages with related salary amounts for paid vacation, holiday, sick, other paid-time-off (PTO), severance, and bonus pay from Worksheet A, column 1 for the appropriate cost center identified on lines 26 through 43, column 2.
These lines provide for the collection of hospital wage data for overhead costs to properly allocate the salary portion of the overhead costs to the appropriate service areas for excluded units. These lines are completed by all hospitals if the ratio of Part II, column 5, sum of lines 9 and 10, divided by the result of column 5, line 1 minus the sum of lines 2, 3, 4.01, 5, 6, 7, 7.01 and 8, equals or exceeds a threshold of 15 percent. However, all hospitals with a ratio greater than 5 percent must complete Part III line 7, for all columns. Calculate the percent to two decimal places for purposes of rounding.
Line 26--Salaries and hours reported on this line correlate to the salaries reported on line 4, column 1 of Worksheet A, for the personnel working in the Employee Benefit Department, or the Human Resources Department. Do not report costs or hours associated with other hospital employees on this line.
Lines 28, 33, and 35--Enter the amount paid for services performed under contract (in accordance with the general contract labor instructions above), rather than by employees, for A&G, housekeeping, and dietary services, respectively. Continue to report on the standard lines (line 27, 32, and 34), the amounts paid for services rendered by employees not under contract.
Line 28--Administrative and General (A&G) costs are expenses a hospital incurs in carrying out its administrative and/or general management functions. Include on line 28, the contract services that are included on Worksheet A, line 5, and subscripts, column 2 (“Administrative and General”). Contract information and data processing services, legal, tax preparation, cost report preparation, and purchasing services are examples of contract labor costs that would be included on this line and must not be reported on lines 11 or 12. Do not include on line 28 the costs for top level management contracts (these costs are reported on line 12).
Rev. 40-63
4005.2 (Cont.) FORM CMS-2552-10 DRAFT
Lines 32 through 35--All hospitals must incur costs for housekeeping and dietary services, either direct, under contract, or both. It is not acceptable to report zeroes for housekeeping or dietary services. Report wages and hours for housekeeping services on either line 32 (direct) or line 33 (contract), and for dietary services, on either line 34 (direct) or line 35 (contract). Hospitals are encouraged to ensure that their contracts clearly specify the salaries, wages, and hours related to all of their contract labor. If, in rare instances, hours for these services cannot be determined exactly from the contract, determine the hours based on a reasonable estimation. Examples of reasonable estimates are regional average hourly rates, including an average of the wages and hours for dietary and housekeeping services of other hospitals in the same CBSA. Hospitals also may conduct time studies to determine hours worked. If regional averages or time studies cannot be used, data from the Bureau of Labor Statistics may be used to obtain average wages and hours for housekeeping and dietary services.
Column 3--Enter on each line, as appropriate, the salary and wages portion (as defined in column 2 instructions) of any reclassifications made on Worksheet A-6.
Column 4--Enter on each line the result of column 2 plus or minus column 3.
Column 5--Enter on each line the number of paid hours corresponding to the amounts reported in column 4. Paid hours include regular hours (including paid lunch hours), overtime hours, paid holiday, vacation and sick leave hours, paid time-off hours, and hours associated with severance pay. For Part II, lines 1 through 15 (including subscripts), lines 26 through 43 (including subscripts), and Part III, line 7, if the hours cannot be determined, then the associated salaries must not be included in columns 2 through 4.
NOTE: The hours must reflect any change reported in column 3; For employees who work a regular work schedule, on call hours are not to be included in the total paid hours (on call hours should only relate to hours associated to a regular work schedule; overtime hours are calculated as one hour when an employee is paid time and a half. No hours are required for bonus pay. The intern and resident hours associated with the salaries reported on line 7 must be based on 2080 hours per year for each full time intern and resident employee. The hours reported for salaried employees who are paid a fixed rate are recorded as 40 hours per week or the number of hours in your standard work week.
NOTE: Workers who are contracted solely for the purpose of providing services on-call can only be included on Worksheet S-3 when they actually work the on-call schedule; that is, they are actually delivering patient care at the hospital, or are at the hospital so as to be available to deliver patient care. If either of these latter two scenarios occur, then both the wages and associated hours actually worked must be included in the appropriate contract labor line on Worksheet S-3.
Column 6--Enter on all lines (except lines 17 through 25), the average hourly wage resulting from dividing column 4 by column 5.
4005.3 Part III - Hospital Wage Index Summary.--This worksheet provides for the calculation of a hospital’s average hourly wage (without overhead allocation, occupational mix adjustment, and inflation adjustment) as well as analysis of the wage data.
Columns 1 through 6--Follow the same instructions discussed in Part II, except for column 6, line 5.
Line 1--From Part II, enter the result of line 1 minus the sum of lines 2, 3, 4.01, 5, 6, 7, 7.01, and 8. Add to this amount lines: 28, 33, and 35.
Line 2--From Part II, enter the sum of lines 9 and 10.
40-64 Rev.
DRAFT FORM CMS-2552-10 4005.4 (Cont.)
Line 3--Enter the result of line 1 minus line 2.
Line 4--From Part II, enter the sum of lines 11, 12, 13, 14, and 15. (Line 16 is omitted from Part III, line 4, because physicians' teaching services are excluded from the wage index.)
Line 5--From Part II, enter the sum of lines 17, 18, and 22. Enter on this line in column 6, the wage-related cost percentage computed by dividing Part III, column 4, line 5, by Part III, column 4, line 3. Round the result to 2 decimal places.
Line 6--Enter the sum of lines 3 through 5.
Line 7--Enter from Part II above, the sum of lines 26 through 43. If the hospital’s ratio for excluded area salaries to net salaries is greater than 5 percent, the hospital must complete all columns for this line. (See instructions in Part II, lines 26 through 43, for calculating the percentage.)
4005.4 Part IV - Wage Related Costs.--The hospital must provide the contractor with a complete list of all core wage related costs included in Part II (§4005.2), lines 17 and 19 through 25. This worksheet provides for the identification of such costs.
The hospital must determine whether each wage related cost “other than core”, reported on line 25, exceeds one (1) percent of the total adjusted salaries net of excludable salaries and meets all of the following criteria:
The costs are not listed on lines 1 through 23, “Wage Related Costs Core”
If any of the additional wage related cost applies to the excluded areas of the hospital, the cost associated with the excluded areas has been removed prior to making the 1 percent threshold test.
The wage related cost has been reported to the IRS, as a fringe benefit if so required by the IRS.
The individual wage related cost is not included in salaries reported on Worksheet S-3, Part II, column 3, line 17.
The wage related cost is not being furnished for the convenience of the employer.
For wage related costs not covered by Medicare reasonable cost principles (excluding the reporting of certain defined benefit pension costs; see instructions below), a hospital shall use GAAP in reporting wage related costs. In addition, some costs such as payroll taxes, which are reported as a wage related cost(s) on Worksheet S-3, Part IV, are not considered fringe benefits for Medicare cost finding.
Enter on each line as applicable the corresponding amount from your accounting books and/or records.
Line 3--Report pension cost for defined benefit pension plans than do not meet the applicable requirements for a qualified pension plan under section 401(a) of the Internal Revenue Code.
The policy adopted in the FFY 2012 IPPS final rule, 76 FR 51586 - 51590, (August 18, 2011), does not change the reporting basis for these costs.
NOTE: These plans generally are not funded by a funding vehicle that is for exclusive benefit of employees or their beneficiaries and do not qualify for special tax benefits, such as tax deferral of employer contributions. For such unfunded defined benefit plans, the costs of these plans are reported on a cash basis which recognizes benefit payments made during the current period. Typically these plans supplement the basic qualified defined benefit plan or provide benefits to a select class of employees, such as executives.
Rev. 40-65
4005.4 (Cont.) FORM CMS-2552-10 DRAFT
Line 4--Commencing with cost reporting periods used for the FFY 2013 wage index, report pension cost for defined benefit pension plans which meet the applicable requirements for a qualified pension plan under §401(a) of the Internal Revenue Code for the wage index. The allowable pension costs to be reported for these defined benefit pension plans shall be determined in accordance with the policy adopted in the FY 2012 IPPS final rule, 76 FR 51586‑51590 (August 18, 2011), and as discussed below. Enter the pension costs from your records or from the Wage Index Pension Cost Schedule (Exhibit 3) below. (See CMS Pub. 15-1, chapter 21, §2142.)
Policy
Defined Benefit Pension Plan: A defined benefit pension plan is a type of deferred compensation plan, which is established and maintained by the employer primarily to provide systematically for the payment of definitely determinable benefits to its employees usually over a period of years, or for life, after retirement. Pension plan benefits are generally measured by, and based on, such factors as age of employees, years of service, and compensation received by employees. This section applies only to defined benefit pension plans which meet the applicable requirements for a qualified pension plan under §401(a) of the Internal Revenue Code. A qualified pension plan is for the exclusive benefit of employees or their beneficiaries and qualifies for special tax benefits, such as tax deferral of employer contributions.
Pension Contributions: Pension costs for a defined benefit pension plan are allowable only to the extent that costs are actually incurred by the provider Such costs are found to have been incurred only if paid directly to participants or beneficiaries under the terms of the plan or paid to a pension fund which meets the applicable tax qualification requirements under §401(a) of the Internal Revenue Code. For purposes of the wage index, provider pension payments shall be measured on a cash-basis without regard to CMS Pub. 15-1, chapter 23, §2305. Payment must be made by check or other negotiable instrument, cash, or legal transfer of assets such as stocks, bonds, real property, and etcetera. A contribution payment shall be deemed to occur on the date it is credited to the fund established for the pension plan, or for provider payments made directly to a plan participant or beneficiary, on the date the provider’s account is debited. Contributions made under a pension plan that covers multiple providers or employers shall be allocated on a basis consistent with plan records. If the plan records do not show a separate accounting of the actuarially determined cost estimates, contribution deposits, and/or assets attributable to each participating provider or employer, the allocation basis must represent a reasonable approximation of the funding attributable to each employer.
Source of Documentation for Pension Contributions: Providers are required to obtain contribution data from the pension trustee, insurance carrier, Schedule B or SB of IRS Form 5500, and if applicable, from accounting records showing the allocation of total plan contributions to each participating provider. These records must be maintained as needed for subsequent periods.
Reasonable Compensation: In order for pension costs to be allowable, the benefits payable under the plan (attributable to employer contributions) together with all other compensation paid to the employee must be reasonable in amount.
Defined Benefit Pension Plan Costs for the Wage Index: The annual pension to be included in the wage index shall be the average annual employer contributions made by or on behalf of the provider (on a cash basis) to all defined benefit plans covered under this section during the averaging period. Contribution payments must satisfy the allowability requirements outlined above; see “Pension Contributions” and “Reasonable Compensation” above. A reversion of plan assets shall be treated as a negative contribution payment and a negative pension cost resulting from a reversion of plan assets shall offset a provider’s other wage related costs.
40-65.1 Rev.
DRAFT FORM CMS-2552-10 4005.4 (Cont.)
The averaging period is generally the 36 consecutive calendar month period centered on the midpoint of the cost reporting period used for the wage index (the cost reporting period used for the wage index shall hereafter be referred to as the wage index cost reporting period). If the midpoint of the wage index cost reporting period is not the first day of a calendar month, use the first day of the midpoint month or the first day of the following month as the midpoint. The same averaging period must be used for all defined benefit plans sponsored by a provider.
A provider who adopts a new defined benefit pension plan and has no other defined benefit plan in existence during the averaging period may elect to exclude from the averaging period all cost reporting periods ending prior to the date the new plan was adopted. No defined benefit pension cost is reportable for a wage index cost reporting period that is excluded from the averaging period in accordance with this paragraph. An election to claim costs for a newly adopted plan based on an averaging period of less than 36 months must be applied on a consistent basis for all wage index cost reporting periods for which the 36-month averaging period contains the plan effective date.
If the wage index cost reporting period does not represent a 12-month period, the annual pension cost otherwise determined in accordance with this section shall be prorated to reflect the number of months in the wage index cost reporting period.
NOTE: For the FY 2013 through FY 2022 wage index only, a provider may include a prefunding installment as a component of pension cost regardless of whether or not the plan(s) which gave rise to the prefunding balance are still in existence. The annual prefunding installment shall equal 1/10th of the prefunding balance. A prefunding installment that is not reflected in the pension cost for a wage index cost reporting period may not be reassigned and added to the pension cost reported for wage index purposes in any subsequent period. The prefunding balance equals the excess, if any, of (i) provider contributions made (on a cash-basis) to its defined benefit pension plans during the look‑back period over (ii) the pension costs included in the wage-index for the same look‑back period. A provider’s share of the total contributions made under a pension plan that covers multiple providers or employers shall be determined on a basis consistent with the methodology used to determine the wage index pension costs for the cost reporting periods included in the prefunding balance. The look-back period shall consist of consecutive provider cost reporting periods commencing no earlier than October 1, 2002 and ending with the provider’s cost reporting period immediately prior to the FY 2013 wage index cost reporting period. The look-back period may not include any cost reporting period for which the provider is unable to provide documentation of the contributions made or the pension costs included in the wage index; all prior cost reporting periods must also be excluded in order to satisfy the requirement that the look-back period consist of consecutive cost reporting periods. A provider who establishes a prefunding balance must submit documentation to the Medicare contractor to support the calculation of the prefunding balance and annual prefunding installment.
Examples
Example 1 (prefunding balance and prefunding installment):
Provider’s FY 2013 wage index cost reporting period is 01/01/2010-12/31/2009. The look-back period therefore ends with the cost reporting period ending 12/31/2008 (immediately prior to the FY 2013 wage index cost reporting period). Assuming the provider has always reported costs on a calendar year basis, the earliest possible cost reporting period in the look-back period is the period commencing 01/01/2003 (first cost reporting period commencing on or after 10/01/2002).
Rev. 40-65.2
4005.4 (Cont.) FORM CMS-2552-10 DRAFT
The provider is able to document its pension contributions (on a cash basis) and the pension costs included in the wage index for all cost reporting periods except for the 2004 year. Therefore, 2004 and all prior cost reporting periods must be excluded from the look-back period. The data for 2005 through 2008 is as follows:
Cost Reporting Year Cash Basis Contributions Wage-Index Pension Costs
2005 $400,000 $500,000
2006 $800,000 $0
2007 $0 $600,000
2008 $650,000 $700,000
Because the pension cost reported in the wage index for 2005 was higher than the cash contributions made during that same period, the provider may elect to drop 2005 (and all prior periods) from the look-back period.
Although the contributions made in 2007 were also less than the pension cost reported for that same period, the provider cannot exclude 2007 without also excluding 2006 (look-back period must consist of consecutive cost reporting periods).
Although the contributions made in 2008 were less than the pension cost reported in that same period, the provider cannot exclude 2008 since the look-back period must end with 2008 because that is the cost reporting period immediately prior to the FY 2013 wage index cost reporting period.
The prefunding balance based on a 2006-2008 look-back period is $150,000 ($1,450,000 [$800,000+$0+$650,000] total contributions - $1,300,000 [$0 + $600,000 + $700,000] in wage index pension costs reported for the same period). The annual prefunding installment is $15,000 (1/10th of $150,000).
Example 2 (pension cost for a 12 month wage index cost reporting period):
Provider’s FY 2013 wage index cost reporting period is 12 months (01/01/2009 – 12/31/2009); the midpoint of wage index cost reporting period is 07/01/2009; the 36‑month averaging period is 01/01/2008 to 12/31/2010 (begins 18 months prior to midpoint and ends 18 months following the midpoint).
Contributions made in wage index cost reporting period 01/01/2009 – 12/31/2009 = $500,000.
Contributions made during 01/01/2008 – 12/31/2008 = $300,000.
Contributions made during 01/01/2010 – 12/31/2010 = $600,000.
Total contributions made during the 36-month averaging period = $1,400,000.
The provider has no prefunding balance or prefunding installment.
The pension cost for the FY 2013 wage index cost reporting period is $466,667 ($1,400,000 total contributions divided by 36 months in the averaging period multiplied by 12 months in the wage index cost reporting period).
40-65.3 |
Rev. |
DRAFT FORM CMS-2552-10 4005.4 (Cont.)
Example 3 (pension cost for a 7 month wage index cost reporting period):
Provider’s FY 2013 wage index cost reporting period is 7 months (01/01/2009 – 07/31/2009); the midpoint of the wage index cost reporting period is 04/15/2009; since the midpoint must be adjusted to the first of the month (either preceding or following); the provider elects to use 04/01/2009 as the midpoint; the 36-month averaging period is 10/01/2007 to 09/30/2010 (begins 18 months prior to midpoint and ends 18 months following the midpoint).
Contributions made in wage index cost reporting period 01/01/2009 – 07/31/2009 = $300,000.
Contributions made during 10/01/2007 – 12/31/2008 = $500,000.
Contributions made during 08/01/2009 – 09/30/2010 = $600,000.
Total contributions made during the 36-month averaging period = $1,400,000.
The provider has documented a prefunding balance of $1,000,000; the annual prefunding installment is therefore $100,000 (1/10th of prefunding balance).
The pension cost for the FY 2013 wage index cost reporting period is $330,555 ($272,222 average pension cost [$1,400,000 total contributions divided by 36 months in the averaging period multiplied by 7 months in the in wage index cost reporting period] plus $58,333 pro-rata prefunding installment [$100,000 annual prefunding installment multiplied by 7/12ths to reflect a 7 month wage index cost reporting period]).
Example 4 (pension cost for a new plan):
Provider’s FY 2015 wage index cost reporting period is 12 months (01/01/2011 – 12/31/2011); the midpoint of the wage index cost reporting period is 07/01/2011; the 36-month averaging period is 01/01/2010 to 12/31/2012 (begins 18 months prior to midpoint and ends 18 months following the midpoint).
The provider adopted a new pension plan effective 07/01/2011 and had no other pension plan in effect prior to that date; therefore, there is no prefunding balance or prefunding installment.
Contributions made during 01/01/2010 - 12/31/2010 =$0 (no plan in existence)
Contributions made in the wage index cost reporting period 01/01/2011 - 12/31/2011 = $500,000.
Contributions made during 01/01/2012 - 12/31/2012 = $1,200,000.
Total contributions during the 36-month averaging period = $1,700,000.
The provider did not report a pension cost attributable to the new plan based on a 36-month averaging period during any prior wage index cost reporting period; therefore it may elect to exclude cost reporting periods ending prior to the 07/01/2011 plan effective date from the averaging period; the 36-month averaging period is, therefore, shortened to 24 months and excludes the period 01/01/2010 to 12/31/2010. The pension cost for the FY 2015 wage index cost reporting period would then be $850,000 ($1,700,000 total contributions divided by 24 months in the averaging period multiplied by 12 months in the wage index reporting period).
Rev. 40-65.4
4005.4 (Cont.) FORM CMS-2552-10 DRAFT
Alternatively, the provider may have reported a pension cost for the FY 2014 wage index (2010 wage index cost reporting period) based on a full 36-month averaging period of 01/01/2009 to 12/31/2011. The pension cost for that prior period would have been $166,667 ($500,000 total contributions divided by 36 months in the averaging period, multiplied by 12 months in wage index cost reporting period). If the provider reported a pension cost for the new plan based on a full 36-month averaging period for the FY 2014 wage index, it must also compute pension costs for the FY 2015 wage index (2011 wage index cost reporting period) using a 36-month averaging period. The pension cost for the 2011 wage index cost reporting period is $566,667 ($1,700,000 total contributions divided by 36 months in the averaging period, multiplied by 12 months in the wage index cost reporting period).
NOTE: Fees paid to external organizations (for example, actuarial fees, claim administration fees, IRS form preparation fees) for providing services that are directly associated with a provider’s wage-related costs, including a provider’s defined benefit pension plan(s), may be included in wage-related costs on Worksheet S-3, Part II for the period in which the expense is incurred (see Worksheet S-3, Part IV, line 6). Such expenses are to be reported as additional costs only if they are paid directly by the provider and NOT out of the plan assets.
Wage Index Pension Cost Schedule:
Use the following instructions and schedule (exhibit 3) to calculate your wage index pension cost and enter the result of line 19 below on Worksheet S-3, Part IV, line 4.
Step 1:
Line 1--Enter the wage index FY for which pension cost is to be determined. This schedule applies to wage index FYs starting with 2013.
Line 2--Enter the provider cost reporting period to be used for the wage index year in line 1. This cost period must commence in the Medicare FY (10/1-9/30) four years prior to the wage index year shown in line 1. For example, the provider cost reporting period for the FY 2013 wage index must commence in the Medicare FY ending September 30, 2009.
Line 3--Enter the midpoint of the provider cost reporting period shown in line 2. This should always be the first day of a calendar month. If the midpoint occurs in the middle of a month, enter either the first day of the midpoint month or the first day of the following month.
Line 4--Enter the date (1st of a month) that occurs 18 months prior to the midpoint date shown in line 3. (Note: This date will not necessarily coincide with the beginning of a cost reporting period.)
Line 5--Enter the date (last day of a month) that occurs 18 months after the midpoint date shown in line 3. (Note: This date will not necessarily coincide with the end of a cost reporting period.)
Step 2:
STEP 2 IS OPTIONAL. Complete step 2 only if all of the following apply:
The provider has a new defined benefit plan that was effective during the averaging period determined in step 1;
The provider had no other defined benefit plan in effect during the averaging period;
The provider did not report pension costs for the new plan in a prior period based on a 36‑month averaging period which included cost reporting periods ending prior to the plan effective date;
The provider elects to report costs for the new pension plan based on a shortened averaging period excluding all cost reporting periods which ended prior to the plan effective date.
40-65.5 Rev.
DRAFT FORM CMS-2552-10 4005.4 (Cont.)
Line 6--Enter the effective date of the new plan that occurs within the averaging period determined in step 1.
Line 7--Enter the first day of the provider's cost reporting period in which the plan was effective. For example, if the plan was effective during the provider's cost reporting period that began on 01/01/2010, enter 01/01/2010.
Line 8--Enter the date from line 7 if it is the first of a calendar month; otherwise enter the first of the month immediately preceding or following the date in line 7.
Step 3:
Line 9--Enter the beginning date of the averaging period from line 4 or line 8, as applicable.
Line 10--Enter the ending date of the averaging period from line 5.
Line 11--Complete the table to show the total provider contributions made (on a cash basis) during the averaging period commencing on the date shown on line 9 and ending on the date shown on line 10. Contributions may be grouped to correspond with the periods shown in supporting documentation. Contributions made under a pension plan that covers multiple providers or employers shall be allocated on a basis consistent with plan records. If the plan does not provide for a separate accounting of the costs, contributions, and/or assets attributable to each participating provider or employer, the allocation basis must represent a reasonable approximation of the costs attributable to each employer. Supporting documentation must show the amounts and dates of deposit for all contributions reported and the data to support the allocation of total plan contributions, if applicable. Examples of acceptable documentation to support the total deposits include pension trust or insurance statements, or Schedule SB of IRS Form 5500.
Line 12--Enter the total number of calendar months included in the averaging period (enter "36" unless Step 2 was completed for a new plan).
Line 13--Total the contributions listed in the table under line 11.
Line 14--The average monthly contribution during the averaging period is line 13 divided by line 12.
Line 15--Enter the number of (full or partial) months in the provider's cost reporting period shown on line 2.
Line 16--The average pension contributions equals line 14 multiplied by line 15.
Step 4:
Line 17--If the provider has established a prefunding balance, enter the annual prefunding installment from line 8 of the Pension Prefunding Worksheet. If the provider has not elected to establish a pension prefunding balance, enter zero (0).
Line 18--The reportable prefunding installment is the amount shown on line 17 multiplied by line 15 divided by 12.
Line 19--The reportable pension cost for the wage index equals line 18 plus line 16. Enter the result on Worksheet S-3, Part, IV, line 4.
Rev. |
40-65.6 |
4005.4 (Cont.) FORM CMS-2552-10 DRAFT
Exhibit 3
Wage Index Pension Cost Schedule
Provider Name: ________________________________________________________ CCN: __________
Step 1: Determine the 3-Year Averaging Period
1. Wage Index fiscal year ending. _ _________
2. Provider cost reporting period used for Wage Index year shown on line 1. from: ________ to: __________
3. Midpoint of provider's cost reporting period shown on line 2. (adjust response to first of month) __________
4. Date beginning the 3-year averaging period. (subtract 18 months from midpoint shown on line 3) __________
5 Date ending the 3-year averaging period. (add 18 months to midpoint shown on line 3) __________
Step 2: Adjust Averaging Period for a New Plan (See instructions)
(Leave this section blank if the provider has not elected to use an adjusted averaging period)
6. Effective date of pension plan. _________
7. First day of the provider cost reporting period containing the pension plan effective date. _________
8. Starting date of the adjusted averaging period. (date on line 7 if first of the month, otherwise adjust
response to first of month) ________
If this date occurs after the period shown on line 2 (Step 1), stop here and see instructions. No cost is reportable for a period which is excluded from the averaging period.
Step 3: Average Pension Contributions During the Averaging Period
9. Beginning date of averaging period from line 4 or line 8. __________
10. Ending date of averaging period from line 5. __________
11. Enter provider contributions made during the averaging period shown on lines 9 & 10. Add additional lines as necessary if more than 15 contributions are made during the cost reporting period.
(Data may be grouped within the averaging period to agree with documentation records (enter beginning date of grouped date range))
Deposit Date(s) Contributions Deposit Date(s) Contributions
1. _____________ 16. _________________ _______
2. _____________ 17. _________________ _______
3. _____________ 18. _________________ _______
4. _____________ 19. _________________ _______
5. _____________ 20. _________________ _______
6. _____________ 21. _________________ _______
7. _____________ 22. _________________ _______
8. _____________ 23. _________________ _______
9. _____________ 24. _________________ _______
10. _____________ 25. _________________ _______
11. _____________ 26. _________________ _______
12. _____________ 27. _________________ _______
13. _____________ 28. _________________ _______
14. _____________ 29. _________________ _______
15. _____________ 30. _________________ _______
12. Total number of months included in the averaging period. __________
13. Total contributions made during averaging period. __________
14. Average monthly contribution. (line 13 divided by line 12) __________
15. Number of months in provider cost reporting period on line 2. __________
16. Average pension contributions. (line 14 multiplied by line 15) __________
Step 4: Total Pension Cost for Wage Index
17. Annual prefunding installment from line 8 of pension prefunding worksheet, if applicable. ___________
18. Reportable prefunding installment. (line 17 multiplied by line 15 divided by 12) __________
19. Total Pension Cost for Wage Index. (line 16 plus line 18) __________
Prepared By: ________________________________________________________ Date: __________
40-65.7 |
Rev. |
DRAFT FORM CMS-2552-10 4005.5
(Continuation of Worksheet S-3, Part IV Instructions)
Line 21--Report costs of executive deferred compensation plans and awards for executives. The policy adopted in the FFY 2012 IPPS final rule; 76 FR 51586 - 51590 (August 18, 2011) does not change the reporting basis for these costs. Examples of executive deferred compensation include special stock option or bonus plans and sum certain postemployment awards that are not available to other employees.
NOTE: Costs reported on line 21 excludes costs of executive deferred compensation that are defined contribution pension plans, tax-sheltered annuity plans, nonqualified defined benefit plans and qualified defined benefit plans that are available to other employees that is reportable on lines 1 through 4, respectively.
4005.5 Part V - Contract Labor and Benefit Costs.--This section identifies the contract labor costs and benefit costs for the hospital complex and applicable subproviders and units.
Definitions:
Contract Labor Costs--Enter the amount paid for services furnished under contract, rather than by employees, for direct patient care, as defined in the instructions for Worksheet S-3, Part II, line 11. The amount of Contract Labor report on S-3, Part II, line 11 should agree with the amount reported on S-3, Part V, line 2. This is only for the hospital (not including excluded areas). The remainder of Worksheet S-3, Part V, should reflect Contract Labor as defined on Worksheet S-3, Part II, line 11, (direct patient care for all of the excluded areas) with the aggregate total reported on line 1.
Benefit Costs--Enter the amount of employee benefit costs, also referred to as wage-related costs. Worksheet S-3, Part IV, provides a list of core wage-related costs. The core wage-related costs reported on S-3, Part IV, line 24, which is spread on Worksheet S-3, Part II, lines 17 and 19-25, must be reported by component on Worksheet S-3, Part V. The amount reported on Worksheet S-3, Part V, line 1, must agree to the allowable amount reported on Worksheet S-3, Part IV, line 24. Worksheet S-3, Part V, line 2, must agree to the amount reported on Worksheet S-3, Part II, line 17. Each excluded area must contain their share of wage related costs so that lines 19 through 25 on Worksheet S-3, Part II, will agree to Worksheet S-3, Part V, lines 3 through 18.
Identify the contract labor costs and benefit costs for each component on the applicable line.
Rev. 40-65.8
4006 FORM CMS-2552-10 DRAFT
4006. WORKSHEET S-4 - HOSPITAL-BASED HOME HEALTH AGENCY STATISTICAL DATA
In accordance with 42 CFR 413.20(a), 42 CFR 413.24(a), and 42 CFR 413.24(c), you are required to maintain statistical records for proper determination of costs payable under titles V, XVIII, and XIX. The statistics required on this worksheet pertain to a hospital-based home health agency. The data maintained is dependent upon the services provided by the agency, number of program home health aide hours, total agency home health aide hours, program unduplicated census count, and total unduplicated census count. In addition, FTE data are required by employee staff, contracted staff, and total. Complete a separate S-4 for each hospital-based home health agency.
Line 1--Enter the number of hours applicable to home health aide services.
Line 2--Enter the unduplicated count of all individual patients and title XVIII patients receiving home visits or other care provided by employees of the agency or under contracted services during the reporting period. Count each individual only once. However, because a patient may be covered under more than one health insurance program, the total census count (column 5, line 2) may not equal the sum of columns 1 through 4, line 2. For purposes of calculating the unduplicated census, if a beneficiary has received healthcare in more than one CBSA, you must prorate the count of that beneficiary so as not to exceed a total of (1). A provider is to also query the beneficiary to determine if he or she has received healthcare from another provider during the year, e.g., Maine versus Florida for beneficiaries with seasonal residence.
Lines 3 through 18--Lines 3 through 18 provide statistical data related to the human resources of the HHA. The human resources statistics are required for each of the job categories specified in lines 3 through 18.
Enter the number of hours in your normal work week.
Report in column 1 the full time equivalent (FTE) employees on the HHA’s payroll. These are staff for which an IRS Form W-2 is used.
Report in column 2 the FTE contracted and consultant staff of the HHA.
Compute staff FTEs for column 1 as follows: Add all hours for which employees were paid and divide by 2080 hours. Round to two decimal places, e.g., .04447 is rounded to .04. Compute contract FTEs for column 2 as follows. Add all hours for which contracted and consultant staff worked and divide by 2080 hours.
If employees are paid for unused vacation, unused sick leave, etcetera, exclude these paid hours from the numerator in the calculations.
Line 19--Enter in column 1 the number of CBSAs that you serviced during this cost reporting period.
Line 20--Enter each 5-digit CBSA and/or non-CBSA (rural) code where the reported HHA visits were performed. Subscript the line to accommodate the number of CBSAs you service. Rural CBSA codes are assembled by placing the digits “999” in front of the two digit State code, e.g., for the State of Maryland the rural CBSA code is 99921.
PPS Activity Data--Applicable for Medicare Services.
In accordance with 42 CFR 413.20 and §1895 of the Social Security Act, home health agencies transitioned from a cost based reimbursement system to a prospective payment system (PPS) effective for home health services rendered on or after October 1, 2000.
40-66 Rev.
DRAFT FORM CMS-2552-10 4006 (Cont.)
The statistics required on this worksheet pertain to home health services furnished on or after October 1, 2000. The data to be maintained, depending on the services provided by the agency, includes the number of aggregate program visits furnished in each episode of care payment category for each covered discipline, the corresponding aggregate program charges imposed in each episode of care payment category for each covered discipline, total visits and total charges for each episode of care payment category, total number of episodes and total number of outlier episodes for each episode of care payment category, and total medical supply charges for each episode of care payment category.
HHA Visits--See CMS Pub. 15-2, chapter 32, §3205, page 32-13 for the definition of an HHA visit.
Episode of Care--Under home health PPS the 60 day episode is the basic unit of payment where the episode payment is specific to one individual beneficiary. Beneficiaries are covered for an unlimited number of non-overlapping episodes. The duration of a full length episode will be 60 days. An episode begins with the start of care date and must end by the 60th day from the start of care.
Less than a full Episode of Care--When 4 or fewer visits are provided by the HHA in a 60 day episode period, the result is a low utilization payment adjustment (LUPA). In this instance the HHA will be reimbursed based on a standardized per visit payment.
An episode may end before the 60th day in the case of a beneficiary elected transfer, or a discharge and readmission to the same HHA (including for an intervening inpatient stay). This type of situation results in a partial episode payment (PEP) adjustment.
Use lines 21 through 32 to identify the number of visits and the corresponding visit charges for each discipline for each episode payment category. Lines 33 and 35 identify the total number of visits and the total corresponding charges, respectively, for each episode payment category. Line 36 identifies the total number of episodes completed for each episode payment category. Line 37 identifies the total number of outlier episodes completed for each episode payment category. Outlier episodes do not apply to 1) Full Episodes without Outliers, and 2) LUPA Episodes. Line 38 identifies the total medical supply charges incurred for each episode payment category. Column 5 displays the sum total of data for columns 1 through 4. The statistics and data required on this worksheet are obtained from the PS&R report.
When an episode of care is initiated in one fiscal year and concludes in the subsequent fiscal year, all statistical data (i.e., cost, charges, counts, etc…) associated with that episode of care will appear on the PS&R of the fiscal year in which the episode of care is concluded. Similarly, all data required in the cost report for a given fiscal year must only be associated with services rendered during episodes of care that conclude during the fiscal year. Title XVIII visits reported on this worksheet will not agree with the title XVIII visits reported on Worksheet H-3, sum of columns 2 and 3, line 14.
Columns 1 through 4--Enter data pertaining to title XVIII patients only. Enter, as applicable, in the appropriate columns 1 through 4, lines 21 through 32, the number of aggregate program visits furnished in each episode of care payment category for each covered discipline and the corresponding aggregate program visit charges imposed for each covered discipline for each episode of care payment category. The visit counts and corresponding charge data are mutually exclusive for all episode of care payment categories. For example, visit counts and the corresponding charges that appear in column 4 (PEP only Episodes) will not include any visit counts and corresponding charges that appear in column 3 (LUPA Episodes) and vice versa. This is true for all episode of care payment categories in columns 1 through 4.
Rev. 40-67
4006 (Cont.) FORM CMS-2552-10 DRAFT
Line 33--Enter in columns 1 through 4 for each episode of care payment category, respectively, the sum total of visits from lines 21, 23, 25, 27, 29, and 31.
Line 34--Enter in columns 1 through 4 for each episode of care payment category, respectively, the charges for services paid under PPS and not identified on any previous lines.
Line 35--Enter in columns 1 through 4 for each episode of care payment category, respectively, the sum total of visit charges from lines 22, 24, 26, 28, 30, 32, and 34.
Line 36--Enter in columns 1 through 4 for each episode of care payment category, respectively, the total number of episodes (standard/non-outlier) of care rendered and concluded in the provider’s fiscal year.
Line 37--Enter in columns 2 and 4, for each episode of care payment category identified, respectively, the total number of outlier episodes of care rendered and concluded in the provider’s fiscal year. Outlier episodes do not apply to columns 1 and 3 (Full Episodes without Outliers and LUPA Episodes, respectively).
NOTE: Lines 36 and 37 are mutually exclusive.
Line 38--Enter in columns 1 through 4, for each episode of care payment category, respectively, the total non-routine medical supply charges for services rendered and concluded in the provider’s fiscal year.
Column 5--Enter on lines 21 through 37, respectively, the sum total of amounts from columns 1 through 4.
40-68 Rev.
DRAFT FORM CMS-2552-10 4007
4007. WORKSHEET S-5 - HOSPITAL RENAL DIALYSIS DEPARTMENT STATISTICAL DATA
In accordance with 42 CFR 413.20(a), 42 CFR 413.24(a), and 42 CFR 413.24(c), you are required to maintain statistical records for proper determination of costs payable under the Medicare program. The statistics reported on this worksheet pertain to the renal dialysis department. The data maintained, depending on the services provided by the hospital, includes patient data, the number of treatments, number of stations, and home program data.
If you have more than one renal dialysis department, submit one Worksheet S-5 combining all of the renal dialysis departments’ data. You must also have on file (as supporting documentation), a Worksheet S-5 for each renal dialysis department and the appropriate workpapers. File this documentation with exception requests in accordance with CMS Pub. 15-1, chapter 27, §2720. Also enter on the combined Worksheet S-5 the applicable data for each renal dialysis satellite for which you are separately certified (that is, a satellite for which you were issued a satellite CCN).
Section 153(b) of MIPPA amended section 1881(b) of the Act to require the implementation of an ESRD bundled payments system effective January 1, 2011. This new payment system is effectuated on Worksheets I-4 and I-5 (sections 4051 and 4052).
Column Descriptions
Columns 1 and 2--Include in these columns information regarding outpatient hemodialysis patients. Do not include information regarding intermittent peritoneal dialysis. In column 2, report information if you are using high flux dialyzers.
Columns 3 through 6--Report information concerning the provider’s training and home programs. Do not include intermittent peritoneal dialysis information in columns 3 and 5.
Line Descriptions
Line 1--Enter the number of patients receiving dialysis at the end of the cost reporting period.
Line 2--Enter the average number of times patients receive dialysis per week. For CAPD and CCPD patients, enter the number of exchanges per day.
Line 3--Enter the average time for furnishing a dialysis treatment.
Line 4--Enter the average number of exchanges for CAPD.
Line 5--Enter the number of days dialysis is furnished during the cost reporting period.
Line 6--Enter the number of stations used to furnish dialysis treatments at the end of the cost reporting period.
Line 7--Enter the number of treatments furnished per day per station. This number represents the number of treatments that the facility can furnish not the number of treatments actually furnished.
Line 8--Enter your utilization. Compute this number by dividing the number of treatments furnished by the product of lines 5, 6, and 7. This percentage cannot exceed 100 percent.
Line 9--Enter the number of times your facility reuses dialyzers. This number is the average number of times patients reuse a dialyzer. If none, enter zero.
Line 10--Enter the percentage of patients that reuse dialyzers.
Rev. |
40-69 |
4007 (Cont.) FORM CMS-2552-10 DRAFT
Line 10.01.--Indicate whether your facility qualified and was approved as a low-volume facility for this cost reporting period. CMS adjusts the base rate for low-volume ESRD facilities. In order to receive this low-volume adjustment, a facility must attest in accordance with 42 CFR 413.232(f). Effective for cost reporting periods ending on or after June 30, 2015, if you operate multiple renal dialysis departments or home program dialysis departments and one of those facilities is eligible for low-volume, respond yes to this question.
Line 10.02.--Indicate if your facility elected 100 percent PPS effective January 1, 2011. Enter “Y” for yes or “N” for no. This election must have been received by the ESRD facility’s contractor by November 1, 2010. Requests received after this date will not be accepted regardless of postmark or delivery date.
New providers: ESRD facilities certified for Medicare participation on or after January 1, 2011, are paid based on 100 percent of the ESRD PPS payment. ESRD facilities certified for Medicare participation on or after January 1, 2011, enter “Y” for yes.
Line 10.03.--If your facility did not elect to be paid based on 100 percent of the ESRD PPS payment and your cost reporting period is a December 31 fiscal year end, enter the transition period in column 2 as follows: For the fiscal year ending December 31, 2011, enter 1; for the fiscal year ending December 31, 2012, enter 2; for the fiscal year ending December 31, 2013, enter 3; and, for the fiscal year ending December 31, 2014, enter 4 for 100 percent ESRD PPS payment. Column 1 will be blank.
If your cost reporting period ends on a date other than December 31, indicate in column 1 the transition period effective for the portion of the cost reporting period prior to January 1. Indicate in column 2 the transition period effective for the portion of the cost reporting period on and after January 1. For example, a cost reporting period with a fiscal year ending October 31 would indicate the applicable transition periods as follows:
Fiscal year ending October 31, 2011: Leave column 1 blank as this would be pre-bundled ESRD PPS, and enter 1 in column 2 for the period of January 1, 2011, through October 31, 2011.
Fiscal year ending October 31, 2012: Enter 1 in column 1 for the period of November 1, 2011 through December 31, 2011, and enter 2 in column 2 for the period of January 1, 2012 through October 31, 2012.
Fiscal year ending October 31, 2013: Enter 2 in column 1 for the period of November 1, 2012 through December 31, 2012 and enter 3 in column 2 for the period of January 1, 2013 through October 31, 2013.
Fiscal year ending October 31, 2014: Enter 3 in column 1 for the period of November 1, 2013 through December 31, 2013 and enter 4 in column 2 for the period of January 1, 2014 through October 31, 2014.
For all cost reporting periods beginning on or after January 1, 2014, enter 4 in column 2 for 100 percent ESRD PPS payment.
Payments during the transition period 1 are a blend of 25 percent case-mix adjusted ESRD PPS and 75 percent basic case-mix adjusted composite rate (25/75). Payments during the transition period 2 are a blend of 50 percent case-mix adjusted ESRD PPS and 50 percent basic case-mix adjusted composite rate (50/50). Payments during the transition period 3 are a blend of 75 percent case-mix adjusted ESRD PPS and 25 percent basic case-mix adjusted composite rate (75/25). Payments for services rendered on and after January 1, 2014 are 100 percent ESRD PPS.
Line 11--Enter the number of patients who are awaiting a transplant at the end of the cost reporting period.
Line 12--Enter the number of patients who received a transplant during the fiscal year.
40-70 Rev.
09-13 FORM CMS-2552-10 4007 (Cont.)
Line 13--Enter the direct product cost net of discount and rebates for Epoetin (EPO). Include all EPO cost for patients receiving outpatient, home (Method I or II (claims that would have been processed as Method II are processed as Method I for services rendered on or after January 1, 2011)), or training dialysis treatments. This amount includes EPO cost furnished in the renal department or any other department if furnished to an end stage renal disease dialysis patient. Report on this line the amount of EPO cost included in line 74 of Worksheet A. Effective for cost reporting periods ending after December 31, 2012, do not use this line; report these costs on line 22 (and subscripts), column 2.
Line 14--Based on the instructions contained on line 13, enter the amount of EPO included on line 94 (home dialysis program) from Worksheet A. Effective for cost reporting periods ending after December 31, 2012, do not use this line; report these costs on line 22 (and subscripts), column 3.
Erythropoiesis-Stimulating Agents (ESA) Statistics--Effective January 1, 2005 and prior to January 1, 2011, Medicare paid for ESAs based on the Average Sales Price Drug Pricing File. Effective January 1, 2011, payment for ESAs is included in the ESRD PPS payment.
Line 15--Enter the number of EPO units furnished relating to the renal dialysis department. Effective for cost reporting periods ending after December 31, 2012, do not use this line; report the number of ESA units furnished on line 22 (and subscripts), column 4.
Line 16--Enter the number of EPO units furnished relating to the home dialysis program. Effective for cost reporting periods ending after December 31, 2012, do not use this line; report the number of ESA units furnished on line 22, (and subscripts), column 5.
Line 17--Enter the direct product cost net of discount and rebates for darbepoetin alfa (Aranesp) Include all Aranesp cost for patients receiving outpatient, home (Method I or II (claims that would have been processed as Method II are processed as Method I for services rendered on or after January 1, 2011)), or training dialysis treatments. This amount includes Aranesp cost furnished in the renal department or any other department if furnished to an end stage renal disease dialysis patient. Report on this line the amount of Aranesp cost included in line 74 of Worksheet A. Effective for cost reporting periods ending after December 31, 2012, do not use this line; report these costs on line 22 (and subscripts), column 2.
Line 18--Based on the instructions contained on line 17, enter the dollar amount of Aranesp included on line 94 (home dialysis program) from Worksheet A. Effective for cost reporting periods ending after December 31, 2012, do not use this line; report these costs on line 22 (and subscripts), column 3.
Line 19--Enter the number of micrograms (mcgrs) of Aranesp furnished relating to the renal dialysis department. Effective for cost reporting periods ending after December 31, 2012, do not use this line; report the number of ESA units furnished on line 22 (and subscripts), column 4.
Line 20--Enter the number of micrograms of Aranesp furnished relating to the home dialysis program. Effective for cost reporting periods ending after December 31, 2012, do not use this line; report the number of ESA units furnished on line 22 (and subscripts), column 5.
Line 21--Identify how physicians are paid for medical services provided to Medicare beneficiaries. Under the monthly capitation payment (MCP) methodology, contractors pay physicians for their Part B medical services. Under the initial method, the renal facility pays for physicians’ Part B medical services. The facility’s payment rate is increased in accordance with 42 CFR 414.313. There are a limited number of facilities electing this method.
Line 22--Identify each ESA separately on line 22 and subscripts. Complete this line effective for cost reporting periods ending after December 31, 2012. Enter in column 1, the name of the ESA
Rev. 4 40-70.1
4007 (Cont.) FORM CMS-2552-10 09-13
administered to renal dialysis patients. Enter in column 2, the direct product cost net of discounts and rebates for ESAs administered to renal dialysis patients. These costs are included in line 74 of Worksheet A. Include all ESA costs for patients receiving outpatient, home, or training dialysis treatments. This amount includes ESA costs furnished in the renal department or any other department if furnished to an end stage renal disease dialysis patient. Enter in column 3 the direct product cost net of discounts and rebates for ESAs administered to home dialysis patients. These costs are included in line 94 of Worksheet A.
Include all ESA costs for patients receiving self-care home dialysis treatments. This amount includes ESA costs furnished in the home dialysis program for an end stage renal disease dialysis patient. Enter in column 4, the total ESA units furnished to renal dialysis department patients during the cost reporting period. Enter in column 5, the total ESA units furnished to home program dialysis patients during the cost reporting period.
40-70.2 |
Rev. 4 |
DRAFT FORM CMS-2552-10 4008
4008. WORKSHEET S-6 - HOSPITAL-BASED COMMUNITY MENTAL HEALTH CENTER AND OTHER OUTPATIENT REHABILITATION PROVIDER STATISTICAL DATA
In accordance with 42 CFR 413.20(a), 42 CFR 413.24(a), and 42 CFR 413.24(c), maintain statistical records for proper determination of costs payable under the Medicare program. The statistics reported on this worksheet pertain to hospital-based community mental health centers (CMHCs), comprehensive outpatient rehabilitation facilities (CORFs), outpatient rehabilitation facilities (ORFs) which generally furnishes outpatient physical therapy (OPT), outpatient occupational therapy (OOT), or outpatient speech pathology (OSP). If you have more than one hospital-based component, complete a separate worksheet for each facility.
Additionally, only CMHCs are required to complete the corresponding Worksheet J series. However, all CMHCs, CORFs, ORFs, OPTs, OOTs, and OSPs must complete the applicable Worksheet A cost center for the purpose of overhead allocation.
This worksheet provides statistical data related to the human resources of the community mental health center. FTE data is required by employee staff, contracted staff, and total. The human resources statistics are required for each of the job categories specified on lines 1 through 17. Enter any additional categories needed on line 18.
Enter the number of hours in your normal work week in the space provided.
Report in column 1 the full time equivalent (FTE) employees on the CMHC or outpatient rehabilitation provider's payroll. These are staff for which an IRS Form W-2 was issued.
Report in column 2 the FTE contracted and consultant staff of the CMHC or outpatient rehabilitation provider.
Compute staff FTEs for column 1 as follows: Add hours for which employees were paid divided by 2080 hours, and round to two decimal places, e.g., round .04447 to .04. Compute contract FTEs for column 2 as follows. Add all hours for which contracted and consultant staff worked divided by 2080 hours, and round to two decimal places.
If employees are paid for unused vacation, unused sick leave, etcetera, exclude the paid hours from the numerator in the calculations.
Rev. 40-71
4009 FORM CMS-2552-10 DRAFT
4009. WORKSHEET S-7 - PROSPECTIVE PAYMENT FOR SKILLED NURSING FACILITIES STATISTICAL DATA
In accordance with 42 CFR 413.20(a), 42 CFR 413.24(a), and 42 CFR 413.24(c), you are required to maintain statistical records for proper determination of costs payable under the Medicare program. Public Law 105-33 (Balanced Budget Act of 1997) requires that all SNFs be reimbursed under PPS for cost reporting periods beginning on and after July 1, 1998.
Line 1--If this facility contains a hospital-based SNF, if all patients were covered under managed care or if there was no Medicare utilization, enter “Y” for yes. If the response is yes, do not complete the rest of this worksheet.
Line 2--Does this hospital have an agreement under either section 1883 or 1913 of the Act for swingbeds? Enter “Y” for yes or “N” for no in column 1. If yes, enter arrangement date (mm/dd/yyyy) in column 2.
Column Descriptions for Lines 3 Through 200
Column 1--The case mix resource utilization group (RUGs) designations are already entered in this column.
Column 2--Enter the number of days associated with SNF services. All SNF payment data will be reported as a total amount paid under the RUG PPS payment system on Worksheet E-3, Part VI, line 1 and will be generated from the PS&R or your records.
Column 3--Enter the number of days associated with the swing beds. All swingbed SNF payment data will be reported as a total amount paid under the RUG PPS payment system on Worksheet E-2, line 1 and will be generated from the PS&R or your records.
Column 4--Enter the sum total of columns 2 and 3.
Line 201--Enter in column 1, the CBSA code in effect at the beginning of the cost reporting period. Enter in column 2, the CBSA code in effect on or after October 1 of the current cost reporting period, if applicable.
Lines 202 through 206--A notice published in the 68 FR 46036 - 46072 (August 4, 2003), provided for an increase in RUG payments to hospital based SNFs for payments on or after October 1, 2003. Congress expects this increase to be used for direct patient care and related expenses. Lines 202 through 206 are identified as following: 202 - Staffing, 203 - Recruitment, 204 - Retention of Employees, 205 - Training, and 206 - Other. Enter in column 1 the direct patient care expenses and related expenses in accordance with the above referenced Federal Register citation. Enter in column 2, the ratio, expressed as a percentage, of total expenses for each category to total SNF revenue from Worksheet G-2, Part I, line 7, column 3. For each line, indicate in column 3, whether the increased RUG payments received reflects increases associated with direct patient care and related expenses by responding “Y” for yes. Indicate “N” for no if there was no increase in spending in any of these areas. If the increased spending is in an area not previously identified in areas one through four, identify on the “Other (Specify)” line(s), the cost center(s) description and the corresponding information as indicated above.
40-72 Rev.
DRAFT FORM CMS-2552-10 4010
4010. WORKSHEET S-8 - HOSPITAL-BASED RHC/FQHC STATISTICAL DATA
In accordance with 42 CFR 413.20(a), 42 CFR 413.24(a), and 42 CFR 413.24(c), you are required to maintain separate statistical records for proper determination of costs payable under the Medicare program. The statistics reported on this worksheet pertain to hospital-based RHCs/FQHCs. If you have more than one of these clinics/centers, complete a separate worksheet for each. Hospital-based RHCs/FQHCs may elect to file a consolidated cost report pursuant to CMS Pub. 100-4, chapter 9, §30.8. Effective for cost reporting periods beginning on and after October 1, 2014, Hospital-based FQHCs no longer complete Worksheet S-8 and must complete Worksheet S-11 to report statistical data.
Lines 1 and 2--Enter the full address of the hospital-based RHC/FQHC.
Line 3--For hospital-based FQHCs only, enter your appropriate designation of “R” for rural or “U” for urban. See CMS Pub. 100-04, chapter 9, §20.6.2 for information regarding urban and rural designations. If you are uncertain of your designation, contact your contractor. Hospital‑based RHCs do not complete this line.
Lines 4 through 9--In column 1, enter the applicable grant award number(s). In column 2, enter the date(s) awarded.
Line 10--If the facility provides other than hospital-based RHC or FQHC services (e.g., laboratory or physician services), answer “Y” for yes and enter the type of operation on subscripts of line 11, otherwise enter “N” for no.
Line 11--Enter in columns 1 through 14 the starting and ending hours in the applicable columns for the days that the facility is available to provide hospital-based RHC/FQHC services. Enter the starting and ending hours in the applicable columns 1 through 14 for the days that the facility is available to provide other than hospital-based RHC/FQHC services. When entering time, do so as military time, e.g., 2:00 p.m. is 1400.
Line 12--Have you received an approval for an exception to the productivity standards? Enter a “Y” for yes or an “N” for no.
Line 13--Is this a consolidated cost report as defined in CMS Pub. 100-04, chapter 9, §30.8? If yes, enter in column 2, the number of providers included in this report, complete line 14, and complete only one worksheet series M for the consolidated group. If no, complete a separate Worksheet S-8 for each component accompanied by a corresponding Worksheet M series.
Line 14--Identify clinic/center name and CCN number filing the consolidated cost report.
Rev. |
40-73 |
4010.1 FORM CMS-2552-10 DRAFT
4010.1. WORKSHEET S-11 - HOSPITAL-BASED FQHC IDENTIFICATION DATA
In accordance with 42 CFR 413.20(a), 42 CFR 413.24(a), and 42 CFR 413.24(c), you are required to maintain statistical records for proper determination of costs payable under the Medicare program. The statistics reported on this worksheet pertain to hospital-based FQHCs and are effective for cost reporting periods beginning on or after October 1, 2014. Hospital‑based FQHCs may elect to file a consolidated cost report pursuant to CMS Pub. 100‑04, chapter 9, §30.8. If you have more than one hospital-based FQHC reported on Worksheet S-2, Part I, line 16, and its subscripts, complete a separate Worksheet S-11, Part I, for each.
This worksheet consists of three parts:
Part I - Hospital-Based FQHC Identification Data
Part II - Hospital-Based FQHC Consolidated Cost Report Participant Identification Data
Part III - Hospital-Based FQHC Statistical Data
4010.2. Part I - Hospital-Based FQHC Identification Data--The information required on this worksheet is needed to properly identify the hospital-based FQHC(s) listed on Worksheet S‑2, Part I, line 16, and its subscripts, or in the case of a consolidated cost report, the primary hospital-based FQHC. In the case of a consolidated cost report, only the primary FQHC completes the entire Worksheet S-11, Part I. All other hospital-based FQHCs filing under a consolidated cost report must be listed on line 9 and its subscripts and must complete a separate Worksheet S-11, Part II.
Line 1--Enter the hospital-based FQHC site name in column 1. Indicate the type of control under which the hospital-based FQHC operates by entering a number from the list below in column 2.
1 = Voluntary Nonprofit, Corporation 7 = Governmental, Federal
2 = Voluntary Nonprofit, Other 8 = Governmental, State
3 = Proprietary, Individual 9 = Governmental, County
4 = Proprietary, Corporation 10 = Governmental, City
5 = Proprietary, Partnership 11 = Governmental, Other
6 = Proprietary, Other
Enter the date the hospital-based FQHC terminated its participation in the Medicare program (if applicable) in column 3. In column 4, enter a “V” for a voluntary termination or an “I” for an involuntary termination.
If the hospital-based FQHC changed ownership immediately prior to the beginning of the cost reporting period enter the date of the change of ownership in column 5. Also submit the name and address of the new owner and a copy of the sales agreement with the cost report.
Line 2--Enter the Hospital-based FQHC’s street address in column 1 and the post office box in column 2 (if applicable).
Line 3--Enter the city in column 1, state in column 2, ZIP code in column 3, county in column 4, and the appropriate designation (“U” for urban or “R” for rural) in column 5. See CMS Pub. 100-04, chapter 9, §20.6.2, for information regarding urban and rural designations. If you are uncertain of your designation, contact your contractor.
40-73.1 |
Rev. |
DRAFT FORM CMS-2552-10 4010.2 (Cont.)
Line 4--Indicate whether this hospital-based FQHC is owned, leased or controlled by an entity that operates multiple FQHCs. Enter a “Y” for yes or an “N” for no. If yes, complete lines 5 through 7. Otherwise, skip to line 8.
Lines 5 through 7--Enter the name of the entity that owns, leases or controls the hospital-based FQHC, the street address, post office box (if applicable), HRSA grant award number assigned to the organization, city, state, and ZIP code.
Line 8--Indicate whether this hospital-based FQHC is filing a consolidated cost report under CMS Pub. 100‑04, chapter 9, §30.8. Enter “Y” for yes or “N” for no. If yes, enter in column 2, the date the hospital-based FQHC requested approval to file a consolidated cost report, and in column 3, the date the contractor approved the hospital-based FQHCs request to file a consolidated cost report.
Line 9--If the response to line 8, column 1 is yes, list on line 9, and its subscripts, each hospital‑based FQHC that is part of this consolidated cost report, excluding the primary hospital-based FQHC listed on line 1. Enter in column 1 the site name; column 2 the CCN, column 3 the CBSA, column 4 the date the hospital-based FQHC requested approval to file as part of a consolidated cost report, and column 5 the date the contractor approved the hospital-based FQHCs request to file as part of a consolidated cost report. Each hospital-based FQHC listed on line 9 and its subscripts must complete a separate Worksheet S-11, Part II.
Line 10--There are 3 types of organizations that are eligible to enroll in Medicare as a hospital‑based FQHC. Indicate in column 1, the type of organization this hospital-based FQHC is by entering a number from the list below. If your response in column 1 is “1” or “3”, enter any or all of the alpha character (s) associated with the response in column 2. For example if you entered “1” in column 1, enter in column 2, “A”, “B”, “C” and/or “D.” An organization receiving a grant under §330 of the Public Health Service (PHS) Act or an outpatient health program/facility can operate as any or all of the subcategories listed under the respective numeric options presented below.
An organization receiving a grant(s) under §330 of the PHS Act:
Community Health Centers
Migrant and Seasonal Agricultural Workers Health Centers
Health Care for the Homeless Health Centers
Health Centers for Residents of Public Housing
Health Center Program Look-Alikes; Organizations that have been identified by HRSA as meeting the definition of “Health Center” under §330 of the PHS Act, but not receiving grant funding under §330; or,
Outpatient health program/facility operated by:
A tribe or tribal organization under the Indian Self-Determination Act
An urban Indian organization under title V of the Indian Health Care Improvement Act
Other
Line 11--Indicate if your hospital-based FQHC received a grant under §330 of the PHS Act during this cost reporting period. If this is a consolidated cost report, did the primary hospital-based FQHC reported on line 1, column 2 receive a grant under §330 of the PHS Act during this cost reporting period? Enter “Y” for yes or “N” for no.
Rev. 40-73.2
4010.2 (Cont.) FORM CMS-2552-10 DRAFT
Line 12--If the response to line 11 is yes, indicate in column 1, the type of grant that was awarded from the list below. Enter the date of the grant award in column 2, and enter the grant award number in column 3. If you received more than one grant subscript this line accordingly.
1 = Community Health Center (§330(e), PHS Act)
2 = Migrant and Seasonal Agricultural Workers Health Center (§330(g), PHS Act)
3 = Health Care for the Homeless Health Centers (§330(h), PHS Act)
4 = Health Centers for Residents of Public Housing (§330(i), PHS Act)
5 = Other
Line 13--Indicate if your hospital-based FQHC submitted an initial deeming or annual redeeming application for medical malpractice coverage to HRSA under the Federal Tort Claims Act (FTCA). Enter “Y” for yes or “N” for no in column 1. If column 1 is yes, enter the effective date of coverage in column 2.
Line 14--Indicate if the hospital-based FQHC received a THC development grant authorized under Part C of title VII of the PHS Act from HRSA for the purpose of establishing new accredited or expanded primary care residency programs. Enter “Y” for yes or “N” for no in column 1. If yes, enter the number of FTE residents your hospital-based FQHC trained using THC funding in column 2.
4010.3. Part II - Hospital-Based FQHC Consolidated Cost Report Participant Identification Data--For each hospital-based FQHC that is included on Worksheet S-11, Part I, line 9, and its subscripts, a separate Worksheet S-11, Part II, must be completed in the identical sequence that the consolidated hospital-based FQHCs are reported on Worksheet S-11, Part I, line 9, and its subscripts. Do not complete this worksheet for the primary hospital-based FQHC reported on Worksheet S-11, Part I, line 1.
Line 1--Enter the hospital-based FQHC site name in column 1 and the certification date in column 2. Indicate the type of control under which the hospital-based FQHC operates by entering a number from the list below in column 3.
1 = Voluntary Nonprofit, Corporation 7 = Governmental, Federal
2 = Voluntary Nonprofit, Other 8 = Governmental, State
3 = Proprietary, Individual 9 = Governmental, County
4 = Proprietary, Corporation 10 = Governmental, City
5 = Proprietary, Partnership 11 = Governmental, Other
6 = Proprietary, Other
Enter the date the hospital-based FQHC terminated its participation in the Medicare program (if applicable) in column 4. In column 5, enter a “V” for a voluntary termination or an “I” for an involuntary termination.
If the hospital-based FQHC changed ownership immediately prior to the beginning of the cost reporting period enter the date of the change of ownership in column 6. Also submit the name and address of the new owner and a copy of the sales agreement with the cost report.
Line 2--Enter the hospital-based FQHC’s street address in column 1 and the post office box in column 2 (if applicable).
40-73.3 Rev.
DRAFT FORM CMS-2552-10 4010.3
Line 3--Enter the city in column 1, state in column 2, ZIP code in column 3, county in column 4, and the appropriate designation (“U” for urban or “R” for rural) in column 5. See CMS Pub. 100-04, chapter 9, §20.6.2, for information regarding urban and rural designations. If you are uncertain of your designation, contact your contractor.
Line 4--There are 3 types of organizations that are eligible to enroll in Medicare as a hospital-based FQHC. Indicate in column 1, the type of organization this hospital-based FQHC is by entering a number from the list below. If your response in column 1 is “1” or “3”, enter any or all of the alpha characters associated with the response in column 2. For example if you entered “1” in column 1, enter in column 2, “A”, “B”, “C” and/or “D”. An organization receiving a grant under §330 of the PHS Act or an outpatient health program/facility can operate as any or all of the subcategories listed under the respective numeric options below.
An organization receiving a grant(s) under §330 of the PHS Act:
Community Health Centers
Migrant and Seasonal Agricultural Workers Health Centers
Health Care for the Homeless Health Centers
Health Centers for Residents of Public Housing
Health Center Program Look-Alikes; Organizations that have been identified by HRSA as meeting the definition of “Health Center” under §330 of the PHS Act, but not receiving grant funding under §330; or,
Outpatient health program/facility operated by:
A tribe or tribal organization under the Indian Self-Determination Act
An urban Indian organization under title V of the Indian Health Care Improvement Act
Other
Line 5--Indicate if your hospital-based FQHC received a grant under §330 of the PHS Act during this cost reporting period. Enter “Y” for yes or “N” for no.
Line 6--If the response to line 5 is yes, indicate in column 1, the type of grant that was awarded from the list below. Enter the date of the grant award in column 2 and enter the grant award number in column 3. If you received more than one grant subscript this line accordingly.
1 = Community Health Center (§330(e), PHS Act)
2 = Migrant and Seasonal Agricultural Workers Health Center (§330(g), PHS Act)
3 = Health Care for the Homeless Health Center (§340(d), PHS Act)
4 = Health Centers for Residents of Public Housing ((§330(i), PHS Act)
5 = Other
Line 7--Indicate if this hospital-based FQHC submitted an initial deeming or annual redeeming application for medical malpractice coverage to HRSA under the FTCA. Enter “Y” for yes or “N” for no in column 1. If column 1 is yes, enter the effective date of coverage in column 2.
Line 8--Indicate if the hospital-based FQHC received a THC development grant authorized under Part C of title VII of the PHS Act from HRSA for the purpose of establishing new accredited or expanded primary care residency programs. Enter “Y” for yes or “N” for no in column 1. If yes, enter the number of FTE residents your FQHC trained using THC funding in column 2.
Rev. 40-73.4
4010.4 FORM CMS-2552-10 DRAFT
4010.4. Part III - Hospital-Based FQHC Statistical Data--This part collects statistical data regarding the number and types of visits by title. If you have more than one hospital-based FQHC reported on Worksheet S-2, Part I, line 16 and its subscripts, complete a separate Worksheet S-11, Part III, for each. If you elected to file consolidated, complete one Worksheet S‑11, Part III, for the primary hospital-based FQHC and all subcomponents.
Only those visits associated with a beneficiary receiving services under the Medicare fee for service program are included in column 2. However, visits attributable to beneficiaries enrolled in a Medicare Advantage plan must be included in column 4. For the purposes of the Medicare program, a beneficiary who receives care at a hospital-based FQHC can be seen for three types of visits:
Medical Visit
Medical Visit for Subsequent Illness or Injury
Mental Health Visit
Column 0--Use this column only when you are filing a consolidated cost report to identify each hospital-based FQHC listed on Worksheet S-11, Part I, line 9, and subscripts in the exact same order.
Columns 1 through 3--Enter the number of medical visits and mental health visits for each program (title V, title XVIII and title XIX). Include dually eligible (Medicare/Medicaid) beneficiaries in column 2.
Column 4--Enter the total medical visits and mental health visits for all patients. The total hospital-based FQHC medical and mental health visits in column 4 may not equal the sum of the visits reported in columns 1 through 3, as visits paid by other insurers (i.e., private pay) are included in this column.
Line 1--Enter the number of medical visits applicable to columns 1 through 4. Each visit to the hospital-based FQHC by the beneficiary counts as a single visit, even in the case where a beneficiary returns to the hospital-based FQHC in the same day for a subsequent illness or injury. If you are filing under a consolidated cost report, line 1 must contain the medical visits exclusively for the primary CCN and you must subscript line 1 to report the number of medical visits for each additional hospital-based FQHC included in this consolidated cost report. Each subscript of line 1, column 0, must contain a corresponding CCN from Worksheet S-11, Part I, line 9, and subscripts, in the exact same order. Enter the number of medical visits applicable to columns 1 through 4, for each hospital-based FQHC listed on line 1 and its subscripts.
Line 2--Enter the total number of medical visits (sum of line 1 and its subscripts) for each applicable column.
Line 3--Enter the number of mental health visits applicable to columns 1 through 4. Each visit to the hospital-based FQHC by the beneficiary counts as a single visit, even in the case where a beneficiary returns to the hospital-based FQHC in the same day for a subsequent illness or injury. If you are filing under a consolidated cost report, line 3 must contain the mental health visits exclusively for the primary CCN and you must subscript line 3 to report the number of mental health visits for each additional hospital-based FQHC included in this consolidated cost report. Each subscript of line 3, column 0, must contain a corresponding CCN from Worksheet S-11, Part I, line 9, and subscripts, in the exact same order. Enter the number of mental health visits applicable to columns 1 through 4, for each hospital-based FQHC listed on line 3, and its subscripts.
Line 4--Enter the total number of mental health visits (sum of line 3 and its subscripts) for each applicable column.
40-73.5 Rev.
DRAFT FORM CMS-2552-10 4010.4 (Cont.)
Page reserved for future use.
Rev. 40-73.6
4011 FORM CMS-2552-10 DRAFT
4011. WORKSHEET S-9 - HOSPITAL-BASED HOSPICE IDENTIFICATION DATA
In accordance with 42 CFR 418.310 hospice providers of service participating in the Medicare program are required to submit annual information for health care services rendered to Medicare beneficiaries. Also, 42 CFR 413.24(f) requires cost reports from providers on an annual basis. The data submitted on the cost reports supports management of Federal programs. The statistics required on this worksheet pertain to a hospital-based hospice. Complete a separate Worksheet S-9 for each hospital-based hospice.
4011.1 Part I - Enrollment Days for Cost Reporting Periods Beginning Before October 1, 2015.--
NOTE: Columns 1 and 2 contain the days identified in column 3 and 4. Column 3 and 4 identify the SNF and NF days out of the total for title XVIII and XIX.
Lines 1 through 4--Enter on lines 1 through 4 the enrollment days applicable to each level of care (LOC). Enrollment days are unduplicated days of care received by a hospice patient. A day is recorded for each day a hospice patient receives one of four levels of care. Where a patient moves from one LOC to another, count only one day of care for that patient for the last type of care rendered. For line 4, an inpatient care day should be reported only where the hospice provides or arranges to provide the inpatient care.
Line 5--Enter the total of columns 1 through 6 for lines 1 through 4.
For the purposes of the Medicare and Medicaid hospice programs, a patient electing hospice can receive only one of the following four types of care per day:
Hospice Continuous Home Care (HCHC) Day - A HCHC day is a day on which the hospice patient is not in an inpatient facility, and receives continuous care during a period of crisis in order to maintain the individual at home. A day consists of a minimum of 8 hours and a maximum of 24 hours of predominantly nursing care. For each day a beneficiary received 8 or more hours of predominantly nursing care, count the day as one HCHC day. Note: Do not count days by dividing the total hours by 24.
Hospice Routine Home Care (HRHC) Day - A HRHC day is a day on which the hospice patient is at home and not receiving HCHC.

 Hospice
Inpatient Respite Care
(HIRC) Day
- An HIRC
day is a day on which the hospice
patient receives care in an approved
inpatient facility, to
provide respite for the individual’s family or other persons
caring for the individual at home.
Hospice
Inpatient Respite Care
(HIRC) Day
- An HIRC
day is a day on which the hospice
patient receives care in an approved
inpatient facility, to
provide respite for the individual’s family or other persons
caring for the individual at home.


 Hospice
General Inpatient Care
(HGIP) Day
- A HGIP
day is a day on which the hospice
patient receives care in a Medicare
certified hospice facility, hospital
or SNF for pain control or acute or
chronic symptom management which cannot be managed in other settings.
Hospice
General Inpatient Care
(HGIP) Day
- A HGIP
day is a day on which the hospice
patient receives care in a Medicare
certified hospice facility, hospital
or SNF for pain control or acute or
chronic symptom management which cannot be managed in other settings.
 Column
Descriptions
Column
Descriptions

 Column
1--Enter only the unduplicated
Medicare days applicable to the four types of care. Enter on line 5
the total unduplicated Medicare days.
Column
1--Enter only the unduplicated
Medicare days applicable to the four types of care. Enter on line 5
the total unduplicated Medicare days.

 Column
2--Enter only the unduplicated
Medicaid days applicable to the four types of care. Enter on line 5
the total unduplicated Medicaid days.
Column
2--Enter only the unduplicated
Medicaid days applicable to the four types of care. Enter on line 5
the total unduplicated Medicaid days.

 Column
3--Enter only the unduplicated days
applicable to the four types of care for all Medicare hospice
patients residing in a skilled nursing facility. Enter on line 5 the
total unduplicated days.
Column
3--Enter only the unduplicated days
applicable to the four types of care for all Medicare hospice
patients residing in a skilled nursing facility. Enter on line 5 the
total unduplicated days.

40-74 Rev.
DRAFT FORM CMS-2552-10 4011.2

 Column
4--Enter only the unduplicated days
applicable to the four types of care for all Medicaid hospice
patients residing in a nursing facility. Enter on line 5,
the total unduplicated days.
Column
4--Enter only the unduplicated days
applicable to the four types of care for all Medicaid hospice
patients residing in a nursing facility. Enter on line 5,
the total unduplicated days.
 Column
5--Enter in column 5,
only the days applicable to the four types of care for all other non-
Medicare or Medicaid hospice patients. Enter on line 5 the total
unduplicated days.
Column
5--Enter in column 5,
only the days applicable to the four types of care for all other non-
Medicare or Medicaid hospice patients. Enter on line 5 the total
unduplicated days.

 Column
6--Enter the total days for each
type of care, (i.e., sum of columns 1, 2,
and 5). The amount entered in column 6, line 5,
should represent the total days provided by the hospice.
Column
6--Enter the total days for each
type of care, (i.e., sum of columns 1, 2,
and 5). The amount entered in column 6, line 5,
should represent the total days provided by the hospice.

 NOTE:
Convert continuous home care hours into days so that column 6, line
5,
reflects the actual total number of days provided by the hospice.
NOTE:
Convert continuous home care hours into days so that column 6, line
5,
reflects the actual total number of days provided by the hospice.
 4011.2 Part
II - Census Data for
Cost Reporting Periods Beginning Before October 1, 2015.--
4011.2 Part
II - Census Data for
Cost Reporting Periods Beginning Before October 1, 2015.--
NOTE: Columns 1 and 2 contain the days identified in columns 3 and 4. Columns 3 and 4 identify the SNF and NF days out of the total for title XVIII and XIX.

 Line
6--Enter the total number of
patients receiving hospice care within the cost reporting period for
the appropriate payer source.
Line
6--Enter the total number of
patients receiving hospice care within the cost reporting period for
the appropriate payer source.




 The
total under this line should equal the actual number of patients
served during the cost reporting period for each program. Thus, if a
patient’s total stay overlapped two reporting periods, the stay
should be counted once in each reporting period. The patient who
initially elects the hospice benefit, is discharged or revokes the
benefit, and then elects the benefit again within a reporting period
is considered to be a new admission with a new election and should be
counted twice.
The
total under this line should equal the actual number of patients
served during the cost reporting period for each program. Thus, if a
patient’s total stay overlapped two reporting periods, the stay
should be counted once in each reporting period. The patient who
initially elects the hospice benefit, is discharged or revokes the
benefit, and then elects the benefit again within a reporting period
is considered to be a new admission with a new election and should be
counted twice.


 A
patient transferring from another hospice is considered to be a new
admission and would be included in the count. If a patient entered a
hospice under a payer source other than Medicare and then
subsequently elects Medicare hospice benefit, count the patient once
for each pay source.
A
patient transferring from another hospice is considered to be a new
admission and would be included in the count. If a patient entered a
hospice under a payer source other than Medicare and then
subsequently elects Medicare hospice benefit, count the patient once
for each pay source.


 The
difference between line 6 and line 9 is that line 6 should equal the
actual number of patients served during the reporting period for each
program, whereas under line 9, patients are counted once, even if
their stay overlaps more than one reporting period.
The
difference between line 6 and line 9 is that line 6 should equal the
actual number of patients served during the reporting period for each
program, whereas under line 9, patients are counted once, even if
their stay overlaps more than one reporting period.


 Line
7--Enter the total title XVIII
Unduplicated Continuous Care hours billable to Medicare. When
computing the Unduplicated Continuous Care hours, count only one hour
regardless of number of services or therapies provided simultaneously
within that hour.
Line
7--Enter the total title XVIII
Unduplicated Continuous Care hours billable to Medicare. When
computing the Unduplicated Continuous Care hours, count only one hour
regardless of number of services or therapies provided simultaneously
within that hour.


 Line
8--Enter the average length of stay
for the reporting period. Include only the days for which a hospice
election was in effect. The average length of stay for patients with
a payer source other than Medicare and Medicaid is not limited to the
number of days under a hospice election. Line 5 divided by line
6.
Line
8--Enter the average length of stay
for the reporting period. Include only the days for which a hospice
election was in effect. The average length of stay for patients with
a payer source other than Medicare and Medicaid is not limited to the
number of days under a hospice election. Line 5 divided by line
6.









 The
statistics for a patient who had periods of stay with the hospice
under more than one program is included in the respective columns.
For example, patient A enters the hospice under Medicare hospice
benefit, stays 90 days, revokes the election for 70 days (and thus
goes back into regular Medicare coverage), then reelects the Medicare
hospice benefits for an additional 45 days, under a new benefit
period and dies (patient B).
The
statistics for a patient who had periods of stay with the hospice
under more than one program is included in the respective columns.
For example, patient A enters the hospice under Medicare hospice
benefit, stays 90 days, revokes the election for 70 days (and thus
goes back into regular Medicare coverage), then reelects the Medicare
hospice benefits for an additional 45 days, under a new benefit
period and dies (patient B).
Rev. 40-75
4011.2 (Cont.) FORM CMS-2552-10 DRAFT
Medicare patient C was in the program on the first day of the year and died on January 29 for a total length of stay of 29 days. Patient D was admitted with private insurance for 27 days, then their private insurance ended and Medicaid covered an additional 92 days. Patient E, with private insurance, received hospice care for 87 days. The average length of stay (LOS) (assuming these are the only patients the hospice served during the cost reporting period) is computed as follows:
 Medicare
Days (90 & 45 & 29) 164 days
Medicare
Days (90 & 45 & 29) 164 days
 Patient
(A, B & C)
Patient
(A, B & C)

 Medicare
Patients /3
Medicare
Patients /3
----
 Average
LOS Medicare 54.67 Days
Average
LOS Medicare 54.67 Days
 Medicaid
Days Patient D (92) 92 Days
Medicaid
Days Patient D (92) 92 Days
 Medicaid
Patient 1
Medicaid
Patient 1
 Average
LOS Medicaid 92 Days
Average
LOS Medicaid 92 Days
 Other
(Insurance) Days (87 & 27) 114 Days
Other
(Insurance) Days (87 & 27) 114 Days
 Other
Payments (D & E) 2
Other
Payments (D & E) 2
 Average
LOS (Other) 54 Days
Average
LOS (Other) 54 Days
 All
Patients (90+45+29+92+87+27) 370 Days
All
Patients (90+45+29+92+87+27) 370 Days
 Total
number of patients 6
Total
number of patients 6
 Average
LOS for all patients 61.67 Days
Average
LOS for all patients 61.67 Days
 Enter
the hospice’s average length of stay, without regard to payer
source, in column 6, line 8.
Enter
the hospice’s average length of stay, without regard to payer
source, in column 6, line 8.





 Line
9--Enter the unduplicated census
count of the hospice for all patients initially admitted and filing
an election statement with the hospice within a reporting period for
the appropriate payer source. Do not include the number of patients
receiving care under subsequent election periods (see
CMS Pub. 100-02, chapter
9, §10). However, the patient
who initially elects the hospice benefit, is discharged or revokes
the benefits, and elects the benefit again within the reporting
period is considered a new admission with each new election and
should be counted twice.
Line
9--Enter the unduplicated census
count of the hospice for all patients initially admitted and filing
an election statement with the hospice within a reporting period for
the appropriate payer source. Do not include the number of patients
receiving care under subsequent election periods (see
CMS Pub. 100-02, chapter
9, §10). However, the patient
who initially elects the hospice benefit, is discharged or revokes
the benefits, and elects the benefit again within the reporting
period is considered a new admission with each new election and
should be counted twice.
The total under this line should equal the unduplicated number of patients served during the reporting period for each program. Thus, you would not include a patient if their stay was counted in a previous cost reporting period. If a patient enters a hospice source other than Medicare and subsequently becomes eligible for Medicare and elects the Medicare hospice benefit, then count that patient only once in the Medicare column, even though he/she may have had a period in another payer source prior to the Medicare election. A patient transferring from another hospice is considered to be a new admission and is included in the count.
40-76 Rev.
DRAFT FORM CMS-2552-10 4011.4
4011.3. Part III - Enrollment Days for Cost Reporting Periods Beginning On or After October 1, 2015--This section collects unduplicated days data.
Lines 10 through 13--Enter the enrollment days applicable to each LOC in columns 1 through 3. Include dually eligible (Medicare/Medicaid) beneficiaries in column 1. Enrollment days are unduplicated days of care received by a hospice patient. Report a day for each day a hospice patient received one of four levels of care -- HCHC, HRHC, HIRC, or HGIP. When a patient was transferred from one LOC to another, count the day of transfer as one day of care at the LOC billed. Report an HIRC day on line 12, only when the hospice provided or arranged to provide the inpatient respite care.
Enter the total unduplicated days by LOC (sum of columns 1 through 3) in column 4.
Line 14--Enter the total unduplicated days (sum of lines 10 through 13) in each column, as applicable.
4011.4. Part IV - Contracted Statistical Data for Cost Reporting Periods Beginning On or After October 1, 2015--This section collects unduplicated days data for inpatient services at a contracted facility. The days reported in Part IV are a subset of the days reported in Part III.
Lines 15 and 16--Enter the contracted inpatient service enrollment days applicable to each LOC in columns 1 through 3. Include dually eligible (Medicare/Medicaid) beneficiaries in column 1. Enrollment days are unduplicated days of care received by a hospice patient. Report a day for each day a hospice patient received HIRC or HGIP care at a contracted facility. When a patient was transferred from one LOC to another, count the day of transfer as one day of care at the LOC billed. Enter the total unduplicated days by LOC (sum of columns 1 through 3) in column 4.
Rev. 40-76.1
4011.4 (Cont.) FORM CMS-2552-10 DRAFT
This page is reserved for future use.
40-76.2 Rev.
DRAFT FORM CMS-2552-10 4012
4012. Worksheet S-10 - Hospital Uncompensated and Indigent Care Data--Section 112(b) of the Balanced Budget Refinement Act (BBRA) requires that short-term acute care hospitals (§1886(d) of the Act) submit cost reports containing data on the cost incurred by the hospital for providing inpatient and outpatient hospital services for which the hospital is not compensated. Charity care charge data, as referenced in section 4102 of American Recovery and Reinvestment Act of 2009, may be used to calculate the EHR technology incentive payments made to §1886(d) hospitals and critical access hospitals (CAHs). CAHs, as well as §1886(d) hospitals, are required to complete this worksheet. Note that this worksheet does not produce the estimate of the cost of treating uninsured patients required for disproportionate share payments under the Medicaid program.
Definitions:
Uncompensated care--Defined as charity care and bad debt which includes non-Medicare bad debt and non-reimbursable Medicare bad debt. Uncompensated care does not include courtesy allowances or discounts given to patients.
Charity care--Health services for which a hospital demonstrates that the patient is unable to pay. Charity care results from a hospital's policy to provide all or a portion of services free of charge to patients who meet certain financial criteria. For Medicare purposes, charity care is not reimbursable and unpaid amounts associated with charity care are not considered as an allowable Medicare bad debt. (Additional guidance provided in the instruction for line 20.)
Non-Medicare bad debt--Health services for which a hospital determines the non-Medicare patient has the financial capacity to pay, but the non-Medicare patient is unwilling to settle the claim. (Additional guidance provided in the instruction for line 25.)
Non-reimbursable Medicare bad debt--The amount of allowable Medicare coinsurance and deductibles considered to be uncollectible but are not reimbursed by Medicare under the requirements of 42 CFR 413.89 and CMS Pub. 15-1, chapter 3. (Additional guidance provided in the instruction for line 25.)
Net revenue--Actual payments received or expected to be received from a payer (including co-insurance payments from the patient) for services delivered during this cost reporting period. Net revenue will typically be charges (gross revenue) less contractual allowance. (Applies to lines 2, 9, and 13.)
Instructions:
Cost to charge ratio:
Line 1--Enter the cost-to-charge ratio resulting from Worksheet C, Part I, line 202, column 3, divided by Worksheet C, Part I, line 202, column 8.
For all inclusive rate providers that do not complete Worksheet C, Part I, enter your cost‑to‑charge ratio as calculated in accordance with CMS Pub. 15-1, chapter 22, §2208.
Medicaid
NOTE: The amount on line 18 should not include the amounts on lines 2 and 5. That is, the amounts on lines 2 and 5 are mutually exclusive from the amount on line 18.
Line 2--Enter the inpatient and outpatient payments received or expected for title XIX covered services delivered during this cost reporting period. Include payments for an expansion SCHIP program, which covers recipients who would have been eligible for coverage under title XIX. Include payments for all covered services except physician or other professional services, and include payments received from Medicaid managed care programs. If not separately identifiable,
Rev. |
40-77 |
4012 (Cont.) FORM CMS-2552-10 DRAFT
disproportionate share (DSH) and supplemental payments should be included in this line. For these payments, report the amount received or expected for the cost reporting period, net of associated provider taxes or assessments.
Line 3--Enter “Y” for yes if you received or expect to receive any DSH or supplemental payments from Medicaid relating to this cost reporting period. Otherwise enter “N” for no.
Line 4--If you answered yes to question 3, enter “Y” for yes if all of the DSH or supplemental payments you received from Medicaid are included in line 2. Otherwise enter “N” for no and complete line 5.
Line 5--If you answered no to question 4, enter the DSH or supplemental payments the hospital received or expects to receive from Medicaid relating to this cost reporting period that were not included in line 2, net of associated provider taxes or assessments.
Line 6--Enter all charges (gross revenue) for title XIX covered services delivered during this cost reporting period. These charges should relate to the services for which payments were reported on line 2.
Line 7--Calculate the Medicaid cost by multiplying line 1 times line 6.
Line 8--Enter the difference between net revenue and costs for Medicaid by subtracting the sum of lines 2 and 5 from line 7. If line 7 is less than the sum of lines 2 and 5, then enter zero.
State Children’s Health Insurance Program:
Line 9--Enter all payments received or expected for services delivered during this cost reporting period that were covered by a stand-alone SCHIP program. Stand-alone SCHIP programs cover recipients who are not eligible for coverage under title XIX. Include payments for all covered services except physician or other professional services, and include any payments received from SCHIP managed care programs.
Line 10--Enter all charges (gross revenue) for services delivered during this cost reporting period that were covered by a stand-alone SCHIP program. These charges should relate to the services for which payments were reported on line 9.
Line 11--Calculate the stand-alone SCHIP cost by multiplying line 1 times line 10.
Line 12--Enter the difference between net revenue and costs for stand-alone SCHIP by subtracting line 9 from line 11. If line 11 is less than line 9, then enter zero.
Other state or local indigent care program:
Line 13--Enter all payments received or expected for services delivered during this cost reporting period for patients covered by a state or local government indigent care program (other than Medicaid or SCHIP), where such payments and associated charges are identified with specific patients and documented through the provider's patient accounting system. Include payments for all covered services except physician or other professional services, and include payments from managed care programs.
Line 14--Enter all charges (gross revenue) for services delivered during this cost reporting period for patients covered by a state or local government program, where such charges and associated payments are documented through the provider's patient accounting system. These charges should relate to the services for which payments were reported on line 13.
40-78 |
Rev. |
DRAFT FORM CMS-2552-10 4012 (Cont.)
Line 15--Calculate the costs for patients covered by a state or local government program by multiplying line 1 times line 14.
Line 16--Calculate the difference between net revenue and costs for patients covered by a state or local government program by subtracting line 13 from line 15. If line 15 is less than line 13, then enter zero.
Uncompensated care:
Line 17--Enter the value of all non-government grants, gifts and investment income received during this cost reporting period that were restricted to funding uncompensated or indigent care. Include interest or other income earned from any endowment fund for which the income is restricted to funding uncompensated or indigent care.
Line 18--Enter all grants, appropriations or transfers received or expected from government entities for this cost reporting period for purposes related to operation of the hospital, including funds for general operating support as well as for special purposes (including but not limited to funding uncompensated care). Include funds from the Federal Section 1011 program, if applicable, which helps hospitals finance emergency health services for undocumented aliens. While Federal Section 1011 funds were allotted for federal fiscal years 2005 through 2008, any unexpended funds will remain available after that time period until fully expended even after federal fiscal year 2008. If applicable, report amounts received from charity care pools net of related provider taxes or assessments. Do not include funds from government entities designated for non-operating purposes, such as research or capital projects.
Line 19--Calculate the total unreimbursed cost for Medicaid, SCHIP, and state and local indigent care programs by entering the sum of lines 8, 12, and 16.
Line 20--Enter the total initial payment obligation of patients who are given a full or partial discount based on the hospital’s charity care criteria (measured at full charges), for care delivered during this cost reporting period for the entire facility. For uninsured patients, including patients with coverage from an entity that does not have a contractual relationship with the provider (column 1), this is the patient’s total charges. For patients covered by a public program or private insurer with which the provider has a contractual relationship (column 2), these are the deductible and coinsurance payments required by the payer. Include charity care for all services except physician and other professional services. Do not include charges for either uninsured patients given discounts without meeting the hospital's charity care criteria or patients given courtesy discounts. Charges for non-covered services provided to patients eligible for Medicaid or other indigent care program (including charges for days exceeding a length‑of‑stay limit) can be included, if such inclusion is specified in the hospital's charity care policy and the patient meets the hospital's charity care criteria.
Line 21--Calculate the cost of initial obligation of patients approved for charity care by multiplying line 1 times line 20. Use column 1 for uninsured patients, including patients with coverage from an entity that does not have a contractual relationship with the provider, and use column 2 for patients covered by a public program or private insurer with which the provider has a contractual relationship.
Line 22--Enter payments received or expected from patients who have been approved for partial charity care for services delivered during this cost reporting period. Include such payments for all services except physician or other professional services. Payments from payers should not be included on this line. Use column 1 for uninsured patients, including patients with coverage from an entity that does not have a contractual relationship with the provider, and use column 2 for patients covered by a public program or private insurer with which the provider has a contractual relationship.
Rev. |
40-79 |
4012 (Cont.) FORM CMS-2552-10 DRAFT
Line 23--Calculate the cost of charity care by subtracting line 22 from line 21. Use column 1 for uninsured patients, including patients with coverage from an entity that does not have a contractual relationship with the provider, and use column 2 for patients covered by a public program or private insurer with which the provider has a contractual relationship.
Line 24--Enter “Y” for yes if any charges for patient days beyond a length-of-stay limit imposed on patients covered by Medicaid or other indigent care program are included in the amount reported in line 20, column 2, and complete line 25. Otherwise enter “N” for no.
Line 25--If you answered yes to question 24, enter charges for patient days beyond a length-of-stay limit imposed on patients covered by Medicaid or other indigent care program for services delivered during this cost reporting period. The amount must match the amount of such charges included in line 20, column 2.
Line 26--Enter the total facility (entire hospital complex) amount of bad debts written off on balances owed by patients during this cost reporting period. Include such bad debts for all services except physician and other professional services. The amount reported must also include the amounts reported on Worksheets E, Part A, line 64; E, Part B, line 34; E‑2, line 17, columns 1 and 2; E-3, Part I, line 11; E-3, Part II, line 23; E-3, Part III, line 24; E‑3, Part IV, line 14; E-3, Part V, line 25; E-3, Part VI, line 8; E-3, Part VII, line 34; I‑5, line 5 (line 5.05, column 2 for cost reporting periods that overlap or begin on or after or January 1, 2011); J‑3, line 21; and M-3, line 23. For privately insured patients, do not include bad debts that were the obligation of the insurer rather than the patient.
Line 27--Enter the total facility (entire hospital complex) Medicare reimbursable (also referred to adjusted) bad debts as the sum of Worksheets E, Part A, line 65; E, Part B, line 35; E‑2, line 17, columns 1 and 2 (line 17.01, columns 1 and 2 for cost reporting periods that begin on or after October 1, 2012); E-3, Part I, line 12; E-3, Part II, line 24; E-3, Part III, line 25; E‑3, Part IV, line 15; E-3, Part V, line 26; E-3, Part VI, line 10; I-5, line 11; J‑3, line 21 (line 22 for cost reporting periods that begin on or after October 1, 2012); and M‑3, line 23 (line 23.01 for cost reporting periods that begin on or after October 1, 2012).
Line 28--Calculate the non-Medicare and non-reimbursable Medicare bad debt expense by subtracting line 27 from line 26.
Line 29--Calculate the cost of non-Medicare and non-reimbursable Medicare bad debt expense by multiplying line 1 times line 28.
Line 30--Calculate the cost of uncompensated care by entering the sum of lines 23, column 3 and line 29.
Line 31--Calculate the cost of unreimbursed and uncompensated care and by entering the sum of lines 19 and 30.
40-80 Rev.
DRAFT FORM CMS-2552-10 4013
4013. WORKSHEET A - RECLASSIFICATION AND ADJUSTMENT OF TRIAL BALANCE OF EXPENSES
In accordance with 42 CFR 413.20, the methods of determining costs payable under title XVIII involve using data available from the institution's basic accounts, as usually maintained, to arrive at equitable and proper payment for services. Worksheet A provides for recording the trial balance of expense accounts from your accounting books and records. It also provides for the necessary reclassifications and adjustments to certain accounts. The cost centers on this worksheet are listed in a manner which facilitates the transfer of the various cost center data to the cost finding worksheets (e.g., on Worksheets A, B, C, and D, the line numbers are consistent). While providers are expected to maintain their accounting books and general ledger in a manner consistent with the standard cost centers/departments identified on this worksheet, not all of the cost centers listed apply to all providers using these forms. For example, IPPS providers may contain a Burn Intensive Care Unit, where CAHs may not furnish this type of service.
Do not include on this worksheet items not claimed in the cost report because they conflict with the regulations, manuals, or instructions but which you wish nevertheless to claim and contest. Enter amounts on the appropriate settlement worksheet (Worksheet E, Part A, line 75; Worksheet E, Part B, line 44; Worksheet E-2, line 23; and Worksheet E-3, Parts I, II, III, IV, V, VI, and VII, lines 22, 35, 36, 26, 34, 19, and 43, respectively). For provider based-facilities enter the protested amounts on line 35 of Worksheet H-4, Part II for home health agencies; line 30 of Worksheet J-3 for CMHCs; and line 30 of Worksheet M-3 for RHC/FQHC providers.
If the cost elements of a cost center are separately maintained on your books, maintain a reconciliation of the costs per the accounting books and records to those on this worksheet. This reconciliation is subject to review by your contractor.
Standard (i.e., preprinted) CMS line numbers and cost center descriptions cannot be changed. If you need to use additional or different cost center descriptions, add (subscript) additional lines to the cost report. Where an added cost center description bears a logical relationship to a standard line description, the added label must be inserted immediately after the related standard line. The added line is identified as a numeric subscript of the immediately preceding line. For example, if two lines are added between lines 7 and 8, identify them as lines 7.01 and 7.02. If additional lines are added for general service cost centers, add corresponding columns for cost finding.
Also, submit the working trial balance of the facility with the cost report. A working trial balance is a listing of the balances of the accounts in the general ledger to which adjustments are appended in supplementary columns and is used as a basic summary for financial statements.
Do not use lines 24 through 29, 47 through 49, 77 through 87, 102 through 104, 119 through 189, and 195 through 199.
Rev. 40-81
4013 (Cont.) FORM CMS-2552-10 DRAFT
Cost center coding is a methodology for standardizing the meaning of cost center labels as used by health care providers on the Medicare cost reports. Form CMS-2552-10 provides for preprinted cost center descriptions on Worksheet A. In addition, a space is provided for a cost center code. The preprinted cost center labels are automatically coded by CMS approved cost reporting software. These cost center descriptions are hereafter referred to as the standard cost centers. Additionally, nonstandard cost center descriptions have been identified through analysis of frequently used labels.
The use of this coding methodology allows providers to continue to use labels for cost centers that have meaning within the individual institution. The five digit cost center codes that are associated with each provider label in their electronic file provide standardized meaning for data analysis. You are required to compare any added or changed label to the descriptions offered on the standard or nonstandard cost center tables. A description of cost center coding and the table of cost center codes are in §4095, Table 5.
Columns 1, 2, and 3--The expenses listed in these columns must be the same as listed in your accounting books and records and/or trial balance.
List on the appropriate lines in columns 1, 2, and 3, the total expenses incurred during the cost reporting period. These expenses are detailed between salaries (column 1) and other than salaries (column 2).
Include in column 1 only direct salaries and wages plus related salary amounts for paid vacation, holiday, sick, other paid-time-off (PTO), severance, and bonus pay. Refer to the instructions at Worksheet S-3, Part II, column 2, line 1, for the definition of bonus pay and PTO salary cost.
NOTE: Paid vacation, holiday, sick, other PTO, severance, and bonus pay must be reported with related direct salaries or wages in column 1. Do not report wage-related costs in column 1, as defined in §4005.4.
The sum of columns 1 and 2 equals the sum of column 3. Record any needed reclassifications and/or adjustments in columns 4 and 6, as appropriate.
Column 4--With the exception of the reclassification of capital-related costs which are reclassified via Worksheet A-7, all reclassifications in this column are made via Worksheet A-6. Worksheet A-6 need not be completed by all providers and is completed only to the extent that the reclassifications are needed and appropriate in the particular circumstance. Show reductions to expenses as negative numbers.
The net total of the entries in column 4 must equal zero on line 200.
Column 5--Adjust the amounts entered in column 3 by the amounts in column 4 (increase or decrease) and extend the net balances to column 5. Column 5, line 200, must equal column 3, line 200.
Column 6--Enter on the appropriate lines in column 6 the amounts of any adjustments to expenses indicated on Worksheet A-8, column 2. The total on Worksheet A, column 6, line 200, equals Worksheet A-8, column 2, line 50.
Column 7--Adjust the amounts in column 5 by the amounts in column 6 (increase or decrease), and extend the net balances to column 7.
Transfer the amounts in column 7 to the appropriate lines on Worksheet B, Part I, column 0.
40-82 Rev.
DRAFT FORM CMS-2552-10 4013 (Cont.)
Line Descriptions
The trial balance of expenses is broken down into general service, inpatient routine service, ancillary service, outpatient service, other reimbursable, special purpose, and nonreimbursable cost center categories to facilitate the transfer of costs to the various worksheets. The line numbers on Worksheet A are used on subsequent worksheets, for example, the categories of ancillary service cost centers, outpatient service cost centers, and other reimbursable cost centers appear on Worksheet C, Part I, using the same line numbers as on Worksheet A.
NOTE: The category titles do not have line numbers. Only cost centers, data items, and totals have line numbers.
Lines 1 through 23--These lines are for the general service cost centers. These costs are expenses incurred in operating the facility as a whole that are not directly associated with furnishing patient care such as, but not limited to mortgage, rent, plant operations, administrative salaries, utilities, telephone charges, computer hardware and software costs, etcetera. General service cost centers furnish services to both general service areas and to other cost centers in the provider.
Lines 1 and 2--The capital cost centers on lines 1 and 2 include depreciation, leases and rentals for the use of facilities and/or equipment, and interest incurred in acquiring land or depreciable assets used for patient care.
NOTE: Do not include in these cost centers costs incurred for the repair or maintenance of equipment or facilities; amounts specifically included in rentals or lease payments for repair and/or maintenance agreements; interest expense incurred to borrow working capital or for any purpose other than the acquisition of land or depreciable assets used for patient care; general liability insurance or any other form of insurance to provide protection other than the replacement of depreciable assets; or taxes other than those assessed on the basis of some valuation of land or depreciable assets used for patient care. However, if no amount of the lease payment is identified in the lease agreement for maintenance, you are not required to carve out a portion of the lease payment to represent the maintenance portion. Thus, the entire lease payment is considered a capital-related cost subject to the provisions of 42 CFR 413.130(b).
 When
you are dealing with a related organization, you are essentially
dealing with yourself and Medicare considers the costs to you equal
to the cost to the related organization. Therefore, for costs
applicable to services, facilities, and supplies furnished by
organizations related by common ownership or control (see 42 CFR
413.17 and CMS Pub.
15-1, chapter 10), the reimbursable cost includes the costs for these
items at the cost to the supplying organization unless the exception
provided in 42 CFR 413.17(d) and CMS Pub. 15-1, chapter
10, §1010,
is applicable, not to exceed the price of comparable services,
facilities, or supplies that could be purchased elsewhere in the open
market.
When
you are dealing with a related organization, you are essentially
dealing with yourself and Medicare considers the costs to you equal
to the cost to the related organization. Therefore, for costs
applicable to services, facilities, and supplies furnished by
organizations related by common ownership or control (see 42 CFR
413.17 and CMS Pub.
15-1, chapter 10), the reimbursable cost includes the costs for these
items at the cost to the supplying organization unless the exception
provided in 42 CFR 413.17(d) and CMS Pub. 15-1, chapter
10, §1010,
is applicable, not to exceed the price of comparable services,
facilities, or supplies that could be purchased elsewhere in the open
market.
Rev. |
40-83 |
4013 (Cont.) FORM CMS-2552-10 DRAFT
The policy of cost incurred from related organizations applies to capital-related and non-capital‑related costs. If you include costs incurred by a related organization on your cost report, the nature of the costs (e.g., capital-related or operating costs) do not change. Treat capital-related costs incurred by the related organization as capital-related costs to you.
 If
the price of comparable services, facilities, or supplies that could
be purchased elsewhere in the open market is lower than the cost to
the supplying related organization; if the exception in CFR 413.17(d)
and CMS Pub. 15-1, chapter 10, §1010,
applies; or if the supplying organization is not related to you, then
no part of the charge to you is a capital-related
cost unless the services, facilities, or supplies are capital-related
in nature.
If
the price of comparable services, facilities, or supplies that could
be purchased elsewhere in the open market is lower than the cost to
the supplying related organization; if the exception in CFR 413.17(d)
and CMS Pub. 15-1, chapter 10, §1010,
applies; or if the supplying organization is not related to you, then
no part of the charge to you is a capital-related
cost unless the services, facilities, or supplies are capital-related
in nature.
In the case of leased equipment, the fact that the lease or rental is for a depreciable asset is sufficient for consideration as a capital-related item, but a distinction must be made between the lease of equipment and the purchase of services. A lease of equipment is considered a capital‑related cost while a purchase of service is considered an operating cost. Generally, for the agreement to be considered a lease or rental (and therefore a capital-related cost), the agreement must convey to the provider the possession, use, and enjoyment of the asset. Each agreement must be examined on its own merits. Factors that would weigh in favor of treating a particular agreement as a lease of equipment include the following:
The equipment is operated by personnel employed by the provider or an organization related to the provider within the meaning of CMS Pub. 15-1, chapter 10.
The physicians who perform the services with or interpret the tests from the equipment are associated with the provider.
The agreement is memorialized in one document rather than in two or more documents (e.g., one titled a "Lease Agreement" and one titled a "Service Agreement").
The document memorializing the agreement is titled a “lease agreement.” If one or more of the documents memorializing the agreement are titled “Service Agreements,” this indicates a purchase of services.
The provider holds the certificate of need (CON) for the services furnished with the equipment.

