Transformed - Medicaid Statistical Information System (T-MSIS)
Medicaid Statistical Information System (MSIS) and the Transformed - Medicaid Statistical Information System (T-MSIS) (CMS-R-284)
1 - T-MSIS V2_0 Data Dictionary - 2015-11-24.xlsx
Transformed - Medicaid Statistical Information System (T-MSIS)
OMB: 0938-0345
⚠️ Notice: This form may be outdated. More recent filings and information on OMB 0938-0345 can be found here:
Document [xlsx]
Download: xlsx | pdf
Record Segment Definitions
Rec Segment Keys & Constraints
Record Segment Relationships
Data Element Definitions, Etc.
Overview
Cover SheetRecord Segment Definitions
Rec Segment Keys & Constraints
Record Segment Relationships
Data Element Definitions, Etc.
Sheet 1: Cover Sheet

|
|||||
| Centers for Medicaid and CHIP Services (CMCS) | |||||
| Transformed Medicaid Statistical Information System (T-MSIS) | |||||
| Data Dictionary | |||||
| Version: Nov15v2.0 | |||||
| Last Modified: 11/19/2015 | |||||
Sheet 2: Record Segment Definitions
| Record Segment Names, Identifiers, and Definitions | ||||
| Record Segment Name | Record Identifier | Record Segment Definition | Record Segment Length | |
| Claim Inpatient File | ||||
| FILE-HEADER-RECORD-IP | CIP00001 | A record containing metadata necessary to identify the file itself, when it was created and the number of records it contains. | 2,100 | |
| CLAIM-HEADER-RECORD-IP | CIP00002 | A record to capture data about an inpatient claim or encounter that applies to the claim in its totality. | 2,100 | |
| CLAIM-LINE-RECORD-IP | CIP00003 | A record to capture data about specific goods or services rendered to a Medicaid/CHIP enrollee during the hospital stay. | 2,100 | |
| Claim Long-term Care File | ||||
| FILE-HEADER-RECORD-LT | CLT00001 | A record containing metadata necessary to identify the file itself, when it was created and the number of records it contains. | 1,900 | |
| CLAIM-HEADER-RECORD-LT | CLT00002 | A record to capture data about a long-term care claim or encounter that applies to the claim in its totality. | 1,900 | |
| CLAIM-LINE-RECORD-LT | CLT00003 | A record to capture data about specific goods or services rendered to a Medicaid/CHIP enrollee during a long-term care stay. | 1,900 | |
| Claim Other File | ||||
| FILE-HEADER-RECORD-OT | COT00001 | A record containing metadata necessary to identify the file itself, when it was created and the number of records it contains. | 1,750 | |
| CLAIM-HEADER-RECORD-OT | COT00002 | A record to capture data about an other type of claim or encounter (besides IP, LT, and RX) that applies to the claim in its totality. | 1,750 | |
| CLAIM-LINE-RECORD-OT | COT00003 | A record to capture data about specific goods or services rendered to a Medicaid/CHIP enrollee during an outpatient visit. | 1,750 | |
| Claim Prescription File | ||||
| FILE-HEADER-RECORD-RX | CRX00001 | A record containing metadata necessary to identify the file itself, when it was created and the number of records it contains. | 1,450 | |
| CLAIM-HEADER-RECORD-RX | CRX00002 | A record to capture data about a pharmacy claim or encounter that applies to the claim in its totality. | 1,450 | |
| CLAIM-LINE-RECORD-RX | CRX00003 | A record to capture data about specific prescription goods or services rendered to a Medicaid/CHIP enrollee. | 1,450 | |
| Eligible File | ||||
| FILE-HEADER-RECORD-ELIGIBILITY | ELG00001 | A record containing metadata necessary to identify the file itself, when it was created and the number of records it contains. | 1,000 | |
| PRIMARY-DEMOGRAPHICS-ELIGIBILITY | ELG00002 | A record to capture basic demographic information about the individual. | 1,000 | |
| VARIABLE-DEMOGRAPHICS-ELIGIBILITY | ELG00003 | A record to capture additional demographic information that is more prone to periodic changes. | 1,000 | |
| ELIGIBLE-CONTACT-INFORMATION | ELG00004 | A record to capture addresses, phone numbers, and email addresses of the individual. | 1,000 | |
| ELIGIBILITY-DETERMINANTS | ELG00005 | A record to capture factors that influence an individual’s eligibility for basic Medicaid/CHIP, as well as the various waivers and demonstrations. (The data elements in this record segment are categorical data elements that will only have one valid value at any given point in time.) | 1,000 | |
| HEALTH-HOME-SPA-PARTICIPATION-INFORMATION | ELG00006 | A record to capture the eligible person's participation in the state's health home initiative. | 1,000 | |
| HEALTH-HOME-SPA-PROVIDERS | ELG00007 | A record to capture the identity of the health home entity in which the eligible person is enrolled, as well as the identity of the provider with primary responsibility for coordinating the delivery of health home services. | 1,000 | |
| HEALTH-HOME-CHRONIC-CONDITIONS | ELG00008 | A record to capture an eligible person's chronic conditions that qualified him/her for participation in the health home initiative. | 1,000 | |
| LOCK-IN-INFORMATION | ELG00009 | A record to capture the provider, or providers, to whom the eligible person is restricted, as well as the time periods during which the lock-in provisions are in force. | 1,000 | |
| MFP-INFORMATION | ELG00010 | A record to capture information about an eligible person's participation in the Money Follows the Person demonstration program. | 1,000 | |
| STATE-PLAN-OPTION-PARTICIPATION | ELG00011 | A record to capture the identity of the State Plan Options in which an eligible person is enrolled. | 1,000 | |
| WAIVER-PARTICIPATION | ELG00012 | A record to capture the identity of the waivers in which an eligible person is enrolled. | 1,000 | |
| LTSS-PARTICIPATION | ELG00013 | A record to capture the level of care an eligible person receives at various points in time while in a long-term care facility. | 1,000 | |
| MANAGED-CARE-PARTICIPATION | ELG00014 | A record to capture information about an eligible person's enrollment in a managed care plan. | 1,000 | |
| ETHNICITY-INFORMATION | ELG00015 | A record to capture information about an eligible person's ethnicity. | 1,000 | |
| RACE-INFORMATION | ELG00016 | A record to capture information about an eligible person's race. | 1,000 | |
| DISABILITY-INFORMATION | ELG00017 | A record to capture information about an eligible person's disabilities. | 1,000 | |
| 1115A-DEMONSTRATION-INFORMATION | ELG00018 | A record to capture an eligible person's 1115A participation. | 1,000 | |
| HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME | ELG00020 | A record to capture an eligible person's chronic conditions for which an eligible person is receiving home and community-based care. | 1,000 | |
| ENROLLMENT-TIME-SPAN-SEGMENT | ELG00021 | A record to capture the eligible person's type of enrollment and time spans of enrollment. | 1,000 | |
| Managed Care Plan Information File | ||||
| FILE-HEADER-RECORD-MANAGED-CARE | MCR00001 | A record containing metadata necessary to identify the file itself, when it was created and the number of records it contains. | 1,000 | |
| MANAGED-CARE-MAIN | MCR00002 | A record to capture basic, generally static information about a managed care entity. | 1,000 | |
| MANAGED-CARE-LOCATION-AND-CONTACT-INFO | MCR00003 | A record to capture addresses, phone numbers, fax numbers, and email addresses of the managed care organization. | 1,000 | |
| MANAGED-CARE-SERVICE-AREA | MCR00004 | A record to capture the zip codes, counties, or other geographic descriptors that define the managed care entity’s service area. | 1,000 | |
| MANAGED-CARE-OPERATING-AUTHORITY | MCR00005 | A record to capture information about the operating authority, waivers and demonstrations under which a managed care entity is contracted with the state. | 1,000 | |
| MANAGED-CARE-PLAN-POPULATION-ENROLLED | MCR00006 | A record to capture the identity of the Medicaid/CHIP eligibility groups that the managed care entity is authorized to enroll. | 1,000 | |
| MANAGED- CARE-ACCREDITATION-ORGANIZATION | MCR00007 | A record to capture information concerning the accreditations that the managed care entity has. | 1,000 | |
| NATIONAL-HEALTH-CARE-ENTITY-ID-INFO | MCR00008 | A record to capture the national health plan identifiers associated with the managed care entity. | 1,000 | |
| CHPID-SHPID-RELATIONSHIPS | MCR00009 | A record to link a managed care entity Sub-Health Plan IDs with the appropriate Controlling Health Plan IDs. | 1,000 | |
| Provider File | ||||
| FILE-HEADER-RECORD-PROVIDER | PRV00001 | A record containing metadata necessary to identify the file itself, when it was created and the number of records it contains. | 1,100 | |
| PROV-ATTRIBUTES-MAIN | PRV00002 | A record to capture basic, generally static information about each provider. | 1,100 | |
| A provider is an individual person (medical or non-medical), a group of individuals, or an organization (e.g. institution, facility, agency, hospital, nursing facility, home health agency, school, or transportation organization) that delivers or facilitates health-related treatments, health care services, or living supports. | ||||
| PROV-LOCATION-AND-CONTACT-INFO | PRV00003 | A record to capture addresses, phone numbers, and email addresses of the provider. | 1,100 | |
| Each PRVDR_LOCATION_AND_CONTACT _INFO record segment represents the set of contact information for a single provider location. | ||||
| The state can enter as many sets of contact information (i.e., multiple PRVDR_LOCATION_ AND_CONTACT_INFO record segments) as it considers necessary. The value selected for the ADDR-TYPE field describes the type of contact information on that particular record (e.g., provider service location, provider billing address, etc.). The PROV-LOCATION-ID differentiates one PRVDR_LOCATION_ AND_CONTACT_INFO record segment from another when the ADDR-TYPE value on both records is the same. | ||||
| PROV-LICENSING-INFO | PRV00004 | A record to capture licensing and accreditation information relevant to the provider. | 1,100 | |
| PROV-IDENTIFIERS | PRV00005 | A record to capture the identifiers assigned to the provider entity by various governmental, professional, and payer entities. | 1,100 | |
| PROV-TAXONOMY-CLASSIFICATION | PRV00006 | A record to classify the provider into areas of specialty, as well as the authorized categories of service for which the provider entity has been authorized by the state to render to Medicaid/CHIP eligibles. | 1,100 | |
| PROV-MEDICAID-ENROLLMENT | PRV00007 | A record to capture the provider’s periods of participation in the state's Medicaid/CHIP programs, and the reason for a change in enrollment status. | 1,100 | |
| PROV-AFFILIATED-GROUPS | PRV00008 | A record to capture a provider’s relationship(s) with other provider(s) . | 1,100 | |
| PROV-AFFILIATED-PROGRAMS | PRV00009 | A record to capture the Medicaid/CHIP health plans, waivers, health home entities, etc. that the provider entity is associated with. | 1,100 | |
| PROV-BED-TYPE-INFO | PRV00010 | A record to capture the number on beds available for various categories of bed at provider entities that are facilities. | 1,100 | |
| Third-party Liability File | ||||
| FILE-HEADER-RECORD-TPL | TPL00001 | A record containing metadata necessary to identify the file itself, when it was created and the number of records it contains. | 900 | |
| TPL-MEDICAID-ELIGIBLE-PERSON-MAIN | TPL00002 | A record to capture basic, generally static information to identify Medicaid/CHIP enrollees for whom third party funds may be available to offset some or all of their Medicaid/CHIP costs. | 900 | |
| TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO | TPL00003 | A record to capture insurance policy information needed to facilitate pursuit of the third party liability. | 900 | |
| TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES | TPL00004 | A record to capture TPL insurance coverage information to support the applicability assessment of the third party insurance coverage to the Medicaid/CHIP costs incurred on behalf of the Medicaid/CHIP enrollee. | 900 | |
| TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION | TPL00005 | A record to flag Medicaid/CHIP enrollees who potentially have non-insurance sources of funds that could be used to offset Medicaid/CHIP expenditures. | 900 | |
| TPL-ENTITY-CONTACT-INFORMATION | TPL00006 | A record to capture addresses, phone numbers, and email addresses of the entity providing TPL insurance coverage. | 900 |
Sheet 3: Rec Segment Keys & Constraints
| Record Segment Keys and Constraints | |||||
| (a) = Data element is part of the record segment key, but is not considered when evaluating the date constraints | |||||
| File Name | File Segment (with Record-ID) | Key Field Identifier | Data Element Name | Intra-Record Segment Constraints | Inter-Record Segment Constraints |
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | RECORD-ID | None | ||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | DATA-DICTIONARY-VERSION | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | SUBMISSION-TRANSACTION-TYPE | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | FILE-ENCODING-SPECIFICATION | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | DATA-MAPPING-DOCUMENT-VERSION | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | FILE-NAME | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | SUBMITTING-STATE | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | DATE-FILE-CREATED | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | START-OF-TIME-PERIOD | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | END-OF-TIME-PERIOD | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | FILE-STATUS-INDICATOR | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | SSN-INDICATOR | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | TOT-REC-CNT | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | SEQUENCE-NUMBER | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | STATE-NOTATION | |||
| CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | FILLER | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | RECORD-ID | None. The claim (or encounter record) should be submitted as it was adjudicated (or received) | None | |
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | 1 | SUBMITTING-STATE | ||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | RECORD-NUMBER | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | 2 | ICN-ORIG | ||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | 3 | ICN-ADJ | ||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | SUBMITTER-ID | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | MSIS-IDENTIFICATION-NUM | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CROSSOVER-INDICATOR | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | TYPE-OF-HOSPITAL | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | 1115A-DEMONSTRATION-IND | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ADJUSTMENT-IND | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ADJUSTMENT-REASON-CODE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ADMISSION-TYPE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DRG-DESCRIPTION | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ADMITTING-DIAGNOSIS-CODE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ADMITTING-DIAGNOSIS-CODE-FLAG | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-1 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-FLAG-1 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-POA-FLAG-1 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-2 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-FLAG-2 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-POA-FLAG-2 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-3 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-FLAG-3 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-POA-FLAG-3 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-4 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-FLAG-4 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-POA-FLAG-4 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-5 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-FLAG-5 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-POA-FLAG-5 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-6 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-FLAG-6 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-POA-FLAG-6 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-7 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-FLAG-7 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-POA-FLAG-7 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-8 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-FLAG-8 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-POA-FLAG-8 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-9 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-FLAG-9 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-POA-FLAG-9 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-10 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-FLAG-10 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-POA-FLAG-10 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-11 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-FLAG-11 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-POA-FLAG-11 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-12 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-CODE-FLAG-12 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-POA-FLAG-12 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-RELATED-GROUP | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DIAGNOSIS-RELATED-GROUP-IND | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-1 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-MOD-1 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-FLAG-1 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-DATE-1 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-2 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-MOD-2 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-FLAG-2 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-DATE-2 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-3 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-MOD-3 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-FLAG-3 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-DATE-3 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-4 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-MOD-4 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-FLAG-4 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-DATE-4 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-5 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-MOD-5 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-FLAG-5 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-DATE-5 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-6 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-MOD-6 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-FLAG-6 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROCEDURE-CODE-DATE-6 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ADMISSION-DATE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ADMISSION-HOUR | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DISCHARGE-DATE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DISCHARGE-HOUR | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | 4 | ADJUDICATION-DATE | ||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | MEDICAID-PAID-DATE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | TYPE-OF-CLAIM | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | TYPE-OF-BILL | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CLAIM-STATUS | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CLAIM-STATUS-CATEGORY | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | SOURCE-LOCATION | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CHECK-NUM | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CHECK-EFF-DATE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ALLOWED-CHARGE-SRC | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CLAIM-PYMT-REM-CODE-1 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CLAIM-PYMT-REM-CODE-2 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CLAIM-PYMT-REM-CODE-3 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CLAIM-PYMT-REM-CODE-4 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | TOT-BILLED-AMT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | TOT-ALLOWED-AMT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | TOT-MEDICAID-PAID-AMT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | TOT-COPAY-AMT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | TOT-MEDICARE-DEDUCTIBLE-AMT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | TOT-MEDICARE-COINS-AMT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | TOT-TPL-AMT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | TOT-OTHER-INSURANCE-AMT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OTHER-INSURANCE-IND | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OTHER-TPL-COLLECTION | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | SERVICE-TRACKING-TYPE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | SERVICE-TRACKING-PAYMENT-AMT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | FIXED-PAYMENT-IND | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | FUNDING-CODE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | FUNDING-SOURCE-NONFEDERAL-SHARE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | MEDICARE-COMB-DED-IND | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROGRAM-TYPE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PLAN-ID-NUMBER | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | NATIONAL-HEALTH-CARE-ENTITY-ID | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PAYMENT-LEVEL-IND | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | MEDICARE-REIM-TYPE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | NON-COV-DAYS | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | NON-COV-CHARGES | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | MEDICAID-COV-INPATIENT-DAYS | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CLAIM-LINE-COUNT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | FORCED-CLAIM-IND | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | HEALTH-CARE-ACQUIRED-CONDITION-IND | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-01 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-02 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-03 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-04 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-05 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-06 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-07 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-08 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-09 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-10 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-EFF-DATE-01 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-EFF-DATE-02 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-EFF-DATE-03 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-EFF-DATE-04 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-EFF-DATE-05 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-EFF-DATE-06 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-EFF-DATE-07 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-EFF-DATE-08 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-EFF-DATE-09 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-EFF-DATE-10 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-END-DATE-01 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-END-DATE-02 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-END-DATE-03 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-END-DATE-04 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-END-DATE-05 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-END-DATE-06 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-END-DATE-07 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-END-DATE-08 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-END-DATE-09 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OCCURRENCE-CODE-END-DATE-10 | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BIRTH-WEIGHT-GRAMS | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PATIENT-CONTROL-NUM | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ELIGIBLE-LAST-NAME | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ELIGIBLE-FIRST-NAME | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ELIGIBLE-MIDDLE-INIT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DATE-OF-BIRTH | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | HEALTH-HOME-PROV-IND | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | WAIVER-TYPE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | WAIVER-ID | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BILLING-PROV-NUM | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BILLING-PROV-NPI-NUM | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BILLING-PROV-TAXONOMY | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BILLING-PROV-TYPE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BILLING-PROV-SPECIALTY | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ADMITTING-PROV-NPI-NUM | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ADMITTING-PROV-NUM | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ADMITTING-PROV-SPECIALTY | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ADMITTING-PROV-TAXONOMY | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ADMITTING-PROV-TYPE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | REFERRING-PROV-NUM | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | REFERRING-PROV-NPI-NUM | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | REFERRING-PROV-TAXONOMY | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | REFERRING-PROV-TYPE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | REFERRING-PROV-SPECIALTY | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DRG-OUTLIER-AMT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | DRG-REL-WEIGHT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | MEDICARE-HIC-NUM | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OUTLIER-CODE | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OUTLIER-DAYS | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PATIENT-STATUS | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BMI | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | REMITTANCE-NUM | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | SPLIT-CLAIM-IND | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BORDER-STATE-IND | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BENEFICIARY-COINSURANCE-AMOUNT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BENEFICIARY-COINSURANCE-DATE-PAID | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BENEFICIARY-COPAYMENT-AMOUNT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BENEFICIARY-COPAYMENT-DATE-PAID | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BENEFICIARY-DEDUCTIBLE-AMOUNT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CLAIM-DENIED-INDICATOR | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | COPAY-WAIVED-IND | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | HEALTH-HOME-ENTITY-NAME | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | THIRD-PARTY-COINSURANCE-AMOUNT-PAID | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | THIRD-PARTY-COINSURANCE-DATE-PAID | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | THIRD-PARTY-COPAYMENT-AMOUNT-PAID | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | THIRD-PARTY-COPAYMENT-DATE-PAID | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | MEDICAID-AMOUNT-PAID-DSH | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | HEALTH-HOME-PROVIDER-NPI | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | MEDICARE-BENEFICIARY-IDENTIFIER | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | OPERATING-PROV-TAXONOMY | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | UNDER-DIRECTION-OF-PROV-NPI | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | UNDER-DIRECTION-OF-PROV-TAXONOMY | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | UNDER-SUPERVISION-OF-PROV-NPI | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | UNDER-SUPERVISION-OF-PROV-TAXONOMY | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | MEDICARE-PAID-AMT | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | STATE-NOTATION | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | PROV-LOCATION-ID | |||
| CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | FILLER | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | RECORD-ID | None. The claim (or encounter record) should be submitted as it was adjudicated (or received) | There must be an active CLAIM-HEADER-RECORD-IP-CIP00002 record in the current IP claim file submission that matches on: -- SUBMITTING-STATE -- ICN-ORIG -- ICN-ADJ -- ADJUDICATION-DATE. |
|
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | 1 | SUBMITTING-STATE | ||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | RECORD-NUMBER | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | MSIS-IDENTIFICATION-NUM | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | 2 | ICN-ORIG | ||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | 3 | ICN-ADJ | ||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | 4 | LINE-NUM-ORIG | ||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | 5 | LINE-NUM-ADJ | ||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | LINE-ADJUSTMENT-IND | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | LINE-ADJUSTMENT-REASON-CODE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | SUBMITTER-ID | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CLAIM-LINE-STATUS | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | BEGINNING-DATE-OF-SERVICE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | ENDING-DATE-OF-SERVICE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | REVENUE-CODE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | IMMUNIZATION-TYPE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | IP-LT-QUANTITY-OF-SERVICE-ACTUAL | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | IP-LT-QUANTITY-OF-SERVICE-ALLOWED | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | REVENUE-CHARGE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | ALLOWED-AMT | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | TPL-AMT | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | MEDICAID-PAID-AMT | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | MEDICAID-FFS-EQUIVALENT-AMT | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | BILLING-UNIT | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | TYPE-OF-SERVICE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | SERVICING-PROV-NUM | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | SERVICING-PROV-NPI-NUM | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | SERVICING-PROV-TAXONOMY | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | SERVICING-PROV-TYPE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | SERVICING-PROV-SPECIALTY | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | OPERATING-PROV-NPI-NUM | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | OTHER-TPL-COLLECTION | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | PROV-FACILITY-TYPE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | BENEFIT-TYPE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | XIX-MBESCBES-CATEGORY-OF-SERVICE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | XXI-MBESCBES-CATEGORY-OF-SERVICE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | OTHER-INSURANCE-AMT | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | STATE-NOTATION | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | HCPCS-RATE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | NATIONAL-DRUG-CODE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | NDC-UNIT-OF-MEASURE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | NDC-QUANTITY | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | 6 | ADJUDICATION-DATE | ||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | SELF-DIRECTION-TYPE | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | PRE-AUTHORIZATION-NUM | |||
| CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | FILLER | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | RECORD-ID | None | ||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | DATA-DICTIONARY-VERSION | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | SUBMISSION-TRANSACTION-TYPE | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | FILE-ENCODING-SPECIFICATION | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | DATA-MAPPING-DOCUMENT-VERSION | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | FILE-NAME | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | SUBMITTING-STATE | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | DATE-FILE-CREATED | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | START-OF-TIME-PERIOD | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | END-OF-TIME-PERIOD | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | FILE-STATUS-INDICATOR | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | SSN-INDICATOR | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | TOT-REC-CNT | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | SEQUENCE-NUMBER | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | STATE-NOTATION | |||
| CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | FILLER | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | RECORD-ID | None. The claim (or encounter record) should be submitted as it was adjudicated (or received) | None. | |
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | 1 | SUBMITTING-STATE | ||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | RECORD-NUMBER | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | 2 | ICN-ORIG | ||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | 3 | ICN-ADJ | ||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | SUBMITTER-ID | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | MSIS-IDENTIFICATION-NUM | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CROSSOVER-INDICATOR | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | 1115A-DEMONSTRATION-IND | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ADJUSTMENT-IND | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ADJUSTMENT-REASON-CODE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ADMITTING-DIAGNOSIS-CODE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ADMITTING-DIAGNOSIS-CODE-FLAG | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-CODE-1 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-CODE-FLAG-1 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-POA-FLAG-1 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-CODE-2 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-CODE-FLAG-2 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-POA-FLAG-2 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-CODE-3 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-CODE-FLAG-3 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-POA-FLAG-3 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-CODE-4 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-CODE-FLAG-4 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-POA-FLAG-4 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-CODE-5 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-CODE-FLAG-5 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DIAGNOSIS-POA-FLAG-5 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ADMISSION-DATE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ADMISSION-HOUR | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DISCHARGE-DATE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DISCHARGE-HOUR | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BEGINNING-DATE-OF-SERVICE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ENDING-DATE-OF-SERVICE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | 4 | ADJUDICATION-DATE | ||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | MEDICAID-PAID-DATE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | TYPE-OF-CLAIM | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | TYPE-OF-BILL | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLAIM-STATUS | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLAIM-STATUS-CATEGORY | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | SOURCE-LOCATION | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CHECK-NUM | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CHECK-EFF-DATE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLAIM-PYMT-REM-CODE-1 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLAIM-PYMT-REM-CODE-2 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLAIM-PYMT-REM-CODE-3 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLAIM-PYMT-REM-CODE-4 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | TOT-BILLED-AMT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | TOT-ALLOWED-AMT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | TOT-MEDICAID-PAID-AMT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | TOT-COPAY-AMT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | TOT-MEDICARE-DEDUCTIBLE-AMT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | TOT-MEDICARE-COINS-AMT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | TOT-TPL-AMT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | TOT-OTHER-INSURANCE-AMT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OTHER-INSURANCE-IND | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OTHER-TPL-COLLECTION | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | SERVICE-TRACKING-TYPE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | SERVICE-TRACKING-PAYMENT-AMT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | FIXED-PAYMENT-IND | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | FUNDING-CODE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | FUNDING-SOURCE-NONFEDERAL-SHARE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | MEDICARE-COMB-DED-IND | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | PROGRAM-TYPE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | PLAN-ID-NUMBER | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | NATIONAL-HEALTH-CARE-ENTITY-ID | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | PAYMENT-LEVEL-IND | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | MEDICARE-REIM-TYPE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | NON-COV-DAYS | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | NON-COV-CHARGES | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | MEDICAID-COV-INPATIENT-DAYS | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLAIM-LINE-COUNT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | FORCED-CLAIM-IND | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | HEALTH-CARE-ACQUIRED-CONDITION-IND | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-01 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-02 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-03 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-04 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-05 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-06 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-07 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-08 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-09 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-10 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-EFF-DATE-01 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-EFF-DATE-02 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-EFF-DATE-03 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-EFF-DATE-04 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-EFF-DATE-05 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-EFF-DATE-06 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-EFF-DATE-07 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-EFF-DATE-08 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-EFF-DATE-09 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-EFF-DATE-10 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-END-DATE-01 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-END-DATE-02 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-END-DATE-03 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-END-DATE-04 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-END-DATE-05 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-END-DATE-06 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-END-DATE-07 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-END-DATE-08 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-END-DATE-09 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | OCCURRENCE-CODE-END-DATE-10 | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | PATIENT-CONTROL-NUM | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ELIGIBLE-LAST-NAME | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ELIGIBLE-FIRST-NAME | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ELIGIBLE-MIDDLE-INIT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DATE-OF-BIRTH | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | HEALTH-HOME-PROV-IND | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | WAIVER-TYPE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | WAIVER-ID | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BILLING-PROV-NUM | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BILLING-PROV-NPI-NUM | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BILLING-PROV-TAXONOMY | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BILLING-PROV-TYPE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BILLING-PROV-SPECIALTY | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | REFERRING-PROV-NUM | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | REFERRING-PROV-NPI-NUM | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | REFERRING-PROV-TAXONOMY | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | REFERRING-PROV-TYPE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | REFERRING-PROV-SPECIALTY | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | MEDICARE-HIC-NUM | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | PATIENT-STATUS | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BMI | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | REMITTANCE-NUM | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | LTC-RCP-LIAB-AMT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | DAILY-RATE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ICF-IID-DAYS | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | LEAVE-DAYS | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | NURSING-FACILITY-DAYS | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | SPLIT-CLAIM-IND | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BORDER-STATE-IND | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BENEFICIARY-COINSURANCE-AMOUNT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BENEFICIARY-COINSURANCE-DATE-PAID | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BENEFICIARY-COPAYMENT-AMOUNT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BENEFICIARY-COPAYMENT-DATE-PAID | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BENEFICIARY-DEDUCTIBLE-AMOUNT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLAIM-DENIED-INDICATOR | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | COPAY-WAIVED-IND | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | HEALTH-HOME-ENTITY-NAME | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | THIRD-PARTY-COINSURANCE-AMOUNT-PAID | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | THIRD-PARTY-COINSURANCE-DATE-PAID | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | THIRD-PARTY-COPAYMENT-AMOUNT-PAID | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | THIRD-PARTY-COPAYMENT-DATE-PAID | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | HEALTH-HOME-PROVIDER-NPI | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | MEDICARE-BENEFICIARY-IDENTIFIER | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | UNDER-DIRECTION-OF-PROV-NPI | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | UNDER-DIRECTION-OF-PROV-TAXONOMY | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | UNDER-SUPERVISION-OF-PROV-NPI | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | UNDER-SUPERVISION-OF-PROV-TAXONOMY | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ADMITTING-PROV-NPI-NUM | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ADMITTING-PROV-NUM | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ADMITTING-PROV-SPECIALTY | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ADMITTING-PROV-TAXONOMY | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ADMITTING-PROV-TYPE | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | MEDICARE-PAID-AMT | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | STATE-NOTATION | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | PROV-LOCATION-ID | |||
| CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | FILLER | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | RECORD-ID | None. The claim (or encounter record) should be submitted as it was adjudicated (or received) | There must be an active CLAIM-HEADER-RECORD-LT-CLT00002 record in the current LT claim file submission that matches on: -- SUBMITTING-STATE -- ICN-ORIG -- ICN-ADJ -- ADJUDICATION-DATE. |
|
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | 1 | SUBMITTING-STATE | ||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | RECORD-NUMBER | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | MSIS-IDENTIFICATION-NUM | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | 2 | ICN-ORIG | ||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | 3 | ICN-ADJ | ||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | 4 | LINE-NUM-ORIG | ||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | 5 | LINE-NUM-ADJ | ||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | LINE-ADJUSTMENT-IND | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | LINE-ADJUSTMENT-REASON-CODE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | SUBMITTER-ID | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLAIM-LINE-STATUS | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | BEGINNING-DATE-OF-SERVICE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | ENDING-DATE-OF-SERVICE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | REVENUE-CODE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | IMMUNIZATION-TYPE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | IP-LT-QUANTITY-OF-SERVICE-ACTUAL | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | IP-LT-QUANTITY-OF-SERVICE-ALLOWED | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | REVENUE-CHARGE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | ALLOWED-AMT | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | TPL-AMT | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | OTHER-INSURANCE-AMT | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | MEDICAID-PAID-AMT | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | MEDICAID-FFS-EQUIVALENT-AMT | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | BILLING-UNIT | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | TYPE-OF-SERVICE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | SERVICING-PROV-NUM | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | SERVICING-PROV-NPI-NUM | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | SERVICING-PROV-TAXONOMY | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | SERVICING-PROV-TYPE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | SERVICING-PROV-SPECIALTY | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | OTHER-TPL-COLLECTION | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | BENEFIT-TYPE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | PROV-FACILITY-TYPE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | XIX-MBESCBES-CATEGORY-OF-SERVICE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | XXI-MBESCBES-CATEGORY-OF-SERVICE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | STATE-NOTATION | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | NATIONAL-DRUG-CODE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | NDC-UNIT-OF-MEASURE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | NDC-QUANTITY | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | HCPCS-RATE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | 6 | ADJUDICATION-DATE | ||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | SELF-DIRECTION-TYPE | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | PRE-AUTHORIZATION-NUM | |||
| CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | FILLER | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | RECORD-ID | None | ||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | DATA-DICTIONARY-VERSION | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | SUBMISSION-TRANSACTION-TYPE | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | FILE-ENCODING-SPECIFICATION | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | DATA-MAPPING-DOCUMENT-VERSION | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | FILE-NAME | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | SUBMITTING-STATE | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | DATE-FILE-CREATED | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | START-OF-TIME-PERIOD | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | END-OF-TIME-PERIOD | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | FILE-STATUS-INDICATOR | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | SSN-INDICATOR | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | TOT-REC-CNT | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | SEQUENCE-NUMBER | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | STATE-NOTATION | |||
| CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | FILLER | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | RECORD-ID | None. The claim (or encounter record) should be submitted as it was adjudicated (or received) | None | |
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | 1 | SUBMITTING-STATE | ||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | RECORD-NUMBER | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | 2 | ICN-ORIG | ||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | 3 | ICN-ADJ | ||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | SUBMITTER-ID | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | MSIS-IDENTIFICATION-NUM | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | CROSSOVER-INDICATOR | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | 1115A-DEMONSTRATION-IND | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | ADJUSTMENT-IND | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | ADJUSTMENT-REASON-CODE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | DIAGNOSIS-CODE-1 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | DIAGNOSIS-CODE-FLAG-1 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | DIAGNOSIS-POA-FLAG-1 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | DIAGNOSIS-CODE-2 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | DIAGNOSIS-CODE-FLAG-2 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | DIAGNOSIS-POA-FLAG-2 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BEGINNING-DATE-OF-SERVICE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | ENDING-DATE-OF-SERVICE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | 4 | ADJUDICATION-DATE | ||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | MEDICAID-PAID-DATE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | TYPE-OF-CLAIM | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | TYPE-OF-BILL | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | CLAIM-STATUS | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | CLAIM-STATUS-CATEGORY | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | SOURCE-LOCATION | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | CHECK-NUM | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | CHECK-EFF-DATE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | CLAIM-PYMT-REM-CODE-1 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | CLAIM-PYMT-REM-CODE-2 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | CLAIM-PYMT-REM-CODE-3 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | CLAIM-PYMT-REM-CODE-4 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | TOT-BILLED-AMT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | TOT-ALLOWED-AMT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | TOT-MEDICAID-PAID-AMT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | TOT-COPAY-AMT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | TOT-MEDICARE-DEDUCTIBLE-AMT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | TOT-MEDICARE-COINS-AMT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | TOT-TPL-AMT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | TOT-OTHER-INSURANCE-AMT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OTHER-INSURANCE-IND | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OTHER-TPL-COLLECTION | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | SERVICE-TRACKING-TYPE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | SERVICE-TRACKING-PAYMENT-AMT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | FIXED-PAYMENT-IND | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | FUNDING-CODE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | FUNDING-SOURCE-NONFEDERAL-SHARE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | MEDICARE-COMB-DED-IND | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | PROGRAM-TYPE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | PLAN-ID-NUMBER | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | NATIONAL-HEALTH-CARE-ENTITY-ID | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | PAYMENT-LEVEL-IND | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | MEDICARE-REIM-TYPE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | CLAIM-LINE-COUNT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | FORCED-CLAIM-IND | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | HEALTH-CARE-ACQUIRED-CONDITION-IND | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-01 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-02 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-03 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-04 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-05 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-06 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-07 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-08 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-09 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-10 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-EFF-DATE-01 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-EFF-DATE-02 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-EFF-DATE-03 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-EFF-DATE-04 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-EFF-DATE-05 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-EFF-DATE-06 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-EFF-DATE-07 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-EFF-DATE-08 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-EFF-DATE-09 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-EFF-DATE-10 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-END-DATE-01 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-END-DATE-02 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-END-DATE-03 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-END-DATE-04 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-END-DATE-05 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-END-DATE-06 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-END-DATE-07 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-END-DATE-08 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-END-DATE-09 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | OCCURRENCE-CODE-END-DATE-10 | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | PATIENT-CONTROL-NUM | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | ELIGIBLE-LAST-NAME | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | ELIGIBLE-FIRST-NAME | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | ELIGIBLE-MIDDLE-INIT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | DATE-OF-BIRTH | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | HEALTH-HOME-PROV-IND | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | WAIVER-TYPE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | WAIVER-ID | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BILLING-PROV-NUM | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BILLING-PROV-NPI-NUM | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BILLING-PROV-TAXONOMY | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BILLING-PROV-TYPE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BILLING-PROV-SPECIALTY | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | REFERRING-PROV-NUM | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | REFERRING-PROV-NPI-NUM | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | REFERRING-PROV-TAXONOMY | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | REFERRING-PROV-TYPE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | REFERRING-PROV-SPECIALTY | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | MEDICARE-HIC-NUM | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | PLACE-OF-SERVICE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BMI | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | REMITTANCE-NUM | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | DAILY-RATE | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BORDER-STATE-IND | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BENEFICIARY-COINSURANCE-AMOUNT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BENEFICIARY-COINSURANCE-DATE-PAID | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BENEFICIARY-COPAYMENT-AMOUNT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BENEFICIARY-COPAYMENT-DATE-PAID | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BENEFICIARY-DEDUCTIBLE-AMOUNT | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | CLAIM-DENIED-INDICATOR | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COPAY-WAIVED-IND | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | HEALTH-HOME-ENTITY-NAME | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | THIRD-PARTY-COINSURANCE-AMOUNT-PAID | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | THIRD-PARTY-COINSURANCE-DATE-PAID | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | THIRD-PARTY-COPAYMENT-AMOUNT-PAID | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | THIRD-PARTY-COPAYMENT-DATE-PAID | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | DATE-CAPITATED-AMOUNT-REQUESTED | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | CAPITATED-PAYMENT-AMT-REQUESTED | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | HEALTH-HOME-PROVIDER-NPI | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | MEDICARE-BENEFICIARY-IDENTIFIER | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | UNDER-DIRECTION-OF-PROV-NPI | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | UNDER-DIRECTION-OF-PROV-TAXONOMY | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | UNDER-SUPERVISION-OF-PROV-NPI | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | UNDER-SUPERVISION-OF-PROV-TAXONOMY | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | STATE-NOTATION | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | PROV-LOCATION-ID | |||
| CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | FILLER | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | RECORD-ID | None. The claim (or encounter record) should be submitted as it was adjudicated (or received) | There must be an active CLAIM-HEADER-RECORD-OT-COT00002 record in the current OT claim file submission that matches on: -- SUBMITTING-STATE -- ICN-ORIG -- ICN-ADJ -- ADJUDICATION-DATE. |
|
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | 1 | SUBMITTING-STATE | ||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | RECORD-NUMBER | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | MSIS-IDENTIFICATION-NUM | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | 2 | ICN-ORIG | ||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | 3 | ICN-ADJ | ||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | 4 | LINE-NUM-ORIG | ||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | 5 | LINE-NUM-ADJ | ||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | LINE-ADJUSTMENT-IND | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | LINE-ADJUSTMENT-REASON-CODE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | SUBMITTER-ID | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | CLAIM-LINE-STATUS | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | BEGINNING-DATE-OF-SERVICE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | ENDING-DATE-OF-SERVICE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | REVENUE-CODE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | PROCEDURE-CODE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | PROCEDURE-CODE-DATE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | PROCEDURE-CODE-FLAG | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | PROCEDURE-CODE-MOD-1 | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | IMMUNIZATION-TYPE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | BILLED-AMT | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | ALLOWED-AMT | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COPAY-AMT | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | TPL-AMT | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | MEDICAID-PAID-AMT | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | MEDICAID-FFS-EQUIVALENT-AMT | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | MEDICARE-PAID-AMT | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | OT-RX-CLAIM-QUANTITY-ACTUAL | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | OT-RX-CLAIM-QUANTITY-ALLOWED | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | TYPE-OF-SERVICE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | HCBS-SERVICE-CODE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | HCBS-TAXONOMY | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | SERVICING-PROV-NUM | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | SERVICING-PROV-NPI-NUM | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | SERVICING-PROV-TAXONOMY | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | SERVICING-PROV-TYPE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | SERVICING-PROV-SPECIALTY | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | OTHER-TPL-COLLECTION | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | TOOTH-DESIGNATION-SYSTEM | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | TOOTH-NUM | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | TOOTH-QUAD-CODE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | TOOTH-SURFACE-CODE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | ORIGINATION-ADDR-LN1 | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | ORIGINATION-ADDR-LN2 | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | ORIGINATION-CITY | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | ORIGINATION-STATE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | ORIGINATION-ZIP-CODE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | DESTINATION-ADDR-LN1 | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | DESTINATION-ADDR-LN2 | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | DESTINATION-CITY | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | DESTINATION-STATE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | DESTINATION-ZIP-CODE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | BENEFIT-TYPE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | XIX-MBESCBES-CATEGORY-OF-SERVICE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | XXI-MBESCBES-CATEGORY-OF-SERVICE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | OTHER-INSURANCE-AMT | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | STATE-NOTATION | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | NATIONAL-DRUG-CODE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | PROCEDURE-CODE-MOD-2 | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | PROCEDURE-CODE-MOD-3 | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | PROCEDURE-CODE-MOD-4 | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | HCPCS-RATE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | 6 | ADJUDICATION-DATE | ||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | SELF-DIRECTION-TYPE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | PRE-AUTHORIZATION-NUM | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | NDC-UNIT-OF-MEASURE | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | NDC-QUANTITY | |||
| CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | FILLER | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | RECORD-ID | None | ||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | DATA-DICTIONARY-VERSION | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | SUBMISSION-TRANSACTION-TYPE | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | FILE-ENCODING-SPECIFICATION | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | DATA-MAPPING-DOCUMENT-VERSION | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | FILE-NAME | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | SUBMITTING-STATE | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | DATE-FILE-CREATED | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | START-OF-TIME-PERIOD | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | END-OF-TIME-PERIOD | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | FILE-STATUS-INDICATOR | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | SSN-INDICATOR | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | TOT-REC-CNT | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | SEQUENCE-NUMBER | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | STATE-NOTATION | |||
| CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | FILLER | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | RECORD-ID | None. The claim (or encounter record) should be submitted as it was adjudicated (or received) | None | |
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | 1 | SUBMITTING-STATE | ||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | RECORD-NUMBER | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | 2 | ICN-ORIG | ||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | 3 | ICN-ADJ | ||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | SUBMITTER-ID | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | MSIS-IDENTIFICATION-NUM | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CROSSOVER-INDICATOR | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | 1115A-DEMONSTRATION-IND | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | ADJUSTMENT-IND | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | ADJUSTMENT-REASON-CODE | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | 4 | ADJUDICATION-DATE | ||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | MEDICAID-PAID-DATE | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | TYPE-OF-CLAIM | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CLAIM-STATUS | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CLAIM-STATUS-CATEGORY | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | SOURCE-LOCATION | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CHECK-NUM | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CHECK-EFF-DATE | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CLAIM-PYMT-REM-CODE-1 | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CLAIM-PYMT-REM-CODE-2 | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CLAIM-PYMT-REM-CODE-3 | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CLAIM-PYMT-REM-CODE-4 | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | TOT-BILLED-AMT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | TOT-ALLOWED-AMT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | TOT-MEDICAID-PAID-AMT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | TOT-COPAY-AMT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | TOT-MEDICARE-DEDUCTIBLE-AMT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | TOT-MEDICARE-COINS-AMT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | TOT-TPL-AMT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | TOT-OTHER-INSURANCE-AMT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | OTHER-INSURANCE-IND | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | OTHER-TPL-COLLECTION | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | SERVICE-TRACKING-TYPE | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | SERVICE-TRACKING-PAYMENT-AMT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | FIXED-PAYMENT-IND | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | FUNDING-CODE | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | FUNDING-SOURCE-NONFEDERAL-SHARE | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | PROGRAM-TYPE | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | PLAN-ID-NUMBER | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | NATIONAL-HEALTH-CARE-ENTITY-ID | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | PAYMENT-LEVEL-IND | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | MEDICARE-REIM-TYPE | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CLAIM-LINE-COUNT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | FORCED-CLAIM-IND | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | PATIENT-CONTROL-NUM | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | ELIGIBLE-LAST-NAME | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | ELIGIBLE-FIRST-NAME | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | ELIGIBLE-MIDDLE-INIT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | DATE-OF-BIRTH | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | HEALTH-HOME-PROV-IND | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | WAIVER-TYPE | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | WAIVER-ID | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | BILLING-PROV-NUM | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | BILLING-PROV-NPI-NUM | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | BILLING-PROV-TAXONOMY | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | BILLING-PROV-SPECIALTY | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | PRESCRIBING-PROV-NUM | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | PRESCRIBING-PROV-NPI-NUM | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | PRESCRIBING-PROV-TAXONOMY | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | PRESCRIBING-PROV-TYPE | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | PRESCRIBING-PROV-SPECIALTY | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | MEDICARE-HIC-NUM | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | REMITTANCE-NUM | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | BORDER-STATE-IND | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | DATE-PRESCRIBED | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | PRESCRIPTION-FILL-DATE | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | COMPOUND-DRUG-IND | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | BENEFICIARY-COINSURANCE-AMOUNT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | BENEFICIARY-COPAYMENT-AMOUNT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | BENEFICIARY-COPAYMENT-DATE-PAID | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | BENEFICIARY-COINSURANCE-DATE-PAID | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | BENEFICIARY-DEDUCTIBLE-AMOUNT | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CLAIM-DENIED-INDICATOR | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | COPAY-WAIVED-IND | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | HEALTH-HOME-ENTITY-NAME | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | THIRD-PARTY-COINSURANCE-AMOUNT-PAID | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | THIRD-PARTY-COINSURANCE-DATE-PAID | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | THIRD-PARTY-COPAYMENT-AMOUNT-PAID | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | THIRD-PARTY-COPAYMENT-DATE-PAID | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | DISPENSING-PRESCRIPTION-DRUG-PROV-NPI | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | DISPENSING-PRESCRIPTION-DRUG-PROV-TAXONOMY | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | HEALTH-HOME-PROVIDER-NPI | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | MEDICARE-BENEFICIARY-IDENTIFIER | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | STATE-NOTATION | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | DISPENSING-PRESCRIPTION-DRUG-PROV-NUM | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | MEDICARE-COMB-DED-IND | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | PROV-LOCATION-ID | |||
| CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | FILLER | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | RECORD-ID | None. The claim (or encounter record) should be submitted as it was adjudicated (or received) | There must be an active CLAIM-HEADER-RECORD-RX-COT00002 record in the current RX claim file submission that matches on: -- SUBMITTING-STATE -- ICN-ORIG -- ICN-ADJ -- ADJUDICATION-DATE. |
|
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | 1 | SUBMITTING-STATE | ||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | RECORD-NUMBER | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | MSIS-IDENTIFICATION-NUM | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | 2 | ICN-ORIG | ||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | 3 | ICN-ADJ | ||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | 4 | LINE-NUM-ORIG | ||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | 5 | LINE-NUM-ADJ | ||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | LINE-ADJUSTMENT-IND | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | LINE-ADJUSTMENT-REASON-CODE | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | SUBMITTER-ID | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CLAIM-LINE-STATUS | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | NATIONAL-DRUG-CODE | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | BILLED-AMT | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | ALLOWED-AMT | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | COPAY-AMT | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | TPL-AMT | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | MEDICAID-PAID-AMT | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | MEDICAID-FFS-EQUIVALENT-AMT | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | MEDICARE-DEDUCTIBLE-AMT | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | MEDICARE-COINS-AMT | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | MEDICARE-PAID-AMT | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | OT-RX-CLAIM-QUANTITY-ALLOWED | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | OT-RX-CLAIM-QUANTITY-ACTUAL | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | UNIT-OF-MEASURE | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | TYPE-OF-SERVICE | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | HCBS-SERVICE-CODE | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | HCBS-TAXONOMY | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | OTHER-TPL-COLLECTION | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | DAYS-SUPPLY | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | NEW-REFILL-IND | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | BRAND-GENERIC-IND | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | DISPENSE-FEE | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | PRESCRIPTION-NUM | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | DRUG-UTILIZATION-CODE | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | DTL-METRIC-DEC-QTY | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | COMPOUND-DOSAGE-FORM | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | REBATE-ELIGIBLE-INDICATOR | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | IMMUNIZATION-TYPE | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | BENEFIT-TYPE | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | XIX-MBESCBES-CATEGORY-OF-SERVICE | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | XXI-MBESCBES-CATEGORY-OF-SERVICE | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | OTHER-INSURANCE-AMT | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | STATE-NOTATION | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | 6 | ADJUDICATION-DATE | ||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | SELF-DIRECTION-TYPE | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | PRE-AUTHORIZATION-NUM | |||
| CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | FILLER | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | RECORD-ID | None | ||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | DATA-DICTIONARY-VERSION | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | SUBMISSION-TRANSACTION-TYPE | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | FILE-ENCODING-SPECIFICATION | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | DATA-MAPPING-DOCUMENT-VERSION | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | FILE-NAME | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | SUBMITTING-STATE | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | DATE-FILE-CREATED | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | START-OF-TIME-PERIOD | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | END-OF-TIME-PERIOD | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | FILE-STATUS-INDICATOR | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | SSN-INDICATOR | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | TOT-REC-CNT | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | SEQUENCE-NUMBER | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | STATE-NOTATION | |||
| ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | FILLER | |||
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | RECORD-ID | None | ||
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | RECORD-NUMBER | |||
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELIGIBLE-FIRST-NAME | |||
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELIGIBLE-LAST-NAME | |||
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELIGIBLE-MIDDLE-INIT | |||
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | SEX | |||
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | DATE-OF-BIRTH | |||
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | DATE-OF-DEATH | |||
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | (a) | PRIMARY-DEMOGRAPHIC-ELEMENT-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE and MSIS-IDENTIFICATION_NUM | |
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | PRIMARY-DEMOGRAPHIC-ELEMENT-END-DATE | |||
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | STATE-NOTATION | |||
| ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | FILLER | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | RECORD-NUMBER | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | MARITAL-STATUS | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | MARITAL-STATUS-OTHER-EXPLANATION | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | SSN | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | SSN-VERIFICATION-FLAG | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | INCOME-CODE | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | VETERAN-IND | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | CITIZENSHIP-IND | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | CITIZENSHIP-VERIFICATION-FLAG | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | IMMIGRATION-STATUS | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | IMMIGRATION-VERIFICATION-FLAG | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | IMMIGRATION-STATUS-FIVE-YEAR-BAR-END-DATE | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | PRIMARY-LANGUAGE-ENGL-PROF-CODE | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | PRIMARY-LANGUAGE-CODE | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | HOUSEHOLD-SIZE | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | PREGNANCY-IND | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | MEDICARE-HIC-NUM | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | MEDICARE-BENEFICIARY-IDENTIFIER | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | CHIP-CODE | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | (a) | VARIABLE-DEMOGRAPHIC-ELEMENT-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE and MSIS-IDENTIFICATION_NUM | |
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | VARIABLE-DEMOGRAPHIC-ELEMENT-END-DATE | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | STATE-NOTATION | |||
| ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | FILLER | |||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | RECORD-NUMBER | |||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | 3 | ADDR-TYPE | ||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELIGIBLE-ADDR-LN1 | |||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELIGIBLE-ADDR-LN2 | |||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELIGIBLE-ADDR-LN3 | |||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELIGIBLE-CITY | |||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELIGIBLE-STATE | |||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELIGIBLE-ZIP-CODE | |||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELIGIBLE-COUNTY-CODE | |||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELIGIBLE-PHONE-NUM | |||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | TYPE-OF-LIVING-ARRANGEMENT | |||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | (a) | ELIGIBLE-ADDR-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE MSIS-IDENTIFICATION_NUM, and ADDR-TYPE | |
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELIGIBLE-ADDR-END-DATE | |||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | STATE-NOTATION | |||
| ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | FILLER | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | RECORD-NUMBER | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | 3 | MSIS-CASE-NUM | ||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | MEDICAID-BASIS-OF-ELIGIBILITY | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | DUAL-ELIGIBLE-CODE | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | 4 | PRIMARY-ELIGIBILITY-GROUP-IND | ||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELIGIBILITY-GROUP | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | LEVEL-OF-CARE-STATUS | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | SSDI-IND | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | SSI-IND | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | SSI-STATE-SUPPLEMENT-STATUS-CODE | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | SSI-STATUS | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | STATE-SPEC-ELIG-GROUP | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | CONCEPTION-TO-BIRTH-IND | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELIGIBILITY-CHANGE-REASON | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | MAINTENANCE-ASSISTANCE-STATUS | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | RESTRICTED-BENEFITS-CODE | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | TANF-CASH-CODE | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | 5 | ELIGIBILITY-DETERMINANT-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE and MSIS-IDENTIFICATION_NUM, and MSIS-CASE-NUM | |
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELIGIBILITY-DETERMINANT-END-DATE | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | STATE-NOTATION | |||
| ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | FILLER | |||
| ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | RECORD-NUMBER | |||
| ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | 3 | HEALTH-HOME-SPA-NAME | ||
| ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | 4 | HEALTH-HOME-ENTITY-NAME | ||
| ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | (a) | HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, HEALTH-HOME-SPA-NAME, and HEALTH-HOME-ENTITY-NAME | |
| ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | HEALTH-HOME-SPA-PARTICIPATION-END-DATE | |||
| ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | HEALTH-HOME-ENTITY-EFF-DATE | |||
| ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | STATE-NOTATION | |||
| ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | FILLER | |||
| ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | RECORD-ID | There must be an active HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | RECORD-NUMBER | |||
| ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | 3 | HEALTH-HOME-SPA-NAME | ||
| ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | 4 | HEALTH-HOME-ENTITY-NAME | ||
| ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | 5 | HEALTH-HOME-PROV-NUM | ||
| ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | (a) | HEALTH-HOME-SPA-PROVIDER-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, HEALTH-HOME-SPA-NAME, HEALTH-HOME-ENTITY-NAME, and HEALTH-HOME-PROV-NUM | |
| ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | HEALTH-HOME-SPA-PROVIDER-END-DATE | |||
| ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | HEALTH-HOME-ENTITY-EFF-DATE | |||
| ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | STATE-NOTATION | |||
| ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | FILLER | |||
| ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | RECORD-NUMBER | |||
| ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | 3 | HEALTH-HOME-CHRONIC-CONDITION | ||
| ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | 4 | HEALTH-HOME-CHRONIC-CONDITION-OTHER-EXPLANATION | ||
| ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | (a) | HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, HEALTH-HOME-CHRONIC-CONDITION, and HEALTH-HOME-CHRONIC-CONDITION-OTHER-EXPLANATION | |
| ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | HEALTH-HOME-CHRONIC-CONDITION-END-DATE | |||
| ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | STATE-NOTATION | |||
| ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | FILLER | |||
| ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | RECORD-NUMBER | |||
| ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | 3 | LOCKIN-PROV-NUM | ||
| ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | 4 | LOCKIN-PROV-TYPE | ||
| ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | (a) | LOCKIN-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM,LOCKIN-PROV-NUM, and LOCKIN-PROV-TYPE | |
| ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | LOCKIN-END-DATE | |||
| ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | STATE-NOTATION | |||
| ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | FILLER | |||
| ELIGIBLE | MFP-INFORMATION-ELG00010 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | MFP-INFORMATION-ELG00010 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | MFP-INFORMATION-ELG00010 | RECORD-NUMBER | |||
| ELIGIBLE | MFP-INFORMATION-ELG00010 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | MFP-INFORMATION-ELG00010 | MFP-LIVES-WITH-FAMILY | |||
| ELIGIBLE | MFP-INFORMATION-ELG00010 | MFP-QUALIFIED-INSTITUTION | |||
| ELIGIBLE | MFP-INFORMATION-ELG00010 | MFP-QUALIFIED-RESIDENCE | |||
| ELIGIBLE | MFP-INFORMATION-ELG00010 | MFP-REASON-PARTICIPATION-ENDED | |||
| ELIGIBLE | MFP-INFORMATION-ELG00010 | MFP-REINSTITUTIONALIZED-REASON | |||
| ELIGIBLE | MFP-INFORMATION-ELG00010 | (a) | MFP-ENROLLMENT-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE and MSIS-IDENTIFICATION_NUM | |
| ELIGIBLE | MFP-INFORMATION-ELG00010 | MFP-ENROLLMENT-END-DATE | |||
| ELIGIBLE | MFP-INFORMATION-ELG00010 | STATE-NOTATION | |||
| ELIGIBLE | MFP-INFORMATION-ELG00010 | FILLER | |||
| ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | RECORD-NUMBER | |||
| ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | 3 | STATE-PLAN-OPTION-TYPE | ||
| ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | (a) | STATE-PLAN-OPTION-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, and STATE-PLAN-OPTION-TYPE | |
| ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | STATE-PLAN-OPTION-END-DATE | |||
| ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | STATE-NOTATION | |||
| ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | FILLER | |||
| ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | RECORD-NUMBER | |||
| ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | 3 | WAIVER-ID | ||
| ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | WAIVER-TYPE | |||
| ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | (a) | WAIVER-ENROLLMENT-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, and WAIVER-ID | |
| ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | WAIVER-ENROLLMENT-END-DATE | |||
| ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | STATE-NOTATION | |||
| ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | FILLER | |||
| ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | RECORD-NUMBER | |||
| ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | 3 | LTSS-LEVEL-CARE | ||
| ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | 4 | LTSS-PROV-NUM | ||
| ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | (a) | LTSS-ELIGIBILITY-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, LTSS-LEVEL-CARE, and LTSS-PROV-NUM | |
| ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | LTSS-ELIGIBILITY-END-DATE | |||
| ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | STATE-NOTATION | |||
| ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | FILLER | |||
| ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | RECORD-NUMBER | |||
| ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | 3 | MANAGED-CARE-PLAN-ID | ||
| ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | MANAGED-CARE-PLAN-TYPE | |||
| ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | NATIONAL-HEALTH-CARE-ENTITY-ID | |||
| ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | |||
| ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | (a) | MANAGED-CARE-PLAN-ENROLLMENT-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, and MANAGED-CARE-PLAN-ID | |
| ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | MANAGED-CARE-PLAN-ENROLLMENT-END-DATE | |||
| ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | STATE-NOTATION | |||
| ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | FILLER | |||
| ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | RECORD-NUMBER | |||
| ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | 3 | ETHNICITY-CODE | ||
| ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | (a) | ETHNICITY-DECLARATION-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, and ETHNICITY-CODE | |
| ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ETHNICITY-DECLARATION-END-DATE | |||
| ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | STATE-NOTATION | |||
| ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | FILLER | |||
| ELIGIBLE | RACE-INFORMATION-ELG00016 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | RACE-INFORMATION-ELG00016 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | RACE-INFORMATION-ELG00016 | RECORD-NUMBER | |||
| ELIGIBLE | RACE-INFORMATION-ELG00016 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | RACE-INFORMATION-ELG00016 | 3 | RACE | ||
| ELIGIBLE | RACE-INFORMATION-ELG00016 | 4 | RACE-OTHER | ||
| ELIGIBLE | RACE-INFORMATION-ELG00016 | CERTIFIED-AMERICAN-INDIAN/ALASKAN-NATIVE-INDICATOR | |||
| ELIGIBLE | RACE-INFORMATION-ELG00016 | (a) | RACE-DECLARATION-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, RACE, and RACE-OTHER | |
| ELIGIBLE | RACE-INFORMATION-ELG00016 | RACE-DECLARATION-END-DATE | |||
| ELIGIBLE | RACE-INFORMATION-ELG00016 | STATE-NOTATION | |||
| ELIGIBLE | RACE-INFORMATION-ELG00016 | FILLER | |||
| ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | RECORD-NUMBER | |||
| ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | 3 | DISABILITY-TYPE-CODE | ||
| ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | (a) | DISABILITY-TYPE-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, and DISABILITY-TYPE-CODE | |
| ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | DISABILITY-TYPE-END-DATE | |||
| ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | STATE-NOTATION | |||
| ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | FILLER | |||
| ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | RECORD-NUMBER | |||
| ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | 3 | 1115A-DEMONSTRATION-IND | ||
| ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | (a) | 1115A-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, and 1115A-DEMONSTRATION-IND | |
| ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | 1115A-END-DATE | |||
| ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | STATE-NOTATION | |||
| ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | FILLER | |||
| ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | RECORD-NUMBER | |||
| ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | 3 | HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-CODE | ||
| ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | (a) | HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, and HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-CODE | |
| ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-END-DATE | |||
| ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | STATE-NOTATION | |||
| ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | FILLER | |||
| ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | RECORD-ID | There must be an active PRIMARY DEMOGRAPHICS - ELIGIBILITY-ELG00002 record in the current Eligibility file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | 1 | SUBMITTING-STATE | ||
| ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | RECORD-NUMBER | |||
| ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | 2 | MSIS-IDENTIFICATION-NUM | ||
| ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | 3 | ENROLLMENT-TYPE | ||
| ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | (a) | ENROLLMENT-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, and ENROLLMENT-TYPE | |
| ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ENROLLMENT-END-DATE | |||
| ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | STATE-NOTATION | |||
| ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | FILLER | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | RECORD-ID | None | ||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | DATA-DICTIONARY-VERSION | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | SUBMISSION-TRANSACTION-TYPE | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | FILE-ENCODING-SPECIFICATION | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | DATA-MAPPING-DOCUMENT-VERSION | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | FILE-NAME | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | SUBMITTING-STATE | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | DATE-FILE-CREATED | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | START-OF-TIME-PERIOD | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | END-OF-TIME-PERIOD | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | FILE-STATUS-INDICATOR | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | TOT-REC-CNT | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | SEQUENCE-NUMBER | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | STATE-NOTATION | |||
| MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | FILLER | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | RECORD-ID | None | ||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | 1 | SUBMITTING-STATE | ||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | RECORD-NUMBER | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | 2 | STATE-PLAN-ID-NUM | ||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MANAGED-CARE-CONTRACT-EFF-DATE | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MANAGED-CARE-CONTRACT-END-DATE | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MANAGED-CARE-NAME | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MANAGED-CARE-PROGRAM | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MANAGED-CARE-PLAN-TYPE | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | REIMBURSEMENT-ARRANGEMENT | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MANAGED-CARE-PROFIT-STATUS | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | CORE-BASED-STATISTICAL-AREA-CODE | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | PERCENT-BUSINESS | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MANAGED-CARE-SERVICE-AREA | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | (a) | MANAGED-CARE-MAIN-REC-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE and STATE-PLAN-ID-NUM | |
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MANAGED-CARE-MAIN-REC-END-DATE | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | STATE-NOTATION | |||
| MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | FILLER | |||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | RECORD-ID | There must be an active MANAGED-CARE-MAIN-MCR00002 record in the current Managed Care file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records. | ||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | 1 | SUBMITTING-STATE | ||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | 2 | RECORD-NUMBER | ||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | 3 | STATE-PLAN-ID-NUM | ||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | 4 | MANAGED-CARE-LOCATION-ID | ||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | (a) | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, STATE-PLAN-ID-NUM, MANAGED-CARE-LOCATION-ID, and MANAGED-CARE-ADDR-TYPE | |
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-END-DATE | |||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | 5 | MANAGED-CARE-ADDR-TYPE | ||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MANAGED-CARE-ADDR-LN1 | |||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MANAGED-CARE-ADDR-LN2 | |||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MANAGED-CARE-ADDR-LN3 | |||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MANAGED-CARE-CITY | |||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MANAGED-CARE-STATE | |||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MANAGED-CARE-ZIP-CODE | |||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MANAGED-CARE-COUNTY | |||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MANAGED-CARE-TELEPHONE | |||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MANAGED-CARE-EMAIL | |||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MANAGED-CARE-FAX-NUMBER | |||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | STATE-NOTATION | |||
| MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | FILLER | |||
| MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | RECORD-ID | There must be an active MANAGED-CARE-MAIN-MCR00002 record in the current Managed Care file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records | ||
| MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | 1 | SUBMITTING-STATE | ||
| MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | RECORD-NUMBER | |||
| MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | 2 | STATE-PLAN-ID-NUM | ||
| MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | 3 | MANAGED-CARE-SERVICE-AREA-NAME | ||
| MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | (a) | MANAGED-CARE-SERVICE-AREA-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, STATE-PLAN-ID-NUM, and MMANAGED-CARE-SERVICE-AREA-NAME | |
| MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MANAGED-CARE-SERVICE-AREA-END-DATE | |||
| MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | STATE-NOTATION | |||
| MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | FILLER | |||
| MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | RECORD-ID | There must be an active MANAGED-CARE-MAIN-MCR00002 record in the current Managed Care file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records | ||
| MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | 1 | SUBMITTING-STATE | ||
| MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | RECORD-NUMBER | |||
| MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | 2 | STATE-PLAN-ID-NUM | ||
| MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | 3 | OPERATING-AUTHORITY | ||
| MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | 4 | WAIVER-ID | ||
| MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | (a) | MANAGED-CARE-OP-AUTHORITY-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, STATE-PLAN-ID-NUM, OPERATING-AUTHORITY, and WAIVER-ID | |
| MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MANAGED-CARE-OP-AUTHORITY-END-DATE | |||
| MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | STATE-NOTATION | |||
| MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | FILLER | |||
| MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | RECORD-ID | There must be an active MANAGED-CARE-MAIN-MCR00002 record in the current Managed Care file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records | ||
| MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | 1 | SUBMITTING-STATE | ||
| MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | RECORD-NUMBER | |||
| MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | 2 | STATE-PLAN-ID-NUM | ||
| MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | 3 | MANAGED-CARE-PLAN-POP | ||
| MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | (a) | MANAGED-CARE-PLAN-POP-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, STATE-PLAN-ID-NUM, and MANAGED-CARE-PLAN-POP | |
| MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MANAGED-CARE-PLAN-POP-END-DATE | |||
| MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | STATE-NOTATION | |||
| MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | FILLER | |||
| MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | RECORD-ID | There must be an active MANAGED-CARE-MAIN-MCR00002 record in the current Managed Care file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records | ||
| MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | 1 | SUBMITTING-STATE | ||
| MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | RECORD-NUMBER | |||
| MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | 2 | STATE-PLAN-ID-NUM | ||
| MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | 3 | ACCREDITATION-ORGANIZATION | ||
| MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | (a) | DATE-ACCREDITATION-ACHIEVED | No overlapping date spans for a given combination of SUBMTTING-STATE, STATE-PLAN-ID-NUM, ACCREDITATION-ORGANIZATION | |
| MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | DATE-ACCREDITATION-END | |||
| MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | STATE-NOTATION | |||
| MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | FILLER | |||
| MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | RECORD-ID | There must be an active MANAGED-CARE-MAIN-MCR00002 record in the current Managed Care file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records | ||
| MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | 1 | SUBMITTING-STATE | ||
| MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | RECORD-NUMBER | |||
| MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | 2 | STATE-PLAN-ID-NUM | ||
| MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | 3 | NATIONAL-HEALTH-CARE-ENTITY-ID | ||
| MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | 4 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | ||
| MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | NATIONAL-HEALTH-CARE-ENTITY-NAME | |||
| MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | (a) | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, STATE-PLAN-ID-NUM, NATIONAL-HEALTH-CARE-ENTITY-ID, and NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | |
| MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-END-DATE | |||
| MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | STATE-NOTATION | |||
| MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | FILLER | |||
| MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | RECORD-ID | There must be an active NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 record in the current Managed Care file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records | ||
| MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | 1 | SUBMITTING-STATE | ||
| MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | RECORD-NUMBER | |||
| MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | 2 | STATE-PLAN-ID-NUM | ||
| MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | 3 | CHPID | ||
| MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | 4 | SHPID | ||
| MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | (a) | CHPID-SHPID-RELATIONSHIP-EFF-DATE | No overlapping date spans for a given combination ofSUBMTTING-STATE, STATE-PLAN-ID-NUM, CHPID, and SHPID | |
| MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | CHPID-SHPID-RELATIONSHIP-END-DATE | |||
| MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | STATE-NOTATION | |||
| MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | FILLER | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | RECORD-ID | None | ||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | DATA-DICTIONARY-VERSION | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | SUBMISSION-TRANSACTION-TYPE | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | FILE-ENCODING-SPECIFICATION | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | DATA-MAPPING-DOCUMENT-VERSION | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | FILE-NAME | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | SUBMITTING-STATE | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | DATE-FILE-CREATED | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | START-OF-TIME-PERIOD | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | END-OF-TIME-PERIOD | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | FILE-STATUS-INDICATOR | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | TOT-REC-CNT | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | SEQUENCE-NUMBER | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | STATE-NOTATION | |||
| PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | FILLER | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | RECORD-ID | None | ||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | 1 | SUBMITTING-STATE | ||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | RECORD-NUMBER | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | 2 | SUBMITTING-STATE-PROV-ID | ||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | (a) | PROV-ATTRIBUTES-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE and STATE-PLAN-ID-NUM | |
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PROV-ATTRIBUTES-END-DATE | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PROV-DOING-BUSINESS-AS-NAME | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PROV-LEGAL-NAME | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PROV-ORGANIZATION-NAME | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PROV-TAX-NAME | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | FACILITY-GROUP-INDIVIDUAL-CODE | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | TEACHING-IND | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PROV-FIRST-NAME | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PROV-MIDDLE-INITIAL | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PROV-LAST-NAME | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | SEX | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | OWNERSHIP-CODE | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PROV-PROFIT-STATUS | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | DATE-OF-BIRTH | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | DATE-OF-DEATH | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | ACCEPTING-NEW-PATIENTS-IND | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | STATE-NOTATION | |||
| PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | FILLER | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | RECORD-ID | There must be an active PROV-ATTRIBUTES-MAIN-PRV00002 record in the current Provider file submission, and the effective date span of the child record segment must be fully contained within the set of effective date spans of the associated active parent records | ||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | 1 | SUBMITTING-STATE | ||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | 2 | RECORD-NUMBER | ||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | 3 | SUBMITTING-STATE-PROV-ID | ||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | 4 | PROV-LOCATION-ID | ||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | (a) | PROV-LOCATION-AND-CONTACT-INFO-EFF-DATE | No overlapping date spans for a given combination ofSUBMTTING-STATE, STATE-PLAN-ID-NUM, PROV-LOCATION-ID, and ADDR-TYPE | |
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PROV-LOCATION-AND-CONTACT-INFO-END-DATE | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | 5 | ADDR-TYPE | ||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | ADDR-LN1 | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | ADDR-LN2 | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | ADDR-LN3 | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | ADDR-CITY | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | ADDR-STATE | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | ADDR-ZIP-CODE | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | ADDR-TELEPHONE | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | ADDR-EMAIL | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | ADDR-FAX-NUM | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | ADDR-BORDER-STATE-IND | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | ADDR-COUNTY | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | STATE-NOTATION | |||
| PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | FILLER | |||
| PROVIDER | PROV-LICENSING-INFO-PRV00004 | RECORD-ID | There must be both an active PROV-ATTRIBUTES-MAIN-PRV00002 record segment and a PROV-LOCATION-AND-CONTACT-INFO-PRV00003 record in the current Provider file submission. In addition, the effective date span of the child record segment must be fully contained within the set of effective date spans of all active parent records. | ||
| PROVIDER | PROV-LICENSING-INFO-PRV00004 | 1 | SUBMITTING-STATE | ||
| PROVIDER | PROV-LICENSING-INFO-PRV00004 | RECORD-NUMBER | |||
| PROVIDER | PROV-LICENSING-INFO-PRV00004 | 2 | SUBMITTING-STATE-PROV-ID | ||
| PROVIDER | PROV-LICENSING-INFO-PRV00004 | 3 | PROV-LOCATION-ID | ||
| PROVIDER | PROV-LICENSING-INFO-PRV00004 | (a) | PROV-LICENSE-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, SUBMITTING-STATE-PROV-ID, PROV-LOCATION-ID, LICENSE-TYPE, and LICENSE-ISSUING-ENTITY-ID | |
| PROVIDER | PROV-LICENSING-INFO-PRV00004 | PROV-LICENSE-END-DATE | |||
| PROVIDER | PROV-LICENSING-INFO-PRV00004 | 4 | LICENSE-TYPE | ||
| PROVIDER | PROV-LICENSING-INFO-PRV00004 | 5 | LICENSE-ISSUING-ENTITY-ID | ||
| PROVIDER | PROV-LICENSING-INFO-PRV00004 | 6 | LICENSE-OR-ACCREDITATION-NUMBER | ||
| PROVIDER | PROV-LICENSING-INFO-PRV00004 | STATE-NOTATION | |||
| PROVIDER | PROV-LICENSING-INFO-PRV00004 | FILLER | |||
| PROVIDER | PROV-IDENTIFIERS-PRV00005 | RECORD-ID | There must be both an active PROV-ATTRIBUTES-MAIN-PRV00002 record segment and a PROV-LOCATION-AND-CONTACT-INFO-PRV00003 record in the current provider file submission. In addition, the effective date span of the child record segment must be fully contained within the set of effective date spans of all active parent records. | ||
| PROVIDER | PROV-IDENTIFIERS-PRV00005 | 1 | SUBMITTING-STATE | ||
| PROVIDER | PROV-IDENTIFIERS-PRV00005 | RECORD-NUMBER | |||
| PROVIDER | PROV-IDENTIFIERS-PRV00005 | 2 | SUBMITTING-STATE-PROV-ID | ||
| PROVIDER | PROV-IDENTIFIERS-PRV00005 | 3 | PROV-LOCATION-ID | ||
| PROVIDER | PROV-IDENTIFIERS-PRV00005 | 4 | PROV-IDENTIFIER-TYPE | ||
| PROVIDER | PROV-IDENTIFIERS-PRV00005 | 5 | PROV-IDENTIFIER-ISSUING-ENTITY-ID | ||
| PROVIDER | PROV-IDENTIFIERS-PRV00005 | (a) | PROV-IDENTIFIER-EFF-DATE | No overlapping date spans for a given combination of SUBMITTING-STATE, SUBMITTING-STATE-PROV-ID, PROV-LOCATION-ID, PROV-IDENTIFIER-TYPE, PROV-IDENTIFIER-ISSUING-ENTITY-ID, and PROV-IDENTIFIER | |
| PROVIDER | PROV-IDENTIFIERS-PRV00005 | PROV-IDENTIFIER-END-DATE | |||
| PROVIDER | PROV-IDENTIFIERS-PRV00005 | 6 | PROV-IDENTIFIER | ||
| PROVIDER | PROV-IDENTIFIERS-PRV00005 | STATE-NOTATION | |||
| PROVIDER | PROV-IDENTIFIERS-PRV00005 | FILLER | |||
| PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | RECORD-ID | There must be an active PROV-ATTRIBUTES-MAIN-PRV00002 record segment in the current provider file submission. In addition, the effective date span of the child record segment must be fully contained within the set of effective date spans of all active parent records. | ||
| PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | 1 | SUBMITTING-STATE | ||
| PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | RECORD-NUMBER | |||
| PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | 2 | SUBMITTING-STATE-PROV-ID | ||
| PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | 3 | PROV-CLASSIFICATION-TYPE | ||
| PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | 4 | PROV-CLASSIFICATION-CODE | ||
| PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | (a) | PROV-TAXONOMY-CLASSIFICATION-EFF-DATE | No overlapping date spans for a given combination of SUBMITTING-STATE, SUBMITTING-STATE-PROV-ID, PROV-CLASSIFICATION-TYPE, PROV-CLASSIFICATION-CODE | |
| PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PROV-TAXONOMY-CLASSIFICATION-END-DATE | |||
| PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | STATE-NOTATION | |||
| PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | FILLER | |||
| PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | RECORD-ID | There must be an active PROV-ATTRIBUTES-MAIN-PRV00002 record segment in the current provider file submission. In addition, the effective date span of the child record segment must be fully contained within the set of effective date spans of all active parent records. | ||
| PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | 1 | SUBMITTING-STATE | ||
| PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | RECORD-NUMBER | |||
| PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | 2 | SUBMITTING-STATE-PROV-ID | ||
| PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | (a) | PROV-MEDICAID-EFF-DATE | No overlapping date spans for a given combination of SUBMITTING-STATE, SUBMITTING-STATE-PROV-ID, and PROV-MEDICIAD-ENROLLMENT-STATUS-CODE | |
| PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PROV-MEDICAID-END-DATE | |||
| PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | 3 | PROV-MEDICAID-ENROLLMENT-STATUS-CODE | ||
| PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | STATE-PLAN-ENROLLMENT | |||
| PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PROV-ENROLLMENT-METHOD | |||
| PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | APPL-DATE | |||
| PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | STATE-NOTATION | |||
| PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | FILLER | |||
| PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | RECORD-ID | There must be an active PROV-ATTRIBUTES-MAIN-PRV00002 record in the current provider file submission for both the SUBMITTING-STATE-PROV-ID and the SUBMITTING-STATE-PROV-ID-OF-AFFILIATED-ENTITY, and the effective date span of the child record segment must be fully contained within the set of effective date spans of all active parent records. | ||
| PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | 1 | SUBMITTING-STATE | ||
| PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | RECORD-NUMBER | |||
| PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | 2 | SUBMITTING-STATE-PROV-ID | ||
| PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | 3 | SUBMITTING-STATE-PROV-ID-OF-AFFILIATED-ENTITY | ||
| PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | (a) | PROV-AFFILIATED-GROUP-EFF-DATE | No overlapping date spans for a given combination of SUBMITTING-STATE and SUBMITTING-STATE-PROV-ID | |
| PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PROV-AFFILIATED-GROUP-END-DATE | |||
| PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | STATE-NOTATION | |||
| PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | FILLER | |||
| PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | RECORD-ID | There must be an active PROV-ATTRIBUTES-MAIN-PRV00002 record in the current provider file submission for the SUBMITTING-STATE-PROV-ID and the effective date span of the child record segment must be fully contained within the set of effective date spans of all active parent records. | ||
| PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | 1 | SUBMITTING-STATE | ||
| PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | RECORD-NUMBER | |||
| PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | 2 | SUBMITTING-STATE-PROV-ID | ||
| PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | 3 | AFFILIATED-PROGRAM-TYPE | ||
| PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | 4 | AFFILIATED-PROGRAM-ID | ||
| PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | (a) | PROV-AFFILIATED-PROGRAM-EFF-DATE | No overlapping date spans for a given combination of SUBMITTING-STATE, SUBMITTING-STATE-PROV-ID, AFFILIATED-PROGRAM-TYPE, and AFFILIATED-PROGRAM-ID | |
| PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PROV-AFFILIATED-PROGRAM-END-DATE | |||
| PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | STATE-NOTATION | |||
| PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | FILLER | |||
| PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | RECORD-ID | There must be both an active PROV-ATTRIBUTES-MAIN-PRV00002 record segment and a PROV-LOCATION-AND-CONTACT-INFO-PRV00003 record in the current provider file submission. In addition, the effective date span of the child record segment must be fully contained within the set of effective date spans of all active parent records. | ||
| PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | 1 | SUBMITTING-STATE | ||
| PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | RECORD-NUMBER | |||
| PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | 2 | SUBMITTING-STATE-PROV-ID | ||
| PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | 3 | PROV-LOCATION-ID | ||
| PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | (a) | BED-TYPE-EFF-DATE | No overlapping date spans for a given combination of SUBMITTING-STATE, SUBMITTING-STATE-PROV-ID, PROV-LOCATION-ID, and BED-TYPE-CODE | |
| PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | BED-TYPE-END-DATE | |||
| PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | 4 | BED-TYPE-CODE | ||
| PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | BED-COUNT | |||
| PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | STATE-NOTATION | |||
| PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | FILLER | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | RECORD-ID | None | ||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | DATA-DICTIONARY-VERSION | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | SUBMISSION-TRANSACTION-TYPE | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | FILE-ENCODING-SPECIFICATION | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | DATA-MAPPING-DOCUMENT-VERSION | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | FILE-NAME | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | SUBMITTING-STATE | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | DATE-FILE-CREATED | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | START-OF-TIME-PERIOD | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | END-OF-TIME-PERIOD | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | FILE-STATUS-INDICATOR | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | SSN-INDICATOR | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TOT-REC-CNT | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | SEQUENCE-NUMBER | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | STATE-NOTATION | |||
| TPL | FILE-HEADER-RECORD-TPL-TPL00001 | FILLER | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | RECORD-ID | None | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | 1 | SUBMITTING-STATE | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | RECORD-NUMBER | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | 2 | MSIS-IDENTIFICATION-NUM | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL-HEALTH-INSURANCE-COVERAGE-IND | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL-OTHER-COVERAGE-IND | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | ELIGIBLE-FIRST-NAME | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | ELIGIBLE-MIDDLE-INIT | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | ELIGIBLE-LAST-NAME | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | (a) | ELIG-PRSN-MAIN-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE and MSIS-IDENTIFICATION_NUM | |
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | ELIG-PRSN-MAIN-END-DATE | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | STATE-NOTATION | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | FILLER | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | RECORD-ID | There must be both an active TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 record segment and a TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 record in the current TPL file submission. In addition, the effective date span of the child record segment must be fully contained within the set of effective date spans of all active parent records. | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | 1 | SUBMITTING-STATE | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | RECORD-NUMBER | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | 2 | MSIS-IDENTIFICATION-NUM | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | 3 | INSURANCE-CARRIER-ID-NUM | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | 4 | INSURANCE-PLAN-ID | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | 5 | GROUP-NUM | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | 6 | MEMBER-ID | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | INSURANCE-PLAN-TYPE | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | COVERAGE-TYPE | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | ANNUAL-DEDUCTIBLE-AMT | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | POLICY-OWNER-FIRST-NAME | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | POLICY-OWNER-LAST-NAME | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | POLICY-OWNER-SSN | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | POLICY-OWNER-CODE | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | (a) | INSURANCE-COVERAGE-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE and MSIS-IDENTIFICATION_NUM, INSURANCE-CARRIER-ID-NUM, INSURANCE-PLAN-ID, GROUP-NUM, MEMBER-ID, and COVERAGE-TYPE | |
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | INSURANCE-COVERAGE-END-DATE | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | STATE-NOTATION | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | FILLER | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | RECORD-ID | There must be an active TPL-ENTITY-CONTACT-INFORMATION-TPL00006 record segment in the current TPL file submission. In addition, the effective date span of the child record segment must be fully contained within the set of effective date spans of all active parent records. | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | 1 | SUBMITTING-STATE | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | RECORD-NUMBER | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | 2 | INSURANCE-CARRIER-ID-NUM | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | 3 | INSURANCE-PLAN-ID | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | INSURANCE-PLAN-TYPE | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | 4 | COVERAGE-TYPE | ||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | (a) | INSURANCE-CATEGORIES-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, INSURANCE-CARRIER-ID-NUM, INSURANCE-PLAN-ID, and COVERAGE-TYPE | |
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | INSURANCE-CATEGORIES-END-DATE | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | STATE-NOTATION | |||
| TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | FILLER | |||
| TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | RECORD-ID | There must be an active TPL-ELIGIBLE-PERSON-MAIN-TPL00002 record segment in the current TPL file submission. In addition, the effective date span of the child record segment must be fully contained within the set of effective date spans of all active parent records. | ||
| TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | 1 | SUBMITTING-STATE | ||
| TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | RECORD-NUMBER | |||
| TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | 2 | MSIS-IDENTIFICATION-NUM | ||
| TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | 3 | TYPE-OF-OTHER-THIRD-PARTY-LIABILITY | ||
| TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | (a) | OTHER-TPL-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, MSIS-IDENTIFICATION_NUM, and TYPE-OF-OTHER-THIRD-PARTY-LIABILITY | |
| TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | OTHER-TPL-END-DATE | |||
| TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | STATE-NOTATION | |||
| TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | FILLER | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | RECORD-ID | None | ||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | 1 | SUBMITTING-STATE | ||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | RECORD-NUMBER | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | 2 | INSURANCE-CARRIER-ID-NUM | ||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | 3 | TPL-ENTITY-ADDR-TYPE | ||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | INSURANCE-CARRIER-ADDR-LN1 | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | INSURANCE-CARRIER-ADDR-LN2 | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | INSURANCE-CARRIER-ADDR-LN3 | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | INSURANCE-CARRIER-CITY | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | INSURANCE-CARRIER-STATE | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | INSURANCE-CARRIER-ZIP-CODE | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | INSURANCE-CARRIER-PHONE-NUM | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | (a) | TPL-ENTITY-CONTACT-INFO-EFF-DATE | No overlapping date spans for a given combination of SUBMTTING-STATE, INSURANCE-CARRIER-ID-NUM, and TPL-ENTITY-ADDR-TYPE | |
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL-ENTITY-CONTACT-INFO-END-DATE | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | STATE-NOTATION | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | INSURANCE-CARRIER-NAIC-CODE | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | INSURANCE-CARRIER-NAME | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | NATIONAL-HEALTH-CARE-ENTITY-ID | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | NATIONAL-HEALTH-CARE-ENTITY-NAME | |||
| TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | FILLER |
Sheet 4: Record Segment Relationships
| Record Segment Relationships | ||||||||||||||||
| Claim IP File | ||||||||||||||||
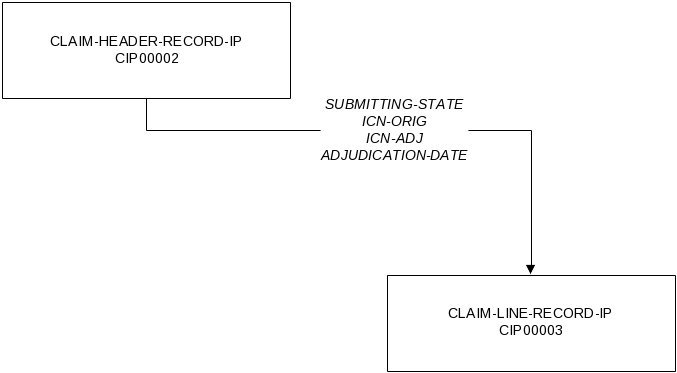
|
||||||||||||||||
| Claim LT File | ||||||||||||||||
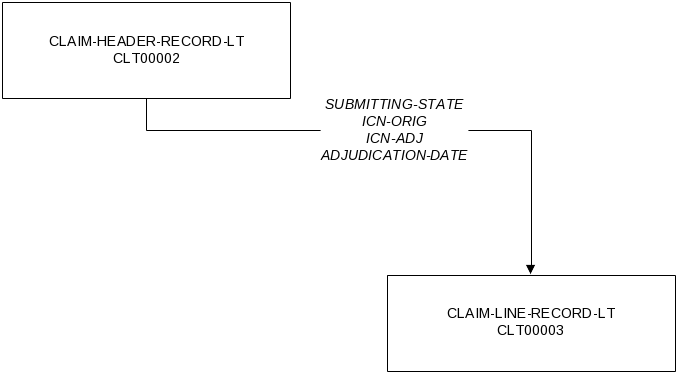
|
||||||||||||||||
| Claim OT File | ||||||||||||||||
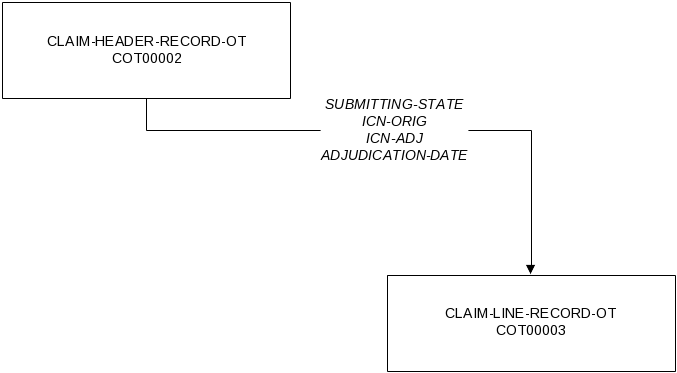
|
||||||||||||||||
| Claim RX File | ||||||||||||||||
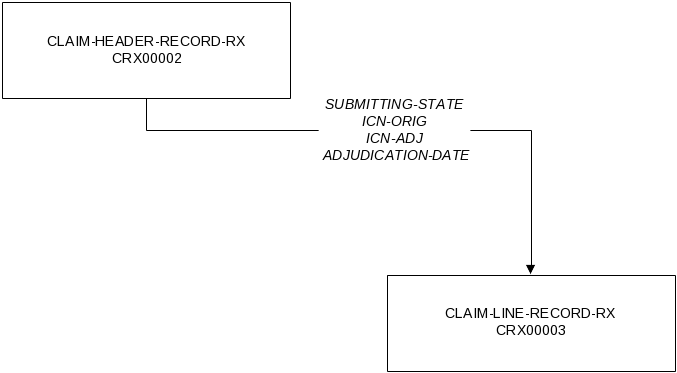
|
||||||||||||||||
| Eligible File | ||||||||||||||||
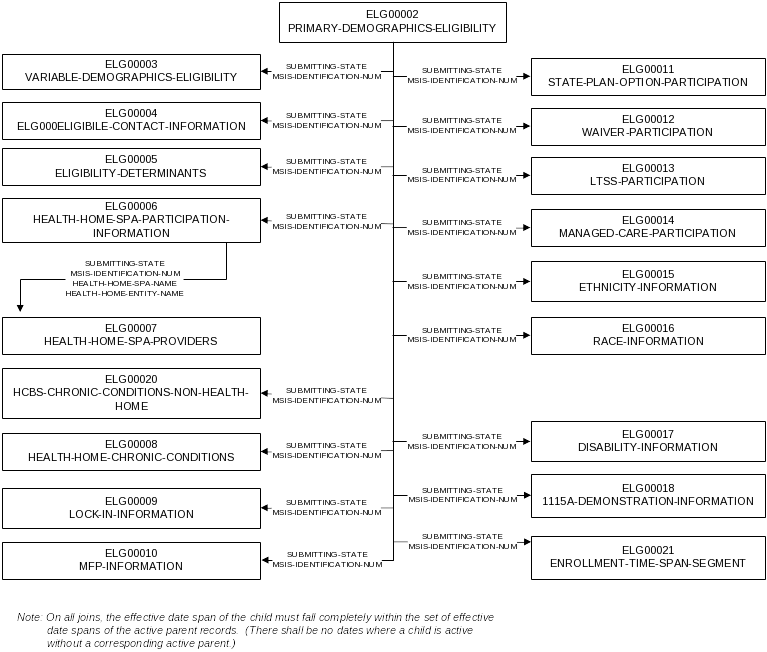
|
||||||||||||||||
| Provider File | ||||||||||||||||
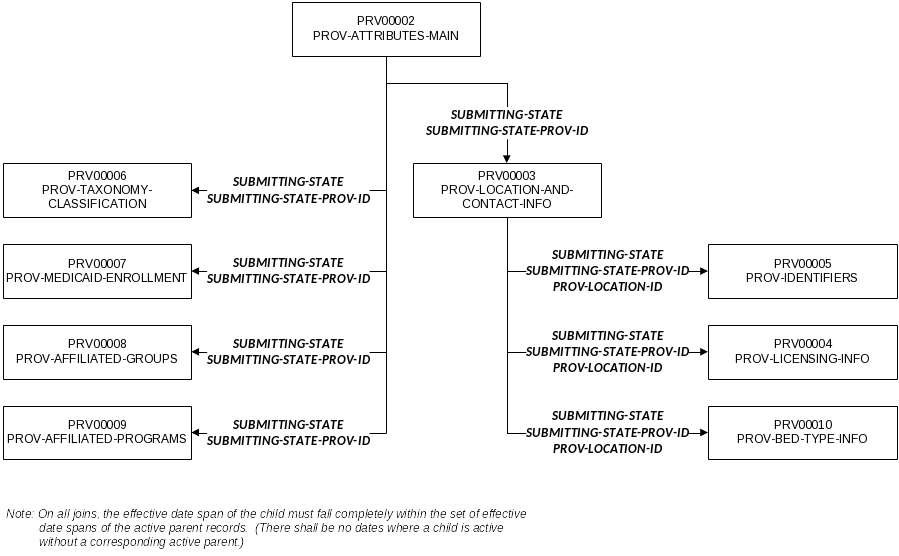
|
||||||||||||||||
| Managed Care File | ||||||||||||||||
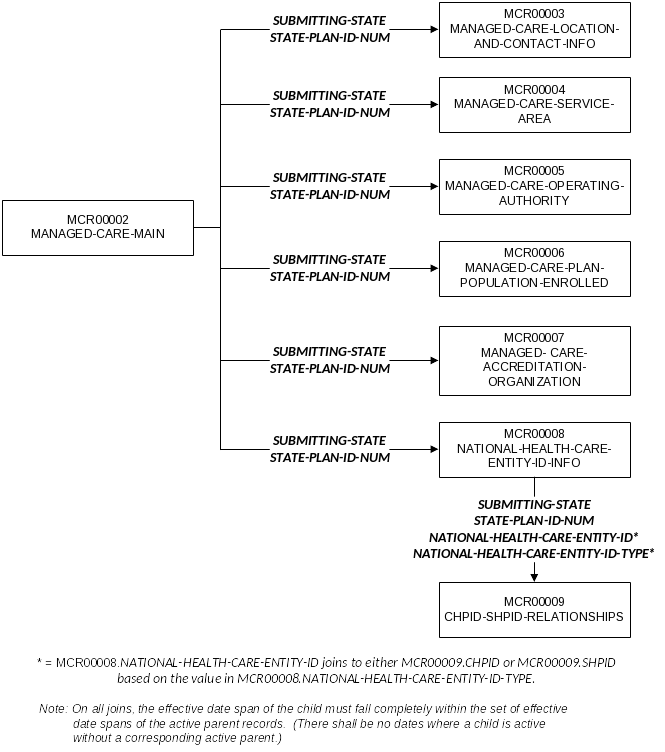
|
||||||||||||||||
| TPL File | ||||||||||||||||
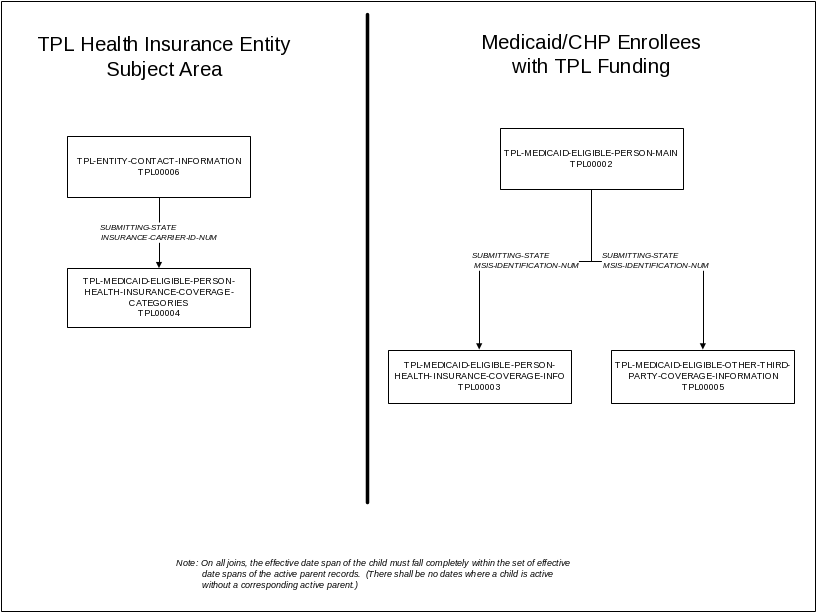
|
||||||||||||||||
Sheet 5: Data Element Definitions, Etc.
