Record Abstraction
Emergency Epidemic Investigation Data Collections - Expedited Reviews
Appendix 1. Medical Record Abstraction Form
2014004XXX_Legionnaires' Disease_Alabama 2014
OMB: 0920-1011
Form Approved
OMB No. 0920-1011
Exp. Date 03/31/2017
Medical Record Abstraction Form
Medical Record Abstraction Form <Example. Modify to fit current outbreak.>
Legionnaires ’ disease in an Acute Care Hospital
Medical Record # ___________
Abstractor Initials: _________
Today’s Date: ____________ (mm/dd/yyyy)
Information Source (check all that apply):
____ hospital chart
____ other (if other specify) ______________
I. PATIENT INFORMATION
Name: __________________________________________________________
Gender: _______
DOB: _______________ Age: _____ Race/Ethnicity: _____________________
Type of Residence: Home LTCF Other ___________
Address: _______________________________________ Apt: ______________________
City: ______________________ County: ______________ State: ____Zip Code: _____________
Phone number:__________________
CASE DEFINITIONS <Modify to fit current outbreak>
A definitely nosocomial case of LD associated with Hospital A:
Signs or symptoms of pneumonia AND
Laboratory confirmation of Legionella AND
Continuously hospitalized at Hospital A for the entire 10 days prior to onset, OR
The patient had exposure to Hospital A during the 10 days prior to onset AND a clinical respiratory isolate matches an environmental isolate from Hospital A by molecular methods
A probably nosocomial case of LD associated with Hospital A:
Signs or symptoms of pneumonia AND
Laboratory confirmation of Legionella AND
Exposure to Hospital A (including but not limited to: overnight stay, outpatient visit, visitor, employee, volunteer) during a portion of the 2-10 days prior to onset
A suspected case of LD associated with Hospital A:
Signs or symptoms of pneumonia AND
No Legionella test performed or results unavailable AND
No other laboratory-confirmed diagnosis for the pneumonia AND
Exposure to Hospital A (including but not limited to: overnight stay, outpatient visit, visitor, employee, volunteer) during the 2-10 days prior to onset
A person is considered to have signs or symptoms of pneumonia if the following were present:
Cough or shortness of breath, AND at least one of the following: fever >100.5°F, nausea, diarrhea (3 or more stools in 24 hrs.), confusion, malaise, or headache, OR
Physician diagnosis of pneumonia, OR
Chest x-ray consistent with pneumonia.
Laboratory criteria for confirmed legionellosis:
Isolation of any Legionella organism from respiratory secretions, lung tissue, pleural fluid, or other normally sterile fluid, OR
Detection of Legionella pneumophila serogroup 1 (Lp1) urinary antigen using validated reagents, OR
Fourfold or greater rise in antibody titer to Lp1 using validated reagents.
Laboratory criteria for probable legionellosis:
Fourfold or greater rise in antibody titer to non-Lp1 Legionella species using validated reagents.
Detection of specific Legionella antigen or staining of the organism in respiratory secretions, lung tissue or pleural fluid by direct fluorescent antibody (DFA) staining, immunohistochemistry (IHC) or other similar method, using validated reagents
Detection of Legionella species by a validated nucleic acid assay.
II. LEGIONELLA-SPECIFIC TESTING
Respiratory specimen collected and processed specifically for Legionella culture?
_____ Yes (See 1a. below) ______ No (See 1b. below) _____ Unknown
If YES,
Specimen type: (e.g., expectorated sputum, BAL, etc.) __________________
Collected Date: ____/____/ ____ Laboratory Name:____________________
Results:________________________________________________________
If NO,
Respiratory specimen collected for any culture?
_____ Yes ______ No _____ Unknown
If Yes,
Specimen type: (e.g., expectorated sputum, BAL, etc.) ____________________
Collected Date: ____/____/ ____ Laboratory: ___________________________
Results:__________________________________________________________
Urine specimen collected for Legionella urine antigen testing?
