Transformed - Medicaid Statistical Information System (T-MSIS)
Medicaid Statistical Information System (MSIS) and the Transformed - Medicaid Statistical Information System (T-MSIS) (CMS-R-284)
2 - T-MSIS V2_0 Data Dictionary Appendices - 2015-11-24
Transformed - Medicaid Statistical Information System (T-MSIS)
OMB: 0938-0345
T-MSIS Data Dictionary Appendices
Version:
Nov15v2.0
T-MSIS
Data Dictionary Appendices


Contents
Managed Care Plan Information File Valid Values 11
CORE-BASED-STATISTICAL-AREA-CODE 13
FILE-ENCODING-SPECIFICATION 14
MANAGED-CARE-SERVICE-AREA-NAME 24
NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE 26
SUBMISSION-TRANSACTION-TYPE 30
FACILITY-GROUP-INDIVIDUAL-CODE 40
FILE-ENCODING-SPECIFICATION 41
PROV-MEDICAID-ENROLLMENT-STATUS-CODE 58
SUBMISSION-TRANSACTION-TYPE 64
CERTIFIED-AMERICAN-INDIAN/ALASKAN-NATIVE-INDICATOR 70
CITIZENSHIP-VERIFICATION-FLAG 73
FILE-ENCODING-SPECIFICATION 83
HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-CODE 86
HEALTH-HOME-CHRONIC-CONDITION 87
IMMIGRATION-VERIFICATION-FLAG 90
MAINTENANCE-ASSISTANCE-STATUS 95
MEDICAID-BASIS-OF-ELIGIBILITY 98
MFP-REASON-PARTICIPATION-ENDED 102
MFP-REINSTITUTIONALIZED-REASON 103
NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE 104
PRIMARY-LANGUAGE-ENGL-PROF-CODE 107
SSI-STATE-SUPPLEMENT-STATUS-CODE 113
SUBMISSION-TRANSACTION-TYPE 118
Third-party Liability File Valid Values 122
FILE-ENCODING-SPECIFICATION 125
NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE 130
SUBMISSION-TRANSACTION-TYPE 134
TPL-HEALTH-INSURANCE-COVERAGE-IND 137
TYPE-OF-OTHER-THIRD-PARTY-LIABILITY 139
ADMITTING-DIAGNOSIS-CODE-FLAG 147
CLAIM-PYMT-REM-CODE-1 to CLAIM-PYMT-REM-CODE-4 168
CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT 171
DIAGNOSIS-CODE-1 to DIAGNOSIS-CODE-12 177
DIAGNOSIS-CODE-FLAG-1 to DIAGNOSIS-CODE-FLAG-12 178
DIAGNOSIS-POA-FLAG-1 to DIAGNOSIS-POA-FLAG-12 179
DISPENSING-PRESCRIPTION-DRUG-PROV-NPI 181
DISPENSING-PRESCRIPTION-DRUG-PROV-TAXONOMY 182
FILE-ENCODING-SPECIFICATION 187
FUNDING-SOURCE-NONFEDERAL-SHARE 193
HEALTH-CARE-ACQUIRED-CONDITION-IND 198
LINE-ADJUSTMENT-REASON-CODE 204
OCCURRENCE-CODE-01 to OCCURRENCE-CODE-10 209
PRESCRIBING-PROV-SPECIALTY 219
PROCEDURE-CODE 1 TO PROCEDURE-CODE-6 222
PROCEDURE-CODE-FLAG-1 - PROCEDURE-CODE-FLAG-6 223
SUBMISSION-TRANSACTION-TYPE 240
UNDER-DIRECTION-OF-PROV-NPI 255
UNDER-DIRECTION-OF-PROV-TAXONOMY 256
UNDER-SUPERVISION-OF-PROV-NPI 257
UNDER-SUPERVISION-OF-PROV-TAXONOMY 258
XIX-MBESCBES-CATEGORY-OF-SERVICE 261
XXI-MBESCBES-CATEGORY-OF-SERVICE 262
Appendix B: Home and Community-Based Services (HCBS) Taxonomy 263
Appendix C: Comprehensive Eligibility Crosswalk 280
Appendix D: Types of Service (TOS) Reference 293
Appendix E: Program Type Reference 303
Appendix F: Eligibility Group Table 310
Appendix G: ISO 639 Language Codes Reference 323
Appendix I: MBES CBES Category of Service Line Definitions for the 64.9 Base Form 357
Appendix J: MBES CBES Category of Service Line Definitions for the 21 Form 387
Appendix K: Crosswalk of T-MSIS to MSIS Type of Service Values 392
Appendix M: Crosswalk of T-MSIS, MSIS and MMA Duel Eligible Code 460
Appendix N: Coding Specific Data Elements for Claim Files 462
Appendix O: TYPE-OF-SERVICE Hierarchy Table 464
Appendix P: CMS Guidance Library 465
Appendix P.01: Submitting Adjustment Claims to TMSIS 466
Appendix P.03: Full File Replacement Submissions for Non-Claim T-MSIS File revised 478
Appendix P.04: Non-Claim Full File Refreshes - Amount of History Required 482
Appendix P.05: Populating Qualifier Fields and Their Associated Value Fields 485
Appendix P.06: IIFI (Inter/Intra-File Indices) 493
Appendix P.07: Finding Provider Roles on STD Transactions 516
Appendix Q: Terms and Abbreviations 9
Appendix A: Valid Values
Managed Care Plan Information File Valid Values

Managed
Care Plan Information File Valid Values
ACCREDITATION-ORGANIZATION
Code |
Description |
01 |
National committee for quality assurance – excellent |
02 |
National committee for quality assurance – commendable |
03 |
National committee for quality assurance – provisional |
04 |
National committee for quality assurance – new plan – no longer a valid accreditation level |
05 |
URAC – full |
06 |
URAC – conditional |
07 |
URAC – provisional |
08 |
Accreditation Association for Ambulatory Health Care, Inc. (AAAHC) – 3 years |
09 |
Accreditation Association for Ambulatory Health Care, Inc. (AAAHC) – 1 year - no longer valid accreditation level |
10 |
Accreditation Association for Ambulatory Health Care, Inc. (AAAHC) – 6 months - no longer valid accreditation level |
11 |
Not accredited |
12 |
Other |
13 |
National committee for quality assurance-- accredited |
14 |
National committee for quality assurance - interim |
15 |
National committee for quality assurance - denied |
Additional accreditation information can be found at:
NCQA
http://www.ncqa.org/Programs/Accreditation/HealthPlanHP/AccreditationLevels.aspx
AAAHC
http://www.aaahc.org/en/accreditation/General-information/policies/terms-of-accreditation/
CORE-BASED-STATISTICAL-AREA-CODE
Code |
Description |
1 |
The MCO’s service area falls partially or entirely inside one or more metropolitan areas. |
2 |
The MCO’s service area falls partially or entirely inside one or more micropolitan areas, but not within any metropolitan areas. |
3 |
The MCO’s service area falls entirely outside of all metropolitan and micropolitan areas. |
Managed
Care Plan Information File Valid Values
FILE-ENCODING-SPECIFICATION
Code |
Description |
FIX |
The file follows a fixed length format. |
PSV |
The file follows a pipe-delimited format. |
Managed
Care Plan Information File Valid Values

Managed
Care Plan Information File Valid Values
FILE-NAME
Code |
Description |
MNGDCARE |
Managed Care Plan Information File |

Managed
Care Plan Information File Valid Values
FILE-STATUS-INDICATOR
Code |
Description |
P |
Production File |
T |
Test File |

Managed
Care Plan Information File Valid Values
MANAGED-CARE-ADDR-TYPE
Code |
Description |
1 |
MCO’s corporate address and contact information |
2 |
MCO’s mailing address |
3 |
MCO’s service location address |
4 |
MCO’s Billing address and contact information |
5 |
CEO’s address and contact information |
6 |
CFO’s address and contact information |
7 |
Other |

Managed
Care Plan Information File Valid Values
MANAGED-CARE-COUNTY
|

Managed
Care Plan Information File Valid Values
MANAGED-CARE-PLAN-POP
See Appendix F: Eligibility Group Table for listing of valid values. |

Managed
Care Plan Information File Valid Values
MANAGED-CARE-PLAN-TYPE
Code |
Description |
01 |
Comprehensive MCO |
02 |
Traditional PCCM Provider |
03 |
Enhanced PCCM Provider |
04 |
HIO |
05 |
Medical-only PIHP (risk or non-risk/non-comprehensive/with inpatient hospital or institutional services) |
06 |
Medical-only PAHP (risk or non-risk/non-comprehensive/no inpatient hospital or institutional services) |
07 |
Long Term Care (LTC) PIHP |
08 |
Mental Health (MH) PIHP |
09 |
Mental Health (MH) PAHP |
10 |
Substance Use Disorders (SUD) PIHP |
11 |
Substance Use Disorders (SUD) PAHP |
12 |
Mental Health (MH) and Substance Use Disorders (SUD) PIHP |
13 |
Mental Health (MH) and Substance Use Disorders (SUD) PAHP |
14 |
Dental PAHP |
15 |
Transportation PAHP |
16 |
Disease Management PAHP |
17 |
PACE |
18 |
Pharmacy PAHP |
99 |
Unknown |
60 |
Accountable Care Organization |
70 |
Health/Medical Home |
80 |
Integrated Care For Dual Eligibles |

Managed
Care Plan Information File Valid Values
MANAGED-CARE-PROFIT-STATUS
01 |
501(C)(3) NON-PROFIT |
02 |
FOR-PROFIT, CLOSELY HELD |
03 |
FOR-PROFIT, PUBLICLY TRADED |
04 |
OTHER |
99 |
Unknown |

Managed
Care Plan Information File Valid Values
MANAGED-CARE-PROGRAM
1 |
Medicaid State Plan |
2 |
CHIP State Plan |
3 |
Both Medicaid and CHIP |

Managed
Care Plan Information File Valid Values
MANAGED-CARE-SERVICE-AREA
1 |
Statewide- The managed care entity provides services to beneficiaries throughout the entire state. |
2 |
County- The managed care entity provides services to beneficiaries in specified counties. |
3 |
City- The managed care entity provides services to beneficiaries in specified cities. |
4 |
Region- The managed care entity provides services to beneficiaries in specified regions, not defined by individual counties within the state (“region” is state-defined). |
5 |
Zip Code- The managed care entity program provides services to beneficiaries in specified zip codes. |
6 |
Other- The managed care entity provides services to beneficiaries in "other" area(s), not Statewide, County, City, or Region. |

Managed
Care Plan Information File Valid Values
MANAGED-CARE-SERVICE-AREA-NAME
|

Managed
Care Plan Information File Valid Values
MANAGED-CARE-STATE
|

Managed
Care Plan Information File Valid Values
NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE
1 |
Controlling Health Plan (CHP) ID – the national health plan identifier of a health plan that either controls its own business activities, actions, or policies, or is controlled by an entity that is not a health plan and exercises sufficient control over the subhealth plan(s) under it so as to direct its own business activities, actions, or policies, as well as those of any subhealth plans under it. Every health plan will have a CHP. |
2 |
Subhealth Plan (SHP) ID – the national health plan identifier of a health plan whose business activities, actions, or policies are directed by a controlling health plan. All subhealth HPIDs should be reported. Note: While all health plans will have a CHP, not all plans will have one or more SHPs. |
3 |
Other Entity Identifier (OEID) – a national identifier for entities that are not health plans, health care providers, or individuals (as defined in 45 CFR 160.103), but that need to be identified in standard transactions (including, for example, third party administrators, transaction vendors, clearinghouses, and other payers). Other entities are not required to obtain an OEID, but they could obtain and use one if they need to be identified in covered transactions. |

Managed
Care Plan Information File Valid Values
OPERATING-AUTHORITY
01 |
1115 demonstration waiver program – demonstration projects under which most provisions of Section 1902 of the Social Security Act are waived and/or expenditures that would not otherwise be eligible for FFP are authorized. States use these to expand eligibility, restructure Medicaid coverage and secure programmatic flexibility. |
02 |
1915(b) waiver program – waivers of most provisions of Section 1902 of the Social Security Act in order to limit beneficiaries’ freedom of choice of provider; selectively contract with providers; or provide additional services to beneficiaries (State may include BBA special populations) |
03 |
1932(a) state plan option to use managed care for MCO and PCCM programs – mandatory managed care programs implemented through the state plan (State must exclude or permit voluntary enrollment of specific populations) |
04 |
1915(a) voluntary managed care program – an MCO managed care program in which enrollment is voluntary and therefore does not require a waiver.
|
05 |
Concurrent 1915(b)/1915(c) waivers– programs, or portions thereof, operating under both 1915(b) managed care and 1915(c) home and community-based services waivers. |
06 |
Concurrent 1915(a)/1915(c) waivers– programs, or portions thereof, operating under both 1915(a) voluntary managed care and 1915(c) home and community-based services waiver |
07 |
Concurrent 1932(a)/1915(c) waivers - programs, or portions thereof, operating under both 1932(a) managed care and 1915(c) home and community-based services waiver. |
08 |
PACE – program that provides pre-paid, capitated comprehensive, health care services to the frail elderly. |
09 |
1905(t) voluntary PCCM program – A PCCM managed care program in which enrollment is voluntary and therefore does not require a waiver. |
10 |
1937benchmark benefit program—programs to provide benefits that differ from Medicaid state plan benefits using managed care and implemented through the state plan. |
11 |
1902(a)(70) non-emergency medical transportation program –non-emergency medical transportation brokerage programs implemented through the state plan which can vary scope of services, operate on a less-than-statewide basis, and limit freedom of choice |
12 |
Concurrent 1915(b)/1915(i) HCBS state plan services - the optional 1915(i) state plan Home and Community-Based Services (HCBS) benefit operated in conjunction with a 1915(b) managed care waiver program. |
13 |
Concurrent 1915(a)/ 1915(i) HCBS state plan services - the optional 1915(i) state plan Home and Community-Based Services (HCBS) benefit operated in conjunction with a 1915(a) voluntary managed care program. |
14 |
Concurrent 1932(a)/ 1915(i) HCBS state plan services - the optional 1915(i) state plan Home and Community-Based Services (HCBS) benefit operated in conjunction with a 1932(a) managed care state plan option. |
15 |
1945 Health Homes. |

Managed
Care Plan Information File Valid Values
RECORD-ID
MCR00001 |
FILE-HEADER-RECORD-MANAGED-CARE |
MCR00002 |
MANAGED-CARE-MAIN |
MCR00003 |
MANAGED-CARE-LOCATION-AND-CONTACT-INFO |
MCR00004 |
MANAGED-CARE-SERVICE-AREA |
MCR00005 |
MANAGED-CARE-OPERATING-AUTHORITY |
MCR00006 |
MANAGED-CARE-PLAN-POPULATION-ENROLLED |
MCR00007 |
MANAGED-CARE-ACCREDITATION-ORGANIZATION |
MCR00008 |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO |
MCR00009 |
CHPID-SHPID-RELATIONSHIP |

Managed
Care Plan Information File Valid Values
REIMBURSEMENT-ARRANGEMENT
01 |
Risk-based Capitation, no incentives or risk-sharing |
02 |
Risk-based Capitation with Incentive Arrangements |
03 |
Risk-based Capitation with other risk-sharing Arrangements |
04 |
Non-Risk Capitation |
05 |
Fee-For-Service |
06 |
Primary Care Case Management Payment |
07 |
Other |
08 |
Primary Care Case Management Payment plus Fee-For-Service |
88 |
Not Applicable |
99 |
Unknown |

Managed
Care Plan Information File Valid Values
SUBMISSION-TRANSACTION-TYPE
C |
Create File—a file that contains a complete set of transactions/changes processed since the last Create file submission. States may submit only one valid Create file per reporting period and data file type. |
R |
Replacement File—a Replacement submission is a replacement of the month’s data. It will completely replace the immediate prior submission. If a later replacement entry is received, it will overwrite the previous replacement, as well as a prior Create or Update submission for the same data type and reporting period. |
U |
Update File—a file that contains T-MSIS record segments created in response to business rule rejects. Note: The records in an Update file are not generated as a result of a change processed in the state’s Medicaid or Medicaid-related systems during the current reporting month. These Update file record segments may be unchanged from the ones submitted previously for various reasons (for example, the state may be unable to process a change record in their Medicaid / Medicaid-related systems to correct the issue because the state is simply passing through to T-MSIS data that originated outside of the state’s systems).[1] Conversely, the records may be different from those previously submitted, but the change is the result of a fix whose root cause problem was an issue in the T-MSIS file-creation or replacement process at CMS. Regardless, the record was not generated from a change that occurred in the state’s source data. |

Managed
Care Plan Information File Valid Values
SUBMITTING-STATE
|
Provider File Valid Values

Provider
File Valid Values
ACCEPTING-NEW-PATIENTS-IND
0 |
No |
1 |
Yes |
8 |
N/A – The individual only practices as a member of a group. |

Provider
File Valid Values
ADDR-BORDER-STATE-IND
Code |
Description |
0 |
No |
1 |
Yes |
8 |
N/A - State does not distinguish “border state providers”. |
ADDR-COUNTY
Provider
File Valid Values

Provider
File Valid Values
ADDR-STATE
|

Provider
File Valid Values
ADDR-TYPE
1 |
Provider Billing |
2 |
Provider Mailing |
3 |
Provider Practice |
4 |
Provider Service Location |

Provider
File Valid Values
AFFILIATED-PROGRAM-TYPE
1 |
Health Plan (NHP-ID) – The value in the AFFILIATED-PROGRAM-ID data element contains the National Health Plan Identifier of health plan in which the provider is enrolled to provide services including through the state plan and a waiver. |
2 |
Health Plan (state-assigned health plan ID) – The value in the AFFILIATED-PROGRAM-ID data element contains the state-assigned health plan Identifier of health plan in which the provider is enrolled to provide services including through the state plan and a waiver. |
3 |
Waiver – The value in the AFFILIATED-PROGRAM-ID data element contains an identifier for the waiver in which a provider is allowed to deliver services to eligible beneficiaries. |
4 |
Health Home Entity – The value in the AFFILIATED-PROGRAM-ID data element contains the name of the health home in which a provider is participating. The health home entity is responsible for providing health home services to the patient in conformance with the Health Home SPA. This is the name that the state uses to uniquely identify the health home team. This entity can be a designated provider (e.g., physician, clinic, behavioral health organization), a health team which links to a designated provider, or a health team (physicians, nurses, behavioral health professionals). |
5 |
Other – The value in the AFFILIATED-PROGRAM-ID data element contains an identifier for something other than a health plan, waiver, or health home entity |

Provider
File Valid Values
BED-TYPE-CODE
|
|
1 |
Intermediate Care Facility for the Intellectually Disabled |
2 |
Inpatient |
3 |
Nursing Facility |
4 |
Title 18 Skilled Nursing Facility (T18 SNF) |
8 |
Not Applicable |

Provider
File Valid Values
FACILITY-GROUP-INDIVIDUAL-CODE
01 |
Facility – The entity identified by the associated SUBMITTING-STATE-PROV-ID is a facility. |
02 |
Group – The entity identified by the associated SUBMITTING-STATE-PROV-ID is a group of individual practitioners. |
03 |
Individual – The entity identified by the associated SUBMITTING-STATE-PROV-ID is an individual practitioner. |

Provider
File Valid Values
FILE-ENCODING-SPECIFICATION
FIX |
The file follows a fixed length format. |
PSV |
The file follows a pipe-delimited format. |

Provider
File Valid Values
FILE-NAME
PROVIDER |
Provider File |

Provider
File Valid Values
FILE-STATUS-INDICATOR
P |
Production file |
T |
Test file |

Provider
File Valid Values
LICENSE-TYPE
1 |
State, county, or municipality professional or business license |
2 |
DEA license |
3 |
Professional society accreditation |
4 |
CLIA accreditation |
5 |
Other |

Provider
File Valid Values
OWNERSHIP-CODE
01 |
Voluntary – Non-Profit – Religious Organizations |
02 |
Voluntary – Non-Profit – Other |
03 |
Voluntary – multiple owners |
04 |
Proprietary – Individual |
05 |
Proprietary – Corporation |
06 |
Proprietary – Partnership |
07 |
Proprietary – Other |
08 |
Proprietary – multiple owners |
09 |
Government – Federal |
10 |
Government – State |
11 |
Government – City |
12 |
Government – County |
13 |
Government – City-County |
14 |
Government – Hospital District |
15 |
Government – State and City/County |
16 |
Government – other multiple owners |
17 |
Voluntary /Proprietary |
18 |
Proprietary/Government |
19 |
Voluntary/Government |
88 |
N/A – The individual only practices as part of a group, e.g., as an employee |
Provider
File Valid Values
PROV-CLASSIFICATION-TYPE
1 |
Taxonomy code |
2 |
Provider specialty code |
3 |
Provider type code |
4 |
Authorized category of service code |
NOTE: The valid value code ‘47’ in the PROV-CLASSIFICATION-TYPE = 2 (Provider Specialty Code) can be used now.
“47" = Independent Diagnostic Testing Facility (IDTF)”
Provider
File Valid Values
Code |
Description |
01 |
General Practice |
02 |
General Surgery |
03 |
Allergy/Immunology |
04 |
Otolaryngology |
05 |
Anesthesiology |
06 |
Cardiology |
07 |
Dermatology |
08 |
Family Practice |
09 |
Interventional Pain Management |
10 |
Gastroenterology |
11 |
Internal Medicine |
12 |
Osteopathic Manipulative Therapy |
13 |
Neurology |
14 |
Neurosurgery |
15 |
Speech Language Pathologist |
16 |
Obstetrics/Gynecology |
17 |
Hospice and Palliative Care |
18 |
Ophthalmology |
19 |
Oral Surgery (dentists only) |
20 |
Orthopedic Surgery |
21 |
Cardiac Electrophysiology |
22 |
Pathology |
23 |
Sports Medicine |
24 |
Plastic and Reconstructive Surgery |
25 |
Physical Medicine and Rehabilitation |
26 |
Psychiatry |
27 |
Geriatric Psychiatry |
28 |
Colorectal Surgery (formerly proctology) |
29 |
Pulmonary Disease |
30 |
Diagnostic Radiology |
31 |
Cardiac Rehabilitation & Intensive Cardiac Rehabilitation |
32 |
Anesthesiologist Assistant |
33 |
Thoracic Surgery |
34 |
Urology |
35 |
Chiropractic |
36 |
Nuclear Medicine |
37 |
Pediatric Medicine |
38 |
Geriatric Medicine |
39 |
Provider
File Valid Values |
40 |
Hand Surgery |
41 |
Optometry |
42 |
Certified Nurse Midwife |
43 |
Certified Registered Nurse Anesthetist (CRNA) |
44 |
Infectious Disease |
45 |
Mammography Center |
46 |
Endocrinology |
47 |
Independent Diagnostic Testing Facility (IDTF) |
48 |
Podiatry |
49 |
Ambulatory Surgical Center |
50 |
Nurse Practitioner |
51 |
Medical Supply Company with Orthitist |
52 |
Medical Supply Company with Prosthetist |
53 |
Medical Supply Company with Orthitist-Prosthetist |
54 |
Other Medical Supply Company |
55 |
Individual Certified Orthotist |
56 |
Individual Certified Prosthetist |
57 |
Individual Certified Orthitist-Prosthetist |
58 |
Medical Supply Company with Pharmacist |
59 |
Ambulance Service Provider |
60 |
Public Health or Welfare Agency |
61 |
Voluntary Health or Charitable Agency |
62 |
Psychologist, Clinical |
63 |
Portable X-Ray Supplier |
64 |
Audiologist |
65 |
Physical Therapist in Private Practice |
66 |
Rheumatology |
67 |
Occupational Therapist in Private Practice |
68 |
Psychologist, Clinical |
69 |
Clinical Laboratory |
70 |
Single or Multispecialty Clinic or Group Practice |
71 |
Registered Dietitian or Nutrition Professional |
72 |
Pain Management |
73 |
Mass Immunization Roster Biller |
74 |
Radiation Therapy Center |
75 |
Slide Preparation Facility |
76 |
Peripheral Vascular Disease |
77 |
Vascular Surgery |
78 |
Cardiac Surgery |
79 |
Addiction Medicine |
80 |
Licensed Clinical Social Worker |
81 |
Critical Care (Intensivists) |
82 |
Hematology |
83 |
Hematology/Oncology |
84 |
Preventive Medicine |
85 |
Maxillofacial Surgery |
86 |
Neuropsychiatry |
87 |
All Other Suppliers |
89 |
Certified Clinical Nurse Specialist |
90 |
Medical Oncology |
91 |
Surgical Oncology |
92 |
Radiation Oncology |
93 |
Emergency Medicine |
94 |
Interventional Radiology |
95 |
Advance Diagnostic Imaging |
96 |
Optician |
97 |
Physician Assistant |
98 |
Gynecological/Oncology |
A0 |
Hospital-General |
A1 |
Skilled Nursing Facility |
A2 |
Intermediate Care Nursing Facility |
A3 |
Other Nursing Facility |
A4 |
Home Health Agency |
A5 |
Pharmacy |
A6 |
Medical Supply Company with Respiratory Therapist |
A7 |
Department Store |
A8 |
Grocery Store |
A9 |
Indian Health Service facility |
B1 |
Oxygen supplier |
B2 |
Pedorthic personnel |
B3 |
Medical supply company with pedorthic personnel |
B4 |
Rehabilitation Agency |
B5 |
Ocularist |
Provider
File Valid Values
Provider
File Valid Values
-
PROV-CLASSIFICATION-TYPE = 3 (Provider Type Code)
Provider Type Code
Provider Type Description
01
Physician
02
Speech Language Pathologist
03
Oral Surgery (Dentist only)
04
Cardiac Rehabilitation and Intensive Cardiac Rehabilitation
05
Anesthesiology Assistant
06
Chiropractic
07
Optometry
08
Certified Nurse Midwife
09
Certified Registered Nurse Anesthetist (CRNA)
10
Mammography Center
11
Independent Diagnostic Testing Facility (IDTF)
12
Podiatry
13
Ambulatory Surgical Center
14
Nurse Practitioner
15
Medical Supply Company with Orthotist
16
Medical Supply Company with Prosthetist
17
Medical Supply Company with Orthotist-Prosthetist
18
Other Medical Supply Company
19
Individual Certified Orthotist
20
Individual Certified Prosthetist
21
Individual Certified Prosthetist-Orthotist
22
Medical Supply Company with Pharmacist
23
Ambulance Service Provider
24
Public Health or Welfare Agency
25
Voluntary Health or Charitable Agency
26
Psychologist, Clinical
27
Portable X-Ray Supplier
28
Audiologist
29
Physical Therapist in Private Practice
30
Occupational Therapist in Private Practice
31
Clinical Laboratory
32
Clinic or Group Practice
33
Registered Dietitian or Nutrition Professional
34
Mass Immunizer Roster Biller
35
Radiation Therapy Center
36
Slide Preparation Facility
37
Licensed Clinical Social Worker
38
Certified Clinical Nurse Specialist
39
Advance Diagnostic Imaging
40
Optician
41
Physician Assistant
42
Hospital-General
43
Skilled Nursing Facility
44
Intermediate Care Nursing Facility
45
Other Nursing Facility
46
Home Health Agency
47
Pharmacy
48
Medical Supply Company with Respiratory Therapist
49
Department Store
50
Grocery Store
51
Indian Health Service facility
52
Oxygen supplier
5t3
Pedorthic personnel
54
Medical supply company with pedorthic personnel
55
Rehabilitation Agency
56
Ocularist
57
All Other
Provider
File Valid Values
Code |
Description |
001 |
Inpatient hospital services, other than services in an institution for mental diseases |
002 |
Outpatient hospital services |
003 |
Rural health clinic services |
004 |
Other ambulatory services furnished by a rural health clinic |
005 |
Professional laboratory services |
006 |
Technical laboratory services |
007 |
Professional radiological services |
008 |
Technical radiological services |
009 |
Nursing facility services for individuals age 21 or older (other than services in an institution for mental disease) |
010 |
Early and periodic screening and diagnosis and treatment (EPSDT) services |
011 |
Family planning services and supplies for individuals of child-bearing age |
012 |
Physicians' services |
013 |
Medical and surgical services of a dentist |
014 |
Outpatient substance abuse treatment services. |
015 |
Medical or other remedial care or services, other than physicians' services, provided by licensed practitioners within the scope of practice as defined under State law |
016 |
Home health services - Nursing services |
017 |
Home health services - Home health aide services |
018 |
Home health services - Medical supplies, equipment, and appliances suitable for use in the home |
019 |
Home health services - Physical therapy provided by a home health agency or by a facility licensed by the State to provide medical rehabilitation services |
020 |
Home health services - Occupational therapy provided by a home health agency or by a facility licensed by the State to provide medical rehabilitation services |
021 |
Home health services - Speech pathology and audiology services provided by a home health agency or by a facility licensed by the State to provide medical rehabilitation services |
022 |
Private duty nursing services |
023 |
Advanced practice nurse services |
024 |
Pediatric nurse |
025 |
Nurse-midwife service |
026 |
Nurse practitioner services |
027 |
Respiratory care for ventilator-dependent individuals |
028 |
Clinic services |
029 |
Dental services |
030 |
Physical therapy services (when not provided under home health services) |
031 |
Occupational therapy services (when not provided under home health services) |
032 |
Speech, hearing, and language disorders services (when not provided under home health services) |
033 |
Prescribed drugs |
034 |
Over-the-counter medications. |
035 |
Dentures |
036 |
Prosthetic devices |
037 |
Eyeglasses |
038 |
Hearing Aids |
039 |
Diagnostic services |
040 |
Screening services |
041 |
Preventive services |
042 |
Well-baby and well-child care services as defined by the State. |
043 |
Rehabilitative services |
044 |
Inpatient hospital services for individuals age 65 or older in institutions for mental diseases |
045 |
Nursing facility services for individuals age 65 or older in institutions for mental diseases |
046 |
Intermediate care facility (ICF/IIDICF/IID) services |
047 |
Nursing facility services, other than in institutions for mental diseases |
048 |
Inpatient psychiatric services for individuals under age 21 |
049 |
Outpatient mental health services, other than Outpatient substance abuse treatment services. This TOS includes services furnished in a State-operated mental hospital and including community-based services. |
050 |
Inpatient substance abuse treatment services and residential substance abuse treatment services. |
051 |
Personal care services |
052 |
Primary care case management services |
053 |
Targeted case management services |
054 |
Case Management services other than those that meet the definition of primary care case management services or targeted case management services |
055 |
Care coordination services. |
056 |
Transportation services |
057 |
Enabling services |
058 |
Services furnished in a religious nonmedical health care institution |
059 |
Skilled nursing facility services for individuals under age 21 |
060 |
Emergency hospital services |
061 |
Critical access hospital services |
062 |
HCBS - Case management services |
063 |
HCBS - Homemaker services |
064 |
HCBS - Home health aide services |
065 |
HCBS - Personal care services |
066 |
HCBS - Adult day health services |
067 |
HCBS - Habilitation services |
068 |
HCBS - Respite care services |
069 |
HCBS - Day treatment or other partial hospitalization services, psychosocial rehabilitation services and clinic services (whether or not furnished in a facility) for individuals with chronic mental illness |
070 |
HCBS - Day Care |
071 |
HCBS - Training for family members |
072 |
HCBS - Minor modification to the home |
073 |
HCBS - Other services requested by the agency and approved by CMS as cost effective and necessary to avoid institutionalization |
074 |
HCBS - Expanded habilitation services - Prevocational services |
075 |
HCBS - Expanded habilitation services - Educational services |
076 |
HCBS - Expanded habilitation services - Supported employment services, which facilitate paid employment |
077 |
HCBS-65-plus - Case management services |
078 |
HCBS-65-plus - Homemaker services |
079 |
HCBS-65-plus - Home health aide services |
080 |
HCBS-65-plus - Personal care services |
081 |
HCBS-65-plus - Adult day health services |
082 |
HCBS-65-plus - Respite care services |
083 |
HCBS-65-plus - Other medical and social services |
084 |
Sterilizations |
085 |
Prenatal care and pre-pregnancy family planning services and supplies. |
086 |
Other Pregnancy-related Procedures |
087 |
Hospice services |
088 |
Any other health care services or items specified by the Secretary and not excluded under regulations. |
115 |
Residential care |