| V2.0 T-MSIS Data Dictionary | ||||||||||
| RowNo |
|
|
|
|
|
|
|
|
|
|
| 1 | CIP001 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the CLAIM-HEADER-RECORD-IP record segment is CIP00002 | Required | Value must be equal to a valid value. | CIP00001 - FILE-HEADER-RECORD-IP | 4/30/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP001-0001 |
| 2 | CIP001 | RECORD-ID | Must be populated on every record | 4/30/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP001-0002 | |||
| 3 | CIP001 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP001-0003 | |||
| 4 | CIP002 | DATA-DICTIONARY-VERSION | A data element to capture the version of the T-MSIS data dictionary that was used to build the file. | Required | Use the version number specified on the title page of the data dictionary | 2/25/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP002-0001 | |
| 5 | CIP003 | SUBMISSION-TRANSACTION-TYPE | A data element to identify the whether the transactions in the file are original submissions of the data, a resubmission of a previously submitted file, or corrections of edit rejects. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP003-0001 |
| 6 | CIP004 | FILE-ENCODING-SPECIFICATION | A data element to denote whether the file is in fixed length line format or pipe-delimited format | Required | Value must be equal to a valid value. | FLF The file follows a fixed length format. PSV The file follows a pipe-delimited format. |
4/30/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP004-0001 |
| 7 | CIP005 | DATA-MAPPING-DOCUMENT-VERSION | A data element to identify the version of the T-MSIS data mapping document used to build the file. | Required | Use the version number specified on the title page of the data mapping document | 2/25/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP005-0001 | |
| 8 | CIP006 | FILE-NAME | The name identifying the subject area to which the records in its file relate. Each T-MSIS submission file should only contain records for one subject area (i.e., Eligible, Third-party Liability, Provider, Managed Care Plan Information, IP claims, LT claims, Rx claims, or OT claims). | Required | Value must be equal to a valid value. | CLAIM-IP - Inpatient Claim/Encounters File - Claims/encounters with TYPE-OF-SERVICE = 001, 058, 084, 086, 090, 091, 092, 093, 123, or 132. (Note: In CLAIMIP, TYPE-OF-SERVICE 086 and 084 refer only to services received on an inpatient basis.) |
10/10/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP006-0001 |
| 9 | CIP007 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be numeric |
http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP007-0001 |
| 10 | CIP007 | SUBMITTING-STATE | Value must be equal to a valid value. | 2/25/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP007-0002 | |||
| 11 | CIP007 | SUBMITTING-STATE | Must be populated on every record. | 4/30/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP007-0003 | |||
| 12 | CIP007 | SUBMITTING-STATE | SUBMITTING-STATE must be equal across all record segments for a given record. | 4/30/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP007-0004 | |||
| 13 | CIP008 | DATE-FILE-CREATED | The date on which the file was created. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP008-0001 | |
| 14 | CIP008 | DATE-FILE-CREATED | Value must be a valid date | 4/30/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP008-0002 | |||
| 15 | CIP008 | DATE-FILE-CREATED | Date must be equal to or later than the date entered in the END-OF-TIME-PERIOD field. | 10/10/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP008-0003 | |||
| 16 | CIP009 | START-OF-TIME-PERIOD | Beginning date of the time period covered by this file. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP009-0001 | |
| 17 | CIP009 | START-OF-TIME-PERIOD | Value must be a valid date | 4/30/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP009-0002 | |||
| 18 | CIP010 | END-OF-TIME-PERIOD | Last date of the reporting period covered by the file to which this Header Record is attached. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP010-0001 | |
| 19 | CIP010 | END-OF-TIME-PERIOD | Value must be a valid date | 4/30/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP010-0002 | |||
| 20 | CIP011 | FILE-STATUS-INDICATOR | A code to indicate whether the records in the file are test or production records. | Required | Value must be equal to a valid value. | P Production File T Test File |
2/25/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP011-0001 |
| 21 | CIP012 | SSN-INDICATOR | Indicates whether the state uses the eligible person's social security number (SSN) instead of an MSIS identification number as the unique, unchanging eligible person identifier. | Required | Value must be equal to a valid value. | 0 State does not use SSN as MSIS-IDENTIFICATION-NUMBER 1 State uses SSN as MSIS-IDENTIFICATION-NUMBER |
4/30/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP012-0001 |
| 22 | CIP012 | SSN-INDICATOR | A state's SSN/Non-SSN designation on the eligibility file should match on the claims files. | 4/30/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP012-0002 | |||
| 23 | CIP012 | SSN-INDICATOR | States that are non SSN states must not submit MSIS Identification Numbers and SSNs that match for eligible individuals. | 4/30/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP012-0003 | |||
| 24 | CIP013 | TOT-REC-CNT | A count of all records in the file except for the file header record. This count will be used as a control total to help assure that the file did not become corrupted during transmission. | Required | An integer value with no commas | 10/10/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP013-0001 | |
| 25 | CIP275 | SEQUENCE-NUMBER | To enable state’s to sequentially number files, when related, follow-on files are necessary (i.e., update files, replacement files). This should begin with 1 for the original Create submission type and be incremented by one for each Replacement or Update submission for the same reporting period and file type (subject area). | Required | Field is required on all 'C', 'U', and 'R' record files. | 10/10/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP275-0001 | |
| 26 | CIP275 | SEQUENCE-NUMBER | Must be numeric and > 0 | 10/10/2013 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP275-0002 | |||
| 27 | CIP014 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP014-0001 | |
| 28 | CIP014 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP014-0002 | |||
| 29 | CIP015 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | CLAIMIP | FILE-HEADER-RECORD-IP-CIP00001 | CIP015-0001 | |||
| 30 | CIP016 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the CLAIM-HEADER-RECORD-IP record segment is CIP00002. | Required | Value must be equal to a valid value. | CIP00002 - CLAIM-HEADER-RECORD-IP | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP016-0001 |
| 31 | CIP016 | RECORD-ID | Must be populated on every record | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP016-0002 | |||
| 32 | CIP016 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP016-0003 | |||
| 33 | CIP017 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP017-0001 |
| 34 | CIP017 | SUBMITTING-STATE | Value must be numeric |
4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP017-0002 | |||
| 35 | CIP017 | SUBMITTING-STATE | Must be populated on every record | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP017-0003 | |||
| 36 | CIP017 | SUBMITTING-STATE | SUBMITTING-STATE must be equal across all record segments for a given record. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP017-0004 | |||
| 37 | CIP018 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP018-0001 | |
| 38 | CIP018 | RECORD-NUMBER | Must be numeric | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP018-0002 | |||
| 39 | CIP018 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP018-0003 | |||
| 40 | CIP019 | ICN-ORIG | A unique number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies an original claim. | Required | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP019-0001 | |
| 41 | CIP019 | ICN-ORIG | Record the value exactly as it appears in the State system. Do not pad. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP019-0002 | |||
| 42 | CIP019 | ICN-ORIG | This field should always be populated with the claim identification number assigned to the original paid/denied claim. This identification number should remain constant and be carried forward onto any adjustment claims. The intention is for this earliest claim identification number to be the link that ties the original claim and all adjustment claims together. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP019-0003 | |||
| 43 | CIP019 | ICN-ORIG | This field should not be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP019-0004 | |||
| 44 | CIP020 | ICN-ADJ | A unique claim number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies the adjustment claim for an original transaction. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP020-0001 | |
| 45 | CIP020 | ICN-ADJ | Record the value exactly as it appears in the State system. Do not pad. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP020-0002 | |||
| 46 | CIP020 | ICN-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP020-0003 | |||
| 47 | CIP021 | SUBMITTER-ID | The Submitter ID number is the value that identifies the provider/trading partner/clearing house organization to the state’s claim adjudication system. |
Conditional | Value must not be null | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP021-0001 | |
| 48 | CIP022 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Conditional | MSIS Identification Number must be reported | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP022-0001 | |
| 49 | CIP022 | MSIS-IDENTIFICATION-NUM | For non-SSN States, this field must contain an identification number assigned by the State. The format of the State ID numbers must be supplied to CMS. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP022-0002 | |||
| 50 | CIP022 | MSIS-IDENTIFICATION-NUM | For TYPE-OF-CLAIM = 4 or D or X (lump sum adjustments), this field must begin with an ‘&’. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP022-0003 | |||
| 51 | CIP022 | MSIS-IDENTIFICATION-NUM | For SSN States, this field must contain the Eligible's Social Security Number. If the SSN is unknown and a temporary number is assigned, this field will contain that number. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP022-0004 | |||
| 52 | CIP023 | CROSSOVER-INDICATOR | An indicator specifying whether the claim is a crossover claim where a portion is paid by Medicare. | Required | Value must be equal to a valid value. | 0 Not Crossover Claim 1 Crossover Claim 9 Unknown |
4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP023-0001 |
| 53 | CIP023 | CROSSOVER-INDICATOR | If Crossover Indicator is Yes, there must be Medicare enrollment in the Eligible file for the same time period (by date of service). | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP023-0002 | |||
| 54 | CIP023 | CROSSOVER-INDICATOR | Detail records should be created for all crossover claims. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP023-0003 | |||
| 55 | CIP024 | TYPE-OF-HOSPITAL | This code denotes the type of hospital on the claim (servicing provider). | Required | Value must be equal to a valid value. | 00 Not a hospital 01 Inpatient Hospital 02 Outpatient Hospital 03 Critical Access Hospital 04 Swing Bed Hospital 05 Inpatient Psychiatric Hospital 06 IHS Hospital 07 Children’s Hospital 08 Other 99 Unknown |
10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP024-0001 |
| 56 | CIP025 | 1115A-DEMONSTRATION-IND | Indicates that the individual participates in an 1115(A) demonstration. 1115(A) is a Center for Medicare and Medicaid Innovation (CMMI) demonstration. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP025-0001 |
| 57 | CIP025 | 1115A-DEMONSTRATION-IND | If 1115A-DEMONSTRATION-IND set to Yes on claim then there must be a 1115A-DEMONSTRATION-IND set to Yes (1115 participant) in the T-MSIS Eligible file with the same MSIS ID and/or SSN, an 1115A-EFF-DATE < the begin date of service and an 1115A-END-DATE > the end date of service on the claim. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP025-0002 | |||
| 58 | CIP026 | ADJUSTMENT-IND | Code indicating type of adjustment record. | Required | Value must be equal to a valid value. | 0 Original Claim / Encounter 1 Void of a prior submission 2 Re-submittal 3 Credit Adjustment (negative supplemental) 4 Debit Adjustment (positive supplemental) 5 Credit Gross Adjustment. 6 Debit Gross Adjustment 9 Unknown |
4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP026-0001 |
| 59 | CIP027 | ADJUSTMENT-REASON-CODE | Claim adjustment reason codes communicate why a claim was paid differently than it was billed. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-adjustment-reason-codes/ | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP027-0001 |
| 60 | CIP027 | ADJUSTMENT-REASON-CODE | If there is no adjustment to a claim, then there is no adjustment reason code. (Also see: CLAIM-PYMT-REM-CODE). If claim record does not represent an adjustment, 8-fill | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP027-0002 | |||
| 61 | CIP028 | ADMISSION-TYPE | The basic types of admission for Inpatient hospital stays and a code indicating the priority of this admission. | Required | Value must be equal to a valid value. | 1 EMERGENCY The patient requires immediate medical intervention as a result of severe, life threatening or potentially disabling conditions. Generally, the patient is admitted through the emergency room. 2 URGENT The patient requires immediate attention for the care and treatment of a physical or mental disorder. Generally, the patient is admitted to the first available and suitable accommodation. 3 ELECTIVE The patient’s condition permits adequate time to schedule the availability of a suitable accommodation. 4 NEWBORN The patient is a newborn delivered either inside the admitting hospital (UB04 FL 15 value 5 [A baby born inside the admitting hospital] or outside of the hospital (UB04 FL 15 value “6” [A baby born outside the admitting hospital]). 5 TRAUMA The patient visits a trauma center ( A trauma center means a facility licensed or designated by the State or local government authority authorized to do so, or as verified by the American College of surgeons and involving a trauma activation.) 8 NOT AVALIABLE 9 UNKNOWN |
4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP028-0001 |
| 62 | CIP028 | ADMISSION-TYPE | Value as it is reported in FL 14 - Type of Admission/Visit on the UB04. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP028-0002 | |||
| 63 | CIP029 | DRG-DESCRIPTION | Description of the associated state-specific DRG code. If using standard MS-DRG classification system, leave blank |
Conditional | Value must originate from the DRGS list or be blank. | http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY-2013-IPPS-Final-Rule-Home-Page-Items/FY2013-Final-Rule-Tables.html?DLPage=1&DLSort=0&DLSortDir=ascending | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP029-0001 |
| 64 | CIP029 | DRG-DESCRIPTION | States using the federal code should leave DRG-description blank; otherwise they should use a code that legitimately belongs to their code set. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP029-0002 | |||
| 65 | CIP030 | ADMITTING-DIAGNOSIS-CODE | The ICD-9/10-CM Diagnosis Code provided at the time of admission by the physician. | Required | Code full valid ICD 9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 “. Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP030-0001 |
| 66 | CIP030 | ADMITTING-DIAGNOSIS-CODE | E-codes are not valid as Admitting Diagnosis Codes. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP030-0002 | |||
| 67 | CIP030 | ADMITTING-DIAGNOSIS-CODE | The diagnosis provided by the physician at the time of admission which describes the patient's condition upon admission to the hospital. Since the Admitting Diagnosis is formulated before all tests and examinations are complete, it may be stated in the form of a problem or symptom and it may differ from any of the final diagnoses recorded in the medical record. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP030-0003 | |||
| 68 | CIP030 | ADMITTING-DIAGNOSIS-CODE | Enter invalid codes exactly as they appear in the State system. Do not 8- or 9-fill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP030-0004 | |||
| 69 | CIP030 | ADMITTING-DIAGNOSIS-CODE | CMS is not expecting ADMITTING-DIAGNOSIS-CODE-FLAG "2" (ICD-10) to be used until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP030-0005 | |||
| 70 | CIP031 | ADMITTING-DIAGNOSIS-CODE-FLAG | A flag that identifies the coding system used for the ADMITTING-DIAGNOSIS-CODE. | Required | Value must be equal to a valid value. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP031-0001 |
| 71 | CIP031 | ADMITTING-DIAGNOSIS-CODE-FLAG | The state must use a code that belongs to the code set that they report they are using. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP031-0002 | |||
| 72 | CIP031 | ADMITTING-DIAGNOSIS-CODE-FLAG | CMS is not expecting ADMITTING-DIAGNOSIS-CODE-FLAG "2" (ICD-10) to be used until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP031-0003 | |||
| 73 | CIP032 | DIAGNOSIS-CODE-1 | DIAGNOSIS-CODE-1 through DIAGNOSIS-CODE-2: Primary and Second ICD-9/10-CM code found on the claim. | Required | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". |
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP032-0001 |
| 74 | CIP032 | DIAGNOSIS-CODE-1 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP032-0002 | |||
| 75 | CIP032 | DIAGNOSIS-CODE-1 | Provide diagnosis coding as submitted on bill. |
2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP032-0003 | |||
| 76 | CIP032 | DIAGNOSIS-CODE-1 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP032-0004 | |||
| 77 | CIP032 | DIAGNOSIS-CODE-1 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP032-0005 | |||
| 78 | CIP032 | DIAGNOSIS-CODE-1 | The primary diagnosis code goes into DIAGNOSIS-CODE1 | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP032-0006 | |||
| 79 | CIP032 | DIAGNOSIS-CODE-1 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP032-0007 | |||
| 80 | CIP032 | DIAGNOSIS-CODE-1 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP032-0008 | |||
| 81 | CIP033 | DIAGNOSIS-CODE-FLAG-1 | DIAGNOSIS-CODE-FLAG-1 through DIAGNOSIS-CODE-FLAG-2: Code flag for the Primary and Second ICD-9/10-CM code found on the claim. | Required | Value must be equal to a valid value. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP033-0001 |
| 82 | CIP033 | DIAGNOSIS-CODE-FLAG-1 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP033-0002 | |||
| 83 | CIP033 | DIAGNOSIS-CODE-FLAG-1 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP033-0003 | |||
| 84 | CIP033 | DIAGNOSIS-CODE-FLAG-1 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP033-0004 | |||
| 85 | CIP034 | DIAGNOSIS-POA-FLAG-1 | A code to identify conditions that are present at the time the order for inpatient admission occurs; conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP034-0001 |
| 86 | CIP034 | DIAGNOSIS-POA-FLAG-1 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP034-0002 | |||
| 87 | CIP035 | DIAGNOSIS-CODE-2 | DIAGNOSIS-CODE-1 through DIAGNOSIS-CODE-2: Primary and Second ICD-9/10-CM code found on the claim. | Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". |
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP035-0001 |
| 88 | CIP035 | DIAGNOSIS-CODE-2 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP035-0002 | |||
| 89 | CIP035 | DIAGNOSIS-CODE-2 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP035-0003 | |||
| 90 | CIP035 | DIAGNOSIS-CODE-2 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP035-0004 | |||
| 91 | CIP035 | DIAGNOSIS-CODE-2 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP035-0005 | |||
| 92 | CIP035 | DIAGNOSIS-CODE-2 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP035-0006 | |||
| 93 | CIP035 | DIAGNOSIS-CODE-2 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 12. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP035-0007 | |||
| 94 | CIP035 | DIAGNOSIS-CODE-2 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP035-0008 | |||
| 95 | CIP036 | DIAGNOSIS-CODE-FLAG-2 | DIAGNOSIS-CODE-FLAG-1 through DIAGNOSIS-CODE-FLAG-2: Code flag for the Primary and Second ICD-9/10-CM code found on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP036-0001 |
| 96 | CIP036 | DIAGNOSIS-CODE-FLAG-2 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP036-0002 | |||
| 97 | CIP036 | DIAGNOSIS-CODE-FLAG-2 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP036-0003 | |||
| 98 | CIP036 | DIAGNOSIS-CODE-FLAG-2 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP036-0004 | |||
| 99 | CIP037 | DIAGNOSIS-POA-FLAG-2 | A code to identify conditions that are present at the time the order for inpatient admission occurs; conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP037-0001 |
| 100 | CIP037 | DIAGNOSIS-POA-FLAG-2 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP037-0002 | |||
| 101 | CIP038 | DIAGNOSIS-CODE-3 | DIAGNOSIS-CODE-3 through DIAGNOSIS-CODE-5: The third through fifth ICD-9/10-CM codes that appear on the claim. | Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". |
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP038-0001 |
| 102 | CIP038 | DIAGNOSIS-CODE-3 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP038-0002 | |||
| 103 | CIP038 | DIAGNOSIS-CODE-3 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP038-0003 | |||
| 104 | CIP038 | DIAGNOSIS-CODE-3 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP038-0004 | |||
| 105 | CIP038 | DIAGNOSIS-CODE-3 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP038-0005 | |||
| 106 | CIP038 | DIAGNOSIS-CODE-3 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP038-0006 | |||
| 107 | CIP038 | DIAGNOSIS-CODE-3 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 12. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP038-0007 | |||
| 108 | CIP039 | DIAGNOSIS-CODE-4 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00003 | CIP038-0008 | |||
| 109 | CIP039 | DIAGNOSIS-CODE-FLAG-3 | DIAGNOSIS-CODE-FLAG-3 through DIAGNOSIS-CODE-FLAG-5: Code flag for the third through fifth ICD-9/10-CM codes that appear on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP039-0001 |
| 110 | CIP039 | DIAGNOSIS-CODE-FLAG-3 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP039-0002 | |||
| 111 | CIP039 | DIAGNOSIS-CODE-FLAG-3 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP039-0003 | |||
| 112 | CIP039 | DIAGNOSIS-CODE-FLAG-3 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP039-0004 | |||
| 113 | CIP040 | DIAGNOSIS-POA-FLAG-3 | A code to identify conditions that are present at the time the order for inpatient admission occurs; conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP040-0001 |
| 114 | CIP040 | DIAGNOSIS-POA-FLAG-3 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP040-0002 | |||
| 115 | CIP041 | DIAGNOSIS-CODE-4 | DIAGNOSIS-CODE-3 through DIAGNOSIS-CODE-5: The third through fifth ICD-9/10-CM codes that appear on the claim. | Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". |
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP041-0001 |
| 116 | CIP041 | DIAGNOSIS-CODE-4 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP041-0002 | |||
| 117 | CIP041 | DIAGNOSIS-CODE-4 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP041-0003 | |||
| 118 | CIP041 | DIAGNOSIS-CODE-4 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP041-0004 | |||
| 119 | CIP041 | DIAGNOSIS-CODE-4 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP041-0005 | |||
| 120 | CIP041 | DIAGNOSIS-CODE-4 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP041-0006 | |||
| 121 | CIP041 | DIAGNOSIS-CODE-4 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 12. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP041-0007 | |||
| 122 | CIP041 | DIAGNOSIS-CODE-4 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP041-0008 | |||
| 123 | CIP042 | DIAGNOSIS-CODE-FLAG-4 | DIAGNOSIS-CODE-FLAG-3 through DIAGNOSIS-CODE-FLAG-5: Code flag for the third through fifth ICD-9/10-CM codes that appear on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP042-0001 |
| 124 | CIP042 | DIAGNOSIS-CODE-FLAG-4 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP042-0002 | |||
| 125 | CIP042 | DIAGNOSIS-CODE-FLAG-4 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP042-0003 | |||
| 126 | CIP042 | DIAGNOSIS-CODE-FLAG-4 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP042-0004 | |||
| 127 | CIP043 | DIAGNOSIS-POA-FLAG-4 | A code to identify conditions that are present at the time the order for inpatient admission occurs; conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP043-0001 |
| 128 | CIP043 | DIAGNOSIS-POA-FLAG-4 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP043-0002 | |||
| 129 | CIP044 | DIAGNOSIS-CODE-5 | DIAGNOSIS-CODE-3 through DIAGNOSIS-CODE-5: The third through fifth ICD-9/10-CM codes that appear on the claim. | Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". |
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP044-0001 |
| 130 | CIP044 | DIAGNOSIS-CODE-5 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP044-0002 | |||
| 131 | CIP044 | DIAGNOSIS-CODE-5 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP044-0003 | |||
| 132 | CIP044 | DIAGNOSIS-CODE-5 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP044-0004 | |||
| 133 | CIP044 | DIAGNOSIS-CODE-5 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP044-0005 | |||
| 134 | CIP044 | DIAGNOSIS-CODE-5 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP044-0006 | |||
| 135 | CIP044 | DIAGNOSIS-CODE-5 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 12. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP044-0007 | |||
| 136 | CIP044 | DIAGNOSIS-CODE-5 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP044-0008 | |||
| 137 | CIP045 | DIAGNOSIS-CODE-FLAG-5 | DIAGNOSIS-CODE-FLAG-3 through DIAGNOSIS-CODE-FLAG-5: Code flag for the third through fifth ICD-9/10-CM codes that appear on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP045-0001 |
| 138 | CIP045 | DIAGNOSIS-CODE-FLAG-5 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP045-0002 | |||
| 139 | CIP045 | DIAGNOSIS-CODE-FLAG-5 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP045-0003 | |||
| 140 | CIP045 | DIAGNOSIS-CODE-FLAG-5 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP045-0004 | |||
| 141 | CIP046 | DIAGNOSIS-POA-FLAG-5 | A code to identify conditions that are present at the time the order for inpatient admission occurs; conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP046-0001 |
| 142 | CIP046 | DIAGNOSIS-POA-FLAG-5 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP046-0002 | |||
| 143 | CIP047 | DIAGNOSIS-CODE-6 | DIAGNOSIS-CODE-6 through DIAGNOSIS-CODE-12: The sixth through twelfth ICD-9/10-CM codes that appear on the claim. |
Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP047-0001 |
| 144 | CIP047 | DIAGNOSIS-CODE-6 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP047-0002 | |||
| 145 | CIP047 | DIAGNOSIS-CODE-6 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP047-0003 | |||
| 146 | CIP047 | DIAGNOSIS-CODE-6 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP047-0004 | |||
| 147 | CIP047 | DIAGNOSIS-CODE-6 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP047-0005 | |||
| 148 | CIP047 | DIAGNOSIS-CODE-6 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP047-0006 | |||
| 149 | CIP047 | DIAGNOSIS-CODE-6 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 12. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP047-0007 | |||
| 150 | CIP047 | DIAGNOSIS-CODE-6 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP047-0008 | |||
| 151 | CIP048 | DIAGNOSIS-CODE-FLAG-6 | DIAGNOSIS-CODE-FLAG-6 through DIAGNOSIS-CODE-FLAG-12: Code flag for the sixth through twelfth ICD-9/10-CM codes that appear on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP048-0001 |
| 152 | CIP048 | DIAGNOSIS-CODE-FLAG-6 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP048-0002 | |||
| 153 | CIP048 | DIAGNOSIS-CODE-FLAG-6 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP048-0003 | |||
| 154 | CIP048 | DIAGNOSIS-CODE-FLAG-6 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP048-0004 | |||
| 155 | CIP049 | DIAGNOSIS-POA-FLAG-6 | A flag that indicates “Present on Admission” for DIAGNOSIS CODE 1 - 12. A code to identify conditions that are present at the time the order for inpatient admission occurs; conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP049-0001 |
| 156 | CIP049 | DIAGNOSIS-POA-FLAG-6 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP049-0002 | |||
| 157 | CIP050 | DIAGNOSIS-CODE-7 | DIAGNOSIS-CODE-6 through DIAGNOSIS-CODE-12: The sixth through twelfth ICD-9/10-CM codes that appear on the claim. |
Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP050-0001 |
| 158 | CIP050 | DIAGNOSIS-CODE-7 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP050-0002 | |||
| 159 | CIP050 | DIAGNOSIS-CODE-7 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP050-0003 | |||
| 160 | CIP050 | DIAGNOSIS-CODE-7 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP050-0004 | |||
| 161 | CIP050 | DIAGNOSIS-CODE-7 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP050-0005 | |||
| 162 | CIP050 | DIAGNOSIS-CODE-7 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP050-0006 | |||
| 163 | CIP050 | DIAGNOSIS-CODE-7 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 12. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP050-0007 | |||
| 164 | CIP050 | DIAGNOSIS-CODE-7 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP050-0008 | |||
| 165 | CIP051 | DIAGNOSIS-CODE-FLAG-7 | DIAGNOSIS-CODE-FLAG-6 through DIAGNOSIS-CODE-FLAG-12: Code flag for the sixth through twelfth ICD-9/10-CM codes that appear on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP051-0001 |
| 166 | CIP051 | DIAGNOSIS-CODE-FLAG-7 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP051-0002 | |||
| 167 | CIP051 | DIAGNOSIS-CODE-FLAG-7 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP051-0003 | |||
| 168 | CIP051 | DIAGNOSIS-CODE-FLAG-7 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP051-0004 | |||
| 169 | CIP052 | DIAGNOSIS-POA-FLAG-7 | A flag that indicates “Present on Admission” for DIAGNOSIS CODE 1 - 12. A code to identify conditions that are present at the time the order for inpatient admission occurs; conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP052-0001 |
| 170 | CIP052 | DIAGNOSIS-POA-FLAG-7 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP052-0002 | |||
| 171 | CIP053 | DIAGNOSIS-CODE-8 | DIAGNOSIS-CODE-6 through DIAGNOSIS-CODE-12: The sixth through twelfth ICD-9/10-CM codes that appear on the claim. |
Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP053-0001 |
| 172 | CIP053 | DIAGNOSIS-CODE-8 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP053-0002 | |||
| 173 | CIP053 | DIAGNOSIS-CODE-8 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP053-0003 | |||
| 174 | CIP053 | DIAGNOSIS-CODE-8 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP053-0004 | |||
| 175 | CIP053 | DIAGNOSIS-CODE-8 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP053-0005 | |||
| 176 | CIP053 | DIAGNOSIS-CODE-8 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP053-0006 | |||
| 177 | CIP053 | DIAGNOSIS-CODE-8 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 12. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP053-0007 | |||
| 178 | CIP053 | DIAGNOSIS-CODE-8 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP053-0008 | |||
| 179 | CIP054 | DIAGNOSIS-CODE-FLAG-8 | DIAGNOSIS-CODE-FLAG-6 through DIAGNOSIS-CODE-FLAG-12: Code flag for the sixth through twelfth ICD-9/10-CM codes that appear on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP054-0001 |
| 180 | CIP054 | DIAGNOSIS-CODE-FLAG-8 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP054-0002 | |||
| 181 | CIP054 | DIAGNOSIS-CODE-FLAG-8 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP054-0003 | |||
| 182 | CIP054 | DIAGNOSIS-CODE-FLAG-8 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP054-0004 | |||
| 183 | CIP055 | DIAGNOSIS-POA-FLAG-8 | A flag that indicates “Present on Admission” for DIAGNOSIS CODE 1 - 12. A code to identify conditions that are present at the time the order for inpatient admission occurs; conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP055-0001 |
| 184 | CIP055 | DIAGNOSIS-POA-FLAG-8 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP055-0002 | |||
| 185 | CIP056 | DIAGNOSIS-CODE-9 | DIAGNOSIS-CODE-6 through DIAGNOSIS-CODE-12: The sixth through twelfth ICD-9/10-CM codes that appear on the claim. |
Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP056-0001 |
| 186 | CIP056 | DIAGNOSIS-CODE-9 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP056-0002 | |||
| 187 | CIP056 | DIAGNOSIS-CODE-9 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP056-0003 | |||
| 188 | CIP056 | DIAGNOSIS-CODE-9 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP056-0004 | |||
| 189 | CIP056 | DIAGNOSIS-CODE-9 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP056-0005 | |||
| 190 | CIP056 | DIAGNOSIS-CODE-9 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP056-0006 | |||
| 191 | CIP056 | DIAGNOSIS-CODE-9 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 12. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP056-0007 | |||
| 192 | CIP056 | DIAGNOSIS-CODE-9 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP056-0008 | |||
| 193 | CIP057 | DIAGNOSIS-CODE-FLAG-9 | DIAGNOSIS-CODE-FLAG-6 through DIAGNOSIS-CODE-FLAG-12: Code flag for the sixth through twelfth ICD-9/10-CM codes that appear on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP057-0001 |
| 194 | CIP057 | DIAGNOSIS-CODE-FLAG-9 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP057-0002 | |||
| 195 | CIP057 | DIAGNOSIS-CODE-FLAG-9 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP057-0003 | |||
| 196 | CIP057 | DIAGNOSIS-CODE-FLAG-9 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP057-0004 | |||
| 197 | CIP058 | DIAGNOSIS-POA-FLAG-9 | A flag that indicates “Present on Admission” for DIAGNOSIS CODE 1 - 12. A code to identify conditions that are present at the time the order for inpatient admission occurs; conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. All UNUSED diagnosis and occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP058-0001 |
| 198 | CIP058 | DIAGNOSIS-POA-FLAG-9 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP058-0002 | |||
| 199 | CIP059 | DIAGNOSIS-CODE-10 | DIAGNOSIS-CODE-6 through DIAGNOSIS-CODE-12: The sixth through twelfth ICD-9/10-CM codes that appear on the claim. |
Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP059-0001 |
| 200 | CIP059 | DIAGNOSIS-CODE-10 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP059-0002 | |||
| 201 | CIP059 | DIAGNOSIS-CODE-10 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP059-0003 | |||
| 202 | CIP059 | DIAGNOSIS-CODE-10 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP059-0004 | |||
| 203 | CIP059 | DIAGNOSIS-CODE-10 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP059-0005 | |||
| 204 | CIP059 | DIAGNOSIS-CODE-10 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP059-0006 | |||
| 205 | CIP059 | DIAGNOSIS-CODE-10 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 12. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP059-0007 | |||
| 206 | CIP059 | DIAGNOSIS-CODE-10 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP059-0008 | |||
| 207 | CIP060 | DIAGNOSIS-CODE-FLAG-10 | DIAGNOSIS-CODE-FLAG-6 through DIAGNOSIS-CODE-FLAG-12: Code flag for the sixth through twelfth ICD-9/10-CM codes that appear on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP060-0001 |
| 208 | CIP060 | DIAGNOSIS-CODE-FLAG-10 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP060-0002 | |||
| 209 | CIP060 | DIAGNOSIS-CODE-FLAG-10 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP060-0003 | |||
| 210 | CIP060 | DIAGNOSIS-CODE-FLAG-10 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP060-0004 | |||
| 211 | CIP061 | DIAGNOSIS-POA-FLAG-10 | A flag that indicates “Present on Admission” for DIAGNOSIS CODE 1 - 12. A code to identify conditions that are present at the time the order for inpatient admission occurs; conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP061-0001 |
| 212 | CIP061 | DIAGNOSIS-POA-FLAG-10 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP061-0002 | |||
| 213 | CIP062 | DIAGNOSIS-CODE-11 | DIAGNOSIS-CODE-6 through DIAGNOSIS-CODE-12: The sixth through twelfth ICD-9/10-CM codes that appear on the claim. |
Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP062-0001 |
| 214 | CIP062 | DIAGNOSIS-CODE-11 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP062-0002 | |||
| 215 | CIP062 | DIAGNOSIS-CODE-11 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP062-0003 | |||
| 216 | CIP062 | DIAGNOSIS-CODE-11 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP062-0004 | |||
| 217 | CIP062 | DIAGNOSIS-CODE-11 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP062-0005 | |||
| 218 | CIP062 | DIAGNOSIS-CODE-11 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP062-0006 | |||
| 219 | CIP062 | DIAGNOSIS-CODE-11 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 12. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP062-0007 | |||
| 220 | CIP062 | DIAGNOSIS-CODE-11 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP062-0008 | |||
| 221 | CIP063 | DIAGNOSIS-CODE-FLAG-11 | DIAGNOSIS-CODE-FLAG-6 through DIAGNOSIS-CODE-FLAG-12: Code flag for the sixth through twelfth ICD-9/10-CM codes that appear on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP063-0001 |
| 222 | CIP063 | DIAGNOSIS-CODE-FLAG-11 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP063-0002 | |||
| 223 | CIP063 | DIAGNOSIS-CODE-FLAG-11 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP063-0003 | |||
| 224 | CIP063 | DIAGNOSIS-CODE-FLAG-11 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP063-0004 | |||
| 225 | CIP064 | DIAGNOSIS-POA-FLAG-11 | A flag that indicates “Present on Admission” for DIAGNOSIS CODE 1 - 12. A code to identify conditions that are present at the time the order for inpatient admission occurs; conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP064-0001 |
| 226 | CIP064 | DIAGNOSIS-POA-FLAG-11 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP064-0002 | |||
| 227 | CIP065 | DIAGNOSIS-CODE-12 | DIAGNOSIS-CODE-6 through DIAGNOSIS-CODE-12: The sixth through twelfth ICD-9/10-CM codes that appear on the claim. |
Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP065-0001 |
| 228 | CIP065 | DIAGNOSIS-CODE-12 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP065-0002 | |||
| 229 | CIP065 | DIAGNOSIS-CODE-12 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP065-0003 | |||
| 230 | CIP065 | DIAGNOSIS-CODE-12 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP065-0004 | |||
| 231 | CIP065 | DIAGNOSIS-CODE-12 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP065-0005 | |||
| 232 | CIP065 | DIAGNOSIS-CODE-12 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP065-0006 | |||
| 233 | CIP065 | DIAGNOSIS-CODE-12 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 12. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP065-0007 | |||
| 234 | CIP065 | DIAGNOSIS-CODE-12 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP065-0008 | |||
| 235 | CIP066 | DIAGNOSIS-CODE-FLAG-12 | DIAGNOSIS-CODE-FLAG-6 through DIAGNOSIS-CODE-FLAG-12: Code flag for the sixth through twelfth ICD-9/10-CM codes that appear on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP066-0001 |
| 236 | CIP066 | DIAGNOSIS-CODE-FLAG-12 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP066-0002 | |||
| 237 | CIP066 | DIAGNOSIS-CODE-FLAG-12 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP066-0003 | |||
| 238 | CIP066 | DIAGNOSIS-CODE-FLAG-12 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP066-0004 | |||
| 239 | CIP067 | DIAGNOSIS-POA-FLAG-12 | A flag that indicates “Present on Admission” for DIAGNOSIS CODE 1 - 12. A code to identify conditions that are present at the time the order for inpatient admission occurs; conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP067-0001 |
| 240 | CIP067 | DIAGNOSIS-POA-FLAG-12 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP067-0002 | |||
| 241 | CIP068 | DIAGNOSIS-RELATED-GROUP | Code representing the Diagnosis Related Group (DRG) that is applicable for the inpatient services being rendered. | Conditional | Enter DRG used by the state | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP068-0001 | |
| 242 | CIP068 | DIAGNOSIS-RELATED-GROUP | If DRGs are not used, 8-fill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP068-0002 | |||
| 243 | CIP068 | DIAGNOSIS-RELATED-GROUP | Only a state that pays the claim by DRG should report this information | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP068-0003 | |||
| 244 | CIP069 | DIAGNOSIS-RELATED-GROUP-IND | An indicator identifying the grouping algorithm used to assign Diagnosis Related Group (DRG) values. | Conditional | Values are generated by combining two types of information: Position 1-2, State/Group generating DRG: If state specific system, fill with two digit US postal code representation for state. If CMS Grouper, fill with “HG”. If any other system, fill with “XX”. Position 3-4, fill with the number that represents the DRG version used (01-98). For example, “HG15" would represent CMS Grouper version 15. If version is unknown, fill with “99". |
2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP069-0001 | |
| 245 | CIP069 | DIAGNOSIS-RELATED-GROUP-IND | If Value is unknown, fill the field with “9999". | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP069-0002 | |||
| 246 | CIP069 | DIAGNOSIS-RELATED-GROUP-IND | This field is required if DIAGNOSIS-RELATED-GROUP is populated. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP069-0003 | |||
| 247 | CIP069 | DIAGNOSIS-RELATED-GROUP-IND | This field is required if DIAGNOSIS-RELATED-GROUP is populated. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP069-0004 | |||
| 248 | CIP069 | DIAGNOSIS-RELATED-GROUP-IND | This field is required if DIAGNOSIS-RELATED-GROUP is populated. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP069-0005 | |||
| 249 | CIP069 | DIAGNOSIS-RELATED-GROUP-IND | This field is required if DIAGNOSIS-RELATED-GROUP is populated. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP069-0006 | |||
| 250 | CIP069 | DIAGNOSIS-RELATED-GROUP-IND | If a non-DRG paying state, set field to "8888" | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP069-0007 | |||
| 251 | CIP070 | PROCEDURE-CODE-1 | A procedure code based on ICD-9 and ICD-10 used by the state to identify the procedures performed during the hospital stay referenced by this claim. The principal procedure and related info should be recorded in PROCEDURE-CODE-1, PROCEDURE-CODE-MOD-1, PROCEDURE-CODE-DATE-1, and PROCEDURE-CODE-FLAG-1. The principal procedure is performed for definitive treatment rather than for diagnostic or exploratory purposes. It is closely related to either the principal diagnosis or to complications that arise during other treatments. Use PROCEDURE-CODE-2 through PROCEDURE-CODE-6 (and related data elements) to record secondary, tertiary, etc. procedures. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html http://www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/index.html?redirect=/medhcpcsgeninfo/ http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Relative-Value-Files.html http://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx Additional CPT codes are available for a fee through professional organizations. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP070-0001 |
| 252 | CIP070 | PROCEDURE-CODE-1 | If PROCDURE-CODE-FLAG-1 = {10 through 87, state-specific coding systems} valid codes must be supplied by the State. For national coding systems, code should conform to the nationally recognized formats: | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP070-0002 | |||
| 253 | CIP070 | PROCEDURE-CODE-1 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP070-0003 | |||
| 254 | CIP071 | PROCEDURE-CODE-MOD-1 | The procedure code modifier used with the (Principal) Procedure Code 1. For example, some states use modifiers to indicate assistance in surgery or anesthesia services. | NA | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP071-0001 |
| 255 | CIP071 | PROCEDURE-CODE-MOD-1 | If no Principal Procedure (procedure-code-1) was performed, 8-fill | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP071-0002 | |||
| 256 | CIP071 | PROCEDURE-CODE-MOD-1 | Value must be 8-filled if corresponding procedure code is 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP071-0003 | |||
| 257 | CIP071 | PROCEDURE-CODE-MOD-1 | Always leave blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). Modifiers do not exist for ICD-9/10 procedure codes for claims/encounters and will never be applicable. | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP071-0004 | |||
| 258 | CIP072 | PROCEDURE-CODE-FLAG-1 | A flag that identifies the coding system used for PROCDURE-CODE-1. | Conditional | Value must be equal to a valid value. | 01 CPT 4 02 ICD-9 CM 06 HCPCS (Both National and Regional HCPCS) 07 ICD-10-PCS (Will be implemented on 10/1/2014) 10-87 Other Systems 88 Not Applicable 99 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP072-0001 |
| 259 | CIP072 | PROCEDURE-CODE-FLAG-1 | If no Principal Procedure (procedure-code-1) was performed, 8-fill | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP072-0002 | |||
| 260 | CIP072 | PROCEDURE-CODE-FLAG-1 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP072-0003 | ||||
| 261 | CIP073 | PROCEDURE-CODE-DATE-1 | The date upon which the PROCEDURE-CODE-1 was performed. | Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP073-0001 | |
| 262 | CIP073 | PROCEDURE-CODE-DATE-1 | Value must be a valid date | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP073-0002 | |||
| 263 | CIP073 | PROCEDURE-CODE-DATE-1 | If the corresponding procedure code is 8-filled, then this procedure code date must be 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP073-0003 | |||
| 264 | CIP073 | PROCEDURE-CODE-DATE-1 | Date must occur before the ENDING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP073-0004 | |||
| 265 | CIP073 | PROCEDURE-CODE-DATE-1 | Date must occur on or after the BEGINNING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP073-0005 | |||
| 266 | CIP073 | PROCEDURE-CODE-DATE-1 | This date must occur on or before the DATE-OF-DEATH in the Eligible file. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP073-0006 | |||
| 267 | CIP073 | PROCEDURE-CODE-DATE-1 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP073-0007 | |||
| 268 | CIP074 | PROCEDURE-CODE-2 | A procedure code based on ICD-9 and ICD-10 used by the state to identify the procedures performed during the hospital stay referenced by this claim. The principal procedure and related info should be recorded in PROCEDURE-CODE-1, PROCEDURE-CODE-MOD-1, PROCEDURE-CODE-DATE-1, and PROCEDURE-CODE-FLAG-1. The principal procedure is performed for definitive treatment rather than for diagnostic or exploratory purposes. It is closely related to either the principal diagnosis or to complications that arise during other treatments. Use PROCEDURE-CODE-2 through PROCEDURE-CODE-6 (and related data elements) to record secondary, tertiary, etc. procedures. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html http://www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/index.html?redirect=/medhcpcsgeninfo/ http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Relative-Value-Files.html http://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx Additional CPT codes are available for a fee through professional organizations. |
10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP074-0001 |
| 269 | CIP074 | PROCEDURE-CODE-2 | Enter as many procedures as are reported after the principal procedure up to five additional codes. Remaining fields should be 8-filled (e.g., if claim contains two additional procedures, they would be reported in PROCDURE-CODE-2 and PROCDURE-CODE-3. Remaining fields PROCDURE-CODE-4 through PROCDURE-CODE-6 would all be 8-filled.) | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP074-0002 | |||
| 270 | CIP074 | PROCEDURE-CODE-2 | If PROCDURE-CODE-FLAG-2 = {10 through 87, state-specific coding systems} valid codes must be supplied by the State. For national coding systems, code should conform to the nationally recognized formats: | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP074-0003 | |||
| 271 | CIP074 | PROCEDURE-CODE-2 | o ICD-9/10-CM (corresponding PROCDURE-CODE-FLAG = 02/07): Positions 1-2 must be numeric, positions 3-4 must be numeric or blank, positions 5-8 must be blank. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP074-0004 | |||
| 272 | CIP074 | PROCEDURE-CODE-2 | Value can include both National and Local (Regional) codes. For National codes (position 1=“A”-“V”) positions 2-5 must be numeric; for Local (Regional) codes, positions 2-5 must be alphanumeric (e.g., “X1234" or “WW234"). | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP074-0005 | |||
| 273 | CIP074 | PROCEDURE-CODE-2 | If no PROCEDURE-CODE-2 was performed, 8-fill | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP074-0006 | |||
| 274 | CIP074 | PROCEDURE-CODE-2 | Note: An eighth character is provided for future expansion of this field. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP074-0007 | |||
| 275 | CIP074 | PROCEDURE-CODE-2 | If the corresponding procedure code flag is 8-filled, then this procedure code should be 8- filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP074-0008 | |||
| 276 | CIP074 | PROCEDURE-CODE-2 | If the corresponding procedure code flag is not 8-filled, then this procedure code must not be 8- filled | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP074-0009 | |||
| 277 | CIP074 | PROCEDURE-CODE-2 | Value must be different from the preceding procedure code values. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP074-0010 | |||
| 278 | CIP074 | PROCEDURE-CODE-2 | Do not use multiple instances of PROCEDURE-CODE if the preceding PROCEDURE-CODE element is not populated. (i.e. if PROCEDURE-CODE-2 is populated, but PROCEDURE-CODE-3 is blank-filled, then PROCEDURE-CODE-4 must also not be valued. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP074-0011 | |||
| 279 | CIP074 | PROCEDURE-CODE-2 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP074-0012 | |||
| 280 | CIP075 | PROCEDURE-CODE-MOD-2 | A series of procedure code modifiers used with the corresponding Procedure Codes. For example, some states use modifiers to indicate assistance in surgery or anesthesia services. |
NA | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP075-0001 |
| 281 | CIP075 | PROCEDURE-CODE-MOD-2 | If no corresponding procedure (PROCDURE-CODE-2 through PROCDURE-CODE-6) was performed, 8-fill | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP075-0002 | |||
| 282 | CIP075 | PROCEDURE-CODE-MOD-2 | Value must be 8-filled if corresponding procedure code is 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP075-0003 | |||
| 283 | CIP075 | PROCEDURE-CODE-MOD-2 | Do not use multiple instances of PROCEDURE-CODE-MOD if the preceding PROCEDURE-CODE-MOD element is not populated. (i.e. if PROCEDURE-CODE-MOD-2 is populated, but PROCEDURE-CODE-MOD-3 is blank-filled, then PROCEDURE-CODE-MOD-4 must also not be valued. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP075-0004 | |||
| 284 | CIP075 | PROCEDURE-CODE-MOD-2 | Always leave blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). Modifiers do not exist for ICD-9/10 procedure codes for claims/encounters and will never be applicable. | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP075-0005 | |||
| 285 | CIP076 | PROCEDURE-CODE-FLAG-2 | A series of flags that identifies the coding system used for the associated procedure codes (PROCDURE-CODE-2 through PROCDURE-CODE-6) | Conditional | Value must be equal to a valid value. | 01 CPT 4 02 ICD-9 CM 06 HCPCS (Both National and Regional HCPCS) 07 ICD-10-CM PCS (Will be implemented on 10/1/2014) 10-87 Other Systems 88 Not Applicable 99 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP076-0001 |
| 286 | CIP076 | PROCEDURE-CODE-FLAG-2 | If no second procedure was performed, 8-fill. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP076-0002 | |||
| 287 | CIP076 | PROCEDURE-CODE-FLAG-2 | Do not use multiple instances of PROCEDURE-CODE-FLAG if the preceding PROCEDURE-CODE-FLAG element is not populated. (i.e. if PROCEDURE-CODE-FLAG-2 is populated, but PROCEDURE-CODE-FLAG-3 is blank-filled, then PROCEDURE-CODE-FLAG-4 must also not be valued. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP076-0003 | |||
| 288 | CIP076 | PROCEDURE-CODE-FLAG-2 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP076-0004 | |||
| 289 | CIP077 | PROCEDURE-CODE-DATE-2 | The date on which the procedure 2 – 6 was performed. | Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP077-0001 | |
| 290 | CIP077 | PROCEDURE-CODE-DATE-2 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP077-0002 | |||
| 291 | CIP077 | PROCEDURE-CODE-DATE-2 | If the corresponding procedure code is 8-filled, then this procedure code date must be 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP077-0003 | |||
| 292 | CIP077 | PROCEDURE-CODE-DATE-2 | Date must occur before the ENDING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP077-0004 | |||
| 293 | CIP077 | PROCEDURE-CODE-DATE-2 | Date must occur on or after the BEGINNING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP077-0005 | |||
| 294 | CIP077 | PROCEDURE-CODE-DATE-2 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP077-0006 | |||
| 295 | CIP078 | PROCEDURE-CODE-3 | A procedure code based on ICD-9 and ICD-10 used by the state to identify the procedures performed during the hospital stay referenced by this claim. The principal procedure and related info should be recorded in PROCEDURE-CODE-1, PROCEDURE-CODE-MOD-1, PROCEDURE-CODE-DATE-1, and PROCEDURE-CODE-FLAG-1. The principal procedure is performed for definitive treatment rather than for diagnostic or exploratory purposes. It is closely related to either the principal diagnosis or to complications that arise during other treatments. Use PROCEDURE-CODE-2 through PROCEDURE-CODE-6 (and related data elements) to record secondary, tertiary, etc. procedures. |
Conditional | Enter as many procedures as are reported after the principal procedure up to five additional codes. Remaining fields should be 8-filled (e.g., if claim contains two additional procedures, they would be reported in PROCDURE-CODE-2 and PROCDURE-CODE-3. Remaining fields PROCDURE-CODE-4 through PROCDURE-CODE-6 would all be 8-filled.) | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html http://www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/index.html?redirect=/medhcpcsgeninfo/ http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Relative-Value-Files.html http://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx Additional CPT codes are available for a fee through professional organizations. |
10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP078-0001 |
| 296 | CIP078 | PROCEDURE-CODE-3 | Value must be equal to a valid value. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP078-0002 | |||
| 297 | CIP078 | PROCEDURE-CODE-3 | If PROCDURE-CODE-FLAG-3 = {10 through 87, state-specific coding systems} valid codes must be supplied by the State. For national coding systems, code should conform to the nationally recognized formats: | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP078-0003 | |||
| 298 | CIP078 | PROCEDURE-CODE-3 | o ICD-9/10-CM (corresponding PROCDURE-CODE-FLAG = 02/07): Positions 1-2 must be numeric, positions 3-4 must be numeric or blank, positions 5-8 must be blank. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP078-0004 | |||
| 299 | CIP078 | PROCEDURE-CODE-3 | Value can include both National and Local (Regional) codes. For National codes (position 1=“A”-“V”) positions 2-5 must be numeric; for Local (Regional) codes, positions 2-5 must be alphanumeric (e.g., “X1234" or “WW234"). | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP078-0005 | |||
| 300 | CIP078 | PROCEDURE-CODE-3 | If no PROCEDURE-CODE-3 was performed, 8-fill | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP078-0006 | |||
| 301 | CIP078 | PROCEDURE-CODE-3 | Note: An eighth character is provided for future expansion of this field. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP078-0007 | |||
| 302 | CIP078 | PROCEDURE-CODE-3 | If the corresponding procedure code flag is 8-filled, then this procedure code should be 8- filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP078-0008 | |||
| 303 | CIP078 | PROCEDURE-CODE-3 | If the corresponding procedure code flag is not 8-filled, then this procedure code must not be 8- filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP078-0009 | |||
| 304 | CIP078 | PROCEDURE-CODE-3 | Value must be different from the preceding procedure code values. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP078-0010 | |||
| 305 | CIP078 | PROCEDURE-CODE-3 | Do not use multiple instances of PROCEDURE-CODE if the preceding PROCEDURE-CODE element is not populated. (i.e. if PROCEDURE-CODE-2 is populated, but PROCEDURE-CODE-3 is blank-filled, then PROCEDURE-CODE-4 must also not be valued. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP078-0011 | |||
| 306 | CIP078 | PROCEDURE-CODE-3 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP078-0012 | |||
| 307 | CIP079 | PROCEDURE-CODE-MOD-3 | A series of procedure code modifiers used with the corresponding Procedure Codes. For example, some states use modifiers to indicate assistance in surgery or anesthesia services. |
NA | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP079-0001 |
| 308 | CIP079 | PROCEDURE-CODE-MOD-3 | Value must be 8-filled if corresponding procedure code is 8-filled | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP079-0002 | |||
| 309 | CIP079 | PROCEDURE-CODE-MOD-3 | Do not use multiple instances of PROCEDURE-CODE-MOD if the preceding PROCEDURE-CODE-MOD element is not populated. (i.e. if PROCEDURE-CODE-MOD-2 is populated, but PROCEDURE-CODE-MOD-3 is blank-filled, then PROCEDURE-CODE-MOD-4 must also not be valued. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP079-0003 | |||
| 310 | CIP079 | PROCEDURE-CODE-MOD-3 | If no corresponding procedure (PROCDURE-CODE-2 through PROCDURE-CODE-6) was performed, 8-fill | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP079-0004 | |||
| 311 | CIP079 | PROCEDURE-CODE-MOD-3 | Always leave blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). Modifiers do not exist for ICD-9/10 procedure codes for claims/encounters and will never be applicable. | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP079-0005 | |||
| 312 | CIP080 | PROCEDURE-CODE-FLAG-3 | A series of flags that identifies the coding system used for the associated procedure codes (PROCDURE-CODE-2 through PROCDURE-CODE-6) | Conditional | Value must be equal to a valid value. | 01 CPT 4 02 ICD-9 CM 06 HCPCS (Both National and Regional HCPCS) 07 ICD-10-CM PCS (Will be implemented on 10/1/2014) 10-87 Other Systems 88 Not Applicable 99 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP080-0001 |
| 313 | CIP080 | PROCEDURE-CODE-FLAG-3 | If no third procedure was performed, 8-fill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP080-0002 | |||
| 314 | CIP080 | PROCEDURE-CODE-FLAG-3 | Do not use multiple instances of PROCEDURE-CODE-FLAG if the preceding PROCEDURE-CODE-FLAG element is not populated. (i.e. if PROCEDURE-CODE-FLAG-2 is populated, but PROCEDURE-CODE-FLAG-3 is blank-filled, then PROCEDURE-CODE-FLAG-4 must also not be valued. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP080-0003 | |||
| 315 | CIP080 | PROCEDURE-CODE-FLAG-3 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP080-0004 | |||
| 316 | CIP081 | PROCEDURE-CODE-DATE-3 | The date on which the procedure 2 – 6 was performed |
Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP081-0001 | |
| 317 | CIP081 | PROCEDURE-CODE-DATE-3 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP081-0002 | |||
| 318 | CIP081 | PROCEDURE-CODE-DATE-3 | If the corresponding procedure code is 8-filled, then this procedure code date must be 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP081-0003 | |||
| 319 | CIP081 | PROCEDURE-CODE-DATE-3 | Date must occur before the ENDING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP081-0004 | |||
| 320 | CIP081 | PROCEDURE-CODE-DATE-3 | Date must occur on or after the BEGINNING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP081-0005 | |||
| 321 | CIP081 | PROCEDURE-CODE-DATE-3 | This date must occur on or before the DATE-OF-DEATH in the Eligible file. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP081-0006 | |||
| 322 | CIP081 | PROCEDURE-CODE-DATE-3 | Do not use multiple instances of PROCEDURE-CODE-DATE if the preceding PROCEDURE-CODE-DATE element is not populated. (i.e. if PROCEDURE-CODE-DATE-2 is populated, but PROCEDURE-CODE-DATE-3 is blank-filled, then PROCEDURE-CODE-DATE-4 must also not be valued. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP081-0007 | |||
| 323 | CIP081 | PROCEDURE-CODE-DATE-3 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP081-0008 | |||
| 324 | CIP082 | PROCEDURE-CODE-4 | A procedure code based on ICD-9 and ICD-10 used by the state to identify the procedures performed during the hospital stay referenced by this claim. The principal procedure and related info should be recorded in PROCEDURE-CODE-1, PROCEDURE-CODE-MOD-1, PROCEDURE-CODE-DATE-1, and PROCEDURE-CODE-FLAG-1. The principal procedure is performed for definitive treatment rather than for diagnostic or exploratory purposes. It is closely related to either the principal diagnosis or to complications that arise during other treatments. Use PROCEDURE-CODE-2 through PROCEDURE-CODE-6 (and related data elements) to record secondary, tertiary, etc. procedures. |
Conditional | Enter as many procedures as are reported after the principal procedure up to five additional codes. Remaining fields should be 8-filled (e.g., if claim contains two additional procedures, they would be reported in PROCDURE-CODE-2 and PROCDURE-CODE-3. Remaining fields PROCDURE-CODE-4 through PROCDURE-CODE-6 would all be 8-filled.) | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html http://www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/index.html?redirect=/medhcpcsgeninfo/ http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Relative-Value-Files.html http://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx Additional CPT codes are available for a fee through professional organizations. |
10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP082-0001 |
| 325 | CIP082 | PROCEDURE-CODE-4 | Value must be equal to a valid value. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP082-0002 | |||
| 326 | CIP082 | PROCEDURE-CODE-4 | If PROCDURE-CODE-FLAG-1 = {10 through 87, state-specific coding systems} valid codes must be supplied by the State. For national coding systems, code should conform to the nationally recognized formats: | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP082-0003 | |||
| 327 | CIP082 | PROCEDURE-CODE-4 | o ICD-9/10-CM (corresponding PROCDURE-CODE-FLAG = 02/07): Positions 1-2 must be numeric, positions 3-4 must be numeric or blank, positions 5-8 must be blank. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP082-0004 | |||
| 328 | CIP082 | PROCEDURE-CODE-4 | Value can include both National and Local (Regional) codes. For National codes (position 1=“A”-“V”) positions 2-5 must be numeric; for Local (Regional) codes, positions 2-5 must be alphanumeric (e.g., “X1234" or “WW234"). | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP082-0005 | |||
| 329 | CIP082 | PROCEDURE-CODE-4 | If no PROCEDURE-CODE-4 was performed, 8-fill | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP082-0006 | |||
| 330 | CIP082 | PROCEDURE-CODE-4 | Note: An eighth character is provided for future expansion of this field. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP082-0007 | |||
| 331 | CIP082 | PROCEDURE-CODE-4 | If PROCEDURE-CODE-2 AND PROCEDURE-CODE-3 = "88888888", then PROCEDURE-CODE-4 must = "88888888". | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP082-0008 | |||
| 332 | CIP082 | PROCEDURE-CODE-4 | Do not use multiple instances of PROCEDURE-CODE if the preceding PROCEDURE-CODE element is not populated. (i.e. if PROCEDURE-CODE-2 is populated, but PROCEDURE-CODE-3 is blank-filled, then PROCEDURE-CODE-4 must also not be valued. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP082-0009 | |||
| 333 | CIP082 | PROCEDURE-CODE-4 | If the corresponding procedure code flag is 8-filled, then this procedure code should be 8- filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP082-0010 | |||
| 334 | CIP082 | PROCEDURE-CODE-4 | If the corresponding procedure code flag is 8-filled, then this procedure code should be 8- filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP082-0011 | |||
| 335 | CIP082 | PROCEDURE-CODE-4 | Value must be different from the preceding procedure code values. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP082-0012 | |||
| 336 | CIP082 | PROCEDURE-CODE-4 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP082-0013 | |||
| 337 | CIP083 | PROCEDURE-CODE-MOD-4 | A series of procedure code modifiers used with the corresponding Procedure Codes. For example, some states use modifiers to indicate assistance in surgery or anesthesia services. |
NA | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP083-0001 |
| 338 | CIP083 | PROCEDURE-CODE-MOD-4 | Value must be 8-filled if corresponding procedure code is 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP083-0002 | |||
| 339 | CIP083 | PROCEDURE-CODE-MOD-4 | If the corresponding procedure code flag is not 8-filled, then this procedure code must not be 8- filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP083-0003 | |||
| 340 | CIP083 | PROCEDURE-CODE-MOD-4 | Do not use multiple instances of PROCEDURE-CODE-MOD if the preceding PROCEDURE-CODE-MOD element is not populated. (i.e. if PROCEDURE-CODE-MOD-2 is populated, but PROCEDURE-CODE-MOD-3 is blank-filled, then PROCEDURE-CODE-MOD-4 must also not be valued. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP083-0004 | |||
| 341 | CIP083 | PROCEDURE-CODE-MOD-4 | If no corresponding procedure (PROCDURE-CODE-2 through PROCDURE-CODE-6) was performed, 8-fill | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP083-0005 | |||
| 342 | CIP083 | PROCEDURE-CODE-MOD-4 | Always leave blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). Modifiers do not exist for ICD-9/10 procedure codes for claims/encounters and will never be applicable. | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP083-0006 | |||
| 343 | CIP084 | PROCEDURE-CODE-FLAG-4 | A series of flags that identifies the coding system used for the associated procedure codes (PROCDURE-CODE-2 through PROCDURE-CODE-6) | Conditional | Value must be equal to a valid value. | 01 CPT 4 02 ICD-9 CM 06 HCPCS (Both National and Regional HCPCS) 07 ICD-10-CM PCS (Will be implemented on 10/1/2014) 10-87 Other Systems 88 Not Applicable 99 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP084-0001 |
| 344 | CIP084 | PROCEDURE-CODE-FLAG-4 | If no fourth procedure was performed, 8-fill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP084-0002 | |||
| 345 | CIP084 | PROCEDURE-CODE-FLAG-4 | Do not use multiple instances of PROCEDURE-CODE-FLAG if the preceding PROCEDURE-CODE-FLAG element is not populated. (i.e. if PROCEDURE-CODE-FLAG-2 is populated, but PROCEDURE-CODE-FLAG-3 is blank-filled, then PROCEDURE-CODE-FLAG-4 must also not be valued. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP084-0003 | |||
| 346 | CIP084 | PROCEDURE-CODE-FLAG-4 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP084-0004 | |||
| 347 | CIP085 | PROCEDURE-CODE-DATE-4 | The date on which the procedure 2 – 6 was performed |
Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP085-0001 | |
| 348 | CIP085 | PROCEDURE-CODE-DATE-4 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP085-0002 | |||
| 349 | CIP085 | PROCEDURE-CODE-DATE-4 | If the corresponding procedure code is 8-filled, then this procedure code date must be 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP085-0003 | |||
| 350 | CIP085 | PROCEDURE-CODE-DATE-4 | Date must occur before the ENDING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP085-0004 | |||
| 351 | CIP085 | PROCEDURE-CODE-DATE-4 | Date must occur on or after the BEGINNING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP085-0005 | |||
| 352 | CIP085 | PROCEDURE-CODE-DATE-4 | This date must occur on or before the DATE-OF-DEATH in the Eligible file. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP085-0006 | |||
| 353 | CIP085 | PROCEDURE-CODE-DATE-4 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP085-0007 | |||
| 354 | CIP086 | PROCEDURE-CODE-5 | A procedure code based on ICD-9 and ICD-10 used by the state to identify the procedures performed during the hospital stay referenced by this claim. The principal procedure and related info should be recorded in PROCEDURE-CODE-1, PROCEDURE-CODE-MOD-1, PROCEDURE-CODE-DATE-1, and PROCEDURE-CODE-FLAG-1. The principal procedure is performed for definitive treatment rather than for diagnostic or exploratory purposes. It is closely related to either the principal diagnosis or to complications that arise during other treatments. Use PROCEDURE-CODE-2 through PROCEDURE-CODE-6 (and related data elements) to record secondary, tertiary, etc. procedures. |
Conditional | Enter as many procedures as are reported after the principal procedure up to five additional codes. Remaining fields should be 8-filled (e.g., if claim contains two additional procedures, they would be reported in PROCDURE-CODE-2 and PROCDURE-CODE-3. Remaining fields PROCDURE-CODE-4 through PROCDURE-CODE-6 would all be 8-filled.) | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html http://www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/index.html?redirect=/medhcpcsgeninfo/ http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Relative-Value-Files.html http://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx Additional CPT codes are available for a fee through professional organizations. |
10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP086-0001 |
| 355 | CIP086 | PROCEDURE-CODE-5 | Value must be equal to a valid value. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP086-0002 | |||
| 356 | CIP086 | PROCEDURE-CODE-5 | If PROCDURE-CODE-FLAG-1 = {10 through 87, state-specific coding systems} valid codes must be supplied by the State. For national coding systems, code should conform to the nationally recognized formats: | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP086-0003 | |||
| 357 | CIP086 | PROCEDURE-CODE-5 | o ICD-9/10-CM (corresponding PROCDURE-CODE-FLAG = 02/07): Positions 1-2 must be numeric, positions 3-4 must be numeric or blank, positions 5-8 must be blank. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP086-0004 | |||
| 358 | CIP086 | PROCEDURE-CODE-5 | Value can include both National and Local (Regional) codes. For National codes (position 1=“A”-“V”) positions 2-5 must be numeric; for Local (Regional) codes, positions 2-5 must be alphanumeric (e.g., “X1234" or “WW234"). | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP086-0005 | |||
| 359 | CIP086 | PROCEDURE-CODE-5 | If no PROCEDURE-CODE-5 was performed, 8-fill | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP086-0006 | |||
| 360 | CIP086 | PROCEDURE-CODE-5 | Note: An eighth character is provided for future expansion of this field. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP086-0007 | |||
| 361 | CIP086 | PROCEDURE-CODE-5 | Do not use multiple instances of PROCEDURE-CODE if the preceding PROCEDURE-CODE element is not populated. (i.e. if PROCEDURE-CODE-2 is populated, but PROCEDURE-CODE-3 is blank-filled, then PROCEDURE-CODE-4 must also not be valued. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP086-0008 | |||
| 362 | CIP086 | PROCEDURE-CODE-5 | If the corresponding procedure code flag is 8-filled, then this procedure code should be 8- filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP086-0009 | |||
| 363 | CIP086 | PROCEDURE-CODE-5 | If the corresponding procedure code flag is not 8-filled, then this procedure code must not be 8- filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP086-0010 | |||
| 364 | CIP086 | PROCEDURE-CODE-5 | Value must be different from the preceding procedure code values. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP086-0011 | |||
| 365 | CIP086 | PROCEDURE-CODE-5 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP086-0012 | |||
| 366 | CIP087 | PROCEDURE-CODE-MOD-5 | A series of procedure code modifiers used with the corresponding Procedure Codes. For example, some states use modifiers to indicate assistance in surgery or anesthesia services. |
NA | A list of valid codes must be supplied by the state prior to submission of any file data. | Valid values are supplied by the state. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP087-0001 |
| 367 | CIP087 | PROCEDURE-CODE-MOD-5 | Value must be 8-filled if corresponding procedure code is 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP087-0002 | |||
| 368 | CIP087 | PROCEDURE-CODE-MOD-5 | Do not use multiple instances of PROCEDURE-CODE-MOD if the preceding PROCEDURE-CODE-MOD element is not populated. (i.e. if PROCEDURE-CODE-MOD-2 is populated, but PROCEDURE-CODE-MOD-3 is blank-filled, then PROCEDURE-CODE-MOD-4 must also not be valued. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP087-0003 | |||
| 369 | CIP087 | PROCEDURE-CODE-MOD-5 | If no corresponding procedure (PROCDURE-CODE-2 through PROCDURE-CODE-6) was performed, 8-fill | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP087-0004 | |||
| 370 | CIP087 | PROCEDURE-CODE-MOD-5 | Always leave blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). Modifiers do not exist for ICD-9/10 procedure codes for claims/encounters and will never be applicable. | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP087-0005 | |||
| 371 | CIP088 | PROCEDURE-CODE-FLAG-5 | A series of flags that identifies the coding system used for the associated procedure codes (PROCDURE-CODE-2 through PROCDURE-CODE-6) | Conditional | Value must be equal to a valid value. | 01 CPT 4 02 ICD-9 CM 06 HCPCS (Both National and Regional HCPCS) 07 ICD-10-CM PCS (Will be implemented on 10/1/2014) 10-87 Other Systems 88 Not Applicable 99 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP088-0001 |
| 372 | CIP088 | PROCEDURE-CODE-FLAG-5 | If no fifth procedure was performed, 8-fill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP088-0002 | |||
| 373 | CIP088 | PROCEDURE-CODE-FLAG-5 | Do not use multiple instances of PROCEDURE-CODE-FLAG if the preceding PROCEDURE-CODE-FLAG element is not populated. (i.e. if PROCEDURE-CODE-FLAG-2 is populated, but PROCEDURE-CODE-FLAG-3 is blank-filled, then PROCEDURE-CODE-FLAG-4 must also not be valued. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP088-0003 | |||
| 374 | CIP088 | PROCEDURE-CODE-FLAG-5 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP088-0004 | |||
| 375 | CIP089 | PROCEDURE-CODE-DATE-5 | The date on which the procedure 2 – 6 was performed. | Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP089-0001 | |
| 376 | CIP089 | PROCEDURE-CODE-DATE-5 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP089-0002 | |||
| 377 | CIP089 | PROCEDURE-CODE-DATE-5 | If the corresponding procedure code is 8-filled, then this procedure code date must be 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP089-0003 | |||
| 378 | CIP089 | PROCEDURE-CODE-DATE-5 | Date must occur before the ENDING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP089-0004 | |||
| 379 | CIP089 | PROCEDURE-CODE-DATE-5 | Date must occur on or after the BEGINNING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP089-0005 | |||
| 380 | CIP089 | PROCEDURE-CODE-DATE-5 | This date must occur on or before the DATE-OF-DEATH in the Eligible file. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP089-0006 | |||
| 381 | CIP089 | PROCEDURE-CODE-DATE-5 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP089-0007 | |||
| 382 | CIP090 | PROCEDURE-CODE-6 | A procedure code based on ICD-9 and ICD-10 used by the state to identify the procedures performed during the hospital stay referenced by this claim. The principal procedure and related info should be recorded in PROCEDURE-CODE-1, PROCEDURE-CODE-MOD-1, PROCEDURE-CODE-DATE-1, and PROCEDURE-CODE-FLAG-1. The principal procedure is performed for definitive treatment rather than for diagnostic or exploratory purposes. It is closely related to either the principal diagnosis or to complications that arise during other treatments. Use PROCEDURE-CODE-2 through PROCEDURE-CODE-6 (and related data elements) to record secondary, tertiary, etc. procedures. |
Conditional | Enter as many procedures as are reported after the principal procedure up to five additional codes. Remaining fields should be 8-filled (e.g., if claim contains two additional procedures, they would be reported in PROCDURE-CODE-2 and PROCDURE-CODE-3. Remaining fields PROCDURE-CODE-4 through PROCDURE-CODE-6 would all be 8-filled.) | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html http://www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/index.html?redirect=/medhcpcsgeninfo/ http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Relative-Value-Files.html http://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx Additional CPT codes are available for a fee through professional organizations. |
10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP090-0001 |
| 383 | CIP090 | PROCEDURE-CODE-6 | Value must be equal to a valid value. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP090-0002 | |||
| 384 | CIP090 | PROCEDURE-CODE-6 | If PROCDURE-CODE-FLAG-1 = {10 through 87, state-specific coding systems} valid codes must be supplied by the State. For national coding systems, code should conform to the nationally recognized formats: | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP090-0003 | |||
| 385 | CIP090 | PROCEDURE-CODE-6 | o ICD-9/10-CM (corresponding PROCDURE-CODE-FLAG = 02/07): Positions 1-2 must be numeric, positions 3-4 must be numeric or blank, positions 5-8 must be blank. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP090-0004 | |||
| 386 | CIP090 | PROCEDURE-CODE-6 | Value can include both National and Local (Regional) codes. For National codes (position 1=“A”-“V”) positions 2-5 must be numeric; for Local (Regional) codes, positions 2-5 must be alphanumeric (e.g., “X1234" or “WW234"). | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP090-0005 | |||
| 387 | CIP090 | PROCEDURE-CODE-6 | If no PROCEDURE-CODE-6 was performed, 8-fill | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP090-0006 | |||
| 388 | CIP090 | PROCEDURE-CODE-6 | Note: An eighth character is provided for future expansion of this field. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP090-0007 | |||
| 389 | CIP090 | PROCEDURE-CODE-6 | Do not use multiple instances of PROCEDURE-CODE if the preceding PROCEDURE-CODE element is not populated. (i.e. if PROCEDURE-CODE-2 is populated, but PROCEDURE-CODE-3 is blank-filled, then PROCEDURE-CODE-4 must also not be valued. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP090-0008 | |||
| 390 | CIP090 | PROCEDURE-CODE-6 | If the corresponding procedure code flag is 8-filled, then this procedure code should be 8- filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP090-0009 | |||
| 391 | CIP090 | PROCEDURE-CODE-6 | If the corresponding procedure code flag is not 8-filled, then this procedure code must not be 8- filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP090-0010 | |||
| 392 | CIP090 | PROCEDURE-CODE-6 | Value must be different from the preceding procedure code values. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP090-0011 | |||
| 393 | CIP090 | PROCEDURE-CODE-6 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP090-0012 | |||
| 394 | CIP091 | PROCEDURE-CODE-MOD-6 | A series of procedure code modifiers used with the corresponding Procedure Codes. For example, some states use modifiers to indicate assistance in surgery or anesthesia services. |
NA | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP091-0001 |
| 395 | CIP091 | PROCEDURE-CODE-MOD-6 | Value must be 8-filled if corresponding procedure code is 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP091-0002 | |||
| 396 | CIP091 | PROCEDURE-CODE-MOD-6 | Do not use multiple instances of PROCEDURE-CODE-MOD if the preceding PROCEDURE-CODE-MOD element is not populated. (i.e. if PROCEDURE-CODE-MOD-2 is populated, but PROCEDURE-CODE-MOD-3 is blank-filled, then PROCEDURE-CODE-MOD-4 must also not be valued. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP091-0003 | |||
| 397 | CIP091 | PROCEDURE-CODE-MOD-6 | If no corresponding procedure (PROCDURE-CODE-2 through PROCDURE-CODE-6) was performed, 8-fill | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP091-0004 | |||
| 398 | CIP091 | PROCEDURE-CODE-MOD-6 | Always leave blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). Modifiers do not exist for ICD-9/10 procedure codes for claims/encounters and will never be applicable. | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP091-0005 | |||
| 399 | CIP092 | PROCEDURE-CODE-FLAG-6 | A series of flags that identifies the coding system used for the associated procedure codes (PROCDURE-CODE-2 through PROCDURE-CODE-6) | Conditional | Value must be equal to a valid value. | 01 CPT 4 02 ICD-9 CM 06 HCPCS (Both National and Regional HCPCS) 07 ICD-10-CM PCS (Will be implemented on 10/1/2014) 10-87 Other Systems 88 Not Applicable 99 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP092-0001 |
| 400 | CIP092 | PROCEDURE-CODE-FLAG-6 | If no sixth procedure was performed, 8-fill. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP092-0002 | |||
| 401 | CIP092 | PROCEDURE-CODE-FLAG-6 | Do not use multiple instances of PROCEDURE-CODE-FLAG if the preceding PROCEDURE-CODE-FLAG element is not populated. (i.e. if PROCEDURE-CODE-FLAG-2 is populated, but PROCEDURE-CODE-FLAG-3 is blank-filled, then PROCEDURE-CODE-FLAG-4 must also not be valued. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP092-0003 | |||
| 402 | CIP092 | PROCEDURE-CODE-FLAG-6 | Value must be 8-filled if there are no MEDICAID-COV-INPATIENT-DAYS. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP092-0004 | |||
| 403 | CIP092 | PROCEDURE-CODE-FLAG-6 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP092-0005 | |||
| 404 | CIP093 | PROCEDURE-CODE-DATE-6 | The date on which the procedure 2 – 6 was performed. | Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP093-0001 | |
| 405 | CIP093 | PROCEDURE-CODE-DATE-6 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP093-0002 | |||
| 406 | CIP093 | PROCEDURE-CODE-DATE-6 | If the corresponding procedure code is 8-filled, then this procedure code date must be 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP093-0003 | |||
| 407 | CIP093 | PROCEDURE-CODE-DATE-6 | Date must occur before the ENDING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP093-0004 | |||
| 408 | CIP093 | PROCEDURE-CODE-DATE-6 | Date must occur on or after the BEGINNING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP093-0005 | |||
| 409 | CIP093 | PROCEDURE-CODE-DATE-6 | This date must occur on or before the DATE-OF-DEATH in the Eligible file. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP093-0006 | |||
| 410 | CIP093 | PROCEDURE-CODE-DATE-6 | CMS is not expecting PROCEDURE-CODE-FLAG-1 through 6 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP093-0007 | |||
| 411 | CIP094 | ADMISSION-DATE | The date on which the recipient was admitted to a hospital or long term care facility. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP094-0001 | |
| 412 | CIP094 | ADMISSION-DATE | Value must be a valid date | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP094-0002 | |||
| 413 | CIP094 | ADMISSION-DATE | ADMISSION-DATE must occur on or before the ADJUDICATION-DATE | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP094-0003 | |||
| 414 | CIP094 | ADMISSION-DATE | ADMISSION-DATE must occur on or before the DISCHARGE-DATE | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP094-0004 | |||
| 415 | CIP094 | ADMISSION-DATE | ADMISSION-DATE must occur on or after the DATE-OF-BIRTH listed in Eligible Record. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP094-0005 | |||
| 416 | CIP094 | ADMISSION-DATE | ADMISSION-DATE must occur on or before the DATE-OF-DEATH listed in Eligible Record. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP094-0006 | |||
| 417 | CIP095 | ADMISSION-HOUR | The time of admission to a hospital or long term care facility. | Conditional | Value must be a valid hour in military time format (00 to 23). | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP095-0001 |
| 418 | CIP096 | DISCHARGE-DATE | The date on which the recipient was discharged from a hospital or long term care facility. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP096-0001 | |
| 419 | CIP096 | DISCHARGE-DATE | Value must be a valid date | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP096-0002 | |||
| 420 | CIP096 | DISCHARGE-DATE | If a complete, valid date of discharge is not available or is unknown, fill with 99999999 | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP096-0003 | |||
| 421 | CIP096 | DISCHARGE-DATE | This date must occur on or after the ADMISSION-DATE. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP096-0004 | |||
| 422 | CIP096 | DISCHARGE-DATE | This date must occur on or after the ADJUDICATION-DATE. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP096-0005 | |||
| 423 | CIP096 | DISCHARGE-DATE | This field is required if TYPE-OF-SERVICE does not equal a capitated payment (Valid values for capitated payment include 119, 120, 122). | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP096-0006 | |||
| 424 | CIP096 | DISCHARGE-DATE | This date must occur on or after the DATE-OF-BIRTH in the Eligible Record. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP096-0007 | |||
| 425 | CIP096 | DISCHARGE-DATE | This date must occur on or before the DATE-OF-DEATH in the Eligible record | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP096-0008 | |||
| 426 | CIP097 | DISCHARGE-HOUR | The time of discharge for inpatient claims or end time of treatment for outpatient claims. | Conditional | Value must be a valid hour in military time format (00 to 23). | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP097-0001 |
| 427 | CIP098 | ADJUDICATION-DATE | The date on which the payment status of the claim was finally adjudicated by the state. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP098-0001 | |
| 428 | CIP098 | ADJUDICATION-DATE | Value must be a valid date | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP098-0002 | |||
| 429 | CIP098 | ADJUDICATION-DATE | For Adjustment Records (ADJUSTMENT-INDICATOR<> 0), use date of final adjudication when possible. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP098-0003 | |||
| 430 | CIP098 | ADJUDICATION-DATE | For Encounter Records (TYPE-OF-CLAIM=3, C, W); use date the encounter was processed by the state. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP098-0004 | |||
| 431 | CIP098 | ADJUDICATION-DATE | If a complete, valid date is not available or is unknown, 9-fil | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP098-0005 | |||
| 432 | CIP098 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or before END-OF-TIME-PERIOD included in the T-MSIS HEADER RECORD | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP098-0006 | |||
| 433 | CIP098 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or after the ADMISSION-DATE | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP098-0007 | |||
| 434 | CIP098 | ADJUDICATION-DATE | This date must occur on or after the DATE-OF-BIRTH in the Eligible Record when the eligible is not a CHIP unborn child. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP098-0008 | |||
| 435 | CIP098 | ADJUDICATION-DATE | A Medicaid or CHIP eligible individual should not have had a claim adjudicated before their five-year immigration ineligible status has expired, except when the eligible is an unborn child in the CHIP program. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP098-0009 | |||
| 436 | CIP099 | MEDICAID-PAID-DATE | The date Medicaid paid on this claim or adjustment. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP099-0001 | |
| 437 | CIP099 | MEDICAID-PAID-DATE | Value must be a valid date | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP099-0002 | |||
| 438 | CIP100 | TYPE-OF-CLAIM | A code indicating what kind of payment is covered in this claim. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP100-0001 |
| 439 | CIP100 | TYPE-OF-CLAIM | States should only submit CHIP claims for CHIP eligibles | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP100-0002 | |||
| 440 | CIP100 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the basis of eligibility. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP100-0003 | |||
| 441 | CIP100 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the maintenance assistance status. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP100-0004 | |||
| 442 | CIP100 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the restricted benefits code. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP100-0005 | |||
| 443 | CIP100 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the TANF code. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP100-0006 | |||
| 444 | CIP101 | TYPE-OF-BILL | A data element corresponding with UB-04 form locator FL4 that classifies the claim as to the type of facility (2nd digit), type of care (3rd digit) and the billing record's sequence in the episode of care (4th digit). (Note that the 1st digit is always zero.) | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP101-0001 |
| 445 | CIP102 | CLAIM-STATUS | The health care claim status codes convey the status of an entire claim. | Required | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-codes/ | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP102-0001 |
| 446 | CIP103 | CLAIM-STATUS-CATEGORY | The general category of the claim status (accepted, rejected, pended, finalized, additional information requested, etc.), which is then further detailed in the companion data element CLAIM-STATUS |
Required | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-category-codes/ | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP103-0001 |
| 447 | CIP104 | SOURCE-LOCATION | The field denotes the claims payment system from which the claim was extracted | Required | Value must be equal to a valid value. | 01 MMIS 02 Non-MMIS CHIP Payment System 03 Pharmacy Benefits Manager (PBM) Vendor 04 Dental Benefits Manager Vendor 05 Transportation Provider System 06 Mental Health Claims Payment System 07 Financial Transaction/Accounting System 08 Other State Agency Claims Payment System 09 County/Local Government Claims Payment System 10 Other Vendor/Other Claims Payment System 20 Managed Care Organization (MCO) 99 Unknown source |
4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP104-0001 |
| 448 | CIP105 | CHECK-NUM | The check or EFT number. |
Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9),, dashes (-), and spaces. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP105-0001 | |
| 449 | CIP105 | CHECK-NUM | If there is a valid check date there should also be a valid check number. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP105-0002 | |||
| 450 | CIP106 | CHECK-EFF-DATE | Date the check is issued to the payee, or if Electronic Funds Transfer (EFT), the date the transfer is made. | Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP106-0001 | |
| 451 | CIP106 | CHECK-EFF-DATE | Value must be a valid date | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP106-0002 | |||
| 452 | CIP106 | CHECK-EFF-DATE | Could be the same as Remittance Date. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP106-0003 | |||
| 453 | CIP106 | CHECK-EFF-DATE | If there is a valid check number, there should also be a valid check date. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP106-0004 | |||
| 454 | CIP107 | ALLOWED-CHARGE-SRC | These codes indicate how each allowed charge was determined. | Conditional | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP107-0001 |
| 455 | CIP107 | ALLOWED-CHARGE-SRC | Claims records for an eligible individual should not indicate Medicare as the source to indicate how an allowed charge was determined on the claim, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP107-0002 | |||
| 456 | CIP108 | CLAIM-PYMT-REM-CODE-1 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP108-0001 |
| 457 | CIP109 | CLAIM-PYMT-REM-CODE-2 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP109-0001 |
| 458 | CIP110 | CLAIM-PYMT-REM-CODE-3 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP110-0001 |
| 459 | CIP111 | CLAIM-PYMT-REM-CODE-4 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP111-0001 |
| 460 | CIP112 | TOT-BILLED-AMT | The total amount charged for this claim at the claim header level as submitted by the provider. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP112-0001 | |
| 461 | CIP112 | TOT-BILLED-AMT | The total amount should be the sum of each of the billed amounts submitted at the claim detail level. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP112-0002 | |||
| 462 | CIP112 | TOT-BILLED-AMT | If TYPE-OF-CLAIM = "4", then TOT-BILLED-AMT must = "00000000". | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP112-0003 | |||
| 463 | CIP112 | TOT-BILLED-AMT | If TYPE-OF-CLAIM = 3, C, W (encounter record) this field should either be zero-filled or contain the amount paid by the plan to the provider. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP112-0004 | |||
| 464 | CIP113 | TOT-ALLOWED-AMT | The claim header level maximum amount determined by the payer as being 'allowable' under the provisions of the contract prior to the determination of actual payment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP113-0001 | |
| 465 | CIP113 | TOT-ALLOWED-AMT | The sum of the allowed amounts at the detailed levels must equal TOT-ALLOWED-AMT | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP113-0002 | |||
| 466 | CIP114 | TOT-MEDICAID-PAID-AMT | The total amount paid by Medicaid on this claim or adjustment at the claim header level, which is the sum of the amounts paid by Medicaid at the detail level for the claim. | Required | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP114-0001 | |
| 467 | CIP115 | TOT-COPAY-AMT | The total amount paid by Medicaid/CHIP enrollee for each office or emergency department visit or purchase of prescription drugs in addition to the amount paid by Medicaid/CHIP. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP115-0001 | |
| 468 | CIP116 | TOT-MEDICARE-DEDUCTIBLE-AMT | The amount paid by Medicaid/CHIP, on this claim at the claim header level, toward the beneficiary’s Medicare deductible. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP116-0001 | |
| 469 | CIP116 | TOT-MEDICARE-DEDUCTIBLE-AMT | If the Medicare deductible amount can be identified separately from Medicare coinsurance payments, code that amount in this field. If the Medicare coinsurance and deductible payments cannot be separated, fill this field with the combined payment amount and code space in TOT-MEDICARE-COINS-AMT | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP116-0002 | |||
| 470 | CIP116 | TOT-MEDICARE-DEDUCTIBLE-AMT | The total medicare deductible amount must be less than or equal the total billed amount. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP116-0003 | |||
| 471 | CIP116 | TOT-MEDICARE-DEDUCTIBLE-AMT | If TOT-MEDICARE-COINS-AMT = "88888", then TOT-MEDICARE-DEDUCTIBLE-AMT must = "88888". | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP116-0004 | |||
| 472 | CIP116 | TOT-MEDICARE-DEDUCTIBLE-AMT | If TOT-MEDICARE-COINS-AMT = "99999", then TOT-MEDICARE-DEDUCTIBLE-AMT must = "99999". | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP116-0005 | |||
| 473 | CIP117 | TOT-MEDICARE-COINS-AMT | The amount paid by Medicaid/CHIP, on this claim at the claim header level, toward the beneficiary’s Medicare coinsurance. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP117-0001 | |
| 474 | CIP117 | TOT-MEDICARE-COINS-AMT | Value should be reported as not applicable if the TYPE-OF-CLAIM is an encounter (valid values = 3, C, W) | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP117-0002 | |||
| 475 | CIP117 | TOT-MEDICARE-COINS-AMT | Value must be less than TOT-BILLED-AMT. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP117-0003 | |||
| 476 | CIP117 | TOT-MEDICARE-COINS-AMT | Value must be 8-filled if 'TOT-MEDICARE-DEDUCTIBLE-AMT' is 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP117-0004 | |||
| 477 | CIP117 | TOT-MEDICARE-COINS-AMT | If the Medicare deductible amount can be identified separately from Medicare coinsurance payments, code that amount in this field. If the Medicare coinsurance and deductible payments cannot be separated, fill this field with the combined payment amount and code space in TOT-MEDICARE-COINS-AMT | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP117-0005 | |||
| 478 | CIP118 | TOT-TPL-AMT | Third Party Liability (TPL) refers to the legal obligation of third parties, i.e., certain individuals, entities, or programs, to pay all or part of the expenditures for medical assistance furnished under a state plan. This is the total amount denoted at the claim header level paid by the third party. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP118-0001 | |
| 479 | CIP118 | TOT-TPL-AMT | The absolute value of TOT-TPL-AMT must be < The absolute value of (TOT-BILLED-AMT - (minus) TOT-MEDICARE-COINS-AMT + (plus) TOT-MEDICARE-DEDUCTIBLE-AMT). | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP118-0002 | |||
| 480 | CIP119 | TOT-OTHER-INSURANCE-AMT | The amount paid by insurance other than Medicare or Medicaid on this claim. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP119-0001 | |
| 481 | CIP121 | OTHER-INSURANCE-IND | The field denotes whether the insured party is covered under other insurance plan | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP121-0001 |
| 482 | CIP122 | OTHER-TPL-COLLECTION | This data element indicates that the claim is for a beneficiary for whom other third party resource development and collection activities are in progress, when the liability is not another health insurance plan for which the eligible is a beneficiary | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 Third Party Resource is Casualty/Tort 002 Third Party Resource is Estate 003 Third Party Resource is Lien (TEFRA) 004 Third Party Resource is Lien (Other) 005 Third Party Resource is Worker’s Compensation 006 Third Party Resource is Medical Malpractice 007 Third Party Resource is Other 999 Classification of Third Party Resource is Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP122-0001 |
| 483 | CIP123 | SERVICE-TRACKING-TYPE | A code to categorize service tracking claims. A “service tracking claim” is used to report lump sum payments that cannot be attributed to a single enrollee. (Note: Use an encounter record to report services provided under a capitated payment arrangement.) | Conditional | Value must be equal to a valid value. | 00 Not a Service Tracking Claim 01 Drug Rebate 02 DSH Payment 03 Lump Sum Payment 04 Cost Settlement 05 Supplemental 06 Other 99 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP123-0001 |
| 484 | CIP124 | SERVICE-TRACKING-PAYMENT-AMT | On service tracking claims, the lump sum amount paid to the provider. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP124-0001 | |
| 485 | CIP124 | SERVICE-TRACKING-PAYMENT-AMT | Required on service tracking records | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP124-0002 | |||
| 486 | CIP124 | SERVICE-TRACKING-PAYMENT-AMT | Amount paid for services received by an individual patient, when the state accepts a lump sum form a provider that covered similar services delivered to more than one patient, such as a group screening for EPSDT. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP124-0003 | |||
| 487 | CIP124 | SERVICE-TRACKING-PAYMENT-AMT | For service tracking payments, ensure that the TOT-MEDICAID-PAID-AMOUNT is 0 filled and provide payment amount in SERVICE-TRACKING-PAYMENT-AMT only. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP124-0004 | |||
| 488 | CIP124 | SERVICE-TRACKING-PAYMENT-AMT | If there is a service tracking type, then there must also be a service tracking payment amount. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP124-0005 | |||
| 489 | CIP124 | SERVICE-TRACKING-PAYMENT-AMT | If SERVICE-TRACKING-TYPE <> "00" or "99", then SERVICE-TRACKING-PAYMENT-AMT must BE<> 000000000000. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP124-0006 | |||
| 490 | CIP125 | FIXED-PAYMENT-IND | This indicator indicates that the reimbursement amount included on the claim is for a fixed payment. Fixed payments are made by the state to insurers or providers for premiums or eligible coverage, not for a particular service. For example, some states have Primary Care Case Management (PCCM) programs where the state pays providers a monthly patient management fee of $3.50 for each eligible participant under their care. This fee is considered a fixed payment. It is very important for states to correctly identify fixed payments. Fixed payments do not have a defined “medical record” associated with the payment; therefore, fixed payments are not subject to medical record request and medical record review. |
Conditional | Value must be equal to a valid value. | 0 Not Fixed Payment 1 FFS Fixed Payment |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP125-0001 |
| 491 | CIP126 | FUNDING-CODE | A code to indicate the source of non-federal share funds. | Required | Value must be equal to a valid value. | A Medicaid Agency B CHIP Agency C Mental Health Service Agency D Education Agency E Child and Family Services Agency F County G City H Providers I Other |
10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP126-0001 |
| 492 | CIP127 | FUNDING-SOURCE-NONFEDERAL-SHARE | A code to indicate the type of non-federal share used by the state to finance its expenditure to the provider. | Required | Value must be equal to a valid value. When states have multiple sources of FUNDING-SOURCE-NONFEDERAL-SHARE, States are to report the portion which represents the largest proportion as the FUNDING-SOURCE-NONFEDERAL-SHARE. |
01 State appropriations to the Medicaid agency 02 Intergovernmental transfers (IGT) 03 Certified public expenditures (CPE) 04 Provider taxes 05 Donations |
9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP127-0001 |
| 493 | CIP128 | MEDICARE-COMB-DED-IND | Code indicating that the amount paid by Medicaid/CHIP on this claim toward the recipient's Medicare deductible was combined with their coinsurance amount because the amounts could not be separated. |
Conditional | Value must be equal to a valid value. | 0 Amount not combined with coinsurance amount 1 Amount combined with coinsurance amount 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP128-0001 |
| 494 | CIP128 | MEDICARE-COMB-DED-IND | If claim is not a Crossover claim, or if a type of claim is “3,” “C” or “W” (an encounter claim), set value to “0” | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP128-0002 | |||
| 495 | CIP128 | MEDICARE-COMB-DED-IND | Claims records for an eligible individual should not indicate Medicare paid any combined deductible amount on the claim, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP128-0003 | |||
| 496 | CIP129 | PROGRAM-TYPE | Code indicating special Medicaid program under which the service was provided. Refer to Appendix E for information on the various program types. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP129-0001 |
| 497 | CIP129 | PROGRAM-TYPE | Value for 1915 (c) waiver must correspond to the values for 1915(c) waiver in the Waiver Type. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP129-0002 | |||
| 498 | CIP129 | PROGRAM-TYPE | If PROGRAM-TYPE=Community First Choice (11) then [T-MSIS ELIGIBLE FILE] STATE-PLAN-OPTION-TYPE must = 01 for the same time period. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP129-0003 | |||
| 499 | CIP129 | PROGRAM-TYPE | If PROGRAM-TYPE=1915(i) (value=13) then [T-MSIS ELIGIBLE FILE] STATE-PLAN-OPTION-TYPE must = 02 for the same time period. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP129-0004 | |||
| 500 | CIP130 | PLAN-ID-NUMBER | A unique number, assigned by the state, which represents the health plan under which the non-fee-for-service encounter was provided including through the state plan and a waiver. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP130-0001 | |
| 501 | CIP130 | PLAN-ID-NUMBER | Use the number as it is carried in the state’s system. (TYPE-OF-CLAIM=3, C, W) | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP130-0002 | |||
| 502 | CIP130 | PLAN-ID-NUMBER | This data element must equal the BILLING-PROV-NUM if the TYPE-OF-SERVICE is a capitation payment. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP130-0003 | |||
| 503 | CIP130 | PLAN-ID-NUMBER | The managed care ID on the individual's eligible record must match that which is included on any claims records for the eligible individual. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP130-0004 | |||
| 504 | CIP131 | NATIONAL-HEALTH-CARE-ENTITY-ID | The national identifier of the health care entity (controlling health plan, subhealth plan, or other entity) at the most granular sub-health plan level of the Medicaid or CHIP health plan in which an individual is enrolled. (See 45 CFR 162 Subpart E. http://www.gpo.gov/fdsys/pkg/FR-2012-09-05/pdf/2012-21238.pdf | NA | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP131-0001 | |
| 505 | CIP131 | NATIONAL-HEALTH-CARE-ENTITY-ID | Large health plans are required to obtain national health plan identifiers by November 5, 2014, small health plans by November 5, 2015. States may report prior to these dates if available. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP131-0002 | |||
| 506 | CIP131 | NATIONAL-HEALTH-CARE-ENTITY-ID | This field is required for all managed care claims and encounters with dates of service on or after the mandated dates above. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP131-0003 | |||
| 507 | CIP131 | NATIONAL-HEALTH-CARE-ENTITY-ID | NATIONAL-HEALTH-CARE-ENTITY-IDs on managed care claims and encounters must match NATIONAL-HEALTH-CARE-ENTITY-IDs on file for the individual in the eligibility subject area or the TPL subject area | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP131-0004 | |||
| 508 | CIP132 | PAYMENT-LEVEL-IND | The field denotes whether the claim payment is made at the header level or the detail level. | Required | Value must be equal to a valid value. | 1 Claim Header – Sum of Line Item payments 2 Claim Detail – Individual Line Item payments |
4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP132-0001 |
| 509 | CIP132 | PAYMENT-LEVEL-IND | Payment fields at either the claim header or line on encounter records should be left blank. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP132-0002 | |||
| 510 | CIP133 | MEDICARE-REIM-TYPE | This code indicates the type of Medicare Reimbursement. | Conditional | Value must be equal to a valid value. | 01 IPPS - Acute Inpatient PPS 02 LTCHPPS - Long-term Care Hospital PPS 03 SNFPPS - Skilled Nursing Facility PPS 04 HHPPS - Home Health PPS 05 IRFPPS - Inpatient Rehabilitation Facility PPS 06 IPFPPS - Inpatient Psychiatric Facility PPS 07 OPPS - Outpatient PPS 08 Fee Schedules (for physicians, DME, ambulance, and clinical lab) 09 Part C Hierarchical Condition Category Risk Assessment (CMS-HCC RA) Capitation Payment Model |
10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP133-0001 |
| 511 | CIP133 | MEDICARE-REIM-TYPE | If this is a crossover Medicare claim, the claim must have a MEDICARE-REIM-TYPE. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP133-0002 | |||
| 512 | CIP134 | NON-COV-DAYS | The number of days of institutional long-term care not covered by the payer for this sequence as qualified by the payer organization. The number of non-covered days does not refer to days not covered for any other service. | Conditional | Must contain number of non-covered days. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP134-0001 | |
| 513 | CIP134 | NON-COV-DAYS | The sum of Non-Covered Days and Covered Days must not exceed Total Length of Stay (Statement Covers Period - Thru Date minus Admission Date\Start of Care) for any payer sequence. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP134-0002 | |||
| 514 | CIP135 | NON-COV-CHARGES | The charges for institutional long-term care, which are not reimbursable by the primary payer. The non-covered charges do not refer to charges not covered for any other service. | Conditional | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP135-0001 | |
| 515 | CIP136 | MEDICAID-COV-INPATIENT-DAYS | The number of inpatient days covered by Medicaid on this claim. For states that combine delivery/birth services on a single claim, include covered days for both the mother and the neonate in this field. |
Conditional | Must contain number of covered days. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP136-0001 | |
| 516 | CIP136 | MEDICAID-COV-INPATIENT-DAYS | This field is applicable when: - A CLAIMIP record includes at least one accommodation revenue code = (values 100-219) in REVENUE-CODE-(1-23) fields. |
2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP136-0002 | |||
| 517 | CIP136 | MEDICAID-COV-INPATIENT-DAYS | This total must not be greater than double the duration between the DISCHARGE-DATE and the ADMISSION-DATE, plus one day. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP136-0003 | |||
| 518 | CIP136 | MEDICAID-COV-INPATIENT-DAYS | This field is required if the Type of Service is 001, 058, 084, 086, 090, 091, 092, 093, 123, 132. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP136-0004 | |||
| 519 | CIP136 | MEDICAID-COV-INPATIENT-DAYS | This field is required if the value for UB-REV-CODE is between 100-219. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP136-0005 | |||
| 520 | CIP137 | CLAIM-LINE-COUNT | The total number of lines on the claim | Required | Must be populated on every record | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP137-0001 | |
| 521 | CIP137 | CLAIM-LINE-COUNT | If the number of claim lines is above the state-approved limit, the record will be split and the split-claim-ind will equal 1. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP137-0002 | |||
| 522 | CIP137 | CLAIM-LINE-COUNT | The claim line count should equal the sum of the claim lines for this record. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP137-0003 | |||
| 523 | CIP138 | FORCED-CLAIM-IND | This code indicates if the claim was processed by forcing it through a manual override process. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP138-0001 |
| 524 | CIP139 | HEALTH-CARE-ACQUIRED-CONDITION-IND | This code indicates whether the claim has a Health Care Acquired Condition. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP139-0001 |
| 525 | CIP140 | OCCURRENCE-CODE-01 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP140-0001 |
| 526 | CIP140 | OCCURRENCE-CODE-01 | Required if reported on the claim. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP140-0002 | |||
| 527 | CIP140 | OCCURRENCE-CODE-01 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP140-0003 | |||
| 528 | CIP141 | OCCURRENCE-CODE-02 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP141-0001 |
| 529 | CIP141 | OCCURRENCE-CODE-02 | Required if reported on the claim. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP141-0002 | |||
| 530 | CIP141 | OCCURRENCE-CODE-02 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP141-0003 | |||
| 531 | CIP142 | OCCURRENCE-CODE-03 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP142-0001 |
| 532 | CIP142 | OCCURRENCE-CODE-03 | Required if reported on the claim. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP142-0002 | |||
| 533 | CIP142 | OCCURRENCE-CODE-03 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP142-0003 | |||
| 534 | CIP143 | OCCURRENCE-CODE-04 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP143-0001 |
| 535 | CIP143 | OCCURRENCE-CODE-04 | Required if reported on the claim. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP143-0002 | |||
| 536 | CIP143 | OCCURRENCE-CODE-04 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP143-0003 | |||
| 537 | CIP144 | OCCURRENCE-CODE-05 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP144-0001 |
| 538 | CIP144 | OCCURRENCE-CODE-05 | Required if reported on the claim. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP144-0002 | |||
| 539 | CIP144 | OCCURRENCE-CODE-05 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP144-0003 | |||
| 540 | CIP145 | OCCURRENCE-CODE-06 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP145-0001 |
| 541 | CIP145 | OCCURRENCE-CODE-06 | Required if reported on the claim. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP145-0002 | |||
| 542 | CIP145 | OCCURRENCE-CODE-06 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP145-0003 | |||
| 543 | CIP146 | OCCURRENCE-CODE-07 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP146-0001 |
| 544 | CIP146 | OCCURRENCE-CODE-07 | Required if reported on the claim. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP146-0002 | |||
| 545 | CIP146 | OCCURRENCE-CODE-07 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP146-0003 | |||
| 546 | CIP147 | OCCURRENCE-CODE-08 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP147-0001 |
| 547 | CIP147 | OCCURRENCE-CODE-08 | Required if reported on the claim. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP147-0002 | |||
| 548 | CIP147 | OCCURRENCE-CODE-08 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP147-0003 | |||
| 549 | CIP148 | OCCURRENCE-CODE-09 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP148-0001 |
| 550 | CIP148 | OCCURRENCE-CODE-09 | Required if reported on the claim. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP148-0002 | |||
| 551 | CIP148 | OCCURRENCE-CODE-09 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP148-0003 | |||
| 552 | CIP149 | OCCURRENCE-CODE-10 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP149-0001 |
| 553 | CIP149 | OCCURRENCE-CODE-10 | Required if reported on the claim. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP149-0002 | |||
| 554 | CIP149 | OCCURRENCE-CODE-10 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP149-0003 | |||
| 555 | CIP150 | OCCURRENCE-CODE-EFF-DATE-01 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP150-0001 | |
| 556 | CIP150 | OCCURRENCE-CODE-EFF-DATE-01 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP150-0002 | |||
| 557 | CIP150 | OCCURRENCE-CODE-EFF-DATE-01 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP150-0003 | |||
| 558 | CIP150 | OCCURRENCE-CODE-EFF-DATE-01 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP150-0004 | |||
| 559 | CIP150 | OCCURRENCE-CODE-EFF-DATE-01 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP150-0005 | |||
| 560 | CIP150 | OCCURRENCE-CODE-EFF-DATE-01 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP150-0006 | |||
| 561 | CIP151 | OCCURRENCE-CODE-EFF-DATE-02 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP151-0001 | |
| 562 | CIP151 | OCCURRENCE-CODE-EFF-DATE-02 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP151-0002 | |||
| 563 | CIP151 | OCCURRENCE-CODE-EFF-DATE-02 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP151-0003 | |||
| 564 | CIP151 | OCCURRENCE-CODE-EFF-DATE-02 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP151-0004 | |||
| 565 | CIP151 | OCCURRENCE-CODE-EFF-DATE-02 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP151-0005 | |||
| 566 | CIP151 | OCCURRENCE-CODE-EFF-DATE-02 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP151-0006 | |||
| 567 | CIP152 | OCCURRENCE-CODE-EFF-DATE-03 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP152-0001 | |
| 568 | CIP152 | OCCURRENCE-CODE-EFF-DATE-03 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP152-0002 | |||
| 569 | CIP152 | OCCURRENCE-CODE-EFF-DATE-03 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP152-0003 | |||
| 570 | CIP152 | OCCURRENCE-CODE-EFF-DATE-03 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP152-0004 | |||
| 571 | CIP152 | OCCURRENCE-CODE-EFF-DATE-03 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP152-0005 | |||
| 572 | CIP152 | OCCURRENCE-CODE-EFF-DATE-03 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP152-0006 | |||
| 573 | CIP153 | OCCURRENCE-CODE-EFF-DATE-04 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP153-0001 | |
| 574 | CIP153 | OCCURRENCE-CODE-EFF-DATE-04 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP153-0002 | |||
| 575 | CIP153 | OCCURRENCE-CODE-EFF-DATE-04 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP153-0003 | |||
| 576 | CIP153 | OCCURRENCE-CODE-EFF-DATE-04 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP153-0004 | |||
| 577 | CIP153 | OCCURRENCE-CODE-EFF-DATE-04 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP153-0005 | |||
| 578 | CIP153 | OCCURRENCE-CODE-EFF-DATE-04 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP153-0006 | |||
| 579 | CIP154 | OCCURRENCE-CODE-EFF-DATE-05 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP154-0001 | |
| 580 | CIP154 | OCCURRENCE-CODE-EFF-DATE-05 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP154-0002 | |||
| 581 | CIP154 | OCCURRENCE-CODE-EFF-DATE-05 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP154-0003 | |||
| 582 | CIP154 | OCCURRENCE-CODE-EFF-DATE-05 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP154-0004 | |||
| 583 | CIP154 | OCCURRENCE-CODE-EFF-DATE-05 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP154-0005 | |||
| 584 | CIP154 | OCCURRENCE-CODE-EFF-DATE-05 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP154-0006 | |||
| 585 | CIP155 | OCCURRENCE-CODE-EFF-DATE-06 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP155-0001 | |
| 586 | CIP155 | OCCURRENCE-CODE-EFF-DATE-06 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP155-0002 | |||
| 587 | CIP155 | OCCURRENCE-CODE-EFF-DATE-06 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP155-0003 | |||
| 588 | CIP155 | OCCURRENCE-CODE-EFF-DATE-06 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP155-0004 | |||
| 589 | CIP155 | OCCURRENCE-CODE-EFF-DATE-06 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP155-0005 | |||
| 590 | CIP155 | OCCURRENCE-CODE-EFF-DATE-06 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP155-0006 | |||
| 591 | CIP156 | OCCURRENCE-CODE-EFF-DATE-07 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP156-0001 | |
| 592 | CIP156 | OCCURRENCE-CODE-EFF-DATE-07 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP156-0002 | |||
| 593 | CIP156 | OCCURRENCE-CODE-EFF-DATE-07 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP156-0003 | |||
| 594 | CIP156 | OCCURRENCE-CODE-EFF-DATE-07 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP156-0004 | |||
| 595 | CIP156 | OCCURRENCE-CODE-EFF-DATE-07 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP156-0005 | |||
| 596 | CIP156 | OCCURRENCE-CODE-EFF-DATE-07 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP156-0006 | |||
| 597 | CIP157 | OCCURRENCE-CODE-EFF-DATE-08 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP157-0001 | |
| 598 | CIP157 | OCCURRENCE-CODE-EFF-DATE-08 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP157-0002 | |||
| 599 | CIP157 | OCCURRENCE-CODE-EFF-DATE-08 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP157-0003 | |||
| 600 | CIP157 | OCCURRENCE-CODE-EFF-DATE-08 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP157-0004 | |||
| 601 | CIP157 | OCCURRENCE-CODE-EFF-DATE-08 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP157-0005 | |||
| 602 | CIP157 | OCCURRENCE-CODE-EFF-DATE-08 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP157-0006 | |||
| 603 | CIP158 | OCCURRENCE-CODE-EFF-DATE-09 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP158-0001 | |
| 604 | CIP158 | OCCURRENCE-CODE-EFF-DATE-09 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP158-0002 | |||
| 605 | CIP158 | OCCURRENCE-CODE-EFF-DATE-09 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP158-0003 | |||
| 606 | CIP158 | OCCURRENCE-CODE-EFF-DATE-09 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP158-0004 | |||
| 607 | CIP158 | OCCURRENCE-CODE-EFF-DATE-09 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP158-0005 | |||
| 608 | CIP158 | OCCURRENCE-CODE-EFF-DATE-09 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP158-0006 | |||
| 609 | CIP159 | OCCURRENCE-CODE-EFF-DATE-10 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP159-0001 | |
| 610 | CIP159 | OCCURRENCE-CODE-EFF-DATE-10 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP159-0002 | |||
| 611 | CIP159 | OCCURRENCE-CODE-EFF-DATE-10 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP159-0003 | |||
| 612 | CIP159 | OCCURRENCE-CODE-EFF-DATE-10 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP159-0004 | |||
| 613 | CIP159 | OCCURRENCE-CODE-EFF-DATE-10 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP159-0005 | |||
| 614 | CIP159 | OCCURRENCE-CODE-EFF-DATE-10 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP159-0006 | |||
| 615 | CIP160 | OCCURRENCE-CODE-END-DATE-01 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP160-0001 | |
| 616 | CIP160 | OCCURRENCE-CODE-END-DATE-01 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP160-0002 | |||
| 617 | CIP160 | OCCURRENCE-CODE-END-DATE-01 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP160-0003 | |||
| 618 | CIP160 | OCCURRENCE-CODE-END-DATE-01 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP160-0004 | |||
| 619 | CIP160 | OCCURRENCE-CODE-END-DATE-01 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP160-0005 | |||
| 620 | CIP160 | OCCURRENCE-CODE-END-DATE-01 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP160-0006 | |||
| 621 | CIP161 | OCCURRENCE-CODE-END-DATE-02 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP161-0001 | |
| 622 | CIP161 | OCCURRENCE-CODE-END-DATE-02 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP161-0002 | |||
| 623 | CIP161 | OCCURRENCE-CODE-END-DATE-02 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP161-0003 | |||
| 624 | CIP161 | OCCURRENCE-CODE-END-DATE-02 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP161-0004 | |||
| 625 | CIP161 | OCCURRENCE-CODE-END-DATE-02 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP161-0005 | |||
| 626 | CIP161 | OCCURRENCE-CODE-END-DATE-02 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP161-0006 | |||
| 627 | CIP162 | OCCURRENCE-CODE-END-DATE-03 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP162-0001 | |
| 628 | CIP162 | OCCURRENCE-CODE-END-DATE-03 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP162-0002 | |||
| 629 | CIP162 | OCCURRENCE-CODE-END-DATE-03 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP162-0003 | |||
| 630 | CIP162 | OCCURRENCE-CODE-END-DATE-03 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP162-0004 | |||
| 631 | CIP162 | OCCURRENCE-CODE-END-DATE-03 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP162-0005 | |||
| 632 | CIP162 | OCCURRENCE-CODE-END-DATE-03 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP162-0006 | |||
| 633 | CIP163 | OCCURRENCE-CODE-END-DATE-04 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP163-0001 | |
| 634 | CIP163 | OCCURRENCE-CODE-END-DATE-04 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP163-0002 | |||
| 635 | CIP163 | OCCURRENCE-CODE-END-DATE-04 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP163-0003 | |||
| 636 | CIP163 | OCCURRENCE-CODE-END-DATE-04 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP163-0004 | |||
| 637 | CIP163 | OCCURRENCE-CODE-END-DATE-04 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP163-0005 | |||
| 638 | CIP163 | OCCURRENCE-CODE-END-DATE-04 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP163-0006 | |||
| 639 | CIP164 | OCCURRENCE-CODE-END-DATE-05 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP164-0001 | |
| 640 | CIP164 | OCCURRENCE-CODE-END-DATE-05 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP164-0002 | |||
| 641 | CIP164 | OCCURRENCE-CODE-END-DATE-05 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP164-0003 | |||
| 642 | CIP164 | OCCURRENCE-CODE-END-DATE-05 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP164-0004 | |||
| 643 | CIP164 | OCCURRENCE-CODE-END-DATE-05 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP164-0005 | |||
| 644 | CIP164 | OCCURRENCE-CODE-END-DATE-05 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP164-0006 | |||
| 645 | CIP165 | OCCURRENCE-CODE-END-DATE-06 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP165-0001 | |
| 646 | CIP165 | OCCURRENCE-CODE-END-DATE-06 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP165-0002 | |||
| 647 | CIP165 | OCCURRENCE-CODE-END-DATE-06 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP165-0003 | |||
| 648 | CIP165 | OCCURRENCE-CODE-END-DATE-06 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP165-0004 | |||
| 649 | CIP165 | OCCURRENCE-CODE-END-DATE-06 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP165-0005 | |||
| 650 | CIP165 | OCCURRENCE-CODE-END-DATE-06 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP165-0006 | |||
| 651 | CIP166 | OCCURRENCE-CODE-END-DATE-07 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP166-0001 | |
| 652 | CIP166 | OCCURRENCE-CODE-END-DATE-07 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP166-0002 | |||
| 653 | CIP166 | OCCURRENCE-CODE-END-DATE-07 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP166-0003 | |||
| 654 | CIP166 | OCCURRENCE-CODE-END-DATE-07 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP166-0004 | |||
| 655 | CIP166 | OCCURRENCE-CODE-END-DATE-07 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP166-0005 | |||
| 656 | CIP166 | OCCURRENCE-CODE-END-DATE-07 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP166-0006 | |||
| 657 | CIP167 | OCCURRENCE-CODE-END-DATE-08 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP167-0001 | |
| 658 | CIP167 | OCCURRENCE-CODE-END-DATE-08 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP167-0002 | |||
| 659 | CIP167 | OCCURRENCE-CODE-END-DATE-08 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP167-0003 | |||
| 660 | CIP167 | OCCURRENCE-CODE-END-DATE-08 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP167-0004 | |||
| 661 | CIP167 | OCCURRENCE-CODE-END-DATE-08 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP167-0005 | |||
| 662 | CIP167 | OCCURRENCE-CODE-END-DATE-08 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP167-0006 | |||
| 663 | CIP168 | OCCURRENCE-CODE-END-DATE-09 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP168-0001 | |
| 664 | CIP168 | OCCURRENCE-CODE-END-DATE-09 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP168-0002 | |||
| 665 | CIP168 | OCCURRENCE-CODE-END-DATE-09 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP168-0003 | |||
| 666 | CIP168 | OCCURRENCE-CODE-END-DATE-09 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP168-0004 | |||
| 667 | CIP168 | OCCURRENCE-CODE-END-DATE-09 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP168-0005 | |||
| 668 | CIP168 | OCCURRENCE-CODE-END-DATE-09 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP168-0006 | |||
| 669 | CIP169 | OCCURRENCE-CODE-END-DATE-10 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP169-0001 | |
| 670 | CIP169 | OCCURRENCE-CODE-END-DATE-10 | Value must be a valid date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP169-0002 | |||
| 671 | CIP169 | OCCURRENCE-CODE-END-DATE-10 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP169-0003 | |||
| 672 | CIP169 | OCCURRENCE-CODE-END-DATE-10 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP169-0004 | |||
| 673 | CIP169 | OCCURRENCE-CODE-END-DATE-10 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP169-0005 | |||
| 674 | CIP169 | OCCURRENCE-CODE-END-DATE-10 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP169-0006 | |||
| 675 | CIP170 | BIRTH-WEIGHT-GRAMS | The weight of a newborn at time of birth in grams (applicable to newborns only). | Conditional | Required for a claim involving child birth | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP170-0001 | |
| 676 | CIP171 | PATIENT-CONTROL-NUM | A patient's unique number assigned by the provider agency during claim submission, which identifies the client or the client’s episode of service within the provider’s system to facilitate retrieval of individual financial and clinical records and posting of payment | Conditional | Must be numeric (0-9) and/or alphabetic (A-Z). Special characters are invalid entries | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP171-0001 | |
| 677 | CIP172 | ELIGIBLE-LAST-NAME | The last name of the individual to whom the services were provided. (The patients name should be captured as it appears on the claim record, it does not need to be the same as it appears on the eligibility file. The MSIS-IDENTIFICATION-NUM will be used to associate a claim record with the appropriate eligibility data.) | Required | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP172-0001 | |
| 678 | CIP172 | ELIGIBLE-LAST-NAME | When populating the eligible person’s name on T-MSIS Claim Files, use the patient’s name from the claim transaction rather than the eligible person’s name from the T-MSIS Eligible File. | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP172-0002 | |||
| 679 | CIP173 | ELIGIBLE-FIRST-NAME | The first name of the individual to whom the services were provided.(The patients name should be captured as it appears on the claim record, it does not need to be the same as it appears on the eligibility file. The MSIS-IDENTIFICATION-NUM will be used to associate a claim record with the appropriate eligibility data.) | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP173-0001 | |
| 680 | CIP173 | ELIGIBLE-FIRST-NAME | When populating the eligible person’s name on T-MSIS Claim Files, use the patient’s name from the claim transaction rather than the eligible person’s name from the T-MSIS Eligible File. | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP173-0002 | |||
| 681 | CIP174 | ELIGIBLE-MIDDLE-INIT | The middle initial of the individual to whom the services were provided. (The patients name should be captured as it appears on the claim record, it does not need to be the same as it appears on the eligibility file. The MSIS-IDENTIFICATION-NUM will be used to associate a claim record with the appropriate eligibility data.) | Conditional | Value must be an alphabetic character, or a blank (A-Z, a-z, ) | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP174-0001 | |
| 682 | CIP174 | ELIGIBLE-MIDDLE-INIT | Leave blank if not available. When populating the eligible person’s name on T-MSIS Claim Files, use the patient’s name from the claim transaction rather than the eligible person’s name from the T-MSIS Eligible File. |
9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP174-0002 | |||
| 683 | CIP175 | DATE-OF-BIRTH | Date of birth of the individual to whom the services were provided. | Required | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP175-0001 | |
| 684 | CIP175 | DATE-OF-BIRTH | Value must be a valid date | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP175-0002 | |||
| 685 | CIP175 | DATE-OF-BIRTH | The numeric form for days and months from 1 to 9 must have a zero as the first digit. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP175-0003 | |||
| 686 | CIP175 | DATE-OF-BIRTH | The patient’s date of birth shall be reported in numeric form as follows – 2 digit month, 2 digit day, and 4 digit year | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP175-0004 | |||
| 687 | CIP175 | DATE-OF-BIRTH | A patient's age should not be greater than 112 years. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP175-0005 | |||
| 688 | CIP176 | HEALTH-HOME-PROV-IND | This code indicates whether the claim is submitted by a provider or provider group enrolled in the Health Home care model. Health home providers provide service for patients with chronic illnesses. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 8 Not Applicable 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP176-0001 |
| 689 | CIP176 | HEALTH-HOME-PROV-IND | If a state has not yet begun collecting this information, HEALTH-HOME-PROV-IND, this field should be defaulted to the value “8.” | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP176-0002 | |||
| 690 | CIP176 | HEALTH-HOME-PROV-IND | If there is a HEALTH-HOME-ENTITY-NAME then HEALTH-HOME-PROV-IND must indicate yes. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP176-0003 | |||
| 691 | CIP176 | HEALTH-HOME-PROV-IND | States should not submit claim records for an eligible individual that indicate the claim was submitted by a provider or provider group enrolled in a health home model if the eligible individual is not enrolled in the health home program. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP176-0004 | |||
| 692 | CIP176 | HEALTH-HOME-PROV-IND | States that do not specify an eligible individual's health home provider number, if applicable, should not report claims that indicate the claim is submitted by a provider or provider group enrolled in the health home model. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP176-0005 | |||
| 693 | CIP177 | WAIVER-TYPE | Code for specifying waiver type under which the eligible individual is covered during the month and receiving services/under which claim is submitted. | Conditional | Enter the WAIVER-TYPE assigned | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP177-0001 |
| 694 | CIP177 | WAIVER-TYPE | Value must correspond to associated WAIVER-ID | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP177-0002 | |||
| 695 | CIP177 | WAIVER-TYPE | An ineligible individual cannot have a category for federal reimbursement for Medicaid or CHIP (CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT <> 01,02) | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP177-0003 | |||
| 696 | CIP178 | WAIVER-ID | Field specifying the waiver or demonstration which authorized payment for a claim. These IDs must be the approved, full federal waiver ID number assigned during the state submission and CMS approval process. The categories of demonstration and waiver programs include: 1915(b)(1); 1915(b)(2); 1915(b)(3), and 1915(b)(4) managed care waivers; 1915(c) home and community based services waivers; combined 1915(b) and 1915(c) managed home and community based services waivers and 1115 demonstrations. | Conditional | Valid values are supplied by the state. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ||
| 697 | CIP178 | WAIVER-ID | Report the full federal waiver identifier. | 11/9/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP178-0002 | |||
| 698 | CIP178 | WAIVER-ID | If the goods & services rendered do not fall under a waiver, leave this field blank. | 11/9/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP178-0004 | |||
| 699 | CIP178 | WAIVER-ID | If there's a waiver type, there should be a corresponding waiver id. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP178-0005 | |||
| 700 | CIP179 | BILLING-PROV-NUM | A unique identification number assigned by the state to a provider or capitation plan. This should represent the entity billing for the service. | Required | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP179-0001 |
| 701 | CIP179 | BILLING-PROV-NUM | If value is invalid, record it exactly as it appears in the state system. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP179-0002 | |||
| 702 | CIP179 | BILLING-PROV-NUM | For encounter records (TYPE-OF-CLAIM = 3, C, W), this represents the entity billing (or reporting) to the managed care plan (See PLAN-ID-NUMBER for reporting capitation plan-ID). Capitation PLAN-ID should be used in this field only for capitation payments (TYPE-OF-SERVICE = 119, 120, 122) | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP179-0003 | |||
| 703 | CIP179 | BILLING-PROV-NUM | Billing Provider must not be an individual or group on inpatient hospital claims. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP179-0004 | |||
| 704 | CIP180 | BILLING-PROV-NPI-NUM | The National Provider ID (NPI) of the billing entity responsible for billing a patient for healthcare services. The billing provider can also be servicing, referring, or prescribing provider. Can be admitting provider except for Long Term Care. |
Required | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP180-0001 |
| 705 | CIP180 | BILLING-PROV-NPI-NUM | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP180-0002 | |||
| 706 | CIP180 | BILLING-PROV-NPI-NUM | For encounter records (TYPE-OF-CLAIM = 3, C, W), the BILLIN-PROV-NPI-NUM field should be populated with the NPI of the provider or entity billing (or reporting) to the managed care plan. For financial transactions (i.e., expenditure transactions or recoupments of previously made expenditures that do not flow through the usual claim adjudication/adjustment process or encounter record reporting process), the BILLIN-PROV-NPI-NUM field should be populated with the NPI of the provider or entity to which the financial transaction was addressed, unless the transaction is a payment/recoupment made-to/received-from a managed care plan, in which case the BILLING-PROV-NPI-NUM should be left blank. For financial transactions with managed care plans, the plan's ID should be reported in the PLAN-ID-NUMBER field and the BILLING-PROV-NPI-NUM should be left blank. |