_____ Yes ______ No _____ Unknown
Collected Date: ____/____/ ____ Laboratory Name: ________________________
Results: ____________________________________________________________
Serum sample collected for Legionella serologic testing?
_____ Yes ______ No _____ Unknown
If Yes,
Collected Date: ____/____/ ____ Laboratory: _______________________________
Type of assay (e.g., Lp1 only, Lp1-6 pooled antigen, Legionella species pooled antigen, etc.) _________________________________________________________________
Results: ______________________________________________________________
If convalescent serum samples were collected, please provide the same information for each:
Collected Date: ____/____/ ____ Laboratory: _________________________________
Type of assay (e.g., Lp1 only, Lp1-6 pooled antigen, Legionella species pooled antigen, etc.) __________________________________________________________________
Results:________________________________________________________________
Collected Date: ____/____/ ____ Laboratory: __________________________________
Type of assay (e.g., Lp1 only, Lp1-6 pooled antigen, Legionella species pooled antigen, etc.) ___________________________________________________________________
Results:_________________________________________________________________
PCR testing for Legionella?
_____ Yes ______ No _____ Unknown
Collected Date: ____/____/ ____ Laboratory Name: ________________________________
Results: ____________________________________________________________________
DFA or IHC for Legionella species?
_____ Yes ______ No _____ Unknown
Collected Date: ____/____/ ____ Laboratory Name:_________________________________
Results: ____________________________________________________________________
Outcome: ____ Still Hospitalized ____ Transferred to another facility (list:______________) ____ Discharged Home ____ Deceased ____ Unknown
If deceased,
Date of death: __________ (mm/dd/yyyy)
Was a post-mortem examination performed? ___Yes ___No ____Unknown
If yes, are tissue specimens available? ____ Yes ____No ____ Unknown
III. SIGNS AND SYMPTOMS
Shortness of breath: |
_____ Yes (Onset Date: _________) |
______ No |
_____ Unknown |
Cough: |
_____ Yes (Onset Date: _________) |
______ No |
_____ Unknown |
Hemoptysis: |
_____ Yes (Onset Date: _________) |
______ No |
_____ Unknown |
Myalgias: |
_____ Yes (Onset Date: _________) |
______ No |
_____ Unknown |
Fever (self-report): |
_____ Yes (Onset Date: _________) |
______ No |
_____ Unknown |
Fever >100.5°F: |
_____ Yes (Onset Date: _________) |
______ No |
_____ Unknown |
Diarrhea (3 stools/24h): |
_____ Yes (Onset Date: _________) |
______ No |
_____ Unknown |
Nausea: |
_____ Yes (Onset Date: _________) |
______ No |
_____ Unknown |
Malaise: |
_____ Yes (Onset Date: _________) |
______ No |
_____ Unknown |
Headache: |
_____ Yes (Onset Date: _________) |
______ No |
_____ Unknown |
Other (____________): |
_____ Yes (Onset Date: _________) |
______ No |
_____ Unknown |
Other (____________): |
_____ Yes (Onset Date: _________) |
______ No |
_____ Unknown |
Other (____________): |
_____ Yes (Onset Date: _________) |
______ No |
_____ Unknown |
List date of earliest symptom onset (MM/DD/YYYY): ____/ _____/ ________
IMPORTANT: How to calculate incubation period
USE A CALENDAR! Start at the date of earliest symptom onset (Q.7) and count backward 2-10 days. This is the incubation period. See example below.