The basis for determining the lease payment is units of time and is not volume sensitive (e.g., numbers of scans).
The provider attends to such matters as utilization review, quality assurance, and risk management for the services involving the equipment.
The provider schedules the patients for services involving the equipment.
The provider furnishes any supplies required to be used with the equipment.
 The
provider’s access to the equipment is not subject to
interruption without notice or interruption on very short notice.
The
provider’s access to the equipment is not subject to
interruption without notice or interruption on very short notice.
If the supplying organization is not related to you (see 42 CFR 413.17), no part of the charge to you is a capital-related cost unless the services, facilities, or supplies are capital-related in nature.
40-84 Rev.
DRAFT FORM CMS-2552-10 4013 (Cont.)
 Under
certain circumstances, costs associated with minor equipment are
considered capital-related costs. See CMS Pub. 15-1, chapter
1, §106,
for three methods of writing off the cost of minor equipment.
Amounts treated as expenses under method (a) are not capital-related
costs because they are treated as operating expenses. Amounts
included in expense under method (b) are capital-related costs
because such amounts represent the amortization of the cost of
tangible assets over a projected useful life. Amounts determined
under method (c) are capital-related costs because method (c) is a
method of depreciation.
Under
certain circumstances, costs associated with minor equipment are
considered capital-related costs. See CMS Pub. 15-1, chapter
1, §106,
for three methods of writing off the cost of minor equipment.
Amounts treated as expenses under method (a) are not capital-related
costs because they are treated as operating expenses. Amounts
included in expense under method (b) are capital-related costs
because such amounts represent the amortization of the cost of
tangible assets over a projected useful life. Amounts determined
under method (c) are capital-related costs because method (c) is a
method of depreciation.
 Section
1886(g) of the Act, as implemented by 42 CFR, Part 412, Subpart M,
requires that the reasonable cost-based payment methodology for
hospital inpatient capital-related costs be replaced with an
inpatient prospective payment methodology for hospitals paid under
IPPS, effective for cost reporting periods beginning on or after
October 1, 1991. Hospitals and hospital distinct part units (IPFs,
IRFs, and LTCH) excluded from IPPS pursuant to 42 CFR, Part 412,
Subpart B, are paid for capital-related costs under their respective
PPS payment systems. Also, CAHs are reimbursed on a reasonable cost
basis under 42 CFR 413.70.
Section
1886(g) of the Act, as implemented by 42 CFR, Part 412, Subpart M,
requires that the reasonable cost-based payment methodology for
hospital inpatient capital-related costs be replaced with an
inpatient prospective payment methodology for hospitals paid under
IPPS, effective for cost reporting periods beginning on or after
October 1, 1991. Hospitals and hospital distinct part units (IPFs,
IRFs, and LTCH) excluded from IPPS pursuant to 42 CFR, Part 412,
Subpart B, are paid for capital-related costs under their respective
PPS payment systems. Also, CAHs are reimbursed on a reasonable cost
basis under 42 CFR 413.70.
Lines 1 and 2--Capital costs are defined as all allowable capital-related costs for land and depreciable assets, with additional recognition of costs for capital-related items and services that are legally obligated by an enforceable contract (See CMS Pub. 15-1, chapter 28, §2800.) Betterment or improvement costs related to capital are included in capital assets. (See 42 CFR 412.302.) Capital costs incurred as a result of extraordinary circumstances are included in capital. (See 42 CFR 412.348(g).) Direct assignment of capital costs must be done in accordance with CMS Pub. 15-1, chapter 23, §§2307 and 2313.
Capital costs include the following:
 1. Allowable
depreciation on assets based on the useful life guidelines used to
determine depreciation expense in the hospital’s base period,
which cannot be subsequently changed.
1. Allowable
depreciation on assets based on the useful life guidelines used to
determine depreciation expense in the hospital’s base period,
which cannot be subsequently changed.
2. Allowable capital-related interest expense. Except as provided in subsections a through c below, the amount of allowable capital-related interest expense recognized as capital is limited to the amount the hospital was legally obligated to pay.
a. An increase in interest expense is recognized if the increase is due to periodic fluctuations of rates in variable interest rate loans or to periodic fluctuations of rates at the time of conversion from a variable rate loan to a fixed rate loan when no other changes in the terms of the loan are made.
b. If the terms of a debt instrument are revised, the amount of interest recognized associated with the original capital cannot exceed the amount that would have been recognized during the same period prior to the revision of the debt instrument.
 c. Investment
income (excluding income from funded depreciation accounts and other
exclusions from investment income offset cited in CMS Pub. 15-1,
chapter 2, §202.2)
is used to reduce capital interest expense based in each cost
reporting period.
c. Investment
income (excluding income from funded depreciation accounts and other
exclusions from investment income offset cited in CMS Pub. 15-1,
chapter 2, §202.2)
is used to reduce capital interest expense based in each cost
reporting period.
Rev. 40-85
4013 (Cont.) FORM CMS-2552-10 DRAFT
3. Allowable capital-related lease and rental costs for land and depreciable assets.
a. The cost of lease renewals and the acquisition of assets continuously leased (e.g., capitalized leases) are recognized provided that the same asset remains in use, the asset has a useful life of at least 3 years, and the annual lease payment is $1000 or more for each item or service.
b. If a hospital-owned asset is sold or given to another party and that same asset is then leased back by the hospital, the amount of allowable capital-related costs recognized as capital costs is limited to the amount allowed for that asset in the last cost reporting period during which it was owned by the hospital.
4. The appropriate portion of the capital-related costs of related organizations under 42 CFR 413.17 that would be recognized as capital costs if these costs had been incurred directly by the hospital.
 Unless
there is a change of ownership, the hospital must continue the same
cost finding methods for capital costs. This includes its practices
for the direct assignment of capital-related costs and its cost
allocation bases in. If there is a change of ownership, the new
owners may request that the contractor approve a change in order to
be consistent with their established cost finding practices.
Unless
there is a change of ownership, the hospital must continue the same
cost finding methods for capital costs. This includes its practices
for the direct assignment of capital-related costs and its cost
allocation bases in. If there is a change of ownership, the new
owners may request that the contractor approve a change in order to
be consistent with their established cost finding practices.
If a hospital desires to change its cost finding method for the direct assignment of capital costs, the request for change must be made in writing to the contractor prior to the beginning of the cost reporting period for which the change is to apply. The request must include justification as to why the change will result in more accurate and more appropriate cost finding. The contractor does not approve the change unless it determines that there is reasonable justification for the change.
Line 3--In accordance with 42 CFR 412.302(b)(4), enter all other capital-related costs, including but not limited to taxes, insurance, and license and royalty fees on depreciable assets. This line also includes any directly allocated home office other capital cost. After reclassifications in column 4 and adjustments in column 6, the balance in column 7 must equal zero. This line cannot be subscripted.
PPS providers paid 100 percent Federal complete line 3, column 2 and Worksheet A-7, Parts I (if applicable), II, and III.
40-86 Rev.
DRAFT FORM CMS-2552-10 4013 (Cont.)
Line 4--Enter in column 1, the direct salaries and salary amounts for paid vacation, holiday, sick, other paid-time-off (PTO), severance, and bonus pay incurred only for employees in the employee benefits department and/or the human resources department. In accordance with CMS Pub. 15-1, chapter 23, §2307, if your accounting system directly allocates employee benefits to individual cost centers, enter in column 2 the employee benefits cost of employees in the employee benefits and/or human resources department. If your accounting system does not directly allocate all or a portion of the employee benefits to all the individual cost centers, then enter in column 2 the total employee benefits cost and/or residual employee benefits costs of all hospital employees.
Line 5--Enter A&G costs on this line. A&G includes a wide variety of provider administrative costs such as but not limited to cost of executive staff, legal and accounting services, facility administrative services (not already included in other general service cost centers), etcetera. If this line is componentized into more than one cost center, eliminate line 5. Componentized A&G lines must begin with subscripted line 5.01 and continue in sequential and consecutive order except where this manual specifies otherwise.
Line 6--Maintenance and repairs are any activity to maintain the facility and grounds such as, but not limited to, costs of routine painting, plumbing and electrical repairs, mowing and snow removal.
Line 7--Operation of plant includes the cost such as, but not limited to, the internal hospital environment including air conditioning (both heating and cooling systems and ventilation) and other mechanical systems.
Line 8--Laundry and linen services includes the cost of routine laundry and linen services whether performed in-house or by outside contractors.
Line 9--Housekeeping includes the cost of routine housekeeping activities such as mopping, vacuuming, cleaning restrooms, lobbies, waiting areas and otherwise maintaining patient and non-patient care areas.
Line 10--Dietary includes the cost of preparing meals for patients.
Line 11--Cafeteria includes the cost of preparing food for provider personnel, physicians working at the provider, visitors to the provider.
Line 12--Maintenance of personnel includes the cost of room and board furnished to employees. (See CMS Pub. 15-1, chapter 7, §704.3.)
Line 13--Nursing administration normally includes only the cost of nursing administration. The salary cost of direct nursing services, including the salary cost of nurses who render direct service in more than one patient care area, is directly assigned to the various patient care cost centers in which the services were rendered. Direct nursing services include gross salaries and wages of head nurses, registered nurses, licensed practical and vocational nurses, aides, orderlies, and ward clerks.
However, if your accounting system fails to specifically identify all direct nursing services to the applicable patient care cost centers, then the salary cost of all direct nursing service is included in this cost center.
Line 14--Central services and supply includes the costs of supplies and services which are requested by departments throughout the provider, including medical supplies charged to patients.
Rev. 40-87
4013 (Cont.) FORM CMS-2552-10 DRAFT
Line 15--Pharmacy includes the cost of drugs and pharmacy supplies requested by patient care departments and drugs charged to patients.
Line 16--Medical records and medical records library includes the direct costs of the medical records cost center including the medical records library. The general library and the medical library are not included in this cost center but are reported in the A&G cost center.
Line 17--Social service includes the cost of explaining health care resources and policies to patients, family and professional staff; assistance in planning for post-hospital patient needs; assisting patients and families receive needed follow-up care by referral to health care resources and providing advocacy through appropriate organizations.
Line 19--The services of a nonphysician anesthetist generally are paid for by the Part B contractor based on a fee schedule rather than on reasonable cost basis through the cost report. As such, the salary and fringe benefit costs included on line 19 generally are not reimbursed through the cost report.
NOTE: Any costs are included on this line are limited to salary and employee benefit costs.
However, payment for the nonphysician anesthetists on a fee basis may not apply to a qualified rural hospital or CAH if the facility employed or contracted with not more than one FTE (2080 hours) nonphysician anesthetist and, if (1) the hospital had 800 or fewer surgical procedures (including inpatient and outpatient procedures) requiring anesthesia services, and (2) each nonphysician employed by or under contract with the hospital has agreed not to bill under Part B of title XVIII for professional services furnished. 42 CFR 412.113(c)(2)(i)
Payment under the fee schedule applies to qualified hospitals and CAHs unless the hospital establishes, before the beginning of each calendar year, that it did not exceed 800 surgical procedures requiring anesthesia in the previous year. 42 CFR 412.113(c)(2)(ii)
Hospitals which do not qualify for the exception and are therefore subject to the fee schedule payment method must remove the salary and fringe benefit costs from line 19. The total amount is reported on Worksheet A-8, line 28 and in column 6, line 19, of this worksheet. This removes these costs from the cost reported in column 7.
40-88 Rev.
DRAFT FORM CMS-2552-10 4013 (Cont.)
Lines 20 and 23--If you operate an approved nursing or allied health education program that meets the criteria of 42 CFR 413.85 and 412.113(b), both classroom and clinical portions of the costs are allowable as pass-through costs as defined in 42 CFR 413.85.
Classroom costs are those costs associated with formal, didactic instruction on a specific topic or subject in a classroom that meets at regular, scheduled intervals over a specific time period (e.g., semester or quarter) and for which a student receives a grade.
Clinical training is defined as involving the acquisition and use of the skills of a nursing or allied health profession or trade in the actual environment in which these skills will be used by the student upon graduation. While it may involve occasional or periodic meetings to discuss or analyze cases, critique performance, or discuss specific skills or techniques, it involves no classroom instruction.
If you do not operate the program, the classroom portion of the costs is not allowable as a pass- through cost and therefore not reported on lines 20 and 23 of the Form CMS-2552-10. This cost may, however, be allowable as routine service operating cost. (See CMS Pub. 15-1, chapter 4, §404.2.) The clinical portions of these costs are allowable as pass-through costs if the following conditions as set forth in 42 CFR 413.85 are met:
1. The hospital must have claimed and have been paid for clinical costs (described above) during its latest cost reporting period that ended on or before October 1, 1989.
2. The proportion of the hospital’s total allowable costs that is attributable to the clinical training costs of the approved program and allowable under 42 CFR 413.85 during a cost reporting period does not exceed the proportion of total allowable costs that were attributable to the clinical training costs during the hospital’s most recent cost reporting period ending on or before October 1, 1989.
3. The hospital receives a benefit for the support it furnishes to the education program through the provision of clinical services by nursing and allied health students participating in the program.
4. The clinical training costs must be incurred by the provider or by an educational institution related to the provider by common ownership or control as defined by 42 CFR 413.17(b) and CMS Pub. 15-1, chapter 10, §1002 (cost to related organizations). Costs incurred by a third party, regardless of its relationship to either the provider or the educational institution, are not allowed.
5. The costs incurred by the hospital for the program do not exceed the costs that would have been incurred by the hospital if the program had been operated by the hospital.
6. The clinical training must occur on the premises of the hospital; i.e., in the hospital itself or in the physical area immediately adjacent to the hospital buildings or in other areas and structures located within 250 yards of the main buildings.
Rev. 40-89
4013 (Cont.) FORM CMS-2552-10 DRAFT
Line 20--Enter the cost for the nursing school.
Line 21--Enter the cost of intern and resident salaries and salary-related fringe benefits. Do not include salary and salary-related fringe benefits applicable to teaching physicians which are included in line 22.
Line 22--Enter the other costs applicable to interns and residents in an approved teaching program.
Line 23--For this line establish a separate cost center for each paramedical education program (e.g., one for medical records or hospital administration). If additional lines are needed, subscript line 23 consecutively and sequentially. If the direct costs are included in the costs of an ancillary cost center, reclassify them on Worksheet A-6 to line 23. Appropriate statistics are required on Worksheet B-1 to ensure that overhead expenses are properly allocated to this cost center. Identify all other medical education costs on line 23.99. These costs, if present and applicable, may be used on Worksheet D, Parts III and IV.
Lines 24 through 29--Reserved for future use.
Lines 30 through 46--These lines are for the inpatient routine service cost centers.
Line 30--The purpose of this cost center is to accumulate the incurred routine service cost applicable to adults and pediatrics (general routine care) in a hospital. Do not include incurred costs applicable to subproviders or any other cost centers which are treated separately.
Lines 31 through 35--Use lines 31 through 35 to record the cost applicable to intensive care type inpatient hospital units. (See 42 CFR 413.53(b) and (d) and CMS Pub. 15-1, chapter 22, §2202.7.) Label line 35 appropriately to indicate the purpose for which it is being used.
Lines 36 through 39--Reserved for future use.
Line 40--Use this line to record the IPF service costs of a subprovider. Hospital units that are excluded units from IPPS are treated as subproviders for cost reporting purposes.
Line 41--Use this line to record the IRF service costs of a subprovider. Hospital units that are excluded units from IPPS are treated as subproviders for cost reporting purposes.
Line 42--Use this line to record the inpatient routine service costs of other subproviders as applicable.
Line 43--Use this line to record the costs associated with the nursery.
Line 44--Use this line to record the costs of SNFs certified for titles V, XVIII, or XIX if your State accepts one level of care.
Line 45--Use this line to record the cost of NFs certified for title V or title XIX but not certified as an SNF for title XVIII. Subscript this line to record the cost of ICF/IID. Do not report nursing facility costs on this subscripted line.
40-90 Rev.
DRAFT FORM CMS-2552-10 4013 (Cont.)
Line 46--Use this cost center to accumulate the direct costs incurred in maintaining long term care services not specifically required to be included in other cost centers. A long term care unit refers to a unit where the average length of stay for all patients is greater than 25 days. The beds in this unit are not certified for title XVIII.
Lines 47 through 49--Reserved for future use.
Lines 50 through 76--Use for ancillary service cost centers.
Line 57--Use this line to record direct costs associated with computed tomography (CT) services.
Line 58--Use this line to record direct costs associated with magnetic resonance imaging (MRI) services.
Line 59--Use this line to record direct costs associated with cardiac catheterization services.
Line 60--Use this line to record direct costs associated with laboratory services.
Line 61--Use this line to record costs when a pathologist continues to bill non-program patients for clinical laboratory tests and is compensated by you for services related to such tests for program beneficiaries. When you pay the pathologist an amount for administrative and supervisory duties for the clinical laboratory for program beneficiaries only, include the cost in this cost center.
NOTE: No overhead expenses are allocated to this cost center since it relates to services for program beneficiaries only. The cost reporting treatment is similar to that of services furnished under arrangement to program beneficiaries only. (See CMS Pub. 15-1, chapter 23, §2314.) These costs are apportioned among the various programs on the basis of program charges for provider clinical laboratory tests for all programs for which you reimburse the pathologist.
Line 62--Include the direct expenses incurred in obtaining blood directly from donors as well as obtaining whole blood and packed red blood cells from suppliers. Do not include in this cost center the processing fee charged by suppliers. The processing charge is included in the blood storing, processing, and transfusion cost center. Identify this line with the appropriate cost center code (06250) (Table 5 - Electronic Reporting Specifications) for the cost of administering blood clotting factors to hemophiliacs. (See §4452 of BBA 1997, OBRA 1989 & 1993.)
Line 63--Include the direct expenses incurred for processing, storing, and transfusing whole blood, packed red blood cells, and blood derivatives. Also include the processing fee charged by suppliers.
Rev. 40-91
4013 (Cont.) FORM CMS-2552-10 DRAFT
Line 71--Include on this line medical supplies charged to patients other than the high cost implantable devices reported on line 72. Obtain the expense amounts from your records as follows depending on how you accumulate these expenses in your general ledger (GL). (1) If the expenses for chargeable medical supplies are accumulated together with non-chargeable medical supplies in the “Central Services” GL account and are reported in that cost center (line 14 on Worksheet A), do not include the chargeable medical supplies expenses on Worksheet A, line 71. Rather, allocate the costs in column 14 of Worksheet B to line 71 (and other lines) using the recommended “costed requisitions” statistics. (2) If the expenses for chargeable medical supplies are reported in a separate GL account, include these expenses on Worksheet A, line 71, column 2. (3) If the expenses for chargeable medical supplies are reported in a specific subaccount(s) under the GL accounts for various routine and ancillary departments (i.e., operating room, adults and pediatrics, or clinic), report the sum of the balances in that subaccount(s) on Worksheet A, line 71, column 2. If you reported the total balance (i.e., including the amounts for chargeable medical supplies) of the various GL accounts (i.e., operating room, adults and pediatrics, or clinic), in those respective cost centers in column 2 of Worksheet A, reclassify the cost of the chargeable medical supplies from those cost centers to the “medical supplies charged to patients” cost center (line 71). (See CMS Pub. 15-1, chapter 23, §2308.2, and 42 CFR 413.53(a)(1).)
Line 72--Include on this line high cost implantable devices charged to patients bearing the revenue codes established by the NUBC as indicated in the 73 FR 48462 (August 19, 2008), and not reported on line 71. Obtain the expense amounts from your records as follows depending on how you accumulate these expenses in your general ledger (GL). (1) If the expenses for chargeable implantable devices are accumulated together with non-chargeable implantable devices in the “Central Services” GL account and are reported in that cost center (line 14 on Worksheet A), do not include the high cost chargeable implantable devices expenses on Worksheet A, line 72. Rather, allocate the costs in column 14 of Worksheet B to line 72 (and other lines) using the recommended “costed requisitions” statistics. (2) If the expenses for high cost chargeable implantable devices are reported in a separate GL account, include these expenses on Worksheet A, line 72, column 2. (3) If the expenses for high cost chargeable implantable devices are reported in a specific subaccount(s) under the GL accounts for various routine and ancillary departments (i.e., operating room, adults and pediatrics, or clinic), report the sum of the balances in that subaccount(s) on Worksheet A, line 72, column 2. If you reported the total balance (i.e., including the amounts for high cost chargeable implantable devices) of the various GL accounts (i.e., operating room, adults and pediatrics, or clinic), in those respective cost centers in column 2 of Worksheet A, reclassify the cost of the high cost chargeable implantable devices from those cost centers to the “implantable devices charged to patients” cost center (line 72). (See CMS Pub. 15-1, chapter 23, §2308.2, and 42 CFR 413.53(a)(1).)
40-92 Rev.
DRAFT FORM CMS-2552-10 4013 (Cont.)
Line 74--If you furnish renal dialysis treatments, account for such costs by establishing this separate ancillary service cost center. In accumulating costs applicable to the cost center, include no other ancillary services even though they are routinely administered during the course of the dialysis treatment. However, if you physically perform a few minor routine laboratory services associated with dialysis in the renal dialysis department, such costs remain in the renal dialysis cost center. Outpatient maintenance dialysis services are reimbursed under the composite rate reimbursement system. For purposes of determining overhead attributable to ESAs, include the cost of the drug in this cost center. The drug costs will be removed on Worksheet B-2 after stepdown.
Effective for services rendered on or after January 1, 2011, ESRD services are paid under the ESRD PPS.
NOTE: ESRD physician supervisory services are not included as your costs under the composite rate reimbursement system or ESRD PPS. Supervisory services are included in the physician’s monthly capitation rate.
Line 75--Enter the cost of ASCs that are not separately certified as a distinct part but which have a separate surgical suite. Do not include the costs of the ancillary services provided to ASC patients. Include only the surgical suite costs (i.e., those used in lieu of operating or recovery rooms).
Lines 77 through 87--Reserved for future use.
Lines 88 through 93--Use these lines for outpatient service cost centers.
NOTE: For lines 88 through 90 and 93, any ancillary service billed as clinic, RHC, and FQHC services must be reclassified to the appropriate ancillary cost center, e.g., radiology-diagnostic, laboratory.
Line 88--Use this line to report the costs of hospital-based RHCs. If more than one is maintained, subscript the line. See Table 5 in §4095 for the proper cost center code for hospital‑based RHCs.
In accordance with CMS Pub. 100-04, chapter 9, §40A, compensation paid to a physician for RHC services rendered in a hospital-based RHC is cost-reimbursed. Where the physician agreement compensates for RHC services as well as non-RHC services, or services furnished in the hospital, the related compensation must be eliminated on Worksheet A-8 and billed to the Part B contractor. If not specified in the agreement, a time study must be used to allocate the physician compensation.
Line 89--Use this line to report the costs of hospital-based FQHCs. If more than one is maintained, subscript the line. See Table 5 in §4095 for the proper cost center code for FQHCs.
In accordance with CMS Pub. 100-04, chapter 9, §40, compensation paid to a physician for FQHC services rendered in a hospital-based FQHC is cost-reimbursed. Where the physician agreement compensates for FQHC services as well as non-FQHC services, or services furnished in the hospital, the related compensation must be eliminated on Worksheet A-8 and billed to the Part B contractor. If not specified in the agreement, a time study must be used to allocate the physician compensation.
Rev. 40-93
4013 (Cont.) FORM CMS-2552-10 DRAFT
Line 90--Enter the cost applicable to the clinic not included on lines 88 and 89. If you have two or more clinics which are separately costed, separately report each such clinic. Subscript this line to report each clinic. If you do not separately cost each clinic, you may combine the cost of all clinics on the clinic line.
Line 91--Enter the costs of the emergency room cost center.
Line 92--Do not use this line on this worksheet. If you have a distinct part area specifically designated for observation (e.g., where observation patients are not placed in a general acute care area bed), report this on a subscripted line 92.01.
NOTE: It is possible to have both a distinct observation bed area and a non-distinct area (for example, where your distinct part observation bed area is only staffed from 7:00 a.m. - 10:00 p.m. Patients entering your hospital needing observation bed care after 10:00 p.m. and before 7:00 a.m. are placed in a general inpatient routine care bed). If patients entering the distinct part observation bed area are charged differently than the patients placed in the general inpatient routine care bed, separate the costs into distinct observation bed costs and non-distinct observation bed costs. However, if the charge is the same for both patients, report all costs and charges as distinct part observation beds.
Line 93--Use this line to report the costs of other outpatient services not previously identified on lines 88 through 90. If more than one other service is offered, subscript the line. See Table 5 in §4095 for the proper cost center code for this line.
Lines 94 through 98 and 100--Use these lines for other reimbursable cost centers (other than HHA and CMHC).
Line 94--Use this line to accumulate the direct costs incurred for self-care home dialysis. For purposes of determining overhead attributable ESAs, include the cost of the drug in this cost center. The drug costs will be removed on Worksheet B-2 after stepdown.
A Medicare beneficiary dialyzing at home has the option to deal directly with the Medicare program and make individual arrangements for securing the necessary supplies and equipment to dialyze at home. Under this arrangement, the beneficiary is responsible for dealing directly with the various suppliers and the Medicare program to arrange for payment. The beneficiary is also responsible to the suppliers for the deductible and 20 percent Medicare coinsurance requirement. You do not receive composite rate payment for a patient who chooses this option. However, if you provide any direct home support services to a beneficiary who selects this option, you are reimbursed on the same reasonable cost basis for these services as for other outpatient services. These costs are entered on line 93 and are notated as cost reimbursed. You may service Medicare beneficiaries who elect this option and others who deal directly with you. In this case, set up two home program dialysis cost centers (using a subscript for the second cost center) to properly classify costs between the two categories of beneficiaries (those subject to cost reimbursement and those subject to the composite rate).
Effective for services rendered on or after January 1, 2011, ESRD services are paid under the ESRD PPS.
40-94 Rev.
DRAFT FORM CMS-2552-10 4013 (Cont.)

 Line
95--Report all ambulance costs on
this line for both owned and operated services and services under
arrangement. No subscripting is allowed for this line.
Line
95--Report all ambulance costs on
this line for both owned and operated services and services under
arrangement. No subscripting is allowed for this line.
Lines 96 and 97--Use these lines to report durable medical equipment rented or sold, respectively. Enter the direct expenses incurred in renting or selling durable medical equipment (DME) items to patients. Also, include all direct expenses incurred by you in requisitioning and issuing DME to patients.
For a hospital-based SNF, report support surfaces by subscripting line 97 and use the proper cost center code.
Line 99--This cost center accumulates the direct costs for outpatient rehabilitation providers (CORFs and OPTs) and CMHCs. However, only CMHCs complete the J series worksheets. Use lines 99 through 99.09 for CMHCs, 99.10 through 99.19 for CORFs, 99.20 through 99.29 for OPTs, lines 99.30 through 99.39 for OOTs, and lines 99.40 through 99.49 for OSPs. If you have multiple components, subscript this line using the proper cost center code.
Line 100--Use this line if your hospital operates an intern and resident program not approved by Medicare.
Line 101--This cost center accumulates costs specific to HHA services. If you have more than one certified hospital-based HHA, subscript line 101 for each HHA.
Hospital-based HHAs are operated and managed in a variety of ways within the context of the health care complexes of which they are components. In some instances, there are discrete management and administrative functions pertaining to the HHA, the cost of which is readily identifiable from the books and records.
In other instances, the administration and management of the hospital-based HHA is integrated with the administration and management of the health care complex to such an extent that the cost of administration and management of the home health agency can be neither identified nor derived from the books and records of the health care complex. In other instances, the cost of administration and management of the HHA is integrated with the administration and management of the health care complex, but the cost of the HHA administration and management can be derived through cost finding. However, in most cases, even when the cost of HHA administration and management can be either identified or derived, the extent to which the costs are applicable to the services furnished by the hospital-based HHA is not readily identifiable.
Even when the costs of administration and management of a provider-based HHA can be identified or derived, such costs do not generally include all of the general service costs (i.e., overhead costs) applicable to the HHA. Therefore, allocation of general service costs through cost finding is necessary for the determination of the full costs of the hospital-based HHA.
When the hospital-based HHA can identify discrete management and administrative costs from its books and records, these costs are included on line 101.
Rev. 40-95
4013 (Cont.) FORM CMS-2552-10 DRAFT
Similar situations occur for the services furnished by the hospital-based HHA. For example, in some instances, physical therapy services are furnished by a discrete HHA physical therapy department. In other instances, physical therapy services are furnished to the patient of the hospital-based HHA by an integrated physical therapy department of a hospital health care complex in such a manner that the direct costs of furnishing the physical therapy services to the patients of the hospital-based HHA cannot be readily identified or derived. In other instances, physical therapy services are furnished to patients of the hospital-based HHA by an integrated physical therapy department of a hospital health care complex in such a manner that the costs of physical therapy services furnished to patients of the hospital-based HHA can be readily identified or derived.
When you maintain a separate therapy department for the HHA apart from the hospital therapy department furnishing services to other patients of the hospital health care complex or when you are able to reclassify costs from an integrated therapy department to an HHA therapy cost center, make a reclassification entry on Worksheet A-6 to the appropriate HHA therapy cost center. Make a similar reclassification to the appropriate line for other ancillaries when the HHA costs are readily identifiable.
NOTE: This cost report provides separate HHA cost centers for all therapy services. If services are provided to HHA patients from a shared hospital ancillary cost center, make the cost allocation on Worksheet H-1, Part II.
Lines 102 through 104--Reserved for future use.
Lines 105 through 117--Use these lines for special purpose cost centers. Special purpose cost centers include kidney, heart, liver, lung, pancreas, intestinal, and islet acquisition costs as well as costs of other organ acquisitions which are nonreimbursable but which CMS requires for data purposes, cost centers which must be reclassified but which require initial identification, and ASC and hospice costs which are needed for rate setting purposes.
NOTE: Prorate shared acquisition costs (e.g., coordinator salaries, donor awareness programs) among the type of organ acquisitions. Generally, this is done based on the number of organs procured. Further, if multiple organs have been procured from a community hospital or an independent organ procurement organization, prorate the cost among the type of acquisitions involved.
These cost centers include the cost of services purchased under arrangement or billed directly to the hospital in connection with the acquisition of organs. Such direct costs include but are not limited to:
Fees for physician services (preadmission for transplant donor and recipient tissue-typing and all tissue-typing services performed on cadaveric donors);
Cost for organs acquired from other providers or organ procurement organizations;
Transportation costs of organs;
Organ recipient registration fees;
40-96 Rev.
DRAFT FORM CMS-2552-10 4013 (Cont.)
Surgeons' fees for excising cadaveric donor organs; and
Tissue-typing services furnished by independent laboratories.
NOTE: No amounts or fees paid to a donor, their estate, heirs, or assigns in exchange for an organ or for the right to remove or transplant an organ are included in organ acquisition costs. Also, such amounts or fees are not included in any other revenue producing or general service cost center.
Only hospitals which are certified transplant centers are reimbursed directly by the Medicare program for organ acquisition costs. All such costs are accumulated on Worksheet D-4.
Hospitals which are not certified transplant centers are not reimbursed by the Medicare program for organ acquisition costs. Such hospitals sell any organs excised to a certified transplant center or an organ procurement organization. The costs are accumulated in the applicable organ acquisition cost center and flow through cost finding to properly allocate overhead costs to this cost center. However, only a certified transplant center completes Worksheet D-4.
Line 105--Record any costs in connection with kidney acquisitions. This cost center flows through cost finding and accumulates any appropriate overhead costs.
Line 106--Record any costs in connection with heart acquisitions. This cost center flows through cost finding and accumulates any appropriate overhead costs.
Line 107--Record any costs in connection with liver acquisitions. This cost center flows through cost finding and accumulates any appropriate overhead costs.
Line 108--Record any costs in connection with lung acquisitions. This cost center flows through cost finding and accumulates any appropriate overhead costs.
Line 109--Record any costs in connection with pancreas acquisitions. This cost center flows through cost finding and accumulates any appropriate overhead costs.
Line 110--Record any costs in connection with intestinal acquisitions. This cost center flows through cost finding and accumulates any appropriate overhead costs.
Line 111--Record the costs associated with the acquisition of the pancreas that is used to isolate the islet cells that are used for transplant. Do not include in this cost any costs associated with the isolation of the islet cells as these costs will be included as an add-on to the DRG payment. (See CR 5505, dated March 2, 2007).
Line 112--Record any costs related to organ acquisitions, which are not already recorded on lines 105 through 111 and subscripts. This cost center flows through cost finding and accumulates any appropriate overhead costs.
Line 113--Enter all interest paid by the facility. After reclassifications in column 4 and adjustments in column 6, the balance in column 7 must equal zero. This line cannot be subscripted.
NOTE: If capital-related and working capital interest are commingled on this line, reclassify working capital interest to A&G expense. Reclassify capital-related interest to lines 1 and 2, as appropriate, in accordance with the instructions for those lines.
Rev. 40-97
4013 (Cont.) FORM CMS-2552-10 DRAFT
Line 114--Include only utilization review costs of the hospital-based SNF. All costs are either reclassified or adjusted in total depending on the scope of the review. If the scope of the review covers all patients, all allowable costs are reclassified in column 4 to A&G expenses (line 5). If the scope of the review covers only Medicare patients or Medicare, title V, and title XIX patients, then (1) in column 4, reclassify to A&G expenses all allowable costs other than physicians' compensation and (2) deduct in column 6 the compensation paid to the physicians for their personal services on the utilization review committee. The amount reported on Worksheet E-2, column 1, line 7, must equal the amount adjusted on Worksheet A-8.
Line 115--Enter the direct costs of an ASC as defined in 42 CFR 416.2. An ASC operated by a hospital must be a separately identifiable entity, physically, administratively, and financially independent and distinct from other operations of the hospital. In addition, the ASC must have an agreement with CMS as required by 42 CFR 416.25. Under this restriction, hospital outpatient departments providing ambulatory surgery (among other services) are not eligible to be classified as ASCs. Those ASCs which meet the definition in 42 CFR 416.2 and are currently treated as an outpatient cost center on the hospital’s Medicare cost report are reimbursed through a prospectively determined standard overhead amount. For cost reporting purposes, an eligible ASC is treated as a nonreimbursable cost center to ensure that overhead costs are properly allocated since the cost is not reimbursable in this cost report.
Line 116--The regulations at 42 CFR 418 provide for coverage of hospice care for terminally ill Medicare beneficiaries who elect to receive care from a participating hospice.
Line 117--Enter other special purpose cost centers not previously identified. Review Table 5 in §4095 for the proper cost center code.
Lines 119 through 189--Reserved for future use.
Lines 190 through 194--Record the costs applicable to nonreimbursable cost centers to which general service costs apply. If additional lines are needed for nonreimbursable cost centers other than those shown, subscript one or more of these lines with a numeric code. The subscripted lines must be appropriately labeled to indicate the purpose for which they are being used. However, when the expense (direct and all applicable overhead) attributable to any nonallowable cost area is so insignificant as not to warrant establishment of a nonreimbursable cost center and the sum total of all such expenses is so insignificant as not to warrant the establishment of a composite nonreimbursable cost center, these expenses are adjusted on Worksheet A-8. (See CMS Pub. 15‑1, chapter 23, §2328.)
Line 194--Establish a nonreimbursable cost center to accumulate the cost incurred by you for services related to the physicians’ private practice. Such costs include depreciation costs for the space occupied, movable equipment used by the physicians’ offices, administrative services, medical records, housekeeping, maintenance and repairs, operation of plant, drugs, medical supplies, and nursing services. Do not include costs applicable to services rendered to hospital patients by hospital-based physicians since such costs may be included in hospital costs.
Lines 195 through 199--Reserved for future use.
Line 200--Sum of lines 118 through 199.
40-98 Rev.
DRAFT FORM CMS-2552-10 4014
4014. WORKSHEET A-6 - RECLASSIFICATIONS
This worksheet provides for the reclassification of certain costs to effect proper cost allocation under cost finding. For each reclassification adjustment, assign an alpha character in column 1 to identify each reclassification entry, e.g., A, B, C. DO NOT USE NUMERIC DESIGNATIONS. All reclassification entries must have a corresponding Worksheet A line number reference in columns 3 and 7. In column 10, indicate the column of Worksheet A-7 impacted by the reclassification, where applicable. If more than one column on Worksheet A-7 is impacted by one reclassification, report each entry as a separate line to properly report each column impacted on Worksheet A-7. If you directly assign the capital-related costs, i.e., insurance, taxes, and other, reclassify these costs to line 3. Do not reclassify other capital-related costs reported or reclassified to line 3 of Worksheet A back to the other capital lines, lines 1 or 2, of Worksheet A. This is accomplished through Worksheet A-7.
Submit with the cost report copies of any workpapers used to compute the reclassifications effected on this worksheet.
Identify any reclassifications made as salary and other costs in the appropriate column. However, when transferring to Worksheet A, transfer the sum of the two columns.
NOTE: Salary amounts paid to an employee in addition to direct salaries or wages (such as paid vacation, holiday, sick, other paid-time-off (PTO), severance, and bonus pay) must be reported on Worksheet A, column 1, of the same cost center as the employees direct salaries and wages. For example, if the indirect salaries (such as paid vacation, holiday, sick, other paid-time-off (PTO), severance, and bonus pay) are reported in the “Employee Benefits” cost center or in column 2 of the cost where the related direct salary and wages are reported, a reclassification entry must be made to reclassify them to column 1 of the cost center(s) in which the related direct salaries and wages are reported.
If there is any reclassification to general service cost centers for compensation of provider-based physicians, make the appropriate adjustment for RCE limitation on Worksheet A-8-2. (See §4018.)
Examples of reclassifications that may be needed are:
Reclassification of related organization rent expenses included in the A&G cost center which are applicable to lines 1 and 2 of Worksheet A. See instructions for Worksheet A-8-1 for treatment of rental expenses for related organizations.
Reclassification of interest expense included on Worksheet A, column 3, line 113, which is applicable to funds borrowed for A&G purposes (e.g., operating expenses) or for the purchase of buildings and fixtures or movable equipment. Allocate interest on funds borrowed for operating expenses with A&G expenses.
Reclassification of employee benefits expenses (e.g., employee health service, hospitalization insurance, workers compensation, employee group insurance, social security taxes, unemployment taxes, annuity premiums, past service benefits, and pensions) included in the A&G cost center.
Reclassification of utilization review cost applicable to the hospital-based SNF to A&G costs. If the scope of the utilization review covers the entire population, reclassify the total allowable utilization review cost included on Worksheet A, column 3, line 114. However, if the scope of the utilization review in the hospital-based SNF covers only Medicare patients or Medicare and title XIX patients, only the allowable utilization review costs included on
Rev. 40-99
4014 (Cont.) FORM CMS-2552-10 DRAFT
Worksheet A, column 3, line 114 (other than the compensation of physicians for their personal services on utilization review committees), are reclassified to A&G costs.
The appropriate adjustment for physicians’ compensation is made on Worksheet A-8. For further explanations concerning utilization review in skilled nursing facilities, see CMS Pub. 15‑1, chapter 21, §2126.2.
Reclassification of any dietary cost included in the dietary cost center which is applicable to the cafeteria, nursery, and to any other cost centers such as gift, flower, coffee shops, and canteen.
Reclassification of any direct expenses included in the central service and supply cost center which are directly applicable to other cost centers such as intern-resident service, intravenous therapy, and oxygen (inhalation) therapy.
Reclassification of any direct expenses included in the laboratory cost center which are directly applicable to other cost centers such as whole blood and packed red blood cells or electrocardiology.
Reclassification of any direct expenses included in the radiology-diagnostic cost center which are directly applicable to other cost centers such as radiology-therapeutic, radioisotope, or electrocardiology.
When you purchase services (e.g., physical therapy) under arrangements for Medicare patients but do not purchase such services under arrangements for non-Medicare patients, your books reflect only the cost of the Medicare services. However, if you do not use the grossing up technique for purposes of allocating overhead and if you incur related direct costs applicable to both Medicare and non-Medicare patients (e.g., paramedics or aides who assist a physical therapist in performing physical therapy services), reclassify the related costs on Worksheet A-6 from the ancillary service cost center. Allocate them as part of A&G expense. However, when you purchase services that include performing administrative functions such as completion of medical records, training, etcetera, as described in CMS Pub. 15‑1, chapter 14, §1412.5, the overall charge includes the provision of these services. Therefore, for cost reporting purposes, these related services are NOT reclassified to A&G.
If a beneficiary receives outpatient renal dialysis for an extended period of time and you furnish a meal, the cost of this meal is not an allowable cost for Medicare. Make an adjustment on Worksheet A-8. However, the dietary counseling cost attributable to a dialysis patient is an allowable cost. Reclassify this cost from the dietary cost center, line 10, to the renal dialysis cost center, line 74.
When interns and residents are employed to replace anesthetists, you must reclassify the related direct costs from the intern and resident cost center to the anesthesiology cost center. (See 49 FR 208 (January 3, 1984).)
NOTE: These interns and residents do not qualify for the indirect medical education adjustment and must be excluded for the intern and resident FTE for that purpose. (See 42 CFR 412.113(c).)
If you incur costs for an unpaid guarantee for emergency room physician availability, attach a separate worksheet showing the computation of the necessary reclassification. (See CMS Pub. 15-1, chapter 21, §2109.)
Reclassification of the costs of malpractice insurance premiums, self-insurance fund contributions, and uninsured malpractice losses incurred either through deductible or coinsurance provisions, as a result of an award in excess of reasonable coverage limits, or as a government provider to the A&G cost center.
40-100 Rev.
DRAFT FORM CMS-2552-10 4015.1
4015. WORKSHEET A-7 - RECONCILIATION OF CAPITAL COST CENTERS
This worksheet consists of three parts:
Part I - Analysis of Changes in Capital Asset Balances.
Part II - Reconciliation of amounts from worksheet A, column 2, lines 1 and 2.
Part III - Reconciliation of Capital Cost Centers.
See the instructions for Worksheet A for a definition of capital. All providers must complete Parts I, II, and III.
NOTE: Include assets which are directly allocated to the provider from the home office or related organization and the related other capital costs in Parts I and II of this worksheet.
The intent of Worksheet A-7, Part I, is to reflect assets which relate to the hospital. However, examine the cost finding elections made at the time you submit the cost report to consider the cost finding treatment of SNF, HHA, hospice, subproviders, CORF, CMHC, the physician office building, and any other nonallowable cost centers.
Where you have elected to cost find any of these areas through the cost report, related assets must be included in Worksheet A-7, Part I, as appropriate, to properly allocate the related insurance, taxes, etcetera.
4015.1 Part I - Analysis of Changes in Capital Asset Balances.--This part enables the Medicare program to analyze the changes that occurred in your capital asset balances during the current reporting period. Complete this worksheet only once for the entire hospital complex (certified and non-certified components). However, only include in Part I assets that relate to hospital services or are commingled and cannot be separated.
Columns 1 and 6--Enter the balance recorded in your books of accounts at the beginning of your cost reporting period (column 1) and at the end of your cost reporting period (column 6). You must submit a reconciliation demonstrating that the amount reported on Part I, column 6, line 10, agrees with the total fixed assets on Worksheet G, plus any directly allocated assets from the home office or related organization, less any assets not allocated through the cost finding method on Worksheet B. Include fully depreciated assets still used for patient care.
Columns 2 through 4--Enter the cost of capital assets acquired by purchase in column 2 and the fair market value at date acquired of donated assets in column 3. Enter the sum of columns 2 and 3 in column 4.
NOTE: The amounts in Part I, column 2, must also include transfers of assets from a change of ownership.
Column 5--Enter the cost or other approved basis of all capital assets sold, retired, or disposed of in any other manner during your cost reporting period.
Column 6--Enter the sum of columns 1 and 4, minus column 5.
Column 7--Enter the initial acquisition cost of fully depreciated assets for each category. An asset that is fully depreciated and continues to be used in the facility must be recorded in this column. There will be no depreciation expense recorded after the asset is fully depreciated.
Rev. 40-101
4015.1 (Cont.) FORM CMS-2552-10 DRAFT
Line Descriptions
Line 7--If you acquired certified HIT assets and are an EHR technology meaningful user (Worksheet S-2, Part I, line 167, is yes) in accordance with ARRA 2009, section 4102, enter the corresponding amounts on this line.
Line 9--If you have included in lines 1 through 7 of Part I any of the following, enter those amounts on line 9.
Capitalized a lease in accordance with generally accepted accounting principles (GAAP) and included it in the assets reported on Worksheet G,
Excess of amounts paid for the acquisition of assets over their fair values or the amount recognized under §2314 of DEFRA for transactions after July 18, 1984, or
Construction in progress at the end of the cost reporting period.
Line 10--Enter line 8 minus line 9.
4015.2 Part II - Reconciliation of Amounts From Worksheet A, Column 2, Lines 1 and 2.--The purpose of this worksheet is to segregate and specifically identify the depreciation and capital-related costs which are directly assigned to Worksheet A, column 2, lines 1 and 2.
Columns 9 - 14--Enter in columns 9 through 14, the depreciation and other capital-related costs. (Do not report in columns 12 through 14 any amounts previously reported in Part III, columns 5 through 7). The sum of columns 9 through 14 of this part, which is reported in column 15, lines 1 and 2, must agree with the amounts reported on Worksheet A, column 2, lines 1 and 2.
4015.3 Part III - Reconciliation of Capital Cost Centers.--Use this part to allocate allowable insurance, taxes, and other capital expenditures (not including depreciation, lease, and interest expense) to the capital-related cost centers. This part also summarizes the amounts in the capital-related cost centers on Worksheet A, lines 1 and 2, column 7.
Lines 1 and 2--The allowable costs for other capital-related expenses (including but not limited to taxes, insurance, and license and royalty fees on depreciable assets) are apportioned by applying the ratio of the hospital's capital related building and fixtures and capital related movable equipment gross asset value to total asset value in each cost reporting period. These lines compute the appropriate gross asset ratios used in allocating other capital-related costs in columns 5 through 7.
Line 3--Enter the sum of lines 1 and 2. Column 4 must equal 1.000000.
Columns 1 through 4, Lines 1 and 2--Use these columns and lines to compute ratios of capital related building and fixtures and capital related movable equipment gross asset values to total gross asset values. Use these ratios on columns 5 through 7 to allocate other capital costs (insurance, taxes, and other) to the capital-related cost center lines (Worksheet A, lines 1 and 2).
Column 1--Enter on line 1 your gross asset value (asset value before accumulated depreciation) for buildings and fixtures (which also includes old land and land improvements). Enter on line 2 your gross asset value for movable equipment.
NOTE: Part III, column 1, line 3, must agree with the sum of Part I, column 6, line 8.
Column 2--Enter in column 2, line as appropriate, any amounts that you have included in column 1, lines 1 and 2, and which were reported on line 8 of Part I, as appropriate.
Column 3--Enter column 1 less column 2.
40-102 Rev.
DRAFT FORM CMS-2552-10 4015.2 (Cont.)
Column 4--Enter on lines 1 and 2 the amount in column 3, lines as applicable, divided by the amount in column 3, line 3. Round the resulting ratio to six decimal places.
Columns 5 through 7--These columns provide for the allocation of other capital-related costs (taxes, insurance, and other) to the capital-related cost center lines (Worksheet A, lines 1 and 2).
Line 3--Enter in column 5 capital expenditures relating to insurance. Enter in column 6 capital expenditures relating to State and local taxes on property and equipment. Enter in column 7 other capital expenditures (not including taxes, insurance, depreciation, lease, and interest expense). Enter in column 8, the sum of the amounts reported in columns 5 through 7.
Lines 1 and 2--Apply the ratios developed in column 4, line as applicable, to allocate the other capital costs reported in line 3.
Column 8--Line 3 must be equal to or less than the amount on Worksheet A, line 3, column 3. The amount reported becomes the reclassification entry on Worksheet A, column 4 which will zero-out the balance on line 3. If you directly assign other capital-related costs, see Part II for proper disclosure of these costs.
Columns 9 through 15--These lines summarize the amounts in the capital-related cost centers (Worksheet A, lines 1 and 2, column 7).
NOTE: The amount entered in these columns must be net of reclassifications and adjustments identified on Worksheets A-6, A-8 and A-8-1.
Column 9--Enter the amount reported in Part II above, from column 9, lines 1 and 2, adjusted by the amounts identified on Worksheets A-6, A-8 and A-8-1.
Column 10--Enter the amount reported in Part II, column 10, lines 1 and 2, relating to capital‑related lease expense, adjusted by the amounts identified on Worksheets A-6, A-8, and A-8-1. (See CMS Pub. 15-1, chapter 28, §2806.1.) Report insurance, taxes, and license and royalty fees associated with leased assets in columns 12, 13, and 14 of this worksheet, respectively.
Column 11--Enter the amount reported in Part II, column 11, lines 1 and 2, relating to capital‑related interest expense, adjusted by the amounts identified on Worksheets A-6, A-8, and A-8-1.
Column 12--Enter the amount from column 5 plus any additional amounts reported in Part II, column 12 adjusted by amounts identified on Worksheets A-6, A-8, and A-8-1.
Column 13--Enter the amount from column 6 plus any additional amounts reported in Part II, column 13 adjusted by amounts identified on Worksheets A-6, A-8, and A-8-1.
Column 14--Enter the amount from column 7 plus any additional amounts reported in Part II, column 14 adjusted by amounts identified on Worksheets A-6, A-8, and A-8-1.
Column 15--Enter the sum of columns 9 through 14. The amounts from column 15, lines 1 and 2, must equal the amounts on Worksheet A, column 7, lines 1 and 2.
Rev. 40-103
4016 FORM CMS-2552-10 DRAFT
4016. WORKSHEET A-8 - ADJUSTMENTS TO EXPENSES
In accordance with 42 CFR 413.9(c)(3), if your operating costs include amounts not related to patient care, these amounts are not reimbursable under the program. If your operating costs include amounts flowing from the provision of luxury items or services (i.e., those items or services substantially in excess of or more expensive than those generally considered necessary for the provision of needed health services), such amounts are not allowable.
This worksheet provides for the adjustments in support of those listed on Worksheet A, column 6. These adjustments, required under the Medicare principles of reimbursement, are made on the basis of cost or amount received (revenue) only if the cost (including direct cost and all applicable overhead) cannot be determined. If the total direct and indirect cost can be determined, enter the cost. Submit with the cost report a copy of any work papers used to compute a cost adjustment. Once an adjustment to an expense is made on the basis of cost, you may not determine the required adjustment to the expense on the basis of revenue in future cost reporting periods. Enter the following symbols in column 1 to indicate the basis for adjustment: "A" for cost or "B" for amount received. Line descriptions indicate the more common activities which affect allowable costs or result in costs incurred for reasons other than patient care and, thus, require adjustments.
Types of adjustments entered on this worksheet include (1) those needed to adjust expenses to reflect actual expenses incurred; (2) those items which constitute recovery of expenses through sales, charges, fees, etcetera.; (3) those items needed to adjust expenses in accordance with the Medicare principles of reimbursement; and (4) those items which are provided for separately in the cost apportionment process.
If an adjustment to an expense affects more than one cost center, record the adjustment to each cost center on a separate line on Worksheet A-8.
NOTE: When adjustments affect capital, they must be appropriately identified as impacting capital related building and fixtures or capital related movable equipment. If these adjustments affect other capital-related costs, indicate in column 5, the capital-related cost category shown on Worksheet A-7, Part III, columns 9 through 14.
Enter additional costs as positive amounts. Enter reductions of cost as a negative number. Enter a net total (if a reduction of cost) as a negative number.
Line Descriptions
Lines 1 through 3--Enter the investment income to be applied against interest expense. (See CMS Pub. 15-1, chapter 2, §202.2, for an explanation.)
Line 7--For patient telephones, make an adjustment on this line or establish a nonreimbursable cost center. When this line is used, base the adjustment on cost. Revenue is not used. (See CMS Pub. 15-1, chapter 23, §2328.)
Line 10--Enter the total provider-based physician adjustments for personal patient care services and RCE limitations. Obtain this amount from Worksheet A-8-2, column 18, sum of all lines.
NOTE: Make the adjustment to Worksheet A, column 6 for each applicable cost center from Worksheet A-8-2, column 18, line as appropriate.
Line 12--Obtain this amount from section A, column 6 of Worksheet A-8-1.
NOTE: Worksheet A-8-1 represents the detail of the various cost centers on Worksheet A which must be adjusted.
40-104 Rev.
DRAFT FORM CMS-2552-10 4016 (Cont.)
Line 21--Enter the cash received from the imposition of interest, finance, or penalty charges on overdue receivables. Use this income to offset the allowable administration and general costs. (See CMS Pub. 15-1, chapter 21, §2110.2.)
Line 22--Enter the interest expense imposed by the contractor on Medicare overpayments. Also, enter interest expense on borrowing made to repay Medicare overpayments.
Line 23--Enter, if applicable, the amount from Worksheet A-8-3, line 65.
Line 24--Enter, if applicable, the amount from Worksheet A-8-3, line 65.
Line 25--This line pertains to the hospital-based SNF only. When the utilization review covers only Medicare patients or Medicare and title XIX patients, allocate 100 percent of the reasonable compensation paid to the physicians for their services on utilization review committees to the health care programs. Apportion all other allowable costs applicable to utilization review which cover only health care program patients among all users of the hospital-based SNF. Reclassify such other costs on Worksheet A-6. Enter the physicians’ compensation for service on utilization review committees which cover only health care program patients in the hospital‑based SNF. The amount entered equals the amount shown on Worksheet A, column 6, line 114. (See CMS Pub. 15-1, chapter 21, §2126.2.) If the utilization review costs pertain to more than one program, the amount entered on Worksheet E-2, column 1, line 7, must equal the amount adjusted on Worksheet A-8.
Lines 26 and 27--When depreciation expense computed in accordance with the Medicare principles of reimbursement differs from depreciation expenses per your books, enter the difference on lines 26 and 27, as applicable. Use line 26 capital related buildings and fixtures costs and line 27 for new capital related movable equipment costs. Personal use of assets requires adjustment to depreciation expense, e.g., automotive used 50% for business and 50% personal.
Line 28--This adjustment is required for salaries and fringe benefits paid to nonphysician anesthetists reimbursed on a fee schedule. (See the instructions for Worksheet A, line 19.)
Line 29--Sections 1861(s)(2)(K), 1842(b)(6)(C), and 1842(b)(12) of the Act provide for coverage of and separate payment for services performed by a physician assistant. The physician assistant is an employee of the hospital and payment is made to the employer of the physician assistant. Make an adjustment on Worksheet A-8 for any payments made directly to the physician assistant for services rendered. This avoids any duplication of payments.
Line 30--Enter, if applicable, the amount from Worksheet A-8-3, line 65, for occupational therapy services rendered.
Line 31--Enter, if applicable, the amount from Worksheet A-8-3, line 65, for speech pathology services rendered.
Line 32--For CAHs, where applicable in accordance with ARRA of 2009, section 4102, remove the current year depreciation expense associated with purchased assets for which the total cost or remaining un-depreciated cost was reimbursed either in the current or prior cost reporting period as EHR incentive payment if such depreciation was included on Worksheet A, line 2 (capital‑related movable equipment) or any other line. This includes the depreciation expense for EHR assets purchased in the current cost reporting period, as well as depreciation expense related to the remaining net book value (i.e., un-depreciated basis) of EHR assets purchased in prior cost reporting periods which were not fully depreciated at the beginning of the current cost reporting period.
Also, use this line to remove that portion of the annual rent/lease expense applicable to EHR assets leased under a virtual purchase lease which equals the depreciation expense for this asset since the total cost of the asset (or the un-depreciated cost if the lease was initiated in a prior cost reporting period), was claimed as EHR incentive payment. Also remove any portion of the total
Rev. 40-105
4016 (Cont.) FORM CMS-2552-10 DRAFT
rental charge which exceeds the actual cost of ownership of the EHR asset. (See CMS Pub. 15‑1, chapter 1, §110.B.2.) In accordance with CMS Pub. 15-1, chapter 1, §110.B.2, the actual cost of ownership of an asset leased under a virtual purchase lease includes not only the depreciation expense, but insurance and interest as well. For example, if the depreciation for the asset is $50,000 per year, the insurance is $3,000 per year, the interest is $10,000 per year, and the rental charge is $70,000 per year, the rental expense must be limited to the cost of ownership which in this example is $63,000. Since the adjustment to limit the rent expense to the cost of ownership is $7,000, the actual adjustment on this line will be to reduce the allowable rent expense for this EHR asset by $57,000 (i.e., $50,000 depreciation portion and $7,000 excess rental charge over the cost of ownership).
Lines 33 through 49--Enter any additional adjustments which are required under the Medicare principles of reimbursement. Label the lines appropriately to indicate the nature of the required adjustments. If the number of blank lines is not sufficient, subscript lines 33 through 49. The grossing up of costs in accordance with provisions of CMS Pub. 15-1, chapter 23, §2314, is an example of an adjustment entered on these lines and is explained below.
If you furnish ancillary services to health care program patients under arrangements with others but simply arrange for such services for non-health care program patients and do not pay the non-health care program portion of such services, your books reflect only the costs of the health care program portion. Therefore, allocation of indirect costs to a cost center which includes only the cost of the health care program portion results in excessive assignment of indirect costs to the health care programs. Since services were also arranged for the non-health care program patients, allocate part of the overhead costs to those groups.
In the foregoing situation, do not allocate indirect costs to the cost center unless your contractor determines that you are able to gross up both the costs and the charges for services to non-health care program patients so that both costs and charges for services to non-health care program patients are recorded as if you had provided such services directly. See the instructions for Worksheet C, Part I, for grossing up of your charges.
Meals furnished by you to an outpatient receiving dialysis treatment also require an adjustment. These costs are nonallowable for title XVIII reimbursement. Therefore, the cost of these meals must be adjusted.
In accordance with CMS Pub. 100-04, chapter 9, §40, compensation paid to a physician for RHC services rendered in a hospital-based RHC is cost reimbursed. Where the physician agreement compensates for RHC services as well as non-RHC services, or services furnished in the hospital, the related compensation must be eliminated on Worksheet A-8 and billed to the Part B contractor. If not specified in the agreement, a time study must be used to allocate the physician compensation.
If the hospital performs ESRD services and costs are reported on either line 74, 94, or both, these costs should include the cost of all ESAs. Do not report the cost of these drugs claimed in any other cost center. These costs will be removed later on Worksheet B-2.
If the hospital pays membership dues to an organization that performs lobbying and political activities, the portion of the dues associated with these non-allowable activities must be removed from costs.
Line 30.99 (hardcoded)--When the hospital enters into a contractual arrangement with a hospice for the use of general inpatient routine beds, enter the amount received under contract from the hospice. This amount must be used to offset general inpatient routine care costs on Worksheet A, line 30.
Line 50--Enter the sum of lines 1 through 49. Transfer the amounts in column 2 to the appropriate lines on Worksheet A, column 6.
40-106 Rev.
DRAFT FORM CMS-2552-10 4017
4017. WORKSHEET A-8-1 - STATEMENT OF COSTS OF SERVICES FROM RELATED ORGANIZATIONS AND HOME OFFICE COSTS
In accordance with 42 CFR 413.17, costs applicable to services, facilities, and supplies furnished to you by organizations related to you by common ownership or control are includable in your allowable cost at the cost to the related organization, except for the exceptions outlined in 42 CFR 413.17(d). This worksheet provides for the computation of any needed adjustments to costs applicable to services, facilities, and supplies furnished to the hospital by organizations related to you or costs associated with the home office. In addition, it shows certain information concerning the related organizations with which you have transacted business as well as home office costs. (See CMS Pub. 15-1, chapter 10, and §2150, respectively.)
Part A--Cost applicable to home office costs, services, facilities, and supplies furnished to you by organizations related to you by common ownership or control are includable in your allowable cost at the cost to the related organizations. However, such cost must not exceed the amount a prudent and cost conscious buyer pays for comparable services, facilities, or supplies that are purchased elsewhere.
Columns 1, 2 and 3--In column3, enter the specific expense category from your books and/or records associated with the acquisition of services, facilities, and/or supplies from related organizations. In columns 1 and 2, enter the Worksheet A line number and the Worksheet A cost center name where the expenses were reported.
Column 4--Enter the allowable cost from the books and/or records of the related organization which includes only the actual cost incurred by the related organization for services, facilities, and/or supplies and excludes any markup, profit or amounts that otherwise exceed the acquisition cost of such items.
Column 5--Enter the amount included on Worksheet A for services, facilities, and/or supplies acquired from related organizations.
Column 6--Enter the result of column 4 minus column 5.
Column 7--Enter the specific column of Worksheet A-7, Part III, columns 9 through 14, impacted by the adjustment.
Part B--Use this part to show your relationship to organizations for which transactions were identified in Part A. Show the requested data relative to all individuals, partnerships, corporations, or other organizations having either a related interest to you, a common ownership with you, or control over you as defined in CMS Pub. 15-1, chapter 10, in columns 1 through 6, as appropriate.
Complete only those columns which are pertinent to the type of relationship which exists.
Columns 1 and 2--Enter in column 1, the appropriate symbol which describes your relationship to the related organization. If the symbol A, D, E, F, or G is entered in column 1, enter the name of the related individual in column 2.
Column 3--If the individual indicated in column 2 or the organization indicated in column 4 has a financial interest in you, enter the percent of ownership as a ratio.
Column 4--Enter the name of the related corporation, partnership, or other organization.
Column 5--If you or the individual indicated in column 2 has a financial interest in the related organizations, enter the percent of ownership in such organization as a ratio.
Column 6--Enter the type of business in which the related organization engages (e.g., medical drugs and/or supplies, laundry and linen service).
Rev. 40-107
4018 FORM CMS-2552-10 DRAFT
4018. WORKSHEET A-8-2 - PROVIDER-BASED PHYSICIAN ADJUSTMENTS
In accordance with 42 CFR 413.9, 42 CFR 415.55, 42 CFR 415.60, 42 CFR 415.70, and 42 CFR 415.102(d), you may claim as allowable cost only those costs which you incur for physician services that benefit the general patient population of the provider or which represent availability services in a hospital emergency room under specified conditions. (See 42 CFR 415.150 and 42 CFR 415.164 for an exception for teaching physicians under certain circumstances.) 42 CFR 415.70 imposes limits on the amount of physician compensation which may be recognized as a reasonable provider cost.
Worksheet A-8-2 provides for the computation of the allowable provider-based physician cost you incur. 42 CFR 415.60 provides that the physician compensation paid by you must be allocated between services to individual patients (professional services), services that benefit your patients generally (provider services), and nonreimbursable services such as research. Only provider services are reimbursable to you through the cost report. This worksheet also provides for the computation of the reasonable compensation equivalent (RCE) limits required by 42 CFR 415.70. The methodology used in this worksheet applies the RCE limit to the total physician compensation attributable to provider services reimbursable on a reasonable cost basis. Enter the total provider-based physician adjustment for personal care services and RCE limitations applicable to the compensation of provider-based physicians directly assigned to or reclassified to general service cost centers. RCE limits are not applicable to a medical director, chief of medical staff, or to the compensation of a physician employed in a capacity not requiring the services of a physician, e.g., controller. RCE limits also do not apply to critical access hospitals, however the professional component must still be removed on this worksheet. CAHs need only complete columns 1 through 5 and 18. Transfer for CAHs the amount from column 4 to column 18.
NOTE: 42 CFR 415.70(a)(2) provides that limits established under this section do not apply to costs of physician compensation attributable to furnishing inpatient hospital services paid for under the prospective payment system implemented under 42 CFR 412.
Limits established under this section apply to inpatient services subject to the TEFRA rate of increase ceiling (see 42 CFR 413.40), outpatient services for all titles, and to title XVIII, Part B inpatient services.
Since the methodology used in this worksheet applies the RCE limit in total, make the adjustment required by 42 CFR 415.70(a)(2) on Worksheet C, Part I. Base this adjustment on the RCE disallowance amounts entered in column 17 of Worksheet A-8-2.
Where several physicians work in the same department, see CMS Pub. 15-1, chapter 21, §2182.6C, for a discussion of applying the RCE limit in the aggregate for the department versus on an individual basis to each of the physicians in the department.
NOTE: The adjustments generated from this worksheet for physician compensation are limited to the cost centers on Worksheet A, lines 4 through 99, 108 through 112, and 115, and subscripts as allowed.
Column Descriptions
Columns 1 and 10--Enter the line numbers from Worksheet A for each cost center that contained compensation for physicians who are subject to RCE limits.
Columns 2 and 11--Enter the description of the cost center used on Worksheet A. When RCE limits are applied on an individual basis to each physician in a department, list each physician on successive lines directly under the cost center description line, or list the first physician on the same line as the cost center description line and then each successive line below for each additional physician in that cost center.
40-108 Rev.
DRAFT FORM CMS-2552-10 4018 (Cont.)
List each physician using an individual identifier (not the physician’s name, NPI, UPIN or social security number of the individual), but rather, Dr. A, Dr. B, …, Dr. AA, Dr. BB, etcetera. However, the identity of the physician must be made available to your contractor/contractor upon audit. When RCE limits are applied on a departmental basis, insert the word "aggregate" (instead of the physician identifiers) on the line below the cost center description.
Columns 3 through 9 and 12 through 18--When the aggregate method is used, enter the data for each of these columns on the aggregate line for each cost center. When the individual method is used, enter the data for each column on the individual physician identifier lines for each cost center.
Column 3--Enter the total physician compensation paid by you for each cost center. Physician compensation means monetary payments, fringe benefits, deferred compensation, costs of physician membership in professional societies, continuing education, malpractice, and any other items of value (excluding office space or billing and collection services) that you or other organizations furnish a physician in return for the physician's services. (See 42 CFR 415.60(a).) Include the compensation in column 3 of Worksheet A or, if necessary, through appropriate reclassifications on Worksheet A-6 or as a cost paid by a related organization through Worksheet A-8-1.
Column 4--Enter the amount of total remuneration included in column 3 applicable to the physician's services to individual patients (professional component). These services are reimbursed on a reasonable charge basis by the Part B contractor in accordance with 42 CFR 415.102(a). The written allocation agreement between you and the physician specifying how the physician spends his or her time is the basis for this computation. (See 42 CFR 415.60(f).)
Column 5--Enter the amount of the total remuneration included in column 3, for each cost center, applicable to general services to you (provider component). The written allocation agreement is the basis for this computation. (See 42 CFR 415.60(f).)
NOTE: 42 CFR 415.60(b) requires that physician compensation be allocated between physician services to patients, the provider, and nonallowable services such as research. Physicians' nonallowable services must not be included in columns 4 or 5. The instructions for column 18 insure that the compensation for nonallowable services included in column 3 is correctly eliminated on Worksheet A-8.
Column 6--Enter for each line of data, as applicable, the reasonable compensation equivalent (RCE) limit applicable to the physician's compensation included in that cost center. The amount entered is the limit applicable to the physician specialty as published in the Federal Register before any allowable adjustments. The final notice on the annual update to RCE limits published in the 50 FR 7126 (February 20, 1985) contains Table 1, Estimates of FTE Annual Average Net Compensation Levels for 1984. Updates were published in 68 FR 45459 (August 1, 2003) and 79 FR 50162 (August 22, 2014). Obtain the RCE applicable to the specialty from this table. If the physician specialty is not identified in the table, use the RCE for the total category in the table. The beginning date of the cost reporting period determines which calendar year (CY) RCE is used. Your location governs which of the three geographical categories are applicable: non-metropolitan areas, metropolitan areas less than one million, or metropolitan areas greater than one million.
Column 7--Enter for each line of data, the physician's hours allocated to provider services. For example, if a physician works 2080 hours per year and 50 percent of his/her time is spent on provider services, then enter 1040 in this column. The hours entered are the actual hours for which the physician is compensated by you for furnishing services of a general benefit to your patients. If the physician is paid for unused vacation, unused sick leave, etcetera, exclude the hours so paid from the hours entered. Time records or other documentation that supports this allocation must be available for verification by your contractor upon request. (See CMS Pub. 15-1, chapter 21, §2182.3E.)
Rev. 40-109
4018 (Cont.) FORM CMS-2552-10 DRAFT
Column 8--Enter the unadjusted RCE limit for each line of data. This amount is the product of the RCE amount entered in column 6 and the ratio of the physician’s provider component hours entered in column 7 to 2080 hours.
Column 9--Enter for each line of data five percent of the amounts entered in column 8.
Column 12--You may adjust upward, up to five percent of the computed limit (column 9), to take into consideration the actual costs of membership for physicians in professional societies and continuing education paid by you.
Enter for each line of data the actual amounts of these expenses paid by you.
Column 13--Enter for each line of data the result of multiplying column 5 by column 12, and dividing that amount by column 3.
Column 14--You may also adjust upward the computed RCE limit in column 8 to reflect the actual malpractice expense incurred by you for the services of a physician or group of physicians to your patients.
Enter for each line of data the actual amounts of these malpractice expenses paid by you.
Column 15--Enter for each line of data the result of multiplying column 5 by column 14, and dividing that amount by column 3.
Column 16--Enter for each line of data the sum of columns 8 and 15, plus the lesser of column 9 or 13.
Column 17--Compute the RCE disallowance for each cost center by subtracting the RCE limit in column 16 from your component remuneration in column 5. If the result is a negative amount, enter zero. Transfer the amounts for each cost center to Worksheet C, Part I, column 4, for all hospitals subject to PPS. (See 42 CFR 412.)
Column 18--The adjustment for each cost center entered represents the PBP elimination from costs entered on Worksheet A-8, column 2, line 10, and on Worksheet A, column 6, to each cost center affected. Compute the amount by deducting, for each cost center, the lesser of the amounts recorded in column 5 (provider component remuneration) or column 16 (adjusted RCE limit) from the total remuneration recorded in column 3.
NOTE: If you incur cost for unpaid guarantee for emergency room physician availability, attach a separate worksheet showing the computation of the necessary reclassification. (See CMS Pub. 15-1, chapter 21, §2109.)
Line Descriptions
Line 200--Enter the total of lines 1 through 11 for columns 3 through 5, 7 through 9, and 12 through 18.
40-110 Rev.
DRAFT FORM CMS-2552-10 4019.1
4019. WORKSHEET A-8-3 - REASONABLE COST DETERMINATION FOR THERAPY SERVICES FURNISHED BY OUTSIDE SUPPLIERS
This worksheet provides for the computation of any needed adjustments to costs applicable to therapy services furnished by outside suppliers in CAHs. Therapy services rendered by non‑CAH providers are either subject to fee schedule reimbursement or the corresponding PPS reimbursement. Consequently, only CAHs complete this worksheet. The information required on this worksheet provides, in the aggregate, all data for therapy services furnished by all outside suppliers in determining the reasonableness of therapy costs.
If you contract with an outside supplier for therapy services, the potential for limitation and the amount of payment you receive depend on several factors:
An initial test to determine whether these services are categorized as intermittent part time or full time services;
The location where the services are rendered, i.e., at your site or an alternate site.
Whether detailed time and mileage records are maintained by the outside supplier;
Add-ons for supervisory functions, aides, overtime, equipment and supplies; and
Contractor determinations of reasonableness of rates charged by the supplier compared with the going rates in the area.
4019.1 Part I - General Information--This part provides for furnishing certain information concerning therapy services furnished by outside suppliers.
Line 1--Enter the number of weeks that services were performed on site. Count only those weeks during which a supervisor, therapist or an assistant was on site. (See CMS Pub. 15-1, chapter 14.)
Line 2--Multiply the amount on line 1 by 15 hours per week. This calculation is used to determine whether services are full-time or intermittent part-time.
Line 3--Enter the number of days in which the supervisor or therapist (only report the therapists for respiratory therapy) was on site. Count only one day when both the supervisor and therapist were at the site during the same day.
Line 4--Enter the number of days in which the therapy assistant (PT, OT, or SP only) was on site. Do not include days when either the supervisor or therapist was also at the site during the same day.
NOTE: Count an unduplicated day for each day the contractor has at least one employee on site. For example, if the contractor furnishes a supervisor, therapist and assistant on one day, count one therapist day. If the contractor provides two assistants on one day (and no supervisors or therapists), count one assistant day.
Line 5--Enter the number of unduplicated visits made by the supervisor or therapist. Count only one visit when both the supervisor and therapist were present during the same visit.
Line 6--Enter the number of unduplicated visits made by the therapy assistant. Do not include in the count the visits when either the supervisor or therapist was present during the same visit.
Line 7--Enter the standard travel expense rate applicable. (See CMS Pub. 15-1, chapter 14.)
Rev. 40-111
4019.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 8--Enter the optional travel expense rate applicable. (See CMS Pub. 15-1, chapter 14.) Use this rate only for services for which time records are available.
Line 9--Enter in the appropriate columns the total number of hours worked for each category.
Line 10--Enter in each column the appropriate adjusted hourly salary equivalency amount (AHSEA). This amount is the prevailing hourly salary rate plus the fringe benefit and expense factor described in CMS Pub. 15-1, chapter 14. This amount is determined on a periodic basis for appropriate geographical areas and is published as an exhibit at the end of CMS Pub. 15-1, chapter 14. Use the appropriate exhibit for the period of this cost report.
Enter in column 1 the supervisory AHSEA, adjusted for administrative and supervisory responsibilities. Determine this amount in accordance with the provisions of CMS Pub. 15-1, chapter 14, §1412.5. Enter in columns 2, 3, and 4 (for therapists, assistants, aides, and trainees respectively), the AHSEA from either the appropriate exhibit found in CMS Pub. 15-1, chapter 14 or from the latest publication of rates. If the going hourly rate for assistants in the area is unobtainable, use no more than 75 percent of the therapist AHSEA. The cost of services of a therapy aide or trainee is evaluated at the hourly rate, not to exceed the hourly rate paid to your employees of comparable classification and/or qualification, e.g., nurses' aides. (See CMS Pub. 15-1, chapter 14, §1412.2.)
Line 11--Enter the standard travel allowance equal to one half of the AHSEA. Enter in columns 1 and 2, one half of the amount in column 2, line 10. Enter in column 3, one half of the amount in column 3, line 10. (See CMS Pub. 15-1, chapter 14, §1402.4.)
Lines 12 and 13--Enter the number of travel hours and number of miles driven, respectively, if time records of visits are kept. (See CMS Pub. 15-1, chapter 14, §§1402.5 and 1403.1.) Subscript this line into two categories of provider site and provider offsite as necessary. For example, report line 12 - provider site and line 12.01 - provider offsite.
NOTE: There is no travel allowance for aides employed by outside suppliers.
4019.2 Part II - Salary Equivalency Computation--This part provides for the computation of the full-time or intermittent part-time salary equivalency.
When you furnish therapy services from outside suppliers to health care program patients but simply arrange for such services for non health care program patients and do not pay the non health care program portion of such services, your books reflect only the cost of the health care program portion. Where you can gross up costs and charges in accordance with provisions of CMS Pub. 15-1, chapter 23, §2314, complete Part II, lines 14 through 20, and 23, in all cases and lines 21 and 22, where appropriate. See §2810 for instructions regarding grossing up costs and charges. However, where you cannot gross up costs and charges, complete lines 14 through 20, and 23.
Line 14 - 20--To compute the total salary equivalency allowance amounts, multiply the total hours worked (line 9) by the adjusted hourly salary equivalency amount for supervisors, therapists, assistants, aides and trainees (for respiratory therapy only).
Line 17--Enter the sum of lines 14 and 15 for respiratory therapy, or sum of lines 14 through 16 for all others.
Line 20--Enter the sum of lines 17 through 19 for respiratory therapy, or sum of lines 17 and 18 for all other.
40-112 Rev.
DRAFT FORM CMS-2552-10 4019.4
Lines 21 and 22--If the sum of hours in columns 1 and 2 for respiratory therapy, or 1 through 3 for all others, line 9, is less than or equal to the product found on line 2, complete these lines. (See the exception above where you cannot gross up costs and charges, and services are provided to program patients only.)
Line 21--Enter the result of line 17 divided by the sum of columns 1 and 2, line 9, for respiratory therapy, or columns 1 through 3, line 9, for all others.
Line 22--Enter the result of line 2 times line 21.
Line 23--If there are no entries on lines 21 and 22, enter the amount on line 20. Otherwise, enter the sum of the amounts on lines 18, 19, and 22 for respiratory therapy, or lines 18 and 22 for all others.
4019.3 Part III - Standard and Optional Travel Allowance and Travel Expense Computation - Provider Site--This part provides for the computation of the standard and optional travel allowance and travel expense for services rendered on site.