Provider
File Valid Values
PROV-ENROLLMENT-METHOD
Code |
Description |
1 |
Enrolled through use of Medicare enrollment system (State did not require that provider submit application. Rather Provider is active Medicare provider and state Medicaid program accepted these credentials as sufficient to participate as state Medicaid provider.) |
2 |
Enrolled through use of state-based provider application |
3 |
Other |

Provider
File Valid Values
PROV-IDENTIFIER-TYPE
Code |
Description |
1 |
State-specific Medicaid Provider ID |
2 |
NPI |
3 |
Medicare ID |
4 |
NCPDP ID |
5 |
Federal Tax ID |
6 |
State Tax ID |
7 |
SSN |
8 |
Other |

Provider
File Valid Values
PROV-MEDICAID-ENROLLMENT-STATUS-CODE
Code |
Description |
01 |
Active - Active Do Not Pay |
02 |
Active - Active Reinstated |
03 |
Active - Active |
04 |
Active - Eligibility Verification |
05 |
Active - Encounter Only |
06 |
Active - Financial Trans Only |
20 |
Denied - Denied Two Provider Numbers |
21 |
Denied - For Other Reasons |
22 |
Denied - Invalid License |
23 |
Denied - Not Eligible |
24 |
Denied - Same Number Assigned |
40 |
Pending - Enrollment |
41 |
Pending - License/Cert Verification |
42 |
Pending - Missing Documentation |
43 |
Pending - No License/Temp License |
44 |
Pending - NPI Invalid |
45 |
Pending - Rate Determination |
46 |
Pending - Signed Agreement |
47 |
Pending - Status Approval |
48 |
Pending - W9 Missing or Incomplete |
60 |
Term - Abuse of billing privileges |
61 |
Term - Action Taken by Medicaid/CHIP |
62 |
Term - Action Taken by Medicare |
63 |
Term - Change of Ownership |
64 |
Term - Failure to report a change of address/ownership |
65 |
Term - False or misleading information |
66 |
Term - Federal exclusion/ debarment, etc. |
67 |
Term - Felony conviction |
68 |
Term - Involuntary Termination |
69 |
Term - License Expired |
70 |
Term - License Revoked |
71 |
Term - Loss of license or other State action |
72 |
Term - Medicare/Medicaid Exclusion |
73 |
Term - Medicaid Authority |
74 |
Term - Medicare Termination |
75 |
Term - Misuse of billing number |
76 |
Term - No Claims Activity |
77 |
Term - Non-Compliance |
78 |
Term - Onsite review/ Provider is no longer operational |
79 |
Term - Other |
80 |
Term - Provider Deceased |
81 |
Term - State exclusion/ debarment, etc. |
82 |
Term - Unknown |
83 |
Term - Voluntary Termination |
Provider
File Valid Values

Provider
File Valid Values
PROV-PROFIT-STATUS
01 |
501(C)(3) NON-PROFIT |
02 |
FOR-PROFIT, CLOSELY HELD |
03 |
FOR-PROFIT, PUBLICLY TRADED |
04 |
OTHER |
88 |
N/A – The individual only practices as part of a group |
99 |
Unknown |

Provider
File Valid Values
RECORD-ID
PRV00001 |
FILE-HEADER-RECORD-PROVIDER |
PRV00002 |
PROV-ATTRIBUTES-MAIN |
PRV00003 |
PROV-LOCATION-AND-CONTACT-INFO |
PRV00004 |
PROV-LICENSING-INFO |
PRV00005 |
PROV-IDENTIFIERS |
PRV00006 |
PROV-TAXONOMY-CLASSIFICATION |
PRV00007 |
PROV-MEDICAID-ENROLLMENT |
PRV00008 |
PROV-AFFILIATED-GROUPS |
PRV00009 |
PROV-AFFILIATED-PROGRAMS |
PRV00010 |
PROV-BED-TYPE-INFO |

Provider
File Valid Values
SEX
F |
Female |
M |
Male |
U |
Unknown |

Provider
File Valid Values
STATE-PLAN-ENROLLMENT
1 |
Medicaid |
2 |
CHIP |
3 |
Both Medicaid and CHIP |
4 |
Not state plan affiliated |

Provider
File Valid Values
SUBMISSION-TRANSACTION-TYPE
C |
Create File—a file that contains a complete set of transactions/changes processed since the last Create file submission. States may submit only one valid Create file per reporting period and data file type. |
R |
Replacement File—a Replacement submission is a replacement of the month’s data. It will completely replace the immediate prior submission. If a later replacement entry is received, it will overwrite the previous replacement, as well as a prior Create or Update submission for the same data type and reporting period. |
U |
Update File—a file that contains T-MSIS record segments created in response to business rule rejects. Note: The records in an Update file are not generated as a result of a change processed in the state’s Medicaid or Medicaid-related systems during the current reporting month. These Update file record segments may be unchanged from the ones submitted previously for various reasons (for example, the state may be unable to process a change record in their Medicaid / Medicaid-related systems to correct the issue because the state is simply passing through to T-MSIS data that originated outside of the state’s systems).[1] Conversely, the records may be different from those previously submitted, but the change is the result of a fix whose root cause problem was an issue in the T-MSIS file-creation or replacement process at CMS. Regardless, the record was not generated from a change that occurred in the state’s source data. |

Provider
File Valid Values
SUBMITTING-STATE
|

Provider
File Valid Values
TEACHING-IND
0 |
No |
1 |
Yes |
Eligible File Valid Values

Eligible
File Valid Values
1115A-DEMONSTRATION-IND
0 |
Not an 1115(A) participant |
1 |
1115(A) participant |

Eligible
File Valid Values
ADDR-TYPE
01 |
Primary home address and contact information, used for the eligibility determination process |
02 |
Primary work address and contact information |
03 |
Secondary residence and contact information |
04 |
Secondary work address and contact information |
05 |
Other category of address and contact information |
06 |
Eligible person’s official mailing address |

Eligible
File Valid Values
CERTIFIED-AMERICAN-INDIAN/ALASKAN-NATIVE-INDICATOR
0 |
Not applicable |
1 |
No, Individual does not have CDIB |
2 |
Yes, Individual does have CDIB |
9 |
Applicable but unknown |

Eligible
File Valid Values
CHIP-CODE
0 |
Individual was not Medicaid eligible and not eligible for separate CHIP for the month |
1 |
Individual was Medicaid eligible, but was not included in either Medicaid-Expansion CHIP or a separate title XXI CHIP) program for the month |
2 |
Individual was included in the Medicaid-Expansion CHIP program and subject to enhanced Federal matching for the month |
3 |
Individual was not Medicaid-Expansion CHIP eligible, but was included in a separate title XXI CHIP program for the month. |
4 |
Individual was both Medicaid-Eligible and Separate CHIP eligible during the same month |
9 |
CHIP status unknown |

Eligible
File Valid Values
CITIZENSHIP-IND
0 |
No |
1 |
Yes |
9 |
Unknown |

Eligible
File Valid Values
CITIZENSHIP-VERIFICATION-FLAG
0 |
No |
1 |
Yes |
9 |
Unknown |

Eligible
File Valid Values
CONCEPTION-TO-BIRTH-IND
0 |
No |
1 |
Yes |
9 |
Unknown |

Eligible
File Valid Values
DISABILITY-TYPE-CODE
01 |
Individual is deaf or has serious difficulty hearing. |
02 |
Individual is blind or has serious difficulty seeing, even when wearing glasses. |
03 |
Individual has serious difficulty concentrating, remembering, or making decisions because of a physical, mental, or emotional condition. (Applicable only to people who are 5 years old or older.) |
|
|
04 |
Individual has serious difficulty walking or climbing stairs. (Applicable only to people who are 5 years old or older.) |
05 |
Individual has difficulty dressing or bathing. (Applicable only to people who are 5 years old or older.) |
06 |
Individual has difficulty doing errands alone such as visiting a doctor's office or shopping because of a physical, mental, or emotional condition. (Applicable only to people who are 15 years old or older.) |
07 |
Other |
08 |
None |
99 |
Unknown |

Eligible
File Valid Values
DUAL-ELIGIBLE-CODE
00 |
Eligible is not a Medicare beneficiary |
01 |
Eligible is entitled to Medicare- QMB only |
02 |
Eligible is entitled to Medicare- QMB AND Medicaid coverage |
03 |
Eligible is entitled to Medicare- SLMB only |
04 |
Eligible is entitled to Medicare- SLMB AND Medicaid coverage |
05 |
Eligible is entitled to Medicare- QDWI |
06 |
Eligible is entitled to Medicare- Qualifying individuals |
08 |
Eligible is entitled to Medicare- Other Dual Eligibles (Non QMB, SLMB, QDWI or QI) |
09 |
Eligible is entitled to Medicare – Other (This code is to be used only with specific CMS approval.) |
10 |
Separate CHIP Eligible is entitled to Medicare |
99 |
Eligible's Medicare status is unknown. |

Eligible
File Valid Values
ELIGIBILITY-CHANGE-REASON
01 |
Excess income |
02 |
Excess assets |
03 |
Income reduced |
04 |
Aged out of program |
05 |
No longer in the foster care system |
06 |
Death |
07 |
No longer disabled |
08 |
No longer institutionalized |
09 |
No longer in need of long-term care services resides |
10 |
Obtained employer sponsored insurance (ESI) |
11 |
Gained access to public employees health plan |
12 |
Obtained other coverage (not ESI or public employees health plan) |
13 |
Failure to respond |
14 |
Failure to pay premium or enrollment fees |
15 |
Moved to a different state |
16 |
Voluntary request for termination |
17 |
Lack of verifications |
18 |
Fraud |
19 |
Suspension due to incarceration |
20 |
Residence in an Institution for Mental Disease (IMD) |
21 |
Suspension/Termination with reason unknown |
22 |
Other |

Eligible
File Valid Values
ELIGIBILITY-GROUP
See Appendix F: Eligibility Group Table for listing of valid values. |

Eligible
File Valid Values
ELIGIBLE-COUNTY-CODE
http://www.census.gov/geo/reference/codes/cou.html
|

Eligible
File Valid Values
ELIGIBLE-STATE
|

Eligible
File Valid Values
ENROLLMENT-TYPE
1 |
Medicaid |
2 |
CHIP |
9 |
Unknown |

Eligible
File Valid Values
ETHNICITY-CODE
Code |
Description |
0 |
Not of Hispanic or, Latino/a, or Spanish origin |
1 |
Mexican, Mexican American, Chicano/a |
2 |
Puerto Rican |
3 |
Cuban |
4 |
Another Hispanic, Latino, or Spanish origin |
5 |
Hispanic or Latino Unknown |
6 |
Ethnicity Unspecified |
9 |
Ethnicity Unknown |

Eligible
File Valid Values
FILE-ENCODING-SPECIFICATION
Code |
Description |
FIX |
The file follows a fixed length format. |
PSV |
The file follows a pipe-delimited format |

Eligible
File Valid Values
FILE-NAME
Code |
Description |
ELIGIBLE |
Eligible File |

Eligible
File Valid Values
FILE-STATUS-INDICATOR
Code |
Description |
P |
Production file |
T |
Test file |

Eligible
File Valid Values
HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-CODE
Code |
Description |
001 |
Aged |
002 |
Physical Disabilities |
003 |
Intellectual Disabilities |
004 |
Autism Spectrum Disorder |
005 |
Developmental Disabilities |
006 |
Mental Illness and/or Serious Emotional Disturbance |
007 |
Brain Injury |
008 |
HIV/AIDs |
009 |
Technology Dependent or Medically Fragile |
010 |
Disabled (other) |

Eligible
File Valid Values
HEALTH-HOME-CHRONIC-CONDITION
Code |
Description |
A |
Mental health |
B |
Substance abuse |
C |
Asthma |
D |
Diabetes |
E |
Heart disease |
F |
Overweight (BMI of >25) |
G |
HIV/AIDS |
H |
Other |

Eligible
File Valid Values
HOUSEHOLD-SIZE
Code |
Description |
01 |
1 person |
02 |
2 people |
03 |
3 people |
04 |
4 people |
05 |
5 people |
06 |
6 people |
07 |
7 people |
08 |
8 or more people |
99 |
Unknown number of people |

Eligible
File Valid Values
IMMIGRATION-STATUS
1 |
Qualified non-citizen |
2 |
Lawfully present under CHIPRA 214 |
3 |
Eligible only for payment for emergency services |
8 |
Not Applicable (U.S. citizen) |
9 |
Unknown |

Eligible
File Valid Values
IMMIGRATION-VERIFICATION-FLAG
0 |
No |
1 |
Yes |
9 |
Unknown |

Eligible
File Valid Values
INCOME-CODE
01 |
Individual’s State-defined family income is from 0 to 100% of the FPL |
02 |
Individual’s State-defined family income is from 101 to 133% of the FPL |
03 |
Individual’s State-defined family income is from 134 to 150% of the FPL |
04 |
Individual’s State-defined family income is from 151 to 200% of the FPL |
05 |
Individual’s State-defined family income is from 201 to 255% of the FPL |
06 |
Individual’s State-defined family income is from 256 to 300% of the FPL |
07 |
Individual’s State-defined family income is from 301 to 400% of the FPL |
08 |
Individual’s State-defined family income is over 400% of the FPL |
88 |
Not Applicable |
99 |
Unknown |

Eligible
File Valid Values
LEVEL-OF-CARE-STATUS
001 |
Hospital as defined in 42 CFR §440.10 |
002 |
Inpatient psychiatric facility for individuals under age 21 as provided in 42 CFR § 440.160 |
003 |
Nursing Facility |
004 |
ICF/IDD |
005 |
Other Type of Facility |
888 |
Not Applicable (Not in LTSS program) |
999 |
Unknown |

Eligible
File Valid Values
LOCKIN-PROV-TYPE
For a list of provider type codes, see the PROV-CLASSIFICATION-CODE in PROVIDER-FILE where PROV-CLASSIFICATION-TYPE = 3 (Provider Type Code). |

Eligible
File Valid Values
LTSS-LEVEL-CARE
1 |
Skilled Care |
2 |
Intermediate Care |
3 |
Custodial Care |
9 |
Unknown |

Eligible
File Valid Values
MAINTENANCE-ASSISTANCE-STATUS
0 |
Individual was not eligible for Medicaid this month |
1 |
Receiving Cash or eligible under section 1931 of the Act |
2 |
Medically Needy |
3 |
Poverty Related |
4 |
Other |
5 |
1115 - Demonstration expansion eligible |
9 |
Status is unknown |

Eligible
File Valid Values
MANAGED-CARE-PLAN-TYPE
00 |
Not applicable, individual is eligible for Medicaid or CHIP but not enrolled in a managed care plan |
01 |
Individual is enrolled in a Comprehensive MCO |
02 |
Individual is enrolled in a Traditional PCCM Provider arrangement |
03 |
Individual is enrolled in an Enhanced PCCM Provider arrangement |
04 |
Individual is enrolled in a HIO |
05 |
Individual is enrolled in a Medical-only PIHP (risk or non-risk/non-comprehensive/with inpatient hospital or institutional services) |
06 |
Individual is enrolled in a Medical-only PAHP (risk or non-risk/non-comprehensive/no inpatient hospital or institutional services) |
07 |
Individual is enrolled a Long Term Care (LTC) PIHP |
08 |
Individual is enrolled a Mental Health (MH) PIHP |
09 |
Individual is enrolled in a Mental Health (MH) PAHP |
10 |
Individual is enrolled in a Substance Use Disorders (SUD) PIHP |
11 |
Individual is enrolled in a Substance Use Disorders (SUD) PAHP |
12 |
Individual is enrolled in a Mental Health (MH) and Substance Use Disorders (SUD) PIHP |
13 |
Individual is enrolled in a Mental Health (MH) and Substance Use Disorders (SUD) PAHP |
14 |
Individual is enrolled in a Dental PAHP |
15 |
Individual is enrolled in a Transportation PAHP |
16 |
Individual is enrolled in a Disease Management PAHP |
17 |
Individual is enrolled in Program for All-Inclusive Care for the Elderly (PACE) |
18 |
Pharmacy PAHP |
60 |
Accountable Care Organization |
70 |
Health/Medical Home |
80 |
Integrated Care For Dual Eligibles |
99 |
Individual’s managed care plan status is unknown |

Eligible
File Valid Values
MARITAL-STATUS
01 |
Legally Married (to opposite sex), spouse present |
02 |
Legally Married (to opposite sex), spouse absent |
03 |
Legally Married (to same sex), spouse present |
04 |
Legally Married (to same sex), spouse absent |
05 |
Partnered or in Civil Union (to opposite sex), spouse present |
06 |
Partnered or in Civil Union (to opposite sex), spouse absent |
07 |
Partnered or in Civil Union (to same sex), spouse present |
08 |
Partnered or in Civil Union (to same sex), spouse absent |
09 |
Legally separated (and not married or partnered) |
10 |
Divorced (and not currently married or partnered) |
11 |
Separated (and not currently married or partnered) |
12 |
Widower/Widow (and not currently married or partnered) |
13 |
Never married/partnered |
14 |
Other |
99 |
Unknown |

Eligible
File Valid Values
MEDICAID-BASIS-OF-ELIGIBILITY
00 |
Individual was not eligible for Medicaid at any time during the month |
01 |
Aged Individual |
02 |
Blind/Disabled Individual |
03 |
Not used |
04 |
Child (not Child of Unemployed Adult, not Foster Care Child) |
05 |
Adult (not based on unemployed status) |
06 |
Child of Unemployed Adult (optional) |
07 |
Unemployed Adult (optional) |
08 |
Foster Care Child |
10 |
Refugee Medical Assistance (45 CFR Sub-part G) |
11 |
Individual covered under the Breast and Cervical Cancer Prevention and Treatment Act of 2000 |
99 |
Eligibility status unknown |

Eligible
File Valid Values
MFP-LIVES-WITH-FAMILY
0 |
No |
1 |
Yes |
2 |
Non Participation |
9 |
Unknown |

Eligible
File Valid Values
MFP-QUALIFIED-INSTITUTION
00 |
Default- Non Participation |
01 |
Nursing Facility |
02 |
ICF/IID (Intermediate Care Facilities for individuals with Intellectual Disabilities) |
03 |
IMD (Institution for Mental Diseases) |
04 |
Hospital |
05 |
Other |
99 |
Unknown |

Eligible
File Valid Values
MFP-QUALIFIED-RESIDENCE
00 |
Default - Non Participation |
01 |
Home owned by participant |
02 |
Home owned by family member |
03 |
Apartment leased by participant, not assisted living |
04 |
Apartment leased by participant, assisted living |
05 |
Group home of no more than 4 people |
99 |
Unknown |

Eligible
File Valid Values
MFP-REASON-PARTICIPATION-ENDED
00 |
Default – No Participation |
01 |
Completed 365 days of participation |
02 |
Suspended eligibility |
03 |
Re-institutionalized |
04 |
Died |
05 |
Moved |
06 |
No longer needed services |
07 |
Other |
99 |
Unknown |

Eligible
File Valid Values
MFP-REINSTITUTIONALIZED-REASON
00 |
Default- Non Participation |
01 |
Acute care hospitalization followed by long term rehabilitation |
02 |
Deterioration in cognitive functioning |
03 |
Deterioration in health |
04 |
Deterioration in mental health |
05 |
Loss of housing |
06 |
Loss of personal care giver |
07 |
By request of participant or guardian |
08 |
Lack of sufficient community services |
99 |
Unknown |

Eligible
File Valid Values
NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE
1 |
Controlling Health Plan (CHP) ID – the national health plan identifier of a health plan that either controls its own business activities, actions, or policies, or is controlled by an entity that is not a health plan and exercises sufficient control over the subhealth plan(s) under it so as to direct its own business activities, actions, or policies, as well as those of any subhealth plans under it. |
2 |
Subhealth Plan (SHP) ID – the national health plan identifier of a health plan whose business activities, actions, or policies are directed by a controlling health plan. All subhealth HPIDs should be reported. |
3 |
Other Entity Identifier (OEID) – a national identifier for entities that are not health plans, health care providers, or individuals (as defined in 45 CFR 160.103), but that need to be identified in standard transactions (including, for example, third party administrators, transaction vendors, clearinghouses, and other payers). Other entities are not required to obtain an OEID, but they could obtain and use one if they need to be identified in covered transactions. |

Eligible
File Valid Values
PREGNANCY-IND
0 |
No |
1 |
Yes |
9 |
Unknown |

Eligible
File Valid Values
PRIMARY-LANGUAGE-CODE
See language codes in Appendix G: ISO 639 Language Codes Reference for a list of all valid language codes |

Eligible
File Valid Values
PRIMARY-LANGUAGE-ENGL-PROF-CODE
0 |
Very Well |
1 |
Well |
2 |
Not well |
3 |
No spoken proficiency |
9 |
Unknown |

Eligible
File Valid Values
RACE
001 |
White |
002 |
Black or African American |
003 |
American Indian or Alaskan Native |
004 |
Asian Indian |
005 |
Chinese |
006 |
Filipino |
007 |
Japanese |
008 |
Korean |
009 |
Vietnamese |
010 |
Other Asian |
011 |
Asian Unknown |
012 |
Native Hawaiian |
013 |
Guamanian or Chamorro |
014 |
Samoan |
015 |
Other Pacific Islander |
016 |
Native Hawaiian or Other Pacific Islander Unknown |
017 |
Unspecified |
999 |
Unknown |

Eligible
File Valid Values
RECORD-ID
ELG00001 |
FILE-HEADER-RECORD-ELIGIBILITY |
ELG00002 |
PRIMARY-DEMOGRAPHICS-ELIGIBILITY |
ELG00003 |
VARIABLE-DEMOGRAPHICS-ELIGIBILITY |
ELG00004 |
ELIGIBILE-CONTACT-INFORMATION |
ELG00005 |
ELIGIBILITY-DETERMINANTS |
ELG00006 |
HEALTH-HOME-SPA-PARTICIPATION-INFORMATION |
ELG00007 |
HEALTH-HOME-SPA-PROVIDERS |
ELG00008 |
HEALTH-HOME-CHRONIC-CONDITIONS |
ELG00009 |
LOCK-IN-INFORMATION |
ELG00010 |
MFP-INFORMATION |
ELG00011 |
STATE-PLAN-OPTION-PARTICIPATION |
ELG00012 |
WAIVER-PARTICIPATION |
ELG00013 |
LTSS-PARTICIPATION |
ELG00014 |
LTSS-PARTICIPATION |
ELG00015 |
ETHNICITY-INFORMATION |
ELG00016 |
RACE-INFORMATION |
ELG00017 |
DISABILITY-INFORMATION |
ELG00018 |
1115A-DEMONSTRATION-INFORMATION |
ELG00020 |
HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME |
ELG00021 |
ENROLLMENT-TIME-SPAN |