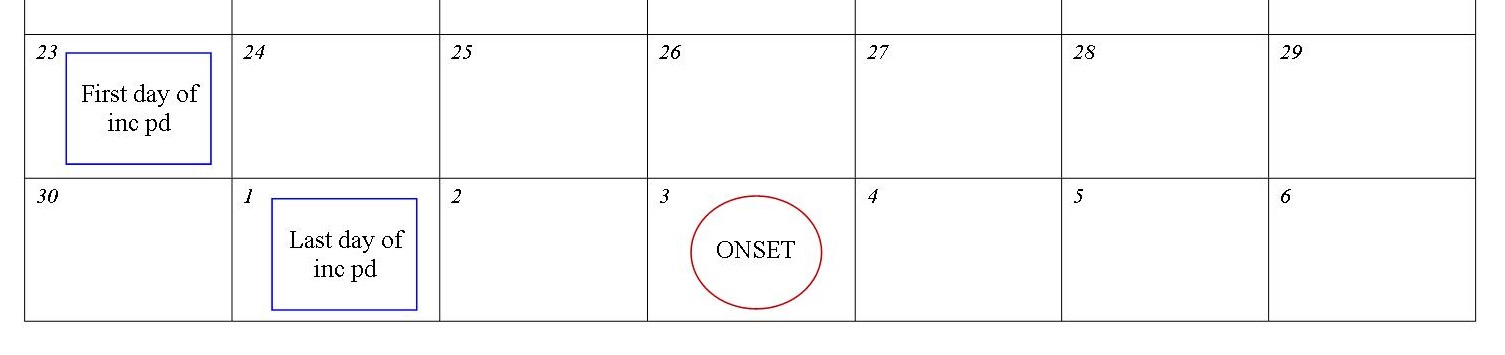
Document incubation period here: ____/ ____/ ____/ to ____/ ____/ ____
Document any radiographic testing in the 14 days after onset of symptoms of LD:
Chest X-ray: _____ Yes ______ No _____ Unknown
CT scan: _____ Yes ______ No _____ Unknown
If Yes, when and what were the findings?
Date: ____/____ / _____
Result: ____ New Infiltrate ____ Old / Unchanged Infiltrate ____ Indeterminate ____ No infiltrate ____ Not available
Findings: ______________________________________________________________
IV. EXPOSURE HISTORY
Document the patient’s general location for each day during their incubation period. (Additional details regarding specific location(s) within Hospital A will be asked later.)
Date (start with first date of inc pd from top of this page) |
Location (e.g., Hospital A, Hospital B, Home, LTCF, travel location) |
Water Exposures/Activities (e.g., took pre-op shower, whirlpool spa in gym) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Type of exposures to Hospital A during incubation period (check all that apply): _____ Inpatient _____ Outpatient _____ Visitor _____ Volunteer _____ Employee
Case Classification (see p. 2 for case definitions): ______ Definitely Nosocomial ______ Probably Nosocomial ______ Suspect Case ______ Not Nosocomial
If Not Nosocomial, END HERE. Otherwise, continue to next page.
VI. MEDICAL HISTORY
COPD/Emphysema/Chronic Lung Disease: |
_____ Yes |
______ No/Unknown |
Diabetes: |
_____ Yes |
______ No/Unknown |
Congestive Heart Failure: |
_____ Yes |
______ No/Unknown |
History of stroke/CVA: |
_____ Yes |
______ No/Unknown |
Chronic Renal Insuffiency (CRI/CKD) or End-Stage Renal Disease (ESRD): |
_____ Yes |
______ No/Unknown |
Cirrhosis / Liver Disease: |
_____ Yes |
______ No/Unknown |
Cancer (Type: _____________________): |
_____ Yes |
______ No/Unknown |
Organ Transplant: |
_____ Yes |
______ No/Unknown |
HIV/AIDS: |
_____ Yes |
______ No/Unknown |
Dementia: |
_____ Yes |
______ No/Unknown |
Taking Immunosuppressive drugs (e.g., corticosteroids or chemotherapy): |
_____ Yes |
______ No/Unknown |
Other (___________________________): |
_____ Yes |
______ No/Unknown |
Other (___________________________): |
_____ Yes |
______ No/Unknown |
Current Smoker (or quit in the past year): _____ Yes _____No _____ Unknown
Former Smoker: _____ Yes _____No _____Unknown
VII. CLINICAL AND EXPOSURE INFORMATION FOR EACH HOSPITALIZATION TO HOSPITAL A PRIOR TO ONSET
Beginning at the First Day of Incubation Period (top of p. 5), complete this section for each hospitalization to Hospital A in the 10 days prior to symptom onset. If patient had only outpatient or other exposures (was not inpatient at Hospital A), skip to p. 11.