2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP180-0003 | |||
| 707 | CIP180 | BILLING-PROV-NPI-NUM | Billing Provider must be enrolled | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP180-0005 | |||
| 708 | CIP180 | BILLING-PROV-NPI-NUM | Billing Provider must not be an individual or group on inpatient hospital claims. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP180-0006 | |||
| 709 | CIP181 | BILLING-PROV-TAXONOMY | For CLAIMIP and CLAIMLT files, the taxonomy code for the institution billing for the beneficiary. |
Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP181-0001 |
| 710 | CIP181 | BILLING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP181-0002 | |||
| 711 | CIP181 | BILLING-PROV-TAXONOMY | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122) | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP181-0003 | |||
| 712 | CIP182 | BILLING-PROV-TYPE | A code describing the type of entity billing for the service. | Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP182-0001 |
| 713 | CIP182 | BILLING-PROV-TYPE | For encounter records (TYPE-OF-CLAIM= 3, C, W), this represents the entity billing (or reporting) to the Managed Care Plan (see PLAN-ID-NUMBER for reporting capitation plan-ID). CAPITATION-PLAN-ID should be used in this field only for premium payments (TYPE-OF-SERVICE=119, 120, 122). | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP182-0002 | |||
| 714 | CIP182 | BILLING-PROV-TYPE | The state should use Taxonomy Crosswalk.pdf to crosswalk state codes to CMS codes | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP182-0003 | |||
| 715 | CIP183 | BILLING-PROV-SPECIALTY | This code describes the area of specialty for the billing provider. | Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP183-0001 |
| 716 | CIP184 | ADMITTING-PROV-NPI-NUM | The National Provider ID (NPI) of the doctor responsible for admitting a patient to a hospital or other inpatient health facility. | Conditional | Valid characters include only numbers (0-9) | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP184-0001 | |
| 717 | CIP184 | ADMITTING-PROV-NPI-NUM | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP184-0002 | ||
| 718 | CIP184 | ADMITTING-PROV-NPI-NUM | IF TYPE-OF-SERVICE= "119", "120", "121", or "122", then ADMITTING-PROV-NPI-NUM should be blank. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP184-0004 | |||
| 719 | CIP185 | ADMITTING-PROV-NUM | The Medicaid ID of the doctor responsible for admitting a patient to a hospital or other inpatient health facility. | Required | A list of valid codes must be supplied by the state prior to submission of any file data. | Valid values are supplied by the state. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP185-0001 |
| 720 | CIP185 | ADMITTING-PROV-NUM | If value is invalid, record it exactly as it appears in the state system | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP185-0002 | |||
| 721 | CIP185 | ADMITTING-PROV-NUM | Note: Once a national provider ID numbering system is in place, the national number should be used. If the State’s legacy ID number is also available then that number can be entered in this field. |
2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP185-0003 | |||
| 722 | CIP186 | ADMITTING-PROV-SPECIALTY | This code describes the area of specialty for the admitting provider. | Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP186-0001 |
| 723 | CIP187 | ADMITTING-PROV-TAXONOMY | The taxonomy code for the admitting provider. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP187-0001 |
| 724 | CIP187 | ADMITTING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP187-0002 | |||
| 725 | CIP188 | ADMITTING-PROV-TYPE | A code describing the type of admitting provider. If the state uses state-specific codes, they should map their internal codes to the CMS standard list provided. |
Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP188-0001 |
| 726 | CIP189 | REFERRING-PROV-NUM | A code describing the type of provider (i.e. doctor) who referred the patient. If the state uses state-specific codes, they should map their internal codes to the CMS standard list provided. |
Conditional | A list of valid codes must be supplied by the state prior to submission of any file data. | Valid values are supplied by the state. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP189-0001 |
| 727 | CIP189 | REFERRING-PROV-NUM | If Value is invalid, record it exactly as it appears in the State system. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP189-0002 | |||
| 728 | CIP189 | REFERRING-PROV-NUM | If the referring provider number is not available, but the physician’s Drug Enforcement Agency (DEA) ID is on the State file, then the State should use the DEA ID for this data element. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP189-0003 | |||
| 729 | CIP190 | REFERRING-PROV-NPI-NUM | The National Provider ID (NPI) of the provider who recommended the servicing provider to the patient. | Conditional | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP190-0001 |
| 730 | CIP190 | REFERRING-PROV-NPI-NUM | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP190-0002 | |||
| 731 | CIP190 | REFERRING-PROV-NPI-NUM | The field should be blank if the transaction is for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122). | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP190-0003 | |||
| 732 | CIP191 | REFERRING-PROV-TAXONOMY | For CLAIMIP and CLAIMLT files, the taxonomy code for the referring provider. | NA | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP191-0001 |
| 733 | CIP191 | REFERRING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP191-0002 | |||
| 734 | CIP191 | REFERRING-PROV-TAXONOMY | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122) | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP191-0003 | |||
| 735 | CIP192 | REFERRING-PROV-TYPE | A code describing the type of provider (i.e. doctor) who referred the patient. If the state uses state-specific codes, they should map their internal codes to the CMS standard list provided. |
NA | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP192-0001 |
| 736 | CIP193 | REFERRING-PROV-SPECIALTY | This code indicates the area of specialty of the referring provider. | NA | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP193-0001 |
| 737 | CIP194 | DRG-OUTLIER-AMT | The additional payment on a claim that is associated with either a cost outlier or length of stay outlier. Outlier payments compensate hospitals paid on a fixed amount per Medicare "diagnosis related group" discharge with extra dollars for patient stays that substantially exceed the typical requirements for patient stays in the same DRG category. |
Conditional | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP194-0001 | |
| 738 | CIP194 | DRG-OUTLIER-AMT | If there is an outlier-code then there must be an outlier amount. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP194-0002 | |||
| 739 | CIP195 | DRG-REL-WEIGHT | The relative weight for the DRG on the claim. Each year CMS assigns a relative weight to each DRG. These weights indicate the relative costs for treating patients during the prior year. The national average charge for each DRG is compared to the overall average. This ratio is published annually in the Federal Register for each DRG. A DRG with a weight of 2.0000 means that charges were historically twice the average; a DRG with a weight of 0.5000 was half the average. | Conditional | State specific | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP195-0001 | |
| 740 | CIP196 | MEDICARE-HIC-NUM | Health Insurance Claim (HIC) Number as it appears on the patient’s Medicare card. |
Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9) |
4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP196-0001 | |
| 741 | CIP196 | MEDICARE-HIC-NUM | "Railroad Retirees" - Railroad Retirement Board (RRB) HIC numbers generally have two alpha characters as a prefix to the number. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP196-0002 | |||
| 742 | CIP196 | MEDICARE-HIC-NUM | If this is a crossover Medicare claim, the Bene must have a MEDICARE-HIC-Num. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP196-0003 | |||
| 743 | CIP196 | MEDICARE-HIC-NUM | States should not submit records for an eligible individual where the eligible's Medicare HIC Number does not match in the associated claim record, if applicable. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP196-0004 | |||
| 744 | CIP196 | MEDICARE-HIC-NUM | Claims records for an eligible individual should not indicate a valid Medicare HIC number, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP196-0005 | |||
| 745 | CIP197 | OUTLIER-CODE | This code indicates the Type of Outlier Code or DRG Source. | Conditional | Value must be equal to a valid value. | 00 No Outlier 01 Day Outlier 02 Cost Outlier 06 Valid DRG Received from the intermediary 07 CMS Developed DRG 08 CMS Developed DRG Using Patient Status Code 09 Not Group able 10 Composite of cost outliers |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP197-0001 |
| 746 | CIP197 | OUTLIER-CODE | If there is an outlier-amount, then there is an outlier-code. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP197-0002 | |||
| 747 | CIP198 | OUTLIER-DAYS | This field specifies the number of days paid as outliers under Prospective Payment System (PPS) and the days over the threshold for the DRG | Conditional | Must be numeric | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP198-0001 | |
| 748 | CIP198 | OUTLIER-DAYS | Used in conjunction with OUTLIER-CODE field. The field identifies two mutually exclusive conditions. The first, for PPS providers (codes 0, 1, and 2), classifies stays of exceptional cost or length (outliers). The second, for non-PPS providers (codes 6, 7, 8, and 9), denotes the source for developing the DRG. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP198-0002 | |||
| 749 | CIP198 | OUTLIER-DAYS | If the unit of the outlier is days, then the outlier-days should not be missing. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP198-0003 | |||
| 750 | CIP199 | PATIENT-STATUS | A code indicating the Patients status as of the ENDING-DATE-OF-SERVICE. Values used are from UB-04. This is also referred to as DISCHARGE-STATUS. | Required | Value must be equal to a valid value. | http://www.cms.hhs.gov/MLNMattersArticles/downloads/SE0801.pdf | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP199-0001 |
| 751 | CIP199 | PATIENT-STATUS | If the date of death is valued, then the patient status should indicate that the patient has expired. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP199-0002 | |||
| 752 | CIP199 | PATIENT-STATUS | Obtain the Patient Discharge Status valid value set which is published in the UB-04 Data Specifications Manual. To order the current edition of the UB-04 Data Specifications Manual go to: http://www.nubc.org/subscriber/index.dhtml American Hospital Association 155 North Wacker Drive, Suite 400 Chicago, IL 60606 Phone: 312-422-3000 Fax: 312-422-4500 |
To order the current edition of the UB-04 Data Specifications Manual go to: http://www.nubc.org/subscriber/index.dhtml American Hospital Association 155 North Wacker Drive, Suite 400 Chicago, IL 60606 Phone: 312-422-3000 Fax: 312-422-4500 |
9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00003 | CIP199-0003 | ||
| 753 | CIP201 | BMI | A key index for relating a person's body weight to their height. The body mass index (BMI) is a person's weight in kilograms (kg) divided by their height in meters (m) squared. | Optional | SI units: BMI = mass (kg) / (height(m))2 Imperial/US Customary units: BMI = mass (lb) * 703/ (height(in))2 BMI = mass (lb) * 4.88/ (height(ft))2 BMI = mass (st) * 9840/ (height(in))2 |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP201-0001 | |
| 754 | CIP201 | BMI | CMS is relieving states of the responsibility to: (a) Provide these data. (b) Document a mitigation plan in the Source-to-Target-Mapping Matrix Addendum B whenever the data elements cannot be populated all of the time. However if a state determines that it can populate one or more of these fields and wishes to do so, they are encouraged to do so and will not incur any Addendum B mitigation plan documentation expectations. |
9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP201-0002 | |||
| 755 | CIP202 | REMITTANCE-NUM | The Remittance Advice Number is a sequential number that identifies the current Remittance Advice (RA) produced for a provider. The number is incremented by one each time a new RA is generated. The first five (5) positions are Julian date YYDDD format. The RA is the detailed explanation of the reason for the payment amount. The RA number is not the check number. | Required | Limit characters to alphabet (A-Z, a-z), numerals (0-9).. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP202-0001 | |
| 756 | CIP202 | REMITTANCE-NUM | Value must not be null | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP202-0002 | |||
| 757 | CIP202 | REMITTANCE-NUM | If there is a remittance date, then there must also be a remittance number. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP202-0003 | |||
| 758 | CIP203 | SPLIT-CLAIM-IND | An indicator that denotes that claims in excess of a pre-determined number of claim lines (threshold determined by the individual state) will be split during processing | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP203-0001 |
| 759 | CIP203 | SPLIT-CLAIM-IND | If the claim has been split, the Transaction Handling Code indicator will indicate a Split Payment and Remittance (1000 BPR01 = U). | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP203-0002 | |||
| 760 | CIP204 | BORDER-STATE-IND | This code indicates whether an individual received services or equipment across state borders. (The provider location is out of state, but for payment purposes the provider is treated as an in-state provider.) | Conditional | Value must be equal to a valid value. | 0 No 1 Yes |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP204-0001 |
| 761 | CIP206 | BENEFICIARY-COINSURANCE-AMOUNT | The amount of money the beneficiary paid towards coinsurance. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP206-0001 | |
| 762 | CIP206 | BENEFICIARY-COINSURANCE-AMOUNT | If no coinsurance is applicable enter 0.00 | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP206-0002 | |||
| 763 | CIP206 | BENEFICIARY-COINSURANCE-AMOUNT | If it is unknown whether coinsurance was paid, 9 fill | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP206-0003 | |||
| 764 | CIP207 | BENEFICIARY-COINSURANCE-DATE-PAID | The date the beneficiary paid the coinsurance amount. | Conditional | Date format should be CCYYMMDD (National Data Standard) | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP207-0001 | |
| 765 | CIP207 | BENEFICIARY-COINSURANCE-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP207-0002 | |||
| 766 | CIP207 | BENEFICIARY-COINSURANCE-DATE-PAID | If no coinsurance is applicable, 8-fill | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP207-0003 | |||
| 767 | CIP208 | BENEFICIARY-COPAYMENT-AMOUNT | The amount of money the beneficiary paid towards a copayment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP208-0001 | |
| 768 | CIP208 | BENEFICIARY-COPAYMENT-AMOUNT | If no copayment is applicable enter 0.00 | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP208-0002 | |||
| 769 | CIP209 | BENEFICIARY-COPAYMENT-DATE-PAID | The date the beneficiary paid the copayment amount. | Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP209-0001 | |
| 770 | CIP209 | BENEFICIARY-COPAYMENT-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP209-0002 | |||
| 771 | CIP209 | BENEFICIARY-COPAYMENT-DATE-PAID | If no coinsurance is applicable, 8-fill | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP209-0003 | |||
| 772 | CIP210 | BENEFICIARY-DEDUCTIBLE-AMOUNT | The amount of money the beneficiary paid towards an annual deductible. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP210-0001 | |
| 773 | CIP210 | BENEFICIARY-DEDUCTIBLE-AMOUNT | If no deductible is applicable enter 0.00 | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP210-0002 | |||
| 774 | CIP210 | BENEFICIARY-DEDUCTIBLE-AMOUNT | If it is unknown whether a deductible was paid, 9 fill | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP210-0003 | |||
| 775 | CIP211 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | The date the beneficiary paid the deductible amount. | Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP211-0001 | |
| 776 | CIP211 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP211-0002 | |||
| 777 | CIP211 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | If no coinsurance is applicable, 8-fill | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP211-0003 | |||
| 778 | CIP212 | CLAIM-DENIED-INDICATOR | An indicator to identify a claim that the state refused pay in its entirety. | Conditional | Value must be equal to a valid value. | 0 Denied: The payment of claim in its entirety was denied by the state. 1 Not Denied: The state paid some or all of the claim. |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP212-0001 |
| 779 | CIP212 | CLAIM-DENIED-INDICATOR | It is expected that states will submit all denied claims to CMS. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP212-0002 | |||
| 780 | CIP212 | CLAIM-DENIED-INDICATOR | If the Type of Claim indicates the claim was denied, then this indicator must also indicate the claim was denied. | 10/10/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP212-0003 | |||
| 781 | CIP213 | COPAY-WAIVED-IND | An indicator signifying that the copay was waived by the provider. | Optional | Value must be equal to a valid value. | 0 Not Waived: The provider did not waive the beneficiary’s copayment 1 Waived: The provider waived the beneficiary’s copayment 8 Not Applicable: The benefit plan does not have a copay in this circumstance |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP213-0001 |
| 782 | CIP214 | HEALTH-HOME-ENTITY-NAME | A free-form text field to indicate the health home program that authorized payment for the service on the claim. The name entered should be the name that the state uses to uniquely identify the team. A “Health Home Entity” can be a designated provider (e.g., physician, clinic, behavioral health organization), a health team which links to a designated provider, or a health team (physicians, nurses, behavioral health professionals). Because an identification numbering schema has not been established, the entities’ names are being used instead. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP214-0001 |
| 783 | CIP214 | HEALTH-HOME-ENTITY-NAME | States should not submit records for an eligible individual where the eligible's health home entity name does not match in the associated claim record, if applicable. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP214-0002 | |||
| 784 | CIP216 | THIRD-PARTY-COINSURANCE-AMOUNT-PAID | The amount of money paid by a third party on behalf of the beneficiary towards coinsurance on the claim or claim line item | Optional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP216-0001 | |
| 785 | CIP217 | THIRD-PARTY-COINSURANCE-DATE-PAID | The date the third party paid the coinsurance amount | Optional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP217-0001 | |
| 786 | CIP217 | THIRD-PARTY-COINSURANCE-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP217-0002 | |||
| 787 | CIP218 | THIRD-PARTY-COPAYMENT-AMOUNT-PAID | The amount the third party paid the copayment amount. | Optional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP218-0001 | |
| 788 | CIP218 | THIRD-PARTY-COPAYMENT-AMOUNT-PAID | If the field is not applicable, 8-fill | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP218-0002 | |||
| 789 | CIP219 | THIRD-PARTY-COPAYMENT-DATE-PAID | The date the third party paid the copayment amount. | Optional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP219-0001 | |
| 790 | CIP219 | THIRD-PARTY-COPAYMENT-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP219-0002 | |||
| 791 | CIP220 | MEDICAID-AMOUNT-PAID-DSH | The amount included in the TOT-MEDICAID-PAID-AMT that is attributable to a Disproportionate Share Hospital (DSH) payment, when the state makes DSH payments by claim. |
Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP220-0001 | |
| 792 | CIP221 | HEALTH-HOME-PROVIDER-NPI | The National Provider ID (NPI) of the health home provider. | Conditional | The value must be a valid NPI | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP221-0001 |
| 793 | CIP221 | HEALTH-HOME-PROVIDER-NPI | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP221-0002 | |||
| 794 | CIP222 | MEDICARE-BENEFICIARY-IDENTIFIER | The individual’s Medicare Beneficiary Identifier (MBI) Identification Number. Note: MBI replaces the HICN with an entirely new Medicare Beneficiary Identifier (MBI) for purposes of provider billing, if applicable. CMS interfaces with non-payment exchange partners would remain HICN-based, while interfaces with payment partners would use the new MBI. |
NA | Valid characters in the text string are limited to alpha characters (A-Z, a-z) and numbers (0-9) | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP222-0001 | |
| 795 | CIP222 | MEDICARE-BENEFICIARY-IDENTIFIER | If individual is NOT enrolled in Medicare, 8-fill field | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP222-0002 | |||
| 796 | CIP222 | MEDICARE-BENEFICIARY-IDENTIFIER | Field should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files) until such time as the Medicare Beneficiary Identifier is implemented (no target date has been established). | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP222-0003 | |||
| 797 | CIP223 | OPERATING-PROV-TAXONOMY | The Provider Taxonomy of the provider who performed an operation on the patient. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP223-0001 |
| 798 | CIP223 | OPERATING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion. |
2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP223-0002 | |||
| 799 | CIP223 | OPERATING-PROV-TAXONOMY | Left-fill unused bytes with spaces. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP223-0003 | |||
| 800 | CIP224 | UNDER-DIRECTION-OF-PROV-NPI | The National Provider ID (NPI) of the provider who directed the care of a patient that another provider administered. | NA | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ||
| 801 | CIP224 | UNDER-DIRECTION-OF-PROV-NPI | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP224-0002 | |||
| 802 | CIP224 | UNDER-DIRECTION-OF-PROV-NPI | Field should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). This data element is a duplicate of the “Under-Supervision-of-Prov-NPI” field and as such do not need to be populated. | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP224-0003 | |||
| 803 | CIP225 | UNDER-DIRECTION-OF-PROV-TAXONOMY | The Provider Taxonomy of the provider who directed the care of a patient that another provider administered. | NA | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP225-0001 |
| 804 | CIP225 | UNDER-DIRECTION-OF-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP225-0002 | |||
| 805 | CIP225 | UNDER-DIRECTION-OF-PROV-TAXONOMY | Left-fill unused bytes with spaces | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP225-0003 | |||
| 806 | CIP225 | UNDER-DIRECTION-OF-PROV-TAXONOMY | Field should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). This data element is a duplicate of the “Under-Supervision-of-Prov-Taxonomy” field and as such do not need to be populated. | 9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP225-0004 | |||
| 807 | CIP226 | UNDER-SUPERVISION-OF-PROV-NPI | The National Provider ID (NPI) of the provider who supervised another provider. | NA | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | ||
| 808 | CIP226 | UNDER-SUPERVISION-OF-PROV-NPI | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP226-0002 | |||
| 809 | CIP227 | UNDER-SUPERVISION-OF-PROV-TAXONOMY | The Provider Taxonomy of the provider who supervised another provider. | NA | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP227-0001 |
| 810 | CIP227 | UNDER-SUPERVISION-OF-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP227-0002 | |||
| 811 | CIP227 | UNDER-SUPERVISION-OF-PROV-TAXONOMY | Left-fill unused bytes with spaces | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP227-0003 | |||
| 812 | CIP228 | MEDICARE-PAID-AMT | The amount paid by Medicare on this claim or adjustment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP228-0001 | |
| 813 | CIP228 | MEDICARE-PAID-AMT | If the service was covered by Medicare but Medicare had no liability for the bill, zero-fill. MEDICARE-PAID-AMT should reflect the actual amount paid by Medicare. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP228-0002 | |||
| 814 | CIP228 | MEDICARE-PAID-AMT | For claims where Medicare payment is only available at the header level, report the entire payment amount the T-MSIS record corresponding to the line item with the highest charge. Zero fill Medicare Amount Paid on all other T-MSIS records created from the original claim. | 2/25/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP228-0003 | |||
| 815 | CIP228 | MEDICARE-PAID-AMT | Claims records for an eligible individual should not indicate Medicare paid any amount on the claim, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP228-0004 | |||
| 816 | CIP229 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP229-0001 | |
| 817 | CIP229 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP229-0002 | |||
| 818 | CIP289 | PROV-LOCATION-ID | A code to uniquely identify the geographic location where the provider’s services were performed. The value should correspond to an active value in the PROV-LOCATION-ID field in the provider subject area. | Required | 11/9/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP289-0001 | ||
| 819 | CIP289 | PROV-LOCATION-ID | For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. | 11/9/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP289-0002 | |||
| 820 | CIP230 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | CLAIMIP | CLAIM-HEADER-RECORD-IP-CIP00002 | CIP230-0001 | |||
| 821 | CIP231 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the CLAIM-HEADER-RECORD-IP record segment is CIP00002 | Required | Value must be equal to a valid value. | CIP00003 - CLAIM-LINE-RECORD-IP | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP231-0001 |
| 822 | CIP231 | RECORD-ID | Must be populated on every record | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP231-0002 | |||
| 823 | CIP231 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP231-0003 | |||
| 824 | CIP232 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP232-0001 |
| 825 | CIP232 | SUBMITTING-STATE | Must be populated on every record. | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP232-0002 | |||
| 826 | CIP232 | SUBMITTING-STATE | Value must be numeric |
4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP232-0003 | |||
| 827 | CIP232 | SUBMITTING-STATE | SUBMITTING-STATE must be equal across all record segments for a given record. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP232-0004 | |||
| 828 | CIP233 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP233-0001 | |
| 829 | CIP233 | RECORD-NUMBER | Must be numeric | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP233-0002 | |||
| 830 | CIP233 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP233-0003 | |||
| 831 | CIP234 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Conditional | MSIS Identification Number must be reported | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP234-0001 | |
| 832 | CIP234 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state ID numbers must be supplied to CMS | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP234-0002 | |||
| 833 | CIP234 | MSIS-IDENTIFICATION-NUM | For TYPE-OF-CLAIM = 4 or D (lump sum adjustments), this field must begin with an ‘&’. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP234-0003 | |||
| 834 | CIP234 | MSIS-IDENTIFICATION-NUM | For SSN states, this field must contain the Eligible's Social Security Number. If the SSN is unknown and a temporary number is assigned, this field will contain that number. | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP234-0004 | |||
| 835 | CIP235 | ICN-ORIG | A unique number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies an original claim. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP235-0001 | |
| 836 | CIP235 | ICN-ORIG | Record the value exactly as it appears in the State system. Do not pad. | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP235-0002 | |||
| 837 | CIP235 | ICN-ORIG | This field should always be populated with the claim identification number assigned to the original paid/denied claim. This identification number should remain constant and be carried forward onto any adjustment claims. The intention is for this earliest claim identification number to be the link that ties the original claim and all adjustment claims together. | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP235-0003 | |||
| 838 | CIP235 | ICN-ORIG | This field should not be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP235-0004 | |||
| 839 | CIP236 | ICN-ADJ | A unique claim number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies the adjustment claim for an original transaction. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP236-0001 | |
| 840 | CIP236 | ICN-ADJ | Record the value exactly as it appears in the State system. Do not pad. | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP236-0002 | |||
| 841 | CIP236 | ICN-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP236-0003 | |||
| 842 | CIP237 | LINE-NUM-ORIG | A unique number to identify the transaction line number that is being reported on the original claim. | Required | Record the value exactly as it appears in the State system. Do not pad. This field should also be completed on adjustment claims to reflect the LINE-NUMBER of the INTERNAL-CONTROL-NUMBER on the claim that is being adjusted. | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP237-0001 | |
| 843 | CIP238 | LINE-NUM-ADJ | A unique number to identify the transaction line number that identifies the line number on the adjustment ICN. | Conditional | Record the value exactly as it appears in the state system. Do not pad | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP238-0001 | |
| 844 | CIP238 | LINE-NUM-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0. | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP238-0002 | |||
| 845 | CIP239 | LINE-ADJUSTMENT-IND | Code indicating type of adjustment record claim/encounter represents at claim detail level. | Conditional | Value must be equal to a valid value. | 0 Original Claim/Encounter 1 Void of a prior submission 2 Re-submittal 3 Credit Adjustment (negative supplemental) 4 Debit Adjustment (positive supplemental) 5 Credit Gross Adjustment. 6 Debit Gross Adjustment 9 Unknown |
11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP239-0001 |
| 846 | CIP239 | LINE-ADJUSTMENT-IND | If there is a line adjustment number, then there must be a line-adjustment indicator. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP239-0002 | |||
| 847 | CIP239 | LINE-ADJUSTMENT-IND | If there is a line adjustment reason, then there must be a line adjustment indicator. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP239-0003 | |||
| 848 | CIP240 | LINE-ADJUSTMENT-REASON-CODE | Claim adjustment reason codes communicate why a service line was paid differently than it was billed. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-adjustment-reason-codes/ | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP240-0001 |
| 849 | CIP240 | LINE-ADJUSTMENT-REASON-CODE | If there is no adjustment to a line, then there is no adjustment reason code. (Also see: CLAIM-PYMT-REM-CODE) | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP240-0002 | |||
| 850 | CIP241 | SUBMITTER-ID | The Submitter ID number is the value that identifies the provider/trading partner/clearing house organization to the state’s claim adjudication system. |
Conditional | Value must not be null | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP241-0001 | |
| 851 | CIP242 | CLAIM-LINE-STATUS | The claim line status codes identify the status of a specific detail claim line rather than the entire claim. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-codes/ | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP242-0001 |
| 852 | CIP243 | BEGINNING-DATE-OF-SERVICE | For services received during a single encounter with a provider, the date the service covered by this claim was received. For services involving multiple encounters on different days, or periods of care extending over two or more days, this would be the date on which the service covered by this claim began. For capitation premium payments, the date on which the period of coverage related to this payment began. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP243-0001 | |
| 853 | CIP243 | BEGINNING-DATE-OF-SERVICE | Value must be a valid date | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP243-0002 | |||
| 854 | CIP243 | BEGINNING-DATE-OF-SERVICE | The beginning date of service must occur before or be the same as the end of time period | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP243-0003 | |||
| 855 | CIP243 | BEGINNING-DATE-OF-SERVICE | Date must occur before or be the same as Ending Date of Service | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP243-0004 | |||
| 856 | CIP243 | BEGINNING-DATE-OF-SERVICE | Date must occur before or be the same as adjudication date. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP243-0005 | |||
| 857 | CIP243 | BEGINNING-DATE-OF-SERVICE | Date must occur on or before Date of Death. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP243-0006 | |||
| 858 | CIP243 | BEGINNING-DATE-OF-SERVICE | The beginning date of service must occur before the DATE-OF-BIRTH when the person is eligible as an unborn CHIP child or beginning date of service must occur on or after the DATE-OF-BIRTH when the person is eligible through Medicaid or is eligible as a non-unborn CHIP child . | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP243-0007 | |||
| 859 | CIP243 | BEGINNING-DATE-OF-SERVICE | A Medicaid claim record for an eligible individual, if applicable, cannot have a Beginning Date of Service after the eligible individual's Medicaid enrollment has ended. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP243-0008 | |||
| 860 | CIP243 | BEGINNING-DATE-OF-SERVICE | A CHIP claim record for an individual eligible for separate CHIP cannot have a Beginning Date of Service after the eligible individual's CHIP enrollment has ended. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP243-0009 | |||
| 861 | CIP244 | ENDING-DATE-OF-SERVICE | For services received during a single encounter with a provider, the date the service covered by this claim was received. For services involving multiple encounters on different days, or periods of care extending over two or more days, the date on which the service covered by this claim ended. For capitation premium payments, the date on which the period of coverage related to this payment ends/ended. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP244-0001 | |
| 862 | CIP244 | ENDING-DATE-OF-SERVICE | Value must be a valid date | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP244-0002 | |||
| 863 | CIP244 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must occur after or be the same as the BEGINNING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP244-0003 | |||
| 864 | CIP244 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must be on or before the ADJUDICATION-DATE. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP244-0004 | |||
| 865 | CIP244 | ENDING-DATE-OF-SERVICE | Date must occur on or before the Date of Death. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP244-0005 | |||
| 866 | CIP244 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must be on or after DATE-OF-BIRTH | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP244-0006 | |||
| 867 | CIP244 | ENDING-DATE-OF-SERVICE | Date must occur before or be the same as End of Time Period. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP244-0007 | |||
| 868 | CIP245 | REVENUE-CODE | A code which identifies a specific accommodation, ancillary service or billing calculation (as defined by UB-04 Billing Manual). | Required | Only valid codes as defined by the “National Uniform Billing Committee” should be used. | Revenue code is a data set that health care providers or insurers usually pay for to use. These values will change annually. | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP245-0001 |
| 869 | CIP245 | REVENUE-CODE | Enter all UB-04 Revenue Codes listed on the claim | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP245-0002 | |||
| 870 | CIP245 | REVENUE-CODE | Value must be a valid code | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP245-0003 | |||
| 871 | CIP245 | REVENUE-CODE | If value invalid, record it exactly as it appears in the state system | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP245-0004 | |||
| 872 | CIP248 | IMMUNIZATION-TYPE | This field identifies the type of immunization provided in order to track additional detail not currently contained in CPT codes. | Conditional | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP248-0001 |
| 873 | CIP249 | IP-LT-QUANTITY-OF-SERVICE-ACTUAL | On facility claim entries, this field is to capture the actual service quantify by revenue code category, e.g., number of days in a particular type of accommodation, pints of blood, etc. However, when HCPCS codes are required for services, the units are equal to the number of times the procedure/service being reported was performed. | Required | Must be numeric | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP249-0001 | |
| 874 | CIP249 | IP-LT-QUANTITY-OF-SERVICE-ACTUAL | This field is only applicable when the service being billed can be quantified in discrete units, e.g., a number of visits or the number of units of a prescription/refill that were filled | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP249-0002 | |||
| 875 | CIP249 | IP-LT-QUANTITY-OF-SERVICE-ACTUAL | For use with CLAIMIP and CLAIMLT claims. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP249-0003 | |||
| 876 | CIP250 | IP-LT-QUANTITY-OF-SERVICE-ALLOWED | On facility claim entries, this field is to capture maximum allowable quantity by revenue code category, e.g., number of days in a particular type of accommodation, pints of blood, etc. However, when HCPCS codes are required for services, the units are equal to the number of times the procedure/service being reported was performed. | Conditional | Must be numeric | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP250-0001 | |
| 877 | CIP250 | IP-LT-QUANTITY-OF-SERVICE-ALLOWED | This field is only applicable when the service being billed can be quantified in discrete units, e.g., a number of visits or the number of units of a prescription/refill that were filled | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP250-0002 | |||
| 878 | CIP250 | IP-LT-QUANTITY-OF-SERVICE-ALLOWED | For use with CLAIMIP and CLAIMLT claims. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP250-0003 | |||
| 879 | CIP251 | REVENUE-CHARGE | The total charge for the related UB-04 Revenue Code (REVENUE-CODE). Total charges include both covered and non-covered charges (as defined by UB-04 Billing Manual) | Required | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP251-0001 | |
| 880 | CIP251 | REVENUE-CHARGE | Enter charge for each UB-04 Revenue Code listed on the claim | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP251-0002 | |||
| 881 | CIP251 | REVENUE-CHARGE | The total amount should be the sum of each of the charged amounts submitted at the claim detail level | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP251-0003 | |||
| 882 | CIP251 | REVENUE-CHARGE | If TYPE-OF-CLAIM = 3, C, W (encounter record) this field should either be zero-filled or contain the amount paid by the plan to the provider. If TYPE-OF-SERVICE =119, 120, 121 or 122, this field should be “00000000" filled.” | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP251-0004 | |||
| 883 | CIP251 | REVENUE-CHARGE | The absolute value of the sum of claim line charges (REVENUE-CHARGE) must be less than or equal to the absolute value of the TOT-BILLED-AMT | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP251-0005 | |||
| 884 | CIP251 | REVENUE-CHARGE | Value must be 8-filled if the revenue code is 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP251-0006 | |||
| 885 | CIP251 | REVENUE-CHARGE | Value must not be 8-filled if the revenue code is not 8-filled. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP251-0007 | |||
| 886 | CIP252 | ALLOWED-AMT | The maximum amount displayed at the claim line level as determined by the payer as being "allowable" under the provisions of the contract prior to the determination of actual payment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP252-0001 | |
| 887 | CIP253 | TPL-AMT | Third Party Liability (TPL) refers to the legal obligation of third parties, i.e., certain individuals, entities, or programs, to pay all or part of the expenditures for medical assistance furnished under a state plan. This is the total amount denoted at the claim detail level paid by the third party. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP253-0001 | |
| 888 | CIP254 | MEDICAID-PAID-AMT | The amount paid by Medicaid on this claim or adjustment at the claim detail level. | Required | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP254-0001 | |
| 889 | CIP254 | MEDICAID-PAID-AMT | For claims where Medicaid payment is only available at the header level, report the entire payment amount on the MSIS record corresponding to the line item with the highest charge. Zero fill Medicaid Amount Paid on all other MSIS records created from the original claim. | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP254-0002 | |||
| 890 | CIP254 | MEDICAID-PAID-AMT | For Crossover claims with Medicare Coinsurance and/or Deductibles, enter the sum of those amounts in the Medicaid-Amount-Paid field, if the providers were reimbursed by Medicaid for them. If the Coinsurance and Deductibles were not paid by the state, then report the Medicaid-Amount-Paid as $0 | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP254-0003 | |||
| 891 | CIP255 | MEDICAID-FFS-EQUIVALENT-AMT | The MEDICAID-FFS-EQUIVALENT-AMT field should be populated with the amt that would have been paid had the services been provided on a FFS basis. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP255-0001 | |
| 892 | CIP255 | MEDICAID-FFS-EQUIVALENT-AMT | Required when TYPE-OF-CLAIM = C, 3, or W | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP255-0002 | |||
| 893 | CIP256 | BILLING-UNIT | Unit of billing that is used for billing services by the facility. | Conditional | Value must be equal to a valid value. | 01 Per Day 02 Per Hour 03 Per Case 04 Per Encounter 05 Per Week 06 Per Month 07 Other Arrangements 99 Unknown |
11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP256-0001 |
| 894 | CIP257 | TYPE-OF-SERVICE | A code to categorize the services provided to a Medicaid or CHIP enrollee. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP257-0001 |
| 895 | CIP257 | TYPE-OF-SERVICE | All claims for inpatient psychiatric care provided in a separately administered psychiatric wing or psychiatric hospital are included in the CLAIMIP file. | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP257-0002 | |||
| 896 | CIP257 | TYPE-OF-SERVICE | Experience has demonstrated there can be instances when more than one service area category could be applicable for a provided service. The following hierarchy rules apply to these instances: o The specific service categories of sterilizations and other pregnancy-related procedures take precedence over provider categories, such as inpatient hospital or outpatient hospital. o Services of a physician employed by a clinic are reported under clinic services if the clinic is the billing entity. X-rays processed by the clinic in the course of treatment, however, are reported under X-ray services. o Services of a registered nurse attending a resident in a NF are reported (if they qualified under the coverage rules) under home health services if they were not billed as part of the NF bill. |
2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP257-0003 | |||
| 897 | CIP257 | TYPE-OF-SERVICE | See Appendix D for information on the various types of service. |
2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP257-0004 | |||
| 898 | CIP257 | TYPE-OF-SERVICE | Inpatient Claim/Encounters File - Claims/encounters with TYPE-OF-SERVICE = 001, 058, 060, 084, 086, 090, 091, 092, 093, 123, 132, or 135. (Note: In CLAIMIP, TYPE-OF-SERVICE 086 and 084 refer only to services received on an inpatient basis.) |
9/23/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP257-0005 | |||
| 899 | CIP257 | TYPE-OF-SERVICE | Males cannot receive midwife services or other pregnancy-related procedures. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP257-0006 | |||
| 900 | CIP260 | SERVICING-PROV-NUM | A unique number to identify the provider who treated the recipient. |
Required | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP260-0001 |
| 901 | CIP260 | SERVICING-PROV-NUM | If value is invalid, record it exactly as it appears in the state system. | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP260-0002 | |||
| 902 | CIP260 | SERVICING-PROV-NUM | For institutional providers and other providers operating as a group, The SERVICING-PROV-NUM should be for the individual who rendered the service. | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP260-0003 | |||
| 903 | CIP260 | SERVICING-PROV-NUM | If “Servicing” provider and the “Billing” provider are the same then use the same number in both fields. |
2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP260-0004 | |||
| 904 | CIP260 | SERVICING-PROV-NUM | Note: Once a national provider ID numbering system is in place, the national number should be used. If only the state’s legacy ID number is available then that number can be entered in this field. |
2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP260-0005 | |||
| 905 | CIP260 | SERVICING-PROV-NUM | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122). | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP260-0006 | |||
| 906 | CIP261 | SERVICING-PROV-NPI-NUM | The NPI of the health care professional who delivers or completes a particulay medical service or non-surgical procedure. The SERVICING-PROV-NPI-NUM is required when rendering provider is different than the attending provider and state or federal regulatory requirements call for a "combined claim" (i.e., a claim that includes both facility and professional components). Examples are Medicaid clinic bills or critical access hospital claims. | Conditional | Valid characters include only numbers (0-9) | 11/9/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP261-0001 | |
| 907 | CIP261 | SERVICING-PROV-NPI-NUM | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP261-0002 | ||
| 908 | CIP261 | SERVICING-PROV-NPI-NUM | The field should be blank if the transaction is for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122). | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP261-0004 | |||
| 909 | CIP262 | SERVICING-PROV-TAXONOMY | The taxonomy code for the institution billing/caring for the beneficiary. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP262-0001 |
| 910 | CIP262 | SERVICING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion. | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP262-0002 | |||
| 911 | CIP262 | SERVICING-PROV-TAXONOMY | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122) | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP262-0003 | |||
| 912 | CIP263 | SERVICING-PROV-TYPE | A code describing the type of provider (i.e. doctor or facility) responsible for treating a patient. This represents the attending physician if available. If the state uses state-specific codes, they should map their internal codes to the CMS standard list provided. |
Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP263-0001 |
| 913 | CIP264 | SERVICING-PROV-SPECIALTY | This code indicates the area of specialty for the servicing provider. | Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP264-0001 |
| 914 | CIP265 | OPERATING-PROV-NPI-NUM | The National Provider ID (NPI) of the provider who performed the surgical procedures on the beneficiary | Conditional | Valid characters include only numbers (0-9) | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP265-0001 | |
| 915 | CIP265 | OPERATING-PROV-NPI-NUM | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP265-0002 | ||
| 916 | CIP265 | OPERATING-PROV-NPI-NUM | The field should be blank if the transaction is for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122). | 2/25/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP265-0003 | |||
| 917 | CIP266 | OTHER-TPL-COLLECTION | This data element indicates that the claim is for a beneficiary for whom other third party resource development and collection activities are in progress, when the liability is not another health insurance plan for which the eligible is a beneficiary | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 Third Party Resource is Casualty/Tort 002 Third Party Resource is Estate 003 Third Party Resource is Lien (TEFRA) 004 Third Party Resource is Lien (Other) 005 Third Party Resource is Worker’s Compensation 006 Third Party Resource is Medical Malpractice 007 Third Party Resource is Other 999 Classification of Third Party Resource is Unknown |
11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP266-0001 |
| 918 | CIP267 | PROV-FACILITY-TYPE | The type of facility for the servicing provider using the HIPAA provider taxonomy codes. |
Required | A value is required for CLAIMIP records | See Appendix A for listing of valid values. See Appendix N for Crosswalk of Provider Taxonomy Codes to Provider Facility Type Categories. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP267-0001 |
| 919 | CIP268 | BENEFIT-TYPE | The benefit category corresponding to the service reported on the claim or encounter record. Note: The code definitions in the valid value list originate from the Medicaid and CHIP Program Data System’s (MACPro’s) benefit type list. See Appendix H: Benefit Types for descriptions of the categories. |
Required | Value must be equal to a valid value. | See Appendix H for listing of valid values. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP268-0001 |
| 920 | CIP269 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | This code indicates if the claim was matched with Title XIX or Title XXI. | Required | Value must be equal to a valid value. | 01 Federal funding under Title XIX 02 Federal funding under Title XXI 03 Federal funding under ACA 04 Federal funding under other legislation |
4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP269-0001 |
| 921 | CIP269 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | If an individual is not eligible for S-CHIP, then any associated claims records should not have reimbursed with federal funding under Title XXI. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP269-0002 | |||
| 922 | CIP269 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | If an individual is not eligible for Medicaid, then any associated claims records should not have reimbursed with federal funding under Title XIX. | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP269-0003 | |||
| 923 | CIP270 | XIX-MBESCBES-CATEGORY-OF-SERVICE | A code indicating the category of service for the paid claim. The category of service is the line item from the CMS-64 form that states use to report their expenditures and request federal financial participation. | Conditional | Value must be equal to a valid value. | See Appendix I for listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP270-0001 |
| 924 | CIP270 | XIX-MBESCBES-CATEGORY-OF-SERVICE | Males cannot receive services where the category of service is "Other Pregnancy-related Procedures", "Nurse Mid-wife", "Freestanding Birth Center" or "Tobacco Cessation for Pregnant Women". | 4/30/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP270-0002 | |||
| 925 | CIP271 | XXI-MBESCBES-CATEGORY-OF-SERVICE | A code indicating the category of service for the paid claim. The category of service is the line item from the CMS-21 form that states use to report their expenditures and request federal financial participation. Refer to Attachment 8 for definitions on the various categories of service. | Conditional | Value must be equal to a valid value. | See Appendix J for listing of valid values. | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP271-0001 |
| 926 | CIP272 | OTHER-INSURANCE-AMT | The amount paid by insurance other than Medicare or Medicaid on this claim. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP272-0001 | |
| 927 | CIP273 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP273-0001 | |
| 928 | CIP273 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP273-0002 | |||
| 929 | CIP279 | HCPCS-RATE | For inpatient hospital facility claims, the accommodation rate is captured here. This data element is expected to capture data from the HIPAA 837I claim loop 2400 SV206 or UB-04 FL 44 (only if the value represents an accommodation rate). | Conditional | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP279-0001 | ||
| 930 | CIP284 | NATIONAL-DRUG-CODE | A code in National Drug Code (NDC) format indicating the drug, device, or medical supply covered by this claim. | Conditional | Position 10-12 must be Alpha Numeric or blank | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP284-0001 | |
| 931 | CIP284 | NATIONAL-DRUG-CODE | Position 1-5 must be Numeric | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP284-0002 | |||
| 932 | CIP284 | NATIONAL-DRUG-CODE | Position 6-9 must be Alpha Numeric | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP284-0003 | |||
| 933 | CIP284 | NATIONAL-DRUG-CODE | Drug code formats must be supplied by State in advance of submitting any file data. States must inform CMS of the NDC segments used and their size (e.g., {5, 4, 2} or {5, 4} as defined in the National Drug Code Directory). | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP284-0004 | |||
| 934 | CIP284 | NATIONAL-DRUG-CODE | If the Drug Code is less than 11 characters in length, the value must be left justified and padded with spaces. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP284-0005 | |||
| 935 | CIP284 | NATIONAL-DRUG-CODE | If Durable Medical Equipment or supply is prescribed by a physician and provided by a pharmacy then HCPCS or state specific codes can be put in the NDC field. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP284-0006 | |||
| 936 | CIP284 | NATIONAL-DRUG-CODE | This field is applicable for pharmacy/drug and DME services that are provided to Medicaid/CHIP in an in-patient facility/setting. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP284-0007 | |||
| 937 | CIP285 | NDC-UNIT-OF-MEASURE | A code to indicate the basis by which the quantity of the National Drug Code is expressed. |
Conditional | Value must be equal to a valid value. Valid Value Definition: F2 International Unit GR Gram ME Milligram ML Milliliter UN Unit |
F2 International Unit ML Milliliter GR Gram UN Unit |
11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP285-0001 |
| 938 | CIP285 | NDC-UNIT-OF-MEASURE | Enter the unit of measure for each corresponding quantity value. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP285-0002 | |||
| 939 | CIP278 | NDC-QUANTITY | This field is to capture the actual quantity of the National Drug Code being prescribed on this in-patient claim. | Conditional | Must be numeric | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP278-0001 | |
| 940 | CIP278 | NDC-QUANTITY | This field is only applicable when the NDC code being billed can be quantified in discrete units, e.g., the number of units of a prescription/refill that were filled. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP278-0002 | |||
| 941 | CIP286 | ADJUDICATION-DATE | The date on which the payment status of the claim was finally adjudicated by the state. | Required | Date format is CCYYMMDD (National Data Standard). | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP286-0001 | |
| 942 | CIP286 | ADJUDICATION-DATE | Value must be a valid date | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP286-0002 | |||
| 943 | CIP286 | ADJUDICATION-DATE | For Adjustment Records (ADJUSTMENT-INDICATOR<> 0), use date of final adjudication when possible. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP286-0003 | |||
| 944 | CIP286 | ADJUDICATION-DATE | For Encounter Records (TYPE-OF-CLAIM=3, C, W); use date the encounter was processed by the state. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP286-0004 | |||
| 945 | CIP286 | ADJUDICATION-DATE | If a complete, valid date is not available or is unknown, 9-fil | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP286-0005 | |||
| 946 | CIP286 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or before END-OF-TIME-PERIOD included in the T-MSIS HEADER RECORD | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP286-0006 | |||
| 947 | CIP286 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or after the ADMISSION-DATE | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP286-0007 | |||
| 948 | CIP286 | ADJUDICATION-DATE | This date must occur on or after the DATE-OF-BIRTH in the Eligible Record when the eligible is not a CHIP unborn child. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP286-0008 | |||
| 949 | CIP286 | ADJUDICATION-DATE | A Medicaid or CHIP eligible individual should not have had a claim adjudicated before their five-year immigration ineligible status has expired, except when the eligible is an unborn child in the CHIP program. | 10/10/2013 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP286-0009 | |||
| 950 | CIP287 | SELF-DIRECTION-TYPE | This data element is not applicable to this file type. | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 Hiring Authority 002 Budget Authority 003 Hiring and Budget Authority 999 Type of Authority Is Unknown |
11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP287-0001 |
| 951 | CIP288 | PRE-AUTHORIZATION-NUM | A number, code or other value that indicates the services provided on this claim have been authorized by the payee or other service organization, or that a referral for services has been approved. (Also called Prior Authorization or Referral Number). | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP288-0001 | |
| 952 | CIP274 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | CLAIMIP | CLAIM-LINE-RECORD-IP-CIP00003 | CIP274-0001 | |||
| 953 | CLT001 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the CLAIM-HEADER-RECORD-IP record segment is CIP00002 | Required | Value must be equal to a valid value. | CLT00001 - FILE-HEADER-RECORD-LT | 4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT001-0001 |
| 954 | CLT001 | RECORD-ID | Must be populated on every record | 4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT001-0002 | |||
| 955 | CLT001 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT001-0003 | |||
| 956 | CLT002 | DATA-DICTIONARY-VERSION | A data element to capture the version of the T-MSIS data dictionary that was used to build the file. | Required | Use the version number specified on the title page of the data dictionary | 2/25/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT002-0001 | |
| 957 | CLT003 | SUBMISSION-TRANSACTION-TYPE | A data element to identify the whether the transactions in the file are original submissions of the data, a resubmission of a previously submitted file, or corrections of edit rejects. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT003-0001 |
| 958 | CLT004 | FILE-ENCODING-SPECIFICATION | A data element to denote whether the file is in fixed length line format or pipe-delimited format. | Required | Value must be equal to a valid value. | FLF - The file follows a fixed length format. PSV - The file follows a pipe-delimited format. |
4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT004-0001 |
| 959 | CLT005 | DATA-MAPPING-DOCUMENT-VERSION | A data element to identify the version of the T-MSIS data mapping document used to build the file. | Required | Use the version number specified on the title page of the data mapping document. | 2/25/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT005-0001 | |
| 960 | CLT006 | FILE-NAME | The name identifying the subject area to which the records in its file relate. Each T-MSIS submission file should only contain records for one subject area (i.e., Eligible, Third-party Liability, Provider, Managed Care Plan Information, IP claims, LT claims, Rx claims, or OT claims). | Required | Value must be equal to a valid value. | CLAIM-LT - Long Term Care Claims/Encounters File - Claims/encounters with TYPE-OF-SERVICE 009, 044, 045, 046, 047, 048, 059, or 133 (all mental hospital, and NF services). (Note: Individual services billed by a long-term care facility belong in this file regardless of service type.) |
4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT006-0001 |
| 961 | CLT007 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT007-0001 |
| 962 | CLT007 | SUBMITTING-STATE | Must be populated on every record. | 2/25/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT007-0002 | |||
| 963 | CLT007 | SUBMITTING-STATE | Value must be numeric |
4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT007-0003 | |||
| 964 | CLT007 | SUBMITTING-STATE | SUBMITTING-STATE must be equal across all record segments for a given record. |
4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT007-0004 | |||
| 965 | CLT008 | DATE-FILE-CREATED | The date on which the file was created. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT008-0001 | |
| 966 | CLT008 | DATE-FILE-CREATED | Value must be a valid date | 4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT008-0002 | |||
| 967 | CLT008 | DATE-FILE-CREATED | Date must be equal to or later than the date entered in the END-OF-TIME-PERIOD field. | 10/10/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT008-0003 | |||
| 968 | CLT009 | START-OF-TIME-PERIOD | Beginning date of the time period covered by this file. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT009-0001 | |
| 969 | CLT009 | START-OF-TIME-PERIOD | The date must be a valid date. | 4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT009-0002 | |||
| 970 | CLT010 | END-OF-TIME-PERIOD | Last date of the reporting period covered by the file to which this Header Record is attached. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT010-0001 | |
| 971 | CLT010 | END-OF-TIME-PERIOD | Value must be a valid date | 4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT010-0002 | |||
| 972 | CLT011 | FILE-STATUS-INDICATOR | A code to indicate whether the records in the file are test or production records. | Required | Value must be equal to a valid value. | P Production File T Test File |
2/25/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT011-0001 |
| 973 | CLT012 | SSN-INDICATOR | Indicates whether the state uses the eligible person's social security number (SSN) instead of an MSIS identification number as the unique, unchanging eligible person identifier. | Required | Value must be equal to a valid value. | 0 State does not use SSN as MSIS-IDENTIFICATION-NUMBER 1 State uses SSN as MSIS-IDENTIFICATION-NUMBER |
4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT012-0001 |
| 974 | CLT012 | SSN-INDICATOR | A state's SSN/Non-SSN designation on the eligibility file should match on the claims files. | 4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT012-0002 | |||
| 975 | CLT012 | SSN-INDICATOR | States that are non SSN states must not submit MSIS Identification Numbers and SSNs that match for eligible individuals. | 4/30/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT012-0003 | |||
| 976 | CLT013 | TOT-REC-CNT | A count of all records in the file except for the file header record. This count will be used as a control total to help assure that the file did not become corrupted during transmission. | Required | An integer value with no commas | 10/10/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT013-0001 | |
| 977 | CLT227 | SEQUENCE-NUMBER | To enable state’s to sequentially number files, when related, follow-on files are necessary (i.e., update files, replacement files). This should begin with 1 for the original Create submission type and be incremented by one for each Replacement or Update submission for the same reporting period and file type (subject area). | Required | Field is required on all 'C', 'U', and 'R' record files. | 10/10/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT227-0001 | |
| 978 | CLT227 | SEQUENCE-NUMBER | Must be numeric and > 0 | 10/10/2013 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT227-0002 | |||
| 979 | CLT014 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT014-0001 | |
| 980 | CLT014 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT014-0002 | |||
| 981 | CLT015 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | CLAIMLT | FILE-HEADER-RECORD-LT-CLT00001 | CLT015-0001 | |||
| 982 | CLT016 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the CLAIM-HEADER-RECORD-IP record segment is CIP00002 | Required | For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. | CLT00002- CLAIM-HEADER-RECORD-LT | 11/9/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT016-0001 |
| 983 | CLT016 | RECORD-ID | Must be populated on every record | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT016-0002 | |||
| 984 | CLT016 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT016-0003 | |||
| 985 | CLT017 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT017-0001 |
| 986 | CLT017 | SUBMITTING-STATE | Must be populated on every record. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT017-0002 | |||
| 987 | CLT017 | SUBMITTING-STATE | Value must be numeric |
4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT017-0003 | |||
| 988 | CLT017 | SUBMITTING-STATE | SUBMITTING-STATE must be equal across all record segments for a given record. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT017-0004 | |||
| 989 | CLT018 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT018-0001 | |
| 990 | CLT018 | RECORD-NUMBER | Must be numeric | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT018-0002 | |||
| 991 | CLT018 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT018-0004 | |||
| 992 | CLT019 | ICN-ORIG | A unique number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies an original claim. | Required | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT019-0001 | |
| 993 | CLT019 | ICN-ORIG | Record the value exactly as it appears in the State system. Do not pad. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT019-0002 | |||
| 994 | CLT019 | ICN-ORIG | This field should always be populated with the claim identification number assigned to the original paid/denied claim. This identification number should remain constant and be carried forward onto any adjustment claims. The intention is for this earliest claim identification number to be the link that ties the original claim and all adjustment claims together. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT019-0003 | |||
| 995 | CLT019 | ICN-ORIG | This field should not be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT019-0004 | |||
| 996 | CLT020 | ICN-ADJ | A unique claim number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies the adjustment claim for an original transaction. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT020-0001 | |
| 997 | CLT020 | ICN-ADJ | Record the value exactly as it appears in the State system. Do not pad. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT020-0002 | |||
| 998 | CLT020 | ICN-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT020-0003 | |||
| 999 | CLT021 | SUBMITTER-ID | The Submitter ID number is the value that identifies the provider/trading partner/clearing house organization to state’s claim adjudication system. | Conditional | Value must not be null | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT021-0001 | |
| 1000 | CLT022 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Conditional | MSIS Identification Number must be reported | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT022-0001 | |
| 1001 | CLT022 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state ID numbers must be supplied to CMS | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT022-0002 | |||
| 1002 | CLT022 | MSIS-IDENTIFICATION-NUM | For TYPE-OF-CLAIM = 4 or D (lump sum adjustments), this field must begin with an ‘&’. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT022-0003 | |||
| 1003 | CLT022 | MSIS-IDENTIFICATION-NUM | For SSN states, this field must contain the Eligible's Social Security Number. If the SSN is unknown and a temporary number is assigned, this field will contain that number. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT022-0004 | |||
| 1004 | CLT023 | CROSSOVER-INDICATOR | An indicator specifying whether the claim is a crossover claim where a portion is paid by Medicare. | Required | Value must be equal to a valid value. | 0 Not Crossover Claim 1 Crossover Claim 9 Unknown |
4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT023-0001 |
| 1005 | CLT023 | CROSSOVER-INDICATOR | If Crossover Indicator is Yes, there must be Medicare enrollment in the Eligible file for the same time period (by date of service). | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT023-0002 | |||
| 1006 | CLT023 | CROSSOVER-INDICATOR | Detail records should be created for all crossover claims. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT023-0003 | |||
| 1007 | CLT024 | 1115A-DEMONSTRATION-IND | Indicates that the individual participates in an 1115(A) demonstration. 1115(A) is a Center for Medicare and Medicaid Innovation (CMMI) demonstration. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT024-0001 |
| 1008 | CLT024 | 1115A-DEMONSTRATION-IND | If 1115A-DEMONSTRATION-IND set to Yes on claim then there must be a 1115A-DEMONSTRATION-IND set to Yes (1115 participant) in the T-MSIS Eligible file with the same MSIS ID and/or SSN, an 1115A-EFF-DATE < the begin date of service and an 1115A-END-DATE > the end date of service on the claim. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT024-0002 | |||
| 1009 | CLT025 | ADJUSTMENT-IND | Code indicating type of adjustment record. | Required | Value must be equal to a valid value. | 0 Original Claim / Encounter 1 Void of a prior submission 2 Re-submittal 3 Credit Adjustment (negative supplemental) 4 Debit Adjustment (positive supplemental) 5 Credit Gross Adjustment. 6 Debit Gross Adjustment 9 Unknown |
4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT025-0001 |
| 1010 | CLT026 | ADJUSTMENT-REASON-CODE | Claim adjustment reason codes communicate why a claim was paid differently than it was billed. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-adjustment-reason-codes/ | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT026-0001 |
| 1011 | CLT026 | ADJUSTMENT-REASON-CODE | If there is no adjustment to a claim, then there is no adjustment reason code. (Also see: CLAIM-PYMT-REM-CODE). If claim record does not represent an adjustment, 8-fill | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT026-0002 | |||
| 1012 | CLT027 | ADMITTING-DIAGNOSIS-CODE | The ICD-9/10-CM Diagnosis Code provided at the time of admission by the physician. | Required | Code full valid ICD 9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 “. Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT027-0001 |
| 1013 | CLT027 | ADMITTING-DIAGNOSIS-CODE | E-codes are not valid as Admitting Diagnosis Codes. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT027-0002 | |||
| 1014 | CLT027 | ADMITTING-DIAGNOSIS-CODE | The diagnosis provided by the physician at the time of admission which describes the patient's condition upon admission to the hospital. Since the Admitting Diagnosis is formulated before all tests and examinations are complete, it may be stated in the form of a problem or symptom and it may differ from any of the final diagnoses recorded in the medical record. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT027-0003 | |||
| 1015 | CLT027 | ADMITTING-DIAGNOSIS-CODE | CMS is not expecting ADMITTING-DIAGNOSIS-CODE-FLAG "2" (ICD-10) to be used until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT027-0004 | |||
| 1016 | CLT027 | ADMITTING-DIAGNOSIS-CODE | Enter invalid codes exactly as they appear in the State system. Do not 8- or 9-fill. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT027-0004 | |||
| 1017 | CLT028 | ADMITTING-DIAGNOSIS-CODE-FLAG | A flag that identifies the coding system used for the ADMITTING-DIAGNOSIS- CODE. | Required | Value must be equal to a valid value. | 01 ICD-9 02 ICD-10 03 Other 99 Unknown |
4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT028-0001 |
| 1018 | CLT028 | ADMITTING-DIAGNOSIS-CODE-FLAG | The state must use a code that belongs to the code set that they report they are using. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT028-0002 | |||
| 1019 | CLT028 | ADMITTING-DIAGNOSIS-CODE-FLAG | CMS is not expecting ADMITTING-DIAGNOSIS-CODE-FLAG "2" (ICD-10) to be used until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT028-0003 | |||
| 1020 | CLT029 | DIAGNOSIS-CODE-1 | DIAGNOSIS-CODE-1 through DIAGNOSIS-CODE-2: Primary and Second ICD-9/10-CM code found on the claim. | Required | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". |
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT029-0001 |
| 1021 | CLT029 | DIAGNOSIS-CODE-1 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT029-0002 | |||
| 1022 | CLT029 | DIAGNOSIS-CODE-1 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. |
2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT029-0003 | |||
| 1023 | CLT029 | DIAGNOSIS-CODE-1 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT029-0004 | |||
| 1024 | CLT029 | DIAGNOSIS-CODE-1 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT029-0005 | |||
| 1025 | CLT029 | DIAGNOSIS-CODE-1 | The primary diagnosis code goes into DIAGNOSIS-CODE1 | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT029-0006 | |||
| 1026 | CLT029 | DIAGNOSIS-CODE-1 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT029-0007 | |||
| 1027 | CLT029 | DIAGNOSIS-CODE-1 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT029-0008 | |||
| 1028 | CLT030 | DIAGNOSIS-CODE-FLAG-1 | A flag that identifies the coding system used for the DIAGNOSIS CODE 1 - 12 DIAGNOSIS-CODE-FLAG-1 through DIAGNOSIS-CODE-FLAG-2: Code flag for the Primary and Second ICD-9/10-CM code found on the claim. |
Required | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT030-0001 |
| 1029 | CLT030 | DIAGNOSIS-CODE-FLAG-1 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT030-0002 | |||
| 1030 | CLT030 | DIAGNOSIS-CODE-FLAG-1 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT030-0003 | |||
| 1031 | CLT030 | DIAGNOSIS-CODE-FLAG-1 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT030-0004 | |||
| 1032 | CLT031 | DIAGNOSIS-POA-FLAG-1 | A code to identify conditions that are present at the time the order for inpatient admission occurs – conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. 1 Exempt from POA reporting. This code is the equivalent of a blank on the UB-04. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT031-0001 |
| 1033 | CLT031 | DIAGNOSIS-POA-FLAG-1 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT031-0002 | |||
| 1034 | CLT032 | DIAGNOSIS-CODE-2 | DIAGNOSIS-CODE-1 through DIAGNOSIS-CODE-2: Primary and Second ICD-9/10-CM code found on the claim. | Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". |
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT032-0001 |
| 1035 | CLT032 | DIAGNOSIS-CODE-2 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT032-0002 | |||
| 1036 | CLT032 | DIAGNOSIS-CODE-2 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT032-0003 | |||
| 1037 | CLT032 | DIAGNOSIS-CODE-2 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT032-0004 | |||
| 1038 | CLT032 | DIAGNOSIS-CODE-2 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT032-0005 | |||
| 1039 | CLT032 | DIAGNOSIS-CODE-2 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT032-0006 | |||
| 1040 | CLT032 | DIAGNOSIS-CODE-2 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 5. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT032-0007 | |||
| 1041 | CLT032 | DIAGNOSIS-CODE-2 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT032-0008 | |||
| 1042 | CLT033 | DIAGNOSIS-CODE-FLAG-2 | DIAGNOSIS-CODE-FLAG-1 through DIAGNOSIS-CODE-FLAG-2: Code flag for the Primary and Second ICD-9/10-CM code found on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT033-0001 |
| 1043 | CLT033 | DIAGNOSIS-CODE-FLAG-2 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT033-0002 | |||
| 1044 | CLT033 | DIAGNOSIS-CODE-FLAG-2 | If DIAGNOSIS-CODE-FLAG-1 through 12 = "2" (ICD-10) should not be used until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT033-0003 | |||
| 1045 | CLT033 | DIAGNOSIS-CODE-FLAG-2 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT033-0004 | |||
| 1046 | CLT034 | DIAGNOSIS-POA-FLAG-2 | A code to identify conditions that are present at the time the order for inpatient admission occurs – conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. 1 Exempt from POA reporting. This code is the equivalent of a blank on the UB-04. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT034-0001 |
| 1047 | CLT034 | DIAGNOSIS-POA-FLAG-2 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT034-0002 | |||
| 1048 | CLT035 | DIAGNOSIS-CODE-3 | DIAGNOSIS-CODE-3 through DIAGNOSIS-CODE-5: The third through fifth ICD-9/10-CM codes that appear on the claim. | Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". |
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT035-0001 |
| 1049 | CLT035 | DIAGNOSIS-CODE-3 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT035-0002 | |||
| 1050 | CLT035 | DIAGNOSIS-CODE-3 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT035-0003 | |||
| 1051 | CLT035 | DIAGNOSIS-CODE-3 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT035-0004 | |||
| 1052 | CLT035 | DIAGNOSIS-CODE-3 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT035-0005 | |||
| 1053 | CLT035 | DIAGNOSIS-CODE-3 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT035-0006 | |||
| 1054 | CLT035 | DIAGNOSIS-CODE-3 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 5. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT035-0007 | |||
| 1055 | CLT035 | DIAGNOSIS-CODE-3 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT035-0008 | |||
| 1056 | CLT036 | DIAGNOSIS-CODE-FLAG-3 | DIAGNOSIS-CODE-FLAG-3 through DIAGNOSIS-CODE-FLAG-5: Code flag for the third through fifth ICD-9/10-CM codes that appear on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT036-0001 |
| 1057 | CLT036 | DIAGNOSIS-CODE-FLAG-3 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT036-0002 | |||
| 1058 | CLT036 | DIAGNOSIS-CODE-FLAG-3 | If DIAGNOSIS-CODE-FLAG-1 through 12 = "2" (ICD-10) should not be used until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT036-0003 | |||
| 1059 | CLT036 | DIAGNOSIS-CODE-FLAG-3 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT036-0004 | |||
| 1060 | CLT037 | DIAGNOSIS-POA-FLAG-3 | A code to identify conditions that are present at the time the order for inpatient admission occurs – conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. 1 Exempt from POA reporting. This code is the equivalent of a blank on the UB-04. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT037-0001 |
| 1061 | CLT037 | DIAGNOSIS-POA-FLAG-3 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT037-0002 | |||
| 1062 | CLT038 | DIAGNOSIS-CODE-4 | DIAGNOSIS-CODE-3 through DIAGNOSIS-CODE-5: The third through fifth ICD-9/10-CM codes that appear on the claim. | Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". |
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT038-0001 |
| 1063 | CLT038 | DIAGNOSIS-CODE-4 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT038-0002 | |||
| 1064 | CLT038 | DIAGNOSIS-CODE-4 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT038-0003 | |||
| 1065 | CLT038 | DIAGNOSIS-CODE-4 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT038-0004 | |||
| 1066 | CLT038 | DIAGNOSIS-CODE-4 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT038-0005 | |||
| 1067 | CLT038 | DIAGNOSIS-CODE-4 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT038-0006 | |||
| 1068 | CLT038 | DIAGNOSIS-CODE-4 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 5. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT038-0007 | |||
| 1069 | CLT038 | DIAGNOSIS-CODE-4 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT038-0008 | |||
| 1070 | CLT039 | DIAGNOSIS-CODE-FLAG-4 | DIAGNOSIS-CODE-FLAG-3 through DIAGNOSIS-CODE-FLAG-5: Code flag for the third through fifth ICD-9/10-CM codes that appear on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT039-0001 |
| 1071 | CLT039 | DIAGNOSIS-CODE-FLAG-4 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT039-0002 | |||
| 1072 | CLT039 | DIAGNOSIS-CODE-FLAG-4 | If DIAGNOSIS-CODE-FLAG-1 through 12 = "2" (ICD-10) should not be used until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT039-0003 | |||
| 1073 | CLT039 | DIAGNOSIS-CODE-FLAG-4 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT039-0004 | |||
| 1074 | CLT040 | DIAGNOSIS-POA-FLAG-4 | A code to identify conditions that are present at the time the order for inpatient admission occurs – conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. 1 Exempt from POA reporting. This code is the equivalent of a blank on the UB-04. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT040-0001 |
| 1075 | CLT040 | DIAGNOSIS-POA-FLAG-4 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT040-0002 | |||
| 1076 | CLT041 | DIAGNOSIS-CODE-5 | DIAGNOSIS-CODE-3 through DIAGNOSIS-CODE-5: The third through fifth ICD-9/10-CM codes that appear on the claim. | Conditional | Code valid ICD-9/10 CM codes without a decimal point. For example: 210.5 is coded as "2105 ". |
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT041-0001 |
| 1077 | CLT041 | DIAGNOSIS-CODE-5 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT041-0002 | |||
| 1078 | CLT041 | DIAGNOSIS-CODE-5 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT041-0003 | |||
| 1079 | CLT041 | DIAGNOSIS-CODE-5 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT041-0004 | |||
| 1080 | CLT041 | DIAGNOSIS-CODE-5 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT041-0005 | |||
| 1081 | CLT041 | DIAGNOSIS-CODE-5 | CLAIMLT/CLAIMIP: Provide diagnosis coding as submitted on bill. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT041-0006 | |||
| 1082 | CLT041 | DIAGNOSIS-CODE-5 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 - 5. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT041-0007 | |||
| 1083 | CLT041 | DIAGNOSIS-CODE-5 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 12 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT041-0008 | |||
| 1084 | CLT042 | DIAGNOSIS-CODE-FLAG-5 | DIAGNOSIS-CODE-FLAG-3 through DIAGNOSIS-CODE-FLAG-5: Code flag for the third through fifth ICD-9/10-CM codes that appear on the claim. | Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT042-0001 |
| 1085 | CLT042 | DIAGNOSIS-CODE-FLAG-5 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT042-0002 | |||
| 1086 | CLT042 | DIAGNOSIS-CODE-FLAG-5 | If DIAGNOSIS-CODE-FLAG-1 through 12 = "2" (ICD-10) should not be used until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT042-0003 | |||
| 1087 | CLT042 | DIAGNOSIS-CODE-FLAG-5 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT042-0004 | |||
| 1088 | CLT043 | DIAGNOSIS-POA-FLAG-5 | A code to identify conditions that are present at the time the order for inpatient admission occurs – conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. 1 Exempt from POA reporting. This code is the equivalent of a blank on the UB-04. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT043-0001 |
| 1089 | CLT043 | DIAGNOSIS-POA-FLAG-5 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT043-0002 | |||
| 1090 | CLT044 | ADMISSION-DATE | The date on which the recipient was admitted to a hospital or long term care facility. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT044-0001 | |
| 1091 | CLT044 | ADMISSION-DATE | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT044-0002 | |||
| 1092 | CLT044 | ADMISSION-DATE | ADMISSION-DATE must occur on or before the ADJUDICATION-DATE | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT044-0003 | |||
| 1093 | CLT044 | ADMISSION-DATE | ADMISSION-DATE must occur on or before the DISCHARGE-DATE | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT044-0004 | |||
| 1094 | CLT044 | ADMISSION-DATE | ADMISSION-DATE must occur on or after the DATE-OF-BIRTH listed in Eligible Record. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT044-0005 | |||
| 1095 | CLT044 | ADMISSION-DATE | ADMISSION-DATE must occur on or before the DATE-OF-DEATH listed in Eligible Record. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT044-0006 | |||
| 1096 | CLT045 | ADMISSION-HOUR | The time of admission to a hospital or long term care facility. | Conditional | Value must be a valid hour in military time format (00 to 23). | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT045-0001 |
| 1097 | CLT046 | DISCHARGE-DATE | The date on which the recipient was discharged from a hospital or long term care facility. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT046-0001 | |
| 1098 | CLT046 | DISCHARGE-DATE | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT046-0002 | |||
| 1099 | CLT046 | DISCHARGE-DATE | This date must occur on or after the ADMISSION-DATE. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT046-0003 | |||
| 1100 | CLT046 | DISCHARGE-DATE | This date must occur on or before the ADJUDICATION-DATE. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT046-0004 | |||
| 1101 | CLT046 | DISCHARGE-DATE | This field is required if TYPE-OF-SERVICE does not equal a capitated payment (Valid values for capitated payment include 119, 120, 122). | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT046-0005 | |||
| 1102 | CLT046 | DISCHARGE-DATE | This date must occur on or after the DATE-OF-BIRTH in the Eligible Record. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT046-0006 | |||
| 1103 | CLT046 | DISCHARGE-DATE | This date must occur on or before the DATE-OF-DEATH in the Eligible record | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT046-0007 | |||
| 1104 | CLT047 | DISCHARGE-HOUR | The time of discharge for inpatient claims or end time of treatment for outpatient claims. | Conditional | Value must be a valid hour in military time format (00 to 23). | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT047-0001 |
| 1105 | CLT048 | BEGINNING-DATE-OF-SERVICE | For services received during a single encounter with a provider, the date the service covered by this claim was received. For services involving multiple encounters on different days, or periods of care extending over two or more days, this would be the date on which the service covered by this claim began. For capitation premium payments, the date on which the period of coverage related to this payment began. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT048-0001 | |
| 1106 | CLT048 | BEGINNING-DATE-OF-SERVICE | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT048-0002 | |||
| 1107 | CLT048 | BEGINNING-DATE-OF-SERVICE | The beginning date of service must occur before or be the same as the end of time period | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT048-0003 | |||
| 1108 | CLT048 | BEGINNING-DATE-OF-SERVICE | Date must occur before or be the same as Ending Date of Service | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT048-0004 | |||
| 1109 | CLT048 | BEGINNING-DATE-OF-SERVICE | Date must occur before or be the same as adjudication date. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT048-0005 | |||
| 1110 | CLT048 | BEGINNING-DATE-OF-SERVICE | Date must occur on or before Date of Death. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT048-0006 | |||
| 1111 | CLT048 | BEGINNING-DATE-OF-SERVICE | The beginning date of service must occur before the DATE-OF-BIRTH when the person is eligible as an unborn CHIP child or beginning date of service must occur on or after the DATE-OF-BIRTH when the person is eligible through Medicaid or is eligible as a non-unborn CHIP child . | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT048-0007 | |||
| 1112 | CLT048 | BEGINNING-DATE-OF-SERVICE | A Medicaid claim record for an eligible individual, if applicable, cannot have a Beginning Date of Service after the eligible individual's Medicaid enrollment has ended. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT048-0008 | |||
| 1113 | CLT048 | BEGINNING-DATE-OF-SERVICE | A CHIP claim record for an individual eligible for separate CHIP cannot have a Beginning Date of Service after the eligible individual's CHIP enrollment has ended. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT048-0009 | |||
| 1114 | CLT049 | ENDING-DATE-OF-SERVICE | For services received during a single encounter with a provider, the date the service covered by this claim was received. For services involving multiple encounters on different days, or periods of care extending over two or more days, the date on which the service covered by this claim ended. For capitation premium payments, the date on which the period of coverage related to this payment ends/ended. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT049-0001 | |
| 1115 | CLT049 | ENDING-DATE-OF-SERVICE | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT049-0002 | |||
| 1116 | CLT049 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must occur after or be the same as the BEGINNING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT049-0003 | |||
| 1117 | CLT049 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must be on or before the ADJUDICATION-DATE. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT049-0004 | |||
| 1118 | CLT049 | ENDING-DATE-OF-SERVICE | Date must occur on or before Date of Death. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT049-0005 | |||
| 1119 | CLT049 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must be on or after DATE-OF-BIRTH | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT049-0006 | |||
| 1120 | CLT049 | ENDING-DATE-OF-SERVICE | Date must occur before or be the same as End of Time Period. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT049-0007 | |||
| 1121 | CLT050 | ADJUDICATION-DATE | The date on which the payment status of the claim was finally adjudicated by the state. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT050-0001 | |
| 1122 | CLT050 | ADJUDICATION-DATE | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT050-0002 | |||
| 1123 | CLT050 | ADJUDICATION-DATE | For Adjustment Records (ADJUSTMENT-INDICATOR<> 0), use date of final adjudication when possible. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT050-0003 | |||
| 1124 | CLT050 | ADJUDICATION-DATE | For Encounter Records (TYPE-OF-CLAIM=3, C, W); use date the encounter was processed by the state. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT050-0004 | |||
| 1125 | CLT050 | ADJUDICATION-DATE | If a complete, valid date is not available or is unknown, 9-fil | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT050-0005 | |||
| 1126 | CLT050 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or before END-OF-TIME-PERIOD included in the T-MSIS HEADER RECORD | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT050-0006 | |||
| 1127 | CLT050 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or after the ADMISSION-DATE | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT050-0007 | |||
| 1128 | CLT050 | ADJUDICATION-DATE | This date must occur on or after the DATE-OF-BIRTH in the Eligible Record when the eligible is not a CHIP unborn child. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT050-0008 | |||
| 1129 | CLT050 | ADJUDICATION-DATE | A Medicaid or CHIP eligible individual should not have had a claim adjudicated before their five-year immigration ineligible status has expired, except when the eligible is an unborn child in the CHIP program. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT050-0009 | |||
| 1130 | CLT051 | MEDICAID-PAID-DATE | The date Medicaid paid on this claim or adjustment. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT051-0001 | |
| 1131 | CLT051 | MEDICAID-PAID-DATE | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT051-0002 | |||
| 1132 | CLT052 | TYPE-OF-CLAIM | A code indicating what kind of payment is covered in this claim. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT052-0001 |
| 1133 | CLT052 | TYPE-OF-CLAIM | States should only submit CHIP claims for CHIP eligibles | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT052-0002 | |||
| 1134 | CLT052 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the basis of eligibility. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT052-0003 | |||
| 1135 | CLT052 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the maintenance assistance status. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT052-0004 | |||
| 1136 | CLT052 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the restricted benefits code. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT052-0005 | |||
| 1137 | CLT052 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the TANF code. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT052-0006 | |||
| 1138 | CLT053 | TYPE-OF-BILL | A data element corresponding with UB-04 form locator FL4 that classifies the claim as to the type of facility (2nd digit), type of care (3rd digit) and the billing record's sequence in the episode of care (4th digit). (Note that the 1st digit is always zero.) | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT053-0001 |
| 1139 | CLT054 | CLAIM-STATUS | The health care claim status codes convey the status of an entire claim. | Required | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-codes/ | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT054-0001 |
| 1140 | CLT055 | CLAIM-STATUS-CATEGORY | The general category of the claim status (accepted, rejected, pended, finalized, additional information requested, etc.), which is then further detailed in the companion data element CLAIM-STATUS. | Required | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-category-codes/ | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT055-0001 |
| 1141 | CLT056 | SOURCE-LOCATION | The field denotes the claims payment system from which the claim was extracted. | Required | Value must be equal to a valid value. | 01 MMIS 02 Non-MMIS CHIP Payment System 03 Pharmacy Benefits Manager (PBM) Vendor 04 Dental Benefits Manager Vendor 05 Transportation Provider System 06 Mental Health Claims Payment System 07 Financial Transaction/Accounting System 08 Other State Agency Claims Payment System 09 County/Local Government Claims Payment System 10 Other Vendor/Other Claims Payment System 20 Managed Care Organization (MCO) 99 Unknown source |
4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT056-0001 |
| 1142 | CLT057 | CHECK-NUM | The check or EFT number. |
Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9),, dashes (-), and spaces. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT057-0001 | |
| 1143 | CLT057 | CHECK-NUM | If there is a valid check date there should also be a valid check number. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT057-0002 | |||
| 1144 | CLT058 | CHECK-EFF-DATE | Date the check is issued to the payee, or if Electronic Funds Transfer (EFT), the date the transfer is made. | Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT058-0001 | |
| 1145 | CLT058 | CHECK-EFF-DATE | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT058-0002 | |||
| 1146 | CLT058 | CHECK-EFF-DATE | Could be the same as Remittance Date. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT058-0003 | |||
| 1147 | CLT058 | CHECK-EFF-DATE | If there is a valid check number, there should also be a valid check date. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT058-0004 | |||
| 1148 | CLT059 | CLAIM-PYMT-REM-CODE-1 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT059-0001 |
| 1149 | CLT060 | CLAIM-PYMT-REM-CODE-2 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT060-0001 |
| 1150 | CLT061 | CLAIM-PYMT-REM-CODE-3 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT061-0001 |
| 1151 | CLT062 | CLAIM-PYMT-REM-CODE-4 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT062-0001 |
| 1152 | CLT063 | TOT-BILLED-AMT | The total amount charged for this claim at the claim header level as submitted by the provider. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT063-0001 | |
| 1153 | CLT063 | TOT-BILLED-AMT | The total amount should be the sum of each of the billed amounts submitted at the claim detail level. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT063-0002 | |||
| 1154 | CLT063 | TOT-BILLED-AMT | If TYPE-OF-CLAIM = "4", then TOT-BILLED-AMT must = "00000000". | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT063-0003 | |||
| 1155 | CLT063 | TOT-BILLED-AMT | If TYPE-OF-CLAIM = 3, C, W (encounter record) this field should either be zero-filled or contain the amount paid by the plan to the provider. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT063-0004 | |||
| 1156 | CLT064 | TOT-ALLOWED-AMT | The claim header level maximum amount determined by the payer as being 'allowable' under the provisions of the contract prior to the determination of actual payment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT064-0001 | |
| 1157 | CLT064 | TOT-ALLOWED-AMT | The sum of the allowed amounts at the detailed levels must equal TOT-ALLOWED-AMT | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT064-0002 | |||
| 1158 | CLT065 | TOT-MEDICAID-PAID-AMT | The total amount paid by Medicaid on this claim or adjustment at the claim header level, which is the sum of the amounts paid by Medicaid at the detail level for the claim. | Required | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT065-0001 | |
| 1159 | CLT066 | TOT-COPAY-AMT | The total amount paid by Medicaid/CHIP enrollee for each office or emergency department visit or purchase of prescription drugs in addition to the amount paid by Medicaid/CHIP. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT066-0001 | |
| 1160 | CLT067 | TOT-MEDICARE-DEDUCTIBLE-AMT | The amount paid by Medicaid/CHIP, on this claim at the claim header level, toward the beneficiary’s Medicare deductible. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT067-0001 | |
| 1161 | CLT067 | TOT-MEDICARE-DEDUCTIBLE-AMT | The total medicare deductible amount must be less than or equal the total billed amount. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT067-0002 | |||
| 1162 | CLT067 | TOT-MEDICARE-DEDUCTIBLE-AMT | If TOT-MEDICARE-COINS-AMT = "88888", then TOT-MEDICARE-DEDUCTIBLE-AMT must = "88888". | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT067-0003 | |||
| 1163 | CLT067 | TOT-MEDICARE-DEDUCTIBLE-AMT | If TOT-MEDICARE-COINS-AMT = "99999", then TOT-MEDICARE-DEDUCTIBLE-AMT must = "99999". | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT067-0004 | |||
| 1164 | CLT068 | TOT-MEDICARE-COINS-AMT | The amount paid by Medicaid/CHIP, on this claim at the claim header level, toward the beneficiary’s Medicare coinsurance. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT068-0001 | |
| 1165 | CLT068 | TOT-MEDICARE-COINS-AMT | Value should be reported as not applicable if the TYPE-OF-CLAIM is an encounter (valid values = 3, C, W) | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT068-0002 | |||
| 1166 | CLT068 | TOT-MEDICARE-COINS-AMT | Value must be less than TOT-BILLED-AMT. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT068-0003 | |||
| 1167 | CLT068 | TOT-MEDICARE-COINS-AMT | Value must be 8-filled if TOT-MEDICARE-DEDUCTIBLE-AMT is 8-filled. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT068-0004 | |||
| 1168 | CLT069 | TOT-TPL-AMT | Third Party Liability (TPL) refers to the legal obligation of third parties, i.e., certain individuals, entities, or programs, to pay all or part of the expenditures for medical assistance furnished under a state plan. This is the total amount denoted at the claim header level paid by the third party. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT069-0001 | |
| 1169 | CLT069 | TOT-TPL-AMT | The absolute value of TOT-TPL-AMT must be < the absolute value of ( (TOT-BILLED-AMT - (minus) TOT-MEDICARE-COINS-AMT + (plus) TOT-MEDICARE-DEDUCTIBLE-AMT) ) | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT069-0002 | |||
| 1170 | CLT070 | TOT-OTHER-INSURANCE-AMT | The amount paid by insurance other than Medicare or Medicaid on this claim. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT070-0001 | |
| 1171 | CLT071 | OTHER-INSURANCE-IND | The field denotes whether the insured party is covered under other insurance plan | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 9 Unknown |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT071-0001 |
| 1172 | CLT072 | OTHER-TPL-COLLECTION | This data element indicates that the claim is for a beneficiary for whom other third party resource development and collection activities are in progress, when the liability is not another health insurance plan for which the eligible is a beneficiary. | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 Third Party Resource is Casualty/Tort 002 Third Party Resource is Estate 003 Third Party Resource is Lien (TEFRA) 004 Third Party Resource is Lien (Other) 005 Third Party Resource is Worker’s Compensation 006 Third Party Resource is Medical Malpractice 007 Third Party Resource is Other 999 Classification of Third Party Resource is Unknown |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT072-0001 |
| 1173 | CLT073 | SERVICE-TRACKING-TYPE | A code to categorize service tracking claims. A “service tracking claim” is used to report lump sum payments that cannot be attributed to a single enrollee. (Note: Use an encounter record to report services provided under a capitated payment arrangement.) | Conditional | Value must be equal to a valid value. | 00 Not a Service Tracking Claim 01 Drug Rebate 02 DSH Payment 03 Lump Sum Payment 04 Cost Settlement 05 Supplemental 06 Other 99 Unknown |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT073-0001 |
| 1174 | CLT074 | SERVICE-TRACKING-PAYMENT-AMT | On service tracking claims, the lump sum amount paid to the provider. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT074-0001 | |
| 1175 | CLT074 | SERVICE-TRACKING-PAYMENT-AMT | Required on service tracking records | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT074-0002 | |||
| 1176 | CLT074 | SERVICE-TRACKING-PAYMENT-AMT | Amount paid for services received by an individual patient, when the state accepts a lump sum form a provider that covered similar services delivered to more than one patient, such as a group screening for EPSDT. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT074-0003 | |||
| 1177 | CLT074 | SERVICE-TRACKING-PAYMENT-AMT | For service tracking payments, ensure that the TOT-MEDICAID-PAID-AMOUNT is 0 filled and provide payment amount in SERVICE-TRACKING-PAYMENT-AMT only. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT074-0004 | |||
| 1178 | CLT074 | SERVICE-TRACKING-PAYMENT-AMT | If there is a service tracking type, then there must also be a service tracking payment amount. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT074-0005 | |||
| 1179 | CLT074 | SERVICE-TRACKING-PAYMENT-AMT | If SERVICE-TRACKING-TYPE <> "00" or "99", then SERVICE-TRACKING-PAYMENT-AMT must BE<> 000000000000. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT074-0006 | |||
| 1180 | CLT075 | FIXED-PAYMENT-IND | This code indicates that the reimbursement amount included on the claim is for a fixed payment. Fixed payments are made by the state to insurers or providers for premiums or eligible coverage, not for a particular service. For example, some states have Primary Care Case Management (PCCM) programs where the state pays providers a monthly patient management fee of $3.50 for each eligible participant under their care. This fee is considered a fixed payment. It is very important for states to correctly identify fixed payments. Fixed payments do not have a defined “medical record” associated with the payment; therefore, fixed payments are not subject to medical record request and medical record review. |
Conditional | Value must be equal to a valid value. | 0 Not Fixed Payment 1 FFS Fixed Payment |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT075-0001 |
| 1181 | CLT076 | FUNDING-CODE | A code to indicate the source of non-federal share funds. | Required | Value must be equal to a valid value. | A Medicaid Agency B CHIP Agency C Mental Health Service Agency D Education Agency E Child and Family Services Agency F County G City H Providers I Other |
10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT076-0001 |
| 1182 | CLT077 | FUNDING-SOURCE-NONFEDERAL-SHARE | A code to indicate the type of non-federal share used by the state to finance its expenditure to the provider. | Required | Value must be equal to a valid value. When states have multiple sources of FUNDING-SOURCE-NONFEDERAL-SHARE, States are to report the portion which represents the largest proportion as the FUNDING-SOURCE-NONFEDERAL-SHARE. |
01 State appropriations to the Medicaid agency 02 Intergovernmental transfers (IGT) 03 Certified public expenditures (CPE) 04 Provider taxes 05 Donations |
9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT077-0001 |
| 1183 | CLT078 | MEDICARE-COMB-DED-IND | Code indicating that the amount paid by Medicaid/CHIP on this claim toward the recipient's Medicare deductible was combined with their coinsurance amount because the amounts could not be separated. | Conditional | Value must be equal to a valid value. | 0 Amount not combined with coinsurance amount 1 Amount combined with coinsurance amount 9 Unknown |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT078-0001 |
| 1184 | CLT078 | MEDICARE-COMB-DED-IND | If claim is not a Crossover claim, or if a type of claim is “3,” “C” or “W” (an encounter claim), set value to “0” | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT078-0002 | |||
| 1185 | CLT078 | MEDICARE-COMB-DED-IND | Claims records for an eligible individual should not indicate Medicare paid any combined deductible amount on the claim, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT078-0003 | |||
| 1186 | CLT079 | PROGRAM-TYPE | Code indicating special Medicaid program under which the service was provided. Refer to Appendix E for information on the various program types. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT079-0001 |
| 1187 | CLT079 | PROGRAM-TYPE | Value for 1915 (c) waiver must correspond to the values for 1915(c) waiver in the Waiver Type. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT079-0002 | |||
| 1188 | CLT079 | PROGRAM-TYPE | If PROGRAM-TYPE=Community First Choice (11) then [T-MSIS ELIGIBLE FILE] STATE-PLAN-OPTION-TYPE must = 01 for the same time period. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT079-0003 | |||
| 1189 | CLT079 | PROGRAM-TYPE | If PROGRAM-TYPE=1915(i) (value=13) then [T-MSIS ELIGIBLE FILE] STATE-PLAN-OPTION-TYPE must = 02 for the same time period. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT079-0004 | |||
| 1190 | CLT080 | PLAN-ID-NUMBER | A unique number, assigned by the state, which represents the health plan under which the non-fee-for-service encounter was provided including through the state plan and a waiver. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT080-0001 | |
| 1191 | CLT080 | PLAN-ID-NUMBER | Use the number as it is carried in the state’s system. (TYPE-OF-CLAIM=3, C, W OR TYPE-OF-SERVICE=119, 120, 122) | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT080-0002 | |||
| 1192 | CLT080 | PLAN-ID-NUMBER | If TYPE-OF-CLAIM <> Encounter or Capitation Payment, 8-fill. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT080-0003 | |||
| 1193 | CLT080 | PLAN-ID-NUMBER | This data element must equal the BILLING-PROV-NUM if the TYPE-OF-SERVICE is a capitation payment. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT080-0004 | |||
| 1194 | CLT080 | PLAN-ID-NUMBER | The managed care ID on the individual's eligible record must match that which is included on any claims records for the eligible individual. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT080-0005 | |||
| 1195 | CLT081 | NATIONAL-HEALTH-CARE-ENTITY-ID | The national identifier of the health care entity (controlling health plan, subhealth plan, or other entity) at the most granular sub-health plan level of the Medicaid or CHIP health plan in which an individual is enrolled. (See 45 CFR 162 Subpart E. http://www.gpo.gov/fdsys/pkg/FR-2012-09-05/pdf/2012-21238.pdf | NA | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT081-0001 | |
| 1196 | CLT081 | NATIONAL-HEALTH-CARE-ENTITY-ID | Large health plans are required to obtain national health plan identifiers by November 5, 2014, small health plans by November 5, 2015. States may report prior to these dates if available. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT081-0002 | |||
| 1197 | CLT081 | NATIONAL-HEALTH-CARE-ENTITY-ID | This field is required for all managed care claims and encounters with dates of service on or after the mandated dates above. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT081-0003 | |||
| 1198 | CLT081 | NATIONAL-HEALTH-CARE-ENTITY-ID | NATIONAL-HEALTH-CARE-ENTITY-IDs on managed care claims and encounters must match NATIONAL-HEALTH-CARE-ENTITY-IDs on file for the individual in the eligibility subject area or the TPL subject area | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT081-0004 | |||
| 1199 | CLT082 | PAYMENT-LEVEL-IND | The field denotes whether the claim payment is made at the header level or the detail level. | Required | Value must be equal to a valid value. | 1 Claim Header – Sum of Line Item payments 2 Claim Detail – Individual Line Item payments |
4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT082-0001 |
| 1200 | CLT082 | PAYMENT-LEVEL-IND | Payment fields at either the claim header or line on encounter records should be left blank. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT082-0002 | |||
| 1201 | CLT083 | MEDICARE-REIM-TYPE | This code indicates the type of Medicare Reimbursement. | Conditional | Value must be equal to a valid value. | 01 IPPS - Acute Inpatient PPS 02 LTCHPPS - Long-term Care Hospital PPS 03 SNFPPS - Skilled Nursing Facility PPS 04 HHPPS - Home Health PPS 05 IRFPPS - Inpatient Rehabilitation Facility PPS 06 IPFPPS - Inpatient Psychiatric Facility PPS 07 OPPS - Outpatient PPS 08 Fee Schedules (for physicians, DME, ambulance, and clinical lab) 09 Part C Hierarchical Condition Category Risk Assessment (CMS-HCC RA) Capitation Payment Model |
10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT083-0001 |
| 1202 | CLT083 | MEDICARE-REIM-TYPE | If this is a crossover Medicare claim, the claim must have a MEDICARE-REIM-TYPE. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT083-0002 | |||
| 1203 | CLT084 | NON-COV-DAYS | The number of days of institutional long-term care not covered by the payer for this sequence as qualified by the payer organization. The number of non-covered days does not refer to days not covered for any other service. | Conditional | Must contain number of non-covered days. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT084-0001 | |
| 1204 | CLT084 | NON-COV-DAYS | The sum of Non-Covered Days and Covered Days must not exceed Total Length of Stay (Statement Covers Period - Thru Date minus Admission Date\Start of Care) for any payer sequence. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT084-0002 | |||
| 1205 | CLT085 | NON-COV-CHARGES | The charges for institutional long-term care, which are not reimbursable by the primary payer. The non-covered charges do not refer to charges not covered for any other service. | Conditional | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT085-0001 | |
| 1206 | CLT086 | MEDICAID-COV-INPATIENT-DAYS | The number of inpatient psychiatric days covered by Medicaid on this claim. | Conditional | Populate this field with a valid numeric entry. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT086-0001 | |
| 1207 | CLT086 | MEDICAID-COV-INPATIENT-DAYS | This field is applicable when: - A CLAIMLT record has TYPE-OF-SERVICE = 048, 044, 045, or 50 (inpatient mental health/psychiatric services). |
2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT086-0002 | |||
| 1208 | CLT086 | MEDICAID-COV-INPATIENT-DAYS | This total must not be greater than double the duration between the DISCHARGE-DATE and the ADMISSION-DATE, plus one day. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT086-0003 | |||
| 1209 | CLT086 | MEDICAID-COV-INPATIENT-DAYS | This field is required if the Type of Service is 046 or 009. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT086-0004 | |||
| 1210 | CLT087 | CLAIM-LINE-COUNT | The total number of lines on the claim. | Required | Must be populated on every record | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT087-0001 | |
| 1211 | CLT087 | CLAIM-LINE-COUNT | If the number of claim lines is above the state-approved limit, the record will be split and the split-claim-ind will equal 1. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT087-0002 | |||
| 1212 | CLT087 | CLAIM-LINE-COUNT | The claim line count should equal the sum of the claim lines for this record. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT087-0003 | |||
| 1213 | CLT090 | FORCED-CLAIM-IND | This code indicates if the claim was processed by forcing it through a manual override process. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT090-0001 |
| 1214 | CLT091 | HEALTH-CARE-ACQUIRED-CONDITION-IND | This code indicates whether the individual included on the claim has a Health Care Acquired Condition. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 9 Unknown |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT091-0001 |
| 1215 | CLT092 | OCCURRENCE-CODE-01 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT092-0001 |
| 1216 | CLT092 | OCCURRENCE-CODE-01 | Required if reported on the claim. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT092-0002 | |||
| 1217 | CLT092 | OCCURRENCE-CODE-01 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT092-0003 | |||
| 1218 | CLT093 | OCCURRENCE-CODE-02 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT093-0001 |
| 1219 | CLT093 | OCCURRENCE-CODE-02 | Required if reported on the claim. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT093-0002 | |||
| 1220 | CLT093 | OCCURRENCE-CODE-02 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT093-0003 | |||
| 1221 | CLT094 | OCCURRENCE-CODE-03 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT094-0001 |
| 1222 | CLT094 | OCCURRENCE-CODE-03 | Required if reported on the claim. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT094-0002 | |||
| 1223 | CLT094 | OCCURRENCE-CODE-03 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT094-0003 | |||
| 1224 | CLT095 | OCCURRENCE-CODE-04 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT095-0001 |
| 1225 | CLT095 | OCCURRENCE-CODE-04 | Required if reported on the claim. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT095-0002 | |||
| 1226 | CLT095 | OCCURRENCE-CODE-04 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT095-0003 | |||
| 1227 | CLT096 | OCCURRENCE-CODE-05 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT096-0001 |
| 1228 | CLT096 | OCCURRENCE-CODE-05 | Required if reported on the claim. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT096-0002 | |||
| 1229 | CLT096 | OCCURRENCE-CODE-05 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT096-0003 | |||
| 1230 | CLT097 | OCCURRENCE-CODE-06 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT097-0001 |
| 1231 | CLT097 | OCCURRENCE-CODE-06 | Required if reported on the claim. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT097-0002 | |||
| 1232 | CLT097 | OCCURRENCE-CODE-06 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT097-0003 | |||
| 1233 | CLT098 | OCCURRENCE-CODE-07 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT098-0001 |
| 1234 | CLT098 | OCCURRENCE-CODE-07 | Required if reported on the claim. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT098-0002 | |||
| 1235 | CLT098 | OCCURRENCE-CODE-07 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT098-0003 | |||
| 1236 | CLT099 | OCCURRENCE-CODE-08 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT099-0001 |
| 1237 | CLT099 | OCCURRENCE-CODE-08 | Required if reported on the claim. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT099-0002 | |||
| 1238 | CLT099 | OCCURRENCE-CODE-08 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT099-0003 | |||
| 1239 | CLT100 | OCCURRENCE-CODE-09 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT100-0001 |
| 1240 | CLT100 | OCCURRENCE-CODE-09 | Required if reported on the claim. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT100-0002 | |||
| 1241 | CLT100 | OCCURRENCE-CODE-09 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT100-0003 | |||
| 1242 | CLT101 | OCCURRENCE-CODE-10 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT101-0001 |
| 1243 | CLT101 | OCCURRENCE-CODE-10 | Required if reported on the claim. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT101-0002 | |||
| 1244 | CLT101 | OCCURRENCE-CODE-10 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT101-0003 | |||
| 1245 | CLT102 | OCCURRENCE-CODE-EFF-DATE-01 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT102-0001 | |
| 1246 | CLT102 | OCCURRENCE-CODE-EFF-DATE-01 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT102-0002 | |||
| 1247 | CLT102 | OCCURRENCE-CODE-EFF-DATE-01 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT102-0003 | |||
| 1248 | CLT102 | OCCURRENCE-CODE-EFF-DATE-01 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT102-0004 | |||
| 1249 | CLT102 | OCCURRENCE-CODE-EFF-DATE-01 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT102-0005 | |||
| 1250 | CLT102 | OCCURRENCE-CODE-EFF-DATE-01 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT102-0006 | |||
| 1251 | CLT103 | OCCURRENCE-CODE-EFF-DATE-02 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT103-0001 | |
| 1252 | CLT103 | OCCURRENCE-CODE-EFF-DATE-02 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT103-0002 | |||
| 1253 | CLT103 | OCCURRENCE-CODE-EFF-DATE-02 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT103-0003 | |||
| 1254 | CLT103 | OCCURRENCE-CODE-EFF-DATE-02 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT103-0004 | |||
| 1255 | CLT103 | OCCURRENCE-CODE-EFF-DATE-02 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT103-0005 | |||
| 1256 | CLT103 | OCCURRENCE-CODE-EFF-DATE-02 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT103-0006 | |||
| 1257 | CLT104 | OCCURRENCE-CODE-EFF-DATE-03 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT104-0001 | |
| 1258 | CLT104 | OCCURRENCE-CODE-EFF-DATE-03 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT104-0002 | |||
| 1259 | CLT104 | OCCURRENCE-CODE-EFF-DATE-03 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT104-0003 | |||
| 1260 | CLT104 | OCCURRENCE-CODE-EFF-DATE-03 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT104-0004 | |||
| 1261 | CLT104 | OCCURRENCE-CODE-EFF-DATE-03 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT104-0005 | |||
| 1262 | CLT104 | OCCURRENCE-CODE-EFF-DATE-03 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT104-0006 | |||
| 1263 | CLT105 | OCCURRENCE-CODE-EFF-DATE-04 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT105-0001 | |
| 1264 | CLT105 | OCCURRENCE-CODE-EFF-DATE-04 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT105-0002 | |||
| 1265 | CLT105 | OCCURRENCE-CODE-EFF-DATE-04 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT105-0003 | |||
| 1266 | CLT105 | OCCURRENCE-CODE-EFF-DATE-04 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT105-0004 | |||
| 1267 | CLT105 | OCCURRENCE-CODE-EFF-DATE-04 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT105-0005 | |||
| 1268 | CLT105 | OCCURRENCE-CODE-EFF-DATE-04 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT105-0006 | |||
| 1269 | CLT106 | OCCURRENCE-CODE-EFF-DATE-05 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT106-0001 | |
| 1270 | CLT106 | OCCURRENCE-CODE-EFF-DATE-05 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT106-0002 | |||
| 1271 | CLT106 | OCCURRENCE-CODE-EFF-DATE-05 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT106-0003 | |||
| 1272 | CLT106 | OCCURRENCE-CODE-EFF-DATE-05 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT106-0004 | |||
| 1273 | CLT106 | OCCURRENCE-CODE-EFF-DATE-05 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT106-0005 | |||
| 1274 | CLT106 | OCCURRENCE-CODE-EFF-DATE-05 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT106-0006 | |||
| 1275 | CLT107 | OCCURRENCE-CODE-EFF-DATE-06 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT107-0001 | |
| 1276 | CLT107 | OCCURRENCE-CODE-EFF-DATE-06 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT107-0002 | |||
| 1277 | CLT107 | OCCURRENCE-CODE-EFF-DATE-06 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT107-0003 | |||
| 1278 | CLT107 | OCCURRENCE-CODE-EFF-DATE-06 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT107-0004 | |||
| 1279 | CLT107 | OCCURRENCE-CODE-EFF-DATE-06 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT107-0005 | |||
| 1280 | CLT107 | OCCURRENCE-CODE-EFF-DATE-06 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT107-0006 | |||
| 1281 | CLT108 | OCCURRENCE-CODE-EFF-DATE-07 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT108-0001 | |
| 1282 | CLT108 | OCCURRENCE-CODE-EFF-DATE-07 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT108-0002 | |||
| 1283 | CLT108 | OCCURRENCE-CODE-EFF-DATE-07 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT108-0003 | |||
| 1284 | CLT108 | OCCURRENCE-CODE-EFF-DATE-07 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT108-0004 | |||
| 1285 | CLT108 | OCCURRENCE-CODE-EFF-DATE-07 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT108-0005 | |||
| 1286 | CLT108 | OCCURRENCE-CODE-EFF-DATE-07 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT108-0006 | |||
| 1287 | CLT109 | OCCURRENCE-CODE-EFF-DATE-08 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT109-0001 | |
| 1288 | CLT109 | OCCURRENCE-CODE-EFF-DATE-08 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT109-0002 | |||
| 1289 | CLT109 | OCCURRENCE-CODE-EFF-DATE-08 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT109-0003 | |||
| 1290 | CLT109 | OCCURRENCE-CODE-EFF-DATE-08 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT109-0004 | |||
| 1291 | CLT109 | OCCURRENCE-CODE-EFF-DATE-08 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT109-0005 | |||
| 1292 | CLT109 | OCCURRENCE-CODE-EFF-DATE-08 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT109-0006 | |||
| 1293 | CLT110 | OCCURRENCE-CODE-EFF-DATE-09 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT110-0001 | |
| 1294 | CLT110 | OCCURRENCE-CODE-EFF-DATE-09 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT110-0002 | |||
| 1295 | CLT110 | OCCURRENCE-CODE-EFF-DATE-09 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT110-0003 | |||
| 1296 | CLT110 | OCCURRENCE-CODE-EFF-DATE-09 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT110-0004 | |||
| 1297 | CLT110 | OCCURRENCE-CODE-EFF-DATE-09 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT110-0005 | |||
| 1298 | CLT110 | OCCURRENCE-CODE-EFF-DATE-09 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT110-0006 | |||
| 1299 | CLT111 | OCCURRENCE-CODE-EFF-DATE-10 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT111-0001 | |
| 1300 | CLT111 | OCCURRENCE-CODE-EFF-DATE-10 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT111-0002 | |||
| 1301 | CLT111 | OCCURRENCE-CODE-EFF-DATE-10 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT111-0003 | |||
| 1302 | CLT111 | OCCURRENCE-CODE-EFF-DATE-10 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT111-0004 | |||
| 1303 | CLT111 | OCCURRENCE-CODE-EFF-DATE-10 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT111-0005 | |||
| 1304 | CLT111 | OCCURRENCE-CODE-EFF-DATE-10 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT111-0006 | |||
| 1305 | CLT112 | OCCURRENCE-CODE-END-DATE-01 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT112-0001 | |
| 1306 | CLT112 | OCCURRENCE-CODE-END-DATE-01 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT112-0002 | |||
| 1307 | CLT112 | OCCURRENCE-CODE-END-DATE-01 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT112-0003 | |||
| 1308 | CLT112 | OCCURRENCE-CODE-END-DATE-01 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT112-0004 | |||
| 1309 | CLT112 | OCCURRENCE-CODE-END-DATE-01 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT112-0005 | |||
| 1310 | CLT112 | OCCURRENCE-CODE-END-DATE-01 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT112-0006 | |||
| 1311 | CLT113 | OCCURRENCE-CODE-END-DATE-02 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT113-0001 | |
| 1312 | CLT113 | OCCURRENCE-CODE-END-DATE-02 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT113-0002 | |||
| 1313 | CLT113 | OCCURRENCE-CODE-END-DATE-02 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT113-0003 | |||
| 1314 | CLT113 | OCCURRENCE-CODE-END-DATE-02 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT113-0004 | |||
| 1315 | CLT113 | OCCURRENCE-CODE-END-DATE-02 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT113-0005 | |||
| 1316 | CLT113 | OCCURRENCE-CODE-END-DATE-02 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT113-0006 | |||
| 1317 | CLT114 | OCCURRENCE-CODE-END-DATE-03 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT114-0001 | |
| 1318 | CLT114 | OCCURRENCE-CODE-END-DATE-03 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT114-0002 | |||
| 1319 | CLT114 | OCCURRENCE-CODE-END-DATE-03 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT114-0003 | |||
| 1320 | CLT114 | OCCURRENCE-CODE-END-DATE-03 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT114-0004 | |||
| 1321 | CLT114 | OCCURRENCE-CODE-END-DATE-03 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT114-0005 | |||
| 1322 | CLT114 | OCCURRENCE-CODE-END-DATE-03 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT114-0006 | |||
| 1323 | CLT115 | OCCURRENCE-CODE-END-DATE-04 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT115-0001 | |
| 1324 | CLT115 | OCCURRENCE-CODE-END-DATE-04 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT115-0002 | |||
| 1325 | CLT115 | OCCURRENCE-CODE-END-DATE-04 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT115-0003 | |||
| 1326 | CLT115 | OCCURRENCE-CODE-END-DATE-04 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT115-0004 | |||
| 1327 | CLT115 | OCCURRENCE-CODE-END-DATE-04 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT115-0005 | |||
| 1328 | CLT115 | OCCURRENCE-CODE-END-DATE-04 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT115-0006 | |||
| 1329 | CLT116 | OCCURRENCE-CODE-END-DATE-05 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT116-0001 | |
| 1330 | CLT116 | OCCURRENCE-CODE-END-DATE-05 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT116-0002 | |||
| 1331 | CLT116 | OCCURRENCE-CODE-END-DATE-05 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT116-0003 | |||
| 1332 | CLT116 | OCCURRENCE-CODE-END-DATE-05 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT116-0004 | |||
| 1333 | CLT116 | OCCURRENCE-CODE-END-DATE-05 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT116-0005 | |||
| 1334 | CLT116 | OCCURRENCE-CODE-END-DATE-05 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT116-0006 | |||
| 1335 | CLT117 | OCCURRENCE-CODE-END-DATE-06 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT117-0001 | |
| 1336 | CLT117 | OCCURRENCE-CODE-END-DATE-06 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT117-0002 | |||
| 1337 | CLT117 | OCCURRENCE-CODE-END-DATE-06 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT117-0003 | |||
| 1338 | CLT117 | OCCURRENCE-CODE-END-DATE-06 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT117-0004 | |||
| 1339 | CLT117 | OCCURRENCE-CODE-END-DATE-06 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT117-0005 | |||
| 1340 | CLT117 | OCCURRENCE-CODE-END-DATE-06 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT117-0006 | |||
| 1341 | CLT118 | OCCURRENCE-CODE-END-DATE-07 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT118-0001 | |
| 1342 | CLT118 | OCCURRENCE-CODE-END-DATE-07 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT118-0002 | |||
| 1343 | CLT118 | OCCURRENCE-CODE-END-DATE-07 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT118-0003 | |||
| 1344 | CLT118 | OCCURRENCE-CODE-END-DATE-07 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT118-0004 | |||
| 1345 | CLT118 | OCCURRENCE-CODE-END-DATE-07 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT118-0005 | |||
| 1346 | CLT118 | OCCURRENCE-CODE-END-DATE-07 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT118-0006 | |||
| 1347 | CLT119 | OCCURRENCE-CODE-END-DATE-08 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT119-0001 | |
| 1348 | CLT119 | OCCURRENCE-CODE-END-DATE-08 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT119-0002 | |||
| 1349 | CLT119 | OCCURRENCE-CODE-END-DATE-08 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT119-0003 | |||
| 1350 | CLT119 | OCCURRENCE-CODE-END-DATE-08 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT119-0004 | |||
| 1351 | CLT119 | OCCURRENCE-CODE-END-DATE-08 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT119-0005 | |||
| 1352 | CLT119 | OCCURRENCE-CODE-END-DATE-08 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT119-0006 | |||
| 1353 | CLT120 | OCCURRENCE-CODE-END-DATE-09 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT120-0001 | |
| 1354 | CLT120 | OCCURRENCE-CODE-END-DATE-09 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT120-0002 | |||
| 1355 | CLT120 | OCCURRENCE-CODE-END-DATE-09 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT120-0003 | |||
| 1356 | CLT120 | OCCURRENCE-CODE-END-DATE-09 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT120-0004 | |||
| 1357 | CLT120 | OCCURRENCE-CODE-END-DATE-09 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT120-0005 | |||
| 1358 | CLT120 | OCCURRENCE-CODE-END-DATE-09 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT120-0006 | |||
| 1359 | CLT121 | OCCURRENCE-CODE-END-DATE-10 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT121-0001 | |
| 1360 | CLT121 | OCCURRENCE-CODE-END-DATE-10 | Value must be a valid date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT121-0002 | |||
| 1361 | CLT121 | OCCURRENCE-CODE-END-DATE-10 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT121-0003 | |||
| 1362 | CLT121 | OCCURRENCE-CODE-END-DATE-10 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT121-0004 | |||
| 1363 | CLT121 | OCCURRENCE-CODE-END-DATE-10 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT121-0005 | |||
| 1364 | CLT121 | OCCURRENCE-CODE-END-DATE-10 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT121-0006 | |||
| 1365 | CLT122 | PATIENT-CONTROL-NUM | A patient's unique number assigned by the provider agency during claim submission, which identifies the client or the client’s episode of service within the provider’s system to facilitate retrieval of individual financial and clinical records and posting of payment. | Conditional | Must be numeric (0-9) and/or alphabetic (A-Z). Special characters are invalid entries | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT122-0001 | |
| 1366 | CLT123 | ELIGIBLE-LAST-NAME | The last name of the individual to whom the services were provided. (The patients name should be captured as it appears on the claim record, it does not need to be the same as it appears on the eligibility file. The MSIS-IDENTIFICATION-NUM will be used to associate a claim record with the appropriate eligibility data.) | Required | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT123-0001 | |
| 1367 | CLT123 | ELIGIBLE-LAST-NAME | When populating the eligible person’s name on T-MSIS Claim Files, use the patient’s name from the claim transaction rather than the eligible person’s name from the T-MSIS Eligible File. | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT123-0002 | |||
| 1368 | CLT124 | ELIGIBLE-FIRST-NAME | The first name of the individual to whom the services were provided. (The patients name should be captured as it appears on the claim record, it does not need to be the same as it appears on the eligibility file. The MSIS-IDENTIFICATION-NUM will be used to associate a claim record with the appropriate eligibility data.) | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT124-0001 | |
| 1369 | CLT124 | ELIGIBLE-FIRST-NAME | When populating the eligible person’s name on T-MSIS Claim Files, use the patient’s name from the claim transaction rather than the eligible person’s name from the T-MSIS Eligible File. | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT124-0002 | |||
| 1370 | CLT125 | ELIGIBLE-MIDDLE-INIT | The middle initial of the individual to whom the services were provided. | Conditional | Value must be an alphabetic character, or a blank (A-Z, a-z, ) | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT125-0001 | |
| 1371 | CLT125 | ELIGIBLE-MIDDLE-INIT | Leave blank if not available When populating the eligible person’s name on T-MSIS Claim Files, use the patient’s name from the claim transaction rather than use the eligible person’s name from the T-MSIS Eligible File. |
9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT125-0002 | |||
| 1372 | CLT126 | DATE-OF-BIRTH | Date of birth of the individual to whom the services were provided. | Required | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT126-0001 | |
| 1373 | CLT126 | DATE-OF-BIRTH | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT126-0002 | |||
| 1374 | CLT126 | DATE-OF-BIRTH | The numeric form for days and months from 1 to 9 must have a zero as the first digit. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT126-0003 | |||
| 1375 | CLT126 | DATE-OF-BIRTH | The patient’s date of birth shall be reported in numeric form as follows – 2 digit month, 2 digit day, and 4 digit year | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT126-0004 | |||
| 1376 | CLT126 | DATE-OF-BIRTH | A patient's age should not be greater than 112 years. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT126-0005 | |||
| 1377 | CLT127 | HEALTH-HOME-PROV-IND | This code indicates whether the claim is submitted by a provider or provider group enrolled in the Health Home care model. Health home providers provide service for patients with chronic illnesses. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 8 Not Applicable 9 Unknown |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT127-0001 |
| 1378 | CLT127 | HEALTH-HOME-PROV-IND | If a state has not yet begun collecting this information, HEALTH-HOME-PROV-IND, this field should be defaulted to the value “8.” | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT127-0002 | |||
| 1379 | CLT127 | HEALTH-HOME-PROV-IND | If there is a HEALTH-HOME-ENTITY-NAME then HEALTH-HOME-PROV-IND must indicate yes. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT127-0003 | |||
| 1380 | CLT127 | HEALTH-HOME-PROV-IND | States should not submit claim records for an eligible individual that indicate the claim was submitted by a provider or provider group enrolled in a health home model if the eligible individual is not enrolled in the health home program. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT127-0004 | |||
| 1381 | CLT127 | HEALTH-HOME-PROV-IND | States that do not specify an eligible individual's health home provider number, if applicable, should not report claims that indicate the claim is submitted by a provider or provider group enrolled in the health home model. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT127-0005 | |||
| 1382 | CLT128 | WAIVER-TYPE | Code for specifying waiver type under which the eligible individual is covered during the month and receiving services/under which claim is submitted. | Conditional | Enter the WAIVER-TYPE assigned | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT128-0001 |
| 1383 | CLT128 | WAIVER-TYPE | Value must correspond to associated WAIVER-ID | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT128-0002 | |||
| 1384 | CLT128 | WAIVER-TYPE | An ineligible individual cannot have a category for federal reimbursement for Medicaid or CHIP (CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT <> 01,02) | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT128-0003 | |||
| 1385 | CLT129 | WAIVER-ID | Field specifying the waiver or demonstration which authorized payment for a claim. These IDs must be the approved, full federal waiver ID number assigned during the state submission and CMS approval process. The categories of demonstration and waiver programs include: 1915(b)(1); 1915(b)(2); 1915(b)(3), and 1915(b)(4) managed care waivers; 1915(c) home and community based services waivers; combined 1915(b) and 1915(c) managed home and community based services waivers and 1115 demonstrations. | Conditional | Valid values are supplied by the state. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ||