Eligible
File Valid Values
RESTRICTED-BENEFITS-CODE
0 |
Individual is not eligible for Medicaid or CHIP during the month. |
1 |
Individual is eligible for Medicaid or CHIP and entitled to the full scope of Medicaid or CHIP benefits. |
2 |
Individual is eligible for Medicaid or Medicaid-Expansion CHIP, but only entitled to restricted benefits based on alien status. |
3 |
Individual is eligible for Medicaid but only entitled to restricted benefits based on Medicare dual-eligibility status (e.g., QMB, SLMB, QDWI, QI). |
4 |
Individual is eligible for Medicaid or CHIP but only entitled to restricted benefits for pregnancy-related services. |
5 |
Individual is eligible for Medicaid or Medicaid-Expansion CHIP but, for reasons other than alien, dual-eligibility or pregnancy-related status, is only entitled to restricted benefits (e.g., restricted benefits based upon substance abuse, medically needy or other criteria). |
6 |
Individual is eligible for Medicaid or Medicaid-Expansion CHIP but only entitled to restricted benefits for family planning services. |
7 |
Individual is eligible for Medicaid and entitled to Medicaid benefits under an alternative package of benchmark-equivalent coverage, as enacted by the Deficit Reduction Act of 2005. |
D |
Individual is eligible for Medicaid and entitled to benefits under a “Money Follows the Person” (MFP) rebalancing demonstration, as enacted by the Deficit Reduction Act of 2005, to allow States to develop community based long term care opportunities. |
9 |
Individual's benefit restrictions are unknown. |
A |
Individual is eligible for Medicaid and entitled to benefits under the Psychiatric Residential Treatment Facilities Demonstration Grant Program (PRTF), as enacted by the Deficit Reduction Act of 2005. PRTF grants assist States to help provide community alternatives to psychiatric resident treatment facilities for children. |
B |
Individual is eligible for Medicaid and entitled to Medicaid benefits using a Health Opportunity Account (HOA) |
C |
Individual is eligible for S-separate CHIP dental coverage (supplemental dental wraparound benefit to employer-sponsored insurance) |

Eligible
File Valid Values
SEX
F |
Female |
M |
Male |
U |
Unknown |

Eligible
File Valid Values
SSDI-IND
0 |
No |
1 |
Yes |
9 |
Unknown |

Eligible
File Valid Values
SSI-STATE-SUPPLEMENT-STATUS-CODE
000 |
Not Applicable |
001 |
Mandatory |
002 |
Optional |
999 |
Unknown |
SSI-STATUS
Eligible
File Valid Values |
Not Applicable |
001 |
SSI |
002 |
SSI Eligible Spouse |
003 |
SSI Pending a Final Determination of Disposal of Resources Exceeding SSI Dollar Limits |
999 |
Unknown |

Eligible
File Valid Values
SSN-INDICATOR
0 |
State does not use SSN as MSIS-IDENTIFICATION-NUMBER |
1 |
State uses SSN as MSIS-IDENTIFICATION-NUMBER |

Eligible
File Valid Values
SSN-VERIFICATION-FLAG
0 |
SSN not verified |
1 |
SSN successfully verified by SSA |
2 |
SSN is pending SSA verification |
9 |
Unknown |

Eligible
File Valid Values
STATE-PLAN-OPTION-TYPE
00 |
Not Applicable |
01 |
Community First Choice |
02 |
1915(i) |
03 |
1915(j) |
04 |
1932(a) |
05 |
1915(a) |
06 |
1937 (Alternative Benefit Plans) |
99 |
Unknown |

Eligible
File Valid Values
SUBMISSION-TRANSACTION-TYPE
C |
Create File—a file that contains a complete set of transactions/changes processed since the last Create file submission. States may submit only one valid Create file per reporting period and data file type. |
R |
Replacement File—a Replacement submission is a replacement of the month’s data. It will completely replace the immediate prior submission. If a later replacement entry is received, it will overwrite the previous replacement, as well as a prior Create or Update submission for the same data type and reporting period. |
U |
Update File—a file that contains T-MSIS record segments created in response to business rule rejects. Note: The records in an Update file are not generated as a result of a change processed in the state’s Medicaid or Medicaid-related systems during the current reporting month. These Update file record segments may be unchanged from the ones submitted previously for various reasons (for example, the state may be unable to process a change record in their Medicaid / Medicaid-related systems to correct the issue because the state is simply passing through to T-MSIS data that originated outside of the state’s systems).[1] Conversely, the records may be different from those previously submitted, but the change is the result of a fix whose root cause problem was an issue in the T-MSIS file-creation or replacement process at CMS. Regardless, the record was not generated from a change that occurred in the state’s source data. |

Eligible
File Valid Values
SUBMITTING-STATE
|

Eligible
File Valid Values
TANF-CASH-CODE
0 |
Individual was not eligible for Medicaid. |
1 |
Individual did not receive TANF benefits |
2 |
Individual did receive TANF benefits (States should only use this value if they can accurately separate eligible receiving TANF benefits from other 1931 eligible reported into MAS 1) |
9 |
Individual’s TANF status is unknown |

Eligible
File Valid Values
VETERAN-IND
0 |
No |
1 |
Yes |
9 |
Unknown |

Eligible
File Valid Values
WAIVER-TYPE
00 |
Not Eligible- The individual was not eligible for Medicaid or CHIP |
01 |
1115 Other demonstration – Such waivers may also be called a research, experimental, demonstration or pilot waiver, or refer to consumer-directed care or expanded eligibility. It may cover the entire state or just a geographic entity or specific population. |
02 |
1915(b)(1) – These waivers permit freedom-of-choice or mandatory managed care with some voluntary managed care. |
03 |
1915(b)(2) – These waivers allow states to use enrollment brokers. |
04 |
1915(b)(3) – These waivers allow states to use savings to provide additional services that are not in the State Plan. |
05 |
1915(b)(4) – These waivers allow fee for service selective contracting. |
06 |
1915(c) – Aged and Disabled |
07 |
1915(c) – Aged |
08 |
1915(c) – Physical Disabilities |
09 |
1915(c) – Intellectual Disabilities |
10 |
1915(c) – Intellectual and Developmental Disabilities |
11 |
1915(c) – Brain Injury |
12 |
1915(c) – HIV/AIDS |
13 |
1915(c) – Technology Dependent or Medically Fragile |
14 |
1915(c) –Disabled (other) |
15 |
1915(c) - Enrolled in 1915(c) waiver for unspecified or unknown populations |
16 |
1915(c) - Autism/Autism spectrum disorder |
17 |
1915(c) – Developmental Disabilities |
18 |
1915(c) – Mental Illness - Age 18 or Older |
19 |
1915(c) – Mental Illness - Under Age 18 |
20 |
Concurrent 1915(b)(c) – A concurrent HCBS/1915(c) waiver is one where the approved waiver services are delivered through a managed care authority – e.g., 1115(a), 1915(a), 1915(b), or 1932(a) |
21 |
1115 HIFA Waiver – The associated Waiver-ID is for a HIFA (Health Insurance and Flexibility and Accountability) waiver. May also be called demonstration waiver or refer to the eligibility expansion. |
22 |
1115 Pharmacy Plus Waiver – The associated Waiver-ID is for Pharmacy waiver coverage. Includes waivers under 1115 demonstration authority which are primarily intended to increase coverage or expand eligibility for pharmacy benefits. The associated Waiver-ID is for another type of waiver. |
23 |
1115 Disaster-Related Waiver – The associated Waiver-ID is for a disaster-related waiver that allows for coverage related to a hurricane or other disaster. |
24 |
1115 Family Planning-ONLY waiver – The associated Waiver-ID-Number is for a Family Planning-ONLY waiver. In these waivers, the beneficiary’s Medicaid-covered benefits are restricted to Family Planning Services. |
88 |
Not Applicable - The individual is eligible for Medicaid or CHIP, but is NOT enrolled in a waiver. |
99 |
Unknown – The associated Waiver-ID is for an unknown type of waiver. |
Third-party Liability File Valid Values

Third-party
Liability File Valid Values
COVERAGE-TYPE
01 |
Drug |
02 |
Professional (Physician) Visit - Office |
03 |
Dental Care |
04 |
Inpatient Hospital |
05 |
Outpatient Hospital |
06 |
Nursing Home |
07 |
Vision |
08 |
Durable Med Equip (rent) |
09 |
Durable Med Equip (purchase) |
10 |
Home Health |
11 |
Mental health—outpatient |
12 |
Mental health –inpatient |
13 |
Psychiatric care- outpatient |
14 |
Psychiatric care- inpatient |
15 |
Rehabilitation |
16 |
Cancer |
17 |
Emergency Services |
18 |
Chiropractic |
19 |
Surgical |
20 |
Diagnostic Medical, including X-ray and Lab Services |
21 |
PT/OT/ST |
22 |
Hospice |
23 |
Transportation |
98 |
Other |
99 |
Unknown |

Third-party
Liability File Valid Values
FILE-ENCODING-SPECIFICATION
FLF |
The file follows a fixed length format. |
PSV |
The file follows a pipe-delimited format. |

Third-party
Liability File Valid Values
FILE-NAME
TPL-FILE |
Third Party Liability File |

Third-party
Liability File Valid Values
FILE-STATUS-INDICATOR
P |
Production file |
T |
Test |

Third-party
Liability File Valid Values
INSURANCE-CARRIER-STATE

Third-party
Liability File Valid Values
INSURANCE-PLAN-TYPE
01 |
Medical or comprehensive health insurance plan (e.g. HMO) |
02 |
Dental health insurance plan |
03 |
Vision health insurance plan |
04 |
Prenatal/delivery health insurance plan |
05 |
Long term care health insurance plan (Long Term PIHP) |
06 |
Transportation health insurance plan (Transportation PAHP) |
07 |
A managed care plan |
08 |
Disease management health insurance plan (Disease Management PAHP) |
09 |
PAHP (Medical only) |
10 |
Comprehensive health insurance and Long Term Care (hybrid) |
11 |
Other health insurance plan |
12 |
Veterans Administration health benefits |
13 |
Indian Health Service Program health benefits |
14 |
TRICARE health benefits |
15 |
Eligible enrolled in private LTC insurance |
16 |
Fee-for-Service insurance |
99 |
Health insurance plan type is unknown |

Third-party
Liability File Valid Values
NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE
1 |
Controlling Health Plan (CHP) ID – the national health plan identifier of a health plan that either controls its own business activities, actions, or policies, or is controlled by an entity that is not a health plan and exercises sufficient control over the subhealth plan(s) under it so as to direct its own business activities, actions, or policies, as well as those of any subhealth plans under it. |
2 |
Subhealth Plan (SHP) ID – the national health plan identifier of a health plan whose business activities, actions, or policies are directed by a controlling health plan. All subhealth HPIDs should be reported. |
3 |
Other Entity Identifier (OEID) – a national identifier for entities that are not health plans, health care providers, or individuals (as defined in 45 CFR 160.103), but that need to be identified in standard transactions (including, for example, third party administrators, transaction vendors, clearinghouses, and other payers). Other entities are not required to obtain an OEID, but they could obtain and use one if they need to be identified in covered transactions. |

Third-party
Liability File Valid Values
POLICY-OWNER-CODE
01 |
Self |
02 |
Spouse |
03 |
Custodial Parent |
04 |
Noncustodial Parent (Child Support Enforcement in effect) |
05 |
Noncustodial Parent without child support enforcement in effect |
06 |
Grandparent |
07 |
Guardian |
08 |
Domestic Partner |
09 |
Other |
99 |
Unknown |

Third-party
Liability File Valid Values
RECORD-ID
TPL00001 |
FILE-HEADER-RECORD-TPL |
TPL00002 |
TPL-MEDICAID-ELIGIBLE-PERSON-MAIN |
TPL00003 |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO |
TPL00004 |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES |
TPL00005 |
TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION |
TPL00006 |
TPL-ENTITY-CONTACT-INFORMATION |

Third-party
Liability File Valid Values
SSN-INDICATOR
0 |
State does not use SSN as MSIS-IDENTIFICATION-NUMBER |
1 |
State uses SSN as MSIS-IDENTIFICATION-NUMBER |

Third-party
Liability File Valid Values
SUBMISSION-TRANSACTION-TYPE
C |
Create File—a file that contains a complete set of transactions/changes processed since the last Create file submission. States may submit only one valid Create file per reporting period and data file type. |
R |
Replacement File—a Replacement submission is a replacement of the month’s data. It will completely replace the immediate prior submission. If a later replacement entry is received, it will overwrite the previous replacement, as well as a prior Create or Update submission for the same data type and reporting period. |
U |
Update File—a file that contains T-MSIS record segments created in response to business rule rejects. Note: The records in an Update file are not generated as a result of a change processed in the state’s Medicaid or Medicaid-related systems during the current reporting month. These Update file record segments may be unchanged from the ones submitted previously for various reasons (for example, the state may be unable to process a change record in their Medicaid / Medicaid-related systems to correct the issue because the state is simply passing through to T-MSIS data that originated outside of the state’s systems).[1] Conversely, the records may be different from those previously submitted, but the change is the result of a fix whose root cause problem was an issue in the T-MSIS file-creation or replacement process at CMS. Regardless, the record was not generated from a change that occurred in the state’s source data. |

Third-party
Liability File Valid Values
SUBMITTING-STATE

Third-party
Liability File Valid Values
TPL-ENTITY-ADDR-TYPE
06 |
TPL-Entity Corporate Location |
07 |
TPL-Entity Mailing |
08 |
TPL-Entity Satellite Location |
09 |
TPL-Entity Billing |
10 |
TPL-Entity Correspondence |
11 |
TPL-Other |

Third-party
Liability File Valid Values
TPL-HEALTH-INSURANCE-COVERAGE-IND
0 |
Eligible individual has no TPL insurance coverage. |
1 |
Eligible individual does have TPL insurance coverage. |

Third-party
Liability File Valid Values
TPL-OTHER-COVERAGE-IND
0 |
Eligible individual has no other TPL funding available. |
1 |
Eligible individual does have other TPL funding available. |

Third-party
Liability File Valid Values
TYPE-OF-OTHER-THIRD-PARTY-LIABILITY
1 |
Tort/Casualty Claim |
2 |
Medical Malpractice |
3 |
Estate (an estate, annuity or designated trust) |
4 |
Liens |
5 |
Worker’s Compensation |
6 |
Payments from an individual or group who has either voluntarily or been assigned legal responsibility for the health care of one or more Medicaid recipients; fraternal groups; unions |
7 |
Other – unidentified |
9 |
Unknown |
Claims Files Valid Values
All valid values for CLAIM-IP, CLAIM-LT, CLAIM-OT, and CLAIM-RX files are included

Claims
Files Valid Values
1115A-DEMONSTRATION-IND
0 |
No |
1 |
Yes |

Claims
Files Valid Values
ADJUSTMENT-IND
0 |
Original Claim / Encounter |
1 |
Void of a prior submission |
2 |
Re-submittal |
3 |
Credit Adjustment (negative supplemental) |
4 |
Debit Adjustment (positive supplemental) |
5 |
Credit Gross Adjustment |
6 |
Debit Gross Adjustment |
9 |
Unknown |

Claims
Files Valid Values
ADJUSTMENT-REASON-CODE
http://www.wpc-edi.com/reference/codelists/healthcare/claim-adjustment-reason-codes/ |

Claims
Files Valid Values
ADMISSION-HOUR
00 |
0:00-0:59 |
01 |
1:00-1:59 |
02 |
2:00-2:59 |
03 |
3:00-3:59 |
04 |
4:00-4:59 |
05 |
5:00-5:59 |
06 |
6:00-6:59 |
07 |
7:00-7:59 |
08 |
8:00-8:59 |
09 |
9:00-9:59 |
10 |
10:00-10:59 |
11 |
11:00-11:59 |
12 |
12:00-12:59 |
13 |
13:00-13:59 |
14 |
14:00-14:59 |
15 |
15:00-15:59 |
16 |
16:00-16:59 |
17 |
17:00-17:59 |
18 |
18:00-18:59 |
19 |
19:00-19:59 |
20 |
20:00-20:59 |
21 |
21:00-21:59 |
22 |
22:00-22:59 |
23 |
23:00-23:59 |

Claims
Files Valid Values
ADMISSION-TYPE
1 |
EMERGENCY |
The patient requires immediate medical intervention as a result of severe, life threatening or potentially disabling conditions. Generally, the patient is admitted through the emergency room. |
2 |
URGENT |
The patient requires immediate attention for the care and treatment of a physical or mental disorder. Generally, the patient is admitted to the first available and suitable accommodation. |
3 |
ELECTIVE |
The patient’s condition permits adequate time to schedule the availability of a suitable accommodation. |
4 |
NEWBORN |
The patient is a newborn delivered either inside the admitting hospital (UB04 FL 15 value “5” [A baby born inside the admitting hospital] or outside of the hospital (UB04 FL 15 value “6” [A baby born outside the admitting hospital]). |
5 |
TRAUMA |
The patient visits a trauma center( A trauma center means a facility licensed or designated by the State or local government authority authorized to do so, or as verified by the American College of surgeons and involving a trauma activation.) |
8 |
NOT AVALIABLE |
|
9 |
UNKNOWN |
|

Claims
Files Valid Values
ADMITTING-DIAGNOSIS-CODE
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html |
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html |

Claims
Files Valid Values
ADMITTING-DIAGNOSIS-CODE-FLAG
1 |
ICD-9 |
2 |
ICD-10 |
3 |
Other |
9 |
Unknown |

Claims
Files Valid Values
ADMITTING-PROV-NPI-NUM
ADMITTING-PROV-SPECIALTY
See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. |
Claims
Files Valid Values

Claims
Files Valid Values
ADMITTING-PROV-TAXONOMY

Claims
Files Valid Values
ADMITTING-PROV-TYPE
See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values. |
ALLOWED-CHARGE-SRC
Claims
Files Valid Values |
Priced using QMB Pricing |
2 |
Lab panel bundled |
4 |
Priced using RBRVS |
5 |
Anesthesia pricing |
7 |
APC priced |
|
|
A |
Manually priced |
B |
By report |
C |
Maximum fee |
D |
Percent of charges |
E |
Reimbursement Rate |
F |
Lower level screening fee |
G |
Billed Charges |
H |
Denied |
I |
Medicare Coins and deductible |
K |
Medicare allowed amount |
M |
Medicare prevailing |
P |
DRG |
R |
DRG w/cost outlier |
U |
DRG priced by proration |
V |
Mid-level priced |
Z |
ATP Bundled |
9 |
Unknown |
BENEFIT-TYPE
Code Value |
Claims
Files Valid Vales |
|
Mandatory Benefits for Categorically Needy (Mandatory and Options for Coverage) Individuals and Optional Benefits for Medically Needy Individuals |
001 |
Inpatient Hospital Services |
002 |
Outpatient Hospital Services |
003 |
Rural health clinic services |
004 |
FQHC services |
005 |
Other Laboratory and X-Ray Services |
006 |
Nursing Facility Services for 21 and over |
007 |
EPSDT |
008 |
Family Planning Services |
009 |
Mandatory tobacco cessation counseling for pregnant women under 1905(a)(4)(D) |
010 |
Physicians' Services |
011 |
Medical and Surgical Services Furnished by a Dentist |
012 |
Nurse-midwife services |
013 |
Certified pediatric or family nurse practitioners' services |
014 |
Free Standing Birth Center Services |
015 |
Home Health Services - Intermittent or part-time nursing services provided by a home health agency |
016 |
Home Health Services - Home Health Aide Services Provided by a Home Health Agency |
017 |
Home Health Services - Medical supplies, equipment, and appliances suitable for use in the home |
|
Optional Benefits for Categorically Needy (Mandatory and Options for Coverage) and Medically Needy Individuals |
018 |
Medical care and any type of remedial care recognized under State law - Podiatrists' Services |
019 |
Claims
Files Valid Values |
020 |
Medical care and any type of remedial care recognized under State law - Chiropractors' Services |
021 |
Medical care and any type of remedial care recognized under State law - Other Practitioners' Services within scope of practice as defined by State law |
022 |
Home Health Services - Physical therapy; occupational therapy; speech pathology; audiology provided by a home health agency |
023 |
Private Duty Nursing |
024 |
Clinic Services |
025 |
Dental Services |
026 |
Physical Therapy and Related Services - Physical Therapy |
027 |
Physical Therapy and Related Services - Occupational Therapy |
028 |
Physical Therapy and Related Services - Services for individuals with speech, hearing and language disorders |
029 |
Prescription drugs, dentures, and prosthetic devices; and eyeglasses - Prescribed Drugs |
030 |
Prescription drugs, dentures, and prosthetic devices; and eyeglasses - Dentures |
031 |
Prescription drugs, dentures, and prosthetic devices; and eyeglasses - Prosthetic Devices |
032 |
Prescription drugs, dentures, and prosthetic devices; and eyeglasses - Eyeglasses |
033 |
Other diagnostic, screening, preventive, and rehabilitative services - Diagnostic Services |
034 |
Other diagnostic, screening, preventive, and rehabilitative services - Screening Services |
035 |
Other diagnostic, screening, preventive, and rehabilitative services - Preventive Services |
036 |
Other diagnostic, screening, preventive, and rehabilitative services - Rehabilitative Services |
037 |
Services for individuals over age 65 in IMDs - Inpatient hospital services |
038 |
Services for individuals over age 65 in IMDs - Nursing facility services |
039 |
Intermediate Care Facility Services for individuals with intellectual disabilities or persons with related conditions |
040 |
Inpatient psychiatric facility services for under 21 |
041 |
Hospice Care |
042 |
Case Management Services and TB related services - Case management services as defined in the State Plan in accordance with section 1905(a)(19) or 1915(g) |
043 |
Case Management Services and TB related services - Special TB related services under section 1902(z)(2) |
044 |
Respiratory care services under 1902(e)9)(A) through (C) |
045 |
Personal care services |
046 |
Primary care case management services |
047 |
Special sickle-cell anemia-related services |
048 |
Any other medical care and any other type of remedial care recognized under State law, specified by the Secretary - Transportation |
049 |
Any other medical care and any other type of remedial care recognized under State law, specified by the Secretary - Services provided in religious non-medical health care facilities |
050 |
Any other medical care and any other type of remedial care recognized under State law, specified by the Secretary - Nursing facility services for patients under 21 |
051 |
Any other medical care and any other type of remedial care recognized under State law, specified by the Secretary - Emergency hospital services |
052 |
Any other medical care and any other type of remedial care recognized under State law, specified by the Secretary - Critical Access Hospitals |
053 |
Extended services for pregnant women - Additional Services for any other medical conditions that may complicate pregnancy |
054 |
Community First Choice |
055 |
Health Home Services |
|
Special Benefit Provisions |
056 |
Limited Pregnancy-Related Services for Pregnant Women with Income Above the Applicable Income Limit |
057 |
Ambulatory prenatal care for pregnant women furnished during a presumptive eligibility period |
058 |
Benefits for Families Receiving Transitional Medical Assistance |
059 |
Standards for Coverage of Transplant Services |
060 |
School-Based Services Payment Methodologies |
061 |
Indian Health Services and Tribal Health Facilities |
062 |
Methods and Standards to Assure High Quality Care |
|
Coordination of Medicaid with Medicare and Other Insurance |
063 |
Medicare Premium Payments |
064 |
Medicare Coinsurance and Deductibles |
065 |
Other Medical Insurance Premium Payments |
|
Special Benefit Programs |
066 |
Programs for Distribution of Pediatric Vaccines |
|
Home and Community-Based Services |
067 |
Laboratory and x-ray services |
068 |
Home Health Services - Home health aide services provided by a home health agency |
069 |
Private duty nursing services |
070 |
Physical Therapy and Related Services - Audiology services |
071 |
Extended services for pregnant women - Additional Pregnancy-related and postpartum services for a 60-day period after the pregnancy ends and any remaining days in the month in which the 60th day falls. |
072 |
Home and Community Care for Functionally Disabled Elderly individuals as defined and described in the State Plan |
073 |
Emergency services for certain legalized aliens and undocumented aliens |
074 |
Licensed or Otherwise State-Approved Free-Standing Birthing Center and other ambulatory services that are offered by a freestanding birth center |
075 |
Homemaker |
076 |
Home Health Aide |
077 |
Adult Day Health services |
078 |
Claims
Files Valid Values |
079 |
Habilitation: Residential Habilitation |
080 |
Habilitation: Supported Employment |
081 |
Habilitation: Education (non IDEA available) |
082 |
Habilitation: Day Habilitation |
083 |
Habilitation: Pre-Vocational |
084 |
Habilitation: Other Habilitative Services |
085 |
Respite |
086 |
Day Treatment (mental health service) |
087 |
Psychosocial rehabilitation |
088 |
Environmental Modifications (Home Accessibility Adaptations) |
089 |
Vehicle Modifications |
090 |
Non-Medical Transportation |
091 |
Special Medical Equipment (minor assistive Devices) |
092 |
Home Delivered meals |
093 |
Assistive Technology (i.e., communication devices) |
094 |
Personal Emergency Response (PERS) |
095 |
Nursing Services |
096 |
Community Transition Services |
097 |
Adult Foster Care |
098 |
Day Supports (non-habilitative) |
099 |
Supported Employment |
100 |
Supported Living Arrangements |
101 |
Supports for Consumer Direction (Supports Facilitation) |
102 |
Participant Directed Goods and Services |
103 |
Senior Companion (Adult Companion Services) |
104 |
Assisted Living |
|
Other |
105 |
Program for All-inclusive Care for the Elderly (PACE) Services |
106 |
Self-directed Personal Assistance Services under 1915(j) |

Claims
Files Valid Values
BILLING-PROV-NPI-NUM

Claims
Files Valid Values
BILLING-PROV-SPECIALTY
See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values.

Claims
Files Valid Values
BILLING-PROV-TAXONOMY

Claims
Files Valid Values
BILLING-PROV-TYPE
See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values.