 Lines
24 through
28--Complete these lines for the
computation of the standard travel allowance and standard travel
expense for therapy services performed at your site. One standard
travel allowance is recognized for each day an outside supplier
performs skilled therapy services at your site. For example, if a
contracting organization sends three therapists to you each day, only
one travel allowance is recognized per day. (See CMS Pub. 15-1,
chapter 14, §1403.1,
for a discussion of standard travel allowance and §1412.6 for a
discussion of standard travel expense.)
Lines
24 through
28--Complete these lines for the
computation of the standard travel allowance and standard travel
expense for therapy services performed at your site. One standard
travel allowance is recognized for each day an outside supplier
performs skilled therapy services at your site. For example, if a
contracting organization sends three therapists to you each day, only
one travel allowance is recognized per day. (See CMS Pub. 15-1,
chapter 14, §1403.1,
for a discussion of standard travel allowance and §1412.6 for a
discussion of standard travel expense.)
 Line
24--Include the standard travel
allowance for supervisors and therapists. This standard travel
allowance for supervisors does not take into account the additional
allowance for administrative and supervisory responsibilities. (See
CMS Pub. 15-1, chapter 14, §1402.4.)
Line
24--Include the standard travel
allowance for supervisors and therapists. This standard travel
allowance for supervisors does not take into account the additional
allowance for administrative and supervisory responsibilities. (See
CMS Pub. 15-1, chapter 14, §1402.4.)
Line 25--Include the standard travel allowance for assistants for physical therapy, occupational therapy, and speech pathology.
Line 26--Enter the amount from line 24 for respiratory therapy, or the sum of lines 24 and 25 for physical therapy, occupational therapy, or speech pathology.
Line 27--Enter the result of line 7 times line 3 for respiratory therapy, or line 7 times the sum of lines 3 and 4 for all others.
Lines 29 through 35--Complete these lines for computing the optional travel allowance and expense when proper records are maintained.
Line 31--Enter the amount on line 29 for respiratory therapy or the sum of lines 29 and 30 for all others.
Line 32--Enter the result of line 8 times the sum of columns 1 and 2, line 13 for respiratory therapy or columns 1, 2, and 3, line 13 for all other.
Lines 33 through 35--Enter an amount in one of these lines depending on the method utilized.
 4019.4 Part
IV - Standard and Optional Travel Allowance and Standard Travel
Expense Computation - Services outside Provider Site--This
part provides for the computation of the standard travel allowance,
the standard travel expense, the optional travel allowance, and the
optional travel expense. (See CMS Pub. 15-1, chapter
14, §§1402ff, 1403.1,
and 1412.6.)
4019.4 Part
IV - Standard and Optional Travel Allowance and Standard Travel
Expense Computation - Services outside Provider Site--This
part provides for the computation of the standard travel allowance,
the standard travel expense, the optional travel allowance, and the
optional travel expense. (See CMS Pub. 15-1, chapter
14, §§1402ff, 1403.1,
and 1412.6.)
Rev. 40-113
4019.4 (Cont.) FORM CMS-2552-10 DRAFT
 Lines
36 through
39--Complete these lines for the
computation of the standard travel allowance and standard travel
expense for therapy services performed in conjunction with offsite
visits. Only use these lines if you do not use the optional method
of computing travel. A standard travel allowance is recognized for
each visit to a patient’s residence. If services are furnished
to more than one patient at the same location, only one standard
travel allowance is permitted, regardless of the number of patients
treated.
Lines
36 through
39--Complete these lines for the
computation of the standard travel allowance and standard travel
expense for therapy services performed in conjunction with offsite
visits. Only use these lines if you do not use the optional method
of computing travel. A standard travel allowance is recognized for
each visit to a patient’s residence. If services are furnished
to more than one patient at the same location, only one standard
travel allowance is permitted, regardless of the number of patients
treated.
Lines 40 through 43--Complete the optional travel allowance and optional travel expense computations for physical therapy, occupational therapy, and speech pathology services in conjunction with home health services only. Compute the optional travel allowance on lines 40 through 42. Compute the optional travel expense on line 43.
 Lines
44 through
46--Choose and complete only one of
the options on lines 44 through 46. However, use lines 45 and 46
only if you maintain time records of visits. (See CMS Pub. 15-1,
chapter 14, §1402.5.)
Lines
44 through
46--Choose and complete only one of
the options on lines 44 through 46. However, use lines 45 and 46
only if you maintain time records of visits. (See CMS Pub. 15-1,
chapter 14, §1402.5.)
 4019.5 Part
V - Overtime Computation--This part
provides for the computation of an overtime allowance when an
individual employee of the outside supplier performs services for you
in excess of your standard work week. No overtime allowance is given
to a therapist who receives an additional allowance for supervisory
or administrative duties. (See CMS Pub. 15-1, chapter 14,
§1412.4.)
4019.5 Part
V - Overtime Computation--This part
provides for the computation of an overtime allowance when an
individual employee of the outside supplier performs services for you
in excess of your standard work week. No overtime allowance is given
to a therapist who receives an additional allowance for supervisory
or administrative duties. (See CMS Pub. 15-1, chapter 14,
§1412.4.)
Line 47--Enter in the appropriate columns the total overtime hours worked. Where the total hours in column 5 are either zero or, equal to or greater than 2080, the overtime computation is not applicable. Make no further entries on lines 48 through 55 (If there is a short period prorate the hours). Enter zero in each column of line 56. Enter in column 5 the sum of the hours recorded in columns 1, 3 and 4 for respiratory therapy, and columns 1 through 3 for physical therapy, speech pathology, and occupational therapy.
Line 48--Enter in the appropriate column the overtime rate (the AHSEA from line 10, column as appropriate, multiplied by 1.5).
Line 50--Enter the percentage of overtime hours by class of employee. Determine this amount by dividing each column on line 47 by the total overtime hours in column 5, line 47.
Line 51--Use this line to allocate your standard work year for one full-time employee. Enter the numbers of hours in your standard work year for one full-time employee in column 5. Multiply the standard work-year in column 5 by the percentage on line 50 and enter the result in the corresponding columns.
Line 52--Enter in columns 1 through 3 for physical therapy, speech pathology, and occupational therapy the AHSEA from Part I, line 10, columns 2 through 4, as appropriate. Enter in columns 1, 3 and 4,the AHSEA from Part I, line 10, columns 2, 4 and 5, for respiratory therapy.
Line 56--Enter in column 5, the sum of the amounts recorded in columns 1, 3, and 4, for respiratory therapy, and columns 1 through 3, for physical therapy, speech pathology, and occupational therapy.
4019.6 Part VI - Computation of Therapy Limitation and Excess Cost Adjustment--This part provides for the calculation of the adjustment to the therapy service costs in determining the reasonableness of therapy cost.
Line 58--Enter the amount reported on lines 33, 34, or 35.
Line 59--Enter the amount reported on lines 44, 45, or 46.
40-114 Rev.
DRAFT FORM CMS-2552-10 4019.6 (Cont.)
Lines 61 and 62--When the outside supplier provides the equipment and supplies used in furnishing direct services to your patients, the actual cost of the equipment and supplies incurred by the outside supplier (as specified in CMS Pub. 15-1, chapter 14, §1412.1) is considered an additional allowance in computing the limitation.
Line 64--Enter the amounts paid and/or payable to the outside suppliers for the hospital, if applicable, for therapy services rendered during the period as reported in the cost report. This includes any payments for supplies, equipment use, overtime, or any other expenses related to supplying therapy services for you. Add all subscripted lines together for purposes of calculating the amount to be entered on this line.
Line 65--Enter the excess cost over the limitation, i.e., line 64 minus line 63. If the amount is negative, enter a zero. Transfer this amount to Worksheet A-8, line 23 for respiratory therapy; line 24 for physical therapy; line 30 for occupational therapy; and line 31 for speech pathology.
Rev. 40-115
4020 FORM CMS-2552-10 DRAFT
4020. WORKSHEET B, PART I - COST ALLOCATION - GENERAL SERVICE COSTS AND WORKSHEET B-1 - COST ALLOCATION - STATISTICAL BASIS
Base cost data on an approved method of cost finding and on the accrual basis of accounting except where government institutions operate on a cash basis of accounting. (See 42 CFR 413.24(a).) Cost data based on such basis of accounting is acceptable subject to appropriate treatment of capital expenditures. Cost finding is the process of recasting the data derived from the accounts ordinarily kept by you to ascertain costs of the various types of services rendered. It is the determination of these costs by the allocation of direct costs and proration of indirect costs. The various cost finding methods recognized are outlined in 42 CFR 413.24. Worksheets B, Part I, and B-1 have been designed to accommodate the stepdown method of cost finding.
The provider can elect to change the order of allocation and/or allocation statistics, as appropriate, for the current cost reporting period if a request is received by the contractor, in writing, 90 days prior to the end of that reporting period. The contractor has 60 days to make a decision and notify the provider of that decision or the change is automatically accepted. The change must be shown to more accurately allocate the overhead or should demonstrate simplification in maintaining the changed statistics. If a change in statistics is requested, the provider must maintain both sets of statistics until an approval is made. If both sets are not maintained and the request is denied, the provider reverts back to the previously approved methodology. The provider must include with the request all supporting documentation and a thorough explanation of why the alternative approach should be used. (See CMS Pub. 15-1, chapter 23, §2313.)
Simplified Cost Allocation Methodology
As an alternative approach to the cost finding methods identified in CMS Pub. 15-1, chapter 23, §2306, the provider may request a simplified cost allocation methodology. This methodology reduces the number of statistical bases a provider maintains. It may result in reducing Medicare reimbursement. A comparison is recommended if the possible loss reimbursement is surpassed by the reduced costs of maintaining voluminous statistics. The following statistical bases must be used for purposes of allocating overhead cost centers. There can be no deviation of the prescribed statistics and it must be utilized for all the following cost centers.
Buildings and Fixtures Square Footage
Movable Equipment Square Footage
Maintenance and Repairs Square Footage
Operation of Plant Square Footage
Housekeeping Square Footage
Employee Benefits Salaries
Cafeteria* Salaries
Administrative and General Accumulated Costs
Laundry and Linen Patient Days
Dietary** Patient Days
Social Service Patient Days
Maintenance of Personnel Eliminated and moved to A&G for simplified cost finding
Nursing Administration Nursing Salaries
Central Services and Supply Costed Requisitions
Pharmacy Costed Requisitions
Medical Records and Library Gross Patient Revenue
Nursing School* Assigned Time
Interns and Residents Assigned Time
Paramedical Education Assigned Time
Nonphysician Anesthetists 100 percent to Anesthesiology
40-116 Rev.
DRAFT FORM CMS-2552-10 4020 (Cont.)
NOTE: The election of the alternative method discussed above cannot result in inappropriately shifting costs.
*Contract labor is not included and is not grossed up.
**If this is a meals on wheels program, a Worksheet A-8 adjustment is required.
Once the simplified method is elected, the provider must continue to use this method for no less than 3 years, unless a change of ownership occurs.
The 90-day and 60-day rule previously discussed in this section still applies (CMS Pub. 15-1, chapter 23, §2313).
Continuation of the Standard Allocation Methodology Instructions
Worksheet B, Part I, provides for the allocation of the expenses of each general service cost center to those cost centers which receive the services. The cost centers serviced by the general service cost centers include all cost centers within your organization, other general service cost centers, inpatient routine service cost centers, ancillary service cost centers, outpatient service cost centers, other reimbursable cost centers, special purpose cost centers, and nonreimbursable cost centers. Obtain the total direct expenses from Worksheet A, column 7.
All direct graduate medical education costs (inpatient and outpatient in approved programs) are reimbursed based on a specific amount per resident as computed on Worksheet E-4. Costs applicable to interns and residents must still be allocated in columns 21 and 22. These costs are, however, eliminated from total costs in column 25, unless you qualify for an exception. See the instructions for column 25 for a more detailed explanation.
Worksheet B-l provides for the proration of the statistical data needed to equitably allocate the expenses of the general service cost centers on Worksheet B, Part I. To facilitate the allocation process, the general format of Worksheets B, Part I, and B-1 is identical. Each general service cost center has the same line number as its respective column number across the top. Also, the column and line numbers for each general service cost center are identical on the two worksheets. In addition, the line numbers for each routine service, ancillary outpatient service, other reimbursable, special purpose, and nonreimbursable cost center are identical on the two worksheets. The cost centers and line numbers are also consistent with Worksheet A. If you have subscripted any lines on Worksheet A, subscript the same lines on these worksheets.
NOTE: General service columns 1 through 23 and subscripts thereof must be consistent on Worksheets B, Parts I, and II; H-2, Part I; J-1, Part I; K-5, Part I; and L-1, Part I.
The statistical basis shown at the top of each column on Worksheet B-1 is the recommended basis of allocation of the cost center indicated which must be used by all providers completing this form (Form CMS-2552-10), even if a basis of allocation other than the recommended basis of allocation was used in the previous iteration of the cost report (Form CMS-2552-96). If a different basis of allocation is used, you must indicate the basis of allocation actually used at the top of the column subject to the applicable provisions of CMS Pub. 15-1, chapter 23, §2313. Additionally, the following overhead cost center statistics can be substituted for the recommended statistics printed on Worksheet B-1 subject to the applicable provisions of CMS Pub. 15-1, chapter 23, §2313.
Cost Center Statistical Basis
Housekeeping Square Footage
Cafeteria FTEs
Maintenance of Personnel Eliminate and move to A&G
Medical Records Gross Patient Revenue
Rev. 40-117
4020 (Cont.) FORM CMS-2552-10 DRAFT
Most cost centers are allocated on different statistical bases. However, for those cost centers with the same basis (e.g., square feet), the total statistical base over which the costs are allocated differs because of the prior elimination of cost centers that have been closed.
The general service cost centers are ordered sequentially such that the cost centers that render the most services to and receive the least services from other cost centers are listed first. When closing the general service cost centers, first close the cost centers that render the most services to and receive the least services from other cost centers. List the cost centers in this sequence from left to right on the worksheets. However, your circumstances may be such that a more accurate result is obtained by allocating to certain cost centers in a sequence different from that followed on these worksheets.
NOTE: General service cost centers are not allocated to provider-based physician (PBP) clinical lab service (line 61) because this cost center is treated as a purchased service under arrangements provided only to program beneficiaries.
If the amount of any cost center on Worksheet A, column 7, has a credit balance, show this amount as a credit balance on Worksheet B, Part I, column 0. Allocate the costs from the applicable overhead cost centers in the normal manner to the cost center showing a credit balance. After receiving costs from the applicable overhead cost centers, if a general service cost center has a credit balance at the point it is allocated, do not allocate the general service cost center. Rather, enter the credit balance in parentheses on line 201 as well as on the first line of the column and on line 202. This enables column 24, line 202, to crossfoot to columns 0 and 4A, line 202 if the provider has intern & resident costs or a post-stepdown adjustment in column 25. However, column 26 will cross foot to columns 0 and 4A if the provider has no interns & residents costs or a post-stepdown adjustment in column 25. After receiving costs from the applicable overhead cost centers, if a revenue producing cost center has a credit balance on Worksheet B, Part I, column 26, do not carry forward a credit balance to any worksheet.
On Worksheet B-1, enter on the first line in the column of the cost center being allocated the total statistical base over which the expenses are allocated (e.g., in column 1, capital‑related cost - building and fixtures, enter on line 1 the total square feet of the building on which depreciation was taken). For all cost centers to which the capital-related cost is allocated, enter that portion of the total statistical base applicable to each. The sum of the statistical base applied to each cost center receiving the services rendered must equal the total base entered on the first line. Use accumulated cost for allocating A&G expenses.
Do not include any statistics related to services furnished under arrangements except if:
Both Medicare and non-Medicare costs of arranged for services are recorded in your records; or
Your contractor determines that you are able to (and do) gross up the costs and charges for services to non-Medicare patients so that both cost and charges are recorded as if you had furnished such services directly to all patients. (See CMS Pub. 15-1, chapter 23, §2314.)
Enter on line 202 of Worksheet B-l the total expenses of the cost center being allocated. Obtain this amount from Worksheet B, Part I, from the same column and line number used to enter the statistical base on Worksheet B-1. (In the case of capital-related costs - buildings and fixtures, this amount is on Worksheet B, Part I, column 1, line 1.)
Divide the amount entered on line 202 by the total statistic entered in the same column on the first line. Enter the resulting unit cost multiplier on line 203. Round the unit cost multiplier to six decimal places.
40-118 Rev.
DRAFT FORM CMS-2552-10 4020 (Cont.)
Multiply the unit cost multiplier by that portion of the total statistics applicable to each cost center receiving the services rendered. Enter the result of each computation on Worksheet B, Part I, in the corresponding column and line. (See §4000.1 for rounding standards.)
After applying the unit cost multiplier to all the cost centers receiving the services rendered, the total cost (line 202) of all the cost centers receiving the allocation on Worksheet B, Part I, must equal the amount entered on the first line. Perform the preceding procedures for each general service cost center. Complete the column for each cost center on both Worksheets B, Part I, and B-1 before proceeding to the column for the next cost center.
If a general service cost center has a credit balance at the point it is allocated on Worksheet B, Part I, do not allocate the general service cost centers. However, display the statistic departmentally, but do not calculate a unit cost multiplier for lines 203 and 205 on Worksheet B‑1. Use line 204 of Worksheet B-1 in conjunction with the allocation of capital‑related costs on Worksheet B, Part II. Complete line 204 for all columns after Worksheets B, Part I, and B-1 are completed and the amount of direct and indirect capital-related cost is determined on Worksheet B, Part II, column 2A. Use line 205 for all columns in allocating the direct and indirect capital-related cost on Worksheet B, Part II. Compute the unit cost multiplier (after the amount entered on line 204 has been determined) by dividing the capital-related costs recorded on line 204 by the total statistic entered in the same column on the first line. Round the unit cost multipliers to six decimal places. (See instructions for Worksheet B, Part II, for the complete methodology and exceptions.)
Do not use line 200 to allocate costs on Worksheet B, Part I.
Since intern and resident costs are segregated into two cost centers, properly allocate general service costs applicable to each center. A listing of general service cost centers which may be applicable and the appropriate allocation to the separate cost centers for the intern and resident costs is presented below.
Salary &
Salary Related
Cost Center Fringe Benefits Other
Capital Related Costs - Bldgs. & Fixtures X
Capital Related Costs - Movable Equipment X
Employee Benefits X X
Administrative and General X X
Maintenance and Repair X
Operation of Plant X
Housekeeping X
Cafeteria X X
Maintenance of Personnel X
Rev. 40-119
4020 (Cont.) FORM CMS-2552-10 DRAFT
After the costs of the general service cost center have been allocated on Worksheet B, Part I, enter in column 24, the sum of the costs in columns 4A through 23, for lines 30 through 201. Once overhead is allocated to these cost centers, they are closed and the costs are not further allocated to the revenue producing cost centers.
Since costs applicable to direct graduate medical education costs (inpatient and outpatient in approved programs) are reimbursed based on a specific amount per resident, exclude these costs from the total costs in column 26. Enter on each line in column 25 the sum of the amounts shown on each line in columns 21 and 22. If you qualify for the exception (cost reimbursed hospital such as CAHs do not offset I&R costs), enter only the amounts from Worksheet B-2.
In addition, when an adjustment to expenses is required after cost allocation, enter the amount applicable to each cost center in column 25 of Worksheet B, Part I. Corresponding adjustments to Worksheet B, Part II, may be applicable for capital-related cost adjustments. Submit a supporting worksheet showing the computation of the adjustments in addition to completing Worksheet B-2.
NOTE: The amount reported in column 25 must equal both the sum of the amounts shown in columns 21 and 22 and the amount on Worksheet B-2, unless you qualify for the exception. See the instructions for column 25 for a more detailed explanation.
Other examples of adjustments to expenses which may be required after cost allocation are (1) the allocation of available costs between the certified portion and the non-certified portion of a distinct part provider, and (2) costs attributable to unoccupied beds in a hospital with a restrictive admission policy. (See CMS Pub. 15-1, chapter 23, §§2342-2344.3.)
After the adjustments have been entered on Worksheet B, Part I, column 25, subtract the amounts in column 25 from the amounts in column 24, and enter the resulting amounts in column 26 for each line. The cost subtotal entered in column 24, line 202 must equal the total costs entered in column 0, line 202.
Transfer the totals in column 26, lines 30 through 46 (inpatient routine service cost centers), lines 50 through 76 (ancillary service cost centers), lines 88 through 93 (outpatient service cost centers), lines 94 through 101 (other reimbursable cost centers), and 105 through 117 (special purpose cost centers) to Worksheet C, Parts I and II, column l, lines 30 through 98. For provider based RHC/FQHCs transfer the total costs to Worksheet M-2.
40-120 Rev.
DRAFT FORM CMS-2552-10 4020 (Cont.)
Transfer the total cost in column 26, line 100 (intern/resident services not in approved teaching program) to Worksheet D-2, Part I, column 2, line 1.
The total outpatient rehabilitation costs in column 26, line 93, and subscripts, must agree with Worksheet J-1, Part I, column 26, line 22, for each provider type.
Do not transfer ASC costs from column 26, line 115. Do not transfer the nonreimbursable cost center totals (lines 190 through 193).
NOTE: Do not transfer negative numbers.
Column Descriptions
Column 1--Include only capital costs for building and fixtures. See the instructions for Worksheet A, line 1, for a discussion capital-related costs for building and fixtures.
Column 2--Include only capital costs for movable equipment. See the instructions for Worksheet A, line 2, for a discussion capital-related costs for movable equipment.
Worksheet B, Part I, Column 25--Hospitals other than CAHs--Accumulate in this column the costs for interns and residents. Except as provided in 42 CFR 413.77(e)(1), the costs of interns and residents (direct graduate medical education costs for inpatient and outpatient in approved programs) for PPS and TEFRA hospitals are paid on a per resident amount (PRA) through Worksheet E-4. In order to avoid duplicate payments of interns and residents costs, enter the sum of the amounts reported on each line in columns 21 and 22 in the appropriate line of column 25. When an adjustment to expenses is required after cost allocation, enter on the appropriate lines in this column the amounts from Worksheet B-2. The total of columns 21 and 22 and the appropriate lines on Worksheet B-2 must equal the total of column 25.
NOTE: In accordance with 42 CFR 413.77(e), if a hospital did not have any approved medical residency programs or did not participate in Medicare during the base period but either condition changes in a cost reporting period beginning on or after October 1, 2006 and the residents are not on duty during the first month of the cost reporting period in which the hospital first begins to train residents, the contractor establishes a PRA using information from the first cost reporting period immediately following the cost reporting period during which the hospital participates in Medicare and residents began training at the hospital. Any interns and residents costs incurred during the cost reporting period, prior to the base period used to calculate the PRA, are reimbursed as pass-through costs based on reasonable costs on Worksheets D, Parts III and IV, and D‑2, Part II, if applicable. If Worksheet S-2, Part I, line 57, column 1, is “Y” and column 2 is “N”, do not include in column 25 the interns and residents costs from columns 21 and 22.
If Worksheet S-2, Part I, Line 57, column 1, contains an “N” or column 2 contains a “Y”, include in column 25 the interns and residents in approved programs costs from columns 21 and 22 because these costs will be reimbursed on a PRA basis through Worksheet E-4.
CAHs--If you are CAH and responded “Y” to Worksheet S-2, Part I, question 107 (indicating that you have an I&R training program), the GME elimination is not performed. Consequently, do not include in column 25 the intern and resident costs from columns 21 and 22.
Rev. 40-121
4020 (Cont.) FORM CMS-2552-10 DRAFT
Worksheet B-1, Column 5A--Enter the costs attributable to the difference between the total accumulated cost reported on Worksheet B, Part I, column 4A, line 202, and the accumulated cost reported on Worksheet B-1, column 5, line 5. Enter any amounts reported on Worksheet B, Part I, column 4A, for (1) any service provided under arrangements to program patients and which is not grossed up and (2) negative balances. Enter a negative one (-1) in the accumulated cost column to identify the cost center which should be excluded from receiving any A&G costs. If some of the costs from that cost center are to receive A&G costs then enter in the reconciliation column the amount not to receive A&G costs to assure that only those costs to receive overhead receive the proper allocation. Including a statistical cost which does not relate to the allocation of A&G expenses causes an improper distribution of overhead. In addition, report on line 5 the A&G costs reported on Worksheet B, Part I, column 5, line 5, since these costs are not included on Worksheet B-1, column 5, as an accumulated cost statistic.
For componentized A&G cost centers, the accumulated cost center line number must match the reconciliation column number. Include in the column number the alpha character "A", i.e., if the accumulated cost center for A&G is line 5.03 (Other A&G), the reconciliation column designation must be 5A.03.
Worksheet B-1, Column 5--The A&G expenses are allocated on the basis of accumulated costs. Therefore, the amount entered on Worksheet B-l, column 5, line 5, is the difference between the amounts entered on Worksheet B, Part I, column 4A and Worksheet B-1, column 5A. A negative cost center balance in the statistics for allocating A&G expenses causes an improper distribution of this overhead cost center. Exclude negative balances from the allocation statistics.
Worksheet B-1, Column 23--Enter the appropriate statistics based on assigned time. If, however, the use of assigned time is not appropriate for that paramedical education program (i.e., a non‑direct patient care cost center), a different statistical basis may be used. For example, if you have a paramedical education program for hospital administration, using assigned time as the statistical basis may be inappropriate. Use accumulated costs as the statistical basis for allocating hospital administrative paramedical education program costs.
40-122 Rev.
DRAFT FORM CMS-2552-10 4021
4021. WORKSHEET B, PART II - ALLOCATION OF CAPITAL-RELATED COSTS
This worksheet provides for the determination of direct and indirect capital-related costs allocated to those cost centers which receive the services. The cost centers serviced by the general service cost centers include all cost centers within your organization, other general service cost centers, inpatient routine service cost centers, ancillary service cost centers, outpatient service cost centers, other reimbursable cost centers, special purpose cost centers, and nonreimbursable cost centers. Hospitals receiving 100 percent Federal rate for IPPS capital payments complete Worksheet B, Part II in its entirety.
NOTE: Unless there is a change in ownership or the provider has elected the alternative method described in §4017, the hospital must continue the same cost finding methods (including its cost finding bases) in effect in the hospital's prior cost reporting period. If there is a change in ownership, the new owners may request that the contractor approve a change in order to be consistent with their established cost finding practices. (See CMS Pub. 15-1, chapter 23, §2313.)
Part II is completed by all IPPS hospitals and IPPS excluded hospitals which were part of a complex subject to IPPS. Freestanding hospitals excluded from IPPS are not required to complete Part II.
See the instructions for Worksheet A, lines 1 and 2, for a discussion of capital-related costs.
Use these worksheets in conjunction with Worksheets B, Part I and B-1. The format and allocation process employed are identical to that used on Worksheets B, Part I and B-1. Any cost centers, subscripted lines, and/or columns added to Worksheet A are also added to Worksheet B, Part II, in the same sequence.
Column 0--Where capital-related costs have been directly assigned to specific cost centers on Worksheet A, column 7, in accordance with CMS Pub. 15-1, chapter 23, §2307, enter in this column those amounts directly assigned from your records. Where you include cost incurred by a related organization, the portion of these costs that are capital-related costs is considered directly assigned capital-related costs of the applicable cost center. For example, if you are part of a chain organization that includes some costs incurred by the home office of the chain organization in your A&G cost center, the amount so included represents capital-related costs included in this column.
Columns l and 2--Obtain the amounts entered in columns l and 2, lines 4 through 199, from the corresponding columns and lines on Worksheet B, Part I.
Column 2A--Enter the sum of columns 0 through 2 for each line.
Enter on line 204 of Worksheet B-l for each column the capital-related costs allocated. Report these costs on the first line of each column on Worksheet B, Part II. (See exceptions below.) Complete a unit cost multiplier for each column by dividing the amount on line 204 of Worksheet B-l by the statistic reported on the first line of the same column. Enter the unit cost multiplier on line 205 and round to six decimal places, e.g., .0622438 is rounded to .062244. The allocation process on Worksheet B, Part II, is identical to that used on Worksheets B, Part I, and B-l.
Multiply the unit cost multipliers on line 205 by the portion of the total statistic on Worksheet B‑1 applicable to each cost center. Enter the result of each computation on Worksheet B, Part II, respectively, in the corresponding column and line.
Rev. 40-123
4021 (Cont.) FORM CMS-2552-10 DRAFT
After the unit cost multipliers have been applied to all the cost centers, the total cost on Worksheet B, Part II, line 202, of all the cost centers receiving the allocation must equal the amount allocated on the first line of the column. However, this is not true in circumstances described in the second paragraph of exceptions below. Perform these procedures for each general service cost center. Complete the column for each cost center on Worksheets B-1 and B, Part II, before proceeding to the column for the next cost center.
EXCEPTIONS: When a general service cost center is not allocated on Worksheet B, Part I, because it has a negative balance at the point it is to be allocated, the capital‑related cost for the same general service cost center on Worksheet B, Part II, is not allocated. Enter the total capital-related cost on line 201, the negative cost center line. This enables column 2A, line 202, to cross foot to column 26, line 202, if no intern and resident cost or post step-down adjustments are identified in column 25. Otherwise column 2A, line 202, will crossfoot to line 24.
When a general service cost center has a negative direct cost balance on Worksheet B, Part I, column 0, and the negative balance becomes positive through the cost allocation process, adjust the amount of capital-related cost determined on Worksheet B, Part II, for that general cost center to reflect the amount allocated on Worksheet B, Part I. Determine the adjusted amounts of capital-related cost allocated on Worksheet B, Part II, by dividing the capital-related cost by the total indirect cost allocated to the specific cost center on Worksheet B, Part I. (Do not include the negative direct cost.) Then multiply that ratio by the net amount allocated on Worksheet B, Part I, for that specific cost center. For cross footing purposes, enter the adjusted capital-related costs on the first line of the column and the differences between the total capital-related cost and the adjusted capital-related cost on line 201 of Worksheet B, Part II. This enables column 2A, line 202, to cross foot to column 26, line 202, if no intern and resident cost or post step-down adjustments are identified in column 25. Otherwise column 2A, line 202, will crossfoot to line 24.
After all the capital-related costs of the general service cost centers have been allocated on Worksheet B, Part II, enter in column 24, the sum of columns 2A through 23 for lines 30 through 201.
When an adjustment to expenses is required after cost allocation, show the amount applicable to each cost center in column 25 of Worksheet B, Part II. Submit a supporting worksheet showing the computation of the adjustment in addition to completing Worksheet B-2.
Adjustments to expenses which may be required after cost allocation include (1) the allocation of available costs between the certified portion and the noncertified portion of a distinct part provider, and (2) costs attributable to unoccupied beds of a hospital with a restrictive admission policy. (See CMS Pub. 15-1, chapter 23, §§2342-2344.3.)
After the adjustments have been entered on Worksheet B, Part II, column 25, subtract the amounts in column 25 from the amounts in column 24, and enter the resulting amounts in column 26 for each line. The total costs entered in column 26, line 202, must equal the total costs entered in column 2A, line 202, if no intern and resident cost or post step-down adjustments are identified in column 25, otherwise column 2A, line 202, will equal line 24.
On Worksheet B, Part II, columns 19 through 23, lines 30 through 194, are shaded because the full amount of nonphysician anesthetists and medical education costs is obtained from Worksheet B, Part I, columns 19 through 23. Enter these amounts on line 200 for cross footing purposes. If column 20 is subscripted for additional education cost centers qualifying as educational pass through costs (see the instructions for Worksheet A, lines 20 through 23), the subscripted column(s) must be shaded similarly to column 20.
40-124 Rev.
DRAFT FORM CMS-2552-10 4021 (Cont.)
Since capital-related cost, non-physician anesthetists, and approved education programs are not included in the operating cost per discharge, columns 19 through 23, lines 30 through 194, are shaded on Worksheet B, Part II, for all lines except 19 through 23, 200, 201, and 202. These are the only lines and columns where an approved educational cost center can be shown. For purposes of this paragraph only, the statistic for line 200 is the sum of the statistics on lines 30 through 117 and 190 through 194 on Worksheet B-1 for the same column. Enter these amounts on line 200 for cross footing purposes. Use line 200 of Worksheet B-1, columns 19 through 23, for this purpose in the allocation of capital-related cost on Worksheet B, Part II. Use the statistic on line 200 together with the statistics on lines 19 through 23 of Worksheet B-1 to allocate columns 19 through 23 of Worksheet B, Part II. If column 20 is subscripted for additional education cost centers qualifying as educational pass through costs (see the instructions for Worksheet A, lines 20 through 23), the subscripted column(s) must be shaded similarly to columns 20 through 23
The total for each column includes lines 200 and 201 for cross footing purposes.
Transfer:
From Worksheet B, Part II, Column 26 To Worksheet D, Part I
Line 30 - Adults and Pediatrics Column l, line 30 for the hospital
Lines 31-35 - Intensive Care Column 1, lines 31 through 35
Type Inpatient Hospital Units
Line 40 - IPF Subprovider Column l, line 40
Line 41 - IRF Subprovider Column l, line 41
Line 42 - Subprovider Column l, line 42
Line 43 - Nursery Column 1, line 43 for titles V and XIX
From Worksheet B, Part II, Column 26 To Worksheet D-l, Part III
Line 44 - SNF Line 75 for the SNF
Sum of lines 44 and 45 Line 75 for the NF
From Worksheet B, Part II, Column 26 To Worksheet D, Part II
Lines 50-76 - Ancillary Services Column l, lines 50-76
Lines 90, 91, subscripts of 92, Column l, lines 90, 91, subscripts
and 93 - Outpatient Service Cost of 92, and 93
Lines 94, 95, and 98 - Other Column l, lines 94, 95, and 98
Reimbursable Cost Centers
To Worksheet C, Part II, Column 2
Lines 50-98 Lines 50-98
Rev. 40-125
4022 FORM CMS-2552-10 DRAFT
4022. WORKSHEET B-2 - POST STEP-DOWN ADJUSTMENTS
This worksheet provides an explanation of the post step down adjustments reported in column 25 of Worksheets B, Parts I and II, and L-1, Part I.
Column Descriptions
Column 1--Enter a brief description of the post step down adjustment.
Column 2--Make post step down adjustments on Worksheets B, Parts I and II, and L-1, Part I. Enter the worksheet part to which the post step down adjustment applies. For lines 74 and/or 94, remove the amount for ESAs (i.e., Epoetin and Aranesp) reported on Worksheet S-5 lines 13, 14, 17, 18, and subscripts of line 22, columns 2 and 3.
Use the codes below to identify the worksheet in which the adjustment applies:
Code Worksheet
1 B, Part I
2 B, Part II
3 L-1, Part I
Column 3--Enter the worksheet line number to which the adjustment applies.
Column 4--Enter the amount of the adjustment. Transfer these amounts to the appropriate lines on Worksheets B, Parts I, and II, or L-1, Part I, column 25.
Line Descriptions
Line 1--Enter the amount of the EPO adjustment for the renal dialysis inpatient department from Worksheet S-5, line 13. Do not use this line effective for cost reporting periods ending after December 31, 2012.
Line 2--Enter the amount of the EPO adjustment for the home dialysis program from Worksheet S-5, line 14. Do not use this line effective for cost reporting periods ending after December 31, 2012.
Line 3--Enter the amount of the Aranesp adjustment for the renal dialysis inpatient department from Worksheet S-5, line 17. Do not use this line effective for cost reporting periods ending after December 31, 2012.
Line 4--Enter the amount of the Aranesp adjustment for the home dialysis program from Worksheet S-5, line 18. Do not use this line effective for cost reporting periods ending after December 31, 2012.
Line 5--Enter the amount of the ESA adjustment for the renal dialysis inpatient department from Worksheet S-5, sum of the subscripts of line 22, column 2. Complete this line effective for cost reporting periods ending after December 31, 2012.
Line 6--Enter the amount of the ESA adjustment for the home dialysis program from Worksheet S-5, sum of the subscripts of line 22, column 3. Complete this line effective for cost reporting periods ending after December 31, 2012.
Lines 7 through 59--Enter any additional adjustments that are required under the Medicare principles of reimbursement. Label the lines appropriately to indicate the nature of the required adjustments. If the number of blank lines is not sufficient, use additional Worksheets B-2.
40-126 Rev.
DRAFT FORM CMS-2552-10 4023.1
4023. WORKSHEET C - COMPUTATION OF RATIO OF COST TO CHARGES AND OUTPATIENT CAPITAL REDUCTION
4023.1 Computation of Ratio of Cost to Charges--This worksheet computes the ratio of cost to charges for inpatient services, ancillary services, outpatient services, and other reimbursable services. All charges entered on this worksheet must comply with CMS Pub. 15-1, chapter 22, §§2202.4 and 2203. This ratio is used on Worksheet D, Part V, for titles V and XIX, and for title XVIII; Worksheet D-3; Worksheet D-4; Worksheet H-3, Part II; and Worksheet J-2, Part II, to determine the program's share of ancillary service costs in accordance with 42 CFR 413.53. This worksheet is also needed to determine the adjusted total costs used on Worksheet D-1 because of your status as IPPS, TEFRA, or other.
42 CFR 413.106(f)(3) provides that the costs of therapy services furnished under arrangements to a hospital inpatient are exempt from the guidelines for physical therapy and respiratory therapy if such costs are subject to the provisions of 42 CFR 413.40 (rate of increase ceiling) or 42 CFR 412 (inpatient prospective payment). However, therapy services furnished under arrangements to CAHs are subject to the provisions of 42 CFR 413.106.
42 CFR 415.70(a)(2) provides that RCE limits do not apply to the costs of physician compensation attributable to furnishing inpatient hospital services (provider component) paid for under 42 CFR 412ff.
To facilitate the cost finding methodology, apply the therapy limits and RCE limits to total departmental costs. This worksheet provides the mechanism for adjusting the costs after cost finding to comply with 42 CFR 413.106(f)(3) and 42 CFR 415.70(a)(2). This is done by computing a series of ratios in columns 9 through 11. In column 9, a ratio referred to as the “cost or other ratio” is computed based on the ratio of total reasonable cost to total charges. This ratio is used by you or your components not subject to IPPS or TEFRA (e.g., hospital-based SNFs and CAHs). Also use this ratio for Part B services still subject to cost reimbursement. In column 10, compute a TEFRA inpatient ratio. This ratio reflects the add-back of respiratory therapy/physical therapy (RT/PT) limitations to total cost since TEFRA inpatient costs are not subject to these limits. (TEFRA inpatient services are subject to RCE limits.) In column 11, compute an IPPS inpatient ratio. This ratio reflects the add-back of RT/PT and RCE limitations to total cost since inpatient hospital services covered by IPPS are not subject to any of these limitations.
Column Descriptions
The following provider components may be subject to 42 CFR 413.40 or 42 CFR 412.1(a)ff:
Hospital Part A inpatient services for title XVIII,
Hospital subprovider Part A inpatient services for title XVIII,
Hospital inpatient services for titles V and XIX, and
Hospital subprovider services for titles V and XIX.
All components or portions of components not subject to IPPS, IPF PPS, IRF PPS, LTC PPS, or TEFRA, e.g., CAH services, are classified as “Cost or Other.”
The following matrix summarizes the columns completed for Cost or Other, TEFRA Inpatient, and IPPS:
__________Columns______________
Cost or TEFRA IPPS, IPF-PPS,
Type of Service Other Inpatient IRF-PPS Inpatient
Inpatient routine service cost centers
(lines 30-46) 1-3 1-3 1-5
Rev. 40-127
4023.1 (Cont.) FORM CMS-2552-10 DRAFT
Inpatient ancillary
(lines 50-93) 1, 8, 9 1-3, 8-10 1-9, 11
Other Reimbursable
(lines 94-98) 1, 8, 9 1-3, 8-10 1-9, 11
Other Reimbursable
(lines 99-101) 1, 8 1-3, 8 1-8
Special Purpose
(lines 105-117) 1, 8 1-3, 8 1-8
Column 1--Enter on each line the amount from the corresponding line of Worksheet B, Part I, column 26. Transfer the amount on line 92 from Worksheet D-1, Part IV, line 89, if you do not have a distinct observation bed area. If you have a distinct observation bed area, subscript line 92 into line 92.01, and transfer the appropriate amount from Worksheet B, Part I, column 26. In a complex comprised of an acute care hospital with an excluded unit(s) (excluded from IPPS), only the acute care hospital may report observation bed costs. Any services provided by the RHC/FQHC outside the benefits package for those clinics are reported by the hospital in its appropriate ancillary cost center, but not in the RHC/FQHC cost center lines 88 and 89. Do not bring forward any cost center with a credit balance from Worksheet B, Part I, column 26.
Column 2--Enter the amount of therapy limits applied to the cost center on lines 65 to 68. Obtain these amounts from Worksheet A-8, lines 23, 24, 30 and 31 respectively.
NOTE: Complete this column only when the hospital or subprovider is subject to PPS or TEFRA rate of increasing ceiling (see 42 CFR 412, subpart N and P, and 42 CFR 413.40, respectively). If the hospital and all subproviders have correctly indicated that their payment system is in the “other” category on Worksheet S-2, do not complete columns 2 through 5, 10, and 11.
Column 3--Enter on each cost center line the sum of columns 1 and 2.
Column 4--Only complete this section if you or your subproviders are subject to IPPS, IPF PPS, IRF PPS, or LTC PPS. Enter on each line the amount of the RCE disallowance. Obtain these amounts from the sum of the amounts for the corresponding line on Worksheet A-8-2, column 17.
Column 5--Complete this section only if you or your subproviders are subject to a PPS. Enter on each cost center line the sum of the amounts entered in columns 3 and 4.
Columns 6 and 7--Enter on each cost center line the total inpatient and outpatient gross patient charges including charges for charity care patients and, where applicable, standard customary charges for items reimbursed on a fee schedule (e.g., DME, oxygen, prosthetics, and orthotics). Also include the total inpatient and outpatient gross charges for cost centers which have a credit balance on Worksheet B, Part I, column 26 and, therefore, do not contain “cost” in column 1 of Worksheet C, Part I.

 Total
charges on Worksheet C, Part I, for each department are for provider
services only. Therefore, Medicare charges on Worksheets D, Parts II
and IV, D-2, D-3, and D-4,
must also include provider services only. When reporting charges for
a complex, e.g., hospital, subprovider, SNF, charges for like
services must be uniform. (See CMS Pub. 15-1, chapter
22, §2203.)
Total
charges on Worksheet C, Part I, for each department are for provider
services only. Therefore, Medicare charges on Worksheets D, Parts II
and IV, D-2, D-3, and D-4,
must also include provider services only. When reporting charges for
a complex, e.g., hospital, subprovider, SNF, charges for like
services must be uniform. (See CMS Pub. 15-1, chapter
22, §2203.)
40-128 Rev.
DRAFT FORM CMS-2552-10 4023.1 (Cont.)
When certain services are furnished under arrangements and an adjustment is made on Worksheet A-8 to gross up costs, gross up the related charges entered on Worksheet C, Part I, in accordance with CMS Pub. 15-1, chapter 23, §2314. If no adjustment is made on Worksheet A‑8, show only the charges you actually billed on Worksheet C, Part I.
NOTE: Any cost center that includes CRNA charges must exclude these charges unless the hospital qualifies for the rural exception as outlined in §4013. All cost centers for which CRNA costs are excluded on Worksheet A-8 must also exclude the charges associated with these costs.
NOTE: Any charges for ancillary services provided to clinic, RHC and FQHC patients must be reclassified to the appropriate ancillary cost center, e.g., radiology-diagnostic, laboratory. A similar adjustment must be made to program charges.
Report on line 92 all charges for observation bed services provided in the inpatient routine care area of the hospital. The charges relate to all payer classes and include those observation bed charges for patients released as outpatients and those patients admitted as inpatients. If you have a distinct observation bed unit, report your gross charges on line 92.01 (which was subscripted on Worksheet A).
Column 8--Enter the total of columns 6 and 7.
Column 9 through 11--Cost to charge ratios are not calculated for lines 99 through 117. The corresponding locations on Worksheet C, Part I are shaded.
Column 9, lines 50 through 98--Always complete this column. Divide the cost for each cost center in column 1 by the total charges for the cost center in column 8 to determine the ratio of total cost to total charges (referred to as the "Cost or Other" ratio) for that cost center. Enter the resultant departmental ratios in this column. Round ratios to 6 decimal places.
Column 10, lines 50 through 98--Complete this section only when the hospital or its subprovider is subject to the TEFRA rate of increase ceiling. (See 42 CFR 413.40.) Divide the amount reported in column 3 (which represents the total cost adjusted for the add-back of amounts excluded on Worksheet A-8 for the RT/PT limits) for each cost center by the total charges for the cost center in column 8.
This computation determines the RT/PT adjusted ratio of cost to charges (referred to as the TEFRA inpatient ratio) for each cost center. Enter the resultant departmental ratio. Round ratios to 6 decimal places.
Column 11, lines 50 through 98--Complete this section only when the hospital is subject to IPPS or LTC PPS or when its subprovider is subject to its respective PPS reimbursement methodology. (See 42 CFR 412.1(a) through 412.125, 42 CFR 412, subparts O, N, and P, respectively). Divide the amount reported in column 5 (which represents the total cost adjusted for the add-back of amounts excluded on Worksheet A-8 for the RT/PT and the RCE limits) for each cost center by the total charges for the cost center in column 8.
This computation determines the RCE/RT/PT adjusted ratio of cost to charges (referred to as the PPS inpatient ratio) for each cost center. Enter the resultant departmental ratio. Round ratios to 6 decimal places.
Line Descriptions
Lines 30 - 117--These cost centers have the same line numbers as the respective cost centers on Worksheets A, B, and B-1. This design facilitates referencing throughout the cost report.
Rev. 40-129
4023.1 (Cont.) FORM CMS-2552-10 DRAFT
Therefore, if you have subscripted any lines on those worksheets, you must subscript the same lines on this worksheet.
NOTE: The worksheet line numbers start at line 30 because of the line referencing feature.
Line 200--For each of the columns 1 through 5 (total costs), respectively, enter the sum of lines 30 through 199 for all unshaded lines in accordance with Worksheet C, Part I.
For each of the columns 6, 7, and 8 (total charges), respectively, enter the sum of lines 30 through 60, and 62 through 199, for all unshaded lines in accordance with Worksheet C, Part I. Since the charges on line 61 are also included on line 60 (laboratory), the charges on line 61 must be excluded to avoid overstating total charges.
Line 201--Enter the amounts from line 92 for columns 1, 3, and 5. Calculate the observation bed cost on line 92 using the routine cost per diem from Worksheet D-1 because it is part of routine costs and as such has been included in the amounts reported on line 30 for the hospital. Therefore, in order to arrive at the total allowable costs, subtract this cost to avoid reporting these costs twice.
Line 201, columns 6, 7, and 8, are shaded.
Line 202--For columns 1, 3, and 5, subtract line 201 from line 200, and enter the result.
Transfer Referencing
Costs--The costs of the inpatient routine service cost centers are transferred:
From Worksheet C
(Columns 1, 3, or 5) To
Line 30 Wkst. D-1, Part I, line 21
Lines 31 - 35 Wkst. D-1, Part II, lines 43 - 47
Line 40, 41, 42 and subscripts Separate Wkst. D-1, Part I, line 21
Line 43 (titles V and XIX only) Wkst. D-1, Part II, line 42
Line 44 (title XVIII only) Separate Wkst. D-1, Part I, line 21
Line 45 and subscripts (titles V and Separate Wkst. D-1, Part I, line 21
XIX only)
Charges--Transfer the total charges for each of lines 50 through 98, column 8, to Worksheet D, Part IV, column 7, lines as appropriate.
Ratios
Cost or Other Ratios--The "Cost or Other" ratio is transferred from column 9:
For To
Hospital, subprovider, SNF, NF, swing
bed-SNF, and swing bed-NF:
1. Inpatient ancillary services for Wkst. D-3, column 1,
titles V, XVIII, Part A, and XIX for each cost center
Ancillary services furnished by the Wkst. H-3, Part II,
hospital-based HHA column 1, line as appropriate
40-130 Rev.
DRAFT FORM CMS-2552-10 4023.2
For To
Hospital-based Wkst. J-2, Part II,
CMHC (titles V, XVIII, and XIX) column 3, line as appropriate
shared ancillary services
TEFRA Inpatient Ratio--Transfer the TEFRA inpatient ratio on lines 50 through 94 and 96 through 98 from column 10 for hospital or subprovider components for titles V, XVIII, Part A, and XIX inpatient services subject to the TEFRA rate of increase ceiling (see 42 CFR 413.40) to Worksheet D-3, column 1, for each cost center.
PPS Inpatient Ratio--Transfer the PPS inpatient ratio on lines 50 through 94 and 96 through 98 from column 11, for hospital or subprovider components for titles V, XVIII, Part A, and XIX inpatient services subject to IPPS (see 42 CFR 412.1(a) through 412.125) to Worksheet D-3, column 1, for each cost center. The transfer of the PPS inpatient ratio also applies when the facility is an IPF subject to IPF PPS, a LTCH subject to LTCH PPS, or an IRF subject to IRF PPS (see 42 CFR 412, subparts N, O, and P, respectively).
4023.2 Part II - Calculation of Outpatient Services Cost to Charge Ratios Net of Reductions for Medicaid Only.--This worksheet is not applicable for title XVIII. It is only applicable for select state Medicaid programs. This worksheet computes the outpatient cost to charge ratios reflecting the following:
The percentage of capital reduction as identified on Worksheet S-2, Part I, line 95, the applicable column.
The reduction in reasonable costs of hospital outpatient services (other than the capital‑related costs of such services (also known as operating reduction)) is based upon the percentage entered on Worksheet S-2, Part I, line 97, the applicable column.
Column Descriptions
Column 1--Enter the amounts for each cost center from Worksheet B, Part I, column 26, as appropriate. Transfer the amount on line 92 from Worksheet D-1, Part IV, line 89 for the hospital and if you use inpatient routine beds as observation beds. If you have a distinct observation bed area, add subscripted line 92.01 and transfer the appropriate amount from Worksheet B, Part I, column 26. Do not bring forward costs in any cost center with a credit balance from Worksheet B, Part I, column 26.
Column 2--Enter the sum of the amounts for each cost center from Worksheet B, Part II, as appropriate. Do not bring forward costs in any cost center with a credit balance on Worksheet B, Part I, Worksheet B, Part II. For line 92, enter the amounts from Worksheet D-1, Part IV, column 5, line 90. Combine the hospital and subprovider amounts if applicable.
Column 3--For each line, subtract column 2 from column 1, and enter the result.
Column 4--Multiply column 2 by the appropriate capital reduction percentage, and enter the result.
Column 5--Multiply column 3 by the outpatient reasonable cost reduction percentage, and enter the result.
Column 6--Subtract columns 4 and 5 from column 1, and enter the result.
Column 7--Enter the total charges from Worksheet C, Part I, column 8.
Column 8--Divide column 6 by column 7, and enter the result.
Rev. 40-131
4024 FORM CMS-2552-10 DRAFT
4024. WORKSHEET D - COST APPORTIONMENT
Worksheet D consists of the following five parts:
Part I - Apportionment of Inpatient Routine Service Capital Costs
Part II - Apportionment of Inpatient Ancillary Service Capital Costs
Part III - Apportionment of Inpatient Routine Service Other Pass Through Costs
Part IV - Apportionment of Inpatient/Outpatient Ancillary Service Other Pass Through Costs
Part V - Apportionment of Medical and Other Health Services Costs
At the top of each part, indicate by checking the appropriate boxes the health care program, provider component, and the payment system, as applicable, for which the part is prepared.
NOTE: Only hospital components subject to PPS or TEFRA complete Worksheet D, Parts I through IV. New children’s and new cancer hospitals complete only Worksheet D, Parts III and IV (line 85 of Worksheet S-2, Part I, has a “Y” response). CAHs do not complete Parts I through IV. Hospital based SNF and NF providers are added to the Worksheet D, Part III and will also complete a separate Worksheet D, Part IV.
Line Descriptions for Parts I Through V
Lines 30 through 43 (for Parts I and III) and lines 44 and 45 (for Part III) and 50 through 98 (for Parts II, IV, and V)--These cost centers have the same line numbers as the respective cost centers on Worksheets A, B, B-1, and C. This design facilitates referencing throughout the cost report. Therefore, any lines subscripted on those worksheets, must subscripted on this worksheet.
4024.1 Part I - Apportionment of Inpatient Routine Service Capital Costs--This part computes the amount of capital-related costs applicable to hospital inpatient routine service costs. Complete only one Worksheet D, Part I, for each title. Report hospital and subprovider information on the same worksheet, lines as appropriate. Complete this part for all payment methods.
Column 1--Enter on each line the capital-related cost for each cost center, as appropriate. Obtain this amount from Worksheet B, Part II, column 26.
Column 2--Compute the amount of the swing bed adjustment. If you have a swing bed agreement or have elected the swing bed optional method of reimbursement, determine the amount for the cost center in which the swing beds are located by multiplying the amounts in column 1 by the ratio of the amount entered on Worksheet D-1, line 26, to the amount entered on Worksheet D-1, Part I, line 21.
Column 3--For each line, subtract the amount, if any, in column 2 from the amount in column 1, and enter the result.
Column 4--Enter on each line the total patient days, excluding swing bed days, for that cost center. For line 30, enter the total days reported on Worksheet S-3, Part I, column 8, the sum of lines 1 and 28. For lines 31 through 43, enter the days from Worksheet S-3, Part I, column 8, lines 8 through 12, 13, and 16-18 (as applicable), respectively.
Column 5-- Divide the capital costs of each cost center in column 3 by the total patient days in column 4 for each line to determine the capital per diem cost. Enter the resultant per diem cost in column 5.
Column 6--Enter the program inpatient days for the applicable cost centers. For line 30, enter the days reported on Worksheet S-3, Part I, columns 5, 6, or 7, as appropriate, line 1. For lines
40-132 Rev.
DRAFT FORM CMS-2552-10 4024.2
31 through 43, enter the days from Worksheet S-3, Part I, columns 5, 6, or 7, as appropriate, lines 8 through 12, 13, and 16-18 (as applicable), respectively.
NOTE: When you place overflow general care patients temporarily in an intensive care type inpatient hospital unit because all beds available for general care patients are occupied, count the days as intensive care type inpatient hospital days for purposes of computing the intensive care type inpatient hospital unit per diem. However, count the program days as general routine days in computing program reimbursement. (See CMS Pub. 15-1, chapter 22, §2217.) Add any program days for general care patients of the component who temporarily occupied beds in an intensive care or other special care unit to line 30, and decrease the appropriate intensive care or other special care unit by those days.
Column 7--Multiply the per diem in column 5 by the inpatient program days in column 6 to determine the program’s share of capital costs applicable to inpatient routine services, as applicable.
4024.2 Part II - Apportionment of Inpatient Ancillary Service Capital Costs--This worksheet is provided to compute the amount of capital costs applicable to hospital inpatient ancillary services for titles V, XVIII, Part A, and XIX. Complete a separate copy of this worksheet for each subprovider for titles V, XVIII, Part A, and XIX, as applicable. In this case, enter the subprovider component number in addition to showing the provider number.
Make no entries on this worksheet for any costs centers with a negative balance on Worksheet B, Part I, column 26.
Column 1--Enter on each line the capital-related costs for each cost center, as appropriate. Obtain this amount from Worksheet B, Part II, column 26. For the hospital component or subprovider, if applicable, enter on line 92 the amount from Worksheet D-1, Part IV, column 1, line 90.
Column 2--Enter on each line the total charges applicable to each cost center as shown on Worksheet C, Part I, column 8.
Column 3--Divide the capital cost of each cost center in column 1 by the charges in column 2 for each line to determine the cost to charge ratio. Round the ratios to six decimal places, e.g., round 0321514 to .032151. Enter the resultant departmental ratio in column 3.
Column 4--Enter on each line the appropriate title V, XVIII, Part A, or XIX inpatient charges from Worksheet D-3, column 2. For title XVIII, enter on line 92, the observation bed charges applicable to title XVIII patients subsequently admitted after being treated in the observation area. Enter on line 96 the Medicare charges for medical equipment rented by an inpatient. The charges are reimbursed under the DRG. However, you are entitled to the capital-related cost pass through applicable to this medical equipment.
NOTE: Program charges for PPS providers are reported in the cost reporting period in which the discharge is reported. TEFRA providers report charges in the cost reporting period in which they occur.
Do not include in Medicare charges any charges identified as MSP/LCC.
Column 5--Multiply the capital ratio in column 3 by the program charges in column 4 to determine the program’s share of capital costs applicable to titles V, XVIII, Part A, or XIX inpatient ancillary services, as appropriate.
Rev. 40-133
4024.3 FORM CMS-2552-10 DRAFT
4024.3 Part III - Apportionment of Inpatient Routine Service Other Pass Through Costs--This part computes the amount of pass through costs other than capital applicable to hospital inpatient routine service costs. Determine capital-related inpatient routine service costs on Worksheet D, Part I. Complete only one Worksheet D, Part III for each title. Report hospital, subprovider, hospital-based SNF, NF and ICF/IID (if applicable) information on the same worksheet, lines as appropriate. SNFs are now required to report medical education costs as a pass through cost.
Column 1--Transfer from Worksheet B, Part I, column 20, for each applicable line, (plus or minus post step down adjustments reported on Worksheet B-2, if applicable), the applicable medical education costs for nursing school when Worksheet S-2, Part I, line 60, is yes. Do not transfer the costs if the response is no.
Column 2--Transfer from Worksheet B, Part I, column 23, for each applicable line, (plus or minus post step down adjustments reported on Worksheet B-2, if applicable), the applicable medical education costs for paramedical education (allied health) when Worksheet S-2, Part I, line 60, is yes. Do not transfer the costs if the response is no.
Column 3--Transfer from Worksheet B, Part I, the sum of columns 21 and 22, for each applicable line, plus or minus post step down adjustments (reported on Worksheet B-2), the applicable medical education costs for interns and residents when Worksheet S-2, Part I, line 57, column 1 is yes and column 2 is no. Otherwise do not transfer the costs.
NOTE: If you qualify for the exception in 42 CFR 413.77(e)(1), because this is the first cost reporting period in which you are training residents in approved programs and the residents were not on duty during the first month of this cost reporting period, then all direct graduate medical education costs are reimbursed as a pass through based on reasonable cost.
Column 4--Compute the amount of the swing bed adjustment. If you have a swing bed agreement, determine the amount for the cost center in which the swing beds are located by multiplying the sum of the amounts in columns 1 through 3 by the ratio of the amount entered on Worksheet D-1, Part I, line 26, to the amount entered on Worksheet D-1, Part I, line 21.
Column 5--Enter the sum of columns 1 through 3 (including subscripts) minus column 4.
Column 6--Enter on each line the total patient days, excluding swing bed days, for that cost center. Transfer these amounts from the appropriate Worksheet D, Part I, column 4. For SNFs enter total patient days from Worksheet S-3, Part I, column 8, line 19.
Column 7--Enter the per diem cost for each line by dividing the cost of each cost center in column 5 by the total patient days in column 6.
Column 8--Enter the program inpatient days for the applicable cost centers. Transfer these amounts from the appropriate Worksheet D, Part I, column 6. For SNF (line 44) enter the program days from Worksheet S-3, Part I, column 6, line 19.
Column 9--Multiply the per diem cost in column 7 by the inpatient program days in column 8 to determine the program's share of pass through costs applicable to inpatient routine services, as applicable. Transfer the sum of the amounts on lines 30 through 35 and 43 to Worksheet D-1, Part I, line 50, for the hospital. If you are a title XVIII hospital paid under IPPS, also transfer this sum to Worksheet E, Part A, line 57. Transfer the amounts on lines 40 through 42 to the
40-134 Rev.
DRAFT FORM CMS-2552-10 4024.4
appropriate Worksheet D-1, line 50 for the subprovider. Also transfer the amount on line 40 to Worksheet E-3, Part II, line 28 and the amount on line 41 to Worksheet E-3, Part III, line 29. For hospital-based SNF, NF or ICF/IID that follow Medicare principles, transfer the amount in column 9, line 44 to Worksheet E-3, Part VI, line 2 or for NF or ICF/IID to Worksheet E-3, Part VII, line 26, as applicable.
4024.4 Part IV - Apportionment of Inpatient/Outpatient Ancillary Service Other Pass Through Costs--The TEFRA rate of increase limitation applies to inpatient operating costs. In order to determine inpatient operating costs, it is necessary to exclude capital-related and medical education costs as these costs are reimbursed separately. Hospitals and subprovider components subject to IPPS and/or OPPS must also exclude direct medical education costs as these costs are reimbursed separately. Determine capital-related inpatient ancillary costs on Worksheet D, Part II. SNFs are required to report medical education costs as a pass through cost. Prepare a separate Worksheet D, Part IV for the SNF and NF or ICF/IID (if applicable).
This worksheet is provided to compute the amount of pass through costs other than capital applicable to hospital inpatient and outpatient ancillary services for titles V, XVIII, Part A, and XIX. Complete a separate copy of this worksheet for each subprovider for titles V, XVIII, Part A, and XIX, as applicable. In this case, enter the subprovider component number in addition to showing the provider number.
Make no entries on this worksheet for any costs centers with a negative balance on Worksheet B, Part I, column 26.
Column 1--Transfer from Worksheet B, Part I, column 19, for each applicable line (plus or minus any adjustments reported on Worksheet B-2, if applicable) the nonphysician anesthetist’s costs which qualify for a reasonable cost payment in accordance with 42 CFR 412.113(c). (See also §4013, line 19 description for more information.)
Column 2--Transfer from Worksheet B, Part I, column 20, for each applicable line, (plus or minus post step down adjustments made on Worksheet B-2, if applicable), the applicable medical education costs for nursing school when Worksheet S-2, Part I, line 60, is yes. Do not transfer the costs if the response is no. For the hospital only, enter on line 92, observation beds, the amount from Worksheet D-1, Part IV, column 5, line 91.
Column 3--Transfer from Worksheet B, Part I, column 23, for each applicable line, (plus or minus post step down adjustments made on Worksheet B-2, if applicable), the applicable medical education costs for paramedical education (allied health) when Worksheet S‑2, Part I, line 60, is yes. Do not transfer the costs if the response is no. For the hospital component only, enter on line 92 the observation bed amount from Worksheet D-1, Part IV, column 5, line 92.
Column 4--Transfer from Worksheet B, Part I, the sum of columns 21 and 22, for each applicable line, (plus or minus post step down adjustments made on Worksheet B-2, if applicable), the applicable medical education costs for interns and residents when Worksheet S‑2, Part I, line 57, column 1, is yes, and column 2, is no, otherwise do not transfer the costs. For the hospital only, enter on line 92, observation beds, the amount from Worksheet D-1, Part IV, column 5, line 93.
Rev. 40-135
4024.4 (Cont.) FORM CMS-2552-10 DRAFT
NOTE: If you qualify for the exception in 42 CFR 413.77(e)(1) because this is the first cost reporting period in which you are training residents in approved programs and the residents were not on duty during the first month of this cost reporting period, then all direct graduate medical education costs for interns and residents in approved programs are reimbursed as a pass through based on reasonable cost.
Column 5--This column represents total inpatient other pass-through costs. Enter on each appropriate line the sum of the amounts entered on the corresponding lines in columns 1 through 4 and applicable subscripts.
Column 6--This column represents outpatient other pass-through costs. Enter on each appropriate line the sum of the amounts entered on the corresponding lines in columns 2, 3 and 4 and applicable subscripts.
Column 7--Enter on each line the charges applicable to each cost center as shown on Worksheet C, Part I, column 8.
Column 8--Divide the cost of each cost center in column 5 by the charges in column 7 for each line to determine the cost/charge ratio. Round the ratios to six decimal places, e.g., round .0321514 to .032151. Enter the resultant departmental ratio in column 8.
Column 9--This column computes the outpatient ratio of cost to charges. Divide the cost of each cost center in column 6 by the charges in column 7 for each line to determine the cost/charge ratio. Round the ratios to six decimal places, e.g., round .0321514 to .032151. Enter the resultant departmental ratio in column 9.
Column 10--Enter on each line titles V, XVIII, Part A, or XIX inpatient charges from Worksheet D‑3. Do not include in Medicare charges any charges identified as MSP/LCC.
Column 11--Multiply the ratio in column 8, by the charges in column 10, to determine the program's share of pass through costs applicable to titles V, XVIII, Part A, or XIX inpatient ancillary services, as appropriate.
For hospitals and subproviders, transfer column 11, line 200, to Worksheet D-1, Part II, column 1, line 51. If you are an IPPS hospital, also transfer this amount to Worksheet E, Part A, line 58. If you are an IPF or IPF subprovider, also transfer this amount to Worksheet E-3, Part II, line 28. If you are an IRF or IRF subprovider, also transfer this amount to Worksheet E‑3, Part III, line 29. For SNFs for title XVIII transfer the amount on line 200 to Worksheet E-3, Part VI, line 3, or titles V and XIX, SNFs, NFs and ICF/IIDs to Worksheet E-3, Part VII, line 26, as applicable.
Column 12--Enter on each line titles XVIII, Part B, V or XIX (if applicable), outpatient charges from Worksheet D, Part V, column 2, and applicable subscripts. Do not include in Medicare charges any charges identified as MSP/LCC.
Column 13--Multiply the ratio in column 9, by the charges in column 12, to determine the program's share of pass through costs applicable to titles XVIII, Part B, V or XIX (if applicable) outpatient ancillary services, as appropriate.
For providers subject to OPPS, transfer column 13, line 200, to Worksheet E, Part B, line 9.
4024.5 Part V - Apportionment of Medical and Other Health Services Costs--This worksheet provides for the apportionment of costs applicable to hospital outpatient services reimbursable under titles V, XVIII, and XIX. Title XVIII is reimbursed in accordance with 42 CFR 413.53. For services rendered on and after August 1, 2000, outpatient services are subject to outpatient PPS.
40-136 Rev.
DRAFT FORM CMS-2552-10 4024.5 (Cont.)
Enter in the appropriate cost center the program charges from the PS&R or from provider records.
Providers exempt from outpatient PPS (i.e., CAHs), complete columns 3, 4, 6 and 7. All other providers subscript columns 2 and 5 as necessary. Include charges for vaccine, i.e., pneumococcal, flu, hepatitis, and osteoporosis as indicated on line 73 below.
Exclude charges for which costs were excluded on Worksheet A-8. For example, CRNA costs reimbursed on a fee schedule are excluded from total cost on Worksheet A-8. For titles V and XIX, enter the appropriate outpatient service charges.
NOTE: Do not enter CORF, OPT, OSP, OOT, or CMHC charges on Worksheet D, Part V. Report only charges for CMHCs on Worksheet J-2.
For title XVIII, complete a separate Worksheet D, Part V, for each provider component as applicable. Enter the applicable component number in addition to the hospital provider number. Make no entries in columns 5 through 7 of this worksheet for any cost centers with a negative balance on Worksheet B, Part I, column 26. However, complete columns 1 through 4 for such cost centers.
In accordance with ACA, section 3121 as amended by the Medicare and Medicaid Extenders Act (MMEA) of 2010, section 108, the Temporary Payroll Tax Cut Continuation Act of 2011, section 308, and the Middle Class Tax Relief and Job Creation Act of 2012, section 3002, hold harmless payments are extended for rural hospitals with 100 or fewer beds through December 31, 2012; SCHs and EACHs regardless of bed size through February 29, 2012; and SCHs and EACHs with 100 or fewer beds through December 31, 2012. As such, rural hospitals and SCHs or EACHs that qualify and whose cost reporting period overlaps the effective date, (Worksheet S-2, Part I, line 120, column 1 or 2, is yes), must subscript column 2 and enter the applicable charges that correspond to the respective portion of the cost reporting period.
In accordance with ACA 2010, section 3138, cancer hospitals must utilize a predetermined payment to cost ratio (PCR) to calculate the corresponding transitional outpatient payment effective for services rendered beginning January 1, 2012. The PCR may be revised each calendar year. Where the cost reporting period overlaps a PCR revision date, subscript column 2 and the corresponding column 5 to represent the portion of the cost reporting period that corresponds to each unique PCR. See section 4030.2 for further instruction/information.
Column 1--Enter on each line in column 1 the ratio from the corresponding line on Worksheet C, column 9.
Columns 2 through 4--General Instructions--Do not include in Medicare charges any charges identified as MSP/LCC.
Column 2--PPS Reimbursed Services--Enter the charges for services rendered which are subject to the prospective payment system. These charges should not include services paid under the fee schedule such as physical therapy, speech pathology or occupational therapy. Create separate subscripted column (e.g. 2.01, 2.02) when a cost reporting period overlaps the effective dates for the various transitional corridor payments and/or when a provider experiences a geographic reclassification from urban to rural. However, no subscripting is required when a provider geographically reclassifies from rural to urban. The subscripting of this column will directly correspond to the subscripts of Worksheet E, Part B, lines 2 through 8.
Do not include in any column services excluded from OPPS because they are paid under another fee schedule, e.g., rehabilitation services and clinical diagnostic lab.
Column 3--Cost Reimbursed Services Subject to Deductibles and Coinsurance--Enter the charges for services rendered which are subject to cost reimbursement. This includes services rendered by CAHs.
Rev. 40-137
4024.5 (Cont.) FORM CMS-2552-10 DRAFT
Include the charges for drugs and supplies related to ESRD dialysis (excluding EPO and Aranesp, and any drugs or supplies paid under the composite rate), and corneal tissue on line 73.
Column 4--Cost Reimbursed Services Not Subject to Deductibles and Coinsurance--Vaccine Cost Apportionment--This column provides for the apportionment of costs which are not subject to deductible and coinsurance i.e., Pneumococcal, Influenza, Hepatitis B and Osteoporosis. Enter such charges for services which are not subject to deductible and coinsurance.
Column 5--Multiply the charges in column 2, and subscripts, if necessary, by the ratios in column 1, and enter the result. Line 200 equals the sum of lines 50 through 98.
Column 6--Multiply the charges in column 3 by the ratios in column 1, and enter the result. Line 200 equals the sum of lines 50 through 98.
Column 7--Multiply the charges in column 4 by the ratios in column 1, and enter the result. Line 200 equals the sum of lines 50 through 98.
Line Descriptions
Line 60--Generally, for title XVIII, Medicare outpatient covered clinical laboratory services are paid on a fee basis, and should not be included on this line. Outpatient CAH clinical laboratory services will be paid on a reasonable cost basis not subject to deductibles and coinsurance. In addition, hospital outpatient laboratory testing by a hospital laboratory with fewer than 50 beds in a qualified rural area will also be paid on a reasonable cost basis not subject to deductibles and coinsurance, for cost reporting periods beginning on or after July 1, 2010, but before July 1, 2012 (Patient Protection and Affordable Care Act of 2010, section 3122, amended by the MMEA, §109). For title V and XIX purposes, follow applicable State program instructions.
For CAHs, outpatient clinical laboratory diagnostic tests are paid at 101 percent of reasonable costs, and the beneficiary is not required to be physically present in the CAH at the time the specimen is collected. As such, enter the corresponding charges on this line. See MIPPA 2008, section 148 and CR 6395, transmittal 1729, dated May 8, 2009.
Line 61--Enter the program charges for provider clinical laboratory tests for which the provider reimburses the pathologist. See §4013 for a more complete description on the use of this cost center. For title XVIII, do not include charges for outpatient clinical diagnostic laboratory services. For titles V and XIX purposes, follow applicable State program instructions.
NOTE: Since the charges on line 61 are also included on line 60, laboratory, reduce the total charges to prevent double counting. Make this adjustment on line 201.
Line 71--Enter in columns 2 and 3 the charges for medical supplies charged to patients which are not paid on a fee schedule. Do not report the charges for prosthetics and orthotics.
Line 72--Enter in columns 2 and 3, the charges for implantable devices charged to patients which are not paid on a fee schedule. Do not report the charges for prosthetics and orthotics.
Line 73--Enter the program charges for drugs charged to patients. Enter in column 2, charges for vaccines and drugs reimbursed at 100 percent under OPPS. Include in column 3, charges for drugs paid at 80 percent of cost subject to deductibles and coinsurance, such as osteoporosis drugs and drugs paid under OPPS such as hepatitis vaccines. Include in column 4, vaccine charges for vaccines reimbursed at 100 percent of cost such as pneumococcal and influenza vaccines not subject to deductibles and coinsurance.
Line 74--The only renal dialysis services entered on this line are for inpatients that are not reimbursed under the composite rate regulations. (See 42 CFR 413.170.) Therefore, include only inpatient Part B charges on this line in column 3. Enter the related costs in column 6.
40-138 Rev.
DRAFT FORM CMS-2552-10 4024.5 (Cont.)
Line 75--Enter in column 3, the outpatient ASC facility charges and Part B charges for the hospital nondistinct part ambulatory surgery center. These charges represent the ASC facility charge only (i.e., in lieu of operating or recovery room charges), and do not include charges for the ancillary services provided to the patient.
Lines 88 - 93--Use these lines for outpatient service cost centers.
NOTE: For lines 88, 89 and 90, any ancillary service billed as clinic, RHC, or FQHC services must be reclassified to the appropriate ancillary cost center, e.g., radiology-diagnostic, PBP clinical lab services - program only. A similar adjustment must be made to program charges.
Line 92--Enter in column 2, the title XVIII Part B charges for observation beds. These are the charges for patients who were treated in the nondistinct observation beds and released. These patients were not admitted as inpatients.
Line 94--The only home program dialysis services which are cost reimbursed are those rendered to beneficiaries who have elected the option to deal directly with Medicare. Home program dialysis services reimbursed under the composite rate regulation (see 42 CFR 413.170) are not included on this line. This line includes costs applicable to equipment-related expenses only.
Line 95--For PPS hospital providers ambulance services are reimbursed under the ambulance fee schedule. As such, do not report charges for ambulance services rendered (column 2 for non PPS hospitals).
However, for CAHs eligible for cost reimbursement for ambulance services (billed as exempt from the ambulance fee schedule), charges for ambulance services on line 95 are transferred from your records or PS&R report type 85C. Enter charges in column 3 and multiply column 1 times column 3. Enter the result in column 6.
Lines 96 and 97--For title XVIII, DME is paid on a fee schedule through the contractor and, therefore, is not paid through the cost report.
Line 200--Enter the sum of lines 50 through 98.
Line 201--Enter in columns 3 and 4 program charges for provider clinical laboratory tests where the physician bills the provider for program patients only. Obtain this amount from line 61.
Line 202--Enter in columns 3, 4, 6, and 7, and subscripts, the amount on line 200, plus or minus the amounts on line 201, if applicable.
Transfer Referencing: For title XVIII, transfer the sum of the amounts in columns 3 and 4 and applicable subscripts, line 202, to Worksheet E, Part B, line 12 (ancillary services charges). Make no transfers of swing bed charges to Worksheet E-2 since no LCC comparison is made.
For titles V and XIX (other than IPPS), transfer the sum of the amounts in columns 2, 3, and /or 4 plus subscripts as applicable, line 202, plus the amount from Worksheet D-3, column 2, line 202, to the appropriate Worksheet E-3, Part VII, line 9.
For titles V and XIX (under IPPS), transfer the amount in columns 2, 3 and /or 4, plus subscripts as applicable, line 202, to the appropriate Worksheet E-3, Part VII, line 9.
Rev. 40-139
4024.5 (Cont.) FORM CMS-2552-10 DRAFT
NOTE: If the amount on line 202 includes charges for professional patient care services of provider-based physicians, eliminate the amount of the professional component charges from the total charges, and transfer the net amount as indicated. Submit a schedule showing these computations with the cost report.
Transfer References
Title XVIII, Titles V or XIX or
Part B Title XVIII,
From Wkst. D, Part V Swing Bed To Part B
Column 6, line 202 and column 7, N/A Wkst. E, Part B,
line 73 and subscripts col. 1 ( & subscripts), line 1
Columns 5, line 202 N/A Wkst. E, Part B,
col. 1 ( & subscripts),
line 2
Sum of columns 2, 3 and 4 as N/A Wkst. E, Part B,
applicable (SNF only), line 202 line 12 or Wkst. E-3,
Part VII, col. 1, line
9 for titles V or XIX
Sum of column 6 and 7 (SNF only) Wkst E-2 Wkst. E, Part B,
line 202 col. 2, line 3 line 1 or Wkst. E-3,
Part VII, col. 1, line 2
for titles V or XIX
40-140 Rev. 2
DRAFT FORM CMS-2552-10 4025
4025. WORKSHEET D-1 - COMPUTATION OF INPATIENT OPERATING COST
This worksheet provides for the computation of hospital inpatient operating cost in accordance with 42 CFR 413.53 (determination of cost of services to beneficiaries), 42 CFR 413.40 (ceiling on rate of hospital cost increases), and 42 CFR 412.1 through 412.125 (prospective payment). All providers must complete this worksheet.
Complete a separate copy of this worksheet for the hospital (including CAH), each subprovider, hospital-based SNF, and hospital-based other nursing facility. Also, complete a separate copy of this worksheet for each health care program under which inpatient operating costs are computed. When this worksheet is completed for a component, show both the hospital and component numbers.
At the top of each page, indicate by checking the appropriate line the health care program, provider component, and the payment system for which the page is prepared.
Worksheet D-1 consists of the following four parts:
Part I - All Provider Components
Part II - Hospital and Subproviders Only
Part III - Skilled Nursing Facility, Other Nursing Facility, and ICF/IID Only
Part IV - Computation of Observation Bed Pass Through Cost
NOTE: If you have made a swing bed election for your certified SNF, treat the SNF costs and patient days as though they were hospital swing bed-SNF type costs and patient days on Parts I and II of this worksheet. Do not complete Part III for the SNF. (See CMS Pub. 15-1, chapter 22, §2230.9B.)
Definitions
The following definitions apply to days used on this worksheet.
Inpatient Day--The number of days of care charged to a beneficiary for inpatient hospital services is always documented in units of full days. A day begins at midnight and ends 24 hours later. Use the midnight to midnight method in reporting the days of care for beneficiaries even if the hospital uses a different definition for statistical or other purposes.
A part of a day, including the day of admission, counts as a full day. However, do not count the day of discharge or death, or a day on which a patient begins a leave of absence, as a day. If both admission and discharge or death occur on the same day, consider the day a day of admission and count it as one inpatient day.
Include a maternity patient in the labor/delivery room ancillary area at midnight in the census of the inpatient routine (general or intensive) care area only if the patient has occupied an inpatient routine bed at some time since admission. Count no days of inpatient routine care for a maternity inpatient who is discharged (or dies) without ever occupying an inpatient routine bed. However, once a maternity patient has occupied an inpatient routine bed, at each subsequent census include the patient in the census of the inpatient routine care area to which she is assigned, even if the patient is located in an ancillary area (labor/delivery room or another ancillary area) at midnight. In some cases, a maternity patient may occupy an inpatient bed only on the day of discharge if the day of discharge differs from the day of admission. For purposes of apportioning the cost of inpatient routine care, count this single day of routine care as the day of admission (to routine care) and discharge. This day is considered as one day of inpatient routine care. (See CMS Pub. 15-1, chapter 22, §2205.2.)
Rev. 40-141
4025 (Cont.) FORM CMS-2552-10 DRAFT
When an inpatient is occupying any other ancillary area (e.g., surgery or radiology) at the census taking hour prior to occupying an inpatient bed, do not record the patient’s occupancy in the ancillary area as an inpatient day in the ancillary area. However, include the patient in the inpatient census of the routine care area.
When the patient occupies a bed in more than one patient care area in one day, count the inpatient day only in the patient care area in which the patient was located at the census taking hour.
Newborn Inpatient Day--Newborn inpatient days are the days that an infant occupies a newborn bed in the nursery. Include an infant remaining in the hospital after the mother is discharged who does not occupy a newborn bed in the nursery, an infant delivered outside the hospital and later admitted to the hospital but not occupying a newborn bed in the nursery, or an infant admitted or transferred out of the nursery for an illness in inpatient days. Also, include an infant born in and remaining in the hospital and occupying a newborn bed in the nursery after the mother is discharged in newborn inpatient days.
Private Room Inpatient Day--Private room inpatient days are the days that an inpatient occupies a private room. If you have only private rooms, report your days statistic as general inpatient days. Inpatient private room days are used for computing any private room differential adjustment on Worksheet D-1, Part I, if you have a mixture of different type rooms to accommodate patients. Do not count swing bed-SNF or swing bed-NF type services rendered in a private room as private room days.
Inpatient Swing Bed Days--Inpatient swing bed days are the days applicable to swing bed-SNF or swing bed-NF type services. See 413.53(a)(2)
Intensive Care Type Inpatient Days--Intensive care type inpatient days are those days applicable to services rendered in intensive care type inpatient hospital units. These units must meet the requirements specified in CMS Pub. 15-1, chapter 22, §2202.7.II.A.
NOTE: When you place overflow general care patients temporarily in an intensive care type inpatient hospital unit because all beds available for general care patients are occupied, count the days as intensive care type inpatient hospital days for purposes of computing the intensive care type inpatient hospital unit per diem. However, count the program days as general routine days in computing program reimbursement. (See CMS Pub. 15-1, chapter 22, §2217.)
Observation Beds--Observation beds, for purposes of this worksheet, are those beds in general routine areas of the hospital which are not organized as a distinct, separately staffed observation area and which are used to house patients for observation. These beds need not be used full time for observation patients. These beds are not to be confused with a subintensive care unit (i.e., definitive observation unit, a stepdown from intensive care reported as an inpatient cost center following surgical intensive care (line 34)). If you have a distinct observation bed unit (an outpatient cost center), report the costs of this unit on the subscripted line 92.01 on Worksheet A.
4025.1 Part I - All Provider Components--This part provides for the computation of the total general inpatient routine service cost net of swing bed cost and private room cost differential for each separate provider component. When this worksheet is completed for a component, show both the hospital and component numbers.
Line Descriptions
Lines 1 through 16--Inpatient days reported, unless specifically stated, exclude days applicable to newborn and intensive care type patient stays. Report separately the required statistics for the hospital, each subprovider, hospital-based SNF, hospital-based other nursing facility and ICF/IID. Obtain the information from your records and/or Worksheet S-3, Part I, columns and lines as indicated.
40-142 Rev.
DRAFT FORM CMS-2552-10 4025.1 (Cont.)
Line 1--Enter the total general routine inpatient days, including private room days, swing bed days, observation bed days, and hospice days, as applicable. Do not include routine care days rendered in an intensive care type inpatient hospital unit. Enter the total days from Worksheet S‑3, Part I, column 8, for the component and lines as indicated: hospitals from lines 7 and 28; subproviders from lines 16 through 18, as applicable, and 28, if applicable; SNFs from line 19; and NFs from line 20. If you answered yes to line 92 of Worksheet S-2, the NF days come from line 19 for the SNF level of care and line 20 for the NF level of care, and you will need to prepare a separate Worksheet D-1 for each level of care for title XIX.
Line 2--Enter the total general routine inpatient days. Include private room days and exclude swing bed and newborn days. Hospitals enter the sum of the days entered on Worksheet S-3, Part I, column 8, lines 1 and 28. Subproviders, SNFs, and NFs enter the days from line 1 of this worksheet.
Line 3--Enter the total private room days excluding swing bed private room days and observation bed days. If you have only private room days, do not complete this line.
Line 4--Enter the result of line 2, minus line 3, minus total observation bed days from Worksheet S‑3, Part I, column 8, line 28. The result will be semi-private room days exclusive of swing bed semi-private room days and observation bed days. If you have only private room days, such days will be included in this line.
NOTE: For purposes of this computation, the program does not distinguish between semi‑private and ward accommodations. (See CMS Pub. 15-1, chapter 22, §2207.3.)
Line 5--Enter the total swing bed-SNF type inpatient days, including private room days, through December 31 of your cost reporting period. If you are on a calendar year end, report all swing bed-SNF type inpatient days.
Line 6--Enter the total swing bed-SNF type inpatient days, including private room days, after December 31 of your cost reporting period. If you are on a calendar year end, enter zero. The sum of lines 5 and 6 equals Worksheet S-3 Part I, line 5, column 8.
Line 7--Enter the total swing bed-NF type inpatient days, including private room days, through December 31 of your cost reporting period. If you are on a calendar year end, report all swing bed-NF type inpatient days. This line includes title V, title XIX, and all other payers.
Line 8--Enter the total swing bed-NF type inpatient days, including private room days, after December 31 of your cost reporting period. If you are on a calendar year end, enter zero. This line includes title V, title XIX, and all other payers. The sum of lines 7 and 8 equals Worksheet S-3, Part I, line 6, column 8.
NOTE: Obtain the amounts entered on lines 5 and 7 from your records.
Line 9--Enter the total program general routine inpatient days as follows:
Type of Provider From
Hospital Wkst. S-3, Part I, cols. 5, 6, or 7, line 1
Subprovider Wkst. S-3, Part I, cols. 5, 6, or 7, line 16, 17, or 18 as applicable
SNF Wkst. S-3, Part I, cols. 5, 6, or 7, line 19
NF Wkst. S-3, Part I, cols. 5, 6, or 7, for SNF only level of care; line 19. If line 92 of Wkst S-2, Part I is a “Y”, two D-1s must be completed for title XIX using line 19 for SNF level of care and line 20 for the NF level of care; or line 20 only for NF level of care.
Rev. 40-143
4025.1 (Cont.) FORM CMS-2552-10 DRAFT
Include private room days and exclude swing bed and newborn days for each provider component. Add any program days for general care patients of the component who temporarily occupied beds in an intensive care or other special care unit. (See CMS Pub. 15-1, chapter 22, §2217.)
NOTE: If Worksheet S-2, line 92 columns 1 or 2, as applicable is “Y” for yes, then Worksheet D-1 for title XIX (for the SNF and NF component) must be completed. The results are to be combined and transferred to title XIX SNF, Worksheet E-3, Part VII, line 1.
Line 10--Enter the title XVIII swing bed-SNF type inpatient days, including private room days, through December 31 of your cost reporting period. If you are on a calendar year end, report all program swing bed-SNF type inpatient days. Combine titles V and XIX for all SNF lines if your State recognizes only SNF level of care.
Line 11--Enter the title XVIII swing bed-SNF type inpatient days, including private room days, after December 31 of your cost reporting period. If you are on a calendar year end, enter zero.
Line 12--Enter the total titles V or XIX swing bed-NF type inpatient days, including private room days, through December 31 of your cost reporting period. If you are on a calendar year end, report all program swing bed-NF type inpatient days.
Line 13--Enter the total titles V or XIX swing bed-NF type inpatient days, including private room days, after December 31 of your reporting period. If you are on a calendar year end, enter zero.
NOTE: If you are participating in both titles XVIII and XIX, complete, at a minimum, a separate Worksheet D-1, Part I, for title XIX, lines 9, 12, and 13. If these data are not supplied, the cost report is considered incomplete and is rejected.
Line 14--Enter the total medically necessary private room days applicable to the program, excluding swing bed days, for each provider component.
Line 15--Enter, for titles V or XIX only, the total nursery inpatient days from Worksheet S-3, Part I, column 8, line 13.
Line 16--Enter, for titles V or XIX only, the total nursery inpatient days applicable to the program from Worksheet S-3, Part I, columns 5 and 7, respectively, line 13.
Lines 17 through 27--These lines provide for the carve out of reasonable cost of extended care services furnished by a swing bed hospital. Under the carve out method, the total costs attributable to SNF type and NF type routine services furnished to all classes of patients are subtracted from total general inpatient routine service costs before computing the average cost per diem for general routine hospital care. The rates on lines 17 through 20 are supplied by your contractor.
Line 17--Enter the Medicare swing-bed SNF rate applicable to the calendar year in which inpatient days on line 5 occurred. If the swing-bed SNF rate for the prior calendar year is higher, enter that rate instead. (See CMS Pub. 15-1, chapter 22, §2230ff.) Critical access hospitals do not complete this line.
Line 18--Enter the Medicare swing-bed SNF rate applicable to the calendar year in which inpatient days on line 6 occurred. If the swing-bed SNF rate for the prior calendar year is higher, enter that rate instead. (See CMS Pub. 15-1, chapter 22, §2230ff.) Critical access hospitals do not complete this line.
40-144 Rev.
DRAFT FORM CMS-2552-10 4025.1 (Cont.)
Line 19--Enter the average Statewide rate per patient day paid under the State Medicaid plan for routine services furnished by nursing facilities (other than NFs for individuals with intellectual disabilities) in that State. This rate is approximated by taking the average rate from the prior calendar year (i.e. the calendar year preceding the year relating to inpatient days reported on line 7), updated to approximate the current year rate. Obtain the proper rate from your contractor.
Line 20--Enter the average Statewide rate per patient day paid under the State Medicaid plan for routine services furnished by nursing facilities (other than NFs for individuals with intellectual disabilities) in that State. This rate is approximated by taking the average rate from the prior calendar year (i.e. the calendar year preceding the year relating to inpatient days reported on line 8), updated to approximate the current year rate. Obtain the proper rate from your contractor.
Line 21--Enter the total general inpatient routine service costs for the applicable provider component.
For titles V, XVIII, and XIX, enter the amounts from Worksheet C, Part I, line 30, for adults and pediatrics or lines 40, 41, or 42, as applicable for the subprovider, as appropriate:
COST or OTHER Inpatient - Column 1 (includes CAHs)
TEFRA Inpatient - Column 3 (includes cancer and children’s hospitals)
PPS Inpatient - Column 5 (includes acute, IPFs, IRFs, & LTCHs)
SNF/NF Inpatient Routine--For title XVIII, transfer this amount from Worksheet C, Part I, column 5, line 44 (SNF). For titles V and XIX, transfer this amount from Worksheet B, Part I, column 26, line 45 (NF) or 45.01 ICF/IID.
Line 22--Enter the product of the days on line 5 multiplied by the amount on line 17.
Line 23--Enter the product of the days on line 6 multiplied by the amount on line 18.
Line 24--Enter the product of the days on line 7 multiplied by the amount on line 19.
Line 25--Enter the product of the days on line 8 multiplied by the amount on line 20.
Line 26--Enter the sum of the amounts on lines 22 through 25. This amount represents the total reasonable cost for swing bed-SNF type and NF type inpatient services.
For critical access hospitals, subtract the sum of lines 24 and 25 from the amount reported on line 21. Divide that result by the patient days equal to lines 2, 5, and 6 above to arrive at a per diem (retain this amount for the calculation required on lines 38, 64 and 65). Multiply the per diem by the total days reported on lines 5 and 6. Add that result to the amounts reported on lines 24 and 25.
Line 27--Subtract the amount on line 26 from the amount on line 21. This amount represents the general inpatient routine service cost net of swing bed-SNF type and NF type inpatient costs.
Lines 28 through 36--All providers must complete lines 28 through 36. PPS providers complete these lines for data purposes only. However, if line 4 equals line 2 above, or if line 3 above is zero, you are not to complete these lines.
Line 28--Enter the total charges for general inpatient routine services, excluding charges for swing bed-SNF type and NF type inpatient services and observation bed days (from your records).
Rev. 40-145
4025.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 29--Enter the total charges for private room accommodations, excluding charges for private room accommodations for swing bed-SNF type and NF type inpatient services and observation bed days (from your records).
Line 30--Enter the total charges for semi-private room and ward accommodations, excluding semi-private room accommodation charges for swing bed-SNF type and NF type services (from your records).
Line 31--Enter the general inpatient routine cost to charge ratio (rounded to six decimal places) by dividing the total inpatient general routine service costs (line 27) by the total inpatient general routine service charges (line 28).
Line 32--Enter the average per diem charge (rounded to two decimal places) for private room accommodations by dividing the amount on line 29 by the days on line 3.
Line 33--Enter the average per diem charge (rounded to two decimal places) for semi-private accommodations by dividing the amount on line 30 by the days on line 4.
Line 34--Subtract the average per diem charge for all semi-private accommodations (line 33) from the average per diem charge for all private room accommodations (line 32) to determine the average per diem private room charge differential. If a negative amount results from this computation, enter zero on line 34.
Line 35--Multiply the average per diem private room charge differential (line 34) by the inpatient general routine cost to charge ratio (line 31) to determine the average per diem private room cost differential (rounded to two decimal places).
Line 36--Multiply the average per diem private room cost differential (line 35) by the private room accommodation days (excluding private room accommodation days applicable to swing bed-SNF type and NF type services) (line 3) to determine the total private room accommodation cost differential adjustment.
Line 37--Subtract the private room cost differential adjustment (line 36) from the general inpatient routine service cost net of swing bed-SNF type and NF type costs (line 27) to determine the adjusted general inpatient routine service cost net of swing bed-SNF type service costs, NF type service costs, and the private room accommodation cost differential adjustment. If line 4 equals line 2, enter the amount from line 27 above.
4025.2 Part II - Hospital and Subproviders Only--This part provides for the apportionment of inpatient operating costs to titles V, XVIII, and XIX and the calculation of program excludable cost for all hospitals and subproviders. For hospitals reimbursed under TEFRA, it provides for the application of a ceiling on the rate of cost increase for the hospital and subproviders. When the worksheet is completed for a component, show both the hospital and component numbers.
CAHs are also required to complete this worksheet.
Line Descriptions
Line 38--For non-IPPS providers, (includes CAHs), divide the adjusted general inpatient routine service cost (line 37) by the total general inpatient routine service days including private room (excluding swing bed and newborn) days (line 2) to determine the general inpatient routine service average cost per diem (rounded to two decimal places).
For PPS providers (includes IRFs, IPFs, and LTCHs under 100 percent PPS), divide the sum of lines 36 and 37, by the inpatient days reported on line 2.
40-146 Rev.
DRAFT FORM CMS-2552-10 4025.2 (Cont.)
For CAHs the per diem, unless there is an adjustment for private room differential, should be equal to the per diem calculated in the formula on line 26. If this is a CAH and there is a private room differential, process as a non-PPS provider.
Line 39--Multiply the total program inpatient days including private room (excluding swing bed and newborn) days (line 9) by the adjusted general inpatient routine service average cost per diem (line 38) to determine the general inpatient service cost applicable to the program.
Line 40--Multiply the medically necessary private room (excluding swing bed) days applicable to the program (line 14) by the average per diem private room cost differential (line 35) to determine the reimbursable medically necessary private room cost applicable to the program. PPS providers including IRF, IPF and LTCH, reimbursed at 100 percent Federal rate enter zero.
Line 41--Add lines 39 and 40 to determine the total general inpatient routine service cost applicable to the program.
Line 42--This line is for titles V and XIX only and provides for the apportionment of your inpatient routine service cost of the nursery, as appropriate.
Column 1--Enter the total inpatient cost applicable to the nursery from Worksheet C, Part I, line 43.
TEFRA, COST, or OTHER Inpatient Column 3
PPS Inpatient, or IPF, IRF, and LTCH PPS Column 5
Column 2--Enter the total inpatient days applicable to the nursery from line 15.
Column 3--Divide the total inpatient cost in column 1 by the total inpatient days in column 2 (rounded to two decimal places).
Column 4--Enter the program nursery days from line 16.
Column 5--Multiply the average per diem cost in column 3 by the program nursery days in column 4.
Lines 43 through 47--These lines provide for the apportionment of the hospital inpatient routine service cost of intensive care type inpatient hospital units (excluding nursery) to the program.
Column 1--Enter on the appropriate line the total inpatient routine cost applicable to each of the indicated intensive care type inpatient hospital units from Worksheet C, Part I, lines 31 through 35, as appropriate.
TEFRA, COST, or OTHER Inpatient Column 3
PPS Inpatient, or IPF, IRF and LTCH PPS Column 5
Column 2--Enter on the appropriate line the total inpatient days applicable to each of the indicated intensive care type inpatient units. Transfer these inpatient days from Worksheet S-3, Part I, column 8, lines 8 through 12, as appropriate.
Column 3--For each line, divide the total inpatient cost in column 1 by the total inpatient days in column 2 (rounded to two decimal places).
Column 4--Enter on the appropriate line the program days applicable to each of the indicated intensive care type inpatient hospital units. Transfer these inpatient days from Worksheet S-3, Part I, columns 5, 6, or 7, as appropriate, lines 8 through 12.
Rev. 40-147
4025.2 (Cont.) FORM CMS-2552-10 DRAFT
NOTE: When you place overflow general care patients temporarily in an intensive care type inpatient hospital unit because all beds available for general care patients are occupied, count the days as intensive care type unit days for the purpose of computing the intensive care type unit per diem. The days are included in column 2. However, count the program days as general routine days in computing program reimbursement. Enter the program days on line 9 and not in column 4, lines 43 through 47, as applicable. (See CMS Pub. 15-1, chapter 22, §2217.)
Column 5--Multiply the average cost per diem in column 3 by the program days in column 4.
Line 48--Enter the total program inpatient ancillary service cost from the appropriate Worksheet D-3, column 3, line 200.
Line 49--Enter the sum of the amounts on lines 41 through 48. When this worksheet is completed for components, neither subject to prospective payment, nor subject to the target rate of increase ceiling (i.e., "Other" box is checked), transfer this amount to Worksheet E-3, Part V, line 1, or Part VII, line 1, as appropriate. Do not complete lines 50-63.
For all inclusive rate providers (Method E) apply the percentage to the sum of the aforementioned lines (lines 41 through 48) based on the provider type designated on Worksheet S-2, column 4, line 3 (see CMS Pub. 15-1, chapter 22, §2208).
Lines 50-53--These lines compute total program inpatient operating cost less program capital-related, nonphysician anesthetists, and approved medical education costs. Complete these lines for all provider components.
Line 50--Enter on the appropriate worksheet the total pass through costs including capital-related costs applicable to program inpatient routine services. Transfer capital-related inpatient routine cost from Worksheet D, Part I, column 7, sum of lines 30 through 35 and line 43 for the hospital, and line 40, 41, or 42, as applicable, for the subprovider. Add that amount to the other pass through costs from Worksheet D, Part III, column 9, sum of lines 30 through 35 and line 43 for the hospital, and line 40, 41, or 42, as applicable, for the subprovider.
Line 51--Enter the total pass through costs including capital-related costs applicable to program inpatient ancillary services. Transfer capital-related inpatient ancillary costs from Worksheet D, Part II, column 5, line 200. Add that amount to the other pass through costs from Worksheet D, Part IV, column 11, line 200.
Line 52--Enter the sum of lines 50 and 51.
Line 53--Enter total program inpatient operating cost (line 49) less program capital-related, nonphysician anesthetists (if appropriate), and approved medical education costs (line 52).
Lines 54 through 63--Except for those hospitals specified below, all hospitals (and distinct part hospital units) excluded from prospective payment are reimbursed under cost reimbursement principles and are subject to the ceiling on the rate of hospital cost increases (TEFRA). (See 42 CFR 413.40.) CAHs do not complete these lines as reimbursement is based on reasonable cost. The following hospitals are reimbursed under special provisions and, therefore, are not generally subject to TEFRA or prospective payment:
Hospitals reimbursed under approved State cost control systems (see 42 CFR 403.300 through 403.322);
Nonparticipating hospitals furnishing emergency services to Medicare beneficiaries.
40-148 Rev.
DRAFT FORM CMS-2552-10 4025.2 (Cont.)
For your components subject to the prospective payment system or not otherwise subject to the rate of increase ceiling as specified above, make no entries on lines 54 through 63.
NOTE: A new non-PPS hospital or subprovider (lines 85 and/or 86 of Worksheet S-2 with a “Y” response) is cost reimbursed for all cost reporting periods through the end of its first 12 month cost reporting period. The 12 month cost reporting period also becomes the TEFRA base period unless an exemption under 42 CFR 413.40 (f) is granted. If such an exemption is granted, cost reimbursement continues through the end of the exemption period. The last 12 month period of the exemption is the TEFRA base period.
Line 54--Enter the number of program discharges including deaths (excluding newborn and DOAs) for the component from Worksheet S-3, Part I, columns 12 through 14 (as appropriate), lines 14 and 16 through 18 (as appropriate). A patient discharge, including death, is a formal release of a patient.
Line 55--Enter the target amount per discharge as obtained from your contractor. The target amount establishes a limitation on allowable rates of increase for hospital inpatient operating cost. The rate of increase ceiling limits the amount by which your inpatient operating cost may increase from one cost reporting period to the next. (See 42 CFR 413.40.)
Line 56--Multiply the number of discharges on line 54 by the target amount per discharge on line 55 to determine the rate of increase ceiling.
Line 57--Subtract line 53 from line 56 to determine the difference between adjusted inpatient operating cost and the target amount.
Line 58 through 62--This line provides incentive payments when your cost per discharge for the cost reporting period subject to the ceiling is less than the applicable target amount per discharge. In addition bonus payments are provided for hospitals who have received PPS exempt payments for three or more previous cost reporting periods and whose operating costs are less than the target amount, expected costs (lesser of actual costs or the target amount for the previous year), or trended costs (lesser of actual operating costs or the target amount in 1996; or for hospitals where its third full cost reporting period was after 1996 the inpatient operating cost per discharge), updated and compounded by the market basket. It also provides for an adjustment when the cost per discharge exceeds the applicable target amount per discharge. If line 57 is zero, enter zero on lines 58 through 62. New providers skip lines 58 through 62, and go to line 63.
Line 58--If line 57 is a positive amount (actual inpatient operating cost is less than the target amount), enter on line 58 the lesser of 15 percent of line 57 or 2 percent of line 56. If line 57 is negative, do not complete line 58 (leave blank), however, complete line 62 for calculation of any adjustments to the operating costs.
Line 59--Enter the inpatient operating cost per discharge updated and compounded by the market basket for each year through the current reporting year.
Line 60--Enter from the prior year cost report, the lesser of the hospital’s inpatient operating cost per discharge (line 53/line 54) or line 55, updated by the market basket.
Line 61--If (line 53/line 54) is less than the lower of lines 55, 59 or 60, enter the lesser of 50 percent of the amount by which operating costs (line 53) are less than expected costs (line 54 times line 60), or 1 percent of the target amount (line 56); otherwise enter zero. (42 CFR 413.40(d)(4)(i))
Rev. 40-149
4025.2 (Cont.) FORM CMS-2552-10 DRAFT
Line 62--If line 57 is a negative amount (actual inpatient operating cost is greater than the target amount) and line 53 is greater than 110 percent of line 56, enter on this line the lesser of (1) or (2): (1) 50 percent of the result of (line 53 minus 110 percent of line 56), or (2) 10 percent of line 56; otherwise enter zero. (42 CFR 413.40(d)(3))
Line 63--Allowable Cost Plus incentive Payment--If line 57 is a positive amount, enter the sum of lines 52, 53, 58, and 61 (if applicable). If line 57 is a negative amount enter the sum of lines 52, 56, and 62. If line 57 is zero, enter the sum of lines 52 and 56. New providers enter the lesser of lines 53 or 56 plus line 52.
Line 64--Enter the amount of Medicare swing bed-SNF type inpatient routine cost through December 31 of the cost reporting period. Determine this amount by multiplying the program swing bed-SNF type inpatient days on line 10 by the rate used on line 17. For CAHs multiply line 10 times the per diem calculated on line 38.
Line 65--Enter the amount of Medicare swing bed-SNF type inpatient routine cost for the period after December 31 of the cost reporting period. Determine this amount by multiplying the program swing bed-SNF type inpatient days on line 11 by the rate used on line 18. For CAHs multiply line 11 times the per diem calculated on line 38.
Line 66--Enter the sum of lines 64 and 65. For CAHs only transfer this amount to Worksheet E‑2, column 1, line 1.
Line 67--Enter the amount of titles V or XIX swing bed-NF type inpatient routine cost through December 31 of the cost reporting period. Determine this amount by multiplying the program swing bed-NF type inpatient days on line 12 by the rate used on line 19.
Line 68--Enter the amount of titles V or XIX swing bed-NF type inpatient routine cost for the period after December 31 of the cost reporting period. Determine this amount by multiplying the program swing bed-NF type inpatient days on line 13 by the rate used on line 20.
Line 69--Enter the sum of lines 67 and 68. Transfer this amount to the appropriate Worksheet E‑2, column 1, line 2. If your state recognizes only one level of care obtain the amount from line 66.
4025.3 Part III - Skilled Nursing Facility, Other Nursing Facility, and Intermediate Care Facility for Individuals with Intellectual Disabilities Only--This part provides for the apportionment of inpatient operating costs to titles V, XVIII, and XIX. Hospital-based SNFs complete lines 70 through 74 and 83 through 86 for data purposes only as SNFs are reimbursed under SNF PPS for title XVIII. Complete lines 70-89 for titles V and XIX. When this worksheet is completed for a component, show both the hospital and component numbers. Any reference to the nursing facility will also apply to the ICF/IID unit.
Line Descriptions
Line 70--Enter the hospital-based SNF or other nursing facility routine service cost from Part I, line 37.
Line 71--Calculate the adjusted general inpatient routine service cost per diem by dividing the amount on line 70 by inpatient days, including private room days, shown on Part I, line 2.
Line 72--Calculate the routine service cost by multiplying the program inpatient days, including the private room days in Part I, line 9, by the per diem amount on line 71.
40-150 Rev.
DRAFT FORM CMS-2552-10 4025.3 (Cont.)
Line 73--Calculate the medically necessary private room cost applicable to the program by multiplying the days shown in Part I, line 14, by the per diem in Part I, line 35.
Line 74--Add lines 72 and 73 to determine the total reasonable program general inpatient routine service cost.
Lines 75 through 82--Apportionment of Inpatient Operating Costs for Other Nursing Facilities (NF)--These lines are used for titles V and/or XIX only. For title XVIII Medicare, skip lines 75 through 82, and continue with line 83.
Line 75--Enter the capital-related cost allocated to the general inpatient routine service cost center. For titles V and XIX, transfer this amount from Worksheet B, Part II, column 26, line 45 (NF).
Line 76--Calculate the per diem capital-related cost by dividing the amount on line 75 by the days in Part I, line 2.
Line 77--Calculate the program capital-related cost by multiplying line 76 by the days in Part I, line 9.
Line 78--Calculate the inpatient routine service cost by subtracting line 77 from line 74.
Line 79--Enter the aggregate charges to beneficiaries for excess costs obtained from your records.
Line 80--Enter the total program routine service cost for comparison to the cost limitation. Obtain this amount by subtracting line 79 from line 78.
Line 81--Enter the inpatient routine service cost per diem limitation. This amount is provided by your state contractor.
Line 82--Enter the inpatient routine service cost limitation. Obtain this amount by multiplying the number of inpatient days shown on Part I, line 9 by the cost per diem limitation on line 81.
Line 83--For titles V and XIX, enter the amount of reimbursable inpatient routine service cost determined by adding line 77 to the lesser of line 80 or line 82. If you are a provider not subject to the inpatient routine service cost limit, enter the sum of lines 77 and 80. For title XVIII, enter the amount from line 74.
Line 84-- Enter the program ancillary service amount from Worksheet D-3, column 3, line 200.
Line 85--Enter (only when Worksheet D-1 is used for a hospital-based SNF and NF) the applicable program's share of the reasonable compensation paid to physicians for services on utilization review committees to an SNF and/or NF. Include the amount eliminated from total costs on Worksheet A-8, line 25. If the utilization review costs are for more than one program, the sum of all the Worksheet D-1 amounts reported on this line must equal the amount adjusted on Worksheet A-8, line 25.
Line 86--Calculate the total program inpatient operating cost by adding the amounts on lines 83 through 85. Transfer this amount to the appropriate Worksheet E-3, Part VII, line 1 except for SNFs subject to SNF PPS. For NF and ICF/IID, transfer this amount to Worksheet E-3, Part VII, line 1 for titles V and XIX.
Rev. 40-151
4025.4 FORM CMS-2552-10 DRAFT
4025.4 Part IV - Computation of Observation Bed Pass Through Cost--This part provides for the computation of the total observation bed costs and the portion of costs subject to reimbursement as a pass through cost for observation beds that are only in the general acute care routine area of the hospital. For title XIX, insert the amount calculated for title XVIII for the hospital, if applicable. To avoid duplication of reporting observation bed costs, do not transfer the title XIX amount to Worksheet C.
Line 87--Transfer the total observation bed days from Worksheet S-3, Part I, column 8, line 28. NOTE: Observation days are only recognized and reported in the inpatient routine area of the hospital.
Line 88--Calculate the result of general inpatient routine cost on line 27 divided by line 2.
Line 89--Multiply the number of days on line 87 by the cost per diem on line 88 and enter the result. Transfer this amount to Worksheet C, Parts I and II, column 1, line 92.
Lines 90 through 93--These lines compute the observation bed costs used to apportion the routine pass through costs and capital-related costs associated with observation beds for PPS, TEFRA, and new children’s and new cancer providers. Lines 90 through 93 correspond to specific medical education programs reported on Worksheet D, Part III, columns 1, 2, and 3, respectively.
Column 1--For line 90, transfer the amount from Worksheet D, Part I, column 1, line 30, for the hospital. For line 91 through 93, enter the cost from Worksheet D, Part III, columns 1, 2 and 3, line 30.
Column 2--Enter on each line the general inpatient routine cost from line 27. Enter the same amount on each line.
Column 3--Divide column 1 by column 2, for each line, and enter the result. If there are no costs in column 1, enter 0 in column 3.
Column 4--Enter the total observation cost from line 89. Enter the same amount on each line.
Column 5--Multiply the ratio in column 3 by the amount in column 4. Use this cost to apportion routine pass through costs associated with observation beds on Worksheet D, Parts II and IV.
Transfer the amount in column 5:
From To To
Wkst. D-1, Part IV Wkst. D, Part II Wkst D, Part IV
Col. 5, line 90 Col. 1, line 92
Col. 5, line 91 Col. 2, line 92
Col. 5, line 92 Col. 3, line 92
Col. 5, line 93 Col. 4, line 92
40-152 Rev.
12-10 FORM CMS-2552-10 4026.1
4026. WORKSHEET D-2 - APPORTIONMENT OF COST OF SERVICES RENDERED BY INTERNS AND RESIDENTS
4026.1 Part I - Not in Approved Teaching Program.--Use this part only if you have interns and residents who are not in an approved teaching program. (See CMS Pub. 15-1, chapter 4.) If you have more than one hospital-based outpatient rehabilitation provider, subscript line 17 to accommodate reporting data for each.
Column 1--Enter the percentage of time that interns and residents are assigned to each of the indicated patient care areas on lines 1 through 19 and 21 through 26 (from your records).
Column 2--Enter on line 1 the total cost of services rendered in all patient care areas from Worksheet B, Part I, column 26, line 100. Multiply the amount in column 1 by the total cost in column 2, line 1. Enter the resulting amounts on the appropriate lines in column 2.
Inpatient
Column 3--Enter the total inpatient days applicable to the various patient care areas of the complex.
Inpatient Days From
Description Enter in Col. 3 Worksheet D-1
Adults & Pediatrics line 2 Part I, col. 1, line 1
Intensive Care Unit line 3 Part II, col. 2, line 43
Coronary Care Unit line 4 Part II, col. 2, line 44
Burn Intensive Care Unit line 5 Part II, col. 2, line 45
Surgical Intensive
Care Unit line 6 Part II, col. 2, line 46
Other Intensive Care
Type Unit line 7 Part II, col. 2, line 47
Nursery line 8 S-3, Part I, col. 8, line 13
IPF - Inpatient Routine line 10 Part I, col. 1, line 1
IPF - Inpatient Routine line 11 Part I, col. 1, line 1
Subprovider line 12 Part I, col. 1, line 1
SNF line 13 Part I, col. 1, line 1
NF line 14 Part I, col. 1, line 1
Column 4--Divide the allocated expenses in column 2 by the inpatient days in column 3 to arrive at the average per diem cost for each cost center.
For swing bed-SNF or swing bed-NF facilities, transfer the per diem amount in column 4, line 2, to Worksheet E-2, column 1 (for titles V and XIX) or column 2 (for title XVIII), line 4.
Rev. 1 40-153
4026.1 (Cont.) FORM CMS-2552-10 12-10
Columns 5, 6, and 7--Enter in the appropriate column the health care program inpatient days for each patient care area.
Titles V and XIX
Enter in column 5 for
title V or column 7
Description for title XIX From Worksheet D-1
Adults & Pediatrics line 2 Part I, col. 1, line 9
Intensive Care Unit line 3 Part II, col. 4, line 43
Coronary Care Unit line 4 Part II, col. 4, line 44
Burn Intensive Care line 5 Part II, col. 4, line 45
Unit
Surgical Intensive line 6 Part II, col. 4, line 46
Care Type Unit
Other Intensive line 7 Part II, col. 4, line 47
Care Type Unit
Nursery line 8 Part II, col. 4, line 42
IPF - Inpatient Routine line 10 Part I, col. 1, line 1
IRF - Inpatient Routine line 11 Part I, col. 1, line 1
Subprovider line 12 Part I, col. 1, line 1
SNF line 13 Part I, col. 1, line 1
NF line 14 Part I, col. 1, line 1
Title XVIII--Enter in column 6, lines 2 through 13, as appropriate, the total number of days in which beneficiaries were inpatients of the provider and had Medicare Part B coverage. Such days are determined without regard to whether Part A benefits were available. Submit a reconciliation with the cost report demonstrating the computation of Medicare Part B inpatient days. The following reconciliation format is recommended:
Part A Part A Coverage Medicare
Cost Inpatient plus Part B minus But No Part B = Part B
Center Days Only Days Days Coverage Days
Part A Inpatient Days--Enter the Medicare Part A inpatient days from Worksheet D-1.
Cost Center From Worksheet D-1
Adults & Pediatrics Part I, column 1, line 9
Intensive Care Unit Part II, column 4, line 43
Coronary Care Unit Part II, column 4, line 44
Burn Intensive Care Type Unit Part II, column 4, line 45
Surgical Intensive Care Type Unit Part II, column 4, line 46
Other Intensive Care Type Unit Part II, column 4, line 47
IPF - Inpatient Routine Part I, column 1, line 9
IRF - Inpatient Routine Part I, column 1, line 9
Subprovider Part I, column 1, line 9
Skilled Nursing Facility Part I, column 1, line 9
Part B Only Days--Enter the total number of days from your records in which inpatients were covered under Medicare Part B but did not have Part A benefits available.
No Part B Days--Enter the total number of days from your records in which inpatients were covered under Medicare Part A but did not have Part B benefits available.
40-154 Rev. 1
DRAFT FORM CMS-2552-10 4026.1 (Cont.)
Columns 8, 9, and 10--Multiply the average cost per day in column 4 by the health care program days in columns 5, 6, and 7, respectively. Enter the resulting amounts in columns 8, 9, and 10, as appropriate, for each cost center.
Outpatient
Column 3--Enter the total charges applicable to each outpatient service area. Obtain the total charges from Worksheet C, column 8, lines 88 through 93.
Column 4--Compute the total outpatient cost to charge ratio by dividing costs in column 2 by charges in column 3 for each cost center.
Columns 5, 6, and 7--Enter in these columns program charges for outpatient services. Do not include in Medicare charges any charges identified as MSP/LCC.
Titles V and XIX:
Sum of _
Enter in col. 5 for Worksheet D, Part V,
title V or col. 7 Worksheet D-3, sum of cols. 2 - 4
Description for title XIX col. 2 (& applicable subscripts)
RHC line 21 line 88 line 88
FQHC line 22 line 89 line 89
Clinic line 23 line 90 line 90
Emergency line 24 line 91 line 91
Observation Beds line 25 line 92 line 92
Other Outpatient line 26 line 93 line 93
Title XVIII:
From
Enter in col. Worksheet D, Part V
6 for Title Worksheet cols. 2 - 4 Less Part A
Description XVIII D-3, col. 2 (& applicable subscripts) Only Charges
RHC line 21 line 88 plus line 88 minus
FQHC line 22 line 89 plus line 89 minus From
Clinic line 23 line 90 plus line 90 minus Provider
Emergency line 24 line 91 plus line 91 minus Records
Observation Beds line 25 line 92 plus line 92 minus
Other Outpatient line 26 line 93 plus line 93 minus
NOTE: Submit a reconciliation worksheet with the cost report showing the computations used for the charges for column 6.
If you have subproviders, the amounts entered in these columns are the sum of the hospital and subprovider Worksheets D-3 and D, Part V.
Columns 8, 9, and 10, lines 21-26--Compute program outpatient costs for titles V and XIX and title XVIII, Part B cost by multiplying the cost to charge ratio in column 4 by the program outpatient charges in columns 5, 6, and 7. Enter the resulting amounts in columns 8, 9, and 10, as appropriate, for each cost center.
Rev. 40-155
4026.1 (Cont.) FORM CMS-2552-10 DRAFT
Transfer program expenses.
From Title V (Column 8)/Title XIX (Column 10)
Hospital: Sum of lines 9 and 27 TO Worksheet E-3, Part VII, line 19
Subprovider: lines 10-12, as applicable TO Worksheet E-3, Part VII, line 19
Other Nursing Facility: line 14 TO Worksheet E-3, Part VII, line 19
From Title XVIII (Column 9) (only if Part II is not utilized)
Hospital: Sum of lines 9 and 27 TO Worksheet E, Part B, line 22
Subprovider: line 10-12, as applicable TO Worksheet E, Part B, line 22
Skilled Nursing Facility: line 13 TO Worksheet E, Part B, line 22
4026.2 Part II - In An Approved Teaching Program (Title XVIII, Part B Inpatient Routine Costs Only)--This part provides for reimbursement for inpatient routine services rendered by interns and residents in approved teaching programs to Medicare beneficiaries who have Part B coverage and are not entitled to benefits under Part A. (See CMS Pub. 15-1, chapter 4, and chapter 21, §2120.) Do not complete this section unless you qualify for the new teaching hospital exception for graduate medical education payments in 42 CFR 413.77(e)(1).
Column 1--Enter the amounts allocated in the cost finding process to the indicated cost centers. Obtain these amounts from Worksheet B, Part I, sum of the amounts in columns 21 and 22, as adjusted for any post stepdown adjustments applicable to interns and residents in approved teaching programs.
Column 2--Enter the adjustment for interns and residents costs applicable to swing bed services but allocated to hospital routine cost. Compute these amounts as follows:
Interns and
Swing Residents Costs Total
Inpatient = Allocated to Swing
Bed Adults & times Bed divided Total
Amount Pediatrics Days by Days
For line Wkst. D-2, Wkst. D-1, Wkst. D-1,
30 (SNF) col. 1, line 29 sum of lines 5 line 1
and 6
For line Wkst. D-2, Wkst. D-1, Wkst. D-1,
31 (NF) col. 1, line 29 sum of lines 7 line 1
and 8
The amount subtracted from line 29 must equal the sum of the amounts computed for lines 30 and 31.
40-156 Rev.
DRAFT FORM CMS-2552-10 4026.3
If you have swing beds in your IPF subprovider, complete line 38 to adjust for swing bed costs. Compute the swing bed amounts as explained above except that the interns and residents costs allocated to adults and pediatrics (line 38) comes from Worksheet D-2, column 1, line 38. The amount subtracted from line 38 must equal the sum of subscripts of line 38, as applicable. If you have swing beds in your IRF subprovider, complete line 39 to adjust for swing bed costs. Compute the swing bed amounts as explained above except that the interns and residents costs allocated to adults and pediatrics (line 39) comes from Worksheet D-2, column 1, line 39. The amount subtracted from line 39 must equal the sum of subscripts of line 39, as applicable.
Column 3--Enter on lines 29 and 38 through 40, as applicable, the amounts in column 1 minus the amount in column 2. Enter on line 30 the amount from column 2. Enter on lines 32 through 36 and 41 the amounts from column 1.
Column 4--Enter the total inpatient days applicable to the various patient care areas of the complex. (See instructions for Part I, column 3. For line 30, this is from Worksheet D-1, sum of lines 5 and 6.)
Column 5--Divide the allocated expense in column 3 by the inpatient days in column 4 to arrive at the average per diem cost for each cost center.
Column 6--Enter on lines 29, 30, 32 through 36, and 38 through 41, as applicable, the total number of days in which inpatients were covered under Medicare Part B but did not have Part A benefits available.
Column 7--Multiply the average per diem cost in column 5 by the number of inpatient days in column 6 to arrive at the expense applicable to title XVIII for each cost center. Transfer the amount on line 30, or lines 38 through 40 if you are a subprovider with a swing bed, to Worksheet E-2, column 2, line 6.
For columns 1, 3, and 7, enter on line 37 the sum of the amounts on line 29 plus the sum of the amounts on lines 32 through 36.
Transfer the expenses on lines 37 through 41 to the appropriate lines on Part III, column 4, whenever you complete both Parts I and II.
However, when only Part II is completed, transfer the amount entered in column 7, lines 37 through 41 to Worksheet E, Part B, line 22, as appropriate.
4026.3 Part III - Summary for Title XVIII (To be completed only if both Parts I and II are used)--Do not complete this section unless you qualify for the exception for graduate medical education payments in 42 CFR 413.77(e)(1). This part is applicable to Medicare only and is provided to summarize the amounts apportioned to the program in Parts I and II. This part is completed only if both Parts I and II are used.
Transfer title XVIII expenses.
Description From Column 6
Hospital Line 45 TO Worksheet E, Part B, line 22
Subprovider Line 46-48 TO Worksheet E, Part B, line 22
SNF Line 49 TO Worksheet E, Part B, line 22
Rev. 40-157
4027 FORM CMS-2552-10 DRAFT
4027. WORKSHEET D-3 - INPATIENT ANCILLARY SERVICE COST APPORTIONMENT
This worksheet provides for the apportionment of cost applicable to hospital inpatient services reimbursable under titles V, XVIII and XIX as indicated in 42 CFR 413.53. All hospital filing a full cost report, including CAHs (Worksheet S-2, line 105, is marked “Y”) must complete this worksheet. Complete a separate copy of this worksheet for each sub-provider, distinct part SNF and NF, swing-bed SNF and NF, or any other component. Identify the health care program, provider component, and the payment system by checking the appropriate boxes at the top of the worksheet.
The cost centers on this worksheet have the same line numbers as the respective cost centers on Worksheets A, B, B-1, and C. This design facilitates referencing throughout the cost report.
Column 1--Enter the ratio of cost to charges developed for each cost center from Worksheet C, lines 50 through 94 and 96 through 98. The ratios in columns 10 and 11 of Worksheet C are used only for hospital or subprovider components for titles V, XVIII, and XIX inpatient services subject to the TEFRA rate of increase ceiling (see 42 CFR 413.40) or PPS (see 42 CFR 412, Subpart N, O, or P), respectively. Use the ratios in column 9 in all other cases.
Column 2--Enter from the PS&R or your records the inpatient program charges applicable to the provider component services only (not professional component) in the appropriate cost centers as detailed below. Also include charges for cost centers with a negative balance on Worksheet B, Part I, column 26. Do not include program charges for swing bed services and Medicare charges identified as MSP/LCC.
Lines 30 - 35--Enter the program charges from the PS&R or your records (hospital only).
Lines 40 - 42--Enter in column 2 the inpatient program charges for the subproviders’ component only. For subprovider components do not complete lines 30-35 and 43. For a Hospital complex do not complete lines 40-42.
Line 43--Enter the charges for your nursery department for which you were reimbursed. Complete this for Medicaid services only.
Line 61--Enter the program charges for your clinical laboratory tests for which you reimburse the pathologist. See the instructions for Worksheet A (see §4013) for a more complete discussion on the use of this cost center.
NOTE: Since the charges on line 61 are also included on line 60, laboratory, you must reduce total charges to prevent double counting. Make this adjustment on line 201.
40-158 Rev.
DRAFT FORM CMS-2552-10 4027 (Cont.)
Line 73--Enter only the program charges for drugs charged to patients that are not paid a predetermined amount.
Lines 88 through 90 and 93--Do not enter on these lines program charges related to any inpatient ancillary services (e.g., radiology- diagnostic, laboratory) provided in a clinic, RHC, or FQHC and billed as inpatient services. Instead, reclassify such program charges to the related ancillary cost centers.
Lines 92 and 92.01--Enter on these lines, as applicable, the program charges for observation bed services if the patient was subsequently admitted as an inpatient. However, these program charges can only be reported on the main hospital’s (e.g., acute care hospital, freestanding psychiatric hospital, freestanding rehabilitation hospital) Worksheet D-3. (That is, program charges for observation bed services provided to patients subsequently admitted as inpatients to an acute hospital’s excluded psychiatric or rehabilitation unit must be reported on Worksheet D‑3 of the acute hospital.)
Lines 96 and 97--Do not enter program charges for oxygen rented or sold as the fee schedule applies for these services.
Line 200--Enter the total of the amounts in columns 2 and 3, lines 50 through 94 and 96 through 98.
Line 201--Enter in column 2 program charges for your clinical laboratory tests when the physician bills you for program patients only. Obtain this amount from line 61.
Line 202--Enter in column 2 the amount on line 200 less the amount on line 201.
Transfer the amount in column 2, line 202, as follows.
For title XVIII, Part A (other reimbursement), transfer the amount to Worksheet E-3, Part V, line 8. Do not transfer this amount if you are reimbursed under PPS or TEFRA. No transfers of swing bed charges are made to Worksheet E-2 since no LCC comparison is made. For titles V and XIX (if not a PPS provider), transfer the amount plus the amount from Worksheet D, Part V, sum of columns 3 and 4, line 202, to Worksheet E-3, Part VII, column 1, line 9.
Rev. 40-159
4027 (Cont.) FORM CMS-2552-10 DRAFT
Column 3--Multiply the indicated program charges in column 2 by the ratio in column 1 to determine the program inpatient expenses.
Transfer column 3, line 200, as follows:
Type of Provider TO
Hospital Wkst. D-1, Part II, col. 1, line 48
Subprovider Wkst. D-1, Part II, col. 1, line 48
SNF Wkst. D-1, Part III, col. 1, line 84
NF Wkst. D-1, Part III, col. 1, line 84
Swing Bed-SNF Wkst. E-2, col. 1, line 3
Swing Bed-NF Wkst. E-2, col. 1, line 3
40-160 Rev.
09-14 FORM CMS-2552-10 4028.1
4028. WORKSHEET D-4 - COMPUTATION OF ORGAN ACQUISITION COSTS AND CHARGES FOR HOSPITALS WHICH ARE CERTIFIED TRANSPLANT CENTERS
Only certified transplant centers (CTCs) are reimbursed directly by the Medicare program for organ acquisition cost. This worksheet provides for the computation and accumulation of organ acquisition costs and charges for CTCs. Check the appropriate box (heart, liver, lung, pancreas, intestine, kidney, or islet) to determine which organ acquisition cost is being computed. Use a separate worksheet for each type of organ.
Hospitals that are not CTCs are not reimbursed by the Medicare program for organ acquisition costs and do not complete this worksheet. Such hospitals have to obtain revenue by the sale of any organs excised to an organ procurement organization (OPO) or CTC.
Worksheet D-4 consists of the following four parts:
Part I - Computation of Organ Acquisition Cost (Inpatient Routine and Ancillary Services)
Part II - Computation of Organ Acquisition Cost (Other than Inpatient Routine and Ancillary Service Costs)
Part III - Summary of Costs and Charges
Part IV - Statistics
4028.1 Part I - Computation of Organ Acquisition Costs (Inpatient Routine and Ancillary Services)--
Lines 1 through 7--These lines provide for the computation of inpatient routine service costs applicable to organ acquisition and for the accumulation of inpatient routine service charges for organ acquisition.
Column 1--Enter on lines 1 through 6, as appropriate, the inpatient routine charges applicable to organ acquisition. Enter on line 7 the sum of the amounts reported on lines 1 through 6.
Column 2--Enter on lines 1 through 6, as appropriate, the average per diem cost from Worksheet D-1:
To
Worksheet D-4, From Worksheet D-1,
Description Part I, Col. 2 Part II
Adults & Pediatrics line 1 col. 1, line 38
Intensive Care line 2 col. 3, line 43
Coronary Care line 3 col. 3, line 44
Burn Intensive Care Type Unit line 4 col. 3, line 45
Surgical Intensive Care Type Unit line 5 col. 3, line 46
Other Intensive Care Type Unit line 6 col. 3, line 47
Column 3--Enter from your records on lines 1 through 6, as appropriate, total organ acquisition days (Medicare and non-Medicare). An organ acquisition day is an inpatient day of care rendered to an organ donor patient who is hospitalized for the surgical removal of an organ for transplant or a day of care rendered to a cadaver in an inpatient routine service area for the purpose of surgical removal of its organs for transplant. Enter on line 7 the sum of the days on lines 1 through 6.
Column 4--Enter on lines 1 through 6, as appropriate, the amount in column 2 multiplied by the amount in column 3. Enter on line 7 the sum of lines 1 through 6.
Rev. 6 40-161
4028.1 (Cont.) FORM CMS-2552-10 09-14
Lines 8 through 40--These lines provide for the computation of ancillary service cost applicable to organ acquisition. These lines also provide for the accumulation of inpatient and outpatient organ acquisition ancillary charges.
Column 1--Enter on lines 8 through 40 the "cost or other" cost to charges ratio from Worksheet C, column 9.
Column 2--Enter from your records inpatient and outpatient organ acquisition ancillary charges. Enter on line 41 the sum of lines 8 through 40.
Column 3--Enter on lines 8 through 40 the organ acquisition costs. Compute this amount by multiplying the ratio in column 1 by the amount in column 2 for each cost center. Enter on line 41 the sum of lines 8 through 40.
4028.2 Part II - Computation of Organ Acquisition Costs (Other Than Inpatient Routine and Ancillary Service Costs)--
Lines 42 through 47--Use these lines to apportion the cost of inpatient services attributable to organ acquisitions rendered in each of the inpatient routine areas by interns and residents not in an approved teaching program.
Column 1--Enter on the appropriate lines the average per diem cost of interns and residents not in an approved teaching program in each of the inpatient routine areas. Obtain these amounts from Worksheet D-2, Part I, column 4, lines as indicated.
Column 2--Enter the number of organ acquisition days in each of the inpatient routine areas from Part I, column 3, lines 1 through 6, as appropriate.
Column 3--Multiply the per diem amount in column 1 by the number of days in column 2 for each cost center.
Line 48--For columns 2 and 3, enter the sum of lines 42 through 47.
Lines 49 through 54--These lines provide for the computation of the cost of outpatient services attributable to organ acquisitions rendered in each of the outpatient service areas by interns and residents not in an approved teaching program.
Column 1--Enter on the appropriate lines the organ acquisition charges in each of the outpatient service areas. Obtain these amounts from Part I, column 2, lines 35 through 40, as appropriate.
Column 2--Enter the ratio of the outpatient costs of interns and residents not in an approved teaching program to the hospital outpatient service charges in each of the outpatient service areas. Obtain these ratios from Worksheet D-2, Part I, column 4, lines as indicated.
Column 3--Multiply the charges in column 1 by the ratios in column 2 for each cost center. Enter the sum of lines 49 through 54 on line 55.
40-162 Rev. 6
DRAFT FORM CMS-2552-10 4028.3
4028.3 Part III - Summary of Costs and Charges--
Line 56--Enter in column 1 the sum of the costs in Part I, column 4, line 7 and column 3, line 41. Enter in column 3 the sum of the charges in Part I, column 1, line 7, and column 2, line 41.
Line 57--Enter in column 1 the cost of inpatient services of interns and residents not in an approved teaching program from Part II, column 3, line 48. Enter in column 3 your charges for the services for which the cost is entered in column 1. If you do not charge separately for the services of interns and residents, enter zero in column 3.
Line 58--Enter in column 1 the cost of outpatient services of interns and residents not in an approved teaching program from Part II, column 3, line 55. Enter in column 3 the provider charges for the services for which the cost is entered in column 1. If you do not charge separately for the services of interns and residents, enter zero in column 3.
Line 59--Enter in column 1 the direct organ acquisition costs and allocated general service costs from Worksheet B, Part I, column 26, lines 105, 106, 107, 108, 109, 110, or 111, whichever is applicable.
These direct costs include, but are not limited to, the cost of services purchased under arrangements or billed directly to you for:
Fees for physician services (preadmission donor and recipient tissue typing),
Costs for organs acquired from other providers or organ procurement organizations,
Transportation costs of organs,
Organ recipient registration fees,
Surgeon’s fees for excising cadaveric organs, and
Tissue typing services furnished by independent laboratories.
NOTE: Transportation costs to ship organs outside of the United States are not an allowable cost.
If you have a schedule of charges which represents the various direct organ acquisition costs included in column 1, enter in column 3 the total of the charges which are applicable to the costs in column 1. However, if you have no such schedule of charges, enter the amount from column 1 in column 3.
Line 60--Teaching hospitals or subproviders electing to be reimbursed for services of physicians on the basis of reasonable cost (see 42 CFR 415.160 and CMS Pub. 15-1, chapter 21, §2148), enter the cost of physicians. For cost reporting periods ending before June 30, 2014, transfer the amount from Worksheet D-5, Part II, column 3, lines 24 through 30, as applicable. For cost reporting periods ending on or after June 30, 2014, transfer the amount from Worksheet D-5, Part IV, lines 24 through 30, as applicable.
Line 61--Enter in columns 1 and 3 the sum of lines 56 through 60. This amount must be equal to or greater than the amount reported on line 66 (revenues for organs sold).
Line 62--Enter the number of total usable organs excised and purchased minus all unusable or discarded organs that could not be transplanted (usable organs equals Worksheet D-4, Part IV, line 74, sum of columns 1 and 2, minus Worksheet D-4, Part IV, line 83, sum of columns 1 and 2). For islets since the number of islets cells injected into a recipient will vary depending on
Rev. 40-163
4028.3 (Cont.) FORM CMS-2552-10 DRAFT
the patient, enter the number of patients who received islets injections. Each patient is allowed a maximum of two islet injections per inpatient stay.
Line 63--Enter the total Medicare usable organs that are included on line 62. Medicare usable organs include organs transplanted into Medicare beneficiaries (this excludes Medicare Advantage beneficiaries), organs sent to military hospitals (that have a reciprocal sharing agreement with the Organ Procurement Organization (OPO) in effect prior to March 3, 1988 and approved by the contractor), organs that had partial payments by a primary insurance payer in addition to Medicare, organs sent to other providers and organs sent to OPOs. Do not include organs used for research, organs sent to military hospitals (without a reciprocal sharing agreement with the OPO) in effect prior to March 3, 1988 and approved by the contractor), organs sent to veterans’ hospitals, organs sent outside the United States, organs transplanted into non-Medicare beneficiaries, organs that were totally paid by primary insurance other than Medicare, organs that were paid by a Medicare Advantage plan, and organs procured from a non-certified OPO.
Line 64--Enter line 63 divided by line 62.
Line 65--Enter in column 1, the Medicare costs calculated by multiplying the ratio in column 2, line 64 by the total costs in column 1, line 61. Enter in column 3, the Medicare charges calculated by multiplying the ratio in column 2, line 64, by the total charges in column 3, line 61.
Line 66--Enter in columns 1 and 3, the total revenue applicable to:
Organs (included on line 63) furnished to other providers, organs sent to OPOs, and organs sent to military hospitals with a reciprocal sharing agreement with the OPO in effect prior to March 3, 1988, and approved by the contractor.
Organs that were partially reimbursed by another primary insurer other than Medicare and were included on line 63.
NOTE: When the primary payer makes a single payment for the transplant and acquisition, it is necessary to prorate the amount received between the transplant and the acquisition based on the charges submitted to the payer. Report the primary payer amounts applicable to organ transplants on Worksheet E, Part A, line 60. Report the primary payer amounts applicable to organ acquisition on this line.
Line 67--Enter the amount entered on line 65 minus the amount on line 66.
Line 68--Enter in all columns the total amount of organ acquisition charges billed to Medicare under Part B. This occurs when organs are transplanted into Medicare beneficiaries who, on the day of transplantation, are not entitled to Part A benefits. This computation reflects an adjustment between Medicare Part A and Part B costs and charges so that the amount added under Part B is the same amount subtracted under Part A.
Line 69--For columns 1 and 3, subtract line 68 from line 67. For columns 2 and 4, transfer that amount from line 68.
40-164 Rev.
09-14 FORM CMS-2552-10 4028.4
4028.4 Part IV - Statistics.--
Lines 70 through 84--The data entered are data applicable to living donors (column 1) and cadaveric donors (column 2). Use column 1 (living related) for kidney, partial liver, and partial lung transplants. If you complete this worksheet for hearts, pancreases, intestines, whole livers, whole lungs, or islets do not complete column 1.
Line 74--Enter the sum of lines 70 through 73.
Lines 75 through 82--Enter in columns 1 and 2 the appropriate number of organs sold (or transplanted). Enter in column 3 the revenue applicable to organs furnished to other providers, organ procurement organizations and others, and for organs transplanted into non-Medicare patients. Such revenues must be determined under the accrual method of accounting. If organs are transplanted into non-Medicare patients who are not liable for payment on a charge basis, and as such there is no revenue applicable to the related organ acquisitions, the amount entered on these lines must also include an amount representing the acquisition cost of the organs transplanted into such patients. Determine this amount by multiplying the average cost of organ acquisition by the number of organs transplanted into non-Medicare patients not liable for payment on a charge basis.
Compute the average cost of organ acquisition by dividing the total cost of organ acquisition (including the inpatient routine service costs and the inpatient ancillary service costs applicable to organ acquisitions) by the total number of organs transplanted into all patients and furnished to others. If the average cost cannot be determined in the manner described, then use the appropriate standard organ acquisition charge in lieu of the average cost.
Line 83--Enter in columns 1 and 2 the applicable number of unusable organs.
Line 84--Enter the sum of lines 75 through 83. These totals equal the totals on line 74, columns 1 and 2.
Rev. 6 40-165
4029 FORM CMS-2552-10 09-14
4029. WORKSHEET D-5 - APPORTIONMENT OF COST FOR PHYSICIANS’ SERVICES IN A TEACHING HOSPITAL
A teaching hospital engaged in an approved GME residency program in accordance with 42 CFR 415.152, may elect to receive payment on a reasonable cost basis for the direct medical and surgical services of its physicians in lieu of fee schedule payments that might otherwise be made for these services. These services, and the supervision of interns and residents furnishing care to individual beneficiaries, are covered as hospital services for which Medicare pays the hospital on a reasonable cost basis. Teaching hospitals that have elected to be paid for these services on a reasonable cost basis in accordance with 42 CFR 415.160, are subject to RCEs. This worksheet provides for the computation of the RCE limits by medical specialty and the apportionment of reimbursable adjusted cost to titles V, XVIII, and XIX in accordance with 42 CFR 415.162 and CMS Pub. 15-1, chapter 21, §2148.
NOTE: CAHs do not complete this worksheet.
If such election is made, direct medical and surgical services to program patients, including supervision of interns and residents, rendered in a teaching hospital by physicians on the hospital staff are reimbursable as provider services on a reasonable cost basis. In addition, certain medical school costs may be reimbursed. Payments for services donated by volunteer physicians to program patients are made to a fund designated by the organized medical staff the teaching hospital or medical school.
Limits on the amount of physician compensation which may be recognized as a reasonable provider cost are imposed in accordance with 42 CFR 415.70.
Worksheet D-5 consists of four parts:
Part I - Reasonable Compensation Equivalent Computation for Cost Reporting Periods Ending Before June 30, 2014
Part II - Apportionment of Cost for Physicians’ Services in a Teaching Hospital for Cost Reporting Periods Ending Before June 30, 2014
Part III - Reasonable Compensation Equivalent Computation for Cost Reporting Periods Ending On or After June 30, 2014
Part IV - Apportionment of Cost for Physicians’ Services in a Teaching Hospital for Cost Reporting Periods Ending On or After June 30, 2014
Effective for cost reporting periods ending on or after June 30, 2014, do not complete Worksheet D-5, Parts I and II, but complete Worksheet D-5, Parts III and IV.
4029.1 Part I - Reasonable Compensation Equivalent Computation for Cost Reporting Periods Ending Before June 30, 2014--This part provides for the computation of the RCE limit by medical specialty of the physician on the hospital staff or physician on the medical school faculty. Complete separate parts for the hospital staff physicians and for physicians on the medical staff faculty. This part must be completed by applicable hospitals for cost reporting periods ending before June 30, 2014.
Where several physicians work in the same specialty, see CMS Pub. 15-1, chapter 21, §2182.6C, for a discussion of applying the RCE limit in the aggregate for the specialty versus on an individual basis to each of the physicians in the specialty.
40-166 Rev. 6
DRAFT FORM CMS-2552-10 4029.1 (Cont.)
When RCE limits are applied on an individual basis to each physician in a medical specialty, prepare a supporting worksheet identical in columnar format to Worksheet D-5, Part I, for each medical specialty. Enter on the first line under columns 1 and 9 the line number applicable to the medical specialty (as displayed on Worksheet D-5, Part I). Enter the name of the medical specialty on the first line in columns 2 and 10. Following the first line, use a separate line to compute the adjusted cost of physician’s direct medical and surgical services (column 16) for each physician.
 Enter
the total amount from column 16 of the supporting worksheet in column
16 of the line on Worksheet D-5, Part I, corresponding to the medical
specialty for which the supporting worksheet is prepared. If the
individual physician method is used, list each physician using an
individual identifier that is not the name or social security number
of the physician (e.g., Dr. A, Dr. B). However, the identity of the
physician must be made available to your contractor.
Enter
the total amount from column 16 of the supporting worksheet in column
16 of the line on Worksheet D-5, Part I, corresponding to the medical
specialty for which the supporting worksheet is prepared. If the
individual physician method is used, list each physician using an
individual identifier that is not the name or social security number
of the physician (e.g., Dr. A, Dr. B). However, the identity of the
physician must be made available to your contractor.
NOTE: The method used on Worksheet D-5 (i.e., aggregate or individual physician) must be the same as the method used on Worksheet A-8-2.
Column Descriptions
Column 3--Enter for each medical specialty the amount of the total cost included in Worksheet A-8-2, column 3. When the individual physician method is used, enter in column 3 of the supporting worksheet the amount included on Worksheet A-8-2, column 3, for that physician.
Column 4--Enter for each medical specialty the amount of the cost included in Worksheet A-8-2, column 4, for the direct medical and surgical services, including the supervision of interns and residents by physicians on the hospital staff or by physicians on the faculty of a medical school, as appropriate.
If the individual physician method is used, enter in column 4 of the supporting worksheet the amount included on Worksheet A-8-2, column 4, for the indicated physician.