Hospitalization #____
Date of admission: ____/____/ ____ Date of discharge: ____/____/____
Admitted to ICU? _____ Yes ______ No _____ Unknown
If yes, # of days in ICU _______
Intubated? _____ Yes ______ No _____ Unknown
Discharge diagnosis: (Complete all)
Legionellosis? _____ Yes ______ No _____ Unknown
Pneumonia? _____ Yes ______ No _____ Unknown
If yes, Etiology: ____________________ Lab Test(s): _______________________
Other Dx: _________________________________________________________________
Chest X-ray? _____ Yes ______ No _____ Unknown
CT scan? _____ Yes ______ No _____ Unknown
If Yes, when and what were the findings?
Date: ____/____ / _____
Result: ____ New Infiltrate ____ Old / Unchanged Infiltrate ____ Indeterminate ____ No infiltrate ____ Not available
Findings: ________________________________________________________________
List all campuses, buildings, and rooms the patient stayed in during this visit:
Name of Campus |
Building |
Room# |
Reason for Visit |
Admit Date |
Discharge Date |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Was patient ambulatory? _____ Yes ______ No ______ Unknown
Did patient leave building during hospitalization? _____ Yes _____ No _____ Unknown
Showered in facility? _____ Yes ______ No ______ Unknown
How often? _____ Daily ______ Weekly ______ Monthly ______ Unknown
Used CPAP/BiPAP while in facility? _____ Yes ______ No ______ Unknown
Nebulized medications while in facility? _____ Yes ______ No ______ Unknown
Document any antibiotic therapies that the patient received during this hospitalization:
Antibiotic |
Check if given |
Dose |
Route |
Start Date |
End Date |
Check if continued as outpatient |
Levofloxacin (Levoquin) |
|
|
|
|
|
|
Azithromycin (Zithromax) |
|
|
|
|
|
|
Ciprofloxacin (Cipro) |
|
|
|
|
|
|
Erythromycin
|
|
|
|
|
|
|
Ceftriaxone (Rocephin) |
|
|
|
|
|
|
Other (specify): ___________ |
|
|
|
|
|
|
Other (specify): ___________ |
|
|
|
|
|
|
Hospitalization #____
Date of admission: ____/____/ ____ Date of discharge: ____/____/____
Admitted to ICU? _____ Yes ______ No _____ Unknown
If yes, # of days in ICU _______
Intubated? _____ Yes ______ No _____ Unknown
Discharge diagnosis: (Complete all)
Legionellosis? _____ Yes ______ No _____ Unknown
Pneumonia? _____ Yes ______ No _____ Unknown
If yes, Etiology: ____________________ Lab Test(s): _______________________
Other Dx: _________________________________________________________________
Chest X-ray? _____ Yes ______ No _____ Unknown
CT scan? _____ Yes ______ No _____ Unknown
If Yes, when and what were the findings?