Claims
Files Valid Values
BILLING-UNIT
01 |
Per Day |
02 |
Per Hour |
03 |
Per Case |
04 |
Per Encounter |
05 |
Per Week |
06 |
Per Month |
07 |
Other Arrangements |
99 |
Unknown |

Claims
Files Valid Values
BORDER-STATE-IND
0 |
No |
1 |
Yes |

Claims
Files Valid Values
BRAND-GENERIC-IND
0 |
Non-Drug |
1 |
Generic |
2 |
Brand |
3 |
Multi-Source |
4 |
Single-Source |

Claims
Files Valid Values
CLAIM-DENIED-INDICATOR
0 |
Denied: The payment of claim in its entirety was denied by the state. |
1 |
Not Denied: The state paid some or all of the claim. |

Claims
Files Valid Values
CLAIM-LINE-STATUS
http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-codes/
|

Claims
Files Valid Values
CLAIM-PYMT-REM-CODE-1 to CLAIM-PYMT-REM-CODE-4
http://www.wpc-edi.com/reference/codelists/healthcare/remittance-advice-remark-codes) |

Claims
Files Valid Values
CLAIM-STATUS
http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-codes/ |

Claims
Files Valid Values
CLAIM-STATUS-CATEGORY
http://www.wpc-edi.com/reference/codelists/healthcare/claim-status-category-codes/ |

Claims
Files Valid Values
CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT
01 |
Federal funding under Title XIX |
02 |
Federal funding under Title XXI |
03 |
Federal funding under ACA |
04 |
Federal funding under other legislation |

Claims
Files Valid Values
COMPOUND-DOSAGE-FORM
01 |
Capsule |
02 |
Ointment |
03 |
Cream |
04 |
Suppository |
05 |
Powder |
06 |
Emulsion |
07 |
Liquid |
10 |
Tablet |
11 |
Solution |
12 |
Suspension |
13 |
Lotion |
14 |
Shampoo |
15 |
Elixir |
16 |
Syrup |
17 |
Lozenge |
18 |
Enema |

Claims
Files Valid Values
COMPOUND-DRUG-IND
0 |
Not Compound |
1 |
Compound |
9 |
Unknown |

Claims
Files Valid Values
COPAY-WAIVED-IND
0 |
Not Waived: The provider did not waive the beneficiary’s copayment, |
1 |
Waived: The provider waived the beneficiary’s copayment. |
8 |
Not Applicable: The benefit plan does not have a copay in this circumstance |

Claims
Files Valid Values
CROSSOVER-INDICATOR
0 |
Not Crossover Claim |
1 |
Crossover Claim |
9 |
Unknown |

Claims
Files Valid Values
DESTINATION-STATE
|

Claims
Files Valid Values
DIAGNOSIS-CODE-1 to DIAGNOSIS-CODE-12
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes.html |
http://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/ICD10.html |

Claims
Files Valid Values
DIAGNOSIS-CODE-FLAG-1 to DIAGNOSIS-CODE-FLAG-12
1 |
ICD-9 |
2 |
ICD-10 |
3 |
Other |
9 |
Unknown |
Claims
Files Valid Values
DIAGNOSIS-POA-FLAG-1 to DIAGNOSIS-POA-FLAG-12
Y |
Diagnosis was present at time of inpatient admission |
N |
Diagnosis was not present at time of inpatient admission |
U |
Documentation insufficient to determine if condition was present at the time of inpatient admission |
W |
Clinically undetermined. Provider unable to clinically determine whether the condition was present at the time of inpatient admission. |
BLANK |
Exempt from POA reporting. |

Claims
Files Valid Values
DISCHARGE-HOUR
00 |
0:00-0:59 |
01 |
1:00-1:59 |
02 |
2:00-2:59 |
03 |
3:00-3:59 |
04 |
4:00-4:59 |
05 |
5:00-5:59 |
06 |
6:00-6:59 |
07 |
7:00-7:59 |
08 |
8:00-8:59 |
09 |
9:00-9:59 |
10 |
10:00-10:59 |
11 |
11:00-11:59 |
12 |
12:00-12:59 |
13 |
13:00-13:59 |
14 |
14:00-14:59 |
15 |
15:00-15:59 |
16 |
16:00-16:59 |
17 |
17:00-17:59 |
18 |
18:00-18:59 |
19 |
19:00-19:59 |
20 |
20:00-20:59 |
21 |
21:00-21:59 |
22 |
22:00-22:59 |
23 |
23:00-23:59 |

Claims
Files Valid Values
DISPENSING-PRESCRIPTION-DRUG-PROV-NPI
DISPENSING-PRESCRIPTION-DRUG-PROV-TAXONOMY

Claims
Files Valid Values
DRG-DESCRIPTION
http://www.cms.hhs.gov/MedicareFeeforSvcPartsAB/Downloads/DRGdesc06.pdf |

Claims
Files Valid Values
DRUG-UTILIZATION-CODE
439-E4 (Reason for Service Code) for the Conflict Codes |
|
AD |
Additional Drug Needed |
AN |
Prescription Authentication |
AR |
Adverse Drug Reaction |
AT |
Additive Toxicity |
CD |
Chronic Disease Management |
CH |
Call Help Desk |
CS |
Patient Complaint/Symptom |
DA |
Drug-Allergy |
DC |
Drug-Disease (Inferred) |
DD |
Drug-Drug Interaction |
DF |
Drug-Food interaction |
DI |
Drug Incompatibility |
DL |
Drug-Lab Conflict |
DM |
Apparent Drug Misuse |
DS |
Tobacco Use |
ED |
Patient Education/Instruction |
ER |
Overuse |
EX |
Excessive Quantity |
HD |
High Dose |
IC |
Iatrogenic Condition |
ID |
Ingredient Duplication |
LD |
Low Dose |
LK |
Lock In Recipient |
LR |
Underuse |
MC |
Drug-Disease (Reported) |
MN |
Insufficient Duration |
MS |
Missing Information/Clarification |
MX |
Excessive Duration |
NA |
Drug Not Available |
NC |
Non-covered Drug Purchase |
ND |
New Disease/Diagnosis |
NF |
Non-Formulary Drug |
NN |
Unnecessary Drug |
NP |
New Patient Processing |
NR |
Lactation/Nursing Interaction |
NS |
Insufficient Quantity |
OH |
Alcohol Conflict |
PA |
Drug-Age |
PC |
Patient Question/Concern |
PG |
Drug-Pregnancy |
PH |
Preventive Health Care |
PN |
Prescriber Consultation |
PP |
Plan Protocol |
PR |
Prior Adverse Reaction |
PS |
Product Selection Opportunity |
RE |
Suspected Environmental Risk |
RF |
Health Provider Referral |
44Ø-E5 (Professional Service Code) for the Intervention Codes |
|
ØØ |
No intervention |
AS |
Patient assessment |
CC |
Coordination of care |
DE |
Dosing evaluation/determination |
FE |
Formulary enforcement |
GP |
Generic product selection |
MA |
Medication administration |
MØ |
Prescriber consulted |
MR |
Medication review |
PE |
Patient education/instruction |
PH |
Patient medication history |
PM |
Patient monitoring |
PØ |
Patient consulted |
PT |
Perform laboratory test |
RØ |
Pharmacist consulted other source |
RT |
Recommend laboratory test |
SC |
Self-care consultation |
SW |
Literature search/review |
TC |
Payer/processor consulted |
TH |
Therapeutic product interchange |
441-E6 (Result of Service Code) for the Output Codes |
|
ØØ |
Not Specified |
1A |
Filled As Is, False Positive |
1B |
Filled Prescription As Is |
1C |
Filled, With Different Dose |
1D |
Filled, With Different Directions |
1E |
Filled, With Different Drug |
1F |
Filled, With Different Quantity |
1G |
Filled, With Prescriber Approval |
1H |
Brand-to-Generic Change |
1J |
Rx-to-OTC Change |
1K |
Filled with Different Dosage Form |
2A |
Prescription Not Filled |
2B |
Not Filled, Directions Clarified |
3A |
Recommendation Accepted |
3B |
Recommendation Not Accepted |
3C |
Discontinued Drug |
3D |
Regimen Changed |
3E |
Therapy Changed |
3F |
Therapy Changed-cost increased acknowledged |
3G |
Drug Therapy Unchanged |
3H |
Follow-Up/Report |
3J |
Patient Referral |
3K |
Instructions Understood |
3M |
Compliance Aid Provided |
3N |
Medication Administered |

Claims
Files Valid Values
FILE-ENCODING-SPECIFICATION
FLF |
The file follows a fixed length format. |
PSV |
The file follows a pipe-delimited format. |

Claims
Files Valid Values
FILE-NAME
CLAIM-IP |
Inpatient Claim/Encounters File - Claims/encounters with TYPE-OF-SERVICE = 001, 058, 084, 086, 090, 091, 092, 093, 123, or 132. (Note : In CLAIMIP, TYPE-OF-SERVICE 086 and 084 refer only to services received on an inpatient basis.) |
CLAIM-LT |
Long
Term Care Claims/Encounters File - Claims/encounters with
TYPE-OF-SERVICE = 009, 044, 045, 046, 047, 048, 059, or 133 (all
mental hospital, and NF services). |
CLAIM-OT |
Other Claims/Encounters File - Claims/encounters with TYPE-OF-SERVICE= 002, 003, 004, 005, 006, 007, 008, 010, 011, 012, 013, 015, 016, 017, 018, 019, 020, 021, 022, 025, 026, 027, 028, 029, 030, 031, 032, 035, 036, 037, 039, 040, 041, 043, 051, 052, 053, 054, 056, 060, 061, 062, 063, 064, 065, 066, 067, 068, 069, 073, 074, 075, 076, 077, 078, 079, 080, 081, 082, 083, 087, 115, 119, 120, 121, 122, 131, or 134. |
CLAIM-RX |
Pharmacy Claims/Encounters File - Claims/encounters with TYPE-OF-SERVICE= 033, 034, or 131. |

Claims
Files Valid Values
FILE-STATUS-INDICATOR
P |
Production File |
T |
Test File |

Claims
Files Valid Values
FIXED-PAYMENT-IND
0 |
Not Fixed Payment |
1 |
FFS Fixed Payment |

Claims
Files Valid Values
FORCED-CLAIM-IND
0 |
No |
1 |
Yes |

Claims
Files Valid Values
FUNDING-CODE
A |
Medicaid Agency |
B |
CHIP Agency |
C |
Mental Health Service Agency |
D |
Education Agency |
E |
Child and Family Services Agency |
F |
County |
G |
City |
H |
Providers |
I |
Other |

Claims
Files Valid Values
FUNDING-SOURCE-NONFEDERAL-SHARE
01 |
State appropriations to the Medicaid agency |
02 |
Intergovernmental transfers (IGT) |
03 |
Certified public expenditures (CPE) |
04 |
Provider taxes |
05 |
Donations |
06 |
State appropriations to the CHIP agency |
HCBS-SERVICE-CODE
Claims
Files Valid Values |
|
1 |
The HCBS service was provided under 1915(i) |
2 |
The HCBS service was provided under 1915(j) |
3 |
The HCBS service was provided under 1915(k) |
4 |
The HCBS service was provided under a 1915(c) HCBS Waiver |
5 |
The HCBS service was provided under an 1115 waiver |
6 |
The HCBS service was not provided under the statutes identified above and was of an acute care nature |
7 |
The HCBS service was not provided under the statutes identified above and was of a long term care nature |
8 |
The service is not an HCBS service (i.e. the HCBS classification is not applicable) |
9 |
Unknown |

Claims
Files Valid Values
HCBS-TAXONOMY
01010 |
Case Management |
02011 |
Group Living, Residential Habilitation |
02012 |
Group Living, Mental Health Services |
02013 |
Group Living, Other |
02021 |
Shared Living, Residential Habilitation |
02022 |
Shared Living, Mental Health Services |
02023 |
Shared Living, Other |
02031 |
In-e Residential Habilitation |
02032 |
In-Home Round-The-Clock Mental Health Services |
02033 |
In-Home Round-The-Clock Services, Other |
03010 |
Job Development |
03021 |
Ongoing Supported Employment, Individual |
03022 |
Ongoing Supported Employment, Group |
03030 |
Career Planning |
04010 |
Prevocational Services |
04020 |
Day Habilitation |
04030 |
Education Services |
04040 |
Day Treatment/Partial Hospitalization |
04050 |
Adult Day Health |
04060 |
Adult Day Services (Social Model) |
04070 |
Community Integration |
04080 |
Medical Day Care for Children |
05010 |
Private Duty Nursing |
05020 |
Skilled Nursing |
06010 |
Home Delivered Meals |
07010 |
Rent and Food Expenses For Live-In Caregiver |
08010 |
Home-Based Habilitation |
08020 |
Home Health Aide |
08030 |
Personal Care |
08040 |
Companion |
08050 |
Homemaker |
08060 |
Chore |
09011 |
Respite, Out-Of-Home |
09012 |
Respite, In-Home |
09020 |
Caregiver Counseling and/or Training |
10010 |
Mental Health Assessment |
10020 |
Assertive Community Treatment |
10030 |
Crisis Intervention |
10040 |
Behavior Support |
10050 |
Peer Specialist |
10060 |
Counseling |
10070 |
Psychosocial Rehabilitation |
10080 |
Clinic Services |
10090 |
Other Mental Health and Behavioral Services |
11010 |
Health Monitoring |
11020 |
Claims
Files Valid Values |
11030 |
Medication Assessment and/or Management |
11040 |
Nutrition Consultation |
11050 |
Physician Services |
11060 |
Prescription Drugs |
11070 |
Dental Services |
11080 |
Occupational Therapy |
11090 |
Physical Therapy |
11100 |
Speech, Hearing, And Language Therapy |
11110 |
Respiratory Therapy |
11120 |
Cognitive Rehabilitative Therapy |
11130 |
Other Therapies |
12010 |
Financial Management Services In Support Of Participant Direction |
12020 |
Information and Assistance In Support Of Participant Direction |
13010 |
Participant Training |
14010 |
Personal Emergency Response System (Pers) |
14020 |
Home and/or Vehicle Accessibility Adaptations |
14031 |
Equipment and Technology |
14032 |
Supplies |
15010 |
Non-Medical Transportation |
16010 |
Community Transition Services |
17010 |
Goods and Services |
17020 |
Interpreter |
17030 |
Housing Consultation |
17990 |
Other |

Claims
Files Valid Values
HCPCS-RATE
http://www.cms.gov/Medicare/Coding/MedHCPCSGenInfo/index.html?redirect=/medhcpcsgeninfo/ |

Claims
Files Valid Values
HEALTH-CARE-ACQUIRED-CONDITION-IND
0 |
No |
1 |
Yes |
9 |
Unknown |

Claims
Files Valid Values
HEALTH-HOME-ENTITY-NAME
The field can contain any alphanumeric characters, digits or symbols except the "pipe" (|).

Claims
Files Valid Values
HEALTH-HOME-PROVIDER-NPI

Claims
Files Valid Values
HEALTH-HOME-PROV-IND
0 |
No |
1 |
Yes |
8 |
Not Applicable |
9 |
Unknown |

Claims
Files Valid Values
IMMUNIZATION-TYPE
00 |
None |
01 |
Anthrax |
02 |
Cervical Cancer) |
03 |
Diphtheria |
04 |
Hepatitis A |
05 |
Hepatitis B |
06 |
Haemophilus influenza type b (Hib) |
07 |
Human Papillomavirus (HPV) |
08 |
H1N1 Flu |
09 |
Seasonal Flu |
10 |
Japanese Encephalitis |
11 |
Lyme Disease |
12 |
Measles |
13 |
Meningococcal |
14 |
Monkey pox |
15 |
Mumps |
16 |
Pertussis |
17 |
Pneumococcal |
18 |
Poliomyelitis |
19 |
Rabies |
20 |
Rotavirus |
21 |
Rubella |
22 |
Shingles |
23 |
Smallpox |
24 |
Tetanus |
25 |
Tuberculosis |
26 |
Typhoid Fever |
27 |
Varicella |
28 |
Yellow Fever |
29 |
Other |
88 |
Not Applicable |
99 |
Unknown |

Claims
Files Valid Values
LINE-ADJUSTMENT-IND
0 |
Original Claim/Encounter |
1 |
Void of a prior submission |
2 |
Re-submittal |
3 |
Credit Adjustment (negative supplemental) |
4 |
Debit Adjustment (positive supplemental) |
5 |
Credit Gross Adjustment. |
6 |
Debit Gross Adjustment |
9 |
Unknown |

Claims
Files Valid Values
LINE-ADJUSTMENT-REASON-CODE
http://www.wpc-edi.com/reference/codelists/healthcare/claim-adjustment-reason-codes/ |

Claims
Files Valid Values
MEDICARE-COMB-DED-IND
0 |
Amount not combined with coinsurance amount |
1 |
Amount combined with coinsurance amount |
9 |
Unknown |

Claims
Files Valid Values
MEDICARE-REIM-TYPE
01 |
IPPS - Acute Inpatient PPS |
02 |
LTCHPPS - Long-term Care Hospital PPS |
03 |
SNFPPS - Skilled Nursing Facility PPS |
04 |
HHPPS - Home Health PPS |
05 |
IRFPPS - Inpatient Rehabilitation Facility PPS |
06 |
IPFPPS - Inpatient Psychiatric Facility PPS |
07 |
OPPS - Outpatient PPS |
08 |
Fee Schedules (for physicians, DME, ambulance, and clinical lab) |
09 |
Part C Hierarchical Condition Category Risk Assessment (CMS-HCC RA) Capitation Payment Model |

Claims
Files Valid Values
NEW-REFILL-IND
00 |
New Prescription |
01-98 |
Number of Refill(s) |
99 |
Unknown |

Claims
Files Valid Values
NDC-UNIT-OF-MEASURE
Code |
Description |
F2 |
International Unit |
ML |
Milliliter |
ME |
Milligram |
GR |
Gram |
UN |
Unit |

Claims
Files Valid Values
OCCURRENCE-CODE-01 to OCCURRENCE-CODE-10
http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R1104cp.pdf |

Claims
Files Valid Values
OPERATING-PROV-NPI-NUM

Claims
Files Valid Values
OPERATING-PROV-TAXONOMY

Claims
Files Valid Values
ORIGINATION-STATE
|

Claims
Files Valid Values
OTHER-INSURANCE-IND
0 |
No |
1 |
Yes |
9 |
Unknown |

Claims
Files Valid Values
OTHER-TPL-COLLECTION
000 |
Not Applicable |
001 |
Third Party Resource is Casualty/Tort |
002 |
Third Party Resource is Estate |
003 |
Third Party Resource is Lien (TEFRA) |
004 |
Third Party Resource is Lien (Other) |
005 |
Third Party Resource is Worker’s Compensation |
006 |
Third Party Resource is Medical Malpractice |
007 |
Third Party Resource is Other |
999 |
Classification of Third Party Resource is Unknown |

Claims
Files Valid Values
OUTLIER-CODE
00 |
No Outlier |
01 |
Day Outlier |
02 |
Cost Outlier |
06 |
Valid DRG Received from the intermediary |
07 |
CMS Developed DRG |
08 |
CMS Developed DRG Using Patient Status Code |
09 |
Not Group able |
10 |
Composite of cost outliers |

Claims
Files Valid Values
PATIENT-STATUS
http://www.cms.hhs.gov/MLNMattersArticles/downloads/SE0801.pdf |
To order the current edition of the UB-04 Data Specifications Manual go to: http://www.nubc.org/subscriber/index.dhtml
American
Hospital Association
155 North Wacker Drive, Suite 400
Chicago,
IL 60606
Phone: 312-422-3000
Fax: 312-422-4500

Claims
Files Valid Values
PAYMENT-LEVEL-IND
1 |
Claim Header – Sum of Line Item payments |
2 |
Claim Detail – Individual Line Item payments |

Claims
Files Valid Values
PLACE-OF-SERVICE
http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c26.pdf |

Claims
Files Valid Values
PRESCRIBING-PROV-SPECIALTY
See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values. |

Claims
Files Valid Values
PRESCRIBING-PROV-TAXONOMY

Claims
Files Valid Values
PRESCRIBING-PROV-TYPE
See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values.

Claims
Files Valid Values
PROCEDURE-CODE 1 TO PROCEDURE-CODE-6

Claims
Files Valid Values
PROCEDURE-CODE-FLAG-1 - PROCEDURE-CODE-FLAG-6
01 |
CPT 4 |
02 |
ICD-9 CM |
06 |
HCPCS (Both National and Regional HCPCS) |
07 |
ICD-10 - CM PCS (Will be implemented on 10/1/2014) |
10-87 |
Other Systems |
88 |
Not Applicable |
99 |
Unknown |

Claims
Files Valid Values
PROGRAM-TYPE
Code |
Description |
00 |
No Special Program |
01 |
EPSDT |
02 |
Family Planning |
03 |
Rural Health Clinic |
04 |
Federally Qualified Health Centers (FQHC) |
05 |
Indian Health Services |
07 |
Home and Community Based Care Waiver Services |
08 |
Money Follows the Person (MFP) |
10 |
BIP - Balancing Incentive Payment |
11 |
Community First Choice (1915(k)) |
12 |
Medicaid Emergency Psychiatric Demonstration |
13 |
Home and Community Based Services (HCBS) State Plan Option (1915(i)) |
14 |
State Plan CHIP |
15 |
Psychiatric Residential Treatment Facilities Demonstration Grant Program (PRTF) |
16 |
1915(j) (Self- directed personal assistance services/personal care under State Plan or 1915(c) waiver) |
99 |
Unknown |

Claims
Files Valid Values
PROV-FACILITY-TYPE
Source: |
|
|||
|
|
|
||
|
Provider Facility Type Code |
Provider Facility Type Description |
||
|
100000000 |
Individuals or Groups (of Individuals) |
||
|
170000000 |
Non-Individual - Other Service Providers |
||
|
250000000 |
Non-Individual - Agencies |
||
|
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
||
|
270000000 |
Non-Individual - Hospital Units |
||
|
280000000 |
Non-Individual - Hospitals |
||
|
290000000 |
Non-Individual - Laboratories |
||
|
300000000 |
Non-Individual - Managed Care Organizations |
||
|
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
||
|
320000000 |
Non-Individual - Residential Treatment Facilities |
||
|
330000000 |
Non-Individual - Suppliers |
||
|
340000000 |
Non-Individual - Transportation Services |
||
|
380000000 |
Non-Individual - Respite Care Facility |
||
|
(Note: Appendix L takes the WPC taxonomy codes and relates each one to its provider facility type code) |
|||

Claims
Files Valid Values
REBATE-ELIGIBLE-INDICATOR
0 |
NDC is not eligible for drug rebate program. (Manufacturer does not have a rebate agreement.) |
1 |
NDC is eligible for drug rebate program |
2 |
NDC is exempt from the drug rebate program (biological and medical devices) |
9 |
The drug rebate eligibility of the is unknown |

Claims
Files Valid Values
RECORD-ID
CIP00001 |
FILE-HEADER-RECORD-IP |
CIP00002 |
CLAIM-HEADER-RECORD-IP |
CIP00003 |
CLAIM-LINE-RECORD-IP |
CLT00001 |
FILE-HEADER-RECORD-LT |
CLT00002 |
CLAIM-HEADER-RECORD-LT |
CLT00003 |
CLAIM-LINE-RECORD-LT |
COT00001 |
FILE-HEADER-RECORD-OT |
COT00002 |
CLAIM-HEADER-RECORD-OT |
COT00003 |
CLAIM-LINE-RECORD-OT |
CRX00001 |
FILE-HEADER-RECORD-RX |
CRX00002 |
CLAIM-HEADER-RECORD-RX |
CRX00003 |
CLAIM-LINE-RECORD-RX |

Claims
Files Valid Values
REFERRING-PROV-NPI-NUMBER

Claims
Files Valid Values
REFERRING-PROV-SPECIALTY
See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values.

Claims
Files Valid Values
REFERRING-PROV-TAXONOMY
|
|

Claims
Files Valid Values
REFERRING-PROV-TYPE
See Appendix A under PROV-CLASSIFICATION-CODE #3 for a listing of valid values.

Claims
Files Valid Values
SELF-DIRECTION-TYPE
000 |
Not Applicable |
001 |
Hiring Authority |
002 |
Budget Authority |
003 |
Hiring and Budget Authority |
999 |
Type of Authority Is Unknown |

Claims
Files Valid Values
SERVICE-TRACKING-TYPE
00 |
Not a Service Tracking Claim |
01 |
Drug Rebate |
02 |
DSH Payment |
03 |
Lump Sum Payment |
04 |
Cost Settlement |
05 |
Supplemental |
06 |
Other |
99 |
Unknown |

Claims
Files Valid Values
SERVICING-PROV-NPI-NUM

Claims
Files Valid Values
SERVICING-PROV-SPECIALTY
See Appendix A under PROV-CLASSIFICATION-CODE #2 for a listing of valid values.

Claims
Files Valid Values
SERVICING-PROV-TAXONOMY

Claims
Files Valid Values
SOURCE-LOCATION
01 |
MMIS |
02 |
Non-MMIS CHIP Payment System |
03 |
Pharmacy Benefits Manager (PBM) Vendor |
04 |
Dental Benefits Manager Vendor |
05 |
Transportation Provider System |
06 |
Mental Health Claims Payment System |
07 |
Financial Transaction/Accounting System |
08 |
Other State Agency Claims Payment System |
09 |
County/Local Government Claims Payment System |
10 |
Other Vendor/Other Claims Payment System |
20 |
Managed Care Organization (MCO) |
99 |
Unknown source |

Claims
Files Valid Values
SPLIT-CLAIM-IND
0 |
No |
1 |
Yes |
9 |
Unknown |

Claims
Files Valid Values
SSN-INDICATOR
0 |
State does not use SSN as MSIS-IDENTIFICATION-NUMBER |
1 |
State uses SSN as MSIS-IDENTIFICATION-NUMBER |

Claims
Files Valid Values
SUBMISSION-TRANSACTION-TYPE
C |
Create File—a file that contains a complete set of transactions/changes processed since the last Create file submission. States may submit only one valid Create file per reporting period and data file type. |
R |
Replacement File—a Replacement submission is a replacement of the month’s data. It will completely replace the immediate prior submission. If a later replacement entry is received, it will overwrite the previous replacement, as well as a prior Create or Update submission for the same data type and reporting period. |
U |
Update File—a file that contains T-MSIS record segments created in response to business rule rejects. Note: The records in an Update file are not generated as a result of a change processed in the state’s Medicaid or Medicaid-related systems during the current reporting month. These Update file record segments may be unchanged from the ones submitted previously for various reasons (for example, the state may be unable to process a change record in their Medicaid / Medicaid-related systems to correct the issue because the state is simply passing through to T-MSIS data that originated outside of the state’s systems).[1] Conversely, the records may be different from those previously submitted, but the change is the result of a fix whose root cause problem was an issue in the T-MSIS file-creation or replacement process at CMS. Regardless, the record was not generated from a change that occurred in the state’s source data. |
SUBMITTING-STATE
Claims
Files Valid Values |

Claims
Files Valid Values
TOOTH-DESIGNATION-SYSTEM
JO |
ANSI/ADA/ISO Specification No. 3950 |
JP |
ADA’s Universal/National Tooth Designation system |

Claims
Files Valid Values
TOOTH-NUM
Primary Dentition:
|

Claims
Files Valid Values
TOOTH-QUAD-CODE
00 |
Entire Oral Cavity |
01 |
Maxillary Area |
02 |
Mandibular Area |
03 |
Upper Right Sextant |
04 |
Upper Anterior Sextant |
05 |
Upper Left Sextant |
06 |
Lower Left Sextant |
07 |
Lower Anterior Sextant |
08 |
Lower Right Sextant |
09 |
Other Area of Oral Cavity (An area specified in an annexed document or further explanation available.) |
10 |
Upper Right Quadrant (Right Refers to the oral and skeletal structures on the right side.) |
20 |
Upper Left Quadrant (Left Refers to the oral and skeletal structures on the left side.) |
30 |
Lower Left Quadrant |
40 |
Lower Right Quadrant |

Claims
Files Valid Values
TOOTH-SURFACE-CODE
B |
Buccal – The surface of the tooth which is closest to the cheek. |
D |
Distal – The surface of the tooth facing away from an invisible line drawn vertically through the center of the face. |
F |
Facial – The surface of a tooth that is directed towards the face. |
I |
Incisal – The cutting edges of the anterior teeth. |
L |
Lingual – The surface of the tooth that is directed towards the tongue. |
M |
Mesial – The surface of a tooth which faces toward an invisible line drawn vertically through the center of the face. |
O |
Occlusa – The surfaces of the posterior (back) teeth which provides the chewing function. |

Claims
Files Valid Values
TYPE-OF-BILL
2nd Digit-Type of Facility |
|
1 |
Hospital |
2 |
Skilled Nursing |
3 |
Home Health |
4 |
Religious Nonmedical (Hospital) |
5 |
Reserved for national assignment (discontinued effective 10/1/05). |
6 |
Intermediate Care |
7 |
Clinic or Hospital Based Renal Dialysis Facility (requires special information in second digit below). |
8 |
Special facility or hospital ASC surgery (requires special information in second digit below). |
9 |
Reserved for National Assignment |
3rd Digit-Bill Classification (Except Clinics and Special Facilities) |
|
1 |
Inpatient |
2 |
Inpatient |
3 |
Outpatient |
4 |
Other |
5 |
Intermediate Care - Level I |
6 |
Intermediate Care - Level II |
7 |
Reserved for national assignment (discontinued effective 10/1/05). |
8 |
Swing Bed (may be used to indicate billing for SNF level of care in a hospital with an approved swing bed agreement). |
9 |
Reserved for National Assignment |
3rd Digit-Classification (Clinics Only) |
|
1 |
Rural Health Clinic (RHC) |
2 |
Hospital Based or Independent Renal Dialysis Facility |
3 |
Free Standing Provider-Based Federally Qualified Health Center (FQHC) |
4 |
Other Rehabilitation Facility (ORF) |
5 |
Comprehensive Outpatient Rehabilitation Facility (CORF) |
6 |
Community Mental Health Center (CMHC) |
7-8 |
Reserved for National Assignment |
9 |
OTHER |
3rd Digit-Classification (Special Facilities Only) |
|
1 |
Hospice (Nonhospital Based) |
2 |
Hospice (Hospital Based) |
3 |
Ambulatory Surgical Center Services to Hospital Outpatients |
4 |
Free Standing Birthing Center |
5 |
Critical Access Hospital |
6-8 |
Reserved for National Assignment |
9 |
OTHER |
4th Digit-Frequency |
|
A |
Admission/Election Notice |
B |
Hospice/Medicare Coordinated Care Demonstration/Religious Nonmedical Health Care Institution Termination/Revocation Notice |
C |
Hospice Change of Provider Notice |
D |
Claims
Files Valid Values |
E |
Hospice Change of Ownership |
F |
Beneficiary Initiated Adjustment Claim |
G |
CWF Initiated Adjustment Claim |
H |
CMS Initiated Adjustment Claim |
I |
FI Adjustment Claim (Other than QIO or Provider |
J |
Initiated Adjustment Claim-Other |
K |
OIG Initiated Adjustment Claim |
M |
MSP Initiated Adjustment Claim |
P |
QIO Adjustment Claim |
0 |
Nonpayment/Zero Claims |
1 |
Admit Through Discharge Claim |
2 |
Interim-First Claim |
3 |
Interim-Continuing Claims (Not valid for PPS Bills) |
4 |
Interim-Last Claim (Not valid for PPS Bills) |
5 |
Late Charge Only |
7 |
Replacement of Prior Claim |
8 |
Void/Cancel of a Prior Claim |
9 |
Final Claim for a Home Health PPS Episode |