 Column
5--Enter for each line of data the
reasonable compensation equivalent (RCE) limit applicable to the
physician’s compensation. The amount entered is the limit
applicable to the physician specialty. Obtain the RCE applicable to
the specialty from the table listed in the 68 FR 45488
(August
1, 2003).
If the physician specialty is not identified in the table, use the
RCE for the total category in the table. The beginning date of the
cost reporting period determines which calendar year (CY) RCE is
used. Your location governs which of the three geographical
categories are applicable: non-metropolitan areas, metropolitan areas
less than one million, or metropolitan areas greater than one
million.
Column
5--Enter for each line of data the
reasonable compensation equivalent (RCE) limit applicable to the
physician’s compensation. The amount entered is the limit
applicable to the physician specialty. Obtain the RCE applicable to
the specialty from the table listed in the 68 FR 45488
(August
1, 2003).
If the physician specialty is not identified in the table, use the
RCE for the total category in the table. The beginning date of the
cost reporting period determines which calendar year (CY) RCE is
used. Your location governs which of the three geographical
categories are applicable: non-metropolitan areas, metropolitan areas
less than one million, or metropolitan areas greater than one
million.

 Column
6--Enter the physician’s hours
allocated to professional services (i.e., professional component
hours) in all components (e.g., hospitals, subproviders) of the
health care complex. If the physician is paid for unused vacation,
unused sick leave, etcetera,
exclude the hours so paid from the hours entered in this column.
Time records or other documentation that supports this allocation
must be available for verification by your contractor upon request.
(See CMS Pub. 15-1, chapter 21, §2182.3E.)
Column
6--Enter the physician’s hours
allocated to professional services (i.e., professional component
hours) in all components (e.g., hospitals, subproviders) of the
health care complex. If the physician is paid for unused vacation,
unused sick leave, etcetera,
exclude the hours so paid from the hours entered in this column.
Time records or other documentation that supports this allocation
must be available for verification by your contractor upon request.
(See CMS Pub. 15-1, chapter 21, §2182.3E.)
 Column
7--Enter the unadjusted RCE limit
for each line of data. This amount is the product of the RCE amount
entered in column 5 and the ratio of the physician’s
professional component hours entered in column 6 to 2080 hours.
Column
7--Enter the unadjusted RCE limit
for each line of data. This amount is the product of the RCE amount
entered in column 5 and the ratio of the physician’s
professional component hours entered in column 6 to 2080 hours.
Column 8--Enter for each line of data five percent of the amounts entered in column 7.
Rev. 40-167
4029.1 (Cont.) FORM CMS-2552-10 DRAFT
Column 11--You may adjust upward, up to five percent of the computed limit (column 8), the computed RCE limit in column 7 to take into consideration the actual costs of membership for physicians in professional societies and continuing education paid by the provider or medical school.
Enter for each line of data the actual amounts of these expenses paid by the provider or medical school.
Column 12--Enter for each line of data, the result of multiplying column 4 by column 11, and dividing by column 3.
 Column
13--You may also adjust upward the
computed RCE limit in column 7 to reflect the actual malpractice
expense incurred by the provider or by the medical school, as
appropriate, for the services of a physician or group of physicians
to provider patients.
Column
13--You may also adjust upward the
computed RCE limit in column 7 to reflect the actual malpractice
expense incurred by the provider or by the medical school, as
appropriate, for the services of a physician or group of physicians
to provider patients.
Enter for each line of data the actual amounts of these malpractice expenses paid by the provider (or medical school, if applicable).
Column 14--Enter for each line of data, the result of multiplying column 4 by column 13, and dividing by column 3.
Column 15--Enter for each line of data, the sum of columns 7 and 14 plus the lesser of columns 8 or 12.
Column 16--Enter for each line of data, the adjusted cost of direct medical and surgical services, including the supervision of interns and residents (i.e., the lesser of column 4 or column 15).
Line Descriptions
Line 11--Total the amounts in columns 3 through 8 and 11 through 16.
 4029.2 Part
II - Apportionment of Cost for Physicians’ Services in a
Teaching Hospital for Cost Reporting Periods Ending Before June 30,
2014--This part provides for the
accumulation and apportionment of reimbursable cost for titles V,
XVIII, and XIX using the aggregate per diem method of apportionment
(see CMS Pub. 15-1, chapter 22, §2218) for the adjusted direct
medical and surgical services, including the supervision of interns
and residents, rendered by physicians to patients in a teaching
hospital which makes the election described in CMS Pub. 15‑1,
chapter 21, §2148. Complete a separate Part II for the hospital
and for each subprovider for cost reporting periods ending before
June 30, 2014.
4029.2 Part
II - Apportionment of Cost for Physicians’ Services in a
Teaching Hospital for Cost Reporting Periods Ending Before June 30,
2014--This part provides for the
accumulation and apportionment of reimbursable cost for titles V,
XVIII, and XIX using the aggregate per diem method of apportionment
(see CMS Pub. 15-1, chapter 22, §2218) for the adjusted direct
medical and surgical services, including the supervision of interns
and residents, rendered by physicians to patients in a teaching
hospital which makes the election described in CMS Pub. 15‑1,
chapter 21, §2148. Complete a separate Part II for the hospital
and for each subprovider for cost reporting periods ending before
June 30, 2014.
Line Descriptions

 Line
1--Enter in the appropriate column,
the adjusted cost of direct medical and surgical services, including
the supervision of interns and residents, rendered to all patients by
physicians on the hospital staff (column 1) and by physicians on the
medical school faculty (column 2), as determined in accordance with
CMS Pub. 15-1, chapter 21, §2148. Transfer these amounts from
Part I, column 16, line 11. Enter the same amount on each
component’s Part II.
Line
1--Enter in the appropriate column,
the adjusted cost of direct medical and surgical services, including
the supervision of interns and residents, rendered to all patients by
physicians on the hospital staff (column 1) and by physicians on the
medical school faculty (column 2), as determined in accordance with
CMS Pub. 15-1, chapter 21, §2148. Transfer these amounts from
Part I, column 16, line 11. Enter the same amount on each
component’s Part II.
 Line
2--Enter in column 1, the sum of the
hospital inpatient days and the hospital outpatient visit days for
all patients in the hospital and each hospital subprovider. Compute
these days in the manner described in CMS Pub. 15-1,
chapter 22, §2218.C. Enter in column 2, the same number of days
as entered in column 1. Make the same entries on each component’s
Part II.
Line
2--Enter in column 1, the sum of the
hospital inpatient days and the hospital outpatient visit days for
all patients in the hospital and each hospital subprovider. Compute
these days in the manner described in CMS Pub. 15-1,
chapter 22, §2218.C. Enter in column 2, the same number of days
as entered in column 1. Make the same entries on each component’s
Part II.
40-168 Rev.
DRAFT FORM CMS-2552-10 4029.3
Line 3--Enter the result obtained by dividing the cost of services on line 1 by the sum of the days on line 2 for each category of physicians.
Lines 4 through 16--Enter in column 1, on the appropriate line, the reimbursable days and outpatient visit days for titles V, XVIII, and XIX for the hospital and each hospital subprovider, as applicable. Lines 10 through 16 contain the total of the title XVIII organ acquisition days and outpatient visit days. Enter in column 2 the same number of days as entered in column 1. Compute these days from your records in the manner described in CMS Pub. 15-1, chapter 22, §2218.C. Do not complete lines 10 through 16 for an IRF, IPF or hospital subprovider(s).
Line 17--Do not use.
Lines 18 through 31--Enter on the appropriate line the result of multiplying the days entered on lines 4 through 16 by the average cost per diem from line 3. Enter the total of columns 1 and 2 in column 3 for each line. The total becomes a part of the reimbursement settlement through the transfers denoted on this worksheet.
4029.3 Part III - Reasonable Compensation Equivalent Computation for Cost Reporting Periods Ending On or After June 30, 2014--This part provides for the computation of the RCE limit of the physician on the hospital staff or physician on the medical school faculty. This part must be completed by applicable hospitals for cost reporting periods ending on or after June 30, 2014.
Column Descriptions
Columns 1 through 5, 9 through 11, and 13--For each line in columns 1 through 4, transfer the information from the corresponding columns on Worksheet A-8-2. For each line in column 5, transfer the amount from Worksheet A-8-2, column 6. For each line in columns 9 and 10, transfer the information from Worksheet A-8-2, columns 10 and 11, respectively. For each line in columns 11 and 13, transfer the amounts from Worksheet A-8-2, columns 12 and 14, respectively.

 Column
6--For each line, enter the
physician’s hours allocated to professional services (i.e.,
professional component hours) in all components (e.g., hospitals,
subproviders) of the health care complex. If the physician is paid
for unused vacation, unused sick leave, etcetera,
exclude the hours so paid from the hours entered in this column.
Time records or other documentation supporting this allocation must
be available for verification by your contractor upon request. (See
CMS Pub. 15-1, chapter 21, §2182.3E.)
Column
6--For each line, enter the
physician’s hours allocated to professional services (i.e.,
professional component hours) in all components (e.g., hospitals,
subproviders) of the health care complex. If the physician is paid
for unused vacation, unused sick leave, etcetera,
exclude the hours so paid from the hours entered in this column.
Time records or other documentation supporting this allocation must
be available for verification by your contractor upon request. (See
CMS Pub. 15-1, chapter 21, §2182.3E.)
 Column
7--For each line, enter the
unadjusted RCE limit calculated by multiplying the RCE amount in
column 5 by the ratio of the physician’s professional component
hours entered in column 6 to 2080 hours (column 5 x (column 6 ÷
2080)).
Column
7--For each line, enter the
unadjusted RCE limit calculated by multiplying the RCE amount in
column 5 by the ratio of the physician’s professional component
hours entered in column 6 to 2080 hours (column 5 x (column 6 ÷
2080)).
Column 8--For each line, enter five percent of the amount entered in column 7.
Column 12--For each line, enter the professional component share of column 11 by multiplying column 4 by column 11 and dividing by column 3.
Column 14--Enter for each line of data the result of multiplying column 4 by column 13, and dividing by column 3.
Column 15--For each line, enter the sum of column 7 plus column 14, plus the lesser of column 8 or 12.
Column 16--For each line, enter the lesser of column 4 or column 15.
Rev. 40-168.1
4029.3 (Cont.) FORM CMS-2552-10 DRAFT
Line Descriptions
Line 200--Total the amounts in columns 3 through 8 and columns 11 through 16.
 4029.4 Part
IV - Apportionment of Cost for Physicians’ Services in a
Teaching Hospital for Cost Reporting Periods Ending On or After June
30, 2014--This part provides for the
accumulation and apportionment of reimbursable cost for titles V,
XVIII, and XIX using the aggregate per diem method of apportionment
(see CMS Pub. 15-1, chapter 22, §2218) for the adjusted direct
medical and surgical services, including the supervision of interns
and residents, rendered by physicians to patients in a teaching
hospital which makes the election described in CMS Pub. 15-1,
chapter 21, §2148. Complete a separate Part IV for the hospital
and each hospital subprovider for cost reporting periods ending on or
after June 30, 2014.
4029.4 Part
IV - Apportionment of Cost for Physicians’ Services in a
Teaching Hospital for Cost Reporting Periods Ending On or After June
30, 2014--This part provides for the
accumulation and apportionment of reimbursable cost for titles V,
XVIII, and XIX using the aggregate per diem method of apportionment
(see CMS Pub. 15-1, chapter 22, §2218) for the adjusted direct
medical and surgical services, including the supervision of interns
and residents, rendered by physicians to patients in a teaching
hospital which makes the election described in CMS Pub. 15-1,
chapter 21, §2148. Complete a separate Part IV for the hospital
and each hospital subprovider for cost reporting periods ending on or
after June 30, 2014.
Line Descriptions