Date: ____/____ / _____
Result: ____ New Infiltrate ____ Old / Unchanged Infiltrate ____ Indeterminate ____ No infiltrate ____ Not available
Findings: ________________________________________________________________
List all campuses, buildings, and rooms the patient stayed in during this visit:
Name of Campus |
Building |
Room# |
Reason for Visit |
Admit Date |
Discharge Date |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Was patient ambulatory? _____ Yes ______ No ______ Unknown
Did patient leave building during hospitalization? _____ Yes _____ No _____ Unknown
Showered in facility? _____ Yes ______ No ______ Unknown
How often? _____ Daily ______ Weekly ______ Monthly ______ Unknown
Used CPAP/BiPAP while in facility? _____ Yes ______ No ______ Unknown
Nebulized medications while in facility? _____ Yes ______ No ______ Unknown
Document any antibiotic therapies that the patient received during this hospitalization:
Antibiotic |
Check if given |
Dose |
Route |
Start Date |
End Date |
Check if continued as outpatient |
Levofloxacin (Levoquin) |
|
|
|
|
|
|
Azithromycin (Zithromax) |
|
|
|
|
|
|
Ciprofloxacin (Cipro) |
|
|
|
|
|
|
Erythromycin
|
|
|
|
|
|
|
Ceftriaxone (Rocephin) |
|
|
|
|
|
|
Other (specify): ___________ |
|
|
|
|
|
|
Other (specify): ___________ |
|
|
|
|
|
|
Hospitalization #____
Date of admission: ____/____/ ____ Date of discharge: ____/____/____
Admitted to ICU? _____ Yes ______ No _____ Unknown
If yes, # of days in ICU _______
Intubated? _____ Yes ______ No _____ Unknown
Discharge diagnosis: (Complete all)
Legionellosis? _____ Yes ______ No _____ Unknown
Pneumonia? _____ Yes ______ No _____ Unknown
If yes, Etiology: ____________________ Lab Test(s): _______________________
Other Dx: _________________________________________________________________
Chest X-ray? _____ Yes ______ No _____ Unknown
CT scan? _____ Yes ______ No _____ Unknown
If Yes, when and what were the findings?
Date: ____/____ / _____
Result: ____ New Infiltrate ____ Old / Unchanged Infiltrate ____ Indeterminate ____ No infiltrate ____ Not available
Findings: ________________________________________________________________
List all campuses, buildings, and rooms the patient stayed in during this visit:
Name of Campus |
Building |
Room# |
Reason for Visit |
Admit Date |
Discharge Date |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Was patient ambulatory? _____ Yes ______ No ______ Unknown
Did patient leave building during hospitalization? _____ Yes _____ No _____ Unknown
Showered in facility? _____ Yes ______ No ______ Unknown
How often? _____ Daily ______ Weekly ______ Monthly ______ Unknown
Used CPAP/BiPAP while in facility? _____ Yes ______ No ______ Unknown
Nebulized medications while in facility? _____ Yes ______ No ______ Unknown
Document any antibiotic therapies that the patient received during this hospitalization:
Antibiotic |
Check if given |
Dose |
Route |
Start Date |
End Date |
Check if continued as outpatient |
Levofloxacin (Levoquin) |
|
|
|
|
|
|
Azithromycin (Zithromax) |
|
|
|
|
|
|
Ciprofloxacin (Cipro) |
|
|
|
|
|
|
Erythromycin
|
|
|
|
|
|
|
Ceftriaxone (Rocephin) |
|
|
|
|
|
|
Other (specify): ___________ |
|
|
|
|
|
|
Other (specify): ___________ |
|
|
|
|
|
|
VIII. OUTPATIENT VISITS to Hospital A or associated clinics (including rehab visits)
Did patient have any outpatient visits during the 2-10 days prior to symptom onset?
_____ Yes _____ No _____ Unknown
If yes, list location of visits and name of clinic:
Name of Campus |
Clinic (e.g., Primary Care, Cardiology) |
Building |
Room# |
Date(s) of Visit |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
IX. OTHER EXPOSURES
Did patient have any other exposure to Hospital A in the 2-10 days prior to symptom onset (e.g., visitor, volunteer, employee)? _____ Yes _____ No _____ Unknown
Please note these exposures: ________________________________________________
Page
Public reporting burden of this collection of information is estimated to average 15 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not required to respond to a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information including suggestions for reducing this burden to CDC/ATSDR Reports Clearance Officer; 1600 Clifton Road NE, MS D-74 Atlanta, Georgia 30333; ATTN: PRA (0920-1011)
| File Type | application/msword |
| File Title | Medical Record Abstraction Form |
| Author | deocadmin |
| Last Modified By | CDC |
| File Modified | 2014-05-23 |
| File Created | 2014-05-23 |
© 2026 OMB.report | Privacy Policy