| 1386 | CLT129 | WAIVER-ID | Report the full federal waiver identifier. | 11/9/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT129-0002 | |||
| 1387 | CLT129 | WAIVER-ID | If the goods & services rendered do not fall under a waiver, leave this field blank. | 11/9/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT129-0004 | |||
| 1388 | CLT129 | WAIVER-ID | If there's a waiver type, there should be a corresponding waiver id. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT129-0005 | |||
| 1389 | CLT130 | BILLING-PROV-NUM | A unique identification number assigned by the state to a provider or capitation plan. This should represent the entity billing for the service. | Required | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT130-0001 |
| 1390 | CLT130 | BILLING-PROV-NUM | If value is invalid, record it exactly as it appears in the state system. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT130-0002 | |||
| 1391 | CLT130 | BILLING-PROV-NUM | For encounter records (TYPE-OF-CLAIM = 3, C, W), this represents the entity billing (or reporting) to the managed care plan (See PLAN-ID-NUMBER for reporting capitation plan-ID). Capitation PLAN-ID should be used in this field only for capitation payments (TYPE-OF-SERVICE = 119, 120, 122). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT130-0003 | |||
| 1392 | CLT131 | BILLING-PROV-NPI-NUM | The National Provider ID (NPI) of the billing provider responsible for billing for the service on the claim. The billing provider can also be servicing, referring, or prescribing provider; can be admitting provider except for Long Term Care. | Required | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT131-0001 |
| 1393 | CLT131 | BILLING-PROV-NPI-NUM | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT131-0002 | |||
| 1394 | CLT131 | BILLING-PROV-NPI-NUM | For encounter records (TYPE-OF-CLAIM = 3, C, W), the BILLIN-PROV-NPI-NUM field should be populated with the NPI of the provider or entity billing (or reporting) to the managed care plan. For financial transactions (i.e., expenditure transactions or recoupments of previously made expenditures that do not flow through the usual claim adjudication/adjustment process or encounter record reporting process), the BILLIN-PROV-NPI-NUM field should be populated with the NPI of the provider or entity to which the financial transaction was addressed, unless the transaction is a payment/recoupment made-to/received-from a managed care plan, in which case the BILLING-PROV-NPI-NUM should be left blank. For financial transactions with managed care plans, the plan's ID should be reported in the PLAN-ID-NUMBER field and the BILLING-PROV-NPI-NUM should be left blank. |
2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT131-0004 | |||
| 1395 | CLT131 | BILLING-PROV-NPI-NUM | Billing Provider must be enrolled | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT131-0005 | |||
| 1396 | CLT132 | BILLING-PROV-TAXONOMY | For CLAIMIP and CLAIMLT files, the taxonomy code for the institution billing for the beneficiary. | Conditional | Value must be in the set of valid values | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT132-0001 |
| 1397 | CLT132 | BILLING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT132-0002 | |||
| 1398 | CLT132 | BILLING-PROV-TAXONOMY | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122) | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT132-0003 | |||
| 1399 | CLT133 | BILLING-PROV-TYPE | A code describing the type of entity billing for the service. | Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT133-0001 |
| 1400 | CLT133 | BILLING-PROV-TYPE | For encounter records (TYPE-OF-CLAIM= 3, C, W), this represents the entity billing (or reporting) to the Managed Care Plan (see PLAN-ID-NUMBER for reporting capitation plan-ID). CAPITATION-PLAN-ID should be used in this field only for premium payments (TYPE-OF-SERVICE=119, 120, 122). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT133-0002 | |||
| 1401 | CLT133 | BILLING-PROV-TYPE | The state should use Taxonomy Crosswalk.pdf to crosswalk state codes to CMS codes | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT133-0003 | |||
| 1402 | CLT134 | BILLING-PROV-SPECIALTY | This code describes the area of specialty for the billing provider. | Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT134-0001 |
| 1403 | CLT135 | REFERRING-PROV-NUM | A code describing the type of provider (i.e. doctor) who referred the patient. If the state uses state-specific codes, they should map their internal codes to the CMS standard list provided. |
Conditional | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT135-0001 |
| 1404 | CLT135 | REFERRING-PROV-NUM | If value is invalid, record it exactly as it appears in the State system. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT135-0002 | |||
| 1405 | CLT135 | REFERRING-PROV-NUM | If the Referring Provider Number is not available, but the physician’s Drug Enforcement Agency (DEA) ID is on the state file, then the state should use the DEA ID for this data element. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT135-0003 | |||
| 1406 | CLT136 | REFERRING-PROV-NPI-NUM | The National Provider ID (NPI) of the provider who recommended the servicing provider to the patient. | Conditional | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT136-0001 |
| 1407 | CLT136 | REFERRING-PROV-NPI-NUM | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT136-0002 | |||
| 1408 | CLT136 | REFERRING-PROV-NPI-NUM | The field should be blank if the transaction is for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122). | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT136-0003 | |||
| 1409 | CLT137 | REFERRING-PROV-TAXONOMY | For CLAIMIP and CLAIMLT files, the taxonomy code for the referring provider. | NA | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT137-0001 |
| 1410 | CLT137 | REFERRING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT137-0002 | |||
| 1411 | CLT137 | REFERRING-PROV-TAXONOMY | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122) | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT137-0003 | |||
| 1412 | CLT138 | REFERRING-PROV-TYPE | A code describing the type of provider (i.e. doctor) who referred the patient. If the state uses state-specific codes, they should map their internal codes to the CMS standard list provided. |
NA | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT138-0001 |
| 1413 | CLT139 | REFERRING-PROV-SPECIALTY | This code indicates the area of specialty of the referring provider. | NA | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT139-0001 |
| 1414 | CLT140 | MEDICARE-HIC-NUM | Health Insurance Claim (HIC) Number as it appears on the patient’s Medicare card. | Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9) |
4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT140-0001 | |
| 1415 | CLT140 | MEDICARE-HIC-NUM | "Railroad Retirees" - Railroad Retirement Board (RRB) HIC numbers generally have two alpha characters as a prefix to the number. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT140-0002 | |||
| 1416 | CLT140 | MEDICARE-HIC-NUM | If this is a crossover Medicare claim, the Bene must have a MEDICARE-HIC-Num. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT140-0003 | |||
| 1417 | CLT140 | MEDICARE-HIC-NUM | States should not submit records for an eligible individual where the eligible's Medicare HIC Number does not match in the associated claim record, if applicable. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT140-0004 | |||
| 1418 | CLT140 | MEDICARE-HIC-NUM | Claims records for an eligible individual should not indicate a valid Medicare HIC number, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT140-0005 | |||
| 1419 | CLT141 | PATIENT-STATUS | A code indicating the patient’s status as of the ENDING-DATE-OF-SERVICE. Values used are from UB-04. This is also referred to as discharge status. | Required | Value must be equal to a valid value. | To order the current edition of the UB-04 Data Specifications Manual go to: http://www.nubc.org/subscriber/index.dhtml American Hospital Association 155 North Wacker Drive, Suite 400 Chicago, IL 60606 Phone: 312-422-3000 Fax: 312-422-4500 | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT141-0001 |
| 1420 | CLT141 | PATIENT-STATUS | If the date of death is valued, then the patient status should indicate that the patient has expired. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT141-0002 | |||
| 1421 | CLT141 | PATIENT-STATUS | Obtain the Patient Discharge Status valid value set which is published in the UB-04 Data Specifications Manual. To order the current edition of the UB-04 Data Specifications Manual go to: http://www.nubc.org/subscriber/index.dhtml American Hospital Association 155 North Wacker Drive, Suite 400 Chicago, IL 60606 Phone: 312-422-3000 Fax: 312-422-4500 |
9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT141-0003 | |||
| 1422 | CLT143 | BMI | A key index for relating a person's body weight to their height. The body mass index (BMI) is a person's weight in kilograms (kg) divided by their height in meters (m) squared. | Optional | SI units: BMI = mass (kg) / (height(m))2 Imperial/US Customary units: BMI = mass (lb) * 703/ (height(in))2 BMI = mass (lb) * 4.88/ (height(ft))2 BMI = mass (st) * 9840/ (height(in))2 |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT143-0001 | |
| 1423 | CLT143 | BMI | CMS is relieving states of the responsibility to: (a) Provide this data element. (b) Document a mitigation plan in the Source-to-Target-Mapping Matrix Addendum B whenever the data element cannot be populated all of the time. However if a state determines that it can populate the field and wishes to do so, they are encouraged to do so and will not incur any Addendum B mitigation plan documentation expectations. |
9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT143-0002 | |||
| 1424 | CLT144 | REMITTANCE-NUM | The Remittance Advice Number is a sequential number that identifies the current Remittance Advice (RA) produced for a provider. The number is incremented by one each time a new RA is generated. The first five (5) positions are Julian date YYDDD format. The RA is the detailed explanation of the reason for the payment amount. The RA number is not the check number. |
Required | Limit characters to alphabet (A-Z, a-z), numerals (0-9). | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT144-0001 | |
| 1425 | CLT144 | REMITTANCE-NUM | Value must not be null | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT144-0002 | |||
| 1426 | CLT144 | REMITTANCE-NUM | If there is a remittance date, then there must also be a remittance number. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT144-0003 | |||
| 1427 | CLT145 | LTC-RCP-LIAB-AMT | The total amount paid by the patient for services where they are required to use their personal funds to cover part of their care before Medicaid funds can be utilized. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT145-0001 | |
| 1428 | CLT145 | LTC-RCP-LIAB-AMT | The absolute value of the remaining long term care liability must be less than the absolute value of the sum of the other payments on a claim. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT145-0002 | |||
| 1429 | CLT146 | DAILY-RATE | The amount a policy will pay per day for a covered service. In some cases for OT claims this is referred to as a flat rate. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT146-0001 | |
| 1430 | CLT147 | ICF-IID-DAYS | The number of days of intermediate care for individuals with an intellectual disability that were paid for in whole or in part by Medicaid. | Conditional | Populate this field with a valid numeric entry. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT147-0001 | |
| 1431 | CLT147 | ICF-IID-DAYS | If value exceeds 99998 days, code as 99998. (e.g., code 100023 as 99998) | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT147-0002 | |||
| 1432 | CLT147 | ICF-IID-DAYS | ICF-IID-DAYS include every day of intermediate care facility services for individuals with an intellectual disability that is at least partially paid for by the State, even if private or third party funds are used for some portion of the payment. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT147-0003 | |||
| 1433 | CLT147 | ICF-IID-DAYS | The absolute value must be less than or equal to the absolute value of length of stay. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT147-0004 | |||
| 1434 | CLT147 | ICF-IID-DAYS | ICF-IID-DAYS is applicable only for TYPE-OF-SERVICE = 046. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT147-0005 | |||
| 1435 | CLT147 | ICF-IID-DAYS | If TYPE-OF-SERVICE = Mental Hospital Services for the Aged, Inpatient Psychiatric Facility Services for Individuals <22, or Nursing Facility services, then ICF-IID-DAYS must = “88888”. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT147-0006 | |||
| 1436 | CLT147 | ICF-IID-DAYS | For all claims for psychiatric services or nursing facility care services (TYPE-OF-SERVICE = 009, 044, 045, 047, 048, or 050), 8-fill. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT147-0007 | |||
| 1437 | CLT147 | ICF-IID-DAYS | ICF-IID-DAYS is applicable only for TYPE-OF-SERVICE = 046. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT147-0008 | |||
| 1438 | CLT147 | ICF-IID-DAYS | If ICF-IID-DAYS is greater than zero and less than 88887 then LEVEL-OF-CARE-STATUS in ELIGIBLE for the associated MSIS-IDENTIFIER (or SSN depending on which value is used as the unique identifier for enrollees) must be ICF/IID for the same month as the begin and end date of service. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT147-0009 | |||
| 1439 | CLT148 | LEAVE-DAYS | The number of days, during the period covered by Medicaid, on which the patient did not reside in the long term care facility. | Conditional | Populate this field with a valid numeric entry. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT148-0001 | |
| 1440 | CLT148 | LEAVE-DAYS | LEAVE-DAYS is applicable only for TYPE-OF-SERVICE = 046, 009, 047, 045, or 050 - Intermedicate Care Facility for Individuals with Intellectual Disabilities, or Nursing Facility services. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT148-0002 | |||
| 1441 | CLT148 | LEAVE-DAYS | If TYPE-OF-SERVICE = Nursing Facility then LEAVE-DAYS must be < NURSING-FACILITY-DAYS. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT148-0003 | |||
| 1442 | CLT149 | NURSING-FACILITY-DAYS | The number of days of nursing care included in this claim that were paid for, in whole or in part, by Medicaid. Includes days during which nursing facility received partial payment for holding a bed during patient leave days. | Conditional | Populate this field with a valid numeric entry. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT149-0001 | |
| 1443 | CLT149 | NURSING-FACILITY-DAYS | NURSING-FACILITY-DAYS include every day of nursing care services that is at least partially paid for by the state, even if private or third party funds are used for some portion of the payment. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT149-0002 | |||
| 1444 | CLT149 | NURSING-FACILITY-DAYS | If value exceeds 99998 days, code as 99998 | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT149-0003 | |||
| 1445 | CLT149 | NURSING-FACILITY-DAYS | For all claims for psychiatric services or intermediate care services for individuals with intellectual disabilities (TYPE-OF-SERVICE = 044, 045, 046, 048, 050), 8-fill | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT149-0004 | |||
| 1446 | CLT149 | NURSING-FACILITY-DAYS | The value for NURSING-FACILITY-DAYS must be less than or equal to the difference between the dates of service. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT149-0005 | |||
| 1447 | CLT149 | NURSING-FACILITY-DAYS | This field is required where the Type of Services indicates it is a Nursing Facility (048, 044, or 046). | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT149-0006 | |||
| 1448 | CLT149 | NURSING-FACILITY-DAYS | If TYPE-OF-SERVICE = Nursing Facility services (048, 044, or 046), then NURSING-FACILITY-DAYS must be greater than LEAVE-DAYS. |
10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT149-0007 | |||
| 1449 | CLT149 | NURSING-FACILITY-DAYS | If NURSING-FACILITY-DAYS is greater than zero and less than 88887 then LEVEL-OF-CARE-STATUS in EL for the associated MSIS-IDENTIFIER must be Nursing Facility for the same month as the begin and end date of service. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT149-0008 | |||
| 1450 | CLT150 | SPLIT-CLAIM-IND | An indicator that denotes that claims in excess of a pre-determined number of claim lines (threshold determined by the individual state) will be split during processing. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 9 Unknown |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT150-0001 |
| 1451 | CLT150 | SPLIT-CLAIM-IND | If the claim has been split, the Transaction Handling Code indicator will indicate a Split Payment and Remittance (1000 BPR01 = U). | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT150-0002 | |||
| 1452 | CLT151 | BORDER-STATE-IND | This code indicates whether an individual received services or equipment across state borders. (The provider location is out of state, but for payment purposes the provider is treated as an in-state provider.) | Conditional | Value must be equal to a valid value. | 0 No 1 Yes |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT151-0001 |
| 1453 | CLT153 | BENEFICIARY-COINSURANCE-AMOUNT | The amount of money the beneficiary paid towards coinsurance. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT153-0001 | |
| 1454 | CLT153 | BENEFICIARY-COINSURANCE-AMOUNT | If no coinsurance is applicable enter 0.00 | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT153-0002 | |||
| 1455 | CLT154 | BENEFICIARY-COINSURANCE-DATE-PAID | The date the beneficiary paid the coinsurance amount. | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT154-0001 | |
| 1456 | CLT154 | BENEFICIARY-COINSURANCE-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT154-0002 | |||
| 1457 | CLT154 | BENEFICIARY-COINSURANCE-DATE-PAID | If no coinsurance is applicable, 8-fill | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT154-0003 | |||
| 1458 | CLT155 | BENEFICIARY-COPAYMENT-AMOUNT | The amount of money the beneficiary paid towards a copayment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT155-0001 | |
| 1459 | CLT155 | BENEFICIARY-COPAYMENT-AMOUNT | If no copayment is applicable enter 0.00 | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT155-0002 | |||
| 1460 | CLT156 | BENEFICIARY-COPAYMENT-DATE-PAID | The date the beneficiary paid the copayment amount. | Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT156-0001 | |
| 1461 | CLT156 | BENEFICIARY-COPAYMENT-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT156-0002 | |||
| 1462 | CLT156 | BENEFICIARY-COPAYMENT-DATE-PAID | If no coinsurance is applicable, 8-fill | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT156-0003 | |||
| 1463 | CLT157 | BENEFICIARY-DEDUCTIBLE-AMOUNT | The amount of money the beneficiary paid towards an annual deductible. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT157-0001 | |
| 1464 | CLT157 | BENEFICIARY-DEDUCTIBLE-AMOUNT | If no deductible is applicable enter 0.00 | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT157-0002 | |||
| 1465 | CLT158 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | The date the beneficiary paid the deductible amount. | Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT158-0001 | |
| 1466 | CLT158 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT158-0002 | |||
| 1467 | CLT158 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | If no coinsurance is applicable, 8-fill | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT158-0003 | |||
| 1468 | CLT159 | CLAIM-DENIED-INDICATOR | An indicator to identify a claim that the state refused pay in its entirety. | Conditional | Value must be equal to a valid value. | 0 Denied: The payment of claim in its entirety was denied by the state. 1 Not Denied: The state paid some or all of the claim. |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT159-0001 |
| 1469 | CLT159 | CLAIM-DENIED-INDICATOR | It is expected that states will submit all denied claims to CMS. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT159-0002 | |||
| 1470 | CLT159 | CLAIM-DENIED-INDICATOR | If the Type of Claim indicates the claim was denied, then this indicator must also indicate the claim was denied. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT159-0003 | |||
| 1471 | CLT160 | COPAY-WAIVED-IND | An indicator signifying that the copay was waived by the provider. | Optional | Value must be equal to a valid value. | 0 Not Waived: The provider did not waive the beneficiary’s copayment 1 Waived: The provider waived the beneficiary’s copayment 8 Not Applicable: The benefit plan does not have a copay in this circumstance |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT160-0001 |
| 1472 | CLT161 | HEALTH-HOME-ENTITY-NAME | A free-form text field to indicate the health home that authorized payment for the service on the claim. The name entered should be the name that the state uses to uniquely identify the team. A “Health Home Entity” can be a designated provider (e.g., physician, clinic, behavioral health organization), a health team which links to a designated provider, or a health team (physicians, nurses, behavioral health professionals). Because an identification numbering schema has not been established, the entities’ names are being used instead. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT161-0001 | |
| 1473 | CLT161 | HEALTH-HOME-ENTITY-NAME | States should not submit records for an eligible individual where the eligible's health home entity name does not match in the associated claim record, if applicable. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT161-0002 | |||
| 1474 | CLT163 | THIRD-PARTY-COINSURANCE-AMOUNT-PAID | The amount of money paid by a third party on behalf of the beneficiary towards coinsurance on the claim or claim line item. | Optional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT163-0001 | |
| 1475 | CLT164 | THIRD-PARTY-COINSURANCE-DATE-PAID | The date the third party paid the coinsurance amount. | Optional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT164-0001 | |
| 1476 | CLT164 | THIRD-PARTY-COINSURANCE-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT164-0002 | |||
| 1477 | CLT165 | THIRD-PARTY-COPAYMENT-AMOUNT-PAID | The amount the third party paid toward the copayment amount. | Optional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT165-0001 | |
| 1478 | CLT166 | THIRD-PARTY-COPAYMENT-DATE-PAID | The date the third party paid the copayment amount | Optional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT166-0001 | |
| 1479 | CLT166 | THIRD-PARTY-COPAYMENT-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT166-0002 | |||
| 1480 | CLT167 | HEALTH-HOME-PROVIDER-NPI | The National Provider ID (NPI) of the health home provider. | Conditional | The value must be a valid NPI | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT167-0001 |
| 1481 | CLT167 | HEALTH-HOME-PROVIDER-NPI | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT167-0002 | |||
| 1482 | CLT168 | MEDICARE-BENEFICIARY-IDENTIFIER | The individual’s Medicare Beneficiary Identifier (MBI) Identification Number. Note: MBI replaces the HICN with an entirely new Medicare Beneficiary Identifier (MBI) for purposes of provider billing, if applicable. CMS interfaces with non-payment exchange partners would remain HICN-based, while interfaces with payment partners would use the new MBI. |
NA | Valid characters in the text string are limited to alpha characters (A-Z, a-z) and numbers (0-9) | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT168-0001 | |
| 1483 | CLT168 | MEDICARE-BENEFICIARY-IDENTIFIER | If individual is NOT enrolled in Medicare, 8-fill field | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT168-0002 | |||
| 1484 | CLT168 | MEDICARE-BENEFICIARY-IDENTIFIER | Field should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files) until such time as the Medicare Beneficiary Identifier is implemented (no target date has been established). | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT168-0003 | |||
| 1485 | CLT169 | UNDER-DIRECTION-OF-PROV-NPI | The National Provider ID (NPI) of the provider who directed the care of a patient that another provider administered. | NA | The value must be a valid NPI | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT169-0001 |
| 1486 | CLT169 | UNDER-DIRECTION-OF-PROV-NPI | Field should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). This data element is a duplicate of the “Under-Supervision-of-Prov-NPI” field and as such do not need to be populated. | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT169-0002 | |||
| 1487 | CLT170 | UNDER-DIRECTION-OF-PROV-TAXONOMY | The Provider Taxonomy of the provider who directed the care of a patient that another provider administered. | NA | Must be in the set of valid values | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT170-0001 |
| 1488 | CLT170 | UNDER-DIRECTION-OF-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT170-0002 | |||
| 1489 | CLT170 | UNDER-DIRECTION-OF-PROV-TAXONOMY | Left-fill unused bytes with spaces | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT170-0003 | |||
| 1490 | CLT170 | UNDER-DIRECTION-OF-PROV-TAXONOMY | Field should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). This data element is a duplicate of the “Under-Supervision-of-Prov-Taxonomy” field and as such do not need to be populated. | 9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT170-0004 | |||
| 1491 | CLT171 | UNDER-SUPERVISION-OF-PROV-NPI | The National Provider ID (NPI) of the provider who supervised another provider. | NA | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | ||
| 1492 | CLT171 | UNDER-SUPERVISION-OF-PROV-NPI | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT171-0002 | |||
| 1493 | CLT172 | UNDER-SUPERVISION-OF-PROV-TAXONOMY | The Provider Taxonomy of the provider who supervised another provider. | NA | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT172-0001 |
| 1494 | CLT172 | UNDER-SUPERVISION-OF-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT172-0002 | |||
| 1495 | CLT172 | UNDER-SUPERVISION-OF-PROV-TAXONOMY | Left-fill unused bytes with spaces | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT172-0003 | |||
| 1496 | CLT174 | ADMITTING-PROV-NPI-NUM | The National Provider ID (NPI) of the doctor responsible for admitting a patient to a hospital or other inpatient health facility. | Conditional | Valid characters include only numbers (0-9) | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT174-0001 | |
| 1497 | CLT174 | ADMITTING-PROV-NPI-NUM | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT174-0002 | ||
| 1498 | CLT174 | ADMITTING-PROV-NPI-NUM | IF TYPE-OF-SERVICE= "119", "120", "121", or "122", then ADMITTING-PROV-NPI-NUM should be blank. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT174-0004 | |||
| 1499 | CLT175 | ADMITTING-PROV-NUM | The Medicaid ID of the doctor responsible for admitting a patient to a hospital or other inpatient health facility. | Required | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT175-0001 |
| 1500 | CLT175 | ADMITTING-PROV-NUM | If value is invalid, record it exactly as it appears in the state system | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT175-0002 | |||
| 1501 | CLT175 | ADMITTING-PROV-NUM | Note: Once a national provider ID numbering system is in place, the national number should be used. If the State’s legacy ID number is also available then that number can be entered in this field. |
2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT175-0003 | |||
| 1502 | CLT176 | ADMITTING-PROV-SPECIALTY | This code describes the area of specialty for the admitting provider. | Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT176-0001 |
| 1503 | CLT177 | ADMITTING-PROV-TAXONOMY | The taxonomy code for the admitting provider. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT177-0001 |
| 1504 | CLT177 | ADMITTING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT177-0002 | |||
| 1505 | CLT178 | ADMITTING-PROV-TYPE | A code describing the type of admitting provider. If the state uses state-specific codes, they should map their internal codes to the CMS standard list provided. |
Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT178-0001 |
| 1506 | CLT179 | MEDICARE-PAID-AMT | The amount paid by Medicare on this claim or adjustment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT179-0001 | |
| 1507 | CLT179 | MEDICARE-PAID-AMT | If the service was covered by Medicare but Medicare had no liability for the bill, zero-fill. MEDICARE-PAID-AMT should reflect the actual amount paid by Medicare. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT179-0002 | |||
| 1508 | CLT179 | MEDICARE-PAID-AMT | For claims where Medicare payment is only available at the header level, report the entire payment amount the T-MSIS record corresponding to the line item with the highest charge. Zero fill Medicare Amount Paid on all other T-MSIS records created from the original claim. | 2/25/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT179-0003 | |||
| 1509 | CLT179 | MEDICARE-PAID-AMT | Claims records for an eligible individual should not indicate Medicare paid any amount on the claim, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT179-0004 | |||
| 1510 | CLT173 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT173-0001 | |
| 1511 | CLT173 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT173-0002 | |||
| 1512 | CLT237 | PROV-LOCATION-ID | A code to uniquely identify the geographic location where the provider’s services were performed. The value should correspond to an active value in the PROV-LOCATION-ID field in the provider subject area. | Required | Limit characters to alphabet (A-Z), numerals (0-9).. | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT237-0001 | |
| 1513 | CLT237 | PROV-LOCATION-ID | The value should correspond with one of the location identifiers recorded in the provider’s demographic records in the T-MSIS data set | 10/10/2013 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT237-0002 | |||
| 1514 | CLT183 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | CLAIMLT | CLAIM-HEADER-RECORD-LT-CLT00002 | CLT183-0001 | |||
| 1515 | CLT184 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the CLAIM-HEADER-RECORD-IP record segment is CIP00002 | Required | Value must be equal to a valid value. | CLT00003- CLAIM-LINE-RECORD-LT | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT184-0001 |
| 1516 | CLT184 | RECORD-ID | Must be populated on every record | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT184-0002 | |||
| 1517 | CLT184 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT184-0003 | |||
| 1518 | CLT185 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT185-0001 |
| 1519 | CLT185 | SUBMITTING-STATE | Must be populated on every record. | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT185-0002 | |||
| 1520 | CLT185 | SUBMITTING-STATE | Value must be numeric |
4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT185-0003 | |||
| 1521 | CLT185 | SUBMITTING-STATE | SUBMITTING-STATE must be equal across all record segments for a given record. | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT185-0004 | |||
| 1522 | CLT186 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT186-0001 | |
| 1523 | CLT186 | RECORD-NUMBER | Must be numeric | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT186-0002 | |||
| 1524 | CLT186 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT186-0004 | |||
| 1525 | CLT187 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Conditional | MSIS Identification Number must be reported | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT187-0001 | |
| 1526 | CLT187 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state ID numbers must be supplied to CMS | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT187-0002 | |||
| 1527 | CLT187 | MSIS-IDENTIFICATION-NUM | For TYPE-OF-CLAIM = 4 or D (lump sum adjustments), this field must begin with an ‘&’. | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT187-0003 | |||
| 1528 | CLT187 | MSIS-IDENTIFICATION-NUM | For SSN states, this field must contain the Eligible's Social Security Number. If the SSN is unknown and a temporary number is assigned, this field will contain that number. | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT187-0004 | |||
| 1529 | CLT188 | ICN-ORIG | A unique number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies an original claim. | Required | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT188-0001 | |
| 1530 | CLT188 | ICN-ORIG | Record the value exactly as it appears in the State system. Do not pad. | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT188-0002 | |||
| 1531 | CLT188 | ICN-ORIG | This field should always be populated with the claim identification number assigned to the original paid/denied claim. This identification number should remain constant and be carried forward onto any adjustment claims. The intention is for this earliest claim identification number to be the link that ties the original claim and all adjustment claims together. | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT188-0003 | |||
| 1532 | CLT188 | ICN-ORIG | This field should not be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT188-0004 | |||
| 1533 | CLT189 | ICN-ADJ | A unique claim number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies the adjustment claim for an original transaction. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT189-0001 | |
| 1534 | CLT189 | ICN-ADJ | Record the value exactly as it appears in the State system. Do not pad. | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT189-0002 | |||
| 1535 | CLT189 | ICN-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT189-0003 | |||
| 1536 | CLT190 | LINE-NUM-ORIG | A unique number to identify the transaction line number that is being reported on the original claim. | Required | Record the value exactly as it appears in the State system. Do not pad. This field should also be completed on adjustment claims to reflect the LINE-NUMBER of the INTERNAL-CONTROL-NUMBER on the claim that is being adjusted. | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT190-0001 | |
| 1537 | CLT191 | LINE-NUM-ADJ | A unique number to identify the transaction line number that identifies the line number on the adjustment ICN. | Conditional | Record the value exactly as it appears in the state system. Do not pad | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT191-0001 | |
| 1538 | CLT191 | LINE-NUM-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0. Otherwise, if there is a line adjustment indicator, then there should be a line adjustment number. |
2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT191-0002 | |||
| 1539 | CLT191 | LINE-NUM-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0. | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT191-0003 | |||
| 1540 | CLT192 | LINE-ADJUSTMENT-IND | Code indicating type of adjustment record claim/encounter represents at claim detail level. | Conditional | Value must be equal to a valid value. | 0 Original Claim/Encounter 1 Void of a prior submission 2 Re-submittal 3 Credit Adjustment (negative supplemental) 4 Debit Adjustment (positive supplemental) 5 Credit Gross Adjustment. 6 Debit Gross Adjustment 9 Unknown |
11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT192-0001 |
| 1541 | CLT192 | LINE-ADJUSTMENT-IND | If there is a line adjustment number, then there must be a line-adjustment indicator. | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT192-0002 | |||
| 1542 | CLT192 | LINE-ADJUSTMENT-IND | If there is a line adjustment reason, then there must be a line adjustment indicator. | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT192-0003 | |||
| 1543 | CLT193 | LINE-ADJUSTMENT-REASON-CODE | Claim adjustment reason codes communicate why a service line was paid differently than it was billed. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-adjustment-reason-codes/ | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT193-0001 |
| 1544 | CLT193 | LINE-ADJUSTMENT-REASON-CODE | If there is no adjustment to a line, then there is no adjustment reason code. (Also see: CLAIM-PYMT-REM-CODE) | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT193-0002 | |||
| 1545 | CLT194 | SUBMITTER-ID | The Submitter ID number is the value that identifies the provider/trading partner/clearing house organization to state’s claim adjudication system. | Conditional | Value must not be null | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT194-0001 | |
| 1546 | CLT195 | CLAIM-LINE-STATUS | The claim line status codes identify the status of a specific detail claim line rather than the entire claim. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-codes/ | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT195-0001 |
| 1547 | CLT196 | BEGINNING-DATE-OF-SERVICE | For services received during a single encounter with a provider, the date the service covered by this claim was received. For services involving multiple encounters on different days or periods of care extending over two or more days, the date on which the service covered by this claim began. For capitation premium payments, the date on which the period of coverage related to this payment began. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT196-0001 | |
| 1548 | CLT196 | BEGINNING-DATE-OF-SERVICE | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT196-0002 | |||
| 1549 | CLT196 | BEGINNING-DATE-OF-SERVICE | The beginning date of service must occur before or be the same as the ending date of service. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT196-0003 | |||
| 1550 | CLT196 | BEGINNING-DATE-OF-SERVICE | The beginning date of service must occur before or be the same as the end of time period. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT196-0004 | |||
| 1551 | CLT196 | BEGINNING-DATE-OF-SERVICE | Date must occur before or be the same as adjudication date. | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT196-0005 | |||
| 1552 | CLT196 | BEGINNING-DATE-OF-SERVICE | Date must occur on or before Date of Death. | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT196-0006 | |||
| 1553 | CLT196 | BEGINNING-DATE-OF-SERVICE | Date must occur on or after Date of Birth | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT196-0007 | |||
| 1554 | CLT196 | BEGINNING-DATE-OF-SERVICE | A Medicaid claim record for an eligible individual, if applicable, cannot have a Beginning Date of Service after the eligible individual's Medicaid enrollment has ended. | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT196-0008 | |||
| 1555 | CLT196 | BEGINNING-DATE-OF-SERVICE | A CHIP claim record for an individual eligible for separate CHIP cannot have a Beginning Date of Service after the eligible individual's CHIP enrollment has ended. | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT196-0009 | |||
| 1556 | CLT197 | ENDING-DATE-OF-SERVICE | For services received during a single encounter with a provider, the date the service covered by this claim was received. For services involving multiple encounters on different days, or periods of care extending over two or more days, the date on which the service covered by this claim ended. For capitation premium payments, the date on which the period of coverage related to this payment ends/ended. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT197-0001 | |
| 1557 | CLT197 | ENDING-DATE-OF-SERVICE | Value must be a valid date | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT197-0002 | |||
| 1558 | CLT197 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must occur after or be the same as the BEGINNING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT197-0003 | |||
| 1559 | CLT197 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must be on or before the ADJUDICATION-DATE. | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT197-0004 | |||
| 1560 | CLT197 | ENDING-DATE-OF-SERVICE | Date must occur on or before Date of Death, when a DATE-OF-DEATH is not unknown or not applicable. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT197-0005 | |||
| 1561 | CLT197 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must be on or after DATE-OF-BIRTH | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT197-0006 | |||
| 1562 | CLT197 | ENDING-DATE-OF-SERVICE | Date must occur before or be the same as End of Time Period. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT197-0007 | |||
| 1563 | CLT198 | REVENUE-CODE | A code which identifies a specific accommodation, ancillary service or billing calculation (as defined by UB-04 Billing Manual). | Required | Only valid codes as defined by the “National Uniform Billing Committee” should be used. | Revenue code is a data set that health care providers or insurers usually pay for to use. These values will change annually. | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT198-0001 |
| 1564 | CLT198 | REVENUE-CODE | Enter all UB-04 Revenue Codes listed on the claim | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT198-0002 | |||
| 1565 | CLT198 | REVENUE-CODE | Value must be a valid code | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT198-0003 | |||
| 1566 | CLT198 | REVENUE-CODE | If value invalid, record it exactly as it appears in the state system | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT198-0004 | |||
| 1567 | CLT201 | IMMUNIZATION-TYPE | This field identifies the type of immunization provided in order to track additional detail not currently contained in CPT codes. | Conditional | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT201-0001 |
| 1568 | CLT202 | IP-LT-QUANTITY-OF-SERVICE-ACTUAL | On facility claim entries, this field is to capture the actual service quantify by revenue code category, e.g., number of days in a particular type of accommodation, pints of blood, etc. However, when HCPCS codes are required for services, the units are equal to the number of times the procedure/service being reported was performed. | Must be numeric | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT202-0001 | ||
| 1569 | CLT202 | IP-LT-QUANTITY-OF-SERVICE-ACTUAL | This field is only applicable when the service being billed can be quantified in discrete units, e.g., a number of visits or the number of units of a prescription/refill that were filled | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT202-0002 | |||
| 1570 | CLT202 | IP-LT-QUANTITY-OF-SERVICE-ACTUAL | For use with CLAIMIP and CLAIMLT claims. For CLAIMOT and CLAIMRX claims/encounter records, use the OT-RX-CLAIM-QUANTITY-ACTUAL field | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT202-0003 | |||
| 1571 | CLT203 | IP-LT-QUANTITY-OF-SERVICE-ALLOWED | On facility claim entries, this field is to capture maximum allowable quantity by revenue code category, e.g., number of days in a particular type of accommodation, pints of blood, etc. However, when HCPCS codes are required for services, the units are equal to the number of times the procedure/service being reported was performed. | Must be numeric | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT203-0001 | ||
| 1572 | CLT203 | IP-LT-QUANTITY-OF-SERVICE-ALLOWED | This field is only applicable when the service being billed can be quantified in discrete units, e.g., a number of visits or the number of units of a prescription/refill that were filled | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT203-0002 | |||
| 1573 | CLT203 | IP-LT-QUANTITY-OF-SERVICE-ALLOWED | For use with CLAIMIP and CLAIMLT claims. For CLAIMOT and CLAIMRX claims/encounter records, use the OT-RX-CLAIM-QUANTITY-ACTUAL field | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT203-0003 | |||
| 1574 | CLT204 | REVENUE-CHARGE | The total charge for the related UB-04 Revenue Code (REVENUE-CODE) for the billing period. Total charges include both covered and non-covered charges (as defined by UB-04 Billing Manual. | Required | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT204-0001 | |
| 1575 | CLT204 | REVENUE-CHARGE | Enter charge for each UB-04 Revenue Code listed on the claim | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT204-0002 | |||
| 1576 | CLT204 | REVENUE-CHARGE | The total amount should be the sum of each of the charged amounts submitted at the claim detail level | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT204-0003 | |||
| 1577 | CLT204 | REVENUE-CHARGE | If TYPE-OF-CLAIM = 3, C, W (encounter record) this field should either be zero-filled or contain the amount paid by the plan to the provider. If TYPE-OF-SERVICE =119, 120, or 122, this field should be “00000000" filled.” | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT204-0004 | |||
| 1578 | CLT204 | REVENUE-CHARGE | The absolute value of the sum of claim line charges (REVENUE-CHARGE) must be less than or equal to absolute value of TOT-BILLED-AMT. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT204-0005 | |||
| 1579 | CLT204 | REVENUE-CHARGE | Value must be 8-filled if the revenue code is 8-filled. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT204-0006 | |||
| 1580 | CLT204 | REVENUE-CHARGE | Value must not be 8-filled if the revenue code is not 8-filled. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT204-0007 | |||
| 1581 | CLT205 | ALLOWED-AMT | The maximum amount displayed at the claim line level as determined by the payer as being "allowable" under the provisions of the contract prior to the determination of actual payment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT205-0001 | |
| 1582 | CLT206 | TPL-AMT | Third Party Liability (TPL) refers to the legal obligation of third parties, i.e., certain individuals, entities, or programs, to pay all or part of the expenditures for medical assistance furnished under a state plan. This is the total amount denoted at the claim detail level paid by the third party. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT206-0001 | |
| 1583 | CLT207 | OTHER-INSURANCE-AMT | The amount paid by insurance other than Medicare or Medicaid on this claim. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT207-0001 | |
| 1584 | CLT208 | MEDICAID-PAID-AMT | The amount paid by Medicaid on this claim or adjustment at the claim detail level. | Required | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT208-0001 | |
| 1585 | CLT208 | MEDICAID-PAID-AMT | For claims where Medicaid payment is only available at the header level, report the entire payment amount on the MSIS record corresponding to the line item with the highest charge. Zero fill Medicaid Amount Paid on all other MSIS records created from the original claim. | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT208-0002 | |||
| 1586 | CLT208 | MEDICAID-PAID-AMT | For Crossover claims with Medicare Coinsurance and/or Deductibles, enter the sum of those amounts in the Medicaid-Amount-Paid field, if the providers were reimbursed by Medicaid for them. If the Coinsurance and Deductibles were not paid by the state, then report the Medicaid-Paid-Amt as $0 | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT208-0003 | |||
| 1587 | CLT209 | MEDICAID-FFS-EQUIVALENT-AMT | The MEDICAID-FFS-EQUIVALENT-AMT field should be populated with the amt that would have been paid had the services been provided on a FFS basis. | Conditional | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT209-0001 | |
| 1588 | CLT209 | MEDICAID-FFS-EQUIVALENT-AMT | Required when TYPE-OF-CLAIM = C, 3, or W | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT209-0002 | |||
| 1589 | CLT210 | BILLING-UNIT | Unit of billing that is used for billing services by the facility. | Conditional | Value must be equal to a valid value. | 01 Per Day 02 Per Hour 03 Per Case 04 Per Encounter 05 Per Week 06 Per Month 07 Other Arrangements 99 Unknown |
11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT210-0001 |
| 1590 | CLT211 | TYPE-OF-SERVICE | A code to categorize the services provided to a Medicaid or CHIP enrollee. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT211-0001 |
| 1591 | CLT211 | TYPE-OF-SERVICE | All claims for inpatient psychiatric care provided in a separately administered psychiatric wing or psychiatric hospital are included in the CLAIMLTfile. | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT211-0002 | |||
| 1592 | CLT211 | TYPE-OF-SERVICE | Experience has demonstrated there can be instances when more than one service area category could be applicable for a provided service. The following hierarchy rules apply to these instances: The specific service categories of sterilizations and other pregnancy-related procedures take precedence over provider categories, such as inpatient hospital or outpatient hospital. Services of a physician employed by a clinic are reported under clinic services if the clinic is the billing entity. X-rays processed by the clinic in the course of treatment, however, are reported under X-ray services. Services of a registered nurse attending a resident in a NF are reported (if they qualified under the coverage rules) under home health services if they were not billed as part of the NF bill. |
2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT211-0003 | |||
| 1593 | CLT211 | TYPE-OF-SERVICE | See Appendix D for information on the various types of service. |
2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT211-0004 | |||
| 1594 | CLT211 | TYPE-OF-SERVICE | Long Term Care Claims/Encounters File - Claims/encounters with TYPE-OF-SERVICE = 009, 044, 045, 046, 047, 048, 050, 059, or 133 (all mental hospital, and NF services). (Note: Individual services billed by a long-term care facility belong in this file regardless of service type.) |
9/23/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT211-0005 | |||
| 1595 | CLT212 | SERVICING-PROV-NUM | A unique number to identify the provider who treated the recipient. |
Required | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT212-0001 |
| 1596 | CLT212 | SERVICING-PROV-NUM | If value is invalid, record it exactly as it appears in the state system. | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT212-0002 | |||
| 1597 | CLT212 | SERVICING-PROV-NUM | If “Servicing” provider and the “Billing” provider are the same then use the same number in both fields. |
2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT212-0003 | |||
| 1598 | CLT212 | SERVICING-PROV-NUM | Note: Once a national provider ID numbering system is in place, the national number should be used. If only the state’s legacy ID number is available then that number can be entered in this field. |
2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT212-0004 | |||
| 1599 | CLT212 | SERVICING-PROV-NUM | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122). | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT212-0005 | |||
| 1600 | CLT213 | SERVICING-PROV-NPI-NUM | The NPI of the health care professional who delivers or completes a particulay medical service or non-surgical procedure. The SERVICING-PROV-NPI-NUM is required when rendering provider is different than the attending provider and state or federal regulatory requirements call for a "combined claim" (i.e., a claim that includes both facility and professional components). Examples are Medicaid clinic bills or critical access hospital claims. | Conditional | Valid characters include only numbers (0-9) | 11/9/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT213-0001 | |
| 1601 | CLT213 | SERVICING-PROV-NPI-NUM | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT213-0002 | ||
| 1602 | CLT213 | SERVICING-PROV-NPI-NUM | The field should be blank if the transaction is for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122). | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT213-0004 | |||
| 1603 | CLT214 | SERVICING-PROV-TAXONOMY | The taxonomy code for the institution billing/caring for the beneficiary. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT214-0001 |
| 1604 | CLT214 | SERVICING-PROV-TAXONOMY | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122) | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT214-0002 | |||
| 1605 | CLT214 | SERVICING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion. | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT214-0003 | |||
| 1606 | CLT215 | SERVICING-PROV-TYPE | A code describing the type of provider (i.e. doctor or facility) responsible for treating a patient. This represents the attending physician if available. If the state uses state-specific codes, they should map their internal codes to the CMS standard list provided. |
Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values. | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT215-0001 |
| 1607 | CLT216 | SERVICING-PROV-SPECIALTY | This code indicates the area of specialty for the servicing provider. | Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT216-0001 |
| 1608 | CLT217 | OTHER-TPL-COLLECTION | This data element indicates that the claim is for a beneficiary for whom other third party resource development and collection activities are in progress, when the liability is not another health insurance plan for which the eligible is a beneficiary. | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 Third Party Resource is Casualty/Tort 002 Third Party Resource is Estate 003 Third Party Resource is Lien (TEFRA) 004 Third Party Resource is Lien (Other) 005 Third Party Resource is Worker’s Compensation 006 Third Party Resource is Medical Malpractice 007 Third Party Resource is Other 999 Classification of Third Party Resource is Unknown |
11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT217-0001 |
| 1609 | CLT218 | BENEFIT-TYPE | The benefit category corresponding to the service reported on the claim or encounter record. Note: The code definitions in the valid value list originate from the Medicaid and CHIP Program Data System’s (MACPro’s) benefit type list. See Appendix H: Benefit Types for descriptions of the categories. |
Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 2/25/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT218-0001 |
| 1610 | CLT219 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | This code indicates if the claim was matched with Title XIX or Title XXI. | Required | Value must be equal to a valid value. | 01 Federal funding under Title XIX 02 Federal funding under Title XXI 03 Federal funding under ACA 04 Federal funding under other legislation |
10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT219-0001 |
| 1611 | CLT219 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | If an individual is not eligible for S-CHIP, then any associated claims records should not have reimbursed with federal funding under Title XXI. | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT219-0002 | |||
| 1612 | CLT219 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | If an individual is not eligible for Medicaid, then any associated claims records should not have reimbursed with federal funding under Title XIX. | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT219-0003 | |||
| 1613 | CLT221 | PROV-FACILITY-TYPE | The type of facility for the servicing provider using the HIPAA provider taxonomy codes. | Required | A value is required for CLAIMLT records | See Appendix A for listing of valid values. See Appendix N for Crosswalk of Provider Taxonomy Codes to Provider Facility Type Categories. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT221-0001 |
| 1614 | CLT224 | XIX-MBESCBES-CATEGORY-OF-SERVICE | A code indicating the category of service for the paid claim. The category of service is the line item from the CMS-64 form that states use to report their expenditures and request federal financial participation | Conditional | Value must be equal to a valid value. | See Appendix I for listing of valid values. | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT224-0001 |
| 1615 | CLT224 | XIX-MBESCBES-CATEGORY-OF-SERVICE | Males cannot receive services where the category of service is "Other Pregnancy-related Procedures", "Nurse Mid-wife", "Freestanding Birth Center" or "Tobacco Cessation for Pregnant Women". | 4/30/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT224-0002 | |||
| 1616 | CLT225 | XXI-MBESCBES-CATEGORY-OF-SERVICE | A code indicating the category of service for the paid claim. The category of service is the line item from the CMS-21 form that states use to report their expenditures and request federal financial participation. Refer to Attachment 8 for definitions on the various categories of service. | Conditional | Value must be equal to a valid value. | See Appendix J for listing of valid values. | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT225-0001 |
| 1617 | CLT226 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT226-0001 | |
| 1618 | CLT226 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT226-0002 | |||
| 1619 | CLT228 | NATIONAL-DRUG-CODE | A code in National Drug Code (NDC) format indicating the drug, device, or medical supply covered by this claim. | Conditional | Position 10-12 must be Alpha Numeric or blank | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT228-0001 | |
| 1620 | CLT228 | NATIONAL-DRUG-CODE | Position 1-5 must be Numeric | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT228-0002 | |||
| 1621 | CLT228 | NATIONAL-DRUG-CODE | Position 6-9 must be Alpha Numeric | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT228-0003 | |||
| 1622 | CLT228 | NATIONAL-DRUG-CODE | Drug code formats must be supplied by State in advance of submitting any file data. States must inform CMS of the NDC segments used and their size (e.g., {5, 4, 2} or {5, 4} as defined in the National Drug Code Directory). | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT228-0004 | |||
| 1623 | CLT228 | NATIONAL-DRUG-CODE | If the Drug Code is less than 11 characters in length, the value must be left justified and padded with spaces. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT228-0005 | |||
| 1624 | CLT228 | NATIONAL-DRUG-CODE | If Durable Medical Equipment or supply is prescribed by a physician and provided by a pharmacy then HCPCS or state specific codes can be put in the NDC field. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT228-0006 | |||
| 1625 | CLT228 | NATIONAL-DRUG-CODE | This field is applicable for pharmacy/drug and DME services that are provided to Medicaid/CHIP recipients living in a long-term care facility. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT228-0007 | |||
| 1626 | CLT229 | NDC-UNIT-OF-MEASURE | A code to indicate the basis by which the quantity of the National Drug Code is expressed. |
Conditional | Value must be equal to a valid value. Valid Value Definition: F2 International Unit GR Gram ME Milligram ML Milliliter UN Unit |
F2 International Unit ML Milliliter GR Gram UN Unit |
11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT229-0001 |
| 1627 | CLT229 | NDC-UNIT-OF-MEASURE | Enter the unit of measure for each corresponding quantity value. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT229-0002 | |||
| 1628 | CLT230 | NDC-QUANTITY | This field is to capture the actual quantity of the National Drug Code being prescribed on this long term care claim. | Conditional | Must be numeric | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT230-0001 | |
| 1629 | CLT230 | NDC-QUANTITY | This field is only applicable when the NDC code being billed can be quantified in discrete units, e.g., the number of units of a prescription/refill that were filled. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT230-0002 | |||
| 1630 | CLT231 | HCPCS-RATE | For inpatient hospital facility claims, the accommodation rate is captured here. This data element is expected to capture data from the HIPAA 837I claim loop 2400 SV206 or UB-04 FL 44 (only if the value represents an accommodation rate) | Conditional | Must be numeric | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT231-0001 | |
| 1631 | CLT233 | ADJUDICATION-DATE | The date on which the payment status of the claim was finally adjudicated by the state. | Required | Date format is CCYYMMDD (National Data Standard). | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT233-0001 | |
| 1632 | CLT233 | ADJUDICATION-DATE | Value must be a valid date | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT233-0002 | |||
| 1633 | CLT233 | ADJUDICATION-DATE | For Adjustment Records (ADJUSTMENT-INDICATOR<> 0), use date of final adjudication when possible. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT233-0003 | |||
| 1634 | CLT233 | ADJUDICATION-DATE | For Encounter Records (TYPE-OF-CLAIM=3, C, W); use date the encounter was processed by the state. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT233-0004 | |||
| 1635 | CLT233 | ADJUDICATION-DATE | If a complete, valid date is not available or is unknown, 9-fil | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT233-0005 | |||
| 1636 | CLT233 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or before END-OF-TIME-PERIOD included in the T-MSIS HEADER RECORD | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT233-0006 | |||
| 1637 | CLT233 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or after the ADMISSION-DATE | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT233-0007 | |||
| 1638 | CLT233 | ADJUDICATION-DATE | This date must occur on or after the DATE-OF-BIRTH in the Eligible Record. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT233-0008 | |||
| 1639 | CLT233 | ADJUDICATION-DATE | A Medicaid or CHIP eligible individual should not have had a claim adjudicated before their five-year immigration ineligible status has expired, except when the eligible is an unborn child in the CHIP program. | 10/10/2013 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT233-0009 | |||
| 1640 | CLT234 | SELF-DIRECTION-TYPE | This data element is not applicable to this file type. | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 Hiring Authority 002 Budget Authority 003 Hiring and Budget Authority 999 Type of Authority Is Unknown |
11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT234-0001 |
| 1641 | CLT235 | PRE-AUTHORIZATION-NUM | A number, code or other value that indicates the services provided on this claim have been authorized by the payee or other service organization, or that a referral for services has been approved. (Also called Prior Authorization or Referral Number). | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT235-0001 | |
| 1642 | CLT238 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | CLAIMLT | CLAIM-LINE-RECORD-LT-CLT00003 | CLT238-0001 | |||
| 1643 | COT001 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the CLAIM-HEADER-RECORD-IP record segment is CIP00002 | Required | Value must be equal to a valid value. | COT00001 - FILE-HEADER-RECORD-OT | 4/30/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT001-0001 |
| 1644 | COT001 | RECORD-ID | Must be populated on every record | 4/30/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT001-0002 | |||
| 1645 | COT001 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT001-0003 | |||
| 1646 | COT002 | DATA-DICTIONARY-VERSION | A data element to capture the version of the T-MSIS data dictionary that was used to build the file. | Required | Use the version number specified on the title page of the data dictionary | 2/25/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT002-0001 | |
| 1647 | COT003 | SUBMISSION-TRANSACTION-TYPE | A data element to identify the whether the transactions in the file are original submissions of the data, a resubmission of a previously submitted file, or corrections of edit rejects. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT003-0001 |
| 1648 | COT004 | FILE-ENCODING-SPECIFICATION | A data element to denote whether the file is in fixed length line format or pipe-delimited format. | Required | Value must be equal to a valid value. | FLF - The file follows a fixed length format. PSV - The file follows a pipe-delimited format. |
4/30/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT004-0001 |
| 1649 | COT005 | DATA-MAPPING-DOCUMENT-VERSION | A data element to identify the version of the T-MSIS data mapping document used to build the file. | Required | Use the version number specified on the title page of the data mapping document | 2/25/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT005-0001 | |
| 1650 | COT006 | FILE-NAME | The name identifying the subject area to which the records in its file relate. Each T-MSIS submission file should only contain records for one subject area (i.e., Eligible, Third-party Liability, Provider, Managed Care Plan Information, IP claims, LT claims, Rx claims, or OT claims). | Required | Value must be equal to a valid value. | CLAIM-OT - Other Claims/Encounters File - Claims/encounters with any TYPE-OF-SERVICE code 002, 003, 004, 005, 006, 007, 008, 010, 011, 012, 013, 014, 015, 016, 017, 018, 019, 020, 021, 022, 025, 026, 027, 028, 029, 030, 031, 032, 035, 036, 037, 039, 040, 041, 043, 051, 052, 053, 054, 056, 060, 061, 062, 063, 064, 065, 066, 067, 068, 069, 073, 074, 075, 076, 077, 078, 079, 080, 081, 082, 083, 087, 115, 119, 120, 121, 122, or 134. | 10/10/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT006-0001 |
| 1651 | COT007 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT007-0001 |
| 1652 | COT007 | SUBMITTING-STATE | Must be populated on every record. | 2/25/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT007-0002 | |||
| 1653 | COT007 | SUBMITTING-STATE | Value must be numeric |
2/25/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT007-0003 | |||
| 1654 | COT007 | SUBMITTING-STATE | SUBMITTING-STATE must be equal across all record segments for a given record. | 2/25/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT007-0004 | |||
| 1655 | COT008 | DATE-FILE-CREATED | The date on which the file was created. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT008-0001 | |
| 1656 | COT008 | DATE-FILE-CREATED | Value must be a valid date | 4/30/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT008-0002 | |||
| 1657 | COT008 | DATE-FILE-CREATED | Date must be equal to or later than the date entered in the END-OF-TIME-PERIOD field. | 4/30/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT008-0003 | |||
| 1658 | COT009 | START-OF-TIME-PERIOD | Beginning date of the time period covered by this file. | Required | Date format is CCYYMMDD (National Data Standard). |
4/30/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT009-0001 | |
| 1659 | COT009 | START-OF-TIME-PERIOD | The date must be a valid date. | 4/30/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT009-0002 | |||
| 1660 | COT010 | END-OF-TIME-PERIOD | Last date of the reporting period covered by the file to which this Header Record is attached. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT010-0001 | |
| 1661 | COT010 | END-OF-TIME-PERIOD | Value must be a valid date | 4/30/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT010-0002 | |||
| 1662 | COT011 | FILE-STATUS-INDICATOR | A code to indicate whether the records in the file are test or production records. | Required | Value must be equal to a valid value. | P Production File T Test File |
2/25/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT011-0001 |
| 1663 | COT012 | SSN-INDICATOR | Indicates whether the state uses the eligible person's social security number (SSN) instead of an MSIS identification number as the unique, unchanging eligible person identifier. | Required | Value must be equal to a valid value. | 0 State does not use SSN as MSIS-IDENTIFICATION-NUMBER 1 State uses SSN as MSIS-IDENTIFICATION-NUMBER |
4/30/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT012-0001 |
| 1664 | COT012 | SSN-INDICATOR | A state's SSN/Non-SSN designation on the eligibility file should match on the claims files. | 4/30/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT012-0002 | |||
| 1665 | COT012 | SSN-INDICATOR | States that are non SSN states must not submit MSIS Identification Numbers and SSNs that match for eligible individuals. | 4/30/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT012-0003 | |||
| 1666 | COT013 | TOT-REC-CNT | A count of all records in the file except for the file header record. This count will be used as a control total to help assure that the file did not become corrupted during transmission. | Required | An integer value with no commas | 10/10/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT013-0001 | |
| 1667 | COT216 | SEQUENCE-NUMBER | To enable state’s to sequentially number files, when related, follow-on files are necessary (i.e., update files, replacement files). This should begin with 1 for the original Create submission type and be incremented by one for each Replacement or Update submission for the same reporting period and file type (subject area). | Required | Field is required on all 'C', 'U', and 'R' record files. | 10/10/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT216-0001 | |
| 1668 | COT216 | SEQUENCE-NUMBER | Must be numeric and > 0 | 10/10/2013 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT216-0002 | |||
| 1669 | COT014 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT014-0001 | |
| 1670 | COT014 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT014-0002 | |||
| 1671 | COT015 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | CLAIMOT | FILE-HEADER-RECORD-OT-COT00001 | COT015-0001 | |||
| 1672 | COT016 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the CLAIM-HEADER-RECORD-IP record segment is CIP00002 | Required | Value must be equal to a valid value. | COT00002 - CLAIM-HEADER-RECORD-OT | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT016-0001 |
| 1673 | COT016 | RECORD-ID | Must be populated on every record | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT016-0002 | |||
| 1674 | COT016 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT016-0003 | |||
| 1675 | COT017 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT017-0001 |
| 1676 | COT017 | SUBMITTING-STATE | Must be populated on every record. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT017-0002 | |||
| 1677 | COT017 | SUBMITTING-STATE | Value must be numeric |
4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT017-0003 | |||
| 1678 | COT017 | SUBMITTING-STATE | SUBMITTING-STATE must be equal across all record segments for a given record. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT017-0004 | |||
| 1679 | COT018 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT018-0001 | |
| 1680 | COT018 | RECORD-NUMBER | Must be numeric | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT018-0002 | |||
| 1681 | COT018 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT018-0004 | |||
| 1682 | COT019 | ICN-ORIG | A unique number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies an original claim. | Required | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT019-0001 | |
| 1683 | COT019 | ICN-ORIG | Record the value exactly as it appears in the State system. Do not pad. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT019-0002 | |||
| 1684 | COT019 | ICN-ORIG | This field should always be populated with the claim identification number assigned to the original paid/denied claim. This identification number should remain constant and be carried forward onto any adjustment claims. The intention is for this earliest claim identification number to be the link that ties the original claim and all adjustment claims together. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT019-0003 | |||
| 1685 | COT019 | ICN-ORIG | This field should not be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT019-0004 | |||
| 1686 | COT020 | ICN-ADJ | A unique claim number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies the adjustment claim for an original transaction. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT020-0001 | |
| 1687 | COT020 | ICN-ADJ | Record the value exactly as it appears in the State system. Do not pad. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT020-0002 | |||
| 1688 | COT020 | ICN-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT020-0003 | |||
| 1689 | COT021 | SUBMITTER-ID | The Submitter ID number is the value that identifies the provider/trading partner/clearing house organization to state’s claim adjudication system. | Conditional | Value must not be null | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT021-0001 | |
| 1690 | COT022 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Conditional | MSIS Identification Number must be reported | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT022-0001 | |
| 1691 | COT022 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state ID numbers must be supplied to CMS | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT022-0002 | |||
| 1692 | COT022 | MSIS-IDENTIFICATION-NUM | For TYPE-OF-CLAIM = 4 or D (lump sum adjustments), this field must begin with an ‘&’. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT022-0003 | |||
| 1693 | COT022 | MSIS-IDENTIFICATION-NUM | For SSN states, this field must contain the Eligible's Social Security Number. If the SSN is unknown and a temporary number is assigned, this field will contain that number. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT022-0004 | |||
| 1694 | COT023 | CROSSOVER-INDICATOR | An indicator specifying whether the claim is a crossover claim where a portion is paid by Medicare. | Required | Value must be equal to a valid value. | 0 Not Crossover Claim 1 Crossover Claim 9 Unknown |
4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT023-0001 |
| 1695 | COT023 | CROSSOVER-INDICATOR | If Crossover Indicator is Yes, there must be Medicare enrollment in the Eligible file for the same time period (by date of service). | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT023-0002 | |||
| 1696 | COT023 | CROSSOVER-INDICATOR | Detail records should be created for all crossover claims. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT023-0003 | |||
| 1697 | COT024 | 1115A-DEMONSTRATION-IND | Indicates that the individual participates in an 1115(A) demonstration. 1115(A) is a Center for Medicare and Medicaid Innovation (CMMI) demonstration. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT024-0001 |
| 1698 | COT024 | 1115A-DEMONSTRATION-IND | If 1115A-DEMONSTRATION-IND set to Yes on claim then there must be a 1115A-DEMONSTRATION-IND set to Yes (1115 participant) in the T-MSIS Eligible file with the same MSIS ID and/or SSN, an 1115A-EFF-DATE < the begin date of service and an 1115A-END-DATE > the end date of service on the claim. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT024-0002 | |||
| 1699 | COT025 | ADJUSTMENT-IND | Code indicating the type of adjustment record. | Required | Value must be equal to a valid value. | 0 Original Claim/Encounter 1 Void of a prior submission 2 Re-submittal 3 Credit Adjustment (negative supplemental) 4 Debit Adjustment (positive supplemental) 5 Credit Gross Adjustment. 6 Debit Gross Adjustment 9 Unknown |
4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT025-0001 |
| 1700 | COT026 | ADJUSTMENT-REASON-CODE | Claim adjustment reason codes communicate why a claim was paid differently than it was billed. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-adjustment-reason-codes/ | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT026-0001 |
| 1701 | COT026 | ADJUSTMENT-REASON-CODE | If there is no adjustment to a claim, then there is no adjustment reason code. (Also see: CLAIM-PYMT-REM-CODE). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT026-0002 | |||
| 1702 | COT027 | DIAGNOSIS-CODE-1 | DIAGNOSIS-CODE-1 through DIAGNOSIS-CODE-2: Primary and Second ICD-9/10-CM code found on the claim. | Required | Code valid ICD-9/10‑CM codes without a decimal point. For example: 210.5 is coded as "2105". | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html" | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT027-0001 |
| 1703 | COT027 | DIAGNOSIS-CODE-1 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT027-0002 | |||
| 1704 | COT027 | DIAGNOSIS-CODE-1 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT027-0003 | |||
| 1705 | COT027 | DIAGNOSIS-CODE-1 | The primary diagnosis code goes into DIAGNOSIS-CODE-1 | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT027-0004 | |||
| 1706 | COT027 | DIAGNOSIS-CODE-1 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT027-0005 | |||
| 1707 | COT027 | DIAGNOSIS-CODE-1 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT027-0006 | |||
| 1708 | COT027 | DIAGNOSIS-CODE-1 | CLAIMOT: Code Specific ICD-9/10-CM code. There are many types of claims that aren’t expected to have diagnosis codes, such as transportation, DME, lab, etc. Do not add vague and unspecified diagnosis codes to those claims. |
2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT027-0007 | |||
| 1709 | COT027 | DIAGNOSIS-CODE-1 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 2 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT027-0008 | |||
| 1710 | COT028 | DIAGNOSIS-CODE-FLAG-1 | CLAIMIP, CLAIMLT, CLAIMOT: A flag that identifies the coding system used for the DIAGNOSIS CODE 1 - 12 CLAIMIP, CLAIMOT, CLAIMOT: DIAGNOSIS-CODE-FLAG-1 through DIAGNOSIS-CODE-FLAG-2: Code flag for the Primary and Second ICD-9/10-CM code found on the claim. |
Required | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT028-0001 |
| 1711 | COT028 | DIAGNOSIS-CODE-FLAG-1 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. |
2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT028-0002 | |||
| 1712 | COT028 | DIAGNOSIS-CODE-FLAG-1 | If DIAGNOSIS-CODE-FLAG-1 through 12 = "2" (ICD-10) should not be used until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT028-0003 | |||
| 1713 | COT028 | DIAGNOSIS-CODE-FLAG-1 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT028-0004 | |||
| 1714 | COT029 | DIAGNOSIS-POA-FLAG-1 | A code to identify conditions that are present at the time the order for inpatient admission occurs – conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT029-0001 |
| 1715 | COT029 | DIAGNOSIS-POA-FLAG-1 | Field should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). The POA (present on admission) flag is only applicable on inpatient claims/encounters. | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT029-0002 | |||
| 1716 | COT029 | DIAGNOSIS-POA-FLAG-1 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT029-0003 | |||
| 1717 | COT030 | DIAGNOSIS-CODE-2 | DIAGNOSIS-CODE-1 through DIAGNOSIS-CODE-2: Primary and Second ICD-9/10-CM code found on the claim | Conditional | Code valid ICD-9/10‑CM codes without a decimal point. For example: 210.5 is coded as "2105". | http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html" | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT030-0001 |
| 1718 | COT030 | DIAGNOSIS-CODE-2 | Limit characters to alphabet (A-Z, a-z), numerals (0-9) and spaces. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT030-0002 | |||
| 1719 | COT030 | DIAGNOSIS-CODE-2 | Include all digits where applicable. ICD-9 codes are up to 5 positions long. ICD-10 codes are up to 7 positions long. Both ICD-9-CM and ICD-10-CM have a minimum length of 3 positions. Embedded blanks are not allowed | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT030-0003 | |||
| 1720 | COT030 | DIAGNOSIS-CODE-2 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT030-0004 | |||
| 1721 | COT030 | DIAGNOSIS-CODE-2 | Enter invalid codes exactly as they appear in the State system. Do not 8-fill or 9-fill these items. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT030-0005 | |||
| 1722 | COT030 | DIAGNOSIS-CODE-2 | CLAIMOT: Code Specific ICD-9/10-CM code. There are many types of claims that aren’t expected to have diagnosis codes, such as transportation, DME, lab, etc. Do not add vague and unspecified diagnosis codes to those claims. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT030-0006 | |||
| 1723 | COT030 | DIAGNOSIS-CODE-2 | Do not report duplicate diagnosis codes across DIAGNOSIS-CODE data elements 1 -2. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT030-0007 | |||
| 1724 | COT030 | DIAGNOSIS-CODE-2 | CMS is not expecting DIAGNOSIS-CODE-FLAG-1 through 2 to be populated with valid value "2" (ICD-10) until until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT030-0008 | |||
| 1725 | COT031 | DIAGNOSIS-CODE-FLAG-2 | CLAIMIP, CLAIMOT, CLAIMOT: A flag that identifies the coding system used for the DIAGNOSIS CODE 1 - 12 CLAIMIP, CLAIMOT, CLAIMOT: DIAGNOSIS-CODE-FLAG-1 through DIAGNOSIS-CODE-FLAG-2: Code flag for the Primary and Second ICD-9/10-CM code found on the claim. |
Conditional | If the diagnosis code is blank-filled, then the corresponding diagnosis code flag should also be blank-filled. Any diagnosis code that IS NOT blank MUST have a diagnosis code flag that is either ‘9’ or ‘0’. | 1 ICD-9 2 ICD-10 3 Other 9 Unknown |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT031-0001 |
| 1726 | COT031 | DIAGNOSIS-CODE-FLAG-2 | For implementation date edits, Beginning Date of Service will be used for OT claims, and Ending Date of Service will be used for IP and LT claims. This is to be in alignment with the Medicare requirements. |
2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT031-0002 | |||
| 1727 | COT031 | DIAGNOSIS-CODE-FLAG-2 | If DIAGNOSIS-CODE-FLAG-1 through 12 = "2" (ICD-10) should not be used until the ICD-10 coding schema is implemented (currently targeted for 10/1/2015). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT031-0003 | |||
| 1728 | COT031 | DIAGNOSIS-CODE-FLAG-2 | All UNUSED diagnosis code flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT031-0004 | |||
| 1729 | COT032 | DIAGNOSIS-POA-FLAG-2 | A code to identify conditions that are present at the time the order for inpatient admission occurs – conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery. POA indicator is used to identify certain preventable conditions that are: (a) high cost or high volume or both, (b) result in the assignment of a case to a Diagnosis Related Group (DRG)* that has a higher payment when present as a secondary diagnosis, and (c) could reasonably have been prevented through the application of evidence-based guidelines. *States that do not use the grouper methodology may use CMS-approved methodology that is prospective in nature. |
Conditional | NOTE: The code “1” is no longer valid on claims submitted under the version 5010 format, effective January 1, 2011. The POA field will instead be left blank for codes exempt from POA reporting. See http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R756OTN.pdf for a listing of exempt diagnoses. | Y Diagnosis was present at time of inpatient admission N Diagnosis was not present at time of inpatient admission U Documentation insufficient to determine if condition was present at the time of inpatient admission W Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. BLANK Exempt from POA reporting. |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT032-0001 |
| 1730 | COT032 | DIAGNOSIS-POA-FLAG-2 | Field should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). The POA (present on admission) flag is only applicable on inpatient claims/encounters. | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT032-0002 | |||
| 1731 | COT032 | DIAGNOSIS-POA-FLAG-2 | All UNUSED diagnosis code POA flag fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT032-0003 | |||
| 1732 | COT033 | BEGINNING-DATE-OF-SERVICE | For services received during a single encounter with a provider, the date the service covered by this claim was received. For services involving multiple encounters on different days, or periods of care extending over two or more days, this would be the date on which the service covered by this claim began. For capitation premium payments, the date on which the period of coverage related to this payment began. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT033-0001 | |
| 1733 | COT033 | BEGINNING-DATE-OF-SERVICE | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT033-0002 | |||
| 1734 | COT033 | BEGINNING-DATE-OF-SERVICE | The beginning date of service must occur before or be the same as the end of time period | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT033-0003 | |||
| 1735 | COT033 | BEGINNING-DATE-OF-SERVICE | Date must occur before or be the same as Ending Date of Service | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT033-0004 | |||
| 1736 | COT033 | BEGINNING-DATE-OF-SERVICE | Date must occur before or be the same as adjudication date. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT033-0005 | |||
| 1737 | COT033 | BEGINNING-DATE-OF-SERVICE | Date must occur on or before Date of Death. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT033-0006 | |||
| 1738 | COT033 | BEGINNING-DATE-OF-SERVICE | The beginning date of service must occur before the DATE-OF-BIRTH when the person is eligible as an unborn CHIP child or beginning date of service must occur on or after the DATE-OF-BIRTH when the person is eligible through Medicaid or is eligible as a non-unborn CHIP child . | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT033-0007 | |||
| 1739 | COT033 | BEGINNING-DATE-OF-SERVICE | A Medicaid claim record for an eligible individual, if applicable, cannot have a Beginning Date of Service after the eligible individual's Medicaid enrollment has ended. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT033-0008 | |||
| 1740 | COT033 | BEGINNING-DATE-OF-SERVICE | A CHIP claim record for an individual eligible for separate CHIP cannot have a Beginning Date of Service after the eligible individual's CHIP enrollment has ended. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT033-0009 | |||
| 1741 | COT034 | ENDING-DATE-OF-SERVICE | For services received during a single encounter with a provider, the date the service covered by this claim was received. For services involving multiple encounters on different days, or periods of care extending over two or more days, the date on which the service covered by this claim ended. For capitation premium payments, the date on which the period of coverage related to this payment ends/ended. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT034-0001 | |
| 1742 | COT034 | ENDING-DATE-OF-SERVICE | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT034-0002 | |||
| 1743 | COT034 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must occur after or be the same as the BEGINNING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT034-0003 | |||
| 1744 | COT034 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must be on or before the ADJUDICATION-DATE. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT034-0004 | |||
| 1745 | COT034 | ENDING-DATE-OF-SERVICE | Date must occur on or before Date of Death, when a DATE-OF-DEATH is not unknown or not applicable. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT034-0005 | |||
| 1746 | COT034 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must be on or after DATE-OF-BIRTH | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT034-0006 | |||
| 1747 | COT034 | ENDING-DATE-OF-SERVICE | Date must occur before or be the same as End of Time Period. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT034-0007 | |||
| 1748 | COT035 | ADJUDICATION-DATE | The date on which the payment status of the claim was finally adjudicated by the state. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT035-0001 | |
| 1749 | COT035 | ADJUDICATION-DATE | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT035-0002 | |||
| 1750 | COT035 | ADJUDICATION-DATE | For Adjustment Records (ADJUSTMENT-INDICATOR<> 0), use date of final adjudication when possible. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT035-0003 | |||
| 1751 | COT035 | ADJUDICATION-DATE | For Encounter Records (TYPE-OF-CLAIM=3, C, W); use date the encounter was processed by the state. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT035-0004 | |||
| 1752 | COT035 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or before END-OF-TIME-PERIOD included in the T-MSIS HEADER RECORD | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT035-0005 | |||
| 1753 | COT035 | ADJUDICATION-DATE | This date must occur on or after the DATE-OF-BIRTH in the Eligible Record when the eligible is not a CHIP unborn child. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT035-0006 | |||
| 1754 | COT035 | ADJUDICATION-DATE | A Medicaid or CHIP eligible individual should not have had a claim adjudicated before their five-year immigration ineligible status has expired, except when the eligible is an unborn child in the CHIP program. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT035-0007 | |||
| 1755 | COT036 | MEDICAID-PAID-DATE | The date Medicaid paid on this claim or adjustment. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT036-0001 | |
| 1756 | COT036 | MEDICAID-PAID-DATE | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT036-0002 | |||
| 1757 | COT037 | TYPE-OF-CLAIM | A code indicating what kind of payment is covered in this claim | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT037-0001 |
| 1758 | COT037 | TYPE-OF-CLAIM | States should only submit CHIP claims for CHIP eligibles | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT037-0002 | |||
| 1759 | COT037 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the basis of eligibility. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT037-0003 | |||
| 1760 | COT037 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the maintenance assistance status. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT037-0004 | |||
| 1761 | COT037 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the restricted benefits code. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT037-0005 | |||
| 1762 | COT037 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the TANF code. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT037-0006 | |||
| 1763 | COT038 | TYPE-OF-BILL | A data element corresponding with UB-04 form locator FL4 that classifies the claim as to the type of facility (2nd digit), type of care (3rd digit) and the billing record's sequence in the episode of care (4th digit). (Note that the 1st digit is always zero.) | Conditional | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT038-0001 |
| 1764 | COT039 | CLAIM-STATUS | The health care claim status codes convey the status of an entire claim. |
Required | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-codes | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT039-0001 |
| 1765 | COT040 | CLAIM-STATUS-CATEGORY | The general category of the claim status (accepted, rejected, pended, finalized, additional information requested, etc.), which is then further detailed in the companion data element CLAIM-STATUS. | Required | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-category-codes/ | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT040-0001 |
| 1766 | COT041 | SOURCE-LOCATION | The field denotes the claim payment system from which the claim was adjudicated. | Required | Value must be equal to a valid value. | 01 MMIS 02 Non-MMIS CHIP Payment System 03 Pharmacy Benefits Manager (PBM) Vendor 04 Dental Benefits Manager Vendor 05 Transportation Provider System 06 Mental Health Claims Payment System 07 Financial Transaction/Accounting System 08 Other State Agency Claims Payment System 09 County/Local Government Claims Payment System 10 Other Vendor/Other Claims Payment System 20 Managed Care Organization (MCO) 99 Unknown source |
4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT041-0001 |
| 1767 | COT042 | CHECK-NUM | The check or EFT number | Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9),, dashes (-), and spaces. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT042-0001 | |
| 1768 | COT042 | CHECK-NUM | If there is a valid check date there should also be a valid check number. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT042-0002 | |||
| 1769 | COT043 | CHECK-EFF-DATE | Date the check is issued to the payee, or if Electronic Funds Transfer (EFT), the date the transfer is made. | Conditional | Date format should be CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT043-0001 | |
| 1770 | COT043 | CHECK-EFF-DATE | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT043-0002 | |||
| 1771 | COT043 | CHECK-EFF-DATE | Could be the same as Remittance Date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT043-0003 | |||
| 1772 | COT043 | CHECK-EFF-DATE | If there is a valid check number, there should also be a valid check date. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT043-0004 | |||
| 1773 | COT044 | CLAIM-PYMT-REM-CODE-1 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT044-0001 |
| 1774 | COT045 | CLAIM-PYMT-REM-CODE-2 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT045-0001 |
| 1775 | COT046 | CLAIM-PYMT-REM-CODE-3 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT046-0001 |
| 1776 | COT047 | CLAIM-PYMT-REM-CODE-4 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT047-0001 |
| 1777 | COT048 | TOT-BILLED-AMT | The total amount charged for this claim at the claim header level as submitted by the provider. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT048-0001 | |
| 1778 | COT048 | TOT-BILLED-AMT | The total amount should be the sum of each of the billed amounts submitted at the claim detail level. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT048-0002 | |||
| 1779 | COT048 | TOT-BILLED-AMT | If TYPE-OF-CLAIM = "4", then TOT-BILLED-AMT must = "00000000". | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT048-0003 | |||
| 1780 | COT048 | TOT-BILLED-AMT | If TYPE-OF-CLAIM = 3, C, W (encounter record) this field should either be zero-filled or contain the amount paid by the plan to the provider. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT048-0004 | |||
| 1781 | COT049 | TOT-ALLOWED-AMT | The claim header level maximum amount determined by the payer as being 'allowable' under the provisions of the contract prior to the determination of actual payment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT049-0001 | |
| 1782 | COT049 | TOT-ALLOWED-AMT | The sum of the allowed amounts at the detailed levels must equal TOT-ALLOWED-AMT | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT049-0002 | |||
| 1783 | COT050 | TOT-MEDICAID-PAID-AMT | The total amount paid by Medicaid on this claim or adjustment at the claim header level, which is the sum of the amounts paid by Medicaid at the detail level for the claim. | Required | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT050-0001 | |
| 1784 | COT051 | TOT-COPAY-AMT | The total amount paid by Medicaid/CHIP enrollee for each office or emergency department visit or purchase of prescription drugs in addition to the amount paid by Medicaid/CHIP. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT051-0001 | |
| 1785 | COT052 | TOT-MEDICARE-DEDUCTIBLE-AMT | The amount paid by Medicaid/CHIP, on this claim at the claim header level, toward the beneficiary’s Medicare deductible. |
Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT052-0001 | |
| 1786 | COT052 | TOT-MEDICARE-DEDUCTIBLE-AMT | The total medicare deductible amount must be less than or equal the total billed amount. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT052-0002 | |||
| 1787 | COT052 | TOT-MEDICARE-DEDUCTIBLE-AMT | If TOT-MEDICARE-COINS-AMT = "88888", then TOT-MEDICARE-DEDUCTIBLE-AMT must = "8888". | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT052-0003 | |||
| 1788 | COT052 | TOT-MEDICARE-DEDUCTIBLE-AMT | If TOT-MEDICARE-COINS-AMT = "9999", then TOT-MEDICARE-DEDUCTIBLE-AMT must = "0999". | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT052-0004 | |||
| 1789 | COT053 | TOT-MEDICARE-COINS-AMT | The amount paid by Medicaid/CHIP, on this claim, toward the recipient's Medicare coinsurance at the claim detail level. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT053-0001 | |
| 1790 | COT053 | TOT-MEDICARE-COINS-AMT | Value should be reported as not applicable if the TYPE-OF-CLAIM is an encounter (valid values = 3, C, W) | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT053-0002 | |||
| 1791 | COT053 | TOT-MEDICARE-COINS-AMT | Value must be less than TOT-BILLED-AMT. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT053-0003 | |||
| 1792 | COT053 | TOT-MEDICARE-COINS-AMT | Value must be 8-filled if TOT-MEDICARE-DEDUCTIBLE-AMT is 8-filled. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT053-0004 | |||
| 1793 | COT053 | TOT-MEDICARE-COINS-AMT | If the Medicare deductible amount can be identified separately from Medicare coinsurance payments, code that amount in this field. If the Medicare coinsurance and deductible payments cannot be separated, fill this field with the combined payment amount and code space in TOT-MEDICARE-COINS-AMT. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT053-0005 | |||
| 1794 | COT054 | TOT-TPL-AMT | Third Party Liability (TPL) refers to the legal obligation of third parties, i.e., certain individuals, entities, or programs, to pay all or part of the expenditures for medical assistance furnished under a state plan. This is the total amount denoted at the claim header level paid by the third party. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT054-0001 | |
| 1795 | COT054 | TOT-TPL-AMT | Absolute value of TOT-TPL-AMT must be < Absolute value of (TOT-BILLED-AMT - (minus) TOT-MEDICARE-COINS-AMT + (plus) TOT-MEDICARE-DEDUCTIBLE-AMT). | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT054-0002 | |||
| 1796 | COT056 | TOT-OTHER-INSURANCE-AMT | The amount paid by insurance other than Medicare or Medicaid on this claim. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT056-0001 | |
| 1797 | COT057 | OTHER-INSURANCE-IND | The field denotes whether the insured party is covered under other insurance plan. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 9 Unknown |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT057-0001 |
| 1798 | COT058 | OTHER-TPL-COLLECTION | This data element indicates that the claim is for a beneficiary for whom other third party resource development and collection activities are in progress, when the liability is not another health insurance plan for which the eligible is a beneficiary. | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 Third Party Resource is Casualty/Tort 002 Third Party Resource is Estate 003 Third Party Resource is Lien (TEFRA) 004 Third Party Resource is Lien (Other) 005 Third Party Resource is Worker’s Compensation 006 Third Party Resource is Medical Malpractice 007 Third Party Resource is Other 999 Classification of Third Party Resource is Unknown |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT058-0001 |
| 1799 | COT059 | SERVICE-TRACKING-TYPE | A code to categorize service tracking claims. A “service tracking claim” is used to report lump sum payments that cannot be attributed to a single enrollee. (Note: Use an encounter record to report services provided under a capitated payment arrangement.) | Conditional | Value must be equal to a valid value. | 00 Not a Service Tracking Claim 01 Drug Rebate 02 DSH Payment 03 Lump Sum Payment 04 Cost Settlement 05 Supplemental 06 Other 99 Unknown |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT059-0001 |
| 1800 | COT060 | SERVICE-TRACKING-PAYMENT-AMT | On service tracking claims, the lump sum amount paid to the provider. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT060-0001 | |
| 1801 | COT060 | SERVICE-TRACKING-PAYMENT-AMT | Required on service tracking records | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT060-0002 | |||
| 1802 | COT060 | SERVICE-TRACKING-PAYMENT-AMT | Amount paid for services received by an individual patient, when the state accepts a lump sum form a provider that covered similar services delivered to more than one patient, such as a group screening for EPSDT | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT060-0003 | |||
| 1803 | COT060 | SERVICE-TRACKING-PAYMENT-AMT | For service tracking payments, ensure that the TOT-MEDICAID-PAID-AMOUNT is 0 filled and provide payment amount in SERVICE-TRACKING-PAYMENT-AMT only. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT060-0004 | |||
| 1804 | COT060 | SERVICE-TRACKING-PAYMENT-AMT | If there is a service tracking type, then there must also be a service tracking payment amount. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT060-0005 | |||
| 1805 | COT060 | SERVICE-TRACKING-PAYMENT-AMT | If SERVICE-TRACKING-TYPE <> "00" or "99", then SERVICE-TRACKING-PAYMENT-AMT must BE<> 000000000000. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT060-0006 | |||
| 1806 | COT061 | FIXED-PAYMENT-IND | This code indicates that the reimbursement amount included on the claim is for a fixed payment. Fixed payments are made by the state to insurers or providers for premiums or eligible coverage, not for a particular service. For example, some states have Primary Care Case Management (PCCM) programs where the state pays providers a monthly patient management fee of $3.50 for each eligible participant under their care. This fee is considered a fixed payment. It is very important for states to correctly identify fixed payments. Fixed payments do not have a defined “medical record” associated with the payment; therefore, fixed payments are not subject to medical record request and medical record review. |
Conditional | Value must be equal to a valid value. | 0 Not Fixed Payment 1 FFS Fixed Payment |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT061-0001 |
| 1807 | COT062 | FUNDING-CODE | A code to indicate the source of non-federal share funds. | Required | Value must be equal to a valid value. | A Medicaid Agency B CHIP Agency C Mental Health Service Agency D Education Agency E Child and Family Services Agency F County G City H Providers I Other |
10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT062-0001 |
| 1808 | COT063 | FUNDING-SOURCE-NONFEDERAL-SHARE | A code to indicate the type of non-federal share used by the state to finance its expenditure to the provider. | Required | Value must be equal to a valid value. When states have multiple sources of FUNDING-SOURCE-NONFEDERAL-SHARE, States are to report the portion which represents the largest proportion as the FUNDING-SOURCE-NONFEDERAL-SHARE. |
01 State appropriations to the Medicaid agency 02 Intergovernmental transfers (IGT) 03 Certified public expenditures (CPE) 04 Provider taxes 05 Donations |
9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT063-0001 |
| 1809 | COT064 | MEDICARE-COMB-DED-IND | Code indicating that the amount paid by Medicaid/CHIP on this claim toward the recipient's Medicare deductible was combined with their coinsurance amount because the amounts could not be separated. | Conditional | Value must be equal to a valid value. | 0 Amount not combined with coinsurance amount 1 Amount combined with coinsurance amount 9 Unknown |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT064-0001 |
| 1810 | COT064 | MEDICARE-COMB-DED-IND | If claim is not a Crossover claim, or if a type of claim is “3,” “C” or “W” (an encounter claim), set value to “0” | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT064-0002 | |||
| 1811 | COT064 | MEDICARE-COMB-DED-IND | Claims records for an eligible individual should not indicate Medicare paid any combined deductible amount on the claim, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT064-0003 | |||
| 1812 | COT064 | MEDICARE-COMB-DED-IND | If claim is not a Crossover claim, or if a type of claim is “3,” “C” or “W” (an encounter claim), set value to “0” | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT064-0004 | |||
| 1813 | COT064 | MEDICARE-COMB-DED-IND | Claims records for an eligible individual should not indicate Medicare paid any combined deductible amount on the claim, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT064-0005 | |||
| 1814 | COT065 | PROGRAM-TYPE | Code indicating special Medicaid program under which the service was provided. Refer to Appendix E for information on the various program types. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT065-0001 |
| 1815 | COT065 | PROGRAM-TYPE | Value for 1915 (c) waiver must correspond to the values for 1915(c) waiver in the Waiver Type. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT065-0002 | |||
| 1816 | COT065 | PROGRAM-TYPE | If PROGRAM-TYPE=Community First Choice (11) then [T-MSIS ELIGIBLE FILE] STATE-PLAN-OPTION-TYPE must = 01 for the same time period. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT065-0003 | |||
| 1817 | COT065 | PROGRAM-TYPE | If PROGRAM-TYPE=1915(i) (value=13) then [T-MSIS ELIGIBLE FILE] STATE-PLAN-OPTION-TYPE must = 02 for the same time period. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT065-0004 | |||
| 1818 | COT066 | PLAN-ID-NUMBER | A unique number, assigned by the state, which represents the health plan under which the non-fee-for-service encounter was provided including through the state plan and a waiver. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT066-0001 | |
| 1819 | COT066 | PLAN-ID-NUMBER | Use the number as it is carried in the state’s system. (TYPE-OF-CLAIM=3, C, W OR TYPE-OF-SERVICE=119, 120, 122). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT066-0002 | |||
| 1820 | COT066 | PLAN-ID-NUMBER | If TYPE-OF-CLAIM<>3, C, W (Encounter Record) AND TYPE-OF-SERVICE<> {119, 120, 121, 122), 8-fill | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT066-0003 | |||
| 1821 | COT066 | PLAN-ID-NUMBER | If TYPE-OF-CLAIM <> Encounter or Capitation Payment, 8-fill. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT066-0004 | |||
| 1822 | COT066 | PLAN-ID-NUMBER | This data element must equal the BILLING-PROV-NUM if the TYPE-OF-SERVICE is a capitation payment. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT066-0005 | |||
| 1823 | COT066 | PLAN-ID-NUMBER | The managed care ID on the individual's eligible record must match that which is included on any claims records for the eligible individual. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT066-0006 | |||
| 1824 | COT067 | NATIONAL-HEALTH-CARE-ENTITY-ID | The national identifier of the health care entity (controlling health plan, subhealth plan, or other entity) at the most granular sub-health plan level of the Medicaid or CHIP health plan in which an individual is enrolled. See 45 CFR 162 Subpart E. http://www.gpo.gov/fdsys/pkg/FR-2012-09-05/pdf/2012-21238.pdf | NA | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT067-0001 | |
| 1825 | COT067 | NATIONAL-HEALTH-CARE-ENTITY-ID | Large health plans are required to obtain national health plan identifiers by November 5, 2014, small health plans by November 5, 2015. States may report prior to these dates if available. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT067-0002 | |||
| 1826 | COT067 | NATIONAL-HEALTH-CARE-ENTITY-ID | This field is required for all managed care claims and encounters with dates of service on or after the mandated dates above | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT067-0003 | |||
| 1827 | COT067 | NATIONAL-HEALTH-CARE-ENTITY-ID | NATIONAL-HEALTH-CARE-ENTITY-IDs on managed care claims and encounters must match NATIONAL-HEALTH-CARE-ENTITY-IDs on file for the individual in the eligibility subject area or the TPL subject area. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT067-0004 | |||
| 1828 | COT068 | PAYMENT-LEVEL-IND | The field denotes whether the claim payment is made at the header level or the detail level. | Required | Value must be equal to a valid value. | 1 Claim Header – Sum of Line Item payments 2 Claim Detail – Individual Line Item payments |
4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT068-0001 |
| 1829 | COT068 | PAYMENT-LEVEL-IND | Payment fields at either the claim header or line on encounter records should be left blank | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT068-0002 | |||
| 1830 | COT069 | MEDICARE-REIM-TYPE | This code indicates the type of Medicare Reimbursement. |
Conditional | Value must be equal to a valid value. | 01 IPPS - Acute Inpatient PPS 02 LTCHPPS - Long-term Care Hospital PPS 03 SNFPPS - Skilled Nursing Facility PPS 04 HHPPS - Home Health PPS 05 IRFPPS - Inpatient Rehabilitation Facility PPS 06 IPFPPS - Inpatient Psychiatric Facility PPS 07 OPPS - Outpatient PPS 08 Fee Schedules (for physicians, DME, ambulance, and clinical lab) 09 Part C Hierarchical Condition Category Risk Assessment (CMS-HCC RA) Capitation Payment Model |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT069-0001 |
| 1831 | COT069 | MEDICARE-REIM-TYPE | If this is a crossover Medicare claim, the claim must have a MEDICARE-REIM-TYPE. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT069-0002 | |||
| 1832 | COT070 | CLAIM-LINE-COUNT | The total number of lines on the claim. | Required | Must be populated on every record | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT070-0001 | |
| 1833 | COT070 | CLAIM-LINE-COUNT | If the number of claim lines is above the state-approved limit, the record will be split and the split-claim-ind will equal 1. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT070-0002 | |||
| 1834 | COT070 | CLAIM-LINE-COUNT | The claim line count should equal the sum of the claim lines for this record. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT070-0003 | |||
| 1835 | COT072 | FORCED-CLAIM-IND | This code indicates if the claim was processed by forcing it through a manual override process. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT072-0001 |
| 1836 | COT073 | HEALTH-CARE-ACQUIRED-CONDITION-IND | This code indicates whether the individual included on the claim has a Health Care Acquired Condition. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 9 Unknown |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT073-0001 |
| 1837 | COT073 | HEALTH-CARE-ACQUIRED-CONDITION-IND | For additional coding information refer to the following site : https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalAcqCond/index.html?redirect=/hospitalacqcond/05_Coding.asp#TopOfPage |
4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT073-0002 | |||
| 1838 | COT074 | OCCURRENCE-CODE-01 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT074-0001 |
| 1839 | COT074 | OCCURRENCE-CODE-01 | Required if reported on the claim. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT074-0002 | |||
| 1840 | COT074 | OCCURRENCE-CODE-01 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT074-0003 | |||
| 1841 | COT075 | OCCURRENCE-CODE-02 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT075-0001 |
| 1842 | COT075 | OCCURRENCE-CODE-02 | Required if reported on the claim. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT075-0002 | |||
| 1843 | COT075 | OCCURRENCE-CODE-02 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT075-0003 | |||
| 1844 | COT076 | OCCURRENCE-CODE-03 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT076-0001 |
| 1845 | COT076 | OCCURRENCE-CODE-03 | Required if reported on the claim. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT076-0002 | |||
| 1846 | COT076 | OCCURRENCE-CODE-03 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT076-0003 | |||
| 1847 | COT077 | OCCURRENCE-CODE-04 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT077-0001 |
| 1848 | COT077 | OCCURRENCE-CODE-04 | Required if reported on the claim. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT077-0002 | |||
| 1849 | COT077 | OCCURRENCE-CODE-04 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT077-0003 | |||
| 1850 | COT078 | OCCURRENCE-CODE-05 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT078-0001 |
| 1851 | COT078 | OCCURRENCE-CODE-05 | Required if reported on the claim. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT078-0002 | |||
| 1852 | COT078 | OCCURRENCE-CODE-05 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT078-0003 | |||
| 1853 | COT079 | OCCURRENCE-CODE-06 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT079-0001 |
| 1854 | COT079 | OCCURRENCE-CODE-06 | Required if reported on the claim. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT079-0002 | |||
| 1855 | COT079 | OCCURRENCE-CODE-06 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT079-0003 | |||
| 1856 | COT080 | OCCURRENCE-CODE-07 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT080-0001 |
| 1857 | COT080 | OCCURRENCE-CODE-07 | Required if reported on the claim. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT080-0002 | |||
| 1858 | COT080 | OCCURRENCE-CODE-07 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT080-0003 | |||
| 1859 | COT081 | OCCURRENCE-CODE-08 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT081-0001 |
| 1860 | COT081 | OCCURRENCE-CODE-08 | Required if reported on the claim. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT081-0002 | |||
| 1861 | COT081 | OCCURRENCE-CODE-08 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT081-0003 | |||
| 1862 | COT082 | OCCURRENCE-CODE-09 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT082-0001 |
| 1863 | COT082 | OCCURRENCE-CODE-09 | Required if reported on the claim. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT082-0002 | |||
| 1864 | COT082 | OCCURRENCE-CODE-09 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT082-0003 | |||
| 1865 | COT083 | OCCURRENCE-CODE-10 | A code to describe to describe specific event(s) relating to this billing period covered by the claim. (These are FLs 31, 32, 33, 34, 35, and 36 - Occurrence Codes on the UB04.) These fields can be used for either occurrences or occurrence spans. |
Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT083-0001 |
| 1866 | COT083 | OCCURRENCE-CODE-10 | Required if reported on the claim. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT083-0002 | |||
| 1867 | COT083 | OCCURRENCE-CODE-10 | All UNUSED occurrence code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT083-0003 | |||
| 1868 | COT084 | OCCURRENCE-CODE-EFF-DATE-01 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT084-0001 | |
| 1869 | COT084 | OCCURRENCE-CODE-EFF-DATE-01 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT084-0002 | |||
| 1870 | COT084 | OCCURRENCE-CODE-EFF-DATE-01 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT084-0003 | |||
| 1871 | COT084 | OCCURRENCE-CODE-EFF-DATE-01 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT084-0004 | |||
| 1872 | COT084 | OCCURRENCE-CODE-EFF-DATE-01 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT084-0005 | |||
| 1873 | COT084 | OCCURRENCE-CODE-EFF-DATE-01 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT084-0006 | |||
| 1874 | COT085 | OCCURRENCE-CODE-EFF-DATE-02 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT085-0001 | |
| 1875 | COT085 | OCCURRENCE-CODE-EFF-DATE-02 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT085-0002 | |||
| 1876 | COT085 | OCCURRENCE-CODE-EFF-DATE-02 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT085-0003 | |||
| 1877 | COT085 | OCCURRENCE-CODE-EFF-DATE-02 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT085-0004 | |||
| 1878 | COT085 | OCCURRENCE-CODE-EFF-DATE-02 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT085-0005 | |||
| 1879 | COT085 | OCCURRENCE-CODE-EFF-DATE-02 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT085-0006 | |||
| 1880 | COT086 | OCCURRENCE-CODE-EFF-DATE-03 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT086-0001 | |
| 1881 | COT086 | OCCURRENCE-CODE-EFF-DATE-03 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT086-0002 | |||
| 1882 | COT086 | OCCURRENCE-CODE-EFF-DATE-03 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT086-0003 | |||
| 1883 | COT086 | OCCURRENCE-CODE-EFF-DATE-03 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT086-0004 | |||
| 1884 | COT086 | OCCURRENCE-CODE-EFF-DATE-03 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT086-0005 | |||
| 1885 | COT086 | OCCURRENCE-CODE-EFF-DATE-03 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT086-0006 | |||
| 1886 | COT087 | OCCURRENCE-CODE-EFF-DATE-04 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT087-0001 | |
| 1887 | COT087 | OCCURRENCE-CODE-EFF-DATE-04 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT087-0002 | |||
| 1888 | COT087 | OCCURRENCE-CODE-EFF-DATE-04 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT087-0003 | |||
| 1889 | COT087 | OCCURRENCE-CODE-EFF-DATE-04 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT087-0004 | |||
| 1890 | COT087 | OCCURRENCE-CODE-EFF-DATE-04 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT087-0005 | |||
| 1891 | COT087 | OCCURRENCE-CODE-EFF-DATE-04 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT087-0006 | |||
| 1892 | COT088 | OCCURRENCE-CODE-EFF-DATE-05 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT088-0001 | |
| 1893 | COT088 | OCCURRENCE-CODE-EFF-DATE-05 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT088-0002 | |||
| 1894 | COT088 | OCCURRENCE-CODE-EFF-DATE-05 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT088-0003 | |||
| 1895 | COT088 | OCCURRENCE-CODE-EFF-DATE-05 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT088-0004 | |||
| 1896 | COT088 | OCCURRENCE-CODE-EFF-DATE-05 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT088-0005 | |||
| 1897 | COT088 | OCCURRENCE-CODE-EFF-DATE-05 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT088-0006 | |||
| 1898 | COT089 | OCCURRENCE-CODE-EFF-DATE-06 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT089-0001 | |
| 1899 | COT089 | OCCURRENCE-CODE-EFF-DATE-06 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT089-0002 | |||
| 1900 | COT089 | OCCURRENCE-CODE-EFF-DATE-06 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT089-0003 | |||
| 1901 | COT089 | OCCURRENCE-CODE-EFF-DATE-06 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT089-0004 | |||
| 1902 | COT089 | OCCURRENCE-CODE-EFF-DATE-06 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT089-0005 | |||
| 1903 | COT089 | OCCURRENCE-CODE-EFF-DATE-06 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT089-0006 | |||
| 1904 | COT090 | OCCURRENCE-CODE-EFF-DATE-07 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT090-0001 | |
| 1905 | COT090 | OCCURRENCE-CODE-EFF-DATE-07 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT090-0002 | |||
| 1906 | COT090 | OCCURRENCE-CODE-EFF-DATE-07 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT090-0003 | |||
| 1907 | COT090 | OCCURRENCE-CODE-EFF-DATE-07 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT090-0004 | |||
| 1908 | COT090 | OCCURRENCE-CODE-EFF-DATE-07 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT090-0005 | |||
| 1909 | COT090 | OCCURRENCE-CODE-EFF-DATE-07 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT090-0006 | |||
| 1910 | COT091 | OCCURRENCE-CODE-EFF-DATE-08 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT091-0001 | |
| 1911 | COT091 | OCCURRENCE-CODE-EFF-DATE-08 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT091-0002 | |||
| 1912 | COT091 | OCCURRENCE-CODE-EFF-DATE-08 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT091-0003 | |||
| 1913 | COT091 | OCCURRENCE-CODE-EFF-DATE-08 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT091-0004 | |||
| 1914 | COT091 | OCCURRENCE-CODE-EFF-DATE-08 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT091-0005 | |||
| 1915 | COT091 | OCCURRENCE-CODE-EFF-DATE-08 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT091-0006 | |||
| 1916 | COT092 | OCCURRENCE-CODE-EFF-DATE-09 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT092-0001 | |
| 1917 | COT092 | OCCURRENCE-CODE-EFF-DATE-09 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT092-0002 | |||
| 1918 | COT092 | OCCURRENCE-CODE-EFF-DATE-09 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT092-0003 | |||
| 1919 | COT092 | OCCURRENCE-CODE-EFF-DATE-09 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT092-0004 | |||
| 1920 | COT092 | OCCURRENCE-CODE-EFF-DATE-09 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT092-0005 | |||
| 1921 | COT092 | OCCURRENCE-CODE-EFF-DATE-09 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT092-0006 | |||
| 1922 | COT093 | OCCURRENCE-CODE-EFF-DATE-10 | The start date of the corresponding occurrence code or occurrence span codes. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT093-0001 | |
| 1923 | COT093 | OCCURRENCE-CODE-EFF-DATE-10 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT093-0002 | |||
| 1924 | COT093 | OCCURRENCE-CODE-EFF-DATE-10 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT093-0003 | |||
| 1925 | COT093 | OCCURRENCE-CODE-EFF-DATE-10 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT093-0004 | |||
| 1926 | COT093 | OCCURRENCE-CODE-EFF-DATE-10 | Value must be less than or equal to the corresponding OCCURRENCE-CODE-END-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT093-0005 | |||
| 1927 | COT093 | OCCURRENCE-CODE-EFF-DATE-10 | All UNUSED occurrence code effective date fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT093-0006 | |||
| 1928 | COT094 | OCCURRENCE-CODE-END-DATE-01 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT094-0001 | |
| 1929 | COT094 | OCCURRENCE-CODE-END-DATE-01 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT094-0002 | |||
| 1930 | COT094 | OCCURRENCE-CODE-END-DATE-01 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT094-0003 | |||
| 1931 | COT094 | OCCURRENCE-CODE-END-DATE-01 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT094-0004 | |||
| 1932 | COT094 | OCCURRENCE-CODE-END-DATE-01 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT094-0005 | |||
| 1933 | COT094 | OCCURRENCE-CODE-END-DATE-01 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT094-0006 | |||
| 1934 | COT095 | OCCURRENCE-CODE-END-DATE-02 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT095-0001 | |
| 1935 | COT095 | OCCURRENCE-CODE-END-DATE-02 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT095-0002 | |||
| 1936 | COT095 | OCCURRENCE-CODE-END-DATE-02 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT095-0003 | |||
| 1937 | COT095 | OCCURRENCE-CODE-END-DATE-02 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT095-0004 | |||
| 1938 | COT095 | OCCURRENCE-CODE-END-DATE-02 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT095-0005 | |||
| 1939 | COT095 | OCCURRENCE-CODE-END-DATE-02 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT095-0006 | |||
| 1940 | COT096 | OCCURRENCE-CODE-END-DATE-03 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT096-0001 | |
| 1941 | COT096 | OCCURRENCE-CODE-END-DATE-03 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT096-0002 | |||
| 1942 | COT096 | OCCURRENCE-CODE-END-DATE-03 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT096-0003 | |||
| 1943 | COT096 | OCCURRENCE-CODE-END-DATE-03 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT096-0004 | |||
| 1944 | COT096 | OCCURRENCE-CODE-END-DATE-03 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT096-0005 | |||
| 1945 | COT096 | OCCURRENCE-CODE-END-DATE-03 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT096-0006 | |||
| 1946 | COT097 | OCCURRENCE-CODE-END-DATE-04 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT097-0001 | |
| 1947 | COT097 | OCCURRENCE-CODE-END-DATE-04 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT097-0002 | |||
| 1948 | COT097 | OCCURRENCE-CODE-END-DATE-04 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT097-0003 | |||
| 1949 | COT097 | OCCURRENCE-CODE-END-DATE-04 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT097-0004 | |||
| 1950 | COT097 | OCCURRENCE-CODE-END-DATE-04 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT097-0005 | |||
| 1951 | COT097 | OCCURRENCE-CODE-END-DATE-04 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT097-0006 | |||
| 1952 | COT098 | OCCURRENCE-CODE-END-DATE-05 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT098-0001 | |
| 1953 | COT098 | OCCURRENCE-CODE-END-DATE-05 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT098-0002 | |||
| 1954 | COT098 | OCCURRENCE-CODE-END-DATE-05 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT098-0003 | |||
| 1955 | COT098 | OCCURRENCE-CODE-END-DATE-05 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT098-0004 | |||
| 1956 | COT098 | OCCURRENCE-CODE-END-DATE-05 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT098-0005 | |||
| 1957 | COT098 | OCCURRENCE-CODE-END-DATE-05 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT098-0006 | |||
| 1958 | COT099 | OCCURRENCE-CODE-END-DATE-06 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT099-0001 | |
| 1959 | COT099 | OCCURRENCE-CODE-END-DATE-06 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT099-0002 | |||
| 1960 | COT099 | OCCURRENCE-CODE-END-DATE-06 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT099-0003 | |||
| 1961 | COT099 | OCCURRENCE-CODE-END-DATE-06 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT099-0004 | |||
| 1962 | COT099 | OCCURRENCE-CODE-END-DATE-06 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT099-0005 | |||
| 1963 | COT099 | OCCURRENCE-CODE-END-DATE-06 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT099-0006 | |||
| 1964 | COT100 | OCCURRENCE-CODE-END-DATE-07 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT100-0001 | |
| 1965 | COT100 | OCCURRENCE-CODE-END-DATE-07 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT100-0002 | |||
| 1966 | COT100 | OCCURRENCE-CODE-END-DATE-07 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT100-0003 | |||
| 1967 | COT100 | OCCURRENCE-CODE-END-DATE-07 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT100-0004 | |||
| 1968 | COT100 | OCCURRENCE-CODE-END-DATE-07 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT100-0005 | |||
| 1969 | COT100 | OCCURRENCE-CODE-END-DATE-07 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT100-0006 | |||
| 1970 | COT101 | OCCURRENCE-CODE-END-DATE-08 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT101-0001 | |
| 1971 | COT101 | OCCURRENCE-CODE-END-DATE-08 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT101-0002 | |||
| 1972 | COT101 | OCCURRENCE-CODE-END-DATE-08 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT101-0003 | |||
| 1973 | COT101 | OCCURRENCE-CODE-END-DATE-08 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT101-0004 | |||
| 1974 | COT101 | OCCURRENCE-CODE-END-DATE-08 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT101-0005 | |||
| 1975 | COT101 | OCCURRENCE-CODE-END-DATE-08 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT101-0006 | |||
| 1976 | COT102 | OCCURRENCE-CODE-END-DATE-09 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT102-0001 | |
| 1977 | COT102 | OCCURRENCE-CODE-END-DATE-09 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT102-0002 | |||
| 1978 | COT102 | OCCURRENCE-CODE-END-DATE-09 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT102-0003 | |||
| 1979 | COT102 | OCCURRENCE-CODE-END-DATE-09 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT102-0004 | |||
| 1980 | COT102 | OCCURRENCE-CODE-END-DATE-09 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT102-0005 | |||
| 1981 | COT102 | OCCURRENCE-CODE-END-DATE-09 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT102-0006 | |||
| 1982 | COT103 | OCCURRENCE-CODE-END-DATE-10 | The last date that the corresponding occurrence code or occurrence span code was applicable. | Conditional | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT103-0001 | |
| 1983 | COT103 | OCCURRENCE-CODE-END-DATE-10 | Value must be a valid date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT103-0002 | |||
| 1984 | COT103 | OCCURRENCE-CODE-END-DATE-10 | If the occurrence date span is a single day, then populate the OCCURRENCE-CODE-EFF-DATE and OCCURRENCE-CODE-END-DATE fields with the same date | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT103-0003 | |||
| 1985 | COT103 | OCCURRENCE-CODE-END-DATE-10 | Required when the corresponding OCCURRENCE-CODE field is populated | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT103-0004 | |||
| 1986 | COT103 | OCCURRENCE-CODE-END-DATE-10 | Value must correspond to the OCCURRENCE-CODE value | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT103-0005 | |||
| 1987 | COT103 | OCCURRENCE-CODE-END-DATE-10 | Value must be greater than or equal to the corresponding OCCURRENCE-CODE-EFF-DATE field | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT103-0006 | |||
| 1988 | COT104 | PATIENT-CONTROL-NUM | A patient's unique number assigned by the provider agency during claim submission, which identifies the client or the client’s episode of service within the provider’s system to facilitate retrieval of individual financial and clinical records and posting of payment. | Conditional | Must be numeric (0-9) and/or alphabetic (A-Z). Special characters are invalid entries | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT104-0001 | |
| 1989 | COT105 | ELIGIBLE-LAST-NAME | The last name of the individual to whom the services were provided. (The patients name should be captured as it appears on the claim record, it does not need to be the same as it appears on the eligibility file. The MSIS-IDENTIFICATION-NUM will be used to associate a claim record with the appropriate eligibility data.) | Required | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT105-0001 | |
| 1990 | COT105 | ELIGIBLE-LAST-NAME | When populating the eligible person’s name on T-MSIS Claim Files, use the patient’s name from the claim transaction rather than the eligible person’s name from the T-MSIS Eligible File. | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT105-0002 | |||
| 1991 | COT106 | ELIGIBLE-FIRST-NAME | The first name of the individual to whom the services were provided. (The patients name should be captured as it appears on the claim record, it does not need to be the same as it appears on the eligibility file. The MSIS-IDENTIFICATION-NUM will be used to associate a claim record with the appropriate eligibility data.) | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT106-0001 | |
| 1992 | COT106 | ELIGIBLE-FIRST-NAME | When populating the eligible person’s name on T-MSIS Claim Files, use the patient’s name from the claim transaction rather than the eligible person’s name from the T-MSIS Eligible File. | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT106-0002 | |||
| 1993 | COT107 | ELIGIBLE-MIDDLE-INIT | The middle initial of the individual to whom the services were provided. (The patients name should be captured as it appears on the claim record, it does not need to be the same as it appears on the eligibility file. The MSIS-IDENTIFICATION-NUM will be used to associate a claim record with the appropriate eligibility data.) | Conditional | Value must be an alphabetic character, or a blank (A-Z, a-z, ) | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT107-0001 | |
| 1994 | COT107 | ELIGIBLE-MIDDLE-INIT | Leave blank if not available When populating the eligible person’s name on T-MSIS Claim Files, use the patient’s name from the claim transaction rather than the eligible person’s name from the T-MSIS Eligible File. |
9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT107-0002 | |||
| 1995 | COT108 | DATE-OF-BIRTH | Date of birth of the individual to whom the services were provided. | Required | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT108-0001 | |
| 1996 | COT108 | DATE-OF-BIRTH | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT108-0002 | |||
| 1997 | COT108 | DATE-OF-BIRTH | The numeric form for days and months from 1 to 9 must have a zero as the first digit. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT108-0003 | |||
| 1998 | COT108 | DATE-OF-BIRTH | The patient’s date of birth shall be reported in numeric form as follows – 2 digit month, 2 digit day, and 4 digit year | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT108-0004 | |||
| 1999 | COT108 | DATE-OF-BIRTH | A patient's age should not be greater than 112 years. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT108-0005 | |||
| 2000 | COT109 | HEALTH-HOME-PROV-IND | This code indicates whether the claim is submitted by a provider or provider group enrolled in the Health Home care model. Health home providers provide service for patients with chronic illnesses. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 8 Not Applicable 9 Unknown |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT109-0001 |
| 2001 | COT109 | HEALTH-HOME-PROV-IND | If a state has not yet begun collecting this information, HEALTH-HOME-PROVIDER-IND, this field should be defaulted to the value “8.” | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT109-0002 | |||
| 2002 | COT109 | HEALTH-HOME-PROV-IND | If there is a HEALTH-HOME-ENTITY-NAME then HEALTH-HOME-PROV-IND must indicate yes. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT109-0003 | |||
| 2003 | COT109 | HEALTH-HOME-PROV-IND | States should not submit claim records for an eligible individual that indicate the claim was submitted by a provider or provider group enrolled in a health home model if the eligible individual is not enrolled in the health home program. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT109-0004 | |||
| 2004 | COT109 | HEALTH-HOME-PROV-IND | States that do not specify an eligible individual's health home provider number, if applicable, should not report claims that indicate the claim is submitted by a provider or provider group enrolled in the health home model. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT109-0005 | |||
| 2005 | COT110 | WAIVER-TYPE | Code for specifying waiver type under which the eligible individual is covered during the month and receiving services/under which claim is submitted. | Conditional | Enter the WAIVER-TYPE assigned | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT110-0001 |
| 2006 | COT110 | WAIVER-TYPE | Value must correspond to associated WAIVER-ID | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT110-0002 | |||
| 2007 | COT110 | WAIVER-TYPE | An ineligible individual cannot have a category for federal reimbursement for Medicaid or CHIP (CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT <> 01,02) | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT110-0003 | |||
| 2008 | COT111 | WAIVER-ID | Field specifying the waiver or demonstration which authorized payment for a claim. These IDs must be the approved, full federal waiver ID number assigned during the state submission and CMS approval process. The categories of demonstration and waiver programs include: 1915(b)(1); 1915(b)(2); 1915(b)(3), and 1915(b)(4) managed care waivers; 1915(c) home and community based services waivers; combined 1915(b) and 1915(c) managed home and community based services waivers and 1115 demonstrations. | Conditional | Valid values are supplied by the state. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | ||
| 2009 | COT111 | WAIVER-ID | Report the full federal waiver identifier. | 11/9/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT111-0002 | |||
| 2010 | COT111 | WAIVER-ID | If the goods & services rendered do not fall under a waiver, leave this field blank. | 11/9/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT111-0004 | |||
| 2011 | COT111 | WAIVER-ID | If there's a waiver type, there should be a corresponding waiver id. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT111-0005 | |||
| 2012 | COT112 | BILLING-PROV-NUM | A unique identification number assigned by the state to a provider or capitation plan. This should represent the entity billing for the service. | Required | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT112-0001 |
| 2013 | COT112 | BILLING-PROV-NUM | If value is invalid, record it exactly as it appears in the state system. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT112-0002 | |||
| 2014 | COT112 | BILLING-PROV-NUM | For encounter records (TYPE-OF-CLAIM = 3, C, W), this represents the entity billing (or reporting) to the managed care plan (See PLAN-ID-NUMBER for reporting capitation plan-ID). Capitation PLAN-ID should be used in this field only for capitation payments (TYPE-OF-SERVICE = 119, 120, 122). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT112-0003 | |||
| 2015 | COT113 | BILLING-PROV-NPI-NUM | The National Provider ID (NPI) of the billing provider responsible for billing for the service on the claim. The billing provider can also be servicing, referring, or prescribing provider; can be admitting provider except for Long Term Care. |
Conditional | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT113-0001 |
| 2016 | COT113 | BILLING-PROV-NPI-NUM | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT113-0002 | |||
| 2017 | COT113 | BILLING-PROV-NPI-NUM | For encounter records (TYPE-OF-CLAIM = 3, C, W), the BILLIN-PROV-NPI-NUM field should be populated with the NPI of the provider or entity billing (or reporting) to the managed care plan. For financial transactions (i.e., expenditure transactions or recoupments of previously made expenditures that do not flow through the usual claim adjudication/adjustment process or encounter record reporting process), the BILLIN-PROV-NPI-NUM field should be populated with the NPI of the provider or entity to which the financial transaction was addressed, unless the transaction is a payment/recoupment made-to/received-from a managed care plan, in which case the BILLING-PROV-NPI-NUM should be left blank. For financial transactions with managed care plans, the plan's ID should be reported in the PLAN-ID-NUMBER field and the BILLING-PROV-NPI-NUM should be left blank. |
2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT113-0003 | |||
| 2018 | COT113 | BILLING-PROV-NPI-NUM | If legacy identifiers are available for providers, then report the legacy IDs in the Provider ID field and the NPI in this field. If only the legacy Provider ID is available, then 9-fill the National Provider ID and enter the legacy IDs in the Provider ID fields. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT113-0004 | |||
| 2019 | COT113 | BILLING-PROV-NPI-NUM | Billing Provider must be enrolled | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT113-0006 | |||
| 2020 | COT114 | BILLING-PROV-TAXONOMY | For CLAIMOT and CLAIMRX files, the taxonomy code for the provider billing for the service. | Conditional | Value must be in the set of valid values | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT114-0001 |