 Line
1--Enter the adjusted cost of direct
medical and surgical services, including the supervision of interns
and residents, rendered to all patients by physicians, determined in
accordance with CMS Pub. 15-1, chapter 21, §2148. Transfer
these amounts from Part III, column 16, line 200. When completing
this worksheet for multiple components of a health care complex,
enter the same amount on each component’s Part IV worksheet.
Line
1--Enter the adjusted cost of direct
medical and surgical services, including the supervision of interns
and residents, rendered to all patients by physicians, determined in
accordance with CMS Pub. 15-1, chapter 21, §2148. Transfer
these amounts from Part III, column 16, line 200. When completing
this worksheet for multiple components of a health care complex,
enter the same amount on each component’s Part IV worksheet.
 Line
2--Enter the sum of the hospital
inpatient days and the hospital outpatient visit days for all
patients in the hospital and each hospital subprovider. Compute
these days in the manner described in CMS Pub. 15-1, chapter 22,
§2218.C. When completing this worksheet for the hospital or
hospital subprovider(s), enter the same amount on each component’s
Part IV.
Line
2--Enter the sum of the hospital
inpatient days and the hospital outpatient visit days for all
patients in the hospital and each hospital subprovider. Compute
these days in the manner described in CMS Pub. 15-1, chapter 22,
§2218.C. When completing this worksheet for the hospital or
hospital subprovider(s), enter the same amount on each component’s
Part IV.
Line 3--Enter the result obtained by dividing the cost of services on line 1 by the sum of the days on line 2.
Lines 4 through 16--For each line, enter the reimbursable days and outpatient visit days for titles V, XVIII, and XIX for the hospital and each subprovider. Lines 10 through 16 contain the total of the title XVIII organ acquisition days and outpatient visit days. Compute these days from your records in the manner described in CMS Pub. 15-1, chapter 22, §2218.C.
Lines 18 through 30--For each line, enter the result of multiplying the days entered on lines 4 through 16 by the average cost per diem from line 3. The total becomes a part of the reimbursement settlement through the transfers denoted on this worksheet. Transfer the amounts as follows:
From Worksheet D-5, Part IV To Worksheet
Line 18 plus line 19 E-3, Part VII, line 20 (title V hospital or component)
Line 20 E, Part A, line 56 (Medicare IPPS hospital)
E-3, Part I, line 3 (TEFRA hospital)
E-3, Part II, line 15 (IPF)
E-3, Part III, line 16 (IRF)
E-3, Part IV, line 6 (LTCH)
E-3, Part V, line 17 (Cost reimbursement)
Line 21 E, Part B, line 23 (Medicare hospital Part B)
Line 22 plus line 23 E-3, Part VII, line 20 (title XIX hospital or component)
Sum of lines 24 through 30 D-4, Part III, line 60
40-168.2 Rev.
DRAFT FORM CMS-2552-10 4030.1
4030. WORKSHEET E - CALCULATION OF REIMBURSEMENT SETTLEMENT
Worksheet E, Parts A and B, calculate title XVIII settlement for inpatient hospital services under inpatient PPS (IPPS) and title XVIII (Part B) settlement for medical and other health services. Worksheet E-3 computes title XVIII, Part A settlement for non-IPPS hospitals, settlements under titles V and XIX, and settlements for title XVIII SNFs reimbursed under a prospective payment system. Worksheet E-4 computes total direct graduate medical education costs.
Worksheet E consists of the following two parts:
Part A - Inpatient Hospital Services Under PPS
Part B - Medical and Other Health Services
Application of Lesser of Reasonable Cost or Customary Charges--Worksheet E, Part B, allows for the computation of the lesser of reasonable costs or customary charges (LCC), where applicable, for services covered under Part B. Make a separate computation on each of these worksheets. In addition, make separate computations to determine whether the services on any or all of these worksheets are exempt from LCC. For example, the provider may meet the nominality test for the services on Worksheet E, Part B, and, therefore, be exempt from LCC only for these services.
For those provider Part B services exempt from LCC for this reason, reimbursement for the affected services is based on 80 percent of reasonable cost net of the Part B deductible amounts.
4030.1 Part A - Inpatient Hospital Services Under IPPS--
For SCH/MDH status change and/or geographical reclassification (see 42 CFR 412.102/103) subscript column 1 for lines 1-3, 22, 28, 29, 33, 34, 41, 45, 47, and 48. If you responded “1” and “2” or “2” and “1”, respectively to Worksheet S-2, Part I, questions 26 and 27, which indicated your facility experienced a change in geographic classification status during the year, subscript column 1 and report the payments before the reclassification in column 1 and on or after the reclassification in column 1.01.
Enter on lines 1 through 3 in column 1 the applicable payment data for the period applicable to SCH status. Enter on lines 1 through 3 in column 1.01 the payment data for the period in which the provider did not retain SCH status. The data for lines 1 through 3 must be obtained from the provider's records or the PS&R.
For IPPS hospitals participating in Model 4 of the Bundled Payments for Care Improvement (BPCI) initiative, Indirect Medical Education (IME) and Disproportionate Share Hospital (DSH) payments will be calculated based on the non-discounted base DRG payment that would have been made in the absence of the model, as will outlier payments and hospital capital payments (see Change Request 8196, dated February 15, 2013). Enter on lines 1.03 and 2.02, in column 1 the applicable payment data for the cost reporting period.
Line Descriptions
Line 1--The amount entered on this line is the sum of the federal specific operating portion (DRG payments) paid for PPS discharges during the cost reporting period and the DRG payments made for PPS transfers during the cost reporting period. For cost reporting periods overlapping October 1, 2013, do not complete line 1, but complete lines 1.01 and 1.02. For cost reporting periods beginning on or after October 1, 2013, use this line and do not complete lines 1.01 and 1.02.
Rev. 40-169
4030.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 1.01--For cost reporting periods that overlap October 1, 2013, enter the amount of the federal specific operating portion (DRG payments) paid for PPS discharges and transfers occurring prior to October 1, 2013. For example, a calendar year provider would include DRG payments for discharges occurring during the period of (January 1 through September 30). Do not complete for cost reporting periods beginning on or after October 1, 2013.
Line 1.02--For cost reporting periods that overlap October 1, 2013, enter the amount of the federal specific operating portion (DRG payments) paid for PPS discharges and transfers occurring on or after October 1, 2013. For example, a calendar year provider would include DRG payments for discharges occurring during the period of (October 1 through December 31).
Do not complete for cost reporting periods beginning on or after October 1, 2013.
Line 1.03--Enter the amount of the federal specific operating portion (DRG payments) for Model 4 bundled payments for care improvement (BPCI) initiative, effective for discharges occurring on or after October 1, 2013.
Line 2--Enter the amount of outlier payments made for PPS discharges during the period. See 42 CFR 412, Subpart F for a discussion of these items.
Line 2.01--For inpatient PPS services rendered during the cost reporting period, enter the operating outlier reconciliation amount for operating expenses from line 92.
Line 2.02--Effective for discharges occurring on or after October 1, 2013, enter the amount of outlier payments made for Model 4 BPCI discharges during the cost reporting period.
Line 3--Hospitals receive payments for indirect medical education for managed care patients based on the DRG payment that would have been made if the service had not been a managed care service. The PS&R will capture in conjunction with the PPS PRICER the simulated payments. Enter the total managed care “simulated payments” from the PS&R.
Line 4--Enter the result of dividing the number of bed days available (Worksheet S-3, Part I, column 3, line 14) by the number of days in the cost reporting period (365 or 366 in case of leap year). Effective for cost reporting periods beginning on or after October 1, 2012, enter the result of dividing the number of bed days available (Worksheet S-3, Part I, column 3, line 14, plus line 32) by the number of days in the cost reporting period (365 or 366 in case of leap year).
NOTE: Reduce the bed days available by swing bed days (Worksheet S-3, Part I, column 8, sum of lines 5 and 6), and the number of observation days (Worksheet S-3, Part I, column 8, line 28). In addition, effective for cost reporting periods beginning on or after October 1, 2011, reduce the bed days available by the number of non-distinct part hospice days (Worksheet S-3, Part I, column 8, line 24.10) and effective for cost reporting periods beginning on or after October 1, 2012, the number of outpatient ancillary labor and delivery days (Worksheet S-3, Part I, column 8, line 32.01).
Indirect Medical Educational Adjustment Calculation for Hospitals--Calculate the IME adjustment only if you answered “yes” to line 56 on Worksheet S-2 and complete lines 5 to 29, as applicable. In addition, a hospital may be entitled to the IME adjustment if Worksheet S-2, line 56 is “no” and lines 13 and/or 14 are greater than zero. (See 42 CFR 412.105.) Hospitals that incur indirect costs for graduate medical education programs are eligible for an additional payment as defined in 42 CFR 412.105(d). This section calculates the additional payment by applying the applicable multiplier of the adjustment factor for such hospitals.
40-170 Rev.
DRAFT FORM CMS-2552-10 4030.1 (Cont.)
Line 15--Enter in the sum of lines 12 through 14 divided by three.
Line 16--Enter the number of FTE residents in the initial years of the program that meet the rolling average exception. (See 42 CFR 412.105(f)(1)(v))
Line 17--Enter the additional FTEs for residents that were displaced by program or hospital closure, which you would not be able to count without a temporary cap adjustment (See 42 CFR 412.105(f)(1)(v)).
Line 18--Enter the sum of lines 15, 16 and 17.
Line 19--Enter the current year resident to bed ratio. Line 18 divided by line 4.
Line 20--In general, enter from the prior year cost report the intern and resident to bed ratio by dividing line 12 by line 4 (divide line 3.14 by line 3 if the prior year cost report was the Form CMS-2552-96). However, if the provider is participating in training residents in a new medical residency training program(s) under 42 CFR 413.79(e), add to the numerator of the prior year intern and resident to bed ratio the number of FTE residents in the current cost reporting period that are in the initial period of years of a new program (i.e., the period of years is the minimum accredited length of the program). If the provider is participating in a Medicare GME affiliation agreement under 42 CFR 413.79(f), and the provider increased its current year FTE cap and current year FTE count due to this affiliation agreement, identify the lower of: a) the difference between the current year numerator and the prior year numerator, and b) the number by which the FTE cap increased per the affiliation agreement, and add the lower of these two numbers to the prior year’s numerator (see 66 FR 39880 (August 1, 2001)). If the hospital is participating in a valid emergency Medicare GME affiliation agreement under a §1135 waiver, and a portion of this cost report falls within the time frame covered by that emergency affiliation agreement, then, effective on and after October 1, 2008, enter the current year resident to bed ratio from line 19 (see 73 FR 48649 (August 19, 2008), and 42 CFR 412.105(f)(1)(vi)). Effective for cost reporting periods beginning on or after 10/1/02, if the hospital is training FTE residents in the current year that were displaced by the closure of another hospital or program, also adjust the numerator of the prior year ratio for the number of current year FTE residents that were displaced by hospital or program closure (42 CFR 412.105(a)(1)(iii)). The amount added to the prior year’s numerator is the displaced resident FTE amount that you would not be able to count without a temporary cap adjustment. This is the same amount of displaced resident FTEs entered on line 17.
Line 21--Enter the lesser of lines 19 or 20.
Line 22--Calculate the IME payment adjustment as follows: Multiply the appropriate multiplier of the adjustment factor (currently 1.35) times {((1 + line 21) to the .405 power) - 1} times {the sum of lines 1, 1.01, 1.02, 1.03 and 3}.
IME Adjustment Calculation for the Add-on--Computation of IME payments for additional allopathic and osteopathic resident cap slots received under 42 CFR 412.105(f)(1)(iv)(C)(1)--Complete lines 23 through 28 only where the amount on line 23 is greater than zero (0).
Line 23--Section 422 IME FTE Cap--Enter the number of allopathic and osteopathic IME FTE residents cap slots the hospital received under 42 CFR 412.105(f)(1)(iv)(C)(1), section 422 of the MMA.
Rev. 40-171
4030.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 24--IME FTE Resident Count Over the Cap--Subtract line 9 from line 10 and enter the result here. If the result is zero or negative, the hospital does not need to use the 422 IME cap. Therefore, do not complete lines 25 through 28.
Line 25--Section 422 Allowable IME FTE Resident Count--If the count on line 24 is greater than zero, enter the lower of line 23 or line 24.
Line 26--Resident to Bed Ratio for Section 422--Divide line 25 by line 4.
Line 27--IME Adjustment Factor for Section 422 IME Residents--Enter the result of the following: .66 times [({1 + line 26} to the .405 power) - 1].
Line 28--IME Add On Adjustment--Enter the sum of lines 1, 1.01, 1.02, 1.03 and 3, multiplied by the factor on line 27.
Line 29--Total IME Payment--Enter the sum of lines 22 and 28.
Disproportionate Share Adjustment--Section 1886(d)(5)(F) of the Act, as implemented by 42 CFR 412.106, requires additional Medicare payments to hospitals with a disproportionate share of low income patients. Calculate the amount of the Medicare disproportionate share adjustment on lines 30 through 34. Complete lines 33 and 34 only if you are an IPPS hospital and answered yes to line 22, column 1 of Worksheet S-2, Part I.
Line 30--Enter the percentage of SSI recipient patient days to Medicare Part A patient days. (Obtain the percentage from your contractor.)
Line 31--Enter the percentage resulting from the calculation of Medicaid patient days (Worksheet S‑2, Part I, columns 1 through 6, line 24) to total days reported on Worksheet S-3, Part I, column 8, line 14, plus line 32, minus the sum of lines 5 and 6, plus employee discount days reported on line 30.
Line 32--Add lines 30 and 31 to equal the hospital’s DSH patient percentage.
Line 33--Compare the percentage on line 32 with the criteria described in 42 CFR 412.106(c) and (d). Enter the payment adjustment factor calculated in accordance with 42 CFR 412.106(d). Hospitals qualifying for DSH in accordance with 42 CFR 412.106(c)(2) (Pickle Amendment hospitals), if Worksheet S-2, Part I, line 22, column 2 is “Y” for yes, enter 35.00 percent on line 33.
Line 34--Multiply line 33 by line 1 for cost reporting periods ending on or before September 30, 2013. Effective for cost reporting periods that overlap October 1, 2013, enter the sum of {(line 33 times line 1.01), plus ((line 33 times the sum of lines 1.02 and 1.03) times 25 percent)}. For cost reporting periods beginning on or after October 1, 2013, multiply (line 33 times the sum of lines 1 and 1.03) times 25 percent.
Section 3133 of the ACA provides that for services occurring on or after October 1, 2013 a subsection (d) (i.e., IPPS hospital) hospital which is entitled to a receive a DSH payment will receive two separately calculated payments. The “empirically justified Medicare DSH payment” which represents 25 percent of the amount the hospital would have received under 42 CFR 412.106(d) is calculated on line 34. The “additional payment for uncompensated care” payment is calculated on lines 35 through 36.
40-172 Rev.
DRAFT FORM CMS-2552-10 4030.1 (Cont.)
Uncompensated Care Adjustment--Section 3133 of the ACA: (1) provides that for discharges occurring on or after October 1, 2013, subsection (d) hospitals’ Medicare DSH payments are reduced by 75 percent (to the empirically justified Medicare DSH payment); and (2) established an uncompensated care payment amount which represents the remaining 75 percent of the DSH payments and distributes a portion of this amount to each qualifying DSH hospital based on its share of uncompensated care. Effective for cost reporting periods overlapping or beginning on or after October 1, 2013, complete lines 35 through 36, columns 1 and 2, as applicable only if you are a subsection (d) hospital and answered yes to Worksheet S-2, Part I, line 22, column 1.
If Worksheet S-2, Part I, line 22, column 1, is “Y” and Worksheet S-2, Part I, line 22.01, columns 1 and 2, are “Y”, do not complete lines 35 and 35.01. If Worksheet S-2, Part I, line 22.01, either column 1 or 2, is “N”, complete only the column with the “N” response for lines 35 and 35.01. A response of “Y” for both questions indicates that a hospital uncompensated care payment has been pre-determined for your hospital for the applicable FFY.
NOTE: For cost reporting periods that overlap October 1, 2013, column 1 should be left blank and only column 2 should be completed. For cost reporting periods that begin on October 1, complete only column 2 (i.e, enter “N” for no in column 1 or leave column 1 blank).
Line 35--If Worksheet S-2, Part I, line 22, column 1 is “Y” and Worksheet S-2, Part I, line 22.01, column 1 or 2 is “N”, enter in the corresponding column the full amount (for all eligible IPPS hospitals) available for uncompensated care payments for the appropriate FFY. For example, for a cost reporting period ending December 31, 2013, enter zero in column 1 for the portion of the cost reporting period that began prior to October 1, 2013, and enter the FFY14 uncompensated care payment amount of $9,046,380,143 in column 2.
Line 35.01--If Worksheet S-2, Part I, line 22.01, column 1 or 2, is “N”, enter the applicable factor 3 value determined by CMS for uncompensated care payments for the appropriate FFY in columns 1 and 2, respectively. If you are a new hospital, Worksheet S-2, Part I, line 47, column 2, is “Y”, factor 3 must be calculated. In determining factor 3 the numerator is the current year cost report Medicaid days (Worksheet S-2, Part I, line 24, sum of columns 1 through 6) plus the SSI days published for the applicable FFY divided by the denominator which is a fixed amount obtained from the applicable FFY IPPS rule. For FFY14 the denominator is 36,429,747 (this represents the total IPPS hospitals Medicaid days and SSI days for FFY14). Round this factor 3 to 9 decimal places.
Line 35.02-- If Worksheet S-2, Part I, line 22, column 1 is “Y” and Worksheet S-2, Part I, line 22.01, column 1 or 2 is “Y”, enter the hospital uncompensated care payment amount determined by CMS for the appropriate FFY in columns 1 and 2. If Worksheet S-2, Part I, line 22, column 1 is “Y” and Worksheet S-2, Part I, line 22.01, column 1 or 2 is “N”, then CMS did not determine the hospital uncompensated care payment amount for that FFY. Compute this amount by multiplying line 35 times line 35.01, for columns 1 and 2, respectively. If Worksheet S-2, Part I, line 22, column 1, is “N” and/or line 34 above is zero, enter zero on this line.
Line 35.03--Enter the pro rata share of the hospital’s uncompensated care payment in columns 1 and 2. Enter in column 1 (line 35.02 times the number of days in the cost reporting period prior to October 1 divided by the total days in the FFY). Enter in column 2 (line 35.02 times the number of days in the cost reporting period on or after October 1 divided by the total days in the FFY).
For example, a calendar year cost reporting period January 1, 2013 through December 31, 2013, enter zero in column 1, for the period of (January 1, 2013 through September 30, 2013) this period is prior to FFY 14; enter in column 2, for the period of (October 1, 2013 through December 31, 2013 (FFY 14)), (92 days/365 days in FFY 14) times line 35.02, column 2.
Rev. 40-172.1
4030.1 (Cont.) FORM CMS-2552-10 DRAFT
As another example, a calendar year cost reporting period of January 1, 2014 through December 31, 2014, enter in column 1, for the period (January 1, 2014 through September 30, 2014 (FFY 14)), (273 days/365 days in FFY 14) times lines 35.02, column 1; enter in column 2, for the period of (October 1, 2014 through December 31, 2014 (FFY 15)), (92 days/365days in FFY 15) times line 35.02, column 2.
Line 36--Enter the hospital’s uncompensated care adjustment amount, (the sum of columns 1 and 2, line 35.03.)
Lines 37 through 39--Reserved for future use.
Additional Payment for High Percentage of ESRD Beneficiary Discharges--Calculate the additional payment amount allowable for a high percentage of ESRD beneficiary discharges pursuant to 42 CFR 412.104. When the average weekly cost per dialysis treatment changes within a cost reporting period, create an additional column (column 1.01) for lines 41 and 45.
Line 40--Enter total Medicare discharges excluding discharges for MS-DRGs 652, 682, 683, 684, and 685 (see 73 FR 48447 and 48520 (August 19, 2008)). Effective for cost reporting periods beginning on or after October 1, 2011, enter total Medicare discharges (see 76 FR 51693 (August 18, 2011)) for all Medicare beneficiaries entitled to Medicare Part A. Individuals entitled to Medicare Part A include individuals receiving benefits under original Medicare, individuals whose inpatient benefits are exhausted or whose stay was not covered by Medicare, and individuals enrolled in Medicare Advantage Plans, cost contracts under §1876 of the Act (HMOs), and competitive medical plans (CMPs). These discharges, excluding discharges for MS-DRGs 652, 682, 683, 684, and 685, must be included in the denominator of the calculation for the purpose of determining eligibility for the ESRD additional payment to hospitals.
40-172.2 Rev.
DRAFT FORM CMS-2552-10 4030.1 (Cont.)
Line 41--Enter total Medicare discharges for ESRD beneficiaries who received dialysis treatment during an inpatient stay (see 69 FR 49087 (August 11, 2004)) excluding MS-DRGs 652, 682, 683, 684, and 685 (see 73 FR 48520 and 48447 (August 19, 2008)). Effective for cost reporting periods beginning on or after October 1, 2011, enter total Medicare discharges (see 76 FR 51693 (August 18, 2011)) for all ESRD Medicare beneficiaries entitled to Medicare Part A who receive inpatient dialysis. Individuals entitled to Medicare Part A include individuals receiving benefits under original Medicare, individuals whose inpatient benefits are exhausted or whose stay was not covered by Medicare, and individuals enrolled in Medicare Advantage Plans, cost contracts under §1876 of the Act (HMOs), and CMPs. These discharges, excluding discharges for MS‑DRGs 652, 682, 683, 684, and 685, must be included in the numerator of the calculation for the purpose of determining eligibility for the ESRD additional payment to hospitals.
Line 41.01--Enter total Medicare discharges for ESRD beneficiaries who received dialysis treatment during an inpatient stay (see 69 FR 49087 (August 11, 2004)) excluding MS-DRGs 652, 682, 683, 684, and 685 (see 73 FR 48520 and 48447 (August 19, 2008)). The discharges on this line are associated with Medicare covered and paid hospital stays, and are included in the discharges in Worksheet S-3, Part I, column 13, line 14. These discharges are a subset of the discharges on line 41. The discharges on this line are only used to determine the ESRD add-on payment, not eligibility for the add-on payment.
Line 42--Divide line 41, sum of columns 1 and 1.01, by line 40. If the result is less than 10 percent, you do not qualify for the ESRD adjustment.
Line 43--Enter the total Medicare ESRD inpatient days excluding MS-DRGs 652, 682, 683, 684, and 685, as applicable. The Medicare ESRD inpatient days must be included in the Medicare inpatient days reported in Worksheet S-3, Part I, column 6, line 14 and are part of a Medicare covered stay.
Line 44--Enter the average length of stay expressed as a ratio to 7 days. For cost reporting periods ending before June 30, 2014, divide line 43 by line 41, sum of columns 1 and 1.01, and divide that result by 7 days. For cost reporting periods ending on or after June 30, 2014, divide line 43 by line 41.01, sum of columns 1 and 1.01, and divide that result by 7 days.
Line 45--Enter the average weekly cost per dialysis treatment calculated by multiplying the unadjusted composite rate per treatment by 3. For example, the average weekly cost per dialysis treatment for CY 2013 is $435.60 ($145.20 times the average weekly number of treatments of 3). This amount is subject to change on an annual basis. Consult the appropriate CMS change request for future rates
Line 46--For cost reporting periods ending before June 30, 2014, enter the ESRD payment adjustment (line 44, column 1 times line 45, column 1 times line 41, column 1 plus, if applicable, line 44, column 1 times line 45, column 1.01 times line 41, column 1.01). For cost reporting periods ending on or after June 30, 2014, enter the ESRD payment adjustment (line 44, column 1 times line 45, column 1 times line 41.01, column 1 plus, if applicable, line 44, column 1 times line 45, column 1.01 times line 41.01, column 1.01).
Rev. 40-173
4030.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 47--Enter the sum of lines 1, 1.01, 1.02, 2, 2.01, 2.02, 29, 34, 36 and 46.
Line 48--Sole community hospitals are paid the highest of the federal payment rate, the hospital-specific rate (HSR) determined based on a federal fiscal year 1982 base period (see 42 CFR 412.73), the hospital-specific rate determined based on a federal fiscal year 1987 base period (See 42 CFR 412.75), for cost reporting periods beginning on or after October 1, 2000, the hospital-specific rate determined based on a federal fiscal year 1996 base period (See 42 CFR 412.77), or for cost reporting periods beginning on or after January 1, 2009, the hospital-specific rate determined based on a federal fiscal year 2006 base period (See 42 CFR 412.78). Medicare dependent hospitals are paid the highest of the federal payment rate, or the federal rate plus 75 percent of the amount of the excess over the federal rate of the highest rate for the 1982, 1987, or 2002 (See 42 CFR 412.79), base period hospital specific rate. For SCHs and Medicare dependent/small rural hospitals, enter the applicable hospital-specific payments.
For sole community hospitals only, the hospital-specific payment amount entered on this line is supplied by your contractor. Calculate it by multiplying the sum of the DRG weights for the period (per the PS&R) by the final per discharge hospital-specific rate for the period. For new hospital providers established after 1987, do not complete this line. Use the hospital specific rate based on the higher of the cost reporting periods beginning in FFY 1982, 1987, or 1996.
Additionally, for sole community hospitals only (effective for cost reporting periods beginning on or after January 1, 2009), use the highest of the determined hospital specific rate based on federal fiscal year 1982, 1987, 1996, or 2006.
For MDH discharges occurring on or after October 1, 2006, and before April 1, 2015, an MDH can use a FFY 2002 hospital specific rate. The MDH program ends on March 31, 2015.
Line 49--For SCHs, enter the greater of line 47 or 48. For MDH discharges occurring on or after October 1, 2006, and before April 1, 2015, if line 47 is greater than line 48, enter the amount on line 47. Where line 48 is greater than line 47, enter the amount on line 47, plus 75 percent of the amount that line 48 exceeds line 47. Hospitals not qualifying as SCH or MDH providers will enter the amount from line 47.
For hospitals subscripting column 1 of line 47 due to a change in geographic location, this computation will be computed separately for each column, and the sum of the calculations will be entered in column 1 of this line.
Line 50--Enter the payment for inpatient program capital costs from Worksheet L, Part I, line 12; or Part II, line 5, as applicable.
Line 51--Enter the special exceptions payment for inpatient program capital, if applicable pursuant to 42 CFR 412.348(f) by entering the result of Worksheet L, Part III, line 13 less Worksheet L, Part III, line 17. If this amount is negative, enter zero on this line.
Line 52--Enter the amount from Worksheet E-4, line 49. Complete this line only for the hospital component.
Obtain the payment amounts for lines 53 and 54 from your contractor.
Line 53--Enter the amount of Nursing and Allied Health Managed Care payments if applicable.
Line 54--Enter the special add-on payment for new technologies (see 42 CFR 412.87 and 412.88).
Line 55--Enter the net organ acquisition cost from Worksheet(s) D-4, Part III, column 1, line 69.
40-174 Rev.
09-14 FORM CMS-2552-10 4030.1 (Cont.)
Line 56--Teaching hospitals or subproviders electing to be reimbursed for services of physicians on the basis of reasonable cost (see 42 CFR 415.160 and CMS Pub. 15-1, chapter 21, §2148), enter the cost of physicians. For cost reporting periods ending before June 30, 2014, transfer the amount from Worksheet D-5, Part II, column 3, line 20. For cost reporting periods ending on or after June 30, 2014, transfer the amount from Worksheet D-5, Part IV, line 20.
Line 57--Enter the routine service other pass through costs from Worksheet D, Part III, column 9, lines 30 through 35 for the hospital.
Line 58--Enter the ancillary service other pass through costs from Worksheet D, Part IV, column 11, line 200.
Line 59--Enter the sum of lines 49 through 58.
Line 60--Enter the amounts paid or payable by workers’ compensation and other primary payers when program liability is secondary to that of the primary payer. There are six situations under which Medicare payment is secondary to a primary payer:
Workers' compensation,
No fault coverage,
General liability coverage,
Working aged provisions,
Disability provisions, and
Working ESRD provisions.
Generally, when payment by the primary payer satisfies the total liability of the program beneficiary, for cost reporting purposes only, treat the services as if they were non-program services. (The primary payment satisfies the beneficiary's liability when you accept that payment as payment in full. This is noted on no-pay bills submitted by you in these situations.) Include the patient days and charges in total patient days and charges but do not include them in program patient days and charges. In this situation, enter no primary payer payment on line 60. In addition, exclude amounts paid by other primary payers for outpatient dialysis services reimbursed under the composite rate system.
However, when the payment by the primary payer does not satisfy the beneficiary's obligation, the program pays the lesser of (a) the amount it otherwise pays (without regard to the primary payer payment or deductible and coinsurance) less the primary payer payment, or (b) the amount it otherwise pays (without regard to the primary payer payment or deductible and coinsurance) less applicable deductible and coinsurance. Credit primary payer payment toward the beneficiary's deductible and coinsurance obligation.
When the primary payment does not satisfy the beneficiary's liability, include the covered days and charges in program days and charges and include the total days and charges in total days and charges for cost apportionment purposes. Enter the primary payer payment on line 60 to the extent that primary payer payment is not credited toward the beneficiary's deductible and coinsurance. Do not enter primary payer payments credited toward the beneficiary's deductible and coinsurance on line 60.
Enter the primary payer amounts applicable to organ transplants. However, do not enter the primary payer amounts applicable to organ acquisitions. Report these amounts on Worksheet D-4, Part III, line 66.
If you are subject to PPS, include the covered days and charges in the program days and charges, and include the total days and charges in the total days and charges for inpatient and pass through cost apportionment. Furthermore, include the DRG amounts applicable to the patient stay on line 1. Enter the primary payer payment on line 60 to the extent that the primary payer payment is not credited toward the beneficiary's deductible and coinsurance. Do not enter primary payer payments credited toward the beneficiary's deductibles.
Rev. 6 40-175
4030.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 61--Enter the result of line 59 minus line 60.
Line 62--Enter from the PS&R or your records the deductibles billed to program patients excluding deductibles and coinsurance associated with Model 4 BPCI payments.
Line 63--Enter from the PS&R or your records the coinsurance billed to program patients excluding deductibles and coinsurance associated with Model 4 BPCI payments.
Line 64--Enter the program allowable bad debts, reduced by the bad debt recoveries. If recoveries exceed the current year’s bad debts, line 64 and 65 will be negative.
Line 65--Enter the result of line 64 (including negative amounts) times 70 percent for cost reporting periods that begin prior to October 1, 2012. For cost reporting periods that begin on or after October 1, 2012, enter the result of line 64 times 65 percent.
Line 66--Enter the gross allowable bad debts for dual eligible beneficiaries. This amount is reported for statistical purposes only. These amounts must also be reported on line 64.
Line 67--Enter the sum of lines 61 and 65 minus the sum of lines 62 and 63.
Line 68--Enter from the PS&R, the partial or full credits received from manufacturers for replaced devices applicable to MS-DRGs listed in the IPPS final rule for the applicable cost reporting period. See CMS Pub. 100-04, chapter 3, §100.8.
Line 69--Enter the time value of money for operating expenses, the capital outlier reconciliation amount and time value of money for capital-related expenses by entering the sum of lines 93, 95, and 96.
For SCHs, if the hospital specific payment amount on line 48, is greater than the federal specific payment amount on line 47, do not complete this line.
Line 70--Enter any other adjustments. Specify the adjustment in the space provided. Hardcoded subscripts of this line are identified as such.
Line 70.92--Enter the discount amount for the bundled payments for care improvement initiative (also referred to as Model 1) in accordance with ACA 2010, §3023, effective for discharges occurring on or after October 1, 2013. This demonstration actually began April 1, 2013, however the discounted payments begin October 1, 2013. Obtain this amount from the PS&R.
Line 70.93--Enter the payment adjustment amount for the hospital value-based purchasing (HVBP) program in accordance with ACA 2010, §300, effective for discharges occurring on or after October 1, 2012. Obtain this amount from the PS&R.
Line 70.94--Enter the adjustment amount resulting from the hospital readmissions reduction program in accordance with ACA 2010, §3025, effective for discharges occurring on or after October 1, 2012. Obtain this amount from the PS&R.
Line 70.95--Enter the program share of any recovery of accelerated depreciation applicable to prior periods resulting from your termination or a decrease in Medicare utilization. (See CMS Pub. 15-1, chapter 1, §§136-136.16, and 42 CFR 413.134(d)(3)(i).)
40-176 Rev.
DRAFT FORM CMS-2552-10 4030.1 (Cont.)
Line 70.96 through 70.98 (lines 70.96 and 70.97 are hardcoded)--Effective for discharges occurring during federal fiscal years 2011 through 2015 (discharges before April 1, 2015) (e.g., standard federal fiscal years: October 1, 2010 through September 30, 2011; October 1, 2011 through September 30, 2012; etcetera), temporary improved/changed payments are mandated by §§3125 and 10314 ACA of 2010 and subsequent legislation, as addressed in 42 CFR 412.101. For cost reporting periods that are concurrent with the federal fiscal year (10/1 through 9/30), use line 70.97 only. For cost reporting periods that overlap October 1 for years 2010, 2011, 2012, 2013, 2014 and 2015 (discharges occurring before April 1, 2015), enter on lines 70.96 (Low volume adjustment (enter the corresponding federal year for the period prior to 10/1)) and line 70.97 (Low volume adjustment (enter the corresponding federal year for the period ending on or after 10/1)), and if necessary line 70.98 (low volume adjustments for additional portions of the cost reporting period, if necessary), the Medicare inpatient payment adjustment for low volume hospitals as applicable in accordance with Exhibit 4 (low volume adjustment calculation schedule and corresponding instructions).
Line 71--Enter the result of line 67 plus or minus lines 69, 70.93, 70.94, 70.96, 70.97, 70.98, and line 70 and its subscripts not previously identified, minus lines 68, 70.92 and 70.95.
Line 71.01--For cost reporting periods that overlap or begin on or after April 1, 2013, enter the sequestration adjustment amount as follows: [(2 percent times (total days in the cost reporting period that occur during the sequestration period beginning on or after April 1, 2013, divided by total days in the entire cost reporting period, rounded to four decimal places)) times line 71].
Line 72--Enter the total interim payments (received or receivable) from Worksheet E-1, column 2, line 4. For contractor final settlements, enter the amount reported on Worksheet E-1, column 2, line 5.99 on line 73. Included in the interim payments are the amounts received as the estimated nursing and allied health managed care payments and capital, IME, DSH and outlier payments associated with Model 4 BPCI.
Line 74--Enter line 71 minus the sum of lines 71.01, 72 and 73. Transfer to Worksheet S, Part III.
Line 75--Enter the program reimbursement effect of protested items. Estimate the reimbursement effect of the non-allowable items by applying a reasonable methodology which closely approximates the actual effect of the item as if it had been determined through the normal cost finding process. (See CMS Pub. 15-2, chapter 1, §115.2.) Attach a schedule showing the details and computations for this line.
Lines 76 through 89 were intentionally skipped to accommodate future revisions to this worksheet.
DO NOT COMPLETE THE REMAINDER OF WORKSHEET E, PART A. LINES 90 THROUGH 96 ARE FOR CONTRACTOR USE ONLY.
Line 90--Enter the original operating outlier amount from line 2 sum of all columns of this Worksheet E, Part A prior to the inclusion of lines 92, 93, 95, and 96 of Worksheet E, Part A.
Line 91--Enter the original capital outlier amount from Worksheet L, part I, line 2.
Line 92--Enter the operating outlier reconciliation adjustment amount in accordance with CMS Pub. 100-4, chapter 3, §§20.1.2.5-20.1.2.7.
Line 93--Enter the capital outlier reconciliation adjustment amount in accordance with CMS Pub. 100-4, chapter 3, §§20.1.2.5-20.1.2.7.
Rev. 40-176.1
4030.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 94--Enter the interest rate used to calculate the time value of money. (See CMS Pub. 100‑04, chapter 3, §§20.1.2.5-20.1.2.7.)
Line 95--Enter the operating time value of money for operating related expenses.
Line 96--Enter the capital time value of money for capital-related expenses.
NOTE: If a cost report is reopened more than one time, subscript lines 90 through 96, respectively, one time for each time the cost report is reopened.
Instructions For Completing Exhibit 4--
Low Volume Adjustment Calculation Schedule:
Sections 3125 and 10314 of ACA 2010 and subsequent legislation amended the low-volume hospital adjustment in §1886(d)(12) of the Social Security Act by revising, for FFYs 2011 through 2015 (discharges before April 1, 2015) the definition of a low-volume hospital and the methodology for calculating the low-volume payment adjustment. CMS implemented these changes to the low-volume payment adjustment in the regulations at 42 CFR 412.101 in the FFY 2011 IPPS final rule (75 FR 50238 through 50275 (March 7, 2013)).
The legislative amendments referenced in the preceding paragraph provide for a temporary change in the low-volume adjustment for qualifying hospitals for FFYs 2011 through 2015 (discharges before April 1, 2015) as follows:
Those hospitals with 200 or fewer Medicare discharges will receive an adjustment of an additional 25 percent for each discharge; and
Those with more than 200 and fewer than 1,600 Medicare discharges will receive an adjustment of an additional percentage for each discharge. This adjustment is calculated using the formula [(4/14) - (Medicare discharges/5600)].
And to qualify as a low-volume hospital, the hospital must meet both of the following criteria:
Be more than 15 road miles from the nearest subsection (d) hospital; and
Have fewer than 1,600 Medicare discharges based on the latest available Medicare Provider Analysis and Review (MedPAR) data.
CMS provided a table listing the IPPS hospitals with fewer than 1,600 Medicare discharges and their low-volume percentage add-on, if applicable, for FFYs 2011 through 2015 (discharges before April 1, 2015). However, this list is not a list of all hospitals that qualify for the low-volume adjustment since it does not reflect whether or not the hospital meets the mileage criteria. Hospitals were required to request low-volume status in writing to their contractor and provide documentation that they met the mileage criteria.
The low-volume payment adjustment for eligible hospitals is based on their total per discharge payments made under §1886 of the Act, including capital IPPS payments, DSH payments, IME payments, and outlier payments. For SCHs and MDHs, the low‑volume payment adjustment for eligible hospitals is based on either the federal rate or the hospital-specific payment (HSP) rate, whichever results in a greater operating IPPS payment. The low-volume payment amount calculated by the IPPS Pricer is an interim payment amount and is subject to adjustment during year end cost report settlement if any of the payment amounts upon which the low-volume payment amount is based are also recalculated at cost report settlement (for example, payments for DSH and IME or federal rate versus HSP rate payments for SCHs and MDHs).
40-176.2 Rev.
DRAFT FORM CMS-2552-10 4030.1 (Cont.)
NOTE: Because a hospital’s eligibility for the low-volume payment adjustment and/or a hospital’s applicable low-volume adjustment percentage can change during its cost reporting period (for example, a hospital with a cost report that spans the start of the FFY), it is necessary to determine the low-volume payment amount using the applicable low-volume adjustment percentage for the FFY and payment amounts listed above for a hospital’s discharges that occur during the FFY for each FFY included by the hospital’s cost reporting period.
After the cost report is calculated for settlement the low-volume payment adjustment must be calculated. The low-volume payment amount must be calculated by FFY. Therefore, if the cost report overlaps a FFY the information computed on Worksheet E, Part A must be recomputed by FFY accordingly. The amounts may not be prorated but must be calculated using the appropriate information. The following payment amounts are multiplied by the low-volume payment adjustment percentage by FFY:
Operating Federal IPPS payments;
Operating HSR payments;
Operating Outlier payments including any Operating Outlier Reconciliation amounts;
Operating IME payments;
Operating IME payments for Medicare Advantage patients;
Operating DSH payments;
ESRD Adjustment payments;
Total Capital IPPS payment
New Technology payments; and
Capital Outlier Reconciliation amounts (if applicable, see instructions)
Complete Exhibit 4 to compute the low-volume adjustment payment applicable to this cost reporting period. The following Exhibit 4 is designed to simulate the Medicare cost report and must be completed after the cost report is calculated for settlement.
Column 0--Line references are comparable to the actual line references on Worksheet E, Part A and Worksheet L, Part I.
Column 1--Enter from Worksheet E, Part A, and Worksheet L, Part I, the amounts reported on the corresponding lines of the Medicare cost report.
Column 2--Enter amounts related to discharges occurring in the cost reporting period either pre-entitlement (discharges occurring in the cost reporting period prior to October 1) or post-entitlement (discharges occurring in the cost reporting period on or after October 1). Discharges occurring in these periods are not eligible for the low-volume adjustment.
In addition, if there are discharges occurring during FFY 2011 through 2015 (discharges before April 1, 2015) and the provider was not eligible for the low-volume adjustment for the entire eligibility period, report the information relative to those discharges in this column, for example, where a provider has a cost reporting period ending June 30, 2011, which began prior to the October 1, 2010 effective date of the provision. Or where the low-volume adjustment for discharges occurring in this cost reporting period is effective for discharges on or after October, 1, 2010; however, the provider did not request the low-volume adjustment until November 15, 2010 and the low-volume adjustment was implemented within 30 days of the request. The period of time from October 1, 2010 until the contractor notified the provider of eligibility, which should be no later than December 15, 2010, is considered a period of ineligibility.
Rev. 40-176.3
4030.1 (Cont.) FORM CMS-2552-10 09-14
Column 3--Enter amounts related to discharges occurring during the provider’s low-volume eligibility period and prior to October 1st. If the cost reporting period is not concurrent with a federal year of October 1st through September 30th, do not include discharges occurring on or after October 1st in this column.
If the provider goes in and out of eligibility for discharges occurring prior to October 1st, add all discharges for the eligibility periods prior to October 1st and include in this column. If the provider’s classification (i.e. SCH to small rural) changes during the eligibility period, use subscripted column 3.01 to accommodate the change for discharges occurring prior to October 1st.
Column 4--Enter amounts related to discharges occurring during the provider’s low-volume eligibility period and on or after October 1st. If the cost reporting period is concurrent with a federal year of October 1st through September 30th, report all discharges occurring on or after October 1st in this column. If the provider goes in and out of eligibility for discharges occurring on or after October 1st, add all discharges for the eligibility periods on or after October 1st and include in this column. If the provider’s classification (i.e. SCH to small rural) changes during the eligibility period, use subscripted column 4.01 to accommodate the change for discharges occurring on or after October 1st.
Columns 3, 3.01, 4, and 4.01--Use the beginning and ending dates of the applicable portion of the cost reporting period as the respective column headings.
Column 5--Subtotal columns 2 through 4 and applicable subscripts. Column 5 must equal column 1 and any resulting rounding difference must be applied to the highest value in columns 2 through 4 and applicable subscripts.
Line Descriptions
Line 1--The amount entered on this line is computed as the sum of the Federal operating portion (DRG payment) paid for PPS discharges during the cost reporting period and the DRG payments made for PPS transfers during the cost reporting period. The PS&R information must be split and reported in columns 2 through 4 and must concur with the PS&R paid through date used to calculate the cost report for settlement.
Line 1.01 (Corresponds to Worksheet E, Part A, line 1.01)--Enter the DRG amounts other than outlier payments for discharges occurring prior to October 1, 2013, in column 3.
Line 1.02 (Corresponds to Worksheet E, Part A, line 1.02)--Enter the DRG amounts other than outlier payments for discharges occurring on or after October 1, 2013, in column 4.
Line 1.03 (Corresponds to Worksheet E, Part A, line 1.03)--Enter the DRG for federal specific operating payments for Model 4 BPCI on this line. The PS&R information must be split and reported in columns 2 through 4 and must concur with the PS&R paid through date used to calculate the cost report for settlement.
Line 2--Enter the amount of outlier payments made for PPS discharges occurring during the cost reporting period. The PS&R information must be split and reported in columns 2 through 4 and must concur with the PS&R paid through date used to calculate the cost report for settlement.
40-176.4 Rev. 6
DRAFT FORM CMS-2552-10 4030.1 (Cont.)
Line 2.01 (Corresponds to Worksheet E, Part A, line 2.02)--Enter the outlier payment for discharges for Model 4 BPCI on this line. The PS&R information must be split and reported in columns 2 through 4 and must concur with the PS&R paid through date used to calculate the cost report for settlement.
Line 3 (Corresponds to Worksheet E, Part A, line 2.01)--For inpatient PPS services rendered during the cost reporting period, enter the operating outlier reconciliation amount for operating expenses from line Worksheet E, Part A, line 92 for each respective period. The lump sum utility produces a claim by claim output. If the provider has two different low-volume hospital adjustment percentages during its cost reporting period, the contractor must report the operating and capital outlier reconciliation adjustment amounts for the discharges occurring in each of the federal fiscal years spanned by the cost report separately. The sum of columns 2 through 4 must equal the amount reported on Worksheet E, Part A, line 2.01.
Line 4 (Corresponds to Worksheet E, Part A, line 3)--Enter the indirect medical education for managed care patients based on the DRG payment that would have been made if the service had not been a managed care service. The PS&R will capture, in conjunction with the PPS PRICER, the simulated payments. Enter the total managed care “simulated payments” from the PS&R. The PS&R information must be split and reported in columns 2 through 4 and must concur with the PS&R paid through date used to calculate the cost report for settlement.
Line 5 (Corresponds to Worksheet E, Part A, line 21)--Enter the ratio calculated from Worksheet E, Part A, line 21, in columns 2 through 4.
Line 6 (Corresponds to Worksheet E, Part A, line 22)--Calculate the IME payment adjustment as follows: Multiply the appropriate multiplier of the adjustment factor (currently 1.35) times {((1 + line 5) to the .405 power) - 1} times {the sum of line 1, 1.01, 1.02, 1.03 + line 4}. The sum of columns 2 through 4 must equal the amount reported on Worksheet E, Part A, line 22.
Line 7 (Corresponds to Worksheet E, Part A, line 27)-- Enter the ratio calculated from Worksheet E, Part A, line 27, in columns 2 through 4.
Line 8 (Corresponds to Worksheet E, Part A, Line 28)--IME Add On Adjustment--Enter the sum of lines 1, 1.01, 1.02, 1.03 and 4, multiplied by the factor on line 7.
Line 9 (Corresponds to Worksheet E, Part A, line 29)--Total IME Payment--Enter the sum of lines 6 and 8. The sum of columns 2 through 4 must equal the amount reported on Worksheet E, Part A, line 29.
Line 10 (Corresponds to Worksheet E, Part A, line 33)--Enter the DSH percentage calculated from Worksheet E, Part A, line 33, in columns 2 through 4.
Line 11 (Corresponds to Worksheet E, Part A, line 34)--Multiply line 10 by line 1 for cost reporting periods ending on or before September 30, 2013. Effective for cost reporting periods that overlap October 1, 2013, enter the sum of {(line 10 times line 1.01), plus ((line 10 times the sum of lines 1.02 and 1.03) times 25 percent)}. For cost reporting periods beginning on or after October 1, 2013, multiply (line 10 times the sum of lines 1 and 1.03) times 25 percent. The sum of columns 2 through 4 must equal the amount reported on Worksheet E, Part A, line 34.
Rev. 40-176.5
4030.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 11.01 (Corresponds to Worksheet E, Part A, line 35.03)--Enter the uncompensated care payments.
For cost reporting periods that overlap or begin on or after October 1, 2013, when you are eligible for the low volume payment adjustment for the entire cost reporting period, enter in column 3, the uncompensated care payments from Worksheet E, Part A, column 1, line 35.03, and enter in column 4, the uncompensated care payments from Worksheet E, Part A, column 2, line 35.03.
For cost reporting periods that overlap or begin on or after October 1, 2013, when you are not eligible for the low volume payment adjustment for any portion of the cost reporting period, enter the uncompensated care payments as follows:
Enter in column 3, the uncompensated care payment eligible for the low volume payment adjustment for the portion of the cost reporting period prior to October 1 (calculated as the amount from Worksheet E, Part A, column 1, line 35.03 times the ratio of the number of days prior to October 1 in the cost reporting period eligible for the low volume payment adjustment divided by the total days in the cost reporting period prior to October 1).
Enter in column 4, the uncompensated care payment eligible for the low volume payment adjustment for the portion of the cost reporting period on and after October 1 (calculated as the amount from Worksheet E, Part A, column 2, line 35.03 times the ratio of the number of days on and after October 1 in the cost reporting period eligible for the low volume payment adjustment divided by the total days in the cost reporting period on and after October 1).
Enter in column 2, the uncompensated care payments not eligible for the low volume payment adjustment (calculated as the total uncompensated care payment, from Worksheet E, Part A, line 35.03, sum of columns 1 and 2, minus the sum of the uncompensated care payments reported in columns 3 and 4 of this exhibit). The sum of columns 2 through 4, must equal Worksheet E, Part A, line 36.
Line 12 (Corresponds to Worksheet E, Part A, line 46)--Prorate in columns 2 through 4 the amount reported on Worksheet E, Part A, line 46, based on the ratio of days in each applicable period to total days in the cost reporting period. The sum of columns 2 through 4 must equal the amount reported on Worksheet E, Part A, line 46.
Line 13 (Corresponds to Worksheet E, Part A, line 47)--Enter the sum of lines 1, 1.01, 1.02, 2, 2.01, 3, 9, 11, 11.01 and 12. The sum of columns 2 through 4 must equal the amount reported on Worksheet E, Part A, line 47.
Line 14 (Corresponds to Worksheet E, Part A, line 48)--For SCHs and Medicare dependent/small rural hospitals, enter the applicable hospital-specific payments. The sum of columns 2 through 4 must equal the amount reported on Worksheet E Part A, line 48. If Worksheet E, Part A, line 47 is greater than Worksheet E, Part A, line 48, do not complete this line.
40-176.6 Rev.
DRAFT FORM CMS-2552-10 4030.1 (Cont.)
Line 15 (Corresponds to Worksheet E, Part A, line 49)--Enter in column 1, the amount from Worksheet E, Part A, line 49. For SCHs, if line 13, column 1 is greater than line 14, column 1, enter in columns 2 through 4, the amount reported on line 13, for each applicable column. If line 14, column 1, is greater than line 13, column 1, enter in columns 2 through 4, the amount reported on line 14, for each applicable column. For MDH discharges occurring on or after October 1, 2006, and before April 1, 2015, if line 13, column 1 is greater than line 14, column 1, enter in columns 2 through 4, the amount reported on line 13, for each applicable column. If line 14, column 1, is greater than line 13, column 1, enter in columns 2 through 4, the amount on line 13, for each applicable column, plus or minus 75 percent of the difference between line 14 minus line 13 for each applicable column. Hospitals not qualifying as SCH or MDH providers will enter in columns 2 through 4, the amount from line 13, for each applicable column. The sum of columns 2 through 4 must equal the amount reported on Worksheet E, Part A, line 49.
Line 16 (Corresponds to Worksheet E, Part A, line 50)--Enter in columns 2 through 4, the amounts computed from line 26, columns 2 through 4. The sum of columns 2 through 4 must equal the amount reported on Worksheet E, Part A, line 50.
Line 17 (Corresponds to Worksheet E, Part A, line 54)--Enter the add-on payment for new technologies. The PS&R information must be split and reported in columns 2 through 4 and must concur with the PS&R paid through date used to calculate the cost report for settlement.
Line 18 (Corresponds to Worksheet E, Part A, line 93)--Enter the capital outlier reconciliation adjustment amount in columns 2 through 4 accordingly. The sum of columns 2 through 4 must equal the amount reported on Worksheet E, Part A, line 93.
Line 19 Subtotal--Enter in columns 2 through 4, the sum of amounts on lines 15, 16, 17 and 18. For SCH, if the hospital specific payment amount on line 14, column 1, is greater than the federal specific payment amount on line 13, column 1, enter in columns 2 through 4, the sum of the amounts on lines 15, 16 and 17.
Line 20 (Corresponds to Worksheet L, Part I, line 1)--Enter the amount of the federal rate portion of the capital DRG payments for other than outlier during this cost reporting period. The PS&R information must be split and reported in columns 2 through 4 and must concur with the PS&R paid through date used to calculate the cost report for settlement. The sum of columns 2 through 4 must equal the amount reported on Worksheet L, Part I, line 1.
Line 20.01 (Corresponds to Worksheet L, Part I, line 1.01)--Enter the Model 4 BPCI Capital DRG other than outlier payments. The PS&R information must be split and reported in columns 2 through 4 and must concur with the PS&R paid through date used to calculate the cost report for settlement. The sum of columns 2 through 4 must equal the amount reported on Worksheet L, Part I, line 1.01.
Line 21 (Corresponds to Worksheet L, Part I, line 2)--Enter the amount of the federal rate portion of the capital outlier payments made for PPS discharges during this cost reporting period. The PS&R information must be split and reported in columns 2 through 4 and must concur with the PS&R paid through date used to calculate the cost report for settlement. The sum of columns 2 through 4 must equal the amount reported on Worksheet L, Part I, line 2.
Rev. 40-176.7
4030.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 21.01 (Corresponds to Worksheet L, Part I, line 2.01)--Enter the Model 4 BPCI Capital DRG outlier payments. The PS&R information must be split and reported in columns 2 through 4 and must concur with the PS&R paid through date used to calculate the cost report for settlement. The sum of columns 2 through 4 must equal the amount reported on Worksheet L, Part I, line 2.01.
Line 22 (Corresponds to Worksheet L, Part I, line 5)--Enter the ratio calculated from Worksheet L, Part I, line 5, in all applicable columns.
Line 23 (Corresponds to Worksheet L, Part I, line 6)--Multiply line 22 by the sum of lines 20 and 20.01. The sum of columns 2 through 4 must equal the amount reported on Worksheet L, Part I, line 6.
Line 24 (Corresponds to Worksheet L, Part I, line 10)--Enter the percentage calculated from Worksheet L, Part I, line 10, in all applicable columns.
Line 25 (Corresponds to Worksheet L, Part I, line 11)--Multiply line 24 by the sum of lines 20 and 20.01, and enter the result. The sum of columns 2 through 4 must equal the amount reported on Worksheet L, Part I, line 11.
Line 26 (Corresponds to Worksheet L, Part I, line 12)--Enter the sum of lines 20, 20.01, 21, 21.01, 23, and 25. Transfer this amount to line 16. The sum of columns 2 through 4 must equal the amount reported on Worksheet L, Part I, line 12.
Low-volume payment adjustment--Effective for discharges occurring during FFYs 2011 through 2015 (discharges before April 1, 2015), compute the amount of the low-volume adjustment as follows:
Line 27--Low-volume adjustment factor--Enter the appropriate adjustment factor in columns 3 and 4.
Line 28 (Corresponds to Worksheet E, Part A, line 70.96 discharges prior to October 1st)--Multiply line 19 by line 27. Transfer this amount to the cost report calculated for settlement, Worksheet E, Part A, line 70.96.
Line 29 (Corresponds to Worksheet E, Part A, line 70.97 discharges on or after October 1st)--Multiply line 19 by line 27. Transfer this amount to the cost report calculated for settlement, Worksheet E, Part A, line 70.97.
40-176.8 Rev.
09-14 FORM CMS-2552-10 4030.1 (Cont.)
EXHIBIT 4
LOW VOLUME ADJUSTMENT CALCULATION SCHEDULE
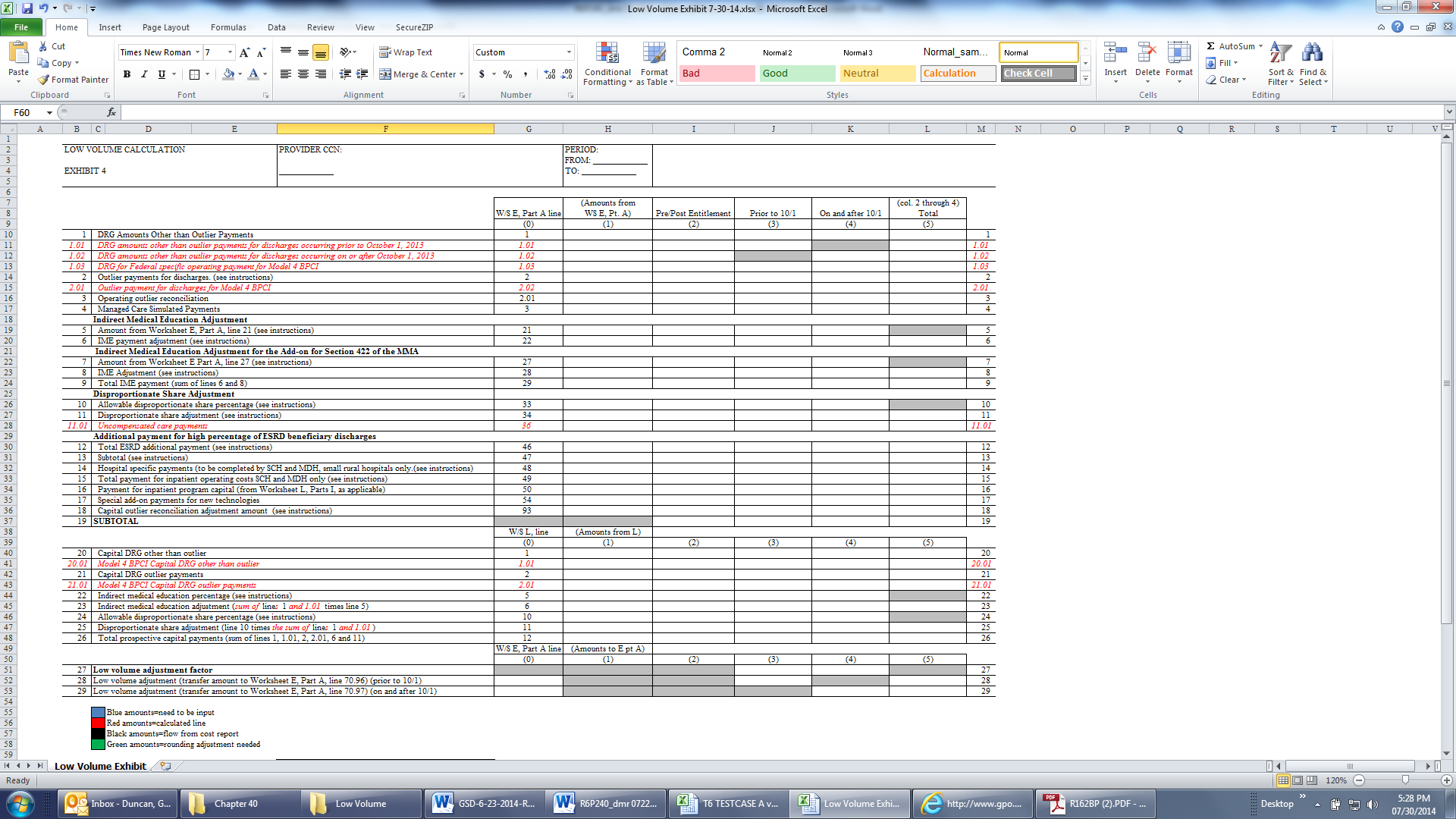
Rev. 6 40-176.9
4030.1 (Cont.) FORM CMS-2552-10 09-14
This page is reserved for future use.
40-176.10 Rev. 6
10-12 FORM CMS-2552-10 4030.2
4030.2 Part B - Medical and Other Health Services--Use Worksheet E, Part B, to calculate reimbursement settlement for hospitals, subproviders, and SNFs.
Use a separate copy of Worksheet E, Part B, for each of these reporting situations. If you have more than one hospital-based subprovider, complete a separate worksheet for each facility. Enter check marks in the appropriate spaces at the top of each page of Worksheet E to indicate the component program for which it is used. When the worksheet is completed for a component, show both the hospital and component numbers. For purposes of prospective payment for outpatient services when the PCR transition date (applicable to cancer hospitals) (see the following paragraph), transitional outpatient payment calculation date, or geographic reclassification date (urban to rural only) (42 CFR 412.103 and 412.230) occurs at other than the cost report period beginning date, complete subscripted column 1.01 in addition to column 1 for lines 2 through 8 only. Order the subscripted columns chronologically as the transition dates or geographic reclassification corresponds to your fiscal year. The dates should also agree with the format on Worksheet D, Part V, columns 2, 2.01, 2.02 and 2.03, etcetera, if applicable.
In accordance with ACA 2010, section 3138, cancer hospitals (as defined in 42 CFR 412.23(f)) must utilize a predetermined PCR to calculate the corresponding transitional outpatient payment effective for services rendered beginning January 1, 2012. Where the cost reporting period overlaps a PCR revision date, subscript column 1 as indicated in the preceding paragraph to correspond to each unique PCR. For calendar year 2012 the PCR for cancer hospitals is 0.91, but is subject to change every calendar year. Enter the applicable PCR(s) on line 5, column 1 and applicable subscripts. See Federal Register, vol. 76, November 30, 2011, page 74206.
NOTE: If you are not a cancer or children’s hospital or covered by ACA section 3121, do not complete lines 2 and 5 through 8.
Line Descriptions
Line 1--Enter the cost of medical and other health services for title XVIII, Part B. This amount also includes the cost of ancillary services furnished to inpatients under the medical and other health services benefit of Medicare Part B. These services are covered in this manner for Medicare beneficiaries with Part B coverage only when Part A benefits are not available. Obtain this amount from Worksheet D, Part V, line 202, columns 6 and 7, for hospitals and enter in column 1. For SNFs transfer the amount from Worksheet D, Part V, columns 6 and 7.
The following providers are temporarily eligible for hold harmless payments and must use columns 1 and 1.01 to correspond to the respective portion of the cost reporting period for lines 2 through 8. Rural hospitals with 100 or fewer beds whose reporting period overlaps December 31, 2012 are eligible through December 31, 2012; SCHs and EACHs regardless of bed size whose reporting period overlaps February 29, 2012 are eligible through February 29, 2012; and SCHs and EACHs with 100 or fewer beds whose reporting period overlaps December 31, 2012 are eligible through December 31, 2012, (Worksheet S-2, Part I, line 120, column 1 or 2 is “Y” for yes).
CAHs are not subject to transitional corridor payments, therefore lines 2 through 9 do not apply to CAHs. Transfer Worksheet D, Part V, columns 6 and 7, line 202.
Line 2--Enter the cost of medical and other health services reimbursed under OPPS from Worksheet D, Part V, column 5 and applicable subscripts, line 202. Subtract from this amount outpatient pass through costs reported on Worksheet D, Part IV, line 200, column 13.
Line 3--Enter the gross PPS payments received including payment for drugs and device pass through payments.
Line 4--Enter the amount of outlier payments made for outpatient PPS services rendered during the cost reporting period.
Rev. 3 40-177
4030.2 (Cont.) FORM CMS-2552-10 10-12
Contractors only, add or subtract as applicable to the gross PPS payments the total outlier reconciliation amount from line 94.
Line 5--Enter the hospital specific payment to cost ratio provided by your contractor. If a new provider does not file a full cost report for a cost reporting period that ends prior to January 1, 2001, the provider is not eligible for transitional corridor payments and should enter zero (0) on this line. (See PM A-01-51)
For cancer hospitals enter a PCR of 0.91 for services rendered during calendar year 2012. Obtain subsequent cancer hospital PCR updates from your contractor or applicable CMS publications.
Line 6--Enter the result of line 2 times line 5.
If the sum of lines 3 and 4 is < line 6 complete lines 7 and 8, otherwise do not complete lines 7 and 8.
Line 7--Enter the result of the sum of lines 3 and 4 divided by line 6.
Line 8--Enter the transitional corridor payment amount calculated based on the following:
a. If the sum of lines 3 and 4 is < line 6 and Worksheet S-2, Part I, line 3, column 4 response is 3 or 7 (cancer or children’s hospital), enter the result of line 6 minus the sum of lines 3 and 4.
In accordance with ACA 2010, section 3121, and MMEA of 2010, section 108, as amended by the Temporary Payroll Tax Cut Continuation Act of 2011, section 308, and the Middle Class Tax Relief and Job Creation Act of 2012, section 3002, the outpatient hold harmless provision is effective for services rendered from January 1, 2010 through February 29, 2012 to all SCHs and EACHs regardless of bed size; and from March 1, 2012 through December 31, 2012 to all SCHs and EACHs with 100 or fewer beds; and from January 1, 2010 through December 31, 2012 for rural hospitals with 100 or fewer beds.
a. For services rendered January 1, 2010 through December 31, 2012, if Worksheet S-2, Part I, line 120, columns 1 or 2 is “Y”, enter 85 percent of the result of line 6 minus the sum of lines 3 and 4.
Line 9--Enter the outpatient ancillary pass through amount from Worksheet D, Part IV, column 13, line 200.
Line 10--If you are an approved CTC, enter the cost of organ acquisition from Worksheet D-4, Part III, column 2, line 69 when Worksheet E is completed for the hospital or the hospital component of a health care complex. Make no entry on line 10 in other situations because the Medicare program reimburses only CTCs for organ acquisition costs.
Line 11--Enter the sum of lines 1 and 10.
Computation of Lesser of Reasonable Cost or Customary Charges--You are paid the lesser of the reasonable cost of services furnished to beneficiaries or the customary charges made by you for the same services. This part provides for the computation of the lesser of reasonable cost or customary charges as defined in 42 CFR 413.13(a).
NOTE: CAHs are not subject to the computation of the lesser of reasonable costs or customary charges. If the component is an CAH, do not complete lines 12 through 20. Instead, enter on line 21 the amount computed on line 11.
40-178 Rev. 3
09-13 FORM CMS-2552-10 4030.2 (Cont.)
Line Descriptions
NOTE: If the medical and other health services reported here qualify for exemption from the application of LCC (see 42 CFR 413.13(c)), also enter the total reasonable cost from line 11 directly on line 21. Still complete lines 6 through 16 to insure that you meet one of the criteria for this exemption.
Lines 12 - 20--These lines provide for the accumulation of charges which relate to the reasonable cost on line 11.
Do not include on these lines: (1) the portion of charges applicable to the excess cost of luxury items or services (see CMS Pub. 15-1, chapter 21, §2104.3) and (2) charges to beneficiaries for excess costs. (See CMS Pub. 15-1, chapter 25, §§2570-2577.)
Line 12--For total charges for medical and other services, enter the sum of Worksheet D, Part V, columns 3 and 4, line 202.
Rev. 4 40-178.1
4030.2 (Cont.) FORM CMS-2552-10 09-13
Line 13--If you are an approved CTC, enter the organ acquisition charges from Worksheet D-4, Part III, column 4, line 69 for the hospital or the hospital component of a health care complex.
Line 14--Enter the sum of lines 12 and 13.
Lines 15 - 18--These lines provide for the reduction of program charges when you do not actually impose such charges on most of the patients liable for payment for services on a charge basis or fail to make reasonable efforts to collect such charges from those patients. If line 17 is greater than zero, multiply line 14 by line 17, and enter the result on line 18. If you impose these charges and make reasonable efforts to collect the charges from patients liable for payment for services on a charge basis, you are not required to complete lines 15 through 17. Enter on line 18 the amount from line 14. In no instance may the customary charges on line 18 exceed the actual charges on line 14. (See 42 CFR 413.13(e).)
Line 19--Enter the excess of the customary charges over the reasonable cost. If line 18 exceeds line 11, enter the difference.
Line 20--Enter the excess of reasonable cost over the customary charges. If line 11, exceeds line 18, enter the difference.
Line 21--Enter the amount from line 11, less any amount reported on line 20 for hospital/services subject to LCC.
For hospital/services that are not subject to LCC in accordance with 42 CFR 413.13 (e.g., CAHs or nominal charge public or private hospitals identified on Worksheet S-2, Part I, lines 155-161), enter the reasonable costs from line 11.
40-178.2 |
Rev. 4 |
09-14 FORM CMS-2552-10 4030.2 (Cont.)
For CAHs enter on this line 101 percent of line 11.
Line 22--Enter the cost of services rendered by interns and residents as follows from Worksheet D-2.
Provider/Component Title XVIII Title XVIII Title XVIII
Hospital Subprovider SNF
Hospital Part I, col. 9, Part I, col. 9, Part I, col. 9,
line 9 plus lines 10, 11 or 12; line 13; or Part II,
line 27; or Part II, or Part II, col. 7, col. 7, line 41; or
col. 7, line 37; or lines 38, 39 or 40 Part III, col. 6,
Part III, col. 6, or Part III, col. 6, line 49
line 45 line 46, 47 or 48
Line 23--Teaching hospitals or subproviders participating in an approved GME program, electing to be reimbursed for services of physicians on the basis of reasonable cost (see 42 CFR 415.160 and CMS Pub. 15-1, chapter 21, §2148), enter the cost of physicians. For cost reporting periods ending before June 30, 2014, transfer the amount from Worksheet D-5, Part II, column 3, line 21. For cost reporting periods ending on or after June 30, 2014, transfer the amount from Worksheet D-5, Part IV, line 21.
Line 24--Enter the sum of lines 3, 4, 8, and 9, all columns.
Computation of reimbursement Settlement
Line 25--Enter the Part B deductibles and the Part B coinsurance billed to Medicare beneficiaries. DO NOT INCLUDE deductibles or coinsurance billed to program patients for physicians' professional services. If a hospital bills beneficiaries a discounted amount for coinsurance, enter on this line the full coinsurance amount not the discounted amount.
Line 26--Enter the deductible and coinsurance relating to the amounts reported on line 24.
NOTE: If these services are exempt from LCC as a result of charges being equal to or less than 60 percent of cost (refer to Worksheet S-2, Part I, lines 155 through 161 columns 1 through 5, as applicable), enter the Part B deductibles billed to program beneficiaries only. Do not enter any Part B coinsurance. For CAHs, enter the deductibles on line 25 and the coinsurance on line 26.
Line 27--Subtract lines 25 and 26 from lines 21 and 24 respectively. Add to that result the sum of lines 22 and 23.
NOTE: If these services are exempt from LCC, (line 21 minus line 25 minus Worksheet D, Part V, line 202, column 7) times 80 percent, then add back Worksheet D, Part V, line 202, column 7, plus lines 22 and 23. Add to that result line 24 minus line 26.
CAHs enter the lesser of (line 21 minus the sum of lines 25 and 26) or 80 percent times the result of (line 21 minus line 25 minus 101% of lab cost (Worksheet D, Part V, column 6, lines 60, 61, and subscripts) minus 101% of costs not subject to deductible and coinsurance (Worksheet D, Part V, column 7, line 202). Add back the aforementioned 101% of lab cost and 101% of cost not subject to deductibles and coinsurance. Add to that result the sum of lines 22 and 23.
Line 28--Enter in column 1 the amount from Worksheet E-4, line 50. Complete this line for the hospital component only.
Line 29--Enter in column 1 the amount from Worksheet E-4, line 36. Complete this line for the hospital component only.
Rev. 6 40-179
4030.2 (Cont.) FORM CMS-2552-10 09-14
Line 30--Enter in column 1 the sum of columns 1 and 1.01, lines 27 through 29.
Line 31--Enter the amounts paid or payable by workers’ compensation and other primary payers when program liability is secondary to that of the primary payer. There are six situations under which Medicare payment is secondary to a primary payer:
Workers’ compensation,
No fault coverage,
General liability coverage,
Working aged provisions,
Disability provisions, and
Working ESRD provisions.
Generally, when payment by the primary payer satisfies the total liability of the program beneficiary, the services are treated as if they were non-program services for cost reporting purposes only. (The primary payment satisfies the beneficiary's liability when you accept that payment as payment in full. This is noted on no-pay bills submitted in these situations.) Include the patient charges in total charges but not in program charges. In this situation, enter no primary payer payment on line 31. In addition, exclude amounts paid by other primary payers for outpatient dialysis services reimbursed under the composite rate system.
However, when the payment by the primary payer does not satisfy the beneficiary's obligation, the program pays the lesser of (a) the amount it otherwise pays (without regard to the primary payer payment or deductible and coinsurance) less the primary payer payment, or (b) the amount it otherwise pays (without regard to the primary payer payment or deductible and coinsurance) less applicable deductible and coinsurance. Credit primary payer payment toward the beneficiary's deductible and coinsurance obligation.
When the primary payment does not satisfy the beneficiary's liability, include the covered charges in program charges, and include the charges in charges for cost apportionment purposes. Enter the primary payer payment on line 31 to the extent that primary payer payment is not credited toward the beneficiary's deductible and coinsurance. Primary payer payments credited toward the beneficiary's deductible and coinsurance are not entered on line 31.
Line 32--Enter line 30 minus line 31.
Line 33--Enter the amount of allowable bad debts for deductibles and coinsurance for ESRD services reimbursed under the composite rate system from Worksheet I-5, line 11.
Allowable bad debts (Exclude bad debts for professional services)
Line 34--Enter from your records allowable bad debts for deductibles and coinsurance net of recoveries for other services, excluding professional services. Do not include ESRD bad debts. These are reported on line 33. Bad debts associated with ambulance services rendered (since these costs are reimbursed on a fee basis) are not allowable. If recoveries exceed the current year’s bad debts, lines 34 and 35 will be negative.
Line 35--Multiply the amount (including negative amounts) on line 34 times 70 percent (hospitals and subproviders only). The reduction does not apply to Critical Access Hospitals.
For cost reporting periods that begin on or after October 1, 2012, multiply the amount (including negative amounts) on line 34 times 65 percent (hospitals and subproviders only).
For CAHs with cost reporting periods beginning on or after October 1, 2012, multiply the amount on line 34 (including negative amounts) times 88 percent. For cost reporting periods beginning on or after October 1, 2013, multiply the amount on line 34 times 76 percent. For cost reporting periods beginning on or after October 1, 2014, multiply the amount on line 34 times 65 percent.
40-180 Rev. 6
DRAFT FORM CMS-2552-10 4030.2 (Cont.)
For SNFs with cost reporting periods beginning prior to October 1, 2012, enter the amount on line 34. For cost reporting periods beginning on or after October 1, 2012, calculate this line as follows: [((line 34 - line 36) * 65 percent) + (line 36 * 88 percent)]. For cost reporting periods beginning on or after October 1, 2013, calculate this line as follows: [((line 34 - line 36) * 65 percent) + (line 36 * 76 percent)]. For cost reporting periods beginning on or after October 1, 2014, multiply the amount on line 34 times 65 percent.
Line 36--Enter the gross allowable bad debts for dual eligible beneficiaries. This amount is reported for statistical purposes only except for the calculation of dual eligible bad debts for SNFs cost reporting periods beginning on or after October 1, 2012. This amount must also be reported on line 34.
Line 37--Enter the sum of lines 32, 33 and 34 or 35 (hospitals and subproviders only). For cost reporting periods beginning on or after October 1, 2012, enter the sum of lines 32, 33 and 35. (hospital, CAH, subproviders and SNFs).
Line 38--Enter the MSP-LCC reconciliation amount. Obtain this amount from the PS&R.
Line 39--Enter any other adjustments. Specify the adjustment in the space provided.
Line 39.98--Enter from the PS&R, the partial or full credits received from manufacturers for replaced devices. See CMS Pub. 100-04, chapter 4, §61.3. This is captured for informational purposes only.
Line 39.99--Enter the program share of any recovery of accelerated depreciation applicable to prior periods resulting from your termination or a decrease in Medicare utilization. (See CMS Pub. 15-1, chapter 1, §§136-136.16, and 42 CFR 413.134(d)(3)(i).)
Line 40--Enter the result of line 37, plus or minus line 39 and its subscripts not previously identified (excluding line 39.98 that is for informational purposes only), minus lines 38 and 39.99.
Line 40.01--For cost reporting periods that overlap or begin on or after April 1, 2013, enter the sequestration adjustment amount as follows: [(2 percent times (total days in the cost reporting period that occur during the sequestration period beginning on or after April 1, 2013, divided by total days in the entire cost reporting period, rounded to four decimal places)) times line 40].
Line 41--Enter interim payments from Worksheet E-1, column 4, line 4. For contractor final settlements, enter the amount reported on line 5.99 on line 42. For contractor purposes it will be necessary to make a reclassification of the bi-weekly pass through payments from Part A to Part B and report that Part B portion on line 42. Maintain the necessary documentation to support the amount of the reclassification.
Line 43--Enter line 40 minus the sum of lines 40.01, 41 and 42. Transfer this amount to Worksheet S, Part III, column 3, line as appropriate.
Line 44--Enter the program reimbursement effect of protested items. Estimate the reimbursement effect of the nonallowable items by a applying reasonable methodology which closely approximates the actual effect of the item as if it had been determined through the normal cost finding process. (See CMS Pub. 15-2, chapter 1, §115.2.) Attach a schedule showing the details and computations for this line.
Lines 45 through 89 were intentionally skipped to accommodate future revisions to this worksheet.
Rev. 40-181
4030.2 (Cont.) FORM CMS-2552-10 DRAFT
DO NOT COMPLETE THE REMAINDER OF WORKSHEET E, PART B. LINES 90 THROUGH 94 ARE FOR CONTRACTOR USE ONLY.
Line 90--Enter the original outlier amount from line 4 (sum of all columns) prior to the inclusion of line 94 of Worksheet E, Part B.
Line 91--Enter the outlier reconciliation adjustment amount in accordance with CMS Pub. 100‑04, chapter 4, §§10.7.2.2-10.7.2.4.
Line 92--Enter the rate used to calculate the time value of money. (See CMS Pub. 100-04, chapter 4, §§10.7.2.2-10.7.2.4.)
Line 93--Enter the time value of money.
Line 94--Enter sum of lines 91 and 93.
NOTE: If a cost report is reopened more than one time, subscript lines 90 through 93, respectively, one time for each time the cost report is reopened.
4031. WORKSHEET E-1 - ANALYSIS OF PAYMENTS TO PROVIDERS FOR SERVICES RENDERED
4031.1 Part I - Analysis of Payments to Providers for Services Rendered--
Complete this worksheet for each component of the health care complex which has a separate provider or subprovider number as shown on Worksheet S-2, Part I. If you have more than one hospital-based subprovider, complete a separate worksheet for each facility. When the worksheet is completed for a component, show both the hospital provider number and the component number. Complete this worksheet only for Medicare interim payments paid by the contractor. Do not complete it for purposes of reporting interim payments for titles V or XIX or for reporting payments made under the composite rate for ESRD services. Providers paid on an interim basis on periodic interim payment (PIP) adjust the interim payments for MSP/LCC claims.
The following components use the indicated worksheet instead of Worksheet E-1:
 Hospital-based
HHAs use Worksheet H-5.
Hospital-based
HHAs use Worksheet H-5.Hospital-based outpatient rehabilitation facilities use Worksheet J-4.
Hospital-based RHCs/FQHCs use Worksheet M-5.
Hospital-based FQHCs under FQHC PPS use Worksheet N-5.
The column headings designate two categories of payments:
Columns 1 and 2 - Inpatient Part A
Columns 3 and 4 - Part B
Complete lines 1 through 4. The remainder of the worksheet is completed by your contractor. All amounts reported on this worksheet must be for services, the costs of which are included in this cost report.
NOTE: When completing the heading, enter the provider number and the component number which corresponds to the provider, subprovider, SNF, or swing bed-SNF which you indicated.
DO NOT reduce any interim payments by recoveries as a result of medical review adjustments where the recoveries were based on a sample percentage applied to the universe of claims reviewed and the PS&R was not also adjusted. DO NOT include fee-schedule payments.
40-182 Rev.
09-14 FORM CMS-2552-10 4031.1 (Cont.)
Line Descriptions
Line 1--Enter the total Medicare interim payments paid to you (excluding payments made under the composite rate for ESRD services), including amounts paid under PPS, pass through payments, and payments from the supplemental PS&R associated with the Model 4 BPCI. The amount entered must reflect the sum of all interim payments paid on individual bills (net of adjustment bills) for services rendered in this cost reporting period. The amount entered must also include amounts withheld from your interim payments due to an offset against overpayments applicable to the prior cost reporting periods. Do not include (1) any retroactive lump sum adjustment amounts based on a subsequent revision of the interim rate, (2) tentative or net settlement amounts, or (3) interim payments payable. If you are reimbursed under the periodic interim payment method of reimbursement, enter the periodic interim payments received for this cost reporting period.
Line 2--Enter the total Medicare interim payments (excluding payments made under the ESRD composite rate) payable on individual bills.
Since the cost in the cost report is on an accrual basis, this line represents the amount of services rendered in the cost reporting period but not paid as of the end of the cost reporting period.
Also, include in column 4 the total Medicare payments payable for servicing home program renal dialysis equipment when the provider elected 100 percent cost reimbursement.
Line 3--Enter the amount of each retroactive lump sum adjustment and the applicable date.
Line 4--Enter the total amount of the interim payments (sum of lines 1, 2, and 3.99). Transfer as follows:
Reimbursement From Transfer
Method Column To
Part B Payments 4 Wkst. E, Part B, line 41
Part A Payments
IPPS 2 Wkst. E, Part A, line 72
TEFRA 2 Wkst. E-3, Part I, line 19
IPF PPS 2 Wkst. E-3, Part II, line 32
IRF PPS 2 Wkst. E-3, Part III, line 33
LTC PPS 2 Wkst. E-3, Part IV, line 23
Cost 2 Wkst. E-3, Part V, line 31
SNF PPS Title XVIII 2 Wkst. E-3, Part VI, line 16
NOTE: For a swing bed-SNF, transfer the column 2, line 4, and column 4, line 4, amounts to Worksheet E-2, columns 1 and 2, line 20, respectively.
DO NOT COMPLETE THE REMAINDER OF WORKSHEET E-1. LINES 5 THROUGH 8 ARE FOR CONTRACTOR USE ONLY. (EXCEPTION: IF WORKSHEET S, PART I, LINE 5 IS “5” (AMENDED COST REPORT), THE PROVIDER MAY COMPLETE THIS SECTION.)
Line 5--List separately each settlement payment after the cost report is received together with the date of payment. If the cost report is reopened after the NPR has been issued, continue to report all settlement payments after the cost report is received separately on this line.
Line 6--Enter the net settlement amount (balance due the provider or balance due the program). Obtain the amounts as follows:
Rev. 6 40-183
4031.1 (Cont.) FORM CMS-2552-10 09-14
Worksheet E-1, From
Column as Indicated Settlement Worksheet
2 Wkst. E, Part A, line 74
4 Wkst. E, Part B, line 43
2 Wkst. E-3, Part I, line 21
2 Wkst. E-3, Part II, line 34
2 Wkst. E-3, Part III, line 35
2 Wkst. E-3, Part IV, line 25
2 Wkst. E-3, Part V, line 33
2 Wkst. E-3, Part VI, line 18
For swing bed-SNF services, column 2 must equal Worksheet E-2, column 1, line 22. Column 4 must equal Worksheet E-2, column 2, line 22.
NOTE: On lines 3, 5, and 6, when a provider to program amount is due, show the amount and date on which the provider agrees to the amount of repayment even though total repayment is not accomplished until a later date.
Line 7--Enter in columns 2 and 4 the sum of lines 4 through 6. Enter amounts due the program as a negative number. These amounts must agree with amount due provider reported on Worksheet E, Part A, line 71 less the amount on line 71.01; Worksheet E, Part B, line 40 less the amount on line 40.01; Worksheet E-2, line 19 less the amount on line 19.01; Worksheet E-3, Part I, line 18 less the amount on line 18.01; Worksheet E-3, Part II, line 31 less the amount on line 31.01; Worksheet E-3, Part III, line 32 less the amount on line 32.01; Worksheet E-3, Part IV, line 22 less the amount on line 22.01; Worksheet E-3, Part V, line 30 less the amount on line 30.01; and Worksheet E-3, Part VI, line 15 less the amount on line 15.01.
Line 8--Enter the contractor name, the contractor number and NPR date in columns 0, 1 and 2, respectively.
4031.2 Part II - Calculation of Reimbursement Settlement for Health Information Technology-
THIS PART IS COMPLETED BY THE CONTRACTOR FOR STANDARD COST REPORTING PERIODS AND BY THE CONTRACTOR FOR NONSTANDARD COST REPORTING PERIODS.
In accordance with the American Recovery and Reinvestment Act (ARRA) of 2009, section 4102, inpatient acute care services under IPPS (providers subject to §1886(d) of the Act) and CAHs are eligible for health information technology (HIT) payments.
This part captures relevant data used to compute the HIT payment and records the single HIT initial payment paid by the contractor to the provider and any corresponding adjustments to this initial payment.
Data Collection Required for the Health Information Technology Calculation--
NOTE: Lines 1 through 7 must transfer data as indicated below for reporting periods which cover exactly 12 months (referred to as standard cost reporting periods and covers a range of 360 through 371 days). For cost reporting periods which cover other than exactly 12 months (less than or greater than 12 months (referred to as nonstandard cost reporting periods and covers a range of less than 360 days or greater than 371 days) lines 1 through 8 must be directly input by the contractor.
40-184 Rev. 6
09-14 FORM CMS-2552-10 4031.2 (Cont.)
NOTE: For standard cost reporting periods, the provider will complete lines 30 and 31 in the “as filed” cost report and the amount computed on line 32 will be transferred to Worksheet S, Part III, column 4. For non-standard cost reporting periods, the “as filed” cost report will display zeros on all lines and a zero will be transferred from line 32 to Worksheet S, Part III, column 4. The contractor must complete this worksheet for nonstandard cost reporting periods.
Line 1--As defined in ARRA, §4102, transfer the total hospital discharges from Worksheet S‑3, Part I, column 15, line 14.
Line 2--Transfer the Medicare days from Worksheet S-3, Part I, column 6, sum of line 1 and lines 8 through 12.
Line 3--Transfer the Medicare HMO days from Worksheet S-3, Part I, column 6, line 2.
Line 4--Transfer the total inpatient days from Worksheet S-3, Part I, column 8, sum of line 1 and lines 8 through 12.
Line 5--Transfer the hospital charges from Worksheet C, Part I, column 8, line 200.
Line 6--Transfer the hospital charity care charges from Worksheet S-10, column 3, line 20.
Line 7--CAHs only, transfer the reasonable costs to purchase certified HIT technology from Worksheet S-2, Part I, line 168.
Line 8--Calculate and enter the HIT payment in accordance with ARRA, §4102, as indicated below. This line can be overridden by the contractor in instances where the provider’s circumstances require a customized HIT calculation.
For CAHs, if Worksheet S-2, lines 105 and 167 are both “Y” for yes, enter the result of {(H1)/(line 4 x H2)} + .20 times the amount on Worksheet S-2, Part I, line 168. (Note: the result of {(H1)/(line 4 x H2)} + .20 cannot exceed 100 percent.) The resulting amount must be fully expensed in the current reporting period. H1 = Line 2 plus line 3. H2 = Total charges from Worksheet C, Part I, column 8, line 200 minus charity care charges from Worksheet S-10, column 3, line 20 divided by Worksheet C, Part I, column 8, line 200. Round the result of H2 to 4 decimal places.
OR
For acute care IPPS hospitals (§1886(d) of the Act), if Worksheet S-2, line 105 is “N” for no and line 167 is “Y” for yes, enter the result of {($2,000,000.00 + H1) x {(H2)/(line 4 x H3)} x H4}. If line 1 is less than 1,150 discharges then H1 equals 0 (zero). If line 1 equals 1,150 through 23,000 discharges, then H1 equals the result of line 1 minus 1,149 times $200. If line 1 is greater than or equal to 23,000 discharges then H1 = $4,370,200 [that is: 23,000 minus 1,149 times $200]. H2 = Line 2 plus line 3. H3 = Total charges from Worksheet C, Part I, column 8, line 200 minus charity care charges from Worksheet S-10, column 3, line 20 divided by Worksheet C, Part I, column 8, line 200. Round the result of H3 to 4 decimal places. H4 = The transition factor from Worksheet S-2, Part I, line 169.
Line 9--If the EHR reporting period ending date on Worksheet S-2, line 170, column 2 is on or after April 1, 2013, enter the sequestration adjustment amount as follows: [2 percent times line 8].
Rev. 6 40-185
4031.2 (Cont.) FORM CMS-2552-10 09-14
Line 10--Calculate and enter the HIT payment after application of the sequestration adjustment by entering the result of line 8 minus line 9.
Lines 11 through 29--Reserved for future use.
Inpatient Hospital Services Under IPPS & CAH--
Line 30--Enter the initial (first) payment received for HIT assets for this cost reporting period. This initial payment is a single payment for the cost reporting period rather than a series of periodic interim payments during the period. This line must be completed by the providers for standard cost reporting periods and by the contractors for nonstandard cost reporting periods.
Line 31--Enter the sum of all additional initial payment adjustments, as applicable for this cost reporting period. Enter a positive amount on this line if the sum of the initial payment adjustments represents an increase to the initial payment. Enter a negative amount on this line if the sum of the initial payment adjustments represents a decrease to the initial payment.
Line 32--Balance Due Provider/(Program)--Calculate and enter the result of line 8 minus the sum of lines 30 and 31. Effective for cost reporting periods that overlap or begin on or after April 1, 2013, calculate and enter the result of line 10 minus the sum of lines 30 and 31. Transfer this amount to Worksheet S, Part III, column 4, line 1.
4032. WORKSHEET E-2 - CALCULATION OF REIMBURSEMENT SETTLEMENT - SWING BEDS
This worksheet provides for the reimbursement calculation for swing bed services rendered to program patients under titles V, XVIII, and XIX. It provides for an accumulation of reimbursable costs determined on various worksheets within the cost report package. It also provides (under Part B) for the computation of the lesser of 80 percent of reasonable cost after deductibles or reasonable cost minus coinsurance and deductibles. These worksheets have been designed so that components must prepare a separate worksheet for swing bed-SNF title XVIII, Parts A and B, and separate worksheets for swing bed-NF for title V and title XIX. Use column 1 only on the worksheets for title V and title XIX. Indicate the use of each worksheet by checking the appropriate boxes.
Lines 1 through 9--Enter in the appropriate column on lines 1 through 7 the indicated costs for each component of the health care complex.
Line 1--Post-hospital swing beds in rural hospitals (other than CAHs) are paid in accordance with SNF PPS. Enter the total PPS payments in column 1 or 2, as applicable, from the provider’s books and records or the PS&R. (See 42 CFR 413.114(a)(2)) For CAHs, transfer 101 percent of the cost of swing-bed SNF inpatient routine services from Worksheet D-1, Part II, line 66.
Do not use lines 2 and 3, column 1 for swing bed SNF PPS providers.
Line 2--Enter the cost of swing bed-NF inpatient routine services from Worksheet D-1, Part II, line 69 (titles V and XIX only). Make no entry on line 2 when Worksheet E-2 is used for swing bed-SNF.
Line 3--Enter the amount of ancillary services provided by swing bed-SNFs for vaccines that are cost reimbursed in column 2. CAHs transfer for title XVIII services 101 percent of the amounts from the applicable worksheets and for swing bed-SNF services that are cost reimbursed transfer 100 percent of the amount from the applicable worksheet:
40-186 Rev. 6
09-14 FORM CMS-2552-10 4032 (Cont.)
Title V from Worksheet D-3, col. 3, line 200
Title XVIII, Part A from Worksheet D-3, col. 3, line 200
Title XVIII, Part B from The sum of Worksheet D, Part V, columns 6 and 7, line 202
Title XIX from Worksheet D-3, col. 3, line 200
Enter title XVIII, Part B amounts only in column 2. Enter all other amounts in column 1.
Line 4--Enter (in column 1 for titles V and XIX and in column 2 for title XVIII) the per diem cost for interns and residents not in an approved teaching program transferred from Worksheet D-2, Part I, column 4, line 2.
Line 5--For title XVIII, enter in column 1 the total number of days in which program swing-bed SNF patients were inpatients. Transfer these days from Worksheet D-1, Part I, sum of lines 10 and 11. For titles V or XIX, enter in column 1 the total number of days in which program swing bed-NF patients were inpatients. Transfer these days from Worksheet D-1, Part I, sum of lines 12 and 13. For title XVIII, enter in column 2 the total number of days in which Medicare swing bed beneficiaries were inpatients and had Medicare Part B coverage. Determine such days without regard to whether Part A benefits were available. Submit a reconciliation with the cost report demonstrating the computation of Medicare Part B inpatient days.
The following reconciliation format is recommended:
Part A Part B Part A Coverage Medicare
Inpatient Plus Only Minus But No Equals Part B
Days Days Part B Days
Days Coverage
NOTE: See §4026.1.
Line 6--Enter the amount on line 4 multiplied by the number of days recorded on line 5. Also, if the hospital qualifies for the exception for graduate medical education payments in 42 CFR 413.77 (d)(1), enter the amount transferred from Worksheet D-2, Part II, column 7, line 30.
Line 7--If Worksheet E-2 is completed for a certified SNF, enter the applicable program's share of the reasonable compensation paid to physicians for services on utilization review committees applicable to the SNF.
Line 8--Enter the sum of lines 1 through 3, plus lines 6 and 7 for each column.
Line 9--Enter any amounts paid and/or payable by workers’ compensation and other primary payers. (See instructions for Worksheet E, Part A, line 60, in §4030.1 for further clarification.)
Line 10--Line 8 minus line 9.
Line 11--Enter the deductible billed to program patients. DO NOT INCLUDE deductible applicable to physician professional services. Obtain this amount from your records.
Line 12--Enter line 10 minus line 11.
Line 13--Enter from your records the amounts billed to program patients for coinsurance. DO NOT INCLUDE coinsurance billed to program patients for physician professional services.
Rev. 6 40-187
4032 (Cont.) FORM CMS-2552-10 09-14
Line 14--In column 2, enter 80 percent of the amount on line 12.
Line 15--Enter the lesser of line 12 less line 13, or line 14.
Line 16--Enter any other adjustments.
Line 17--When Worksheet E-2 is completed for Medicare, enter the amount of bad debts (net of bad debt recoveries) for billed deductibles and coinsurance (excluding bad debts for physician professional services and bad debts arising from covered services paid under a reasonable charge-based methodology or a fee-schedule) for Part A services in column 1 and for Part B services in column 2. If recoveries exceed the current year’s bad debts, line 17 will be negative.
Line 17.01--For cost reporting periods that begin prior to October 1, 2012, enter the amount on line 17. For cost reporting periods that begin on or after October 1, 2012, calculate this line as follows: [((line 17 - line 18) * 65 percent) + (line 18 * 88 percent)]. For cost reporting periods that begin on or after October 1, 2013, calculate this line as follows: [((line 17 - line 18) * 65 percent) + (line 18 * 76 percent)]. For cost reporting periods that begin on or after October 1, 2014, multiply the amount on line 17 by 65 percent.
Line 18--Enter the gross allowable bad debts for dual eligible beneficiaries. For cost reporting periods that begin prior to October 1, 2012, this amount is reported for statistical purposes only. This amount must also be reported on line 17.
Line 19--For title XVIII, Part A, enter in column 1 the sum of lines 15 and 17.01 plus or minus line 16. For title XVIII, Part B, enter in column 2 the sum of lines 15 and 17.01 plus or minus line 16. For titles V and XIX, enter in column 1 the sum of line 15, plus or minus line 16.
Line 19.01--For cost reporting periods that overlap or begin on or after April 1, 2013, enter the sequestration adjustment amount as follows: [(2 percent times (total days in the cost reporting period that occur during the sequestration period beginning on or after April 1, 2013, divided by total days in the entire cost reporting period, rounded to four decimal places)) times line 19].
Line 20--For title XVIII, enter in column 1 the amount from the appropriate Worksheet E-1, column 2, line 4, and enter in column 2 the amount from the appropriate Worksheet E-1, column 4, line 4. For contractor final settlement, report on line 21 the amount from line 5.99 for columns 2 and 4. For titles V and XIX, enter interim payments from your records.
Line 22--Enter the amount recorded on line 19 minus the sum of the amounts on lines 19.01, 20, and 21. This amount shows the balance due provider or the program. Transfer this amount to Worksheet S, Part III, columns as appropriate, lines 5 or 6 for the swing bed-SNF or the swing bed-NF, respectively.
Line 23--Enter the Medicare reimbursement effect of protested items. Estimate the reimbursement effect of the non-allowable items by applying reasonable methodology which closely approximates the actual effect of the item as if it had been determined through the normal cost finding process. (See CMS Pub. 15-2, chapter 1, §115.2.) Attach a schedule showing the supporting details and computations for this line.
40-188 Rev. 6
09-14 FORM CMS-2552-10 4033.1
4033. WORKSHEET E-3 - CALCULATION OF REIMBURSEMENT SETTLEMENT
The five parts of Worksheet E-3 are used to calculate reimbursement settlement:
Part I - Calculation of Medicare Reimbursement Settlement Under TEFRA
Part II - Calculation of Medicare Reimbursement Settlement Under IPF PPS
Part III - Calculation of Medicare Reimbursement Settlement Under IRF PPS
Part IV - Calculation of Medicare Reimbursement Settlement Under LTCH PPS
Part V - Calculation of Reimbursement Settlement for Medicare Part A Services - Cost Reimbursement (CAHs)
Part VI - Calculation of Reimbursement Settlement - All Other Health Services for Part A Services for Title XVIII PPS SNFs
Part VII - Calculation of Reimbursement Settlement - All Other Health Services for Titles V or XIX Services
4033.1 Part I - Calculation of Medicare Reimbursement Settlement Under TEFRA--Use Worksheet E-3, Part I to calculate Medicare reimbursement settlement under TEFRA for cancer and children’s hospitals.
Line Descriptions
Line 1--Enter the amount from Worksheet D-1, Part II, line 63.
Line 2--If you are an approved CTC, enter the cost of organ acquisition from Worksheet(s) D-4, Part III, column 1, line 69. If you are not an approved CTC do not complete line 2.
Line 3--Teaching hospitals participating in an approved GME program, electing to be reimbursed for services of physicians on the basis of reasonable cost (see 42 CFR 415.160 and CMS Pub. 15-1, chapter 21, §2148), enter the cost of physicians. For cost reporting periods ending before June 30, 2014, transfer the amount from Worksheet D-5, Part II, column 3, line 20. For cost reporting periods ending on or after June 30, 2014, transfer the amount from Worksheet D-5, Part IV, line 20.
Line 4--Enter the sum of lines 1, 2 and 3.
Line 5--Enter the amounts paid or payable by workers' compensation and other primary payers when program liability is secondary to that of the primary payer. There are six situations under which Medicare payment is secondary to a primary payer:
Workers' compensation,
No fault coverage,
General liability coverage,
Working aged provisions,
Disability provisions, and
Working ESRD provisions.
Generally, when payment by the primary payer satisfies the total liability of the program beneficiary, for cost reporting purposes only, the services are treated as if they were non-program services. (The primary payment satisfies the beneficiary's liability when you accept that payment as payment in full.
Rev. 6 40-189
4033.1 (Cont.) FORM CMS-2552-10 09-14
This is noted on no-pay bills submitted in these situations.) Include the patient days and charges in total patient days and charges but do not include them in program patient days and charges. In this situation, enter no primary payer payment on line 5. In addition, exclude amounts paid by other primary payers for outpatient dialysis services reimbursed under the composite rate system.
However, when the payment by the primary payer does not satisfy the beneficiary's obligation, the program pays the lesser of (a) the amount it otherwise pays (without regard to the primary payer payment or deductible and coinsurance) less the primary payer payment, or (b) the amount it otherwise pays (without regard to primary payer payment or deductibles and coinsurance) less applicable deductible and coinsurance. Primary payer payment is credited toward the beneficiary's deductible and coinsurance obligation.
When the primary payment does not satisfy the beneficiary's liability, include the covered days and charges in program days and charges, and include the total days and charges in total days and charges for cost apportionment purposes. Enter the primary payer payment on line 5 to the extent that primary payer payment is not credited toward the beneficiary's deductible and coinsurance.
Do not enter on line 5 primary payer payments credited toward the beneficiary's deductible and coinsurance.
Line 6--Enter line 4 minus line 5.
Line 7--Enter the Part A deductibles.
Line 8--Enter line 6 less line 7.
Line 9--Enter the Part A coinsurance.
Line 10--Enter the result of subtracting line 9 from line 8.
Line 11--Enter program allowable bad debts reduced by recoveries. If recoveries exceed the current year’s bad debts, lines 11 and 12 will be negative.
Line 12--Multiply the amount (including negative amounts) from line 11 by 70 percent for cost reporting periods beginning prior to October 1, 2012, and 65 percent for cost reporting periods that begin on or after October 1, 2012.
Line 13--Enter the gross allowable bad debts for dual eligible beneficiaries. This amount is reported for statistical purposes only. This amount must also be reported on line 11.
Line 14--Enter the sum of lines 10 and 12.
Line 15--Enter the amount from Worksheet E-4, line 49 for the hospital component only.
Line 16--DO NOT USE THIS LINE.
40-190 Rev. 6
DRAFT FORM CMS-2552-10 4033.1 (Cont.)
Line 17--Enter any other adjustments. For example, if you change the recording of vacation pay from the cash basis to accrual basis, etc, enter the adjustment. (See CMS Pub. 15-1, chapter 21, §2146.4.) Specify the adjustment in the space provided.
Enter on line 17.99 the program share of any recovery of accelerated depreciation applicable to prior periods resulting from your termination or a decrease in Medicare utilization. (See CMS Pub. 15-1, chapter 1, §§136-136.16, and 42 CFR 413.134(d)(3)(i).) Identify this line as “Recovery of Accelerated Depreciation.”
Line 18--Enter the sum of lines 14, 15, and 16 plus or minus line 17.
Line 18.01--For cost reporting periods that overlap or begin on or after April 1, 2013, enter the sequestration adjustment amount as follows: [(2 percent times (total days in the cost reporting period that occur during the sequestration period beginning on or after April 1, 2013, divided by total days in the entire cost reporting period, rounded to four decimal places)) times line 18].
Line 19--Enter the amount of interim payments from Worksheet E-1, column 2, line 4. For contractor final settlements, report on line 20 the amount on line 5.99.
Line 20--Contractor use only: Report the amount from Worksheet E-1, column 2, line 5.99.
Line 21--Enter line 18 minus the sum of lines 18.01, 19, and 20. Transfer this amount to Worksheet S, Part III, line as appropriate.
Line 22--Enter the program reimbursement effect of protested items. Estimate the reimbursement effect of the nonallowable items by applying a reasonable methodology which closely approximates the actual effect of the item as if it had been determined through the normal cost finding process. (See CMS Pub. 15-2, chapter 1, §115.2.) Attach a schedule showing the details and computations.
Rev. 40-191
4033.2 FORM CMS-2552-10 DRAFT
4033.2 Part II - Calculation of Medicare Reimbursement Settlement Under IPF PPS--Use Worksheet E-3, Part II to calculate Medicare reimbursement settlement under IPF PPS for hospitals and subproviders. (See 42 CFR 412, subpart N.)
Use a separate copy of Worksheet E-3, Part II for each of these reporting situations. Enter check marks in the appropriate spaces at the top of each page of Worksheet E-3, Part II to indicate the component for which it is used. When the worksheet is completed for a component, show both the hospital and component numbers.
Line Descriptions
Line 1--Enter the net Federal IPF PPS payment. This amount excludes payments for outliers, electroconvulsive therapy (ECT), and the teaching adjustment. Obtain this information from the PS&R and/or your records.
Line 2--Enter the net IPF outlier payment. Obtain this from the PS&R and/or your accounting books records.
Line 3--Enter the net IPF payments for ECT. Obtain this from the PS&R and/or your accounting books and records.
NOTE: Complete only line 4 or line 5, but not both.
Line 4--For providers that trained residents in the most recent cost reporting period filed on or before November 15, 2004 (response on Worksheet S-2, Part I, line 71, column 1 is “Y” for yes), enter the unweighted FTE resident count for the most recent cost reporting period filed on or before November 15, 2004. See 69 FR 66922 (November 4, 2004) for a detailed explanation.
Line 4.01--For IPFs that qualify to receive a temporary adjustment to the FTE cap, enter the additional unweighted FTE count for residents that were displaced by program or hospital closure, which you would not be able to count without a temporary cap adjustment under 42 CFR 412.424(d)(1)(iii)(F)(1) or (2).
Line 5--If the response to Worksheet S-2, Part I, line 71, column 2 is “Y” and your facility did not train residents in the most recent cost report filed before November 15, 2004, but qualifies to receive a cap adjustment under 42 CFR 412.424(d)(1)(iii)(D) enter the new program cap adjustment on this line. Do not complete this line until the new program growth period has ended using the method described in 42 CFR 413.79(e)(1)(i) and (ii). If your fiscal year end does not correspond to the program year end, and this cost reporting period includes the beginning of the program year following the new program growth period of the first new program, then prorate the cap adjustment accordingly.
Line 6--Enter the current year unweighted FTE resident count excluding FTEs in the new program growth period. FTEs in the new program growth period are reported on line 7. If your fiscal year end does not correspond to the program year end, and this cost reporting period includes the beginning of the program year following the new program growth period of the first new program, then prorate the FTE count accordingly.
40-192 Rev. 4
09-14 FORM CMS-2552-10 4033.2 (Cont.)
Line 7--Enter the current year unweighted FTE count for residents in the new program growth period. Complete this line only during the new program growth period of the first new program’s existence. If your fiscal year end does not correspond to the program year end, and this cost reporting period includes the beginning of the program year following the new program growth period of the first new program, then prorate the FTE count accordingly.
Line 8--For providers that completed line 4, enter the lower of the FTE count on line 6 or the sum of the cap amounts on lines 4 and 4.01.
For providers that qualify to receive a cap adjustment under 42 CFR 412.424(d)(1)(iii)(D) during the new program growth period of the first new program’s existence, enter the FTE count from line 7.
Beginning with the program year following the new program growth period of the first new program’s existence, enter the lower of the FTE count on line 6 or the FTE count on line 5. Add to this count the FTEs on line 7 if your fiscal year end does not correspond with the program year end, and this cost reporting period includes the beginning of the program year following the new program growth period of the first new program.
Line 9--Enter the total IPF patient days divided by the number of days in the cost reporting period (Worksheet S-3, Part I, column 8, line 1 (independent/freestanding) or 16 and applicable subscripts (subprovider/provider based) divided by the total number of days in cost reporting period). This is the average daily census.
Line 10--Enter the teaching adjustment factor by adding 1 to the ratio of line 8 to line 9. Raise that result to the power of .5150. Subtract 1 from this amount to calculate the teaching adjustment factor. This is expressed mathematically as {(1 + (line 8 / line 9)) to the .5150 power - 1}.
Line 11--Enter the teaching adjustment by multiplying line 1 by line 10.
Line 12--Enter the adjusted net IPF PPS payments by entering the sum of lines 1, 2, 3, and 11.
Line 13--Enter the amount of Nursing and Allied Health Managed Care payments, if applicable. Only complete this line if your facility is a freestanding/independent non-IPPS hospital that does not complete Worksheet E, Part A.
Line 14--DO NOT USE THIS LINE.
Line 15--Teaching IPFs or IPF subproviders participating in an approved GME program, electing to be reimbursed for services of physicians on the basis of reasonable cost (see 42 CFR 415.160 and CMS Pub. 15-1, chapter 21, §2148), enter the cost of physicians. For cost reporting periods ending before June 30, 2014, transfer the amount from Worksheet D-5, Part II, column 3, line 20. For cost reporting periods ending on or after June 30, 2014, transfer the amount from Worksheet D-5, Part IV, line 20.
Line 16--Enter the sum of lines 12, 13, 14 and 15.
Line 17--Enter the amounts paid or payable by workers' compensation and other primary payers when program liability is secondary to that of the primary payer. There are six situations under which Medicare payment is secondary to a primary payer:
Workers' compensation,
No fault coverage,
General liability coverage,
Working aged provisions,
Disability provisions, and
Working ESRD provisions.
Rev. 6 40-193
4033.2 (Cont.) FORM CMS-2552-10 09-14
Generally, when payment by the primary payer satisfies the total liability of the program beneficiary, for cost reporting purposes only, the services are treated as if they were non-program services. (The primary payment satisfies the beneficiary's liability when you accept that payment as payment in full. This is noted on no-pay bills submitted in these situations.) Include the patient days and charges in total patient days and charges but do not include them in program patient days and charges. In this situation, enter no primary payer payment on line 17. In addition, exclude amounts paid by other primary payers for outpatient dialysis services reimbursed under the composite rate system.
However, when the payment by the primary payer does not satisfy the beneficiary's obligation, the program pays the lesser of (a) the amount it otherwise pays (without regard to the primary payer payment or deductible and coinsurance) less the primary payer payment, or (b) the amount it otherwise pays (without regard to primary payer payment or deductibles and coinsurance) less applicable deductible and coinsurance. Primary payer payment is credited toward the beneficiary's deductible and coinsurance obligation.
When the primary payment does not satisfy the beneficiary's liability, include the covered days and charges in program days and charges, and include the total days and charges in total days and charges for cost apportionment purposes. Enter the primary payer payment on line 17 to the extent that primary payer payment is not credited toward the beneficiary's deductible and coinsurance.
Do not enter on line 17 primary payer payments credited toward the beneficiary's deductible and coinsurance.
Line 18--Enter line 16 minus line 17.
Line 19--Enter the Part A deductibles.
Line 20--Enter line 18 minus line 19.
Line 21--Enter the Part A coinsurance.
Line 22--Enter the result of subtracting line 21 from line 20.
Line 23--Enter program allowable bad debts reduced by recoveries. If recoveries exceed the current year’s bad debts, lines 23 and 24 will be negative.
Line 24--Multiply the amount (including negative amounts) from line 23 by 70 percent for cost reporting periods beginning prior to October 1, 2012, and 65 percent for cost reporting periods that begin on or after October 1, 2012.
Line 25--Enter the gross allowable bad debts for dual eligible beneficiaries. This amount is reported for statistical purposes only. This amount must also be reported on line 23.
Line 26--Enter the sum of lines 22 and 24.
Line 27--Enter the amount from Worksheet E-4, line 49 for the hospital component (freestanding IPF) only. Do not complete this line for an IPF unit.
Line 28--Enter the routine service other pass through costs from Worksheet D, Part III, column 9, line 30 for a freestanding facility or line 40 for the IPF subprovider. Add to this amount the ancillary service other pass through costs from Worksheet D, Part IV, column 11, line 200.
40-194 Rev. 6
DRAFT FORM CMS-2552-10 4033.2 (Cont.)
Line 29--Enter the outlier reconciliation amount by entering the sum of lines 51 and 53.
Line 30--Enter any other adjustments. For example, if you change the recording of vacation pay from the cash basis to accrual basis, etcetera, enter the adjustment. (See CMS Pub. 15-1, chapter 21, §2146.4.) Specify the adjustment in the space provided.
Enter on line 30.99 the program share of any recovery of accelerated depreciation applicable to prior periods resulting from your termination or a decrease in Medicare utilization. (See CMS Pub. 15-1, chapter 1, §§136-136.16, and 42 CFR 413.134(d)(3)(i).) Identify this line as “Recovery of Accelerated Depreciation.”
Line 31--Enter the sum of lines 26 through 28, plus or minus lines 29 and 30.
Line 31.01--For cost reporting periods that overlap or begin on or after April 1, 2013, enter the sequestration adjustment amount as follows: [(2 percent times (total days in the cost reporting period that occur during the sequestration period beginning on or after April 1, 2013, divided by total days in the entire cost reporting period, rounded to four decimal places)) times line 31].
Line 32--Enter the amount of interim payments from Worksheet E-1, column 2, line 4. For contractor final settlements, report on line 33 the amount on line 5.99.
Line 34--Enter line 31 minus the sum of lines 31.01, 32, and 33. Transfer this amount to Worksheet S, Part III, line as appropriate.
Line 35--Enter the program reimbursement effect of protested items. Estimate the reimbursement effect of the nonallowable items by applying a reasonable methodology which closely approximates the actual effect of the item as if it had been determined through the normal cost finding process. (See CMS Pub. 15-1, chapter 1, §115.2.) Attach a schedule showing the details and computations.
DO NOT COMPLETE THE REMAINDER OF WORKSHEET E-3, PART II. LINES 50 THROUGH 53 ARE FOR CONTRACTOR USE ONLY.
Line 50--Enter the original outlier amount from Worksheet E-3, Part II, line 2.
Line 51--Enter the outlier reconciliation adjustment amount in accordance with CMS Pub. 100‑04, chapter 3, §§190.7.2.3-190.7.2.5.
Line 52--Enter the interest rate used to calculate the time value of money. (See CMS Pub. 100‑04, chapter 3, §§190.7.2.3-190.7.2.5.)
Line 53--Enter the time value of money.
NOTE: If a cost report is reopened more than one time, subscript lines 50 through 53, respectively, one time for each time the cost report is reopened.
Rev. 40-195
4033.3 FORM CMS-2552-10 DRAFT
4033.3 Part III - Calculation of Medicare Reimbursement Settlement Under IRF PPS--Use Worksheet E-3, Part III, to calculate Medicare reimbursement settlement under IRF PPS for hospitals and subproviders. (See 42 CFR 412, subpart P.)
Use a separate copy of Worksheet E-3, Part III, for each of these reporting situations. Enter check marks in the appropriate spaces at the top of each page of Worksheet E-3, Part III, to indicate the component for which it is used. When the worksheet is completed for a component, show both the hospital and component numbers.
Line Descriptions
Line 1--Enter the net federal IRF PPS payment. The federal payment includes short stay outlier amounts. Exclude low income patient (LIP) and outlier payments. Obtain this information from the PS&R and/or your records.
In accordance with the 78 FR 47869 (August 6, 2013), effective for IRF discharges rendered on or after October 1, 2013, the IRF LIP adjustment factor is updated. Subscript column 1 for lines 1 and 3 for cost reporting periods that overlap October 1, 2013. Enter the net federal IRF PPS payments associated with IRF PPS discharges prior to October 1, 2013 in column 1, and the net federal IRF PPS payments associated with IRF PPS discharges on or after October 1, 2013 in column 1.01, to facilitate the calculation of the LIP adjustment on line 3, columns 1 and 1.01, respectively. Do not subscript column 1 for cost reporting periods beginning on or after October 1, 2013.
Line 2--Enter the Medicare SSI ratio from your contractor as applicable for a freestanding IRF (IRF hospital or facility) or a hospital based IRF (subprovider or subunit).
Line 3--Effective for cost reporting periods ending prior to October 1, 2013, enter the IRF LIP payment as the result of {(1 + (line 2) + (L1/L2)) to the .4613 power - 1} times (line 1). L1 = IRF Medicaid Days from Worksheet S-2, Part I, columns 1 through 6, line 25. L2 = IRF total days from Worksheet S-3, Part I, column 8, lines 1 or 17, as applicable, plus employee discount days (Worksheet S-3, Part I, column 8, line 30 (line 31 for IRF subproviders)).
For cost reporting periods that overlap October 1, 2013, subscript column 1. To calculate the IRF LIP payment for discharges prior to October 1, 2013, enter in column 1 the result of {(1 + (line 2) + (L1/L2)) to the .4613 power - 1} times (line 1, column 1). To calculate the IRF LIP payment for discharges on or after October 1, 2013, enter in column 1.01 the result of {(1 + (line 2) + (L1/L2)) to the .3177 power - 1} times (line 1, column 1.01). Do not subscript column 1 for cost reporting periods beginning on or after October 1, 2013. To calculate the IRF LIP payment for cost reporting periods beginning on or after October 1, 2013, enter in column 1 the result of {(1 + (line 2) +(L1/L2)) to the .3177 power - 1} times line 1.
Line 4--Enter the IRF outlier payment. Obtain this from the PS&R and/or your records.
NOTE: Complete only line 5 or line 6, but not both.
Line 5--For providers that trained residents in the most recent cost reporting period ending on or before November 15, 2004 (response to Worksheet S-2, Part I, line 76, column 1, is “Y” for yes), enter the unweighted FTE resident count for the most recent cost reporting period ending on or before November 15, 2004.
Line 5.01--For IRFs that qualify to receive a temporary adjustment to the FTE cap, enter the additional unweighted FTE count for residents that were displaced by program or hospital closure, which you would not be able to count without a temporary cap adjustment in accordance with 76 FR 47846 (August 5, 2011).
40-196 Rev.
DRAFT FORM CMS-2552-10 4033.3 (Cont.)
Line 6--If the response to Worksheet S-2, Part I, line 76, column 2, is “Y” and your facility did not train residents in the most recent cost reporting period ending on or before November 15, 2004, and qualifies to receive a cap adjustment (see 70 FR 47929 (August 15, 2005)) enter the new cap adjustment on this line. Do not complete this line until the new program growth period has ended using the method described in 42 CFR 413.79(e)(1)(i) and (ii). If your fiscal year end does not correspond to the program year end, and this cost reporting period includes the beginning of the program year following the new program growth period of the first new program, then prorate the cap adjustment accordingly.
Line 7--Enter the current year unweighted FTE resident count excluding FTEs in the new program growth period. FTEs in the new program growth period are reported on line 8. If your fiscal year end does not correspond to the program year end and this cost reporting period includes the beginning of the program year following the new program growth period of the first new program, then prorate the FTE count accordingly.
Line 8--Enter the current year unweighted FTE count for residents in the new program growth period. Complete this line only during the new program growth period of the first new program’s existence. If your fiscal year end does not correspond with the program year end, and this cost reporting period includes the beginning of the program year following the new program growth period of the first new program, then prorate the FTE count accordingly.
Line 9--For providers that completed line 5, enter the lower of the FTE count on line 7, or the sum of the cap amounts on lines 5 and 5.01.
For providers that qualify to receive a cap adjustment (see 70 FR 47929 (August 15, 2005)), during the new program growth period of the first new program’s existence enter the FTE count from line 8.
Beginning with the program year following the new program growth period of the first new program’s existence, enter the lower of the FTE count on line 7, or the FTE count on line 6. Add to this count the FTEs on line 8 if your fiscal year end does not correspond with the program year end, and this cost reporting period includes the beginning of the program year following the new program growth period of the first new program.
Line 10--Enter the total IRF patient days divided by the number of days in the cost reporting period (Worksheet S-3, column 8, line 1 (independent/freestanding), or 17 and applicable subscripts (subprovider/provider based), divided by the total number of days in cost reporting period). This is the average daily census.
NOTE: For cost reporting periods overlapping October 1, 2013, subscript column 1 (add column 1.01) for lines 11 and 12. For cost reporting periods beginning on or after October 1, 2013, do not script column 1.
Line 11--For cost reporting periods ending prior to October 1, 2013, calculate in column 1 the teaching adjustment factor by adding 1 to the ratio of line 9 divided by line 10. Raise that result to the power of .6876. Subtract 1 from this amount to calculate the teaching adjustment factor. This is expressed mathematically as {(1 + (line 9 / line 10)) to the .6876 power - 1}.
In accordance with the 78 FR 47869 (August 6, 2013), effective for IRF discharges rendered on or after October 1, 2013, the teaching adjustment factor is updated. For cost reporting periods that overlap October 1, 2013, subscript column 1.
To calculate the teaching adjustment factor for discharges prior to October 1, 2013, enter in column 1 the result of adding 1 to the ratio of line 9 divided by line 10. Raise that result to the power of .6876 and then subtract 1 from this amount. This is expressed mathematically as {(1 + (line 9 / line 10)) to the .6876 power - 1}. To calculate the teaching adjustment factor for discharges on or after October 1, 2013, enter in column 1.01 the result of adding 1 to the ratio of
Rev. 40-197
4033.3 (Cont.) FORM CMS-2552-10 DRAFT
line 9 divided by line 10. Raise that result to the power of 1.0163 and then subtract 1 from this amount. This is expressed mathematically as {(1 + (line 9 / line 10)) to the 1.0163 power - 1}. Do not subscript column 1 for cost reporting periods beginning on or after October 1, 2013.
To calculate the teaching adjustment factor for cost reporting periods beginning on or after October 1, 2013, enter in column 1 the result of adding 1 to the ratio of line 9 divided by line 10. Raise that result to the power of 1.0163 and then subtract 1 from this amount. This is expressed mathematically as {(1 + (line 9 / line 10)) to the 1.0163 power - 1}.
Line 12--For cost reporting periods ending prior to October 1, 2013, calculate the teaching adjustment by multiplying line 1, by line 11. For cost reporting periods that overlap October 1, 2013, subscript column 1. Calculate the teaching adjustment for discharges prior to October 1, 2013 in column 1 by multiplying line 1, column 1 by line 11, column 1. Calculate the teaching adjustment for discharges on or after October 1, 2013, in column 1.01 by multiplying line 1, column 1.01 by line 11, column 1.01. Do not subscript column 1 for cost reporting periods beginning on or after October 1, 2013. For cost reporting periods beginning on or after October 1, 2013, calculate the teaching adjustment by multiplying line 1, by line 11.
Line 13--Enter the sum of line 1, columns 1 and 1.01; line 3, columns 1 and 1.01; line 4 and line 12, columns 1 and 1.01.
Line 14--Enter the amount of Nursing and Allied Health Managed Care payments, if applicable. Only complete this line if your facility is a freestanding/independent non-IPPS hospital that does not complete Worksheet E, Part A.
Line 15--DO NOT USE THIS LINE.
Line 16--Teaching IRFs or IRF subproviders participating in an approved GME program, electing to be reimbursed for services of physicians on the basis of reasonable cost (see 42 CFR 415.160 and CMS Pub. 15-1, chapter 21, §2148), enter the cost of physicians. For cost reporting periods ending before June 30, 2014, transfer the amount from Worksheet D-5, Part II, column 3, line 20. For cost reporting periods ending on or after June 30, 2014, transfer the amount from Worksheet D-5, Part IV, line 20.
Line 17--Enter the sum of lines 13, 14, 15 and 16.
Line 18--Enter the amounts paid or payable by workers' compensation and other primary payers when program liability is secondary to that of the primary payer. There are six situations under which Medicare payment is secondary to a primary payer:
Workers' compensation,
No fault coverage,
General liability coverage,
Working aged provisions,
Disability provisions, and
Working ESRD provisions.
Generally, when payment by the primary payer satisfies the total liability of the program beneficiary, for cost reporting purposes only, the services are treated as if they were non-program services. (The primary payment satisfies the beneficiary's liability when you accept that payment as payment in full. This is noted on no-pay bills submitted in these situations.) Include the patient days and charges in total patient days and charges but do not include them in program patient days and charges. In this situation, enter no primary payer payment on line 18. In addition, exclude amounts paid by other primary payers for outpatient dialysis services reimbursed under the composite rate system.
40-198 Rev.
DRAFT FORM CMS-2552-10 4033.3 (Cont.)
However, when the payment by the primary payer does not satisfy the beneficiary's obligation, the program pays the lesser of (a) the amount it otherwise pays (without regard to the primary payer payment or deductible and coinsurance) less the primary payer payment, or (b) the amount it otherwise pays (without regard to primary payer payment or deductibles and coinsurance) less applicable deductible and coinsurance. Primary payer payment is credited toward the beneficiary's deductible and coinsurance obligation.
When the primary payment does not satisfy the beneficiary's liability, include the covered days and charges in program days and charges, and include the total days and charges in total days and charges for cost apportionment purposes. Enter the primary payer payment on line 18 to the extent that primary payer payment is not credited toward the beneficiary's deductible and coinsurance.
Do not enter on line 18 primary payer payments credited toward the beneficiary's deductible and coinsurance.
Line 19--Enter line 17 minus line 18.
Line 20--Enter the Part A deductibles.
Line 21--Enter line 19 less line 20.
Line 22--Enter the Part A coinsurance.
Line 23--Enter the result of subtracting line 22 from line 21.
Line 24--Enter program allowable bad debts reduced by recoveries. If recoveries exceed the current year’s bad debts, lines 24 and 25 will be negative.
Line 25--Multiply the amount (including negative amounts) from line 24 by 70 percent for cost reporting periods beginning prior to October 1, 2012, and 65 percent for cost reporting periods that begin on or after October 1, 2012.
Line 26--Enter the gross allowable bad debts for dual eligible beneficiaries. This amount is reported for statistical purposes only. This amount must also be reported on line 24.
Line 27--Enter the sum of lines 23 and 25.
Line 28--Enter the amount from Worksheet E-4, line 49 for the hospital component (freestanding IRF) only. Do not complete this line for an IRF unit.
Line 29--Enter the routine service other pass through costs from Worksheet D, Part III, column 9, line 30 for a freestanding facility or line 41 for IRF the subproviders. Add to this amount the ancillary service other pass through costs from Worksheet D, Part IV, column 11, line 200.
Line 30--Enter the outlier reconciliation amount by entering the sum of lines 51 and 53.
Line 31--Enter any other adjustments. For example, if you change the recording of vacation pay from the cash basis to accrual basis, etc, enter the adjustment. (See CMS Pub. 15-1, chapter 21, §2146.4.) Specify the adjustment in the space provided.
Enter on line 31.99 the program share of any recovery of accelerated depreciation applicable to prior periods resulting from your termination or a decrease in Medicare utilization. (See CMS Pub. 15-1, chapter 1, §§136-136.16, and 42 CFR 413.134(d)(3)(i).) Identify this line as “Recovery of Accelerated Depreciation.”
Line 32--Enter the sum of lines 27, 28, and 29 plus or minus lines 30 and 31.
Rev. 40-199
4033.3 (Cont.) FORM CMS-2552-10 DRAFT
Line 32.01--For cost reporting periods that overlap or begin on or after April 1, 2013, enter the sequestration adjustment amount as follows: [(2 percent times (total days in the cost reporting period that occur during the sequestration period beginning on or after April 1, 2013, divided by total days in the entire cost reporting period, rounded to four decimal places)) times line 32].
Line 33--Enter the amount of interim payments from Worksheet E-1, column 2, line 4. For contractor final settlements, report on line 34 the amount on line 5.99.
Line 35--Enter line 32 minus the sum of lines 32.01, 33, and 34. Transfer this amount to Worksheet S, Part III, line as appropriate.
Line 36--Enter the program reimbursement effect of protested items. Estimate the reimbursement effect of the nonallowable items by applying a reasonable methodology which closely approximates the actual effect of the item as if it had been determined through the normal cost finding process. (See CMS Pub. 15-2, chapter 1, §115.2.) Attach a schedule showing the details and computations.
DO NOT COMPLETE THE REMAINDER OF WORKSHEET E-3, PART III. LINES 50 THROUGH 53 ARE FOR CONTRACTOR USE ONLY.
Line 50--Enter the original outlier amount from Worksheet E-3, Part III, line 4.
Line 51--Enter the outlier reconciliation adjustment amount in accordance with CMS Pub. 100‑04, chapter 3, §§140.2.8-140.2.10.
Line 52--Enter the interest rate used to calculate the time value of money. (See CMS Pub. 100‑04, chapter 3, §§140.2.8-140.2.10)
Line 53--Enter the time value of money.
NOTE: If a cost report is reopened more than one time, subscript lines 50 through 53, respectively, one time for each time the cost report is reopened.
40-199.1 Rev.
09-14 FORM CMS-2552-10 4033.3 (Cont.)
This page is reserved for future use.
Rev. 6 40-199.2
4033.4 FORM CMS-2552-10 09-14
4033.4 Part IV - Calculation of Medicare Reimbursement Settlement Under LTCH PPS--Use Worksheet E-3, Part IV to calculate Medicare reimbursement settlement under LTCH PPS for hospitals. (See 42 CFR 412, subpart O.)
Line Descriptions
Line 1--Enter the net federal LTCH PPS payment including short stay outlier payments. Obtain this information from the PS&R and/or your records.
Line 2--Enter the high cost outlier payments. Obtain this from the PS&R and/or your records.
Line 3--Enter the sum of lines 1 and 2.
Line 4--Enter the amount of Nursing and Allied Health Managed Care payments, if applicable.
Line 5--DO NOT USE THIS LINE.
Line 6--Teaching hospitals participating in an approved GME program, electing to be reimbursed for services of physicians on the basis of reasonable cost (see 42 CFR 415.160 and CMS Pub. 15-1, chapter 21, §2148), enter the cost of physicians. For cost reporting periods ending before June 30, 2014, transfer the amount from Worksheet D-5, Part II, column 3, line 20. For cost reporting periods ending on or after June 30, 2014, transfer the amount from Worksheet D-5, Part IV, line 20.
Line 7--Enter the sum of lines 3, 4, 5 and 6.
Line 8--Enter the amounts paid or payable by workers' compensation and other primary payers when program liability is secondary to that of the primary payer. There are six situations under which Medicare payment is secondary to a primary payer:
Workers' compensation,
No fault coverage,
General liability coverage,
Working aged provisions,
Disability provisions, and
Working ESRD provisions.
Generally, when payment by the primary payer satisfies the total liability of the program beneficiary, for cost reporting purposes only, the services are treated as if they were non-program services. (The primary payment satisfies the beneficiary's liability when you accept that payment as payment in full. This is noted on no-pay bills submitted in these situations.) Include the patient days and charges in total patient days and charges but do not include them in program patient days and charges. In this situation, enter no primary payer payment on line 8. In addition, exclude amounts paid by other primary payers for outpatient dialysis services reimbursed under the composite rate system.
40-200 Rev. 6
DRAFT FORM CMS-2552-10 4033.4 (Cont.)
However, when the payment by the primary payer does not satisfy the beneficiary's obligation, the program pays the lesser of (a) the amount it otherwise pays (without regard to the primary payer payment or deductible and coinsurance) less the primary payer payment, or (b) the amount it otherwise pays (without regard to primary payer payment or deductibles and coinsurance) less applicable deductible and coinsurance. Primary payer payment is credited toward the beneficiary's deductible and coinsurance obligation.
When the primary payment does not satisfy the beneficiary's liability, include the covered days and charges in program days and charges, and include the total days and charges in total days and charges for cost apportionment purposes. Enter the primary payer payment on line 8 to the extent that primary payer payment is not credited toward the beneficiary's deductible and coinsurance.
Do not enter on line 8 primary payer payments credited toward the beneficiary's deductible and coinsurance.
Line 9--Enter line 7 minus line 8.
Line 10--Enter the Part A deductibles.
Line 11--Enter line 9 less line 10.
Line 12--Enter the Part A coinsurance.
Line 13--Enter the result of subtracting line 12 from line 11.
Line 14--Enter program allowable bad debts reduced by recoveries. If recoveries exceed the current year’s bad debts, lines 14 and 15 will be negative.
Line 15--Multiply the amount (including negative amounts) from line 14 by 70 percent for cost reporting periods beginning prior to October 1, 2012, and 65 percent for cost reporting periods that begin on or after October 1, 2012.
Line 16--Enter the gross allowable bad debts for dual eligible beneficiaries. This amount is reported for statistical purposes only. This amount must also be reported on line 14.
Line 17--Enter the sum of lines 13 and 15.
Line 18--Enter the amount from Worksheet E-4, line 49 for the hospital.
Line 19--Enter the routine service other pass through costs from Worksheet D, Part III, column 9, line 30 for a freestanding facility. Add to this amount the ancillary service other pass through costs from Worksheet D, Part IV, column 11, line 200.
Line 20--Enter the outlier reconciliation amount by entering the sum of lines 51 and 53.
Line 21--Enter any other adjustments. For example, if you change the recording of vacation pay from the cash basis to accrual basis, etcetera, enter the adjustment. (See CMS Pub. 15-1, chapter 21, §2146.4.) Specify the adjustment in the space provided.
Rev. 40-201
4033.4 (Cont.) FORM CMS-2552-10 DRAFT
Enter on line 21.99 the program share of any recovery of accelerated depreciation applicable to prior periods resulting from your termination or a decrease in Medicare utilization. (See CMS Pub. 15-1, chapter 1, §§136-136.16, and 42 CFR 413.134(d)(3)(i).) Identify this line as “Recovery of Accelerated Depreciation.”
Line 22--Enter the sum of lines 17, 18, and 19 plus or minus lines 20 and 21.
Line 22.01--For cost reporting periods that overlap or begin on or after April 1, 2013, enter the sequestration adjustment amount as follows: [(2 percent times (total days in the cost reporting period that occur during the sequestration period beginning on or after April 1, 2013, divided by total days in the entire cost reporting period, rounded to four decimal places)) times line 22].
Line 23--Enter the amount of interim payments from Worksheet E-1, column 2, line 4. For contractor final settlements, report on line 24 the amount on line 5.99.
Line 25--Enter line 22 minus the sum of lines 22.01, 23 and 24. Transfer this amount to Worksheet S, Part III, line as appropriate.
Line 26--Enter the program reimbursement effect of protested items. Estimate the reimbursement effect of the nonallowable items by applying a reasonable methodology which closely approximates the actual effect of the item as if it had been determined through the normal cost finding process. (See CMS Pub. 15-2, chapter 1, §115.2.) Attach a schedule showing the details and computations.
DO NOT COMPLETE THE REMAINDER OF WORKSHEET E-3, PART IV. LINES 50 THROUGH 53 ARE FOR CONTRACTOR USE ONLY.
Line 50--Enter the original outlier amount from Worksheet E-3, Part IV, line 2.
Line 51--Enter the outlier reconciliation adjustment amount in accordance with CMS Pub. 100‑04, chapter 3, §§150.26-150.28.
Line 52--Enter the interest rate used to calculate the time value of money. (see CMS Pub. 100‑04, chapter 3, §§150.26-150.28)
Line 53--Enter the time value of money.
NOTE: If a cost report is reopened more than one time, subscript lines 50 through 53, respectively, one time for each time the cost report is reopened.
40-202 Rev.
09-14 FORM CMS-2552-10 4033.5
4033.5 Part V - Calculation of Reimbursement Settlement for Medicare Part A Services - Cost Reimbursement--Use Worksheet E-3, Part V, to calculate reimbursement settlement for Medicare Part A services furnished under cost reimbursement for (1) critical access hospital; and (2) new children’s or new cancer hospital exempt from the rate of increase limits in accordance with 42 CFR 413.40(f).
Line Descriptions
Line 1--Enter the inpatient operating costs for the hospital (CAH, new children’s hospital, or new cancer hospital) from Worksheet D-1, Part II, line 49.
Line 2--Enter the amount of Nursing and Allied Health Managed Care payments, if applicable. Only complete this line if your facility is a CAH.
Line 3--If you are approved as a CTC, enter the cost of organ acquisition from Worksheet D-4, Part III, column 1, line 69 when this worksheet is completed for the hospital (or the hospital component of a health care complex). Make no entry on line 3 in other situations because the Medicare program reimburses only CTCs for organ acquisition costs.
Line 4--Enter the sum of lines 1 through 3.
Line 5--Enter the amounts paid or payable by workers' compensation and other primary payers when program liability is secondary to that of the primary payer. There are six situations under which Medicare payment is secondary to a primary payer:
Workers' compensation,
No fault coverage,
General liability coverage,
Working aged provisions,
Disability provisions, and
Working ESRD provisions.
Generally, when payment by the primary payer satisfies the total liability of the program beneficiary, for cost reporting purposes only, the services are treated as if they were non-program services. (The primary payment satisfies the beneficiary's liability when you accept that payment as payment in full.
This is noted on no-pay bills submitted in these situations.) Include the patient days and charges in total patient days and charges but not in program patient days and charges. In this situation, enter no primary payer payment on line 5. In addition, exclude amounts paid by other primary payers for outpatient dialysis services reimbursed under the composite rate system. However, when the payment by the primary payer does not satisfy the beneficiary's obligation, the program pays the lesser of (a) the amount it otherwise pays (without regard to the primary payer payment or deductible and coinsurance) less the primary payer payment, or (b) the amount it otherwise pays (without regard to primary payer payment or deductibles and coinsurance) less applicable deductible and coinsurance. Primary payer payment is credited toward the beneficiary's deductible and coinsurance obligation.
When the primary payment does not satisfy the beneficiary's liability, include the covered days and charges in program days and charges and include the total days and charges in total days and charges for cost apportionment purposes. Enter the primary payer payment on line 5 to the extent that primary payer payment is not credited toward the beneficiary's deductible and coinsurance. Do not enter on line 5 primary payer payments credited toward the beneficiary's deductible and coinsurance.
Rev. 6 40-203
4033.5 (Cont.) FORM CMS-2552-10 09-14
Line 6--CAHs enter on this line 101 percent of the amount on line 4 minus line 5. For a new children’s or new cancer hospital that is cost reimbursed, enter the result of line 4 minus line 5.
Computation of Lesser of Reasonable Cost or Customary Charges-- This part provides for the computation of the lesser of reasonable cost of services furnished to beneficiaries or customary charges made by you for the same services, as defined in 42 CFR 413.13(a). A new children’s or new cancer hospital exempt from the rate of increase limits must complete lines 7 through 16.
CAHs do not complete lines 7 through 16 as they are exempt from the application of the LCC principle.
Line Descriptions
Lines 7 through 16--These lines provide for the accumulation of charges which relate to the reasonable cost on line 6.
Do not include on these lines (1) the portion of charges applicable to the excess cost of luxury items or services (see CMS Pub. 15-1, chapter 21, §2104.3) and (2) your charges to beneficiaries for excess costs as described in CMS Pub. 15-1, chapter 25, §§2570-2577.
Line 7--Enter the program inpatient routine service charges from your records for the applicable component. Include charges for both routine and special care units. The amounts entered include covered late charges billed to the program when the patient's medical condition is the cause of the stay past the checkout time. Also, these amounts include charges relating to a stay in an intensive care type hospital unit for a few hours when your normal practice is to bill for the partial stay.
Line 8--Enter the total charges for inpatient ancillary services from Worksheet D-3, column 2, sum of lines 50 through 98.
Line 9--If you are an approved CTC, enter the organ acquisition charges from Worksheet D-4, Part III, column 3, line 69 when Worksheet E-3, Part V is completed for the hospital or the hospital component of a health care complex.
Line 10--Enter the sum of lines 7 through 9.
Lines 11 through 14--These lines provide for the reduction of program charges when you do not actually impose such charges on most of the patients liable for payment for services on a charge basis or when you fail to make reasonable efforts to collect such charges from those patients. If line 13 is greater than zero, multiply line 10 by line 13, and enter the result on line 14. If you impose these charges and make reasonable efforts to collect the charges from patients liable for payment for services on a charge basis, you are not required to complete lines 11 through 13. Enter on line 14 the amount from line 10. In no instance may the customary charges on line 14 exceed the actual charges on line 10. (See 42 CFR 413.13(e).)
Line 15--Enter the excess of the customary charges on line 14 over the reasonable cost on line 6.
Line 16--Enter the excess of reasonable cost on line 6 over the customary charges on line 14. Transfer line 16 to line 21.
Line 17--Teaching hospitals participating in an approved GME program, electing to be reimbursed for services of physicians on the basis of reasonable cost (see 42 CFR 415.160 and CMS Pub. 15-1, chapter 21, §2148), enter the cost of physicians. For cost reporting periods ending before June 30, 2014, transfer the amount from Worksheet D-5, Part II, column 3, line 20. For cost reporting periods ending on or after June 30, 2014, transfer the amount from Worksheet D-5, Part IV, line 20. CAHs do not complete this line.
40-204 Rev. 6
DRAFT FORM CMS-2552-10 4033.5 (Cont.)
Computation of Reimbursement Settlement
Line 18--New children’s or new cancer hospitals enter the amount from Worksheet E-4, line 49. CAHs do not complete this line.
Line 19--Enter the sum of lines 6 and 17.
Line 20--Enter the Part A deductibles billed to Medicare beneficiaries.
Line 21-- Enter the amount from line 16. If you are a nominal charge provider, enter zero.
Line 22--Enter line 19 minus lines 20 and 21.
Line 23--Enter from PS&R or your records the coinsurance billed to Medicare beneficiaries.
Line 24--Enter line 22 minus line 23.
Line 25--Enter from your records program allowable bad debts net of recoveries. If recoveries exceed the current year’s bad debts, lines 25 and 26 will be negative.
Line 26--No reduction is required for critical access hospitals for cost reporting periods beginning prior to October 1, 2012, enter the amount from line 25.
Multiply the amount from line 25 (including negative amounts) by 88 percent for cost reporting periods beginning on or after October 1, 2012, 76 percent for cost reporting periods beginning on or after October 1, 2013, and 65 percent for cost reporting periods beginning on or after October 1, 2014.
Line 27--Enter the gross allowable bad debts for dual eligible beneficiaries. This amount is reported for statistical purposes only. This amount must also be reported on line 25.
Line 28--Enter the sum of lines 24 and 26.
Line 29--Enter any other adjustments. For example, if you change the recording of vacation pay from cash basis to accrual basis, enter the adjustment. (See CMS Pub. 15-1, chapter 21, §2146.4.) Specify the adjustment in the space provided.
Enter on line 29.99 the program share of any recovery of accelerated depreciation applicable to prior periods resulting from your termination or a decrease in Medicare utilization. (See CMS Pub. 15-1, chapter 1, §§136-136.16, and 42 CFR 413.134(d)(3)(i).) Identify this line as “Recovery of Accelerated Depreciation.”
Line 30--Enter line 28, plus or minus line 29.
Line 30.01--For cost reporting periods that overlap or begin on or after April 1, 2013, enter the sequestration adjustment amount as follows: [(2 percent times (total days in the cost reporting period that occur during the sequestration period beginning on or after April 1, 2013, divided by total days in the entire cost reporting period, rounded to four decimal places)) times line 30].
Line 31--Enter interim payments from Worksheet E-1, column 2, line 4. For contractor final settlement, report on line 32 the amount from line 5.99.
Line 33--Enter line 30 minus the sum of lines 30.01, 31, and 32. Transfer this amount to Worksheet S, Part III, line as appropriate.
Rev. 40-205
4033.5 (Cont.) FORM CMS-2552-10 09-14
Line 34--Enter the program reimbursement effect of protested items. Estimate the reimbursement effect of the nonallowable items by applying a reasonable methodology which closely approximates the actual effect of the item as if it had been determined through the normal cost finding process. (See CMS Pub. 15-2, chapter 1, §115.2.) Attach a schedule showing the details and computations for this line.
4033.6 Part VI - Calculation of Reimbursement Settlement - Title XVIII Part A PPS SNF Services-- For title XVIII SNFs reimbursed under PPS, complete this part for settlement of Part A services. For Part B services, all SNFs complete Worksheet E, Part B.
When this part is completed for a component, show both the hospital and component numbers.
Computation of Net Costs of Covered Services
Line Descriptions
Prospective Payment Amount
Line 1--Compute the sum of the following amounts obtained your books and records or from the PS&R:
The Resource Utilization Group (RUG) payments made for PPS discharges during the cost reporting period, and
The RUG payments made for PPS transfers during the cost reporting period.
Line 2--Enter the amount from Worksheet D, Part III, column 9, line 44.
Line 3--Enter the amount from Worksheet D, Part IV, column 11, line 200.
Line 4--Enter the sum of lines 1 through 3.
Line 5--Do not use this line as vaccine costs are included on line 1 of Worksheet E, Part B. Line 5 is shaded on Worksheet E-3, Part VI.
Line 6--Enter any deductible amounts imposed.
Line 7--Enter any coinsurance amounts.
Line 8--Enter from your records program allowable bad debts for deductibles and coinsurance net of bad debt recoveries. If recoveries exceed the current year’s bad debts, lines 8 and 9 will be negative.
Line 9--Enter the gross allowable bad debts for dual eligible beneficiaries. This amount must also be reported on line 8. This amount is reported for statistical purposes only for cost reporting periods beginning prior to October 1, 2012.
Line 10--DRA 2005 SNF Bad Debt--Calculate this line as follows for cost reporting periods beginning prior to October 1, 2012: [((line 8 - line 9) * 70 percent) + line 9]. This is the adjusted SNF reimbursable bad debt in accordance with DRA 2005, section 5004.
40-206 Rev. 6
DRAFT FORM CMS-2552-10 4033.6 (Cont.)
In accordance with DRA 2005 SNF Bad Debt as amended by section 3201(b) of the Middle Class Tax Relief and Job Creation Act of 2012, calculate this line as follows: for cost reporting periods beginning on or after October 1, 2012, calculate this line as follows: [((line 8 - line 9) * 65 percent) + (line 9 * 88 percent)]. For cost reporting periods beginning on or after October 1, 2013, calculate this line as follows: [((line 8 - line 9) * 65 percent) + (line 9 * 76 percent)]. For cost reporting periods beginning on or after October 1, 2014, multiply the amount on line 8 by 65 percent.
Line 11--Enter the title XVIII reasonable compensation paid to physicians for services on utilization review committees to an SNF. Include on this line the amount eliminated from total costs on Worksheet A-8. Transfer this amount from Worksheet D-1, Part III, line 85.
Line 12--Enter the result of line 4 plus line 5 minus the sum of lines 6 and 7, plus lines 10 and 11.
Line 13--Enter the amounts paid or payable by workers’ compensation and other primary payers where program liability is secondary to that of the primary payer for inpatient services. Enter only the primary payer amounts applicable to Part A routine and ancillary services.
Line 14--Enter any other adjustments. For example, if you change the recording of vacation pay from the cash basis to accrual basis, etcetera, enter the adjustment. (See CMS Pub. 15-1, chapter 21, §2146.4.) Specify the adjustment in the space provided.
Enter on line 14.99 the program share of any recovery of accelerated depreciation applicable to prior periods resulting from your termination or a decrease in Medicare utilization. (See CMS Pub. 15-1, chapter 1, §§136-136.16, and 42 CFR 413.134(d)(3)(i).) Identify this line as “Recovery of Accelerated Depreciation.”
Line 15--Enter the result of line 12, plus or minus 14, minus line 13.
Line 15.01--For cost reporting periods that overlap or begin on or after April 1, 2013, enter the sequestration adjustment amount as follows: [(2 percent times (total days in the cost reporting period that occur during the sequestration period beginning on or after April 1, 2013, divided by total days in the entire cost reporting period, rounded to four decimal places)) times line 15].
Line 16--For title XVIII, enter the total interim payments from Worksheet E-1, column 2, line 4.
Line 17--For contractor final settlement, report the amount from Worksheet E-1, column 2, line 5.99.
Line 18--Enter line 15 minus the sum of the amounts on lines 15.01, 16 and 17. Transfer this amount to Worksheet S, Part III, line as appropriate.
Line 19--Enter the program reimbursement effect of protested items. Estimate the reimbursement effect of the nonallowable items by applying a reasonable methodology which closely approximates the actual effect of the item as if it had been determined through the normal cost finding process. (See CMS Pub. 15-2, chapter 1, §115.2.) Attach a schedule showing the details and computations.
Rev. 40-207
4033.7 FORM CMS-2552-10 DRAFT
4033.7 Part VII - Calculation of Reimbursement Settlement - All Other Health Services for Titles V or XIX Services--This worksheet calculates reimbursement for titles V or XIX services for hospitals, subproviders, other nursing facilities and ICF/IIDs.
Use a separate copy of this part for each of these reporting situations. Enter check marks in the appropriate spaces at the top of each page of this part to indicate the component and program for which it is used. When this part is completed for a component, show both the hospital and component numbers. Enter check marks in the appropriate spaces to indicate the applicable reimbursement method for inpatient services (e.g., TEFRA, OTHER).
Computation of Net Costs of Covered Services
Line Descriptions
Line 1--Enter the appropriate inpatient operating costs.
Cost Reimbursement
Hospital/CAH or Subprovider - Worksheet D-1, Part II, line 49
Skilled Nursing Facility, Other Nursing Facility, ICF/IID - Worksheet D-1, Part III, line 86. If Worksheet S-2, line 92 is answered “yes”, and multiple Worksheets D-1 are prepared, add the multiple Worksheets D-1 and enter the result.
TEFRA
Hospital or Subprovider - Worksheet D-1, Part II, line 63
NOTE: If you are a new provider reimbursed under TEFRA, use Worksheet D-1, Part II, line 49.
Line 2--Enter the cost of outpatient services for titles V or XIX which is the sum of Worksheet D, Part V, columns 6 and 7 and subscripts where applicable.
Line 3--For titles V and XIX, enter in column 1 the amount paid or payable by the State program for organ acquisition.
Line 4--Enter the sum of lines 1 through 3.
Line 5--Enter in column 1 the amounts paid or payable by workers’ compensation and other primary payers where program liability is secondary to that of the primary payer for inpatient services for titles V and XIX.
Line 6--Enter in column 2 the primary payer amounts applicable to outpatient services for titles V and XIX.
Line 7--Enter line 4 minus the sum of lines 5 and 6.
Computation of Lesser of Reasonable Cost or Customary Charges--You are paid the lesser of the reasonable cost of services furnished to beneficiaries or your customary charges for the same services. This part provides for the computation of the lesser of reasonable cost or customary charges as defined in 42 CFR 413.13(a).
Line Descriptions
Lines 8 through 11--These lines provide for the accumulation of charges which relate to the reasonable cost on line 4.
40-208 Rev.
DRAFT FORM CMS-2552-10 4033.7 (Cont.)
Do not include on these lines (1) the portion of charges applicable to the excess cost of luxury items or services (see CMS Pub. 15-1, chapter 21, §2104.3), and, (2) your charges to beneficiaries for excess costs as described in CMS Pub. 15-1, chapter 25, §§2570-2577.
Line 8--Enter in column 1 the program inpatient routine service charges from your records for the applicable component for title V or XIX. This includes charges for both routine and special care units.
The amounts entered on line 8 include covered late charges billed to the program when the patient's medical condition is the cause of the stay past the checkout time. Also, these amounts include charges relating to a stay in an intensive care type hospital unit for a few hours when your normal practice is to bill for the partial stay.
Line 9--Enter in column 1, the charges from Worksheet D-3, column 2, line 202. Enter in column 2, the sum of the appropriate program ancillary charges from Worksheet D, Part V, columns 3 and/or 4, plus subscripts as applicable, line 202.
Line 10--Enter in column 1, for title V or XIX, the organ acquisition charges from line 3.
Line 11--Enter in column 1, for title V or XIX, the amount of the incentive resulting from the target amount computation on Worksheet D-1, Part II, line 58, if applicable.
Line 12--Enter the sum of the amounts recorded on lines 8 through 11.
Lines 13 through 16--These lines provide for the reduction of program charges when you do not actually impose such charges on most of the patients liable for payment for services on a charge basis or fail to make reasonable efforts to collect such charges from those patients. If line 15 is greater than zero, multiply line 12 by line 15, and enter the result on line 16. If you do impose these charges and make reasonable efforts to collect the charges from patients liable for payment for services on a charge basis, you are not required to complete lines 13 through 15. Enter on line 16 the amount from line 12. In no instance may the customary charges on line 16 exceed the actual charges on line 12.
Line 17--Enter the excess of the customary charges over the reasonable cost. If the amount on line 16 is greater than the amount on line 4, enter the excess.
Line 18--Enter the excess of total reasonable cost over the total customary charges. If the amount on line 4 exceeds the amount on line 16, enter the excess.
Line 19--Enter for title V or XIX, columns 1 and 2, the cost of services rendered by interns and residents as follows from Worksheet D-2:
Col. 1 Col. 2 Col. 1 Col. 2
Title V Title V Title XIX Title XIX
Hospital Part I, Part I, Part I, Part I,
col. 8, col. 8, col. 10, col. 10,
line 9 line 27 line 9 line 27
Subprovider Part I, Part I,
col. 8, col. 10,
lines 10-12 lines 10-12
as applicable as applicable
Nursing Facility, ICF/IID Part I, Part I,
col. 8, col. 10,
line 14 line 14
Rev. 40-209
4033.7 (Cont.) FORM CMS-2552-10 DRAFT
Line 20--Teaching hospitals or subproviders participating in an approved GME program, electing to be reimbursed for services of physicians on the basis of reasonable cost (see 42 CFR 415.160 and CMS Pub. 15-1, chapter 21, §2148), enter the cost of physicians. For cost reporting periods ending before June 30, 2014, transfer the amounts from Worksheet D-5, Part II, column 3, as follows:
From Worksheet D-5, To Worksheet E-3,
Title Part II, column 3 Part VII, line 20:
V Line 18 Column 1
V Line 19 Column 2
XIX Line 22 Column 1
XIX Line 23 Column 2
For cost reporting periods ending on or after June 30, 2014, transfer the amounts from Worksheet D-5, Part IV, as follows:
From To Worksheet E-3,
Title Worksheet D-5, Part IV Part VII, line 20:
V Line 18 Column 1
V Line 19 Column 2
XIX Line 22 Column 1
XIX Line 23 Column 2
Line 21--Enter the lesser of line 4 or line 16. If this is a CAH, or otherwise exempt from lower of cost or charges, transfer the amount from line 4.
Prospective Payment Amount
NOTE: Lines 22 through 26 must only be completed for PPS providers.
Line 22--Enter the total IPPS payments for titles V and/or XIX, as applicable, in column 1. Enter the total OPPS payments for title V or XIX, as applicable, in column 2. Obtain this from your books and records.
Line 23--Enter the amount of outlier payments made for IPPS discharges during the period, in column 1. Enter the outlier payment for OPPS in column 2.
Line 24--Enter in column 1 the payment for inpatient program capital costs from Worksheet L, Part I, line 12; or Part II, line 5, as applicable.
Line 25--Enter in column 1 the result of Worksheet L, Part III, line 13, less Worksheet L, Part III, line 17. If this amount is negative, enter zero on this line.
Line 26--Enter in column 1, the routine and ancillary service other pass through costs from Worksheet D, Part III, column 9, line 200, and from Worksheet D, Part IV, column 11, line 200, respectively. Enter in column 2, the amount from Worksheet D, Part IV, column 13, line 200.
Line 27--For each column, enter the sum of lines 22 through 26.
Line 28--For title V or XIX only, enter the customary charges for IPPS in column 1 and OPPS in column 2.
Line 29--For each column, enter the sum of lines 21 and 27.
40-210 Rev.
09-14 FORM CMS-2552-10 4033.7 (Cont.)
Computation of Reimbursement Settlement
Line 30--For each column, enter the amount, if any, from line 18.
Line 31--For each column, enter the sum of lines 19 and 20 plus line 29 minus lines 5 and 6.
Line 32--For each column, enter any deductible amounts imposed.
Line 33--For each column, enter any coinsurance amounts imposed.
Line 34--For each column, enter from your records reimbursable bad debts for deductibles and coinsurance net of bad debt recoveries.
Line 35--Enter in column 1, the reasonable compensation paid to physicians for services on utilization review committees to an SNF. Include the amount on this line in the amount eliminated from total costs on Worksheet A-8. Transfer this amount from Worksheet D-1, Part III, line 85.
Line 36--For each column, enter the sum of lines 31, 34, and 35 minus the sum of lines 32 and 33.
Line 37--For each column, enter any other adjustments. For example, if you change the recording of vacation pay from the cash basis to the accrual basis, enter the adjustment. (See CMS Pub. 15-1, chapter 21, §2146.4.) Specify the adjustment in the space provided.
Line 38--For each column, enter the result of line 36 plus or minus line 37.
Line 39--Enter the amount from Worksheet E-4, line 31 in column 1.
Line 40--For each column, enter the sum of lines 38 and 39.
Line 41--For each column, enter the interim payments obtained from your records.
Line 42--For each column, enter the result of line 40 minus line 41. Transfer the sum of columns 1 and 2 to Worksheet S, Part III, column 1 (title V) or column 5 (title XIX), line as appropriate.
Line 43--Enter the program reimbursement effect of protested items. Estimate the reimbursement effect of the nonallowable items by applying a reasonable methodology which closely approximates the actual effect of the item as if it had been determined through the normal cost finding process. (See §115.2.) Attach a schedule showing the details and computations.
Rev. 6 40-211
4034 FORM CMS-2552-10 09-14
4034. WORKSHEET E-4 - DIRECT GRADUATE MEDICAL EDUCATION (GME) AND ESRD OUTPATIENT DIRECT MEDICAL EDUCATION COSTS
Use this worksheet to calculate each program's payment (i.e., titles XVIII, V, and XIX) for direct graduate medical education (GME) costs as determined under 42 CFR 413.75 through 413.83. This worksheet applies to the direct graduate medical education cost applicable to interns and residents in approved teaching programs in hospitals and hospital-based providers. Complete this worksheet if the response to line 56 of Worksheet S-2, Part I is yes. The direct medical education costs of the nursing school and paramedical education programs continue to be paid on a reasonable cost basis as determined under 42 CFR 413.85. However, the nursing school and paramedical education costs, formerly paid through the ESRD composite rate as an exception, are paid on this worksheet on the basis of reasonable cost under 42 CFR 413.85. Effective for cost reporting periods beginning on or after October 1, 1997 the unweighted direct graduate medical education FTE is limited to the hospital’s FTE count for the most recent cost reporting period ending on or before December 31, 1996. This limit applies to allopathic and osteopathic residents but excludes dentistry and podiatry. The GME payment is also based on the inclusion of Medicare HMO patients treated in the hospital. This worksheet will also calculate payment for direct GME as determined under 42 CFR 413.79(c)(3) and (4) and IME as determined under 42 CFR 412.105(f)(1)(iv)(B) and (C) for hospitals that received an adjustment (reduction or increase) to their FTE resident caps for direct GME and/or IME under section 422 of Public Law 108-173.
NOTE: Do not complete this worksheet for a cost reporting period prior to the base period used for calculating the per resident amount (PRA) in situations where the hospital did not train residents in approved residency training programs or did not participate in the Medicare program during the base period but either condition changed in a cost reporting period beginning on or after July 1, 1985. 42 CFR 413.77(e)(1) specified that in this situation, any GME costs for the cost reporting period prior to the base period are reimbursed on a reasonable cost basis.
Also, do not complete this worksheet for residents training in the general acute care part of a CAH since the associated costs are reimbursed on a reasonable cost basis.
Complete this worksheet if this is the first month in which residents were on duty during the first month of the cost reporting period or if residents were on duty during the entire prior cost reporting period. (See 42 CFR 413.77(e)(1).)
This worksheet consists of five sections:
1. Computation of Total Direct GME Amount
2. Computation of Program Patient Load
3. Direct Medical Education Costs for ESRD Composite Rate - Title XVIII only
4. Apportionment of Medicare Reasonable Cost (title XVIII only)
5. Allocation of Medicare Direct GME Costs Between Part A and Part B
Computation of Total Direct GME Amount--This section computes the total approved amount.
Line Descriptions
Line 1--Enter the unweighted resident FTE count for allopathic and osteopathic programs for the most recent cost reporting period ending on or before December 31, 1996. If this cost report is less than a full 12 months, contact your contractor. (42 CFR 413.79(c)(2)) Also include here the 30 percent increase to the count for qualified rural hospitals (42 CFR 413.79(c)(2)(i)), and the increase due to primary care residents that were on approved leaves of absence (42 CFR 413.79(i)). Temporarily reduce the cap of a hospital that closed a program(s), if the regulations at 42 CFR 413.79(h)(3)(ii) are applicable. (Effective 10/1/2001.)
40-212 Rev. 6
DRAFT FORM CMS-2552-10 4034 (Cont.)
Line 2--Enter the unweighted resident FTE count for allopathic and osteopathic programs that meet the criteria for an adjustment to the cap for new programs in accordance with 42 CFR 413.79(e). For hospitals qualifying for a cap adjustment under 42 CFR 413.79(e)(1) ) or (e)(3), the cap is effective beginning with the fourth program year of the first new program accredited or begun on or after January 1, 1995, but before October 1, 2012. For hospitals that began training residents in a new program for the first time on or after October 1, 2012, the cap is effective beginning with the sixth program year (see 77 FR August 31, 2012, 53417). For hospitals qualifying for a cap adjustment under 42 CFR 413.79(e)(2), the cap for each new program accredited or begun on or after January 1, 1995, and before August 6, 1997 is reported on this line and is effective in the fourth program year of each of those new programs (see 66 FR August 1, 2001, 39881). The cap adjustment reported on this line should not include any resident FTEs that were already included in the cap on line 1. Do not report new program FTEs during the time frame prior to the effective date of the hospital’s FTE cap on this line. New program FTEs during the time frame prior to the effective date of the hospital’s FTE cap are reported on line 15. For urban hospitals that already have an FTE cap on line 1 but start a rural track program in accordance with 42 CFR 413.75(k), enter the unweighted allopathic or osteopathic FTE count for residents in all years of the rural track program that meet the criteria for an add-on to the cap under 42 CFR 413.79(k). If the rural track program is a new program under 42 CFR 413.79(l) and the urban hospital qualifies for a cap adjustment under 42 CFR 413.79(e)(1) or (e)(3), do not report FTE residents in the rural track program on this line during the time frame prior to the effective date of the hospital’s FTE cap.
Line 3--Enter the section 422 reduction amount to the direct GME cap as specified under 42 CFR 413.79(c)(3).
Line 3.01--Enter the section 5503 reduction amount to the direct GME cap as specified under 42 CFR 413.79(m). If this cost report straddles July 1, 2011, then calculate the prorated section 5503 reduction amount off the cost report and enter the result on this line. (Prorate the cap reduction amount by multiplying it by the ratio of the number of days from July 1, 2011, to the end of the cost reporting period to the total number of days in the cost reporting period). Otherwise enter the full cap reduction amount.
Line 4--Enter the adjustment (increase or decrease) for the unweighted resident FTE count for allopathic or osteopathic programs for affiliated programs in accordance with 42 CFR 413.75(b), 413.79(f), and 63 FR 26336 (May 12, 1998), and 67 FR 50069 (August 1, 2002).
Line 4.01--Enter, as applicable, all or a portion of the amount of the FTE cap slots the hospital was awarded under section 5503 of ACA. The amount of the section 5503 award that is reported on this line is the amount of the section 5503 award that is being “used” in this cost reporting period. In the 5-year evaluation period following implementation of section 5503 (that is, July 1, 2011 through June 30, 2016), at least 75 percent of the slots are to be “used” for additional primary care and/or general surgery residents, while 25 percent of the amount that is reported may be (but need not be) “used” for other purposes. During the 5-year evaluation period, failure to meet the requirements at 42 CFR 413.79(n)(2) of the regulations means loss of a hospital’s section 5503 slots. Therefore, do not automatically report the full amount of the section 5503 slots; only enter the amount of the section 5503 award that equates to at least 75 percent of the FTEs being “used” for additional primary care and/or general surgery FTEs, and no more than 25 percent being used for other FTEs. If, during the 5-year evaluation period, your hospital has not added any primary care or general surgery residents in accordance with receipt of the section 5503 award, leave this line blank and do not report any of the section 5503 award on this line in this cost reporting period. If the amount reported on Worksheet S-2, Part I, line 61.02, column 3, is less than the amount on line 61.01, column 3, then report 0 on this line.
Line 4.02--Enter the amount of increase if the hospital was awarded FTE cap slots from a closed teaching hospital under section 5506 of ACA. Further subscript this line (lines 4.03 through 4.20) as necessary if the hospital receives FTE cap slot awards on more than one occasion under section 5506. Refer to the letter from CMS awarding this hospital the slots under section 5506 to
Rev. 40-213
4034 (Cont.) FORM CMS-2552-10 DRAFT
determine the effective date of the cap increase. If the section 5506 award is phased in over more than one effective date, only report the portions of the section 5506 award as they become effective. If the effective date of the cap increase is not the same as your fiscal year begin date, then prorate the cap increase accordingly. (Prorate the cap increase amount by multiplying it by the ratio of the number of days from the effective date of the cap increase to the end of the cost reporting period to the total number of days in the cost reporting period.)
Line 5--Enter the result of line 1 plus line 2 minus line 3 minus line 3.01 plus or minus line 4 plus line 4.01 plus line 4.02 plus subscripts as applicable. However, if the resulting cap is less than zero, enter zero on this line.
Line 6--Enter the unweighted resident FTE count for allopathic or osteopathic programs for the current year from your records, other than those in the initial years of the program , i.e., the program has not yet completed one cycle of the program (the “period of years” or the minimum accredited length of the program. The residents in programs within the “period of years” are exempt from the rolling average rules. (42 CFR 413.79(d)(5) and (e).) Contact your contractor for instructions on how to complete this line if you have a new program for which the period of years is less than or greater than 3 years. Exclude FTE residents displaced by hospital or program closures that are in excess of the cap for which a temporary cap adjustment is needed (42 CFR 413.79(h)).
Line 7--Enter the lesser of lines 5 or 6.
Line 8--Enter in column 1, the weighted FTE count for primary care physicians and OB/GYN residents in an allopathic or osteopathic program for the current year other than those in the period of years of the program that meet the criteria for an exception to the rolling average rules. Enter in column 2, the weighted FTE count for all other physicians in an allopathic or osteopathic program for the current year other than those in the initial years of the program that meet the criteria for an exception to the rolling average rules. (42 CFR 413.79(d)(5) and (e)). Exclude FTE residents displaced by hospital or program closures that are in excess of the cap for which a temporary cap adjustment is needed (42 CFR 413.79(h)). Enter in column 3 the sum of columns 1 and 2.
Line 9--If line 6 is less than or equal to line 5, enter the amounts from line 8, columns 1 and 2, in columns 1 and 2 of this line. Otherwise, multiply the amount in each column of line 8 by (line 5/line 6). Enter in column 3 the sum of columns 1 and 2. (42 CFR 413.79(c)(2)(iii).)
Line 10--Enter in column 2 the weighted dental and podiatric resident FTE count for the current year.
Line 11--Enter in column 1, the amount from column 1, line 9. Enter in column 2, the sum of the amounts in column 2, lines 9 and 10.
Line 12--Enter in column 1, the weighted FTE count for primary care residents for the prior year, other than those in the initial years of the program that meet the criteria for an exception to the averaging rules (42 CFR 413.79(d)(5)). However, if the period of years during which the FTE residents in any of your new training programs were exempted from the rolling average has expired (see 42 CFR 413.79(d)(5)), also enter on this line the count of FTE residents in that specific primary care program included in Form 2552-96, Worksheet E-3, Part IV, line 3.22 or Form 2552-10, Worksheet E-4, sum of lines 15 and 16 of the prior year’s cost report. If subject to the cap in the prior year Form 2552-96 cost report, report the result of Worksheet E-3, Part IV, line 3.07 times (line 3.04/line 3.05). If subject to the cap in the prior year Form 2552-10 cost report, report the result of Worksheet E-4, column 1, line 8 times (line 5/line 6).
Enter in column 2, the weighted FTE count for nonprimary care residents for the prior year, other than those in the initial years of the program that meet the criteria for an exception to the averaging rules (42 CFR 413.79(d)(5)). However, if the period of years during which the FTE residents in any of your new training programs were exempted from the rolling average has expired (see 42 CFR 413.79(d)(5)), also enter on this line the count of FTE residents in that
40-214 Rev.
DRAFT FORM CMS-2552-10 4034 (Cont.)
specific nonprimary care program included in Form CMS-2552-96, Worksheet E-3, Part IV, line 3.16 or Form CMS-2552-10, Worksheet E-4, sum of lines 15 and 16, of the prior year’s cost report. If subject to the cap in the prior year Form CMS-2552-96 cost report, report the result of Worksheet E-3, Part IV, line 3.08, times (line 3.04/line 3.05), plus line 3.11. If subject to the cap in the prior year Form CMS-2552-10 cost report, report the result of Worksheet E-4, column 2, line 8, times (line 5/line 6), plus line 10.
Line 13--Enter in column 1, the weighted FTE count for primary care residents for the cost reporting year before last, other than those in the initial years of the program that meet the criteria for an exception to the averaging rules (42 CFR 413.79(d)(5)). However, if the period of years during which the FTE residents in any of your new training programs were exempted from the rolling average has expired (see 42 CFR 413.79(d)(5)), also enter on this line the count of FTE residents in that specific primary care program included in Form CMS-2552-96, line 3.22 or for Form CMS-2552-10, sum of lines 15 and 16 of that year’s cost report. If subject to the cap in the year before last Form CMS-2552-96 cost report, report the result of line 3.07 times (line 3.04/line 3.05). If subject to the cap in that year Form CMS-2552-10 cost report, report the result of column 1, line 8, times (line 5/line 6).
Enter in column 2, the weighted FTE count for nonprimary care residents for the cost reporting year before last, other than those in the initial years of the program that meet the criteria for an exception to the averaging rules (42 CFR 413.79(d)(5)). However, if the period of years during which the FTE residents in any of your new training programs were exempted from the rolling average has expired (see 42 CFR 413.79(d)(5)), also enter on this line the count of FTE residents in that specific nonprimary care program included in Form CMS-2552-96, line 3.16 or Form CMS-2552-10, sum of lines 15 and 16 of that year’s cost report. If subject to the cap in the cost reporting year before last, Form CMS-2552-96 cost report, report the result of line 3.08 times (line 3.04/line 3.05) plus line 3.11. If subject to the cap in that year Form CMS-2552-10 cost report, report the result of column 2, line 8, times (line 5/line 6) plus line 10.
Line 14--Enter the rolling average FTE count in each column, by adding lines 11 through 13 and dividing by 3.
Line 15--Enter the weighted number of FTE residents in the initial years of a program that meets the exception to the rolling average rules in column 1 for primary care and in column 2 for nonprimary care FTEs.
Line 16--Enter the temporary weighted FTE residents that were displaced by program or a hospital closure in column 1 for primary care and in column 2 for nonprimary care FTEs, which you would not be able to count without a temporary cap adjustment. (42 CFR 413.79(h).)
Line 17--Enter the sum of lines 14 through 16.
Line 18-- Enter in column 1, the primary care and OB/GYN per resident amount. Enter in column 2, the nonprimary care per resident amount.
Line 19--Enter the result of multiplying lines 17 times line 18. Enter in column 3, the sum of columns 1 and 2.
Line 20--Section 422 Direct GME FTE Cap--Enter the number of unweighted allopathic and osteopathic direct GME FTE resident cap slots the hospital received under 42 CFR 413.79(c)(4).
Line 21--Direct GME FTE Resident Unweighted Count Over/Under the Cap--Subtract line 7 from line 6 and enter the result here. If the result is zero or negative, the hospital does not need to use the direct GME section 422 additional cap and lines 22 through 24 will not be completed.
Rev. 40-215
4034 (Cont.) FORM CMS-2552-10 DRAFT
Line 22--Section 422 Allowable Direct GME FTE Resident Count--If the count on line 21 is less than or equal to the count on line 20, then divide line 8 by line 6, and multiply the resulting ratio by the amount on line 21. If the count on line 21 is greater than the count on line 20, then divide line 8 by line 6, and multiply the resulting ratio by the amount on line 20.
Line 23--Enter the locality adjusted national average per resident amount as specified at 42 CFR 413.77(g), inflated to the hospital’s cost reporting period.
Line 24--Enter the product of lines 22 and 23. This is the allowable section 422 GME cost.
Line 25--Enter the sum of lines 19 and 24. This is the total Part A direct GME cost.
Computation of Program Patient Load--This section computes the ratio of program inpatient days to the total inpatient days. For this calculation, total inpatient days include inpatient days of the hospital along with its subproviders, including distinct part units excluded from the prospective payment system. Record hospital inpatient days of Medicare beneficiaries whose stays are paid by risk basis HMOs and organ acquisition days as non-Medicare days. Do not count inpatient days applicable to nursery, hospital-based SNFs and other nursing facilities, and other non-hospital level of care units for the purpose of determining the Medicare patient load.
Line Descriptions
Line 26--Effective for cost reporting periods beginning prior to October 1, 2013, enter in column 1, for title XVIII, the sum of the days reported on Worksheet S-3, Part I, column 6, lines 1, 8 through 12, and 16 through 18, and subscripts, as applicable. Effective for cost reporting periods beginning on or after October 1, 2013, enter in column 1, for title XVIII, the sum of the days reported on Worksheet S-3, Part I, column 6, lines 1; 8 through 12, and subscripts; 16 through 18 and subscripts; and 32. For titles V or XIX, enter the amounts from columns 5 or 7, respectively, sum of lines 1, 8 through 12, and 16 through 18, and subscripts, as applicable plus column 7, line 32, for title XIX.
For title XVIII, enter in column 2, Medicare managed care days from Worksheet S-3, Part I, column 6, lines 2, 3, and 4. For title XIX, enter in column 2, Medicaid managed care days from Worksheet S-3, Part I, column 7, lines 2, 3, and 4.
Line 27--Effective for cost reporting periods beginning prior to October 1, 2013, transfer to columns 1 and 2, respectively, the sum of the days reported on Worksheet S-3, Part I, column 8, lines 1, 8 through 12, and 16 through 18 and subscripts, as applicable.
Effective for cost reporting periods beginning on or after October 1, 2013, transfer to columns 1 and 2, the sum of the days reported on Worksheet S-3, Part I, column 8, lines 1, 8 through 12, and 16 through 18 and subscripts, as applicable, plus line 32.
Line 28--In each column, divide line 26 by line 27, and enter the result (expressed as a decimal). Column 1 is the title XVIII Part A inpatient utilization and column 2 is the Medicare managed care inpatient utilization.
Line 29--Multiply the amount on line 25, column 1, by the amount reported in each column of line 28.
Line 30--In column 2, enter the amount on line 29, column 2, multiplied by the reduction factor reported in sections D and E of the 65 FR 47038-47039 (August 1, 2000). This is the reduction for direct GME payments for Medicare Advantage.
Line 31--Enter the sum of columns 1 and 2, line 29, less the amount in column 2, line 30.
40-216 |
Rev. 5 |
DRAFT FORM CMS-2552-10 4034 (Cont.)
Direct Medical Education Costs for ESRD Composite Rate Title XVIII Only--This section computes the title XVIII nursing school and paramedical education costs applicable to the ESRD composite rate. These costs are reimbursable based on the reasonable cost principles under 42 CFR 413.85 separate from the ESRD composite rate.
Line Descriptions
Line 32--Enter the amount from Worksheet B, Part I, sum of columns 20 and 23, lines 74 and 94.
Line 33--Enter the amount from Worksheet C, Part I, column 8, sum of lines 74 and 94. This amount represents the total charges for renal and home dialysis.
Line 34--Divide line 32 by line 33, and enter the result. This amount represents the ratio of ESRD direct medical education costs to total ESRD charges.
Line 35--Enter from your records the Medicare outpatient ESRD charges.
Line 36--Enter the result of multiplying line 34 by line 35. This represents the Medicare outpatient ESRD costs. Transfer this amount to Worksheet E, Part B, line 29.
Apportionment of Medicare Reasonable Cost of GME--This section determines the ratio of Medicare reasonable costs applicable to Part A and Part B. The allowable costs of GME on which the per resident amounts are established include GME costs attributable to the entire hospital complex (including non-hospital portions of a health care complex). Therefore, the reasonable costs used in the apportionment between Part A and Part B include the hospital, hospital-based providers, and distinct part units. Do not complete this section for titles V and XIX.
Line Descriptions
Line 37--Include the Part A reasonable cost for the entire hospital complex computed by adding the following amounts:
Hospital and Subprovider(s) - Sum of each Worksheet D-1, Part II, line 49;
Hospital-Based HHAs - Worksheet H-4, Part I, column 1, line 1;
Swing Bed-SNF - Worksheet E-2, line 1, column 1;
Hospital-Based PPS SNF - Sum of Worksheet D-1, Part III, line 74, and Worksheet E‑3, Part VI, column 1, line 4.
Line 38--Enter the organ acquisition costs from Worksheet(s) D-4, Part III, column 1, line 69.
Line 39--Enter the cost of teaching physicians from Worksheet(s) D-5, Part II, column 3, line 20.
Line 40--Enter the total Medicare Part A primary payer amounts for the hospital complex from the applicable worksheets.
PPS hospital and/or subproviders - Worksheet E, Part A, line 60;
TEFRA hospital and/or subproviders - Worksheet E-3, Part I, line 5;
IPF PPS hospital and/or subproviders - Worksheet E-3, Part II, line 17;
IRF PPS hospital and/or subproviders - Worksheet E-3, Part III, line 18;
Rev. 40-216.1
4034 (Cont.) FORM CMS-2552-10 DRAFT
LTC PPS hospital - Worksheet E-3, Part IV, line 8;
Cost reimbursed hospital and/or subproviders - Worksheet E-3, Part V, line 5;
Hospital-based HHAs - Each Worksheet H-4, Part I, column 1, line 9;
Swing Bed SNF and/or NF - Worksheet E-2, column 1, line 9; and
Hospital-based PPS SNF - Worksheet E-3, Part VI, column 1, line 13.
Line 41--Enter the sum of lines 37 through 39 minus line 40.
Line 42--Enter the Part B Medicare reasonable cost. Enter the sum of the amounts on each title XVIII Worksheet E, Part B, columns 1 and 1.01, sum of lines 1, 2, 9, 10, 22, and 23; Worksheet E-2, column 2, line 8; Worksheet H-4, Part I, sum of columns 2 and 3, line 1; Worksheet J-3, column 1, line 1; and Worksheet M-3, line 16.
Line 43--Enter the Part B primary payer amounts. Enter the sum of the amounts on each Worksheet E, Part B, line 31; Worksheet E-2, column 2, line 9; Worksheet H-4, Part I, sum of columns 2 and 3, line 9; Worksheet J-3, line 4; Worksheet M-3, sum of columns 1 and 2, line 17.
Line 44--Enter line 42 minus line 43
Line 45--Enter the sum of lines 41 and 44.
Line 46--Divide line 41 by line 45, and enter the result.
Line 47--Divide line 44 by line 45, and enter the result.
Allocation of Medicare Direct GME Costs Between Part A and Part B--Use this section to compute the GME payments for title XVIII, Part A and Part B, and to compute the total GME payments applicable to titles V and XIX.
Line Descriptions
Line 48--Enter the amount from line 31.
Line 49--Complete for title XVIII only. Multiply line 46 by line 48, and enter the result. If you are a hospital subject to IPPS, transfer this amount to Worksheet E, Part A, line 52. Although this amount includes the Part A GME payments for subproviders, for ease of computation, transfer this amount to the primary hospital component worksheet only. If you are freestanding facility subject to TEFRA, transfer this amount to Worksheet E-3, Part I, line 15. If you are a freestanding IPF PPS, transfer this amount to Worksheet E-3, Part II, line 27. If you are a freestanding IRF PPS, transfer this amount to Worksheet E-3, Part III, line 28. If you are a freestanding LTCH PPS, transfer this amount to Worksheet E-3, Part IV, line 18.
Line 50--Complete for title XVIII only. Multiply line 47 by line 48, and enter the result. Transfer this amount to Worksheet E, Part B, line 28. Although this amount includes the Part B GME payments for subproviders, for ease of computation, transfer this amount to the hospital component only.
SECTIONS 4035 THROUGH 4039 ARE RESERVED FOR FUTURE USE.
40-216.2 Rev.
DRAFT FORM CMS-2552-10 4040
4040. FINANCIAL STATEMENT WORKSHEETS
Prepare these worksheets from your accounting books and records.
Complete all worksheets in the "G" series. Complete Worksheets G and G-1 if you maintain fund-type accounting records, complete separate amounts for General, Specific Purpose, Endowment and Plant funds on Worksheets G and G-1. If you do not maintain fund-type accounting records, complete the general fund column only. Cost reports received with incomplete G worksheets are returned to you for completion. If you do not follow this procedure, you are considered as having failed to file a cost report. Where applicable, Worksheets G, G-1, G-2 and G-3 must be consistent with financial statements prepared by Certified Public Accountants.
4040.1 Worksheet G - Balance Sheet--If the lines on the Worksheet G are not sufficient, use lines 5 (Other receivables), 9 (Other current assets), 44 (Other current liabilities), and 49 (Other long term liabilities), as appropriate, to report the sum of account balances and adjustments. Maintain supporting documentation or subscript the appropriate lines.
Enter accumulated depreciation as a negative amount.
Column 1--General Fund--Use only this fund column when you do not maintain fund-type accounting records. This fund is similar to a general ledger account and records all assets and liabilities of the entity
Column 2--Specific Purpose Fund--These accounts are used for funds held for specific purposes such as research and education.
Column 3--Endowment Fund--These accounts are for amounts restricted for endowment purposes.
Column 4--Plant Fund--These accounts are for amounts restricted for the replacement and expansion of the plant.
Line 1--Cash on Hand and in Banks--The amounts on this line represent the amount of cash on deposit in banks and immediately available for use in financing activities, amounts on hand for minor disbursements and amounts invested in savings accounts and certificates of deposit. Typical accounts would be cash, general checking accounts, payroll checking accounts, other checking accounts, imprest cash funds, saving accounts, certificates of deposit, treasury bills and treasury notes and other cash accounts.
Line 2--Temporary Investments--The amounts on this line represent current securities evidenced by certificates of ownership or indebtedness. Typical accounts would be marketable securities and other current investments.
Line 3--Notes Receivable--The amounts on this line represent current unpaid amounts evidenced by certificates of indebtedness.
Line 4--Accounts Receivable--Include on this line all unpaid inpatient and outpatient billings. Include direct billings to patients for deductibles, co-insurance and other patient chargeable items if they are not included elsewhere.
Line 6--Less: Allowance for Uncollectable Notes and Accounts--These are valuation (or contra-asset) accounts whose credit balances represent the estimated amount of uncollectible receivables from patients and third-party payers. Enter this amount as a negative.
Rev. 40-217
4040.1 (Cont.) FORM CMS-2552-10 DRAFT
Line 7--Inventory--Enter the costs of unused hospital supplies. Perpetual inventory records may be maintained and adjusted periodically to physical count. The extent of inventory control and detailed record-keeping will depend upon the size and organizational complexity of the hospital. Hospital inventories may be valued by any generally accepted method, but the method must be consistently applied from year to year.
Line 8--Prepaid Expenses--Enter the costs incurred which are properly chargeable to a future accounting period.
Line 9--Other Current Assets --These balances include other current assets not included in other asset categories.
Line 10--Due from Other Funds--There are four funds: General Fund, Specific Purpose Fund, Endowment Fund and Plant Fund. These are represented in columns 1 through 4, respectively. Amounts reported in each column should be the amount due from other funds in another column on Worksheet G, line 43 (Due to Other Funds).
The sum of the amounts on line 10, columns 1 through 4 must equal the sum of the amounts on line 43, columns 1 through 4.
Line 12--Land--This balance reflects the cost of land used in hospital operations. Included here is the cost of off-site sewer and water lines, public utility, charges for servicing the land, governmental assessments for street paving and sewers, the cost of permanent roadways and of grading of a non-depreciable nature. Unlike building and equipment, land does not deteriorate with use or with the passage of time; therefore, no depreciation is accumulated.
The cost of land includes (1) the cash purchase price, (2) closing costs such as title and attorney’s fees, (3) real estate broker’s commission, and (4) accrued property taxes and other liens on the land assumed by the purchaser.
Land 13--Land Improvements--Amounts on this line include structural additions made to land, such as driveways, parking lots, sidewalks; as well as the cost of shrubbery, fences and walls, landscaping, on-site sewer and water lines, and underground sprinklers. The cost of land improvements includes all expenditures necessary to make the improvements ready for their intended use.
Line 15--Buildings--This line includes the cost of all buildings and subsequent additions used in hospital operations (including purchase price, closing costs, (attorney fees, title insurance, etcetera), and real estate broker commission). Included are all architectural, consulting and legal fees related to the acquisition or construction of buildings, and interest paid for construction financing.
Line 17--Leasehold Improvements--All expenditures for the improvement of a leasehold used in hospital operations are included on this line.
Line 19--Fixed Equipment--Include the cost of building equipment that has the following general characteristics:
Affixed to the building, not subject to transfer or removal.
A life of more than one year, but less than that of the building to which it is affixed.
Used in hospital operations.
Fixed equipment includes such items as boilers, generators, engines, pumps, and refrigeration machinery, wiring, electrical fixtures, plumbing, elevators, heating system, air conditioning system, etcetera.
40-218 Rev.
08-11 FORM CMS-2552-10 4040.1 (Cont.)
Line 21--Automobiles and Trucks--Enter the cost of automobiles and trucks used in hospital operations.
Line 23--Major movable Equipment--Costs of equipment included on this line has the following general characteristics:
Ability to be moved, as distinguished from fixed equipment (but not automobiles or trucks).
A more or less fixed location in the building.
A unit cost large enough to justify the expense incident to control by means of an equipment ledger and greater than or equal to $5,000.
Sufficient individuality and size to make control feasible by means of identification tags.
A minimum life of usually three years or more.
Used in hospital operations.
Line 25--Minor Equipment-Depreciable--Costs of equipment included on this line has the following general characteristics:
Ability to be moved, as distinguished from fixed equipment.
A more or less fixed location in the building
A unit cost large enough to justify the expense incident to control by means of an equipment ledger but less than $5,000.
Sufficient individuality and size to make control feasible by means of identification tags.
A minimum life of usually three years or more.
Used in hospital operations.
Line 27--Health Information Technology (HIT) Designated Assets--The amounts included here are the acquisition costs of HIT acquired assets in accordance with ARRA 2009, section 4102. Acute care hospitals are required to depreciate such assets in accordance with their applicable depreciation schedules. CAHs are required to identify such assets on this line, but do not depreciate such assets as they will be fully expensed during the year of acquisition.
Line 29--Minor Equipment-Nondepreciable--Costs of equipment included on this line has the following general characteristics:
Location generally not fixed; subject to requisition or use by various departments of the hospital.
Relatively small size.
Subject to storeroom control.
Fairly large number in use.
Generally a useful life of usually approximately three years or less.
Used in hospital operations.
Minor equipment includes such items as, but is not limited to wastebaskets, bed pans, syringes, catheters, basins, glassware, silverware, pots and pans, sheets, blankets, ladders, and surgical instruments.
Lines 14, 16, 18, 20, 22, 24, 26 and 28--Less Accumulated Depreciation--These balances, respectively, include the depreciation accumulated on the related assets used in hospital operations. Enter this amount as a negative.
Line 31--Investments--This field contains the cost of investments purchased with hospital funds and the fair market value (at date of donation) of securities donated to the hospital.
Line 32--Deposits on Leases--Report the amount of deposits on leases. This includes security deposits.
Rev. 2 40-219
4040.1 (Cont.) FORM CMS-2552-10 08-11
Line 33--Due to Owners/Officers--Report the amount loaned to the hospital by owners and/or officers.
Line 34--Other Assets--This is the amount of assets not reported on line 9 (other current assets) or any other line 1 through 33. This could include intangible assets such as goodwill, unamortized loan costs and other organization costs.
Line 35--Total Other Assets--Sum of lines 31 through 34.
Line 36--Total Assets--Sum of lines 11, 30 and 35.
Line 37--Accounts Payable--This amount reflects the amounts due trade creditors and others for supplies and services purchased.
Line 38--Salaries, Wages and Fees Payable--This amount reflects the actual or estimated liabilities of the hospital for salaries and wages/fees payable.
Line 39--Payroll Taxes Payable--This amount reflects the actual or estimated liabilities of the hospital for amounts payable for payroll taxes withheld from salaries and wages, payroll taxes to be paid by the hospital and other payroll deductions, such as hospitalization insurance premiums.
Line 40--Notes and Loans Payable (Short-Term)--The amounts on this line represent current amounts owing as evidenced by certificates of indebtedness coming due in the next 12 months.
Line 41--Deferred Income--Deferred income is received or accrued income which is applicable to services to be rendered within the next accounting period. Deferred income applicable to accounting periods extending beyond the next accounting period is included as other current liabilities. These amounts also reflect the effects of any timing differences between book and tax or third-party reimbursement accounting.
Line 42--Accelerated Payments--Accelerated payments are payments not yet due to be repaid to the contractor.
Line 43--Due to Other Funds--There are four funds: General Fund, Specific Purpose Fund, Endowment Fund and Plant Fund. These are in columns 1 through 4 respectively. Amounts are reported in the fund owing the amount. Each amount recorded as “due to” must also be reported on Worksheet G, line 10 (Due From Other Funds).
The sum of the amounts on line 10, columns 1 through 4 must equal the sum of the amounts on line 41, columns 1 through 4.
Line 44--Other Current Liabilities--This line is used to record any current liabilities not reported on lines 37 through 43.
Line 45--Total Current Liabilities--Enter the sum of lines 37 through 44.
Line 46--Mortgage Payable--This amounts reflects the long-term financing obligation used to purchase real estate/property.
Line 47--Notes Payable--These amounts reflect liabilities of the hospital to vendors, banks and other, evidenced by promissory notes due and payable longer than one year.
40-220 Rev. 2
12-10 FORM CMS-2552-10 4040.1 (Cont.)
Line 48--Unsecured Loans--These amounts are not loaned on the basis of collateral.
Line 49--Other Long-Term Liabilities--This line is used to record any long-term liabilities not reported on lines 46 through 48.
Line 50--Total Long-Term Liabilities--Enter the sum of lines 46 through 49.
Line 51--Total Liabilities--Enter the sum of lines 45 and 50.
Line 52--General Fund Balance--This represents the difference between the total of General Fund assets and General Fund Liabilities in column 1. This amount usually equals the end of period fund balance on Worksheet G-1, column 2, line 19.
Line 53--Specific Purpose Fund--This represents the difference between the total of Specific Purpose Fund assets and Specific Purpose Fund Liabilities in column 2.
Line 54--Donor Created - Endowment Fund Balance - Restricted--The sum of the amounts on lines 54, 55 and 56, represent the difference between the total of Endowment Fund assets and Endowment Fund Liabilities in column 3.
Line 55--Donor Created - Endowment Fund Balance - Unrestricted.
Line 56--Governing Body Created - Endowment Fund Balance.
Line 57--Plant Fund Balance - Invested in Plant--The sum of the amounts on lines 57 and 58, represent the difference between the total of Plant Fund assets and Plant Fund Liabilities in column 4.
Line 58--Plant Fund Balance - Reserves for Plant Improvement, Replacement and Expansion--The credit balances of the restricted funds reported on lines 54 through 56, represent the net amount of each restricted fund’s assets available for its designated purpose. The accounts should be credited for all income earned on restricted fund assets, as well as gains on the disposal of such assets. If, however, such items are treated as General Fund income (considering legal requirements and donor intent), the restricted Fund Balance account is charged, and the Due to General Fund account credited, for such income.
For Investor-Owned Corporations, the accounts on lines 53 through 58 include stock, paid in capital and retained earnings. For Investor-Owned Partnerships, the amounts on lines 53 through 58 include capital and partner’s draw. For Investor-Owned - Division of a Corporation, the amounts on lines 53 through 58 include the division’s or subsidiary’s stock, paid in capital and divisional equity.
Line 59--Total Fund Balances--Enter the sum of lines 52 through 58.
Line 60--Total Liabilities and Fund Balances--Enter the sum of lines 51 and 59.
For each Fund, the amount on line 36 equals the amount on line 60.
Rev. 1 40-221
4040.2 FORM CMS-2552-10 12-10
4040.2 Worksheet G-1 - Statement of Changes in Fund Balances--
Columns 1 and 2--General Fund.
Columns 3 and 4--Specific Purpose Fund--These accounts are used for funds held for specific purposes such as research and education.
Columns 5 and 6--Endowment Fund--These accounts are for amounts restricted for endowment purposes.
Columns 7 and 8--Plant Fund--These accounts are for amounts restricted for the replacement and expansion of the plant.
Line 1--Fund Balance at Beginning of Period--The fund balance at the beginning of the period comes from the prior year cost report Worksheet G-1, line 19, columns 2, 4, 6 and 8, respectively.
Line 2--Net Income--Transfer to column 2, the amount from Worksheet G-3, line 29. Columns 1, 3, 4, 5, 6, 7 and 8 are not completed.
Line 3--Total--For column 2, enter the sum of lines 1 and 2. Leave columns 1, 3, 5 and 7 blank. For columns 4, 6 and 8, bring down the amount on line 1.
Lines 4 through 9--Additions--Most income is included in the net income reported on line 2. Any increases affecting the fund balance not included in net income are reported on these lines. A description (not exceeding 36 characters) is entered for each entry on lines 4 through 9.
Line 10--Total Additions--In columns 2, 4, 6 and 8, enter the sum of lines 4 through 9 columns 1, 3, 5 and 7, respectively.
Line 11--Subtotals--Enter the sum of lines 3 and 10 for columns 2, 4, 6 and 8. Leave columns 1, 3, 5 and 7 blank.
Lines 12 through 17--Deductions--Most expenses are included in the net income reported on line 2. Any decreases affecting the fund balance not included in net income are reported on these lines. A description (not exceeding 36 characters) is entered for each entry on lines 12 through 17.
Line 18--Total Deductions--In columns 2, 4, 6 and 8, enter the sum of lines 12 through 17, columns 1, 3, 5 and 7, respectively.
Line 19--Fund Balance at the end of Period per Balance Sheet--Enter the result of line 11 minus line 18 for columns 2, 4, 6 and 8. Leave columns 1, 3, 5 and 7 blank. The amount in line 19, column 2 must agree with Worksheet G, line 52, column 1. The amount on line 19, column 4 must agree with Worksheet G, line 53, column 2. The amount on line 19, column 6 must agree with the sum of Worksheet G, column 3, lines 54 through 56. The amount on line 19, column 8 must agree with the sum of Worksheet G, column 4, lines 57 and 58.
These amounts will also be used to start next year’s Worksheet G-1.
40-222 Rev. 1
DRAFT FORM CMS-2552-10 4040.3
4040.3 Worksheet G-2, Parts I & II - Statement of Patient Revenues and Operating Expenses--
This worksheet requires the reporting of total patient revenues for the entire facility and operating expenses for the entire facility. If cost report total revenues and total expenses differ from those on your filed financial statements, submit a reconciliation report with the cost report submission. If you have more than one hospital-based HHA and/or more than one outpatient rehabilitation provider, subscript the appropriate lines on Worksheet G-2, Part I, to report the revenue for each multiple based facility separately.
Part I - Patient Revenues--Enter total patient revenues associated with the appropriate cost centers on lines 1-9, 11-15, and 18-25.
Line 1--Hospital--Enter revenues generated by the hospital component of the complex. Obtain these amounts from your accounting books and/or records.
Line 2--Subprovider - IPF--Enter revenues generated by the IPF (also referred to as the IPF excluded unit) of the complex. Obtain this amount from your accounting books and/or records.
Line 3--Subprovider - IRF--Enter revenues generated by the IRF (also referred to as the IRF excluded unit) of the complex. Obtain this amount from your accounting books and/or records.
Line 4--Subprovider - Other--Enter revenues generated by components identified as subproviders of the complex that were not identified on lines 2 or 3. Subscript this line as necessary. Obtain these amounts from your accounting books and/or records.
Line 5--Swing Bed - SNF--Enter the swing bed - SNF revenue from your accounting books and/or records.
Line 6--Swing Bed - NF--Enter the swing bed - NF revenue from your accounting books and/or records.
Line 7--Skilled Nursing Facility--Enter the skilled nursing facility revenue from your accounting books and/or records.
Line 8--Nursing Facility--Enter the nursing facility revenue from your accounting books and/or records.
Line 9--Other Long Term Care-- Enter the revenue generated from other long term care subproviders from your accounting books and/or records. Subscript this line as necessary.
Line 10--Total General Inpatient Routine Care--Sum of lines 1 through 9.
Line 11--Intensive Care Unit--Enter the intensive care unit revenue from your accounting books and/or records.
Line 12--Coronary Care Unit--Enter the coronary care unit revenue from your accounting books and/or records.
Line 13--Burn Intensive Care Unit--Enter the burn intensive care unit revenue from your accounting books and/or records.
Line 14--Surgical Intensive Care Unit--Enter the surgical intensive care unit revenue from your accounting books and/or records.
Rev. 40-223
4040.3 (Cont.) FORM CMS-2552-10 DRAFT
Line 15--Other Special Care-- Enter all other intensive care unit revenue not identified on lines 11 through 14 from your accounting books and/or records. Subscript this line as necessary.
Line 16--Total Intensive Care Type Inpatient Hospital--Sum of lines 11 through 15.
Line 17--Total Inpatient Routine Care Services--Sum of lines 10 and 16.
Line 18--Ancillary Services--Enter in the appropriate column revenue from inpatient ancillary services and outpatient ancillary services from your accounting books and/or records.
Line 19--Outpatient Services--Enter in the appropriate column revenue from outpatient ancillary services from your accounting books and/or records.
Line 20--Rural Health Clinic (RHC)--Enter RHC revenue from your accounting books and/or records. Subscript this line to identify each rural health clinic separately.
Line 21--Federally Qualified Health Center (FQHC)--Enter FQHC revenue from your accounting books and/or records. Subscript this line to identify each federally qualified health center separately.
Line 22--Home Health Agency--Enter home health agency revenue from your accounting books and/or records. If there is more than one home health agency, include the revenues for all home health agencies on this line.
Line 23--Ambulance Services--Enter from your accounting books and/or records the revenue relative to the ambulance service cost reported on Worksheet A, line 95.
Line 24--Outpatient Rehabilitation Providers--Enter in column 2 only, the revenue generated from CMHC, CORF, outpatient therapy providers (OPTs, OOTs and OSPs), and any other outpatient rehabilitation providers. Subscript this line to identify each outpatient rehabilitation provider separately. Obtain this information from your accounting books and/or records.
Line 25--Ambulatory Surgical Center(s)--Enter from your accounting books and/or records the revenue relative to the Ambulatory Surgical Center costs report on Worksheet A, lines 75 and 115.
Line 26--Hospice--Enter from your accounting books and/or records in the appropriate column, the revenue generated from hospice services rendered. If there is more than one hospice, include the revenues for all hospices on this line.
Line 27--Enter in the appropriate column all other revenues not identified on lines 18 through 26.
Line 28--Total Patient Revenues--Enter the sum of lines 17 through 27.
Column 3--For lines 1 through 28, enter the sum of columns 1 and 2, as applicable, in column 3.
Part II - Operating Expenses--Enter the expenses incurred that arise during the ordinary course of operating the hospital complex.
Line 29--Operating Expenses--This amount is transferred from Worksheet A, line 200, column 3.
Lines 30-35--Add (Specify)--Identify on these lines additional operating expenses not included in line 27.
Line 36--Total Additions--Enter on line 36, column 2, the sum of lines 30 to 35, column 1.
40-224 Rev.
DRAFT FORM CMS-2552-10 4040.4
Lines 37 - 41--Deduct (specify)--Identify on these lines deductions from operating expenses not accounted for included in line 29.
Line 42--Total Deductions--Enter on line 42, column 2, the sum of lines 37 to 41, column 1.
Line 43--Total Operating Expenses--Enter on line 43, column 2, the result of line 29, column 2 plus line 36, column 2, less line 42, column 2.
4040.4 Worksheet G-3 - Statement of Revenues and Expenses--
This worksheet requires the reporting of total revenues for the entire facility and total operating expenses for the entire facility. If cost report total revenues and total expenses differ from those on your filed financial statements, submit a reconciliation report with the cost report submission.
Line 1--Total Patient Revenue--Transfer from Worksheet G-2, Part I, line 28, column 3.
Line 2--Less: Allowance and Discounts on Patient’s Accounts--Enter on this line total patient revenues not received. This includes:
Provision for Bad Debts,
Contractual Adjustments,
Charity Discounts,
Teaching Allowances,
Policy Discounts,
Administrative Adjustments, and
Other Deductions from Revenue
Line 3--Net Patient Revenues--Subtract line 2 from line 1.
Line 4--Less: Total Operating Expenses--Transfer from Worksheet G-2, Part II, line 43.
Line 5--Net Income from Service to Patients--Subtract line 4 from line 3.
Lines 6 - 23--Enter on the appropriate line 6 through 23 all other revenue not reported on line 1. Obtain these amounts from your accounting books and/or records.
Line 24--Other (Specify)--Enter from hospital books. Enter all other revenue not reported on lines 6 through 23. Obtain this from your accounting books and/or records. Subscript this line as necessary.
Line 25--Total Other Income--Enter the sum of lines 6 through 24.
Line 26--Total--Enter the sum of lines 5 and 25.
Line 27--Other Expenses (Specify)--Enter all other expenses not reported on lines 6 through 24. Subscript this line as necessary.
Line 28--Total Other Expenses--Enter the sum of line 27 and subscripts.
Line 29--Net Income (or Loss) for the Period--Enter the result of line 26 minus line 28.
Rev. 40-225
4041 FORM CMS-2552-10 DRAFT
4041. WORKSHEET H - ANALYSIS OF HOSPITAL-BASED HOME HEALTH AGENCY COSTS
This worksheet provides for the recording of direct HHA costs such as salaries, fringe benefits, transportation, and contracted services as well as other costs from your accounting books and records to arrive at the identifiable agency cost. This data is required by 42 CFR 413.20. It also provides for the necessary reclassifications and adjustments to certain accounts prior to the cost finding calculations. The direct costs reported in columns 1, 2 and 4 are obtained from your accounting books and records. All of the cost centers listed do not apply to all agencies.
The HHA must maintain the records necessary to determine the split in salary (and employee-related benefits) between two or more cost centers and must adequately substantiate the method used to split the salary and employee-related benefits. These records must be available for audit by your contractor. Your contractor can accept or reject the method used to determine the split in salary. Any deviation or change in methodology to determine splits in salary and employee benefits must be requested in writing and approved by your contractor before any change is effectuated. Where approval of a method has been requested in writing and this approval has been received (prior to the beginning of the cost reporting period), the approved method remains in effect for the requested period and all subsequent periods until you request in writing to change to another method or until your contractor determines that the method is no longer valid due to changes in your operations.
Column 1--Enter all salaries and wages (a salary is the gross amount paid to the employee before taxes and other items are withheld, including deferred compensation, overtime, incentive pay, and bonuses) for the HHA in this column for the actual work performed within the specific area or cost center. For example, if the administrator spends 100 percent of his/her time in the HHA and performs skilled nursing care which accounts for 25 percent of that person’s time, then 75 percent of the administrator’s salary is entered on line 5 (A&G - HHA) and 25 percent of the administrator’s salary is entered on line 6 (skilled nursing care). Enter the sum of column 1, lines 1 through 23, on line 24.