Claims
Files Valid Values
TYPE-OF-CLAIM
1 |
A Fee-For-Service Medicaid or Medicaid-expansion Claim |
2 |
Medicaid or Medicaid-expansion Capitated Payment |
3
|
Medicaid or Medicaid-expansion Managed Care Encounter (a.k.a. “Dummy”) record that simulates a bill for a service rendered to a patient covered under some form of Capitation Plan. This includes billing records submitted by providers to non-state entities (e.g., MCOs, health plans) for which the State has no financial liability since the at risk entity has already received a capitated payment from the State. |
4 |
Medicaid or Medicaid-expansion Service Tracking Claim |
5 |
Medicaid or Medicaid-expansion Supplemental Payment (above capitation fee or above negotiated rate) (e.g., FQHC additional reimbursement) |
A |
Separate CHIP (Title XXI) claim: A Fee-for-Service Claim |
B |
Separate CHIP (Title XXI) claim: Capitated Payment |
C |
Separate CHIP (Title XXI) encounter record that simulates a bill for a service or items rendered to a patient covered under some form of Capitation Plan. This includes billing records submitted by providers to non-State entities (e.g., MCO’s, health plans) for which a state has no financial liability as the at-risk entity has already received a capitated payment from the state |
D |
Separate CHIP (Title XXI) Service Tracking Claim |
E |
Separate CHIP (Title XXI) claim for a supplemental payment (above capitation fee or above negotiated rate) (e.g., FQHC additional reimbursement) |
U |
Other FFS claim |
V |
Other Capitated Payment |
W |
Other Managed Care Encounter |
X |
Non-Medicaid/CHIP service tracking claims |
Y |
Other Supplemental Payment |
Z |
Denied claims |

Claims
Files Valid Values
TYPE-OF-HOSPITAL
00 |
Not a hospital |
01 |
Inpatient Hospital |
02 |
Outpatient Hospital |
03 |
Critical Access Hospital |
04 |
Swing Bed Hospital |
05 |
Inpatient Psychiatric Hospital |
06 |
IHS Hospital |
07 |
Children’s Hospital |
08 |
Other |
99 |
Unknown |

Claims
Files Valid Values
TYPE-OF-SERVICE
TOS
Code |
TOS
Description |
FILE-NAME
|
001 |
Inpatient hospital services, other than services in an institution for mental diseases |
CLAIMIP |
002 |
Outpatient hospital services |
CLAIMOT |
003 |
Rural health clinic services |
CLAIMOT |
004 |
Other ambulatory services furnished by a rural health clinic |
CLAIMOT |
005 |
Professional laboratory services, Technical laboratory services |
CLAIMOT |
006 |
Technical laboratory services |
CLAIMOT |
007 |
Professional radiological services |
CLAIMOT |
008 |
Technical radiological services |
CLAIMOT |
009 |
Nursing facility services for individuals age 21 or older (other than services in an institution for mental disease) |
CLAIMLT |
010 |
Early and periodic screening and diagnosis and treatment (EPSDT) services |
CLAIMOT |
011 |
Family planning services and supplies for individuals of child-bearing age |
CLAIMOT CLAIMRX |
012 |
Physicians' services |
CLAIMOT |
013 |
Medical and surgical services of a dentist |
CLAIMOT |
014 |
Outpatient substance abuse treatment services. |
CLAIMOT |
015 |
Medical or other remedial care or services, other than physicians' services, provided by licensed practitioners within the scope of practice as defined under State law |
CLAIMOT |
016 |
Home health services - Nursing services |
CLAIMOT |
017 |
Home health services - Home health aide services |
CLAIMOT |
018 |
Home health services - Medical supplies, equipment, and appliances suitable for use in the home |
CLAIMOT CLAIMRX |
019 |
Home health services - Physical therapy provided by a home health agency or by a facility licensed by the State to provide medical rehabilitation services |
CLAIMOT |
020 |
Home health services - Occupational therapy provided by a home health agency or by a facility licensed by the State to provide medical rehabilitation services |
CLAIMOT |
021 |
Home health services - Speech pathology and audiology services provided by a home health agency or by a facility licensed by the State to provide medical rehabilitation services |
CLAIMOT |
022 |
Private duty nursing services |
CLAIMOT |
023 |
Advanced practice nurse services |
CLAIMOT |
024 |
Pediatric nurse |
CLAIMOT |
025 |
Nurse-midwife service |
CLAIMOT |
026 |
Nurse practitioner services |
CLAIMOT |
027 |
Respiratory care for ventilator-dependent individuals |
CLAIMOT |
028 |
Clinic services |
CLAIMOT |
029 |
Dental services |
CLAIMOT |
030 |
Physical therapy services (when not provided under home health services) |
CLAIMOT |
031 |
Occupational therapy services (when not provided under home health services) |
CLAIMOT |
032 |
Speech, hearing, and language disorders services (when not provided under home health services) |
CLAIMOT |
033 |
Prescribed drugs |
CLAIMRX |
034 |
Over-the-counter medications. |
CLAIMRX |
035 |
Dentures |
CLAIMOT |
036 |
Medical equipment/prosthetic devices |
CLAIMOT CLAIMRX |
037 |
Eyeglasses |
CLAIMOT |
038 |
Hearing Aids |
CLAIMOT |
039 |
Diagnostic services |
CLAIMOT |
040 |
Screening services |
CLAIMOT |
041 |
Preventive services |
CLAIMOT |
042 |
Well-baby and well-child care services as defined by the State. |
CLAIMOT |
043 |
Rehabilitative services |
CLAIMOT |
044 |
Inpatient hospital services for individuals age 65 or older in institutions for mental diseases |
CLAIMLT |
045 |
Nursing facility services for individuals age 65 or older in institutions for mental diseases |
CLAIMLT |
046 |
Intermediate care facility (ICF/IIDICF/IID) services |
CLAIMLT |
047 |
Nursing facility services, other than in institutions for mental diseases |
CLAIMLT |
048 |
Inpatient psychiatric services for individuals under age 21 |
CLAIMLT |
049 |
Outpatient mental health services, other than Outpatient substance abuse treatment services. This TOS includes services furnished in a State-operated mental hospital and including community-based services. |
CLAIMOT |
050 |
Inpatient substance abuse treatment services and residential substance abuse treatment services. |
CLAIMLT CLAIMOT |
051 |
Personal care services |
CLAIMOT |
052 |
Primary care case management services |
CLAIMOT |
053 |
Targeted case management services |
CLAIMOT |
054 |
Case Management services other than those that meet the definition of primary care case management services or targeted case management services |
CLAIMOT |
055 |
Care coordination services |
CLAIMOT |
056 |
Transportation services |
CLAIMOT |
057 |
Enabling services |
CLAIMOT |
058 |
Services furnished in a religious nonmedical health care institution |
CLAIMIP |
059 |
Skilled nursing facility services for individuals under age 21 |
CLAIMLT |
060 |
Emergency hospital services |
CLAIMIP CLAIMOT |
061 |
Critical access hospital services - OT |
CLAIMOT |
062 |
HCBS - Case management services |
CLAIMOT |
063 |
HCBS - Homemaker services |
CLAIMOT |
064 |
HCBS - Home health aide services |
CLAIMOT |
065 |
HCBS - Personal care services |
CLAIMOT |
066 |
HCBS - Adult day health services |
CLAIMOT |
067 |
HCBS - Habilitation services |
CLAIMOT |
068 |
HCBS - Respite care services |
CLAIMOT |
069 |
HCBS - Day treatment or other partial hospitalization services, psychosocial rehabilitation services and clinic services (whether or not furnished in a facility) for individuals with chronic mental illness |
CLAIMOT |
070 |
HCBS - Day Care |
CLAIMOT |
071 |
HCBS - Training for family members |
CLAIMOT |
072 |
HCBS - Minor modification to the home |
CLAIMOT |
073 |
HCBS - Other services requested by the agency and approved by CMS as cost effective and necessary to avoid institutionalization |
CLAIMOT |
074 |
HCBS - Expanded habilitation services - Prevocational services |
CLAIMOT |
075 |
HCBS - Expanded habilitation services - Educational services |
CLAIMOT |
076 |
HCBS - Expanded habilitation services - Supported employment services, which facilitate paid employment |
CLAIMOT |
077 |
HCBS-65-plus - Case management services |
CLAIMOT |
078 |
HCBS-65-plus - Homemaker services |
CLAIMOT |
079 |
HCBS-65-plus - Home health aide services |
CLAIMOT |
080 |
HCBS-65-plus - Personal care services |
CLAIMOT |
081 |
HCBS-65-plus - Adult day health services |
CLAIMOT |
082 |
HCBS-65-plus - Respite care services |
CLAIMOT |
083 |
HCBS-65-plus - Other medical and social services |
CLAIMOT |
084 |
Sterilizations |
CLAIMIP CLAIMOT |
085 |
Prenatal care and pre-pregnancy family planning services and supplies. |
CLAIMOT CLAIMRX |
086 |
Other Pregnancy-related Procedures |
CLAIMIP CLAIMOT |
087 |
Hospice services |
CLAIMOT |
088 |
Any other health care services or items specified by the Secretary and not excluded under regulations. |
CLAIMOT
|
089 |
Disposable medical supplies. |
CLAIMOT CLAIMRX |
090 |
Critical access hospital services – IP |
CLAIMIP |
091 |
Skilled care – hospital residing |
CLAIMIP |
092 |
Exceptional care – hospital residing |
CLAIMIP |
093 |
Non-acute care – hospital residing |
CLAIMIP |
115 |
Residential care |
CLAIMOT |
119 |
Capitated payments to HMOs, HIOs, or PACE plans |
CLAIMOT |
120 |
Capitated payments for primary care case management (PCCM) |
CLAIMOT |
121 |
Premium payments for private health insurance |
CLAIMOT |
122 |
Capitated payments to prepaid health plans (PHPs) |
CLAIMOT |
123 |
Disproportionate share hospital (DSH) payments |
CLAIMIP CLAIMOT |
127 |
Indian Health Service (IHS) - Family Plan |
CLAIMOT CLAIMRX |
131 |
Drug Rebates |
CLAIMOT CLAIMRX |
132 |
Supplemental payment - inpatient |
CLAIMIP |
133 |
Supplemental payment - nursing |
CLAIMLT |
134 |
Supplemental payment - outpatient |
CLAIMOT |
135 |
EHR payments to provider |
CLAIMIP CLAIMOT |


Claims
Files Valid Values
Claims
Files Valid Values
UNDER-DIRECTION-OF-PROV-NPI

Claims
Files Valid Values
UNDER-DIRECTION-OF-PROV-TAXONOMY

Claims
Files Valid Values
UNDER-SUPERVISION-OF-PROV-NPI

Claims
Files Valid Values
UNDER-SUPERVISION-OF-PROV-TAXONOMY

Claims
Files Valid Values
UNIT-OF-MEASURE
F2 |
International Unit |
ML |
Milliliter |
GR |
Gram |
UN |
Unit |

Claims
Files Valid Values
WAIVER-TYPE
01 |
1115 other demonstration – Such waivers may also be called a research, experimental, demonstration or pilot waiver, or refer to consumer-directed care or expanded eligibility. It may cover the entire state or just a geographic entity or specific population. |
02 |
1915(b)(1) – These waivers permit freedom-of-choice or mandatory managed care with some voluntary managed care... |
03 |
1915(b)(2) – These waivers allow states to use enrollment brokers.. |
04 |
1915(b)(3) – These waivers allow states to use savings to provide additional services that are not in the State Plan.. . |
05 |
1915(b)(4) – These waivers allow fee for service selective contracting. |
06 |
1915(c) – Aged and Disabled |
07 |
1915(c) – Aged |
08 |
1915(c) – Physical Disabilities |
09 |
1915(c) – Intellectual Disabilities |
10 |
1915(c) – Intellectual and Developmental Disabilities |
11 |
1915(c) – Brain Injury |
12 |
1915(c) – HIV/AIDS |
13 |
1915(c) – Technology Dependent or Medically Fragile |
14 |
1915(c) –Disabled (other) |
15 |
1915(c) - Enrolled in 1915(c) waiver for unspecified or unknown populations |
16 |
1915(c) - Autism/Autism spectrum disorder |
17 |
1915(c) – Developmental Disabilities |
18 |
1915(c) – Mental Illness - Age 18 or Older |
19 |
1915(c) – Mental Illness - Under Age 18 |
20 |
Concurrent 1915(b)(c) – A concurrent HCBS/1915(c) waiver is one where the approved waiver services are delivered through a managed care authority – e.g., 1115(a), 1915(a), 1915(b), or 1932(a) |
21 |
1115 HIFA Waiver – The associated Waiver-ID is for a HIFA (Health Insurance and Flexibility and Accountability) waiver. May also be called demonstration waiver or refer to the eligibility expansion. |
22 |
1115 Pharmacy Plus Waiver – The associated Waiver-ID is for Pharmacy waiver coverage. Includes waivers under 1115 demonstration authority which are primarily intended to increase coverage or expand eligibility for pharmacy benefits. The associated Waiver-ID is for another type of waiver. |
23 |
1115 Disaster-Related Waiver – The associated Waiver-ID is for a disaster-related waiver that allows for coverage related to a hurricane or other disaster. |
24 |
1115 Family Planning-ONLY waiver – The associated Waiver-ID-Number is for a Family Planning-ONLY waiver. In these waivers, the beneficiary’s Medicaid-covered benefits are restricted to Family Planning Services. |
88 |
Not Applicable - The individual is eligible for Medicaid or CHIP, but is NOT enrolled in a waiver. |
99 |
Unknown – The associated Waiver-ID is for an unknown type of waiver. |

Claims
Files Valid Values
XIX-MBESCBES-CATEGORY-OF-SERVICE
See Appendix I: MBES CBES Category of Service Line Definitions for the 64.9 Base Form for listing of valid values. |