| 2021 | COT114 | BILLING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT114-0002 | |||
| 2022 | COT114 | BILLING-PROV-TAXONOMY | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122) | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT114-0003 | |||
| 2023 | COT115 | BILLING-PROV-TYPE | A code describing the type of entity billing for the service. | Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT115-0001 |
| 2024 | COT115 | BILLING-PROV-TYPE | For encounter records (TYPE-OF-CLAIM= 3, C, W), this represents the entity billing (or reporting) to the Managed Care Plan (see PLAN-ID-NUMBER for reporting capitation plan-ID). CAPITATION-PLAN-ID should be used in this field only for capitation payments (TYPE-OF-SERVICE=119, 120, 122). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT115-0002 | |||
| 2025 | COT115 | BILLING-PROV-TYPE | The state should use Taxonomy Crosswalk.pdf to crosswalk state codes to CMS codes | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT115-0003 | |||
| 2026 | COT116 | BILLING-PROV-SPECIALTY | This code describes the area of specialty for the billing provider. | Conditional | Must be in the set of valid values | See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT116-0001 |
| 2027 | COT117 | REFERRING-PROV-NUM | A code describing the type of provider (i.e. doctor) who referred the patient. If the state uses state-specific codes, they should map their internal codes to the CMS standard list provided. |
Conditional | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT117-0001 |
| 2028 | COT117 | REFERRING-PROV-NUM | If Value is invalid, record it exactly as it appears in the state system | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT117-0002 | |||
| 2029 | COT117 | REFERRING-PROV-NUM | If the Referring Provider Number is not available, but the physician’s Drug Enforcement Agency (DEA) ID is on the state file, then the state should use the DEA ID for this data element. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT117-0003 | |||
| 2030 | COT118 | REFERRING-PROV-NPI-NUM | The National Provider ID (NPI) of the provider who recommended the servicing provider to the patient. | Conditional | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT118-0001 |
| 2031 | COT118 | REFERRING-PROV-NPI-NUM | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT118-0002 | |||
| 2032 | COT118 | REFERRING-PROV-NPI-NUM | The field should be blank if the transaction is for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122). | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT118-0003 | |||
| 2033 | COT119 | REFERRING-PROV-TAXONOMY | For CLAIMOT files, the taxonomy code for the provider who referred the beneficiary for treatment. | NA | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT119-0001 |
| 2034 | COT119 | REFERRING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT119-0002 | |||
| 2035 | COT119 | REFERRING-PROV-TAXONOMY | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122). | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT119-0003 | |||
| 2036 | COT120 | REFERRING-PROV-TYPE | A code describing the type of provider (i.e. doctor) who referred the patient. If the state uses state-specific codes, they should map their internal codes to the CMS standard list provided |
NA | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT120-0001 |
| 2037 | COT121 | REFERRING-PROV-SPECIALTY | This code indicates the area of specialty of the referring provider. | NA | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT121-0001 |
| 2038 | COT122 | MEDICARE-HIC-NUM | Health Insurance Claim (HIC) Number as it appears on the patient’s Medicare card. | Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9) |
4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT122-0001 | |
| 2039 | COT122 | MEDICARE-HIC-NUM | "Railroad Retirees" - Railroad Retirement Board (RRB) HIC numbers generally have two alpha characters as a prefix to the number. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT122-0002 | |||
| 2040 | COT122 | MEDICARE-HIC-NUM | If this is a crossover Medicare claim, the Bene must have a MEDICARE-HIC-Num. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT122-0003 | |||
| 2041 | COT122 | MEDICARE-HIC-NUM | States should not submit records for an eligible individual where the eligible's Medicare HIC Number does not match in the associated claim record, if applicable. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT122-0004 | |||
| 2042 | COT122 | MEDICARE-HIC-NUM | Claims records for an eligible individual should not indicate a valid Medicare HIC number, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT122-0005 | |||
| 2043 | COT123 | PLACE-OF-SERVICE | A code indicating where the service was performed. CMS 1500 values are used for this data element. | Conditional | Value must be equal to a valid value. | http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c26.pdf | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT123-0001 |
| 2044 | COT123 | PLACE-OF-SERVICE | Note: Value 99 will be counted as error | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT123-0002 | |||
| 2045 | COT123 | PLACE-OF-SERVICE | If there are new valid CMS 1500 PLACE-OF-SERVICE codes that are not listed in this dictionary, these codes may be used and will not trigger an error | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT123-0003 | |||
| 2046 | COT123 | PLACE-OF-SERVICE | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122). | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT123-0004 | |||
| 2047 | COT125 | BMI | A key index for relating a person's body weight to their height. The body mass index (BMI) is a person's weight in kilograms (kg) divided by their height in meters (m) squared. | Optional | SI units: BMI = mass (kg) / (height(m))2 Imperial/US Customary units: BMI = mass (lb) * 703/ (height(in))2 BMI = mass (lb) * 4.88/ (height(ft))2 BMI = mass (st) * 9840/ (height(in))2 |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT125-0001 | |
| 2048 | COT125 | BMI | CMS is relieving states of the responsibility to: (a) Provide these data. (b) Document a mitigation plan in the Source-to-Target-Mapping Matrix Addendum B whenever the data elements cannot be populated all of the time. However if a state determines that it can populate one or more of these fields and wishes to do so, they are encouraged to do so and will not incur any Addendum B mitigation plan documentation expectations. |
9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT125-0002 | |||
| 2049 | COT126 | REMITTANCE-NUM | The Remittance Advice Number is a sequential number that identifies the current Remittance Advice (RA) produced for a provider. The number is incremented by one each time a new RA is generated. The first five (5) positions are Julian date YYDDD format. The RA is the detailed explanation of the reason for the payment amount. The RA number is not the check number. | Required | Limit characters to alphabet (A-Z, a-z), numerals (0-9).. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT126-0001 | |
| 2050 | COT126 | REMITTANCE-NUM | Value must not be null | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT126-0002 | |||
| 2051 | COT126 | REMITTANCE-NUM | If there is a remittance date, then there must also be a remittance number. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT126-0003 | |||
| 2052 | COT127 | DAILY-RATE | The amount a policy will pay per day for a covered service. In some cases for OT claims this is referred to as a flat rate. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT127-0001 | |
| 2053 | COT128 | BORDER-STATE-IND | This code indicates whether an individual received services or equipment across state borders. (The provider location is out of state, but for payment purposes the provider is treated as an in-state provider.) | Conditional | Value must be equal to a valid value. | 0 - No 1 - Yes |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT128-0001 |
| 2054 | COT130 | BENEFICIARY-COINSURANCE-AMOUNT | The amount of money the beneficiary paid towards coinsurance. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT130-0001 | |
| 2055 | COT130 | BENEFICIARY-COINSURANCE-AMOUNT | If no coinsurance is applicable enter 0.00 | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT130-0002 | |||
| 2056 | COT131 | BENEFICIARY-COINSURANCE-DATE-PAID | The date the beneficiary paid the coinsurance amount. | Conditional | Date format should be CCYYMMDD (National Data Standard) | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT131-0001 | |
| 2057 | COT131 | BENEFICIARY-COINSURANCE-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT131-0002 | |||
| 2058 | COT131 | BENEFICIARY-COINSURANCE-DATE-PAID | If no coinsurance is applicable, 8-fill | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT131-0003 | |||
| 2059 | COT132 | BENEFICIARY-COPAYMENT-AMOUNT | The amount of money the beneficiary paid towards a copayment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT132-0001 | |
| 2060 | COT132 | BENEFICIARY-COPAYMENT-AMOUNT | If no copayment is applicable enter 0.00 | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT132-0002 | |||
| 2061 | COT133 | BENEFICIARY-COPAYMENT-DATE-PAID | The date the beneficiary paid the copayment amount. | Conditional | Date format should be CCYYMMDD (National Data Standard) | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT133-0001 | |
| 2062 | COT133 | BENEFICIARY-COPAYMENT-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT133-0002 | |||
| 2063 | COT133 | BENEFICIARY-COPAYMENT-DATE-PAID | If no coinsurance is applicable, 8-fill | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT133-0003 | |||
| 2064 | COT134 | BENEFICIARY-DEDUCTIBLE-AMOUNT | The amount of money the beneficiary paid towards an annual deductible. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT134-0001 | |
| 2065 | COT134 | BENEFICIARY-DEDUCTIBLE-AMOUNT | If no deductible is applicable enter 0.00 | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT134-0002 | |||
| 2066 | COT135 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | The date the beneficiary paid the deductible amount. | Conditional | Date format should be CCYYMMDD (National Data Standard) | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT135-0001 | |
| 2067 | COT135 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT135-0002 | |||
| 2068 | COT135 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | If no coinsurance is applicable, 8-fill | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT135-0003 | |||
| 2069 | COT136 | CLAIM-DENIED-INDICATOR | An indicator to identify a claim that the state refused pay in its entirety. | Conditional | Value must be equal to a valid value. | 0 Denied: The payment of claim in its entirety was denied by the state. 1 Not Denied: The state paid some or all of the claim. |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT136-0001 |
| 2070 | COT136 | CLAIM-DENIED-INDICATOR | It is expected that states will submit all denied claims to CMS. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT136-0002 | |||
| 2071 | COT136 | CLAIM-DENIED-INDICATOR | If the Type of Claim indicates the claim was denied, then this indicator must also indicate the claim was denied. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT136-0003 | |||
| 2072 | COT137 | COPAY-WAIVED-IND | An indicator signifying that the copay was waived by the provider. | Conditional | Value must be equal to a valid value. | 0 Not Waived: The provider did not waive the beneficiary’s copayment 1 Waived: The provider waived the beneficiary’s copayment 8 Not Applicable: The benefit plan does not have a copay in this circumstance |
11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT137-0001 |
| 2073 | COT138 | HEALTH-HOME-ENTITY-NAME | A free-form text field to indicate the health home program that authorized payment for the service on the claim. The name entered should be the name that the state uses to uniquely identify the team. A “Health Home Entity” can be a designated provider (e.g., physician, clinic, behavioral health organization), a health team which links to a designated provider, or a health team (physicians, nurses, behavioral health professionals). Because an identification numbering schema has not been established, the entities’ names are being used instead. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
Field contains invalid characters - HEALTH-HOME-ENTITY-NAME | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT138-0001 |
| 2074 | COT138 | HEALTH-HOME-ENTITY-NAME | States should not submit records for an eligible individual where the eligible's health home entity name does not match in the associated claim record, if applicable. | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT138-0002 | |||
| 2075 | COT140 | THIRD-PARTY-COINSURANCE-AMOUNT-PAID | The amount of money paid by a third party on behalf of the beneficiary towards coinsurance on the claim or claim line item. | Optional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT140-0001 | |
| 2076 | COT141 | THIRD-PARTY-COINSURANCE-DATE-PAID | The date the third party paid the coinsurance amount. | Optional | Date format should be CCYYMMDD (National Data Standard) | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT141-0001 | |
| 2077 | COT141 | THIRD-PARTY-COINSURANCE-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT141-0002 | |||
| 2078 | COT141 | THIRD-PARTY-COINSURANCE-DATE-PAID | If no coinsurance is applicable, 8-fill | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT141-0003 | |||
| 2079 | COT142 | THIRD-PARTY-COPAYMENT-AMOUNT-PAID | The amount the third party paid the copayment amount. | Optional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT142-0001 | |
| 2080 | COT143 | THIRD-PARTY-COPAYMENT-DATE-PAID | The date the third party paid the copayment amount. | Optional | Date format should be CCYYMMDD (National Data Standard) | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT143-0001 | |
| 2081 | COT143 | THIRD-PARTY-COPAYMENT-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT143-0002 | |||
| 2082 | COT143 | THIRD-PARTY-COPAYMENT-DATE-PAID | If no coinsurance is applicable, 8-fill | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT143-0003 | |||
| 2083 | COT144 | DATE-CAPITATED-AMOUNT-REQUESTED | The date that the managed care entity submitted the capitated payment bill to the state. | Conditional | Date format should be CCYYMMDD (National Data Standard) | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT144-0001 | |
| 2084 | COT144 | DATE-CAPITATED-AMOUNT-REQUESTED | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT144-0002 | |||
| 2085 | COT145 | CAPITATED-PAYMENT-AMT-REQUESTED | The amount of the capitated payment bill submitted by the managed care entity to the state. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT145-0001 | |
| 2086 | COT146 | HEALTH-HOME-PROVIDER-NPI | The National Provider ID (NPI) of the health home provider. | Conditional | The value must be a valid NPI | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT146-0001 |
| 2087 | COT146 | HEALTH-HOME-PROVIDER-NPI | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT146-0002 | |||
| 2088 | COT147 | MEDICARE-BENEFICIARY-IDENTIFIER | The individual’s Medicare Beneficiary Identifier (MBI) Identification Number. Note: MBI replaces the HICN with an entirely new Medicare Beneficiary Identifier (MBI) for purposes of provider billing, if applicable. CMS interfaces with non-payment exchange partners would remain HICN-based, while interfaces with payment partners would use the new MBI. |
NA | Valid characters in the text string are limited to alpha characters (A-Z, a-z) and numbers (0-9) | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT147-0001 | |
| 2089 | COT147 | MEDICARE-BENEFICIARY-IDENTIFIER | If individual is NOT enrolled in Medicare, 8-fill field. | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT147-0002 | |||
| 2090 | COT147 | MEDICARE-BENEFICIARY-IDENTIFIER | Field should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files) until such time as the Medicare Beneficiary Identifier is implemented (no target date has been established). | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT147-0003 | |||
| 2091 | COT148 | UNDER-DIRECTION-OF-PROV-NPI | The National Provider ID (NPI) of the provider who directed the care of a patient that another provider administered. | NA | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | ||
| 2092 | COT148 | UNDER-DIRECTION-OF-PROV-NPI | Field should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). This data element is a duplicate of the “Under-Supervision-of-Prov-NPI” field and as such do not need to be populated. | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT148-0002 | |||
| 2093 | COT149 | UNDER-DIRECTION-OF-PROV-TAXONOMY | The Provider Taxonomy of the provider who directed the care of a patient that another provider administered. | NA | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT149-0001 |
| 2094 | COT149 | UNDER-DIRECTION-OF-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT149-0002 | |||
| 2095 | COT149 | UNDER-DIRECTION-OF-PROV-TAXONOMY | Left-fill unused bytes with spaces | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT149-0003 | |||
| 2096 | COT149 | UNDER-DIRECTION-OF-PROV-TAXONOMY | Field should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). This data element is a duplicate of the “Under-Supervision-of-Prov-Taxonomy” field and as such do not need to be populated. | 9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT149-0004 | |||
| 2097 | COT150 | UNDER-SUPERVISION-OF-PROV-NPI | The National Provider ID (NPI) of the provider who supervised another provider. | Conditional | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT150-0001 |
| 2098 | COT150 | UNDER-SUPERVISION-OF-PROV-NPI | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT150-0002 | |||
| 2099 | COT151 | UNDER-SUPERVISION-OF-PROV-TAXONOMY | The Provider Taxonomy of the provider who supervised another provider | NA | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT151-0001 |
| 2100 | COT151 | UNDER-SUPERVISION-OF-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT151-0002 | |||
| 2101 | COT151 | UNDER-SUPERVISION-OF-PROV-TAXONOMY | Left-fill unused bytes with spaces | 2/25/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT151-0003 | |||
| 2102 | COT152 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT152-0001 | |
| 2103 | COT152 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT152-0002 | |||
| 2104 | COT226 | PROV-LOCATION-ID | A code to uniquely identify the geographic location where the provider’s services were performed. The value should correspond to an active value in the PROV-LOCATION-ID field in the provider subject area. | Required | Limit characters to alphabet (A-Z), numerals (0-9).. | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT226-0001 | |
| 2105 | COT226 | PROV-LOCATION-ID | The value should correspond with one of the location identifiers recorded in the provider’s demographic records in the T-MSIS data set | 10/10/2013 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT226-0002 | |||
| 2106 | COT153 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | CLAIMOT | CLAIM-HEADER-RECORD-OT-COT00002 | COT153-0001 | |||
| 2107 | COT154 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the CLAIM-HEADER-RECORD-IP record segment is CIP00002. | Required | Value must be equal to a valid value. | COT00003 - CLAIM-LINE-RECORD-OT | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT154-0001 |
| 2108 | COT154 | RECORD-ID | Must be populated on every record | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT154-0002 | |||
| 2109 | COT154 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT154-0003 | |||
| 2110 | COT155 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT155-0001 |
| 2111 | COT155 | SUBMITTING-STATE | Must be populated on every record. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT155-0002 | |||
| 2112 | COT155 | SUBMITTING-STATE | Value must be numeric |
4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT155-0003 | |||
| 2113 | COT155 | SUBMITTING-STATE | SUBMITTING-STATE must be equal across all record segments for a given record. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT155-0004 | |||
| 2114 | COT156 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT156-0001 | |
| 2115 | COT156 | RECORD-NUMBER | Must be numeric | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT156-0002 | |||
| 2116 | COT156 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT156-0004 | |||
| 2117 | COT157 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Conditional | MSIS Identification Number must be reported | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT157-0001 | |
| 2118 | COT157 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state ID numbers must be supplied to CMS | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT157-0002 | |||
| 2119 | COT157 | MSIS-IDENTIFICATION-NUM | For TYPE-OF-CLAIM = 4 or D (lump sum adjustments), this field must begin with an ‘&’. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT157-0003 | |||
| 2120 | COT157 | MSIS-IDENTIFICATION-NUM | For SSN states, this field must contain the Eligible's Social Security Number. If the SSN is unknown and a temporary number is assigned, this field will contain that number. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT157-0004 | |||
| 2121 | COT158 | ICN-ORIG | A unique number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies an original claim. | Required | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT158-0001 | |
| 2122 | COT158 | ICN-ORIG | Record the value exactly as it appears in the State system. Do not pad. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT158-0002 | |||
| 2123 | COT158 | ICN-ORIG | This field should always be populated with the claim identification number assigned to the original paid/denied claim. This identification number should remain constant and be carried forward onto any adjustment claims. The intention is for this earliest claim identification number to be the link that ties the original claim and all adjustment claims together. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT158-0003 | |||
| 2124 | COT158 | ICN-ORIG | This field should not be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT158-0004 | |||
| 2125 | COT159 | ICN-ADJ | A unique claim number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies the adjustment claim for an original transaction. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT159-0001 | |
| 2126 | COT159 | ICN-ADJ | Record the value exactly as it appears in the State system. Do not pad. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT159-0002 | |||
| 2127 | COT159 | ICN-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT159-0003 | |||
| 2128 | COT160 | LINE-NUM-ORIG | A unique number to identify the transaction line number that is being reported on the original claim. | Required | Record the value exactly as it appears in the State system. Do not pad. This field should also be completed on adjustment claims to reflect the LINE-NUMBER of the INTERNAL-CONTROL-NUMBER on the claim that is being adjusted | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT160-0001 | |
| 2129 | COT161 | LINE-NUM-ADJ | A unique number to identify the transaction line number that identifies the line number on the adjustment ICN. | Conditional | Record the value exactly as it appears in the state system. Do not pad | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT161-0001 | |
| 2130 | COT161 | LINE-NUM-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT161-0002 | |||
| 2131 | COT162 | LINE-ADJUSTMENT-IND | Code indicating type of adjustment record claim/encounter represents at claim detail level. | Conditional | Value must be equal to a valid value. | 0 Original Claim/Encounter 1 Void of a prior submission 2 Re-submittal 3 Credit Adjustment (negative supplemental) 4 Debit Adjustment (positive supplemental) 5 Credit Gross Adjustment. 6 Debit Gross Adjustment 9 Unknown |
11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT162-0001 |
| 2132 | COT162 | LINE-ADJUSTMENT-IND | If there is a line adjustment number, then there must be a line-adjustment indicator. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT162-0002 | |||
| 2133 | COT162 | LINE-ADJUSTMENT-IND | If there is a line adjustment reason, then there must be a line adjustment indicator. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT162-0003 | |||
| 2134 | COT163 | LINE-ADJUSTMENT-REASON-CODE | Claim adjustment reason codes communicate why a service line was paid differently than it was billed. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-adjustment-reason-codes/ | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT163-0001 |
| 2135 | COT163 | LINE-ADJUSTMENT-REASON-CODE | If there is no adjustment to a line, then there is no adjustment reason code. (Also see: CLAIM-PYMT-REM-CODE) | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT163-0002 | |||
| 2136 | COT164 | SUBMITTER-ID | The Submitter ID number is the value that identifies the provider/trading partner/clearing house organization to state’s claim adjudication system. | Conditional | Value must not be null | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT164-0001 | |
| 2137 | COT165 | CLAIM-LINE-STATUS | The claim line status codes identify the status of a specific detail claim line rather than the entire claim. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-codes/ | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT165-0001 |
| 2138 | COT166 | BEGINNING-DATE-OF-SERVICE | For services received during a single encounter with a provider, the date the service covered by this claim was received. For services involving multiple encounters on different days or periods of care extending over two or more days, the date on which the service covered by this claim began. For capitation premium payments, the date on which the period of coverage related to this payment began. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT166-0001 | |
| 2139 | COT166 | BEGINNING-DATE-OF-SERVICE | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT166-0002 | |||
| 2140 | COT166 | BEGINNING-DATE-OF-SERVICE | The beginning date of service must occur before or be the same as the ending date of service. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT166-0003 | |||
| 2141 | COT166 | BEGINNING-DATE-OF-SERVICE | Date must occur before or be the same as adjudication date. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT166-0004 | |||
| 2142 | COT166 | BEGINNING-DATE-OF-SERVICE | Date must occur on or before Date of Death. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT166-0005 | |||
| 2143 | COT166 | BEGINNING-DATE-OF-SERVICE | The beginning date of service must occur before the DATE-OF-BIRTH when the person is eligible as an unborn CHIP child or beginning date of service must occur on or after the DATE-OF-BIRTH when the person is eligible through Medicaid or is eligible as a non-unborn CHIP child . | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT166-0006 | |||
| 2144 | COT166 | BEGINNING-DATE-OF-SERVICE | A Medicaid claim record for an eligible individual, if applicable, cannot have a Beginning Date of Service after the eligible individual's Medicaid enrollment has ended. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT166-0007 | |||
| 2145 | COT166 | BEGINNING-DATE-OF-SERVICE | A CHIP claim record for an individual eligible for separate CHIP cannot have a Beginning Date of Service after the eligible individual's CHIP enrollment has ended. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT166-0008 | |||
| 2146 | COT167 | ENDING-DATE-OF-SERVICE | For services received during a single encounter with a provider, the date the service covered by this claim was received. For services involving multiple encounters on different days, or periods of care extending over two or more days, the date on which the service covered by this claim ended. For capitation premium payments, the date on which the period of coverage related to this payment ends/ended. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT167-0001 | |
| 2147 | COT167 | ENDING-DATE-OF-SERVICE | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT167-0002 | |||
| 2148 | COT167 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must occur after or be the same as the BEGINNING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT167-0003 | |||
| 2149 | COT167 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must be on or before the ADJUDICATION-DATE. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT167-0004 | |||
| 2150 | COT167 | ENDING-DATE-OF-SERVICE | Date must occur on or before Date of Death, when a DATE-OF-DEATH is not unknown or not applicable. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT167-0005 | |||
| 2151 | COT167 | ENDING-DATE-OF-SERVICE | ENDING-DATE-OF-SERVICE must be on or after DATE-OF-BIRTH | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT167-0006 | |||
| 2152 | COT167 | ENDING-DATE-OF-SERVICE | Date must occur before or be the same as End of Time Period. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT167-0007 | |||
| 2153 | COT168 | REVENUE-CODE | A code which identifies a specific accommodation, ancillary service or billing calculation (as defined by UB-04 Billing Manual). | Conditional | Only valid codes as defined by the “National Uniform Billing Committee” should be used. | Revenue code is a data set that health care providers or insurers usually pay for to use. These values will change annually. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT168-0001 |
| 2154 | COT168 | REVENUE-CODE | Enter all UB-04 Revenue Codes listed on the claim | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT168-0002 | |||
| 2155 | COT168 | REVENUE-CODE | Value must be a valid code | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT168-0003 | |||
| 2156 | COT168 | REVENUE-CODE | If value invalid, record it exactly as it appears in the state system | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT168-0004 | |||
| 2157 | COT169 | PROCEDURE-CODE | A field to capture the CPT or HCPCS code that describes a service or good rendered by the provider to an enrollee on the specified date of service. | Required | Value must be a valid code. If PROCDURE-CODE-FLAG-1 = {10 through 87, state-specific coding systems} valid codes must be supplied by the State. For national coding systems, code should conform to the nationally recognized formats: CPT (PROC-CD-FLAG-1=01): Positions 1-5 should be numeric and position 6-7 must be blank. HCPCS (PROC-CD-FLAG-1=06): Position 1 must be an alpha character (“A”-“Z”) and position 6-7 must be blank.. Value can include both National and Local (Regional) codes. For National codes (position 1=“A”-“V”) positions 2-5 must be numeric; for Local (Regional) codes, positions 2-5 must be alphanumeric (e.g., “X1234" or “WW234"). |
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html http://www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/index.html?redirect=/medhcpcsgeninfo/ http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Relative-Value-Files.html http://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx Additional CPT codes are available for a fee through professional organizations. |
10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT169-0001 |
| 2158 | COT169 | PROCEDURE-CODE | If no PROCEDURE-CODE was performed, 8-fill | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT169-0002 | |||
| 2159 | COT169 | PROCEDURE-CODE | ICD-9/10-CM codes are the HIPAA standard for procedure codes on inpatient claims. When ICD-9/10-CM coding is used, the PROCDURE-CODE-FLAG-1=02/07) Positions 1-2 must be numeric, positions 3-4 must be numeric or blank, positions 5-7 must be blank. When ICD-10-PCS coding is used starting 10/1/2014, the PROCDURE-CODE-FLAG-1=07. Positions 1-7 must be alpha or numeric. Position 8 must be blank. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT169-0003 | |||
| 2160 | COT169 | PROCEDURE-CODE | Note: An eighth character is provided for future expansion of this field | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT169-0004 | |||
| 2161 | COT169 | PROCEDURE-CODE | Eligible individuals who are not pregnant cannot have claims with procedures pertaining to labor and delivery. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT169-0005 | |||
| 2162 | COT170 | PROCEDURE-CODE-DATE | The date upon which the procedure was performed. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT170-0001 | |
| 2163 | COT170 | PROCEDURE-CODE-DATE | Value must be a valid date | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT170-0002 | |||
| 2164 | COT170 | PROCEDURE-CODE-DATE | If the corresponding procedure code is 8-filled, then this procedure code date must be 8-filled. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT170-0003 | |||
| 2165 | COT170 | PROCEDURE-CODE-DATE | Date must occur before the ENDING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT170-0004 | |||
| 2166 | COT170 | PROCEDURE-CODE-DATE | Date must occur on or after the BEGINNING-DATE-OF-SERVICE. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT170-0005 | |||
| 2167 | COT170 | PROCEDURE-CODE-DATE | This date must occur on or before the DATE-OF-DEATH in the Eligible file. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT170-0006 | |||
| 2168 | COT171 | PROCEDURE-CODE-FLAG | A flag that identifies the coding system used for the PROCDURE-CODE. | Required | Value must be equal to a valid value. | 01 CPT 4 02 ICD-9 CM 06 HCPCS (Both National and Regional HCPCS) 07 ICD-10-PCS (Will be implemented on 10/1/2014) 10 87 Other Systems 88 Not Applicable 99 Unknown |
10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT171-0001 |
| 2169 | COT171 | PROCEDURE-CODE-FLAG | If no principal procedure was performed, 8-fill | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT171-0002 | |||
| 2170 | COT172 | PROCEDURE-CODE-MOD-1 | A field to capture a modifier code associated with the PROCEDURE-CODE field on the OT claim line. If more than one modifier is reported, the additional codes should be captured in fields "PROCEDURE-CODE-MOD-2" through "PROCEDURE-CODE-MOD-4. | Conditional | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT172-0001 |
| 2171 | COT172 | PROCEDURE-CODE-MOD-1 | If no Principal Procedure was performed, 8-fill | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT172-0002 | |||
| 2172 | COT172 | PROCEDURE-CODE-MOD-1 | All UNUSED diagnosis code fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT172-0003 | |||
| 2173 | COT173 | IMMUNIZATION-TYPE | This field identifies the type of immunization provided in order to track additional detail not currently contained in CPT codes. | Conditional | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT173-0001 |
| 2174 | COT174 | BILLED-AMT | The amount charged at the claim detail level as submitted by the provider. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT174-0001 | |
| 2175 | COT174 | BILLED-AMT | If TYPE-OF-CLAIM = 3, C, W (encounter record) this field should either be zero-filled or contain the amount paid by the plan to the provider. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT174-0002 | |||
| 2176 | COT175 | ALLOWED-AMT | The maximum amount displayed at the claim line level as determined by the payer as being "allowable" under the provisions of the contract prior to the determination of actual payment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT175-0001 | |
| 2177 | COT176 | COPAY-AMT | The copayment amount paid by an enrollee for the service, which does not include the amount paid by the insurance company. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT176-0001 | |
| 2178 | COT177 | TPL-AMT | Third Party Liability (TPL) refers to the legal obligation of third parties, i.e., certain individuals, entities, or programs, to pay all or part of the expenditures for medical assistance furnished under a state plan. This is the total amount denoted at the claim detail level paid by the third party. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT177-0001 | |
| 2179 | COT178 | MEDICAID-PAID-AMT | The amount paid by Medicaid on this claim or adjustment at the claim detail level. | Required | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT178-0001 | |
| 2180 | COT178 | MEDICAID-PAID-AMT | For claims where Medicaid payment is only available at the header level, report the entire payment amount on the MSIS record corresponding to the line item with the highest charge. Zero fill Medicaid Amount Paid on all other MSIS records created from the original claim. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT178-0002 | |||
| 2181 | COT178 | MEDICAID-PAID-AMT | For Crossover claims with Medicare Coinsurance and/or Deductibles, enter the sum of those amounts in the Medicaid-Amount-Paid field, if the providers were reimbursed by Medicaid for them. If the Coinsurance and Deductibles were not paid by the state, then report the Medicaid-Amount-Paid as $0 | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT178-0003 | |||
| 2182 | COT179 | MEDICAID-FFS-EQUIVALENT-AMT | The MEDICAID-FFS-EQUIVALENT-AMT field should be populated with the amt that would have been paid had the services been provided on a FFS basis. | Conditional | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT179-0001 | |
| 2183 | COT179 | MEDICAID-FFS-EQUIVALENT-AMT | Required when TYPE-OF-CLAIM = C, 3, or W | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT179-0002 | |||
| 2184 | COT182 | MEDICARE-PAID-AMT | The amount paid by Medicare on this claim or adjustment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT182-0001 | |
| 2185 | COT182 | MEDICARE-PAID-AMT | If the service was covered by Medicare but Medicare had no liability for the bill, zero-fill. MEDICARE-PAID-AMT should reflect the actual amount paid by Medicare. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT182-0002 | |||
| 2186 | COT182 | MEDICARE-PAID-AMT | For claims where Medicare payment is only available at the header level, report the entire payment amount the MSIS record corresponding to the line item with the highest charge. Zero fill Medicare Amount Paid on all other MSIS records created from the original claim. |
2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT182-0003 | |||
| 2187 | COT182 | MEDICARE-PAID-AMT | Claims records for an eligible individual should not indicate Medicare paid any amount on the claim, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT182-0004 | |||
| 2188 | COT183 | OT-RX-CLAIM-QUANTITY-ACTUAL | The quantity of a drug, service, or product that is rendered/dispensed for a prescription, specific date of service, or billing time span. | Required | Must be numeric | 9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT183-0001 | |
| 2189 | COT183 | OT-RX-CLAIM-QUANTITY-ACTUAL | For use with CLAIMOT and CLAIMRX claims. For CLAIMIP and CLAIMOT claims/encounter records, use the IP-LT-QUANTITY-OF-SERVICE field. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT183-0002 | |||
| 2190 | COT183 | OT-RX-CLAIM-QUANTITY-ACTUAL | Left-fill field with zeros if value is less than 9 bytes long. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT183-0003 | |||
| 2191 | COT183 | OT-RX-CLAIM-QUANTITY-ACTUAL | NOTE: One prescription for 100 250 milligram tablets results in QUANTITY OF SERVICE=100. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT183-0004 | |||
| 2192 | COT183 | OT-RX-CLAIM-QUANTITY-ACTUAL | The value in OT-RX-CLAIM-QUANTITY-ACTUAL must correspond with the value in UNIT-OF-MEASURE. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT183-0005 | |||
| 2193 | COT183 | OT-RX-CLAIM-QUANTITY-ACTUAL | This field is only applicable when the service being billed can be quantified in discrete units, e.g., a number of visits or the number of units of a prescription/refill that were filled. For prescriptions/refills, use the Medicaid Drug Rebate definition of a unit, which is the smallest unit by which the drug is normally measured; e.g. tablet, capsule, milliliter, etc. For drugs not identifiable or dispensed by a normal unit, e.g. powder filled vials, use 1 as the number of units. |
2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT183-0006 | |||
| 2194 | COT184 | OT-RX-CLAIM-QUANTITY-ALLOWED | The maximum allowable quantity of a drug or service that may be dispensed per prescription per date of service or per month. Quantity limits are applied to medications when the majority of appropriate clinical utilizations will be addressed within the quantity allowed. | Conditional | Must be numeric | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT184-0001 | |
| 2195 | COT184 | OT-RX-CLAIM-QUANTITY-ALLOWED | For use with CLAIMOT and CLAIMRX claims. For CLAIMIP and CLAIMOT claims/encounter records, use the IP-LT-QUANTITY-OF-SERVICE field. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT184-0002 | |||
| 2196 | COT184 | OT-RX-CLAIM-QUANTITY-ALLOWED | Left-fill field with zeros if value is less than 9 bytes long. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT184-0003 | |||
| 2197 | COT184 | OT-RX-CLAIM-QUANTITY-ALLOWED | NOTE: One prescription for 100 250 milligram tablets results in OT-RX-CLAIM-QUANTITY-ALLOWED =100. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT184-0004 | |||
| 2198 | COT184 | OT-RX-CLAIM-QUANTITY-ALLOWED | This field is only applicable when the service being billed can be quantified in discrete units, e.g., a number of visits or the number of units of a prescription/refill that were filled. For prescriptions/refills, use the Medicaid Drug Rebate definition of a unit, which is the smallest unit by which the drug is normally measured; e.g. tablet, capsule, milliliter, etc. For drugs not identifiable or dispensed by a normal unit, e.g. powder filled vials, use 1 as the number of units. |
2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT184-0005 | |||
| 2199 | COT184 | OT-RX-CLAIM-QUANTITY-ALLOWED | The value in OT-RX-CLAIM-QUANTITY-ALLOWED must correspond with the value in UNIT-OF-MEASURE. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT184-0006 | |||
| 2200 | COT186 | TYPE-OF-SERVICE | A code to categorize the services provided to a Medicaid or CHIP enrollee. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT186-0001 |
| 2201 | COT186 | TYPE-OF-SERVICE | All claims for inpatient psychiatric care provided in a separately administered psychiatric wing or psychiatric hospital are included in the CLAIMOT file. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT186-0002 | |||
| 2202 | COT186 | TYPE-OF-SERVICE | Experience has demonstrated there can be instances when more than one service area category could be applicable for a provided service. The following hierarchy rules apply to these instances: The specific service categories of sterilizations and other pregnancy-related procedures take precedence over provider categories, such as inpatient hospital or outpatient hospital. Services of a physician employed by a clinic are reported under clinic services if the clinic is the billing entity. X-rays processed by the clinic in the course of treatment, however, are reported under X-ray services. Services of a registered nurse attending a resident in a NF are reported (if they qualified under the coverage rules) under home health services if they were not billed as part of the NF bill. |
2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT186-0003 | |||
| 2203 | COT186 | TYPE-OF-SERVICE | See Appendix D for information on the various types of service. |
2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT186-0004 | |||
| 2204 | COT186 | TYPE-OF-SERVICE | Other Claims/Encounters File - Claims/encounters with TYPE-OF-SERVICE= 002, 003, 004, 005, 006, 007, 008, 010, 011, 012, 013, 014, 015, 016, 017, 018, 019, 020, 021, 022, 023, 024, 025, 026, 027, 028, 029, 030, 031, 032, 035, 036, 037, 038, 039, 040, 041, 042, 043, 049, 050, 051, 052, 053, 054, 055, 056, 057, 060, 061, 062, 063, 064, 065, 066, 067, 068, 069, 070, 071, 072, 073, 074, 075, 076, 077, 078, 079, 080, 081, 082, 083, 084, 085, 087, 088, 089, 115, 119, 120, 121, 122, 123, 127, 131, 134, or 135. | 9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT186-0005 | |||
| 2205 | COT186 | TYPE-OF-SERVICE | Males cannot receive midwife services or other pregnancy-related procedures. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT186-0006 | |||
| 2206 | COT187 | HCBS-SERVICE-CODE | Codes indicating that the service represents a long-term care home and community based service or support for an individual with chronic medical and/or mental conditions. The codes are to help clearly delineate between acute care and long-term care provided in the home and community setting (e.g. 1915(c), 1915(i), 1915(j), and 1915(k) services). | Conditional | Value must be equal to a valid value. | 1 The HCBS service was provided under 1915(i) 2 The HCBS service was provided under 1915(j) 3 The HCBS service was provided under 1915(k) 4 The HCBS service was provided under a 1915(c) HCBS Waiver 5 The HCBS service was provided under an 1115 waiver 6 The HCBS service was not provided under the statutes identified above and was of an acute care nature 7 The HCBS service was not provided under the statutes identified above and was of a long term care nature 8 The service is not an HCBS service (i.e. the HCBS classification is not applicable) 9 Unknown |
11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT187-0001 |
| 2207 | COT188 | HCBS-TAXONOMY | A code that classifies home and community based services listed on the claim into the HCBS taxonomy. | Conditional | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT188-0001 |
| 2208 | COT188 | HCBS-TAXONOMY | If HCBS-SERVICE-CODE = 1 through 8, then populate HCBS-TAXONOMY with one of the values from the list in Appendix B. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT188-0002 | |||
| 2209 | COT188 | HCBS-TAXONOMY | If HCBS-SERVICE-CODE = 9 (It is unknown what authority the HCBS service was provided), then populate HCBS-TAXONOMY based on the assumption that the services is not a 1915(j), 1915(k), 1915(c) waiver, or 1115 waiver service. (See “If HCBS-SERVICE-CODE = 1 through 8” above.) | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT188-0003 | |||
| 2210 | COT189 | SERVICING-PROV-NUM | A unique number to identify the provider who treated the recipient. |
Required | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT189-0001 |
| 2211 | COT189 | SERVICING-PROV-NUM | If value is invalid, record it exactly as it appears in the state system. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT189-0002 | |||
| 2212 | COT189 | SERVICING-PROV-NUM | For institutional providers (TYPE-OF-SERVICE = 002,003, 004 028) and other providers operating as a group, The SERVICING-PROV-NUM should be for the individual who rendered the service. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT189-0003 | |||
| 2213 | COT189 | SERVICING-PROV-NUM | If “Servicing” provider and the “Billing” provider are the same then use the same number in both fields. |
2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT189-0004 | |||
| 2214 | COT189 | SERVICING-PROV-NUM | Note: Once a national provider ID numbering system is in place, the national number should be used. If only the state’s legacy ID number is available then that number can be entered in this field. |
2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT189-0005 | |||
| 2215 | COT189 | SERVICING-PROV-NUM | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122). | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT189-0006 | |||
| 2216 | COT190 | SERVICING-PROV-NPI-NUM | The National Provider ID (NPI) of the rendering/attending provider responsible for the beneficiary. | Conditional | The value must consist of digits 0 through 9 only | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT190-0001 | |
| 2217 | COT190 | SERVICING-PROV-NPI-NUM | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT190-0002 | ||
| 2218 | COT190 | SERVICING-PROV-NPI-NUM | The field should be blank if the transaction is for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122). | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT190-0004 | |||
| 2219 | COT191 | SERVICING-PROV-TAXONOMY | The taxonomy code for the provider who treated the recipient. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT191-0001 |
| 2220 | COT191 | SERVICING-PROV-TAXONOMY | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122) | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT191-0002 | |||
| 2221 | COT191 | SERVICING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT191-0003 | |||
| 2222 | COT192 | SERVICING-PROV-TYPE | A code describing the type of provider (i.e. doctor or facility) who treated the patient. If the state uses state-specific codes, they should map their internal codes to the CMS standard list provided. |
Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT192-0001 |
| 2223 | COT193 | SERVICING-PROV-SPECIALTY | This code indicates the area of specialty for the servicing provider. | Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT193-0001 |
| 2224 | COT194 | OTHER-TPL-COLLECTION | This data element indicates that the claim is for a beneficiary for whom other third party resource development and collection activities are in progress, when the liability is not another health insurance plan for which the eligible is a beneficiary. | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 Third Party Resource is Casualty/Tort 002 Third Party Resource is Estate 003 Third Party Resource is Lien (TEFRA) 004 Third Party Resource is Lien (Other) 005 Third Party Resource is Worker’s Compensation 006 Third Party Resource is Medical Malpractice 007 Third Party Resource is Other 999 Classification of Third Party Resource is Unknown |
11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT194-0001 |
| 2225 | COT195 | TOOTH-DESIGNATION-SYSTEM | A code to identify the tooth numbering system is being used. | Conditional | Enter the value that corresponds to the tooth designation system used to populate the TOOTH-NUMBER, AREA-OF-ORAL-CAVITY, and TOOTH-SURFACE-CODE data elements. | JO ANSI/ADA/ISO Specification No. 3950 JP ADA’s Universal/National Tooth Designation system |
2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT195-0001 |
| 2226 | COT196 | TOOTH-NUM | The tooth number serviced based on the tooth numbering system identified in the TOOTH-DESIGNATION-SYSTEM field. | Conditional | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT196-0001 |
| 2227 | COT196 | TOOTH-NUM | If JO tooth designation system is used: Permanent Upper right quad medial to distal: 11-18 Permanent Upper left quad medial to distal: 22-28 Permanent lower right quad medial to distal: 41-48 Permanent lower left quad medial to distal: 31-38 Primary/Deciduous upper right quad medial to distal: 51-55 Primary/Deciduous upper left quad medial to distal: 61-65 Primary/Deciduous lower left quad medial to distal: 71-75 Primary/Deciduous lower right quad medial to distal: 81-85 |
2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT196-0002 | |||
| 2228 | COT196 | TOOTH-NUM | If JP tooth designation system is used: (Source: "Current Dental Terminology, CDT 2009 - 2010", American Dental Association). |
2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT196-0003 | |||
| 2229 | COT196 | TOOTH-NUM | If the first character of TOOTH-NUM is A through T then beneficiary age must be < 15. (Deciduous teeth are usually all gone by age 12.) | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT196-0004 | |||
| 2230 | COT196 | TOOTH-NUM | If TOOTH-NUM <> missing then TYPE-OF-SERVICE must = Dental | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT196-0005 | |||
| 2231 | COT197 | TOOTH-QUAD-CODE | The area of the oral cavity is designated by a two-digit code. |
Conditional | Value must be equal to a valid value. | 00 Entire Oral Cavity 01 Maxillary Area 02 Mandibular Area 03 Upper Right Sextant 04 Upper Anterior Sextant 05 Upper Left Sextant 06 Lower Left Sextant 07 Lower Anterior Sextant 08 Lower Right Sextant 09 Other Area of Oral Cavity (An area specified in an annexed document or further explanation available.) 10 Upper Right Quadrant (Right Refers to the oral and skeletal structures on the right side.) 20 Upper Left Quadrant (Left Refers to the oral and skeletal structures on the left side.) 30 Lower Left Quadrant 40 Lower Right Quadrant |
11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT197-0001 |
| 2232 | COT197 | TOOTH-QUAD-CODE | IF TOOTH-QUAD-CODE <> missing then TYPE-OF-SERVICE must = Dental | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT197-0002 | |||
| 2233 | COT198 | TOOTH-SURFACE-CODE | A code to identify the tooth’s surface on which the service was performed. |
Conditional | Value must be equal to a valid value. | B Buccal – The surface of the tooth which is closest to the cheek. D Distal – The surface of the tooth facing away from an invisible line drawn vertically through the center of the face. F Facial – The surface of a tooth that is directed towards the face. I Incisal – The cutting edges of the anterior teeth. L Lingual – The surface of the tooth that is directed towards the tongue. M Mesial – The surface of a tooth which faces toward an invisible line drawn vertically through the center of the face. O Occlusa – The surfaces of the posterior (back) teeth which provides the chewing function. |
11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT198-0001 |
| 2234 | COT198 | TOOTH-SURFACE-CODE | IF TOOTH-SURFACE-CODE <> missing then TYPE-OF-SERVICE must = Dental | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT198-0002 | |||
| 2235 | COT199 | ORIGINATION-ADDR-LN1 | The street address of the origination point from which a patient is transported either from home or Long term care facility to a health care provider for healthcare services or vice versa. | Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT199-0001 | |
| 2236 | COT199 | ORIGINATION-ADDR-LN1 | For transportation claims, this is only required if state has captured this information, otherwise it is conditional | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT199-0002 | |||
| 2237 | COT200 | ORIGINATION-ADDR-LN2 | The street address of the origination point from which a patient is transported either from home or Long term care facility to a health care provider for healthcare services or vice versa. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT200-0001 | |
| 2238 | COT200 | ORIGINATION-ADDR-LN2 | For transportation claims, this is only required if state has captured this information, otherwise it is conditional | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT200-0002 | |||
| 2239 | COT200 | ORIGINATION-ADDR-LN2 | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT200-0003 | |||
| 2240 | COT201 | ORIGINATION-CITY | The name of the origination city from which a patient is transported either from home or a long term care facility to a health care provider for healthcare services or vice versa. | Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT201-0001 | |
| 2241 | COT201 | ORIGINATION-CITY | For transportation claims, this is only required if state has captured this information, otherwise it is conditional | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT201-0002 | |||
| 2242 | COT202 | ORIGINATION-STATE | The ANSI 2 numeric code of the origination state in which a patient is transported either from home or a long term care facility to a health care provider to a health care provider for healthcare services or vice versa. | Conditional | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT202-0001 |
| 2243 | COT202 | ORIGINATION-STATE | A value is required transportation claims | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT202-0002 | |||
| 2244 | COT203 | ORIGINATION-ZIP-CODE | The zip code of the origination city from which a patient is transported either from home or a long term care facility to a health care provider for healthcare services or vice versa. | Conditional | The value must consist of digits 0 through 9 only | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT203-0001 | |
| 2245 | COT203 | ORIGINATION-ZIP-CODE | This is only required if state has captured this information, otherwise it is conditional. If the last 4 digits are not populated or used, then the 4-digit extended zip code should be recorded as “0000”. | 9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT203-0002 | |||
| 2246 | COT204 | DESTINATION-ADDR-LN1 | The street address of the destination point to which a patient is transported either from home or a long term care facility to a health care provider for healthcare services or vice versa. | Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT204-0001 | |
| 2247 | COT204 | DESTINATION-ADDR-LN1 | For transportation claims only. Required if state has captured this information, otherwise it is conditional. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT204-0002 | |||
| 2248 | COT205 | DESTINATION-ADDR-LN2 | The street address of the destination point to which a patient is transported either from home or a long term care facility to a health care provider for healthcare services or vice versa. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT205-0001 | |
| 2249 | COT205 | DESTINATION-ADDR-LN2 | For transportation claims only. Required if state has captured this information, otherwise it is conditional. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT205-0002 | |||
| 2250 | COT205 | DESTINATION-ADDR-LN2 | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT205-0003 | |||
| 2251 | COT206 | DESTINATION-CITY | The name of the destination city to which a patient is transported either from home or long term care facility to a health care provider for healthcare services or vice versa. | Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT206-0001 | |
| 2252 | COT206 | DESTINATION-CITY | For transportation claims only. This field is required if state has captured this information, otherwise it is conditional. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT206-0002 | |||
| 2253 | COT207 | DESTINATION-STATE | The ANSI state numeric code for the U.S. state, Territory, or the District of Columbia code of the destination state in which a patient is transported either from home or a long term care facility to a health care provider for healthcare services or vice versa. | Conditional | Value must be in the set of valid values | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT207-0001 |
| 2254 | COT207 | DESTINATION-STATE | For transportation claims only. This field is required if state has captured this information, otherwise it is conditional. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT207-0002 | |||
| 2255 | COT208 | DESTINATION-ZIP-CODE | The zip code of the destination city to which a patient is transported either from home or long term care facility to a health care provider for healthcare services or vice versa. | Conditional | The value must consist of digits 0 through 9 only | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT208-0001 | |
| 2256 | COT208 | DESTINATION-ZIP-CODE | This field is required if state has captured this information, otherwise it is conditional. If the last 4 digits are not populated or used, then the 4-digit extended zip code should be recorded as “0000”. | 9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT208-0002 | |||
| 2257 | COT209 | BENEFIT-TYPE | The benefit category corresponding to the service reported on the claim or encounter record. Note: The code definitions in the valid value list originate from the Medicaid and CHIP Program Data System’s (MACPro’s) benefit type list. See Appendix H: Benefit Types for descriptions of the categories. |
Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 2/25/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT209-0001 |
| 2258 | COT210 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | This code indicates if the claim was matched with Title XIX or Title XXI. | Required | Value must be equal to a valid value. | 01 Federal funding under Title XIX 02 Federal funding under Title XXI 03 Federal funding under ACA 04 Federal funding under other legislation |
4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT210-0001 |
| 2259 | COT210 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | If an individual is not eligible for S-CHIP, then any associated claims records should not have reimbursed with federal funding under Title XXI. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT210-0002 | |||
| 2260 | COT210 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | If an individual is not eligible for Medicaid, then any associated claims records should not have reimbursed with federal funding under Title XIX. | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT210-0003 | |||
| 2261 | COT211 | XIX-MBESCBES-CATEGORY-OF-SERVICE | A code indicating the category of service for the paid claim. The category of service is the line item from the CMS-64 form that states use to report their expenditures and request federal financial participation. | Conditional | Value must be equal to a valid value. | See Appendix I for listing of valid values. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT211-0001 |
| 2262 | COT211 | XIX-MBESCBES-CATEGORY-OF-SERVICE | Males cannot receive services where the category of service is "Other Pregnancy-related Procedures", "Nurse Mid-wife", "Freestanding Birth Center" or "Tobacco Cessation for Pregnant Women". | 4/30/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT211-0002 | |||
| 2263 | COT212 | XXI-MBESCBES-CATEGORY-OF-SERVICE | A code indicating the category of service for the paid claim. The category of service is the line item from the CMS-21 form that states use to report their expenditures and request federal financial participation. Refer to Attachment 8 for definitions on the various categories of service. | Conditional | Value must be equal to a valid value. | See Appendix J for listing of valid values. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT212-0001 |
| 2264 | COT212 | XXI-MBESCBES-CATEGORY-OF-SERVICE | A code indicating the category of service for the paid claim. The category of service is the line item from the CMS-21 form that states use to report their expenditures and request federal financial participation. Refer to Attachment 8 for definitions on the various categories of service. | Conditional | Value must be equal to a valid value. | See Appendix J for listing of valid values. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT212-0002 |
| 2265 | COT213 | OTHER-INSURANCE-AMT | The amount paid by insurance other than Medicare or Medicaid on this claim. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT213-0001 | |
| 2266 | COT214 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT214-0001 | |
| 2267 | COT214 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT214-0002 | |||
| 2268 | COT217 | NATIONAL-DRUG-CODE | A code in National Drug Code (NDC) format indicating the drug, device, or medical supply covered by this claim. | Conditional | Position 10-11 must be Alpha Numeric or blank | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT217-0001 | |
| 2269 | COT217 | NATIONAL-DRUG-CODE | Position 1-5 must be Numeric | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT217-0002 | |||
| 2270 | COT217 | NATIONAL-DRUG-CODE | Position 6-9 must be Alpha Numeric | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT217-0003 | |||
| 2271 | COT217 | NATIONAL-DRUG-CODE | Drug code formats must be supplied by State in advance of submitting any file data. States must inform CMS of the NDC segments used and their size (e.g., {5, 4, 2} or {5, 4} as defined in the National Drug Code Directory). | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT217-0004 | |||
| 2272 | COT217 | NATIONAL-DRUG-CODE | If the Drug Code is less than 11 characters in length, the value must be left justified and padded with spaces. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT217-0005 | |||
| 2273 | COT217 | NATIONAL-DRUG-CODE | If Durable Medical Equipment or supply is prescribed by a physician and provided by a pharmacy then HCPCS or state specific codes can be put in the NDC field. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT217-0006 | |||
| 2274 | COT217 | NATIONAL-DRUG-CODE | This field is applicable only for TYPE-OF-SERVICE = 035, 036, 077, 062, 063, 064, 065, 066, 067, 068, 069, 073, 074, 075, 076, 077, 078, 079, 080, 081, 082, 083, 084, 033, 034. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT217-0007 | |||
| 2275 | COT227 | PROCEDURE-CODE-MOD-2 | A field to capture a modifier code associated with the PROCEDURE-CODE field on the OT claim line. If more than one modifier is reported, the additional codes should be captured in fields "PROCEDURE-CODE-MOD-2" through "PROCEDURE-CODE-MOD-4. | Conditional | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT227-0001 |
| 2276 | COT227 | PROCEDURE-CODE-MOD-2 | If no corresponding procedure (PROCDURE-CODE-2 through PROCDURE-CODE-6) was performed, 8-fill | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT227-0002 | |||
| 2277 | COT227 | PROCEDURE-CODE-MOD-2 | Value must be "Not Applicable" if PROCEDURE-CODE is "Not Applicable". | 9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT227-0003 | |||
| 2278 |
|
PROCEDURE-CODE-MOD-2 | If PROCEDURE-CODE-2 <> "88888888", then PROCEDURE-CODE-MOD-2 must <> "88". | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT227-0004 | |||
| 2279 | COT227 | PROCEDURE-CODE-MOD-2 | Do not use multiple instances of PROCEDURE-CODE-MOD if the preceding PROCEDURE-CODE-MOD element is not populated. (i.e. if PROCEDURE-CODE-MOD-2 is populated, but PROCEDURE-CODE-MOD-3 is blank-filled, then PROCEDURE-CODE-MOD-4 must also not be valued. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT227-0005 | |||
| 2280 | COT218 | PROCEDURE-CODE-MOD-3 | A field to capture a modifier code associated with the PROCEDURE-CODE field on the OT claim line. If more than one modifier is reported, the additional codes should be captured in fields "PROCEDURE-CODE-MOD-2" through "PROCEDURE-CODE-MOD-4. |
Conditional | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT218-0001 |
| 2281 | COT218 | PROCEDURE-CODE-MOD-3 | Value must be "Not Applicable" if PROCEDURE-CODE is "Not Applicable". | 9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT218-0002 | |||
| 2282 |
|
PROCEDURE-CODE-MOD-3 | If PROCEDURE-CODE-3 <> "88888888", then PROCEDURE-CODE-MOD-3 must <> "88". | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT218-0003 | |||
| 2283 | COT218 | PROCEDURE-CODE-MOD-3 | Do not use multiple instances of PROCEDURE-CODE-MOD if the preceding PROCEDURE-CODE-MOD element is not populated. (i.e. if PROCEDURE-CODE-MOD-2 is populated, but PROCEDURE-CODE-MOD-3 is blank-filled, then PROCEDURE-CODE-MOD-4 must also not be valued. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT218-0004 | |||
| 2284 | COT218 | PROCEDURE-CODE-MOD-3 | If no corresponding procedure (PROCDURE-CODE-2 through PROCDURE-CODE-6) was performed, 8-fill | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT218-0005 | |||
| 2285 | COT219 | PROCEDURE-CODE-MOD-4 | A field to capture a modifier code associated with the PROCEDURE-CODE field on the OT claim line. If more than one modifier is reported, the additional codes should be captured in fields "PROCEDURE-CODE-MOD-2" through "PROCEDURE-CODE-MOD-4. |
Conditional | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT219-0001 |
| 2286 | COT219 | PROCEDURE-CODE-MOD-4 | Value must be "Not Applicable" if PROCEDURE-CODE is "Not Applicable". | 9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT219-0002 | |||
| 2287 |
|
PROCEDURE-CODE-MOD-4 | If PROCEDURE-CODE-4 <> "88888888", then PROCEDURE-CODE-MOD-4 must <> "88". | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT219-0003 | |||
| 2288 | COT219 | PROCEDURE-CODE-MOD-4 | Do not use multiple instances of PROCEDURE-CODE-MOD if the preceding PROCEDURE-CODE-MOD element is not populated. (i.e. if PROCEDURE-CODE-MOD-2 is populated, but PROCEDURE-CODE-MOD-3 is blank-filled, then PROCEDURE-CODE-MOD-4 must also not be valued. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT219-0004 | |||
| 2289 | COT219 | PROCEDURE-CODE-MOD-4 | If no corresponding procedure (PROCDURE-CODE-2 through PROCDURE-CODE-6) was performed, 8-fill | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT219-0005 | |||
| 2290 | COT220 | HCPCS-RATE | For outpatient hospital facility claims, HCPCS/CPT is captured here. This data element is expected to capture data from HIPAA 837I claim loop 2400 SV202 or UB-04 FL 44 (only if the value represents a HCPCS/CPT). If HCPCS-RATE is populated then PROCEDURE-CODE should not be populated. | Conditional | Value must be equal to a valid value. | http://www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/index.html?redirect=/medhcpcsgeninfo/ | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT220-0001 |
| 2291 | COT221 | ADJUDICATION-DATE | The date on which the payment status of the claim was finally adjudicated by the state. | Required | Date format is CCYYMMDD (National Data Standard). | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT221-0001 | |
| 2292 | COT221 | ADJUDICATION-DATE | Value must be a valid date | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT221-0002 | |||
| 2293 | COT221 | ADJUDICATION-DATE | For Adjustment Records (ADJUSTMENT-INDICATOR<> 0), use date of final adjudication when possible. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT221-0003 | |||
| 2294 | COT221 | ADJUDICATION-DATE | For Encounter Records (TYPE-OF-CLAIM=3, C, W); use date the encounter was processed by the state. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT221-0004 | |||
| 2295 | COT221 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or before END-OF-TIME-PERIOD included in the T-MSIS HEADER RECORD | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT221-0005 | |||
| 2296 | COT221 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or after the ADMISSION-DATE | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT221-0006 | |||
| 2297 | COT221 | ADJUDICATION-DATE | This date must occur on or after the DATE-OF-BIRTH in the Eligible Record when the eligible is not a CHIP unborn child. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT221-0007 | |||
| 2298 | COT221 | ADJUDICATION-DATE | A Medicaid or CHIP eligible individual should not have had a claim adjudicated before their five-year immigration ineligible status has expired, except when the eligible is an unborn child in the CHIP program. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT221-0008 | |||
| 2299 | COT222 | SELF-DIRECTION-TYPE | A data element to identify how the beneficiary self-directed the service, i.e. Hiring Authority (the beneficiary has decision-making authority to recruit, hire, train and supervise the individuals who furnish his/her services), Budget Authority (The beneficiary has decision-making authority over how the Medicaid funds in a budget are spent), or both Hiring and Budget Authority. | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 Hiring Authority 002 Budget Authority 003 Hiring and Budget Authority 999 Type of Authority Is Unknown |
11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT222-0001 |
| 2300 | COT223 | PRE-AUTHORIZATION-NUM | A number, code, or other value that indicates the services provided on this claim have been authorized by the payee or other service organization, or that a referral for services has been approved. (Also called Prior Authorization or Referral Number). | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT223-0001 | |
| 2301 | COT224 | NDC-UNIT-OF-MEASURE | A code to indicate the basis by which the quantity of the National Drug Code is expressed. |
Conditional | Value must be equal to a valid value. Valid Value Definition: F2 International Unit GR Gram ME Milligram ML Milliliter UN Unit |
F2 International Unit ML Milliliter GR Gram UN Unit |
11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT224-0001 |
| 2302 | COT224 | NDC-UNIT-OF-MEASURE | Enter the unit of measure for each corresponding quantity value. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT224-0002 | |||
| 2303 | COT225 | NDC-QUANTITY | This field is to capture the actual quantity of the National Drug Code being prescribed on this out-patient claim. | Conditional | Must be numeric | 11/3/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT225-0001 | |
| 2304 | COT225 | NDC-QUANTITY | This field is only applicable when the NDC code being billed can be quantified in discrete units, e.g., the number of units of a prescription/refill that were filled. | 10/10/2013 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT225-0002 | |||
| 2305 | COT215 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | CLAIMOT | CLAIM-LINE-RECORD-OT-COT00003 | COT215-0001 | |||
| 2306 | CRX001 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the CLAIM-HEADER-RECORD-IP record segment is CIP00002. | Required | Value must be equal to a valid value. | CRX00001 FILE-HEADER-RECORD-RX |
4/30/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX001-0001 |
| 2307 | CRX001 | RECORD-ID | Must be populated on every record | 4/30/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX001-0002 | |||
| 2308 | CRX001 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX001-0003 | |||
| 2309 | CRX002 | DATA-DICTIONARY-VERSION | A data element to capture the version of the T-MSIS data dictionary that was used to build the file. | Required | Use the version number specified on the title page of the data dictionary | 2/25/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX002-0001 | |
| 2310 | CRX003 | SUBMISSION-TRANSACTION-TYPE | A data element to identify the whether the transactions in the file are original submissions of the data, a resubmission of a previously submitted file, or corrections of edit rejects. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX003-0001 |
| 2311 | CRX004 | FILE-ENCODING-SPECIFICATION | A data element to denote whether the file is in fixed length line format or delimited format. | Required | Value must be equal to a valid value. | FLF - The file follows a fixed length format. PSV - The file follows a pipe-delimited format. |
4/30/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX004-0001 |
| 2312 | CRX005 | DATA-MAPPING-DOCUMENT-VERSION | A data element to identify the version of the T-MSIS data mapping document used to build the file. | Required | Use the version number specified on the title page of the data mapping document | 2/25/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX005-0001 | |
| 2313 | CRX006 | FILE-NAME | The name identifying the subject area to which the records in its file relate. Each T-MSIS submission file should only contain records for one subject area (i.e., Eligible, Third-party Liability, Provider, Managed Care Plan Information, IP claims, LT claims, Rx claims, or OT claims). | Required | Value must be equal to a valid value. | CLAIM-RX - Pharmacy Claims/Encounters File - Claims/encounters with TYPE-OF-SERVICE 033 or 034. |
10/10/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX006-0001 |
| 2314 | CRX007 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX007-0001 |
| 2315 | CRX007 | SUBMITTING-STATE | Must be populated on every record. | 2/25/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX007-0002 | |||
| 2316 | CRX007 | SUBMITTING-STATE | Value must be numeric |
4/30/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX007-0003 | |||
| 2317 | CRX007 | SUBMITTING-STATE | SUBMITTING-STATE must be equal across all record segments for a given record. | 4/30/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX007-0004 | |||
| 2318 | CRX008 | DATE-FILE-CREATED | The date on which the file was created. | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX008-0001 | |
| 2319 | CRX008 | DATE-FILE-CREATED | Value must be a valid date | 4/30/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX008-0002 | |||
| 2320 | CRX008 | DATE-FILE-CREATED | Date must be equal to or later than the date entered in the END-OF-TIME-PERIOD field. |
2/25/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX008-0003 | |||
| 2321 | CRX009 | START-OF-TIME-PERIOD | Beginning date of the time period covered by this file. | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX009-0001 | |
| 2322 | CRX009 | START-OF-TIME-PERIOD | Value must be a valid date | 4/30/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX009-0002 | |||
| 2323 | CRX010 | END-OF-TIME-PERIOD | Last date of the reporting period covered by the file to which this Header Record is attached. | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX010-0001 | |
| 2324 | CRX010 | END-OF-TIME-PERIOD | Value must be a valid date | 4/30/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX010-0002 | |||
| 2325 | CRX011 | FILE-STATUS-INDICATOR | A code to indicate whether the records in the file are test or production records. | Required | Value must be equal to a valid value. | P Production File T Test File |
2/25/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX011-0001 |
| 2326 | CRX012 | SSN-INDICATOR | Indicates whether the state uses the eligible person's social security number (SSN) instead of an MSIS identification number as the unique, unchanging eligible person identifier. | Required | Value must be equal to a valid value. | 0 State does not use SSN as MSIS-IDENTIFICATION-NUMBER 1 State uses SSN as MSIS-IDENTIFICATION-NUMBER |
4/30/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX012-0001 |
| 2327 | CRX012 | SSN-INDICATOR | A state's SSN/Non-SSN designation on the eligibility file should match on the claims files. | 4/30/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX012-0002 | |||
| 2328 | CRX012 | SSN-INDICATOR | States that are non SSN states must not submit MSIS Identification Numbers and SSNs that match for eligible individuals. | 4/30/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX012-0003 | |||
| 2329 | CRX013 | TOT-REC-CNT | A count of all records in the file except for the file header record. This count will be used as a control total to help assure that the file did not become corrupted during transmission. | Required | An integer value with no commas | 10/10/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX013-0001 | |
| 2330 | CRX155 | SEQUENCE-NUMBER | To enable state’s to sequentially number files, when related, follow-on files are necessary (i.e., update files, replacement files). This should begin with 1 for the original Create submission type and be incremented by one for each Replacement or Update submission for the same reporting period and file type (subject area). | Required | Field is required on all 'C', 'U', and 'R' record files. | 10/10/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX155-0001 | |
| 2331 | CRX155 | SEQUENCE-NUMBER | Must be numeric and > 0 | 10/10/2013 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX155-0002 | |||
| 2332 | CRX014 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX014-0001 | |
| 2333 | CRX014 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX014-0002 | |||
| 2334 | CRX015 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | CLAIMRX | FILE-HEADER-RECORD-RX-CRX00001 | CRX015-0001 | |||
| 2335 | CRX016 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the CLAIM-HEADER-RECORD-IP record segment is CIP00002. | Required | Value must be equal to a valid value. | CRX00002 CLAIM-HEADER-RECORD-RX |
4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX016-0001 |
| 2336 | CRX016 | RECORD-ID | Must be populated on every record | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX016-0002 | |||
| 2337 | CRX016 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX016-0003 | |||
| 2338 | CRX017 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX017-0001 |
| 2339 | CRX017 | SUBMITTING-STATE | Must be populated on every record. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX017-0002 | |||
| 2340 | CRX017 | SUBMITTING-STATE | Value must be numeric |
4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX017-0003 | |||
| 2341 | CRX017 | SUBMITTING-STATE | SUBMITTING-STATE must be equal across all record segments for a given record. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX017-0004 | |||
| 2342 | CRX018 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX018-0001 | |
| 2343 | CRX018 | RECORD-NUMBER | Must be numeric | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX018-0002 | |||
| 2344 | CRX018 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX018-0004 | |||
| 2345 | CRX019 | ICN-ORIG | A unique number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies an original claim. | Required | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX019-0001 | |
| 2346 | CRX019 | ICN-ORIG | Record the value exactly as it appears in the state system. Do not pad. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX019-0002 | |||
| 2347 | CRX019 | ICN-ORIG | This field should always be populated with the claim identification number assigned to the original paid/denied claim. This identification number should remain constant and be carried forward onto any adjustment claims. The intention is for this earliest claim identification number to be the link that ties the original claim and all adjustment claims together. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX019-0003 | |||
| 2348 | CRX019 | ICN-ORIG | This field should not be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX019-0004 | |||
| 2349 | CRX020 | ICN-ADJ | A unique claim number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies the adjustment claim for an original transaction. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX020-0001 | |
| 2350 | CRX020 | ICN-ADJ | Record the value exactly as it appears in the State system. Do not pad | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX020-0002 | |||
| 2351 | CRX020 | ICN-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX020-0003 | |||
| 2352 | CRX021 | SUBMITTER-ID | The Submitter ID number is the value that identifies the provider/trading partner/clearing house organization to state’s claim adjudication system. | Required | Value must not be null | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX021-0001 | |
| 2353 | CRX022 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX022-0001 | |
| 2354 | CRX022 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state ID numbers must be supplied to CMS. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX022-0002 | |||
| 2355 | CRX022 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | For SSN states, this field must contain the Eligible's Social Security Number. If the SSN is unknown and a temporary number is assigned, this field will contain that number. |
2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX022-0003 | |
| 2356 | CRX023 | CROSSOVER-INDICATOR | An indicator specifying whether the claim is a crossover claim where a portion is paid by Medicare. | Required | Value must be equal to a valid value. | 0 Not Crossover Claim 1 Crossover Claim 9 Unknown |
4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX023-0001 |
| 2357 | CRX023 | CROSSOVER-INDICATOR | If Crossover Indicator is Yes, there must be Medicare enrollment in the Eligible file for the same time period (by date of service). | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX023-0002 | |||
| 2358 | CRX023 | CROSSOVER-INDICATOR | Detail records should be created for all crossover claims. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX023-0003 | |||
| 2359 | CRX024 | 1115A-DEMONSTRATION-IND | Indicates that the individual participates in an 1115(A) demonstration. 1115(A) is a Center for Medicare and Medicaid Innovation (CMMI) demonstration. | Conditional | Value must be in the set of valid values | 0 No 1 Yes |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX024-0001 |
| 2360 | CRX024 | 1115A-DEMONSTRATION-IND | If 1115A-DEMONSTRATION-IND set to Yes on claim then there must be a 1115A-DEMONSTRATION-IND set to Yes (1115 participant) in the T-MSIS Eligible file with the same MSIS ID and/or SSN, an 1115A-EFF-DATE < the begin date of service and an 1115A-END-DATE > the end date of service on the claim. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX024-0002 | |||
| 2361 | CRX025 | ADJUSTMENT-IND | Code indicating the type of adjustment record. | Required | Value must be in the set of valid values | 0 Original Claim / Encounter 1 Void of a prior submission 2 Re-submittal 3 Credit Adjustment (negative supplemental) 4 Debit Adjustment (positive supplemental) 5 Credit Gross Adjustment. 6 Debit Gross Adjustment 9 Unknown |
4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX025-0001 |
| 2362 | CRX026 | ADJUSTMENT-REASON-CODE | Claim adjustment reason codes communicate why a claim was paid differently than it was billed. | Conditional | Value must be in the set of valid values | http://www.wpc-edi.com/reference/codelists/healthcare/claim-adjustment-reason-codes/ | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX026-0001 |
| 2363 | CRX026 | ADJUSTMENT-REASON-CODE | if there is no adjustment to a claim, then there is no adjustment reason code. (Also see: CLAIM-PYMT-REM-CODE). | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX026-0002 | |||
| 2364 | CRX027 | ADJUDICATION-DATE | The date on which the payment status of the claim was finally adjudicated by the state. |
Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX027-0001 | |
| 2365 | CRX027 | ADJUDICATION-DATE | Value must be a valid date | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX027-0002 | |||
| 2366 | CRX027 | ADJUDICATION-DATE | For Encounter Records (TYPE-OF-CLAIM=3, C, W); use date the encounter was processed by the state. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX027-0003 | |||
| 2367 | CRX027 | ADJUDICATION-DATE | For Adjustment Records (ADJUSTMENT-INDICATOR<> 0), use date of final adjudication when possible. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX027-0004 | |||
| 2368 | CRX027 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or before END-OF-TIME-PERIOD included in the T-MSIS HEADER RECORD | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX027-0005 | |||
| 2369 | CRX027 | ADJUDICATION-DATE | This date must occur on or after the DATE-OF-BIRTH in the Eligible Record when the eligible is not a CHIP unborn child. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX027-0006 | |||
| 2370 | CRX027 | ADJUDICATION-DATE | A Medicaid or CHIP eligible individual should not have had a claim adjudicated before their five-year immigration ineligible status has expired, except when the eligible is an unborn child in the CHIP program. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX027-0007 | |||
| 2371 | CRX028 | MEDICAID-PAID-DATE | The date Medicaid paid on this claim or adjustment. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX028-0001 | |
| 2372 | CRX028 | MEDICAID-PAID-DATE | Value must be a valid date | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX028-0002 | |||
| 2373 | CRX029 | TYPE-OF-CLAIM | A code indicating what kind of payment is covered in this claim. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX029-0001 |
| 2374 | CRX029 | TYPE-OF-CLAIM | States should only submit CHIP claims for CHIP eligibles | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX029-0002 | |||
| 2375 | CRX029 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the basis of eligibility. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX029-0003 | |||
| 2376 | CRX029 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the maintenance assistance status. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX029-0004 | |||
| 2377 | CRX029 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the restricted benefits code. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX029-0005 | |||
| 2378 | CRX029 | TYPE-OF-CLAIM | States should not submit any Medicaid claims records for individuals who were not eligible for Medicaid according to the TANF code. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX029-0006 | |||
| 2379 | CRX030 | CLAIM-STATUS | The health care claim status codes convey the status of an entire claim. |
Required | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-codes/ | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX030-0001 |
| 2380 | CRX031 | CLAIM-STATUS-CATEGORY | The general category of the claim status (accepted, rejected, pended, finalized, additional information requested, etc.), which is then further detailed in the companion data element CLAIM-STATUS. | Required | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-category-codes/ | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX031-0001 |
| 2381 | CRX032 | SOURCE-LOCATION | The field denotes the claim payment system from which the claim was adjudicated. | Required | Value must be equal to a valid value. | 01 MMIS 02 Non-MMIS CHIP Payment System 03 Pharmacy Benefits Manager (PBM) Vendor 04 Dental Benefits Manager Vendor 05 Transportation Provider System 06 Mental Health Claims Payment System 07 Financial Transaction/Accounting System 08 Other State Agency Claims Payment System 09 County/Local Government Claims Payment System 10 Other Vendor/Other Claims Payment System 20 Managed Care Organization (MCO) 99 Unknown source |
4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX032-0001 |
| 2382 | CRX033 | CHECK-NUM | The check or EFT number. | Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9),, dashes (-), and spaces. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX033-0001 | |
| 2383 | CRX033 | CHECK-NUM | If there is a valid check date there should also be a valid check number. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX033-0002 | |||
| 2384 | CRX034 | CHECK-EFF-DATE | Date the check is issued to the payee, or if Electronic Funds Transfer (EFT), the date the transfer is made. | Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX034-0001 | |
| 2385 | CRX034 | CHECK-EFF-DATE | Value must be a valid date | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX034-0002 | |||
| 2386 | CRX034 | CHECK-EFF-DATE | Could be the same as Remittance Date. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX034-0003 | |||
| 2387 | CRX034 | CHECK-EFF-DATE | If there is a valid check number, there should also be a valid check date. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX034-0004 | |||
| 2388 | CRX035 | CLAIM-PYMT-REM-CODE-1 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX035-0001 |
| 2389 | CRX036 | CLAIM-PYMT-REM-CODE-2 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX036-0001 |
| 2390 | CRX037 | CLAIM-PYMT-REM-CODE-3 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX037-0001 |
| 2391 | CRX038 | CLAIM-PYMT-REM-CODE-4 | Remittance Advice Remark Codes are used to convey information about remittance processing or to provide a supplemental explanation for an adjustment already described by a Claim Adjustment Reason Code. Each Remittance Advice Remark Code identifies a specific message as shown in the Remittance Advice Remark Code List. It is a code set used by the health care industry to convey non-financial information critical to understanding the adjudication of a health care claim for payment. It is an external code set whose use is as mandated by the Administrative Simplification provisions of the Health Insurance Portability and Accountably Act of 1996 (P.L.104-191, commonly referred to as HIPAA). | Conditional | Value must be equal to a valid value. | Use the Remittance Advice Remark Codes at the following link: http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX038-0001 |
| 2392 | CRX039 | TOT-BILLED-AMT | The total amount charged for this claim at the claim header level as submitted by the provider. | Conditional | TOT-BILLED-AMT must be a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX039-0001 | |
| 2393 | CRX039 | TOT-BILLED-AMT | The total amount should be the sum of each of the billed amounts submitted at the claim detail level. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX039-0002 | |||
| 2394 | CRX039 | TOT-BILLED-AMT | If TYPE-OF-CLAIM = "4", then TOT-BILLED-AMT must = "00000000". | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX039-0003 | |||
| 2395 | CRX039 | TOT-BILLED-AMT | If TYPE-OF-CLAIM = 3, C, W (encounter record) this field should either be zero-filled or contain the amount paid by the plan to the provider. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX039-0004 | |||
| 2396 | CRX040 | TOT-ALLOWED-AMT | The claim header level maximum amount determined by the payer as being 'allowable' under the provisions of the contract prior to the determination of actual payment. | Conditional | TOT-ALLOWED-AMT must be a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX040-0001 | |
| 2397 | CRX040 | TOT-ALLOWED-AMT | The sum of the allowed amounts at the detailed levels must equal TOT-ALLOWED-AMT | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX040-0002 | |||
| 2398 | CRX041 | TOT-MEDICAID-PAID-AMT | The total amount paid by Medicaid on this claim or adjustment at the claim header level, which is the sum of the amounts paid by Medicaid at the detail level for the claim. | Required | TOT-MEDICAID-PAID-AMT must be a valid dollar amount | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX041-0001 | |
| 2399 | CRX042 | TOT-COPAY-AMT | The total amount paid by Medicaid/CHIP enrollee for each office or emergency department visit or purchase of prescription drugs in addition to the amount paid by Medicaid/CHIP. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX042-0001 | |
| 2400 | CRX043 | TOT-MEDICARE-DEDUCTIBLE-AMT | The amount paid by Medicaid/CHIP on this claim at the claim header level toward the beneficiary’s Medicare deductible. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX043-0001 | |
| 2401 | CRX043 | TOT-MEDICARE-DEDUCTIBLE-AMT | if the Medicare deductible amount can be identified separately from Medicare coinsurance payments, code that amount in this field. If the Medicare coinsurance and deductible payments cannot be separated, fill this field with the combined payment amount and code 0 in TOT-MEDICARE-COINS-AMT. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX043-0002 | |||
| 2402 | CRX043 | TOT-MEDICARE-DEDUCTIBLE-AMT | The total medicare deductible amount must be less than or equal the total billed amount. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX043-0003 | |||
| 2403 | CRX044 | TOT-MEDICARE-COINS-AMT | The amount paid by Medicaid/CHIP on this claim at the claim header level toward the beneficiary’s Medicare coinsurance | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX044-0001 | |
| 2404 | CRX044 | TOT-MEDICARE-COINS-AMT | If the Medicare coinsurance amount can be identified separately from Medicare deductible payments, code that amount in this field. If Medicare coinsurance and deductible payments cannot be separated, fill this field with 99998 and code the combined payment amount in TOT-MEDICARE-DEDUCTIBLE-AMT. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX044-0002 | |||
| 2405 | CRX044 | TOT-MEDICARE-COINS-AMT | For TYPE-OF-CLAIM = 3, C, W (encounter record), 8-fill. | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX044-0003 | |||
| 2406 | CRX045 | TOT-TPL-AMT | Third Party Liability (TPL) refers to the legal obligation of third parties, i.e., certain individuals, entities, or programs, to pay all or part of the expenditures for medical assistance furnished under a state plan. This is the total amount denoted at the claim header level paid by the third party. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX045-0001 | |
| 2407 | CRX045 | TOT-TPL-AMT | Absolute value of TOT-TPL-AMT must be < Absolute value of (TOT-BILLED-AMT - (minus) TOT-MEDICARE-COINS-AMT + (plus) TOT-MEDICARE-DEDUCTIBLE-AMT). | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX045-0002 | |||
| 2408 | CRX047 | TOT-OTHER-INSURANCE-AMT | The amount paid by insurance other than Medicare or Medicaid on this claim. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX047-0001 | |
| 2409 | CRX048 | OTHER-INSURANCE-IND | The field denotes whether the insured party is covered under other insurance plan. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 9 Unknown |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX048-0001 |
| 2410 | CRX049 | OTHER-TPL-COLLECTION | This data element indicates that the claim is for a beneficiary for whom other third party resource development and collection activities are in progress, when the liability is not another health insurance plan for which the eligible is a beneficiary. | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 Third Party Resource is Casualty/Tort 002 Third Party Resource is Estate 003 Third Party Resource is Lien (TEFRA) 004 Third Party Resource is Lien (Other) 005 Third Party Resource is Worker’s Compensation 006 Third Party Resource is Medical Malpractice 007 Third Party Resource is Other 999 Classification of Third Party Resource is Unknown |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX049-0001 |
| 2411 | CRX050 | SERVICE-TRACKING-TYPE | A code to categorize service tracking claims. A “service tracking claim” is used to report lump sum payments that cannot be attributed to a single enrollee. (Note: Use an encounter record to report services provided under a capitated payment arrangement.) | Conditional | Value must be equal to a valid value. | 00 Not a Service Tracking Claim 01 Drug Rebate 02 DSH Payment 03 Lump Sum Payment 04 Cost Settlement 05 Supplemental 06 Other 99 Unknown |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX050-0001 |
| 2412 | CRX051 | SERVICE-TRACKING-PAYMENT-AMT | On service tracking claims, the lump sum amount paid to the provider. | Conditional | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX051-0001 | |
| 2413 | CRX051 | SERVICE-TRACKING-PAYMENT-AMT | Amount paid for services received by an individual patient, when the state accepts a lump sum form a provider that covered similar services delivered to more than one patient, such as a group screening for EPSDT. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX051-0002 | |||
| 2414 | CRX051 | SERVICE-TRACKING-PAYMENT-AMT | Required on service tracking records | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX051-0003 | |||
| 2415 | CRX051 | SERVICE-TRACKING-PAYMENT-AMT | If there is a service tracking type, then there must also be a service tracking payment amount. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX051-0004 | |||
| 2416 | CRX051 | SERVICE-TRACKING-PAYMENT-AMT | For service tracking payments, ensure that the TOT-MEDICAID-PAID-AMOUNT is 0 filled and provide payment amount in SERVICE-TRACKING-PAYMENT-AMT only. | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX051-0005 | |||
| 2417 | CRX052 | FIXED-PAYMENT-IND | This code indicates that the reimbursement amount included on the claim is for a fixed payment. Fixed payments are made by the state to insurers or providers for premiums or eligible coverage, not for a particular service. For example, some states have Primary Care Case Management (PCCM) programs where the state pays providers a monthly patient management fee of $3.50 for each eligible participant under their care. This fee is considered a fixed payment. It is very important for states to correctly identify fixed payments. Fixed payments do not have a defined “medical record” associated with the payment; therefore, fixed payments are not subject to medical record request and medical record review. |
Conditional | Value must be equal to a valid value. | 0 Not Fixed Payment 1 FFS Fixed Payment |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX052-0001 |
| 2418 | CRX053 | FUNDING-CODE | A code to indicate the source of non-federal share funds. | Required | Value must be equal to a valid value. | A Medicaid Agency B CHIP Agency C Mental Health Service Agency D Education Agency E Child and Family Services Agency F County G City H Providers I Other |
10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX053-0001 |
| 2419 | CRX054 | FUNDING-SOURCE-NONFEDERAL-SHARE | A code to indicate the type of non-federal share used by the state to finance its expenditure to the provider. | Required | Value must be equal to a valid value. When states have multiple sources of FUNDING-SOURCE-NONFEDERAL-SHARE, States are to report the portion which represents the largest proportion as the FUNDING-SOURCE-NONFEDERAL-SHARE. |
01 State appropriations to the Medicaid agency 02 Intergovernmental transfers (IGT) 03 Certified public expenditures (CPE) 04 Provider taxes 05 Donations |
9/23/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX054-0001 |
| 2420 | CRX055 | PROGRAM-TYPE | Code indicating special Medicaid program under which the service was provided. Refer to Appendix E for information on the various program types. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX055-0001 |
| 2421 | CRX055 | PROGRAM-TYPE | If PROGRAM-TYPE=Community First Choice (11) then [T-MSIS ELIGIBLE FILE] STATE-PLAN-OPTION-TYPE must = 01 for the same time period. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX055-0002 | |||
| 2422 | CRX055 | PROGRAM-TYPE | If PROGRAM-TYPE=Community First Choice (11) then [T-MSIS ELIGIBLE FILE] STATE-PLAN-OPTION-TYPE must = 01 for the same time period. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX055-0003 | |||
| 2423 | CRX055 | PROGRAM-TYPE | If PROGRAM-TYPE=1915(i) (value=13) then [T-MSIS ELIGIBLE FILE] STATE-PLAN-OPTION-TYPE must = 02 for the same time period. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX055-0004 | |||
| 2424 | CRX055 | PROGRAM-TYPE | Value for 1915 (c) waiver must correspond to the values for 1915(c) waiver in the Waiver Type. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX055-0005 | |||
| 2425 | CRX056 | PLAN-ID-NUMBER | A unique number, assigned by the state, which represents the health plan under which the non-fee-for-service encounter was provided including through the state plan and a waiver. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX056-0001 | |
| 2426 | CRX056 | PLAN-ID-NUMBER | use the number as it is carried in the state’s system. (TYPE-OF-CLAIM=3, C, W OR TYPE-OF-SERVICE=119, 120, 122). |
2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX056-0002 | |||
| 2427 | CRX056 | PLAN-ID-NUMBER | if TYPE-OF-CLAIM<>3, C, W (Encounter Record) AND TYPE-OF-SERVICE<> {119, 120, 121, 122), 8-fill | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX056-0003 | |||
| 2428 | CRX056 | PLAN-ID-NUMBER | If TYPE-OF-CLAIM <> Encounter or Capitation Payment, 8-fill. | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX056-0004 | |||
| 2429 | CRX056 | PLAN-ID-NUMBER | This data element must equal the BILLING-PROV-NUM if the TYPE-OF-SERVICE is a capitation payment. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX056-0005 | |||
| 2430 | CRX056 | PLAN-ID-NUMBER | The managed care ID on the individual's eligible record must match that which is included on any claims records for the eligible individual. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX056-0006 | |||
| 2431 | CRX057 | NATIONAL-HEALTH-CARE-ENTITY-ID | The national identifier of the health care entity (controlling health plan, subhealth plan, or other entity) at the most granular sub-health plan level of the Medicaid or CHIP health plan in which an individual is enrolled. (See 45 CFR 162 Subpart E. http://www.gpo.gov/fdsys/pkg/FR-2012-09-05/pdf/2012-21238.pdf | NA | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX057-0001 | |
| 2432 | CRX057 | NATIONAL-HEALTH-CARE-ENTITY-ID | NA | Large health plans are required to obtain national health plan identifiers by November 5, 2014, small health plans by November 5, 2015. States may report prior to these dates if available. |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX057-0002 | ||
| 2433 | CRX057 | NATIONAL-HEALTH-CARE-ENTITY-ID | This field is required for all managed care claims and encounters with dates of service on or after the mandated dates above. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX057-0003 | |||
| 2434 | CRX057 | NATIONAL-HEALTH-CARE-ENTITY-ID | NATIONAL-HEALTH-CARE-ENTITY-IDs on managed care claims and encounters must match NATIONAL-HEALTH-CARE-ENTITY-IDs on file for the individual in the eligibility subject area or the TPL subject area. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX057-0004 | |||
| 2435 | CRX058 | PAYMENT-LEVEL-IND | The field denotes whether the claim payment is made at the header level or the detail level. | Required | Value must be equal to a valid value. | 1 Claim Header – Sum of Line Item payments 2 Claim Detail – Individual Line Item payments |
4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX058-0001 |
| 2436 | CRX058 | PAYMENT-LEVEL-IND | Payment fields at either the claim header or line on encounter records should be left blank. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX058-0002 | |||
| 2437 | CRX059 | MEDICARE-REIM-TYPE | This code indicates the type of Medicare Reimbursement. | Conditional | Value must be equal to a valid value. | 01 IPPS - Acute Inpatient PPS 02 LTCHPPS - Long-term Care Hospital PPS 03 SNFPPS - Skilled Nursing Facility PPS 04 HHPPS - Home Health PPS 05 IRFPPS - Inpatient Rehabilitation Facility PPS 06 IPFPPS - Inpatient Psychiatric Facility PPS 07 OPPS - Outpatient PPS 08 Fee Schedules (for physicians, DME, ambulance, and clinical lab) 09 Part C Hierarchical Condition Category Risk Assessment (CMS-HCC RA) Capitation Payment Model |
10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX059-0001 |
| 2438 | CRX059 | MEDICARE-REIM-TYPE | If this is a crossover Medicare claim, the claim must have a MEDICARE-REIM-TYPE. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX059-0002 | |||
| 2439 | CRX060 | CLAIM-LINE-COUNT | The total number of lines on the claim. | Required | Must be populated on every record | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX060-0001 | |
| 2440 | CRX060 | CLAIM-LINE-COUNT | The claim line count should equal the sum of the claim lines for this record. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX060-0002 | |||
| 2441 | CRX061 | FORCED-CLAIM-IND | This code indicates if the claim was processed by forcing it through a manual override process. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX061-0001 |
| 2442 | CRX062 | PATIENT-CONTROL-NUM | A patient's unique number assigned by the provider agency during claim submission, which identifies the client or the client’s episode of service within the provider’s system to facilitate retrieval of individual financial and clinical records and posting of payment. | Conditional | Must be numeric (0-9) and/or alphabetic (A-Z). Special characters are invalid entries | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX062-0001 | |
| 2443 | CRX063 | ELIGIBLE-LAST-NAME | The last name of the individual to whom the services were provided. (The patients name should be captured as it appears on the claim record, it does not need to be the same as it appears on the eligibility file. The MSIS-IDENTIFICATION-NUM will be used to associate a claim record with the appropriate eligibility data.) | Required | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX063-0001 | |
| 2444 | CRX063 | ELIGIBLE-LAST-NAME | When populating the eligible person’s name on T-MSIS Claim Files, use the patient’s name from the claim transaction rather than the eligible person’s name from the T-MSIS Eligible File. | 9/23/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX063-0002 | |||
| 2445 | CRX064 | ELIGIBLE-FIRST-NAME | The first name of the individual to whom the services were provided. (The patients name should be captured as it appears on the claim record, it does not need to be the same as it appears on the eligibility file. The MSIS-IDENTIFICATION-NUM will be used to associate a claim record with the appropriate eligibility data.) | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX064-0001 | |
| 2446 | CRX064 | ELIGIBLE-FIRST-NAME | When populating the eligible person’s name on T-MSIS Claim Files, use the patient’s name from the claim transaction rather than the eligible person’s name from the T-MSIS Eligible File. | 9/23/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX064-0002 | |||
| 2447 | CRX065 | ELIGIBLE-MIDDLE-INIT | The middle initial of the individual to whom the services were provided. (The patients name should be captured as it appears on the claim record, it does not need to be the same as it appears on the eligibility file. The MSIS-IDENTIFICATION-NUM will be used to associate a claim record with the appropriate eligibility data.) | Conditional | Value must be an alphabetic character, or a blank (A-Z, a-z, ) | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX065-0001 | |
| 2448 | CRX065 | ELIGIBLE-MIDDLE-INIT | Leave blank if not available When populating the eligible person’s name on T-MSIS Claim Files, use the patient’s name from the claim transaction rather than use the eligible person’s name from the T-MSIS Eligible File. |
9/23/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX065-0002 | |||
| 2449 | CRX066 | DATE-OF-BIRTH | Date of birth of the individual to whom the services were provided. | Required | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX066-0001 | |
| 2450 | CRX066 | DATE-OF-BIRTH | Value must be a valid date | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX066-0002 | |||
| 2451 | CRX066 | DATE-OF-BIRTH | The numeric form for days and months from 1 to 9 must have a zero as the first digit. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX066-0003 | |||
| 2452 | CRX066 | DATE-OF-BIRTH | The patient’s date of birth shall be reported in numeric form as follows – 2 digit month, 2 digit day, and 4 digit year | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX066-0004 | |||
| 2453 | CRX066 | DATE-OF-BIRTH | A patient's age should not be greater than 112 years. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX066-0005 | |||
| 2454 | CRX067 | HEALTH-HOME-PROV-IND | This code indicates whether the claim is submitted by a provider or provider group enrolled in the Health Home care model. Health home providers provide service for patients with chronic illnesses. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 8 Not Applicable 9 Unknown |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX067-0001 |
| 2455 | CRX067 | HEALTH-HOME-PROV-IND | if a state has not yet begun collecting this information, HEALTH-HOME-PROVIDER-IND, this field should be defaulted to the value “8.” | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX067-0002 | |||
| 2456 | CRX067 | HEALTH-HOME-PROV-IND | If there is a HEALTH-HOME-ENTITY-NAME then HEALTH-HOME-PROV-IND must indicate yes. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX067-0003 | |||
| 2457 | CRX067 | HEALTH-HOME-PROV-IND | States should not submit claim records for an eligible individual that indicate the claim was submitted by a provider or provider group enrolled in a health home model if the eligible individual is not enrolled in the health home program. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX067-0004 | |||
| 2458 | CRX067 | HEALTH-HOME-PROV-IND | States that do not specify an eligible individual's health home provider number, if applicable, should not report claims that indicate the claim is submitted by a provider or provider group enrolled in the health home model. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX067-0005 | |||
| 2459 | CRX068 | WAIVER-TYPE | Code for specifying waiver type under which the eligible individual is covered during the month and receiving services/under which claim is submitted. | Conditional | Enter the WAIVER-TYPE assigned | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX068-0001 |
| 2460 | CRX068 | WAIVER-TYPE | Value must correspond to associated WAIVER-ID | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX068-0002 | |||
| 2461 | CRX068 | WAIVER-TYPE | WAIVER-TYPE on claim must match [T-MSIS ELIGIBLE FILE]WAIVER-TYPE for the enrollee for the same time period (by date of service). | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX068-0003 | |||
| 2462 | CRX068 | WAIVER-TYPE | An ineligible individual cannot have a category for federal reimbursement for Medicaid or CHIP (CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT <> 01,02) | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX068-0004 | |||
| 2463 | CRX069 | WAIVER-ID | Field specifying the waiver or demonstration which authorized payment for a claim. These IDs must be the approved, full federal waiver ID number assigned during the state submission and CMS approval process. The categories of demonstration and waiver programs include: 1915(b)(1); 1915(b)(2); 1915(b)(3), and 1915(b)(4) managed care waivers; 1915(c) home and community based services waivers; combined 1915(b) and 1915(c) managed home and community based services waivers and 1115 demonstrations. | Conditional | Valid values are supplied by the state. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | ||
| 2464 | CRX069 | WAIVER-ID | If the goods & services rendered do not fall under a waiver, leave this field blank. | 11/9/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX069-0002 | |||
| 2465 | CRX069 | WAIVER-ID | Report the full federal waiver identifier. | 11/9/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX069-0003 | |||
| 2466 | CRX069 | WAIVER-ID | If there's a waiver type, there should be a corresponding waiver id. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX069-0005 | |||
| 2467 | CRX070 | BILLING-PROV-NUM | A unique identification number assigned by the state to a provider or capitation plan. This should represent the entity billing for the service. | Required | A list of valid codes must be supplied by the state prior to submission of any file data | Valid values are supplied by the state. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX070-0001 |
| 2468 | CRX070 | BILLING-PROV-NUM | For encounter records (TYPE-OF-CLAIM = 3, C, W), this represents the entity billing (or reporting) to the managed care plan (See PLAN-ID-NUMBER for reporting capitation plan-ID). Capitation PLAN-ID should be used in this field only for capitation payments (TYPE-OF-SERVICE = 119, 120, 122). | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX070-0002 | |||
| 2469 | CRX070 | BILLING-PROV-NUM | if value is invalid, record it exactly as it appears in the state system. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX070-0003 | |||
| 2470 | CRX071 | BILLING-PROV-NPI-NUM | The National Provider ID (NPI) of the billing provider responsible for billing for the service on the claim. The billing provider can also be servicing, referring, or prescribing provider; can be admitting provider except for Long Term Care. |
Required | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX071-0001 | |
| 2471 | CRX071 | BILLING-PROV-NPI-NUM | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX071-0002 | ||
| 2472 | CRX071 | BILLING-PROV-NPI-NUM | For encounter records (TYPE-OF-CLAIM = 3, C, W), the BILLIN-PROV-NPI-NUM field should be populated with the NPI of the provider or entity billing (or reporting) to the managed care plan. For financial transactions (i.e., expenditure transactions or recoupments of previously made expenditures that do not flow through the usual claim adjudication/adjustment process or encounter record reporting process), the BILLIN-PROV-NPI-NUM field should be populated with the NPI of the provider or entity to which the financial transaction was addressed, unless the transaction is a payment/recoupment made-to/received-from a managed care plan, in which case the BILLING-PROV-NPI-NUM should be left blank. For financial transactions with managed care plans, the plan's ID should be reported in the PLAN-ID-NUMBER field and the BILLING-PROV-NPI-NUM should be left blank. |
2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX071-0003 | |||
| 2473 | CRX071 | BILLING-PROV-NPI-NUM | Billing Provider must be enrolled | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX071-0004 | |||
| 2474 | CRX072 | BILLING-PROV-TAXONOMY | For CLAIMOT and CLAIMRX files, the taxonomy code for the provider billing for the service. | Conditional | Value must be in the set of valid values | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX072-0001 |
| 2475 | CRX072 | BILLING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX072-0002 | |||
| 2476 | CRX072 | BILLING-PROV-TAXONOMY | Conditional | 8-fill field for capitation or premium payments (TYPE-OF-SERVICE = 119, 120, 121, 122) |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX072-0003 | ||
| 2477 | CRX073 | BILLING-PROV-SPECIALTY | This code describes the area of specialty for the billing provider. | Conditional | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX073-0001 |
| 2478 | CRX074 | PRESCRIBING-PROV-NUM | A unique identification number assigned by the state to the provider who prescribed the drug, device, or supply. This must be the individual’s ID number, not a group identification number. | Required | Valid formats must be supplied by the state in advance of submitting file data. |
Valid values are supplied by the state. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX074-0001 |
| 2479 | CRX074 | PRESCRIBING-PROV-NUM | if value is invalid, record it exactly as it appears in the state system. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX074-0002 | |||
| 2480 | CRX074 | PRESCRIBING-PROV-NUM | if the prescribing physician provider ID is not available, but the physician’s Drug Enforcement Agency (DEA) ID is on the state file, then the State should use the DEA ID for this data element | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX074-0003 | |||
| 2481 | CRX075 | PRESCRIBING-PROV-NPI-NUM | The National Provider ID (NPI) of the provider who prescribed a medication to a patient | Required | NPI must be valid. If provider does not have an NPI, leave the field blank. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX075-0001 |
| 2482 | CRX075 | PRESCRIBING-PROV-NPI-NUM | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX075-0002 | |||
| 2483 | CRX076 | PRESCRIBING-PROV-TAXONOMY | The taxonomy code for the medical provider writing the prescription | NA | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX076-0001 |
| 2484 | CRX076 | PRESCRIBING-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX076-0002 | |||
| 2485 | CRX077 | PRESCRIBING-PROV-TYPE | A code describing the type of entity prescribing the drug, device, or supply If the state uses state-specific codes, they should map their internal codes to the CMS standard list provided |
NA | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX077-0001 |
| 2486 | CRX078 | PRESCRIBING-PROV-SPECIALTY | This code indicates the area of specialty for the PRESCRIBING PROVIDER. | NA | Value must be equal to a valid value. | See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX078-0001 |
| 2487 | CRX079 | MEDICARE-HIC-NUM | Health Insurance Claim (HIC) Number as it appears on the patient’s Medicare card. | Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9) |
4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX079-0001 | |
| 2488 | CRX079 | MEDICARE-HIC-NUM | if individual is NOT enrolled in Medicare, 8-fill field. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX079-0002 | |||
| 2489 | CRX079 | MEDICARE-HIC-NUM | If this is a crossover Medicare claim, the Bene must have a MEDICARE-HIC-Num. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX079-0003 | |||
| 2490 | CRX079 | MEDICARE-HIC-NUM | States should not submit records for an eligible individual where the eligible's Medicare HIC Number does not match in the associated claim record, if applicable. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX079-0004 | |||
| 2491 | CRX079 | MEDICARE-HIC-NUM | Claims records for an eligible individual should not indicate a valid Medicare HIC number, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX079-0005 | |||
| 2492 | CRX081 | REMITTANCE-NUM | The Remittance Advice Number is a sequential number that identifies the current Remittance Advice (RA) produced for a provider. The number is incremented by one each time a new RA is generated. The first five (5) positions are Julian date YYDDD format. The RA is the detailed explanation of the reason for the payment amount. The RA number is not the check number. | Required | Limit characters to alphabet (A-Z, a-z), numerals (0-9).. | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX081-0001 | |
| 2493 | CRX081 | REMITTANCE-NUM | If there is a remittance date, then there must also be a remittance number. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX081-0002 | |||
| 2494 | CRX082 | BORDER-STATE-IND | This code indicates whether an individual received services or equipment across state borders. (The provider location is out of state, but for payment purposes the provider is treated as an in-state provider.) | Conditional | Value must be equal to a valid value. | 0 No 1 Yes |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX082-0001 |
| 2495 | CRX084 | DATE-PRESCRIBED | The date the drug, device, or supply was prescribed by the physician or other practitioner. This should not be confused with the PRESCRIPTION-FILL-DATE, which represents the date the prescription was actually filled by the provider. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX084-0001 | |
| 2496 | CRX084 | DATE-PRESCRIBED | Value must be a valid date | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX084-0002 | |||
| 2497 | CRX084 | DATE-PRESCRIBED | Date must occur on or after Date of Birth | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX084-0003 | |||
| 2498 | CRX084 | DATE-PRESCRIBED | Date must on or before Prescription Fill Date. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX084-0004 | |||
| 2499 | CRX084 | DATE-PRESCRIBED | DATE-PRESCRIBED must occur on or before ADJUDICATION-DATE. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX084-0005 | |||
| 2500 | CRX084 | DATE-PRESCRIBED | Date must occur on or before Date of Death. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX084-0006 | |||
| 2501 | CRX085 | PRESCRIPTION-FILL-DATE | Date the drug, device, or supply was dispensed by the provider. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX085-0001 | |
| 2502 | CRX085 | PRESCRIPTION-FILL-DATE | The date must be a valid date. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX085-0002 | |||
| 2503 | CRX085 | PRESCRIPTION-FILL-DATE | PRESCRIPTION-FILL-DATE must occur on or before END-OF-TIME-PERIOD | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX085-0003 | |||
| 2504 | CRX085 | PRESCRIPTION-FILL-DATE | PRESCRIPTION-FILL-DATE must occur on or after START-OF-TIME-PERIOD | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX085-0004 | |||
| 2505 | CRX085 | PRESCRIPTION-FILL-DATE | PRESCRIPTION-FILL-DATE must occur on or after DATE-PRESCRIBED | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX085-0005 | |||
| 2506 | CRX085 | PRESCRIPTION-FILL-DATE | Date must occur on or after Date of Birth | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX085-0006 | |||
| 2507 | CRX085 | PRESCRIPTION-FILL-DATE | Date must occur on or before Date of Death. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX085-0007 | |||
| 2508 | CRX086 | COMPOUND-DRUG-IND | Indicator to specify if the drug is compound or not. | Conditional | Value must be in the set of valid values | 0 Not Compound 1 Compound 9 Unknown |
4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX086-0001 |
| 2509 | CRX087 | BENEFICIARY-COINSURANCE-AMOUNT | The amount of money the beneficiary paid towards coinsurance. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX087-0001 | |
| 2510 | CRX087 | BENEFICIARY-COINSURANCE-AMOUNT | if no coinsurance is applicable enter 0.00. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX087-0002 | |||
| 2511 | CRX089 | BENEFICIARY-COPAYMENT-AMOUNT | The amount of money the beneficiary paid towards a copayment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX089-0001 | |
| 2512 | CRX089 | BENEFICIARY-COPAYMENT-AMOUNT | if no copayment is applicable enter 0.00. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX089-0002 | |||
| 2513 | CRX090 | BENEFICIARY-COPAYMENT-DATE-PAID | The date the beneficiary paid the copayment amount. | Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX090-0001 | |
| 2514 | CRX088 | BENEFICIARY-COINSURANCE-DATE-PAID | The date the beneficiary paid the coinsurance amount. | Conditional | Date format should be CCYYMMDD (National Data Standard) | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX088-0001 | |
| 2515 | CRX088 | BENEFICIARY-COINSURANCE-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX088-0002 | |||
| 2516 | CRX092 | BENEFICIARY-DEDUCTIBLE-AMOUNT | The amount of money the beneficiary paid towards an annual deductible. |
Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX092-0001 | |
| 2517 | CRX092 | BENEFICIARY-DEDUCTIBLE-AMOUNT | if no deductible is applicable enter 0.00. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX092-0002 | |||
| 2518 | CRX093 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | The date the beneficiary paid the deductible amount. |
Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX093-0001 | |
| 2519 | CRX093 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | Value must be a valid date | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX093-0002 | |||
| 2520 | CRX093 | BENEFICIARY-DEDUCTIBLE-DATE-PAID | if no coinsurance is applicable, 8-fill. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX093-0003 | |||
| 2521 | CRX094 | CLAIM-DENIED-INDICATOR | An indicator to identify a claim that the state refused pay in its entirety. |
Conditional | Value must be in the set of valid values | 0 Denied: The payment of claim in its entirety was denied by the state. 1 Not Denied: The state paid some or the all of the claim. |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX094-0001 |
| 2522 | CRX094 | CLAIM-DENIED-INDICATOR | it is expected that states will submit all denied claims to CMS | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX094-0002 | |||
| 2523 | CRX094 | CLAIM-DENIED-INDICATOR | If the Type of Claim indicates the claim was denied, then this indicator must also indicate the claim was denied. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX094-0003 | |||
| 2524 | CRX095 | COPAY-WAIVED-IND | An indicator signifying that the copay was waived by the provider. |
Optional | Value must be equal to a valid value. | 0 Not Waived: The provider did not waive the beneficiary’s copayment 1 Waived: The provider waived the beneficiary’s copayment 8 Not Applicable: The benefit plan does not have a copay in this circumstance |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX095-0001 |
| 2525 | CRX096 | HEALTH-HOME-ENTITY-NAME | A free-form text field to indicate the health home that authorized payment for the service on the claim. The name entered should be the name that the state uses to uniquely identify the team. A “Health Home Entity” can be a designated provider (e.g., physician, clinic, behavioral health organization), a health team which links to a designated provider, or a health team (physicians, nurses, behavioral health professionals). Because an identification numbering schema has not been established, the entities’ names are being used instead. |
Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX096-0001 | |
| 2526 | CRX096 | HEALTH-HOME-ENTITY-NAME | States should not submit records for an eligible individual where the eligible's health home entity name does not match in the associated claim record, if applicable. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX096-0002 | |||
| 2527 | CRX096 | HEALTH-HOME-ENTITY-NAME | States should not submit records for an eligible individual where the eligible's health home entity name does not match in the associated claim record, if applicable. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX096-0003 | |||
| 2528 | CRX098 | THIRD-PARTY-COINSURANCE-AMOUNT-PAID | The amount of money paid by a third party on behalf of the beneficiary towards coinsurance on the claim or claim line item. |
Optional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX098-0001 | |
| 2529 | CRX099 | THIRD-PARTY-COINSURANCE-DATE-PAID | The date the third party paid the coinsurance amount. |
Conditional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX099-0001 | |
| 2530 | CRX099 | THIRD-PARTY-COINSURANCE-DATE-PAID | The date must be a valid date. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX099-0002 | |||
| 2531 | CRX100 | THIRD-PARTY-COPAYMENT-AMOUNT-PAID | The amount the third party paid the copayment amount. |
Optional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX100-0001 | |
| 2532 | CRX101 | THIRD-PARTY-COPAYMENT-DATE-PAID | The date the third party paid the copayment amount. |
Optional | Date format is CCYYMMDD (National Data Standard). | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX101-0001 | |
| 2533 | CRX101 | THIRD-PARTY-COPAYMENT-DATE-PAID | The date must be a valid date. | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX101-0002 | |||
| 2534 | CRX102 | DISPENSING-PRESCRIPTION-DRUG-PROV-NPI | The National Provider ID (NPI) of the provider responsible for dispensing the prescription drug. | Required | Valid characters include only numbers (0-9) | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX102-0001 | |
| 2535 | CRX102 | DISPENSING-PRESCRIPTION-DRUG-PROV-NPI | The value must be a valid NPI. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 4/30/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX102-0002 | ||
| 2536 | CRX103 | DISPENSING-PRESCRIPTION-DRUG-PROV-TAXONOMY | The Provider Taxonomy of the provider responsible for dispensing the prescription drug. | NA | Value must be in the set of valid values | http://www.wpc-edi.com/reference/ | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX103-0001 |
| 2537 | CRX103 | DISPENSING-PRESCRIPTION-DRUG-PROV-TAXONOMY | Generally, the provider taxonomy requires 10 bytes. However, two additional bytes have been provided for future expansion. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX103-0002 | |||
| 2538 | CRX103 | DISPENSING-PRESCRIPTION-DRUG-PROV-TAXONOMY | Left-fill unused bytes with spaces. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX103-0003 | |||
| 2539 | CRX104 | HEALTH-HOME-PROVIDER-NPI | The National Provider ID (NPI) of the health home provider. | Conditional | Valid characters include only numbers (0-9) | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX104-0001 | |
| 2540 | CRX104 | HEALTH-HOME-PROVIDER-NPI | The value must be a valid NPI. | http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/downloads/npicheckdigit.pdf | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX104-0002 | ||
| 2541 | CRX105 | MEDICARE-BENEFICIARY-IDENTIFIER | The individual’s Medicare Beneficiary Identifier (MBI) Identification Number. Note: MBI replaces the HICN with an entirely new Medicare Beneficiary Identifier (MBI) for purposes of provider billing, if applicable. CMS interfaces with non-payment exchange partners would remain HICN-based, while interfaces with payment partners would use the new MBI. |
NA | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX105-0001 | |
| 2542 | CRX105 | MEDICARE-BENEFICIARY-IDENTIFIER | if individual is NOT enrolled in Medicare, 8-fill field. | 2/25/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX105-0002 | |||
| 2543 | CRX105 | MEDICARE-BENEFICIARY-IDENTIFIER | Field should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files) until such time as the Medicare Beneficiary Identifier is implemented (no target date has been established). | 9/23/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX105-0003 | |||
| 2544 | CRX106 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX106-0001 | |
| 2545 | CRX106 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX106-0002 | |||
| 2546 | CRX156 | DISPENSING-PRESCRIPTION-DRUG-PROV-NUM | The state-specific provider id of the provider who actually dispensed the prescription medication. | Required | Valid formats must be supplied by the state in advance of submitting file data. |
Valid values are supplied by the state. | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX156-0001 |
| 2547 | CRX156 | DISPENSING-PRESCRIPTION-DRUG-PROV-NUM | If value is invalid, record it exactly as it appears in the state system. | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX156-0002 | |||
| 2548 | CRX156 | DISPENSING-PRESCRIPTION-DRUG-PROV-NUM | Note: Once a national provider ID numbering system is in place, the national number should be used. If the state’s legacy ID number is only available, then that number can be entered in this field. | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX156-0003 | |||
| 2549 | CRX160 | MEDICARE-COMB-DED-IND | Code indicating that the amount paid by Medicaid/CHIP on this claim toward the recipient's Medicare deductible was combined with their coinsurance amount because the amounts could not be separated | Conditional | Value must be equal to a valid value. | 0 Amount not combined with coinsurance amount 1 Amount combined with coinsurance amount 9 Unknown |
11/3/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX160-0001 |
| 2550 | CRX160 | MEDICARE-COMB-DED-IND | If claim is not a Crossover claim, or if a type of claim is “3,” “C” or “W” (an encounter claim), set value to “0”. | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX160-0002 | |||
| 2551 | CRX160 | MEDICARE-COMB-DED-IND | Claims records for an eligible individual should not indicate Medicare paid any combined deductible amount on the claim, if the eligible individual is not a dual eligible. | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX160-0003 | |||
| 2552 | CRX161 | PROV-LOCATION-ID | A code to uniquely identify the geographic location where the provider’s services were performed. The value should correspond to an active value in the PROV-LOCATION-ID field in the provider subject area. | Required | Limit characters to alphabet (A-Z), numerals (0-9).. | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX161-0001 | |
| 2553 | CRX161 | PROV-LOCATION-ID | The value should correspond with one of the location identifiers recorded in the provider’s demographic records in the T-MSIS data set | 10/10/2013 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX161-0002 | |||
| 2554 | CRX107 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | CLAIMRX | CLAIM-HEADER-RECORD-RX-CRX00002 | CRX107-0001 | |||
| 2555 | CRX108 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the CLAIM-HEADER-RECORD-IP record segment is CIP00002. | Required | Value must be equal to a valid value. | CRX00003 CLAIM-LINE-RECORD-RX |
4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX108-0001 |
| 2556 | CRX108 | RECORD-ID | Must be populated on every record | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX108-0002 | |||
| 2557 | CRX108 | RECORD-ID | Must be in correct format as shown in definition | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX108-0003 | |||
| 2558 | CRX109 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX109-0001 |
| 2559 | CRX109 | SUBMITTING-STATE | Must be populated on every record. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX109-0002 | |||
| 2560 | CRX109 | SUBMITTING-STATE | Value must be numeric |
4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX109-0003 | |||
| 2561 | CRX109 | SUBMITTING-STATE | SUBMITTING-STATE must be equal across all record segments for a given record. | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX109-0004 | |||
| 2562 | CRX110 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX110-0001 | |
| 2563 | CRX110 | RECORD-NUMBER | Must be numeric | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX110-0002 | |||
| 2564 | CRX110 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX110-0004 | |||
| 2565 | CRX111 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX111-0001 | |
| 2566 | CRX111 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state ID numbers must be supplied to CMS. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX111-0002 | |||
| 2567 | CRX111 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | For SSN states, this field must contain the Eligible's Social Security Number. If the SSN is unknown and a temporary number is assigned, this field will contain that number. |
2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX111-0003 | |
| 2568 | CRX111 | MSIS-IDENTIFICATION-NUM | For TYPE-OF-CLAIM = 4 or D (lump sum adjustments), this field must begin with an ‘&’. | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX111-0004 | |||
| 2569 | CRX112 | ICN-ORIG | A unique number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies an original claim. | Required | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX112-0001 | |
| 2570 | CRX112 | ICN-ORIG | Record the value exactly as it appears in the state system. Do not pad. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX112-0002 | |||
| 2571 | CRX112 | ICN-ORIG | This field should always be populated with the claim identification number assigned to the original paid/denied claim. This identification number should remain constant and be carried forward onto any adjustment claims. The intention is for this earliest claim identification number to be the link that ties the original claim and all adjustment claims together. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX112-0003 | |||
| 2572 | CRX112 | ICN-ORIG | This field should not be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX112-0004 | |||
| 2573 | CRX113 | ICN-ADJ | A unique claim number (up to 21 alpha/numeric characters) assigned by the state’s payment system that identifies the adjustment claim for an original transaction. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX113-0001 | |
| 2574 | CRX113 | ICN-ADJ | Record the value exactly as it appears in the State system. Do not pad | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX113-0002 | |||
| 2575 | CRX113 | ICN-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0 | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX113-0003 | |||