 Column
2--Enter all payroll-related
employee benefits for the HHA in the appropriate cost center in this
column. See CMS Pub. 15-1, chapter21,
§§2144-2145,
for a definition of fringe benefits. Entries are made using the same
basis as that used for reporting salaries and wages in column 1.
Therefore, using the same example as given for column 1, 75 percent
of the administrator’s payroll-related fringe benefits is
entered on line 5 (A&G
- HHA) and 25 percent of the administrator’s
payroll-related fringe benefits is entered on line 6 (skilled nursing
care). Enter the sum of column 2, lines 1 through 23,
on line 24.
Column
2--Enter all payroll-related
employee benefits for the HHA in the appropriate cost center in this
column. See CMS Pub. 15-1, chapter21,
§§2144-2145,
for a definition of fringe benefits. Entries are made using the same
basis as that used for reporting salaries and wages in column 1.
Therefore, using the same example as given for column 1, 75 percent
of the administrator’s payroll-related fringe benefits is
entered on line 5 (A&G
- HHA) and 25 percent of the administrator’s
payroll-related fringe benefits is entered on line 6 (skilled nursing
care). Enter the sum of column 2, lines 1 through 23,
on line 24.
 Report
payroll-related employee benefits in the cost center where the
applicable employee’s compensation is reported. This
assignment is performed on an actual basis or upon the following
basis:
Report
payroll-related employee benefits in the cost center where the
applicable employee’s compensation is reported. This
assignment is performed on an actual basis or upon the following
basis:
FICA based on actual expense by cost center;
Pension and retirement and health insurance (non-union) based on gross salaries of participating individuals by cost centers;
Union health and welfare based on gross salaries of participating union members by cost center; and
All other payroll-related benefits based on gross salaries by cost center.
40-226 Rev.
12-10 FORM CMS-2552-10 4041 (Cont.)
Include nonpayroll-related employee benefits in the administrative and general-HHA cost center. Costs for such items as personal education, recreation activities, and day care are included in the administrative and general - HHA cost center.
Column 3--If the transportation costs, i.e., owning or renting vehicles, public transportation expenses, or payments to employees for driving their private vehicles can be directly assigned to a particular cost center, enter those costs in the appropriate cost center. If these costs are not identifiable to a particular cost center, enter them on line 4. Enter the sum of column 3, lines 1 through 23 on line 24.
Column 4--Enter the contracted and purchased services amounts in the appropriate cost center in this column. If a contracted/purchased service covers more than one cost center, then include the amount applicable to each cost center on each affected cost center line. Enter the sum of column 4, lines 1 through 23 on line 24.
Column 5--From your books and records, enter on the applicable lines all other identifiable costs which have not been reported in columns 1 through 4. Enter the sum of column 5, lines 1 through 23 on line 24.
Column 6--Add the amounts in columns 1 through 5 for each cost center, and enter the totals in column 6.
Column 7--Enter any reclassifications among the cost center expenses listed in column 6 which are needed to effect proper cost allocation. This column need not be completed by all providers, but is completed only to the extent reclassifications are needed and appropriate in the particular circumstances. Show reductions to expenses as negative amounts.
Column 8--Add column 7 to column 6, and extend the net balances to column 8.
Column 9--In accordance with 42 CFR 413ff, enter on the appropriate lines the amounts of any adjustments to expenses required under the Medicare principles of reimbursement. (See §4016.)
Column 10--Adjust the amounts in column 8 by the amounts in column 9, and extend the net balance to column 10.
Transfer the amounts in column 10, lines 1 through 24, to the corresponding lines on Worksheet H-1, Part I, column 0.
Line Descriptions
Lines 1 and 2--These cost centers include depreciation, leases and rentals for the use of facilities and/or equipment, interest incurred in acquiring land or depreciable assets used for patient care, insurance on depreciable assets used for patient care, and taxes on land or depreciable assets used for patient care.
Line 3--Enter the direct expenses incurred in the operation and maintenance of the plant and equipment, maintaining general cleanliness and sanitation of the plant, and protecting employees, visitors, and agency property.
Line 4--Enter all of the cost of transportation except those costs previously directly assigned in column 3. This cost is allocated during the cost finding process.
Rev. 1 40-227
4041 (Cont.) FORM CMS-2552-10 12-10
Line 5--Use this cost center to record the expenses of several costs which benefit the entire facility. Examples include fiscal services, legal services, accounting, data processing, taxes, and malpractice costs.
Line 6--Skilled nursing care is a service that must be provided by or under the supervision of a registered nurse. The complexity of the service, as well as the condition of the patient, are factors to be considered when determining whether skilled nursing services are required. Additionally, the skilled nursing services must be required under the plan of treatment.
Line 7--Enter the direct costs of physical therapy services by or under the direction of a registered physical therapist as prescribed by a physician. The therapist provides evaluation, treatment planning, instruction, and consultation.
Line 8--These services include (1) teaching of compensatory techniques to permit an individual with a physical impairment or limitation to engage in daily activities; (2) evaluation of an individual's level of independent functioning; (3) selection and teaching of task-oriented therapeutic activities to restore sensory-integrative function; and (4) assessment of an individual's vocational potential, except when the assessment is related solely to vocational rehabilitation.
Line 9--These are services for the diagnosis and treatment of speech and language disorders that create difficulties in communication.
Line 10--These services include (1) assessment of the social and emotional factors related to the individual's illness, need for care, response to treatment, and adjustment to care furnished by the facility; (2) casework services to assist in resolving social or emotional problems that may have an adverse effect on the beneficiary's ability to respond to treatment; and (3) assessment of the relationship of the individual's medical and nursing requirements to his or her home situation, financial resources, and the community resources available upon discharge from facility care.
Line 11--Enter the cost of home health aide services. The primary function of a home health aide is the personal care of a patient. The services of a home health aide are given under the supervision of a registered professional nurse and, if appropriate, a physical, speech, or occupational therapist. The assignment of a home health aide to a case must be made in accordance with a written plan of treatment established by a physician which indicates the patient's need for personal care services. The specific personal care services to be provided by the home health aide must be determined by a registered professional nurse and not by the home health aide.
Line 12--The cost of medical supplies reported in this cost center are those costs which are directly identifiable supplies furnished to individual patients and for which a separate charge is made. These supplies are generally specified in the patient’s plan of treatment and furnished under the specific direction of the patient’s physician.
Medical supplies which are not reported on this line are those minor medical and surgical supplies which would not be expected to be specifically identified in the plan of treatment or for which a separate charge is not made. These supplies (e.g., cotton balls, alcohol prep) are items that are frequently furnished to patients in small quantities (even though in certain situations, these items may be used in greater quantity) and are reported in the A&G cost center.
Line 13--Enter the costs of vaccines exclusive of the cost of administering the vaccines. A visit by an HHA nurse for the sole purpose of administering a vaccine is not covered as an HHA visit under the home health benefit, even though the patient may be an eligible home health beneficiary receiving services under a home health plan of treatment. Section 1862(a)(1)(B) of the Act excludes Medicare coverage of vaccines and their administration other than the Part B coverage contained in §1861 of the Act.
40-228 Rev. 1
DRAFT FORM CMS-2552-10 4041 (Cont.)
If the vaccine is administered in the course of an otherwise covered home health visit, the visit is covered as usual, but the cost and charges for the vaccine and its administration must be excluded from the cost and charges of the visit. The HHA is entitled to separate payment for the vaccine and its administration under the Part B vaccine benefit.
The cost of administering pneumococcal, influenza, and hepatitis B vaccines is reimbursed under the outpatient prospective payment system (OPPS), but the actual cost of the pneumococcal, influenza, and hepatitis B vaccines are cost reimbursed. Additionally, the cost of administering the osteoporosis drugs are included in the skilled nursing visit while the actual cost of the osteoporosis drug is reimbursed at reasonable cost.
Enter on this line the vaccine and drug cost (exclusive of the cost to administer these vaccines) incurred for pneumococcal, influenza, and hepatitis B vaccines as well as osteoporosis drugs.
Some of the expenses includable in this cost center are the costs of syringes, cotton balls, bandages, etcetera, but the cost of travel is not permissible as a cost of administering vaccines, nor is the travel cost includable in the A&G cost center. The travel cost is non-reimbursable. Attach a schedule detailing the methodology employed to develop the administration of these vaccines. These vaccines are reimbursable under Part B only.
Line 14--Enter the direct expenses incurred in renting or selling DME items to the patient for the purpose of carrying out the plan of treatment. Also, include all the direct expenses incurred by you in requisitioning and issuing the DME to patients.
Lines 15 through 23--Lines 15 through 23 identify nonreimbursable services commonly provided by a home health agency. These include home dialysis aide services (line 15), respiratory therapy (line 16), private duty nursing (line 17), clinic (line 18), health promotion activities (line 19), day care program (line 20), home delivered meals program (line 21), and homemaker service (line 22). The cost of all other nonreimbursable services are aggregated on line 23. If you are reporting costs for telemedicine, these costs are to be reported on line 23.50. Use this line throughout all applicable worksheets.
Rev. 40-229
4042 FORM CMS-2552-10 DRAFT
4042. WORKSHEET H-1 - COST ALLOCATION - HHA GENERAL SERVICE COST
Worksheet H-1, Part I, provides for the allocation of the expenses of each HHA general service cost center to those cost centers which receive the services. The cost centers serviced by the general service cost centers include all cost centers within the home health agency, i.e., other general service cost centers, reimbursable cost centers, and nonreimbursable cost centers. Obtain the total direct expenses from Worksheet H, column 10. To facilitate transferring amounts from Worksheet H to Worksheet H-1, Part I, the same cost centers with corresponding line numbers (lines 1 through 24) are listed on both worksheets.
 Worksheet
H-1, Part II, provides for the proration of the statistical data
needed to equitably allocate the expenses of the home health agency
general service cost centers on Worksheet H-1, Part I. If there is a
difference between the total accumulated costs reported on the Part
II statistics and the total accumulated costs calculated on Part I,
use the reconciliation column on Part II for reporting any
adjustments. See §4020 for the appropriate usage of the
reconciliation columns. For componentized A&G cost centers, the
accumulated cost center line number must match the reconciliation
column number.
Worksheet
H-1, Part II, provides for the proration of the statistical data
needed to equitably allocate the expenses of the home health agency
general service cost centers on Worksheet H-1, Part I. If there is a
difference between the total accumulated costs reported on the Part
II statistics and the total accumulated costs calculated on Part I,
use the reconciliation column on Part II for reporting any
adjustments. See §4020 for the appropriate usage of the
reconciliation columns. For componentized A&G cost centers, the
accumulated cost center line number must match the reconciliation
column number.
To facilitate the allocation process, the general format of Parts I and II are identical. The column and line numbers for each general service cost center are identical on both parts. In addition, the line numbers for each general, reimbursable, and nonreimbursable cost centers are identical on the two parts of the worksheet. The cost centers and line numbers are also consistent with Worksheet H.
The statistical bases shown at the top of each column on Worksheet H-1, Part II, are the recommended bases of allocation of the cost centers indicated. If a different basis of allocation is used, the provider must indicate the basis of allocation actually used at the top of the column.
Most cost centers are allocated on different statistical bases. However, for those cost centers where the basis is the same (e.g., square feet), the total statistical base over which the costs are to be allocated will differ because of the prior elimination of cost centers that have been closed.
When closing the general service cost center, first close those cost centers that render the most services to and receive the least services from other cost centers. The cost centers are listed in this sequence from left to right on the worksheet. However, the circumstances of an agency may be such that a more accurate result is obtained by allocating to certain cost centers in a sequence different from that followed on these worksheets.
NOTE: The HHA can elect to change the order of allocation and/or allocation statistics, as appropriate, for the current cost reporting period if a request is received by the contractor, in writing, 90 days prior to the end of that reporting period. The contractor has 60 days to make a decision and notify the provider of that decision or the change is automatically accepted. The change must be shown to more accurately allocate the overhead or demonstrate simplification in maintaining the changed statistics. If a change in statistics is requested, the provider must maintain both sets of statistics until an approval is made. If both sets are not maintained and the request is denied, the provider reverts back to the previously approved methodology. The provider must include with the request all supporting documentation and a thorough explanation of why the alternative approach should be used. (See CMS Pub. 15-1, chapter 23, §2313.)
EXCEPTION: A small freestanding HHA, as defined in 42 CFR 413.24(d), does not have to request written permission to use the procedures outlined for small HHAs below.
40-230 Rev.
08-11 FORM CMS-2552-10 4042 (Cont.)
On Worksheet H-1, Part II, enter on the first line in the column of the cost center being allocated the total statistical base over which the expenses are allocated (e.g., in column 1, capital-related - buildings and fixtures, enter on line 1 the total square feet of the building on which depreciation was taken). For all cost centers to which the capital-related cost is allocated, enter that portion of the total statistical base applicable to each. The sum of the statistical base applied to each cost center receiving the services must equal the total base entered on the first line. Use accumulated cost for allocating A&G expenses.
Do not include any statistics related to services furnished under arrangements unless:
Both Medicare and non-Medicare costs of arranged for services are recorded in your records; or
Your contractor determines that you are able to (and do) gross up the costs and charges for services to non-Medicare patients so that both cost and charges are recorded as if you had furnished such services directly to all patients. (See CMS Pub. 15-1, chapter 23, §2314.)
Enter on Worksheet H-1, Part II, line 25, the total expenses of the cost center to be allocated. Obtain this amount from Worksheet H-1, Part I, from the same column and line number used to enter the statistical base on Worksheet H-1, Part II. In the case of capital-related costs - buildings and fixtures, this amount is on Worksheet H-1, Part I, column 1, line 1.
NOTE: On Worksheet H-1, Parts I and II, the first line of each column must equal line 24 of the column. Therefore, when totaling a column exclude from line 24 the amount on the first line of that column.
Divide the amount entered on Worksheet H-1, Part II, line 25 by the total statistical base entered in the same column on the first line. Enter the resulting unit cost multiplier on line 26. Round the unit cost multiplier to six decimal places.
Multiply the unit cost multiplier by that portion of the total statistical base applicable to each cost center receiving the services rendered. Enter the result of each computation on Worksheet H-1, Part I, in the corresponding column and line.
After the unit cost multiplier has been applied to all the cost centers receiving costs, the total expenses (line 24) of all of the cost centers receiving the allocation on Worksheet H-1, Part I, must equal the amount entered on the first line of the cost center being allocated.
The preceding procedures must be performed for each general service cost center. Each cost center must be completed on both Part I and Part II before proceeding to the next cost center.
After all the costs of the general service cost centers have been allocated on Worksheet H-1, Part I, enter in column 6, line 24 the sum of the expenses on lines 6 through 23. The total expenses entered in column 6, line 24, equals the total expenses entered in column 0, line 24.
Column Descriptions
Column 1--Depreciation on buildings and fixtures and expenses pertaining to buildings and fixtures such as insurance, interest, rent, and real estate taxes are combined in this cost center to facilitate cost allocation. Allocate all expenses to the cost centers on the basis of square footage of the occupied area. The square footage may be weighted if the person who occupies a certain area of space spends their time in more than one function. For example, if a person spends 10 percent of time in one function, 20 percent in another function, and 70 percent in still another function, the square footage may be weighted according to the percentages of 10 percent, 20 percent, and 70 percent to the applicable functions.
Rev. 2 40-231
4042 (Cont.) FORM CMS-2552-10 DRAFT
Column 2--Allocate all expenses (e.g., interest, personal property tax) for movable equipment to the appropriate cost centers on the basis of dollar value.
Column 3--Allocate all expenses for plant operation and maintenance based on square feet.
Column 4--The cost of vehicles owned or rented by the agency and all other transportation costs which were not directly assigned to another cost center on Worksheet H, column 3, is included in this cost center. Allocate this expense to the cost centers to which it applies on the basis of miles applicable to each cost center.
This basis of allocation is not mandatory and a provider may use weighted trips rather than actual miles as a basis of allocation for transportation costs which are not directly assigned. However, an HHA must request the use of the alternative method in accordance with CMS Pub. 15-1, chapter 23, §2313. The HHA must maintain adequate records to substantiate the use of this allocation.
Column 5--The A&G expenses are allocated on the basis of accumulated costs after reclassifications and adjustments. Therefore, obtain the amounts to be entered on Worksheet H‑1, Part II, column 5, from Worksheet H-1, Part I, columns 0 through 4.
A negative cost center balance in the statistics for allocating A&G expenses causes an improper distribution of this overhead cost center. Negative balances are excluded from the allocation statistics when A&G expenses are allocated on the basis of accumulated cost.
A&G costs applicable to contracted services may be excluded from the total cost (Worksheet H‑1, Part I, column 0) for purposes of determining the basis of allocation (Worksheet H-1, Part II, column 5) of the A&G costs. This procedure may be followed when the HHA contracts for services to be performed for the HHA and the contract identifies the A&G costs applicable to the purchased services. The contracted A&G costs must be added back to the applicable cost center after allocation of the HHA A&G cost before the reimbursable costs are transferred to Worksheet H-2. A separate worksheet must be included to display the breakout of the contracted A&G costs from the applicable cost centers before allocation and the adding back of these costs after allocation. Contractor approval does not have to be secured in order to use the above described method of cost finding for A&G.
Column 6--For lines 6 through 23, add the amounts on each line in columns 4A and 5, and enter the result for each line in this column.
Transfer the amounts in column 6 to Worksheet H-2, Part I, column 0, as follows:
From Worksheet H-1, To Worksheet H-2,
Part I, Column 6 Part I, Column 0___
Line 6 Line 2
7 3
40-232 Rev.
08-11 FORM CMS-2552-10 4042 (Cont.)
From Worksheet H-1, To Worksheet H-2,
Part I, Column 6 Part I, Column 0_
8 4
9 5
10 6
11 7
12 8
13 9
14 10
15 11
16 12
17 13
18 14
19 15
20 16
21 17
22 18
23 19
Rev. 2 40-233
4043 FORM CMS-2552-10 08-11
4043. WORKSHEET H-2 - ALLOCATION OF GENERAL SERVICE COSTS TO HHA COST CENTERS
Use this worksheet only if you operate a certified hospital-based HHA as part of your complex. If you have more than one hospital-based HHA, complete a separate worksheet for each facility.
4043.1 Part I - Allocation of General Service Costs to HHA Cost Centers.--Worksheet H-2, Part I, provides for the allocation of the expenses of each general service cost center of the hospital to those cost centers which receive the services. Worksheet H-2, Part II provides for the proration of the statistical data needed to equitably allocate the expenses of the general service cost centers on Worksheet H-2, Part I.
Obtain the total direct expenses (column 0, line 20) from Worksheet A, column 7, line 101. Obtain the cost center allocations (column 0, lines 1 through 19) from Worksheet H-1, Part I, lines as indicated, the sum of which agrees with the amount entered on column 0, line 20. The amounts on line 20, columns 0 through 23 and column 25 must agree with the corresponding amounts on Worksheet B, Part I, columns 0 through 23 and column 25, line 101. Complete the amounts entered on lines 1 through 19, columns 1 through 23 and column 25 in accordance with the instructions in §4043.2.
NOTE: Worksheet B, Part I, established the method used to reimburse direct graduate medical education cost (i.e., reasonable cost or the per resident amount). Therefore, this worksheet must follow that method. If Worksheet B, Part I, column 25, excluded the costs of interns and residents, column 25 on this worksheet must also exclude these costs.
In column 24, Part I, enter the total of columns 4A through 23.
In column 27, Part I, enter on line 21, the unit cost multiplier (column 26, line 1, divided by the sum of column 26, line 20 minus column 26, line 1). Round the unit cost multiplier to 6 decimal places. Multiply each amount in column 26, lines 2 through 19 by the unit cost multiplier on line 21, and enter the result on the corresponding line of column 27. On line 20, enter the total of the amounts on lines 2 through 19. The total on line 20 must equal the amount in column 26, line 1.
In column 28, Part I, enter on lines 2 through 19 the sum of columns 26 and 27. The total on line 20 must equal the total in column 27, line 20.
4043.2 Part II - Allocation of General Service Costs to HHA Cost Centers -Statistical Basis--To facilitate the allocation process, the general format of Worksheet H-2, Parts I and II, is identical. Worksheet H-2, Part II, provides for the proration of the statistical data needed to equitably allocate the expenses of the hospital’s general service cost centers on Worksheet H-2, Part I.
The statistical basis shown at the top of each column on Worksheet H-2, Part II, is the recommended basis of allocation of the cost center indicated.
Lines 1 through 19--On Worksheet H-2, Part II, for all cost centers to which the general service cost center is being allocated, enter that portion of the total statistical base applicable to each.
40-234 Rev. 2
08-11 FORM CMS-2552-10 4043.2 (Cont.)
Line 20--Enter the total of lines 1 through 19 for each column. The total in each column must be the same as shown for the corresponding column on Worksheet B-1, line 101.
Line 21--Enter the total expenses for the cost center allocated. Obtain this amount from Worksheet B, Part I, line 101, from the same column used to enter the statistical base on Worksheet H-2, Part II (e.g., in the case of capital-related cost buildings and fixtures, this amount is on Worksheet B, Part I, column 1, line 101).
Line 22--Enter the unit cost multiplier which is obtained by dividing the cost entered on line 21 by the total statistic entered in the same column on line 20. Round the unit cost multiplier to six decimal places.
Multiply the unit cost multiplier by that portion of the total statistic applicable to each cost center receiving the services. Enter the result of each computation on Worksheet H-2, Part I, in the corresponding column and line.
After the unit cost multiplier has been applied to all the cost centers receiving the services, the total cost (line 20, Part I) must equal the total cost on line 21, Part II.
Perform the preceding procedures for each general service cost center.
Rev. 2 40-235
4044 FORM CMS-2552-10 08-11
4044. WORKSHEET H-3 - APPORTIONMENT OF PATIENT SERVICE COSTS
This worksheet provides for the apportionment of home health patient service costs to titles V, XVIII, and XIX. Titles V and XIX use the columns identified as Part A for each program.
4044.1 Part I - Computation of the Aggregate Program Cost.--This part provides for the computation of the total cost and reasonable program cost by discipline based on program patient care visits as required by 42 CFR 413.20, 42 CFR 413.24 and 42 CFR 484.200. HHA services rendered on or after October 1, 2000, §1895 of the Social Security Act requires a home health agency to be paid based on a prospective payment system subject to periodic updates.
Cost Per Visit Computation
Column Descriptions
Column 1--Enter the cost for each discipline from Worksheet H-2, Part I, column 28, lines as indicated. Enter the total on line 7.
Column 2--Where the hospital complex maintains separate Physical Therapy, Occupational Therapy and/or Speech Pathology departments, and these departments provide services to patients of the hospital’s HHA, transfer the amounts from Worksheet H-3 Part II, column 3, lines 1 through 3 to lines 2 through 4 as appropriate. Enter the total on line 7.
Column 3--Enter the sum of columns 1 and 2.
Column 4--Enter the total agency visits from your records for each type of discipline on lines 1 through 6. Total visits reported in column 4 reflect visits rendered for the entire fiscal year and equal the visits reported on S-3, Part I, regardless of when the episode was completed.
Column 5--Compute the average cost per visit for each type of discipline. Divide the number of visits (column 4) into the cost (column 3) for each discipline.
Columns 6 and 9--To determine title XVIII, Part A, V, and XIX cost of service, multiply the number of Medicare covered visits in completed episodes made to beneficiaries (column 6) (from your records) by the average cost per visit amount in column 5 for each discipline. Enter the product in column 9.
NOTE: Statistics in column 7, lines 1 through 7, reflect statistics for services that are part of a home health plan, and thus not subject to deductibles and coinsurance. OBRA 1990 provides for the limited coverage of injectable drugs for osteoporosis. While covered as a home health benefit under Part B, these services are subject to deductibles and coinsurance. Report charges for osteoporosis injections in column 8, line 16, in addition to statistics for services that are not part of a home health plan.
Columns 7 and 10--To determine the Medicare Part B cost of service, not subject to deductibles and coinsurance, multiply the number of Medicare covered visits made in completed episodes to Part B beneficiaries (column 7) (from your records) by the average cost per visit amount in column 5 for each discipline. Enter the product in column 10. Note if the PS&R reports Part B services separately as "subject to and not subject to” deductibles and coinsurance, add the two reports together for each discipline.
Columns 6, 7, 9, 10 and 12--Enter visits and costs as applicable in columns 6, 7, 9, 10, and 12.
40-236 Rev. 2
10-12 FORM CMS-2552-10 4044.1 (Cont.)
NOTE: The sum of visits reported in columns 6 and 7 must equal the corresponding amounts on Worksheet S-4, column 5, lines 21, 23, 25, 27, 29 and 31, respectively. These visits are reported for episodes completed during the fiscal year.
Columns 8 and 11--Do not use these columns.
Column 12--Enter the total program cost for each discipline (sum of columns 9 and 10). Add the amounts on lines 1 through 6, and enter this total on line 7.
Visits by CBSA--Lines 8 through 14--HHAs are paid for home health services under Title XVIII on the basis of the geographic location at which the service is furnished. Enter for each discipline the CBSA code of the location where the home health service was furnished. Subscript each discipline line to accommodate multiple CBSAs serviced by your home health agency.
Column Descriptions
Column 1--Enter the CBSA code in which the corresponding HHA visits were rendered for each discipline on lines 8 through 13.
Columns 2 and 3--Enter the visit count for each of the corresponding disciplines for each CBSA.
Column 4, lines 8 through 14--These lines are shaded to prevent data input.
Line 14--Enter the total program visits for each discipline by adding lines 8 through 13 and subscripts, and enter this total on line 14.
Supplies and Drugs Cost Computation.--Certain services covered by the program and furnished by a home health agency are not included in the cost per visit for apportionment purposes. Since an average cost per visit and HHA PPS do not apply to these items, develop and apply the ratio of total cost to total charges to program charges to arrive at the program cost for these services.
Column 1--Enter the facility costs in column 1, lines 15 and 16, from Worksheet H-2, Part I, column 28, lines 8 and 9, respectively.
Column 2--Enter the shared ancillary costs from Worksheet H-3, Part II, column 3, lines 4 and 5, respectively.
Columns 3 through 5--In column 3, enter the sum total of columns 1 and 2 on lines 15 and 16, respectively. Enter in column 4, lines 15 and 16, respectively, the total charges for such services in accordance with the instructions in §4041, lines 12 and 13. Develop a ratio of total cost (column 3) to total charges (column 4) (from your records), and enter this ratio in column 5.
Columns 6 through 8--Enter in the appropriate column the program charges for drugs and medical supplies charged to patients subject to cost reimbursement. The actual vaccine/drug cost for pneumococcal, influenza, hepatitis B and osteoporosis are cost reimbursed.
Do not enter charges for drugs and medical supplies subject to reimbursement on the basis of a fee schedule.
Rev. 3 |
40-237 |
4044.2 FORM CMS-2552-10 10-12
Line Descriptions for Columns 6 through 8
Line 15--Columns 6 through 11 are shaded to prevent the input of medical supplies charged to patients as all medical supplies are covered under the HHA PPS benefit.
Line 16--This line represents pneumococcal, influenza, and hepatitis B vaccine costs and injectable osteoporosis drugs, but not the administration of these medications. Enter the program covered charges for drugs charged to patients for items not reimbursed on the basis of a fee schedule or OPPS. Enter in column 7 the program charges for pneumococcal vaccine and influenza vaccine exclusive of their respective administration costs. Enter in column 8 the program charges for hepatitis B vaccine and injectable osteoporosis drugs exclusive of their respective administration costs.
Columns 6 and 9--To determine the Medicare cost, multiply the program charges (column 6) by the ratio (column 5) for each line. Enter the product in column 9.
Columns 7 and 10--To determine the Medicare Part B cost, multiply the Medicare charges (column 7) by the ratio (column 5) for each line. Enter the product in column 10.
Columns 8 and 11--To determine the Medicare Part B cost, multiply the Medicare charges (column 8) by the ratio (column 5) for each line. Enter the result in column 11.
4044.2 Part II - Apportionment of Cost of HHA Services Furnished by Shared Hospital Departments.--Use this part only where the hospital complex maintains a separate department for any of the cost centers listed on lines 1 through 5 of this part of the worksheet, and these departments provide services to patients of the hospital's HHA. Subscript lines 1-5, as applicable, if subscripted on Worksheet C, Part I.
Column 1--Where applicable, enter in column 1 the cost to charge ratio from Worksheet C, Part I, column 9, lines as indicated.
Column 2--Where hospital departments provide services to the HHA, enter on the appropriate lines the charges applicable to the hospital-based home health agency.
Column 3--Multiply the amounts in column 2 by the ratios in column 1, and enter the result in column 3. Transfer the amounts in column 3 to Worksheet H-3, Part I as indicated. If lines 1-5 are subscripted, transfer the aggregate of each line.
40-238 Rev. 3
DRAFT FORM CMS-2552-10 4045.1
4045. WORKSHEET H-4 - CALCULATION OF HHA REIMBURSEMENT SETTLEMENT
This worksheet provides for the reimbursement calculation of titles V, XVIII Parts A and B, and XIX. This computation is required by 42 CFR 413.9, 42 CFR 413.13, and 42 CFR 413.30.
Worksheet H-4 consists of the following two parts:
Part I - Computation of the Lesser of Reasonable Cost or Customary Charges
Part II - Computation of HHA Reimbursement Settlement
4045.1 Part I - Computation of Lesser of Reasonable Cost or Customary Charges.--Services not paid based on a fee schedule or OPPS are paid the lesser of the reasonable cost of services furnished to beneficiaries or the customary charges made by the providers for the same services. This part provides for the computation of the lesser of reasonable cost or customary charges as defined in 42 CFR 413.13(a).
NOTE: Nominal charge providers are not subject to the lesser of cost or charges (LCC). Therefore, a nominal charge provider only completes lines 1, 2, and 9 of Part I. Transfer the resulting cost to line 10 of Part II.
Line Descriptions
Line 1--This line provides for the computation of reasonable cost reimbursed program services. Enter the cost of services from Worksheet H-3, Part I as follows:
To Worksheet H-4, Line 1 From Worksheet H-3,
Col. 1, Part A Part I, col. 9, line 16
Col. 2, Part B - Not subject to Part I, col. 10, line 16
deductibles and coinsurance
Col. 3, Part B - Subject to Part I, col. 11, line 16
deductibles and coinsurance
The above table reflects the transfer of the cost of pneumococcal and influenza vaccines from Worksheet H-3, Part I, column 10, line 16, to column 2 of this worksheet, and the cost of hepatitis B vaccines and injectable osteoporosis drugs from worksheet H-3, Part I, column 11, line 9 to column 3 of this worksheet.
Lines 2 through 6--These lines provide for the accumulation of charges which relate to the reasonable cost on line 1. Do not include on these lines (1) the portion of charges applicable to the excess costs of luxury items or services (see CMS Pub. 15-1, chapter 21, §2104.3) and (2) provider charges to beneficiaries for excess costs as described in CMS Pub. 15-1, chapter 25, §2570. When provider operating costs include amounts that flow from the provision of luxury items or services, such amounts are not allowable in computing reimbursable costs.
Enter only the charges for applicable Medicare covered pneumococcal, influenza and hepatitis B vaccines and injectable osteoporosis drugs which are all cost reimbursed.
Line 2--Enter from your records in the applicable column the program charges for Part A, Part B not subject to deductibles and coinsurance, and Part B subject to deductibles and coinsurance.
Rev. 40-239
4045.1 (Cont.) FORM CMS-2552-10 DRAFT
Enter in column 2 the charges for Medicare covered pneumococcal and influenza vaccines (from worksheet H-3, line 16, column 7). In column 3, enter the charges for Medicare covered hepatitis B vaccines and osteoporosis drugs (from worksheet H-3, line 16, column 8).
Lines 3 through 6--These lines provide for the reduction of program charges when the provider does not actually impose such charges (in the case of most patients liable for payment for services on a charge basis) or fails to make reasonable efforts to collect such charges from those patients. If line 5 is greater than zero, multiply line 2 by line 5, and enter the result on line 6. Providers which do impose these charges and make reasonable efforts to collect the charges from patients liable for payment for services on a charge basis are not required to complete lines 3, 4, and 5, but enter on line 6 the amount from line 2. (See 42 CFR 413.13(b).) In no instance may the customary charges on line 6 exceed the actual charges on line 2.
Line 7--Enter in each column the excess of total customary charges (line 6) over the total reasonable cost (line 1). In situations when, in any column, the total charges on line 6 are less than the total cost on line 1 of the applicable column, enter zero on line 7.
Line 8--Enter in each column the excess of total reasonable cost (line 1) over total customary charges (line 6). In situations when, in any column, the total cost on line 1 is less than the customary charges on line 6 of the applicable column, enter zero on line 8.
Line 9--Enter the amounts paid or payable by workers’ compensation and other primary payers where program liability is secondary to that of the primary payer. There are several situations under which program payment is secondary to a primary payer. Some of the most frequent situations in which the Medicare program is a secondary payer include:
Workers’ compensation,
No fault coverage,
General liability coverage,
Working aged provisions,
Disability provisions, and
Working ESRD beneficiary provisions.
Generally, when payment by the primary payer satisfies the total liability of the program beneficiary, for cost reporting purposes only, the services are considered to be nonprogram services. (The primary payment satisfies the beneficiary's liability when the provider accepts that payment as payment in full. The provider notes this on no-pay bills submitted in these situations.) The patient visits and charges are included in total patient visits and charges, but are not included in program patient visits and charges. In this situation, no primary payer payment is entered on line 9.
However, when the payment by the primary payer does not satisfy the beneficiary's obligation, the program pays the lesser of (a) the amount it otherwise pays (without regard to the primary payer payment or deductible and coinsurance) less the primary payer payment, or (b) the amount it otherwise pays (without regard to primary payer payment or deductibles and coinsurance) less applicable deductible and coinsurance. Primary payer payment is credited toward the beneficiary's deductible and coinsurance obligation.
When the primary payer payment does not satisfy the beneficiary's liability, include the covered days and charges in both program visits and charges and total visits and charges for cost apportionment purposes. Enter the primary payer payment on line 9 to the extent that primary payer payment is not credited toward the beneficiary's deductible and coinsurance. Do not enter on line 9 the primary payer payments that are credited toward the beneficiary's deductible and coinsurance. The primary payer rules are more fully explained in 42 CFR 411.
40-240 Rev.
DRAFT FORM CMS-2552-10 4045.2
4045.2 Part II - Computation of HHA Reimbursement Settlement.--
Line 10--Enter in column 1 the amount in Part I, column 1, line 1, less the amount in column 1, line 9. Enter in column 2 the sum of the amounts from Part I, columns 2 and 3, line 1, less the sum of the amounts in columns 2 and 3 on line 9. This line will only include pneumococcal, influenza, hepatitis B and injectable osteoporosis drugs reduced by primary payor amounts.
Lines 11 through 24--Enter in column 1 only for lines 11 through 14, as applicable, the appropriate PPS reimbursement amount for each episode of care payment category as indicated on the worksheet. Enter in column 1 only on lines 15 and 16, as applicable, the appropriate PPS outlier reimbursement amount for each episode of care payment category as indicated on the worksheet. Enter on lines 18 through 20 the total DME, oxygen, prosthetics and orthotics payments, respectively, associated with home health PPS services (bill types 32 and 33). For lines 18 through 20 do not include any payments associated with services paid under bill type 34X. Obtain these amounts from your PS&R report.
Line 21--Enter in column 2 the Part B deductibles billed to program patients. Include any amounts of deductibles satisfied by primary payer payments.
Line 23--If there is an excess of reasonable cost over customary charges in any column on line 8, enter the amount of the excess in the appropriate column.
Line 25--Enter in column 2 all coinsurance billable to program beneficiaries including amounts satisfied by primary payer payments. Coinsurance is applicable for services reimbursable under §1832(a)(2) of the Act.
NOTE: If the component qualifies as a nominal charge provider, enter 20 percent of the costs subject to coinsurance on this line. Compute this amount by subtracting Part B deductibles on line 21 and primary payment amounts in column 3, line 9 from Part B costs subject to coinsurance in column 3, line 1. Multiply the resulting amount by 20 percent and enter it on this line.
Line 27--Enter the allowable bad debts in the appropriate columns. If recoveries exceed the current year’s bad debts, line 27 will be negative. This line is shaded as HHAs cannot generate bad debts.
Line 28--Enter the gross allowable bad debts for dual eligible beneficiaries. This amount is reported for statistical purposes only. This amount must also be reported on line 27. This line is shaded as HHAs cannot generate bad debts.
Line 29--Enter the result of line 26 plus 27.
Line 30--Enter any other adjustments. For example, enter an adjustment from changing the recording of vacation pay from the cash basis to accrual basis. (See CMS Pub. 15-1, chapter 21, §2146.4.)
Line 31--Enter the result of line 29 plus or minus line 30.
Line 31.01--Enter the sequestration adjustment amount from the PS&R report.
Line 32--Enter the interim payment amount from Worksheet H-5, line 4. For contractor final settlement, report on line 33 the amount from Worksheet H-5, line 5.99. For titles V and XIX, enter the interim payments from your records.
Rev. 40-241
4045.2 (Cont.) FORM CMS-2552-10 DRAFT
Line 34--The amounts show the balance due the provider or the program by entering the result of line 31 minus the sum of lines 31.01, 32, and 33. Transfer to Worksheet S, Part III, line 9, as applicable.
Line 35--Enter the program reimbursement effect of protested items. The reimbursement effect of the nonallowable items is estimated by applying a reasonable methodology which closely approximates the actual effect of the item as if it had been determined through the normal cost finding process. (See CMS Pub. 15-2, chapter 1, §115.2.) A schedule showing the supporting details and computations for this line must be attached.
4046. WORKSHEET H-5 - ANALYSIS OF PAYMENTS TO HOSPITAL-BASED HOME HEALTH AGENCIES FOR SERVICES RENDERED TO PROGRAM BENEFICIARIES
Complete this worksheet for Medicare interim payments only. (See 42 CFR 413.64.)
The column headings designate two categories of payments: Part A and Part B.
Complete the identifying information on lines 1 through 4. The remainder of the worksheet is completed by your contractor. Do not include on this worksheet any payments made for DME or medical supplies charged to patients that are paid on the basis of a fee schedule.
Line Descriptions
Line 1--Enter the total Medicare interim payments paid to the HHA for cost and HHA PPS reimbursed services. The amount entered reflects payments for all episodes concluded in this fiscal year. Do not include any payments received for fee scheduled services. The amount entered reflects the sum of all interim payments paid on individual bills (net of adjustment bills) for services rendered in this cost reporting period. The amount entered includes amounts withheld from your interim payments due to an offset against overpayments applicable to prior cost reporting periods. It does not include any retroactive lump sum adjustment amounts based on a subsequent revision of the interim rate, or tentative or net settlement amounts, nor does it include interim payments payable. If you are reimbursed under the periodic interim payment method of reimbursement, enter the periodic interim payments received for this cost reporting period.
Line 2--Enter the total Medicare interim payments payable on individual bills. Since the cost in the cost report is on an accrual basis, this line represents the amount of services rendered in the cost reporting period, but not paid as of the end of the cost reporting period, and does not include payments reported on line 1.
Line 3--Enter the amount of each retroactive lump sum adjustment and the applicable date.
Line 4--Enter the total amount of the interim payments (sum of lines 1, 2, and 3.99). Transfer these totals to the appropriate column on Worksheet H-4, Part II, line 32.
40-242 |
Rev. |
09-14 FORM CMS-2552-10 4046 (Cont.)
DO NOT COMPLETE THE REMAINDER OF WORKSHEET H-5. THE REMAINDER OF THE WORKSHEET IS COMPLETED BY YOUR CONTRACTOR. (EXCEPTION: IF WORKSHEET S, PART I, LINE 5 IS “5” (AMENDED COST REPORT), THE PROVIDER MAY COMPLETE THIS SECTION.)
Line 5--List separately each tentative settlement payment after desk review together with the date of payment. If the cost report is reopened after the NPR has been issued, report all settlement payments prior to the current reopening settlement on line 5.
Line 6--Enter the net settlement amount (balance due to the provider or balance due to the program) for the NPR, or, if this settlement is after a reopening of the NPR, for this reopening. Enter in column 2 the amount on Worksheet H-4, Part II, column 1, line 34. Enter in column 4 the amount on Worksheet H-4, Part II, column 2, line 34.
NOTE: On lines 3, 5, and 6, when an amount is due from the provider to the program, show the amount and date on which you agree to the amount of repayment, even though total repayment is not accomplished until a later date.
Line 7--Enter the total of the amounts on lines 4, 5.99, and 6. Enter in column 2 the amount on Worksheet H-4, Part II, column 1, line 31 less the amount on line 31.01. Enter in column 4 the amount on Worksheet H-4, Part II, column 2, line 31 less the amount on line 31.01.
Line 8--Enter the contractor name, the contractor number and NPR date in columns 0, 1 and 2, respectively.
Rev. 6 40-243
4047 FORM CMS-2552-10 09-14
4047. ANALYSIS OF RENAL DIALYSIS DEPARTMENT COSTS
This worksheet provides for the analysis of the direct and indirect expenses related to the renal dialysis cost centers, allocation of cost between inpatient and outpatient renal dialysis services where separate cost centers are not maintained, and the allocation of the cost to the various modes of outpatient dialysis treatment. The ancillary renal dialysis cost center is serviced by the general cost centers and includes all reimbursable cost centers within the provider organization which provide services to the renal dialysis department. The cost used in the analysis for the renal dialysis department is obtained, in part, from Worksheets A; B, Part I; and C. Complete a separate Worksheet I series for lines 74 and 94 of Worksheet A. In other words, complete one Worksheet I series for line 74 and one for line 94, if appropriate.
4048. WORKSHEET I-1 - ANALYSIS OF RENAL DIALYSIS DEPARTMENT COSTS
This part provides for recording the direct salaries and other direct expenses applicable to the total inpatient and outpatient renal dialysis cost center or outpatient renal dialysis cost center where you maintain a separate and distinct outpatient renal dialysis cost center. If you have more than one renal dialysis department, and/or more than one home dialysis department, submit one Worksheet I series combining the renal dialysis departments and a separate Worksheet I series combining the home dialysis departments. You must also have on file, as supporting documentation, a Worksheet I series for each renal dialysis department and for each home dialysis department along with the appropriate workpapers. File this documentation with exception requests in accordance with CMS Pub. 15-1, chapter 27, §2720. Do not combine the cost of the renal dialysis with home program dialysis reported separately on Worksheet A, lines 74 and 94.
This worksheet also provides for recording the indirect expenses applicable to the total renal or outpatient renal dialysis department obtained from Worksheet B, Part I, columns 1 through 23, line 74 as adjusted for post stepdown adjustments, if any. When completing a separate Worksheet I for home program dialysis, transfer the direct expenses from Worksheet B, Part I, columns 1 through 23, line 94. Do not combine the cost of the renal department with home program dialysis. These costs are listed separately on Worksheet A, lines 74 and 94, respectively.
Column Descriptions
Column 1--Enter on lines 1 through 8 the amounts included from Worksheet A, column 7 for salaries only. Enter on lines 10 through 16 and 18 through 26 the amounts from Worksheet B, Part I, all columns for lines 74 and 94. The subtotal on Worksheet I-1, line 27 agrees with the sum of Worksheet B, Part I, column 26, line 74 or line 94 if a home dialysis cost center was established and used on Worksheet A.
Column 2--This column lists the statistical bases for allocating costs on Worksheet I-3.
Column 3--Enter paid hours per type of staff listed on lines 1 through 6.
Column 4--Enter full time equivalents by dividing column 3 by 2080 hours.
Line Descriptions
Lines 1 through 6--Enter on these lines the direct patients care salaries after adjustments and reclassification that you reported in column 7 of Worksheet A. Direct patient care salary includes only the salary of staff providing direct patient care services. Also include fee paid to non-employees providing direct patient care services. Time spent furnishing administrative or management services by direct patient care personnel is reported on line 8, non-patient care salary.
40-244 Rev. 6
DRAFT FORM CMS-2552-10 4048 (Cont.)
Line 7--Include on this line amounts paid to physicians for their administrative services of managing the renal department. These payments are subject to the limitation contained in CMS Pub. 15-1, chapter 27, §2723.3. Also include payments to physicians for their medical services if the box on line 21 of Worksheet S-5 is marked the initial method. A complete description of the initial method is in CMS Pub. 15-1, chapter 27, §2715. For a renal provider to be paid under the initial method, all renal physicians at the provider must elect the initial method. Under the initial method, renal physicians are paid by the provider for their routine renal medical services and the provider's composite payment rate is increased according to 42 CFR 414.313. No payment to physicians for patient medical services should appear on this line if the monthly capitation payment (MCP) box is marked on Worksheet S-5. Under the MCP, contractors pay physicians directly for their medical services.
Line 8--Enter the amount of salaries paid non-patient care personnel after reclassifications and adjustments that you report in column 7 of Worksheet A.
Lines 10 through 16--Include on the appropriate lines costs directly charged to the renal department after reclassifications and adjustments. Report other direct costs on line 16 that cannot be specifically identified on lines 11 through 15.
Lines 17--Add lines 9 through 16. The total in column 1 must agree with the total on Worksheet A, column 7 for line 74 or line 94, as appropriate.
Lines 18 through 26--Enter the allocated general service costs from Worksheet B, Part I, lines 74 or 94 as listed in the chart below.
NOTE: Line 25 should exclude the costs of EPO and Aranesp administered to ESRD patients in the renal department and home program identified on Worksheet B-2, lines 1, 2, 3 or 4.
Worksheet I-1, Worksheet B,
Part I, Column 1, Part I, Lines 74
Line Number General Service Cost Centers or 94, Columns
18 Capital-Related Costs- 1
Buildings and Fixtures
19 Capital-Related Costs- 2
Moveable Equipment
20 Employee Benefits 4
21 Administrative and General 5
22 Maintenance & Repairs, Operation Sum of 6, 7,
of Plant and Housekeeping and 9
23 Medical Education Programs Sum of 20, 21, 22,
23, and 25 (medical
education only)
Rev. 40-245
4048 (Cont.) FORM CMS-2552-10 DRAFT
24 Central Services & Supplies 14
25 Pharmacy 15
26 Other Allocated Costs Sum of 8, 10,
11, 12, 13, 16,
17, 18, and 19
Line 27--Add lines 18 through 26. This total must agree with the total on Worksheet B, column 26, line 74 or line 94 if a home dialysis cost center was established, less the adjustments for EPO and Aranesp reported on Worksheet B-2, lines 1, 2, 3, or 4 as appropriate.
Lines 28, 29, and 30--These lines provide for the allocation of costs associated with routine dialysis services furnished to renal patients from other ancillary departments. Enter the cost to charge ratio from Worksheet C, Part I, column 9. Payment for routine laboratory services, as defined in the CMS Pub. 100-02, chapter 11, §30.2, is paid for under the composite payment rate. No separate payment is made for routine laboratory tests. The costs of these services are allocated to the renal department based on the provider’s laboratory cost to charge ratio from Worksheet C, Part I, column 9, line 60. Providers must maintain a log of routine laboratory charges for allocating routine laboratory costs to the renal department. The lab charges reported on Worksheet C do not include the lab charges for ESRD therefore those charges must be grossed up in accordance with CMS Pub. 15-1, chapter 23, §2314. The cost to charge ratio must be recalculated and applied against the charges reported in column 3 of this worksheet. Do not gross up ESRD charges. Instead, the cost to charge ratio for lab charges reported on Worksheet C will be used.
Line 31--Enter the sum lines 27 through 30.
40-246 Rev.
08-11 FORM CMS-2552-10 4049
4049. WORKSHEET I-2 - ALLOCATION OF RENAL DEPARTMENT COSTS TO TREATMENT MODALITIES
The purpose of this schedule is to allocate costs to the different services furnished in the renal department. Line 1 combines the costs reported on Worksheet I-1 for allocating costs to the different services furnished in the renal department.
Line 1--Add the costs from Worksheet I-1, and transfer these amounts to line 1 in the following manner:
Worksheet I-2 Worksheet I-2 Column Worksheet I-1
Capital & Main Building Costs 1 Sum of lines 11, 18, and 22
Capital, Machine & Repair Costs 2 Sum of lines 12, 13, and 19
Registered Nurses Direct Patient Care 3 Line 1
Salary
Other Direct Patient Care Salary 4 Sum of lines 2, 3, 4, 5, and 6
Employee Benefits 5 Sum of lines 10 and 20
Drugs 6 Sum of lines 15 and 25
Medical Supplies 7 Sum of lines 14 and 24
Routine Ancillary Services 8 Sum of lines 28, 29, and 30
Subtotal 9 Not applicable
Overhead 10 Sum of lines 7, 8, 16, 21, and 26
Complete columns 1 through 8 and 10 in conjunction with Worksheet I-3, which contains the statistical bases for allocating costs to the proper lines. For each line item in columns 1 through 8 and 10, multiply the statistic entered in the corresponding line and column of Worksheet I-3 by the unit cost multiplier on line 18.
Lines 2 through 11--These lines identify the type of dialysis treatments that are paid for under the composite payment rate system. The total costs (column 11) for these individual dialysis services are transferred to Worksheet I-4.
Transfer the total on Worksheet I-2, column 11 to Worksheet I-4 per the following instructions.
From Worksheet I-2, Column 11 To Worksheet I-4, Column 2
Line 2 Line 1
Line 3 Line 2
Line 4 Line 3
Line 5 Line 4
Line 6 Line 5
Line 7 Line 6
Line 8 Line 7
Line 9 Line 8
Line 10 Line 9
Line 11 Line 10
Rev. 2 40-247
4049 (Cont.) FORM CMS-2552-10 08-11
If you complete a Worksheet I-2 for the renal department and the home program dialysis department, complete a separate Worksheet I-4.
Lines 12 through 16--These services are not paid for under the composite payment rate system. Therefore, the costs of these services are not transferred to Worksheet I-4. Exclude these costs in the calculation of reimbursement composite payment rate bad debts. (See 42 CFR 413.178(d).)
Line 12.--Report inpatient costs. Inpatient dialysis services are paid under the DRG system for Medicare patients.
Line 13.--Report the costs of support services furnished to Method II home patients. Payment for Method II home patient dialysis services are subject to the rules in 42 CFR 414.330. Under Method II, a renal provider is only allowed to bill for support services and not dialysis equipment or supplies. Payment for support services is limited to the lower of the provider’s reasonable cost or the payment limit as defined in the regulation, which is $121.15 per patient per month. This amount includes payment for support services and routine laboratory tests furnished to home patients.
Line 14.--Report the direct costs of EPO net of discounts furnished in the renal department. Include all costs for patients receiving outpatient, home, or training dialysis treatments. This amount includes EPO cost furnished in the renal department or any other department if furnished to an end stage renal dialysis patient. Enter EPO amount for informational purposes only. This amount is not included in the total on line 17.
Line 15.--Report the direct costs of Aranesp net of discounts furnished in the renal department. Include all costs for patients receiving outpatient, home, or training dialysis treatments. This amount includes Aranesp cost furnished in the renal department or any other department if furnished to an end stage renal dialysis patient. Enter Aranesp amount for informational purposes only. This amount is not included in the total on line 17.
Line 16.--Report the costs of other services furnished and billed in the renal department that are paid for outside the composite payment rate.
Line 17--Add columns and enter totals. Since lines 14 and 15, column 9 are shaded, no costs for EPO and Aranesp are included in the total for line 17, column 9 and column 6, lines 14 and 15 should be excluded from total.
Line 18--Enter the amount of medical educational program costs from Worksheet I-1, line 23. Payment for medical educational program costs allocated to the renal department is not included in the composite payment rate.
Line 19--Add lines 17 and 18. This total agrees with the sum of Worksheet I-1, column 1, line 31.
Column Description
Columns 1 through 8--For each line, multiply the unit cost multiplier on Worksheet I-3, line 18 by the statistical base, and enter the result on the corresponding line and column on Worksheet I-2.
Column 9--Add columns 1 through 8 for each line, except lines 14 (EPO) and 15 (Aranesp), and enter the total.
Column 10--Multiply the unit cost multiplier on Worksheet I-3, column 10, line 18 by the line amounts in column 9 of Worksheet I-2, and enter the amount in column 10.
Column 11--Add columns 9 and 10 for each line, and enter the result.
40-248 Rev. 2
DRAFT FORM CMS-2552-10 4050
4050. WORKSHEET I-3 - DIRECT AND INDIRECT RENAL DIALYSIS COST ALLOCATION - STATISTICAL BASIS
To accomplish the allocation of your direct and indirect costs reported on Worksheet I-1 to the different services provided in the department, you must maintain renal department statistics. To facilitate the allocation process, the format of Worksheets I-2 and I-3 is identical.
Line 1--Transfer the amounts on Worksheet I-2, line 1, columns 1 through 10 to Worksheet I-3, line 1, columns 1 through 10.
Lines 2 through 16--Enter on these lines and in the appropriate columns, the statistic for allocating costs to the appropriate line item. The statistical basis used in each column is defined in the column heading and on Worksheet I-1.
NOTE: If you wish to change your allocation basis for a particular general cost center, you must receive written approval from your contractor before the start of your cost reporting period for which the alternative method is used. (See §4017 for Worksheets B and B-1.)
Line 12--Enter, in the area provided, the number of inpatient dialysis treatments furnished during the cost reporting period.
Line 17--Add the statistical basis for each column, except columns 9 and 10.
Line 18--Calculate the unit cost multiplier by dividing the amount on line 1 by the total statistical basis on line 17 for each column. Multiply the unit cost multiplier by the statistical base, and enter the cost on the appropriate line and column number on Worksheet I-2.
Column Descriptions
Column 1--Use the square footage of the renal department to allocate capital and maintenance building costs.
Column 2--Use percentage of time to allocate capital and maintenance equipment costs.
Columns 3 and 4--Use paid hours to allocate registered nurses and direct patient care salary.
Column 5--Use total direct patient care salaries in columns 4 and 5 of Worksheet I-2 to allocate employee benefits.
Columns 6 and 7--Use cost of requisitions to allocate drug and medical supply costs.
Column 8--Use routine laboratory charges to allocate laboratory costs.
Column 10--Use subtotal costs in column 9, Worksheet I-2 to allocate overhead cost. To compute the unit cost multiplier, transfer the amount from Worksheet I-2, line 17, column 9, to Worksheet I-3, line 17, column 10. Do not allocate overhead costs to lines 14 (EPO) or 15 (Aranesp).
Rev. 40-249
4051 FORM CMS-2552-10 DRAFT
4051. WORKSHEET I-4 - COMPUTATION OF AVERAGE COST PER TREATMENT FOR OUTPATIENT RENAL DIALYSIS
This worksheet records the apportionment of total outpatient cost to the types of dialysis treatment furnished by you and shows the computation of expenses of dialysis items and services that you furnished to Medicare dialysis patients. This information is used for overall program evaluation, determining the appropriateness of program reimbursement rates, and meeting statutory requirements for determining the cost of ESRD care.
Complete separate worksheets to report the costs of the renal dialysis department and the home program dialysis department. For cost reporting periods ending on or after June 30, 2015, if you have more than one renal dialysis department or home dialysis department and you are eligible for the low volume payment adjustment (Worksheet S-5, line 10.01, is yes), complete a separate Worksheet I-4, column 1, for each renal dialysis or home dialysis department.
If you have more than one renal dialysis and/or home dialysis department, submit one Worksheet I-4 combining the renal dialysis departments and/or one Worksheet I-4 combining the home dialysis departments as only one average payment rate will apply to each modality. Enter on the combined Worksheet I-4 each provider’s satellite number if you are separately certified as a satellite facility.
In accordance with section 1881(b)(12)(A) of the Act, as added by section 623(d)(1) of MMA 2003, the ESRD payment is replaced by a calculated ESRD composite rate. Section 153(b) of MIPPA amended section 1881(b) of the Act effective for services rendered on or after January 1, 2011, the calculated ESRD composite rate is replaced by an ESRD bundled payment system.
For cost reporting periods that straddle January 1, 2011, report the rates for each modality on Worksheet I-4 as follows: For the portion of the cost reporting period prior to January 1, 2011, enter the average composite rate for each modality in column 7. For the portion of the cost reporting period on and after January 1, 2011, enter the average ESRD PPS payment rate for each modality in column 7.02. For cost reporting periods that straddle January 1, 2012, January 1, 2013, and January 1, 2014, report the average ESRD PPS payment rate for each modality on Worksheet I-4 as follows: For the portion of the cost reporting period prior to January 1, enter the average ESRD PPS payment rate for each modality in column 7.01. For the portion of the cost reporting period on and after January 1, enter the average ESRD PPS payment rate for each modality in column 7.02.
Columns 1 through 3 refer to total outpatient statistics, i.e., to all outpatient dialysis services furnished, whether reimbursed directly by the program or not.
Column 1--Enter on the appropriate lines the total number of outpatient treatments by renal dialysis department or home program department. These statistics include all treatments furnished to all patients in the outpatient renal department, both Medicare and non-Medicare. For cost reporting periods ending on or after June 30, 2015, if Worksheet S-5, line 10.01, is yes and you have more than one renal dialysis or home program department, complete a separate Worksheet I-4 for each individual provider/department number. Combine the separate Worksheet I-4, column 1, data for all renal dialysis departments and home program dialysis departments on their respective summary Worksheet I-4.
Column 2--Enter on the appropriate lines the total cost transferred from Worksheet I-2, columns 11, lines as appropriate.
Column 3--Determine the amounts entered on the appropriate lines by dividing the cost entered on each line in column 2 by the number of treatments entered on each line in column 1.
40-250 Rev.
DRAFT FORM CMS-2552-10 4051 (Cont.)
Line 9--Report continuous ambulatory peritoneal dialysis (CAPD) in terms of weeks. Compute patient weeks by totaling the number of weeks each Method I patient was dialyzed at home using CAPD.
Line 10--Report continuous cycling peritoneal dialysis (CCPD) in terms of weeks. Compute patient weeks by totaling the number of weeks each Method I patient was dialyzed at home by CCPD.
Medicare Treatments
Columns 4 through 7 refer only to treatments furnished to Medicare beneficiaries that were billed to the facility and reimbursed by the program directly. (Amounts entered in these columns are reconcilable to your records.)
Column 4--Enter on the appropriate lines the number of treatments billed to the Medicare program directly. Obtain this information from your records and/or the PS&R. For cost reporting periods that straddle January 1, 2011, enter on column 4 the total number of treatments or patient weeks billed to Medicare for services rendered prior to January 1, 2011.
Column 4.01--For cost reporting periods that straddle January 1, 2012, January 1, 2013 or January 1, 2014, enter the total number of treatments or patient weeks billed to Medicare for services rendered prior to January 1.
Column 4.02--For cost reporting periods that straddle or begin January 1, 2011, January 1, 2012, or January 1, 2013, enter the total number of treatments or patient weeks billed to Medicare for services rendered on and after January 1. For cost reporting periods that straddle January 1, 2014, enter the total number of treatments or patient weeks billed to Medicare for services rendered on and after January 1.
For cost reporting periods beginning on or after January 1, 2014, enter the number of ESRD PPS treatments billed to Medicare in column 4 and eliminate columns 4.01 and 4.02.
Column 5--Determine the amounts entered on the appropriate lines by multiplying the number of treatments entered on each line in column 4 by the average cost per treatment entered on the corresponding line in column 3. For cost reporting periods that straddle or begin on or after January 1, 2011, enter total expenses determined by multiplying the sum of columns 4, 4.01, and 4.02 by the average cost per treatment entered on each corresponding line in column 3. Transfer the total expenses from this column, line 11 to Worksheet I-5, line 1. If you complete a Worksheet I-4 for renal dialysis and a Worksheet I-4 for home dialysis, add the sum of the cost from this column, line 11, and transfer the total to Worksheet I-5, line 1.
Column 6--Total Program Payment--Enter the total program payment by the type of treatment for the reporting period. Since this amount is calculated on a patient basis and is case mix adjusted, the total program payment will be provider specific for each modality. For cost reporting periods that straddle January 1, 2011, enter in column 6 the total program payment by the type of treatment for services rendered prior to January 1, 2011. For cost reporting periods beginning on or after January 1, 2014, enter the total program payment by the type of treatment. Obtain this from the PS&R. Transfer the total from column 6, line 11, to Worksheet I-5, line 2, column 1.
Column 6.01--For cost reporting periods that straddle January 1, 2012, January 1, 2013 or January 1, 2014, enter the total program payment by the type of treatment for Medicare for services rendered prior to January 1. Obtain this from the PS&R. Transfer the total from column 6.01, line 11, to Worksheet I-5, line 2.01, column 1.
Rev. 40-251
4051 (Cont.) FORM CMS-2552-10 DRAFT
Column 6.02--For cost reporting periods that straddle or begin January 1, 2011, January 1, 2012, or January 1, 2013, enter the total program payment by the type of treatment for Medicare for services rendered on and after January 1. For cost reporting periods that straddle January 1, 2014, enter the total program payment by the type of treatment for services rendered on and after January 1. Obtain this from the PS&R. Transfer the total from column 6.02, line 11, to Worksheet I-5, line 2.02, column 1.
For cost reporting periods beginning on or after January 1, 2014, enter the total program payment by the type of treatment in column 6 and eliminate columns 6.01 and 6.02.
The ESRD Medicare payment rate is an average payment calculated based on the total Medicare payments by type of treatment divided by the total ESRD Medicare treatments.
Column 7--Average Payment Rate--For cost reporting periods that straddle January 1, 2011, for the portion of the cost reporting period prior to January 1, 2011, enter the total average payment rate by the type of treatment for the reporting period. Determine the amounts entered on the appropriate lines by dividing the total payments on each corresponding line in column 6 by the number of treatments entered on each line in column 4.
Column 7.01--For cost reporting periods that straddle January 1, 2012, January 1, 2013, or January 1, 2014, report the average ESRD PPS payment rate for each modality in column 7.01 for the portion of the cost reporting period prior to January 1 by entering the result of column 6.01 divided by column 4.01.
Column 7.02--For cost reporting periods that straddle or begin January 1, 2011, January 1, 2012, or January 1, 2013, report the average ESRD PPS payment rate for each modality in column 7.02 for the portion of the cost reporting period on and after January 1 by entering the result of column 6.02 divided by column 4.02. For cost reporting periods that straddle January 1, 2014 report the average ESRD PPS payment rate for each modality in column 7.02 for the portion of the cost reporting period on and after January 1.
The ESRD composite payment rates and the ESRD PPS payment rates are average payments calculated based on the total Medicare payments (by type of treatment) divided by the total corresponding ESRD treatments per the facility’s PS&R data. For example, the total Medicare payment for hemodialysis is divided by the total ESRD hemodialysis treatments.
For cost reporting periods beginning on or after January 1, 2014, enter all ESRD PPS payment rates in column 7, and eliminate columns 7.01 and 7.02 and.
Line 11--Enter in columns 1 and 4 the sum total of lines 1 through 8. Enter in columns 2, 5, and 6 the sum total of lines 1 through 10.
Line 12--Report “total provider treatments” on this line. This line is informational only. This line will be used for contractor verification. Continuous cycling peritoneal dialysis (CCPD) and continuous ambulatory peritoneal dialysis (CAPD) are daily treatment modalities, and ESRD facilities are paid the equivalent of three hemodialysis treatments for each week that CCPD and CAPD treatments are provided.
Compute hemodialysis equivalent treatments for lines 9 and 10 by multiplying the number of weeks reported in column 1 times 3 treatments for each week. Add to this amount the treatments computed on line 11, column 1.
40-251.1 Rev.
DRAFT FORM CMS-2552-10 4052
4052. WORKSHEET I-5 - CALCULATION OF REIMBURSABLE BAD DEBTS - TITLE XVIII - PART B
This worksheet provides for the calculation of reimbursable Part B bad debts relating to outpatient renal dialysis treatments. If you have completed more than one Worksheet I-2 (i.e., one for renal dialysis department and one for home program dialysis), make a consolidated bad debt computation.
Part I - Calculation of Reimbursable Bad Debts Title XVIII – Part B.--Under the composite rate payment system for services prior to January 1, 2011, the contractor pays the facility its allowable ESRD bad debts, up to the facility’s unreimbursed reasonable costs as determined under Medicare principles. Under the ESRD PPS payment system, effective for dates of service on and after January 1, 2011, the contractor pays the facility for allowable ESRD bad debts, up to the facility’s unreimbursed reasonable costs for those items and services associated with the basic case-mix adjusted composite rate portion of the ESRD PPS payment rate. Allowable bad debts must relate to specific Medicare deductibles and coinsurance amounts.
Determination of bad debt amounts for the basic case-mix adjusted composite rate payment portion of the ESRD PPS payment, is based on the percentage of basic composite rate payment costs to total costs on a facility specific basis. The facility specific composite rate percentage is applied to the facility’s total bad debt amounts associated with the ESRD PPS payment. The resulting bad debt amount is used to determine the allowable Medicare bad debt payment in accordance with 42 CFR 413.89 and 42 CFR 413.178 of the regulations. During the transition periods, apply the facility specific composite cost percentage to the bad debt amounts associated with the transition portion of the ESRD PPS payment.
The resulting bad debt amount will be added to the bad debt amount associated with the transition portion of the facility’s ESRD reasonable costs to determine the total allowable Medicare bad debt (For example, a facility that does not elect 100 percent PPS, will be in transition period 1 for services rendered beginning January 1, 2011 through December 31, 2011. Under transition period 1, services rendered during this period are paid based on 75 percent composite rate and 25 percent ESRD PPS payment rate. The facility specific composite cost percentage will be applied to 25 percent of the bad debts and the resulting bad debt amount will be added to the transitional 75 percent to determine the total allowable bad debt pertaining to services rendered during this period).