Claims
Files Valid Values
XXI-MBESCBES-CATEGORY-OF-SERVICE
See Appendix J: MBES CBES Category of Service Line Definitions for the 21 Form for listing of valid values. |
Appendix B: Home and Community-Based Services (HCBS) Taxonomy
The following table defines categories and services in the HCBS Taxonomy. It was approved by CMS in August 2012.
To acknowledge state variation, services and categories are defined based on the minimum definition necessary to establish mutually distinct categories and services. Some services are defined in part by characteristics that are NOT in that service. For example, the difference between companion services and personal care is that companion services do not include assistance with activities of daily living (ADLs) such as bathing, dressing, eating, and toileting.
Some of the services reflected below, including, but not limited to personal care, case management, home health aide, and physician services, may (and in some case, must) also be covered under the Medicaid State Plan. The definitions below only define these services for purposes of Section 1915(c) Waivers and the State Plan Home and Community-Based Services benefit authorized by Section 1915(i). States interested in reflecting services as “extended state plan” services must offer them in accordance with state plan service definitions. Consult with the CMS Division of Benefits and Coverage in those instances to ensure definition alignment.
The services and categories are arranged in order of consideration for placing a particular state service in the taxonomy. If one is not sure how to map a state’s service to the taxonomy, one should first consider Case Management, then Round-the-Clock Services, then Supported Employment, etc.
HCBS Service Taxonomy Values:
Category |
Sub-Category (where applicable) |
Service |
Common Names (where applicable) |
Definition |
01 – Case Management |
|
|
|
The development of a comprehensive, written individualized support plan. In addition, case management often includes assisting people in gaining access to necessary services, assessment of a person's needs, ongoing monitoring of service provision and/or a person's health and welfare, assistance in accessing supports to transition from an institutional setting (but not the transition services themselves); and development of a 24-hour individual back-up plan with formal and informal supports |
|
01010 case management |
|
care
management |
Same definition as category 01. |
02 Round-the-Clock Services |
|
|
|
Services by a provider that has round-the-clock responsibility for the health and welfare of residents, except during the time other services (e.g., day services) are furnished. If these services are provided in a 1915(c) waiver, the state must complete Appendix G-3 of the 1915(c) waiver application regarding medication management and administration. |
|
0201 group living |
|
assisted
living |
Round-the-clock services provided in a residence that is NOT a person’s home or apartment or a single family residence where one or more people with a disability live with a person or family who furnishes services |
|
|
02011 group living, residential habilitation |
|
Assistance in acquiring, retaining, and improving self-help, socialization, and/or adaptive skills by a provider with round-the-clock responsibility for the residents’ health and welfare in a residence that is NOT a person’s own home or apartment or a single family residence where one or more people with a disability live with a person or family who furnishes services. |
|
|
02012 group living, mental health services |
|
Mental health services by a provider with round-the-clock responsibility for the residents’ health and welfare in a residence that is NOT a person’s own home or apartment or a single family residence where one or more people with a disability live with a person or family who furnishes services. |
|
|
02013 group living, other |
|
Health and social services not identified elsewhere in subcategory 0201 by a provider with round-the-clock responsibility for the residents’ health and welfare in a residence that is NOT a person’s own home or apartment or a single family residence where one or more people with a disability live with a person or family who furnishes services. |
|
0202 shared living |
|
adult
foster care |
Round-the-clock services provided in a single family residence where one or more people with a disability live with a person or family who furnishes services. |
|
|
02021 shared living, residential habilitation |
|
Assistance in acquiring, retaining, and improving self-help, socialization, and/or adaptive skills provided in a single family residence where one or more people with a disability live with a person or family who furnishes services and has round-the-clock responsibility for the residents’ health and welfare. |
|
|
02022 shared living, mental health services |
|
Mental health services provided in a single family residence where one or more people with a disability live with a person or family who furnishes services and has round-the-clock responsibility for the residents’ health and welfare. |
|
|
02023 shared living, other |
|
Health and social services not identified elsewhere in subcategory 0202 provided in a single family residence where one or more people with a disability live with a person or family who furnishes services and has round-the-clock responsibility for the residents’ health and welfare. |
|
0203 in-home round-the-clock services |
|
supported living |
Round-the-clock services provided in a person's home or apartment where a provider has round-the-clock responsibility for the person's health and welfare. |
|
|
02031 in-home residential habilitation |
|
Assistance in acquiring, retaining, and improving self-help, socialization, and/or adaptive skills provided in a person's home or apartment where a provider has round-the-clock responsibility for the person's health and welfare. |
|
|
02032 in-home round-the-clock mental health services |
|
Mental health services provided in a person's home or apartment where a provider has round-the-clock responsibility for the person's health and welfare. |
|
|
02033 in-home round-the-clock services, other |
|
Health and social services not identified elsewhere in subcategory 0203 provided in a person's home or apartment where a provider has round-the-clock responsibility for the person's health and welfare. |
03 Supported Employment |
|
|
|
Assistance to help a person obtain or maintain paid employment or self-employment. |
|
0301 job development |
03010 job development |
|
Assistance to locate and obtain paid employment or self-employment. |
|
0302 ongoing supported employment |
|
|
Assistance to maintain paid employment or self-employment. |
|
|
03021 ongoing supported employment, individual |
|
Assistance to maintain self-employment or paid employment in an individual job placement (i.e., person is working with people without disabilities). |
|
|
03022 ongoing supported employment, group |
|
Assistance to maintain paid employment in a group placement (i.e., person is working on a team of people with disabilities). |
|
0303 career planning |
03030 career planning |
|
Focused, time-limited assistance to identify a career direction and develop a plan to achieve employment. |
04 Day Services |
|
|
|
Services other than supported employment typically provided outside the person's home during the working day (i.e., Monday through Friday between 8 a.m. and 5 p.m.). These services provide a range of supports and are often, but not always, provided on a regularly scheduled basis at a site specifically established to provide day services. |
|
|
04010 prevocational services |
|
Time-limited services to provide learning and work experiences, including volunteer work, to acquire general skills that help a person obtain paid employment in integrated community settings. |
|
|
04020 day habilitation |
|
Regularly scheduled activities in settings separate from the participant’s residence, including assistance in acquiring, retaining, and improving self-help, socialization, and/or adaptive skills. This service includes community-based volunteer activities that include acquiring, retaining, and improving self-help, socialization, and adaptive skills. This service can include the supports offered in adult day health, adult day services (social model), and community integration if these supports are provided along with assistance in acquiring, retraining, and improving self-help, socialization, and/or adaptive skills. |
|
|
04030 education services |
|
Services to help a person access post-secondary education. |
|
|
04040 day treatment/ partial hospitalization |
|
Services necessary for the diagnosis or treatment of the person's mental illness provided in a fixed site facility during the working day. |
|
|
04050 adult day health |
|
Skilled health services and other support services, NOT including habilitation (i.e., assistance in acquiring, retaining, and improving self-help, socialization, and/or adaptive skills), provided to adults in a fixed site facility during the working day. This service can include the supports offered in adult day services (social model) if these supports are provided along with skilled health services. |
|
|
04060 adult day services (social model) |
|
Support services, NOT including skilled health services and not including habilitation (i.e., assistance in acquiring, retaining, and improving self-help, socialization, and/or adaptive skills), provided to adults in a fixed site facility during the working day. |
|
|
04070 community integration |
escort |
Assistance in participating in community activities, NOT including assistance with activities of daily living or assistance in acquiring, retraining, and improving self-help, socialization, and/or adaptive skills. This service can include supports furnished in the person’s residence related to community participation. |
|
|
04080 medical day care for children |
|
Medical services beyond typical day care responsibilities provided during the working day for infants, toddlers, and pre-school age children. |
05 Nursing |
|
|
|
Services within the scope of the state's nurse practices act provided by a licensed nurse. |
|
|
05010 private duty nursing |
|
Licensed nursing services provided on a continuous or full-time basis (e.g., for more than 4 consecutive hours per day and for more than 60 days). This service can include the supports offered in health assessment, health monitoring, and medication assessment if the service also includes other services within the scope of the state’s nurse practices act. |
|
|
05020 skilled nursing |
|
Licensed nursing services provided on a part-time or intermittent basis. This service can include the supports offered in health assessment, health monitoring, and medication assessment if the service also includes other services within the scope of the state’s nurse practices act. |
06 Home delivered meals |
|
|
|
Prepared meals sent to a person's home, which may not comprise a full nutritional regimen. |
|
|
06010 home delivered meals |
|
Same definition as category 06. |
07 Rent and Food Expenses for Live-In Caregiver |
|
|
|
Payment for the additional costs of rent and food that can be attributed to an unrelated direct support worker living with the person. This service does not include payment for the direct support worker’s services, which may be covered as part of other services such as personal care. |
|
|
07010 rent and food expenses for live-in caregiver |
|
Same definition as category 07. |
08 Home-Based Services |
|
|
|
Services that support a person in his or her home or apartment, when the provider does not have round-the-clock responsibility for the person's health and welfare. These services can be provided in other community settings, but are primarily furnished in a person’s home or apartment. |
|
|
08010 home-based habilitation |
supported living (provided on an hourly basis) |
Assistance in acquiring, retaining, and improving self-help, socialization, and/or adaptive skills provided in the person's home when the provider does NOT have round-the-clock responsibility for the person's health and welfare. This service can include the supports offered in community integration, home health aide, personal care, companion, and homemaker if these supports are provided along with assistance in acquiring, retraining, and improving self-help, socialization, and/or adaptive skills. |
|
|
08020 home health aide |
|
Assistance with activities of daily living (ADLs) and/or health-related tasks provided in a person's home and possibly other community settings that are supervised by a registered nurse or licensed therapist and provided by a licensed home health agency. Home health aide may include assistance with instrumental activities of daily living (IADLs). Home health aide may include the supports offered in companion and homemaker if these supports are provided along with assistance with ADLs and/or health-related tasks. Home health aide does NOT include habilitation (assistance in acquiring, retaining, and improving self-help, socialization, and/or adaptive skills). |
|
|
08030 personal care |
attendant
care |
Assistance with ADLs and/or health-related tasks provided in a person's home and possibly other community settings, NOT including both provision by a licensed home health agency and a requirement for supervision by a licensed nurse or therapist. Personal care may include assistance with IADLs. Personal care may include the supports offered in companion and homemaker if these supports are provided along with assistance with ADLs and/or health-related tasks. Personal care does NOT include habilitation (assistance in acquiring, retaining, and improving self-help, socialization, and/or adaptive skills). |
|
|
08040 companion |
adult
companion |
Supervision and/or social support provided in a person's home and possibly other community settings. Companion may also include performance of light housekeeping tasks (the supports offered in homemaker). Companion does NOT include assistance with ADLs or habilitation (assistance in acquiring, retaining, and improving self-help, socialization, and/or adaptive skills). |
|
|
08050 homemaker |
|
Performance of light housekeeping tasks provided in a person's home and possibly other community settings NOT including supervision and social support, assistance with ADLs, or habilitation (assistance in acquiring, retaining, and improving self-help, socialization, and/or adaptive skills). |
|
|
08060 chore |
|
Performance of heavy household chores provided in a person's home and possibly other community settings NOT including supervision and social support, assistance with ADLs, or habilitation (assistance in acquiring, retaining, and improving self-help, socialization, and/or adaptive skills). |
09 Caregiver Support |
|
|
|
Assistance to people who provide ongoing support to the person with a disability when assisting the support person is the primary purpose of the service. In most cases, the support person is unpaid. However, respite can be provided to relieve providers who furnish shared living. |
|
0901 respite |
|
|
Short-term services provided because a support person is absent or needs relief when relieving the support person is the primary purpose of the service. |
|
|
09011 respite, out-of-home |
|
Short-term services provided because a support person is absent or needs relief NOT provided in a person's home or apartment when relieving the support person is the primary purpose of the service. |
|
|
09012 respite, in-home |
|
Short-term services provided because a support person is absent or needs relief provided in a person's home or apartment when relieving the support person is the primary purpose of the service. |
|
0902 caregiver counseling and/or training |
09020 caregiver counseling and/or training |
|
Counseling, emotional support, and/or training provided to a family member or friend providing support when providing counseling or training to the support person is the primary purpose of the service. Examples of training topics include a) skills to provide specific treatment regimens or help the person improve function, b) information about the person's disability or conditions, and c) navigation of the service system. |
10 Other Mental Health and Behavioral Services |
|
|
|
Services NOT identified in previous categories that support people in improving or maintaining mental or behavioral health. |
|
|
10010 mental health assessment |
|
Assessment or evaluation of mental health status when the assessment is the primary purpose of the service. This service can include medication assessment if the assessment includes other mental health information. |
|
|
10020 assertive community treatment |
|
A range of mental health supports characterized by assertive engagement of the person, availability 24 hours a day, and support by an interdisciplinary team. |
|
|
10030 crisis intervention |
crisis support |
Response to stabilize a person exhibiting behavior that puts the person at risk of hospitalization or institutionalization. |
|
|
10040 behavior support |
behavior
analysis |
Services specifically to encourage positive behaviors and to decrease challenging behaviors, including a) assessment to identify antecedents to behaviors and b) development of a plan to improve behaviors. |
|
|
10050 peer specialist |
peer support |
Mental health support services provided by a trained and credentialed person with a mental illness. |
|
|
10060 counseling |
|
Individual or group therapy to develop coping skills or improve mental health function. |
|
|
10070 psychosocial rehabilitation |
|
Assistance to improve or restore function in ADLs, IADLs, and social or adaptive skills NOT identified in previous categories or services. |
|
|
10080 clinic services |
|
Services for individuals with chronic mental illness furnished in a clinic or based in a clinic NOT identified in previous categories or services. |
|
|
10090 other mental health and behavioral services |
|
Services NOT identified elsewhere in category 10 that support people in improving or maintaining mental or behavioral health. |
11 Other Health and Therapeutic Services |
|
|
|
Services NOT identified in previous categories that support people in improving or maintaining health or functional capacity. |
|
|
11010 health monitoring |
|
Ongoing monitoring of physical health status when monitoring is the primary purpose of the service. This service can include medication monitoring if other aspects of a person’s health also are monitored. |
|
|
11020 health assessment |
|
Assessment or evaluation of physical health status when the assessment is the primary purpose of the service. This service can include medication assessment if the assessment includes other health information. |
|
|
11030 medication assessment and/or management |
|
Assessment of medication administration and/or possible drug interactions—and/or oversight of ongoing medication administration—when the management of medications is the primary purpose of the service. |
|
|
11040 nutrition consultation |
|
Assistance to a person to help him or her plan and implement changes to nutritional intake. |
|
|
11050 physician services |
|
Services by a licensed physician. This service can include health assessment, medication assessment, and/or mental health assessment if other physician services are also provided. |
|
|
11060 prescription drugs |
|
Prescription drugs. |
|
|
11070 dental services |
|
Services by a licensed dentist. |
|
|
11080 occupational therapy |
|
Services by a licensed occupational therapist. |
|
|
11090 physical therapy |
|
Services by a licensed physical therapist. |
|
|
11100 speech, hearing, and language therapy |
|
Services by a licensed speech, hearing, and language therapist. This service includes services by a speech pathologist or a qualified audiologist. |
|
|
11110 respiratory therapy |
|
Services by a licensed respiratory therapist. |
|
|
11120 cognitive rehabilitative therapy |
|
Assistance to manage or restore cognitive function. |
|
|
11130 other therapies |
|
Therapeutic interventions to maintain or improve function NOT identified in previous categories or services. This service includes specialized interventions such as those using art, music, dance, or trained animals. |
12 Services Supporting Participant Direction |
|
|
|
Services that assist a person and/or his or her representative in managing participant-directed services, as identified in the Participant Direction of Services section of the 1915(c) waiver or 1915(i) State Plan Amendment application. |
|
|
12010 financial management services in support of participant direction |
|
Assistance to help a person and/or representative manage participant-directed services by a) performing financial tasks to facilitate the employment of staff; b) managing the disbursement of funds in a participant-directed budget; and/or c) performing fiscal accounting and making expenditure reports to the person, representative, and/or state authorities. |
|
|
12020 information and assistance in support of participant direction |
|
Training the person and/or representative in directing or managing services. Topics include: a) the person's rights and responsibilities in participant direction; b) recruiting and hiring staff; c) managing staff and solving problems regarding services; and d) managing a participant-directed budget. |
13 Participant Training |
|
|
|
Training provided to a participant when training the participant is the primary purpose of the service. Topics may include: a) specific treatment regimens, b) the person's disability or condition, and c) navigation of the service system. |
|
|
13010 participant training |
|
The same definition as category 13. |
14 Equipment, Technology, and Modifications |
|
|
|
Material goods to help a person improve or maintain function. |
|
1401 personal emergency response system (PERS) |
14010 personal emergency response system (PERS) |
|
Devices that enable participants to signal a response center to secure help in an emergency. This service can include installation, maintenance, and monthly response center fees. |
|
1402 home and/or vehicle accessibility adaptations |
14020 home and/or vehicle accessibility adaptations |
home and/or vehicle modifications |
Physical changes to a private residence, automobile, or van, to accommodate the participant or improve his or her function. |
|
1403 equipment, technology, and supplies |
|
|
The purchase or rent of items, devices, product systems, and/or disposable medical supplies. |
|
|
14031 equipment and technology |
assistive technologyspecialized medical equipment |
The purchase or rent of items, devices, or product systems to increase or maintain a person's functional status. This service can include designing, fitting, adapting, and maintaining equipment, as well as training or technical assistance to use equipment. |
|
|
14032 supplies |
|
The purchase of disposable medical supplies, including nutritional supplements. |
15 Non-Medical Transportation |
|
|
|
Transportation not provided as part of another service such as a round-the-clock service or a day service. This service may include: a) transportation to and from other HCBS services; b) transportation to community activities where HCBS services are not provided; and/or c) the purchase of public transit tokens or passes. |
|
|
15010 non-medical transportation |
|
Same definition as category 15. |
16 Community Transition Services |
|
|
|
Non-recurring set-up expenses for moving to a residence where the person is responsible for living expenses. |
|
|
16010 community transition services |
|
Same definition as category 16. |
17 Other Services |
|
|
|
Services NOT identified in previous categories. |
|
|
17010 goods and services |
Individually directed goods and services |
Services, equipment, or supplies in the person's support plan NOT otherwise provided in the Medicaid program. |
|
|
17020 interpreter |
|
Services provided by an individual to support communication by someone who has limited English proficiency or verbal skills, such as a sign language interpreter or communicator. |
|
|
17030 housing consultation |
|
Information and assistance to help a person identify and select housing. |
|
|
17990 other |
|
Services NOT identified in previous categories and services. |
Appendix C: Comprehensive Eligibility Crosswalk
MAS/BOE - INDIVIDUALS COVERED UNDER SEPARATE CHILDREN’S HEALTH INSURANCE PROGRAMS
(Separate-CHIP)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Children covered under a Title XXI separate CHIP) |
42 CFR 457.310, §2110 (b) of the Act. |
2 |
Legal immigrant children and pregnant women covered under a Title XXI separate CHIP |
§2107(e)(1) of the Act, P.L. 111-3. |
3
|
Children receiving dental-only coverage under a separate CHIP |
§2102 and 2110 (b) of the Act, PL 111-3.
|
4 |
Targeted low-income pregnant women covered under a Title XXI separate CHIP |
§2112 of the Act, PL 111-3 |
5 |
Infants under age 1 born to targeted low-income pregnant women made eligible under a Title XXI separate CHIP |
§2112 of the Act, PL 111-3.
|
6 |
Children who have been granted presumptive eligibility under a Title XXI separate CHIP |
42 CFR 457.355, §2105 of the Act.
|
7 |
Pregnant women who have been granted presumptive eligibility under a Title XXI separate CHIP |
§2112 of the Act, PL 111-3.
|
8 |
Caretaker relatives and children covered under the authority of an 1115 waiver and a Title XXI separate CHIP |
§2107(e) of the Act. |
MAS/BOE - INDIVIDUALS RECEIVING CASH ASSISTANCE OR ELIGIBLE UNDER SECTION 1931 OF THE ACT-AGED
MSIS Coding (MAS-1, BOE-1)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Aged individuals receiving SSI, eligible spouses or persons receiving SSI pending a final determination of disposal of resources exceeding SSI dollar limits; and persons considered to be receiving SSI under §1619(b) of the Act. |
42 CFR 435.120, §1619(b) of the Act, §1902(a)(10)(A)(I)(II) of the Act, PL 99-643, §2. |
2 |
Aged individuals who meet more restrictive requirements than SSI and who are either receiving or not receiving SSI; or who qualify under §1619 of the Act. |
42 CFR 435.121, §1619(b)(3) of the Act, §1902(f) of the Act, PL 99-643, §7. |
3 |
Aged individuals receiving mandatory State supplements. |
42 CFR 435.130. |
4 |
Aged individuals who receive a State supplementary payment (but not SSI) based on need. |
42 CFR 435.230, §1902(a)(10)(A)(ii) of the Act. |
MAS/BOE - INDIVIDUALS RECEIVING CASH ASSISTANCE OR ELIGIBLE UNDER SECTION 1931 OF THE ACT - BLIND/DISABLED
MSIS Coding (MAS-1, BOE-2)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Blind and/or disabled individuals receiving SSI, eligible spouses or persons receiving SSI pending a final determination of blindness, disability, and/or disposal of resources exceeding SSI dollar limits; and persons considered to be receiving SSI under §1619(b) of the Act. |
42 CFR 435.120, §1619(b) of the Act, §1902(a)(10)(A)(I)(II) of the Act, PL 99-643, §2. |
2 |
Blind and/or disabled individuals who meet more restrictive requirements than SSI and who are either receiving or not receiving SSI; or who qualify under §1619. |
42 CFR 435.121, §1619(b)(3) of the Act, §1902(f) of the Act, PL 99-643, §7. |
3 |
Blind and/or disabled individuals receiving mandatory State supplements. |
42 CFR 435.130. |
4 |
Blind and/or disabled individuals who receive a State supplementary payment (but not SSI) based upon need. |
42 CFR 435.230, §1902(a)(10)(A)(ii)of the Act. |
MAS/BOE - INDIVIDUALS RECEIVING CASH ASSISTANCE OR ELIGIBLE UNDER SECTION 1931 OF THE ACT - CHILDREN
MSIS Coding (MAS-1, BOE-4)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Low Income Families with Children qualified under §1931 of the Act. |
42 CFR 435.110, §1902(a)(10)(A)(I)(I) of the Act, §1931 of the Act. |
2 |
Children age 18 who are regularly attending a secondary school or the equivalent of vocational or technical training. |
42 CFR 435.110, §1902(a)(10)(A)(I)(I). |
MAS/BOE - INDIVIDUALS RECEIVING CASH ASSISTANCE OR ELIGIBLE UNDER SECTION 1931 OF THE ACT - ADULTS
MSIS Coding (MAS-1, BOE-5)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Adults deemed essential for well-being of a recipient [see 45 CFR 233.20(a)(2)(vi)] qualified for Medicaid under §1931 of the Act. |
42 CFR 435.110, §1902(a)(10)(A)(I)(I)of the Act, §1931 of the Act. |
2 |
|
42 CFR 435.110, §1902(a)(10)(A)(I)(I)of the Act. |
MAS/BOE - INDIVIDUALS RECEIVING CASH ASSISTANCE OR ELIGIBLE UNDER SECTION 1931 -U CHILDREN
MSIS Coding (MAS-1, BOE-6) - (OPTIONAL)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Unemployed Parent Program - Cash assistance benefits to low income individuals in two parent families where the principle wage earner is employed fewer than 100 hours a month. |
42 CFR 435.110, §1902(a)(10)(A)(I)(I) of the Act, §1931 of the Act. |
2 |
Children age 18 who are regularly attending a secondary school or the equivalent of vocational or technical training. |
42 CFR 435.110, §1902(a)(10)(A)(I)(I) of the Act. |
MAS/BOE - INDIVIDUALS RECEIVING CASH ASSISTANCE OR ELIGIBLE UNDER SECTION 1931 - U ADULTS
MSIS Coding (MAS-1, BOE-7) - (OPTIONAL)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Adults deemed essential for well-being of a recipient (see 45 CFR 233.20(a)(2)(vi)) qualified under §1931 of the Act (Low Income Families with Children). |
42 CFR 435.110, §1902(a)(10)(A)(I)(I) of the Act, §1931 of the Act. |
2 |
|
42 CFR 435.110, §1902(a)(10)(A)(I)(I) of the Act. |
MAS/BOE - MEDICALLY NEEDY - AGED
MSIS Coding (MAS-2, BOE-1)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Aged individuals who would be ineligible if not enrolled in an HMO. Categorically needy individuals are covered under 42 CFR 435.212, and the same rules apply to medically needy individuals. |
42 CFR 435.326. |
2 |
Aged |
42 CFR 435.320, 42 CFR 435.330. |
MAS/BOE - MEDICALLY NEEDY - BLIND/DISABLED
MSIS Coding (MAS-2, BOE-2)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Blind and/or disabled individuals who would be ineligible if not enrolled in an HMO. Categorically needy individuals are covered under 42 CFR 435.212 and the same rules apply to medically needy individuals.
|
42 CFR 435.326. |
2 |
Blind/Disabled |
42 CFR 435.322, 42 CFR 435.324, 42 CFR 435.330. |
3 |
Blind and/or disabled individuals who meet all Medicaid requirements except current blindness and/or disability criteria, and have been continuously eligible since 12/73 under the State's requirements. |
42 CFR 435.340. |
MAS/BOE - MEDICALLY NEEDY - CHILDREN
MSIS Coding (MAS-2, BOE-4)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Individuals under age 18 who, but for income and resources, would be eligible. |
§1902(a)(10)(C)(ii)(I) of the Act, PL 97-248, §137. |
2 |
Infants under the age of 1 and who were born after 9/30/84 to and living in the household of medically needy women. |
§1902(e)(4) of the Act, PL 98-369, §2362. |
3 |
Other financially eligible individuals under age 18-21, as specified by the State. |
42 CFR 435.308. |
4 |
Children who would be ineligible if not enrolled in an HMO. Categorically needy individuals are covered under 42 CFR 435.212 and the same rules apply to medically needy individuals. |
42 CFR 435.326. |
MAS/BOE - MEDICALLY NEEDY - ADULTS
MSIS Coding (MAS-2, BOE-5)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Pregnant women. |
42 CFR 435.301. |
2 |
Caretaker relatives who, but for income and resources, would be eligible. |
42 CFR 435.310. |
3 |
Adults who would be ineligible if not enrolled in an HMO. Categorically needy individuals are covered under 42 CFR 435.212 and the same rules apply to medically needy individuals. |
42 CFR 435.326. |
MAS/BOE - POVERTY RELATED ELIGIBLES - AGED
MSIS Coding (MAS-3, BOE-1)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Qualified Medicare Beneficiaries (QMBs) who are entitled to Medicare Part A, whose income does not exceed 100% of the Federal poverty level, and whose resources do not exceed twice the SSI standard. |
§§1902(a)(10)(E)(I) and 1905(p)(1) of the Act, PL 100-203, §4118(p)(8), PL 100-360, §301(a) & (e), PL 100-485, §608(d)(14), PL 100-647, §8434. |
2 |
Specified Low-Income Medicare Beneficiaries (SLMBs) who meet all of the eligibility requirements for QMB status, except for the income in excess of the QMB income limit, but not exceeding 120% of the Federal poverty level. |
§4501(b) of OBRA 90, as amended in §1902(a)(10)(E) of the Act. |
3 |
Qualifying individuals having higher income than allowed for QMBs or SLMBs.
|
§1902(a)(10)(E)(iv) of the Act. |
4 |
Aged individual not described in S 1902(a)(10)(A)(1) of the Act, with income below the poverty level and resources within state limits, who are entitled to full Medicaid benefits. |
§1902(a)(10)(A)(ii)(X), 1902(m)(1) of the Act, PL 99-509, §§9402 (a) and (b). |
MAS/BOE - POVERTY RELATED ELIGIBLES - BLIND/DISABLED
MSIS Coding (MAS-3, BOE-2)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Qualified Medicare Beneficiaries (QMBs) who are entitled to Medicare Part A, whose income does not exceed 100% of the Federal poverty level, and whose resources do not exceed twice the SSI standard. |
§§1902(a)(10)(E)(I) and 1905(p)(1) of the Act, PL 100-203, §4118(p)(8), PL 100-360, §301(a) & (e), PL 100-485, §608(d)(14), PL 100-647, §8434. |
2 |
Specified Low-Income Medicare Beneficiaries (SLMBs) who meet all of the eligibility requirements for QMB status, except for the income in excess of the QMB income limit, but not exceeding 120% of the Federal poverty level. |
§4501(b) of OBRA 90 as amended in §1902(a)(10)(E)(I) of the Act. |
3 |
Qualifying individuals having higher income than allowed for QMBs or SLMBs. |
§1902(a)(10)(E)(iv) of the Act. |
4 |
Qualified Disabled Working Individuals (QDWIs) who are entitled to Medicare Part A. |
§§1902(a)(10)(E)(ii) and 1905(s) of the Act. |
5 |
Disabled individuals not described in §1902(a)(10)(A)(1) of the Act, with income below the poverty level and resources within state limits, which are entitled to full Medicaid benefits. |
§§1902(a)(10)(A)(ii)(X), 1902(m)(1) and (3) of the Act, P.L. 99-509, §§9402 (a) and (b). |
MAS/BOE - POVERTY RELATED ELIGIBLES - CHILDREN
MSIS Coding (MAS-3, BOE-4)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Infants and children up to age 6 with income at or below 133% of the Federal Poverty Level (FPL). |
§§1902(a)(10)(A)(I)(IV) & (VI), 1902(l)(1)(A), (B), & (C) of the Act, PL 100-360, §302(a)(1), PL 100-485, §608(d)(15). |
2 |
Children under age 19 (born after 9/30/83) whose income is at or below 100% of the Federal poverty level within the State's resource requirements. |
§1902(a)(10)(A)(I) (VII) of the Act. |
3 |
Infants under age 1 whose family income is below 185% of the poverty level and who are within any optional State resource requirements. |
§§1902(a)(10)(A)(ii) (IX) and 1902(l)(1)(D) of the Act, PL 99-509, §§9401(a) & (b), PL 100-203, §4101. |
4 |
Children made eligible under the more liberal income and resource requirements as authorized under §1902(r)(2) of the Act when used to disregard income on a poverty-level-related basis. |
§1902(r)(2) of the Act. |
5 |
Children made eligible by a Title XXI Medicaid expansion under the Child Health Insurance Program (CHIP) |
P.L. 105-100. |
MAS/BOE - POVERTY RELATED ELIGIBLES - ADULTS
MSIS Coding (MAS-3, BOE-5)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Pregnant women with incomes at or below 133% of the Federal Poverty Level. |
§1902(a)(10)(A)(I), (IV) and (VI); §1902(l)(1)(A), (B), & (C) of the Act, PL 100-360, §302(a)(1), PL 100-485, §608(d)(15). |
2 |
Women who are eligible until 60 days after their pregnancy, and whose incomes are below 185% of the FPL and have resources within any optional State resource requirements. |
§§1902(a)(10)(A)(ii)(IX) and 1902(l)(1)(D) of the Act, PL 99-509, §§9401(a) & (b), PL 100-203, §4101. |
3 |
Caretaker relatives and pregnant women made eligible under more liberal income and resource requirements of §1902(r)(2) of the Act when used to disregard income on a poverty-level related basis. |
§1902(r)(2) of the Act. |
4 |