| 2576 | CRX114 | LINE-NUM-ORIG | A unique number to identify the transaction line number that is being reported on the original claim. | Required | Record the value exactly as it appears in the State system. Do not pad. This field should also be completed on adjustment claims to reflect the LINE-NUMBER of the INTERNAL-CONTROL-NUMBER on the claim that is being adjusted. | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX114-0001 | |
| 2577 | CRX115 | LINE-NUM-ADJ | A unique number to identify the transaction line number that identifies the line number on the adjustment ICN. | Conditional | Record the value exactly as it appears in the state system. Do not pad. | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX115-0001 | |
| 2578 | CRX115 | LINE-NUM-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX115-0002 | |||
| 2579 | CRX115 | LINE-NUM-ADJ | This field should be 8-filled if the ADJUSTMENT-INDICATOR = 0. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX115-0003 | |||
| 2580 | CRX116 | LINE-ADJUSTMENT-IND | Code indicating type of adjustment record claim/encounter represents at claim detail level. | Conditional | Value must be equal to a valid value. | 0 Original Claim/Encounter 1 Void of a prior submission 2 Re-submittal 3 Credit Adjustment (negative supplemental) 4 Debit Adjustment (positive supplemental) 5 Credit Gross Adjustment. 6 Debit Gross Adjustment 9 Unknown |
11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX116-0001 |
| 2581 | CRX116 | LINE-ADJUSTMENT-IND | If there is a line adjustment number, then there must be a line-adjustment indicator. | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX116-0002 | |||
| 2582 | CRX116 | LINE-ADJUSTMENT-IND | If there is a line adjustment reason, then there must be a line adjustment indicator. | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX116-0003 | |||
| 2583 | CRX117 | LINE-ADJUSTMENT-REASON-CODE | Claim adjustment reason codes communicate why a service line was paid differently than it was billed. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-adjustment-reason-codes/ | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX117-0001 |
| 2584 | CRX117 | LINE-ADJUSTMENT-REASON-CODE | If there is no adjustment to a line, then there is no adjustment reason code. (Also see: CLAIM-PYMT-REM-CODE) | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX117-0002 | |||
| 2585 | CRX118 | SUBMITTER-ID | The Submitter ID number is the value that identifies the provider/trading partner/clearing house organization to state’s claim adjudication system. | Required | Value must not be null | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX118-0001 | |
| 2586 | CRX119 | CLAIM-LINE-STATUS | The claim line status codes identify the status of a specific detail claim line rather than the entire claim. | Conditional | Value must be equal to a valid value. | http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-codes/ | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX119-0001 |
| 2587 | CRX120 | NATIONAL-DRUG-CODE | A code in National Drug Code (NDC) format indicating the drug, device, or medical supply covered by this claim. | Required | Position 10-11 must be Alpha Numeric or blank | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX120-0001 | |
| 2588 | CRX120 | NATIONAL-DRUG-CODE | Position 1-5 must be Numeric | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX120-0002 | |||
| 2589 | CRX120 | NATIONAL-DRUG-CODE | Position 6-9 must be Alpha Numeric | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX120-0003 | |||
| 2590 | CRX120 | NATIONAL-DRUG-CODE | Drug code formats must be supplied by State in advance of submitting any file data. States must inform CMS of the NDC segments used and their size (e.g., {5, 4, 2} or {5, 4} as defined in the National Drug Code Directory). | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX120-0004 | |||
| 2591 | CRX120 | NATIONAL-DRUG-CODE | If the Drug Code is less than 11 characters in length, the value must be left justified and padded with spaces. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX120-0005 | |||
| 2592 | CRX120 | NATIONAL-DRUG-CODE | If Durable Medical Equipment or supply is prescribed by a physician and provided by a pharmacy then HCPCS or state specific codes can be put in the NDC field. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX120-0006 | |||
| 2593 | CRX120 | NATIONAL-DRUG-CODE | This field is applicable only for TYPE-OF-SERVICE = 035, 036, 077, 062, 063, 064, 065, 066, 067, 068, 069, 073, 074, 075, 076, 077, 078, 079, 080, 081, 082, 083, 084, 033, 034. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX120-0007 | |||
| 2594 | CRX121 | BILLED-AMT | The amount charged at the claim detail level as submitted by the provider. |
Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX121-0001 | |
| 2595 | CRX121 | BILLED-AMT | If TYPE-OF-CLAIM = 3, C, W (encounter record) this field should either be zero-filled or contain the amount paid by the plan to the provider. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX121-0002 | |||
| 2596 | CRX122 | ALLOWED-AMT | The maximum amount displayed at the claim line level as determined by the payer as being "allowable" under the provisions of the contract prior to the determination of actual payment. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX122-0001 | |
| 2597 | CRX123 | COPAY-AMT | The copayment amount paid by an enrollee for the service, which does not include the amount paid by the insurance company. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX123-0001 | |
| 2598 | CRX124 | TPL-AMT | Third Party Liability (TPL) refers to the legal obligation of third parties, i.e., certain individuals, entities, or programs, to pay all or part of the expenditures for medical assistance furnished under a state plan. This is the total amount denoted at the claim header level paid by the third party. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX124-0001 | |
| 2599 | CRX125 | MEDICAID-PAID-AMT | The amount paid by Medicaid on this claim or adjustment at the claim detail level. | Required | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX125-0001 | |
| 2600 | CRX125 | MEDICAID-PAID-AMT | For claims where Medicaid payment is only available at the header level, report the entire payment amount on the MSIS record corresponding to the line item with the highest charge. Zero fill Medicaid Amount Paid on all other MSIS records created from the original claim. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX125-0002 | |||
| 2601 | CRX125 | MEDICAID-PAID-AMT | For Crossover claims with Medicare Coinsurance and/or Deductibles, enter the sum of those amounts in the Medicaid-Amount-Paid field, if the providers were reimbursed by Medicaid for them. If the Coinsurance and Deductibles were not paid by the state, then report the Medicaid-Amount-Paid as $0. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX125-0003 | |||
| 2602 | CRX126 | MEDICAID-FFS-EQUIVALENT-AMT | The MEDICAID-FFS-EQUIVALENT-AMT field should be populated with the amt that would have been paid had the services been provided on a FFS basis. | Conditional | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX126-0001 | |
| 2603 | CRX126 | MEDICAID-FFS-EQUIVALENT-AMT | Required when TYPE-OF-CLAIM = C, 3, or W | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX126-0002 | |||
| 2604 | CRX127 | MEDICARE-DEDUCTIBLE-AMT | The amount paid by Medicaid/CHIP on this claim at the claim line level toward the beneficiary’s Medicare deductible. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX127-0001 | |
| 2605 | CRX127 | MEDICARE-DEDUCTIBLE-AMT | If claim is not a Crossover claim, or if a TYPE-OF-CLAIM = 3, C, W (encounter claim), 8-fill. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX127-0002 | |||
| 2606 | CRX127 | MEDICARE-DEDUCTIBLE-AMT | If the Medicare deductible amount can be identified separately from Medicare coinsurance payments, code that amount in this field. If the Medicare coinsurance and deductible payments cannot be separated, fill this field with the combined payment amount and code space in MEDICARE-COINSURANCE-PAYMENT. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX127-0003 | |||
| 2607 | CRX127 | MEDICARE-DEDUCTIBLE-AMT | Claims records for an eligible individual should not indicate Medicare paid any deductible amount on the claim, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX127-0004 | |||
| 2608 | CRX128 | MEDICARE-COINS-AMT | The amount paid by Medicaid/CHIP on this claim toward the recipient's Medicare coinsurance at the claim detail level. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX128-0001 | |
| 2609 | CRX128 | MEDICARE-COINS-AMT | If the Medicare coinsurance amount can be identified separately from Medicare deductible payments, code that amount in this field. If Medicare coinsurance and deductible payments cannot be separated, fill this field with 99998 and code the combined payment amount in MEDICARE-DEDUCTIBLE-AMT. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX128-0002 | |||
| 2610 | CRX129 | MEDICARE-PAID-AMT | The amount paid by Medicare on this claim or adjustment. | Required | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX129-0001 | |
| 2611 | CRX129 | MEDICARE-PAID-AMT | If the service was covered by Medicare but Medicare had no liability for the bill, zero-fill. MEDICARE-PAID-AMT should reflect the actual amount paid by Medicare. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX129-0002 | |||
| 2612 | CRX129 | MEDICARE-PAID-AMT | For claims where Medicare payment is only available at the header level, report the entire payment amount the T-MSIS record corresponding to the line item with the highest charge. Zero fill Medicare Amount Paid on all other T-MSIS records created from the original claim. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX129-0003 | |||
| 2613 | CRX129 | MEDICARE-PAID-AMT | Claims records for an eligible individual should not indicate Medicare paid any amount on the claim, if the eligible individual is not a dual eligible. | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX129-0004 | |||
| 2614 | CRX131 | OT-RX-CLAIM-QUANTITY-ALLOWED | The maximum allowable quantity of a drug or service that may be dispensed per prescription per date of service or per month. Quantity limits are applied to medications when the majority of appropriate clinical utilizations will be addressed within the quantity allowed. | Conditional | Must be numeric | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX131-0001 | |
| 2615 | CRX131 | OT-RX-CLAIM-QUANTITY-ALLOWED | This field is only applicable when the service being billed can be quantified in discrete units, e.g., a number of visits or the number of units of a prescription/refill that were filled. For prescriptions/refills, use the Medicaid Drug Rebate definition of a unit, which is the smallest unit by which the drug is normally measured; e.g. tablet, capsule, milliliter, etc. For drugs not identifiable or dispensed by a normal unit, e.g. powder filled vials, use 1 as the number of units. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX131-0002 | |||
| 2616 | CRX131 | OT-RX-CLAIM-QUANTITY-ALLOWED | NOTE: One prescription for 100 250 milligram tablets results in OT-RX-CLAIM-QUANTITY-ALLOWED =100. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX131-0003 | |||
| 2617 | CRX131 | OT-RX-CLAIM-QUANTITY-ALLOWED | The value in OT-RX-CLAIM-QUANTITY-ALLOWED must correspond with the value in UNIT-OF-MEASURE. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX131-0004 | |||
| 2618 | CRX131 | OT-RX-CLAIM-QUANTITY-ALLOWED | Left-fill field with zeros if value is less than 9 bytes long. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX131-0005 | |||
| 2619 | CRX131 | OT-RX-CLAIM-QUANTITY-ALLOWED | For use with CLAIMOT and CLAIMRX claims. For CLAIMIP and CLAIMLT claims/encounter records, use the IP-LT-QUANTITY-OF-SERVICE field. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX131-0006 | |||
| 2620 | CRX132 | OT-RX-CLAIM-QUANTITY-ACTUAL | The quantity of a drug, service, or product that is rendered/dispensed for a prescription, specific date of service, or billing time span. |
Required | Must be numeric | 9/23/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX132-0001 | |
| 2621 | CRX132 | OT-RX-CLAIM-QUANTITY-ACTUAL | This field is only applicable when the service being billed can be quantified in discrete units, e.g., a number of visits or the number of units of a prescription/refill that were filled. For prescriptions/refills, use the Medicaid Drug Rebate definition of a unit, which is the smallest unit by which the drug is normally measured; e.g. tablet, capsule, milliliter, etc. For drugs not identifiable or dispensed by a normal unit, e.g. powder filled vials, use 1 as the number of units. |
2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX132-0002 | |||
| 2622 | CRX132 | OT-RX-CLAIM-QUANTITY-ACTUAL | NOTE: One prescription for 100 250 milligram tablets results in QUANTITY OF SERVICE=100. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX132-0003 | |||
| 2623 | CRX132 | OT-RX-CLAIM-QUANTITY-ACTUAL | The value in OT-RX-CLAIM-QUANTITY-ACTUAL must correspond with the value in UNIT-OF-MEASURE. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX132-0004 | |||
| 2624 | CRX132 | OT-RX-CLAIM-QUANTITY-ACTUAL | Left-fill field with zeros if value is less than 9 bytes long. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX132-0005 | |||
| 2625 | CRX132 | OT-RX-CLAIM-QUANTITY-ACTUAL | For use with CLAIMOT and CLAIMRX claims. For CLAIMIP and CLAIMLT claims/encounter records, use the IP-LT-QUANTITY-OF-SERVICE field. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX132-0006 | |||
| 2626 | CRX133 | UNIT-OF-MEASURE | A code to indicate the basis by which the quantity of the drug or supply is expressed. |
Conditional | Value must be equal to a valid value. | F2 International Unit ML Milliliter GR Gram UN Unit |
11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX133-0001 |
| 2627 | CRX133 | UNIT-OF-MEASURE | Enter the unit of measure for each corresponding quantity value. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX133-0002 | |||
| 2628 | CRX134 | TYPE-OF-SERVICE | A code to categorize the services provided to a Medicaid or CHIP enrollee. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX134-0001 |
| 2629 | CRX134 | TYPE-OF-SERVICE | Pharmacy Claims/Encounters File - Claims/encounters with TYPE-OF-SERVICE= 011, 018, 033, 034, 036, 085, 089, 127, or 131. | 9/23/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX134-0002 | |||
| 2630 | CRX134 | TYPE-OF-SERVICE | Experience has demonstrated there can be instances when more than one service area category could be applicable for a provided service. The following hierarchy rules apply to these instances: o The specific service categories of sterilizations and other pregnancy-related procedures take precedence over provider categories, such as inpatient hospital or outpatient hospital. o Services of a physician employed by a clinic are reported under clinic services if the clinic is the billing entity. X-rays processed by the clinic in the course of treatment, however, are reported under X-ray services. o Services of a registered nurse attending a resident in a NF are reported (if they qualified under the coverage rules) under home health services if they were not billed as part of the NF bill. |
2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX134-0003 | |||
| 2631 | CRX134 | TYPE-OF-SERVICE | See Appendix D for information on the various types of service. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX134-0004 | |||
| 2632 | CRX134 | TYPE-OF-SERVICE | All claims for inpatient psychiatric care provided in a separately administered psychiatric wing or psychiatric hospital are included in the CLAIMLT file. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX134-0005 | |||
| 2633 | CRX135 | HCBS-SERVICE-CODE | Codes indicating that the service represents a long-term care home and community based service or support for an individual with chronic medical and/or mental conditions. The codes are to help clearly delineate between acute care and long-term care provided in the home and community setting (e.g. 1915(c), 1915(i), 1915(j), and 1915(k) services). | Conditional | Value must be equal to a valid value. | 1 The HCBS service was provided under 1915(i) 2 The HCBS service was provided under 1915(j) 3 The HCBS service was provided under 1915(k) 4 The HCBS service was provided under a 1915(c) HCBS Waiver 5 The HCBS service was provided under an 1115 waiver 6 The HCBS service was not provided under the statutes identified above and was of an acute care nature 7 The HCBS service was not provided under the statutes identified above and was of a long term care nature 8 The service is not an HCBS service (i.e. the HCBS classification is not applicable) 9 Unknown |
11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX135-0001 |
| 2634 | CRX136 | HCBS-TAXONOMY | A code that classifies home and community based services listed on the claim into the HCBS taxonomy. |
Conditional | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX136-0001 |
| 2635 | CRX136 | HCBS-TAXONOMY | If HCBS-SERVICE-CODE = 1 through 8, then populate HCBS-TAXONOMY with one of the values from the list in Appendix B. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX136-0002 | |||
| 2636 | CRX136 | HCBS-TAXONOMY | If HCBS-SERVICE-CODE = 9 (It is unknown what authority the HCBS service was provided), then populate HCBS-TAXONOMY based on the assumption that the services is not a 1915(j), 1915(k), 1915(c) waiver, or 1115 waiver service. (See “If HCBS-SERVICE-CODE = 1 through 8” above.) | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX136-0003 | |||
| 2637 | CRX137 | OTHER-TPL-COLLECTION | This data element indicates that the claim is for a beneficiary for whom other third party resource development and collection activities are in progress, when the liability is not another health insurance plan for which the eligible is a beneficiary. | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 Third Party Resource is Casualty/Tort 002 Third Party Resource is Estate 003 Third Party Resource is Lien (TEFRA) 004 Third Party Resource is Lien (Other) 005 Third Party Resource is Worker’s Compensation 006 Third Party Resource is Medical Malpractice 007 Third Party Resource is Other 999 Classification of Third Party Resource is Unknown |
11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX137-0001 |
| 2638 | CRX138 | DAYS-SUPPLY | Number of days supply dispensed. | Required | Values should be between -365 and 365. | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX138-0001 | |
| 2639 | CRX138 | DAYS-SUPPLY | For Prescription Drugs, value should be between -365 and 365. | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX138-0002 | |||
| 2640 | CRX139 | NEW-REFILL-IND | Indicator showing whether the prescription being filled was a new prescription or a refill. If it is a refill, the indicator will indicate the number of refills. | Required | Value must be equal to a valid value. | 00 New Prescription 01-98 Number of Refill(s) 99 Unknown |
4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX139-0001 |
| 2641 | CRX140 | BRAND-GENERIC-IND | Indicates whether the drug is a brand name, generic, single-source, or multi-source drug. | Required | Value must be in the set of valid values | 0 Non-Drug 1 Generic 2 Brand 3 Multi-Source 4 Single-Source |
4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX140-0001 |
| 2642 | CRX141 | DISPENSE-FEE | The charge to cover the cost of dispensing the prescription. Dispensing costs include overhead, supplies, and labor, etc. to fill the prescription. | Required | This data element must include a valid dollar amount. | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX141-0001 | |
| 2643 | CRX142 | PRESCRIPTION-NUM | The unique identification number assigned by the pharmacy or supplier to the prescription | Required | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX142-0001 | |
| 2644 | CRX143 | DRUG-UTILIZATION-CODE | A code indicating the conflict, intervention and outcome of a prescription presented for fulfillment. The T-MSIS DRUG-UTILIZATION-CODE data element is composite field comprised of three distinct NCPDP data elements: "Reason for Service Code" (439-E4); "Professional Service Code" (44Ø-E5); and "Result of Service Code" (441-E6). All 3 of these NCPDP fields are situationally required and independent of one another. Pharmacists may report none, one, two or all three. NCPDP situational rules call for one or more of these values in situations where the field(s) could result in different coverage, pricing, patient financial responsibility, drug utilization review outcome, or if the information affects payment for, or documentation of, professional pharmacy service. The NCPDP "Results of Service Code" (bytes 1 & 2 of the T-MSIS DRUG-UTILIZATION-CODE) explains whether the pharmacist filled the prescription, filled part of the prescription, etc. The NCPDP "Professional Service Code" (bytes 3 & 4 of the T-MSIS DRUG-UTILIZATION-CODE) describes what the pharmacist did for the patient. The NCPDP "Result of Service Code" (bytes 5 & 6 of the T-MSIS DRUG-UTILIZATION-CODE) describes the action the pharmacist took in response to a conflict or the result of a pharmacist’s professional service. Because the T-MSIS DRUG-UTILIZATION-CODE data element is a composite field, it is necessary for the state to populate all six bytes if any of the three NCPDP fields has a value. In such situations, use 'spaces' as placeholders for not applicable codes. |
Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX143-0001 |
| 2645 | CRX144 | DTL-METRIC-DEC-QTY | Metric decimal quantity of the product with the appropriate unit of measure (each, gram, or milliliter). | Required | Must be numeric | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX144-0001 | |
| 2646 | CRX145 | COMPOUND-DOSAGE-FORM | The physical form of a dose of medication, such as a capsule or injection. | Conditional | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX145-0001 |
| 2647 | CRX146 | REBATE-ELIGIBLE-INDICATOR | An indicator to identify claim lines with an NDC that is eligible for the drug rebate program. | Conditional | Value must be equal to a valid value. | 0 NDC is not eligible for drug rebate program. (Manufacturer does not have a rebate agreement.) 1 NDC is eligible for drug rebate program 2 NDC is exempt from the drug rebate program (biological and medical devices) 9 The drug rebate eligibility of the is unknown |
11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX146-0001 |
| 2648 | CRX147 | IMMUNIZATION-TYPE | This field identifies the type of immunization provided in order to track additional detail not currently contained in CPT codes. | Conditional | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX147-0001 |
| 2649 | CRX148 | BENEFIT-TYPE | The benefit category corresponding to the service reported on the claim or encounter record. Note: The code definitions in the valid value list originate from the Medicaid and CHIP Program Data System’s (MACPro’s) benefit type list. See Appendix H: Benefit Types for descriptions of the categories. |
Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 2/25/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX148-0001 |
| 2650 | CRX149 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | This code indicates if the claim was matched with Title XIX or Title XXI. |
Required | Value must be equal to a valid value. | 01 Federal funding under Title XIX 02 Federal funding under Title XXI 03 Federal funding under ACA 04 Federal funding under other legislation |
4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX149-0001 |
| 2651 | CRX149 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | If an individual is not eligible for S-CHIP, then any associated claims records should not have reimbursed with federal funding under Title XXI. | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX149-0002 | |||
| 2652 | CRX149 | CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT | If an individual is not eligible for Medicaid, then any associated claims records should not have reimbursed with federal funding under Title XIX. | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX149-0003 | |||
| 2653 | CRX150 | XIX-MBESCBES-CATEGORY-OF-SERVICE | A code indicating the category of service for the paid claim. The category of service is the line item from the CMS-64 form that states use to report their expenditures and request federal financial participation |
Conditional | Value must be equal to a valid value. | See Appendix I for listing of valid values. | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX150-0001 |
| 2654 | CRX150 | XIX-MBESCBES-CATEGORY-OF-SERVICE | Males cannot receive services where the category of service is "Other Pregnancy-related Procedures", "Nurse Mid-wife", "Freestanding Birth Center" or "Tobacco Cessation for Pregnant Women". | 4/30/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX150-0002 | |||
| 2655 | CRX151 | XXI-MBESCBES-CATEGORY-OF-SERVICE | A code indicating the category of service for the paid claim. The category of service is the line item from the CMS-21 form that states use to report their expenditures and request federal financial participation. Refer to Attachment 8 for definitions on the various categories of service. | Conditional | Value must be equal to a valid value. | See Appendix J for listing of valid values. | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX151-0001 |
| 2656 | CRX152 | OTHER-INSURANCE-AMT | The amount paid by insurance other than Medicare or Medicaid on this claim. | Conditional | This data element must include a valid dollar amount. | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX152-0001 | |
| 2657 | CRX153 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX153-0001 | |
| 2658 | CRX153 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX153-0002 | |||
| 2659 | CRX157 | ADJUDICATION-DATE | The date on which the payment status of the claim was finally adjudicated by the state. |
Required | Date format is CCYYMMDD (National Data Standard). | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX157-0001 | |
| 2660 | CRX157 | ADJUDICATION-DATE | Value must be a valid date | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX157-0002 | |||
| 2661 | CRX157 | ADJUDICATION-DATE | For Encounter Records (TYPE-OF-CLAIM=3, C, W); use date the encounter was processed by the state. | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX157-0003 | |||
| 2662 | CRX157 | ADJUDICATION-DATE | For Adjustment Records (ADJUSTMENT-INDICATOR<> 0), use date of final adjudication when possible. | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX157-0004 | |||
| 2663 | CRX157 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or before END-OF-TIME-PERIOD included in the T-MSIS HEADER RECORD | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX157-0005 | |||
| 2664 | CRX157 | ADJUDICATION-DATE | ADJUDICATION-DATE must occur on or after the ADMISSION-DATE | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX157-0006 | |||
| 2665 | CRX157 | ADJUDICATION-DATE | This date must occur on or after the DATE-OF-BIRTH in the Eligible Record when the eligible is not a CHIP unborn child. | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX157-0007 | |||
| 2666 | CRX157 | ADJUDICATION-DATE | A Medicaid or CHIP eligible individual should not have had a claim adjudicated before their five-year immigration ineligible status has expired, except when the eligible is an unborn child in the CHIP program. | 10/10/2013 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX157-0008 | |||
| 2667 | CRX158 | SELF-DIRECTION-TYPE | This data element is not applicable to this file type. | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 Hiring Authority 002 Budget Authority 003 Hiring and Budget Authority 999 Type of Authority Is Unknown |
11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX158-0001 |
| 2668 | CRX159 | PRE-AUTHORIZATION-NUM | A number, code, or other value that indicates the services provided on this claim have been authorized by the payee or other service organization, or that a referral for services has been approved. (Also called Prior Authorization or Referral Number) | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX159-0001 | |
| 2669 | CRX154 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | CLAIMRX | CLAIM-LINE-RECORD-RX-CRX00003 | CRX154-0001 | |||
| 2670 | ELG001 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG001-0001 | |
| 2671 | ELG001 | RECORD-ID | Value must be in the required format | 4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG001-0002 | |||
| 2672 | ELG001 | RECORD-ID | Value must be in the set of valid values | ELG00001 - FILE-HEADER-RECORD-ELIGIBILITY | 10/10/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG001-0003 | ||
| 2673 | ELG001 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG001-0004 | |||
| 2674 | ELG002 | DATA-DICTIONARY-VERSION | A data element to capture the version of the T-MSIS data dictionary that was used to build the file. | Required | Use the version number specified on the title page of the data dictionary | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG002-0001 | |
| 2675 | ELG003 | SUBMISSION-TRANSACTION-TYPE | A data element to identify the whether the transactions in the file are original submissions of the data, a resubmission of a previously submitted file, or corrections of edit rejects. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG003-0001 |
| 2676 | ELG004 | FILE-ENCODING-SPECIFICATION | A data element to denote whether the file is in fixed length line format or delimited format. | Required | Value must be equal to a valid value. | FLF The file follows a fixed length format. PSV The file follows a pipe-delimited format. |
4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG004-0001 |
| 2677 | ELG005 | DATA-MAPPING-DOCUMENT-VERSION | A data element to identify the version of the T-MSIS data mapping document used to build the file. | Required | Use the version number specified on the title page of the data mapping document | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG005-0001 | |
| 2678 | ELG006 | FILE-NAME | The name identifying the subject area to which the records in its file relate. Each T-MSIS submission file should only contain records for one subject area (i.e., Eligible, Third-party Liability, Provider, Managed Care Plan Information, IP claims, LT claims, Rx claims, or OT claims). | Required | Required on every file header | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG006-0001 | |
| 2679 | ELG006 | FILE-NAME | Value must be equal to a valid value. | ELIGIBLE - Eligible file | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG006-0002 | ||
| 2680 | ELG006 | FILE-NAME | The file name must exist in the File Label Internal Dataset Name. | 10/10/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG006-0003 | |||
| 2681 | ELG007 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG007-0001 | |
| 2682 | ELG007 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG007-0002 | ||
| 2683 | ELG007 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG007-0003 | |||
| 2684 | ELG008 | DATE-FILE-CREATED | The date on which the file was created. | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG008-0001 | |
| 2685 | ELG008 | DATE-FILE-CREATED | The date must be a valid date | 4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG008-0002 | |||
| 2686 | ELG008 | DATE-FILE-CREATED | Date must be equal to or later than the date entered in the END-OF-TIME-PERIOD field. | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG008-0003 | |||
| 2687 | ELG008 | DATE-FILE-CREATED | Required on every file header | 4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG008-0004 | |||
| 2688 | ELG008 | DATE-FILE-CREATED | Date must be equal or less than current date | 4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG008-0005 | |||
| 2689 | ELG009 | START-OF-TIME-PERIOD | Beginning day of the month covered by this file. | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG009-0001 | |
| 2690 | ELG009 | START-OF-TIME-PERIOD | Value in DD must equal 01. | 4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG009-0002 | |||
| 2691 | ELG009 | START-OF-TIME-PERIOD | Date must be less than END-OF-TIME-PERIOD | 10/10/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG009-0003 | |||
| 2692 | ELG009 | START-OF-TIME-PERIOD | Value must occur on or before the date the file was created. | 10/10/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG009-0004 | |||
| 2693 | ELG009 | START-OF-TIME-PERIOD | Value must be equal or less than current date. | 10/10/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG009-0005 | |||
| 2694 | ELG010 | END-OF-TIME-PERIOD | Last date of the reporting period covered by the file to which this Header Record is attached. | Required | Value must be a valid date | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG010-0001 | |
| 2695 | ELG010 | END-OF-TIME-PERIOD | Date format is CCYYMMDD (National Data Standard) | 4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG010-0002 | |||
| 2696 | ELG010 | END-OF-TIME-PERIOD | Value for the Date in the End of Time Period (last 2 bytes of the value) must equal "30" in April, June, September, or November; "31" in January, March, May, July, August, October, or December, and "28" or "29" in February. | 10/10/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG010-0003 | |||
| 2697 | ELG010 | END-OF-TIME-PERIOD | Value must be equal or less than DATE-FILE-CREATED. | 4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG010-0004 | |||
| 2698 | ELG010 | END-OF-TIME-PERIOD | Value must be greater than START-OF-TIME-PERIOD | 4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG010-0005 | |||
| 2699 | ELG010 | END-OF-TIME-PERIOD | Value must be equal or less than current date. | 10/10/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG010-0006 | |||
| 2700 | ELG011 | FILE-STATUS-INDICATOR | A code to indicate whether the records in the file are test or production records. | Required | Value must be equal to a valid value. | P Production file T Test file |
2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG011-0001 |
| 2701 | ELG011 | FILE-STATUS-INDICATOR | The dataset name and the value in this field must be consistent (i.e., the production dataset name cannot have a FILE-STATUS-INDICATOR = 'T' | 4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG011-0002 | |||
| 2702 | ELG012 | SSN-INDICATOR | Indicates whether the state uses the eligible person's social security number (SSN) instead of an MSIS identification number as the unique, unchanging eligible person identifier. | Required | Non-SSN States will assign each eligible only one permanent MSIS-ID in his or her lifetime. When reporting eligibility records it is important that the SSN-INDICATOR in the Header record be set to 0 and the MSIS-ID for each record be provided in the MSIS-IDENTIFICATION-NUMBER field; if the MSIS-IDENTIFICATION-NUMBER is not known then this field should be filled with nines. The MSIS-ID identifies the individual and any claims submitted to the system | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG012-0001 | |
| 2703 | ELG012 | SSN-INDICATOR | Provide the SSN in the SOCIAL-SECURITY-NUMBER field; if the SSN is not available the SOCIAL-SECURITY-NUMBER field should be filled with nines. Set the SSN-INDICATOR in the header record to 0. This setting indicates the manner in which the state assigns IDs for the validation program | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG012-0002 | |||
| 2704 | ELG012 | SSN-INDICATOR | SSN States will use the SOCIAL-SECURITY-NUMBER field to provide the MSIS-ID when a permanent SSN is available for the individual. For these states the SSN-Indicator in the header record will be set to 1 and the MSIS-IDENTIFICATION-NUMBER in the eligible record should be blank. | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG012-0003 | |||
| 2705 | ELG012 | SSN-INDICATOR | States that are non SSN states must not submit MSIS Identification Numbers and SSNs that match for eligible individuals. | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG012-0004 | |||
| 2706 | ELG012 | SSN-INDICATOR | Value must be equal to a valid value. | 0 State does not use SSN as MSIS-IDENTIFICATION-NUMBER 1 State uses SSN as MSIS-IDENTIFICATION-NUMBER |
2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG012-0005 | ||
| 2707 | ELG012 | SSN-INDICATOR | States that are SSN states must submit MSIS Identification Numbers and SSNs that match for eligible individuals. | 10/10/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG012-0006 | |||
| 2708 | ELG013 | TOT-REC-CNT | A count of all records in the file except for the file header record. This count will be used as a control total to help assure that the file did not become corrupted during transmission. | Required | An integer value with no commas. | 4/30/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG013-0001 | |
| 2709 | ELG013 | TOT-REC-CNT | Value must equal the count of all records excluding the header record | 10/10/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG013-0002 | |||
| 2710 | ELG013 | TOT-REC-CNT | The total number of records a state submits in the Eligible file should not increase or decrease more than 10% from one month to another. | 2/25/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG013-0003 | |||
| 2711 | ELG247 | SEQUENCE-NUMBER | To enable state’s to sequentially number files, when related, follow-on files are necessary (i.e., update files, replacement files). This should begin with 1 for the original Create submission type and be incremented by one for each Replacement or Update submission for the same reporting period and file type (subject area). | Required | Field is required on all 'C', 'U', and 'R' record files. | 10/10/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG247-0001 | |
| 2712 | ELG247 | SEQUENCE-NUMBER | Must be numeric and > 0 | 10/10/2013 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG247-0002 | |||
| 2713 | ELG014 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG014-0001 | |
| 2714 | ELG014 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG014-0002 | |||
| 2715 | ELG015 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 | ELG015-0001 | |||
| 2716 | ELG016 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG016-0001 | |
| 2717 | ELG016 | RECORD-ID | Value must be in the required format | 4/30/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG016-0002 | |||
| 2718 | ELG016 | RECORD-ID | Value must be equal to a valid value. | ELG00002 - PRIMARY-DEMOGRAPHICS-ELIGIBILITY | 10/10/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG016-0003 | ||
| 2719 | ELG016 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG016-0004 | |||
| 2720 | ELG017 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG017-0001 | |
| 2721 | ELG017 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG017-0002 | ||
| 2722 | ELG017 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG017-0003 | |||
| 2723 | ELG018 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG018-0001 | |
| 2724 | ELG018 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG018-0002 | |||
| 2725 | ELG018 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG018-0005 | |||
| 2726 | ELG019 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG019-0001 | |
| 2727 | ELG019 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG019-0002 | |||
| 2728 | ELG019 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG019-0003 | |||
| 2729 | ELG019 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG019-0004 | |||
| 2730 | ELG019 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG019-0005 | |||
| 2731 | ELG020 | ELIGIBLE-FIRST-NAME | The first name of the individual to whom the services were provided. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG020-0001 | |
| 2732 | ELG021 | ELIGIBLE-LAST-NAME | The last name of the individual to whom the services were provided. | Required | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG021-0001 | |
| 2733 | ELG022 | ELIGIBLE-MIDDLE-INIT | The middle initial of the individual to whom the services were provided. | Conditional | Leave blank if not available | 11/3/2015 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG022-0001 | |
| 2734 | ELG022 | ELIGIBLE-MIDDLE-INIT | Value must be an alphabetic character, or a blank (A-Z, a-z, ) | 4/30/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG022-0002 | |||
| 2735 | ELG023 | SEX | The individual’s biological sex. | Required | Value must be equal to a valid value. | F Female M Male U Unknown |
4/30/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG023-0001 |
| 2736 | ELG023 | SEX | If an eligible individual is a male, he cannot be pregnant. | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG023-0002 | |||
| 2737 | ELG024 | DATE-OF-BIRTH | Individual’s date of birth. | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG024-0001 | |
| 2738 | ELG024 | DATE-OF-BIRTH | Children enrolled in the Separate CHIP prenatal program option must not have a date of birth | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG024-0002 | |||
| 2739 | ELG024 | DATE-OF-BIRTH | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG024-0003 | |||
| 2740 | ELG024 | DATE-OF-BIRTH | The date must be a valid date, unless a complete valid date is not available. | 4/30/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG024-0004 | |||
| 2741 | ELG024 | DATE-OF-BIRTH | An eligible individual's date of birth must not be after his/her date of death. | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG024-0005 | |||
| 2742 | ELG024 | DATE-OF-BIRTH | An eligible individual's date of birth must be on or before the end of time period for the submission. Revise Edit Definition: DATE-OF-BIRTH must be <= END-OF-TIME-PERIOD |
2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG024-0006 | |||
| 2743 | ELG024 | DATE-OF-BIRTH | An eligible individual's date of birth must be on or before the date the file was created. | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG024-0007 | |||
| 2744 | ELG025 | DATE-OF-DEATH | Individual's date of death. | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG025-0001 | |
| 2745 | ELG025 | DATE-OF-DEATH | If individual is not deceased, 8-fill. | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG025-0002 | |||
| 2746 | ELG025 | DATE-OF-DEATH | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG025-0003 | |||
| 2747 | ELG025 | DATE-OF-DEATH | The date must be a valid date, unless a complete valid date is not available or the eligible individual is not deceased. | 4/30/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG025-0004 | |||
| 2748 | ELG025 | DATE-OF-DEATH | The eligible individual's date of death cannot occur earlier than his/her date of birth. | 4/30/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG025-0005 | |||
| 2749 | ELG025 | DATE-OF-DEATH | The eligible individual's date of death indicate that an eligible individual was greater than 125 years old at the time of death. | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG025-0006 | |||
| 2750 | ELG025 | DATE-OF-DEATH | Value cannot be > DATE-FILE-CREATED in Header Record | 4/30/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG025-0007 | |||
| 2751 | ELG025 | DATE-OF-DEATH | For records for an eligible individual across time periods, the eligible individual's Date of Death should not vary. | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG025-0008 | |||
| 2752 | ELG026 | PRIMARY-DEMOGRAPHIC-ELEMENT-EFF-DATE | The first day of the time span during which the values in all data elements in the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created.) This date field is necessary when defining a unique row in a database table. |
Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG026-0001 | |
| 2753 | ELG026 | PRIMARY-DEMOGRAPHIC-ELEMENT-EFF-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG026-0002 | |||
| 2754 | ELG026 | PRIMARY-DEMOGRAPHIC-ELEMENT-EFF-DATE | Whenever the value in one or more of the data elements in the PRIMARY DEMOGRAPHICS– ELIGIBILITY record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG026-0003 | |||
| 2755 | ELG026 | PRIMARY-DEMOGRAPHIC-ELEMENT-EFF-DATE | The effective date of the PRIMARY-DEMOGRAPHICS-ELIGIBILITY record segment must occur on or before the end date for the record segment. | 10/10/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG026-0004 | |||
| 2756 | ELG026 | PRIMARY-DEMOGRAPHIC-ELEMENT-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG026-0005 | |||
| 2757 | ELG027 | PRIMARY-DEMOGRAPHIC-ELEMENT-END-DATE | The last day of the time span during which the values in all data elements in the PRIMARY DEMOGRAPHICS– ELIGIBILITY record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created.) | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG027-0001 | |
| 2758 | ELG027 | PRIMARY-DEMOGRAPHIC-ELEMENT-END-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG027-0002 | |||
| 2759 | ELG027 | PRIMARY-DEMOGRAPHIC-ELEMENT-END-DATE | If there is no end date (i.e., the record is good into the indefinite future) use the “end-of-time” date (99991231) | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG027-0003 | |||
| 2760 | ELG027 | PRIMARY-DEMOGRAPHIC-ELEMENT-END-DATE | Whenever the value in one or more of the data elements in the PRIMARY DEMOGRAPHICS– ELIGIBILITY record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG027-0004 | |||
| 2761 | ELG027 | PRIMARY-DEMOGRAPHIC-ELEMENT-END-DATE | The end date of the PRIMARY-DEMOGRAPHICS-ELIGIBILITY record segment must occur on or after the effective date for the record segment. | 10/10/2013 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG027-0005 | |||
| 2762 | ELG028 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG028-0001 | |
| 2763 | ELG028 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG028-0002 | |||
| 2764 | ELG029 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 | ELG029-0001 | |||
| 2765 | ELG030 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG030-0001 | |
| 2766 | ELG030 | RECORD-ID | Value must be in the required format | 4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG030-0002 | |||
| 2767 | ELG030 | RECORD-ID | Value must be equal to a valid value. | ELG00003 - VARIABLE-DEMOGRAPHICS-ELIGIBILITY | 4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG030-0003 | ||
| 2768 | ELG030 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG030-0004 | |||
| 2769 | ELG031 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG031-0001 | |
| 2770 | ELG031 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG031-0002 | ||
| 2771 | ELG031 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG031-0003 | |||
| 2772 | ELG032 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG032-0001 | |
| 2773 | ELG032 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG032-0002 | |||
| 2774 | ELG032 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG032-0003 | |||
| 2775 | ELG033 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG033-0001 | |
| 2776 | ELG033 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG033-0002 | |||
| 2777 | ELG033 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG033-0003 | |||
| 2778 | ELG033 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG033-0004 | |||
| 2779 | ELG033 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG033-0005 | |||
| 2780 | ELG034 | MARITAL-STATUS | A code to classify eligible individual’s marital/domestic-relationship status. | Required | This element should be reported by the state when the information is material to eligibility (i.e., institutionalization). | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG034-0001 | |
| 2781 | ELG034 | MARITAL-STATUS | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG034-0002 | ||
| 2782 | ELG034 | MARITAL-STATUS | An eligible individual who is younger than 12 years must have a marital status of never married or unknown. | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG034-0003 | |||
| 2783 | ELG035 | MARITAL-STATUS-OTHER-EXPLANATION | A free-text field to capture the description of the marital/domestic-relationship status when MARITAL-STATUS=14 (Other) is selected. | Conditional | Conditional (required when value “14 (Other) appears in MARITAL-STATUS | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG035-0001 | |
| 2784 | ELG035 | MARITAL-STATUS-OTHER-EXPLANATION | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), apostrophes (‘). | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG035-0002 | |||
| 2785 | ELG036 | SSN | The eligible individual's social security number. | Required | For SSN States, value for MSIS Identification Number must = individual's valid Social Security Number and SSN-INDICATOR = 1. | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG036-0001 | |
| 2786 | ELG036 | SSN | Required | If known, this field is to be populated with numeric digits. | 4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG036-0002 | ||
| 2787 | ELG036 | SSN | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligible File so that T-MSIS can associated the temporary MSIS identification number and the social security number. | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG036-0003 | |||
| 2788 | ELG036 | SSN | For NON-SSN States, all states must provide available SSNs on the ELIGIBLE FILE, regardless of the use of this field as the unique MSIS identifier. |
2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG036-0004 | |||
| 2789 | ELG036 | SSN | For records for an eligible individual across time periods in an SSN state, the eligible individual's SSN should not vary. | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG036-0005 | |||
| 2790 | ELG036 | SSN | If the SSN is not available and a temporary identification number has been assigned in the MSIS-IDENTIFICATION-NUMBER field, the SSN field must blank-filled. |
10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG036-0006 | |||
| 2791 | ELG037 | SSN-VERIFICATION-FLAG | A code describing whether the state has verified the social security number (SSN) with the Social Security Administration (SSA). | Required | Value must be equal to a valid value. | 0 SSN not verified 1 SSN vsuccessfully verified by SSA 2 SSN is pending SSA verification 9 Unknown |
4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG037-0001 |
| 2792 | ELG038 | INCOME-CODE | A code indicating the family income level. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG038-0001 |
| 2793 | ELG039 | VETERAN-IND | A flag indicating if the individual served in the active military, naval, or air service. | Required | Value must be equal to a valid value. | 0 NO 1 YES 9 Unknown |
4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG039-0001 |
| 2794 | ELG039 | VETERAN-IND | An eligible individual who is younger than 17 years cannot be a veteran. | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG039-0002 | |||
| 2795 | ELG040 | CITIZENSHIP-IND | Indicates if individual is identified as a U.S. Citizen. | Required | Value must be equal to a valid value. | 0 NO 1 YES 9 Unknown |
4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG040-0001 |
| 2796 | ELG040 | CITIZENSHIP-IND | All eligible individuals flagged as non-citizens with IMMIGRATION-STATUS should also be flagged as non-citizens with CITIZENSHIP-IND | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG040-0002 | |||
| 2797 | ELG041 | CITIZENSHIP-VERIFICATION-FLAG | Indicates the individual is enrolled in Medicaid pending citizenship verification. | Required | Value must be equal to a valid value. | 0 NO 1 YES 9 Unknown |
2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG041-0001 |
| 2798 | ELG042 | IMMIGRATION-STATUS | The immigration status of the individual. | Required | Value must be equal to a valid value. | 1 Qualified non-citizen 2 Lawfully present under CHIPRA 214 3 Eligible only for payment for emergency services 8 Not Applicable (U.S. citizen) 9 Unknown |
4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG042-0001 |
| 2799 | ELG042 | IMMIGRATION-STATUS | All eligible individuals flagged as non-citizens with CITIZENSHIP-IND should also be flagged as non-citizens with IMMIGRATION-STATUS | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG042-0002 | |||
| 2800 | ELG043 | IMMIGRATION-VERIFICATION-FLAG | Indicates the individual is enrolled in Medicaid pending immigration verification. | Conditional | Value must be equal to a valid value. | 0 NO 1 YES 9 Unknown |
11/3/2015 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG043-0001 |
| 2801 | ELG044 | IMMIGRATION-STATUS-FIVE-YEAR-BAR-END-DATE | The date the five-year bar for an individual ends. Section 403 of the Personal Responsibility and Work Opportunity Reconciliation Act of 1996 (PRWORA) provides that certain immigrants who enter the United States on or after August 22, 1996 are not eligible to receive federally-funded benefits, including Medicaid and the State Children’s Health Insurance Program (SCHIP), for five years from the date they enter the country with a status as a “qualified alien.” |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG044-0001 | |
| 2802 | ELG044 | IMMIGRATION-STATUS-FIVE-YEAR-BAR-END-DATE | If not applicable (U.S. Citizen), enter all 8s | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG044-0002 | |||
| 2803 | ELG044 | IMMIGRATION-STATUS-FIVE-YEAR-BAR-END-DATE | If the individual is not a U.S. citizen, then his/her Immigration Status Five Year Bar End Date cannot be designated as not applicable (8-filled) | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG044-0003 | |||
| 2804 | ELG044 | IMMIGRATION-STATUS-FIVE-YEAR-BAR-END-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG044-0004 | |||
| 2805 | ELG044 | IMMIGRATION-STATUS-FIVE-YEAR-BAR-END-DATE | Value must be a valid date | 4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG044-0005 | |||
| 2806 | ELG045 | PRIMARY-LANGUAGE-ENGL-PROF-CODE | A code indicating the level of spoken English proficiency by the individual | Conditional | Value must be equal to a valid value. | 0 Very Well 1 Well 2 Not well 3 No spoken proficiency 9 Unknown |
11/3/2015 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG045-0001 |
| 2807 | ELG045 | PRIMARY-LANGUAGE-ENGL-PROF-CODE | Report this information for individuals 5 years old or older | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG045-0002 | |||
| 2808 | ELG046 | PRIMARY-LANGUAGE-CODE | A code indicating the language the individual speaks other than English at home | Conditional | Value must be equal to a valid value. | See language codes in Appendix G for a list of all valid language codes | 11/3/2015 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG046-0001 |
| 2809 | ELG046 | PRIMARY-LANGUAGE-CODE | See language codes in Appendix G for a list of all valid language codes | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG046-0002 | |||
| 2810 | ELG046 | PRIMARY-LANGUAGE-CODE | Report this information for individuals 5 years old or older | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG046-0003 | |||
| 2811 | ELG047 | HOUSEHOLD-SIZE | Household Size used in the eligibility determination process | Required | Value must be equal to a valid value. | 01 1 person 02 2 people 03 3 people 04 4 people 05 5 people 06 6 people 07 7 people 08 8 or more people 99 Unknown number of people |
4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG047-0001 |
| 2812 | ELG047 | HOUSEHOLD-SIZE | Use this code to indicate Household Size used in the eligibility determination process | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG047-0002 | |||
| 2813 | ELG049 | PREGNANCY-IND | A flag indicating the individual is pregnant | Conditional | Value must be equal to a valid value. | 0 NO 1 YES 9 Unknown |
11/3/2015 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG049-0001 |
| 2814 | ELG049 | PREGNANCY-IND | If an eligible individual is pregnant, she must be a female. | 4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG049-0002 | |||
| 2815 | ELG050 | MEDICARE-HIC-NUM | Health Insurance Claim (HIC) Number as it appears on the patient’s Medicare card. | Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9) |
11/3/2015 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG050-0001 | |
| 2816 | ELG050 | MEDICARE-HIC-NUM | If individual's dual eligibility code indicates he/she is NOT enrolled in Medicare, then Medicare HIC number must be 8-filled. | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG050-0002 | |||
| 2817 | ELG051 | MEDICARE-BENEFICIARY-IDENTIFIER | The individual’s Medicare Beneficiary Identifier (MBI) Identification Number. Note: MBI replaces the HICN with an entirely new Medicare Beneficiary Identifier (MBI) for purposes of provider billing, if applicable. CMS interfaces with non-payment exchange partners would remain HICN-based, while interfaces with payment partners would use the new MBI. |
NA | Limit characters to alphabet (A-Z, a-z), numerals (0-9) |
11/3/2015 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG051-0001 | |
| 2818 | ELG051 | MEDICARE-BENEFICIARY-IDENTIFIER | If individual is NOT enrolled in Medicare, 8-fill field | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG051-0002 | |||
| 2819 | ELG051 | MEDICARE-BENEFICIARY-IDENTIFIER | Field should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files) until such time as the Medicare Beneficiary Identifier is implemented (no target date has been established). | 9/23/2015 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG051-0003 | |||
| 2820 | ELG054 | CHIP-CODE | A code indicating the individual’s inclusion in a STATE Only CHIP Program. | Required | Value must be equal to a valid value. | 0 Individual was not Medicaid eligible and not eligible for separate CHIP for the month 1 Individual was Medicaid eligible, but was not included in either Medicaid-Expansion CHIP or a separate title XXI CHIP) program for the month 2 Individual was included in the Medicaid-Expansion CHIP program and subject to enhanced Federal matching for the month 3 Individual was not Medicaid-Expansion CHIP eligible, but was included in a separate title XXI CHIP program for the month. 4 Individual was both Medicaid-Eligible and Separate CHIP eligible during the same month 9 CHIP status unknown |
4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG054-0001 |
| 2821 | ELG054 | CHIP-CODE | Value is unknown | 4/30/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG054-0002 | |||
| 2822 | ELG054 | CHIP-CODE | If the individual was both Medicaid-Eligible and Separate CHIP eligible during the same month, CHIP-ENROLLMENT and MEDICAID-ENROLLMENT dates must not overlap for the same month | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG054-0003 | |||
| 2823 | ELG057 | VARIABLE-DEMOGRAPHIC-ELEMENT-EFF-DATE | The first day of the time span during which the values in all data elements in the VARIABLE DEMOGRAPHICS - ELIGIBILITY record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG057-0001 | |
| 2824 | ELG057 | VARIABLE-DEMOGRAPHIC-ELEMENT-EFF-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG057-0002 | |||
| 2825 | ELG057 | VARIABLE-DEMOGRAPHIC-ELEMENT-EFF-DATE | Whenever the value in one or more of the data elements in the VARIABLE DEMOGRAPHICS– ELIGIBILITY record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG057-0003 | |||
| 2826 | ELG057 | VARIABLE-DEMOGRAPHIC-ELEMENT-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG057-0004 | |||
| 2827 | ELG057 | VARIABLE-DEMOGRAPHIC-ELEMENT-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG057-0005 | |||
| 2828 | ELG058 | VARIABLE-DEMOGRAPHIC-ELEMENT-END-DATE | The last day of the time span during which the values in all data elements in the VARIABLE DEMOGRAPHICS - ELIGIBILITY record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG058-0001 | |
| 2829 | ELG058 | VARIABLE-DEMOGRAPHIC-ELEMENT-END-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG058-0002 | |||
| 2830 | ELG058 | VARIABLE-DEMOGRAPHIC-ELEMENT-END-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG058-0003 | |||
| 2831 | ELG058 | VARIABLE-DEMOGRAPHIC-ELEMENT-END-DATE | If there is no end date (i.e., the record is good into the indefinite future) use the “end-of-time” date (99991231) | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG058-0004 | |||
| 2832 | ELG058 | VARIABLE-DEMOGRAPHIC-ELEMENT-END-DATE | Whenever the value in one or more of the data elements in the VARIABLE DEMOGRAPHICS– ELIGIBILITY record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG058-0005 | |||
| 2833 | ELG058 | VARIABLE-DEMOGRAPHIC-ELEMENT-END-DATE | The VARIABLE-DEMOGRAPHIC-ELEMENT-END-DATE must occur on or after the VARIABLE-DEMOGRAPHIC-ELEMENT-EFF-DATE | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG058-0006 | |||
| 2834 | ELG058 | VARIABLE-DEMOGRAPHIC-ELEMENT-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG058-0007 | |||
| 2835 | ELG059 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG059-0001 | |
| 2836 | ELG059 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG059-0002 | |||
| 2837 | ELG060 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 | ELG060-0001 | |||
| 2838 | ELG061 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG061-0001 | |
| 2839 | ELG061 | RECORD-ID | Value must be in the required format | 4/30/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG061-0002 | |||
| 2840 | ELG061 | RECORD-ID | Value must be equal to a valid value. | ELG0004 - ELIGIBILE-CONTACT-INFORMATION | 4/30/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG061-0003 | ||
| 2841 | ELG061 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG061-0004 | |||
| 2842 | ELG062 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG062-0001 | |
| 2843 | ELG062 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG062-0002 | ||
| 2844 | ELG062 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG062-0003 | |||
| 2845 | ELG063 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG063-0001 | |
| 2846 | ELG063 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG063-0002 | |||
| 2847 | ELG063 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG063-0003 | |||
| 2848 | ELG064 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG064-0001 | |
| 2849 | ELG064 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG064-0002 | |||
| 2850 | ELG064 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG064-0003 | |||
| 2851 | ELG064 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG064-0004 | |||
| 2852 | ELG064 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG064-0005 | |||
| 2853 | ELG065 | ADDR-TYPE | The type of address and contact information for the eligible submitted in the record segment. | Required | Value must be equal to a valid value. | 01 Primary home address and contact information, used for the eligibility determination process 02 Primary work address and contact information 03 Secondary residence and contact information 04 Secondary work address and contact information 05 Other category of address and contact information 06 Eligible person’s official mailing address |
10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG065-0001 |
| 2854 | ELG065 | ADDR-TYPE | This data element must be populated on every ELIGIBLE-CONTACT-INFORMATION record. | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG065-0002 | |||
| 2855 | ELG066 | ELIGIBLE-ADDR-LN1 | The street address for the type of address indicated. | Required | Line 1 is required and the other two lines can be blank | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG066-0001 | |
| 2856 | ELG066 | ELIGIBLE-ADDR-LN1 | The first line of the address must not be the same as the second or third line of the address (if applicable) | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG066-0002 | |||
| 2857 | ELG066 | ELIGIBLE-ADDR-LN1 | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 4/30/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG066-0003 | |||
| 2858 | ELG067 | ELIGIBLE-ADDR-LN2 | The street address for the type of address indicated. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG067-0001 | |
| 2859 | ELG067 | ELIGIBLE-ADDR-LN2 | The second line of the address must not be the same as the first or third line of the address (if applicable) | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG067-0002 | |||
| 2860 | ELG067 | ELIGIBLE-ADDR-LN2 | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG067-0003 | |||
| 2861 | ELG068 | ELIGIBLE-ADDR-LN3 | The street address for the type of address indicated. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG068-0001 | |
| 2862 | ELG068 | ELIGIBLE-ADDR-LN3 | Line 1 is required and the other two lines can be blank | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG068-0002 | |||
| 2863 | ELG068 | ELIGIBLE-ADDR-LN3 | The third line of the address must not be the same as the first or second line of the address (if applicable) | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG068-0003 | |||
| 2864 | ELG068 | ELIGIBLE-ADDR-LN3 | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG068-0004 | |||
| 2865 | ELG069 | ELIGIBLE-CITY | The city for the type of address indicated in ADDR-TYPE. | Required | The city for the eligible individual's address must be reported. | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG069-0001 | |
| 2866 | ELG069 | ELIGIBLE-CITY | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 4/30/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG069-0002 | |||
| 2867 | ELG070 | ELIGIBLE-STATE | The ANSI state numeric for the U.S. state, Territory, or the District of Columbia code for where the individual eligible to receive healthcare services resides. (The state for the type of address indicated in ADDR-TYPE.) | Required | The state for the eligible individual's address must be reported. | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG070-0001 | |
| 2868 | ELG070 | ELIGIBLE-STATE | The field must be populated on every record | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG070-0002 | |||
| 2869 | ELG070 | ELIGIBLE-STATE | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG070-0003 | |
| 2870 | ELG071 | ELIGIBLE-ZIP-CODE | The zip code for the type of address indicated in ADDR-TYPE. | Required | First 5 bytes (i.e., the 5-digit zip code) is required | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG071-0001 | |
| 2871 | ELG071 | ELIGIBLE-ZIP-CODE | Last 4 bytes are optional. If the last 4 digits are not populated or used, then the 4-digit extended zip code should be recorded as “0000”. | 9/23/2015 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG071-0002 | |||
| 2872 | ELG071 | ELIGIBLE-ZIP-CODE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG071-0003 | |||
| 2873 | ELG072 | ELIGIBLE-COUNTY-CODE | ANSI county numeric code indicating the county for the type of address indicated in ADDR-TYPE. | Required | Dependent value must be equal to a valid value. | http://www.census.gov/geo/reference/codes/cou.html | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG072-0001 |
| 2874 | ELG072 | ELIGIBLE-COUNTY-CODE | The county for the eligible individual's address must be reported. | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG072-0002 | |||
| 2875 | ELG072 | ELIGIBLE-COUNTY-CODE | Value must be numeric. | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG072-0003 | |||
| 2876 | ELG073 | ELIGIBLE-PHONE-NUM | The telephone number of the type of address indicated. | Required | The phone number for the eligible individual must be reported. | 4/30/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG073-0001 | |
| 2877 | ELG073 | ELIGIBLE-PHONE-NUM | Enter digits only (i.e., no parentheses, dashes, periods, commas, spaces, etc.) | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG073-0002 | |||
| 2878 | ELG074 | TYPE-OF-LIVING-ARRANGEMENT | A free-form text field to describe the type of living arrangement used for the eligibility determination process. The field will remain a free-form text data element until MACPro develops a list of valid values. When it becomes available, T-MSIS will align with MACPro valid values listing. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG074-0001 | |
| 2879 | ELG074 | TYPE-OF-LIVING-ARRANGEMENT | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG074-0002 | |||
| 2880 | ELG075 | ELIGIBLE-ADDR-EFF-DATE | The first day of the time span during which the values in all data elements on an ELIGIBLE-CONTACT-INFORMATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG075-0001 | |
| 2881 | ELG075 | ELIGIBLE-ADDR-EFF-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG075-0002 | |||
| 2882 | ELG075 | ELIGIBLE-ADDR-EFF-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG075-0003 | |||
| 2883 | ELG075 | ELIGIBLE-ADDR-EFF-DATE | Value must be equal or less than END-OF-TIME-PERIOD in the header record | 4/30/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG075-0004 | |||
| 2884 | ELG075 | ELIGIBLE-ADDR-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG075-0005 | |||
| 2885 | ELG075 | ELIGIBLE-ADDR-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG075-0006 | |||
| 2886 | ELG076 | ELIGIBLE-ADDR-END-DATE | The last day of the time span during which the values in all data elements on an ELIGIBLE-CONTACT-INFORMATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG076-0001 | |
| 2887 | ELG076 | ELIGIBLE-ADDR-END-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG076-0002 | |||
| 2888 | ELG076 | ELIGIBLE-ADDR-END-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG076-0003 | |||
| 2889 | ELG076 | ELIGIBLE-ADDR-END-DATE | If there is no end date (i.e., the record is good into the indefinite future) use the “end-of-time” date (99991231) | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG076-0004 | |||
| 2890 | ELG076 | ELIGIBLE-ADDR-END-DATE | Whenever the value in one or more of the data elements on the ELIGIBLE-CONTACT-INFORMATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG076-0005 | |||
| 2891 | ELG076 | ELIGIBLE-ADDR-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG076-0006 | |||
| 2892 | ELG077 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG077-0001 | |
| 2893 | ELG077 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG077-0002 | |||
| 2894 | ELG078 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | ELIGIBILE-CONTACT-INFORMATION-ELG00004 | ELG078-0001 | |||
| 2895 | ELG079 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG079-0001 | |
| 2896 | ELG079 | RECORD-ID | Value must be in the required format | 4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG079-0002 | |||
| 2897 | ELG079 | RECORD-ID | Value must be equal to a valid value. | ELG0005 - ELIGIBILITY-DETERMINANTS | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG079-0003 | ||
| 2898 | ELG079 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG079-0004 | |||
| 2899 | ELG080 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG080-0001 | |
| 2900 | ELG080 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG080-0002 | ||
| 2901 | ELG080 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG080-0003 | |||
| 2902 | ELG081 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG081-0001 | |
| 2903 | ELG081 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG081-0002 | |||
| 2904 | ELG081 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG081-0003 | |||
| 2905 | ELG082 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG082-0001 | |
| 2906 | ELG082 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG082-0002 | |||
| 2907 | ELG082 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG082-0003 | |||
| 2908 | ELG082 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG082-0004 | |||
| 2909 | ELG082 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG082-0005 | |||
| 2910 | ELG083 | MSIS-CASE-NUM | The state-assigned number which uniquely identifies the Medicaid case to which the enrollee belongs. The definition of a case varies. There are single-person cases (mostly aged and blind/disabled) and multi-person cases (mostly TANF) in which all members of the case have the same case number, but a unique MSIS identification number. A warning for longitudinal research efforts: a person’s case number may change over time. | Required | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG083-0001 | |
| 2911 | ELG083 | MSIS-CASE-NUM | This field must contain the Medicaid case identification number assigned by the state. The format of the Medicaid case identification number must be supplied to CMS. | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG083-0002 | |||
| 2912 | ELG083 | MSIS-CASE-NUM | If multiple MSIS-CASE-NUMs exist at the state-level, and T-MSIS only allows one Case Number in current T-MSIS DD, please enter the Case Number with the longest eligibility days in that particular month. | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG083-0003 | |||
| 2913 | ELG084 | MEDICAID-BASIS-OF-ELIGIBILITY | A code indicating the individual’s most recent Medicaid eligibility for the month (not including CHIP). Note: This data element will be phased out in lieu of ELIGIBILITY-GROUP | Conditional | Value must be equal to a valid value. | 00 Individual was not eligible for Medicaid at any time during the month 01 Aged Individual 02 Blind/Disabled Individual 03 Not used 04 Child (not Child of Unemployed Adult, not Foster Care Child) 05 Adult (not based on unemployed status) 06 Child of Unemployed Adult (optional) 07 Unemployed Adult (optional) 08 Foster Care Child 10 Refugee Medical Assistance (45 CFR Sub-part G) 11 Individual covered under the Breast and Cervical Cancer Prevention and Treatment Act of 2000 99 Eligibility status unknown |
11/3/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG084-0001 |
| 2914 | ELG084 | MEDICAID-BASIS-OF-ELIGIBILITY | Submit records only for people who were eligible for Medicaid for at least one day during the FEDERAL FISCAL YEAR MONTH. | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG084-0002 | |||
| 2915 | ELG084 | MEDICAID-BASIS-OF-ELIGIBILITY | For people enrolled in non-Medicaid separate CHIP only for the month, MEDICAID-BASIS-OF-ELIGIBILITY must indicate the individual was not eligible for Medicaid during the month. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG084-0003 | |||
| 2916 | ELG084 | MEDICAID-BASIS-OF-ELIGIBILITY | If an eligible individual has a MEDICAID-BASIS-OF-ELIGIBILITY of Foster Care Child, then MAINTENANCE-ASSISTANCE-STATUS must be designated as Other. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG084-0004 | |||
| 2917 | ELG084 | MEDICAID-BASIS-OF-ELIGIBILITY | If an eligible individual has a MEDICAID-BASIS-OF-ELIGIBILITY of Child of an Unemployed Adult or Unemployed Adult, then MAINTENANCE-ASSISTANCE STATUS must be designated as Receiving Cash or eligible under section 1931 of the Act | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG084-0005 | |||
| 2918 | ELG084 | MEDICAID-BASIS-OF-ELIGIBILITY | If an eligible individual has a MEDICAID-BASIS-OF-ELIGIBILITY of Individual covered under the Breast and Cervical Cancer Prevention and Treatment Act of 2000, then MAINTENANCE-ASSISTANCE-STATUS must be designated as Poverty Related. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG084-0006 | |||
| 2919 | ELG084 | MEDICAID-BASIS-OF-ELIGIBILITY | If an eligible individual has a MEDICAID-BASIS-OF-ELIGIBILITY of Aged individual, then his/her date of birth must imply the Recipient was over 64 on the first day of the month | 4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG084-0007 | |||
| 2920 | ELG084 | MEDICAID-BASIS-OF-ELIGIBILITY | If an eligible individual has a MEDICAID-BASIS-OF-ELIGIBILITY of Child (not Child of Unemployed Adult, not Foster Care) or Child of an Unemployed Adult, then his/her date of birth must imply the Recipient was under 21 on the first day of the month | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG084-0008 | |||
| 2921 | ELG084 | MEDICAID-BASIS-OF-ELIGIBILITY | The MEDICAID-BASIS-OF-ELIGIBILITY and MAINTENANCE-ASSISTANCE-STATUS fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files) for enrollment periods encompassing January 1, 2014 and beyond. | 9/23/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG084-0009 | |||
| 2922 | ELG085 | DUAL-ELIGIBLE-CODE | Indicates coverage for individuals entitled to Medicare (Part A and/or B benefits) and eligible for some category of Medicaid benefits. | Conditional | Value must be equal to a valid value. | 00 Eligible is not a Medicare beneficiary 01 Eligible is entitled to Medicare- QMB only 02 Eligible is entitled to Medicare- QMB AND Medicaid coverage 03 Eligible is entitled to Medicare- SLMB only 04 Eligible is entitled to Medicare- SLMB AND Medicaid coverage 05 Eligible is entitled to Medicare- QDWI 06 Eligible is entitled to Medicare- Qualifying individuals 08 Eligible is entitled to Medicare- Other Dual Eligibles (Non QMB, SLMB, QDWI or QI) 09 Eligible is entitled to Medicare – Other (This code is to be used only with specific CMS approval.) 10 Separate CHIP Eligible is entitled to Medicare 99 Eligible's Medicare status is unknown. |
11/3/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG085-0001 |
| 2923 | ELG085 | DUAL-ELIGIBLE-CODE | This field should be populated from the same data that were used to populate the State’s submission of the Medicare Modernization Act (“State MMA File”) monthly file to CMS. In other words, the data values from the State MMA File should match this dual eligible data element. | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG085-0002 | |||
| 2924 | ELG085 | DUAL-ELIGIBLE-CODE | If the eligible individual is a partial dual eligible, then he/she must have a MAINTENANCE-ASSISTANCE-STATUS of Poverty-related | 4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG085-0003 | |||
| 2925 | ELG085 | DUAL-ELIGIBLE-CODE | If the eligible individual is not a dual eligible, he/she must not have a Medicare Beneficiary Identifier | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG085-0004 | |||
| 2926 | ELG085 | DUAL-ELIGIBLE-CODE | If the eligible individual is not a dual eligible, he/she must not have a Medicare Benficiary Identifier | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG085-0005 | |||
| 2927 | ELG085 | DUAL-ELIGIBLE-CODE | If the eligible individual is a dual eligible or enrolled in separate CHIP, then he/she cannot have a maintenance assistance status indicating that he/she is not eligible for Medicaid. | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG085-0006 | |||
| 2928 | ELG085 | DUAL-ELIGIBLE-CODE | If the eligible individual is a dual eligible or enrolled in separate CHIP, then he/she cannot have a basis of eligibility indicating that he/she is not eligible for Medicaid. | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG085-0007 | |||
| 2929 | ELG086 | PRIMARY-ELIGIBILITY-GROUP-IND | A flag indicating the eligibility record is the primary eligibility in cases where there are multiple eligibility records submitted. | Required | Value must be equal to a valid value. | 0 NO 1 YES |
4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG086-0001 |
| 2930 | ELG086 | PRIMARY-ELIGIBILITY-GROUP-IND | A person enrolled in Medicaid/CHIP should always have a primary eligibility group classification for any given day of enrollment. (There may or may not be a secondary eligibility group classification for that same day.) It is expected that an enrollee's eligibility group assignment ( ELG087 - ELIGIBILITY-GROUP) will change over time as his/her situation changes. Whenever the eligibility group assignment changes (i.e., ELG087 has a different value), a separate ELIGIBILITY-DETERMINANTS record segment should be created. In such situations, there would be multiple active ELIGIBILITY-DETERMINANTS record segments, each covering a different effective time span. In such situations, the value in ELG087 would be the primary eligibility group for the effective date span of its respective ELIGIBILITY-DETERMINANTS record segment, and the PRIMARY-ELIGIBILITY-GROUP-IND data element on each of these segments would be set to '1' (YES). |
11/12/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG086-0002 | |||
| 2931 | ELG086 | PRIMARY-ELIGIBILITY-GROUP-IND | Should a situation arise where a Medicaid/CHIP enrollee has been assigned both a primary and a secondary eligibility group, there would be two ELIGIBILITY-DETERMINANTS record segments with overlapping effective time spans - one segment containing the primary eligibility group and the other for the secondary eligibility group. The PRIMARY-ELIGIBILITY-GROUP-IND data element on each of the segments is used to differentiate the primary eligibility group from the secondary. | 11/12/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG086-0003 | |||
| 2932 | ELG087 | ELIGIBILITY-GROUP | The eligibility group applicable to the individual based on the eligibility determination process. The valid value list of eligibility groups aligns with those being used in the Medicaid and CHIP Program Data System (MACPro). | Conditional | Value must be equal to a valid value. | See Appendix F – Eligibility Group Table | 11/3/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG087-0001 |
| 2933 | ELG088 | LEVEL-OF-CARE-STATUS | The level of care required to meet an individual's needs and to determine LTSS program eligibility. | Conditional | Value must be equal to a valid value. | 001 Hospital as defined in 42 CFR §440.10 002 Inpatient psychiatric facility for individuals under age 21 as provided in 42 CFR § 440.160 003 Nursing Facility 004 ICF/IDD 005 Other Type of Facility 888 Not Applicable (Not in LTSS program) 999 Unknown |
11/3/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG088-0001 |
| 2934 | ELG089 | SSDI-IND | A flag indicating if the individual is enrolled in Social Security Disability Insurance (SSDI) administered via the Social Security Administration (SSA). | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 9 Unknown |
11/3/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG089-0001 |
| 2935 | ELG090 | SSI-IND | A flag indicating if the individual receives Supplemental Security Income (SSI) administered via the Social Security Administration (SSA). | Conditional | Value must be equal to a valid value. | 0 No 1 Yes 9 Unknown |
11/3/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG090-0001 |
| 2936 | ELG090 | SSI-IND | If an eligible individual is receiving SSI, then his/her SSI Status cannot be considered not applicable. | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG090-0002 | |||
| 2937 | ELG091 | SSI-STATE-SUPPLEMENT-STATUS-CODE | Indicates the individual's SSI State Supplemental Status. | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 Mandatory 002 Optional 999 Unknown |
11/3/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG091-0001 |
| 2938 | ELG091 | SSI-STATE-SUPPLEMENT-STATUS-CODE | An eligible individual cannot receive SSI State Supplements if they are not receiving SSI. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG091-0002 | |||
| 2939 | ELG092 | SSI-STATUS | Indicates the individual's SSI Status. | Conditional | Value must be equal to a valid value. | 000 Not Applicable 001 SSI 002 SSI Eligible Spouse 003 SSI Pending a Final Determination of Disposal of Resources Exceeding SSI Dollar Limits 999 Unknown |
11/3/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG092-0001 |
| 2940 | ELG092 | SSI-STATUS | An eligible individual cannot have an SSI Status if they are not receiving SSI or if his/her SSI status is pending decision. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG092-0002 | |||
| 2941 | ELG093 | STATE-SPEC-ELIG-GROUP | The composite of eligibility mapping factors used to create the corresponding Maintenance Assistance Status (MAS) and Basis of Eligibility (BOE) values. This field should not include information that already appears elsewhere on the Eligible-File record even if it is part of the MAS and BOE algorithm (e.g., age information computed from DATE-OF-BIRTH or COUNTY-CODE). |
Required | Concatenate alpha numeric representations of the eligibility mapping factors used to create monthly MAS and BOE. State needs to provide composite code reflecting the contents of this field (e.g., bytes 1-2 = aid category; bytes 3 = money code; bytes 4-5 = person code). If six bytes is insufficient to accommodate all of the eligibility factors, the state should select the most critical factors and include them in this field. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG093-0001 | |
| 2942 | ELG093 | STATE-SPEC-ELIG-GROUP | If the value for State Specific Eligibility Group is between 000000 and 999999, then DATE-OF-DEATH cannot be before the start of the reporting month. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG093-0002 | |||
| 2943 | ELG093 | STATE-SPEC-ELIG-GROUP | Value must be one of the valid codes submitted by the State. (States must submit lists of valid State specific eligibility factor codes to CMS in advance of transmitting T-MSIS files, and must update those lists whenever changes occur.) | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG093-0003 | |||
| 2944 | ELG093 | STATE-SPEC-ELIG-GROUP | For this field, always report whatever is present in the State system, even if it is clearly invalid. Fill this field with "9"s only when the State system contains no information | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG093-0004 | |||
| 2945 | ELG093 | STATE-SPEC-ELIG-GROUP | Value > 000000 and < 999999, DATE-OF-DEATH cannot be less than the reporting month. | 4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG093-0005 | |||
| 2946 | ELG094 | CONCEPTION-TO-BIRTH-IND | A flag to identify children eligible through the conception to birth option, which is available only through a separate CHIP Program. | Conditional | Value must be equal to a valid value. | 0 NO 1 YES 9 Unknown |
11/3/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG094-0001 |
| 2947 | ELG094 | CONCEPTION-TO-BIRTH-IND | If the individual is a child eligible through the conception to birth option, then the individual must have his/her eligibility indicate that he/she is eligible only through a separate CHIP program | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG094-0002 | |||
| 2948 | ELG094 | CONCEPTION-TO-BIRTH-IND | If an individual is eligible through the conception to birth option, then any associated claims for the individual must indicate the program type for the claim as State Plan -CHIP | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG094-0003 | |||
| 2949 | ELG094 | CONCEPTION-TO-BIRTH-IND | The CHIP-CODE must equal “3” (Individual was not Medicaid-Expansion CHIP eligible, but was included in a separate title XXI CHIP program) or “4” (Individual was both Medicaid eligible and Separate CHIP eligible.) | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG094-0004 | |||
| 2950 | ELG095 | ELIGIBILITY-CHANGE-REASON | The reason for a change in an individual's eligibility status. Report this reason when there is a change in the individual's eligibility status. | Conditional | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 11/3/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG095-0001 |
| 2951 | ELG096 | MAINTENANCE-ASSISTANCE-STATUS | A code indicating the individual’s maintenance assistance status. See Appendix C for a description of MSIS coding categories. Note: This data element will be phased out in lieu of ELIGIBILITY-GROUP. | Conditional | Value must be equal to a valid value. | 0 Individual was not eligible for Medicaid this month 1 Receiving Cash or eligible under section 1931 of the Act 2 Medically Needy 3 Poverty Related 4 Other 5 1115 - Demonstration expansion eligible 9 Status is unknown |
11/3/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG096-0001 |
| 2952 | ELG096 | MAINTENANCE-ASSISTANCE-STATUS | If the individual has a Maintenance Assistance Status indicating he/she is eligible for Medicaid, then his/her DATE-OF-DEATH cannot have occurred before the start of the time period for the file submission. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG096-0002 | |||
| 2953 | ELG096 | MAINTENANCE-ASSISTANCE-STATUS | If an eligible individual's Medicaid Basis of Eligibility indicates he/she is not eligible, then their Maintenance Assistance Status must also indicate he/she is not eligible. | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG096-0003 | |||
| 2954 | ELG096 | MAINTENANCE-ASSISTANCE-STATUS | If an eligible individual's Medicaid Basis of Eligibility indicates he/she is eligible, then their Maintenance Assistance Status must also indicate he/she is eligible. | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG096-0004 | |||
| 2955 | ELG096 | MAINTENANCE-ASSISTANCE-STATUS | If an eligible individual is not eligible, then he/she must have a populated Medicaid Enrollment End Date. | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG096-0005 | |||
| 2956 | ELG096 | MAINTENANCE-ASSISTANCE-STATUS | The MEDICAID-BASIS-OF-ELIGIBILITY and MAINTENANCE-ASSISTANCE-STATUS fields should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files) for enrollment periods encompassing January 1, 2014 and beyond. | 9/23/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG096-0006 | |||
| 2957 | ELG097 | RESTRICTED-BENEFITS-CODE | A flag that indicates the scope of Medicaid or CHIP benefits to which an individual is entitled to. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG097-0001 |
| 2958 | ELG097 | RESTRICTED-BENEFITS-CODE | If the individual is eligible for Medicaid but only entitled to restricted benefits based on Medicare dual-eligibility status, then his/her dual eligible status must indicate he/she is a partial dual eligible (QMB only, SLMB only, QDWI, or QI) | 4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG097-0002 | |||
| 2959 | ELG097 | RESTRICTED-BENEFITS-CODE | If the individual is eligible for Medicaid or CHIP but only entitled to restricted benefits for pregnancy-related services, then SEX must equal “F” | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG097-0003 | |||
| 2960 | ELG097 | RESTRICTED-BENEFITS-CODE | If an individual is not eligible then his/her restricted benefits status must also indicate that he/she is not eligible. | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG097-0004 | |||
| 2961 | ELG097 | RESTRICTED-BENEFITS-CODE | If an individual receives restricted benefits based on his/her alien status, then he/she must not be a U.S. citizen | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG097-0005 | |||
| 2962 | ELG097 | RESTRICTED-BENEFITS-CODE | If an individual's restricted benefits status indicates that they are entitled to any level of Medicaid or CHIP benefits, then his/her Maintenance Assistance Status and Basis of Eligibility cannot indicate he/she is not eligible. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG097-0006 | |||
| 2963 | ELG097 | RESTRICTED-BENEFITS-CODE | If an individual's restricted benefits status indicated they are entitled to benefits under Money Follows the Person, then he/she must not have an MFP Enrollment End date before the effective date for the Eligibility Determinant record segment. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG097-0007 | |||
| 2964 | ELG098 | TANF-CASH-CODE | A flag that indicates whether the individual received Temporary Assistance for Needy Families (TANF) benefits. | Conditional | Value must be equal to a valid value. | 0 Individual was not eligible for Medicaid. 1 Individual did not receive TANF benefits. 2 Individual did receive TANF benefits (States should only use this value if they can accurately separate eligible receiving TANF benefits from other 1931 eligible reported into MAS 1) 9 Individual’s TANF status is unknown |
11/3/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG098-0001 |
| 2965 | ELG098 | TANF-CASH-CODE | If an individual's TANF Cash Code indicates he/she was not eligible for Medicaid, then his/her Restricted Benefits Code must also indicate he/she was not eligible for Medicaid. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG098-0002 | |||
| 2966 | ELG099 | ELIGIBILITY-DETERMINANT-EFF-DATE | The start date of an individual's reported Eligibility Status. This date field is necessary when defining a unique row in a database table. |
Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG099-0001 | |
| 2967 | ELG099 | ELIGIBILITY-DETERMINANT-EFF-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG099-0002 | |||
| 2968 | ELG099 | ELIGIBILITY-DETERMINANT-EFF-DATE | If it is unknown when eligibility status became effective OR if a complete, valid date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG099-0003 | |||
| 2969 | ELG099 | ELIGIBILITY-DETERMINANT-EFF-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG099-0004 | |||
| 2970 | ELG099 | ELIGIBILITY-DETERMINANT-EFF-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG099-0005 | |||
| 2971 | ELG099 | ELIGIBILITY-DETERMINANT-EFF-DATE | Value must be equal or less than ELIGIBILITY-DETERMINANT-END-DATE | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG099-0006 | |||
| 2972 | ELG099 | ELIGIBILITY-DETERMINANT-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG099-0007 | |||
| 2973 | ELG099 | ELIGIBILITY-DETERMINANT-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG099-0008 | |||
| 2974 | ELG100 | ELIGIBILITY-DETERMINANT-END-DATE | The date that an individual's reported Eligibility Status ended. | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG100-0001 | |
| 2975 | ELG100 | ELIGIBILITY-DETERMINANT-END-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG100-0002 | |||
| 2976 | ELG100 | ELIGIBILITY-DETERMINANT-END-DATE | If it is unknown when eligibility status ended OR if a complete, valid date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG100-0003 | |||
| 2977 | ELG100 | ELIGIBILITY-DETERMINANT-END-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG100-0004 | |||
| 2978 | ELG100 | ELIGIBILITY-DETERMINANT-END-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG100-0005 | |||
| 2979 | ELG100 | ELIGIBILITY-DETERMINANT-END-DATE | Whenever the value in one or more of the data elements on the ELIGIBLE-DETERMINATES record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG100-0006 | |||
| 2980 | ELG100 | ELIGIBILITY-DETERMINANT-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG100-0007 | |||
| 2981 | ELG101 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG101-0001 | |
| 2982 | ELG101 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG101-0002 | |||
| 2983 | ELG102 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | ELIGIBILITY-DETERMINANTS-ELG00005 | ELG102-0001 | |||
| 2984 | ELG103 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG103-0001 | |
| 2985 | ELG103 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG103-0002 | |||
| 2986 | ELG103 | RECORD-ID | Value must be equal to a valid value. | ELG00006 - HEALTH-HOME-SPA-PARTICIPATION-INFORMATION | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG103-0003 | ||
| 2987 | ELG103 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG103-0004 | |||
| 2988 | ELG104 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG104-0001 | |
| 2989 | ELG104 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG104-0002 | ||
| 2990 | ELG104 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG104-0003 | |||
| 2991 | ELG105 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG105-0001 | |
| 2992 | ELG105 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG105-0002 | |||
| 2993 | ELG105 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG105-0003 | |||
| 2994 | ELG106 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG106-0001 | |
| 2995 | ELG106 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG106-0002 | |||
| 2996 | ELG106 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG106-0003 | |||
| 2997 | ELG106 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG106-0004 | |||
| 2998 | ELG106 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG106-0005 | |||
| 2999 | ELG107 | HEALTH-HOME-SPA-NAME | A free-form text field for the name of the health home program approved by CMS. This name needs to be consistent across files to be used for linking. | Conditional | Left justify and right-fill unused bytes with spaces | 11/3/2015 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG107-0001 | |
| 3000 | ELG107 | HEALTH-HOME-SPA-NAME | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG107-0002 | |||
| 3001 | ELG107 | HEALTH-HOME-SPA-NAME | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG107-0003 | |||
| 3002 | ELG108 | HEALTH-HOME-ENTITY-NAME | A field to identify the health home SPA in which an individual is enrolled. Because an identification numbering schema has not been established, the entities’ names are being used instead. | Conditional | Required on every HEALTH-HOME-SPA-PARTICIPATION-INFORMATION record | 11/3/2015 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG108-0001 | |
| 3003 | ELG108 | HEALTH-HOME-ENTITY-NAME | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG108-0002 | |||
| 3004 | ELG108 | HEALTH-HOME-ENTITY-NAME | Right-fill unused bytes if name is less than 100 bytes long | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG108-0003 | |||
| 3005 | ELG109 | HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE | The date on which the individual’s participation in the Health Home Program started. This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG109-0001 | |
| 3006 | ELG109 | HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG109-0002 | |||
| 3007 | ELG109 | HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE | If a complete, valid effective date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG109-0003 | |||
| 3008 | ELG109 | HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG109-0004 | |||
| 3009 | ELG109 | HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG109-0005 | |||
| 3010 | ELG109 | HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE | Value must be equal or less than HEALTH-HOME-SPA-PARTICIPATION-END-DATE | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG109-0006 | |||
| 3011 | ELG109 | HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE | If an individual is not eligible for Medicaid, then he/she should not have a Health Home SPA Participation Effective Date indicating the he/she started participation in the Health Home Program. | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG109-0007 | |||
| 3012 | ELG109 | HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG109-0008 | |||
| 3013 | ELG109 | HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG109-0009 | |||
| 3014 | ELG110 | HEALTH-HOME-SPA-PARTICIPATION-END-DATE | The date on which the individual’s participation in the Health Home Program ended. | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG110-0001 | |
| 3015 | ELG110 | HEALTH-HOME-SPA-PARTICIPATION-END-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG110-0002 | |||
| 3016 | ELG110 | HEALTH-HOME-SPA-PARTICIPATION-END-DATE | If a complete, valid effective date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG110-0003 | |||
| 3017 | ELG110 | HEALTH-HOME-SPA-PARTICIPATION-END-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG110-0004 | |||
| 3018 | ELG110 | HEALTH-HOME-SPA-PARTICIPATION-END-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG110-0005 | |||
| 3019 | ELG110 | HEALTH-HOME-SPA-PARTICIPATION-END-DATE | Whenever the value in one or more of the data elements on the HEALTH-HOME-SPA-PARTICIPATION-INFORMATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG110-0006 | |||
| 3020 | ELG110 | HEALTH-HOME-SPA-PARTICIPATION-END-DATE | Value must be equal or greater than HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG110-0007 | |||
| 3021 | ELG110 | HEALTH-HOME-SPA-PARTICIPATION-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG110-0008 | |||
| 3022 | ELG111 | HEALTH-HOME-ENTITY-EFF-DATE | The date on which the health home entity was approved by CMS to participate in the Health Home Program. | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG111-0001 | |
| 3023 | ELG111 | HEALTH-HOME-ENTITY-EFF-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG111-0002 | |||
| 3024 | ELG111 | HEALTH-HOME-ENTITY-EFF-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG111-0003 | |||
| 3025 | ELG111 | HEALTH-HOME-ENTITY-EFF-DATE | If a complete, valid effective date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG111-0004 | |||
| 3026 | ELG111 | HEALTH-HOME-ENTITY-EFF-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG111-0005 | |||
| 3027 | ELG111 | HEALTH-HOME-ENTITY-EFF-DATE | Value must be equal or less than START-OF-TIME-PERIOD. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG111-0006 | |||
| 3028 | ELG112 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG112-0001 | |
| 3029 | ELG112 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG112-0002 | |||
| 3030 | ELG113 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 | ELG113-0001 | |||
| 3031 | ELG114 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG114-0001 | |
| 3032 | ELG114 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG114-0002 | |||
| 3033 | ELG114 | RECORD-ID | Value must be equal to a valid value. | ELG00007 - HEALTH-HOME-SPA-PROVIDERS | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG114-0003 | ||
| 3034 | ELG114 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG114-0004 | |||
| 3035 | ELG115 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG115-0001 | |
| 3036 | ELG115 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG115-0002 | ||
| 3037 | ELG115 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG115-0003 | |||
| 3038 | ELG116 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG116-0001 | |
| 3039 | ELG116 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG116-0002 | |||
| 3040 | ELG116 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG116-0003 | |||
| 3041 | ELG117 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG117-0001 | |
| 3042 | ELG117 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG117-0002 | |||
| 3043 | ELG117 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG117-0003 | |||
| 3044 | ELG117 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG117-0004 | |||
| 3045 | ELG117 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG117-0005 | |||
| 3046 | ELG118 | HEALTH-HOME-SPA-NAME | A free-form text field for the name of the health home program approved by CMS. This name needs to be consistent across files to be used for linking. | Conditional | Left justify and right-fill unused bytes with spaces | 11/3/2015 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG118-0001 | |
| 3047 | ELG118 | HEALTH-HOME-SPA-NAME | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG118-0002 | |||
| 3048 | ELG119 | HEALTH-HOME-ENTITY-NAME | A field to identify the health home SPA in which an individual is enrolled. Because an identification numbering schema has not been established, the entities’ names are being used instead. | Conditional | Required on every HEALTH-HOME-SPA-PARTICIPATION-INFORMATION record | 11/3/2015 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG119-0001 | |
| 3049 | ELG119 | HEALTH-HOME-ENTITY-NAME | Right-fill unused bytes in name is less than 100 bytes long | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG119-0002 | |||
| 3050 | ELG119 | HEALTH-HOME-ENTITY-NAME | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG119-0003 | |||
| 3051 | ELG119 | HEALTH-HOME-ENTITY-NAME | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG119-0004 | |||
| 3052 | ELG120 | HEALTH-HOME-PROV-NUM | A unique identification number assigned by the state to the individual’s primary care manager for the Health Home in which the individual is enrolled. | Conditional | Valid formats must be supplied by the state in advance of submitting file data | Valid values are supplied by the state. | 11/3/2015 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG120-0001 |
| 3053 | ELG120 | HEALTH-HOME-PROV-NUM | Required on every HEALTH-HOME-SPA-PROVIDERS record | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG120-0002 | |||
| 3054 | ELG120 | HEALTH-HOME-PROV-NUM | Value must exist in the state’s submitted provider information | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG120-0003 | |||
| 3055 | ELG121 | HEALTH-HOME-SPA-PROVIDER-EFF-DATE | The date on which the eligible individual’s affiliation with the health home entity for the provision of health home services became effective. This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG121-0001 | |
| 3056 | ELG121 | HEALTH-HOME-SPA-PROVIDER-EFF-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG121-0002 | |||
| 3057 | ELG121 | HEALTH-HOME-SPA-PROVIDER-EFF-DATE | If a complete, valid effective date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG121-0003 | |||
| 3058 | ELG121 | HEALTH-HOME-SPA-PROVIDER-EFF-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG121-0004 | |||
| 3059 | ELG121 | HEALTH-HOME-SPA-PROVIDER-EFF-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG121-0005 | |||
| 3060 | ELG121 | HEALTH-HOME-SPA-PROVIDER-EFF-DATE | Value must be equal or less than HEALTH-HOME-SPA-PROVIDER-END-DATE | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG121-0006 | |||
| 3061 | ELG121 | HEALTH-HOME-SPA-PROVIDER-EFF-DATE | If an individual is not eligible for Medicaid, then he/she should not have a Health Home SPA Provider Effective Date indicating the he/she started affiliation with a provider entity in the Health Home Program. | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG121-0007 | |||
| 3062 | ELG121 | HEALTH-HOME-SPA-PROVIDER-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG121-0008 | |||
| 3063 | ELG121 | HEALTH-HOME-SPA-PROVIDER-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG121-0009 | |||
| 3064 | ELG122 | HEALTH-HOME-SPA-PROVIDER-END-DATE | The date on which the eligible individual’s affiliation with the health home entity for the provision of health home services ended. | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG122-0001 | |
| 3065 | ELG122 | HEALTH-HOME-SPA-PROVIDER-END-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG122-0002 | |||
| 3066 | ELG122 | HEALTH-HOME-SPA-PROVIDER-END-DATE | If a complete, valid effective date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG122-0003 | |||
| 3067 | ELG122 | HEALTH-HOME-SPA-PROVIDER-END-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG122-0004 | |||
| 3068 | ELG122 | HEALTH-HOME-SPA-PROVIDER-END-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG122-0005 | |||
| 3069 | ELG122 | HEALTH-HOME-SPA-PROVIDER-END-DATE | Whenever the value in one or more of the data elements on the HEALTH-HOME-SPA-PROVIDERS record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG122-0006 | |||
| 3070 | ELG122 | HEALTH-HOME-SPA-PROVIDER-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG122-0007 | |||
| 3071 | ELG123 | HEALTH-HOME-ENTITY-EFF-DATE | The date on which the health home entity was approved by CMS to participate in the Health Home Program. | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG123-0001 | |
| 3072 | ELG123 | HEALTH-HOME-ENTITY-EFF-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG123-0002 | |||
| 3073 | ELG123 | HEALTH-HOME-ENTITY-EFF-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG123-0003 | |||
| 3074 | ELG123 | HEALTH-HOME-ENTITY-EFF-DATE | If a complete, valid effective date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG123-0004 | |||
| 3075 | ELG123 | HEALTH-HOME-ENTITY-EFF-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG123-0005 | |||
| 3076 | ELG123 | HEALTH-HOME-ENTITY-EFF-DATE | Value must be equal or less than START-OF-TIME-PERIOD. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG123-0006 | |||
| 3077 | ELG124 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG124-0001 | |
| 3078 | ELG124 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG124-0002 | |||
| 3079 | ELG125 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | HEALTH-HOME-SPA-PROVIDERS-ELG00007 | ELG125-0001 | |||
| 3080 | ELG126 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG126-0001 | |
| 3081 | ELG126 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG126-0002 | |||
| 3082 | ELG126 | RECORD-ID | Value must be equal to a valid value. | ELG00008 - HEALTH-HOME-CHRONIC-CONDITIONS | 10/10/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG126-0003 | ||
| 3083 | ELG126 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG126-0004 | |||
| 3084 | ELG127 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG127-0001 | |
| 3085 | ELG127 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG127-0002 | ||
| 3086 | ELG127 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG127-0003 | |||
| 3087 | ELG128 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG128-0001 | |
| 3088 | ELG128 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG128-0002 | |||
| 3089 | ELG128 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG128-0003 | |||
| 3090 | ELG129 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG129-0001 | |
| 3091 | ELG129 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG129-0002 | |||
| 3092 | ELG129 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG129-0003 | |||
| 3093 | ELG129 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG129-0004 | |||
| 3094 | ELG129 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG129-0005 | |||
| 3095 | ELG130 | HEALTH-HOME-CHRONIC-CONDITION | The chronic condition used to determine the individual's eligibility for the health home provision. | Conditional | Value must be equal to a valid value. | A Mental health B Substance abuse C Asthma D Diabetes E Heart disease F Overweight (BMI of >25) G HIV/AIDS H Other |
11/3/2015 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG130-0001 |
| 3096 | ELG130 | HEALTH-HOME-CHRONIC-CONDITION | If value H (Other) is selected, identify the chronic condition in HEALTH-HOME-CHRONIC-CONDITION-OTHER-EXPLANATION. | 4/30/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG130-0002 | |||
| 3097 | ELG131 | HEALTH-HOME-CHRONIC-CONDITION-OTHER-EXPLANATION | A free-text field to capture the description of the other chronic condition (or conditions) when value “H” (Other) appears in the HEALTH-HOME-CHRONIC-CONDITION. | Conditional | Conditional (required when value “H” (Other) appears in HEALTH-HOME-CHRONIC-CONDITION | 2/25/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG131-0001 | |
| 3098 | ELG131 | HEALTH-HOME-CHRONIC-CONDITION-OTHER-EXPLANATION | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 2/25/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG131-0002 | |||
| 3099 | ELG132 | HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE | The first day of the time span during which the values in all data elements on a HEALTH-HOME-CHRONIC-CONDITIONS record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created.) This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG132-0001 | |
| 3100 | ELG132 | HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG132-0002 | |||
| 3101 | ELG132 | HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE | If a complete, valid effective date is not available fill with 99999999 | 4/30/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG132-0003 | |||
| 3102 | ELG132 | HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG132-0004 | |||
| 3103 | ELG132 | HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG132-0005 | |||
| 3104 | ELG132 | HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE | Value must be equal or less than HEALTH-HOME-CHRONIC-CONDITION-END-DATE | 2/25/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG132-0006 | |||
| 3105 | ELG132 | HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE | Whenever the value in one or more of the data elements on the HEALTH-HOME-CHRONIC-CONDITIONS record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG132-0007 | |||
| 3106 | ELG132 | HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG132-0008 | |||
| 3107 | ELG132 | HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG132-0009 | |||
| 3108 | ELG133 | HEALTH-HOME-CHRONIC-CONDITION-END-DATE | The last day of the time span during which the values in all data elements on a HEALTH-HOME-CHRONIC-CONDITIONS record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created.) | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG133-0001 | |
| 3109 | ELG133 | HEALTH-HOME-CHRONIC-CONDITION-END-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG133-0002 | |||
| 3110 | ELG133 | HEALTH-HOME-CHRONIC-CONDITION-END-DATE | If a complete, valid effective date is not available fill with 99999999 | 4/30/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG133-0003 | |||
| 3111 | ELG133 | HEALTH-HOME-CHRONIC-CONDITION-END-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG133-0004 | |||
| 3112 | ELG133 | HEALTH-HOME-CHRONIC-CONDITION-END-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG133-0005 | |||
| 3113 | ELG133 | HEALTH-HOME-CHRONIC-CONDITION-END-DATE | If there is no end date (i.e., the record is good into the indefinite future) use the “end-of-time” date (99991231) | 10/10/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG133-0006 | |||
| 3114 | ELG133 | HEALTH-HOME-CHRONIC-CONDITION-END-DATE | Whenever the value in one or more of the data elements on the HEALTH-HOME-CHRONIC-CONDITIONS record segment changes, a new record segment must be created | 10/10/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG133-0007 | |||
| 3115 | ELG133 | HEALTH-HOME-CHRONIC-CONDITION-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG133-0008 | |||
| 3116 | ELG134 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG134-0001 | |
| 3117 | ELG134 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG134-0002 | |||
| 3118 | ELG135 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 | ELG135-0001 | |||
| 3119 | ELG136 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG136-0001 | |
| 3120 | ELG136 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG136-0002 | |||
| 3121 | ELG136 | RECORD-ID | Value must be equal to a valid value. | ELG00009 - LOCK-IN-INFORMATION | 10/10/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG136-0003 | ||
| 3122 | ELG136 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG136-0004 | |||
| 3123 | ELG137 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG137-0001 | |
| 3124 | ELG137 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG137-0002 | ||
| 3125 | ELG137 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG137-0003 | |||
| 3126 | ELG138 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG138-0001 | |
| 3127 | ELG138 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG138-0002 | |||
| 3128 | ELG138 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG138-0003 | |||
| 3129 | ELG139 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG139-0001 | |
| 3130 | ELG139 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG139-0002 | |||
| 3131 | ELG139 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG139-0003 | |||
| 3132 | ELG139 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG139-0004 | |||
| 3133 | ELG139 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG139-0005 | |||
| 3134 | ELG140 | LOCKIN-PROV-NUM | A unique identification number assigned by the state to a provider furnishing locked-in healthcare services to an individual. | Conditional | Valid formats must be supplied by the state in advance of submitting file data | 11/3/2015 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG140-0001 | |
| 3135 | ELG141 | LOCKIN-PROV-TYPE | A code describing the provider type classification for which the provider/beneficiary lock-in relationship exists. | Conditional | The LOCKIN-PROV-TYPE value must exist as an active valid value for the provider in the provider subject area (i.e., the LOCKIN-PROV-TYPE must exist as an active value for the provider in the PROV-CLASSIFICATION-CODE field, where PROV-CLASSIFICATION-TYPE = 3 (Provider Type Code)). | See Appendix A for listing of valid values. | 11/3/2015 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG141-0001 |
| 3136 | ELG142 | LOCKIN-EFF-DATE | The date on which the lock in period begins for an individual with a healthcare service/provider. This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG142-0001 | |
| 3137 | ELG142 | LOCKIN-EFF-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG142-0002 | |||
| 3138 | ELG142 | LOCKIN-EFF-DATE | If a complete, valid effective date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG142-0003 | |||
| 3139 | ELG142 | LOCKIN-EFF-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG142-0004 | |||
| 3140 | ELG142 | LOCKIN-EFF-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG142-0005 | |||
| 3141 | ELG142 | LOCKIN-EFF-DATE | Value must be equal or less than LOCKIN-END-DATE | 4/30/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG142-0006 | |||
| 3142 | ELG142 | LOCKIN-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG142-0007 | |||
| 3143 | ELG142 | LOCKIN-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG142-0008 | |||
| 3144 | ELG143 | LOCKIN-END-DATE | The date on which the lock in period ends for an individual with a healthcare service/provider. | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG143-0001 | |
| 3145 | ELG143 | LOCKIN-END-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG143-0002 | |||
| 3146 | ELG143 | LOCKIN-END-DATE | If a complete, valid effective date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG143-0003 | |||
| 3147 | ELG143 | LOCKIN-END-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG143-0004 | |||
| 3148 | ELG143 | LOCKIN-END-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG143-0005 | |||
| 3149 | ELG143 | LOCKIN-END-DATE | Whenever the value in one or more of the data elements on the LOCK-IN-INFORMATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG143-0006 | |||
| 3150 | ELG143 | LOCKIN-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG143-0007 | |||
| 3151 | ELG144 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG144-0001 | |
| 3152 | ELG144 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG144-0002 | |||
| 3153 | ELG145 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | LOCK-IN-INFORMATION-ELG00009 | ELG145-0001 | |||
| 3154 | ELG146 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG146-0001 | |
| 3155 | ELG146 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG146-0002 | |||
| 3156 | ELG146 | RECORD-ID | Value must be equal to a valid value. | ELG00010 - MFP-INFORMATION | 10/10/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG146-0003 | ||
| 3157 | ELG146 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG146-0004 | |||
| 3158 | ELG147 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG147-0001 | |
| 3159 | ELG147 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG147-0002 | ||
| 3160 | ELG147 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG147-0003 | |||
| 3161 | ELG148 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG148-0001 | |
| 3162 | ELG148 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG148-0002 | |||
| 3163 | ELG148 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG148-0003 | |||
| 3164 | ELG149 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG149-0001 | |
| 3165 | ELG149 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG149-0002 | |||
| 3166 | ELG149 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number. | 2/25/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG149-0003 | |||
| 3167 | ELG149 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG149-0004 | |||
| 3168 | ELG149 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG149-0005 | |||
| 3169 | ELG150 | MFP-LIVES-WITH-FAMILY | A code indicating if the individual lives with his/her family or is not a participant in the MFP program. | Conditional | Value must be equal to a valid value. | 0 NO 1 YES 2 Non Participation 9 Unknown |
11/3/2015 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG150-0001 |
| 3170 | ELG151 | MFP-QUALIFIED-INSTITUTION | A code describing type of qualified institution at the time of transition to the community for an eligible MFP Demonstration participant. | Conditional | Value must be equal to a valid value. | 00 Default- Non Participation 01 Nursing Facility 02 ICF/IID (Intermediate Care Facilities for individuals with Intellectual Disabilities) 03 IMD (Institution for Mental Diseases) 04 Hospital 05 Other 99 Unknown |
11/3/2015 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG151-0001 |
| 3171 | ELG152 | MFP-QUALIFIED-RESIDENCE | A code indicating the type of qualified residence. | Conditional | Value must be equal to a valid value. | 00 Default - Non Participation 01 Home owned by participant 02 Home owned by family member 03 Apartment leased by participant, not assisted living 04 Apartment leased by participant, assisted living 05 Group home of no more than 4 people 99 Unknown |
11/3/2015 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG152-0001 |
| 3172 | ELG153 | MFP-REASON-PARTICIPATION-ENDED | A code describing reason why individual’s participation in the Money Follows the Person Demonstration ended. | Conditional | Value must be equal to a valid value. | 00 Default – No Participation 01 Completed 365 days of participation 02 Suspended eligibility 03 Re-institutionalized 04 Died 05 Moved 06 No longer needed services 07 Other 99 Unknown |
11/3/2015 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG153-0001 |
| 3173 | ELG153 | MFP-REASON-PARTICIPATION-ENDED | If an eligible individual's participation in MFP has ended, then MFP Enrollment End Date cannot be designated as not applicable | 2/25/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG153-0002 | |||
| 3174 | ELG154 | MFP-REINSTITUTIONALIZED-REASON | A code describing reason why individual was re-institutionalized after participation in the Money Follows the Person Demonstration. | Conditional | Value must be equal to a valid value. | 00 Default- Non Participation 01 Acute care hospitalization followed by long term rehabilitation 02 Deterioration in cognitive functioning 03 Deterioration in health 04 Deterioration in mental health 05 Loss of housing 06 Loss of personal care giver 07 By request of participant or guardian 08 Lack of sufficient community services 99 Unknown |
11/3/2015 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG154-0001 |
| 3175 | ELG155 | MFP-ENROLLMENT-EFF-DATE | The date on which the individual’s participation in the Money Follows the Person Demonstration started. This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG155-0001 | |
| 3176 | ELG155 | MFP-ENROLLMENT-EFF-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG155-0002 | |||
| 3177 | ELG155 | MFP-ENROLLMENT-EFF-DATE | If a complete, valid effective date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG155-0003 | |||
| 3178 | ELG155 | MFP-ENROLLMENT-EFF-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG155-0004 | |||
| 3179 | ELG155 | MFP-ENROLLMENT-EFF-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG155-0005 | |||
| 3180 | ELG155 | MFP-ENROLLMENT-EFF-DATE | Value must be equal or less than MFP-ENROLLMENT-END-DATE | 4/30/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG155-0006 | |||
| 3181 | ELG155 | MFP-ENROLLMENT-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG155-0007 | |||
| 3182 | ELG155 | MFP-ENROLLMENT-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG155-0008 | |||
| 3183 | ELG156 | MFP-ENROLLMENT-END-DATE | The date on which the individual’s participation in the Money Follows the Person Demonstration ended. | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG156-0001 | |
| 3184 | ELG156 | MFP-ENROLLMENT-END-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG156-0002 | |||
| 3185 | ELG156 | MFP-ENROLLMENT-END-DATE | If a complete, valid effective date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG156-0003 | |||
| 3186 | ELG156 | MFP-ENROLLMENT-END-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG156-0004 | |||
| 3187 | ELG156 | MFP-ENROLLMENT-END-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG156-0005 | |||
| 3188 | ELG156 | MFP-ENROLLMENT-END-DATE | Whenever the value in one or more of the data elements on the MFP-INFORMATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG156-0006 | |||
| 3189 | ELG156 | MFP-ENROLLMENT-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG156-0007 | |||
| 3190 | ELG157 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG157-0001 | |
| 3191 | ELG157 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG157-0002 | |||
| 3192 | ELG158 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | MFP-INFORMATION-ELG00010 | ELG158-0001 | |||
| 3193 | ELG159 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG159-0001 | |
| 3194 | ELG159 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG159-0002 | |||
| 3195 | ELG159 | RECORD-ID | Value must be equal to a valid value. | ELG00011 - STATE-PLAN-OPTION-PARTICIPATION | 10/10/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG159-0003 | ||
| 3196 | ELG159 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG159-0004 | |||
| 3197 | ELG160 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG160-0001 | |
| 3198 | ELG160 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG160-0002 | ||
| 3199 | ELG160 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG160-0003 | |||
| 3200 | ELG161 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG161-0001 | |
| 3201 | ELG161 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG161-0002 | |||
| 3202 | ELG161 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG161-0003 | |||
| 3203 | ELG162 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG162-0001 | |
| 3204 | ELG162 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG162-0002 | |||
| 3205 | ELG162 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG162-0003 | |||
| 3206 | ELG162 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG162-0004 | |||
| 3207 | ELG162 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG162-0005 | |||
| 3208 | ELG163 | STATE-PLAN-OPTION-TYPE | This field specifies the State Plan Options in which the individual is enrolled. Use on occurrence for each State Plan Option enrollment. | Conditional | Value must be equal to a valid value. | 00 Not Applicable 01 Community First Choice 02 1915(i) 03 1915(j) 04 1932(a) 05 1915(a) 06 1937 (Alternative Benefit Plans) 99 Unknown |
11/3/2015 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG163-0001 |
| 3209 | ELG163 | STATE-PLAN-OPTION-TYPE | If an individual is not eligible, then he/she cannot have a State Plan Option Type. | 2/25/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG163-0002 | |||
| 3210 | ELG164 | STATE-PLAN-OPTION-EFF-DATE | The date on which the individual’s participation in the State Plan Option Type began. This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG164-0001 | |
| 3211 | ELG164 | STATE-PLAN-OPTION-EFF-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG164-0002 | |||
| 3212 | ELG164 | STATE-PLAN-OPTION-EFF-DATE | If a complete, valid effective date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG164-0003 | |||
| 3213 | ELG164 | STATE-PLAN-OPTION-EFF-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG164-0004 | |||
| 3214 | ELG164 | STATE-PLAN-OPTION-EFF-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG164-0005 | |||
| 3215 | ELG164 | STATE-PLAN-OPTION-EFF-DATE | Value must be equal or less than STATE-PLAN-OPTION-END-DATE | 4/30/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG164-0006 | |||
| 3216 | ELG164 | STATE-PLAN-OPTION-EFF-DATE | If an individual is not eligible, then he/she cannot participate in a State Plan Option. | 2/25/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG164-0007 | |||
| 3217 | ELG164 | STATE-PLAN-OPTION-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG164-0008 | |||
| 3218 | ELG164 | STATE-PLAN-OPTION-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG164-0009 | |||
| 3219 | ELG165 | STATE-PLAN-OPTION-END-DATE | The date on which the individual’s participation in the State Plan Option Type ended. | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG165-0001 | |
| 3220 | ELG165 | STATE-PLAN-OPTION-END-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG165-0002 | |||
| 3221 | ELG165 | STATE-PLAN-OPTION-END-DATE | If a complete, valid effective date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG165-0003 | |||
| 3222 | ELG165 | STATE-PLAN-OPTION-END-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG165-0004 | |||
| 3223 | ELG165 | STATE-PLAN-OPTION-END-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG165-0005 | |||
| 3224 | ELG165 | STATE-PLAN-OPTION-END-DATE | Whenever the value in one or more of the data elements on the STATE-PLAN-OPTION-PARTICIPATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG165-0006 | |||
| 3225 | ELG165 | STATE-PLAN-OPTION-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG165-0007 | |||
| 3226 | ELG166 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG166-0001 | |
| 3227 | ELG166 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG166-0002 | |||
| 3228 | ELG167 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | STATE-PLAN-OPTION-PARTICIPATION-ELG00011 | ELG167-0001 | |||
| 3229 | ELG168 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG168-0001 | |
| 3230 | ELG168 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG168-0002 | |||
| 3231 | ELG168 | RECORD-ID | Value must be equal to a valid value. | ELG00012 - WAIVER-PARTICIPATION | 10/10/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG168-0003 | ||
| 3232 | ELG168 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG168-0004 | |||
| 3233 | ELG169 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG169-0001 | |
| 3234 | ELG169 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG169-0002 | ||
| 3235 | ELG169 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG169-0003 | |||
| 3236 | ELG170 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG170-0001 | |
| 3237 | ELG170 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG170-0002 | |||
| 3238 | ELG170 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG170-0005 | |||
| 3239 | ELG171 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG171-0001 | |
| 3240 | ELG171 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG171-0002 | |||
| 3241 | ELG171 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG171-0003 | |||
| 3242 | ELG171 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG171-0004 | |||
| 3243 | ELG171 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG171-0005 | |||
| 3244 | ELG172 | WAIVER-ID | Field specifying the waiver or demonstration which authorized payment for a claim. These IDs must be the approved, full federal waiver ID number assigned during the state submission and CMS approval process. The categories of demonstration and waiver programs include: 1915(b)(1); 1915(b)(2); 1915(b)(3), and 1915(b)(4) managed care waivers; 1915(c) home and community based services waivers; combined 1915(b) and 1915(c) managed home and community based services waivers and 1115 demonstrations. | Conditional | Create as many WAIVER-PARTICIPATION (ELG00012) record segments as necessary to record all waivers that are applicable. | 11/3/2015 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG172-0001 | |
| 3245 | ELG172 | WAIVER-ID | Report the full federal waiver identifier. | Valid values are supplied by the state. | 11/9/2015 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG172-0002 | ||
| 3246 | ELG172 | WAIVER-ID | Value must correspond to the WAIVER-TYPE | 10/10/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG172-0003 | |||
| 3247 | ELG173 | WAIVER-TYPE | Codes for specifying waiver types under which the eligible individual is covered during the month. | Conditional | Please fill in the WAIVER-TYPE fields in sequence (e.g., if an individual is enrolled in two waivers, only the first and second should be used; if only enrolled in one waiver, code WAIVER-TYPE1 | 11/3/2015 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG173-0001 | |
| 3248 | ELG173 | WAIVER-TYPE | Enter the WAIVER-TYPE assigned | See Appendix A for listing of valid values. | 10/10/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG173-0002 | ||
| 3249 | ELG173 | WAIVER-TYPE | If individual was eligible for Medicaid or CHIP but not eligible for a waiver, 8-fill | 10/10/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG173-0003 | |||
| 3250 | ELG174 | WAIVER-ENROLLMENT-EFF-DATE | Date an individual's enrollment under a particular waiver began. This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG174-0001 | |
| 3251 | ELG174 | WAIVER-ENROLLMENT-EFF-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG174-0002 | |||
| 3252 | ELG174 | WAIVER-ENROLLMENT-EFF-DATE | If a complete, valid start date is not available or is unknown, fill with 99999999 | 2/25/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG174-0003 | |||
| 3253 | ELG174 | WAIVER-ENROLLMENT-EFF-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG174-0004 | |||
| 3254 | ELG174 | WAIVER-ENROLLMENT-EFF-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG174-0005 | |||
| 3255 | ELG174 | WAIVER-ENROLLMENT-EFF-DATE | Value must be equal or less than WAIVER-ENROLLMENT-END-DATE | 4/30/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG174-0006 | |||
| 3256 | ELG174 | WAIVER-ENROLLMENT-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG174-0007 | |||
| 3257 | ELG174 | WAIVER-ENROLLMENT-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG174-0008 | |||
| 3258 | ELG175 | WAIVER-ENROLLMENT-END-DATE | Date an individual's enrollment under a particular waiver ended. | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG175-0001 | |
| 3259 | ELG175 | WAIVER-ENROLLMENT-END-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG175-0002 | |||
| 3260 | ELG175 | WAIVER-ENROLLMENT-END-DATE | If a complete, valid end date is not available or is unknown, fill with 99999999 | 2/25/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG175-0003 | |||
| 3261 | ELG175 | WAIVER-ENROLLMENT-END-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG175-0004 | |||
| 3262 | ELG175 | WAIVER-ENROLLMENT-END-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG175-0005 | |||
| 3263 | ELG175 | WAIVER-ENROLLMENT-END-DATE | Whenever the value in one or more of the data elements on the WAIVER-PARTICIPATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG175-0006 | |||
| 3264 | ELG175 | WAIVER-ENROLLMENT-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG175-0007 | |||
| 3265 | ELG176 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG176-0001 | |
| 3266 | ELG176 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG176-0002 | |||
| 3267 | ELG177 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | WAIVER-PARTICIPATION-ELG00012 | ELG177-0001 | |||
| 3268 | ELG178 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG178-0001 | |
| 3269 | ELG178 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG178-0002 | |||
| 3270 | ELG178 | RECORD-ID | Value must be equal to a valid value. | ELG00013 - LTSS-PARTICIPATION | 10/10/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG178-0003 | ||
| 3271 | ELG178 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG178-0004 | |||
| 3272 | ELG179 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG179-0001 | |
| 3273 | ELG179 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG179-0002 | ||
| 3274 | ELG179 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG179-0003 | |||
| 3275 | ELG180 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG180-0001 | |
| 3276 | ELG180 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG180-0002 | |||
| 3277 | ELG180 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG180-0003 | |||
| 3278 | ELG181 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG181-0001 | |
| 3279 | ELG181 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG181-0002 | |||
| 3280 | ELG181 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG181-0003 | |||
| 3281 | ELG181 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG181-0004 | |||
| 3282 | ELG181 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG181-0005 | |||
| 3283 | ELG182 | LTSS-LEVEL-CARE | The level of care provided to the individual by the long term care facility. | Conditional | Value must be equal to a valid value. | 1 Skilled Care 2 Intermediate Care 3 Custodial Care 9 Unknown |
11/3/2015 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG182-0001 |
| 3284 | ELG183 | LTSS-PROV-NUM | A unique identification number assigned by the state to the long term care facility furnishing healthcare services to the individual. | Conditional | Valid formats must be supplied by the state in advance of submitting file data | Valid values are supplied by the state. | 11/3/2015 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG183-0001 |
| 3285 | ELG184 | LTSS-ELIGIBILITY-EFF-DATE | The date on which the individual’s eligibility for long term care nursing home service began. (This field should use the onset date of the eligibility period and not the service span.) This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG184-0001 | |
| 3286 | ELG184 | LTSS-ELIGIBILITY-EFF-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG184-0002 | |||
| 3287 | ELG184 | LTSS-ELIGIBILITY-EFF-DATE | If a complete, valid start date is not available or is unknown, fill with 99999999 | 2/25/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG184-0003 | |||
| 3288 | ELG184 | LTSS-ELIGIBILITY-EFF-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG184-0004 | |||
| 3289 | ELG184 | LTSS-ELIGIBILITY-EFF-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG184-0005 | |||
| 3290 | ELG184 | LTSS-ELIGIBILITY-EFF-DATE | Value must be equal or less than LTSS-ELIGIBILITY-END-DATE | 4/30/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG184-0006 | |||
| 3291 | ELG184 | LTSS-ELIGIBILITY-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG184-0007 | |||
| 3292 | ELG184 | LTSS-ELIGIBILITY-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG184-0008 | |||
| 3293 | ELG185 | LTSS-ELIGIBILITY-END-DATE | The date on which the individual’s eligibility for long term care nursing home service ended. (This field should use the end date of the eligibility period and not the service span.) | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG185-0001 | |