 EXCEPTION:
The transition period payment
method will not apply to ESRD services rendered on and after January
1, 2011, by a facility that (1)
elected 100 percent of the payment
amount to be based on the ESRD PPS Payment, or (2)
was certified for Medicare
participation and began providing dialysis services on or after
January 1, 2011.
EXCEPTION:
The transition period payment
method will not apply to ESRD services rendered on and after January
1, 2011, by a facility that (1)
elected 100 percent of the payment
amount to be based on the ESRD PPS Payment, or (2)
was certified for Medicare
participation and began providing dialysis services on or after
January 1, 2011.
Column 1--Enter the total amounts by line description.
Column 2--This column is used to compute the appropriate reduction to each amount reported in column 1, based on the facility’s transition period and application of their facility specific composite cost ratio.
Line 1--Enter the amount from Worksheet I-4, column 5, line 11. The amount reported is reflective of the provider’s calculated basic composite rate payment cost. If you complete more than one Worksheet I-4 summary (one for renal dialysis department and one for home program dialysis department), enter the sum of the two summary Worksheets I-4, column 5, line 11.
Line 2--Enter the amount from Worksheet I-4, column 6, line 11. For cost reporting periods that overlap January 1, 2011, enter in column 1 the amount from Worksheet I-4, column 6, line 11. Enter in column 2, the amount reported in column 1. For cost reporting periods beginning on or after January 1, 2014, enter in column 1, the sum of the amount from Worksheet I-4, column 6,
Rev. 40-251.2
4052 (Cont.) FORM CMS-2552-10 DRAFT
line 11. If you complete more than one Worksheet I-4 summary, (one for renal dialysis department and one for home program dialysis department), enter the sum of the two summary Worksheets I-4, column 6, line 11.
Enter in column 2 the amount reported in column 1 times the facility specific composite cost ratio from, line 14. For cost reporting periods beginning on or after January 1, 2014, do not complete lines 2.01 and 2.02.
Line 2.01--Enter in column 1 the sum of the amount from Worksheet I-4, column 6, line 11. Enter in column 2 the portion of the amount reported in column 1 as it relates to the ESRD PPS payment times the facility specific composite cost ratio from line 14. Add to this amount the composite cost portion of the payment. For cost reporting periods beginning on or after January 1, 2014, do not complete this line.
Line 2.02--Enter in column 1 the sum of the amount from Worksheet I-4, column 6, line 11. Enter in column 2 the portion of the amount reported in column 1 as it relates to the ESRD PPS payment times the facility specific composite cost ratio from line 14. Add to this amount the composite cost portion of the payment. For cost reporting periods beginning on or after January 1, 2014, do not complete this line.
Line 2.03--Enter the sum of lines 2, 2.01 and 2.02 in columns 1 and 2 accordingly.
Line 2.04--Enter the amount for outlier payments applicable to Medicare (Part B) patients from your records. (Informational only)
Line 3--Enter the amount shown in your records for deductibles billed to Medicare (Part B) for dialysis treatments. For cost reporting periods that overlap January 1, 2011, enter in column 1 the amount shown in your records for deductibles billed to Medicare (Part B) patients for dialysis treatments. Include only deductibles amounts that are related to the payments listed on line 2, column 1, and apply to Medicare beneficiaries under the composite payment rate. Enter in column 2 the amount reported in column 1. For cost reporting periods beginning on or after January 1, 2014, enter in column 1 the amount shown in your records for deductibles billed to Medicare (Part B) patients. Enter in column 2 the amount reported in column 1 times the facility specific composite cost ratio from line 14.
For cost reporting periods beginning on or after January 1, 2014, do not complete lines 3.01 and 3.02.
Line 3.01--Enter in column 1 the amount shown in your records for deductibles billed to Medicare (Part B) patients. Include only deductible amounts that are related to the payments listed on line 2.01, column 1, and apply to Medicare beneficiaries under the ESRD PPS payment rate. Enter in column 2 the portion of the amount reported in column 1, as it relates to the ESRD PPS payment times the facility specific composite cost ratio from line 14. Add to this amount the composite cost portion of the payment.
Line 3.02--Enter in column 1 the amount shown in your records for deductibles billed to Medicare (Part B) patients. Include only deductible amounts that are related to the payments listed on line 2.02, column 1, and apply to Medicare beneficiaries under the ESRD PPS payment rate. Enter in column 2 the portion of the amount reported in column 1, as it relates to the ESRD PPS payment times the facility specific composite cost ratio from line 14. Add to this amount the composite cost portion of the payment.
Line 3.03--Enter the sum of lines 3, 3.01 and 3.02, columns 1 and 2 respectively.
Line 4--Enter the amount shown in your records for coinsurance billed to Medicare (Part B) for dialysis treatments. For cost reporting periods that overlap January 1, 2011, enter in column 1 the amount shown in your records for coinsurance billed to Medicare (Part B) patients for dialysis treatments. Include only coinsurance amounts that are related to the payments listed on line 2, column 1, and apply to Medicare beneficiaries under the composite payment rate. Enter in column 2 the amount reported in column 1. For cost reporting periods beginning on or after
40-251.3 Rev.
DRAFT FORM CMS-2552-10 4052 (Cont.)
January 1, 2014, enter in column 1 the amount shown in your records for coinsurance billed to Medicare (Part B) patients. Enter in column 2 the amount reported in column 1 times the facility specific composite cost ratio from line 14.
For cost reporting periods beginning on or after January 1, 2014, do not complete lines 4.01 and 4.02.
Line 4.01--Enter in column 1 the amount shown in your records for coinsurance billed to Medicare (Part B) patients. Include only coinsurance amounts that are related to the payments listed on line 2.01, column 1, and apply to Medicare beneficiaries under the ESRD PPS payment rate. Enter in column 2 the portion of the amount reported in column 1, as it relates to the ESRD PPS payment times the facility specific composite cost ratio from line 14. Add to this amount the composite cost portion of the payment.
Line 4.02--Enter in column 1 the amount shown in your records for coinsurance billed to Medicare (Part B) patients. Include only coinsurance amounts that are related to the payments listed on line 2.02, column 1, and apply to Medicare beneficiaries under the ESRD PPS payment rate. Enter in column 2 the portion of the amount reported in column 1, as it relates to the ESRD PPS payment times the facility specific composite cost ratio from line 14. Add to this amount the composite cost portion of the payment.
Line 4.03--Enter the sum of lines 4, 4.01 and 4.02, columns 1 and 2 respectively.
Line 5--Enter the uncollectible portion of the amounts entered on lines 3 and 4 reduced by any amount recovered during the cost reporting period. For cost reporting periods that overlap or begin on or after January 1, 2011, enter in column 1 the bad debt amount for deductible and coinsurance, net of recoveries, for services rendered prior to January 1, 2011. Transfer this amount to column 2.
Line 5.01--Enter in column 1 the bad debt amount for deductible and coinsurance, net of recoveries, for services rendered on or after January 1, 2011, but before January 1, 2012. Enter in column 2, 75 percent of the amount in column 1, plus 25 percent of the amount in column 1 times the facility specific composite cost ratio on line 14. If the provider indicated “Y” on Worksheet S-5, line 10.02 and elected 100 percent PPS, do not complete this line, but complete line 5.04.
Line 5.02--Enter in column 1 the bad debt amount for deductible and coinsurance, net of recoveries, for services rendered on or after January 1, 2012, but before January 1, 2013. Enter in column 2, 50 percent of the amount in column 1, plus 50 percent of the amount in column 1 times the facility specific composite cost ratio on line 14. If the provider indicated “Y” on Worksheet S-5, line 10.02 and elected 100 percent PPS, do not complete this line, but complete line 5.04.
Line 5.03--Enter in column 1 the bad debt amount for deductible and coinsurance, net of recoveries, for services rendered on or after January 1, 2013, but before January 1, 2014. Enter in column 2, 25 percent of the amount in column 1, plus 75 percent of the amount in column 1 times the facility specific composite cost ratio on line 14. If the provider indicated “Y” on Worksheet S-5, line 10.02 and elected 100 percent PPS, do not complete this line, but complete line 5.04.
Line 5.04--Enter in column 1 the bad debt amount for deductible and coinsurance, net of recoveries, for services rendered on or after January 1, 2014. Enter in column 2, 100 percent of the amount in column 1, times the facility specific composite cost ratio on line 14. If the provider indicated “Y” on Worksheet S-5, line 10.02 and elected 100 percent PPS, DO NOT complete lines 5.01, 5.02 or 5.03, but enter in column 1, the bad debt amount for deductible and coinsurance, net of recoveries for all services rendered on or after January 1, 2011. Enter in column 2, 100 percent of the amount in column 1, times the facility specific composite cost ratio on line 14.
Rev. 40-251.4
4052 (Cont.) FORM CMS-2552-10 DRAFT
Line 5.05--Enter in column 1 the sum of lines 5 through 5.04, column 1. This amount must reconcile to the provider’s bad debt listing(s). Enter in column 2, the sum of lines 5 through 5.04, column 2.
Line 6--Enter the result of line 5.05, column 2 (including negative amounts) times 88 percent for cost reporting periods beginning on or after October 1, 2012, 76 percent for cost reporting periods beginning on or after October 1, 2013, and 65 percent for cost reporting periods beginning on or after October 1, 2014.
Line 7--Enter the gross allowable bad debts for dual eligible beneficiaries. This amount is reported for statistical purposes only. This amount must also be included in the amount on line 5.05, column 1, i.e., line 7 is a subset of line 5.05, column 1.
Line 8--Enter the sum of lines 3 and 4, less line 5, in column 1. For cost reporting periods that overlap or begin on or after January 1, 2011, enter in column 2, the sum of lines 3.03, column 2 and 4.03 column 2, less line 5.05, column 2.
Line 9--Subtract line 3 from line 2, and enter 80 percent of the difference in column 1. For cost reporting periods that overlap or begin on or after January 1, 2011, subtract line 3.03, column 2 from line 2.03, column 2, and enter 80 percent of the difference in column 2.
Line 10--Enter the result of line 1 minus the sum of lines 8 and 9, in column 1. If the result is negative, enter zero and do not complete line 11. For cost reporting periods that overlap or begin on or after January 1, 2011, enter in column 2, the result of line 1 minus the sum of lines 8 and 9, column 2. For cost reporting periods beginning on or after January 1, 2013, do not complete this line.
Line 11--Enter in column 1, the lesser of line 5 or line 10, column 1. For cost reporting periods that overlap or begin on or after January 1, 2011, enter in column 1, the lesser of line 5.05, column 2 or line 10, column 2. For cost reporting periods that begin on or after October 1, 2012, enter in column 1, the lesser of line 6, column 1, or line 10, column 2. For cost reporting periods beginning on or after January 1, 2013, enter in column 1, the result of line 6, column 1. Transfer the amount on this line to Worksheet E, Part B, line 33.
Part II - Calculation of Facility Specific Composite Cost Percentage.--A facility specific composite cost percentage is applied to the facility’s total bad debt amounts and associated cost data necessary to compute the ESRD facility bad debt payments. This percentage is computed by dividing your facility’s basic composite rate costs by your total allowable expenses.
Line 12--For cost reporting periods that overlap or begin on or after January 1, 2011, enter the total allowable expenses from Worksheet I-4, column 2, line 11, plus Worksheet B-2, sum of the absolute values of lines 1 through 6, column 4.
Line 13--Enter total base composite rate costs from Worksheet I-4, column 2, line 11. If you complete more than one Worksheet I-4 summary, (one for renal dialysis department and one for home program dialysis department), enter the sum of the two summary Worksheets I-4, column 2, line 11.
Line 14--Compute the facility specific composite cost percentage (line 13 divided by line 12).
40-252 Rev.
08-11 FORM CMS-2552-10 4053.2
4053. WORKSHEET J-1 - ALLOCATION OF GENERAL SERVICE COSTS TO COMMUNITY MENTAL HEALTH CENTERS
Use this worksheet only if you operate as part of your complex a certified hospital-based community mental health center (CMHC) furnishing services to Medicare titles XVIII, title XIX, and V. Additionally, while comprehensive outpatient rehabilitation facilities (CORFs), outpatient rehabilitation facilities (ORFs) which generally furnish outpatient physical therapy (OPT), outpatient occupational therapy (OOT), or outpatient speech pathology (OSP) services, do not complete the J series worksheets they must complete the applicable Worksheet A cost center for the purpose of overhead allocation. Only those cost centers that represent services for which the facility is certified are used. If you have more than one hospital-based CMHC, complete a separate worksheet for each facility.
4053.1 Part I - Allocation of General Service Costs to Community Mental Health Center Cost Centers.--Worksheet J-1, Part I, provides for the allocation of the expenses of each general service cost center to those cost centers which receive the services. Obtain the total direct expenses (column 0, line 22) from Worksheet A, column 7, lines as appropriate:
Component From Worksheet A, Column 7
CMHC line 99 and subscripts
Obtain the cost center allocations (column 0, lines 1 through 21) from your records, the sum of which must equal the amount entered on column 0, line 22. The amounts on line 22, columns 0 through 23 and column 25 must equal the corresponding amounts on Worksheet B, Part I, columns 0 through 23 and column 25, lines as appropriate:
Component Worksheet B, Part I, Columns 0 through 23 and 25
CMHC line 99 and subscripts
Complete the amounts entered on lines 1 through 21, columns 1 through 23 and column 25 in accordance with the instructions contained in §4053.2.
NOTE: Worksheet B, Part I, established the method used to reimburse direct graduate medical education cost (i.e., reasonable cost or the per resident amount). Therefore, this worksheet must follow that method. If Worksheet B, Part I, column 25, excluded the costs of interns and residents, column 25 on this worksheet must also exclude these costs.
In column 24, Part I, enter the total of columns 4A through 23.
In column 27, Part I, enter the unit cost multiplier (column 26, line 1 divided by the sum of column 26, line 22 minus column 26, line 1) on line 23. Round the unit cost multiplier to six decimal places. Multiply each amount in column 26, lines 2 through 21, by the unit cost multiplier on line 23, and enter the result on the corresponding line of column 27. On line 22, enter the total of the amounts on lines 2 through 21. The total on line 22 equals the amount in column 26, line 1.
In column 28, Part I, enter on lines 2 through 21 the sum of columns 26 and 27. The total on line 22 equals the total in column 26, line 22.
4053.2 Part II - Allocation of General Service Costs to Community Mental Health Center Cost Centers - Statistical Basis.--Worksheet J-1, Part II, provides for the proration of the statistical data needed to equitably allocate the expenses of the hospital’s general service cost centers on Worksheet J-1, Part I. If there is a difference between the total accumulated costs reported on the Part II statistics and the total accumulated costs calculated on Part I, use the reconciliation column on Part II for reporting any
Rev. 2 40-253
4053.2 (Cont.) FORM CMS-2552-10 08-11
adjustments. See §4020 for the appropriate usage of the reconciliation columns. For subscripted (componentized) A&G cost centers, the accumulated cost center line must match the reconciliation column number.
To facilitate the allocation process, the general format of Worksheet J-1, Parts I and II, is identical. The statistical basis shown at the top of each column on Worksheet J-1, Part II, is the recommended basis of allocation of the cost center indicated and must be consistent with the statistical basis utilized on Worksheet B, Part I.
Lines 1 through 21--On Worksheet J-1, Part II, for all cost centers to which the general service cost center is being allocated, enter that portion of the total statistical base applicable to each.
Line 22--Enter the total of lines 1 through 21 for each column. The total in each column must be the same as shown for the corresponding column on Worksheet B-1, lines as appropriate:
Component Worksheet B-1, Corresponding Column
CMHC line 99
 Line
23--Enter the total expenses for the
cost center allocated. Obtain this amount from Worksheet B, Part I,
lines as appropriate (see §4020), from the same column used to
enter the statistical base on Worksheet J-1, Part II (e.g., for a
CMHC provider, in the case of capital-related cost buildings and
fixtures, this amount is on Worksheet B, Part I, column 1, line 99).
Line
23--Enter the total expenses for the
cost center allocated. Obtain this amount from Worksheet B, Part I,
lines as appropriate (see §4020), from the same column used to
enter the statistical base on Worksheet J-1, Part II (e.g., for a
CMHC provider, in the case of capital-related cost buildings and
fixtures, this amount is on Worksheet B, Part I, column 1, line 99).
Line 24--Enter the unit cost multiplier which is obtained by dividing the cost entered on line 23 by the total statistic entered in the same column on line 22. Round the unit cost multiplier to six decimal places.
Multiply the unit cost multiplier by that portion of the total statistic applicable to each cost center receiving the services. Enter the result of each computation on Worksheet J-1, Part I, in the corresponding column and line.
After the unit cost multiplier has been applied to all the cost centers receiving the services, the total cost (line 22, Part I) must equal the total cost on line 23, Part II.
Perform the preceding procedures for each general service cost center.
40-254 Rev. 2
08-11 FORM CMS-2552-10 4055
4054. WORKSHEET J-2 - COMPUTATION OF COMMUNITY MENTAL HEALTH CENTER PROVIDER COSTS
Use this worksheet only if you operate a hospital-based CMHC. If you have more than one hospital-based CMHC, complete a separate worksheet for each facility.
4054.1 Part I - Apportionment of CMHC Cost Centers.--
Column 1--Enter on each line the total cost for the cost center as previously computed on Worksheet J-1, Part I, column 28. To facilitate the apportionment process, the line numbers are the same on both worksheets. Do not transfer lines 19 and 20 from Worksheet J-1.
Column 2--Enter the charges for each cost center. Obtain the charges from your records.
Column 3--For each cost center, enter the ratio derived by dividing the cost in column 1 by the charges in column 2.
Columns 4, 6, and 8-- For each cost center, enter the charges from your records for title V in column 4 and title XIX in column 8. Enter 0 (zero) for each line in column 6 for title XVIII charges as CMHCs are reimbursed under OPPS. Not all facilities are eligible to participate in all programs.
Columns 5, 7, and 9--For each cost center, enter the costs obtained by multiplying the charges in columns 4, 6, and 8, by the ratio in column 3.
Line 20--Enter the totals of lines 1 through 19 in columns 1, 2, and 4 through 9.
4054.2 Part II - Apportionment of Cost of CMHC Services Furnished by Shared Hospital Departments.--Use this part only when the hospital complex maintains a separate department for any of the cost centers listed on this worksheet, and the department provides services to patients of the hospital's CMHC.
Column 3--For each of the cost centers listed, enter the ratio of cost to charges that is shown on Worksheet C, Part I, column 9 from the appropriate line for each cost center.
Columns 4, 6, and 8--For each cost center, enter the charges from your records for title V in column 4 and title XIX in column 8. Enter 0 (zero) for each line in column 6 for title XVIII charges as CMHCs are reimbursed under OPPS.
Columns 5, 7, and 9--For each cost center, enter the costs obtained by multiplying the charges in columns 4, 6, and 8, respectively, by the ratio in column 3.
Line 28--Enter the totals for columns 4 through 9.
Line 29--Enter the total costs from Part I, columns 5, 7, and 9, line 20 plus columns 5, 7, and 9, line 28 respectively and transfer to Worksheet J-3, line 1.
4055. WORKSHEET J-3 - CALCULATION OF REIMBURSEMENT SETTLEMENT – COMMUNITY MENTAL HEALTH CENTER PROVIDER SERVICES
Submit a separate Worksheet J-3 for each title (V, XVIII, or XIX) under which reimbursement is claimed. If you have more than one hospital-based CMHC, complete a separate worksheet for each facility.
Line 1--Enter the cost of the component's services from Worksheet J-2, Part II, line 29 from columns 5, 7, or 9, as applicable (column 5 for title V, column 7 for title XVIII (enter 0 (zero)), and column 9 for title XIX).
Rev. 2 40-255
4055 (Cont.) FORM CMS-2552-10 DRAFT
Line 2--Enter the gross PPS payments received for services rendered during the cost reporting period excluding outliers. Obtain this amount from the PS&R and/or your records.
Line 3--Enter the total outliers payments received. Obtain this amount from the PS&R and/or your records.
Line 4--Enter the amounts paid and payable by workers’ compensation and other primary payers where program liability is secondary to that of the primary payer (from your records).
Line 5--Title XVIII CMHCs enter the result obtained by subtracting line 4 from the sum of lines 2 and 3. Titles V and XIX providers not reimbursed under PPS enter the total reasonable costs by subtracting line 4 from line 1.
Line 6--Enter the charges for the applicable program services from Worksheet J-2, sum of Parts I and II, columns 4, 6, and 8, as appropriate, lines 20 and 28.
Lines 7 through 10--These lines provide for the reduction of program charges where the provider does not actually impose charges on most of the patients liable for payment for services on a charge basis or fails to make reasonable efforts to collect such charges from those patients. If line 9 is greater than zero, enter on line 10 the product of multiplying the ratio on line 9 by line 6.
Providers that do impose charges and make reasonable efforts to collect the charges from patients liable for payment for services on a charge basis are not required to complete lines 7, 8, and 9, but enter on line 10 the amount from line 6. (See 42 CFR 413.13(e).) In no instance may the customary charges on line 10 exceed the actual charges on line 6.
Do not include on these lines (1) the portion of charges applicable to the excess costs of luxury items or services (see CMS Pub. 15-1, chapter 21, §2104.3) and (2) provider charges to beneficiaries for excess costs as described in CMS Pub. 15-1, chapter 25, §2570. When provider operating costs include amounts that flow from the provision of luxury items or services, such amounts are not allowable in computing reimbursable costs.
Lines 11 and 12--Lines 11 and 12 provide for the computation of the lesser of reasonable cost or customary charges as defined in 42 CFR 413.13(a).
Enter on line 11 the excess of total customary charges (line 10) over the total reasonable cost (line 5). In situations where the total charges on line 10 are less than the total cost on line 5, enter zero (0) on line 11.
Enter on line 12 the excess of total reasonable cost (line 5) over total customary charges (line 10). In situations when in any column the total cost on line 5 is less than the customary charges on line 10, enter zero (0) on line 12.
NOTE: CMHCs not subject to reasonable cost reimbursement do not complete lines 11 and 12.
Line 13--Enter the total reasonable costs from line 5.
Line 14--Enter the Part B deductibles billed to program patients (from your records) excluding coinsurance amounts.
Line 16--If there is an excess of reasonable cost over customary charges, enter the amount from line 12.
Line 18--CMHCs enter 0 (zero) as these services are reimbursed under OPPS. For titles V and XIX, enter 100 percent less the applicable coinsurance.
40-256 Rev.
09-14 FORM CMS-2552-10 4055 (Cont.)
Line 19--Enter the actual coinsurance billed to program patients (from your records).
Line 20--For title XVIII, enter the difference of line 17 minus line 19. For titles V and XIX, enter the difference of line 18 minus line 19.
Line 21--Enter allowable bad debts, net of recoveries, applicable to any deductibles and coinsurance (from your records). If recoveries exceed the current year’s bad debts, line 21 will be negative.
Line 22--Enter the result of line 21 (including negative amounts) times 88 percent for cost reporting periods beginning on or after October 1, 2012, 76 percent for cost reporting periods beginning on or after October 1, 2013, and 65 percent for cost reporting periods beginning on or after October 1, 2014.
Line 23--Enter the gross allowable bad debts for dual eligible beneficiaries. This amount is reported for statistical purposes only. This amount must also be reported on line 21.
Line 24--Enter the result of line 20 plus line 21. For cost reporting periods beginning on or after October 1, 2012, enter the result of line 20 plus line 22.
Line 25--Enter any other adjustment. For example, if you change the recording of vacation pay from the cash basis to the accrual basis (see CMS Pub. 15-1 chapter 21, §2146.4), enter the adjustment. Specify the adjustment in the space provided.
Line 26--Enter the result of line 24 plus or minus line 25.
Line 26.01--For cost reporting periods that overlap or begin on or after April 1, 2013, enter the sequestration adjustment amount as follows: [(2 percent times (total days in the cost reporting period that occur during the sequestration period beginning on or after April 1, 2013, divided by total days in the entire cost reporting period, rounded to four decimal places)) times line 26].
Line 27--Enter the total interim payments applicable to this cost reporting period. For title XVIII, transfer this amount from Worksheet J-4, column 2, line 4.
Line 28--For contractor final settlement, report on this line the amount from Worksheet J-4, line 5.99.
Line 29--Enter the balance due provider/program (line 26 minus lines 26.01, 27 and 28), and transfer this amount to Worksheet S, Part III, columns as appropriate, lines as appropriate.
Line 30--Enter the program reimbursement effect of nonallowable cost report items which you are disputing. Compute the reimbursement effect in accordance with CMS Pub. 15-2, chapter 1, §115.2. Attach a schedule showing the supporting details and computation.
Rev. 6 40-257
4056 FORM CMS-2552-10 09-14
4056. WORKSHEET J-4 - ANALYSIS OF PAYMENTS TO HOSPITAL-BASED COMMUNITY MENTAL HEALTH CENTER FOR SERVICES RENDERED TO PROGRAM BENEFICIARIES
Complete this worksheet for Medicare interim payments only. If you have more than one hospital-based CMHC, complete a separate worksheet for each facility.
Complete the identifying information on lines 1 through 4. The remainder of the worksheet is completed by your contractor.
Line Descriptions
Line 1--Enter the total program interim payments paid to the CMHC. The amount entered reflects the sum of all interim payments paid on individual bills (net of adjustment bills) for services rendered in this cost reporting period. The amount entered includes amounts withheld from the component's interim payments due to an offset against overpayments to the component applicable to prior cost reporting periods. It does not include any retroactive lump sum adjustment amounts based on a subsequent revision of the interim rate, or tentative or net settlement amounts, nor does it include interim payments payable.
Line 2--Enter the total program interim payments payable on individual bills. Since the cost in the cost report is on an accrual basis, this line represents the amount of services rendered in the cost reporting period, but not paid as of the end of the cost reporting period. It does not include payments reported on line 1.
Line 3--Enter the amount of each retroactive lump sum adjustment and the applicable date.
Line 4--Transfer the total interim payments to the title XVIII Worksheet J-3, line 27.
DO NOT COMPLETE THE REMAINDER OF WORKSHEET J-4. LINES 5 THROUGH 7 ARE FOR CONTRACTOR USE ONLY. (EXCEPTION: IF WORKSHEET S, PART I, LINE 5 IS “5” (AMENDED COST REPORT), THE PROVIDER MAY COMPLETE THIS SECTION.)
Line 5--List separately each tentative settlement payment after desk review together with the date of payment. If the cost report is reopened after the NPR has been issued, report all settlement payments prior to the current reopening settlement on line 5.
Line 6--Enter the net settlement amount (balance due to the provider or balance due to the program) for the NPR, or, if this settlement is after a reopening of the NPR, for this reopening.
NOTE: On lines 3, 5, and 6, when an amount is due from the provider to the program, show the amount and date on which the provider agrees to the amount of repayment, even though total repayment is not accomplished until a later date.
Line 7--Enter the sum of the amounts on lines 4, 5.99, and 6 in column 2. The amount in column 2 must equal the amount on Worksheet J-3, line 26 less the amount on line 26.01.
Line 8--Enter the contractor name, the contractor number and NPR date in columns 0, 1 and 2, respectively.
40-258 Rev. 6
DRAFT FORM CMS-2552-10 4057
4057. WORKSHEET K - ANALYSIS OF HOSPITAL-BASED HOSPICE COSTS
In accordance with 42 CFR 413.20, the methods of determining costs payable under title XVIII involve making use of data available from the institution's basic accounts, as usually maintained, to arrive at equitable and proper payment for services. The K series worksheets must be completed by all hospital-based hospices. This worksheet provides for recording the trial balance of expense accounts from your accounting books and records. It also provides for reclassification and adjustments to certain accounts. The cost centers on this worksheet are listed in a manner, which facilitates the transfer of the various cost center data to the cost finding worksheets (e.g., on Worksheets K, K-4, Parts I and II, the line numbers are consistent, and the total line is set at 39). Not all of the cost centers listed apply to all providers using these forms. Effective for cost reporting periods beginning on or after October 1, 2015, do not complete these worksheets, but complete the O series worksheets.
Column 1--Obtain salaries to be reported from Worksheet K-1, column 9, line 3 through 38.
Column 2--Obtain employee benefits to be reported from Worksheet K-2 column 9, lines 3 through 38.
Column 3--If the transportation costs, i.e., owning or renting vehicles, public transportation expenses, or payments to employees for driving their private vehicles can be directly identified to a particular cost center, enter those costs in the appropriate cost center. If these costs are not identified to a particular cost center enter them on line 27.
Column 4--Obtain the contracted services to be reported from Worksheet K-3, col. 9, lines 3 through 38.
Column 5--Enter in the applicable lines all costs which have not been reported in columns 1 through 4.
Column 6--Enter the sum of columns 1 through 5 for each cost center.
Column 7--Enter any reclassifications among cost center expenses in column 6 which are needed to effect proper cost allocation. This column need not be completed by all providers, but is completed only to the extent reclassifications are needed and appropriate in the particular circumstances. Show reductions to expenses as negative amounts.
Column 8--Adjust the amounts entered in column 6 by the amounts in column 7 (increases and decreases) and extend the net balances to column 8. The total of column 8, line 39 must equal the total of column 6, line 39.
Column 9--In accordance with 42 CFR 413.9(c)(3), enter on the appropriate lines the amounts of any adjustments to expenses required under Medicare principles of reimbursements. (See §4016.)
Column 10--Adjust the amounts in column 8 by the amounts in column 9, (increases or decreases) and extend the net balances to column 10.
Transfer the amount in column 10, line 1 through 38 to the corresponding lines on Worksheet K‑4, Part I, column 0, lines 1 through 38.
Line Descriptions
Lines 1 and 2--Capital Related Cost - Buildings and Fixtures and Capital Related Cost -Movable Equipment--These cost centers should include depreciation, leases and rentals for the use of the facilities and/or equipment, interest incurred in acquiring land and depreciable assets used for patient care, insurance on depreciable assets used for patient care and taxes on land or depreciable assets used for patient care.
Rev. 40-259
4057 (Cont.) FORM CMS-2552-10 DRAFT
Do not include in these cost centers the following costs: costs incurred for the repair or maintenance of equipment or facilities; amounts included in the rentals or lease or lease payments for repair and/or maintenance agreements; interest expense incurred to borrow working capital or for any purpose other than the acquisition of land or depreciable assets used for patient care; general liability of depreciable assets; or taxes other than those assessed on the basis of some valuation of land or depreciable assets used for patient care.
Line 3--Plant Operation and Maintenance--This cost center contains the direct expenses incurred in the operation and maintenance of the plant and equipment, maintaining general cleanliness and sanitation of plant, and protecting the employees, visitors, and agency property.
Plant Operation and Maintenance include the maintenance and service of utility systems such as heat, light, water, air conditioning and air treatment. This cost center also includes the cost of maintenance and repair of building, parking facilities and equipment, painting, elevator maintenance, performance of minor renovation of buildings, and equipment. The maintenance of grounds such as landscape and paved areas, streets on the property, sidewalk, fenced areas, fencing, external recreation areas and parking facilities are part of this cost center. The care or cleaning of the interior physical plant, including the care of floors, walls, ceilings, partitions, windows (inside and outside), fixtures and furnishings, and emptying of trash containers, as well as the costs of similar services purchased from an outside organization which maintains the safety and well-being of personnel, visitors and the provider’s facilities, are all included in this cost center.
Line 4--Transportation-Staff--Enter all of the cost of transportation except those costs previously directly assigned in column 3. This cost is allocated during the cost finding process.
Line 5--Volunteer Service Coordination--Enter all of the cost associated with the coordination of service volunteers. This includes recruitment and training costs.
Line 6--Administrative and General--Use this cost center to record expenses of several costs which benefit the entire facility. If the option to componentize (also known as fragmentation or subscripting) A&G costs into more than one cost center is elected, eliminate line 6. Componentized A&G lines must begin with subscripted line 6.01 and continue in sequential order (i.e., 6.01 A&G shared costs, 6.02 A&G reimbursable costs, etcetera) Examples include fiscal services, legal services, accounting, data processing, taxes, and malpractice costs.
Line 7--Inpatient - General Care--This cost center includes costs applicable to patients who receive this level of care because their condition is such that they can no longer be maintained at home. Generally, they require pain control or management of acute and severe clinical problems which cannot be managed in other settings. The costs incurred on this line are those direct costs of furnishing routine and ancillary services associated with inpatient general care for which other provisions are not made on this worksheet.
Costs incurred by a hospice in furnishing direct patient care services to patients receiving general inpatient care either directly from the hospice or under a contractual arrangement in an inpatient facility is to be included in the visiting service costs section.
For a hospice that maintains its own inpatient beds, these costs include (but are not limited to) the costs of furnishing 24 hours nursing care within the facility, patient meals, laundry and linen services, and housekeeping. Plant operation and maintenance cost would be recorded on line 3.
For a hospice that does not maintain its own inpatient beds, but furnishes inpatient general care through a contractual arrangement with another facility, record contracted/purchased costs on Worksheet K-3. Do not include any costs associated with providing direct patient care. These costs are recorded in the visiting services section.
40-260 Rev.
12-10 FORM CMS-2552-10 4057 (Cont.)
Line 8--Inpatient - Respite Care--This cost center includes costs applicable to patients who receive this level of care on an intermittent, nonroutine and occasional basis. The costs included on this line are those direct costs of furnishing routine and ancillary services associated with inpatient respite care for which other provisions are not made on this worksheet. Costs incurred by the hospice in furnishing direct patient care services to patients receiving inpatient respite care either directly by the hospice or under a contractual arrangement in an inpatient facility are to be included in visiting service costs section.
For a hospice that maintains its own inpatient beds, these costs include (but are not limited to) the costs of furnishing 24 hours nursing care within the facility, patient meals, laundry and linen services and housekeeping. Plant operation and maintenance costs would be recorded on line 3.
For A hospice that does not maintain its own inpatient beds, but furnishes inpatient respite care through a contractual arrangement with another facility, record contracted/purchased costs on Worksheet K-3. Do not include any costs associated with providing direct patient care. These costs are recorded in the visiting service costs section.
Line 9--Physician Services--In addition to the palliation and management of terminal illness and related conditions, hospice physician services also include meeting the general medical needs of the patients to the extent that these needs are not met by the attending physician. The amount entered on this line includes costs incurred by the hospice or amounts billed through the hospice for physicians’ direct patient care services.
Line 10--Nursing Care--Generally, nursing services are provided as specified in the plan of care by or under the supervision of a registered nurse at the patient’s residence.
Line 11--Nursing Care-Continuous Home Care--Enter the continuous home care portion of costs for nursing services provided by a registered nurse, licensed practical nurse, or licensed vocational nurse as specified in the plan of care by or under the supervision of a registered nurse at the patient’s residence.
Line 12--Physical Therapy--Physical therapy is the provision of physical or corrective treatment of bodily or mental conditions by the use of physical, chemical, and other properties of heat, light, water, electricity, sound massage, and therapeutic exercise by or under the direction of a registered physical therapist as prescribed by a physician. Therapy and speech-language pathology services may be provided for purposes of symptom control or to enable the individual to maintain activities of daily living and basic functional skills.
Line 13--Occupational Therapy--Occupational therapy is the application of purposeful goal-oriented activity in the evaluation, diagnostic, for the persons whose function is impaired by physical illness or injury, emotional disorder, congenial or developmental disability, and to maintain health. Therapy and speech-language pathology services may be provided for purposes of symptom control or to enable the individual to maintain activities of daily living and basic functional skills.
Line 14--Speech/Language Pathology--These are physician-prescribed services provided by or under the direction of a qualified speech-language pathologist to those with functionally impaired communications skills. This includes the evaluation and management of any existing disorders of the communication process centering entirely, or in part, on the reception and production of speech and language related to organic and/or nonorganic factors. Therapy and speech-language pathology services may be provided for purposes of symptom control or to enable the individual to maintain activities of daily living and basic functional skills.
Line 15--Medical Social Services--This cost center includes only direct expenses incurred in providing Medical Social Services. Medical Social Services consist of counseling and assessment activities, which contribute meaningfully to the treatment of a patient’s condition. These services must be provided by a qualified social worker, under the direction of a physician.
Rev. 1 |
40-261 |
4057 (Cont.) FORM CMS-2552-10 12-10
Lines 16 - 18--Counseling--Counseling Services must be available to both the terminally ill individual and family members or other persons caring for the individual at home. Counseling, including dietary counseling, may be provided both for the purpose of training the individual's family or other care giver to provide care, and for the purpose of helping the individual and those caring for him or her to adjust to the individual's approaching death. This includes dietary, spiritual, and other counseling services provided while the individual is enrolled in the hospice. Costs associated with the provision of such counseling are accumulated in the appropriate counseling cost center. Costs associated with bereavement counseling are recorded on line 35.
Line 19--Home Health Aide And Homemaker--Enter the cost of home health aide and homemaker services. Home health aide services are provided under the general supervision of a registered professional nurse and may be provided by only individuals who have successfully completed a home health aide training and competency evaluation program or competency evaluation program as required in 42 CFR 484.36.
Home health aides may provide personal care services. Aides may also perform household services to maintain a safe and sanitary environment in areas of the home used by the patient, such as changing the bed or light cleaning and laundering essential to the comfort and cleanliness of the patient.
Homemaker services may include assistance in personal care, maintenance of a safe and healthy environment and services to enable the individual to carry out the plan of care.
Line 20--Home Health Aide and Homemaker-Continuous Home Care--Enter the continuous care portion of cost for home health aide and/or homemaker services provided as specified in the plan of care and under the supervision of a registered nurse.
Line 21--Other-- Enter on this line any other visiting cost which cannot be appropriately identified in the services already listed.
Line 22--Drugs, Biological and Infusion Therapy--Only drugs as defined in §1861(t) of the Act and which are used primarily for the relief of pain and symptom control related to the individual's terminal illness are covered. The amount entered on this line includes costs incurred for drugs or biologicals provided to the patients while at home. If a pharmacist dispenses prescriptions and provides other services to patients while the patient is both at home and in an inpatient unit, a reasonable allocation of the pharmacist cost must be made and reported respectively on line 22 (drugs and Biologicals) and line 7 (Inpatient General Care) or line 8 (Inpatient Respite Care) of Worksheet K.
A hospice may, for example, use the number of prescriptions provided in each setting to make that allocation, or may use any other method that results in a reasonable allocation of the pharmacist’s cost in relation to the service rendered.
Infusion therapy may be used for palliative purposes if you determine that these services are needed for palliation. For the purposes of a hospice, infusion therapy is considered to be the therapeutic introduction of a fluid other than blood, such as saline solution, into a vein.
Line 23--Analgesics--Enter the cost of analgesics.
Line 24--Sedatives/Hypnotics--Enter the cost of sedatives/hypnotics.
Line 25--Other Specify--Specify the type and enter the cost of any other drugs which cannot be appropriately identified in the drug cost center already listed.
40-262 |
Rev. 1 |
DRAFT FORM CMS-2552-10 4058
Line 26--Durable Medical Equipment/Oxygen--Durable medical equipment as defined in 42 CFR 410.38 as well as other self-help and personal comfort items related to the palliation or management of the patient’s terminal illness are covered. Equipment is provided by the hospice for use in the patient’s home while he or she is under hospice care.
Line 27--Patient Transportation--Enter all of the cost of transportation except those costs previously directly assigned in column 3. This cost is allocated during the cost finding process.
Line 28--Imaging Services--Enter the cost of imaging services including MRI.
Line 29--Labs and Diagnostics--Enter the cost of laboratory and diagnostic tests.
Line 30--Medical Supplies--The cost of medical supplies reported in this cost center are those costs which are directly identifiable supplies furnished to individual patients.
These supplies are generally specified in the patient's plan of treatment and furnished under the specific direction of the patient's physician.
Line 31--Outpatient Service--Use this line for any outpatient services costs not captured elsewhere. This cost can include the cost of an emergency room department.
Lines 32 through 33--Radiation Therapy and Chemotherapy--Radiation, chemotherapy and other modalities may be used for palliative purposes if you determine that these services are needed for palliation. This determination is based on the patient’s condition and your care giving philosophy.
Line 34--Other--Enter any additional costs involved in providing visiting services which has not been provided for in the previous lines.
Lines 35 through 38--Hospice Non Reimbursable Service--Enter in the appropriate lines the applicable costs. Bereavement program costs consists of counseling services provided to the individual’s family after the individual’s death. In accordance with §1814 (i)(1)(A) of the Act, bereavement counseling is a required hospice service, but it is not reimbursable.
Line 39--Total--Line 39 column 10, should agree with Worksheet A, line 116, column 7.
4058. WORKSHEET K-1 - COMPENSATION ANALYSIS - SALARIES AND WAGES
Enter all salaries and wages for the hospice on this worksheet for the actual work performed within the specific area or cost center in accordance with the column headings. For example, if the administrator also performs visiting services which account for 25 percent of that person's time, then enter 75 percent of the administrator's salary on line 6 (A&G) and 25 percent of the administrator's salary enter on line 10 (nursing care).
The records necessary to determine the split in salary between two or more cost centers must be maintained by the hospice and must adequately substantiate the method used to split the salary. These records must be available for audit by the contractor and the contractor can accept or reject the method used to determine the split in salary. When approval of a method has been requested in writing and this approval has been received prior to the beginning of a cost reporting period, the approved method remains in effect for the requested period and all subsequent periods until you request in writing to change to another method or until the contractor determines that the method is no longer valid due to changes in your operations.
Rev. |
40-263 |
4058 (Cont.) FORM CMS-2552-10 DRAFT
Definitions
Salary--This is gross salary paid to the employee before taxes and other items are withheld, includes deferred compensation, overtime, incentive pay, and bonuses. (See CMS Pub. 15-1, chapter 21.)
Administrator (Column 1)--
Possible Titles: President, Chief Executive Officer
Duties: This position is the highest occupational level in the agency. This individual is the chief management official in the agency. The administrator develops and guides the organization by taking responsibility for planning, organizing, implementing, and evaluating. The administrator is responsible for the application and implementation of established policies. The administrator may act as a liaison among the governing body, the medical staff, and any departments.
The administrator provides for personnel policies and practices that adequately support sound patient care and maintains accurate and complete personnel records. The administrator implements the control and effective utilization of the physical and financial resources of the provider.
Director (Column 2)--
Possible Titles: Medical Director, Director of Nursing, or Executive Director
Duties: The medical director is responsible for helping to establish and assure that the quality of medical care is appraised and maintained. This individual advises the chief executive officer on medical and administrative problems and investigates and studies new developments in medical practices and techniques.
The nursing director is responsible for establishing the objectives for the department of nursing. This individual administers the department of nursing and directs and delegates management of professional and ancillary nursing personnel.
Medical Social Worker (Column 3)--This individual is a person who has at least a bachelor’s degree from a school accredited or approved by the council of social work education. These services must be under the direction of a physician and must be provided by a qualified social worker.
Supervisors (Column 4)--Employees in this classification are primarily involved in the direction, supervision, and coordination of the hospice activities.
When a supervisor performs two or more functions, e.g., supervision of nurses and home health aides, the salaries and wages must be split in proportion with the percent of the supervisor's time spent in each cost center, provided the hospice maintains the proper records (continuous time records) to support the split. If continuous time records are not maintained by the hospice, enter the entire salary of the supervisor on line 6 (A&G) and allocate to all cost centers through stepdown. However, if the supervisor's salary is all lumped in one cost center, e.g., nursing care, and the supervisor's title coincides with this cost center, e.g., nursing supervisor, no adjustment is required.
Total Therapists (Column 6)--Include in column 6, on the line indicated, the cost attributable to the following services:
Physical therapy - line 12
Occupational therapy - line 13
Speech pathology - line 14
40-264 Rev.
DRAFT FORM CMS-2552-10 4059
Therapy and speech-language pathology may be provided for purposes of symptom control or to enable the individual to maintain activities of daily living and basic functional skill.
Physical therapy is the provision of physical or corrective treatment of bodily or mental conditions by the use of physical, chemical, and other properties of heat, light, water, electricity, sound, massage, and therapeutic exercise by or under the direction of a registered physical therapist as prescribed by a physician.
Occupational therapy is the application of purposeful, goal-oriented activity in the evaluation, diagnosis, and/or treatment of persons whose ability to work is impaired by physical illness or injury, emotional disorder, congenital or developmental disability, or the aging process, in order to achieve optimum functioning, to prevent disability, and to maintain health.
Speech-language pathology is the provision of services to persons with impaired functional communications skills by or under the direction of a qualified speech-language pathologist as prescribed by a physician. This includes the evaluation and management of any existing disorders of the communication process centering entirely, or in part, on the reception and production of speech and language related to organic and/or nonorganic factors.
Aides (Column 7)--Included in this classification are specially trained personnel employed for providing personal care services to patients. These employees are subject to Federal wage and hour laws. This function is performed by specially trained personnel who assist individuals in carrying out physician instructions and established plans of care. The reason for the home health aide services must be to provide hands-on, personal care services under the supervision of a registered professional nurse.
Aides may provide personal care services and household services to maintain a safe and sanitary environment in areas of the home used by the patient, such as changing the bed or light cleaning and laundering essential to the comfort and cleanliness of the patient. Additional services include, but are not limited to, assisting the patient with activities of daily living.
All Other (Column 8)--Employees in this classification are those not included in columns 1 - 7. Included in this classification are dietary, spiritual, and other counselors. Counseling Services must be available to both the terminally ill individual and the family members or other persons caring for the individual at home. Counseling, including dietary counseling, may be provided both for the purpose of training the individual's family or other care giver to provide care, and for the purpose of helping the individual and those caring for him or her to adjust to the individual's approaching death. This includes dietary, spiritual and other counseling services provided while the individual is enrolled in the hospice.
Total (Column 9)--Add the amounts of each cost center, columns 1 through 8, and enter the total in column 9. Transfer these totals to Worksheet K, column 1, lines as applicable. To facilitate transferring amounts from Worksheet K-1 to Worksheet K, the same cost centers with corresponding line numbers are listed on both worksheets. Not all of the cost centers are applicable to all agencies. Therefore, use only those cost centers applicable to your hospice.
4059. WORKSHEET K-2 - COMPENSATION ANALYSIS – EMPLOYEE BENEFITS (PAYROLL RELATED)
Enter all payroll-related employee benefits for the hospice on this worksheet. See CMS Pub. 15‑1, chapter 20, for a definition of fringe benefits. Use the same basis as that used for reporting salaries and wages on Worksheet K-1. Therefore, using the same example as given for Worksheet K-1, enter 75 percent of the administrator's payroll-related fringe benefits on line 6 (A&G) and enter 25 percent of the administrator's payroll-related fringe benefits on line 10 (nursing care). Payroll-related employee benefits must be reported in the cost center in which the applicable employee's compensation is reported.
Rev. |
40-265 |
4059 (Cont.) FORM CMS-2552-10 DRAFT
This assignment can be performed on an actual basis or the following basis:
FICA - actual expense by cost center;
Pension and retirement and health insurance (nonunion) (gross salaries of participating individuals by cost center);
Union health and welfare (gross salaries of participating union members by cost center); and
All other payroll-related benefits (gross salaries by cost center). Include non payroll-related employee benefits in the A&G cost center, e.g., cost for personal education, recreation activities, and day care.
Add the amounts of each cost center, columns 1 through 8, and enter the total in column 9. Transfer these totals to Worksheet K, column 2, corresponding lines. To facilitate transferring amounts from Worksheet K-2 to Worksheet K, the same cost centers with corresponding line numbers are listed on both worksheets.
4060. WORKSHEET K-3 - HOSPICE COMPENSATION ANALYSIS - CONTRACTED SERVICES/PURCHASED SERVICES.
The hospice may contract with another entity for the provision of non-core hospice services. However, nursing care, medical social services and counseling are core hospice services and must routinely be provided directly by hospice employees. Supplemental services may be contracted in order to meet unusual staffing needs that cannot be anticipated and that occur so infrequently it would not be practical to hire additional staff to fill these needs. You may also contract to obtain physician specialty services. If contracting is used for any services, maintain professional, financial and administrative responsibility for the services and assure that all staff meet the regulatory qualification requirements.
Enter on this worksheet all contracted and/or purchased services for the hospice. Enter the contracted/purchased cost on the appropriate cost center line within the column heading which best describes the type of services purchased. Costs associated with contracting for general inpatient or respite care would be recorded on this worksheet. For example, where physical therapy services are purchased, enter the contract cost of the therapist in column 6, line 12. If a contracted/purchased service covers more than one cost center, then the amount applicable to each cost center is included on each affected cost center line. Add the amounts of each cost center, columns 1 through 8, and enter the total in column 9. Transfer these totals to Worksheet K, column 4, corresponding lines. To facilitate transferring amounts from Worksheet K-3 to Worksheet K, the same cost centers with corresponding line numbers are listed on both worksheets.
40-266 |
Rev. |
DRAFT FORM CMS-2552-10 4061
4061. WORKSHEET K-4, PART I - COST ALLOCATION - GENERAL SERVICE COSTS AND, PART II - COST ALLOCATION - STATISTICAL BASIS
Worksheet K-4 provides for the allocation of the expenses of each general service cost center to those cost centers, which receive the services. The cost centers serviced by the general service cost centers include all cost centers within the provider organization, i.e., other general service cost centers, reimbursable cost centers, nonreimbursable cost centers. Obtain the total direct expenses from Worksheet K, column 10. To facilitate transferring amounts from Worksheet K to Worksheet K-4, Part I, the same cost centers with corresponding line numbers (lines 3 through 39) are listed on both worksheets.
Worksheet K-4, Part II, provides for the proration of the statistical data needed to equitably allocate the expenses of the general service cost centers on Worksheet K-4, Part I.
To facilitate the allocation process, the general format of Worksheets K-4, Parts I & II are identical. The column and line numbers for each general service cost center are identical on the two worksheets. In addition, the line numbers for each general, reimbursable, nonreimbursable, and special purpose cost centers are identical on the two worksheets. The cost centers and line numbers are also consistent with Worksheets K, K-1, K-2, and K-3.
The statistical bases shown at the top of each column on Worksheet K-4, Part II are the recommended bases of allocation of the cost centers indicated. If a different basis of allocation is used, the provider must indicate the basis of allocation actually used at the top of the column.
Most cost centers are allocated on different statistical bases. However, for those cost centers where the basis is the same (e.g., square feet), the total statistical base over which the costs are to be allocated will differ because of the prior elimination of cost centers that have been closed.
Close the general service cost centers in accordance with 42 CFR 413.24(d)(1) which states, in part, that the cost of nonrevenue-producing cost centers serving the greatest number of other centers, while receiving benefits from the least number of centers, is apportioned first. This is clarified in CMS Pub. 15-1, chapter 23, §2306.1, which further clarify the order of allocation for stepdown purposes. Consequently, first close those cost centers that render the most services to and receive the least services from other cost centers. The cost centers are listed in this sequence from left to right on the worksheet. However, the circumstances of an agency may be such that a more accurate result is obtained by allocating to certain cost centers in a sequence different from that followed on these worksheets.
NOTE: A change in order of allocation and/or allocation statistics is appropriate for the current fiscal year cost if received by the contractor, in writing, within 90 days prior to the end of that fiscal year. The contractor has 60 days to make a decision or the change is automatically accepted. The change must be shown to more accurately allocate the overhead or, if the allocation is accurate, it should be changed due to simplification of maintaining the statistics. If a change in statistics is made, the provider must maintain both sets of statistics until an approval is made. If both sets are not maintained and the request is denied, the provider reverts back to the previously approved methodology. The provider must include with the request all supporting documentation and a thorough explanation of why the alternative approach should be used. (See CMS Pub. 15-1, chapter 23, §2313.)
If the amount of any cost center on Worksheet K, column 10, has a credit balance, show this amount as a credit balance on Worksheet K-4, Part I, column 0. Allocate the costs from the applicable overhead cost centers in the normal manner to the cost center showing a credit balance. After receiving costs from the applicable overhead cost centers, if a general service cost
Rev. |
40-267 |
4061 (Cont.) FORM CMS-2552-10 DRAFT
center has a credit balance at the point it is allocated, do not allocate the general service cost center. Rather, enter the credit balance on the first line of the column and on line 39. This enables column 6, line 39, to crossfoot to columns 0 and 5A, line 39. After receiving costs from the applicable overhead cost centers, if a revenue producing cost center has a credit balance on Worksheet K-4, Part I, column 6, do not carry forward a credit balance to any worksheet.
On Worksheet K-4, Part II, enter on the first line in the column of the cost center the total statistics applicable to the cost center being allocated (e.g., in column 1, capital-related cost - buildings and fixtures, enter on line 1 the total square feet of the building on which depreciation was taken). Use accumulated cost for allocating A&G expenses.
Such statistical base does not include any statistics related to services furnished under arrangements except where both Medicare and non-Medicare costs of arranged-for services are recorded in your records.
For all cost centers (below the cost center being allocated) to which the service rendered is being allocated, enter that portion of the total statistical base applicable to each.
The total sum of the statistical base applied to each cost center receiving the services rendered must equal the total statistics entered on the first line.
Enter on Worksheet K-4, Part II, line 39, the total expenses of the cost center to be allocated. Obtain this amount from Worksheet K-4, Part I from the same column and line number of the same column. In the case of capital-related costs - buildings and fixtures, this amount is on Worksheet K-4, Part I, column 1, line 1.
Divide the amount entered on line 39 by the total statistical base entered in the same column on the first line. Enter the resulting unit cost multiplier on line 40. Round the unit cost multiplier to six decimal places.
Multiply the unit cost multiplier by that portion of the total statistical base applicable to each cost center receiving the services rendered. Enter the result of each computation on Worksheet K-4, Part I in the corresponding column and line.
After the unit cost multiplier has been applied to all the cost centers receiving costs, the total expenses (line 39) of all of the cost centers receiving the allocation on Worksheet K-4, Part I, must equal the amount entered on the first line of the cost center being allocated.
The preceding procedures must be performed for each general service cost center. Each cost center must be completed on Worksheets K-4, Part I & II before proceeding to the next cost center.
After all the costs of the general service cost centers have been allocated on Worksheet K-4, Part I, enter in column 7 the sum of the expenses on lines 7 through 38. The total expenses entered in column 7, line 39, must equal the total expenses entered in column 0, line 39.
Column Descriptions
Column 1--Depreciation on buildings and fixtures and expenses pertaining to buildings and fixtures such as insurance, interest, rent, and real estate taxes are combined in this cost center to facilitate cost allocation.
40-268 |
Rev. |
DRAFT FORM CMS-2552-10 4061 (Cont.)
Allocate all expenses to the cost centers on the basis of square footage of the space occupied. The square footage may be weighted if the person who occupies a certain area of space spends their time in more than one function. For example, if a person spends 10 percent of time in one function, 20 percent in another function, and 70 percent in still another function, the square footage may be weighted according to the percentages of 10 percent, 20 percent, and 70 percent to the applicable functions.
Column 2--Allocate all expenses (e.g., interest, and personal property tax) for movable equipment to the appropriate cost centers on the basis of dollar value.
Column 4--The cost of vehicles owned or rented by the agency and all other transportation costs which were not directly assigned to another cost center on Worksheet K, column 3, is included in this cost center. Allocate this expense to the cost centers to which it applies on the basis of miles applicable to each cost center.
This basis of allocation is not mandatory and a provider may use weighted trips rather than actual miles as a basis of allocation for transportation costs, which are not directly assigned. However, a hospice must request the use of the alternative method in accordance with CMS Pub. 15-1, chapter 23, §2313. The hospice must maintain adequate records to substantiate the use of this allocation.
Column 6--The A&G expenses are allocated on the basis of accumulated costs after reclassifications and adjustments.
Therefore, obtain the amounts to be entered on Worksheet K-4, Part II, column 6, from Worksheet K-4, Part I, columns 0 through 5.
A negative cost center balance in the statistics for allocating A&G expenses causes an improper distribution of this overhead cost center. Negative balances are excluded from the allocation statistics when A&G expenses are allocated on the basis of accumulated cost.
A&G costs applicable to contracted services may be excluded from the total cost (Worksheet K‑4, Part I, column 0) for purposes of determining the basis of allocation (Worksheet K-4, Part II, column 5) of the A&G costs. This procedure may be followed when the hospice contracts for services to be performed for the hospice and the contract identifies the A&G costs applicable to the purchased services
The contracted A&G costs must be added back to the applicable cost center after allocation of the hospice A&G cost before the reimbursable costs are transferred to Worksheet K-5. A separate worksheet must be included to display the breakout of the contracted A&G costs from the applicable cost centers before allocation and the adding back of these costs after allocation. Contractor approval does not have to be secured in order to use the above described method of cost finding for A&G.
Worksheet K-4, Part II, Column 6A--Enter the costs attributable to the difference between the total accumulated cost reported on Worksheet K-4, Part I, column 5A, line 39, and the accumulated cost reported on Worksheet K-4, Part II, column 6, line 6. Enter any amounts reported on Worksheet K‑4, Part I, column 5A, for (1) any service provided under arrangements to program patients only that is not grossed up and (2) negative balances. Including these costs in the statistics for allocating A&G expenses causes an improper distribution of overhead.
In addition, report on line 6 the A&G costs reported on Worksheet K-4, Part I, column 6, line 6, since these costs are not included on Worksheet K-4, Part II, column 6, as an accumulated cost statistic.
Rev. |
40-269 |
4061 (Cont.) FORM CMS-2552-10 DRAFT
The accumulated cost center line number must match the reconciliation column number. Include in the column number the alpha character "A", i.e., if the accumulated cost center for A&G is line 6 (A&G), the reconciliation column designation must be 6A.
Worksheet K-4, Part II, Column 6--The A&G expenses are allocated on the basis of accumulated costs. Therefore, enter the amount from Worksheet K-4, Part I, column 5A.
4062. WORKSHEET K-5 - ALLOCATION OF GENERAL SERVICE COSTS TO HOSPICE COST CENTERS
This worksheet distributes the hospital’s overhead to the specific cost centers of the hospice.
4062.1 Part I - Allocation of General Service Costs to Hospice Cost Centers.--Worksheet K-5, Part I, provides for the allocation of the expenses of each general service cost center of the hospital to those cost centers which receive the services.
Obtain the direct total expenses (column 0, lines 2 through 33) from Worksheet K-4 Part I, lines 7 through 38. The amounts on columns 0 through 23 and column 25, line 34, must agree with the corresponding amounts on Worksheet B, Part I, columns 0 through 23 and column 25, line 116.
Complete the amounts entered on lines 1 through 33, columns 1 through 23 and column 25 in accordance with the instructions in §4062.2.
NOTE: Worksheet B, Part I established the method used to reimburse direct graduate medical education cost (i.e., reasonable cost or the per resident amount). Therefore, this worksheet must follow that method. If Worksheet B, Part I, column 25, excluded the costs of interns and residents, column 25 on this worksheet must also exclude these costs.
In column 24, enter the total of columns 4A through 23.
In column 27, for lines 2 through 33, multiply the amount in column 26, by the unit cost multiplier on line 35, and enter the result in this column. The total of the amounts on lines 2 through 33 must equal the amount in column 26, line 1.
In column 28, enter on lines 2 through 33 the sum of columns 26 and 27. The total on line 34 equals the total in column 26, line 34.
4062.2 Part II - Allocation of General Service Costs to Hospice Cost Centers - Statistical Basis.--Worksheet K-5, Part II, provides for the proration of the statistical data needed to equitably allocate the expenses of the hospital’s general service cost centers on Worksheet K-5, Part I. To facilitate the allocation process, the general format of Worksheet K-5, Parts I and II, is identical.
The statistical basis shown at the top of each column on Worksheet K-5, Part II, is the recommended basis of allocation of the cost center indicated and must be consistent with the statistical basis utilized on Worksheet B, Part I.
Lines 1 - 33--On Worksheet K-5, Part II, for all cost centers to which the general service cost center is being allocated, enter that portion of the total statistical base applicable to each.
Line 34--Enter the total of lines 1 through 33 for each column. The total in each column must be the same as shown for the corresponding column on Worksheet B-1, line 116.
40-270 |
Rev. |
09-14 FORM CMS-2552-10 4063
Line 35--Enter the total expenses for the cost center allocated. Obtain this amount from Worksheet B, Part I, columns as indicated, line 116.
Line 36--Enter the unit cost multiplier which is obtained by dividing the cost entered on line 35 by the total statistic entered in the same column on line 34. Round the unit cost multiplier to six decimal places.
Multiply the unit cost multiplier by that portion of the total statistic applicable to each cost center receiving the services. Enter the result of each computation on Worksheet K-5, Part I, in the corresponding column and line.
After the unit cost multiplier has been applied to all the cost centers receiving the services, the total cost (Part I, line 34) must equal the total cost on line 34, Part II.
Perform the preceding procedures for each general service cost center.
4062.3 Part III - Computation of the Total Hospice Shared Costs.--This worksheet provides for the shared therapy, drugs, or medical supplies from the hospital to the hospice.
Column Description
 Column
1--Where applicable, enter in column
1 the cost to charge ratio from Worksheet C, Part I column 9, lines
as indicated.
Column
1--Where applicable, enter in column
1 the cost to charge ratio from Worksheet C, Part I column 9, lines
as indicated.
Column 2--Where hospital departments provides services to the hospice, enter on the appropriate lines the charges, from the provider’s records, applicable to the hospital-based hospice.
Column 3--Multiply the amount in column 2 by the ratios in column 1 and enter the result in column 3.
Line 11--Sum of column 3 lines 1 through 10.