Adults made eligible by a Title XXI Medicaid expansion under the Child Health Insurance Program (CHIP). |
Title XXI of the Social Security Act. |
MAS/BOE - POVERTY RELATED ELIGIBLES - ADULTS
MSIS Coding (MAS-3, BOE-A)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Women under age 65 who are found to have breast or cervical cancer, or have precancerous conditions. |
§1902(a)(10)(a)(ii)(XVIII), P.L. 106-354. |
MAS/BOE - OTHER ELIGIBLES - AGED
MSIS Coding (MAS-4, BOE-1)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Aged individuals who meet more restrictive requirements than SSI and who are either receiving or not receiving SSI; or who qualify under §1619 of the Act. |
42 CFR 435.121, §1619(b)(3) of the Act, §1902(f) of the Act, PL 99-643, §7. |
2 |
Aged individuals who are ineligible for optional State supplements or SSI due to requirements that do not apply under title XIX. |
42 CFR 435.122. |
3 |
Aged essential spouses considered continuously eligible since 12/73; and some spouses who share hospital or nursing facility rooms for 6 months or more. |
42 CFR 435.131. |
4 |
Institutionalized aged individuals who have been continuously eligible since 12/73 as inpatients or residents of Title XIX facilities. |
42 CFR 435.132. |
5 |
Aged individuals who would be SSI/SSP eligible except for the 8/72 increase in OASDI benefits. |
42 CFR 435.134. |
6 |
Aged individuals who would be eligible for SSI but for title II cost-of-living adjustment(s). |
42 CFR 435.135. |
7 |
Aged aliens who are not lawful, permanent residents or who do not have PRUCOL status, but who are otherwise qualified, and who require emergency care. |
PL 99-509, §9406. |
8 |
Aged individuals who would be eligible for AFDC, SSI, or an optional State supplement if not in a medical institution. |
42.CFR 435.211, §1902(a)(10)(A)(ii) and §1905(a) of the Act. |
9 |
Aged individuals who meet income and resource requirements for AFDC, SSI, or an optional State supplement. |
42 CFR 435.210, §1902(a)(10)(A)(ii) and §1905 of the Act. |
10 |
Aged individuals who have become ineligible and who are enrolled in a qualified HMO or "§1903(m)(2)(G) entity" that has a risk contract. |
42 CFR 435.212 §1902(e)(2), PL 99-272, §9517, PL 100-203, §4113(d). |
11 |
Aged individuals who, solely because of coverage under a home and community based waiver, are not in a medical institution, but who would be eligible if they were. |
42 CFR 435.217, §1902(a)(10)(A)(ii), (VI); 50 PL 100-13. |
12 |
Aged individuals who elect to receive hospice care who would be eligible if in a medical institution. |
§1902(a)(10)(A)(ii), (VII) of the Act, PL 99-272, §9505. |
13 |
Aged individuals in institutions who are eligible under a special income level specified in Supplement 1 to Attachment 2.6-A of the State's title XIX Plan. |
42 CFR 435.236, §1902(a)(10)(A)(ii) of the Act. |
MAS/BOE - OTHER ELIGIBLES - BLIND/DISABLED
MSIS Coding (MAS-4, BOE-2)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Blind and/or disabled individuals who meet more restrictive requirements than SSI, including both those receiving and not receiving SSI payments |
42 CFR 435.121, §1619(b)(3) of the Act, §1902(f) of the Act, PL 99-643, §7. |
2 |
Blind and/or disabled individuals who are ineligible for optional State supplements or SSI due to requirements that do not apply under title XIX. |
42 CFR 435.122. |
3 |
Blind and/or disabled essential spouses considered continuously eligible since 12/73; and some spouses who share hospital or nursing facility rooms for 6 months or more. |
42 CFR 435.131. |
4 |
Institutionalized blind and/or disabled individuals who have been continuously eligible since 12/73 as inpatients or residents of Title XIX facilities. |
42 CFR 435.132. |
5 |
Blind and/or disabled individuals who would be SSI/SSP, eligible except for the 8/72 increase in OASDI benefits. |
42 CFR 435.134. |
6 |
Blind and/or disabled individuals who would be eligible for SSI but for title II cost-of-living adjustment(s). |
42 CFR 435.135, §503 PL 94-566. |
7 |
Blind and/or disabled aliens who are not lawful, permanent residents or who do not have PRUCOL status, but who are otherwise qualified, and who require emergency care. |
PL 99-509, §9406. |
8 |
Blind and/or disabled individuals who meet all Medicaid requirements except current blindness, or disability criteria, who have been continuously eligible since 12/73 under the State's 12/73 requirements. |
42 CFR 435.133. |
9 |
Blind and/or disabled individuals, age 18 or older, who became blind or disabled before age 22 and who lost SSI or State supplementary payments eligibility because of an increase in their OASDI (childhood disability) benefits. |
§1634(c) of the Act; PL 99-643, §6. |
10 |
Blind and/or disabled individuals who would be eligible for AFDC, SSI, or an optional State supplement if not in a medical institution. |
42 CFR 435.211, §§1902(a)(10)(A)(ii) and 1905(a) of the Act. |
11 |
Qualified severely impaired blind or disabled individuals under age 65, who, except for earnings, are eligible for SSI. |
§§1902(a)(10)(A)(I)(II) and 1905(q) of the Act, PL 99-509, §9404 and §1619(b)(8) of the Act, PL 99-643, §7 |
12 |
Blind and/or disabled individuals who meet income and resource requirements for AFDC, SSI, or an optional State supplement. |
42 CFR 435.210, §§1902(a)(10)(A)(ii) and 1905 of the Act. |
13 |
Working disabled individuals who buy-in to Medicaid |
§1902(a)(10)(A)(ii)(XIII). |
14 |
Blind and/or disabled individuals who have become ineligible who are enrolled in a qualified HMO or "§1903(m)(2)(G) entity" that has a risk contract. |
42 CFR 435.212 §1902(e)(2) of the Act; PL 99-272, §9517; PL 100-203, §4113(d). |
15 |
Blind and/or disabled individuals who, solely because of coverage under a home and community based waiver, are not in a medical institution and who would be eligible if they were. |
42 CFR 435.217, §1902(a)(10)(A)(ii)(VI) of the Act, 50 PL 100-13. |
16 |
Blind and/or disabled individuals who elect to receive hospice care, and who would be eligible if in a medical institution. |
§1902(a)(10)(A)(ii)(VII), PL 99-272, §9505 |
17 |
Blind and/or disabled individuals in institutions who are eligible under a special income level specified in Supplement 1 to Attachment 2.6-A of the State's title XIX Plan. |
42 CFR 435.231. §1902(a)(10)(A)(ii) of the Act. |
18 |
Blind and/or disabled widows and widowers who have lost SSI/SSP benefits but are considered eligible for Medicaid until they become entitled to Medicare Part A. |
§1634 of the Act, PL 101-508, §5103. |
19 |
Certain Disabled children, 18 or under, who live at home, but who, if in a medical institution, would be eligible for SSI or a State supplemental payment. |
42 CFR 435.225; §1902(e)(3) of the Act. |
20 |
Continuation of Medicaid eligibility for disabled children who lose SSI benefits because of changes in the definition of disability. |
§1902(a)(10)(A)(ii) of the Act; P.L. 15-32, §491. |
21 |
Disabled individuals with medically improved disabilities made eligible under the Ticket to Work and Work Incentives Improvement Act (TWWIIA) of 1999. |
§1902(a)(10)(A)(ii)(XV) of the Act. |
MAS/BOE - OTHER ELIGIBLES - CHILDREN
MSIS Coding (MAS-4, BOE-4)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Children of families receiving up to 12 months of extended Medicaid benefits (for those eligible after 4/1/90). |
§1925 of the Act, PL 100-485, §303. |
2 |
"Qualified children" under age 19 born after 9/30/83 or at an earlier date at State option, who meet the State's AFDC income and resource requirements. |
§§1902(a)(10)(A)(I)(III) and 1905(n) of the Act, PL 98-369, §2361, PL 99-272, §9511, PL 100-203, §4101. |
3 |
Children of individuals who are ineligible for AFDC-related Medicaid because of requirements that do not apply under title XIX.
|
42 CFR 435.113. |
4 |
Children of individuals who would be eligible for Medicaid under §1931 of the Act (Low income families with children) except for the 7/1/72 (PL 92-325) OASDI increase and were entitled to OASDI and received cash assistance in 8/72. |
42 CFR 435.114. |
5 |
Children whose mothers were eligible for Medicaid at the time of childbirth, and are deemed eligible for one year from birth as long as the mother remained eligible, or would have if pregnant, and the child remains in the same household as the mother. |
42 CFR 435.117, §1902(e)(4) of the Act, PL 98-369, §2362. |
6 |
Children of aliens who are not lawful, permanent residents or who do not have PRUCOL status, but who are otherwise qualified, and who require emergency care. |
PL 99-509, §9406. |
7 |
Children who meet income and resource requirements for AFDC, SSI, or an optional State supplement |
42 CFR 435.210, §1902(a)(10)(A)(ii) and §1905 of the Act. |
8 |
Children who would be eligible for AFDC, SSI, or an optional State supplement if not in a medical institution. |
42 CFR 435.211, §1902(a)(10)(A)(ii) and §1905(a) of the Act. |
9 |
Children who have become ineligible who are enrolled in a qualified HMO or "§1903(m)(2)(G) entity" that has a risk contract. |
42 CFR 435.212, §1902(e)(2) of the Act, PL 99-272, §9517, PL 100-203, §4113(d). |
10 |
Children of individuals who elect to receive hospice care, and who would be eligible if in a medical institution. |
§1902(a)(10)(A)(ii)(VII), PL 99-272, §9505. |
11 |
Children who would be eligible for AFDC if work-related child care costs were paid from earnings rather than received as a State service. |
42 CFR 435.220. |
12 |
Children of individuals who would be eligible for AFDC if the State used the broadest allowable AFDC criteria. |
42 CFR 435.223, §§1902(a)(10)(A)(ii) and 1905(a) of the Act. |
13 |
Children who solely because of coverage under a home and community based waiver, are not in a medical institution, but who would be eligible if they were. |
42 CFR 435.217, §1902(a)(10)(A)(ii)(VI) of the Act. |
14 |
Children not described in §1902(a)(10)(A)(I) of the Act, "Ribikoff Kids", who meet AFDC income and resource requirements, and are under a State-established age (18-21). |
§§1902(a)(10)(A)(ii) and 1905(a)(I) of the Act, PL 97-248, §137. |
MAS/BOE - OTHER ELIGIBLES - ADULTS
MSIS Coding (MAS-4, BOE-5)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Families receiving up to 12 months of extended Medicaid benefits (if eligible on or after 4/1/90). |
§1925 of the Act, PL 100-485, §303. |
2 |
Qualified pregnant women whose pregnancies have been medically verified and who meet the State's AFDC income and resource requirements. |
§§1902(a)(10)(A)(I)(III) and 1905(n) of the Act, PL 98-369, §2361, PL 99-272, §9511, PL 100-203 §4101. |
3 |
Adults who are ineligible for AFDC-related Medicaid because of requirements that do not apply under title XIX. |
42 CFR 435.113. |
4 |
Adults who would be eligible for Medicaid under §1931 of the Act (Low income families with children) except for the 7/1/72 (PL 92-325) OASDI increase; and were entitled to OASDI and received cash assistance in 8/72. |
42 CFR 435.114. |
5 |
Women who were eligible while pregnant, and are eligible for family planning and pregnancy related services until the end of the month in which the 60th day occurs after the pregnancy |
§1902(e)(5) of the Act, PL 98-369, PL 100-203, §4101, PL 100-360, §302(e). |
6 |
Adult aliens who are not lawful, permanent residents or who do not have PRUCOL status, but who are otherwise qualified, and who require emergency care. |
PL 99-509, §9406. |
7 |
Adults who meet the income and resource requirements for AFDC, SSI, or an optional State Supplement. |
42 CFR 435.210, §§1902(a)(10)(A)(ii) and 1905 of the Act. |
8 |
Adults who would be eligible for AFDC, SSI, or an optional State Supplement if not in a medical institution. |
42 CFR 435.211, §§1902(a)(10)(A)(ii) and 1905(a) of the Act. |
9 |
Adults who have become ineligible who are enrolled in a qualified HMO or "§1903(m)(2)(G) entity" that has a risk contract. |
42 CFR 435.212, §1902(e)(2)(A) of the Act, PL 99-272, §9517, PL 100-203, §4113(d). |
10 |
Adults who solely because of coverage under a home and community based waiver, are not in a medical institution, but who would be eligible if they were. |
42 CFR 435.217, §1902(a)(10)(A)(ii)(VI) of the Act. |
11 |
Adults who elect to receive hospice care, and who would be eligible if in a medical institution. |
§1902(a)(10)(A)(ii), (VII); PL 99-272, §9505. |
12 |
Adults who would be eligible for AFDC if work-related child care costs were paid from earnings rather than received as a State service. |
42 CFR 435.220. |
13 |
Pregnant women who have been granted presumptive eligibility. |
§§1902(a)(47) and 1920 of the Act, PL 99-509, §9407. |
14 |
Adults who would be eligible for AFDC if the State used the broadest allowable AFDC criteria. |
42 CFR 435.223, §§1902(a)(10)(A)(ii) and 1905(a) of the Act. |
MAS/BOE - OTHER ELIGIBLES - FOSTER CARE CHILDREN
MSIS Coding (MAS-4, BOE-8)
ITEM |
DESCRIPTION |
CFR/PL CITATIONS |
1 |
Children for whom the State makes adoption assistance or foster care maintenance payments under Title IV-E. |
42 CFR 435.145, §1902(a)(10)(A)(i)(I) of the Act. |
2 |
Children with special needs covered by State foster care payments or under a State adoption assistance agreement which does not involve Title IV-E. |
§1902(a)(10)(A)(ii) (VIII) of the Act, PL 99-272, §9529. |
3 |
Children leave foster care due to age. |
Foster Care Independence Act of 1999. |
MAS/BOE - SECTION 1115 DEMONSTRATION MEDICAID EXPANSION
MSIS Coding (MAS-5, BOE-1)
ITEM |
DESCRIPTION |
CFR/PL CITATION |
1 |
Aged individuals made eligible under the authority of a §1115 waiver due to poverty-level related eligibility expansions. |
§1115(a)(1), (a)(2) & (b)(1) of the Act, §1902(a)(10), and §1903(m) of the Act. |
MAS/BOE - SECTION 1115 DEMONSTRATION MEDICAID EXPANSION
MSIS Coding (MAS-5, BOE-2)
ITEM |
DESCRIPTION |
CFR/PL CITATION |
1 |
Blind and/or disabled individuals made eligible under the authority of a §1115 waiver due to poverty-level-related eligibility |
§1115(a)(1), (a)(2) & (b)(1) of the Act, §1902(a)(10), and §1903(m) of the Act. |
MAS/BOE - SECTION 1115 DEMONSTRATION MEDICAID EXPANSION
MSIS Coding (MAS-5, BOE-4)
ITEM |
DESCRIPTION |
CFR/PL CITATION |
1 |
Children made eligible under the authority of a §1115 waiver due to poverty-level-related eligibility expansions. |
§1115(a)(1), (a)(2) & (b)(1) of the Act, §1902(a)(10), and §1903(m) of the Act. |
MAS/BOE - SECTION 1115 DEMONSTRATION MEDICAID EXPANSION
MSIS Coding (MAS-5, BOE-5)
ITEM |
DESCRIPTION |
CFR/PL CITATION |
1 |
Caretaker relatives, pregnant women and/or adults without dependent children made eligible under the authority of at §1115 waiver due to poverty-level-related eligibility expansions. |
§1115(a)(1) and (a)(2) of the Act, §1902(a)(10), §1903(m). |
Appendix D: Types of Service (TOS) Reference
Definitions of Types of Service
The following definitions are adaptations of those given in the Code of Federal Regulations. These definitions, although abbreviated, are intended to facilitate the classification of medical care and services for reporting purposes. They do not modify any requirements of the Act or supersede in any way the definitions included in the Code of Federal Regulations (CFR).
Effective FY 1999, services provided under Family Planning, EPSDT, Rural Health Clinics, FQHC’s, and Home-and-Community-Based Waiver programs will be coded according to the types of services listed below. Specific programs with which these services are associated will be identified using the program type coding as defined in Attachment 5.
1. Unduplicated Total.--Report the unduplicated total of recipients by maintenance assistance status (MAS) and by basis of eligibility (BOE). A recipient receiving more than one type of service is reported only once in the unduplicated total.
2. Inpatient Hospital Services (TOS Code=001)(See 42 CFR 440.10; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--These are services that are:
o Ordinarily furnished in a hospital for the care and treatment of inpatients;
o Furnished under the direction of a physician or dentist (except in the case of nurse‑midwife services per 42 CFR 440.165); and
o Furnished in an institution that:
- Is maintained primarily for the care and treatment of patients with disorders other than mental health conditions;
- Is licensed or formally approved as a hospital by an officially designated authority for State standard setting;
- Meets the requirements for participation in Medicare (except in the case of medical supervision of nurse‑midwife services per 42 CFR 440.165); and
- Has in effect a utilization review plan applicable to all Medicaid patients that meets the requirements in 42 CFR 482.30 unless a waiver has been granted by the Secretary of Health and Human Services.
Inpatient hospital services do not include nursing facility services furnished by a hospital with swing‑bed approval. However, include services provided in a psychiatric wing of a general hospital if the psychiatric wing is not administratively separated from the general hospital.
3. Mental Health Facility Services (See 42 CFR 440.140, 440.160, and 435.1009).--An institution for mental health conditions is a hospital, nursing facility, or other institution that is primarily engaged in providing diagnosis, treatment or care of individuals with mental health conditions, including medical care, nursing care, and related services. Report totals for services defined under 3a and 3b.
3a. Inpatient Psychiatric Facility Services for Individuals Age 21 and Under (TOS Code=048)(See 42 CFR 440.160; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450). --These are services that:
o Are provided under the direction of a physician;
o Are provided in a psychiatric facility or inpatient program accredited by the Joint Commission on the Accreditation of Hospitals; and,
o Meet the requirements set forth in 42 CFR Part 441, Subpart D (inpatient psychiatric services for individuals age 21 and under in psychiatric facilities or programs).
3b. Other Mental Health Facility Services (Individuals Age 65 or Older) (TOS Code= 044 and 045)(See 42 CFR 440.140).--These are services provided under the direction of a physician for the care and treatment of recipients in an institution for mental health conditions that meets the requirements specified in 42 CFR 440.140.
4. Nursing Facilities (NF) Services(TOS Code=009 and 047)(See 42 CFR 440.40 and 440.155).--These are services provided in an institution (or a distinct part of an institution) which:
o Is primarily engaged in providing to residents:
- Skilled nursing care and related services for residents who require medical or nursing care;
- Rehabilitation services for the rehabilitation of injured, disabled, or sick persons, or
- On a regular basis, health-related care and services to individuals who, because of their mental or physical condition, require care and services (above the level of room and board) which can be made available to them only through institutional facilities, and is not primarily for the care and treatment of mental health conditions; and;
o Meet the requirements for a nursing facility described in subsections 1919(b), (c), and (d) of the Act regarding:
- Requirements relating to provision of services;
- Requirements relating to residents’ rights; and
- Requirements relating to administration and other matters.
NOTE: ICF Services - All Other.--This is combined with nursing facility services.
5. ICF Services for the Intellectually Disabled (TOS Code=046) (See 42 CFR 440.150).--These are services provided in an institution for individuals with intellectual disabilities persons or persons with related conditions if the:
o Primary purpose of the institution is to provide health or rehabilitative services to such individuals;
o Institution meets the requirements in 42 CFR 442, Subpart C (certification of ICF/IID); and
o The individuals with intellectual disabilities recipients for whom payment is requested are receiving active treatment as defined in 42 CFR 483.440(a).
Physicians' Services (TOS Code=012)(See 42 CFR 440.50; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--Whether furnished in a physician's office, a recipient's home, a hospital, a NF, or elsewhere, these are services provided:
o Within the scope of practice of medicine or osteopathy as defined by State law; and
o By, or under, the personal supervision of an individual licensed under State law to practice medicine or osteopathy, or dental medicine or dental surgery if State law allows such services to be provided by either a physician or dentist.
7. Outpatient Hospital Services (TOS Codes=002)(See 42 CFR 440.20; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--These are preventive, diagnostic, therapeutic, rehabilitative, or palliative services that are furnished:
o To outpatients;
o Except in the case of nurse-midwife services (see 42 CFR 440.165), under the direction of a physician or dentist; and
o By an institution that:
- Is licensed or formally approved as a hospital by an officially designated authority for State standard setting; and
- Except in the case of medical supervision of nurse midwife services (see 42 CFR 440.165), meets the requirements for participation in Medicare as a hospital.
8. Prescribed Drugs (TOS Code=033)(See 42 CFR 440.120; 42 CFR § 457.402; 42 CFR § 457.410; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--These are simple or compound substances or mixtures of substances prescribed for the cure, mitigation, or prevention of disease or for health maintenance that are:
o Prescribed by a physician or other licensed practitioner within the scope of professional practice as defined and limited by Federal and State law;
o Dispensed by licensed pharmacists and licensed authorized practitioners in accordance with the State Medical Practice Act; and
o Dispensed by the licensed pharmacist or practitioner on a written prescription that is recorded and maintained in the pharmacist's or practitioner's records.
9. Dental Services (TOS Code=029)(See 42 CFR 440.100; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--These are diagnostic, preventive, or corrective procedures provided by or under the supervision of a dentist in the practice of his or her profession, including treatment of:
o The teeth and associated structures of the oral cavity; and
o Disease, injury, or an impairment that may affect the oral or general health of the recipient.
A dentist is an individual licensed to practice dentistry or dental surgery. Dental services include dental screening and dental clinic services.
NOTE: Include services related to providing and fitting dentures as dental services. Dentures mean artificial structures made by, or under the direction of, a dentist to replace a full or partial set of teeth.
Dental services do not include services provided as part of inpatient hospital, outpatient hospital, non-dental clinic, or laboratory services and billed by the hospital, non‑dental clinic, or laboratory or services which meet the requirements of 42 CFR 440.50(b) (i.e., are provided by a dentist but may be provided by either a dentist or physician under State law).
10. Other Licensed Practitioners' Services (TOS Code=015)(See 42 CFR 440.60; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--These are medical or remedial care or services, other than physician services or services of a dentist, provided by licensed practitioners within the scope of practice as defined under State law. The category “Other Licensed Practitioners' Services” is different than the “Other Care” category. Examples of other practitioners (if covered under State law) are:
o Chiropractors;
o Podiatrists;
o Psychologists; and
o Optometrists.
Other Licensed Practitioners' Services include hearing aids and eyeglasses only if they are billed directly by the professional practitioner. If billed by a physician, they are reported as Physicians' Services. Otherwise, report them under Other Care.
Other Licensed Practitioners' Services do not include prosthetic devices billed by physicians, laboratory or X-ray services provided by other practitioners, or services of other practitioners that are included in inpatient or outpatient hospital bills. These services are counted under the related type of service as appropriate. Devices billed by providers not included under the listed types of service are counted under Other Care.
Report Other Licensed Practitioners' Services that are billed by a hospital as inpatient or outpatient services, as appropriate.
Speech therapists, audiologists, opticians, physical therapists, and occupational therapists are not included within Other Licensed Practitioners' Services.
Chiropractors' services include only services that are provided by a chiropractor (who is licensed by the State) and consist of treatment by means of manual manipulation of the spine that the chiropractor is legally authorized by the State to perform.
11. Clinic Services (TOS Code=028(See 42 CRF 440.90; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--Clinic services include preventive, diagnostic, therapeutic, rehabilitative, or palliative items or services that are provided:
o To outpatients;
o By a facility that is not part of a hospital but is organized and operated to provide medical care to outpatients including services furnished outside the clinic by clinic personnel to individuals without a fixed home or mailing address. For reporting purposes, consider a group of physicians who share, only for mutual convenience, space, services of support staff, etc., as physicians, rather than a clinic, even though they practice under the name of the clinic; and
o Except in the case of nurse-midwife services (see 42 CFR 440.165), are furnished by, or under, the direction of a physician.
NOTE: Place dental clinic services under dental services. Report any services not included above under other care. A clinic staff may include practitioners with different specialties.
12. Laboratory and X‑Ray Services (TOS Code=005, 006, 007, and 008)(See 42 CFR 440.30; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--These are professional or technical laboratory and radiological services that are:
o Ordered and provided by or under the direction of a physician or other licensed practitioner of the healing arts within the scope of his or her practice as defined by State law or ordered and billed by a physician but provided by referral laboratory;
o Provided in an office or similar facility other than a hospital inpatient or outpatient department or clinic; and
o Provided by a laboratory that meets the requirements for participation in Medicare.
X-ray services provided by dentists are reported under dental services.
13. Sterilizations (TOS Code=084)(See 42 CFR 441, Subpart F).--These are medical procedures, treatment or operations for the purpose of rendering an individual permanently incapable of reproducing.
14. Home Health Services (TOS Code=016,017, 018, 019, 020, and 021) (See 42 CFR 440.70; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--These are services provided at the patient's place of residence, in compliance with a physician's written plan of care that is reviewed every 62 days. The following items and services are mandatory.
o Nursing services, as defined in the State Nurse Practice Act, that is provided on a part‑time or intermittent basis by a home health agency (a public or private agency or organization, or part of any agency or organization, that meets the requirements for participation in Medicare). If there is no agency in the area, a registered nurse who:
- Is licensed to practice in the State;
- Receives written orders from the patient's physician;
- Documents the care and services provided; and
- Has had orientation to acceptable clinical and administrative record keeping from a health department nurse;
o Home health aide services provided by a home health agency; and
o Medical supplies, equipment, and appliances suitable for use in the home.
The following therapy services are optional: physical therapy, occupational therapy, or speech pathology and audiology services provided by a home health agency or by a facility licensed by the State to provide these medical rehabilitation services. (See 42 CFR 441.15.)
Place of residence is normally interpreted to mean the patient's home and does not apply to hospitals or NFs. Services received in a NF that are different from those normally provided as part of the institution's care may qualify as home health services. For example, a registered nurse may provide short‑term care for a recipient in a NF during an acute illness to avoid the recipient's transfer to another NF.
15. Personal Support Services.--Report total unduplicated recipients and payments for services defined in 15a through 15i.
15a. Personal Care Services (TOS Code=051)(See 42 CFR 440.167).--These are services furnished to an individual who is not an inpatient or resident of a hospital, nursing facility, intermediate care facility for individuals with intellectual disabilities, or institution for mental health conditions that are:
o Authorized for the individual by a physician in accordance with a plan of treatment or (at the option of the State) otherwise authorized for the individual in accordance with a service plan approved by the State; and
o Provided by an individual who is qualified to provide such services and who is not a member of the individual’s family.
15b. Targeted Case Management Services (TOS Code=053)(See 42 CFR § 440.169; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--These are services that are furnished to individuals eligible under the plan to gain access to needed medical, social, educational, and other services. The agency may make available case management services to:
o Specific geographic areas within a State, without regard to statewide requirement in 42 CFR 431.50; and
o Specific groups of individuals eligible for Medicaid, without regard to the comparability requirements in 42 CFR 440.240.
The agency must permit individuals to freely choose any qualified Medicaid provider except when obtaining case management services in accordance with 42 CFR 431.51.
15c. Rehabilitative Services (TOS Code=043)(See 42 CFR 440.130).--These include any medical or remedial services recommended by a physician or other licensed practitioner of the healing arts within the scope of his/her practice under State law for maximum reduction of physical or mental health condition and restoration of a recipient to his/her best possible functional level.
15d. Physical Therapy, Occupational Therapy, and Services For Individuals With Speech, Hearing, and Language Disorders (TOS Codes=030, 031, and 032)(See 42 CFR 440.110; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--These are services prescribed by a physician or other licensed practitioner within the scope of his or her practice under State law and provided to a recipient by, or under the direction of, a qualified physical therapist, occupational therapist, speech pathologist, or audiologist. It includes any necessary supplies and equipment.
15e. Hospice Services (TOS Code=087)(See 42 CFR 418.202; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--Whether received in a hospice facility or elsewhere, these are services that are:
o Furnished to a terminally ill individual, as defined in 42 CFR 418.3;
o Furnished by a hospice, as defined in 42 CFR 418.3, that meets the requirements for participation in Medicare specified in 42 CFR 418, Subpart C or by others under an arrangement made by a hospice program that meets those requirements and is a participating Medicaid provider; and
o Furnished under a written plan that is established and periodically reviewed by:
The attending physician;
The medical director or physician designee of the program, as described in 42 CFR 418.54; and
- The interdisciplinary group described in 42 CFR 418.68.
15f. Nurse Midwife (TOS Code=025)(See 42 CFR 440.165; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--These are services that are concerned with management and the care of mothers and newborns throughout the maternity cycle and are furnished within the scope of practice authorized by State law or regulation.
15g. Nurse Practitioner (TOS Code=026)(See 42 CFR 440.166; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--These are services furnished by a registered professional nurse who meets State’s advanced educational and clinical practice requirements, if any, beyond the 2 to 4 years of basic nursing education required of all registered nurses.
15h. Private Duty Nursing (TOS Code=022)(See 42 CFR 440.80; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--When covered in the State plan, these are services of registered nurses or licensed practical nurses provided under direction of a physician to recipients in their own homes, hospitals or nursing facilities (as specified by the State).
15i. Religious Non-Medical Health Care Institutions (TOS Code=058)(See 42 CFR 440.170).--These are non-medical health care services equivalent to a hospital or extended care level of care provided in facilities that meet the requirements of Section 1861(ss)(1) of the Act.
16. Other Care (See 42 CFR 440.120(b), (c), and (d), and 440.170(a)).--Report total unduplicated recipients and payments for services in sections 16a, 16b, and 16c. Such services do not meet the definition of, and are not classified under, any of the previously described categories.
16a. Transportation (TOS Code=056)(See 42 CFR 440.170; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--Report totals for services provided under this title to include transportation and other related travel services determined necessary by you to secure medical examinations and treatment for a recipient.
NOTE: Transportation, as defined above, is furnished only by a provider to whom a direct vendor payment can appropriately be made. If other arrangements are made to assure transportation under 42 CFR 431.53, FFP is available as an administrative cost.
16b. Other Pregnancy-related Procedures (TOS Code=086)(See 42 CFR 441, Subpart E; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450).--In accordance with the terms of the DHHS Appropriations Bill and 42 CFR 441, Subpart E, FFP is available for other pregnancy-related procedures:
o When a physician has certified in writing to the Medicaid agency that, on the basis of his or her professional judgment, the life of the mother would be endangered if the fetus were carried to term; or
o When the other pregnancy-related procedure is performed to terminate a pregnancy resulting from an act of rape or incest. FFP is not available for the other pregnancy-related procedure under any other circumstances.
16c. Other Services (TOS Code= 035, 036, 037, 062, 063, 064, 065, 066, 067, 068, 069, 073, 074, 075, 076, 077, 078, 079, 080, 081, 082, 083).--These services do not meet the definitions of any of the previously described service categories. They may include, but are not limited to:
o Prosthetic devices (see 42 CFR 440.120; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450) which are replacement, corrective, or supportive devices prescribed by a physician or other licensed practitioner of the healing arts within the scope of practice as defined by State law to:
- Artificially replace a missing portion of the body;
- Prevent or correct physical deformity or malfunctions; or
- Support a weak or deformed portion of the body.
o Eyeglasses (see 42 CFR 440.120; 42 CFR § 457.402; 42 CFR § 457.420; 42 CFR § 457.430; 42 CFR § 457.431; 457.440; 42 CFR § 457.450). Eyeglasses mean lenses, including frames, and other aids to vision prescribed by a physician skilled in diseases of the eye or an optician. It includes optician fees for services.
o Home and Community‑Based Waiver services (See §1915(c) of the Act and 42 CFR 440.180) that cannot be associated with other TYPE-OF-SERVICE codes (e.g., community homes for the disabled and adult day care.)
17. Capitated Care (See 42 CFR Part 434).--This includes enrollees and capitated payments for the plan types defined in 17 a and b below. Report unduplicated enrolled eligibles and payments for 17 a and b.