| 3294 | ELG185 | LTSS-ELIGIBILITY-END-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG185-0002 | |||
| 3295 | ELG185 | LTSS-ELIGIBILITY-END-DATE | If a complete, valid date is not available fill with 99999999 | 2/25/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG185-0003 | |||
| 3296 | ELG185 | LTSS-ELIGIBILITY-END-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG185-0004 | |||
| 3297 | ELG185 | LTSS-ELIGIBILITY-END-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG185-0005 | |||
| 3298 | ELG185 | LTSS-ELIGIBILITY-END-DATE | Whenever the value in one or more of the data elements on the LTSS-PARTICIPATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG185-0006 | |||
| 3299 | ELG185 | LTSS-ELIGIBILITY-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG185-0007 | |||
| 3300 | ELG186 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG186-0001 | |
| 3301 | ELG186 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG186-0002 | |||
| 3302 | ELG187 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | LTSS-PARTICIPATION-ELG00013 | ELG187-0001 | |||
| 3303 | ELG188 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG188-0001 | |
| 3304 | ELG188 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG188-0002 | |||
| 3305 | ELG188 | RECORD-ID | Value must be equal to a valid value. | ELG00014 - MANAGED-CARE-PARTICIPATION | 10/10/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG188-0003 | ||
| 3306 | ELG188 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG188-0004 | |||
| 3307 | ELG189 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG189-0001 | |
| 3308 | ELG189 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG189-0002 | ||
| 3309 | ELG189 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG189-0003 | |||
| 3310 | ELG190 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG190-0001 | |
| 3311 | ELG190 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG190-0002 | |||
| 3312 | ELG190 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG190-0003 | |||
| 3313 | ELG191 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG191-0001 | |
| 3314 | ELG191 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG191-0002 | |||
| 3315 | ELG191 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG191-0003 | |||
| 3316 | ELG191 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG191-0004 | |||
| 3317 | ELG191 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG191-0005 | |||
| 3318 | ELG192 | MANAGED-CARE-PLAN-ID | The managed care plan identification number under which the eligible individual is enrolled. Use the state’s own identifier. If the state uses the national health plan identifier as its internal number, enter that value in this field as well as the NATIONAL-HEALTH-CARE-ENTITY-ID field. | Conditional | Must be populated on every record | 11/3/2015 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG192-0001 | |
| 3319 | ELG192 | MANAGED-CARE-PLAN-ID | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG192-0002 | |||
| 3320 | ELG192 | MANAGED-CARE-PLAN-ID | If individual is not enrolled in any managed care plan, 8-fill | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG192-0003 | |||
| 3321 | ELG192 | MANAGED-CARE-PLAN-ID | If the MANAGED-CARE-PLAN-ID field is not applicable, then MANAGED-CARE-PLAN-TYPE must be designated as not applicable | 10/10/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG192-0004 | |||
| 3322 | ELG193 | MANAGED-CARE-PLAN-TYPE | The type of managed care plan that corresponds to the MANAGED-CARE-PLAN-ID. | Conditional | Please fill in the MANAGED-CARE-PLAN-TYPE in sequence (e.g., if an individual is enrolled in two managed care plans, only the first and second fields should be used; if only enrolled in one managed care plan, code MANAGED-CARE-PLAN-TYPE1 and 8-fill MANAGED-CARE-PLAN-TYPE2 through MANAGED-CARE-PLAN-TYPE4) | 11/3/2015 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG193-0001 | |
| 3323 | ELG193 | MANAGED-CARE-PLAN-TYPE | Value is not included in the valid code list | See Appendix A for listing of valid values. | 10/10/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG193-0002 | ||
| 3324 | ELG193 | MANAGED-CARE-PLAN-TYPE | Values must correspond to associated MANAGE-CARE-PLAN-ID in state-provided crosswalk | 10/10/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG193-0003 | |||
| 3325 | ELG193 | MANAGED-CARE-PLAN-TYPE | If individual is not enrolled in any managed care plan, 8-fill | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG193-0004 | |||
| 3326 | ELG193 | MANAGED-CARE-PLAN-TYPE | Valid values are supplied by the state. | 4/30/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG193-0005 | |||
| 3327 | ELG194 | NATIONAL-HEALTH-CARE-ENTITY-ID | The national identifier of the health care entity (controlling health plan, subhealth plan, or other entity) at the most granular sub-health plan level of the Medicaid or CHIP health plan in which an individual is enrolled. (See 45 CFR 162 Subpart E. http://www.gpo.gov/fdsys/pkg/FR-2012-09-05/pdf/2012-21238.pdf ) | NA | Large health plans are required to obtain national identifiers by November 5, 2014, small health plans by November 5, 2015. States may report prior to these dates if available | 11/3/2015 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG194-0001 | |
| 3328 | ELG194 | NATIONAL-HEALTH-CARE-ENTITY-ID | Covered entities must use the national identifiers in the standard transactions on or after November 7, 2016 | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG194-0002 | |||
| 3329 | ELG194 | NATIONAL-HEALTH-CARE-ENTITY-ID | Value must be equal to a valid value. | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG194-0003 | |||
| 3330 | ELG194 | NATIONAL-HEALTH-CARE-ENTITY-ID | This field is required for all eligible persons enrolled in managed care on or after the mandated dates above. | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG194-0004 | |||
| 3331 | ELG194 | NATIONAL-HEALTH-CARE-ENTITY-ID | Field cannot be spaces if MANAGED-CARE-PLAN-TYPE not = '88' or '99' | 4/30/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG194-0005 | |||
| 3332 | ELG194 | NATIONAL-HEALTH-CARE-ENTITY-ID | If the eligible person is not enrolled in managed care, fill the field with spaces | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG194-0006 | |||
| 3333 | ELG195 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | The NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE distinguishes “controlling” health plan identifiers (CHPIDs), “subhealth” health plan identifiers (SHPIDs), and other entity identifiers (OEIDs) from one another. (See 45 CFR 162 Subpart E. http://www.gpo.gov/fdsys/pkg/FR-2012-09-05/pdf/2012-21238.pdf | NA | Large health plans are required to obtain national identifiers by November 5, 2014, small health plans by November 5, 2015 | 11/3/2015 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG195-0001 | |
| 3334 | ELG195 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | Covered entities must use the national identifiers in the standard transactions on or after November 7, 2016 | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG195-0002 | |||
| 3335 | ELG195 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | Value must be in the set of valid values | 1 Controlling Health Plan (CHP) ID 2 Subhealth Plan (SHP) ID 3 Other Entity Identifier (OEID) |
10/10/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG195-0003 | ||
| 3336 | ELG195 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | If the type HEALTH-CARE-ENTITY-ID-TYPE is unknown, populate the field with a space | 10/10/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG195-0004 | |||
| 3337 | ELG196 | MANAGED-CARE-PLAN-ENROLLMENT-EFF-DATE | The effective date of an individual's enrollment in a managed care plan. Each instance corresponds to a MANAGED-CARE-PLAN-ID This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG196-0001 | |
| 3338 | ELG196 | MANAGED-CARE-PLAN-ENROLLMENT-EFF-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG196-0002 | |||
| 3339 | ELG196 | MANAGED-CARE-PLAN-ENROLLMENT-EFF-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG196-0003 | |||
| 3340 | ELG196 | MANAGED-CARE-PLAN-ENROLLMENT-EFF-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG196-0004 | |||
| 3341 | ELG196 | MANAGED-CARE-PLAN-ENROLLMENT-EFF-DATE | Value must be equal or less than MANAGED-CARE-PLAN-ENROLLMENT-END-DATE | 4/30/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG196-0005 | |||
| 3342 | ELG196 | MANAGED-CARE-PLAN-ENROLLMENT-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG196-0006 | |||
| 3343 | ELG196 | MANAGED-CARE-PLAN-ENROLLMENT-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG196-0007 | |||
| 3344 | ELG197 | MANAGED-CARE-PLAN-ENROLLMENT-END-DATE | The date an individual's enrollment in a managed care plan ends. Each instance corresponds to a MANAGED-CARE-PLAN-ID | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG197-0001 | |
| 3345 | ELG197 | MANAGED-CARE-PLAN-ENROLLMENT-END-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG197-0002 | |||
| 3346 | ELG197 | MANAGED-CARE-PLAN-ENROLLMENT-END-DATE | If not applicable enter all 8s | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG197-0003 | |||
| 3347 | ELG197 | MANAGED-CARE-PLAN-ENROLLMENT-END-DATE | If it is unknown when the person’s enrollment in the managed care plan ends, enter all 9s | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG197-0004 | |||
| 3348 | ELG197 | MANAGED-CARE-PLAN-ENROLLMENT-END-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG197-0005 | |||
| 3349 | ELG197 | MANAGED-CARE-PLAN-ENROLLMENT-END-DATE | Whenever the value in one or more of the data elements on the MANAGED-CARE-PARTICIPATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG197-0006 | |||
| 3350 | ELG197 | MANAGED-CARE-PLAN-ENROLLMENT-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG197-0007 | |||
| 3351 | ELG198 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG198-0001 | |
| 3352 | ELG198 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG198-0002 | |||
| 3353 | ELG199 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | MANAGED-CARE-PARTICIPATION-ELG00014 | ELG199-0001 | |||
| 3354 | ELG200 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG200-0001 | |
| 3355 | ELG200 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG200-0002 | |||
| 3356 | ELG200 | RECORD-ID | Value must be equal to a valid value. | ELG00015 - ETHNICITY-INFORMATION | 10/10/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG200-0003 | ||
| 3357 | ELG200 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG200-0004 | |||
| 3358 | ELG201 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG201-0001 | |
| 3359 | ELG201 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG201-0002 | ||
| 3360 | ELG201 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG201-0003 | |||
| 3361 | ELG202 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG202-0001 | |
| 3362 | ELG202 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG202-0002 | |||
| 3363 | ELG202 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG202-0003 | |||
| 3364 | ELG203 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG203-0001 | |
| 3365 | ELG203 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG203-0002 | |||
| 3366 | ELG203 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG203-0003 | |||
| 3367 | ELG203 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number | 10/10/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG203-0004 | |||
| 3368 | ELG203 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG203-0005 | |||
| 3369 | ELG204 | ETHNICITY-CODE | A code indicating that the individual’s ethnicity is Hispanic, Latino/a, or Spanish. | Conditional | Value must be equal to a valid value. | 0 Not of Hispanic or, Latino/a, or Spanish origin 1 Mexican, Mexican American, Chicano/a 2 Puerto Rican 3 Cuban 4 Another Hispanic, Latino, or Spanish origin 5 Hispanic or Latino Unknown 6 Ethnicity Unspecified 9 Ethnicity Unknown |
11/3/2015 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG204-0001 |
| 3370 | ELG204 | ETHNICITY-CODE | ETHNICITY-CODE clarifications: • If state has beneficiaries coded in their database as “Hispanic” or “Latino,” then code them in T-MSIS as “Hispanic or Latino Unknown” (valid value “5”). DO NOT USE “Another Hispanic, Latino, or Spanish Origin,” “Ethnicity Unknown” or “Ethnicity Unspecified.” NOTE 1: The “Ethnicity Unspecified” category in T-MSIS (valid value “6”) should be used with an individual who explicitly did not provide information or refused to answer a question. NOTE 2: The “Ethnicity Unknown” category in T-MSIS (valid value “9”) should be used when there is no information contained / available in the state database about a person’s race, ethnicity, or other category. |
9/23/2015 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG204-0002 | |||
| 3371 | ELG204 | ETHNICITY-CODE | Use this code to indicate if the eligible’s demographics include an ethnicity of Hispanic or Latino | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG204-0002 | |||
| 3372 | ELG204 | ETHNICITY-CODE | This determination is independent of indication of RACE-CODE. | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG204-0003 | |||
| 3373 | ELG205 | ETHNICITY-DECLARATION-EFF-DATE | The first day of the time span during which the values in all data elements on an ETHNICITY-INFORMATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created.) This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG205-0001 | |
| 3374 | ELG205 | ETHNICITY-DECLARATION-EFF-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG205-0002 | |||
| 3375 | ELG205 | ETHNICITY-DECLARATION-EFF-DATE | If a complete, valid date is not available or is unknown, fill with 99999999 | 4/30/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG205-0003 | |||
| 3376 | ELG205 | ETHNICITY-DECLARATION-EFF-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG205-0004 | |||
| 3377 | ELG205 | ETHNICITY-DECLARATION-EFF-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG205-0005 | |||
| 3378 | ELG205 | ETHNICITY-DECLARATION-EFF-DATE | Value must be equal or less than ETHNICITY-DECLARATION-END-DATE | 4/30/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG205-0006 | |||
| 3379 | ELG205 | ETHNICITY-DECLARATION-EFF-DATE | Whenever the value in one or more of the data elements on the ETHNICITY-INFORMATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG205-0007 | |||
| 3380 | ELG205 | ETHNICITY-DECLARATION-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG205-0008 | |||
| 3381 | ELG205 | ETHNICITY-DECLARATION-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG205-0009 | |||
| 3382 | ELG206 | ETHNICITY-DECLARATION-END-DATE | The last day of the time span during which the values in all data elements on an ETHNICITY-INFORMATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created.) | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG206-0001 | |
| 3383 | ELG206 | ETHNICITY-DECLARATION-END-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG206-0002 | |||
| 3384 | ELG206 | ETHNICITY-DECLARATION-END-DATE | If it is unknown when the person’s enrollment in the managed care plan ends, enter all 9s | 4/30/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG206-0003 | |||
| 3385 | ELG206 | ETHNICITY-DECLARATION-END-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG206-0004 | |||
| 3386 | ELG206 | ETHNICITY-DECLARATION-END-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG206-0005 | |||
| 3387 | ELG206 | ETHNICITY-DECLARATION-END-DATE | If there is no end date (i.e., the record is good into the indefinite future) use the “end-of-time” date (99991231). | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG206-0006 | |||
| 3388 | ELG206 | ETHNICITY-DECLARATION-END-DATE | Whenever the value in one or more of the data elements on the ETHNICITY-INFORMATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG206-0007 | |||
| 3389 | ELG206 | ETHNICITY-DECLARATION-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG206-0008 | |||
| 3390 | ELG207 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG207-0001 | |
| 3391 | ELG207 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG207-0002 | |||
| 3392 | ELG208 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | ETHNICITY-INFORMATION-ELG00015 | ELG208-0001 | |||
| 3393 | ELG209 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG209-0001 | |
| 3394 | ELG209 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG209-0002 | |||
| 3395 | ELG209 | RECORD-ID | Value must be equal to a valid value. | ELG00016 - RACE-INFORMATION | 10/10/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG209-0003 | ||
| 3396 | ELG209 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG209-0004 | |||
| 3397 | ELG210 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG210-0001 | |
| 3398 | ELG210 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG210-0002 | ||
| 3399 | ELG210 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG210-0003 | |||
| 3400 | ELG211 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG211-0001 | |
| 3401 | ELG211 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG211-0002 | |||
| 3402 | ELG211 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG211-0005 | |||
| 3403 | ELG212 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG212-0001 | |
| 3404 | ELG212 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG212-0002 | |||
| 3405 | ELG212 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG212-0003 | |||
| 3406 | ELG212 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number | 10/10/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG212-0004 | |||
| 3407 | ELG212 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG212-0005 | |||
| 3408 | ELG213 | RACE | A code indicating the individual’s race either in accordance with requirements of Section 4302 of the Affordable Care Act classifications | Conditional | Value must be in the set of valid values | 001 White 002 Black or African American 003 American Indian or Alaskan Native 004 Asian Indian 005 Chinese 006 Filipino 007 Japanese 008 Korean 009 Vietnamese 010 Other Asian 011 Asian Unknown 012 Native Hawaiian 013 Guamanian or Chamorro 014 Samoan 015 Other Pacific Islander 016 Native Hawaiian or Other Pacific Islander Unknown 017 Unspecifed 999 Unknown |
11/3/2015 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG213-0001 |
| 3409 | ELG213 | RACE | RACE code clarifications: • If state has beneficiaries coded in their database as "Asian” with no additional detail, then code them in T-MSIS as “Asian Unknown” (valid value “011”). DO NOT USE “Other Asian,” “Unspecified” or “Unknown.” • If state has beneficiaries coded in their database as “Native Hawaiian or Other Pacific Islander” with no additional detail, then code them in T-MSIS as “Native Hawaiian and Other Pacific Islander Unknown” (valid value “016”). DO NOT USE “Native Hawaiian,” “Other Pacific Islander,” “Unspecified” or “Unknown.” NOTE 1: The “Other Asian” category in T-MSIS (valid value “010”) should be used in situations in which an individual’s specific Asian subgroup is not available in the code set provided (e.g., Malaysian, Burmese). NOTE 2: The “Unspecified” category in T-MSIS (valid value “017”) should be used with an individual who explicitly did not provide information or refused to answer a question. NOTE 3: The “Unknown” category in T-MSIS (valid value “999”) should be used when there is no information contained / available in the state database about a person’s race, ethnicity, or other category. |
9/23/2015 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG213-0002 | |||
| 3410 | ELG214 | RACE-OTHER | A freeform field to document the race of the beneficiary when the beneficiary identifies themselves as Other Asian, Other Pacific Islander (race codes 010 or 015). | Conditional | Use this field only if the RACE is reported as Other Asian (race code 010) or Other Pacific Islander (race code 015). | 11/3/2015 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG214-0001 | |
| 3411 | ELG214 | RACE-OTHER | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. |
4/30/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG214-0002 | |||
| 3412 | ELG215 | CERTIFIED-AMERICAN-INDIAN-ALASKAN-NATIVE-INDICATOR | Indicates that the individual is an American Indian or Alaskan Native whose race status is certified and therefore the state is eligible to receive 100% FFP. To be considered a certified American Indian or Alaskan Native, the individual has completed the Bureau of Indian Affairs certificate process and has received the Certificate of Degree of Indian or Alaska Native Blood (CDIB). |
Conditional | Value must be equal to a valid value. | 0 Not applicable 1 No, Individual does not have CDIB 2 Yes, Individual does have CDIB 9 Applicable but unknown |
11/3/2015 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG215-0001 |
| 3413 | ELG216 | RACE-DECLARATION-EFF-DATE | The first day of the time span during which the values in all data elements on a RACE-INFORMATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG216-0001 | |
| 3414 | ELG216 | RACE-DECLARATION-EFF-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG216-0002 | |||
| 3415 | ELG216 | RACE-DECLARATION-EFF-DATE | If a complete, valid date is not available or is unknown, fill with 99999999 | 4/30/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG216-0003 | |||
| 3416 | ELG216 | RACE-DECLARATION-EFF-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG216-0004 | |||
| 3417 | ELG216 | RACE-DECLARATION-EFF-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG216-0005 | |||
| 3418 | ELG216 | RACE-DECLARATION-EFF-DATE | Value must be equal or less than RACE-DECLARATION-END-DATE | 4/30/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG216-0006 | |||
| 3419 | ELG216 | RACE-DECLARATION-EFF-DATE | Whenever the value in one or more of the data elements on the RACE-INFORMATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG216-0007 | |||
| 3420 | ELG216 | RACE-DECLARATION-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG216-0008 | |||
| 3421 | ELG216 | RACE-DECLARATION-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG216-0009 | |||
| 3422 | ELG217 | RACE-DECLARATION-END-DATE | The last day of the time span during which the values in all data elements on a RACE-INFORMATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG217-0001 | |
| 3423 | ELG217 | RACE-DECLARATION-END-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG217-0002 | |||
| 3424 | ELG217 | RACE-DECLARATION-END-DATE | If a complete, valid date is not available or is unknown, fill with 99999999 | 4/30/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG217-0003 | |||
| 3425 | ELG217 | RACE-DECLARATION-END-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG217-0004 | |||
| 3426 | ELG217 | RACE-DECLARATION-END-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG217-0005 | |||
| 3427 | ELG217 | RACE-DECLARATION-END-DATE | If there is no end date (i.e., the record is good into the indefinite future) use the “end-of-time” date (99991231) | 2/25/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG217-0006 | |||
| 3428 | ELG217 | RACE-DECLARATION-END-DATE | Whenever the value in one or more of the data elements on the RACE-INFORMATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG217-0007 | |||
| 3429 | ELG217 | RACE-DECLARATION-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG217-0008 | |||
| 3430 | ELG218 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG218-0001 | |
| 3431 | ELG218 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG218-0002 | |||
| 3432 | ELG219 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | RACE-INFORMATION-ELG00016 | ELG219-0001 | |||
| 3433 | ELG220 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG220-0001 | |
| 3434 | ELG220 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG220-0002 | |||
| 3435 | ELG220 | RECORD-ID | Value must be equal to a valid value. | ELG00017 - DISABILITY-INFORMATION | 10/10/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG220-0003 | ||
| 3436 | ELG220 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG220-0004 | |||
| 3437 | ELG221 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG221-0001 | |
| 3438 | ELG221 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG221-0002 | ||
| 3439 | ELG221 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG221-0003 | |||
| 3440 | ELG222 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG222-0001 | |
| 3441 | ELG222 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG222-0002 | |||
| 3442 | ELG222 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG222-0003 | |||
| 3443 | ELG223 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG223-0001 | |
| 3444 | ELG223 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG223-0002 | |||
| 3445 | ELG223 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG223-0003 | |||
| 3446 | ELG223 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number | 10/10/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG223-0004 | |||
| 3447 | ELG223 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG223-0005 | |||
| 3448 | ELG224 | DISABILITY-TYPE-CODE | A code to identify disability status in accordance with requirements of Section 4302 of the Affordable Care Act. | Conditional | Must be populated on every record | 11/3/2015 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG224-0001 | |
| 3449 | ELG224 | DISABILITY-TYPE-CODE | Value must be equal to a valid value. | 01 Individual is deaf or has serious difficulty hearing. 02 Individual is blind or has serious difficulty seeing, even when wearing glasses. 03 Individual has serious difficulty concentrating, remembering, or making decisions because of a physical, mental, or emotional condition. (Applicable only to people who are 5 years old or older.) 04 Individual has serious difficulty walking or climbing stairs. (Applicable only to people who are 5 years old or older.) 05 Individual has difficulty dressing or bathing. (Applicable only to people who are 5 years old or older.) 06 Individual has difficulty doing errands alone such as visiting a doctor's office or shopping because of a physical, mental, or emotional condition. (Applicable only to people who are 15 years old or older.) 07 Other 08 None 99 Unknown |
4/30/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG224-0002 | ||
| 3450 | ELG224 | DISABILITY-TYPE-CODE | Report all that apply. | 2/25/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG224-0003 | |||
| 3451 | ELG225 | DISABILITY-TYPE-EFF-DATE | The first day of the time span during which the values in all data elements on a DISABILITY-INFORMATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG225-0001 | |
| 3452 | ELG225 | DISABILITY-TYPE-EFF-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG225-0002 | |||
| 3453 | ELG225 | DISABILITY-TYPE-EFF-DATE | If a complete, valid date is not available or is unknown, fill with 99999999 | 4/30/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG225-0003 | |||
| 3454 | ELG225 | DISABILITY-TYPE-EFF-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG225-0004 | |||
| 3455 | ELG225 | DISABILITY-TYPE-EFF-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG225-0005 | |||
| 3456 | ELG225 | DISABILITY-TYPE-EFF-DATE | Value must be equal or less than DISABILITY-TYPE-END-DATE | 4/30/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG225-0006 | |||
| 3457 | ELG225 | DISABILITY-TYPE-EFF-DATE | Whenever the value in one or more of the data elements on the DISABILITY-INFORMATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG225-0007 | |||
| 3458 | ELG225 | DISABILITY-TYPE-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG225-0008 | |||
| 3459 | ELG225 | DISABILITY-TYPE-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG225-0009 | |||
| 3460 | ELG226 | DISABILITY-TYPE-END-DATE | The last day of the time span during which the values in all data elements on a DISABILITY-INFORMATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created.) | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG226-0001 | |
| 3461 | ELG226 | DISABILITY-TYPE-END-DATE | If not applicable enter all 8s | 4/30/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG226-0002 | |||
| 3462 | ELG226 | DISABILITY-TYPE-END-DATE | If a complete, valid date is not available or is unknown, fill with 99999999 | 4/30/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG226-0003 | |||
| 3463 | ELG226 | DISABILITY-TYPE-END-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG226-0004 | |||
| 3464 | ELG226 | DISABILITY-TYPE-END-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG226-0005 | |||
| 3465 | ELG226 | DISABILITY-TYPE-END-DATE | If there is no end date (i.e., the record is good into the indefinite future) use the “end-of-time” date (99991231) | 2/25/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG226-0006 | |||
| 3466 | ELG226 | DISABILITY-TYPE-END-DATE | Whenever the value in one or more of the data elements on the DISABILITY-INFORMATION record segment changes, a new record segment must be created | 2/25/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG226-0007 | |||
| 3467 | ELG226 | DISABILITY-TYPE-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG226-0008 | |||
| 3468 | ELG227 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG227-0001 | |
| 3469 | ELG227 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG227-0002 | |||
| 3470 | ELG228 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | DISABILITY-INFORMATION-ELG00017 | ELG228-0001 | |||
| 3471 | ELG229 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG229-0001 | |
| 3472 | ELG229 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG229-0002 | |||
| 3473 | ELG229 | RECORD-ID | Value must be equal to a valid value. | ELG00018 - 1115A-DEMONSTRATION-INFORMATION | 10/10/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG229-0003 | ||
| 3474 | ELG229 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG229-0004 | |||
| 3475 | ELG230 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG230-0001 | |
| 3476 | ELG230 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG230-0002 | ||
| 3477 | ELG230 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG230-0003 | |||
| 3478 | ELG231 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG231-0001 | |
| 3479 | ELG231 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG231-0002 | |||
| 3480 | ELG231 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG231-0003 | |||
| 3481 | ELG232 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG232-0001 | |
| 3482 | ELG232 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG232-0002 | |||
| 3483 | ELG232 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG232-0003 | |||
| 3484 | ELG232 | MSIS-IDENTIFICATION-NUM | For SSN states, this field, as well as the SSN field should be populated with the eligible person’s social security number | 2/25/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG232-0004 | |||
| 3485 | ELG232 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG232-0005 | |||
| 3486 | ELG233 | 1115A-DEMONSTRATION-IND | Indicates that the individual participates in an 1115(A) demonstration. 1115(A) is a Center for Medicare and Medicaid Innovation (CMMI) demonstration. | Conditional | Field is required on all records | 11/3/2015 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG233-0001 | |
| 3487 | ELG233 | 1115A-DEMONSTRATION-IND | Value must be equal to a valid value. | 0 No 1 Yes |
4/30/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG233-0002 | ||
| 3488 | ELG233 | 1115A-DEMONSTRATION-IND | If an individual is not participating in an 1115A demonstration, then 1115A effective date should be designated as not applicable. | 2/25/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG233-0003 | |||
| 3489 | ELG234 | 1115A-EFF-DATE | The date on which the individual’s participation in 1115A demonstration began. 1115(A) is a Center for Medicare and Medicaid Innovation demonstration. This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG234-0001 | |
| 3490 | ELG234 | 1115A-EFF-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG234-0002 | |||
| 3491 | ELG234 | 1115A-EFF-DATE | If individual is NOT enrolled in a CMMI 1115A, the field should be 8-filled | 4/30/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG234-0003 | |||
| 3492 | ELG234 | 1115A-EFF-DATE | If a complete, valid date is not available or is unknown, fill with 99999999 | 4/30/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG234-0004 | |||
| 3493 | ELG234 | 1115A-EFF-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG234-0005 | |||
| 3494 | ELG234 | 1115A-EFF-DATE | Value must be equal or less than 1115A-END-DATE | 10/10/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG234-0006 | |||
| 3495 | ELG234 | 1115A-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG234-0007 | |||
| 3496 | ELG234 | 1115A-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG234-0008 | |||
| 3497 | ELG235 | 1115A-END-DATE | The date on which the individual’s participation in 1115A demonstration ended. | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG235-0001 | |
| 3498 | ELG235 | 1115A-END-DATE | The date must be a valid date | 4/30/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG235-0002 | |||
| 3499 | ELG235 | 1115A-END-DATE | If individual is NOT enrolled in CHIP, the field should be 8-filled | 2/25/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG235-0003 | |||
| 3500 | ELG235 | 1115A-END-DATE | If a complete, valid date is not available or is unknown, fill with 99999999 | 4/30/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG235-0004 | |||
| 3501 | ELG235 | 1115A-END-DATE | The value must consist of digits 0 through 9 only | 4/30/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG235-0005 | |||
| 3502 | ELG235 | 1115A-END-DATE | The field should be populated with the “end-of-time” date (i.e., 99991231) for individuals who are currently enrolled | 2/25/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG235-0006 | |||
| 3503 | ELG235 | 1115A-END-DATE | Whenever the value in one or more of the data elements on the 1115A-DEMONSTRATION record segment changes, a new record segment must be created | 10/10/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG235-0007 | |||
| 3504 | ELG235 | 1115A-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG235-0008 | |||
| 3505 | ELG236 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG236-0001 | |
| 3506 | ELG236 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG236-0002 | |||
| 3507 | ELG237 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | 1115A-DEMONSTRATION-INFORMATION-ELG00018 | ELG237-0001 | |||
| 3508 | ELG238 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 4/30/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG238-0001 | |
| 3509 | ELG238 | RECORD-ID | Value must be in required format | 4/30/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG238-0002 | |||
| 3510 | ELG238 | RECORD-ID | Value must be equal to a valid value. | ELG00020 - HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME | 10/10/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG238-0003 | ||
| 3511 | ELG238 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG238-0004 | |||
| 3512 | ELG239 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG239-0001 | |
| 3513 | ELG239 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG239-0002 | ||
| 3514 | ELG239 | SUBMITTING-STATE | Value must be the same on all record segments | 4/30/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG239-0003 | |||
| 3515 | ELG240 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG240-0001 | |
| 3516 | ELG240 | RECORD-NUMBER | Must be populated on every record | 4/30/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG240-0002 | |||
| 3517 | ELG240 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 2/25/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG240-0003 | |||
| 3518 | ELG241 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 2/25/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG241-0001 | |
| 3519 | ELG241 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 2/25/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG241-0002 | |||
| 3520 | ELG241 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 2/25/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG241-0003 | |||
| 3521 | ELG241 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number | 10/10/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG241-0004 | |||
| 3522 | ELG241 | MSIS-IDENTIFICATION-NUM | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG241-0005 | |||
| 3523 | ELG242 | HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-CODE | The chronic condition for which the eligible person is receiving non-Health-Home home and community based care. | Conditional | Value must be equal to a valid value. | 001 Aged 002 Physical Disabilities 003 Intellectual Disabilities 004 Autism Spectrum Disorder 005 Developmental Disabilities 006 Mental Illness and/or Serious Emotional Disturbance 007 Brain Injury 008 HIV/AIDS 009 Technology Dependent or Medically Fragile 010 Disabled (other) |
11/3/2015 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG242-0001 |
| 3524 | ELG243 | HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-EFF-DATE | The date that the state considers to be the onset date for the eligible person to have the chronic condition. This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG243-0001 | |
| 3525 | ELG243 | HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-EFF-DATE | Value must be a valid date. | 2/25/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG243-0002 | |||
| 3526 | ELG243 | HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-EFF-DATE | Overlapping coverage not allowed for same file segment | 10/10/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG243-0003 | |||
| 3527 | ELG243 | HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-EFF-DATE | For parent and child file segments, the effective date of a child record segment must occur before or be concurrent with the effective date of the parent file segment, where submitting state and file segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG243-0004 | |||
| 3528 | ELG244 | HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-END-DATE | The last date on which the state considers the eligible person to have the chronic condition. | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG244-0001 | |
| 3529 | ELG244 | HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-END-DATE | The date must be a valid date | 2/25/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG244-0002 | |||
| 3530 | ELG244 | HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-END-DATE | For parent and child file segments, the end date of a child record segment must occur before or be concurrent with the end date of the parent record segment, where submitting state and record segment-specific identifying number match one another in both record segments. | 10/10/2013 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG244-0003 | |||
| 3531 | ELG245 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG245-0001 | |
| 3532 | ELG245 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG245-0002 | |||
| 3533 | ELG246 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 | ELG246-0001 | |||
| 3534 | ELG248 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Value is required on all record segments | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG248-0001 | |
| 3535 | ELG248 | RECORD-ID | Value must be in required format | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG248-0002 | |||
| 3536 | ELG248 | RECORD-ID | Value must be equal to a valid value. | ELG00021 - ENROLLMENT-TIME-SPAN | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG248-0003 | ||
| 3537 | ELG249 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG249-0001 |
| 3538 | ELG249 | SUBMITTING-STATE | Must be populated on every record. | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG249-0002 | |||
| 3539 | ELG249 | SUBMITTING-STATE | Value must be numeric |
10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG249-0003 | |||
| 3540 | ELG249 | SUBMITTING-STATE | SUBMITTING-STATE must be equal across all record segments for a given record. | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG249-0004 | |||
| 3541 | ELG250 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG250-0001 | |
| 3542 | ELG250 | RECORD-NUMBER | Must be numeric | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG250-0002 | |||
| 3543 | ELG250 | RECORD-NUMBER | Duplicate record number should not exist with in same file | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG250-0003 | |||
| 3544 | ELG250 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG250-0004 | |||
| 3545 | ELG251 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | MSIS Identification Number must be reported | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG251-0001 | |
| 3546 | ELG251 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the state MSIS-ID numbers must be supplied to CMS with the state's MSIS application | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG251-0002 | |||
| 3547 | ELG251 | MSIS-IDENTIFICATION-NUM | In instances where the social security number is not known and a temporary MSIS identification number is used, the MSIS-IDENTIFICATION-NUM field should be populated with the temporary MSIS identification number and the SSN field should be space-filled. When the social security number becomes known, the MSIS-IDENTIFICATION-NUM field should continue to be populated with the temporary MSIS identification number and the SSN field should be populated with the newly acquired social security number for at least one monthly submission of the Eligibility File so that T-MSIS can associated the temporary MSIS identification number and the social security number | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG251-0003 | |||
| 3548 | ELG251 | MSIS-IDENTIFICATION-NUM | For SSN states, the MSIS Identifier and SSN fields should be populated with the eligible person’s social security number. | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG251-0004 | |||
| 3549 | ELG251 | MSIS-IDENTIFICATION-NUM | A child record must have a parent record. | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG251-0005 | |||
| 3550 | ELG252 | ENROLLMENT-TYPE | Identify the type of enrollment that the eligible person has been enrolled into as either Medicaid or CHIP.. | Required | Value must be equal to a valid value. | 1 Medicaid 2 CHIP 9 Unknown |
10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG252-0001 |
| 3551 | ELG252 | ENROLLMENT-TYPE | This data element must be completed for every individual enrolled in the State's Medicaid or CHIP program. | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG252-0002 | |||
| 3552 | ELG253 | ENROLLMENT-EFF-DATE | The first day of enrollment for the ENROLLMENT-TYPE and MSIS-IDENTIFICATION-NUM being reported in the ENROLLMENT-TIME-SPAN-SEGMENT record segment. This date field is necessary when defining a unique row in a database table. |
Required | The date must be in “ccyymmdd” format. | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG253-0001 | |
| 3553 | ELG253 | ENROLLMENT-EFF-DATE | The value must consist of digits 0 through 9 only | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG253-0002 | |||
| 3554 | ELG253 | ENROLLMENT-EFF-DATE | Value must be a valid date | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG253-0003 | |||
| 3555 | ELG253 | ENROLLMENT-EFF-DATE | Whenever the value in one or more of the data elements in the ENROLLMENT-TIME-SPAN-SEGMENT record segment changes, a new record segment must be created. | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG253-0004 | |||
| 3556 | ELG253 | ENROLLMENT-EFF-DATE | Date cannot be greater than ENROLLMENT-END-DATE. | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG253-0005 | |||
| 3557 | ELG254 | ENROLLMENT-END-DATE | The last day of enrollment for the ENROLLMENT-TYPE and MSIS-IDENTIFICATION-NUM being reported in the ENROLLMENT-TIME-SPAN-SEGMENT record segment. | Required | The date must be in “ccyymmdd” format. | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG254-0001 | |
| 3558 | ELG254 | ENROLLMENT-END-DATE | The value must consist of digits 0 through 9 only | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG254-0002 | |||
| 3559 | ELG254 | ENROLLMENT-END-DATE | Value must be a valid date | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG254-0003 | |||
| 3560 | ELG254 | ENROLLMENT-END-DATE | Whenever the value in one or more of the data elements in the ENROLLMENT-TIME-SPAN-SEGMENT record segment changes, a new record segment must be created. | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG254-0004 | |||
| 3561 | ELG255 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses | Optional | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. |
10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG255-0001 | |
| 3562 | ELG255 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG255-0002 | |||
| 3563 | ELG256 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG256-0001 | |||
| 3564 | ELG248 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | ELIGIBLE | ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 | ELG248-0004 | |||
| 3565 | MCR001 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR001-0001 | |
| 3566 | MCR001 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR001-0002 | |||
| 3567 | MCR001 | RECORD-ID | Value must be in the set of valid values | MCR00001 - FILE-HEADER-RECORD-MANAGED-CARE | 10/10/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR001-0003 | ||
| 3568 | MCR001 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR001-0004 | |||
| 3569 | MCR002 | DATA-DICTIONARY-VERSION | A data element to capture the version of the T-MSIS data dictionary that was used to build the file. | Required | Use the version number specified on the title page of the data dictionary. | 2/25/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR002-0001 | |
| 3570 | MCR003 | SUBMISSION-TRANSACTION-TYPE | A data element to identify the whether the transactions in the file are original submissions of the data, a resubmission of a previously submitted file, or corrections of edit rejects. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR003-0001 | |
| 3571 | MCR003 | SUBMISSION-TRANSACTION-TYPE | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 10/10/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR003-0002 | ||
| 3572 | MCR004 | FILE-ENCODING-SPECIFICATION | A data element to denote whether the file is in fixed length line format or delimited format. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR004-0001 | |
| 3573 | MCR004 | FILE-ENCODING-SPECIFICATION | Value must be equal to a valid value. | FLF - The file follows a fixed length format. PSV - The file follows a pipe-delimited format. |
10/10/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR004-0002 | ||
| 3574 | MCR005 | DATA-MAPPING-DOCUMENT-VERSION | A data element to identify the version of the T-MSIS data mapping document used to build the file. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR005-0001 | |
| 3575 | MCR005 | DATA-MAPPING-DOCUMENT-VERSION | Use the version number specified on the title page of the data mapping document | 2/25/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR005-0002 | |||
| 3576 | MCR006 | FILE-NAME | The name identifying the subject area to which the records in its file relate. Each T-MSIS submission file should only contain records for one subject area (i.e., Eligible, Third-party Liability, Provider, Managed Care Plan Information, IP claims, LT claims, Rx claims, or OT claims). | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR006-0001 | |
| 3577 | MCR006 | FILE-NAME | Value must be equal to a valid value. | MNGDCARE Managed Care Plan Information file | 10/10/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR006-0002 | ||
| 3578 | MCR007 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR007-0001 | |
| 3579 | MCR007 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR007-0002 | ||
| 3580 | MCR007 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR007-0003 | |||
| 3581 | MCR008 | DATE-FILE-CREATED | The date on which the file was created. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR008-0001 | |
| 3582 | MCR008 | DATE-FILE-CREATED | Date must be a valid date | 2/25/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR008-0002 | |||
| 3583 | MCR008 | DATE-FILE-CREATED | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR008-0003 | |||
| 3584 | MCR008 | DATE-FILE-CREATED | Date must be equal to or greater than the date entered in the START-OF-TIME-PERIOD field | 2/25/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR008-0004 | |||
| 3585 | MCR008 | DATE-FILE-CREATED | Date must be less than or equal to current date | 10/10/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR008-0005 | |||
| 3586 | MCR009 | START-OF-TIME-PERIOD | Beginning date of the Month covered by this file. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR009-0001 | |
| 3587 | MCR009 | START-OF-TIME-PERIOD | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR009-0002 | |||
| 3588 | MCR009 | START-OF-TIME-PERIOD | Date must be valid Date | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR009-0003 | |||
| 3589 | MCR009 | START-OF-TIME-PERIOD | Value in DD must equal 01. | 2/25/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR009-0004 | |||
| 3590 | MCR009 | START-OF-TIME-PERIOD | Date must be less then current date | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR009-0005 | |||
| 3591 | MCR009 | START-OF-TIME-PERIOD | Date must be equal to or less than the date in the DATE-FILE-CREATED field. | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR009-0006 | |||
| 3592 | MCR009 | START-OF-TIME-PERIOD | Value must be a valid date based on the calendar year | 2/25/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR009-0007 | |||
| 3593 | MCR010 | END-OF-TIME-PERIOD | Last date of the reporting period covered by the file to which this Header Record is attached. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR010-0001 | |
| 3594 | MCR010 | END-OF-TIME-PERIOD | Date must be valid Date | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR010-0002 | |||
| 3595 | MCR010 | END-OF-TIME-PERIOD | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR010-0003 | |||
| 3596 | MCR010 | END-OF-TIME-PERIOD | Value in DD (must be 30 when the MM=04, 06, 09, 11) OR (must be 31 when the MM=01, 03, 05, 07, 08, 10, 12) OR (must be 28 or 29 when the MM=02) | 2/25/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR010-0004 | |||
| 3597 | MCR010 | END-OF-TIME-PERIOD | Date must be less then current date | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR010-0005 | |||
| 3598 | MCR010 | END-OF-TIME-PERIOD | Value must be equal to or greater than START-OF-TIME-PERIOD. | 2/25/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR010-0006 | |||
| 3599 | MCR010 | END-OF-TIME-PERIOD | Value must be a valid date based on the calendar year | 2/25/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR010-0007 | |||
| 3600 | MCR011 | FILE-STATUS-INDICATOR | A code to indicate whether the records in the file are test or production records. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR011-0001 | |
| 3601 | MCR011 | FILE-STATUS-INDICATOR | Value must be equal to a valid value. | P Production File T Test File |
10/10/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR011-0002 | ||
| 3602 | MCR013 | TOT-REC-CNT | A count of all records in the file except for the file header record. This count will be used as a control total to help assure that the file did not become corrupted during transmission. | Required | An integer value with no commas. | 10/10/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR013-0001 | |
| 3603 | MCR013 | TOT-REC-CNT | Value must equal the sum of all records excluding the header record | 4/30/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR013-0002 | |||
| 3604 | MCR112 | SEQUENCE-NUMBER | To enable state’s to sequentially number files, when related, follow-on files are necessary (i.e., update files, replacement files). This should begin with 1 for the original Create submission type and be incremented by one for each Replacement or Update submission for the same reporting period and file type (subject area). | Required | Field is required on all 'C', 'U', and 'R' record files. | 10/10/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR112-0001 | |
| 3605 | MCR112 | SEQUENCE-NUMBER | Must be numeric and > 0 | 10/10/2013 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR112-0002 | |||
| 3606 | MCR014 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR014-0001 | |
| 3607 | MCR014 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR014-0002 | |||
| 3608 | MCR012 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | MNGDCARE | FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 | MCR012-0001 | |||
| 3609 | MCR016 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR016-0001 | |
| 3610 | MCR016 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR016-0002 | |||
| 3611 | MCR016 | RECORD-ID | Value must be in the set of valid values | MCR00002 - MANAGED-CARE-MAIN | 10/10/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR016-0003 | ||
| 3612 | MCR016 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR016-0004 | |||
| 3613 | MCR017 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR017-0001 | |
| 3614 | MCR017 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR017-0002 | ||
| 3615 | MCR017 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR017-0003 | |||
| 3616 | MCR017 | SUBMITTING-STATE | Value must be the same as Header Record in all records | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR017-0004 | |||
| 3617 | MCR018 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 10/10/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR018-0001 | |
| 3618 | MCR018 | RECORD-NUMBER | Must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR018-0002 | |||
| 3619 | MCR018 | RECORD-NUMBER | Duplicate record number should not exist with in same file | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR018-0003 | |||
| 3620 | MCR019 | STATE-PLAN-ID-NUM | Contains the ID number the state issued to the managed care entity. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR019-0001 | |
| 3621 | MCR019 | STATE-PLAN-ID-NUM | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR019-0002 | |||
| 3622 | MCR019 | STATE-PLAN-ID-NUM | Fill in the PLAN-ID-NUM depending on the value selected for the associated PLAN-ID-NUM-INDICATOR. | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR019-0003 | |||
| 3623 | MCR019 | STATE-PLAN-ID-NUM | If the National Health Plan Identifier is available, please enter the number in this field and the NATIONAL-HEALTH-CARE-ENTITY-ID field. If not available, please enter the state’s internal plan ID. Please fill in the PLAN-ID-NUM depending on the value selected for the associated PLAN-ID-NUM-INDICATOR. | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR019-0004 | |||
| 3624 | MCR020 | MANAGED-CARE-CONTRACT-EFF-DATE | The start date of the managed care contract period with the state. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR020-0001 | |
| 3625 | MCR020 | MANAGED-CARE-CONTRACT-EFF-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR020-0002 | |||
| 3626 | MCR020 | MANAGED-CARE-CONTRACT-EFF-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR020-0003 | |||
| 3627 | MCR020 | MANAGED-CARE-CONTRACT-EFF-DATE | Date must be less then current date | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR020-0004 | |||
| 3628 | MCR021 | MANAGED-CARE-CONTRACT-END-DATE | The expiration date of the managed care contract period with the state. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR021-0001 | |
| 3629 | MCR021 | MANAGED-CARE-CONTRACT-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR021-0002 | |||
| 3630 | MCR021 | MANAGED-CARE-CONTRACT-END-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR021-0003 | |||
| 3631 | MCR021 | MANAGED-CARE-CONTRACT-END-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR021-0004 | |||
| 3632 | MCR021 | MANAGED-CARE-CONTRACT-END-DATE | Date must be equal to or greater than MANAGED-CARE-CONTRACT-EFF-DATE | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR021-0005 | |||
| 3633 | MCR022 | MANAGED-CARE-NAME | The name of the managed care entity under contract with the State Medicaid Agency. The name should be as it appears on the contract. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR022-0001 | |
| 3634 | MCR022 | MANAGED-CARE-NAME | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR022-0002 | |||
| 3635 | MCR023 | MANAGED-CARE-PROGRAM | The state program through which a managed care plan is approved to operate. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR023-0001 | |
| 3636 | MCR023 | MANAGED-CARE-PROGRAM | Value must be equal to a valid value. | 1 Medicaid State Plan 2 CHIP State Plan 3 Both Medicaid and CHIP |
10/10/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR023-0002 | ||
| 3637 | MCR024 | MANAGED-CARE-PLAN-TYPE | The type of managed care plan that corresponds to the MANAGED-CARE-PLAN-ID. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR024-0001 | |
| 3638 | MCR024 | MANAGED-CARE-PLAN-TYPE | Value is not included in the valid code list | See Appendix A for listing of valid values. | 10/10/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR024-0002 | ||
| 3639 | MCR024 | MANAGED-CARE-PLAN-TYPE | Left fill with zeros if number is less than 2 bytes long. | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR024-0003 | |||
| 3640 | MCR025 | REIMBURSEMENT-ARRANGEMENT | A code indicating the how the managed care entity is reimbursed. | Required | Must be populated on every record | 10/10/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR025-0001 | |
| 3641 | MCR025 | REIMBURSEMENT-ARRANGEMENT | Value must be equal to a valid value. | 01 Risk-based Capitation, no incentives or risk-sharing 02 Risk-based Capitation with Incentive Arrangements 03 Risk-based Capitation with other risk-sharing Arrangements 04 Non-Risk Capitation 05 Fee-For-Service 06 Primary Care Case Management Payment 07 Other 08 Primary Care Case Management Payment plus Fee-For-Service 88 Not Applicable 99 Unknown |
10/10/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR025-0002 | ||
| 3642 | MCR025 | REIMBURSEMENT-ARRANGEMENT | See Appendix A for definitions of T-MSIS coding categories. | 10/10/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR025-0003 | |||
| 3643 | MCR026 | MANAGED-CARE-PROFIT-STATUS | A code denoting the profit status of managed care entity. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR026-0001 | |
| 3644 | MCR026 | MANAGED-CARE-PROFIT-STATUS | Value must be equal to a valid value. | 01 501(C)(3) NON-PROFIT 02 FOR-PROFIT, CLOSELY HELD 03 FOR-PROFIT, PUBLICLY TRADED 04 OTHER 99 Unknown |
4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR026-0002 | ||
| 3645 | MCR026 | MANAGED-CARE-PROFIT-STATUS | Left fill with zeros if number is less than 2 bytes long. | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR026-0003 | |||
| 3646 | MCR027 | CORE-BASED-STATISTICAL-AREA-CODE | A code signifying whether the MCO’s service area falls into one or more metropolitan or micropolitan statistical areas. Metropolitan and micropolitan statistical areas (metro and micro areas) are geographic entities defined by the U.S. Office of Management and Budget (OMB). The term "Core Based Statistical Area" (CBSA) is a collective term for both metro and micro areas. A metro area contains a core urban area of 50,000 or more population, and a micro area contains an urban core of at least 10,000 (but less than 50,000) population. Each metro or micro area consists of one or more counties and includes the counties containing the core urban area, as well as any adjacent counties that have a high degree of social and economic integration (as measured by commuting to work) with the urban core. The U.S. Office of Management and Budget (OMB) defines metropolitan or micropolitan statistical areas based on published standards. The standards for defining the areas are reviewed and revised once every ten years, prior to each decennial census. Between censuses, the definitions are updated annually to reflect the most recent Census Bureau population estimates. The current definitions are as of December 2009. See the hyperlink below for further information. http://www.whitehouse.gov/sites/default/files/omb/assets/bulletins/b10-02.pdf | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR027-0001 | |
| 3647 | MCR027 | CORE-BASED-STATISTICAL-AREA-CODE | Value is not included in the valid code list | 1 = The MCO’s service area falls partially or entirely inside one or more metropolitan areas. 2 = The MCO’s service area falls partially or entirely inside one or more micropolitan areas, but not within any metropolitan areas. 3 = The MCO’s service area falls entirely outside of all metropolitan and micropolitan areas. |
10/10/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR027-0002 | ||
| 3648 | MCR027 | CORE-BASED-STATISTICAL-AREA-CODE | Whenever a service area straddles two types of areas (e.g., metropolitan & micropolitan, metropolitan & non-CBSA area) classify the service area based on the denser classification. | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR027-0003 | |||
| 3649 | MCR028 | PERCENT-BUSINESS | The percentage of the managed care entity’s total revenue that is derived from contracts with Medicare (Part C and D) in the state and State Medicaid agency contract(s) prior calendar year. Include Medicaid and Medicare in calculation of percentage of business in public programs for IRS health insurer tax exemption as required in ACA. | Required | Please enter a percent of zero through 100. | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR028-0001 | |
| 3650 | MCR028 | PERCENT-BUSINESS | Must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR028-0002 | |||
| 3651 | MCR029 | MANAGED-CARE-SERVICE-AREA | The area under which the managed care entity is under contract to provide services. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR029-0001 | |
| 3652 | MCR029 | MANAGED-CARE-SERVICE-AREA | Value must be equal to a valid value. | 1 Statewide – The managed care entity provides services to beneficiaries throughout the entire state. 2 County – The managed care entity provides services to beneficiaries in specified counties. 3 City – The managed care entity provides services to beneficiaries in specified cities. 4 Region – The managed care entity provides services to beneficiaries in specified regions, not defined by individual counties within the state (“region” is state-defined). 5 Zip Code – The managed care entity program provides services to beneficiaries in specified zip codes. 6 Other – The managed care entity provides services to beneficiaries in "other" area(s), not Statewide, County, City, or Region. |
10/10/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR029-0002 | ||
| 3653 | MCR030 | MANAGED-CARE-MAIN-REC-EFF-DATE | The first day of the time span during which the values in all data elements in the MANAGED-CARE-MAIN record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR030-0001 | |
| 3654 | MCR030 | MANAGED-CARE-MAIN-REC-EFF-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR030-0002 | |||
| 3655 | MCR030 | MANAGED-CARE-MAIN-REC-EFF-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR030-0003 | |||
| 3656 | MCR030 | MANAGED-CARE-MAIN-REC-EFF-DATE | Date must be equal to or less than MANAGED-CARE-MAIN-REC-END-DATE | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR030-0004 | |||
| 3657 | MCR031 | MANAGED-CARE-MAIN-REC-END-DATE | The last day of the time span during which the values in all data elements in the MANAGED-CARE-MAIN record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR031-0001 | |
| 3658 | MCR031 | MANAGED-CARE-MAIN-REC-END-DATE | The date must be in “ccyymmdd” format. | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR031-0002 | |||
| 3659 | MCR031 | MANAGED-CARE-MAIN-REC-END-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR031-0003 | |||
| 3660 | MCR031 | MANAGED-CARE-MAIN-REC-END-DATE | Date must be equal to or greater than MANAGED-CARE-MAIN-REC-EFF-DATE | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR031-0004 | |||
| 3661 | MCR031 | MANAGED-CARE-MAIN-REC-END-DATE | Overlapping coverage not allowed for same Submitting state & Plan ID | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR031-0005 | |||
| 3662 | MCR031 | MANAGED-CARE-MAIN-REC-END-DATE | Managed Care coverage dates must be within Managed Care Contract Date | 4/30/2013 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR031-0006 | |||
| 3663 | MCR032 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR032-0001 | |
| 3664 | MCR032 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR032-0002 | |||
| 3665 | MCR033 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | MNGDCARE | MANAGED-CARE-MAIN-MCR00002 | MCR033-0001 | |||
| 3666 | MCR034 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Must be populated on every record | 10/10/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR034-0001 | |
| 3667 | MCR034 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR034-0002 | |||
| 3668 | MCR034 | RECORD-ID | Value must be equal to a valid value. | MCR00003 - MANAGED-CARE-LOCATION-AND-CONTACT-INFO | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR034-0003 | ||
| 3669 | MCR034 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR034-0004 | |||
| 3670 | MCR035 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR035-0001 | |
| 3671 | MCR035 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR035-0002 | ||
| 3672 | MCR035 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR035-0003 | |||
| 3673 | MCR035 | SUBMITTING-STATE | Value must be the same as Header Record in all records | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR035-0004 | |||
| 3674 | MCR036 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 10/10/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR036-0001 | |
| 3675 | MCR036 | RECORD-NUMBER | Must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR036-0002 | |||
| 3676 | MCR036 | RECORD-NUMBER | Duplicate record number should not exist with in same file | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR036-0003 | |||
| 3677 | MCR037 | STATE-PLAN-ID-NUM | Contains the ID number the state issued to the managed care entity. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR037-0001 | |
| 3678 | MCR037 | STATE-PLAN-ID-NUM | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR037-0002 | |||
| 3679 | MCR037 | STATE-PLAN-ID-NUM | State plan ID num must match a State plan ID num on the MCR-MAIN segment | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR037-0003 | |||
| 3680 | MCR037 | STATE-PLAN-ID-NUM | If the National Health Plan Identifier is available, please enter the number in this field and the NATIONAL-HEALTH-CARE-ENTITY-ID field. If not available, please enter the state’s internal plan ID. Please fill in the PLAN-ID-NUM depending on the value selected for the associated PLAN-ID-NUM-INDICATOR. | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR037-0004 | |||
| 3681 | MCR038 | MANAGED-CARE-LOCATION-ID | A field to differentiate a managed care entity’s service locations through adding a sequential number in this data element identifier field. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR038-0001 | |
| 3682 | MCR038 | MANAGED-CARE-LOCATION-ID | Each of an managed care entity’s locations must have a unique MANAGED-CARE-LOCATION-ID | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR038-0002 | |||
| 3683 | MCR038 | MANAGED-CARE-LOCATION-ID | This data element should be populated if MANAGED-CARE-ADDR-TYPE is 3 (Managed care entity’s service location address) | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR038-0003 | |||
| 3684 | MCR038 | MANAGED-CARE-LOCATION-ID | Use sequential numbers to indicate additional services locations | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR038-0004 | |||
| 3685 | MCR038 | MANAGED-CARE-LOCATION-ID | Right-fill the field if the value is less than 15 bytes long. | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR038-0005 | |||
| 3686 | MCR039 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-EFF-DATE | The first day of the time span during which the values in all data elements in the MANAGED-CARE-LOCATION-AND-CONTACT-INFO record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR039-0001 | |
| 3687 | MCR039 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-EFF-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR039-0002 | |||
| 3688 | MCR039 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR039-0003 | |||
| 3689 | MCR039 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-EFF-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR039-0004 | |||
| 3690 | MCR039 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-EFF-DATE | Whenever the value in one or more of the data elements in the MANAGED-CARE-LOCATION-AND-CONTACT-INFO record segment changes, a new record segment must be created. | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR039-0005 | |||
| 3691 | MCR040 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-END-DATE | The last day of the time span during which the values in all data elements in the MANAGED-CARE-LOCATION-AND-CONTACT-INFO record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR040-0001 | |
| 3692 | MCR040 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-END-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR040-0002 | |||
| 3693 | MCR040 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR040-0003 | |||
| 3694 | MCR040 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-END-DATE | The date must be a valid date. | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR040-0004 | |||
| 3695 | MCR040 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-END-DATE | Date must be equal to or greater than MANAGED-CARE-LOCATION-AND-CONTACT-INFO-EFF-DATE | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR040-0005 | |||
| 3696 | MCR040 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-END-DATE | Overlapping date spans should not exist for a given combination of state/state plan ID/Location ID/Address Type | 10/10/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR040-0006 | |||
| 3697 | MCR040 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR040-0007 | |||
| 3698 | MCR040 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-END-DATE | Active MCR-CARE-MAIN record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR040-0008 | |||
| 3699 | MCR040 | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-END-DATE | Whenever the value in one or more of the data elements in the MANAGED-CARE-LOCATION-AND-CONTACT-INFO record segment changes, a new record segment must be created. | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR040-0009 | |||
| 3700 | MCR041 | MANAGED-CARE-ADDR-TYPE | A code to distinguish various addresses that a managed care entity may have. | Required | This data element must be populated on every MANAGED-CARE-LOCATION-AND-CONTACT-INFO record. | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR041-0001 | |
| 3701 | MCR041 | MANAGED-CARE-ADDR-TYPE | Value must be equal to a valid value. | 1 MCO’s corporate address and contact information 2 MCO’s mailing address 3 MCO’s service location address 4 MCO’s Billing address and contact information 5 CEO’s address and contact information 6 CFO’s address and contact information 7 Other |
10/10/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR041-0002 | ||
| 3702 | MCR042 | MANAGED-CARE-ADDR-LN1 | The managed care entity’s address listed on the contract with the state. | Required | Line 1 is required. Lines 2 through 3 can be blank. | 10/10/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR042-0001 | |
| 3703 | MCR042 | MANAGED-CARE-ADDR-LN1 | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9), dashes (“-“), commas (“,”), periods (“.”), single quotes ('), and spaces. | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR042-0002 | |||
| 3704 | MCR043 | MANAGED-CARE-ADDR-LN2 | The managed care entity’s address listed on the contract with the state. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR043-0001 | |
| 3705 | MCR043 | MANAGED-CARE-ADDR-LN2 | Line 1 is required. Lines 2 through 3 can be blank. | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR043-0002 | |||
| 3706 | MCR043 | MANAGED-CARE-ADDR-LN2 | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR043-0003 | |||
| 3707 | MCR044 | MANAGED-CARE-ADDR-LN3 | The managed care entity’s address listed on the contract with the state. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR044-0001 | |
| 3708 | MCR044 | MANAGED-CARE-ADDR-LN3 | Line 1 is required. Lines 2 through 3 can be blank. | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR044-0002 | |||
| 3709 | MCR044 | MANAGED-CARE-ADDR-LN3 | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR044-0003 | |||
| 3710 | MCR045 | MANAGED-CARE-CITY | The city of the managed care entity’s address as listed on the contract with the state. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR045-0001 | |
| 3711 | MCR045 | MANAGED-CARE-CITY | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9), dashes (“-“), commas (“,”), periods (“.”), single quote ('), and spaces. | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR045-0002 | |||
| 3712 | MCR046 | MANAGED-CARE-STATE | The ANSI state numeric code for the U.S. state, Territory, or the District of Columbia code of the of the managed care entity’s address as listed on the contract with the state. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR046-0001 | |
| 3713 | MCR046 | MANAGED-CARE-STATE | Must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR046-0002 | |||
| 3714 | MCR046 | MANAGED-CARE-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR046-0003 | ||
| 3715 | MCR046 | MANAGED-CARE-STATE | Use the ANSI state code | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR046-0004 | |||
| 3716 | MCR047 | MANAGED-CARE-ZIP-CODE | The zip code of the managed care entity as it appears in the address listed on the contract with the state. | Required | Must be populated on every record | 9/23/2015 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR047-0001 | |
| 3717 | MCR047 | MANAGED-CARE-ZIP-CODE | The value must consist of digits 0 through 9 only | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR047-0002 | |||
| 3718 | MCR047 | MANAGED-CARE-ZIP-CODE | The first five characters are needed. If the four-digit extention is available, that may be filled in using the last four byes. Otherwise, if the last 4 digits are not populated or used, then the 4-digit extended zip code should be recorded as “0000”. | 9/23/2015 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR047-0003 | |||
| 3719 | MCR048 | MANAGED-CARE-COUNTY | The ANSI County numeric code for the county or county equivalent. | Required | Must be populated on every record | 10/10/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR048-0001 | |
| 3720 | MCR048 | MANAGED-CARE-COUNTY | Value must be numeric. | 10/10/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR048-0002 | |||
| 3721 | MCR048 | MANAGED-CARE-COUNTY | Dependent value must be equal to a valid value. | http://www.census.gov/geo/reference/codes/cou.html | 10/10/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR048-0003 | ||
| 3722 | MCR048 | MANAGED-CARE-COUNTY | One county code should be captured for each of a managed care entity’s locations (MANAGED-CARE-LOCATION-IDs). | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR048-0004 | |||
| 3723 | MCR049 | MANAGED-CARE-TELEPHONE | The telephone number, including area code, of the managed care entity as listed on the contract with the state. | Optional | Must be populated on every record | 11/3/2015 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR049-0001 | |
| 3724 | MCR049 | MANAGED-CARE-TELEPHONE | Must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR049-0002 | |||
| 3725 | MCR049 | MANAGED-CARE-TELEPHONE | Enter the digits only (i.e., without parentheses, brackets, dashes, periods, spaces, etc.) | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR049-0003 | |||
| 3726 | MCR050 | MANAGED-CARE-EMAIL | The email address of the managed care entity as listed on the contract with the state. | Optional | Must be populated on every record | 11/3/2015 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR050-0001 | |
| 3727 | MCR050 | MANAGED-CARE-EMAIL | Must contain @ | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR050-0002 | |||
| 3728 | MCR050 | MANAGED-CARE-EMAIL | Must have [email protected] format | 9/23/2015 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR050-0003 | |||
| 3729 | MCR051 | MANAGED-CARE-FAX-NUMBER | A fax number, including area code, as listed on the contract with the state | Optional | Must be populated on every record | 11/3/2015 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR051-0001 | |
| 3730 | MCR051 | MANAGED-CARE-FAX-NUMBER | Must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR051-0002 | |||
| 3731 | MCR051 | MANAGED-CARE-FAX-NUMBER | Enter the digits only (i.e., without parentheses, brackets, dashes, periods, spaces, etc.) | 2/25/2013 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR051-0003 | |||
| 3732 | MCR052 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR052-0001 | |
| 3733 | MCR052 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR052-0002 | |||
| 3734 | MCR053 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | MNGDCARE | MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 | MCR053-0001 | |||
| 3735 | MCR054 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR054-0001 | |
| 3736 | MCR054 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR054-0002 | |||
| 3737 | MCR054 | RECORD-ID | Value must be in the set of valid values | MCR00004 - MANAGED-CARE-SERVICE-AREA | 10/10/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR054-0003 | ||
| 3738 | MCR054 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR054-0004 | |||
| 3739 | MCR055 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR055-0001 | |
| 3740 | MCR055 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR055-0002 | ||
| 3741 | MCR055 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR055-0003 | |||
| 3742 | MCR055 | SUBMITTING-STATE | Value must be the same as Header Record in all records | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR055-0004 | |||
| 3743 | MCR056 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR056-0001 | |
| 3744 | MCR056 | RECORD-NUMBER | Must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR056-0002 | |||
| 3745 | MCR056 | RECORD-NUMBER | Duplicate record number should not exist with in same file | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR056-0003 | |||
| 3746 | MCR057 | STATE-PLAN-ID-NUM | Contains the ID number the state issued to the managed care entity. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR057-0001 | |
| 3747 | MCR057 | STATE-PLAN-ID-NUM | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR057-0002 | |||
| 3748 | MCR057 | STATE-PLAN-ID-NUM | State plan ID num must match a State plan ID num on the MCR-MAIN segment | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR057-0003 | |||
| 3749 | MCR057 | STATE-PLAN-ID-NUM | If the National Health Plan Identifier is available, please enter the number in this field and the NATIONAL-HEALTH-CARE-ENTITY-ID field. If not available, please enter the state’s internal plan ID. Please fill in the PLAN-ID-NUM depending on the value selected for the associated PLAN-ID-NUM-INDICATOR. | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR057-0004 | |||
| 3750 | MCR058 | MANAGED-CARE-SERVICE-AREA-NAME | The specific identifiers for the counties, cities, regions, zip codes and/or other geographic areas that the managed care entity serves. | Required | Must be populated on every record | http://www.census.gov/geo/reference/ansi.html | 10/10/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR058-0001 |
| 3751 | MCR058 | MANAGED-CARE-SERVICE-AREA-NAME | If Managed-care-service-area is 2, 3, 4, 5, or 6 please create/submit a managed-care-service-area-record for each service area. | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR058-0002 | |||
| 3752 | MCR058 | MANAGED-CARE-SERVICE-AREA-NAME | Use ANSI county codes when service area is defined by counties or cities. | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR058-0003 | |||
| 3753 | MCR058 | MANAGED-CARE-SERVICE-AREA-NAME | Put each zip code, city, county, region, or other area descriptor on a separate record. | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR058-0004 | |||
| 3754 | MCR058 | MANAGED-CARE-SERVICE-AREA-NAME | Use 5 digit zip codes when service area definition is zip code based. | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR058-0005 | |||
| 3755 | MCR058 | MANAGED-CARE-SERVICE-AREA-NAME | When entering other area descriptors, valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9), dashes (“-“), commas (“,”), periods (“.”), single quotes ('), and spaces. | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR058-0006 | |||
| 3756 | MCR059 | MANAGED-CARE-SERVICE-AREA-EFF-DATE | The first day of the time span during which the values in all data elements in the MANAGED-CARE-SERVICE-AREA record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR059-0001 | |
| 3757 | MCR059 | MANAGED-CARE-SERVICE-AREA-EFF-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR059-0002 | |||
| 3758 | MCR059 | MANAGED-CARE-SERVICE-AREA-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR059-0003 | |||
| 3759 | MCR059 | MANAGED-CARE-SERVICE-AREA-EFF-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR059-0004 | |||
| 3760 | MCR059 | MANAGED-CARE-SERVICE-AREA-EFF-DATE | Whenever the value in one or more of the data elements in the MANAGED-CARE-SERVICE-AREA record segment changes, a new record segment must be created. | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR059-0005 | |||
| 3761 | MCR060 | MANAGED-CARE-SERVICE-AREA-END-DATE | The last day of the time span during which the values in all data elements in the MANAGED-CARE-SERVICE-AREA record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR060-0001 | |
| 3762 | MCR060 | MANAGED-CARE-SERVICE-AREA-END-DATE | Date format is CCYYMMDD (National Data Standard). | 10/10/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR060-0002 | |||
| 3763 | MCR060 | MANAGED-CARE-SERVICE-AREA-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR060-0003 | |||
| 3764 | MCR060 | MANAGED-CARE-SERVICE-AREA-END-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR060-0004 | |||
| 3765 | MCR060 | MANAGED-CARE-SERVICE-AREA-END-DATE | Date must be equal to or greater than MANAGED-CARE-SERVICE-AREA-EFF-DATE | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR060-0005 | |||
| 3766 | MCR060 | MANAGED-CARE-SERVICE-AREA-END-DATE | Overlapping date spans should not exist for a given combination of state/state plan ID/Service Area Name | 10/10/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR060-0006 | |||
| 3767 | MCR060 | MANAGED-CARE-SERVICE-AREA-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR060-0007 | |||
| 3768 | MCR060 | MANAGED-CARE-SERVICE-AREA-END-DATE | Active MCR-MAIN record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR060-0008 | |||
| 3769 | MCR060 | MANAGED-CARE-SERVICE-AREA-END-DATE | Whenever the value in one or more of the data elements in the MANAGED-CARE-SERVICE-AREA record segment changes, a new record segment must be created | 2/25/2013 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR060-0009 | |||
| 3770 | MCR061 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR061-0001 | |
| 3771 | MCR061 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR061-0002 | |||
| 3772 | MCR062 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | MNGDCARE | MANAGED-CARE-SERVICE-AREA-MCR00004 | MCR062-0001 | |||
| 3773 | MCR063 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR063-0001 | |
| 3774 | MCR063 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR063-0002 | |||
| 3775 | MCR063 | RECORD-ID | Value must be in the set of valid values | MCR00005 - MANAGED-CARE-OPERATING-AUTHORITY | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR063-0003 | ||
| 3776 | MCR063 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR063-0004 | |||
| 3777 | MCR064 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR064-0001 | |
| 3778 | MCR064 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR064-0002 | ||
| 3779 | MCR064 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR064-0003 | |||
| 3780 | MCR064 | SUBMITTING-STATE | Value must be the same as Header Record in all records | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR064-0004 | |||
| 3781 | MCR065 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR065-0001 | |
| 3782 | MCR065 | RECORD-NUMBER | Must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR065-0002 | |||
| 3783 | MCR065 | RECORD-NUMBER | Duplicate record number should not exist with in same file | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR065-0003 | |||
| 3784 | MCR066 | STATE-PLAN-ID-NUM | Contains the ID number the state issued to the managed care entity. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR066-0001 | |
| 3785 | MCR066 | STATE-PLAN-ID-NUM | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR066-0002 | |||
| 3786 | MCR066 | STATE-PLAN-ID-NUM | State plan ID num must match a State plan ID num on the MCR-MAIN segment | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR066-0003 | |||
| 3787 | MCR066 | STATE-PLAN-ID-NUM | If the National Health Plan Identifier is available, please enter the number in this field and the NATIONAL-HEALTH-CARE-ENTITY-ID field. If not available, please enter the state’s internal plan ID. Please fill in the PLAN-ID-NUM depending on the value selected for the associated PLAN-ID-NUM-INDICATOR. | 2/25/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR066-0004 | |||
| 3788 | MCR067 | OPERATING-AUTHORITY | The type of operating authority through which the managed care entity receives its contract authority. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR067-0001 | |
| 3789 | MCR067 | OPERATING-AUTHORITY | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 2/25/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR067-0002 | ||
| 3790 | MCR067 | OPERATING-AUTHORITY | Please fill in the Operating-Authorities that plan is operating under. | 2/25/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR067-0003 | |||
| 3791 | MCR068 | WAIVER-ID | Field specifying the waiver or demonstration which authorized payment for a claim. These IDs must be the approved, full federal waiver ID number assigned during the state submission and CMS approval process. The categories of demonstration and waiver programs include: 1915(b)(1); 1915(b)(2); 1915(b)(3), and 1915(b)(4) managed care waivers; 1915(c) home and community based services waivers; combined 1915(b) and 1915(c) managed home and community based services waivers and 1115 demonstrations. | Required | Report the full federal waiver identifier. | Valid values are supplied by the state. | 11/9/2015 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR068-0001 |
| 3792 | MCR069 | MANAGED-CARE-OP-AUTHORITY-EFF-DATE | The date that the state obtains the authority to operate their managed care program to allow them to contract with various types of managed care plans at the time of the reporting period. This date field is necessary when defining a unique row in a database table. |
Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR069-0001 | |
| 3793 | MCR069 | MANAGED-CARE-OP-AUTHORITY-EFF-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR069-0002 | |||
| 3794 | MCR069 | MANAGED-CARE-OP-AUTHORITY-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR069-0003 | |||
| 3795 | MCR069 | MANAGED-CARE-OP-AUTHORITY-EFF-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR069-0004 | |||
| 3796 | MCR069 | MANAGED-CARE-OP-AUTHORITY-EFF-DATE | Date must be equal to or less than MANAGED-CARE-OP-AUTHORITY-END-DATE | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR069-0005 | |||
| 3797 | MCR069 | MANAGED-CARE-OP-AUTHORITY-EFF-DATE | Whenever the value in one or more of the data elements in the MANAGED-CARE-OPERATING-AUTHORITY record segment changes, a new record segment must be created. | 2/25/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR069-0006 | |||
| 3798 | MCR070 | MANAGED-CARE-OP-AUTHORITY-END-DATE | The date that state authority ends, to operate their managed care program to allow them to contract with various types of managed care plans at the time of the reporting period. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR070-0001 | |
| 3799 | MCR070 | MANAGED-CARE-OP-AUTHORITY-END-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR070-0002 | |||
| 3800 | MCR070 | MANAGED-CARE-OP-AUTHORITY-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR070-0003 | |||
| 3801 | MCR070 | MANAGED-CARE-OP-AUTHORITY-END-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR070-0004 | |||
| 3802 | MCR070 | MANAGED-CARE-OP-AUTHORITY-END-DATE | Date must be equal to or greater than MANAGED-CARE-OP-AUTHORITY-EFF-DATE | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR070-0005 | |||
| 3803 | MCR070 | MANAGED-CARE-OP-AUTHORITY-END-DATE | Overlapping date spans should not exist for a given combination of state/state plan ID/Operating Authority/Waiver ID | 10/10/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR070-0006 | |||
| 3804 | MCR070 | MANAGED-CARE-OP-AUTHORITY-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR070-0007 | |||
| 3805 | MCR070 | MANAGED-CARE-OP-AUTHORITY-END-DATE | Active MCR-MAIN record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR070-0008 | |||
| 3806 | MCR070 | MANAGED-CARE-OP-AUTHORITY-END-DATE | Whenever the value in one or more of the data elements in the MANAGED-CARE-OPERATING-AUTHORITY record segment changes, a new record segment must be created. | 2/25/2013 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR070-0009 | |||
| 3807 | MCR071 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR071-0001 | |
| 3808 | MCR071 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR071-0002 | |||
| 3809 | MCR072 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | MNGDCARE | MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 | MCR072-0001 | |||
| 3810 | MCR073 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR073-0001 | |
| 3811 | MCR073 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR073-0002 | |||
| 3812 | MCR073 | RECORD-ID | Value must be in the set of valid values | MCR00006 - MANAGED-CARE-PLAN-POPULATION-ENROLLED | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR073-0003 | ||
| 3813 | MCR073 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR073-0004 | |||
| 3814 | MCR074 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR074-0001 | |
| 3815 | MCR074 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR074-0002 | ||
| 3816 | MCR074 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR074-0003 | |||
| 3817 | MCR074 | SUBMITTING-STATE | Value must be the same as Header Record in all records | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR074-0004 | |||
| 3818 | MCR075 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR075-0001 | |
| 3819 | MCR075 | RECORD-NUMBER | Must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR075-0002 | |||
| 3820 | MCR075 | RECORD-NUMBER | Duplicate record number should not exist with in same file | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR075-0003 | |||
| 3821 | MCR076 | STATE-PLAN-ID-NUM | Contains the ID number the state issued to the managed care entity. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR076-0001 | |
| 3822 | MCR076 | STATE-PLAN-ID-NUM | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR076-0002 | |||
| 3823 | MCR076 | STATE-PLAN-ID-NUM | State plan ID num must match a State plan ID num on the MCR MAIN segment | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR076-0003 | |||
| 3824 | MCR076 | STATE-PLAN-ID-NUM | If the National Health Plan Identifier is available, please enter the number in this field and the NATIONAL-HEALTH-CARE-ENTITY-ID field. If not available, please enter the state’s internal plan ID. Please fill in the PLAN-ID-NUM depending on the value selected for the associated PLAN-ID-NUM-INDICATOR. | 2/25/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR076-0004 | |||
| 3825 | MCR077 | MANAGED-CARE-PLAN-POP | The eligibility group(s) the state authorizes the managed care entity to enroll. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR077-0001 | |
| 3826 | MCR077 | MANAGED-CARE-PLAN-POP | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 10/10/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR077-0002 | ||
| 3827 | MCR077 | MANAGED-CARE-PLAN-POP | Must be numeric | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR077-0003 | |||
| 3828 | MCR077 | MANAGED-CARE-PLAN-POP | Please submit all Managed Care Plan Populations using the Managed Care Plan Population Enrolled Record-ID 6 (MCR00006). | 2/25/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR077-0004 | |||
| 3829 | MCR078 | MANAGED-CARE-PLAN-POP-EFF-DATE | The effective date that the managed care plan began enrolling the eligibility group(s) that the state authorized. This date field is necessary when defining a unique row in a database table. |
Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR078-0001 | |
| 3830 | MCR078 | MANAGED-CARE-PLAN-POP-EFF-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR078-0002 | |||
| 3831 | MCR078 | MANAGED-CARE-PLAN-POP-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR078-0003 | |||
| 3832 | MCR078 | MANAGED-CARE-PLAN-POP-EFF-DATE | The date must be a valid date. | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR078-0004 | |||
| 3833 | MCR078 | MANAGED-CARE-PLAN-POP-EFF-DATE | Whenever the value in one or more of the data elements in the MANAGED-CARE-OPERATING-AUTHORITY record segment changes, a new record segment must be created. | 2/25/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR078-0005 | |||
| 3834 | MCR079 | MANAGED-CARE-PLAN-POP-END-DATE | The ending date that the managed care plan stopped enrolling the eligibility group(s) that the state authorized. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR079-0001 | |
| 3835 | MCR079 | MANAGED-CARE-PLAN-POP-END-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR079-0002 | |||
| 3836 | MCR079 | MANAGED-CARE-PLAN-POP-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR079-0003 | |||
| 3837 | MCR079 | MANAGED-CARE-PLAN-POP-END-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR079-0004 | |||
| 3838 | MCR079 | MANAGED-CARE-PLAN-POP-END-DATE | Date must be equal to or greater than MANAGED-CARE-PLAN-POP-EFF-DATE | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR079-0005 | |||
| 3839 | MCR079 | MANAGED-CARE-PLAN-POP-END-DATE | Overlapping date spans should not exist for a given combination of state/state plan ID/managed care plan pop | 10/10/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR079-0006 | |||
| 3840 | MCR079 | MANAGED-CARE-PLAN-POP-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR079-0007 | |||
| 3841 | MCR079 | MANAGED-CARE-PLAN-POP-END-DATE | Active MCR-MAIN record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR079-0008 | |||
| 3842 | MCR079 | MANAGED-CARE-PLAN-POP-END-DATE | Whenever the value in one or more of the data elements in the MANAGED-CARE-OPERATING-AUTHORITY record segment changes, a new record segment must be created. | 2/25/2013 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR079-0009 | |||
| 3843 | MCR080 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR080-0001 | |
| 3844 | MCR080 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR080-0002 | |||
| 3845 | MCR081 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | MNGDCARE | MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 | MCR081-0001 | |||
| 3846 | MCR082 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR082-0001 | |
| 3847 | MCR082 | RECORD-ID | Must be in correct format as shown in definition | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR082-0002 | |||
| 3848 | MCR082 | RECORD-ID | Value must be in the set of valid values | MCR00007 - MANAGED-CARE-ACCREDITATION-ORGANIZATION | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR082-0003 | ||
| 3849 | MCR082 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR082-0004 | |||
| 3850 | MCR083 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR083-0001 | |
| 3851 | MCR083 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR083-0002 | ||
| 3852 | MCR083 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR083-0003 | |||
| 3853 | MCR083 | SUBMITTING-STATE | Value must be the same as Header Record in all records | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR083-0004 | |||
| 3854 | MCR084 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 10/10/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR084-0001 | |
| 3855 | MCR084 | RECORD-NUMBER | Must be numeric | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR084-0002 | |||
| 3856 | MCR084 | RECORD-NUMBER | Duplicate record number should not exist with in same file | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR084-0003 | |||
| 3857 | MCR085 | STATE-PLAN-ID-NUM | Contains the ID number the state issued to the managed care entity. | Required | Must be populated on every record | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR085-0001 | |
| 3858 | MCR085 | STATE-PLAN-ID-NUM | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR085-0002 | |||
| 3859 | MCR085 | STATE-PLAN-ID-NUM | State plan ID num must match a State plan ID num on the MCR-MAIN segment | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR085-0003 | |||
| 3860 | MCR085 | STATE-PLAN-ID-NUM | If the National Health Plan Identifier is available, please enter the number in this field and the NATIONAL-HEALTH-CARE-ENTITY-ID field. If not available, please enter the state’s internal plan ID. Please fill in the PLAN-ID-NUM depending on the value selected for the associated PLAN-ID-NUM-INDICATOR. | 2/25/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR085-0004 | |||
| 3861 | MCR086 | ACCREDITATION-ORGANIZATION | Identify the accreditation awarded to the managed care entity. | Conditional | Must be populated on every record | 11/3/2015 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR086-0001 | |
| 3862 | MCR086 | ACCREDITATION-ORGANIZATION | Value must be equal to a valid value. | 01 National committee for quality assurance – excellent 02 National committee for quality assurance – commendable 03 National committee for quality assurance – provisional 05 URAC - full 06 URAC - conditional 07 URAC – provisional 08 Accreditation Association for Ambulatory Health Care, Inc. (AAAHC) – 3 years 11 Not accredited 12 Other 13 National committee for quality assurance – accredited 14 National committee for quality assurance – interim 15 National committee for quality assurance – denied |
9/23/2015 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR086-0002 | ||
| 3863 | MCR087 | DATE-ACCREDITATION-ACHIEVED | The date the organization achieved accreditation. This date field is necessary when defining a unique row in a database table. |
Conditional | Must be populated on every record | 11/3/2015 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR087-0001 | |
| 3864 | MCR087 | DATE-ACCREDITATION-ACHIEVED | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR087-0002 | |||
| 3865 | MCR087 | DATE-ACCREDITATION-ACHIEVED | The date must be a valid date. | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR087-0003 | |||
| 3866 | MCR087 | DATE-ACCREDITATION-ACHIEVED | Date must be less then current date | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR087-0004 | |||
| 3867 | MCR087 | DATE-ACCREDITATION-ACHIEVED | Date must be equal to or less then DATE-ACCREDITATION-END | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR087-0005 | |||
| 3868 | MCR088 | DATE-ACCREDITATION-END | The date when organization’s accreditation ends. | Conditional | Must be populated on every record | 11/3/2015 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR088-0001 | |
| 3869 | MCR088 | DATE-ACCREDITATION-END | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR088-0002 | |||
| 3870 | MCR088 | DATE-ACCREDITATION-END | The date must be a valid date. | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR088-0003 | |||
| 3871 | MCR088 | DATE-ACCREDITATION-END | Date must be equal to or less then DATE-ACCREDITATION-ACHIEVED | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR088-0004 | |||
| 3872 | MCR088 | DATE-ACCREDITATION-END | Overlapping date spans should not exist for a given combination of state/state plan ID/accreditation organization | 10/10/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR088-0005 | |||
| 3873 | MCR088 | DATE-ACCREDITATION-END | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR088-0006 | |||
| 3874 | MCR088 | DATE-ACCREDITATION-END | Active MCR-MAIN record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR088-0007 | |||
| 3875 | MCR089 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR089-0001 | |
| 3876 | MCR089 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR089-0002 | |||
| 3877 | MCR090 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | MNGDCARE | MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 | MCR090-0001 | |||
| 3878 | MCR091 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Must be populated on every record | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR091-0001 | |
| 3879 | MCR091 | RECORD-ID | Must be in correct format as shown in definition | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR091-0002 | |||
| 3880 | MCR091 | RECORD-ID | Value must be in the set of valid values | MCR00008 - NATIONAL-HEALTH-CARE-ENTITY-ID-INFO | 10/10/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR091-0003 | ||
| 3881 | MCR091 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR091-0004 | |||
| 3882 | MCR092 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR092-0001 | |
| 3883 | MCR092 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR092-0002 | ||
| 3884 | MCR092 | SUBMITTING-STATE | Value must be numeric | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR092-0003 | |||
| 3885 | MCR092 | SUBMITTING-STATE | Value must be the same as Header Record in all records | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR092-0004 | |||
| 3886 | MCR093 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 10/10/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR093-0001 | |
| 3887 | MCR093 | RECORD-NUMBER | Must be numeric | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR093-0002 | |||
| 3888 | MCR093 | RECORD-NUMBER | Duplicate record number should not exist with in same file | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR093-0003 | |||
| 3889 | MCR094 | STATE-PLAN-ID-NUM | Contains the ID number the state issued to the managed care entity. | Required | Must be populated on every record | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR094-0001 | |
| 3890 | MCR094 | STATE-PLAN-ID-NUM | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR094-0002 | |||
| 3891 | MCR094 | STATE-PLAN-ID-NUM | State plan ID num must match a State plan ID num on the MCR-MAIN segment | 4/30/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR094-0003 | |||
| 3892 | MCR094 | STATE-PLAN-ID-NUM | If the National Health Plan Identifier is available, please enter the number in this field and the NATIONAL-HEALTH-CARE-ENTITY-ID field. If not available, please enter the state’s internal plan ID. Please fill in the PLAN-ID-NUM depending on the value selected for the associated PLAN-ID-NUM-INDICATOR. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR094-0004 | |||
| 3893 | MCR095 | NATIONAL-HEALTH-CARE-ENTITY-ID | The national health plan identifier(s) or other entity identifier(s) assigned to a managed care entity in accordance with 45 CFR 162 Subpart E. All of the entity’s national health care entity identifiers should be reported using the NATIONAL-HEALTH-CARE-ENTITY-ID-INFO and CHPID-SHPID-RELATIONSHIPS record segments. | NA | Large health plans are required to obtain HPIDs by November 5, 2014, small health plans by November 5, 2015. States may report prior to these dates if available. | 11/3/2015 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR095-0001 | |
| 3894 | MCR095 | NATIONAL-HEALTH-CARE-ENTITY-ID | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR095-0002 | |||
| 3895 | MCR095 | NATIONAL-HEALTH-CARE-ENTITY-ID | Covered entities must use the national identifiers in the standard transactions on or after November 7, 2016. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR095-0003 | |||
| 3896 | MCR095 | NATIONAL-HEALTH-CARE-ENTITY-ID | This field is required for all eligible persons enrolled in managed care on or after the mandated dates above. If the eligible person is not enrolled in managed care, fill the field with spaces. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR095-0004 | |||
| 3897 | MCR095 | NATIONAL-HEALTH-CARE-ENTITY-ID | National identifiers in the eligible file must match either a controlling health plan (CHP) identifier or subhealth plan (SHP) identifier in the Managed Care subject area. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR095-0005 | |||
| 3898 | MCR095 | NATIONAL-HEALTH-CARE-ENTITY-ID | States should not submit records for an eligible individual where the national managed care entity ID for the eligible does not match in the associated managed care record. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR095-0006 | |||
| 3899 | MCR096 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | The NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE distinguishes “controlling” health plan identifiers (CHPIDs), “subhealth” health plan identifiers (SHPIDs), and other entity identifiers (OEIDs) from one another. See 45 CFR 162 Subpart E. http://www.gpo.gov/fdsys/pkg/FR-2012-09-05/pdf/2012-21238.pdf | NA | Large health plans are required to obtain national identifiers by November 5, 2014, small health plans by November 5, 2015. | 1 Controlling Health Plan (CHP) ID 2 Subhealth Plan (SHP) ID 3 Other Entity Identifier (OEID) |
11/3/2015 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR096-0001 |
| 3900 | MCR096 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | Covered entities must use the national identifiers in the standard transactions on or after November 7, 2016. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR096-0002 | |||
| 3901 | MCR096 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | States should not submit records for an eligible individual where the national managed care entity ID for the eligible does not match in the associated managed care record. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR096-0003 | |||
| 3902 | MCR097 | NATIONAL-HEALTH-CARE-ENTITY-NAME | The legal name of the health care entity identified by the corresponding value in the NATIONAL-HEALTH-CARE-ENTITY-ID field. | NA | Must be populated on every record | 11/3/2015 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR097-0001 | |
| 3903 | MCR097 | NATIONAL-HEALTH-CARE-ENTITY-NAME | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote (') |
2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR097-0002 | |||
| 3904 | MCR097 | NATIONAL-HEALTH-CARE-ENTITY-NAME | Use the descriptive name assigned by the state as it exists in the state’s MMIS. | 9/23/2015 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR097-0003 | |||
| 3905 | MCR097 | NATIONAL-HEALTH-CARE-ENTITY-NAME | If a name is not associated with the NATIONAL-HEALTH-CARE-ENTITY-ID in the state’s MMIS, fill the field with 8s. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR097-0004 | |||
| 3906 | MCR097 | NATIONAL-HEALTH-CARE-ENTITY-NAME | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR097-0005 | |||
| 3907 | MCR098 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE | The first day of the time span during which the values in all data elements in the NATIONAL-HEALTH-CARE-ENTITY-ID-INFO record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
NA | Must be populated on every record | 11/3/2015 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR098-0001 | |
| 3908 | MCR098 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR098-0002 | |||
| 3909 | MCR098 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR098-0003 | |||
| 3910 | MCR098 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR098-0004 | |||
| 3911 | MCR098 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE | Date must be less then current date | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR098-0005 | |||
| 3912 | MCR098 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE | Date must be equal to or less then NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-END-DATE | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR098-0006 | |||
| 3913 | MCR098 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE | Whenever the value in one or more of the data elements in the NATIONAL-HEALTH-CARE-ENTITY-ID-INFO record segment changes, a new record segment must be created. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR098-0007 | |||
| 3914 | MCR099 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-END-DATE | The first day of the time span during which the values in all data elements in the NATIONAL-HEALTH-CARE-ENTITY-ID-INFO record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | NA | Must be populated on every record | 11/3/2015 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR099-0001 | |
| 3915 | MCR099 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-END-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR099-0002 | |||
| 3916 | MCR099 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR099-0003 | |||
| 3917 | MCR099 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-END-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR099-0004 | |||
| 3918 | MCR099 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-END-DATE | Date must be equal to or greater then NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR099-0005 | |||
| 3919 | MCR099 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-END-DATE | Overlapping date spans should not exist for a given combination of state/state plan ID/ National Health Care Entity ID/National Health Care Entity ID type | 10/10/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR099-0006 | |||
| 3920 | MCR099 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR099-0007 | |||
| 3921 | MCR099 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-END-DATE | Active MCR-MAIN record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR099-0008 | |||
| 3922 | MCR099 | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-END-DATE | Whenever the value in one or more of the data elements in the NATIONAL-HEALTH-CARE-ENTITY-ID-INFO record segment changes, a new record segment must be created. | 2/25/2013 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR099-0009 | |||
| 3923 | MCR100 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR100-0001 | |
| 3924 | MCR100 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR100-0002 | |||
| 3925 | MCR101 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | MNGDCARE | NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 | MCR101-0001 | |||
| 3926 | MCR102 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Must be populated on every record | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR102-0001 | |
| 3927 | MCR102 | RECORD-ID | Must be in correct format as shown in definition | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR102-0002 | |||
| 3928 | MCR102 | RECORD-ID | Value must be in the set of valid values | MCR00009 - CHPID-SHPID-RELATIONSHIPS | 10/10/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR102-0003 | ||
| 3929 | MCR102 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR102-0004 | |||
| 3930 | MCR103 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR103-0001 | |
| 3931 | MCR103 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR103-0002 | ||
| 3932 | MCR103 | SUBMITTING-STATE | Value must be numeric | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR103-0003 | |||
| 3933 | MCR103 | SUBMITTING-STATE | Value must be the same as Header Record in all records | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR103-0004 | |||
| 3934 | MCR104 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 10/10/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR104-0001 | |
| 3935 | MCR104 | RECORD-NUMBER | Must be numeric | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR104-0002 | |||
| 3936 | MCR104 | RECORD-NUMBER | Duplicate record number should not exist with in same file | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR104-0003 | |||
| 3937 | MCR105 | STATE-PLAN-ID-NUM | Contains the ID number the state issued to the managed care entity. | Required | Must be populated on every record | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR105-0001 | |
| 3938 | MCR105 | STATE-PLAN-ID-NUM | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR105-0002 | |||
| 3939 | MCR105 | STATE-PLAN-ID-NUM | State plan ID num must match a State plan ID num on the MCR-MAIN segment | 4/30/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR105-0003 | |||
| 3940 | MCR105 | STATE-PLAN-ID-NUM | If the National Health Plan Identifier is available, please enter the number in this field and the NATIONAL-HEALTH-CARE-ENTITY-ID field. If not available, please enter the state’s internal plan ID. Please fill in the PLAN-ID-NUM depending on the value selected for the associated PLAN-ID-NUM-INDICATOR. | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR105-0004 | |||
| 3941 | MCR106 | CHPID | A data element to capture the Controlling Health Plan Identifier (CHPID) on the CHPID-SHPID-RELATIONSHIPS record. The CHPID-SHPID-RELATIONSHIPS record links a controlling health plan with its associated sub-health plans. (Sub-health plans are identified by SHPIDs.) |
NA | Must be populated on every record | 11/3/2015 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR106-0001 | |
| 3942 | MCR106 | CHPID | Every CHPID must have an active record in the state’s NATIONAL-HEALTH-CARE-ENTITY-ID-INFO data set in T-MSIS. | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR106-0002 | |||
| 3943 | MCR107 | SHPID | A data element to capture the Subhealth Plan Identifier (SHPID) on the CHPID-SHPID-RELATIONSHIPS record. The CHPID-SHPID-RELATIONSHIPS records link controlling health plans with their associated sub-health plans. (Controlling health plans are identified by CHPIDs.) |
NA | Must be populated on every record | 11/3/2015 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR107-0001 | |
| 3944 | MCR107 | SHPID | Every SHPID must have an active record in the state’s NATIONAL-HEALTH-CARE-ENTITY-ID-INFO data set in T-MSIS. | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR107-0002 | |||
| 3945 | MCR108 | CHPID-SHPID-RELATIONSHIP-EFF-DATE | The first day that the state submitting the CHPID-SHPID-RELATIONSHIPS record segment considers the data therein to be valid and active. The purpose of the effective and end dates on the CHPID-SHPID-RELATIONSHIPS record segment is to permit the submitting state show the span of time during which they consider the CHP ID to SHP ID relationship to be valid. This date field is necessary when defining a unique row in a database table. |
NA | Must be populated on every record | 11/3/2015 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR108-0001 | |
| 3946 | MCR108 | CHPID-SHPID-RELATIONSHIP-EFF-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR108-0002 | |||
| 3947 | MCR108 | CHPID-SHPID-RELATIONSHIP-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR108-0003 | |||
| 3948 | MCR108 | CHPID-SHPID-RELATIONSHIP-EFF-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR108-0004 | |||
| 3949 | MCR108 | CHPID-SHPID-RELATIONSHIP-EFF-DATE | Date must be less then current date | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR108-0005 | |||
| 3950 | MCR108 | CHPID-SHPID-RELATIONSHIP-EFF-DATE | Date must be equal to or less then CHPID-SHPID-RELATIONSHIP-END-DATE | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR108-0006 | |||
| 3951 | MCR109 | CHPID-SHPID-RELATIONSHIP-END-DATE | The last day that the state submitting the CHPID-SHPID-RELATIONSHIPS record segment considers the data therein to be valid and active. The purpose of the effective & end dates on the CHPID-SHPID-RELATIONSHIPS record segment is to permit the submitting state show the span of time during which they consider the CHP ID to SHP ID relationship to be valid. |
NA | Must be populated on every record | 11/3/2015 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR109-0001 | |
| 3952 | MCR109 | CHPID-SHPID-RELATIONSHIP-END-DATE | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR109-0002 | |||
| 3953 | MCR109 | CHPID-SHPID-RELATIONSHIP-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR109-0003 | |||
| 3954 | MCR109 | CHPID-SHPID-RELATIONSHIP-END-DATE | The date must be a valid date. | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR109-0004 | |||
| 3955 | MCR109 | CHPID-SHPID-RELATIONSHIP-END-DATE | Date must be equal to or greater then CHPID-SHPID-RELATIONSHIP-EFF-DATE | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR109-0005 | |||
| 3956 | MCR109 | CHPID-SHPID-RELATIONSHIP-END-DATE | Overlapping date spans should not exist for a given combination of state/state plan ID/CHPID/SHPID | 10/10/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR109-0006 | |||
| 3957 | MCR109 | CHPID-SHPID-RELATIONSHIP-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR109-0007 | |||
| 3958 | MCR109 | CHPID-SHPID-RELATIONSHIP-END-DATE | Active MCR-MAIN & MCR-NATIONAL-ENTITY-ID record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR109-0008 | |||
| 3959 | MCR109 | CHPID-SHPID-RELATIONSHIP-END-DATE | If the time span is open-ended (i.e., there is no end date), then populate the field with “99991231” (end-of-time). | 2/25/2013 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR109-0009 | |||
| 3960 | MCR110 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR110-0001 | |
| 3961 | MCR110 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR110-0002 | |||
| 3962 | MCR111 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | MNGDCARE | CHPID-SHPID-RELATIONSHIPS-MCR00009 | MCR111-0001 | |||
| 3963 | PRV001 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Value must be equal to a valid value. | PRV00001 FILE-HEADER-RECORD-PROVIDER |
4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV001-0001 |
| 3964 | PRV001 | RECORD-ID | Value is required on all record segments | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV001-0002 | |||
| 3965 | PRV001 | RECORD-ID | Value must be in the required format | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV001-0003 | |||
| 3966 | PRV001 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV001-0004 | |||
| 3967 | PRV002 | DATA-DICTIONARY-VERSION | A data element to capture the version of the T-MSIS data dictionary that was used to build the file. | Required | Use the version number specified on the title page of the data dictionary. | 2/25/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV002-0001 | |
| 3968 | PRV003 | SUBMISSION-TRANSACTION-TYPE | A data element to identify the whether the transactions in the file are original submissions of the data, a resubmission of a previously submitted file, or corrections of edit rejects. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV003-0001 |
| 3969 | PRV003 | SUBMISSION-TRANSACTION-TYPE | Must be populated on every record | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV003-0002 | |||
| 3970 | PRV003 | SUBMISSION-TRANSACTION-TYPE | Note: The records in an Update File are not generated as a result of a change processed in the state’s Medicaid or Medicaid-related systems during the current reporting month. These Update File record segments may be unchanged from the ones submitted previously for various reasons (For example, the state may be unable to process a change record in their Medicaid/Medicaid-related systems to correct the issue because the state is simply passing through to T-MSIS data that originated outside of the state’s systems.) Conversely, the records may be different from those previously submitted, but the change is the result of a fix whose root cause problem was an issue in the T-MSIS file creation process. Regardless, the record was not generated from a change that occurred in the state’s source data. | 2/25/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV003-0003 | |||
| 3971 | PRV004 | FILE-ENCODING-SPECIFICATION | A data element to denote whether the file is in fixed length line format or delimited format. | Required | Value must be in the set of valid values | FLF The file follows a fixed length format. PSV The file follows a pip-delimited format. |
4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV004-0001 |
| 3972 | PRV004 | FILE-ENCODING-SPECIFICATION | Must be populated on every record | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV004-0002 | |||
| 3973 | PRV005 | DATA-MAPPING-DOCUMENT-VERSION | A data element to identify the version of the T-MSIS data mapping document used to build the file. | Required | Use the version number specified on the title page of the data mapping document | 2/25/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV005-0001 | |
| 3974 | PRV006 | FILE-NAME | The name identifying the subject area to which the records in its file relate. Each T-MSIS submission file should only contain records for one subject area (i.e., Eligible, Third-party Liability, Provider, Managed Care Plan Information, IP claims, LT claims, Rx claims, or OT claims). | Required | Required on every file header record | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV006-0001 | |
| 3975 | PRV006 | FILE-NAME | Value must be equal to a valid value. | PROVIDER - Provider file |
4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV006-0002 | ||
| 3976 | PRV007 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV007-0001 |
| 3977 | PRV007 | SUBMITTING-STATE | Must be populated on every record | 2/25/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV007-0002 | |||
| 3978 | PRV007 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV007-0003 | |||
| 3979 | PRV007 | SUBMITTING-STATE | Value must be the same on all records | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV007-0004 | |||
| 3980 | PRV008 | DATE-FILE-CREATED | The date on which the file was created. | Required | Date format is CCYYMMDD (National Data Standard). | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV008-0001 | |
| 3981 | PRV008 | DATE-FILE-CREATED | The date must be a valid date. | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV008-0002 | |||
| 3982 | PRV008 | DATE-FILE-CREATED | Must be populated on every record | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV008-0003 | |||
| 3983 | PRV008 | DATE-FILE-CREATED | Date must be equal to or greater than the date entered in the START-OF-TIME-PERIOD field. | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV008-0004 | |||
| 3984 | PRV008 | DATE-FILE-CREATED | Date must be less than or equal to current date | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV008-0005 | |||
| 3985 | PRV009 | START-OF-TIME-PERIOD | Beginning date of the Month covered by this file. | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV009-0001 | |
| 3986 | PRV009 | START-OF-TIME-PERIOD | The date must be a valid date. | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV009-0002 | |||
| 3987 | PRV009 | START-OF-TIME-PERIOD | Must be populated on every record | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV009-0003 | |||
| 3988 | PRV009 | START-OF-TIME-PERIOD | Date must be less then current date | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV009-0004 | |||
| 3989 | PRV009 | START-OF-TIME-PERIOD | Value must be less than or equal to END-OF-TIME-PERIOD | 2/25/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV009-0005 | |||
| 3990 | PRV009 | START-OF-TIME-PERIOD | Date must be equal to or less than the date in the DATE-FILE-CREATED field. | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV009-0006 | |||
| 3991 | PRV010 | END-OF-TIME-PERIOD | Last date of the reporting period covered by the file to which this Header Record is Attached. |
Required | The date must be a valid date. | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV010-0001 | |
| 3992 | PRV010 | END-OF-TIME-PERIOD | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV010-0002 | |||
| 3993 | PRV010 | END-OF-TIME-PERIOD | Must be populated on every record | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV010-0003 | |||
| 3994 | PRV010 | END-OF-TIME-PERIOD | Date must be less then current date | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV010-0004 | |||
| 3995 | PRV010 | END-OF-TIME-PERIOD | Value must be equal to or greater than START-OF-TIME-PERIOD. | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV010-0005 | |||
| 3996 | PRV011 | FILE-STATUS-INDICATOR | A code to indicate whether the records in the file are test or production records. | Required | Value must be equal to a valid value. | P Production T Test |
2/25/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV011-0001 |
| 3997 | PRV011 | FILE-STATUS-INDICATOR | Must be populated on every record | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV011-0002 | |||
| 3998 | PRV011 | FILE-STATUS-INDICATOR | The dataset name and the value in this field must be consistent (i.e., the production dataset name cannot have a FILE-STATUS-INDICATOR = 'T' | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV011-0003 | |||
| 3999 | PRV013 | TOT-REC-CNT | A count of all records in the file except for the file header record. This count will be used as a control total to help assure that the file did not become corrupted during transmission. | Required | An integer value with no commas | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV013-0001 | |
| 4000 | PRV013 | TOT-REC-CNT | Value must equal the sum of all records excluding the header record | 4/30/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV013-0002 | |||
| 4001 | PRV138 | SEQUENCE-NUMBER | To enable state’s to sequentially number files, when related, follow-on files are necessary (i.e., update files, replacement files). This should begin with 1 for the original Create submission type and be incremented by one for each Replacement or Update submission for the same reporting period and file type (subject area). | Required | Field is required on all 'C', 'U', and 'R' record files. | 10/10/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV138-0001 | |
| 4002 | PRV138 | SEQUENCE-NUMBER | Must be numeric and > 0 | 10/10/2013 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV138-0002 | |||
| 4003 | PRV014 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV014-0001 | |
| 4004 | PRV014 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV014-0002 | |||
| 4005 | PRV012 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | PROVIDER | FILE-HEADER-RECORD-PROVIDER-PRV00001 | PRV012-0001 | |||
| 4006 | PRV016 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Value must be equal to a valid value. | PRV00002 PROV-ATTRIBUTES-MAIN |
4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV016-0001 |
| 4007 | PRV016 | RECORD-ID | Value is required on all record segments | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV016-0002 | |||
| 4008 | PRV016 | RECORD-ID | Value must be in the required format | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV016-0003 | |||
| 4009 | PRV016 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV016-0004 | |||
| 4010 | PRV017 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV017-0001 |
| 4011 | PRV017 | SUBMITTING-STATE | Must be populated on every record | 2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV017-0002 | |||
| 4012 | PRV017 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV017-0003 | |||
| 4013 | PRV017 | SUBMITTING-STATE | Value must be the same on all records | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV017-0004 | |||
| 4014 | PRV018 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Value must be an 11-digit integer with no commas. | 10/10/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV018-0001 | |
| 4015 | PRV018 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV018-0003 | |||
| 4016 | PRV019 | SUBMITTING-STATE-PROV-ID | The state-assigned unique identifier for the provider entity. Note that all individuals, practice groups, facilities, and other entities that provide Medicaid/CHIP goods or services to the state’s Medicaid/CHIP enrollees should be reflected in the T-MSIS provider data set. | Required | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV019-0001 | |
| 4017 | PRV020 | PROV-ATTRIBUTES-EFF-DATE | The first day of the time span during which the values in all data elements in the PROV-ATTRIBUTES-MAIN record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created.) This date field is necessary when defining a unique row in a database table. |
Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV020-0001 | |
| 4018 | PRV020 | PROV-ATTRIBUTES-EFF-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV020-0002 | |||
| 4019 | PRV020 | PROV-ATTRIBUTES-EFF-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV020-0003 | |||
| 4020 | PRV020 | PROV-ATTRIBUTES-EFF-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV020-0004 | |||
| 4021 | PRV020 | PROV-ATTRIBUTES-EFF-DATE | Whenever the value in one or more of the data elements in the PROV-ATTRIBUTES-MAIN record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV020-0005 | |||
| 4022 | PRV021 | PROV-ATTRIBUTES-END-DATE | The last day of the time span during which the values in all data elements in the PROV-ATTRIBUTES-MAIN record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Required | Date format is CCYYMMDD (National Data Standard). | 2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV021-0001 | |
| 4023 | PRV021 | PROV-ATTRIBUTES-END-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV021-0002 | |||
| 4024 | PRV021 | PROV-ATTRIBUTES-END-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV021-0003 | |||
| 4025 | PRV021 | PROV-ATTRIBUTES-END-DATE | Must be equal to or greater then eff date | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV021-0004 | |||
| 4026 | PRV021 | PROV-ATTRIBUTES-END-DATE | Whenever the value in one or more of the data elements in the PROV-ATTRIBUTES-MAIN record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV021-0005 | |||
| 4027 | PRV021 | PROV-ATTRIBUTES-END-DATE | Overlapping coverage not allowed for same Submitting state, Prov ID, and Record ID. | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV021-0006 | |||
| 4028 | PRV021 | PROV-ATTRIBUTES-END-DATE | The Date must be less then or equal to DATE-OF-DEATH | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV021-0007 | |||
| 4029 | PRV022 | PROV-DOING-BUSINESS-AS-NAME | The provider’s name that is commonly used by the public when the “doing-business-as” (`) name is different than the legal name. DBA is an abbreviation for "doing business as." Registering a DBA is required to operate a business under a name that differs from the company's legal name. | Required | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV022-0001 | |
| 4030 | PRV022 | PROV-DOING-BUSINESS-AS-NAME | Leave the field empty when the DBA name equals the legal name (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV022-0002 | |||
| 4031 | PRV022 | PROV-DOING-BUSINESS-AS-NAME | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV022-0003 | |||
| 4032 | PRV023 | PROV-LEGAL-NAME | The name as it appears on the provider agreement between the state and the entity. Both persons and other entities can have a legal name. | Required | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV023-0001 | |
| 4033 | PRV023 | PROV-LEGAL-NAME | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV023-0002 | |||
| 4034 | PRV023 | PROV-LEGAL-NAME | Every provider is expected to have a legal name. When the data element is not populated or used, the data element should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV023-0003 | |||
| 4035 | PRV023 | PROV-LEGAL-NAME | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV023-0004 | |||
| 4036 | PRV024 | PROV-ORGANIZATION-NAME | The name of the provider when the provider is an organization. | Required | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV024-0001 | |
| 4037 | PRV024 | PROV-ORGANIZATION-NAME | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV024-0002 | |||
| 4038 | PRV024 | PROV-ORGANIZATION-NAME | Provider Organization Name should be same as last name when provider is an individual | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV024-0003 | |||
| 4039 | PRV024 | PROV-ORGANIZATION-NAME | Enter the first 60 characters if the provider organization name exceeds 60 characters Enter the first 35 characters if the last name exceeds 35 bytes |
4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV024-0004 | |||
| 4040 | PRV024 | PROV-ORGANIZATION-NAME | Use PROV-LAST-NAME when the provider is a person. | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV024-0005 | |||
| 4041 | PRV024 | PROV-ORGANIZATION-NAME | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV024-0006 | |||
| 4042 | PRV025 | PROV-TAX-NAME | The name that the provider entity uses on IRS filings. | Required | Must be populated on every record. | 9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV025-0001 | |
| 4043 | PRV025 | PROV-TAX-NAME | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV025-0002 | |||
| 4044 | PRV025 | PROV-TAX-NAME | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV025-0003 | |||
| 4045 | PRV026 | FACILITY-GROUP-INDIVIDUAL-CODE | A code to identify whether the SUBMITTING-STATE-PROV-ID is assigned to an individual, a group of providers, or a facility. | Required | Value must be equal to a valid value. | 01 Facility – The entity identified by the associated SUBMITTING-STATE-PROV-ID is a facility. 02 Group – The entity identified by the associated SUBMITTING-STATE-PROV-ID is a group of individual practitioners. 03 Individual – The entity identified by the associated SUBMITTING-STATE-PROV-ID is an individual practitioner. |
4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV026-0001 |
| 4046 | PRV026 | FACILITY-GROUP-INDIVIDUAL-CODE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV026-0002 | |||
| 4047 | PRV026 | FACILITY-GROUP-INDIVIDUAL-CODE | Every SUBMITTING-STATE-PROV-ID must be classified using the codes in the valid values list |
2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV026-0003 | |||
| 4048 | PRV027 | TEACHING-IND | A code indicating if the provider’s organization is a teaching facility. | Conditional | Value must be equal to a valid value. | 0 No 1 Yes |
11/3/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV027-0001 |
| 4049 | PRV027 | TEACHING-IND | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV027-0002 | |||
| 4050 | PRV028 | PROV-FIRST-NAME | The first name of the provider when the provider is a person. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV028-0001 | |
| 4051 | PRV028 | PROV-FIRST-NAME | Leave blank if the provider is not a person. |
2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV028-0002 | |||
| 4052 | PRV028 | PROV-FIRST-NAME | Enter the first 35 characters if the first name exceeds 35 bytes | 2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV028-0003 | |||
| 4053 | PRV029 | PROV-MIDDLE-INITIAL | The middle initial of the provider when the provider is a person. | Conditional | Value must be an alphabetic character, or a blank (A-Z, a-z, ) | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV029-0001 | |
| 4054 | PRV029 | PROV-MIDDLE-INITIAL | Leave blank if not available |
2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV029-0002 | |||
| 4055 | PRV029 | PROV-MIDDLE-INITIAL | Leave blank when the provider is not an individual. | 2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV029-0003 | |||
| 4056 | PRV030 | PROV-LAST-NAME | The last name of the provider when the provider is a person. Use PROV-ORGANIZATION-NAME when the provider is an organization. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV030-0001 | |
| 4057 | PRV030 | PROV-LAST-NAME | Leave blank if the provider is not a person. |
2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV030-0002 | |||
| 4058 | PRV030 | PROV-LAST-NAME | Enter the first 35 characters if the first name exceeds 35 bytes | 2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV030-0003 | |||
| 4059 | PRV030 | PROV-LAST-NAME | If the provider is an organization, populate the provider organization name through using the PROV-ORGANIZATION-NAME data element | 2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV030-0004 | |||
| 4060 | PRV031 | SEX | The individual’s biological sex. | Conditional | If populated, the value must be in the list of valid values. | F Female M Male U Unknown |
4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV031-0001 |
| 4061 | PRV031 | SEX | Must be populated when provider is an individual | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV031-0002 | |||
| 4062 | PRV032 | OWNERSHIP-CODE | A code denoting the ownership interest and/or managing control information. The valid values list is a Medicare standard list. | Required | Value must be equal to a valid value. | 01 Voluntary – Non-Profit – Religious Organizations 02 Voluntary – Non-Profit – Other 03 Voluntary – multiple owners 04 Proprietary – Individual 05 Proprietary – Corporation 06 Proprietary – Partnership 07 Proprietary – Other 08 Proprietary – multiple owners 09 Government – Federal 10 Government – State 11 Government – City 12 Government – County 13 Government – City-County 14 Government – Hospital District 15 Government – State and City/County 16 Government – other multiple owners 17 Voluntary /Proprietary 18 Proprietary/Government 19 Voluntary/Government 88 N/A – The individual only practices as part of a group, e.g., as an employee |