 4063. WORKSHEET
K-6 - CALCUALTION HOSPICE OF PER DIEM COST
4063. WORKSHEET
K-6 - CALCUALTION HOSPICE OF PER DIEM COST

 Worksheet
K-6 calculates the average cost per day for a hospice patient. It is
only an average and should not be misconstrued as the absolute.
Worksheet
K-6 calculates the average cost per day for a hospice patient. It is
only an average and should not be misconstrued as the absolute.
Line 1--Transfer the total cost from Worksheet K-5, Part I, column 28, line 34 less column 28, line 33, plus Worksheet K-5, Part III, column 3 line 11. This line reflects the true cost including shared cost and excluding any non-hospice related activity.
Line 2--Enter the total unduplicated days from Worksheet S-9, column 6, line 5.
Line 3--Calculate the aggregate cost per day by dividing the total cost from line 1 by the total number of days from line 2.
Line 4--Enter the unduplicated Medicare days from Worksheet S-9, column 1, line 5.
Line 5--Calculate the aggregate Medicare cost by multiplying the average cost from column 4, line 3 by the number of unduplicated Medicare days on column 1, line 4 to arrive at the average Medicare cost.
Line 6--Enter the unduplicated Medicaid days from Worksheet S-9, column 2, line 5.
Rev. 6 40-271
4063 (Cont.) FORM CMS-2552-10 09-14
Line 7--Calculate the aggregate Medicaid cost by multiplying the average cost from line 3 by the number of unduplicated Medicaid days on line 6 to arrive at the average Medicaid cost.
Line 8--Enter the unduplicated SNF days from Worksheet S-9, column 3, line 5.
Line 9--Calculate the aggregate SNF cost by multiplying the average cost from line 3 by the number of unduplicated SNF days on line 8 to arrive at the average SNF cost.
Line 10--Enter the unduplicated NF days from Worksheet S-9, column 4, line 5.
Line 11--Calculate the aggregate NF cost by multiplying the average cost from line 3 by the number of unduplicated NF days on line 10 to arrive at the average NF cost.
Line 12--Enter the unduplicated Other days from Worksheet S-9, column 5, line 5.
Line 13--Enter the Aggregate cost for other days by multiplying the average cost from line 3 by the number of unduplicated Other days on line 12 to arrive at the average other cost.
40-272 Rev. 6
DRAFT FORM CMS-2552-10 4064.1
4064. WORKSHEET L - CALCULATION OF CAPITAL PAYMENT
Worksheet L, Parts I through III, calculate program settlement for PPS inpatient hospital capital‑related costs in accordance with the final rule for payment of capital-related costs on a prospective payment system pursuant to 42 CFR 412, Subpart M. (See 56 FR 43196 (August 30, 1991).) Only provider components paid under IPPS complete this worksheet.
Worksheet L consists of the following three parts:
Part I - Fully Prospective Method
Part II - Payment Under Reasonable Cost
Part III - Computation of Exception Payments
COMPLETE EITHER PART I OR PART II, OR PARTS I AND III.
At the top of the worksheet, indicate by checking the applicable boxes the health care program, provider component, and the IPPS capital payment method for which the worksheet is prepared.
4064.1 Part I - Fully Prospective Method.--This part computes settlement under the fully prospective method only, as defined in 42 CFR 412.340. Use the fully prospective method for IPPS capital settlement when the hospital's base year hospital-specific rate is below the adjusted federal rate and for IPPS hospitals with cost reporting periods beginning after the capital PPS transition.
Line Descriptions
Line 1--Enter the amount of the federal rate portion of the capital DRG payments for other than outlier during the period.
Line 1.01--Enter the amount of the federal rate portion of the capital DRG payments for other than outlier during the period associated with Model 4 BPCI.
Line 2--Enter the amount of the federal rate portion of the capital outlier payments made for PPS discharges during the period. (See 42 CFR 412.312(c).)
Line 2.01--Enter the amount of the federal rate portion of the capital outlier payments made for PPS discharges during the period associated with Model 4 BPCI. (See 42 CFR 412.312(c).)
Indirect Medical Education Adjustment
Lines 3 - 6
Line 3--Enter the result of dividing the sum of total patient days (Worksheet S-3, Part I, column 8, lines 14 and 30) by the number of days in the cost reporting period (365, or 366 in case of leap year). Do not include statistics associated with an excluded unit (subprovider).
NOTE: Reduce total patient days by nursery days (Worksheet S-3, Part I, column 8, line 13), and swing bed days (Worksheet S-3, Part I, column 8, lines 5 and 6).
Line 4--Obtain the intern and resident amount from Worksheet E, Part A, line 18 plus line 25.
Line 5--Enter the result of the following calculation: {e.2822 x line 4/line 3}-1 where e = 2.71828. (See 42 CFR 412.322(a)(3) for limitation of the percentage of I&Rs to average daily census. Line 4 divided by line 3 cannot exceed 1.5.
Line 6--Multiply line 5 by the sum of lines 1 and 1.01.
Rev. |
40-273 |
4064.1 (Cont.) FORM CMS-2552-10 DRAFT
Capital Disproportionate Share Adjustment
Lines 7 - 11
Enter the amount of the federal rate portion of the additional capital payment amounts relating to the disproportionate share adjustment. Complete these lines if you answered yes to line 45 on Worksheet S-2, Part I. (See 42 CFR 412.312(b)(3).) For hospitals qualifying for disproportionate share in accordance with 42 CFR 412.106(c)(2) (Pickle amendment hospitals), do not complete lines 7 through 9, and enter 11.89 percent on line 10.
Line 7--Enter the percentage of SSI recipient patient days (from your contractor or your records) to Medicare Part A patient days. This amount agrees with the amount reported on Worksheet E, Part A, line 30.
Line 8--Enter the percentage resulting from the calculation of Medicaid patient days (Worksheet S-2, Part I, columns 1 through 6, line 24) to total days reported on Worksheet S-3, Part I, column 8, line 14, plus column 8, line 32, minus the sum of lines 5 and 6, plus employee discount days reported on Worksheet S-3, Part I, column 8, line 30. This amount must agree with the amount reported on Worksheet E, Part A, line 31.
Line 9--Add lines 7 and 8, and enter the result.
Line 10--Enter the percentage that results from the following calculation: (e.2025 x line 9)-1 where e equals 2.71828. If Worksheet S-2, Part I, line 22, column 2, is “Y” (Pickle amendment hospital), enter 11.89 percent.
Line 11--Multiply line 10 by the sum of lines 1 and 1.01, and enter the result.
Line 12--Enter the sum of lines 1, 1.01, 2, 2.01, 6, and 11. For title XVIII, transfer this amount to Worksheet E, Part A, line 50.
4064.2 Part II - Payment Under Reasonable Cost.--This part computes capital settlement under reasonable cost principles subject to the reduction pursuant to 42 CFR 412.324(b). Use the reasonable cost method for capital settlement determinations for new providers under 42 CFR 412.324(b) for the first two years or for titles V or XIX determinations, if applicable. This part may also be completed for cost reporting periods beginning on or after October 1, 2002, for the first two years for new providers under 42 CFR 412.304(c)(2)(i) (response to Worksheet S-2, Part I, line 47, column 1, is “Y”, and column 2 is “N”).
Line Descriptions
Line 1--Enter the amount of program inpatient routine service capital costs. This amount is the sum of the program inpatient routine capital costs from the appropriate Worksheet D, Part I, column 7, sum of the amounts on lines 30 through 35 and 43 for the hospital (lines 40 through 42, as applicable for the subprovider).
Line 2--Enter the amount of program inpatient ancillary capital costs. This amount is the sum of the amounts of program inpatient ancillary capital costs from the appropriate Worksheet D, Part II, column 5, line 200.
Line 3--Enter the sum of lines 1 and 2.
Line 4--Enter a reduction factor of 85 percent.
Line 5--Multiply line 3 by line 4. For title XVIII, transfer the amount to Worksheet E, Part A, line 50.
40-274 Rev.
DRAFT FORM CMS-2552-10 4064.3
4064.3 Part III - Computation of Exception Payments.--This part computes minimum payment levels by class of provider eligible for additional exception payment for extraordinary circumstances pursuant to 42 CFR 412.312(e). Complete this part only if the provider component completed Part I of this worksheet. Complete this part only if the provider qualifies for the exception payment for extraordinary circumstances pursuant to 42 CFR 412.348(f) (the facility indicates “Y” to question 46 on Worksheet S-2, Part I).
Line 1--Enter the amount of program inpatient routine service and ancillary service capital costs. This amount is the sum of the program inpatient routine service capital costs from the appropriate Worksheet D, Part I, column 7, sum of lines 30 through 35 and 43, for the hospital, lines 40 through 42, as applicable for the subprovider, and program inpatient ancillary service capital costs from Worksheet D, Part II, column 5, line 200.
Line 2--Enter program inpatient capital costs for extraordinary circumstances as provided by 42 CFR 412.348(f), if applicable, from Worksheet L-1, sum of Part II, column 7, sum of lines 30 through 35 and 43, for the hospital; lines 40 through 42, as applicable for the subproviders; and Part III, column 5, line 200.
Line 3--Enter line 1 less line 2.
Line 4--Enter the appropriate minimum payment level percentage: The minimum payment levels for portions of cost reporting periods beginning on or after October 1, 2001 are:
SCHs (located in either an urban or a rural area) - 90 percent;
Urban hospitals with at least 100 beds and a disproportionate patient percentage of at least 20.2 percent - 80 percent; and
All other hospitals - 70 percent.
For providers that qualify for an exception payment for extraordinary circumstances pursuant to 42 CFR 412.348(f) in conjunction with 412.312(e) the appropriate minimum payment level is 70 percent.
The minimum payment levels will be revised, if necessary, to keep total payments under the exceptions process at no more than 10 percent of capital prospective payments.
If you were an SCH during a portion of the cost reporting period, compute the minimum payment level percentage by dividing the number of days in your cost reporting period for which you were not an SCH (70 percent factor applicable) by the total number of days in the cost reporting period. Multiply that ratio by 70 percent. Divide the number of days in your cost reporting period for which you were an SCH (90 percent factor applicable) by the total number of days in the cost reporting period. Multiply that ratio by 90 percent. Add the amounts from steps 1 and 2 to compute the capital cost minimum payment level percentage. Display exception percentage in decimal format, e.g., 70 percent is displayed as .70 or 0.70.
Line 5--Enter the product of line 3 multiplied by line 4.
Line 6--Hospitals that did not qualify as sole community providers during the cost reporting period enter a reduction factor of 85 percent. SCHs enter 100 percent. If you were a sole community hospital during a portion of the cost reporting period, compute the capital cost reduction percentage by dividing the number of days in your cost reporting period for which you were not a sole community hospital (reduction factor applicable) by the total number of days in the cost reporting period. Multiply that ratio by 15 percent and subtract the amount from 100. Enter the resulting extraordinary circumstance percentage adjustment in decimal format, e.g., 85 percent is displayed as .85 or 0.85.
Rev. 40-275
4064.3 (Cont.) FORM CMS-2552-10 DRAFT
Line 7--Enter the product of line 2 multiplied by line 6.
Line 8--Enter the sum of lines 5 and 7.
Line 9--Enter the amount from Part I, line 12, if applicable.
Line 10--Enter line 8 less line 9.
Lines 11 - 14--A hospital is entitled to an additional payment if its capital payments for the cost reporting period is less than the applicable minimum payment level. The additional payment equals the difference between the applicable minimum payment level and the capital payments that the hospital would otherwise receive. This additional payment amount is reduced for any amounts by which the hospital’s cumulative payments exceed its cumulative minimum payment levels. The offsetting amounts will be determined based on the amounts by which the hospital’s cumulative payments exceed its cumulative minimum payment levels in the lesser of the preceding 10-year period or the period of time under which the hospital is subject to the prospective payment system for capital-related costs.
A positive amount on line 10 represents the amount of capital payments under the minimum payment level in the current year. This amount must be offset for the amount by which the hospital’s cumulative payments exceed its cumulative minimum payment levels in prior years, as reported on line 11. If the net amount on line 12 remains a positive amount, this amount represents the current year’s additional payment for capital payments under the minimum payment level. Report this amount on line 13. If the net amount on line 12 is a negative amount, this amount represents the reduced amount by which the accumulated capital payment amounts exceeded the accumulated minimum payment levels. In this case, no additional payment is made in the current year. Transfer the amount on line 12 to line 14, and carry it forward to the following cost reporting period.
A negative amount on line 10 represents the amount of capital payments over the minimum payment level in the current year. Add any carry forward of prior years’ amounts of the hospital’s cumulative payments in excess of cumulative minimum payment levels, as reported on line 11, to the current year excess on line 12. The net amount on line 12 represents the total amount by which the accumulated capital payment amounts exceeded the accumulated minimum payment levels. No additional payment is made in the current year. Transfer the amount on line 12 to line 14, and carry it forward to the subsequent cost reporting period.
Line 11--The offsetting amounts will be determined based on the amounts by which the hospital’s cumulative payments exceed its cumulative minimum payment levels in the lesser of the preceding 10-year period or the period of time under which the hospital is subject to the prospective payment system for capital-related costs. Enter the appropriate offset amount as computed pursuant to 42 CFR 412.312(e)(3).
Line 12--Enter the sum of lines 10 and 11.
Line 13--If the amount on line 12 is positive, enter the amount on this line.
Line 14--If the amount on line 12 is negative, enter the amount on this line.
Complete lines 15 through 17 only when line 12 is a positive amount.
Line 15--Enter the current years allowable operating and capital payments calculated from Worksheet E, Part A, line 47, plus the capital payments reported on line 9 above, minus 75 percent of the current year’s operating disproportionate share payment amount reported on Worksheet E, Part A, line 34.
40-276 Rev.
10-12 FORM CMS-2552-10 4065.1
Line 16--Current years operating and capital costs from Worksheet D-1, line 49 minus the sum of D, Part III, lines 30 through 35, column 9 (PPS subproviders use lines 40 through 42, as applicable, column 9), and D, Part IV, column 11, line 200.
Line 17--Enter on this line the current year’s exception offset amount. This is computed as line 15 minus line 16. If this amount is negative, enter zero on this line. If the amount on line 13 is greater than line 17, transfer the amount on line 13, less any reported amount on line 17, to Worksheet E, Part A, line 51.
4065. WORKSHEET L-1 - ALLOCATION OF ALLOWABLE CAPITAL COSTS FOR EXTRAORDINARY CIRCUMSTANCES
This worksheet provides for the determination of direct and indirect capital-related costs associated with capital expenditures for extraordinary circumstances, allocated to inpatient operating costs. Only complete this worksheet for providers that qualify for an additional payment for extraordinary circumstances under 42 CFR 412.348(f) (the facility indicates “Y” to question 46 on worksheet S-2, Part I).
4065.1 Part I - Allocation of Allowable Capital Costs for Extraordinary Circumstances.--Use this part in conjunction with Worksheet B-l. The format and allocation process employed is similar to that used on Worksheets B, Part I and B-1. Any cost center subscripted lines and/or columns added to Worksheet B, Part I, are also added to this worksheet in the same sequence.
Column 0--Assign capital expenditures relating to extraordinary costs to specific cost centers on this worksheet, column 0. Enter on the appropriate lines those capital-related expenditure amounts relating to extraordinary costs which were directly assigned on Worksheet B, Part II. Enter on lines 3 and 4, as applicable, the remaining capital expenditure amounts relating to extraordinary costs which have not been directly assigned.
Columns 1 through 23--Transfer amounts on the top lines of columns 1 and 2 from column 0, line as applicable. For example, transfer line 1, column 0 to line 1, column 1. For all other columns, the top line represents the cross total amount.
For each column, enter on line 203 of this worksheet, Part I, the total statistics of the cost center being allocated. Obtain the individual statistics from Worksheet B-1 from the same column and line number used to allocate cost on this worksheet. (For example, obtain the amount of capital-related costs - buildings and fixtures from Worksheet B-1, column 1, line 1.)
Divide the amount entered on line 203 by the total capital expenses entered in the same column on the first line. Enter the resulting unit cost multiplier on line 204. Round the unit cost multiplier to six decimal places.
Multiply the unit cost multiplier by that portion of the total statistics applicable to each cost center receiving the services. The applicable cost center statistics are reported on Worksheet B-1. Enter the result of each computation on this worksheet in the corresponding column and line. (See §4000.1 for rounding standards.)
After the unit cost multiplier has been applied to all the cost centers receiving the services rendered, the total cost (line 197) of all the cost centers receiving the allocation on this worksheet must equal the amount entered on the first line. Perform the preceding procedures for each general service cost center. Complete the column for one cost center before proceeding to the column for the next cost center.
Rev. 3 40-277
4065.1 (Cont.) FORM CMS-2552-10 10-12
After the capital-related costs of all the general service cost centers have been allocated, enter in column 24 the sum of columns 2A through 23 for lines 30 through 196. (See §4020 for exception regarding negative cost centers.)
When an adjustment is required to capital costs for extraordinary circumstances after cost allocation, show the amount applicable to each cost center in column 25. Submit a supporting schedule showing the computation of the adjustment.
Transfer From Worksheet:
L-1, Part I, Column 26 To Worksheet L-1, Part II
Line 30 - Adults and Pediatrics Column l, line 30 for the hospital
Lines 31 through 35 - Intensive Column 1, lines 31 through 35
Care Type Inpatient Hospital
Units
Lines 40 through 42, as Column l, lines 40 through 42, as applicable
applicable - Subprovider
Line 43 - Nursery Column 1, line 43 for titles V and XIX
To Worksheet L-1, Part III
Lines 50 through 76 - Ancillary Column l, lines 50 through 76
Services
Lines 88 through 91 and 93 - Column l, lines 88 through 91 and 93
Outpatient Service Cost
Subscripts of line 92 - Distinct Column 1, subscripts of line 92
Part Observation Bed Units
Lines 88, 89, 94, 97, and 98 Column l, lines 88, 89, 94, 97, and 98
4065.2 Part II - Computation of Program Inpatient Routine Service Capital Costs for Extraordinary Circumstances.--This part computes the amount of capital costs for extraordinary circumstances applicable to hospital inpatient routine service costs. Complete only one Worksheet L-1, Part II for each title. Report hospital and subprovider information on the same worksheet, lines as appropriate.
Column 1--Enter on each line the capital costs for extraordinary circumstances as appropriate. Obtain this amount from Worksheet L-1, Part I, column 26.
Column 2--Compute the amount of the swing bed adjustment. If you have a swing bed agreement or have elected the swing bed optional method of reimbursement, determine the amount for the cost center in which the swing beds are located by multiplying the amount in column 1 by the ratio of the amount entered on Worksheet D-1, line 26 to the amount entered on Worksheet D-1, line 21.
Column 3--Enter column 1 minus column 2.
Column 4--Enter on each line the total patient days, excluding swing bed days, by cost center from the corresponding lines of Worksheet D, Part I, column 4.
40-278 Rev. 3
DRAFT FORM CMS-2552-10 4065.3
Column 5--Divide the cost of each cost center in column 3 by the total patient days in column 4 for each line to determine the per diem cost capital cost for extraordinary circumstances. Enter the resultant per diem cost in column 5.
Column 6--Enter the program inpatient days for the corresponding cost centers from Worksheet D, Part I, column 6.
Column 7--Multiply the per diem in column 5 by the inpatient program days in column 6 to determine the program’s share of capital costs for extraordinary circumstances applicable to inpatient routine services, as applicable, and enter the result.
4065.3 Part III - Computation of Program Inpatient Ancillary Service Capital Costs For Extraordinary Circumstances.--This part computes the program inpatient ancillary capital costs for extraordinary circumstances for titles V, XVIII, Part A, and XIX. Complete a separate copy of this part for the hospital and each subprovider for titles V, XVIII, Part A, and XIX, as applicable. In this case, enter the subprovider component number in addition to showing the provider number.
Make no entries on this worksheet for any costs centers with a negative balance on Worksheet B, Part I, column 26.
Column 1--Enter on each line the capital-related costs for each cost center as appropriate. Obtain this amount from Worksheet L-1, Part I, column 26.
NOTE: Compute capital costs for extraordinary circumstances relating to non-distinct observation bed units. To compute extraordinary circumstances relating to non-distinct observation bed units, develop a ratio of total observation bed costs to total general routine costs. Compute this ratio, rounded to six decimal places, by dividing the amount from Worksheet L-1, Part I, column 26, line 30 by the amount on Worksheet D-1, line 37. Then multiply this ratio by the general routine capital costs for extraordinary circumstances from Supplemental Worksheet L-1, Part I, column 26, line 30 to obtain the capital costs for extraordinary circumstances relating to non-distinct observation bed units for line 92, column 1. Transfer distinct part observation bed unit costs from Worksheet L-1, Part I, the appropriate subscript of column 26, line 92.
Column 2--Enter on each line the charges applicable to each cost center as shown on Worksheet C, Part I, column 6.
Column 3--Divide the cost of each cost center in column 1 by the charges in column 2 for each line to determine the cost/charge ratio. Round the ratios to six decimal places, e.g., round .0321514 to 032151. Enter the resultant departmental ratios in column 3.
Column 4--Enter on each line the appropriate titles V, XVIII, Part A, or XIX inpatient charges. Transfer these charges from the corresponding lines of Worksheet D, Part II, column 4.
Column 5--Multiply the ratio in column 3 by the charges in column 4 to determine the program’s share of capital costs for extraordinary circumstances applicable to titles V, XVIII, Part A, or XIX inpatient ancillary services, as appropriate.
Rev. 40-279
4066 FORM CMS-2552-10 DRAFT
4066. WORKSHEET M-1 - ANALYSIS OF HOSPITAL-BASED RHC/FQHC COSTS
Use this worksheet only if you operate a certified hospital-based RHC/FQHC. Use only those cost centers that represent services for which the clinic/center is certified. If you have more than one hospital-based RHC/FQHC, complete separate worksheets for each hospital-based RHC/FQHC, unless the clinic/center has received prior contractor approval to file a consolidated cost report (see CMS Pub. 100-4, chapter 9, §30). Effective for cost reporting periods beginning on or after October 1, 2014, hospital-based FQHCs do not complete the M series worksheets but must complete the N series worksheets.
This worksheet is for the recording of direct hospital-based RHC/FQHC costs from your accounting books and records to arrive at the identifiable clinic/center cost. This data is required by 42 CFR 413.20. The worksheet also provides for the necessary reclassifications and adjustments to certain accounts prior to the cost finding calculations.
Column Descriptions
Columns 1 through 3--The expenses listed in these columns must be in accordance with your accounting books and records. If the cost elements of a cost center are maintained separately on your books, a reconciliation of costs per the accounting books and records to those on this worksheet must be maintained by you and are subject to review by your contractor.
Enter on the appropriate lines in columns 1 through 3 the total expenses incurred during the reporting period. Detail the expenses as Salaries (column 1) and Other (column 2). The sum of columns 1 and 2 must equal column 3.
Column 4--Enter any reclassifications among the cost center expenses listed in column 3 which are needed to effect proper cost allocation. This column need not be completed by all hospital-based RHCs/FQHCs, but is completed only to the extent reclassifications are needed and appropriate in the particular circumstances. See §4014 for examples of reclassifications that may be needed. Submit with the cost report copies of any work papers used to compute the reclassifications reported in this column.
The net total of the entries in column 4 must equal zero on line 30 if no reclassifications were reported on worksheet A, column 4, of the appropriate line 88 and/or 89.
Column 5--Add column 4 to column 3, and extend the net balances to column 5. The total of column 5 must equal the total of column 3 on line 30, if no reclassifications were reported on worksheet A, column 4, of the appropriate line 88 and/or 89.
Column 6--In accordance with 42 CFR 413.9(c)(3), enter on the appropriate lines the amounts of any adjustments to expenses required under the Medicare principles of reimbursement. (See §4016.) Submit with the cost report copies of any work papers used to compute the adjustments reported in this column.
NOTE: The allowable cost of the services furnished by Public Health Service personnel may be included in your hospital-based RHCs/FQHCs costs. Obtain this amount from your contractor, and include this as an adjustment to the appropriate lines on column 6.
40-280 Rev.
DRAFT FORM CMS-2552-10 4066 (Cont.)
Column 7--Adjust the amounts in column 5 by the amounts in column 6, and extend the net balance to column 7. The total clinic/center costs on line 32 must equal the net expenses for cost allocation on Worksheet A for the hospital-based RHC/FQHC cost center.
Line Descriptions
Lines 1 through 9--Enter the costs of your health care staff.
Line 10--Enter the sum of the amounts on lines 1 through 9.
Line 11--Enter the cost of physician medical services furnished under agreement.
Line 12--Enter the expenses of physician supervisory services furnished under agreement.
Line 14--Enter the sum of the amounts on lines 11 through 13.
Lines 15 through 20--Enter the expenses of other health care costs.
Line 20--Do not complete this line. Per 42 CFR 413.78(a), the GME payment to the hospital includes all residents working in the hospital healthcare complex; therefore, no separate payment is made to the hospital-based RHC/FQHC for GME costs.
Line 21--Enter the sum of the amounts on lines 15 through 20.
Line 22--Enter the sum of the amounts on lines 10, 14, and 21. Transfer this amount to Worksheet M-2, line 10.
Lines 23 through 27--Enter the expenses applicable to services that are not reimbursable under the RHC/FQHC benefit.
Line 27--Do not complete this line.
Line 28--Enter the sum of the amounts on lines 23 through 27. Transfer the total amount in column 5 to Worksheet M-2, line 11.
Line 29--Enter the overhead expenses directly costed to the hospital-based RHC/FQHC. These expenses may include rent, insurance, interest on mortgage or loans, utilities, depreciation of buildings and fixtures, depreciation of equipment, housekeeping and maintenance expenses, and property taxes. Submit with the cost report supporting documentation to detail and compute the facility costs reported on this line.
Line 30--Enter the expenses related to the administration and management of the hospital-based RHC/FQHC that are directly costed. These expenses may include office salaries, depreciation of office equipment, office supplies, legal fees, accounting fees, insurance, telephone service, fringe benefits, and payroll taxes. Submit with the cost report supporting documentation to detail and compute the administrative costs reported on this line.
Line 31--Enter the sum of the amounts on lines 29 and 30. Transfer the total amount in column 5 to Worksheet M-2, line 14.
Line 32--Enter the sum of the amounts on lines 22, 28, and 31. This is the total hospital-based RHC/FQHC cost. This amount should agree with the amount reported for the hospital-based RHC/FQHC on Worksheet A, column 7.
Rev. 40-281
4067 FORM CMS-2552-10 DRAFT
4067. WORKSHEET M-2 - ALLOCATION OF OVERHEAD TO HOSPITAL-BASED RHC/FQHC SERVICES
Use this worksheet only if you operate a certified hospital-based RHC/FQHC as part of your healthcare complex. If you have more than one hospital-based RHC/FQHC, complete a separate worksheet for each hospital-based RHC/FQHC.
Visits and Productivity.--Worksheet M-2 summarizes the number of hospital-based RHC/FQHC visits furnished by the health care staff and calculates the number of visits to be used in the rate determination. Lines 1 through 9 list the types of practitioners (positions) for whom hospital-based RHC/FQHC visits must be counted and reported.
Column Descriptions
Column 1--Record the number of all full time equivalent (FTE) personnel in each of the applicable staff positions in the hospital-based RHCs/FQHCs practice. (See CMS Pub. 100-04, chapter 9, §40.3, for a definition of FTEs).
Column 2--Record the total visits actually furnished to all patients by all personnel in each of the applicable staff positions in the reporting period. Count visits in accordance with instructions in 42 CFR 405.2463(a) defining a visit.
 Column
3--Productivity standards
established by CMS are applied as a guideline that reflects the total
combined services of the staff. Apply a level of 4200 visits for
each physician and a level of 2100 visits for each nonphysician
practitioner. You are not subject to the productivity standards if
you answered “Yes” to question 12 of Worksheet S-8. If
so, then enter the revised standards established by you and your
contractor.
Column
3--Productivity standards
established by CMS are applied as a guideline that reflects the total
combined services of the staff. Apply a level of 4200 visits for
each physician and a level of 2100 visits for each nonphysician
practitioner. You are not subject to the productivity standards if
you answered “Yes” to question 12 of Worksheet S-8. If
so, then enter the revised standards established by you and your
contractor.
Column 4--For lines 1 through 3, enter the product of column 1 and column 3. This is the minimum number of hospital-based RHC/FQHC visits the personnel in each staff position are expected to furnish.
Column 5--On line 4, enter the greater of the subtotal of the actual visits in column 2 or the minimum visits in column 4.
Contractors have the authority to waive the productivity guideline in cases where you have demonstrated reasonable justification for not meeting the standard. In such cases, the contractor will substitute your actual visits if an exception is granted.
On lines 5 through 7 and 9, enter the actual number of visits for each type of position.
Line Descriptions
Line 1--Enter the number of FTEs and total visits furnished to hospital-based RHC/FQHC patients by staff physicians working at the hospital-based RHC/FQHC on a regular ongoing basis. Also include on this line, physician data (FTEs and visits) for services furnished to hospital-based RHC/FQHC patients by staff physicians working under contractual agreement with you on a regular ongoing basis in the hospital-based RHC/FQHC. These physicians are subject to productivity standards. (See 42 CFR 405.2468(d)(2)(v).)
Line 4--Enter the total of lines 1 through 3 for columns 1, 2 and 4.
Line 5--Enter the number of FTEs and total visits furnished to hospital-based RHC/FQHC patients by visiting nurses working at the hospital-based RHC/FQHC. Visiting nurses provide skilled nursing services to the homebound for services which require the skills of a nurse based on the complexity of the service, e.g., intravenous or intramuscular injections or insertions of catheters. (See CMS Pub. 100-02, chapter 13, §180).
40-282 Rev.
DRAFT FORM CMS-2552-10 4067 (Cont.)
Line 6--Enter the number of FTEs and total visits furnished to hospital-based RHC/FQHC patients by clinical psychologists working at the hospital-based RHC/FQHC. Clinical psychologist services may include the diagnosis, treatment and consultation of a patient. (See CMS Pub. 100-02, chapter 13, §140).
Line 7--Enter the number of FTEs and total visits furnished to hospital-based RHC/FQHC patients by clinical social worker working at the hospital-based RHC/FQHC. Clinical social worker services may include the diagnosis, treatment and consultation of a patient. (See CMS Pub. 100-02, chapter 13, §140).
Line 7.01--Enter the number of FTEs for registered dieticians or nutritional professionals and total visits furnished to hospital-based FQHC patients for medical nutrition therapy (MNT) services provided in hospital-based FQHCs. MNT services apply to hospital-based FQHCs only. (See CMS Pub. 100-02, chapter 13, §210.2.4).
Line 7.02--Enter the number of FTEs for registered dieticians or nutritional professionals and total visits furnished to hospital-based FQHC patients for diabetes self-management training (DSMT) services provided in hospital-based FQHCs. DSMT services apply to hospital-based FQHCs only. (See CMS Pub. 100-02, chapter 13, §210.2.4).
Line 8--Enter the total of lines 4 through 7 (and subscripts).
Line 9--Enter the number of visits furnished to hospital-based RHC/FQHC patients by physicians under agreement with you who do not furnish services to patients on a regular ongoing basis in the hospital-based RHC/FQHC. Physicians’ services under agreements with you are (1) all medical services performed at your site by a non-staff physician who is not the owner or an employee of the facility, and (2) medical services performed at a location other than your site by such a physician for which the physician is compensated by you. While all physician services at your site are included in RHC/FQHC services, physician services furnished in other locations by physicians who are not on your full time staff are paid to you only if your agreement with the physician provides for compensation for such services.
Determination of Total Allowable Cost Applicable To Hospital-Based RHC/FQHC Services.--Use lines 10 through 18 to determine the amount of overhead costs incurred by both the parent provider and the hospital-based RHC/FQHC.
Line 10--Enter the cost of health care services from Worksheet M-1, column 7, line 22.
Line 11--Enter the total non-reimbursable costs from Worksheet M-1, column 7, line 28.
Line 12--Enter the sum of lines 10 and 11 for the cost of all services (excluding overhead).
Line 13--Enter the percentage of hospital-based RHC or FQHC services. This percentage is determined by dividing the amount on line 10 (the cost of health care services) by the amount on line 12 (the cost of all services, excluding overhead).
Line 14--Enter the total hospital-based RHC/FQHC overhead costs incurred from Worksheet M-1, column 7, line 31.
Line 15--Enter the overhead costs incurred by the parent provider allocated to the hospital-based RHC/FQHC. This amount is the difference between the total costs after cost allocation on Worksheet B, Part I, column 26, and Worksheet B, Part I, column 0.
Line 16--Enter the sum of lines 14 and 15 to determine the total overhead costs related to the hospital-based RHC/FQHC.
Rev. 40-283
4067 (Cont.) FORM CMS-2552-10 DRAFT
Line 17--Do not complete this line. Per 42 CFR 413.78(a), the GME payment to the hospital includes all residents working in the hospital healthcare complex; therefore, no separate payment is made to the hospital-based RHC/FQHC for GME costs.
Line 18--Enter the amount from line 16.
Line 19--Enter the overhead amount applicable to hospital-based RHC/FQHC services. It is determined by multiplying the amount on line 13 (the ratio of hospital-based RHC/FQHC services to total services) by the amount on line 18 (total overhead costs).
Line 20--Enter the total allowable cost of hospital-based RHC/FQHC services, the sum of line 10 (cost of hospital-based RHC/FQHC health care services) and line 19 (overhead costs applicable to hospital-based RHC/FQHC services).
4068. WORKSHEET M-3 - CALCULATION OF REIMBURSEMENT SETTLEMENT FOR HOSPITAL-BASED RHC/FQHC SERVICES
This worksheet applies to title XVIII only and provides for the reimbursement calculation for services rendered. Use this worksheet to determine the interim all inclusive rate of payment and the total program payment for the cost reporting period for each hospital-based RHC/FQHC reported.
Determination of Rate For Hospital-Based RHC/FQHC Services.--Worksheet M-3 calculates the cost per visit for hospital-based RHC/FQHC services and applies the screening guideline established by CMS on your health care staff productivity.
Line Descriptions
Line 1--Enter the total allowable cost from Worksheet M-2, line 20.
Line 2--Report vaccine costs on this line from Worksheet M-4.
Line 3--Subtract the amount on line 2 from the amount on line 1 and enter the result.
Line 4--Enter the greater of the minimum or actual visits by the health care staff from Worksheet M‑2, column 5, line 8.
Line 5--Enter the visits made by physicians under agreement from Worksheet M-2, column 5, line 9.
Line 6--Enter the total adjusted visits (sum of lines 4 and 5).
Line 7--Enter the adjusted cost per visit. This is determined by dividing the amount on line 3 by the visits on line 6.
For services rendered from January 1, 2010, through December 31, 2013, the maximum rate per visit entered on line 8 and the outpatient mental health treatment service limitation applied on line 14 both correspond to the same time period (partial calendar year). Consequently, both are entered in the same column and no further subscripting of the columns is necessary.
Lines 8 and 9--The limits are updated every January 1. However, the possibility exists that limits may also be updated other than on January 1. Complete columns 1, 2 and 3, if applicable (add a column 3 for lines 8-14 if the cost reporting overlaps 3 limit update periods) of lines 8 and 9 to identify costs and visits affected by different payment limits for a cost reporting period that overlaps January 1. If only one payment limit is applicable during the cost reporting period (calendar year reporting period), complete column 2 only.
40-284 Rev.
DRAFT FORM CMS-2552-10 4068 (Cont.)
Line 8--Enter the per visit payment limit. Obtain this amount from CMS Pub. 100-04, chapter 4, §20.6, or from your contractor.
NOTE: If you are based in a small rural hospital with less than 50 beds (the bed count is based on the same calculation used on Worksheet E, Part A, line 4), in accordance with 42 CFR 412.105(b), do not apply the per visit payment limit. Transfer the adjusted cost per visit (line 7) to line 9, columns 1 and/or 2.
NOTE: Hospital-based RHCs that are based in a small urban hospital with less than 50 beds (as calculated above) will also be exempt from the per visit limit.
For hospital-based RHCs based in small urban hospitals transfer the adjusted cost per visit (line 7) to line 9, column 1 and/or 2.
Line 9--Enter the lesser of the amount on line 7 or line 8.
Calculation of Settlement.--Complete lines 10 through 29 to determine the total program payment due you for covered hospital-based RHC/FQHC services furnished to program beneficiaries during the reporting period. Complete columns 1 and 2 of lines 10 through 14 to identify costs and visits affected by different payment limits during a cost reporting period.
Line Descriptions
Line 10--Enter the number of program covered visits excluding visits subject to the outpatient mental health services limitation from your contractor records.
Line 11--Enter the subtotal of program cost. This cost is determined by multiplying the rate per visit on line 9 by the number of visits on line 10 (the total number of covered program beneficiary visits for hospital-based RHC/FQHC services during the reporting period).
Line 12--Enter the number of program covered visits subject to the outpatient mental health services limitation from your contractor records.
Line 13--Enter the program covered cost for outpatient mental health services by multiplying the rate per visit on line 9 by the number of visits on line 12.
Line 14--Enter the limit adjustment. In accordance with MIPPA 2008, section 102, the outpatient mental health treatment service limitation applies as follows: For services rendered through December 31, 2009, the limitation is 62.50 percent; services from January 1, 2010, through December 31, 2011, the limitation is 68.75 percent; services from January 1, 2012, through December 31, 2012, the limitation is 75 percent; services from January 1, 2013 through December 31, 2013, the limitation is 81.25 percent; and services on or after January 1, 2014, the limitation is 100 percent. This is computed by multiplying the amount on line 13 by the corresponding outpatient mental health treatment service limit percentage. This limit applies only to therapeutic services, not initial diagnostic services.
NOTE: Section 4104 of ACA eliminates coinsurance and deductible for preventive services, effective for dates of service on or after January 1, 2011. Hospital-based RHCs/FQHCs must provide detailed HCPCS coding for preventive services to ensure coinsurance and deductible are not applied. Hospital-based RHCs/FQHCs must maintain this documentation to apply the appropriate reductions on lines 16.03 and 16.04.
Line 15--Do not complete this line. Per 42 CFR 413.78(a), the GME payment to the hospital includes all residents working in the hospital healthcare complex; therefore, no separate payment is made to the hospital-based RHC/FQHC for GME costs.
Rev. 40-285
4068 (Cont.) FORM CMS-2552-10 DRAFT
Line 16--For cost reporting periods that overlap January 1, 2011, enter in column 1 the sum of lines 11, 14, and 15, column 1 and in column 2, the sum of lines 11, 14, and 15, column 2. For cost reporting periods beginning on or after January 1, 2011, do not use column 1 and enter the total program cost in column 2. This is equal to the sum of the amounts in columns 1 and 2, respectively (and 3 if applicable), lines 11, 14, and 15.
Line 16.01--Enter the total program charges from the contractor’s records (PS&R). For cost reporting periods that overlap January 1, 2011, do not complete column 1 and enter total program charges for services rendered on or after January 1, 2011 in column 2. For cost reporting periods beginning on or after January 1, 2011, enter total program charges in column 2.
Line 16.02--Enter the total program preventive charges from the provider’s records. For cost reporting periods that overlap January 1, 2011, do not complete column 1 and enter total program preventive charges for services rendered on or after January 1, 2011 in column 2. For cost reporting periods beginning on or after January 1, 2011, enter total program preventive charges in column 2.
Line 16.03--Enter the total program preventive costs. For cost reporting periods that overlap January 1, 2011, do not complete column 1 and enter the total program preventive costs ((line 16.02 divided by line 16.01) times line 16) for services rendered on or after January 1, 2011, in column 2. For cost reporting periods beginning on or after January 1, 2011, enter the total program preventive costs ((line 16.02 divided by line 16.01) times line 16, column 2.
Line 16.04.--Enter the total program non-preventive costs. For cost reporting periods that overlap January 1, 2011, do not complete column 1 and enter the total program non- preventive costs ((line 16 minus lines 16.03 and 18) times .80) for services rendered on or after January 1, 2011, in column 2. For cost reporting periods beginning on or after January 1, 2011, enter the total program non- preventive costs ((line 16, column 2, minus lines 16.03 and 18, column 2) times .80) in column 2.
Line 16.05--Enter the total program costs. For cost reporting periods that overlap January 1, 2011, enter total program costs (line 16 times .80) for services rendered prior to January 1, 2011 in column 1, and enter the sum of lines 16.03 and 16.04, in column 2. For cost reporting periods beginning on or after January 1, 2011, enter the sum of lines 16.03 and 16.04, in column 2.
Line 17--Enter the primary payer amounts from your records.
Line 18--Enter the amount credited to the hospital-based RHC's program patients to satisfy their deductible liabilities on the visits on lines 10 and 12 as recorded by the contractor from clinic bills processed during the reporting period. Hospital-based RHCs determine this amount from the interim payment lists provided by the contractor. Hospital-based FQHCs enter zero on this line as deductibles do not apply.
Line 19--Enter the coinsurance amount applicable to the hospital-based RHC/FQHC for program patient visits on lines 10 and 12 as recorded by the contractor from clinic/center bills processed during the reporting period. This line captures data for informational and statistical purposes only. This line does not impact the settlement calculation.
Line 20--Enter the net program costs, excluding vaccines. For cost reporting periods that overlap January 1, 2011, enter the result of subtracting the amount on line 17 from the amount on line 16.05, columns 1 and 2. For cost reporting beginning on or after January 1, 2011, enter the result of subtracting the amount on line 17 from the amount on line 16.05, column 2.
Line 21--Enter the amount from Worksheet M-4, line 16.
40-285.1 Rev.
DRAFT FORM CMS-2552-10 4068 (Cont.)
Line 22--Enter the total allowable Medicare cost, sum of the amounts on lines 20 and 21.
Line 23--Enter your total allowable bad debts, net of recoveries, from your records. If recoveries exceed the current year’s bad debts, line 23 will be negative.
Line 23.01--Enter the result of line 23 (including negative amounts) times 88 percent for cost reporting periods beginning on or after October 1, 2012, 76 percent for cost reporting periods beginning on or after October 1, 2013, and 65 percent for cost reporting periods beginning on or after October 1, 2014.
Line 24--Enter the gross allowable bad debts for dual eligible beneficiaries. This amount is reported for statistical purposes only. This amount must also be reported on line 23.
Line 25--Enter any other adjustment. For example, if you change the recording of vacation pay from the cash basis to the accrual basis (see CMS Pub. 15-1, chapter 21, 2146.4), enter the adjustment. Specify the adjustment in the space provided.
Line 26--Enter the sum of lines 22 and 23 plus or minus line 25. For cost reporting periods beginning on or after October 1, 2012, enter the sum of lines 22 and 23.01 plus or minus line 25.
Line 26.01--For cost reporting periods that overlap or begin on or after April 1, 2013, enter the sequestration adjustment amount as follows: [(2 percent times (total days in the cost reporting period that occur during the sequestration period beginning on or after April 1, 2013, divided by total days in the entire cost reporting period, rounded to four decimal places)) times line 26].
Line 27--Enter the total interim payments from Worksheet M-5 made to you for covered services furnished to program beneficiaries during the reporting period (from contractor records).
Line 28--For contractor use only, enter the on line 5.99 of Worksheet M-5.
Line 29--Enter the total amount due to/from the program (line 26 minus lines 26.01, 27 and 28). Transfer this amount to Worksheet S, Part III, column 3, line 10 and/or 11 as applicable.
Line 30--Enter the program reimbursement effect of protested items. The reimbursement effect of the nonallowable items is estimated by applying a reasonable methodology which closely approximates the actual effect of the item as if it had been determined through the normal cost finding process. (See CMS Pub. 15-1, chapter 1, §115.2.) A schedule showing the supporting details and computations must be attached.
Rev. |
40-285.2 |
4069 FORM CMS-2552-10 DRAFT
4069. WORKSHEET M-4 - COMPUTATION OF HOSPITAL-BASED RHC/FQHC PNEUMOCOCCAL AND INFLUENZA VACCINE COST
The cost and administration of pneumococcal and influenza vaccine to Medicare beneficiaries are 100 percent reimbursable by Medicare. This worksheet provides for the computation of the cost of these vaccines. Additionally, only use this worksheet for vaccines rendered to patients who, at the time of receiving the vaccine(s), were not inpatients or outpatients of the hospital. If a patient simultaneously received vaccine(s) with any Medicare covered services as an inpatient or outpatient of the hospital, those vaccine costs are reimbursed through the hospital and cannot be claimed by the hospital-based RHC/FQHC.
To accommodate vaccines other than the seasonal influenza vaccines covered by Medicare, subscript column 2 (add column 2.01 and 2.02, if necessary). The data entered in all columns (1, 2, and applicable subscripts) for lines 4, 11, and 13 are mutually exclusive. That is, the vaccine costs, the total number of vaccines administered, and the total number of Medicare covered vaccines shall only be represented one time in the appropriate column.
Line 1--Enter the health care staff cost from Worksheet M-1, column 7, line 10.
Line 2--Enter the ratio of the estimated percentage of time involved in administering pneumococcal and influenza vaccine injections to the total health care staff time. Do not include physician service under agreement time in this calculation.
Line 3--Multiply the amount on line 1 by the amount on line 2 and enter the result.
Line 4--Enter the cost of the pneumococcal and influenza vaccine medical supplies from your records.
Line 5--Enter the sum of lines 3 and 4.
Line 6--Enter the amount from Worksheet M-1, column 7, line 22. This is your total direct cost of the facility.
Line 7--Enter the amount from Worksheet M-2, line 19.
Line 8--Divide the amount on line 5 by the amount on line 6 and enter the result.
Line 9--Multiply the amount on line 7 by the amount on line 8 and enter the result.
Line 10--Enter the sum of the amounts on lines 5 and 9.
Line 11--Enter the total number of pneumococcal and influenza vaccine injections from your records.
Line 12--Enter the cost per pneumococcal and influenza vaccine injections by dividing the amount on line 10 by the number on line 11.
Line 13--Enter the number of program pneumococcal and influenza vaccine injections from your records or the PS&R.
Line 14--Enter the program cost for vaccine injections by multiplying the amount on line 12 by the amount on line 13.
40-286 Rev.
DRAFT FORM CMS-2552-10 4070
Line 15--Enter the total cost of pneumococcal and influenza vaccines and their administration by entering the sum of the amount in column 1, line 10 and the amount in column 2 (and applicable subscripts), line 10.
Transfer this amount to Worksheet M-3, line 2.
Line 16--Enter the Medicare cost of pneumococcal and influenza vaccines and their administration costs. This is equal to the sum of the amount in column 1, line 14 plus column 2 (and applicable subscripts), line 14.
Transfer the result to Worksheet M-3, line 21.
4070. WORKSHEET M-5 - ANALYSIS OF PAYMENTS TO HOSPITAL-BASED RHC/FQHC FOR SERVICES RENDERED TO PROGRAM BENEFICIARIES
Complete this worksheet for Medicare interim payments only. If you have more than one hospital-based RHC/ FQHC, complete a separate worksheet for each.
Complete the identifying information on lines 1 through 4. The remainder of the worksheet is completed by your contractor.
Line descriptions
Line 1--Enter the total program interim payments paid to the hospital-based RHC/FQHC. The amount entered reflects the sum of all interim payments paid on individual bills (net of adjustment bills) for services rendered in this cost reporting period. The amount entered includes amounts withheld from the component's interim payments due to an offset against overpayments to the component applicable to prior cost reporting periods. It does not include any retroactive lump sum adjustment amounts based on a subsequent revision of the interim rate, or tentative or net settlement amounts, nor does it include interim payments payable.
Line 2--Enter the total program interim payments payable on individual bills. Since the cost in the cost report is on an accrual basis, this line represents the amount of services rendered in the cost reporting period, but not paid as of the end of the cost reporting period. It does not include payments reported on line 1.
Line 3--Enter the amount of each retroactive lump sum adjustment and the applicable date.
Line 4--Transfer the total interim payments to the title XVIII Worksheet M-3, line 27.
DO NOT COMPLETE THE REMAINDER OF WORKSHEET M-5. LINES 5 THROUGH 7 ARE FOR CONTRACTOR USE ONLY. (EXCEPTION: IF WORKSHEET S, PART I, LINE 5 IS “5” (AMENDED COST REPORT), THE HOSPITAL-BASED RHC/FQHC MAY COMPLETE THIS SECTION.)
Line 5--List separately each tentative settlement payment after desk review together with the date of payment. If the cost report is reopened after the NPR has been issued, report all settlement payments prior to the current reopening settlement on line 5.
Rev. 40-287
4070 (Cont.) FORM CMS-2552-10 DRAFT
Line 6--Enter the net settlement amount (balance due to the hospital-based RHC/FQHC or balance due to the program) for the NPR, or, if this settlement is after a reopening of the NPR, for this reopening.
NOTE: On lines 3, 5, and 6, when an amount is due from the hospital-based RHC/FQHC to the program, show the amount and date on which the hospital-based RHC/FQHC agrees to the amount of repayment, even though total repayment is not accomplished until a later date.
Line 7--Enter the sum of the amounts on lines 4, 5.99, and 6, in column 2. The amount in column 2 must equal the amount on Worksheet M-3, line 26 less the amount on line 26.01.
Line 8--Enter the contractor name, the contractor number and NPR date in columns 0, 1 and 2, respectively.
40-288 Rev.
DRAFT FORM CMS-2552-10 4070 (Cont.)
Reserved for Future Use
Rev. 40-289
4071 FORM CMS-2552-10 DRAFT
4071. WORKSHEET N-1 - RECLASSIFICATION AND ADJUSTMENT OF TRIAL BALANCE OF EXPENSES FOR HOSPITAL-BASED FQHC
Use the N worksheet series if you operate a certified hospital-based FQHC for cost reporting periods beginning on or after October 1, 2014. Use only those cost centers that represent services for which the hospital-based FQHC is certified. If you have more than one hospital-based FQHC, complete a separate worksheet N series for each hospital-based FQHC, unless the hospital-based FQHC has received prior contractor approval to file a consolidated cost report (see CMS Pub. 100-04, chapter 9, §30).
This worksheet is for recording direct costs of the hospital-based FQHC from your accounting books and records. It also provides for the necessary reclassifications and adjustments to certain accounts. If the cost elements of a cost center are maintained separately on your accounting books, a reconciliation of costs per the accounting books and records to those on this worksheet must be maintained and are subject to review by your contractor. The cost centers listed may not apply to every hospital-based FQHC using these forms. For example, a hospital-based FQHC that does not have transportation costs will not complete line 11. Complete only those lines that are applicable.
Column Descriptions
Column 1--Enter direct salaries and wages plus related salary amounts for paid vacation, holiday, sick, other paid-time-off (PTO), severance, and bonus pay.
Column 2--Enter all costs other than salaries.
Column 3--For each cost center, add the amounts in columns 1 and 2 and enter the total in column 3.
Column 4--For each cost center, enter any reclassifications for expenses listed in column 3. The net total of the entries in column 4, line 100, must equal zero if no reclassifications were reported on Worksheet A, column 4, line 89. Show reductions to expenses as negative numbers. This column is completed only to the extent reclassifications are needed and appropriate in the particular circumstances. See §4014 for examples of reclassifications that may be needed. Submit with the cost report copies of any work papers used to compute the reclassifications reported in this column.
Column 5--For each cost center, enter the total of the amount in column 3 plus or minus the amount in column 4. The total on column 5, line 100 must equal the total on column 3, line 100, if no reclassifications were reported on Worksheet A, column 4, line 89.
Column 6--For each cost center, enter on the appropriate lines the amounts of any adjustments to expenses required under the Medicare principles of reimbursement. (See §4016.) Submit with the cost report copies of any work papers used to compute the adjustments reported in this column.
Column 7--For each cost center, enter the total of the amount in column 5 plus or minus the amount in column 6. The amount on line 100 must equal the net expenses for cost allocation on Worksheet A, column 7, line 89.
40-290 Rev.
DRAFT FORM CMS-2552-10 4071 (Cont.)
Line Descriptions
This worksheet groups the trial balance of expenses into general service cost centers, direct patient care cost centers, reimbursable pass through costs, other FQHC services, and nonreimbursable cost centers to facilitate the transfer of costs to the various worksheets.
General Service Cost Centers--
These cost centers include expenses incurred in operating the hospital-based FQHC as a whole that are not directly associated with furnishing patient care such as, but not limited to mortgage, rent, plant operations, administrative salaries, utilities, telephone, and computer hardware and software costs. General service cost centers furnish services to other general service cost centers and to reimbursable and nonreimbursable cost centers.
Lines 1 and 2 - Cap Rel Costs-Bldg & Fix and Cap Rel Costs-Mvble Equip--These cost centers include the capital-related costs for buildings and fixtures and the capital-related costs for movable equipment including depreciation, leases and rentals for the use of facilities and/or equipment, including electronic health records systems, interest incurred in acquiring land and depreciable assets used for patient care, insurance on depreciable assets used for patient care and taxes on land or depreciable assets used for patient care, and, software and hardware updates to electronic health record systems. Do not include costs incurred for the repair or maintenance of equipment or facilities; amounts specifically included in rentals or lease payments for repair and/or maintenance agreements; interest expense incurred to borrow working capital or for any purpose other than the acquisition of land or depreciable assets used for patient care; general liability insurance or any other form of insurance to provide protection other than the replacement of depreciable assets; or taxes other than those assessed on the basis of some valuation of land or depreciable assets used for patient care. However, if no amount of the lease payment is identified in the lease agreement for maintenance, you are not required to carve out a portion of the lease payment to represent the maintenance portion. Thus, the entire lease payment is considered a capital-related cost subject to the provisions of 42 CFR 413.130(b).
Line 3 - Employee Benefits--This cost center includes the costs of the employee benefits department. In addition, this cost center includes the fringe benefits paid to, or on behalf of, an employee when a provider’s accounting system is not designed to accumulate the benefits on a departmentalized or cost center basis. (See CMS Pub. 15-1, chapter 21, §2144.)
Line 4 - Administrative and General--A&G includes a wide variety of administrative costs such as but not limited to cost of fiscal services, legal and accounting services, facility administrative services (not already included in other general service cost centers), etcetera.
Line 5 - Plant Operation and Maintenance--This cost center includes expenses incurred in the plant operation and maintenance of the hospital-based FQHC. These costs include the maintenance and service of utility systems such as heat, light, water, air conditioning and air treatment. This cost center also includes costs incurred in maintaining the facility and grounds, such as costs of routine painting, plumbing, mowing, and snow removal.
Line 6 - Janitorial--This cost center includes the cost of routine janitorial activities such as mopping, vacuuming, cleaning restrooms, lobbies, waiting areas and otherwise maintaining patient and non-patient care areas.
Rev. 40-291
4071 (Cont.) FORM CMS-2552-10 DRAFT
Line 7 - Medical Records--This cost center includes the cost of the medical records department where patient medical records are maintained. The general library and the medical library are not included in this cost center but are included in the A&G cost center. None of the costs associated with electronic health records systems are reported in this cost center.
Line 8 - Subtotal - Administrative Overhead--Enter the total of lines 1 through 7.
Line 9 - Pharmacy--This cost center includes the routine costs of drugs (both prescription and over the counter), pharmacy supplies, pharmacy personnel, pharmacy services, and the non-routine costs of drugs and pharmacy supplies that can be traced to individual patients. Do not include the cost of influenza and pneumococcal vaccines on this line as these costs are reported on lines 47 and 48, respectively.
Line 10 - Medical Supplies--This cost center includes the cost of routine supplies used in the normal course of caring for patients, such as gloves, masks, swabs, or glycerin sticks, and the non-routine medical supplies that can be traced to individual patients. Do not include the cost of medical supplies used in administering influenza and pneumococcal vaccines on this line as these costs are reported on lines 47 and 48, respectively.
Line 11 - Transportation--This cost center includes the cost of owning or renting vehicles, public transportation expenses, parking, tolls, or payments to employees for driving their private vehicles to see patients or for other hospital-based FQHC business.
Line 12 - Other General Service--Use this line to report the costs of other general service costs not previously identified on lines 1 through 11.
Line 13 - Subtotal - Total Overhead--Enter the sum of lines 8 and 9 through 12.
Lines 14 through 22--Reserved for future use.
Direct Care Cost Centers--
Line 23 - Physician--This cost center includes the costs incurred for physicians providing direct patient care services and general supervisory services, participation in the establishment of plans of care, supervision of care and services, periodic review and updating of plans of care, and establishment of governing policies by the governing board. Reclassify the cost for the portion of time physicians spent on general supervisory services or other hospital-based FQHC administrative activities to A&G (line 4).
Line 24 - Physician Services Under Agreement--This cost center includes the costs incurred for physicians who are providing services under agreement.
Line 25 - Physician Assistant--This cost center includes the costs incurred for physician assistants (PAs), including the costs for PAs providing physician services.
Line 26 - Nurse Practitioner--This cost center includes the costs of nursing care provided by nurse practitioners (NPs), including NPs providing physician services.
Line 27 - Visiting Registered Nurse--This cost center only includes the costs of nursing care provided by registered nurses (RNs), who perform visiting nurse services in accordance with CMS Pub. 100-02, chapter 13, §180. Costs associated with RNs who provide services incident to a physician, PA, NP, certified nurse midwife (CNM), clinical psychologist (CP) or clinical social worker (CSW)(See CMS Pub. 100-02, chapter 13, §§110, 120 and 140) are included in line 36.
40-292 Rev.
DRAFT FORM CMS-2552-10 4071 (Cont.)
Line 28 - Visiting Licensed Practical Nurses--This cost center includes the costs of nursing care provided by licensed practical nurses (LPNs) who perform visiting nurse services in accordance with CMS Pub. 100-02, chapter 13, §180. Costs associated with LPNs who provide services incident to a physician, PA, NP, CNM, CP or CSW(See CMS Pub. 100-02, chapter 13, §§110, 120 and 140) are included in line 36.
Line 29 - Certified Nurse Midwife--This cost center includes the costs of nursing care provided by CNM’s.
Line 30 - Clinical Psychologist--This cost center includes the costs of a CP who holds a doctorate in psychology and is licensed or certified by the State in which he or she practices, for diagnostic, assessment, preventative and therapeutic services directed at individuals.
Line 31 - Clinical Social Worker--This cost center includes the costs of a CSW who possesses a master’s degree or doctorate in social work and meets specified criteria established by regulation. The CSW must directly examine the patient, or directly review the patient’s medical information, to provide diagnosis, treatment and consultation.
Line 32 - Laboratory Technician--This cost center includes the costs of a person who, under the supervision of a medical technologist or physician, performs microscopic and bacteriologic tests of human blood, tissue, and fluid for diagnostic and research purposes.
Line 33 - Reg Dietician/Cert DSMT/MNT Educator--This cost center includes the costs of a person who is either a registered dietician or nutritionist who meets specified criteria for providing diabetes self-management training (DSMT) or medical nutrition therapy (MNT) services under the Program.
Line 34 - Physical Therapist--This cost center includes the costs of physical or corrective treatment of bodily or mental conditions by the use of physical, chemical, and other properties of heat, light, water, electricity, sound massage, and therapeutic exercise by or under the direction of a registered physical therapist as prescribed by a physician. Physical therapy services may be provided for purposes of symptom control or to enable the individual to maintain activities of daily living and basic functional skills.
Line 35 - Occupational Therapist--This cost center includes the costs of purposeful goal-oriented activities in the evaluation, diagnosis, and/or treatment of persons whose function is impaired by physical illness or injury, emotional disorder, congenital or developmental disability, or the aging process, in order to achieve optimum functioning, to prevent disability, and to maintain health. Occupational therapy services may be provided for purposes of symptom control or to enable the individual to maintain activities of daily living and basic functional skills.
Line 36 - Other Allied Health Personnel--This cost center includes the cost of RNs and LPNs who provide services incident to a physician, PA, NP, CNM, CP, or CSW in accordance with CMS Pub. 100-02, chapter 13, §§110, 120 and 140 and the cost of other allied health personnel that provide diagnostic, technical, therapeutic and direct patient care and support services to the other health professionals they work with and the patients they serve. An example of other allied health personnel is a medical assistant.
Line 37 - Subtotal Direct Patient Care Services--Enter the total of lines 23 through 36.
Lines 38 through 46--Reserved for future use.
Reimbursable Pass Through Costs--
Line 47 - Pneumococcal Vaccines & Med Supplies--This cost center includes the cost of the pneumococcal vaccines and the medical supplies attributable to pneumococcal vaccinations.
Rev. 40-293
4071 (Cont.) FORM CMS-2552-10 DRAFT
Line 48 - Influenza Vaccines & Med Supplies--This cost center includes the cost of the influenza vaccines and the medical supplies attributable to influenza vaccinations.
Line 49 - Subtotal - Reimbursable Pass Through Costs--Enter the total of lines 47 through 48.
Lines 50 through 59--Reserved for future use.
Other FQHC Services--
Line 60 - Medicare Excluded Services--This cost center includes the cost of routine dental care, hearing tests, eye exams, etcetera, that are excluded from coverage under the Program.
Line 61 - Diagnostic & Screening Lab Tests--This cost center includes the technical component cost of diagnostic and laboratory tests such as electrocardiograms and certain preventative services authorized by the Medicare statute or the national coverage determination process. This cost center does not include venipuncture, which is included in the pharmacy cost center when furnished by the hospital-based FQHC.
Line 62 - Radiology - Diagnostic--This cost center includes the technical component of radiological diagnostic tests such as x-rays and imaging services.
Line 63 - Prosthetic Devices--This cost center includes the costs of devices (other than dental) which replace all or part of an internal body organ including colostomy bags and supplies directly related to colostomy care, replacement of such devices, and one pair of conventional eyeglasses or contact lenses furnished subsequent to each cataract surgery with the insertion of an intraocular lens.
Line 64 - Durable Medical Equipment--This cost center includes the direct costs of DME rented or sold (DME, as defined in 42 CFR 410.38) furnished to an individual patient and all direct expenses incurred in requisitioning and issuing DME to patients.
Line 65 - Ambulance Services--Report all ambulance costs on this line for both owned and operated services and services under arrangement.
Line 66 - Telehealth--This cost center includes the cost of telehealth distant-site services as described in CMS Pub. 100-02, chapter 13, §190.
Line 67 - Other--Use this line to report the costs of other FQHC services not previously identified on lines 60 through 66.
Line 68 - Subtotal Other FQHC Services--Enter the total of lines 60 through 67.
Lines 69 through 77--Reserved for future use.
Nonreimbursable Cost Centers--
Line 78 - Other Nonreimbursable--Use this line to record the costs applicable to other nonreimbursable cost centers not provided for on this worksheet.
Line 79 through 99--Reserved for future use.
Line 100 - Total--Enter the sum of lines 13, 37, 49, 68, and 78.
40-294 Rev.
DRAFT FORM CMS-2552-10 4071.1
4071.1. WORKSHEET N-2 - CALCULATION OF HOSPITAL-BASED FQHC COST PER VISIT
The purpose of Worksheet N-2 is to summarize (1) the hospital-based FQHC medical and mental health visits furnished by practitioners, including health care staff and physicians under agreement, and (2) apportion overhead costs to hospital-based FQHC services to determine the average cost per visit for a medical visit and a mental health visit, by practitioner.
Column 1--Enter the total cost for each practitioner from Worksheet N-1, column 7 as indicated on the worksheet.
Column 2--Enter the total medical and mental health visits actually furnished to all patients by each practitioner during the cost reporting period. Each visit to the hospital-based FQHC by the beneficiary counts as a single visit, even in the case where a beneficiary returns to the hospital-based FQHC in the same day for a subsequent illness or injury. A beneficiary can have up to three medical visits in a day to include the initial visit and two subsequent visits for illness or injury.
NOTE: Column 2, line 11 must equal Worksheet S-11, Part III, column 4, sum of lines 2 and 4. For each line 1 through 10, column 2 must equal the sum of columns 7 and 8.
Column 3--Use this column to allocate costs associated with other direct care costs, sum of Worksheet N-1, column 7, lines 32, 34, 35, and 36. Calculate the UCM related to other direct care costs by dividing the sum of Worksheet N-1, column 7, lines 32, 34, 35, and 36, by Worksheet N-2, column 2, line 11, total medical and mental health visits, and enter the result on line 12. Calculate the costs for lines 1 through 10 by multiplying the visits on each corresponding line, column 2 times the UCM on line 12.
Column 4--Use this column to allocate general service costs, sum of Worksheet N-1, column 7, line 13, plus Worksheet B, Part I, line 89, column 26, minus Worksheet B, Part I, line 89, column zero. Calculate the UCM by dividing Worksheet N-1, column 7, line 13, plus Worksheet B, Part I, line 89, column 26, minus Worksheet B, Part I, line 89, column zero, by Worksheet N-1, column 7, line 100, minus Worksheet N-1, column 7, line 13, and enter the result on line 12. Allocate the general service cost attributable to each practitioner on lines 1 through 10, by multiplying the UCM times the sum of the amounts in columns 1 and 3, for each corresponding line.
Column 5--Enter the sum of columns 1, 3 and 4, for each practitioner.
Column 6--Calculate the average cost per visit by each practitioner by dividing the total cost in column 5 by the total visits in column 2. Enter the result in column 6.
Column 7--Enter the total number of medical visits included in column 2, provided to all patients by each practitioner during the cost reporting period.
Column 8--Enter the total number of mental health visits included in column 2, provided to all patients by each practitioner during the cost reporting period.
Column 9--Enter the total number of medical visits provided to Medicare beneficiaries by each practitioner during the cost reporting period.
Column 10--Enter the total number of mental health visits provided to Medicare beneficiaries by each practitioner during the cost reporting period.
NOTE: Worksheet S-11, Part III, column 2, line 2, must equal column 9, line 11; and Worksheet S-11, Part III, column 2, line 4, must equal column 10, line 11.
Rev. 40-295
4071.1 (Cont.) FORM CMS-2552-10 DRAFT
Column 11--Calculate the Medicare cost per medical visit by practitioner by multiplying the average cost per visit in column 6 by the Medicare visits in column 9.
Column 12--Calculate the Medicare cost per mental health visit by practitioner by multiplying the average cost per visit in column 6 by the Medicare visits in column 10.
Line 11--Enter the sum of lines 1 through 10 for the applicable columns.
Line 13, column 6--Calculate the average cost per visit by dividing column 5, line 11 by column 2, line 11.
Line 13, column 11--Calculate the Medicare average cost per medical visit by dividing column 11, line 11 by column 9, line 11.
Line 13, column 12--Calculate the Medicare average cost per mental health visit by dividing column 12, line 11 by column 10, line 11.
40-296 Rev.
DRAFT FORM CMS-2552-10 4071.2
4071.2. WORKSHEET N-3 - COMPUTATION OF HOSPITAL-BASED FQHC PNEUMOCOCCAL AND INFLUENZA VACCINE COST
The cost and administration of pneumococcal and influenza vaccine to Medicare beneficiaries are 100 percent reimbursable by Medicare. This worksheet provides for the computation of the cost of the pneumococcal and influenza vaccines. Use this worksheet for vaccines rendered to hospital-based FQHC patients who, at the time of receiving the vaccine(s), were not inpatients or outpatients of the hospital. If a patient simultaneously received a vaccine(s) with any Medicare covered services as an inpatient or outpatient of the hospital, those vaccine costs are reimbursed through the hospital provider and cannot be claimed by the hospital-based FQHC.
Line 1.--Enter the health care staff cost from Worksheet N-1, column 7, sum of lines 23, and 25 through 36, in columns 1 and 2, as applicable. Physician services under agreement are excluded from this total.
Line 2.--Enter the ratio of the estimated percentage of time involved in administering pneumococcal and influenza vaccine injections to the total health care staff time. Do not include physician service under agreement time in this calculation. Obtain the estimated percentage of time spent from your accounting books and records.
Line 3.--Multiply the amount on line 1 by the amount on line 2 and enter the result.
Line 4.--Enter the cost of pneumococcal and influenza vaccines and the cost of related medical supplies from Worksheet N-1 column 7, lines 47 and 48, in columns 1 and 2, respectively.
Line 5.--Enter the sum of lines 3 and 4.
Line 6.--Enter the total direct costs of the facility from Worksheet N-1, column 7, line 100.
Line 7.--Enter the administrative overhead of the facility from Worksheet N-1, column 7, line 8.
Line 8.--Divide the amount on line 5 by the amount on line 6 and enter the result.
Line 9.--Multiply the amount on line 7 by the ratio on line 8 and enter the result.
Line 10.--Enter the sum of the amounts on lines 5 and 9.
Line 11.--Enter in columns 1 and 2 respectively, the total number of pneumococcal and influenza vaccine injections from your records.
Line 12.--Compute the cost per pneumococcal and influenza vaccine injection by dividing the costs on line 10 by the number of injections on line 11 and entering the result.
Line 13.--Enter from your records the number of pneumococcal and influenza vaccine injections administered to Medicare beneficiaries, in columns 1 and 2 respectively.
Line 14.--Enter the Medicare cost per pneumococcal and influenza vaccine injection by multiplying the cost per vaccine on line 12 by the number of injections administered to Medicare beneficiaries on line 13.
Line 15.--Enter the total cost of pneumococcal and influenza vaccine and administration by entering the sum of the amounts in columns 1 and 2, line 10.
Line 16.--Enter the Medicare cost of pneumococcal and influenza vaccine and administration by entering the sum of the amount in columns 1 and 2, line 14. Transfer this amount to the Worksheet N-4, line 2.
Rev. 40-297
4071.3 FORM CMS-2552-10 DRAFT
4071.3. WORKSHEET N-4 - CALCULATION OF HOSPITAL-BASED FQHC REIMBURSEMENT SETTLEMENT
This worksheet provides for the reimbursement calculation for hospital-based FQHC services rendered to program patients under the FQHC PPS. It also provides for an accumulation of pneumococcal and influenza vaccine reimbursement and Medicare Advantage (MA) supplemental payments.
Line 1--FQHC services are paid in accordance with the FQHC PPS. Enter the total PPS payments for hospital-based FQHC visits rendered during the cost reporting period. Obtain this from the PS&R report.
Line 2--Enter the Medicare costs for pneumococcal and influenza vaccines and their administration from Worksheet N-3, line 16.
Line 3--Medicare advantage supplemental payments are made to a FQHC when the amount paid by the managed care organization is less than the amount paid under the FQHC PPS on a per visit basis. Enter the total amount of Medicare advantage supplemental payments from the PS&R 778 report. This data is captured for informational purposes only and does not impact cost report settlement.
Line 4--Enter the sum of lines 1 and 2.
Line 5--Enter the primary payer amounts from the PS&R.
Line 6--Enter the result of line 4 minus line 5.
Line 7--Enter the Part B coinsurance.
Line 8--Enter the result of line 6 minus line 7.
Line 9--Enter Medicare allowable bad debts, reduced by bad debt recoveries. If recoveries exceed the current year’s bad debts, lines 9 and 10 will be negative.
Line 10--Multiply the amount (including negative amounts) from line 9 by 65 percent.
Line 11--Enter the gross reimbursable bad debts for dual eligible beneficiaries. This amount is reported for statistical purposes only. These amounts also are included on line 9.
Line 12--Enter the sum of lines 8 and 10.
40-298 Rev.
DRAFT FORM CMS-2552-10 4071.3 (Cont.)
Line 13--This line is used to enter any other adjustments. Enter the amount in column 1 and include a description of the adjustment in the space provided.
Line 14--Enter the result of line 12 plus or minus line 13.
Line 15--Enter the sequestration adjustment amount as [(2 percent times (total days in the cost reporting period that occur during the sequestration period beginning on or after April 1, 2013, divided by total days in the entire cost reporting period, rounded to four decimal places)) times line 14]. Do not apply the sequestration calculation when gross reimbursement is less than zero.
Line 16--Enter the result of line 14 minus line 15.
Line 17--Enter the amount of interim payments from Worksheet N-5, column 2, line 4.
Line 18--FOR CONTRACTOR USE ONLY.--Enter the tentative settlement amount from Worksheet N-5, column 2, line 5.99.
Line 19--Enter the total amount due to/from the program (line 16 minus lines 17 and 18). Transfer this amount to Worksheet S, Part III, column 3, line 11.
Line 20--Enter the Medicare reimbursement effect of protested items. Estimate the reimbursement effect of the non-allowable items by applying a reasonable methodology which closely approximates the actual effect of the item as if it had been determined through the normal cost finding process. (See CMS Pub. 15-2, chapter 1, §115.2.) Attach a schedule showing the supporting details and computations for this line.
Rev. 40-299
4071.4 FORM CMS-2552-10 DRAFT
4071.4. WORKSHEET N-5 - ANALYSIS OF PAYMENTS TO HOSPITAL-BASED FQHC FOR SERVICES RENDERED
Complete lines 1 through 4 of this worksheet for Medicare interim payments only. The remainder of this worksheet is completed by your contractor.
Line descriptions
Line 1--Enter the total Medicare interim payments paid to the hospital-based FQHC. The amount entered must reflect the sum of all interim payments paid on individual bills (net of adjustment bills) for services rendered in this cost reporting period and amounts withheld from your interim payments due to an offset against overpayments applicable to prior cost reporting periods. Do not include MA supplemental payments on this worksheet. Do not include (1) any retroactive lump sum adjustment amounts based on a subsequent revision of the interim rate, (2) tentative or net settlement amounts, or (3) interim payments payable.
Line 2--Enter the total Medicare interim payments payable on individual bills. Since the cost in the cost report is on an accrual basis, this line represents the amount of services rendered in the cost reporting period but not paid as of the end of the cost reporting period. It does not include payments reported on line 1.
Line 3--Enter the amount of each retroactive lump sum adjustment and the applicable date.
Line 4--Enter the total amount of the interim payments (sum of lines 1, 2, and 3.99). Transfer this amount to Worksheet N-4, line 17.
DO NOT COMPLETE THE REMAINDER OF WORKSHEET N-5. LINES 5 THROUGH 8 ARE FOR CONTRACTOR USE ONLY. (EXCEPTION: IF WORKSHEET S, PART I, LINE 5 IS “5” (AMENDED COST REPORT), THE HOSPITAL-BASED FQHC MAY COMPLETE THIS SECTION.)
Line 5--List separately each tentative settlement payment after the cost report is accepted together with the date of payment. If the cost report is reopened after the NPR has been issued, report all settlement payments prior to the current reopening on this line.
Line 6--Enter the net settlement amount (balance due the hospital-based FQHC or balance due the program) for the NPR, or, if this settlement is after a reopening of the NPR, for this reopening. Enter in column 2, the amount from Worksheet N-4, line 19.
NOTE: On lines 3, 5, and 6, when a hospital-based FQHC to program amount is due, show the amount and date the FQHC agrees to the amount of repayment even though total repayment is not accomplished until a later date.
Line 7--Enter the sum of the amounts on lines 4, 5.99, and 6, in column 2. Enter amounts due the program as a negative number. The amount in column 2 must equal the amount on Worksheet N-4, line 16.
40-300 Rev.
DRAFT FORM CMS-2552-10 4072
4072. WORKSHEET O - ANALYSIS OF HOSPITAL-BASED HOSPICE COSTS
The O series of worksheets must be completed by all hospital-based hospices effective for cost reporting periods beginning on or after October 1, 2015. This worksheet is used to record the trial balance of expense accounts from the provider’s accounting books and records. It also provides for reclassifications and adjustments to certain accounts. The cost centers on this worksheet are listed in a manner that facilitates the combination of the various groups of cost centers for purposes of cost finding. Cost centers listed may not apply to every provider using these forms. Complete only those lines that are applicable.
Column Descriptions
For columns 1, 2, 4, and 6, direct patient care service costs (lines 25 through 46) are reported by LOC on Worksheets O-1, O-2, O‑3 and O-4. For each cost center on Worksheet O, enter the sum of the amounts from Worksheets O-1, O-2, O-3, and O-4 for salaries, other costs, reclassifications, and adjustments, in columns 1, 2, 4, and 6, respectively.
Column 1--Enter salaries from the provider’s accounting books and records. Salaries for the direct patient care service cost centers (lines 25 through 46) must equal the sum of amounts reported on the corresponding lines in column 1 of Worksheets O-1, O-2, O-3, and O-4. The total salaries for column 1, line 100, must equal the salaries reported on Worksheet A, column 1, line 116.
Column 2--Enter all costs other than salaries from the provider’s accounting books and records. Other costs for the direct patient care service cost centers (lines 25 through 46) must equal the sum of amounts reported on the corresponding lines in column 2 of Worksheets O-1, O-2, O-3, and O-4. The total other costs for column 2, line 100, must equal the other costs reported on Worksheet A, column 2, line 116.
Column 3--For each cost center, enter the total of column 1 plus 2.
Column 4--Enter any reclassifications among cost center expenses in column 3 that are needed to effect proper cost allocation. This column need not be completed by all providers, but is completed only to the extent reclassifications are needed or reported on Worksheet A, line 116. Show reductions to expenses as negative amounts.
If reclassifications are needed for direct patient care service cost centers (lines 25 through 46), enter the reclassification amounts on the appropriate Worksheets O-1, O-2, O-3, and O-4, column 4, for each level of care.
Reclassifications for the direct patient care service cost centers (lines 25 through 46) must equal the sum of amounts reported on the corresponding lines in column 4 of Worksheets O-1, O-2, O‑3, and O-4. The total reclassifications for column 4, line 100, must equal the reclassifications reported on Worksheet A, column 4, line 116.
Column 5--For each cost center, enter the total of the amount in column 3 plus or minus the amount in column 4.
Rev. 40-301
4072 (Cont.) FORM CMS-2552-10 DRAFT
Column 6--In accordance with 42 CFR 413.9(c)(3), enter on the appropriate lines, the amounts of any adjustments to expenses required under Medicare principles of reimbursements. (See §4016.) This column need not be completed by all providers, but is completed only to the extent adjustments are needed or reported on Worksheet A, column 6, line 116. Show reductions to expenses as negative amounts.
If adjustments are needed for direct patient care service cost centers (lines 25 through 46), enter the adjustment amounts on the appropriate Worksheets O-1, O-2, O-3, and O-4, column 6, for each level of care.
Adjustments for the direct patient care service cost centers (lines 25 through 46) must equal the sum of amounts reported on the corresponding lines in column 6 of Worksheets O-1, O-2, O-3, and O-4. The total adjustments for column 6, line 100, must equal the adjustments reported on Worksheet A, column 6, line 116.
Column 7--For each cost center, enter the total of the amount in column 5 plus or minus the amount in column 6. Transfer the amounts in column 7 for cost centers marked with an asterisk (*) to Worksheet O-5, as follows:
From Worksheet O, Column 7,
Line Number and To Worksheet O-5,
Cost Center Description Column 1:
1 Cap Rel Costs-Bldg & Fixt line 1
2 Cap Rel Costs-Mvble Equip line 2
3 Employee Benefits line 3
4 Administrative & General line 4
5 Plant Operation and Maintenance line 5
6 Laundry & Linen line 6
7 Housekeeping line 7
8 Dietary line 8
9 Nursing Administration line 9
10 Routine Medical Supplies line 10
11 Medical Records line 11
12 Staff Transportation line 12
13 Volunteer Service Coordination line 13
14 Pharmacy line 14
15 Physician Administrative Services line 15
16 Other General Service line 16
60 Bereavement Program line 60
61 Volunteer Program line 61
62 Fundraising line 62
63 Hospice/Palliative Medicine Fellows line 63
64 Palliative Care Program line 64
65 Other Physician Services line 65
66 Residential Care line 66
67 Advertising line 67
68 Telehealth/Telemonitoring line 68
69 Thrift Store line 69
70 Nursing Facility Room and Board line 70
71 Other Nonreimbursable line 71
Line Descriptions
The Worksheet O cost centers are segregated into general service, direct patient care service, and nonreimbursable categories to facilitate the transfer of costs to the various worksheets. The general service cost centers appear on Worksheet O-5, and Worksheets O-6, Parts I and Part II, using the same line numbers as Worksheet O. The direct patient care service cost centers appear on Worksheets O-1, O-2, O-3, and O-4 using the same line numbers as Worksheet O.
40-302 Rev.
DRAFT FORM CMS-2552-10 4072 (Cont.)
General service cost centers (lines 1 through 17) include expenses incurred in operating the facility as a whole that are not directly associated with furnishing patient care such as mortgage, rent, plant operations, administrative salaries, utilities, telephone, and computer hardware and software costs. Except where descriptions are provided below, see §4013 for descriptions of general service cost centers.
Lines 1 and 2 - Cap Rel Costs-Bldg & Fixt and Cap Rel Costs-Mvble Equip--Enter in column 2, the capital-related costs for buildings and fixtures and the capital-related costs for moveable equipment on lines 1 and 2, respectively.
Line 3 - Employee Benefits Department--Enter in columns 1 and 2, the salary and other costs of the employee benefits department and fringe benefits paid (see CMS Pub. 15-1, chapter 21, §2144 and CMS Pub. 15-1, chapter 23, §2307).
Line 4 - Administrative & General--Enter in columns 1 and 2, the salary and other costs of A&G.
If the option to subscript A&G costs into more than one cost center is elected (in accordance with CMS Pub. 15-1, chapter 23, §2313), eliminate line 4. Begin numbering the subscripted A&G cost centers with line 4.01 and continue in sequential order.
Line 5 - Plant Operation and Maintenance--This cost center includes expenses incurred in the operation and maintenance of the plant and equipment (see §4013, Maintenance and repairs, and Operation of plant). Enter in columns 1 and 2, the costs of plant operation and maintenance.
Line 6 - Laundry & Linen Service--Enter in columns 1 and 2, the cost of routine laundry and linen services.
Line 7 - Housekeeping--Enter in columns 1 and 2, the cost of routine housekeeping activities for both patient related and non-patient related areas.
Line 8 - Dietary--Enter in columns 1 and 2, the cost of preparing meals for patients. Do not include the cost of dietary counseling in this cost center; report dietary counseling on line 35.
Line 9 - Nursing Administration--Enter in columns 1 and 2, the cost of overall management and direction of the nursing services. Do not include the cost of direct nursing services reported on lines 27 through 29. The salary cost of direct nursing services, including the salary cost of nurses who render direct service in more than one patient care area, is directly assigned to the various patient care cost centers in which the services were rendered. However, if your accounting system fails to specifically identify all direct nursing services to the applicable direct patient care cost centers, then the salary cost of all direct nursing service is included in this cost center.
Line 10 - Routine Medical Supplies--Enter in columns 1 and 2, the cost of supplies used in the normal course of caring for patients, such as gloves, masks, swabs, or glycerin sticks, that generally are not traceable to individual patients. Do not include the costs of non-routine medical supplies that can be traced to individual patients; report non-rou7tine medical supplies on line 42.
Line 11 - Medical Records--Enter in columns 1 and 2, the cost of the medical records department where patient medical records are maintained. The general library and the medical library are not included in this cost center but are included in the A&G cost center.
Rev. 40-303
4072 (Cont.) FORM CMS-2552-10 DRAFT
Line 12 - Staff Transportation--Enter in columns 1 and 2, the cost of owning or renting vehicles, public transportation expenses, parking, tolls, or payments to employees for driving their private vehicles to see patients or for other hospice business. Staff transportation costs do not include patient transportation costs; report patient transportation costs on line 39.
Line 13 - Volunteer Service Coordination--Enter in columns 1 and 2, the cost of the overall coordination of service volunteers including their recruitment and training costs of volunteers.
Line 14 - Pharmacy--Enter in columns 1 and 2, the costs of drugs (both prescription and over-the-counter), pharmacy supplies, pharmacy personnel, and pharmacy services. Do not report the cost of palliative chemotherapy drugs on this line; report the cost of palliative chemotherapy on line 45.
Line 15 - Physician Administrative Services--Enter in columns 1 and 2, the costs for physicians’ A&G supervisory activities that are included in the hospice payment rates. These activities include participating in the establishment, review and updating of plans of care, supervising care and services, conducting required face-to-face encounters for recertification, and establishing governing policies. These activities are generally performed by the physician serving as the medical director and the physician member of the interdisciplinary group. Nurse practitioners may not serve as or replace the medical director or physician member of the interdisciplinary group.
Line 17 - Patient/Residential Care Services--Do not use this line on this worksheet. This cost center is used on Worksheet O-6 to accumulate in-facility costs not separately identified as HIRC, HGIP, or residential care services that are not part of a separate and distinct residential care unit (e.g., depreciation related to in-facility areas that provide HIRC, HGIP or residential care). The amounts allocated to this cost center on Worksheet O-6 are allocated to HIRC, HGIP and residential care services that are not part of a separate and distinct residential care unit, based on in-facility days. This cost center does not include any costs related to contracted inpatient services.
When a residential care unit is separate and distinct and only used for resident care services (such as hospice home care provided in a residential unit), costs are reported directly on line 66.
Lines 18 through 24--Reserved for future use.
Direct patient care service costs (lines 25 through 46) are reported by LOC on Worksheets O-1, O-2, O‑3 and O-4. For each cost center on Worksheet O, enter the sum of the amounts from Worksheets O-1, O-2, O-3, and O-4 for salaries, other costs, reclassifications, and adjustments in columns 1, 2, 4, and 6, respectively.
Line 25- Inpatient Care - Contracted--This cost center includes the contractual costs paid to another facility for use by the hospice for hospice inpatient care (HIRC or HGIP) in accordance with 42 CFR 418.108(c). This cost center does not include the cost of any direct patient care services or nonreimbursable services provided by hospice staff in the contracted setting. Costs of any services provided by hospice staff in the contracted setting are included in the appropriate direct patient care service or nonreimbursable cost center. Costs in this cost center are excluded from the allocation of A&G costs.
40-304 Rev.
DRAFT FORM CMS-2552-10 4072 (Cont.)
Line 26 - Physician Services--This cost center includes the costs incurred by the hospice for physicians, or nurse practitioners providing physician services, for direct patient care services and general supervisory services, participation in the establishment of plans of care, supervision of care and services, periodic review and updating of plans of care, and establishment of governing policies by the physician member of the interdisciplinary group. (See 42 CFR 418.304.) Reclassify the cost for the portion of time physicians spent on general supervisory services or other hospice administrative activities to Physician Administrative Services (line 15). This cost center must not include costs associated with palliative care or other nonreimbursable physician services. Those nonreimbursable physician services must be reported in the appropriate nonreimbursable cost center.
Line 27 - Nurse Practitioner--This cost center includes the costs of nursing care provided by nurse practitioners. Do not include costs for nurse practitioners providing physician services on this line; report the costs for nurse practitioners providing physician services on line 26.
Line 28 - Registered Nurse--This cost center includes the costs of nursing care provided by registered nurses other than nurse practitioners.
Line 29 - LPN/LVN--This cost center includes the costs of nursing care provided by licensed practical nurses (LPN) or licensed vocational nurses (LVN). Do not include costs for certified nursing assistant (CNA) services on this line; report the costs for CNA services on line 37.
Line 30 - Physical Therapy--This cost center includes the costs of physical or corrective treatment of bodily or mental conditions by the use of physical, chemical, and other properties of heat, light, water, electricity, sound massage, and therapeutic exercise by or under the direction of a registered physical therapist as prescribed by a physician. Physical therapy services may be provided for purposes of symptom control or to enable the individual to maintain activities of daily living and basic functional skills.
Line 31 - Occupational Therapy--This cost center includes the costs of purposeful goal-oriented activities in the evaluation, diagnosis, and/or treatment of persons whose function is impaired by physical illness or injury, emotional disorder, congenital or developmental disability, or the aging process, in order to achieve optimum functioning, to prevent disability, and to maintain health. Occupational therapy services may be provided for purposes of symptom control or to enable the individual to maintain activities of daily living and basic functional skills.
Line 32 - Speech/Language Pathology--This cost center includes the costs of physician-prescribed services provided by or under the direction of a qualified speech/language pathologist to those with functionally impaired communications skills. This includes the evaluation and management of any existing disorders of the communication process centering entirely, or in part, on the reception and production of speech and language related to organic and/or nonorganic factors. Speech/language pathology services may be provided for purposes of symptom control or to enable the individual to maintain activities of daily living and basic functional skills.
Line 33 - Medical Social Services--This cost center includes the cost of the medical social services defined in CMS Pub. 100-02, chapter 9, §40.1.2. Costs for nonreimbursable activities included in this cost center must be reclassified to the appropriate nonreimbursable cost center.
Line 34 - Spiritual Counseling--This cost centers includes the cost of spiritual counseling services. Costs for nonreimbursable activities included in this cost center must be reclassified to the appropriate nonreimbursable cost center.
Line 35 - Dietary Counseling--This cost center includes the costs of dietary counseling services.
Rev. 40-305
4072 (Cont.) FORM CMS-2552-10 DRAFT
Line 36 - Counseling - Other--This cost center include the cost of counseling services not already identified as spiritual, dietary or bereavement counseling. Costs for nonreimbursable activities included in this cost center must be reclassified to the appropriate nonreimbursable cost center.
Line 37 - Hospice Aide and Homemaker Services--This cost center includes the costs of:
Hospice aide services such as personal care services and household services to maintain a safe and sanitary environment in areas of the home used by the patient; and,
Homemaker services such as assistance in the maintenance of a safe and healthy environment and services to enable the individual to carry out the plan of care.
Include the cost of CNAs that meet the criteria for an aide in this cost center.
Line 38 - Durable Medical Equipment/Oxygen--This cost center includes the costs of DME and oxygen, as defined in 42 CFR 410.38 and 42 CFR 418.202(f), furnished to individual HRHC or HCHC patients. Report DME costs by the LOC the patient was receiving at the time the DME/oxygen was delivered. If the LOC of a patient changed after delivery of the DME/Oxygen, the hospice may report the costs proportionally between HRHC and HCHC based on patient days.
Line 39 - Patient Transportation--This cost center includes the costs of ambulance transports of hospice patients, related to the terminal prognosis and occurring after the effective date of the hospice election, that are the responsibility of the hospice. (See CMS Pub. 100-02, chapter 9, §40.1.9.) When a patient is transferred to a new LOC, report the transportation cost to that LOC. For example, a patient in a HGIP LOC is transferred to HRHC LOC and transported to their home, the transportation cost associated with the transfer must be included in the HRHC LOC.
Line 40 - Imaging Services--This cost center includes the costs of imaging services.
Line 41 - Labs and Diagnostics--This cost center includes the costs of laboratory and diagnostic tests.
Line 42 - Medical Supplies - Non-routine--This cost center includes the costs of medical supplies furnished to individual patients for which a separate charge would be applicable. These supplies are specified in the patient's plan of treatment and furnished under the specific direction of the patient's physician. Do not include the cost of routine medical supplies used in the normal course of caring for patients, (such as gloves, masks, swabs, or glycerin sticks) on this line; report routine medical supplies on line 10. When a provider does not track the use of non‑routine medical supplies by LOC, the provider may report the costs proportionally between LOCs based on patient days.
Line 43 - Outpatient Services--This cost center includes the costs of outpatient services costs not captured elsewhere. This cost can include the cost of an emergency room department visit when related to the terminal condition.
Lines 44 and 45 - Palliative Radiation Therapy and Palliative Chemotherapy--These cost centers include costs of radiation, chemotherapy and other modalities used for palliative purposes based on the patient’s condition and the hospice’s caregiving philosophy.
Lines 47 through 49--Reserved for future use.
40-306 Rev.
DRAFT FORM CMS-2552-10 4072 (Cont.)
Lines 50 through 53--Reserved for use on Worksheets O-6, Parts I and II.
Lines 54 through 59--Reserved for future use.
Nonreimbursable cost centers (lines 60 through 71) include costs of nonreimbursable services and programs. Report the costs applicable to nonreimbursable cost centers to which general service costs apply. If additional lines are needed for nonreimbursable cost centers other than those shown, subscript one or more of these lines with a numeric code. The subscripted lines must be appropriately labeled to indicate the purpose for which they are being used. However, when the expense (direct and all applicable overhead) attributable to any non-allowable cost area is so insignificant as to not warrant establishment of a nonreimbursable cost center, remove the expense on Worksheet A-8. (See CMS Pub. 15-1, chapter 23, §2328.)
Line 60 - Bereavement Program--Enter in columns 1 and 2, the salary and other costs of bereavement services, defined as emotional, psychosocial, and spiritual support and services provided before and after the death of the patient to assist with grief, loss, and adjustment (42 CFR 418.3). Bereavement counseling is a required hospice service, but it is not reimbursable (see §1814(I)(1)(A) of the Act).
Line 61 - Volunteer Program--Enter in columns 1 and 2, the salary and other costs of volunteer programs. (See CMS Pub. 15-1, chapter 7.)
Line 62 - Fundraising--Enter in columns 1 and 2, the salary and other costs of fundraising. (See CMS Pub. 15-1, chapter 21, §2136.)
Line 63 - Hospice/Palliative Medicine Fellows--Enter in columns 1 and 2, the salary and other costs of hospice and palliative medicine fellows.
Line 64 - Palliative Care Program--Enter in columns 1 and 2, the salary and other costs of palliative care provided to non-hospice patients. This includes physician services.
Line 65 - Other Physician Services--Enter in columns 1 and 2, the salary and other costs of other physician services that are provided outside of a palliative care program to non-hospice patients.
Line 66 - Residential Care--Enter in columns 1 and 2, the salary and other costs of residential care for patients living in the hospice, but who are not receiving inpatient hospice services. Patients living in the hospice are considered residents, where the hospice is their home. These patients are liable for their room and board charges; however, the outpatient hospice care services provided must be recorded in the direct patient care cost centers on the appropriate HRHC and/or HCHC LOC worksheet.
Lines 67 - Advertising--Enter in columns 1 and 2, the salary and other costs of nonallowable community education, business development, marketing and advertising (see CMS Pub. 15-1, chapter 21, §2136).
Lines 68 - Telehealth/Telemonitoring--Enter in columns 1 and 2, the salary and other costs of telehealth/ telemonitoring services. These costs are nonreimbursable since a hospice is not an approved originating site (see 42 CFR 410.78(b)(3)).
Lines 69 - Thrift Store--Enter in columns 1 and 2, the salary and other costs of thrift stores.
Rev. 40-307
4072.1 FORM CMS-2552-10 DRAFT
Line 70 - Nursing Facility Room and Board--Enter the costs incurred by a hospice for dually eligible beneficiaries residing in a nursing facility (NF) when room and board is paid by the State to the hospice. The full amount paid to the NF by the hospice must be included on this line and offset by the State payment via an adjustment on Worksheet A-8. The residual cost is the net cost incurred.
For example, a dually eligible beneficiary is residing in a NF and has elected the Medicare hospice benefit. The NF charges $100 per day for room and board. The State pays the hospice $95 for the NF room and board. The hospice has a written agreement with the NF that requires full room and board payment of $100 per day. The hospice receives $95 per day, but pays the NF $100 per day, thereby incurring a net cost of $5 per day.
Lines 72 through 99--Reserved for future use.
4072.1. WORKSHEETS O-1, O-2, O-3, AND O-4 - ANALYSIS OF HOSPITAL-BASED HOSPICE COSTS
Worksheet O-1 - Analysis of Hospital-Based Hospice Costs Hospice Continuous Home Care
Worksheet O-2 - Analysis of Hospital-Based Hospice Costs Hospice Routine Home Care
Worksheet O-3 - Analysis of Hospital-Based Hospice Costs Hospice Inpatient Respite Care
Worksheet O-4 - Analysis of Hospital-Based Hospice Costs Hospice General Inpatient Care
Worksheets O-1, O-2, O-3, and O-4 provide for recording the direct patient care costs by LOC, including reclassifications and adjustments. The general format of these worksheets is identical to Worksheet O in order to facilitate the transfer of direct patient care costs to Worksheet O. For each cost center, the sums of the amounts reported in columns 1, 2, 4, and 6 of these worksheets are transferred to the corresponding columns on Worksheet O.
Column 1--For each LOC worksheet, enter salaries from the provider’s accounting books and record.
Column 2--For each LOC worksheet, enter all costs other than salaries from the provider’s accounting books and records.
Column 3--For each cost center, add the amounts in columns 1 and 2 and enter the total in column 3.
Column 4--For each LOC worksheet, enter any reclassification of direct patient care service costs needed to effect proper cost allocation. For each line, the sum of the reclassification entries on Worksheets O-1, O-2, O-3, and O-4, column 4, must equal the amount on the corresponding line of Worksheet O, column 4.
Column 5--For each cost center, enter the total of the amount in column 3 plus or minus the amount in column 4.
Column 6--For each LOC worksheet, enter any adjustments for direct patient care service costs (lines 25 through 46) required under Medicare principles of reimbursements. (See §4016.) Show reductions to expenses as negative amounts. For each line, the sum of the adjustment entries on Worksheets O-1, O-2, O-3 and O-4, column 6, must equal the amount on the corresponding line of Worksheet O, column 6.
40-308 Rev.
DRAFT FORM CMS-2552-10 4072.2
Column 7--For each cost center, enter the total of the amount in column 5 plus or minus the amount in column 6. For each LOC worksheet, transfer the amount on line 100 to the corresponding LOC line on Worksheet O-5, column 1, as follows:
From line 100 of: To Worksheet O-5, column 1, line:
Worksheet O-1 50
Worksheet O-2 51
Worksheet O-3 52
Worksheet O-4 53
4072.2. WORKSHEET O-5 - COST ALLOCATION - DETERMINATION OF HOSPITAL-BASED HOSPICE NET EXPENSES FOR ALLOCATION
Worksheet O-5 determines total expenses of each general service cost center for proper allocation of general service costs to each LOC and to nonreimbursable cost centers. This worksheet combines the direct general service costs reported on Worksheet O, lines 1 through 17 with the overhead allocation of the hospital general service costs reported on Worksheet B Part I, line 116, columns 1 through 18.
Column Descriptions
Column 1--For each general service and nonreimbursable cost center, transfer the amount from the corresponding cost center on Worksheet O, column 7. For each LOC line, transfer amounts as follows:
From column 7,
Line: line 100 of:
50 Worksheet O-1
51 Worksheet O-2
52 Worksheet O-3
53 Worksheet O-4
The total on line 100 of column 1 must equal the amount on Worksheet A, column 7, line 116.
Column 2--For each general service cost center, transfer the amount from the corresponding column on Worksheet B, Part I, line 116 as follows:
From Worksheet B, From Worksheet B,
Line: line 116, column(s): Line: line 116, column(s):
1 1 10 14
2 2 11 16
3 4 12 N/A
4 5, 11, and 12 13 N/A
5 6 and 7 14 15
6 8 15 N/A
7 9 16 18
8 10 17 17
9 13
Column 3--For each line, enter the sum of columns 1 and 2. The total on line 100 of column 3 must equal the amount on Worksheet B, Part I, column 26, line 116. Transfer the amount from each cost center to the corresponding line on Worksheet O-6, Part I, column 0.
Rev. 40-309
4072.3 FORM CMS-2552-10 DRAFT
4072.3. WORKSHEET O-6 - PART I - COST ALLOCATION - HOSPITAL-BASED HOSPICE GENERAL SERVICE COSTS AND WORKSHEET O-6 - PART II - COST ALLOCATION - HOSPITAL-BASED HOSPICE GENERAL SERVICE COSTS STATISTICAL BASIS
In accordance with 42 CFR 413.24, cost data must be based on an approved method of cost finding and on the accrual basis of accounting except where governmental institutions operate on a cash basis of accounting.
Worksheet O-6, Parts I and II, facilitate the step-down method of cost finding. This method recognizes that general services of the hospice are utilized by other general service, LOC, and nonreimbursable cost centers. Worksheet O-6, Part I provides for the equitable allocation of general service costs based on statistical data reported on Worksheet O-6, Part II. To facilitate the allocation process, the general format of Worksheet O-6, Part I is identical to that of Worksheet O-6, Part II. The column and line numbers for each general service cost center are identical on the two worksheets. The direct patient care service cost centers (lines 25 through 46 of Worksheet O) are reported by LOC on lines 50 through 53 of Worksheets O-6, Parts I and II. The line numbers for nonreimbursable cost centers are identical on Worksheet O and Worksheet O-6, Parts I and II.
When certain general service costs are related to in-facility days and are not separately identifiable by LOC or service, Worksheet O-6, Parts I and II, provide for the accumulation of these costs on line 17, Patient/Residential Care Services. The amounts accumulated in this cost center are allocated based on the in-facility days for HIRC, HGIP, and residential care services that are not part of a separate and distinct residential care unit. This cost center does not include any costs related to contracted inpatient services.
The statistical basis shown at the top of each column on Worksheet O-6, Part II is the recommended basis of allocation. The total statistic for cost centers using the same basis (e.g., square feet) may differ with the closing of preceding cost centers. A hospice can elect to change the order of allocation and/or allocation statistics, as appropriate, for the current cost reporting period if a request is submitted in accordance with CMS Pub. 15-1, chapter 23, §2313.
Close the general service cost centers in accordance with 42 CFR 413.24(d)(1) so that the cost centers rendering the most services to and receiving the least services from other cost centers are closed first (see CMS Pub. 15-1, chapter 23, §2306.1). If a more accurate result is obtained by allocating costs in a sequence that differs from the recommended sequence, the hospice must request approval in accordance with CMS Pub. 15-1, chapter 23, §2313.
If the amount of any cost center on Worksheet O-5, column 3, has a negative balance, show this amount as a negative balance on Worksheet O-6, Part I, column 0. Allocate the costs from the overhead cost centers to applicable cost centers, including those with a negative balance. Close a general service cost center with a negative balance by entering the negative balance in parentheses on the first line and on line 100 of the column, and do not allocate. This enables Worksheet O-6, Part I, column 18, line 101 to cross foot to Worksheet O-6, Part I, column 0, line 101. After receiving costs from overhead cost centers, LOC cost centers with negative balances on Worksheet O-6, Part I, column 18, are not transferred to Worksheet O-7.
40-310 Rev.
DRAFT FORM CMS-2552-10 4072.3 (Cont.)
On Worksheet O-6, Part II, enter on the first available line of each column the total statistics applicable to the cost center being allocated (e.g., in column 1, Capital-Related Cost - Buildings & Fixtures, enter on line 1 the total square feet of the building on which depreciation was taken). Use accumulated cost for allocating A&G expenses.
Such statistical base, including accumulated cost for allocating A&G expenses, does not include any statistics related to services furnished under arrangements except where:
Both Medicare and non-Medicare costs of arranged for services are recorded in the hospice’s books/records; or
The contractor determines that the hospice is able to and does gross up the costs and charges for services to non-Medicare patients so that both cost and charges are recorded as if the hospice had furnished such services directly to all patients. (See CMS Pub. 15-1, chapter 23, §2314.)
For each cost center being allocated, enter that portion of the total statistical base applicable to each cost center receiving services. For each column, the sum of the statistics entered for cost centers receiving services must equal the total statistical base entered on the first line.
For each column on Worksheet O-6, Part II, enter on line 101, the total expenses of the cost center to be allocated. Obtain the total expenses from the first line of the corresponding column on Worksheet O-6, Part I, which includes the direct expenses from Worksheet O-6, Part I, column 0 plus the allocated costs from previously closed cost centers. Divide the amount entered on Worksheet O-6, Part II, line 101 by the total statistical base entered in the same column on the first line. Enter the resulting unit cost multiplier (rounded to six decimal places) on line 102.
For each column on Worksheet O-6, Part II, multiply the unit cost multiplier on line 102 by the portion of the total statistical base applicable to each cost center receiving services and enter the result in the corresponding column and line on Worksheet O-6, Part I. For each column on Worksheet O-6, Part I, the sum of the costs allocated (line 100) must equal the total cost on the first line.
After the costs of the general service cost centers have been allocated on Worksheet O-6, Part I, enter on each line of column 18, the sum of the costs in columns 3A through column 17 for lines 50 through 71. The total costs entered on Worksheet O-6, Part I, column 18, line 100 must equal the total costs entered in column 0, line 100.
Column Descriptions
Column 0--For each line, enter the total direct costs from the corresponding line on Worksheet O-5, column 3.
Column 3A--For each line, enter the sum of columns 0 through 3. The sum for each line is the accumulated cost and, unless an adjustment is required, is the Worksheet O-6, Part II, column 4 statistic for allocating A&G costs.
If an adjustment to the accumulated cost statistic on Worksheet O-6, Part II, column 4, is required to properly allocate A&G costs, enter the adjustment amount on Worksheet O-6, Part II, column 4A for the applicable line. For example, when the hospice contracts for HIRC or HGIP services and the contractual costs include A&G costs, the contractual costs reported on Worksheet O-3, column 7, line 25, or Worksheet O-4, column 7, line 25, may be used to reduce the accumulated cost statistic on Worksheet O-6, Part II, column 4A, line 52 or line 53, respectively.
Rev. 40-311
4072.4 FORM CMS-2552-10 DRAFT
For each line, the accumulated cost statistic on Worksheet O-6, Part II, column 4, is the difference between the amount on Worksheet O-6, Part I, column 3A and the adjustment amount on Worksheet O-6, Part II, column 4A. Accumulated cost for A&G is not included in the total statistic for the A&G cost center; therefore, transfer the amount on Worksheet O-6, Part I, column 3A, line 4, to Worksheet O-6, Part II, column 4A, line 4.
The total accumulated cost statistic for Worksheet O-6, Part II, column 4, line 4 is the difference between the total on Worksheet O-6, Part I, column 3A, line 101 and the amounts in column 4A of Worksheet O-6, Part II.
A negative cost center balance in the statistics for allocating A&G expenses causes an improper distribution of this overhead cost center. Negative balances are excluded from the allocation statistics when A&G expenses are allocated on the basis of accumulated cost.
Column 18--Transfer the amounts on lines 50 through 53 as follows:
From Worksheet O-6, Part I, To Worksheet O-8,
column 18: column 3:
line 50 line 1
line 51 line 6
line 52 line 11
line 53 line 16
4072.4. WORKSHEET O-7 - APPORTIONMENT OF HOSPITAL-BASED HOSPICE SHARED SERVICE COSTS BY LEVEL OF CARE
This worksheet calculates the cost of ancillary services provided by hospital ancillary departments to hospital-based hospice patients.
Column Description
 Column
1--For each cost center,
enter in column 1, the cost-to-charge ratio from Worksheet C, Part I,
column 9, line as indicated in column 0.
Column
1--For each cost center,
enter in column 1, the cost-to-charge ratio from Worksheet C, Part I,
column 9, line as indicated in column 0.
Columns 2 through 5--For each cost center, enter the charges, from the provider’s records, for ancillary services provided by hospital ancillary departments to hospital-based hospice patients. Enter the charges by LOC in the appropriate LOC column.
Columns 6 through 9--For each column, calculate cost of ancillary services provided by hospital ancillary departments to hospital-based hospice patients as follows:
Column: Calculation:
6 col. 1 x col. 2
7 col. 1 x col. 3
8 col. 1 x col. 4
9 col. 1 x col. 5
For each column 6 through 9, enter the sum of lines 1 through 10 on line 11.
40-312 Rev.
DRAFT FORM CMS-2552-10 4072.5
4072.5. WORKSHEET O-8 - CALCULATION OF HOSPITAL-BASED HOSPICE PER DIEM COST
Worksheet O-8 calculates the average cost per diem by level of care and in total.
Line1--Enter in column 3, the sum of the total HCHC cost from Worksheet O-6, Part I, column 18, line 50, plus Worksheet O-7, column 6, line 11.
Line 2--Enter in column 3, the total HCHC days from Worksheet S-9, column 4, line 10.
Line 3--Enter in column 3, the average HCHC cost per diem by dividing column 3, line 1 by column 3, line 2.
Line 4--Enter in column 1, the title XVIII - Medicare HCHC days from Worksheet S-9, column 1, line 10. Enter in column 2 the title XIX - Medicaid HCHC days from Worksheet S-9, column 2, line 10.
Line 5--Enter in column 1, the title XVIII - Medicare program cost calculated by multiplying column 3, line 3 by column 1, line 4. Enter in column 2 the title XIX - Medicaid program cost calculated by multiplying column 3, line 3 by column 2, line 4.
Line 6--Enter in column 3, the total HRHC cost from Worksheet O-6, Part I, column 18, line 51, plus Worksheet O-7, column 7, line 11.
Line 7--Enter in column 3, the total HRHC days from Worksheet S-9, column 4, line 11.
Line 8--Enter in column 3, the average HRHC cost per diem by dividing column 3, line 6 by column 3, line 7.
Line 9--Enter in column 1, the title XVIII - Medicare HRHC days from Worksheet S-9, column 1, line 11. Enter in column 2 the title XIX - Medicaid HRHC days from Worksheet S-9, column 2, line 11.
Line 10--Enter in column 1 the title XVIII - Medicare program cost calculated by multiplying column 3, line 8 by column 1, line 9. Enter in column 2, the title XIX - Medicaid program cost calculated by multiplying column 3, line 8 by column 2, line 9.
Line 11--Enter in column 3, the total HIRC cost from Worksheet O-6, Part I, column 18, line 52, plus Worksheet O-7, column 8, line 11.
Line 12--Enter in column 3, the total HIRC days from Worksheet S-9, column 4, line 12.
Line 13--Enter in column 3, the average HIRC cost per diem by dividing column 3, line 11 by column 3, line 12.
Line 14--Enter in column 1, the title XVIII - Medicare HIRC days from Worksheet S-9, column 1, line 12. Enter in column 3 the title XIX - Medicaid HIRC days from Worksheet S-9, column 2, line 12.
Line 15.--Enter in column 1, the title XVIII - Medicare program cost calculated by multiplying column 3, line 13 by column 1, line 14. Enter in column 2 the title XIX - Medicaid program cost calculated by multiplying column 3, line 13 by column 2, line 14.
Line 16--Enter in column 3, the total HGIP cost from Worksheet O-6, Part I, column 18, line 53, plus Worksheet O-7, column 9, line 11.
Line 17--Enter in column 3, the total HGIP days from Worksheet S-9, column 4, line 13.
Rev. 40-313
4072.5 (Cont.) FORM CMS-2552-10 DRAFT
Line 18--Enter in column 3, the average HGIP cost per diem by column 3, line 16 by column 3, line 17.
Line 19--Enter in column 1, the title XVIII - Medicare HGIP days from Worksheet S-9, column 1, line 13. Enter in column 3, the title XIX - Medicaid HGIP days from Worksheet S-9, column 2, line 13.
Line 20--Enter in column 1, the title XVIII - Medicare program cost calculated by multiplying column 3, line 18 by column 1, line 19. Enter in column 2 the title XIX - Medicaid program cost calculated by multiplying column 3, line 18 by column 2, line 19.



 Line
21--Enter in column 3, the
sum of lines 1, 6, 11 and 16.
Line
21--Enter in column 3, the
sum of lines 1, 6, 11 and 16.
Line 22--Enter in column 3, total days from Worksheet S-9, column 4, line 14.
 Line
23--Enter the average cost
per diem by dividing column 3, line 21, by column 3, line 22.
Line
23--Enter the average cost
per diem by dividing column 3, line 21, by column 3, line 22.
40-314 Rev.
DRAFT FORM CMS-2552-10 4090
EXHIBIT 1 - Form CMS-2552-10 Worksheets
The following is a listing of the Form CMS-2552-10 worksheets and the page number location. Changes to worksheets are indicated by redline on this and the subsequent page for this transmittal. Where only the page number changes, no redlining is indicated.
Worksheets Page(s)
Wkst. S, Parts I, II & III 40-503
Wkst. S-2, Part I 40-504 - 40-507
Wkst. S-2, Part II 40-508 - 40-509
Wkst. S-3, Part I 40-510 - 40-511
Wkst. S-3, Parts II & III 40-512 - 40-513
Wkst. S-3, Part IV 40-514
Wkst. S-3, Part V 40-515
Wkst. S-4 40-516
Wkst. S-5 40-517
Wkst. S-6 40-518
Wkst. S-7 40-519 - 40-520
Wkst. S-8 40-521
Wkst. S-9 40-522
Wkst. S-10 40-523
Wkst. S-11, Parts I - III 40-523.1 - 40-523.3
Wkst. A 40-524 - 40-526
Wkst. A-6 40-527
Wkst. A-7, Parts I - III 40-528
Wkst. A-8 40-529
Wkst. A-8-1 40-530
Wkst. A-8-2 40-531
Wkst. A-8-3, Parts I - VI 40-532 - 40-534
Wkst. B, Part I 40-535 - 40-543
Wkst. B, Part II 40-544 - 40-552
Wkst. B-1 40-553 - 40-561
Wkst. B-2 40-562
Wkst. C, Part I 40-563 - 40-564
Wkst. C, Part II 40-565 - 40-566
Wkst. D, Part I 40-567
Wkst. D, Part II 40-568
Wkst. D, Part III 40-569
Wkst. D, Part IV 40-570 - 40-571
Wkst. D, Parts V 40-572
Wkst. D-1, Part I 40-573
Wkst. D-1, Part II 40-574
Wkst. D-1, Parts III & IV 40-575
Wkst. D-2, Parts I - III 40-576 - 40-577
Wkst. D-3 40-578
Wkst. D-4, Part I 40-579
Wkst. D-4, Part II 40-580
Wkst. D-4, Part III 40-581
Wkst. D-5, Part I 40-582
Wkst. D-5, Part II 40-583
Wkst. D-5, Part III 40-583.1
Wkst. D-5, Part IV 40-583.2
Wkst. E, Part A 40-584 - 40-585
Wkst. E, Part B 40-586 - 40-587
Wkst. E-1, Part I 40-588
Rev. 40-501
4090 (Cont.) FORM CMS-2552-10 DRAFT
EXHIBIT 1 - Form CMS-2552-10 Worksheets (Cont.)
Worksheets Page(s)
Wkst. E-1, Part II 40-589
Wkst. E-2 40-590
Wkst. E-3, Part I 40-591
Wkst. E-3, Part II 40-592
Wkst. E-3, Part III 40-593
Wkst. E-3, Part IV 40-594
Wkst. E-3, Part V 40-595
Wkst. E-3, Part VI 40-596
Wkst. E-3, Part VII 40-597
Wkst. E-4 40-598 - 40-599
Wkst. G 40-600 - 40-601
Wkst. G-1 40-602
Wkst. G-2, Parts I & II 40-603
Wkst. G-3 40-604
Wkst. H 40-605
Wkst. H-1, Part I 40-606
Wkst. H-1, Part II 40-607
Wkst. H-2, Part I 40-608 - 40-610
Wkst. H-2, Part II 40-611 - 40-613
Wkst. H-3, Parts I-III 40-614
Wkst. H-4 40-615
Wkst. H-5 40-616
Wkst. I-1 40-617
Wkst. I-2 40-618
Wkst. I-3 40-619
Wkst. I-4 40-620
Wkst. I-5 40-621
Wkst. J-1, Part I 40-622 - 40-624
Wkst. J-1, Part II 40-625 - 40-627
Wkst. J-2, Part I 40-628
Wkst. J-2, Part II 40-629
Wkst. J-3 40-630
Wkst. J-4 40-631
Wkst. K 40-632
Wkst. K-1 40-633
Wkst. K-2 40-634
Wkst. K-3 40-635
Wkst. K-4, Part I 40-636
Wkst. K-4, Part II 40-637
Wkst. K-5, Part I 40-638 - 40-640
Wkst. K-5, Part II 40-641 - 40-643
Wkst. K-5, Part III 40-644
Wkst. K-6 40-645
Wkst. L 40-646
Wkst. L-1, Part I 40-647 - 40-655
Wkst. L-1, Part II 40-656
Wkst. L-1, Part III 40-657 - 40-658
Wkst. M-1 40-659
Wkst. M-2 40-660
Wkst. M-3 40-661
Wkst. M-4 40-662
Wkst. M-5 40-663
40-502 Rev.
DRAFT FORM CMS-2552-10 4090 (Cont.)
EXHIBIT 1 - Form CMS-2552-10 Worksheets
Worksheets Page(s)
Wkst. N-1 40-664 - 40-665
Wkst. N-2 40-666
Wkst. N-3 40-667
Wkst. N-4 40-668
Wkst. N-5 40-669
Wkst. O 40-670 - 40-671
Wkst. O-1 40-672
Wkst. O-2 40-673
Wkst. O-3 40-674
Wkst. O-4 40-675
Wkst. O-5 40-676
Wkst. O-6, Part I 40-677 - 40-678
Wkst. O-6, Part II 40-679 - 40-680
Wkst. O-7 40-681
Wkst. O-8 40-682
Rev. 40-503
4090 (Cont.) FORM CMS-2552-10 DRAFT
This page is reserved for future use.
40-504 Rev.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | CMS |
| File Modified | 0000-00-00 |
| File Created | 2021-01-24 |
© 2026 OMB.report | Privacy Policy