10/10/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV032-0001 |
| 4063 | PRV032 | OWNERSHIP-CODE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV032-0002 | |||
| 4064 | PRV033 | PROV-PROFIT-STATUS | A code denoting the profit status of the provider. | Required | Value must be equal to a valid value. | 01 501(C)(3) NON-PROFIT 02 FOR-PROFIT, CLOSELY HELD 03 FOR-PROFIT, PUBLICLY TRADED 04 OTHER 88 N/A – The individual only practices as part of a group 99 Unknown |
4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV033-0001 |
| 4065 | PRV034 | DATE-OF-BIRTH | Date of birth of the provider. Applicable to individual providers only. | Conditional | Must be populated when provider is an individual | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV034-0001 | |
| 4066 | PRV034 | DATE-OF-BIRTH | Date format is CCYYMMDD (National Data Standard). |
2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV034-0002 | |||
| 4067 | PRV034 | DATE-OF-BIRTH | Date must be less than or equal to current date | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV034-0003 | |||
| 4068 | PRV035 | DATE-OF-DEATH | Date of death of the provider, if applicable. Applicable to individual providers only. | Conditional | Date format is CCYYMMDD (National Data Standard). |
2/25/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV035-0001 | |
| 4069 | PRV035 | DATE-OF-DEATH | Conditional | The date must be a valid date. | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV035-0002 | ||
| 4070 | PRV035 | DATE-OF-DEATH | Date of Death is greater than 0 when provider is not an individual | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV035-0003 | |||
| 4071 | PRV035 | DATE-OF-DEATH | Date must be less then current date | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV035-0004 | |||
| 4072 | PRV035 | DATE-OF-DEATH | Date is less then DATE-OF-BIRTH | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV035-0005 | |||
| 4073 | PRV035 | DATE-OF-DEATH | A provider with a date of death before the submission cannot be listed as a health home provider for an eligible individual. | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV035-0006 | |||
| 4074 | PRV035 | DATE-OF-DEATH | A provider with a date of death before the submission cannot be listed as a lockin provider for an eligible individual. | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV035-0007 | |||
| 4075 | PRV035 | DATE-OF-DEATH | Value must be equal to a valid value. | 4/30/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV035-0008 | |||
| 4076 | PRV036 | ACCEPTING-NEW-PATIENTS-IND | An indicator to identify providers who are accepting new patients | Required | Value must be equal to a valid value. | 0 No 1 Yes 8 N/A – The individual only practices as a member of a group. |
10/10/2013 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV036-0001 |
| 4077 | PRV037 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV037-0001 | |
| 4078 | PRV037 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV037-0002 | |||
| 4079 | PRV038 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | PROVIDER | PROV-ATTRIBUTES-MAIN-PRV00002 | PRV038-0001 | |||
| 4080 | PRV039 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Value must be equal to a valid value. | PRV00003 PROV-LOCATION-AND-CONTACT-INFO |
4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV039-0001 |
| 4081 | PRV039 | RECORD-ID | Value is required on all record segments | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV039-0002 | |||
| 4082 | PRV039 | RECORD-ID | Value must be in the required format | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV039-0003 | |||
| 4083 | PRV039 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV039-0004 | |||
| 4084 | PRV040 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV040-0001 |
| 4085 | PRV040 | SUBMITTING-STATE | Must be populated on every record | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV040-0002 | |||
| 4086 | PRV040 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV040-0003 | |||
| 4087 | PRV040 | SUBMITTING-STATE | Value must be the same on all records | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV040-0004 | |||
| 4088 | PRV041 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Value must be an 11-digit integer with no commas. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV041-0001 | |
| 4089 | PRV041 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV041-0002 | |||
| 4090 | PRV042 | SUBMITTING-STATE-PROV-ID | The state-assigned unique identifier for the provider entity. Note that all individuals, practice groups, facilities, and other entities that provide Medicaid/CHIP goods or services to the state’s Medicaid/CHIP enrollees should be reflected in the T-MSIS provider data set. | Required | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV042-0001 | |
| 4091 | PRV043 | PROV-LOCATION-ID | A code to uniquely identify the geographic locations where the provider performs services. These codes will also be reported in the PROV-LOCATION-ID field on CLAIM-HEADER-RECORD-IP, -LT, -OT, and –RX record segments | Required | Must be numeric | 10/10/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV043-0001 | |
| 4092 | PRV043 | PROV-LOCATION-ID | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV043-0002 | |||
| 4093 | PRV043 | PROV-LOCATION-ID | Each of a provider entity’s locations must have a unique PROV-LOCATION-ID | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV043-0003 | |||
| 4094 | PRV043 | PROV-LOCATION-ID | If a particular license is applicable to all locations, use the value ‘000’ value to represent ‘all’ locations. | 9/23/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV043-0004 | |||
| 4095 | PRV044 | PROV-LOCATION-AND-CONTACT-INFO-EFF-DATE | The first day of the time span during which the values in all data elements in the PROV-LOCATION-AND-CONTACT-INFO record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV044-0001 | |
| 4096 | PRV044 | PROV-LOCATION-AND-CONTACT-INFO-EFF-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV044-0002 | |||
| 4097 | PRV044 | PROV-LOCATION-AND-CONTACT-INFO-EFF-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV044-0003 | |||
| 4098 | PRV044 | PROV-LOCATION-AND-CONTACT-INFO-EFF-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV044-0004 | |||
| 4099 | PRV044 | PROV-LOCATION-AND-CONTACT-INFO-EFF-DATE | Must be equal to or less then end date | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV044-0005 | |||
| 4100 | PRV044 | PROV-LOCATION-AND-CONTACT-INFO-EFF-DATE | Whenever the value in one or more of the data elements in the PROV-LOCATION-AND-CONTACT-INFO record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV044-0006 | |||
| 4101 | PRV045 | PROV-LOCATION-AND-CONTACT-INFO-END-DATE | The last day of the time span during which the values in all data elements in the PROV-LOCATION-AND-CONTACT-INFO record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV045-0001 | |
| 4102 | PRV045 | PROV-LOCATION-AND-CONTACT-INFO-END-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV045-0002 | |||
| 4103 | PRV045 | PROV-LOCATION-AND-CONTACT-INFO-END-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV045-0003 | |||
| 4104 | PRV045 | PROV-LOCATION-AND-CONTACT-INFO-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV045-0004 | |||
| 4105 | PRV045 | PROV-LOCATION-AND-CONTACT-INFO-END-DATE | Whenever the value in one or more of the data elements in the PROV-LOCATION-AND-CONTACT-INFO record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV045-0005 | |||
| 4106 | PRV045 | PROV-LOCATION-AND-CONTACT-INFO-END-DATE | Must be equal to or greater then eff date | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV045-0006 | |||
| 4107 | PRV045 | PROV-LOCATION-AND-CONTACT-INFO-END-DATE | Overlapping coverage not allowed for same Submitting state & Prov ID, Location ID, Address Type | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV045-0007 | |||
| 4108 | PRV045 | PROV-LOCATION-AND-CONTACT-INFO-END-DATE | Active PRV-ATTRIBUTES-MAIN record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV045-0008 | |||
| 4109 | PRV045 | PROV-LOCATION-AND-CONTACT-INFO-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV045-0009 | |||
| 4110 | PRV046 | ADDR-TYPE | The type of address that is stored in the remaining address fields. The data elements in the PROV-LOCATION-AND-CONTACT-INFO record are intended to capture the physical address and other contact information related to a provider. Each PROV-LOCATION-AND-CONTACT-INFO record represents the set of contact information for a single provider location. |
Required | Value must be equal to a valid value. | 1 Billing Provider 2 Provider Mailing 3 Provider Practice 4 Provider Service Location |
2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV046-0001 |
| 4111 | PRV046 | ADDR-TYPE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV046-0002 | |||
| 4112 | PRV046 | ADDR-TYPE | The state can enter as many sets of contact information (i.e., multiple PROV-LOCATION-AND-CONTACT-INFO records) as it considers necessary. The value selected for the ADDR-TYPE field describes the type of contact information on that particular record (e.g., provider service location, provider billing address, etc.). The PROV-LOCATION-ID differentiates one PROV-LOCATION-AND-CONTACT-INFO record from another when the ADDR-TYPE value on both records is the same. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV046-0003 | |||
| 4113 | PRV047 | ADDR-LN1 | The street address, including the street name, street number, and room/suite number or letter, for the location being captured on the PROV-LOCATION-AND-CONTACT-INFO record. |
Required | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 10/10/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV047-0001 | |
| 4114 | PRV047 | ADDR-LN1 | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV047-0002 | |||
| 4115 | PRV047 | ADDR-LN1 | Line 1 is required and the other two lines can be blank. | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV047-0003 | |||
| 4116 | PRV048 | ADDR-LN2 | The street address, including the street name, street number, and room/suite number or letter, for the location being captured on the PROV-LOCATION-AND-CONTACT-INFO record. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV048-0001 | |
| 4117 | PRV048 | ADDR-LN2 | The data elements in the PROV-LOCATION-AND-CONTACT-INFO record are intended to capture the physical address and other contact information related to a provider. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV048-0002 | |||
| 4118 | PRV048 | ADDR-LN2 | Each PROV-LOCATION-AND-CONTACT-INFO record represents the set of contact information for a single provider location. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV048-0003 | |||
| 4119 | PRV048 | ADDR-LN2 | The state can enter as many sets of contact information (i.e., multiple PROV-LOCATION-AND-CONTACT-INFO records) as it considers necessary. The value selected for the ADDR-TYPE field describes the type of contact information on that particular record (e.g., provider service location, provider billing address, etc.). The PROV-LOCATION-ID differentiates one PROV-LOCATION-AND-CONTACT-INFO record from another when the ADDR-TYPE value on both records is the same. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV048-0004 | |||
| 4120 | PRV048 | ADDR-LN2 | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV048-0005 | |||
| 4121 | PRV049 | ADDR-LN3 | The street address, including the street name, street number, and room/suite number or letter, for the location being captured on the PROV-LOCATION-AND-CONTACT-INFO record. |
Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
11/3/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV049-0001 | |
| 4122 | PRV049 | ADDR-LN3 | The third line of the address must not be the same as the first or second line of the address (if applicable) | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV049-0002 | |||
| 4123 | PRV049 | ADDR-LN3 | The data elements in the PROV-LOCATION-AND-CONTACT-INFO record are intended to capture the physical address and other contact information related to a provider. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV049-0003 | |||
| 4124 | PRV049 | ADDR-LN3 | Each PROV-LOCATION-AND-CONTACT-INFO record represents the set of contact information for a single provider location. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV049-0004 | |||
| 4125 | PRV049 | ADDR-LN3 | The state can enter as many sets of contact information (i.e., multiple PROV-LOCATION-AND-CONTACT-INFO records) as it considers necessary. The value selected for the ADDR-TYPE field describes the type of contact information on that particular record (e.g., provider service location, provider billing address, etc.). The PROV-LOCATION-ID differentiates one PROV-LOCATION-AND-CONTACT-INFO record from another when the ADDR-TYPE value on both records is the same. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV049-0005 | |||
| 4126 | PRV049 | ADDR-LN3 | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV049-0006 | |||
| 4127 | PRV050 | ADDR-CITY | The city name for the location being captured on the PROV-LOCATION-AND-CONTACT-INFO record. |
Required | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV050-0001 | |
| 4128 | PRV050 | ADDR-CITY | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV050-0002 | |||
| 4129 | PRV050 | ADDR-CITY | The data elements in the PROV-LOCATION-AND-CONTACT-INFO record are intended to capture the physical address and other contact information related to a provider. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV050-0003 | |||
| 4130 | PRV050 | ADDR-CITY | Each PROV-LOCATION-AND-CONTACT-INFO record represents the set of contact information for a single provider location. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV050-0004 | |||
| 4131 | PRV050 | ADDR-CITY | The state can enter as many sets of contact information (i.e., multiple PROV-LOCATION-AND-CONTACT-INFO records) as it considers necessary. The value selected for the ADDR-TYPE field describes the type of contact information on that particular record (e.g., provider service location, provider billing address, etc.). The PROV-LOCATION-ID differentiates one PROV-LOCATION-AND-CONTACT-INFO record from another when the ADDR-TYPE value on both records is the same. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV050-0005 | |||
| 4132 | PRV051 | ADDR-STATE | The two letter ANSI state numeric code for each U.S. state, territory, and the District of Columbia for the location being captured on the PROV-LOCATION-AND-CONTACT-INFO record. |
Required | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV051-0001 | |
| 4133 | PRV051 | ADDR-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV051-0002 | ||
| 4134 | PRV051 | ADDR-STATE | The data elements in the PROV-LOCATION-AND-CONTACT-INFO record are intended to capture the physical address and other contact information related to a provider. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV051-0003 | |||
| 4135 | PRV051 | ADDR-STATE | Each PROV-LOCATION-AND-CONTACT-INFO record represents the set of contact information for a single provider location. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV051-0004 | |||
| 4136 | PRV051 | ADDR-STATE | The state can enter as many sets of contact information (i.e., multiple PROV-LOCATION-AND-CONTACT-INFO records) as it considers necessary. The value selected for the ADDR-TYPE field describes the type of contact information on that particular record (e.g., provider service location, provider billing address, etc.). The PROV-LOCATION-ID differentiates one PROV-LOCATION-AND-CONTACT-INFO record from another when the ADDR-TYPE value on both records is the same. | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV051-0005 | |||
| 4137 | PRV052 | ADDR-ZIP-CODE | The Zip Code for the location being captured on the PROV-LOCATION-AND-CONTACT-INFO record. |
Required | Value must be numeric | 9/23/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV052-0001 | |
| 4138 | PRV052 | ADDR-ZIP-CODE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV052-0002 | |||
| 4139 | PRV052 | ADDR-ZIP-CODE | If the last 4 digits are not populated or used, then the 4-digit extended zip code should be recorded as “0000”. | 9/23/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV052-0003 | |||
| 4140 | PRV053 | ADDR-TELEPHONE | Enter the digits only (i.e., without parentheses, brackets, dashes, periods, spaces, etc.) | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV053-0001 | |||
| 4141 | PRV053 | ADDR-TELEPHONE | The telephone number for the location being captured on the PROV-LOCATION-AND-CONTACT-INFO record. |
Optional | Must be populated on every record | 11/3/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV053-0002 | |
| 4142 | PRV053 | ADDR-TELEPHONE | Value must be numeric | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV053-0003 | |||
| 4143 | PRV053 | ADDR-TELEPHONE | Enter 10-digit telephone number (includes area code) | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV053-0004 | |||
| 4144 | PRV053 | ADDR-TELEPHONE | If unknown, can be filled using 9’s | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV053-0005 | |||
| 4145 | PRV053 | ADDR-TELEPHONE | Enter numerals only (no parentheses, dashes, periods, etc.) | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV053-0006 | |||
| 4146 | PRV054 | ADDR-EMAIL | The email address of the provider for the location being captured on the PROV-LOCATION-AND-CONTACT-INFO record |
Optional | Must contain @ | 11/3/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV054-0001 | |
| 4147 | PRV054 | ADDR-EMAIL | Must have [email protected] format | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV054-0002 | |||
| 4148 | PRV054 | ADDR-EMAIL | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV054-0003 | |||
| 4149 | PRV055 | ADDR-FAX-NUM | The fax number of the provider for the location being captured on the PROV-LOCATION-AND-CONTACT-INFO record. | Optional | Enter the digits only (i.e., without parentheses, brackets, dashes, periods, spaces, etc.) | 11/3/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV055-0001 | |
| 4150 | PRV055 | ADDR-FAX-NUM | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV055-0002 | |||
| 4151 | PRV055 | ADDR-FAX-NUM | Value must be numeric | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV055-0003 | |||
| 4152 | PRV055 | ADDR-FAX-NUM | Valid fax number including the area code. |
2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV055-0004 | |||
| 4153 | PRV055 | ADDR-FAX-NUM | If unknown, can be filled using 9’s | 2/25/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV055-0005 | |||
| 4154 | PRV056 | ADDR-BORDER-STATE-IND | A code indicating that the location is outside of state boundaries for the location being captured on the PROV-LOCATION-AND-CONTACT-INFO record. (The provider location is out of state, but for payment purposes the provider is treated as an in-state provider.) | Required | Value must be equal to a valid value | 0 No 1 Yes 8 State does not distinguish “border state providers”. |
9/23/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV056-0001 |
| 4155 | PRV056 | ADDR-BORDER-STATE-IND | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV056-0002 | |||
| 4156 | PRV056 | ADDR-BORDER-STATE-IND | Value must be numeric | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV056-0003 | |||
| 4157 | PRV056 | ADDR-BORDER-STATE-IND | If unknown, can be filled using 9s | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV056-0004 | |||
| 4158 | PRV057 | ADDR-COUNTY | The ANSI county code for the location being captured on the PROV-LOCATION-AND-CONTACT-INFO record. |
Required | Dependent value must be equal to a valid value. | http://www.census.gov/geo/reference/codes/cou.html | 10/10/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV057-0001 |
| 4159 | PRV057 | ADDR-COUNTY | Must be populated on every record | 10/10/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV057-0002 | |||
| 4160 | PRV057 | ADDR-COUNTY | Value must be numeric | 4/30/2013 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV057-0003 | |||
| 4161 | PRV058 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV058-0001 | |
| 4162 | PRV058 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV058-0002 | |||
| 4163 | PRV059 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | PROVIDER | PROV-LOCATION-AND-CONTACT-INFO-PRV00003 | PRV059-0001 | |||
| 4164 | PRV060 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Value must be equal to a valid value. | PRV00004 PROV-LICENSING-INFO |
4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV060-0001 |
| 4165 | PRV060 | RECORD-ID | Value is required on all record segments | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV060-0002 | |||
| 4166 | PRV060 | RECORD-ID | Value must be in the required format | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV060-0003 | |||
| 4167 | PRV060 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV060-0004 | |||
| 4168 | PRV061 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV061-0001 |
| 4169 | PRV061 | SUBMITTING-STATE | Must be populated on every record | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV061-0002 | |||
| 4170 | PRV061 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV061-0003 | |||
| 4171 | PRV061 | SUBMITTING-STATE | Value must be the same on all records | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV061-0004 | |||
| 4172 | PRV062 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Value must be an 11-digit integer with no commas. | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV062-0001 | |
| 4173 | PRV062 | RECORD-NUMBER | Must be numeric | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV062-0002 | |||
| 4174 | PRV062 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV062-0003 | |||
| 4175 | PRV063 | SUBMITTING-STATE-PROV-ID | The state-assigned unique identifier for the provider entity. Note that all individuals, practice groups, facilities, and other entities that provide Medicaid/CHIP goods or services to the state’s Medicaid/CHIP enrollees should be reflected in the T-MSIS provider data set. | Conditional | Must be populated on every record | 11/3/2015 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV063-0001 | |
| 4176 | PRV064 | PROV-LOCATION-ID | A code to uniquely identify the geographic locations where the provider performs services. These codes will also be reported in the PROV-LOCATION-ID field on CLAIM-HEADER-RECORD-IP, -LT, -OT, and –RX record segments | Conditional | Must be numeric | 11/3/2015 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV064-0001 | |
| 4177 | PRV064 | PROV-LOCATION-ID | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV064-0002 | |||
| 4178 | PRV064 | PROV-LOCATION-ID | Each of a provider entity’s locations must have a unique PROV-LOCATION-ID | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV064-0003 | |||
| 4179 | PRV064 | PROV-LOCATION-ID | If a particular license is applicable to all locations, use the value ‘000’ value to represent ‘all’ locations. | 9/23/2015 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV064-0004 | |||
| 4180 | PRV065 | PROV-LICENSE-EFF-DATE | The first day of the time span during which the values in all data elements in the PROV-LICENSING-INFO record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created.) This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV065-0001 | |
| 4181 | PRV065 | PROV-LICENSE-EFF-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV065-0002 | |||
| 4182 | PRV065 | PROV-LICENSE-EFF-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV065-0003 | |||
| 4183 | PRV065 | PROV-LICENSE-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV065-0004 | |||
| 4184 | PRV065 | PROV-LICENSE-EFF-DATE | Must be equal to or less then end date | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV065-0005 | |||
| 4185 | PRV065 | PROV-LICENSE-EFF-DATE | Whenever the value in one or more of the data elements in the PROV-LICENSING-INFO record segment changes, a new record segment must be created. | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV065-0006 | |||
| 4186 | PRV066 | PROV-LICENSE-END-DATE | The last day of the time span during which the values in all data elements in the PROV-LICENSING-INFO record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created) | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV066-0001 | |
| 4187 | PRV066 | PROV-LICENSE-END-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV066-0002 | |||
| 4188 | PRV066 | PROV-LICENSE-END-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV066-0003 | |||
| 4189 | PRV066 | PROV-LICENSE-END-DATE | Whenever the value in one or more of the data elements in the PROV-LICENSING-INFO record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV066-0004 | |||
| 4190 | PRV066 | PROV-LICENSE-END-DATE | Must be equal to or greater then eff date | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV066-0005 | |||
| 4191 | PRV066 | PROV-LICENSE-END-DATE | Overlapping coverage not allowed for same Submitting state & Prov ID, Location ID, License Type, License Issuing Entity ID | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV066-0006 | |||
| 4192 | PRV066 | PROV-LICENSE-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV066-0007 | |||
| 4193 | PRV066 | PROV-LICENSE-END-DATE | Active PRV-ATTRIBUTES-MAIN & PRV-LOCATION-CONTACT-INFO record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV066-0008 | |||
| 4194 | PRV067 | LICENSE-TYPE | A code to identify the kind of license or accreditation number that is captured in the LICENSE-OR-ACCREDITATION-NUMBER data element. | Conditional | Value must be equal to a valid value. | 1 State, county, or municipality professional or business license 2 DEA license 3 Professional society accreditation 4 CLIA accreditation 5 Other |
11/3/2015 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV067-0001 |
| 4195 | PRV067 | LICENSE-TYPE | Conditional | Must be populated on every record | 11/3/2015 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV067-0002 | ||
| 4196 | PRV067 | LICENSE-TYPE | Required whenever a Medicaid/CHIP provider is required by the state’s Medicaid/CHIP agency requires one in order to be a Medicaid/CHIP provider. | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV067-0003 | |||
| 4197 | PRV067 | LICENSE-TYPE | If unknown, enter “9.”. | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV067-0004 | |||
| 4198 | PRV068 | LICENSE-ISSUING-ENTITY-ID | A free text field to capture the identity of the entity issuing the license or accreditation. | Conditional | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. |
11/3/2015 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV068-0001 | |
| 4199 | PRV068 | LICENSE-ISSUING-ENTITY-ID | (Enter the applicable state code, county code, municipality name, "DEA", professional society's name, or the CLIA accreditation body's name.) | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV068-0002 | |||
| 4200 | PRV068 | LICENSE-ISSUING-ENTITY-ID | Required whenever a value is captured in the LICENSE-OR-ACCREDITATION-NUMBER data element. | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV068-0003 | |||
| 4201 | PRV068 | LICENSE-ISSUING-ENTITY-ID | If LICENSE-TYPE = 1 (State, county, or municipality professional or business license) and the license-issuing entity is a state, then enter the applicable ANSI state numeric code. | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV068-0004 | |||
| 4202 | PRV068 | LICENSE-ISSUING-ENTITY-ID | If LICENSE-TYPE = 1 (State, county, or municipality professional or business license) and the license-issuing entity is a county, then enter a 5-digit, concatenated code consisting of the ANSI state numeric code plus the ANSI county numeric code of the applicable. | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV068-0005 | |||
| 4203 | PRV068 | LICENSE-ISSUING-ENTITY-ID | If LICENSE-TYPE = 1 (State, county, or municipality professional or business license) and the license-issuing entity is a municipality, then enter a text string with the name of the municipality. | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV068-0006 | |||
| 4204 | PRV068 | LICENSE-ISSUING-ENTITY-ID | If LICENSE-TYPE = 1 (State, county, or municipality professional or business license) and the license-issuing entity is a municipality, then enter a text string with the name of the municipality. | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV068-0007 | |||
| 4205 | PRV068 | LICENSE-ISSUING-ENTITY-ID | If LICENSE-TYPE = 2 (DEA license), then enter the text string “DEA”. | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV068-0008 | |||
| 4206 | PRV068 | LICENSE-ISSUING-ENTITY-ID | If LICENSE-TYPE = 3 (Professional society accreditation), then enter the text string identifying the professional society issuing the accreditation | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV068-0009 | |||
| 4207 | PRV068 | LICENSE-ISSUING-ENTITY-ID | If LICENSE-TYPE = 4 (CLIA accreditation), then enter the text string identifying the CLIA accreditation body’s name | 2/25/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV068-0010 | |||
| 4208 | PRV069 | LICENSE-OR-ACCREDITATION-NUMBER | A data element to capture the license or accreditation number issued to the provider by the licensing entity or accreditation body identified in the LICENSE-ISSUING-ENTITY-ID data element. | Conditional | Required whenever the LICENSE-TYPE and LICENSE-ISSUING-ENTITY-ID data elements are populated | 11/3/2015 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV069-0001 | |
| 4209 | PRV069 | LICENSE-OR-ACCREDITATION-NUMBER | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. |
4/30/2013 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV069-0002 | |||
| 4210 | PRV070 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV070-0001 | |
| 4211 | PRV070 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV070-0002 | |||
| 4212 | PRV071 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | PROVIDER | PROV-LICENSING-INFO-PRV00004 | PRV071-0001 | |||
| 4213 | PRV072 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Value must be in the set of valid values | PRV00005 PROV-IDENTIFIERS |
4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV072-0001 |
| 4214 | PRV072 | RECORD-ID | Value is required on all record segments | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV072-0002 | |||
| 4215 | PRV072 | RECORD-ID | Value must be in the required format | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV072-0003 | |||
| 4216 | PRV072 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV072-0004 | |||
| 4217 | PRV073 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be in the set of valid values | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV073-0001 |
| 4218 | PRV073 | SUBMITTING-STATE | Must be populated on every record | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV073-0002 | |||
| 4219 | PRV073 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV073-0003 | |||
| 4220 | PRV073 | SUBMITTING-STATE | Value must be the same on all records | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV073-0004 | |||
| 4221 | PRV074 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Value must be an 11-digit integer with no commas. | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV074-0001 | |
| 4222 | PRV074 | RECORD-NUMBER | Must be numeric | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV074-0002 | |||
| 4223 | PRV074 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV074-0003 | |||
| 4224 | PRV075 | SUBMITTING-STATE-PROV-ID | The state-assigned unique identifier for the provider entity. Note that all individuals, practice groups, facilities, and other entities that provide Medicaid/CHIP goods or services to the state’s Medicaid/CHIP enrollees should be reflected in the T-MSIS provider data set. | Required | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV075-0001 | |
| 4225 | PRV076 | PROV-LOCATION-ID | A code to uniquely identify the geographic locations where the provider performs services. These codes will also be reported in the PROV-LOCATION-ID field on CLAIM-HEADER-RECORD-IP, -LT, -OT, and –RX record segments | Required | Must be numeric | 10/10/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV076-0001 | |
| 4226 | PRV076 | PROV-LOCATION-ID | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV076-0002 | |||
| 4227 | PRV076 | PROV-LOCATION-ID | Each of a provider entity’s locations must have a unique PROV-LOCATION-ID | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV076-0003 | |||
| 4228 | PRV076 | PROV-LOCATION-ID | If a particular license is applicable to all locations, use the value ‘000’ value to represent ‘all’ locations. | 9/23/2015 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV076-0004 | |||
| 4229 | PRV077 | PROV-IDENTIFIER-TYPE | A code to identify the kind of provider identifier that is captured in the PROV-IDENTIFER data element. | Required | Value must be equal to a valid value. | 1 State-specific Medicaid Provider ID 2 NPI 3 Medicare ID 4 NCPDP ID 5 Federal Tax ID 6 State Tax ID 7 SSN 8 Other |
4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV077-0001 |
| 4230 | PRV077 | PROV-IDENTIFIER-TYPE | Required whenever a value is captured in the PROV-IDENTIFER data element. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV077-0002 | |||
| 4231 | PRV077 | PROV-IDENTIFIER-TYPE | The state should provide the identifiers associated with the provider for identifier types 1 through 7 whenever it is applicable to the provider. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV077-0003 | |||
| 4232 | PRV077 | PROV-IDENTIFIER-TYPE | The state should submit updates to T-MSIS whenever an identifier is retired or issued. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV077-0004 | |||
| 4233 | PRV078 | PROV-IDENTIFIER-ISSUING-ENTITY-ID | A free text field to capture the identity of the entity that issued the provider identifier in the PROV-IDENTIFER data element. | Required | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. |
4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV078-0001 | |
| 4234 | PRV078 | PROV-IDENTIFIER-ISSUING-ENTITY-ID | Required whenever a value is captured in the PROV-IDENTIFER data element. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV078-0002 | |||
| 4235 | PRV078 | PROV-IDENTIFIER-ISSUING-ENTITY-ID | If PROV-IDENTIFIER-TYPE = 1 (State-specific Medicaid Provider ID), then enter the applicable ANSI state numeric code. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV078-0003 | |||
| 4236 | PRV078 | PROV-IDENTIFIER-ISSUING-ENTITY-ID | If PROV-IDENTIFIER-TYPE = 2 (NPI), then enter “CMS.” | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV078-0004 | |||
| 4237 | PRV078 | PROV-IDENTIFIER-ISSUING-ENTITY-ID | If PROV-IDENTIFIER-TYPE = 3 (Medicare). Then enter “CMS” | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV078-0005 | |||
| 4238 | PRV078 | PROV-IDENTIFIER-ISSUING-ENTITY-ID | If PROV-IDENTIFIER-TYPE = 4 (NCPDP ID) then enter “NCPDP” | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV078-0006 | |||
| 4239 | PRV078 | PROV-IDENTIFIER-ISSUING-ENTITY-ID | If PROV-IDENTIFIER-TYPE = 5 (Federal Tax ID), then enter the text string “IRS”. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV078-0007 | |||
| 4240 | PRV078 | PROV-IDENTIFIER-ISSUING-ENTITY-ID | If PROV-IDENTIFIER-TYPE = 6 (State Tax ID), then text string of the name of the state’s taxation division.. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV078-0008 | |||
| 4241 | PRV078 | PROV-IDENTIFIER-ISSUING-ENTITY-ID | If PROV-IDENTIFIER-TYPE = 8 (Other), then enter the name of the entity. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV078-0009 | |||
| 4242 | PRV079 | PROV-IDENTIFIER-EFF-DATE | The first day of the time span during which the values in all data elements in the PROV-IDENTIFIERS record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV079-0001 | |
| 4243 | PRV079 | PROV-IDENTIFIER-EFF-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV079-0002 | |||
| 4244 | PRV079 | PROV-IDENTIFIER-EFF-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV079-0003 | |||
| 4245 | PRV079 | PROV-IDENTIFIER-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV079-0004 | |||
| 4246 | PRV079 | PROV-IDENTIFIER-EFF-DATE | Whenever the value in one or more of the data elements in the PROV-LICENSING-INFO record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV079-0005 | |||
| 4247 | PRV079 | PROV-IDENTIFIER-EFF-DATE | Must be equal to or less then end date | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV079-0006 | |||
| 4248 | PRV080 | PROV-IDENTIFIER-END-DATE | The last day of the time span during which the values in all data elements in the PROV-IDENTIFIERS record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created.) | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV080-0001 | |
| 4249 | PRV080 | PROV-IDENTIFIER-END-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV080-0002 | |||
| 4250 | PRV080 | PROV-IDENTIFIER-END-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV080-0003 | |||
| 4251 | PRV080 | PROV-IDENTIFIER-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV080-0004 | |||
| 4252 | PRV080 | PROV-IDENTIFIER-END-DATE | Whenever the value in one or more of the data elements in the PROV-LICENSING-INFO record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV080-0005 | |||
| 4253 | PRV080 | PROV-IDENTIFIER-END-DATE | Must be equal to or greater then eff date | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV080-0006 | |||
| 4254 | PRV080 | PROV-IDENTIFIER-END-DATE | Overlapping coverage not allowed for same Submitting state & Prov ID, Location ID, Prov Identifier Type, Prov Identifier | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV080-0007 | |||
| 4255 | PRV080 | PROV-IDENTIFIER-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV080-0008 | |||
| 4256 | PRV080 | PROV-IDENTIFIER-END-DATE | Active PRV-ATTRIBUTES-MAIN & PRV-LOCATION-CONTACT-INFO record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV080-0009 | |||
| 4257 | PRV081 | PROV-IDENTIFIER | A data element to capture the various ways used to distinguish providers from one another on claims and other interactions between providers and other entities. The specific type of identifier is shown in the corresponding value in the IDENTIFIER-TYPE data element. | Required | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. |
9/23/2015 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV081-0001 | |
| 4258 | PRV081 | PROV-IDENTIFIER | The value in the PROV-IDENTIFIER data element should be a valid value in the enumeration entity’s identification schema. | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV081-0002 | |||
| 4259 | PRV081 | PROV-IDENTIFIER | The state should submit updates to T-MSIS whenever an identifier is retired or issued | 2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV081-0003 | |||
| 4260 | PRV081 | PROV-IDENTIFIER | The state should provide the identifiers associated with the provider for identifier types 1 through 7 whenever it is applicable to the provider Conditions When CMS Expects a PROV-IDENTIFIER Value: • State-specific Medicaid Provider ID (the state should supply this identifier for every provider, since it is the state itself that is using the identifier in its MMIS.) • NPI (the state should supply this identifier for every provider who is issued an NPI). • Medicare ID (the state should supply this identifier for every provider who is issued a Medicare ID) • NCPDP ID (The state should supply this for every pharmacy.) • Federal Tax ID (the state should supply this identifier for every provider who uses a federal TIN as its identifier with the IRS.) • State Tax ID (the state should supply this identifier for every provider who uses a state TIN as its identifier with the state tax authority.) • SSN (the state should supply this identifier for every provider who uses a social security number as his/her identifier with the IRS and/or the state tax authority.) • Other (whenever the state uses an identifier type other than those listed above that it believes would be useful to analysts using the state’s Medicaid/CHIP data.) |
2/25/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV081-0004 | |||
| 4261 | PRV081 | PROV-IDENTIFIER | The PROV-IDENTIFIER data element must be populated whenever the PROV-IDENTIFIER-TYPE is populated | 4/30/2013 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV081-0005 | |||
| 4262 | PRV082 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV082-0001 | |
| 4263 | PRV082 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV082-0002 | |||
| 4264 | PRV083 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | PROVIDER | PROV-IDENTIFIERS-PRV00005 | PRV083-0001 | |||
| 4265 | PRV084 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Value must be equal to a valid value. | PRV00006 PROV-TAXONOMY-CLASSIFICATION |
4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV084-0001 |
| 4266 | PRV084 | RECORD-ID | Value is required on all record segments | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV084-0002 | |||
| 4267 | PRV084 | RECORD-ID | Value must be in the required format | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV084-0003 | |||
| 4268 | PRV084 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV084-0004 | |||
| 4269 | PRV085 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV085-0001 |
| 4270 | PRV085 | SUBMITTING-STATE | Must be populated on every record | 2/25/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV085-0002 | |||
| 4271 | PRV085 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV085-0003 | |||
| 4272 | PRV085 | SUBMITTING-STATE | Value must be the same on all records | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV085-0004 | |||
| 4273 | PRV086 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Value must be an 11-digit integer with no commas. | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV086-0001 | |
| 4274 | PRV086 | RECORD-NUMBER | Must be numeric | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV086-0002 | |||
| 4275 | PRV086 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV086-0003 | |||
| 4276 | PRV087 | SUBMITTING-STATE-PROV-ID | The state-assigned unique identifier for the provider entity. Note that all individuals, practice groups, facilities, and other entities that provide Medicaid/CHIP goods or services to the state’s Medicaid/CHIP enrollees should be reflected in the T-MSIS provider data set. | Required | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV087-0001 | |
| 4277 | PRV088 | PROV-CLASSIFICATION-TYPE | A code to identify the schema used in the PROV-CLASSIFICATION-CODE field to categorize providers. | Required | Value must be equal to a valid value. | 1 Taxonomy code 2 Provider specialty code 3 Provider type code 4 Authorized category of service code NOTE: The valid value code ‘47’ in the PROV-CLASSIFICATION-TYPE = 2 (Provider Specialty Code) can be used now. “47" = Independent Diagnostic Testing Facility (IDTF)” |
9/23/2015 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV088-0001 |
| 4278 | PRV088 | PROV-CLASSIFICATION-TYPE | Required on every PROV-TAXONOMY-CLASSIFICATION record | 2/25/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV088-0002 | |||
| 4279 | PRV088 | PROV-CLASSIFICATION-TYPE | Provide a value for all 4 provider classification types. Each provider should have a separate PROV-TAXONOMY-CLASSIFICATION-PRV00006 record segment for each of the values – Taxonomy Code, Provider Specialty Code, Provider Type Code, & Authorized Category of Service Code – unless one of the values is not applicable to that provider. | 10/10/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV088-0003 | |||
| 4280 | PRV089 | PROV-CLASSIFICATION-CODE | The code values from the categorization schema identified in the PROV-CLASSIFICATION-TYPE data element. Valid value lists for each PROV-CLASSIFICATION-TYPE code are listed. Note: States should apply these classification schemas consistently across all providers. |
Required | Dependent value must be equal to a valid value. | See Appendix A for listing of valid values. | 9/23/2015 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV089-0001 |
| 4281 | PRV089 | PROV-CLASSIFICATION-CODE | Required on every PROV-TAXONOMY-CLASSIFICATION segment. | 10/10/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV089-0002 | |||
| 4282 | PRV089 | PROV-CLASSIFICATION-CODE | The value in the PROV-CLASSIFICATION-CODE data element must correspond to the valid values set identified in the PROV-CLASSIFICATION-TYPE data element. | 2/25/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV089-0003 | |||
| 4283 | PRV090 | PROV-TAXONOMY-CLASSIFICATION-EFF-DATE | The first day of the time span during which the values in all data elements in the PROV-TAXONOMY-CLASSIFICATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV090-0001 | |
| 4284 | PRV090 | PROV-TAXONOMY-CLASSIFICATION-EFF-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV090-0002 | |||
| 4285 | PRV090 | PROV-TAXONOMY-CLASSIFICATION-EFF-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV090-0003 | |||
| 4286 | PRV090 | PROV-TAXONOMY-CLASSIFICATION-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV090-0004 | |||
| 4287 | PRV090 | PROV-TAXONOMY-CLASSIFICATION-EFF-DATE | Whenever the value in one or more of the data elements in the PROV-LICENSING-INFO record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV090-0005 | |||
| 4288 | PRV090 | PROV-TAXONOMY-CLASSIFICATION-EFF-DATE | Must be equal to or less then end date | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV090-0006 | |||
| 4289 | PRV091 | PROV-TAXONOMY-CLASSIFICATION-END-DATE | The last day of the time span during which the values in all data elements in the PROV-TAXONOMY-CLASSIFICATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Required | Date format is CCYYMMDD (National Data Standard) | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV091-0001 | |
| 4290 | PRV091 | PROV-TAXONOMY-CLASSIFICATION-END-DATE | The date must be a valid date. | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV091-0002 | |||
| 4291 | PRV091 | PROV-TAXONOMY-CLASSIFICATION-END-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV091-0003 | |||
| 4292 | PRV091 | PROV-TAXONOMY-CLASSIFICATION-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV091-0004 | |||
| 4293 | PRV091 | PROV-TAXONOMY-CLASSIFICATION-END-DATE | Whenever the value in one or more of the data elements in the PROV-LICENSING-INFO record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV091-0005 | |||
| 4294 | PRV091 | PROV-TAXONOMY-CLASSIFICATION-END-DATE | Must be equal to or greater then eff date | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV091-0006 | |||
| 4295 | PRV091 | PROV-TAXONOMY-CLASSIFICATION-END-DATE | Overlapping coverage not allowed for same Submitting state & Prov ID, Classification Type, Classification Code | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV091-0007 | |||
| 4296 | PRV091 | PROV-TAXONOMY-CLASSIFICATION-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV091-0008 | |||
| 4297 | PRV091 | PROV-TAXONOMY-CLASSIFICATION-END-DATE | Active PRV-ATTRIBUTES-MAIN record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV091-0009 | |||
| 4298 | PRV092 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV092-0001 | |
| 4299 | PRV092 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV092-0002 | |||
| 4300 | PRV093 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | PROVIDER | PROV-TAXONOMY-CLASSIFICATION-PRV00006 | PRV093-0001 | |||
| 4301 | PRV094 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Value must be equal to a valid value. | PRV00007 PROV-MEDICAID-ENROLLMENT |
4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV094-0001 |
| 4302 | PRV094 | RECORD-ID | Value is required on all record segments | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV094-0002 | |||
| 4303 | PRV094 | RECORD-ID | Value must be in the required format | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV094-0003 | |||
| 4304 | PRV094 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV094-0004 | |||
| 4305 | PRV095 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV095-0001 |
| 4306 | PRV095 | SUBMITTING-STATE | Must be populated on every record | 2/25/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV095-0002 | |||
| 4307 | PRV095 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV095-0003 | |||
| 4308 | PRV095 | SUBMITTING-STATE | Value must be the same on all records | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV095-0004 | |||
| 4309 | PRV096 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Value must be an 11-digit integer with no commas. | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV096-0001 | |
| 4310 | PRV096 | RECORD-NUMBER | Must be numeric | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV096-0002 | |||
| 4311 | PRV096 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV096-0003 | |||
| 4312 | PRV097 | SUBMITTING-STATE-PROV-ID | The state-assigned unique identifier for the provider entity. Note that all individuals, practice groups, facilities, and other entities that provide Medicaid/CHIP goods or services to the state’s Medicaid/CHIP enrollees should be reflected in the T-MSIS provider data set. | Required | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV097-0001 | |
| 4313 | PRV098 | PROV-MEDICAID-EFF-DATE | The first day of the time span during which the values in all data elements on a PROV-MEDICAID record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV098-0001 | |
| 4314 | PRV098 | PROV-MEDICAID-EFF-DATE | The date must be a valid date. | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV098-0002 | |||
| 4315 | PRV098 | PROV-MEDICAID-EFF-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV098-0003 | |||
| 4316 | PRV098 | PROV-MEDICAID-EFF-DATE | Must be numeric | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV098-0004 | |||
| 4317 | PRV098 | PROV-MEDICAID-EFF-DATE | Must be equal to or less then end date | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV098-0005 | |||
| 4318 | PRV099 | PROV-MEDICAID-END-DATE | The last day of the time span during which the values in all data elements on a PROV-MEDICAID record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV099-0001 | |
| 4319 | PRV099 | PROV-MEDICAID-END-DATE | The date must be a valid date. | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV099-0002 | |||
| 4320 | PRV099 | PROV-MEDICAID-END-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV099-0003 | |||
| 4321 | PRV099 | PROV-MEDICAID-END-DATE | Must be numeric | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV099-0004 | |||
| 4322 | PRV099 | PROV-MEDICAID-END-DATE | Must be equal to or greater then eff date | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV099-0005 | |||
| 4323 | PRV099 | PROV-MEDICAID-END-DATE | Overlapping coverage not allowed for same Submitting state & Prov ID, Enrollment Status Code | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV099-0006 | |||
| 4324 | PRV099 | PROV-MEDICAID-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV099-0007 | |||
| 4325 | PRV099 | PROV-MEDICAID-END-DATE | Active PRV-ATTRIBUTES-MAIN record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV099-0008 | |||
| 4326 | PRV100 | PROV-MEDICAID-ENROLLMENT-STATUS-CODE | A code representing the provider’s Medicaid and/or CHIP enrollment status for the time span specified by the PROV-MEDICAID-EFF-DATE and PROV-MEDICAID-END-DATE data elements. Note: The STATE-PLAN-ENROLLMENT data element identifies whether the provider is enrolled in Medicaid, CHIP, or both. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV100-0001 |
| 4327 | PRV100 | PROV-MEDICAID-ENROLLMENT-STATUS-CODE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV100-0002 | |||
| 4328 | PRV100 | PROV-MEDICAID-ENROLLMENT-STATUS-CODE | A health home provider must be active to be an eligible individual's primary care manager for the health home in which the individual is enrolled. | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV100-0003 | |||
| 4329 | PRV100 | PROV-MEDICAID-ENROLLMENT-STATUS-CODE | A lockin provider must be active to be a provider furnishing locked-in healthcare services to an individual. | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV100-0004 | |||
| 4330 | PRV100 | PROV-MEDICAID-ENROLLMENT-STATUS-CODE | A LTSS provider must be active to be a long term care facility furnishing healthcare services to an individual. | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV100-0005 | |||
| 4331 | PRV101 | STATE-PLAN-ENROLLMENT | The state plan with which a provider has an affiliation and is able to provide services to the state’s fee for service enrollees. | Required | Value must be equal to a valid value. | 1 Medicaid 2 CHIP 3 Both Medicaid and CHIP 4 Not state plan affiliated |
10/10/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV101-0001 |
| 4332 | PRV102 | PROV-ENROLLMENT-METHOD | Process by which a provider was enrolled in Medicaid or CHIP. | Required | Value must be equal to a valid value. | 1 Enrolled through use of Medicare enrollment system (State did not require that provider submit application. Rather Provider is active Medicare provider and state Medicaid program accepted these credentials as sufficient to participate as state Medicaid provider.) 2 Enrolled through use of state-based provider application 3 Other |
10/10/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV102-0001 |
| 4333 | PRV103 | APPL-DATE | The date on which the provider applied for enrollment into the State’s Medicaid and/or CHIP program. | Required | Date format is CCYYMMDD (National Data Standard) | 10/10/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV103-0001 | |
| 4334 | PRV103 | APPL-DATE | The date must be a valid date. | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV103-0002 | |||
| 4335 | PRV103 | APPL-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV103-0003 | |||
| 4336 | PRV103 | APPL-DATE | Must be numeric | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV103-0004 | |||
| 4337 | PRV103 | APPL-DATE | APPL-DATE cannot be greater then PROV-MEDICAID-EFF-DATE | 4/30/2013 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV103-0005 | |||
| 4338 | PRV104 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 9/23/2015 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV104-0001 | |
| 4339 | PRV104 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV104-0002 | |||
| 4340 | PRV105 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | PROVIDER | PROV-MEDICAID-ENROLLMENT-PRV00007 | PRV105-0001 | |||
| 4341 | PRV106 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Value must be equal to a valid value. | PRV00008 PROV-AFFILIATED-GROUPS | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV106-0001 |
| 4342 | PRV106 | RECORD-ID | Value is required on all record segments | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV106-0002 | |||
| 4343 | PRV106 | RECORD-ID | Value must be in the required format | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV106-0003 | |||
| 4344 | PRV106 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV106-0004 | |||
| 4345 | PRV107 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV107-0001 |
| 4346 | PRV107 | SUBMITTING-STATE | Must be populated on every record | 2/25/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV107-0002 | |||
| 4347 | PRV107 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV107-0003 | |||
| 4348 | PRV107 | SUBMITTING-STATE | Value must be the same on all records | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV107-0004 | |||
| 4349 | PRV108 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be numeric | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV108-0001 | |
| 4350 | PRV108 | RECORD-NUMBER | Value must be an 11-digit integer with no commas. | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV108-0002 | |||
| 4351 | PRV108 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV108-0003 | |||
| 4352 | PRV109 | SUBMITTING-STATE-PROV-ID | The state-assigned unique identifier for the provider entity. Note that all individuals, practice groups, facilities, and other entities that provide Medicaid/CHIP goods or services to the state’s Medicaid/CHIP enrollees should be reflected in the T-MSIS provider data set. | Conditional | Must be populated on every record | 11/3/2015 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV109-0001 | |
| 4353 | PRV110 | SUBMITTING-STATE-PROV-ID-OF-AFFILIATED-ENTITY | The unique, state-assigned identification number for the group or subpart with which the individual or subpart is associated. (The submitting state's unique identifier for the group. (Note: The group will also in the provider data set as a provider (i.e., the group-as-a-provider).) | Conditional | Must be populated on every record | 11/3/2015 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV110-0001 | |
| 4354 | PRV110 | SUBMITTING-STATE-PROV-ID-OF-AFFILIATED-ENTITY | Right-fill with spaces if the value is not 12 bytes long. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV110-0002 | |||
| 4355 | PRV111 | PROV-AFFILIATED-GROUP-EFF-DATE | The first day of the time span during which the values in all data elements in the PROV-AFFILIATED-GROUPS record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV111-0001 | |
| 4356 | PRV111 | PROV-AFFILIATED-GROUP-EFF-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV111-0002 | |||
| 4357 | PRV111 | PROV-AFFILIATED-GROUP-EFF-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV111-0003 | |||
| 4358 | PRV111 | PROV-AFFILIATED-GROUP-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV111-0004 | |||
| 4359 | PRV111 | PROV-AFFILIATED-GROUP-EFF-DATE | Whenever the value in one or more of the data elements in the PROV-AFFILIATED-GROUPS record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV111-0005 | |||
| 4360 | PRV111 | PROV-AFFILIATED-GROUP-EFF-DATE | Must be equal to or less then end date | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV111-0006 | |||
| 4361 | PRV112 | PROV-AFFILIATED-GROUP-END-DATE | The last day of the time span during which the values in all data elements in the PROV-AFFILIATED-GROUPS record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV112-0001 | |
| 4362 | PRV112 | PROV-AFFILIATED-GROUP-END-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV112-0002 | |||
| 4363 | PRV112 | PROV-AFFILIATED-GROUP-END-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV112-0003 | |||
| 4364 | PRV112 | PROV-AFFILIATED-GROUP-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV112-0004 | |||
| 4365 | PRV112 | PROV-AFFILIATED-GROUP-END-DATE | Whenever the value in one or more of the data elements in the PROV-AFFILIATED-GROUPS record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV112-0005 | |||
| 4366 | PRV112 | PROV-AFFILIATED-GROUP-END-DATE | Must be equal to or greater then eff date | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV112-0006 | |||
| 4367 | PRV112 | PROV-AFFILIATED-GROUP-END-DATE | Overlapping coverage not allowed for same state & Prov ID, Prov ID of Affiliated Entity | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV112-0007 | |||
| 4368 | PRV112 | PROV-AFFILIATED-GROUP-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV112-0008 | |||
| 4369 | PRV112 | PROV-AFFILIATED-GROUP-END-DATE | Active PRV-ATTRIBUTES-MAIN record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV112-0009 | |||
| 4370 | PRV113 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 9/23/2015 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV113-0001 | |
| 4371 | PRV113 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV113-0002 | |||
| 4372 | PRV114 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | PROVIDER | PROV-AFFILIATED-GROUPS-PRV00008 | PRV114-0001 | |||
| 4373 | PRV115 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Value must be equal to a valid value. | PRV00009 PROV-AFFILIATED-PROGRAMS | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV115-0001 |
| 4374 | PRV115 | RECORD-ID | Value is required on all record segments | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV115-0002 | |||
| 4375 | PRV115 | RECORD-ID | Value must be in the required format | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV115-0003 | |||
| 4376 | PRV115 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV115-0004 | |||
| 4377 | PRV116 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV116-0001 |
| 4378 | PRV116 | SUBMITTING-STATE | Must be populated on every record | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV116-0002 | |||
| 4379 | PRV116 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV116-0003 | |||
| 4380 | PRV116 | SUBMITTING-STATE | Value must be the same on all records | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV116-0004 | |||
| 4381 | PRV117 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Value must be an 11-digit integer with no commas. | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV117-0001 | |
| 4382 | PRV117 | RECORD-NUMBER | Must be numeric | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV117-0002 | |||
| 4383 | PRV117 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV117-0003 | |||
| 4384 | PRV118 | SUBMITTING-STATE-PROV-ID | The state-assigned unique identifier for the provider entity. Note that all individuals, practice groups, facilities, and other entities that provide Medicaid/CHIP goods or services to the state’s Medicaid/CHIP enrollees should be reflected in the T-MSIS provider data set. | Conditional | Must be populated on every record | 11/3/2015 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV118-0001 | |
| 4385 | PRV119 | AFFILIATED-PROGRAM-TYPE | A code to identify the category of program that the provider is affiliated. | Conditional | Value must be equal to a valid value. | 1 Health Plan (NHP-ID) – The value in the AFFILIATED-PROGRAM-ID data element contains the National Health Plan Identifier of health plan in which the provider is enrolled to provide services including through the state plan and a waiver. 2 Health Plan (state-assigned health plan ID) – The value in the AFFILIATED-PROGRAM-ID data element contains the state-assigned health plan Identifier of health plan in which the provider is enrolled to provide services including through the state plan and a waiver. 3 Waiver – The value in the AFFILIATED-PROGRAM-ID data element contains an identifier for the waiver in which a provider is allowed to deliver services to eligible beneficiaries. 4 Health Home Entity – The value in the AFFILIATED-PROGRAM-ID data element contains the name of the health home in which a provider is participating. The health home entity is responsible for providing health home services to the patient in conformance with the Health Home SPA. This is the name that the state uses to uniquely identify the health home team. This entity can be a designated provider (e.g., physician, clinic, behavioral health organization), a health team which links to a designated provider, or a health team (physicians, nurses, behavioral health professionals). 5 Other – The value in the AFFILIATED-PROGRAM-ID data element contains an identifier for something other than a health plan, waiver, or health home entity |
11/3/2015 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV119-0001 |
| 4386 | PRV119 | AFFILIATED-PROGRAM-TYPE | Required on every PROV-AFFILIATED-PROGRAMS record. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV119-0002 | |||
| 4387 | PRV120 | AFFILIATED-PROGRAM-ID | A data element to identify the Medicaid/CHIP programs, waivers and demonstrations in which the provider participates. | Conditional | If AFFILIATED-PROGRAM-TYPE <> spaces, then AFFILIATED-PROGRAM-ID must be <> spaces. | 11/3/2015 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV120-0001 | |
| 4388 | PRV120 | AFFILIATED-PROGRAM-ID | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. |
4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV120-0002 | |||
| 4389 | PRV120 | AFFILIATED-PROGRAM-ID | If AFFILIATED-PROGRAM-TYPE = 1 (Health Plan NHP-ID), then the value in AFFILIATED-PROGRAM-ID is the National Health Plan ID of the health plan in which a provider is enrolled to provide services. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV120-0003 | |||
| 4390 | PRV120 | AFFILIATED-PROGRAM-ID | If AFFILIATED-PROGRAM-TYPE = 2 (Health Plan State-assigned health plan ID), then the value in AFFILIATED-PROGRAM-ID is the state-assigned plan ID of the health plan in which a provider is enrolled to provide services. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV120-0004 | |||
| 4391 | PRV120 | AFFILIATED-PROGRAM-ID | If AFFILIATED-PROGRAM-TYPE = 3 (Waiver), then the value in AFFILIATED-PROGRAM-ID is an identifier for a waiver in which a provider is allowed to deliver services to eligible beneficiaries. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV120-0005 | |||
| 4392 | PRV120 | AFFILIATED-PROGRAM-ID | If AFFILIATED-PROGRAM-TYPE = 4 (Health Home Entity), then the value in AFFILIATED-PROGRAM-ID is the name of a health home in which a provider is participating. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV120-0006 | |||
| 4393 | PRV120 | AFFILIATED-PROGRAM-ID | If AFFILIATED-PROGRAM-TYPE = 5 (Other), then the value in AFFILIATED-PROGRAM-ID is an identifier for something other than a health plan, waiver, or health home entity. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV120-0007 | |||
| 4394 | PRV120 | AFFILIATED-PROGRAM-ID | If the value entered into the AFFILIATED-PROGRAM-ID is less than 50 bytes long, right-pad with spaces. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV120-0008 | |||
| 4395 | PRV120 | AFFILIATED-PROGRAM-ID | If the value entered into the AFFILIATED-PROGRAM-ID is more than 50 bytes long, truncate the bytes. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV120-0009 | |||
| 4396 | PRV121 | PROV-AFFILIATED-PROGRAM-EFF-DATE | The first day of the time span during which the values in all data elements in the PROV-AFFILIATED-PROGRAMS record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV121-0001 | |
| 4397 | PRV121 | PROV-AFFILIATED-PROGRAM-EFF-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV121-0002 | |||
| 4398 | PRV121 | PROV-AFFILIATED-PROGRAM-EFF-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV121-0003 | |||
| 4399 | PRV121 | PROV-AFFILIATED-PROGRAM-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV121-0004 | |||
| 4400 | PRV121 | PROV-AFFILIATED-PROGRAM-EFF-DATE | Whenever the value in one or more of the data elements in the PROV-AFFILIATED-PROGRAMS record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV121-0005 | |||
| 4401 | PRV121 | PROV-AFFILIATED-PROGRAM-EFF-DATE | Must be equal to or less then end date | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV121-0006 | |||
| 4402 | PRV122 | PROV-AFFILIATED-PROGRAM-END-DATE | The last day of the time span during which the values in all data elements in the PROV-AFFILIATED-PROGRAMS record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV122-0001 | |
| 4403 | PRV122 | PROV-AFFILIATED-PROGRAM-END-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV122-0002 | |||
| 4404 | PRV122 | PROV-AFFILIATED-PROGRAM-END-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV122-0003 | |||
| 4405 | PRV122 | PROV-AFFILIATED-PROGRAM-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV122-0004 | |||
| 4406 | PRV122 | PROV-AFFILIATED-PROGRAM-END-DATE | Whenever the value in one or more of the data elements in the PROV-AFFILIATED-PROGRAMS record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV122-0005 | |||
| 4407 | PRV122 | PROV-AFFILIATED-PROGRAM-END-DATE | Must be equal to or greater then eff date | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV122-0006 | |||
| 4408 | PRV122 | PROV-AFFILIATED-PROGRAM-END-DATE | Overlapping coverage not allowed for same state & Prov ID, Affiliated Program Type, Affiliated Program ID | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV122-0007 | |||
| 4409 | PRV122 | PROV-AFFILIATED-PROGRAM-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV122-0008 | |||
| 4410 | PRV122 | PROV-AFFILIATED-PROGRAM-END-DATE | Active PRV-ATTRIBUTES-MAIN record must exist in T-MSIS database or contained in the current submission | 4/30/2013 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV122-0009 | |||
| 4411 | PRV123 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 9/23/2015 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV123-0001 | |
| 4412 | PRV123 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV123-0002 | |||
| 4413 | PRV124 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | PROVIDER | PROV-AFFILIATED-PROGRAMS-PRV00009 | PRV124-0001 | |||
| 4414 | PRV125 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Value must be equal to a valid value. | PRV00010 PROV-BED-TYPE-INFO | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV125-0001 |
| 4415 | PRV125 | RECORD-ID | Value is required on all record segments | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV125-0002 | |||
| 4416 | PRV125 | RECORD-ID | Value must be in the required format | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV125-0003 | |||
| 4417 | PRV125 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV125-0004 | |||
| 4418 | PRV126 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV126-0001 |
| 4419 | PRV126 | SUBMITTING-STATE | Must be populated on every record | 2/25/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV126-0002 | |||
| 4420 | PRV126 | SUBMITTING-STATE | Value must be numeric | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV126-0003 | |||
| 4421 | PRV126 | SUBMITTING-STATE | Value must be the same on all records | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV126-0004 | |||
| 4422 | PRV127 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Value must be an 11-digit integer with no commas. | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV127-0001 | |
| 4423 | PRV127 | RECORD-NUMBER | Must be numeric | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV127-0002 | |||
| 4424 | PRV127 | RECORD-NUMBER | RECORD-ID/RECORD-NUMBER combinations should be unique within a state's submission. | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV127-0003 | |||
| 4425 | PRV128 | SUBMITTING-STATE-PROV-ID | The state-assigned unique identifier for the provider entity. Note that all individuals, practice groups, facilities, and other entities that provide Medicaid/CHIP goods or services to the state’s Medicaid/CHIP enrollees should be reflected in the T-MSIS provider data set. | Conditional | Must be populated on every record | 11/3/2015 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV128-0001 | |
| 4426 | PRV129 | PROV-LOCATION-ID | A code to uniquely identify the geographic locations where the provider performs services. These codes will also be reported in the PROV-LOCATION-ID field on CLAIM-HEADER-RECORD-IP, -LT, -OT, and –RX record segments | Conditional | Must be numeric | 11/3/2015 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV129-0001 | |
| 4427 | PRV129 | PROV-LOCATION-ID | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV129-0002 | |||
| 4428 | PRV129 | PROV-LOCATION-ID | Each of a provider entity’s locations must have a unique PROV-LOCATION-ID | 2/25/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV129-0003 | |||
| 4429 | PRV129 | PROV-LOCATION-ID | If a particular license is applicable to all locations, use the value ‘000’ value to represent ‘all’ locations. | 9/23/2015 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV129-0004 | |||
| 4430 | PRV130 | BED-TYPE-EFF-DATE | The first day of the time span during which the values in all data elements in the PROV-BED-TYPE-INFO record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV130-0001 | |
| 4431 | PRV130 | BED-TYPE-EFF-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV130-0002 | |||
| 4432 | PRV130 | BED-TYPE-EFF-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV130-0003 | |||
| 4433 | PRV130 | BED-TYPE-EFF-DATE | Must be equal to or less then end date | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV130-0004 | |||
| 4434 | PRV130 | BED-TYPE-EFF-DATE | The value must consist of digits 0 through 9 only. | 10/10/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV130-0005 | |||
| 4435 | PRV130 | BED-TYPE-EFF-DATE | Whenever the value in one or more of the data elements in the PROV-BED-TYPE-INFO record segment changes, a new record segment must be created. | 2/25/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV130-0006 | |||
| 4436 | PRV131 | BED-TYPE-END-DATE | The last day of the time span during which the values in all data elements in the PROV-BED-TYPE-INFO record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Conditional | Date format is CCYYMMDD (National Data Standard) | 11/3/2015 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV131-0001 | |
| 4437 | PRV131 | BED-TYPE-END-DATE | The date must be a valid date. | 2/25/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV131-0002 | |||
| 4438 | PRV131 | BED-TYPE-END-DATE | Must be populated on every record | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV131-0003 | |||
| 4439 | PRV131 | BED-TYPE-END-DATE | Must be equal to or greater then eff date | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV131-0004 | |||
| 4440 | PRV131 | BED-TYPE-END-DATE | Whenever the value in one or more of the data elements in the PROV-BED-TYPE-INFO record segment changes, a new record segment must be created. | 10/10/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV131-0005 | |||
| 4441 | PRV131 | BED-TYPE-END-DATE | Overlapping coverage not allowed for same Submitting state & Prov ID, Location ID, Bed Type Code | 10/10/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV131-0006 | |||
| 4442 | PRV131 | BED-TYPE-END-DATE | Coverage span date must be fully contained within in the set of effective date spans of all active parent records | 10/10/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV131-0007 | |||
| 4443 | PRV131 | BED-TYPE-END-DATE | Active PRV-ATTRIBUTES-MAIN & PRV-LOCATION-CONTACT-INFO record must exist in T-MSIS database or contained in the current submission | 10/10/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV131-0008 | |||
| 4444 | PRV134 | BED-TYPE-CODE | A code to classify beds available at a facility. | Conditional | Value must be equal to a valid value. | 1 Intermediate Care Facility for the Intellectually Disabled 2 Inpatient 3 Nursing Facility 4 Title 18 Skilled Nursing Facility (T18 SNF) 8 Not Applicable |
11/3/2015 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV134-0001 |
| 4445 | PRV134 | BED-TYPE-CODE | Must be populated on every record | 2/25/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV134-0002 | |||
| 4446 | PRV134 | BED-TYPE-CODE | Report all that apply. | 2/25/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV134-0003 | |||
| 4447 | PRV135 | BED-COUNT | A count of the number of beds available at the facility for the category of bed identified in the BED-TYPE-CODE data element. | Conditional | Value must be numeric | 11/3/2015 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV135-0001 | |
| 4448 | PRV135 | BED-COUNT | Must be greater then zero | 4/30/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV135-0002 | |||
| 4449 | PRV135 | BED-COUNT | Left-fill with zeros if value is less than 5 bytes long | 2/25/2013 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV135-0003 | |||
| 4450 | PRV136 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 9/23/2015 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV136-0001 | |
| 4451 | PRV136 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV136-0002 | |||
| 4452 | PRV137 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | PROVIDER | PROV-BED-TYPE-INFO-PRV00010 | PRV137-0001 | |||
| 4453 | TPL001 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001. | Required | Field is required on all records. | TPL00001 FILE-HEADER-RECORD-TPL | 10/10/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL001-0001 |
| 4454 | TPL001 | RECORD-ID | Value must meet the required format. | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL001-0002 | |||
| 4455 | TPL001 | RECORD-ID | Value must be equal to a valid value. | 10/10/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL001-0003 | |||
| 4456 | TPL001 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL001-0004 | |||
| 4457 | TPL001 | RECORD-ID | The record ID must be the same on all records within this segment. | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL001-0005 | |||
| 4458 | TPL002 | DATA-DICTIONARY-VERSION | A data element to capture the version of the T-MSIS data dictionary that was used to build the file. | Required | Use the version number specified on the title page of the data dictionary | 2/25/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL002-0001 | |
| 4459 | TPL003 | SUBMISSION-TRANSACTION-TYPE | A data element to identify the whether the transactions in the file are original submissions of the data, a resubmission of a previously submitted file, or corrections of edit rejects. | Required | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL003-0001 |
| 4460 | TPL003 | SUBMISSION-TRANSACTION-TYPE | Field is required on all header records. | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL003-0002 | |||
| 4461 | TPL004 | FILE-ENCODING-SPECIFICATION | A data element to denote whether the file is in fixed length line format or delimited format. | Required | Value must be equal to a valid value. | FLF The file follows a fixed length format. PSV The file follows a pipe-delimited format. |
4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL004-0001 |
| 4462 | TPL004 | FILE-ENCODING-SPECIFICATION | Field is required on all header records. | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL004-0002 | |||
| 4463 | TPL005 | DATA-MAPPING-DOCUMENT-VERSION | A data element to identify the version of the T-MSIS data mapping document used to build the file. | Required | Use the version number specified on the title page of the data mapping document | 2/25/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL005-0001 | |
| 4464 | TPL006 | FILE-NAME | The name identifying the subject area to which the records in its file relate. Each T-MSIS submission file should only contain records for one subject area (i.e., Eligible, Third-party Liability, Provider, Managed Care Plan Information, IP claims, LT claims, Rx claims, or OT claims). | Required | Required on every file header record | 2/25/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL006-0001 | |
| 4465 | TPL006 | FILE-NAME | Value must be equal to a valid value. | TPL-FILE - Third-party Liaibility file | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL006-0002 | ||
| 4466 | TPL006 | FILE-NAME | Right-fill with spaces if name is less than 8 bytes long | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL006-0003 | |||
| 4467 | TPL007 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL007-0001 | |
| 4468 | TPL007 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL007-0002 | ||
| 4469 | TPL008 | DATE-FILE-CREATED | The date on which the file was created. | Required | Date format is CCYYMMDD (National Data Standard) | 2/25/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL008-0001 | |
| 4470 | TPL008 | DATE-FILE-CREATED | Value must be a valid date | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL008-0002 | |||
| 4471 | TPL008 | DATE-FILE-CREATED | Date must be equal to or later than the date entered in the END-OF-TIME-PERIOD field. | 2/25/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL008-0003 | |||
| 4472 | TPL008 | DATE-FILE-CREATED | Required on every file header record | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL008-0004 | |||
| 4473 | TPL008 | DATE-FILE-CREATED | Date must be equal or less than current date | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL008-0005 | |||
| 4474 | TPL009 | START-OF-TIME-PERIOD | Beginning date of the month covered by this file. | Required | Date format is CCYYMMDD (National Data Standard) | 10/10/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL009-0001 | |
| 4475 | TPL009 | START-OF-TIME-PERIOD | Value must be a valid date based on the calendar year. | 2/25/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL009-0002 | |||
| 4476 | TPL009 | START-OF-TIME-PERIOD | DD must always be the 1st day of the month. | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL009-0003 | |||
| 4477 | TPL009 | START-OF-TIME-PERIOD | Value for START-OF-TIME-PERIOD must be <= END-OF-TIME-PERIOD | 10/10/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL009-0004 | |||
| 4478 | TPL009 | START-OF-TIME-PERIOD | Value for END-OF-TIME-PERIOD must be < Current Date | 10/10/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL009-0005 | |||
| 4479 | TPL010 | END-OF-TIME-PERIOD | Last date of the reporting period covered by the file to which this Header Record is attached. | Required | Date format is CCYYMMDD (National Data Standard) | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL010-0001 | |
| 4480 | TPL010 | END-OF-TIME-PERIOD | Value must be a valid date | 2/25/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL010-0002 | |||
| 4481 | TPL010 | END-OF-TIME-PERIOD | Value for the Date in the End of Time Period (last 2 bytes of the value) must equal "30" in April, June, September, or November; "31" in January, March, May, July, August, October, or December, and "28" or "29" in February. | 10/10/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL010-0003 | |||
| 4482 | TPL010 | END-OF-TIME-PERIOD | Value must be equal or less than the DATE-FILE-CREATED | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL010-0004 | |||
| 4483 | TPL010 | END-OF-TIME-PERIOD | Value must be less than the current system date. | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL010-0005 | |||
| 4484 | TPL011 | FILE-STATUS-INDICATOR | A code to indicate whether the records in the file are test or production records. | Required | Value must be equal to a valid value. | P - Production T - Test |
2/25/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL011-0001 |
| 4485 | TPL011 | FILE-STATUS-INDICATOR | The dataset name and the value in this field must be consistent (i.e., the production dataset name cannot have a FILE-STATUS-INDICATOR = 'T' | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL011-0002 | |||
| 4486 | TPL012 | SSN-INDICATOR | Indicates whether the state uses the eligible person's social security number (SSN) instead of an MSIS identification number as the unique, unchanging eligible person identifier. | Required | Value must be equal to a valid value. | 0 - State does not use SSN as MSIS-IDENTIFICATION-NUMBER 1 - State uses SSN as MSIS-IDENTIFICATION-NUMBER |
4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL012-0001 |
| 4487 | TPL012 | SSN-INDICATOR | Non-SSN States will assign each eligible only one permanent MSIS-ID in his or her lifetime. When reporting eligibility records it is important that the SSN-INDICATOR in the Header record be set to 0 and the MSIS-ID for each record be provided in the MSIS-IDENTIFICATION-NUMBER field; if the MSIS-IDENTIFICATION-NUMBER is not known then this field should be filled with nines. The MSIS-ID identifies the individual and any claims submitted to the system | 2/25/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL012-0002 | |||
| 4488 | TPL012 | SSN-INDICATOR | States that are non SSN states must not submit MSIS Identification Numbers and SSNs that match for eligible individuals. | 2/25/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL012-0003 | |||
| 4489 | TPL013 | TOT-REC-CNT | A count of all records in the file except for the file header record. This count will be used as a control total to help assure that the file did not become corrupted during transmission. | Required | An integer value with no commas. |
4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL013-0001 | |
| 4490 | TPL013 | TOT-REC-CNT | Value must equal the sum of all records excluding the header record | 4/30/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL013-0002 | |||
| 4491 | TPL088 | SEQUENCE-NUMBER | To enable state’s to sequentially number files, when related, follow-on files are necessary (i.e., update files, replacement files). This should begin with 1 for the original Create submission type and be incremented by one for each Replacement or Update submission for the same reporting period and file type (subject area). | Required | Field is required on all 'C', 'U', and 'R' record files. | 10/10/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL088-0001 | |
| 4492 | TPL088 | SEQUENCE-NUMBER | Must be numeric and > 0 | 10/10/2013 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL088-0002 | |||
| 4493 | TPL014 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 9/23/2015 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL014-0001 | |
| 4494 | TPL014 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL014-0002 | |||
| 4495 | TPL015 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | TPL | FILE-HEADER-RECORD-TPL-TPL00001 | TPL015-0001 | |||
| 4496 | TPL016 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Field is required on all records. | TPL00002 TPL-MEDICAID-ELIGIBLE-PERSON-MAIN | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL016-0001 |
| 4497 | TPL016 | RECORD-ID | Value must meet the required format. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL016-0002 | |||
| 4498 | TPL016 | RECORD-ID | Value must be equal to a valid value. | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL016-0003 | |||
| 4499 | TPL016 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL016-0004 | |||
| 4500 | TPL016 | RECORD-ID | The record ID must be the same on all records within this segment. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL016-0005 | |||
| 4501 | TPL017 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL017-0001 | |
| 4502 | TPL017 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL017-0002 | ||
| 4503 | TPL017 | SUBMITTING-STATE | SUBMITTING-STATE in this file segment must = SUBMITTING-STATE in the file segment FILE-HEADER-RECORD-TPL-TPL00001 | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL017-0003 | |||
| 4504 | TPL018 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL018-0001 | |
| 4505 | TPL018 | RECORD-NUMBER | The value must consist of digits 0 through 9 only | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL018-0002 | |||
| 4506 | TPL018 | RECORD-NUMBER | Value must be distinct (non duplicative within segment for same field). | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL018-0003 | |||
| 4507 | TPL019 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | The Medicare/CHIP enrollee’s MSIS-IDENTIFICATION-NUM must exist in the T-MSIS Eligibility file or in the T-MSIS data repository. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL019-0001 | |
| 4508 | TPL019 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the State ID numbers must be supplied to CMS. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL019-0002 | |||
| 4509 | TPL019 | MSIS-IDENTIFICATION-NUM | For SSN states, this field must contain the Eligible's Social Security Number. If the SSN is unknown and a temporary number is assigned, this field will contain temporary number. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL019-0003 | |||
| 4510 | TPL019 | MSIS-IDENTIFICATION-NUM | If the field value is missing, keep the default value of spaces. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL019-0004 | |||
| 4511 | TPL019 | MSIS-IDENTIFICATION-NUM | MSIS Identification Number must be reported | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL019-0005 | |||
| 4512 | TPL020 | TPL-HEALTH-INSURANCE-COVERAGE-IND | A flag to indicate that the Medicaid/CHIP eligible person has some form of third party insurance coverage. | Conditional | Value must be equal to a valid value. | 0 Eligible individual has no TPL insurance coverage 1 Eligible individual does have TPL insurance coverage |
11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL020-0001 |
| 4513 | TPL020 | TPL-HEALTH-INSURANCE-COVERAGE-IND | If the value is “1,” then there must be one or more instances where the eligible person has some form of third party insurance coverage. (The records for this coverage can exist either in the T-MSIS data repository, or be on one or more TPL-MEDICAID-ELIGIBLE-INSURANCE-COVERAGE-INFO record segments in the current THIRD PARTY LIABILITY (TPL) FILE submission. | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL020-0002 | |||
| 4514 | TPL021 | TPL-OTHER-COVERAGE-IND | A flag to indicate that the Medicaid/CHIP eligible person has some other form of third party funding besides insurance coverage. | Conditional | Value must be equal to a valid value. | 0 Eligible individual has no other TPL funding available 1 Eligible individual does have other TPL funding available |
11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL021-0001 |
| 4515 | TPL022 | ELIGIBLE-FIRST-NAME | The first name of the individual to whom the services were provided. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL022-0001 | |
| 4516 | TPL023 | ELIGIBLE-MIDDLE-INIT | The middle initial of the individual to whom the services were provided. | Conditional | Use only alphabetic characters, (A-Z, a-z) or space ( ). | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL023-0001 | |
| 4517 | TPL024 | ELIGIBLE-LAST-NAME | The last name of the individual to whom the services were provided. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL024-0001 | |
| 4518 | TPL025 | ELIG-PRSN-MAIN-EFF-DATE | The first day of the time span during which the values in all data elements in the ELIG-PRSN-MAIN-EFF-DATE record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Required | The date must be in “ccyymmdd” format. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL025-0001 | |
| 4519 | TPL025 | ELIG-PRSN-MAIN-EFF-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL025-0002 | |||
| 4520 | TPL025 | ELIG-PRSN-MAIN-EFF-DATE | Value must be a valid date | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL025-0003 | |||
| 4521 | TPL025 | ELIG-PRSN-MAIN-EFF-DATE | Whenever the value in one or more of the data elements in the TPL-MEDICAID-ELIGIBLE-PERSON-MAIN record segment changes, a new record segment must be created. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL025-0004 | |||
| 4522 | TPL025 | ELIG-PRSN-MAIN-EFF-DATE | Date cannot be greater than ELIG-PRSN-MAIN-END-DATE. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL025-0005 | |||
| 4523 | TPL025 | ELIG-PRSN-MAIN-EFF-DATE | An eligible individual cannot have relevant record segments effective in the Third Party Liability file after he/she has died. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL025-0006 | |||
| 4524 | TPL026 | ELIG-PRSN-MAIN-END-DATE | The last day of the time span during which the values in all data elements in the ELIG-PRSN-MAIN-EFF-DATE record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Required | The date must be in “ccyymmdd” format. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL026-0001 | |
| 4525 | TPL026 | ELIG-PRSN-MAIN-END-DATE | The value must consist of digits 0 through 9 only | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL026-0002 | |||
| 4526 | TPL026 | ELIG-PRSN-MAIN-END-DATE | The date must be a valid date | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL026-0003 | |||
| 4527 | TPL026 | ELIG-PRSN-MAIN-END-DATE | Whenever the value in one or more of the data elements in the TPL-MEDICAID-ELIGIBLE-PERSON-MAIN record segment changes, a new record segment must be created. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL026-0004 | |||
| 4528 | TPL027 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL027-0001 | |
| 4529 | TPL027 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL027-0002 | |||
| 4530 | TPL028 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 | TPL028-0001 | |||
| 4531 | TPL029 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Field is required on all records. | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL029-0001 | |
| 4532 | TPL029 | RECORD-ID | Value must meet the required format. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL029-0002 | |||
| 4533 | TPL029 | RECORD-ID | Value must be equal to a valid value. | TPL00003 TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL029-0003 | ||
| 4534 | TPL029 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL029-0004 | |||
| 4535 | TPL029 | RECORD-ID | The record ID must be the same on all records within this segment. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL029-0005 | |||
| 4536 | TPL030 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL030-0001 | |
| 4537 | TPL030 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL030-0002 | ||
| 4538 | TPL030 | SUBMITTING-STATE | SUBMITTING-STATE in this file segment must = SUBMITTING-STATE in the file segment FILE-HEADER-RECORD-TPL-TPL00001 | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL030-0003 | |||
| 4539 | TPL031 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL031-0001 | |
| 4540 | TPL031 | RECORD-NUMBER | The value must consist of digits 0 through 9 only | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL031-0002 | |||
| 4541 | TPL031 | RECORD-NUMBER | Value must be distinct (non duplicative within segment for same field). | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL031-0003 | |||
| 4542 | TPL032 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | The Medicare/CHIP enrollee’s MSIS-IDENTIFICATION-NUM must exist in the T-MSIS Eligibility file or in the T-MSIS data repository. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL032-0001 | |
| 4543 | TPL032 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the State ID numbers must be supplied to CMS. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL032-0002 | |||
| 4544 | TPL032 | MSIS-IDENTIFICATION-NUM | For SSN states, this field must contain the Eligible's Social Security Number. If the SSN is unknown and a temporary number is assigned, this field will contain temporary number. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL032-0003 | |||
| 4545 | TPL032 | MSIS-IDENTIFICATION-NUM | If the field value is missing, keep the default value of spaces. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL032-0004 | |||
| 4546 | TPL032 | MSIS-IDENTIFICATION-NUM | MSIS Identification Number must be reported | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL032-0005 | |||
| 4547 | TPL033 | INSURANCE-CARRIER-ID-NUM | The state’s internal identification number of the Third Party Liability (TPL) Insurance carrier. | Conditional | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL033-0001 | |
| 4548 | TPL033 | INSURANCE-CARRIER-ID-NUM | Left justify and pad unused bytes with spaces. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL033-0002 | |||
| 4549 | TPL034 | INSURANCE-PLAN-ID | The ID number issued by the Insurance carrier providing third party liability insurance coverage to beneficiaries. Typically the Plan ID/Plan Num is on the beneficiaries’ insurance card. | Conditional | Enter the insurance plan identification number assigned by the state. |
11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL034-0001 | |
| 4550 | TPL034 | INSURANCE-PLAN-ID | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL034-0002 | |||
| 4551 | TPL034 | INSURANCE-PLAN-ID | If the field value is missing, keep the default value of spaces. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL034-0003 | |||
| 4552 | TPL035 | GROUP-NUM | The group number of the Third Party Liability (TPL) health insurance policy. | Conditional | Left justify and pad unused bytes with spaces. | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL035-0001 | |
| 4553 | TPL035 | GROUP-NUM | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL035-0002 | |||
| 4554 | TPL035 | GROUP-NUM | If the field value is missing, keep the default value of spaces. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL035-0003 | |||
| 4555 | TPL035 | GROUP-NUM | If this field is not applicable, 8-fill. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL035-0004 | |||
| 4556 | TPL036 | MEMBER-ID | Member identification number as it appears on the card issued by the TPL insurance carrier. | Conditional | Use only alphabetic characters, (A-Z, a-z), numerals (0-9), spaces ( ), dashes (-), periods (.), forward slashes (/), single quote(‘). | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL036-0001 | |
| 4557 | TPL036 | MEMBER-ID | Left justify and pad with trailing spaces. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL036-0002 | |||
| 4558 | TPL036 | MEMBER-ID | If the field value is missing, keep the default value of spaces. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL036-0003 | |||
| 4559 | TPL037 | INSURANCE-PLAN-TYPE | Code to classify the type of insurance plan providing TPL coverage. | Conditional | Values must correspond to associated INSURANCE-PLAN-ID. | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL037-0001 | |
| 4560 | TPL037 | INSURANCE-PLAN-TYPE | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL037-0002 | ||
| 4561 | TPL089 | COVERAGE-TYPE | Code indicating the level of coverage being provided under this policy for the insured by the TPL carrier. | Conditional | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL089-0001 |
| 4562 | TPL038 | ANNUAL-DEDUCTIBLE-AMT | Annual amount paid each year by the enrollee in the plan before a health plan benefit begins. | Conditional | The value must consist of digits 0 through 9 only | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL038-0001 | |
| 4563 | TPL044 | POLICY-OWNER-FIRST-NAME | The first name of the owner of the insurance policy. For example, the owner of this may be the Medicaid/CHIP beneficiary. | Conditional | If the TPL insurance is noted under OTHER-THIRD-PARTY-LIABILITY, the liability policy owner information is not needed and 8-fill the POLICY-OWNER field. |
10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL044-0001 | |
| 4564 | TPL044 | POLICY-OWNER-FIRST-NAME | 'If the HEALTH-INSURANCE-COVERAGE-IND equals '1', this field is required' to match coding requirement for POLICY-OWNER-LAST-NAME. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL044-0002 | |||
| 4565 | TPL044 | POLICY-OWNER-FIRST-NAME | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL044-0003 | |||
| 4566 | TPL044 | POLICY-OWNER-FIRST-NAME | Left justify and pad with trailing spaces. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL044-0004 | |||
| 4567 | TPL044 | POLICY-OWNER-FIRST-NAME | If the field value is missing, keep the default value of spaces. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL044-0005 | |||
| 4568 | TPL045 | POLICY-OWNER-LAST-NAME | The last name of the owner of the insurance policy. For example, the owner of this may be the Medicaid/CHIP beneficiary. | Conditional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL045-0001 | |
| 4569 | TPL045 | POLICY-OWNER-LAST-NAME | Left justify and pad with trailing spaces. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL045-0002 | |||
| 4570 | TPL045 | POLICY-OWNER-LAST-NAME | If the field value is missing, keep the default value of spaces. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL045-0003 | |||
| 4571 | TPL045 | POLICY-OWNER-LAST-NAME | If the HEALTH-INSURANCE-COVERAGE-IND equals '1', this field is required. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL045-0004 | |||
| 4572 | TPL045 | POLICY-OWNER-LAST-NAME | If the field is not applicable or the TPL insurance is noted under OTHER-THIRD-PARTY-LIABILITY, 8-fill the field. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL045-0005 | |||
| 4573 | TPL046 | POLICY-OWNER-SSN | The policy owner’s social security number. | Conditional | If known, this field is to be populated with numeric digits. | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL046-0001 | |
| 4574 | TPL046 | POLICY-OWNER-SSN | If the HEALTH-INSURANCE-COVERAGE-IND equals '1', this field is required. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL046-0002 | |||
| 4575 | TPL046 | POLICY-OWNER-SSN | If the field is not applicable or the TPL insurance is noted under OTHER-THIRD-PARTY-LIABILITY, 8-fill the field. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL046-0003 | |||
| 4576 | TPL047 | POLICY-OWNER-CODE | This code identifies the relationship of the policy holder to the Medicaid/CHIP beneficiary. | Conditional | If the TPL insurance is noted under OTHER-THIRD-PARTY-LIABILITY, the liability policy owner information is not applicable, 8-fill the POLICY-OWNER-CODE field. |
11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL047-0001 | |
| 4577 | TPL047 | POLICY-OWNER-CODE | Value must be equal to a valid value. | 01 Self 02 Spouse 03 Custodial Parent 04 Noncustodial Parent (Child Support Enforcement in effect) 05 Noncustodial Parent without child support enforcement in effect 06 Grandparent 07 Guardian 08 Domestic Partner 09 Other 99 Unknown |
10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL047-0002 | ||
| 4578 | TPL048 | INSURANCE-COVERAGE-EFF-DATE | The first day of the time span during which the Medicaid enrollee is covered under the policy. This date field is necessary when defining a unique row in a database table. |
Conditional | The date must be in “ccyymmdd” format. | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL048-0001 | |
| 4579 | TPL048 | INSURANCE-COVERAGE-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL048-0002 | |||
| 4580 | TPL048 | INSURANCE-COVERAGE-EFF-DATE | Value must be a valid date | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL048-0003 | |||
| 4581 | TPL048 | INSURANCE-COVERAGE-EFF-DATE | Whenever the value in one or more of the data elements in the TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO record segment changes, a new record segment must be created. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL048-0004 | |||
| 4582 | TPL048 | INSURANCE-COVERAGE-EFF-DATE | Date cannot be greater than INSURANCE-COVERAGE-END-DATE. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL048-0005 | |||
| 4583 | TPL048 | INSURANCE-COVERAGE-EFF-DATE | If the HEALTH-INSURANCE-COVERAGE-IND equals '1', this field is required. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL048-0006 | |||
| 4584 | TPL048 | INSURANCE-COVERAGE-EFF-DATE | An eligible individual cannot have relevant record segments effective in the Third Party Liability file after he/she has died. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL048-0007 | |||
| 4585 | TPL049 | INSURANCE-COVERAGE-END-DATE | The last day of the time span during which the Medicaid enrollee is covered under the policy. | Conditional | The date must be in “ccyymmdd” format. | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL049-0001 | |
| 4586 | TPL049 | INSURANCE-COVERAGE-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL049-0002 | |||
| 4587 | TPL049 | INSURANCE-COVERAGE-END-DATE | Value must be a valid date | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL049-0003 | |||
| 4588 | TPL049 | INSURANCE-COVERAGE-END-DATE | If there is no end date (i.e., the record is good into the indefinite future) use the “end-of-time” date (99991231). | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL049-0004 | |||
| 4589 | TPL049 | INSURANCE-COVERAGE-END-DATE | Whenever the value in one or more of the data elements in the TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO record segment changes, a new record segment must be created. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL049-0005 | |||
| 4590 | TPL049 | INSURANCE-COVERAGE-END-DATE | If the field is not applicable or the TPL insurance is noted under OTHER-THIRD-PARTY-LIABILITY, 8-fill the field. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL049-0006 | |||
| 4591 | TPL049 | INSURANCE-COVERAGE-END-DATE | If the HEALTH-INSURANCE-COVERAGE-IND equals '1', this field is required. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL049-0007 | |||
| 4592 | TPL049 | INSURANCE-COVERAGE-END-DATE | Overlapping coverage not allowed for same Submitting state, MSIS Identification number, Insurance plan ID, Group number, and Member ID. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL049-0008 | |||
| 4593 | TPL049 | INSURANCE-COVERAGE-END-DATE | Active TPL-MEDICAID-ELIGIBLE-MAIN record with a TPL-HEALTH-INSURANCE-COVERAGE-IND = 1 must exist in T-MSIS database or contained in the current submission | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL049-0009 | |||
| 4594 | TPL049 | INSURANCE-COVERAGE-END-DATE | Coverage date span must be fully contained within the set of effective date spans of all active parent records. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL049-0010 | |||
| 4595 | TPL050 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL050-0001 | |
| 4596 | TPL050 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL050-0002 | |||
| 4597 | TPL051 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 | TPL051-0001 | |||
| 4598 | TPL052 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Field is required on all records. | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL052-0001 | |
| 4599 | TPL052 | RECORD-ID | Value must meet the required format. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL052-0002 | |||
| 4600 | TPL052 | RECORD-ID | Value must be equal to a valid value. | TPL00004 TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL052-0003 | ||
| 4601 | TPL052 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL052-0004 | |||
| 4602 | TPL052 | RECORD-ID | The record ID must be the same on all records within this segment. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL052-0005 | |||
| 4603 | TPL053 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL053-0001 | |
| 4604 | TPL053 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL053-0002 | ||
| 4605 | TPL053 | SUBMITTING-STATE | SUBMITTING-STATE in this file segment must = SUBMITTING-STATE in the file segment FILE-HEADER-RECORD-TPL-TPL00001 | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL053-0003 | |||
| 4606 | TPL054 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL054-0001 | |
| 4607 | TPL054 | RECORD-NUMBER | The value must consist of digits 0 through 9 only | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL054-0002 | |||
| 4608 | TPL054 | RECORD-NUMBER | Value must be distinct (non duplicative within segment for same field). | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL054-0003 | |||
| 4609 | TPL055 | INSURANCE-CARRIER-ID-NUM | The state’s internal identification number of the Third Party Liability (TPL) Insurance carrier. | Required | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL055-0001 | |
| 4610 | TPL055 | INSURANCE-CARRIER-ID-NUM | Field is required on all record segments. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL055-0002 | |||
| 4611 | TPL056 | INSURANCE-PLAN-ID | The ID number issued by the Insurance carrier providing third party liability insurance coverage to beneficiaries. Typically the Plan ID/Plan Num is on the beneficiaries’ insurance card. | Required | Enter the insurance plan identification number assigned by the state. |
10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL056-0001 | |
| 4612 | TPL056 | INSURANCE-PLAN-ID | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL056-0002 | |||
| 4613 | TPL056 | INSURANCE-PLAN-ID | If the field value is missing, keep the default value of spaces. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL056-0003 | |||
| 4614 | TPL057 | INSURANCE-PLAN-TYPE | Code to classify the entity providing TPL coverage. | Optional | Values must correspond to associated INSURANCE-PLAN-ID. | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL057-0001 | |
| 4615 | TPL057 | INSURANCE-PLAN-TYPE | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL057-0002 | ||
| 4616 | TPL058 | COVERAGE-TYPE | Code indicating the level of coverage being provided under this policy for the insured by the TPL carrier. | Conditional | Value must be equal to a valid value. | See Appendix A for listing of valid values. | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL058-0001 |
| 4617 | TPL059 | INSURANCE-CATEGORIES-EFF-DATE | The first day of the time span during which the values in all data elements in the TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Conditional | The date must be in “ccyymmdd” format. | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL059-0001 | |
| 4618 | TPL059 | INSURANCE-CATEGORIES-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL059-0002 | |||
| 4619 | TPL059 | INSURANCE-CATEGORIES-EFF-DATE | Value must be a valid date | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL059-0003 | |||
| 4620 | TPL059 | INSURANCE-CATEGORIES-EFF-DATE | Whenever the value in one or more of the data elements in the TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES record segment changes, a new record segment must be created. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL059-0004 | |||
| 4621 | TPL059 | INSURANCE-CATEGORIES-EFF-DATE | INSURANCE-CATEGORIES-EFF-DATE must be <= INSURANCE-CATEGORIES-END-DATE | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL059-0005 | |||
| 4622 | TPL059 | INSURANCE-CATEGORIES-EFF-DATE | If TPL-HEALTH-INSURANCE-COVERAGE-IND = '1', then INSURANCE-COVERAGE-EFF-DATE must be <> 11111111, 22222222, 33333333, 44444444, 55555555, 66666666, 77777777, 88888888, 99999999. | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL059-0006 | |||
| 4623 | TPL060 | INSURANCE-CATEGORIES-END-DATE | The last day of the time span during which the values in all data elements in the TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Conditional | Date format should be CCYYMMDD (National Data Standard) | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL060-0001 | |
| 4624 | TPL060 | INSURANCE-CATEGORIES-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL060-0002 | |||
| 4625 | TPL060 | INSURANCE-CATEGORIES-END-DATE | Value must be a valid date | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL060-0003 | |||
| 4626 | TPL060 | INSURANCE-CATEGORIES-END-DATE | If there is no end date (i.e., the record is good into the indefinite future) use the “end-of-time” date (99991231). | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL060-0004 | |||
| 4627 | TPL060 | INSURANCE-CATEGORIES-END-DATE | Whenever the value in one or more of the data elements in the TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES record segment changes, a new record segment must be created. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL060-0005 | |||
| 4628 | TPL060 | INSURANCE-CATEGORIES-END-DATE | If the field is not applicable or the TPL insurance is noted under OTHER-THIRD-PARTY-LIABILITY, 8-fill the field. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL060-0006 | |||
| 4629 | TPL060 | INSURANCE-CATEGORIES-END-DATE | If the HEALTH-INSURANCE-COVERAGE-IND equals '1', this field is required. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL060-0007 | |||
| 4630 | TPL060 | INSURANCE-CATEGORIES-END-DATE | If SUBMITTING-STATE, MSIS-IDENTIFICATION-NUM, INSURANCE-CARRIER-ID, INSURANCE-PLAN-ID, and COVERAGE-TYPE in this file segment = the same values of another TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 file segment, then (INSURANCE-COVERAGE-EFF-DATE [segment 1] must be < INSURANCE-CATEGORIES-END-DATE [segment 1]) AND (INSURANCE-CATEGORIES-END-DATE [segment 1] must be < INSURANCE-CATEGORIES-EFF-DATE [segment 2]) AND (INSURANCE-CATEGORIES-EFF-DATE [segment 2] must be < INSURANCE-CATEGORIES-END-DATE [segment 2]. | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL060-0008 | |||
| 4631 | TPL060 | INSURANCE-CATEGORIES-END-DATE | If SUBMITTING-STATE and MSIS-IDENTIFICATION-NUM = SUBMITTING-STATE and MSIS-IDENTIFICATION-NUM on the file segment TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 and on TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003, then (INSURANCE-CATEGORIES-END-DATE must be >= ELIG-PRSN-MAIN-END-DATE) AND (INSURANCE-CATEGORIES-END-DATE must be >= ELIG-PRSN-MAIN-EFF-DATE) AND (INSURANCE-CATEGORIES-END-DATE >= INSURANCE-COVERAGE-END-DATE) AND (INSURANCE-CATEGORIES-END-DATE<=INSURANCE-COVERAGE-EFF-DATE). The segment must have both, a matching, active TPL-MEDICAID-ELIGIBLE-PERSON-MAIN record and a TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO record and the INSURANCE-CATEGORIES-EFF-DATE must be >= ELIG-PRSN-MAIN-EFF-DATE and INSURANCE-COVERAGE-EFF-DATE and INSURANCE-CATEGORIES-END-DATE must be <= ELIG-PRSN-MAIN-END-DATE and INSURANCE-COVERAGE-END-DATE. |
10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL060-0009 | |||
| 4632 | TPL060 | INSURANCE-CATEGORIES-END-DATE | If SUBMITTING-STATE and MSIS-IDENTIFICATION-NUM = SUBMITTING-STATE and MSIS-IDENTIFICATION-NUM on the file segment TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 and on TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003, then (INSURANCE-CATEGORIES-END-DATE must be >= ELIG-PRSN-MAIN-END-DATE) AND (INSURANCE-CATEGORIES-END-DATE must be >= ELIG-PRSN-MAIN-EFF-DATE) AND (INSURANCE-CATEGORIES-END-DATE >= INSURANCE-COVERAGE-END-DATE) AND (INSURANCE-CATEGORIES-END-DATE<=INSURANCE-COVERAGE-EFF-DATE). The segment must have both, a matching, active TPL-MEDICAID-ELIGIBLE-PERSON-MAIN record and a TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO record and the INSURANCE-CATEGORIES-EFF-DATE must be >= ELIG-PRSN-MAIN-EFF-DATE and INSURANCE-COVERAGE-EFF-DATE and INSURANCE-CATEGORIES-END-DATE must be <= ELIG-PRSN-MAIN-END-DATE and INSURANCE-COVERAGE-END-DATE. |
10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL060-0010 | |||
| 4633 | TPL061 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL061-0001 | |
| 4634 | TPL061 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL061-0002 | |||
| 4635 | TPL062 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 | TPL062-0001 | |||
| 4636 | TPL063 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Field is required on all records. | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL063-0001 | |
| 4637 | TPL063 | RECORD-ID | Value must meet the required format. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL063-0002 | |||
| 4638 | TPL063 | RECORD-ID | Value must be equal to a valid value. | TPL00005 TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL063-0003 | ||
| 4639 | TPL063 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL063-0004 | |||
| 4640 | TPL063 | RECORD-ID | The record ID must be the same on all records within this segment. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL063-0005 | |||
| 4641 | TPL064 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL064-0001 | |
| 4642 | TPL064 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL064-0002 | ||
| 4643 | TPL064 | SUBMITTING-STATE | SUBMITTING-STATE in this file segment must = SUBMITTING-STATE in the file segment FILE-HEADER-RECORD-TPL-TPL00001 | 10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL064-0003 | |||
| 4644 | TPL065 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL065-0001 | |
| 4645 | TPL065 | RECORD-NUMBER | The value must consist of digits 0 through 9 only | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL065-0002 | |||
| 4646 | TPL065 | RECORD-NUMBER | Value must be distinct (non duplicative within segment for same field). | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL065-0003 | |||
| 4647 | TPL066 | MSIS-IDENTIFICATION-NUM | A state-assigned unique identification number used to identify a Medicaid/CHIP enrolled individual. | Required | The Medicare/CHIP enrollee’s MSIS-IDENTIFICATION-NUM must exist in the T-MSIS Eligibility file or in the T-MSIS data repository. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL066-0001 | |
| 4648 | TPL066 | MSIS-IDENTIFICATION-NUM | For non-SSN states, this field must contain an identification number assigned by the state. The format of the State ID numbers must be supplied to CMS. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL066-0002 | |||
| 4649 | TPL066 | MSIS-IDENTIFICATION-NUM | For SSN states, this field must contain the Eligible's Social Security Number. If the SSN is unknown and a temporary number is assigned, this field will contain temporary number. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL066-0003 | |||
| 4650 | TPL066 | MSIS-IDENTIFICATION-NUM | If the field value is missing, keep the default value of spaces. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL066-0004 | |||
| 4651 | TPL066 | MSIS-IDENTIFICATION-NUM | MSIS Identification Number must be reported | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL066-0005 | |||
| 4652 | TPL067 | TYPE-OF-OTHER-THIRD-PARTY-LIABILITY | This code identifies the other types of liabilities an individual may have which are not necessarily defined as a health insurance plan listed INSURANCE-TYPE-PLAN. | Conditional | Required | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL067-0001 | |
| 4653 | TPL067 | TYPE-OF-OTHER-THIRD-PARTY-LIABILITY | Value must be equal to a valid value. | 1 Tort/Casualty Claim 2 Medical Malpractice 3 Estate (an estate, annuity or designated trust) 4 Liens 5 Worker’s Compensation 6 Payments from an individual or group who has either voluntarily or been assigned legal responsibility for the health care of one or more Medicaid recipients; fraternal groups; unions 7 Other – unidentified 9 Unknown |
10/10/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL067-0002 | ||
| 4654 | TPL068 | OTHER-TPL-EFF-DATE | The first day of the time span during which the values in all data elements in the TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Conditional | The date must be in “ccyymmdd” format | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL068-0001 | |
| 4655 | TPL068 | OTHER-TPL-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL068-0002 | |||
| 4656 | TPL068 | OTHER-TPL-EFF-DATE | Value must be a valid date | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL068-0003 | |||
| 4657 | TPL068 | OTHER-TPL-EFF-DATE | Whenever the value in one or more of the data elements in the TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION record segment changes, a new record segment must be created. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL068-0004 | |||
| 4658 | TPL068 | OTHER-TPL-EFF-DATE | Date cannot be greater than OTHER-TPL-END-DATE. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL068-0005 | |||
| 4659 | TPL068 | OTHER-TPL-EFF-DATE | If the TPL-OTHER-COVERAGE-IND equals '1', this field is required. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL068-0006 | |||
| 4660 | TPL068 | OTHER-TPL-EFF-DATE | An eligible individual cannot have relevant record segments effective in the Third Party Liability file after he/she has died. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL068-0007 | |||
| 4661 | TPL069 | OTHER-TPL-END-DATE | The last day of the time span during which the values in all data elements in the TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created.) | Conditional | The date must be in “ccyymmdd” format | 11/3/2015 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL069-0001 | |
| 4662 | TPL069 | OTHER-TPL-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL069-0002 | |||
| 4663 | TPL069 | OTHER-TPL-END-DATE | Value must be a valid date | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL069-0003 | |||
| 4664 | TPL069 | OTHER-TPL-END-DATE | If there is no end date (i.e., the record is good into the indefinite future) use the “end-of-time” date (99991231). | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL069-0004 | |||
| 4665 | TPL069 | OTHER-TPL-END-DATE | Whenever the value in one or more of the data elements in the TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION record segment changes, a new record segment must be created. | 2/25/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL069-0005 | |||
| 4666 | TPL069 | OTHER-TPL-END-DATE | If the field is not applicable or the TPL-OTHER-COVERAGE-IND = 0, 8-fill the field. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL069-0006 | |||
| 4667 | TPL069 | OTHER-TPL-END-DATE | If the TPL-OTHER-COVERAGE-IND equals '1', this field is required. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL069-0007 | |||
| 4668 | TPL069 | OTHER-TPL-END-DATE | Overlapping coverage not allowed for same Submitting state , MSIS ID and Type of other third party. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL069-0008 | |||
| 4669 | TPL069 | OTHER-TPL-END-DATE | Active TPL-MEDICAID-ELIGIBLE-MAIN record with TPL-OTHER-COVERAGE-IND = 1 must exist in T-MSIS database or contained in the current submission | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL069-0009 | |||
| 4670 | TPL069 | OTHER-TPL-END-DATE | Coverage categories date span must be fully contained within the set of effective date spans of all active parent records. | 4/30/2013 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL069-0010 | |||
| 4671 | TPL070 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL070-0001 | |
| 4672 | TPL070 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL070-0002 | |||
| 4673 | TPL071 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | TPL | TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 | TPL071-0001 | |||
| 4674 | TPL072 | RECORD-ID | An identifier assigned to each record segment. The first 3 characters identify the subject area. The last 5 bytes are an integer with leading zeros. For example, the RECORD-ID for the PRIMARY DEMOGRAPHICS – ELIGIBILITY record segment is ELG00001 | Required | Field is required on all records. | 10/10/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION- TPL00006 | TPL072-0001 | |
| 4675 | TPL072 | RECORD-ID | Value must meet the required format. | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL072-0002 | |||
| 4676 | TPL072 | RECORD-ID | Value must be equal to a valid value. | TPL00006 TPL-ENTITY-CONTACT-INFORMATION | 10/10/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL072-0003 | ||
| 4677 | TPL072 | RECORD-ID | The record ID and file name must be consistent (i.e., the file cannot have a FILE-NAME of CLAIMRX, but RECORD-IDs associated with eligible file record layouts) | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL072-0004 | |||
| 4678 | TPL072 | RECORD-ID | The record ID must be the same on all records within this segment. | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL072-0005 | |||
| 4679 | TPL073 | SUBMITTING-STATE | The ANSI numeric state code for the U.S. state, territory, or the District of Columbia that has submitted the data. | Required | Must be populated on every record | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL073-0001 | |
| 4680 | TPL073 | SUBMITTING-STATE | Value must be equal to a valid value. | http://www.census.gov/geo/reference/ansi_statetables.html | 10/10/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL073-0002 | ||
| 4681 | TPL073 | SUBMITTING-STATE | SUBMITTING-STATE in this file segment must = SUBMITTING-STATE in the file segment FILE-HEADER-RECORD-TPL-TPL00001 | 10/10/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL073-0003 | |||
| 4682 | TPL074 | RECORD-NUMBER | A sequential number assigned by the submitter to identify each record segment row in the submission file. The RECORD-NUMBER, in conjunction with the RECORD-ID, uniquely identifies a single record within the submission file. | Required | Must be populated on every record | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL074-0001 | |
| 4683 | TPL074 | RECORD-NUMBER | The value must consist of digits 0 through 9 only | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL074-0002 | |||
| 4684 | TPL074 | RECORD-NUMBER | Value must be distinct (non duplicative within segment for same field). | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL074-0003 | |||
| 4685 | TPL075 | INSURANCE-CARRIER-ID-NUM | The state’s internal identification number of the Third Party Liability (TPL) Insurance carrier. | Required | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL075-0001 | |
| 4686 | TPL075 | INSURANCE-CARRIER-ID-NUM | Left justify and pad unused bytes with spaces. | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL075-0002 | |||
| 4687 | TPL076 | TPL-ENTITY-ADDR-TYPE | A code to distinguish various addresses that a TPL entity may have. The state should report whatever types of address they have. | Optional | This data element must be populated on every record within the TPL-ENTITY-CONTACT-INFORMATION record segment. | 11/3/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL076-0001 | |
| 4688 | TPL076 | TPL-ENTITY-ADDR-TYPE | Value must be equal to a valid value. | 06 TPL-Entity Corporate Location 07 TPL-Entity Mailing 08 TPL-Entity Satellite Location 09 TPL-Entity Billing 10 TPL-Entity Correspondence 11 TPL-Other |
2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL076-0002 | ||
| 4689 | TPL077 | INSURANCE-CARRIER-ADDR-LN1 | The street address, including the street name, street number, and room/suite number or letter, for the location for the Third Party Liability (TPL) Insurance carrier. | Optional | Address Line 1 is required and the other two lines can be blank. | 11/3/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL077-0001 | |
| 4690 | TPL077 | INSURANCE-CARRIER-ADDR-LN1 | If the field value is missing, keep the default value of spaces. | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL077-0002 | |||
| 4691 | TPL077 | INSURANCE-CARRIER-ADDR-LN1 | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL077-0003 | |||
| 4692 | TPL078 | INSURANCE-CARRIER-ADDR-LN2 | The street address, including the street name, street number, and room/suite number or letter, for the location for the Third Party Liability (TPL) Insurance carrier. | Optional | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL078-0001 | |
| 4693 | TPL079 | INSURANCE-CARRIER-ADDR-LN3 | The street address, including the street name, street number, and room/suite number or letter, for the location for the Third Party Liability (TPL) Insurance carrier. | Optional | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL079-0001 | |
| 4694 | TPL080 | INSURANCE-CARRIER-CITY | The city of the Third Party Liability (TPL) Insurance carrier. | Optional | Limit characters to alphabet (A-Z, a-z), numerals (0-9), parentheses (()), forward slash (/), dashes (-), periods (.), commas (,), single quote ('), and spaces. | 11/3/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL080-0001 | |
| 4695 | TPL081 | INSURANCE-CARRIER-STATE | The ANSI state numeric code for the U.S. state, Territory, or the District of Columbia code of the Third Party Liability (TPL) Insurance carrier. | Optional | Value must be equal to a valid value. | 11/3/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL081-0001 | |
| 4696 | TPL082 | INSURANCE-CARRIER-ZIP-CODE | The Zip Code of the Third Party Liability (TPL) Insurance carrier. | Optional | Redefined as X(05) and X(04) | 11/3/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL082-0001 | |
| 4697 | TPL082 | INSURANCE-CARRIER-ZIP-CODE | If the field is reported, Zip 5 is required. | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL082-0002 | |||
| 4698 | TPL082 | INSURANCE-CARRIER-ZIP-CODE | The value must consist of digits 0 through 9 only. | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL082-0003 | |||
| 4699 | TPL082 | INSURANCE-CARRIER-ZIP-CODE | If the last 4 digits are not populated or used, then the 4-digit extended zip code should be recorded as “0000”. | 9/23/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL082-0004 | |||
| 4700 | TPL082 | INSURANCE-CARRIER-ZIP-CODE | If the entire zip code field is missing, keep the default value of spaces. | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL082-0005 | |||
| 4701 | TPL083 | INSURANCE-CARRIER-PHONE-NUM | The telephone number of the Third Party Liability (TPL) Insurance carrier. | Optional | Enter numeric characters only (i.e., do not include parentheses, dashes, periods, spaces, etc.) | 11/3/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL083-0001 | |
| 4702 | TPL083 | INSURANCE-CARRIER-PHONE-NUM | The value must consist of digits 0 through 9 only. | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL083-0002 | |||
| 4703 | TPL083 | INSURANCE-CARRIER-PHONE-NUM | If the field value is missing, keep the default value of spaces. | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL083-0003 | |||
| 4704 | TPL084 | TPL-ENTITY-CONTACT-INFO-EFF-DATE | The first day of the time span during which the values in all data elements in the TPL-ENTITY-CONTACT-INFORMATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). This date field is necessary when defining a unique row in a database table. |
Optional | The date must be in “ccyymmdd” format. | 11/3/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL084-0001 | |
| 4705 | TPL084 | TPL-ENTITY-CONTACT-INFO-EFF-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL084-0002 | |||
| 4706 | TPL084 | TPL-ENTITY-CONTACT-INFO-EFF-DATE | Value must be a valid date | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL084-0003 | |||
| 4707 | TPL084 | TPL-ENTITY-CONTACT-INFO-EFF-DATE | Whenever the value in one or more of the data elements in the TPL-ENTITY-CONTACT-INFORMATION record segment changes, a new record segment must be created. | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL084-0004 | |||
| 4708 | TPL084 | TPL-ENTITY-CONTACT-INFO-EFF-DATE | Date cannot be greater than TPL-ENTITY-CONTACT-INFO-END-DATE. | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL084-0005 | |||
| 4709 | TPL085 | TPL-ENTITY-CONTACT-INFO-END-DATE | The last day of the time span during which the values in all data elements in the TPL-ENTITY-CONTACT-INFORMATION record segment are in effect (i.e., the values accurately reflect reality as it is understood to be at the time the record is created). | Optional | The date must be in “ccyymmdd” format. | 11/3/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL085-0001 | |
| 4710 | TPL085 | TPL-ENTITY-CONTACT-INFO-END-DATE | The value must consist of digits 0 through 9 only. | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL085-0002 | |||
| 4711 | TPL085 | TPL-ENTITY-CONTACT-INFO-END-DATE | Value must be a valid date | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL085-0003 | |||
| 4712 | TPL085 | TPL-ENTITY-CONTACT-INFO-END-DATE | If there is no end date (i.e., the record is good into the indefinite future) use the “end-of-time” date (99991231). | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL085-0004 | |||
| 4713 | TPL085 | TPL-ENTITY-CONTACT-INFO-END-DATE | Whenever the value in one or more of the data elements in the TPL-ENTITY-CONTACT-INFORMATION record segment changes, a new record segment must be created. | 2/25/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL085-0005 | |||
| 4714 | TPL085 | TPL-ENTITY-CONTACT-INFO-END-DATE | Overlapping coverage not allowed for same Submitting state , Insurance carrier ID num and TPL entity address type. | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL085-0006 | |||
| 4715 | TPL085 | TPL-ENTITY-CONTACT-INFO-END-DATE | Active TPL-MEDICAID-ELIGIBLE-MAIN with TPL-HEALTH-INSURANCE-COVERAGE-IND = 1 and TPL-MEDICAID-ELIGIBLE-INSURANCE-COVERAGE-INFO records must exist in T-MSIS database or contained in the current submission | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL085-0007 | |||
| 4716 | TPL085 | TPL-ENTITY-CONTACT-INFO-END-DATE | Coverage date span must be fully contained within the set of effective date spans of all active parent records. | 4/30/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL085-0008 | |||
| 4717 | TPL086 | STATE-NOTATION | A free text field for the submitting state to enter whatever information it chooses. | Optional | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). | 9/23/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL086-0001 | |
| 4718 | TPL086 | STATE-NOTATION | For pipe-delimited files, states can populate the STATE-NOTATION field with “n/a,” “n.a.” or leave the field blank (i.e., submitted as "pipe pipe" with nothing in between (||) ) when not using the field to record specific comments. For fixed-length files, states should space-fill the STATE-NOTATION field when not using the field to record specific comments, and right-pad the field with spaces when the field does contain verbiage. |
9/23/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL086-0002 | |||
| 4719 | TPL090 | INSURANCE-CARRIER-NAIC-CODE | The National Association of Insurance Commissioners (NAIC) code of the Third Party Liability (TPL) Insurance carrier. | Optional | Use only alphabetic characters, (A-Z, a-z), numerals (0-9), spaces ( ), dashes (-), periods (.), forward slashes (/), single quotes (‘). | 11/3/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL090-0001 | |
| 4720 | TPL091 | INSURANCE-CARRIER-NAME | The name of the Third Party Liability (TPL) Insurance carrier. | Optional | Field is required on all records. | 11/3/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL091-0001 | |
| 4721 | TPL091 | INSURANCE-CARRIER-NAME | Use only alphabetic characters, (A-Z, a-z), numerals (0-9), spaces ( ), dashes (-), periods (.), forward slashes (/), single quotes (‘). | 10/10/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL091-0002 | |||
| 4722 | TPL091 | INSURANCE-CARRIER-NAME | If the field value is missing, keep the default value of spaces. | 10/10/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL091-0003 | |||
| 4723 | TPL092 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | The NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE distinguishes “controlling” health plan identifiers (CHPIDs), “subhealth” health plan identifiers (SHPIDs), and other entity identifiers (OEIDs) from one another. (See 45 CFR 162 Subpart E. http://www.gpo.gov/fdsys/pkg/FR-2012-09-05/pdf/2012-21238.pdf | NA | Large health plans are required to obtain national identifiers by November 5, 2014, small health plans by November 5, 2015 | 11/3/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL092-0001 | |
| 4724 | TPL092 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | Covered entities must use the national identifiers in the standard transactions on or after November 7, 2016 | 10/10/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL092-0002 | |||
| 4725 | TPL092 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | Value must be in the set of valid values | 1 Controlling Health Plan (CHP) ID 2 Subhealth Plan (SHP) ID 3 Other Entity Identifier (OEID) |
10/10/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL092-0003 | ||
| 4726 | TPL092 | NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE | If the type HEALTH-CARE-ENTITY-ID-TYPE is unknown, populate the field with a space | 10/10/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL092-0004 | |||
| 4727 | TPL093 | NATIONAL-HEALTH-CARE-ENTITY-ID | The national identifier of the health care entity (controlling health plan, subhealth plan, or other entity) at the most granular sub-health plan level of the Medicaid or CHIP health plan in which an individual is enrolled. (See 45 CFR 162 Subpart E. http://www.gpo.gov/fdsys/pkg/FR-2012-09-05/pdf/2012-21238.pdf ) | NA | Large health plans are required to obtain national identifiers by November 5, 2014, small health plans by November 5, 2015. States may report prior to these dates if available. | 11/3/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL093-0001 | |
| 4728 | TPL093 | NATIONAL-HEALTH-CARE-ENTITY-ID | Covered entities must use the national identifiers in the standard transactions on or after November 7, 2016. | 10/10/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL093-0002 | |||
| 4729 | TPL093 | NATIONAL-HEALTH-CARE-ENTITY-ID | This field is required for all eligible persons enrolled in managed care on or after the mandated dates above. If the eligible person is not enrolled in managed care, fill the field with spaces. | 10/10/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL093-0003 | |||
| 4730 | TPL093 | NATIONAL-HEALTH-CARE-ENTITY-ID | Valid characters in the text string are limited to alpha characters (A-Z, a-z), numbers (0-9) | 10/10/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL093-0004 | |||
| 4731 | TPL093 | NATIONAL-HEALTH-CARE-ENTITY-ID | National identifiers in the TPL file must match either a controlling health plan (CHP) identifier or subhealth plan (SHP) identifier in the Managed Care subject area. | 10/10/2013 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL093-0005 | |||
| 4732 | TPL094 | NATIONAL-HEALTH-CARE-ENTITY-NAME | The legal name of the health care entity identified by the corresponding value in the NATIONAL-HEALTH-CARE-ENTITY-ID field. | NA | Use the descriptive name assigned by the state as it exists in the state’s MMIS. | 11/3/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL094-0001 | |
| 4733 | TPL094 | NATIONAL-HEALTH-CARE-ENTITY-NAME | The field can contain any alphanumeric charaters, digits or symbols except the "pipe" (|). |
9/23/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL094-0002 | |||
| 4734 | TPL094 | NATIONAL-HEALTH-CARE-ENTITY-NAME | When this data element is not populated or used, it should be left blank (i.e., submitted as "pipe pipe" with nothing in between (||) on PSV files and space-filled on FLF files). | 9/23/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL094-0003 | |||
| 4735 | TPL087 | FILLER | For pipe-delimited files, FILLER that is shown at the end of each record layout is applicable only to fixed-length files and therefore should be ignored in pipe-delimited files. For fixed-length files, FILLER that is shown at the end of each record layout should be space-filled in fixed-length files. |
9/23/2015 | TPL | TPL-ENTITY-CONTACT-INFORMATION-TPL00006 | TPL087-0001 |
| File Type | application/vnd.openxmlformats-officedocument.spreadsheetml.sheet |
| File Modified | 0000-00-00 |
| File Created | 0000-00-00 |
© 2026 OMB.report | Privacy Policy