17a. Health Maintenance Organization (HMO) and Health Insuring Organization (HIO) (TOS Code=119).--These include plans contracted to provide capitated comprehensive services. An HMO is a public or private organization that contracts on a prepaid capitated risk basis to provide a comprehensive set of services and is federally qualified or State-plan defined. An HIO is an entity that provides for or arranges for the provision of care and contracts on a prepaid capitated risk basis to provide a comprehensive set of services.
17b. Prepaid Health Plans (PHP) (TOS Code=122).--These include plans that are contracted to provide less than comprehensive services. Under a non-risk or risk arrangement, the State may contract with (but not limited to these entities) a physician, physician group, or clinic for a limited range of services under capitation. A PHP is an entity that provides a non-comprehensive set of services on either capitated risk or non-risk basis or the entity provides comprehensive services on a non-risk basis.
NOTE: Include dental, mental health, and other plans covering limited services under PHP.
18. Primary Care Case Management (PCCM) (TOS Code=120)(See §1915(b)(1) of the Act).--The State contracts directly with primary care providers who agree to be responsible for the provision and/or coordination of medical services to Medicaid recipients under their care. Currently, most PCCM programs pay the primary care physician a monthly case management fee. Report these recipients and associated PCCM fees in this section.
NOTE: Where the fee includes services beyond case management, report the enrollees and fees under prepaid health plans (17b).
Appendix E: Program Type Reference
The following definitions describe special Medicaid/CHIP programs that are coded independently of type of service for MSIS purposes. These programs tend to cover bands of services that cut across many types of service.
Program Type 01. Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) (See 42 CFR 440.40(b)).--This includes either general health screening services and vision, dental, and hearing services furnished to Medicaid eligibles under age 21 to fulfill the requirements of the EPSDT program or services rendered based on referrals from EPSDT visits. The Act specifies two sets of EPSDT screenings:
o Periodic screenings, which are provided at distinct intervals determined by the State, and which must include the following services:
- A comprehensive health and developmental history assessment (including assessment of both physical and mental health development);
- A comprehensive unclothed physical exam;
- Appropriate immunizations according to the Advisory Committee on Immunization Practices schedule;
- Laboratory tests (including blood lead level assessment); and
- Health education (including anticipatory guidance); and
o Interperiodic screenings, which are provided when medically necessary to determine the existence of suspected physical or mental illness or conditions.
Program Type 02. Family Planning (See 42 CFR 440.40(c)).-- Only items and procedures clearly provided or performed for family planning purposes and matched at the 90 percent FFP rate should be included as Family Planning. Services covered under this program include, but are not limited to:
o Counseling and patient education and treatment furnished by medical professionals in accordance with State law;
o Laboratory and X-ray services;
o Medically approved methods, procedures, pharmaceutical supplies, and devices to prevent conception;
o Natural family planning methods; and
o Diagnosis and treatment for infertility.
NOTE: CMS’s Revised Financial Management Review Guide for Family Planning Services describes items and procedures eligible for the enhanced match as family planning services.
Program Type 03. Rural Health Clinics (RHC)(See 42 CFR 440.20(b)).--These include services (as allowed by State law) furnished by a rural health clinic which has been certified in accordance with the conditions of 42 CFR Part 491 (certification of certain health facilities). Services performed in RHCs include, but are not limited to:
o Services furnished by a physician within the scope of his or her profession as defined by State law. The physician performs these services in or away from the clinic and has an agreement with the clinic providing that he or she will be paid for these services;
o Services furnished by a physician assistant, nurse practitioner, nurse midwife, or other specialized nurse practitioner (as defined in 42 CFR 405.2401 and 491.2) if the services are furnished in accordance with the requirements specified in 42 CFR 405.2412(a);
o Services and supplies provided in conjunction with professional services furnished by a physician, physician assistant, nurse practitioner, nurse midwife, or specialized nurse practitioner. (See 42 CFR 405.2413 and 405.2415 for the criteria determining whether services and supplies are included here.); or
o Part‑time or intermittent visiting nurse care and related medical supplies (other than drugs and biologicals) if:
- The clinic is located in an area in which the Secretary has determined that there is a shortage of home health agencies (see 42 CFR 405.2417);
- The services are furnished by a registered nurse or licensed practical or vocational nurse employed, or otherwise compensated for the services, by the clinic;
- The services are furnished under a written plan of treatment that is either established and reviewed at least every 60 days by a supervising physician of the clinic, or that is established by a physician, physician's assistant, nurse practitioner, nurse midwife, or specialized nurse practitioner and reviewed and approved at least every 60 days by a supervising physician of the clinic; and
- The services are furnished to a homebound patient. For purposes of visiting nurse services, a homebound recipient means one who is permanently or temporarily confined to a place of residence because of a medical or health condition and leaves the place of residence infrequently. For this purpose, a place of residence does not include a hospital or nursing facility.
Program Type 04. Federally Qualified Health Center (FQHC) (See §1905(a)(2) of the Act).--FQHCs are facilities or programs more commonly known as community health centers, migrant health centers, and health care for the homeless programs. A facility or program qualifies as a FQHC providing services covered under Medicaid if:
o They receive grants under §§329, 330, or 340 of the Public Health Service Act (PHS);
o The Health Resources and Services Administration, PHS, certifies the center as meeting FQHC requirements; or
o The Secretary determines that the center qualifies through waiver of the requirements.
Services performed in FHQCs are defined the same as the services provided by rural health clinics. They may include physician services, services provided by physician assistants, nurse practitioners, clinical psychologists, clinical social workers, and services and supplies incident to such services as are otherwise covered if furnished by a physician or as incident to a physician's services. In certain cases, services to a homebound Medicaid patient may be provided. Any other ambulatory service included in the State's Medicaid plan is considered covered by a FQHC program if the center offers it.
Program Type 05. Indian Health Services (See §1911 of the Act) (See 42 CFR 431.110).--These are services provided by the Indian Health Services (IHS), an agency charged with providing the primary source of health care for American Indian and Alaska Native people who are members of federally recognized tribes and organizations. A State plan must provide that an IHS facility, meeting State plan requirements for Medicaid participants, must be accepted as a Medicaid provider on the same basis as any other qualified provider.
Program Type 06. Home and Community-Based Services for Disabled and Elderly (See §1929 of the Act) and for Individuals Age 65 and Older(MSIS (See 42 CFR 441, Subpart H).--This program is for §1915(d) recipients of home and community-based services for individuals age 65 or older. This is an option within the Medicaid program to provide home and community-based care to functionally disabled individuals age 65 or older who are otherwise eligible for Medicaid or for non-disabled elderly individuals.
Program Type 07. Home and Community Based Waivers (See §1915(c) of the Act and 42 CFR 440.180).--This program includes services furnished under a waiver approved under the provisions in 42 CFR Part 441, Subpart G (home and community-based services; waiver requirements).
Program Type 08. Money Follows Patient (MFP) service package (established by Section 6071 of Deficit Reduction Act of 2005 [Public Law 109-171] and extended by Section 2403 off the Patient Protection and Affordable Care Act of 2010 [Public Law 111-148]) helps States rebalance their long-term care systems through the development of transition programs that move people with Medicaid from institutional-based long-term care to community-based long-term care. To qualify for MFP, Medicaid recipients need to have been in institutional care for at least 90 days, exclusive of Medicare-paid rehabilitation days. Upon the initial transition to community-based long-term care, MFP participants are eligible for MFP benefits for up to 365 days. At the conclusion of MFP eligibility, the person continues as a typical Medicaid beneficiary. While eligible for MFP benefits, the restricted benefits flag in the eligibility file should be set to value 08 whenever the beneficiary has a single day of MFP eligibility during the month.
Any service financed with MFP grant funds is considered an MFP service. MFP services are home- and community-based services (HCBS) financed with MFP grant funds. They can be 1915(c) waiver services or HCBS state plan services. The program has three classes of HCBS, including qualified HCBS (HCBS that the person would have been eligible for regardless of participation in MFP), demonstration HCBS (HCBS that are above and beyond what they would have qualified for as a regular Medicaid beneficiary), and supplemental services (which are typically one-time services someone needs to make the transition to community-based long-term care). States received enhanced matching funds for the qualified and demonstration services, and their regular mating rate for the supplemental services. Examples of MFP-financed services include, but are not limited to:
1915(c) waiver services
Personal care assistance services provided through the state plan
Behavioral health services, including psychosocial rehabilitation
Program Type 10. Balancing Incentive Payments (BIP). The Balancing Incentive Program authorizes grants to States to increase access to non-institutional long-term services and supports (LTSS) as of October 1, 2011.
The Balancing Incentive Program will help States transform their long-term care systems by:
• Lowering costs through improved systems performance & efficiency
• Creating tools to help consumers with care planning & assessment
• Improving quality measurement & oversight
The Balancing Incentive Program also provides new ways to serve more people in home and community-based settings, in keeping with the integration mandate of the Americans with Disabilities Act (ADA), as required by the Olmstead decision. The Balancing Incentive Program was created by the Affordable Care Act of 2010 (Section 10202).
Program Type 11.Community First Choice (1915(k). The “Community First Choice Option” lets States provide home and community-based attendant services to Medicaid enrollees with disabilities under their State Plan.
This option became available on October 1, 2011 and provides a 6 % increase in Federal matching payments to States for expenditures related to this option.
Program Type 12. Psychiatric Rehab Facility For Children. Under the authority of section 2707 of the Patient Protection and Affordable Care Act of 2010 (Affordable Care Act), the Centers for Medicare & Medicaid Services (CMS) is funding the Medicaid Emergency Psychiatric Demonstration, which will be conducted by participating States. This is a 3-year Demonstration that permits participating States to provide payment under the State Medicaid plan to certain non-government psychiatric hospitals for inpatient emergency psychiatric care to Medicaid recipients aged 21 to 64 who have expressed suicidal or homicidal thoughts or gestures, and are determined to be dangerous to themselves or others.
Program Type 13. Home and Community-Based Services (HCBS) State Plan Option (1915(i)). States can offer a variety of services under a State Plan Home and Community-Based Services (HCBS) benefit. People must meet State-defined criteria based on need and typically get a combination of acute-care medical services (like dental services, skilled nursing services) and long-term services (like respite, case management, supported employment and environmental modifications).
1915(i) State plan HCBS: State Options
• Target the HCBS benefit to one or more specific populations
• Establish separate additional needs-based criteria for individual HCBS
• Establish a new Medicaid eligibility group for people who get State plan HCBS
• Define the HCBS included in the benefit, including State- defined and CMS-approved “other services” applicable to the population
• Option to allow any or all HCBS to be self-directed
Program Type 14.State Plan CHIP (See 42 CRF 457) ‘This program is for Title XXI recipients (children age 0 through 18, children receiving prenatal care through the conception to birth option, pregnant women), “Child health assistance” services (as allowed by State law and defined at § 457.402) means payment for part or all of the cost of health benefits coverage provided to targeted low-income children for the following services:
(a) Inpatient hospital services.
(b) Outpatient hospital services.
(c) Physician services.
(d) Surgical services.
(e) Clinic services (including health center services) and other ambulatory health care services.
(f) Prescription drugs and biologicals and the administration of these drugs and biologicals, only if these drugs and biologicals are not furnished for the purpose of causing, or assisting in causing, the death, suicide, euthanasia, or mercy killing of a person.
(g) Over-the-counter medications.
(h) Laboratory and radiological services.
(i) Prenatal care and pre-pregnancy family planning services and supplies.
(j) Inpatient mental health services, other than services described in paragraph (r) of this section but including services furnished in a state-operated mental health hospital and including residential or other 24-hour therapeutically planned structured services.
(k) Outpatient mental health services, other than services described in paragraph (s) of this section but including services furnished in a State-operated mental health hospital and including community-based services.
(l) Durable medical equipment and other medically-related or remedial devices (such as prosthetic devices, implants, eyeglasses, hearing aids, dental devices and adaptive devices).
(m) Disposable medical supplies.
(n) Home and community-based health care services and related supportive services (such as home health nursing services, personal care, assistance with activities of daily living, chore services, day care services, respite care services, training for family members and minor modification to the home.)
(o) Nursing care services (such as nurse practitioner services, nurse midwife services, advanced practice nurse services, private duty nursing, pediatric nurse services and respiratory care services) in a home, school, or other setting.
(p) Other pregnancy-related procedure only if necessary to save the life of the mother or if the pregnancy is the result of rape or incest.
(q) Dental services.
(r) Inpatient substance abuse treatment services and residential substance abuse treatment services.
(s) Outpatient substance abuse treatment services.
(t) Case management services.
(u) Care coordination services.
(v) Physical therapy, occupational therapy, and services for individuals with speech, hearing and language disorders.
(w) Hospice care.
(x) Any other medical, diagnostic, screening, preventive, restorative, remedial, therapeutic, or rehabilitative services (whether in a facility, home, school, or other setting) if recognized by State law and only if the service is—
(1) Prescribed by or furnished by a physician or other licensed or registered practitioner within the scope of practice as defined by State law;
(2) Performed under the general supervision or at the direction of a physician; or
(3) Furnished by a health care facility that is operated by a State or local government or is licensed under State law and operating within the scope of the license.
(y) Premiums for private health care insurance coverage.
(z) Medical transportation.
(aa) Enabling services (such as transportation, translation, and outreach services) only if designed to increase the accessibility of primary and preventive health care services for eligible low-income individuals.
(bb) Any other health care services or items specified by the Secretary and not excluded under this subchapter.
Program Type 15. Psychiatric Residential Treatment Facilities Demonstration Grant Program (PRTF). The Community Alternatives to Psychiatric Residential Treatment Facilities (PRTF) Demonstration Grant Program was authorized by Section 6063 of the Deficit Reduction Act of 2005 to provide up to $218 million to up to 10 states to develop 5-year demonstration programs that provide home and community-based services to children as alternatives to PRTF's. Nine states implemented demonstration grants. These projects were designed to test the cost-effectiveness of providing services in a child’s home or community rather than in a PRTF and whether the services improve or maintain the child’s functioning.
Program Type 16. 1915(j) (Self-directed personal assistance services/personal care under State Plan or 1915(c) waiver). Self-directed personal assistance services (PAS) are personal care and related services provided under the Medicaid State plan and/or section 1915(c) waivers the State already has in place.
• Participation in self-directed PAS is voluntary
• Participants set their own provider qualifications and train their PAS providers Participants determine how much they pay for a service, support or item
Appendix F: Eligibility Group Table
Code |
Eligibility Group |
Short Description |
Citation |
Type |
Category |
MEDICAID MANDATORY COVERAGE |
|||||
01 |
Parents and Other Caretaker Relatives |
Parents and other caretaker relatives of dependent children with household income at or below a standard established by the state. |
42 CFR 435.110; 1902(a)(10)(A)(i)(I); 1931(b) and (d) |
Family/Adult |
Mandatory Coverage |
02 |
Transitional Medical Assistance |
Families with Medicaid eligibility extended for up to 12 months because of earnings. |
408(a)(11)(A);
1902(a)(52); 1902(e)(1)(B); |
Family/Adult |
Mandatory Coverage |
03 |
Extended Medicaid due to Earnings |
Families with Medicaid eligibility extended for 4 months because of increased earnings. |
42
CFR 435.112; 408(a)(11)(A); 1902 (e)(1)(A); |
Family/Adult |
Mandatory Coverage |
04 |
Extended Medicaid due to Spousal Support Collections |
Families with Medicaid eligibility extended for 4 months as the result of the collection of spousal support. |
42 CFR 435.115; 408(a)(11)(B); 1931 (c)(1) |
Family/Adult |
Mandatory Coverage |
05 |
Pregnant Women |
Women who are pregnant or post-partum, with household income at or below a standard established by the state. |
42
CFR 435.116; 1902(a)(10)(A)(i)(III) and (IV);
1902(a)(10)(A)(ii)(I), (IV) and (IX); |
Family/Adult |
Mandatory Coverage |
06 |
Deemed Newborns |
Children born to women covered under Medicaid or a separate CHIP for the date of the child's birth, who are deemed eligible for Medicaid until the child turns age 1 |
42
CFR 435.117; |
Family/Adult |
Mandatory Coverage |
07 |
Infants and Children under Age 19 |
Infants and children under age 19 with household income at or below standards established by the state based on age group. |
42 CFR 435.118 1902(a)(10)(A)(i)(III), (IV), (VI) and (VII); 1902(a)(10)(A)(ii)(IV) and (IX); 1931(b) and (d) |
Family/Adult |
Mandatory Coverage |
08 |
Children with Title IV-E Adoption Assistance, Foster Care or Guardianship Care |
Individuals for whom an adoption assistance agreement is in effect or foster care or kinship guardianship assistance maintenance payments are made under Title IV-E of the Act. |
42 CFR 435.145; 473(b)(3); 1902(a)(10)(A)(i)(I) |
Family/Adult |
Mandatory Coverage |
09 |
Former Foster Care Children |
Individuals under the age of 26, not otherwise mandatorily eligible, who were in foster care and on Medicaid either when they turned age 18 or aged out of foster care. |
42
CFR 435.150; |
Family/Adult |
Mandatory Coverage |
|
|
|
|
|
|
Please note that T-MSIS eligibility grouping # 10 “Individuals at or below 133% FPL Age 19 through 64” has been removed and replaced with expanded groupings 72-75 (see below). |
|||||
72 |
Adult Group - Individuals at or below 133% FPL Age 19 through 64 - newly eligible for all states |
Non-pregnant individuals aged 19 through 64, not otherwise mandatorily eligible, with income at or below 133% FPL. |
42 CFR 435.119; 1902(a)(10)(A)(i)(VIII) |
Family/Adult |
Mandatory Coverage |
73 |
Adult Group - Individuals at or below 133% FPL Age 19 through 64- not newly eligible for non 1905z(3) states |
Non-pregnant individuals aged 19 through 64, not otherwise mandatorily eligible, with income at or below 133% FPL. |
42 CFR 435.119; 1902(a)(10)(A)(i)(VIII) 1905z(3) |
Family/Adult |
Mandatory Coverage |
74 |
Adult Group - Individuals at or below 133% FPL Age 19 through 64 – not newly eligible parent/ caretaker-relative(s) in 1905z(3) states |
Non-pregnant individuals aged 19 through 64, not otherwise mandatorily eligible, with income at or below 133% FPL. |
42 CFR 435.119; 1902(a)(10)(A)(i)(VIII) 1905z(3) |
Family/Adult |
Mandatory Coverage |
75 |
Adult Group - Individuals at or below 133% FPL Age 19 through 64- not newly eligible non-parent/ caretaker-relative(s) in 1905z(3) states |
Non-pregnant individuals aged 19 through 64, not otherwise mandatorily eligible, with income at or below 133% FPL. |
42 CFR 435.119; 1902(a)(10)(A)(i)(VIII) 1905z(3) |
Family/Adult |
Mandatory Coverage |
11 |
Individuals Receiving SSI |
Individuals who are aged, blind or disabled who receive SSI. |
42 CFR 435.120; 1902(a)(10)(A)(i)(II)(aa) |
ABD |
Mandatory Coverage |
12 |
Aged, Blind and Disabled Individuals in 209(b) States |
In 209(b) states, aged, blind and disabled individuals who meet more restrictive criteria than used in SSI. |
42 CFR 435.121; 1902(f) |
ABD |
Mandatory Coverage |
13 |
Individuals Receiving Mandatory State Supplements |
Individuals receiving mandatory State Supplements to SSI benefits. |
42 CFR 435.130 |
ABD |
Mandatory Coverage |
14 |
Individuals Who Are Essential Spouses |
Individuals who were eligible as essential spouses in 1973 and who continue be essential to the well-being of a recipient of cash assistance. |
42 CFR 435.131; 1905(a) |
ABD |
Mandatory Coverage |
15 |
Institutionalized Individuals Continuously Eligible Since 1973 |
Institutionalized individuals who were eligible for Medicaid in 1973 as inpatients of Title XIX medical institutions or intermediate care facilities, and who continue to meet the 1973 requirements. |
42 CFR 435.132 |
ABD |
Mandatory Coverage |
16 |
Blind or Disabled Individuals Eligible in 1973 |
Blind or disabled individuals who were eligible for Medicaid in 1973 who meet all current requirements for Medicaid except for the blindness or disability criteria. |
42 CFR 435.133 |
ABD |
Mandatory Coverage |
17 |
Individuals Who Lost Eligibility for SSI/SSP Due to an Increase in OASDI Benefits in 1972 |
Individuals who would be eligible for SSI/SSP except for the increase in OASDI benefits in 1972, who were entitled to and receiving cash assistance in August, 1972. |
42 CFR 435.134 |
ABD |
Mandatory Coverage |
18 |
Individuals Who Would be Eligible for SSI/SSP but for OASDI COLA increases since April, 1977 |
Individuals who are receiving OASDI and became ineligible for SSI/SSP after April, 1977, who would continue to be eligible if the cost of living increases in OASDI since their last month of eligibility for SSI/SSP/OASDI were deducted from income. |
42 CFR 435.135; |
ABD |
Mandatory Coverage |
19 |
Disabled Widows and Widowers Ineligible for SSI due to Increase in OASDI |
Disabled widows and widowers who would be eligible for SSI /SSP, except for the increase in OASDI benefits due to the elimination of the reduction factor in P.L. 98-21, who therefore are deemed to be SSI or SSP recipients. |
42 CFR 435.137; 1634(b) |
ABD |
Mandatory Coverage |
20 |
Disabled Widows and Widowers Ineligible for SSI due to Early Receipt of Social Security |
Disabled widows and widowers who would be eligible for SSI/SSP, except for the early receipt of OASDI benefits, who are not entitled to Medicare Part A, who therefore are deemed to be SSI recipients. |
42 CFR 435.138; 1634(d) |
ABD |
Mandatory Coverage |
21 |
Working Disabled under 1619(b) |
Blind or disabled individuals who participated in Medicaid as SSI cash recipients or who were considered to be receiving SSI, who would still qualify for SSI except for earnings. |
1619(b); 1902(a)(10)(A)(i)(II)(bb); 1905(q) |
ABD |
Mandatory Coverage |
22 |
Disabled Adult Children |
Individuals who lose eligibility for SSI at age 18 or older due to receipt of or increase in Title II OASDI child benefits. |
1634(c) |
ABD |
Mandatory Coverage |
23 |
Qualified Medicare Beneficiaries |
Individuals with income equal to or less than 100% of the FPL who are entitled to Medicare Part A, who qualify for Medicare cost-sharing. |
1902(a)(10)(E)(i); 1905(p) |
ABD |
Mandatory Coverage |
24 |
Qualified Disabled and Working Individuals |
Working, disabled individuals with income equal to or less than 200% of the FPL, who are entitled to Medicare Part A under section 1818A, who qualify for payment of Medicare Part A premiums. |
1902(a)(10)(E)(ii); 1905(p)(3)(A)(i); 1905(s) |
ABD |
Mandatory Coverage |
25 |
Specified Low Income Medicare Beneficiaries |
Individuals with income between 100% and 120% of the FPL who are entitled to Medicare Part A, who qualify for payment of Medicare Part B premiums. |
1902(a)(10)(E)(iii); 1905(p)(3)(A)(ii) |
ABD |
Mandatory Coverage |
26 |
Qualifying Individuals |
Individuals with income between 120% and 135% of the FPL who are entitled to Medicare Part A, who qualify for payment of Medicare Part B premiums. |
1902(a)(10)(E)(iv); 1905(p)(3)(A)(ii) |
ABD |
Mandatory Coverage |
MEDICAID OPTIONS FOR COVERAGE |
|||||
27 |
Optional Coverage of Parents and Other Caretaker Relatives |
Individuals qualifying as parents or caretaker relatives who are not mandatorily eligible and who have income at or below a standard established by the State. |
42 CFR 435.220; 1902(a)(10)(A)(ii)(I) |
Family/Adult |
Options for Coverage |
28 |
Reasonable Classifications of Individuals under Age 21 |
Individuals under age 21 who are not mandatorily eligible and who have income at or below a standard established by the State. |
42 CFR 435.222; 1902(a)(10)(A)(ii)(I) and (IV) |
Family/Adult |
Options for Coverage |
29 |
Children with Non-IV-E Adoption Assistance |
Children with special needs for whom there is a non-IV-E adoption assistance agreement in effect with a state, who either were eligible for Medicaid or had income at or below a standard established by the state. |
42 CFR 435.227; 1902(a)(10)(A)(ii)(VIII); |
Family/Adult |
Options for Coverage |
30 |
Independent Foster Care Adolescents |
Individuals under an age specified by the State, less than age 21, who were in State-sponsored foster care on their 18th birthday and who meet the income standard established by the State. |
42 CFR 435.226; 1902(a)(10)(A)(ii)(XVII) |
Family/Adult |
Options for Coverage |
31 |
Optional Targeted Low Income Children |
Uninsured children who meet the definition of optional targeted low income children at 42 CFR 435.4, who have household income at or below a standard established by the State. |
42 CFR 435.229 and 435.4; 1902(a)(10)(A)(ii)(XIV); 1905(u)(2)(B) |
Family/Adult |
Options for Coverage |
32 |
Individuals Electing COBRA Continuation Coverage |
Individuals choosing to continue COBRA benefits with income equal to or less than 100% of the FPL. |
1902(a)(10)(F); 1902(u)(1) |
Family/Adult |
Options for Coverage |
33 |
Individuals above 133% FPL under Age 65 |
Individuals under 65, not otherwise mandatorily or optionally eligible, with income above 133% FPL and at or below a standard established by the State. |
CFR 435.218; 1902(hh); 1902(a)(10)(A)(ii)(XX) |
Family/Adult |
Options for Coverage |
34 |
Certain Individuals Needing Treatment for Breast or Cervical Cancer |
Individuals under the age of 65 who have been screened for breast or cervical cancer and need treatment. |
42 CFR 435.213; 1902(a)(10)(A)(ii)(XVIII); 1902(aa) |
Family/Adult |
Options for Coverage |
35 |
Individuals Eligible for Family Planning Services |
Individuals who are not pregnant, with income equal to or below the highest standard for pregnant women, as specified by the State, limited to family planning and related services. |
42 CFR 435.214; 1902(a)(10)(A)(ii)(XXI) |
Family/Adult |
Options for Coverage |
36 |
Individuals with Tuberculosis |
Individuals infected with tuberculosis whose income does not exceed established standards, limited to tuberculosis-related services. |
42 CFR 435.215; 1902(a)(10)(A)(ii)(XII); 1902(z) |
Family/Adult |
Options for Coverage |
37 |
Aged, Blind or Disabled Individuals Eligible for but Not Receiving Cash Assistance |
Individuals who meet the requirements of SSI or Optional State Supplement, but who do not receive cash. |
42 CFR 435.210 & 230; 1902(a)(10)(A)(ii)(I); |
ABD |
Options for Coverage |
38 |
Individuals Eligible for Cash Assistance except for Institutionalization |
Individuals who meet the requirements of AFDC, SSI or Optional State Supplement, and would be eligible if they were not living in a medical institution. |
42 CFR 435.211; 1902(a)(10)(A)(ii)(IV); |
ABD |
Options for Coverage |
39 |
Individuals Receiving Home and Community Based Services under Institutional Rules |
Individuals who would be eligible for Medicaid under the State Plan if in a medical institution, who would live in an institution if they did not receive home and community based services. |
42 CFR 435.217; 1902(a)(10)(A)(ii)(VI) |
ABD |
Options for Coverage |
40 |
Optional State Supplement Recipients - 1634 States, and SSI Criteria States with 1616 Agreements |
Individuals in 1634 States and in SSI Criteria States with agreements under 1616, who receive a state supplementary payment (but not SSI). |
42 CFR 435.232; 1902(a)(10)(A)(ii)(IV) |
ABD |
Options for Coverage |
41 |
Optional State Supplement Recipients - 209(b) States, and SSI Criteria States without 1616 Agreements |
Individuals in 209(b) States and in SSI Criteria States without agreements under 1616, who receive a state supplementary payment (but not SSI). |
42 CFR 435.234; 1902(a)(10)(A)(ii)(XI) |
ABD |
Options for Coverage |
42 |
Institutionalized Individuals Eligible under a Special Income Level |
Individuals who are in institutions for at least 30 consecutive days who are eligible under a special income level. |
42 CFR 435.236; 1902(a)(10)(A)(ii)(V) |
ABD |
Options for Coverage |
43 |
Individuals participating in a PACE Program under Institutional Rules |
Individuals who would be eligible for Medicaid under the State Plan if in a medical institution, who would require institutionalization if they did not participate in the PACE program. |
1934 |
ABD |
Options for Coverage |
44 |
Individuals Receiving Hospice Care |
Individuals who would be eligible for Medicaid under the State Plan if they were in a medical institution, who are terminally ill, and who will receive hospice care. |
1902(a)(10)(A)(ii)(VII); 1905(o) |
ABD |
Options for Coverage |
45 |
Qualified Disabled Children under Age 19 |
Certain children under 19 living at home, who are disabled and would be eligible if they were living in a medical institution. |
1902(e)(3) |
ABD |
Options for Coverage |
46 |
Poverty Level Aged or Disabled |
Individuals who are aged or disabled with income equal to or less than a percentage of the FPL, established by the state (no higher than 100%). |
1902(a)(10)(A)(ii)(X); 1902(m)(1) |
ABD |
Options for Coverage |
47 |
Work Incentives Eligibility Group |
Individuals with a disability with income below 250% of the FPL, who would qualify for SSI except for earned income. |
1902(a)(10)(A)(ii)(XIII) |
ABD |
Options for Coverage |
48 |
Ticket to Work Basic Group |
Individuals with earned income between ages 16 and 64 with a disability, with income and resources equal to or below a standard specified by the State. |
1902(a)(10)(A)(ii)(XV) |
ABD |
Options for Coverage |
49 |
Ticket to Work Medical Improvements Group |
Individuals with earned income between ages 16 and 64 who are no longer disabled but still have a medical impairment, with income and resources equal to or below a standard specified by the State. |
1902(a)(10)(A)(ii)(XVI) |
ABD |
Options for Coverage |
50 |
Family Opportunity Act Children with Disabilities |
Children under 19 who are disabled, with income equal to or less than a standard specified by the State (no higher than 300% of the FPL). |
1902(a)(10)(A)(ii)(XIX); 1902(cc)(1) |
ABD |
Options for Coverage |
51 |
Individuals Eligible for Home and Community-Based Services |
Individuals with income equal to or below 150% of the FPL, who qualify for home and community based services without a determination that they would otherwise live in an institution. |
1902(a)(10)(A)(ii)(XXII); 1915(i) |
ABD |
Options for Coverage |
52 |
Individuals Eligible for Home and Community-Based Services - Special Income Level |
Individuals with income equal to or below 300% of the SSI federal benefit rate, who meet the eligibility requirements for a waiver approved for the State under 1915(c), (d) or (e), or 1115. |
1902(a)(10)(A)(ii)(XXII); 1915(i) |
ABD |
Options for Coverage |
MEDICAID MEDICALLY NEEDY |
|||||
53 |
Medically Needy Pregnant Women |
Women who are pregnant, who would qualify as categorically needy, except for income. |
42 CFR 435.301(b)(1)(i) and (iv); 1902(a)(10)(C)(ii)(II) |
Family/Adult |
Medically Needy |
54 |
Medically Needy Children under Age 18 |
Children under 18 who would qualify as categorically needy, except for income. |
42 CFR 435.301(b)(1)(ii); 1902(a)(10)(C)(ii)(II) |
Family/Adult |
Medically Needy |
55 |
Medically Needy Children Age 18 through 20 |
Children over 18 and under an age established by the State (less than age 21), who would qualify as categorically needy, except for income. |
42 CFR 435.308; 1902(a)(10)(C)(ii)(II) |
Family/Adult |
Medically Needy |
56 |
Medically Needy Parents and Other Caretakers |
Parents and other caretaker relatives of dependent children, eligible as categorically needy except for income. |
42 CFR 435.310 |
Family/Adult |
Medically Needy |
|
Removed – Do Not Use |
|
|
|
|
|
Removed – Do Not Use |
|
|
|
|
59 |
Medically Needy Aged, Blind or Disabled |
Individuals who are age 65 or older, blind or disabled, who are not eligible as categorically needy, who meet income and resource standards specified by the State, or who meet the income standard using medical and remedial care expenses to offset excess income. |
42 CFR 435.320, 435.322, 435.324,and 435.330; 1902(a)(10)(C) |
ABD |
Medically Needy |
60 |
Medically Needy Blind or Disabled Individuals Eligible in 1973 |
Blind or disabled individuals who were eligible for Medicaid as Medically Needy in 1973 who meet all current requirements for Medicaid except for the blindness or disability criteria. |
42 CFR 435.340 |
ABD |
Medically Needy |
CHIP COVERAGE |
|||||
61 |
Targeted Low-Income Children |
Uninsured children under age 19 who do not have access to public employee coverage and whose household income is within standards established by the state. |
42 CFR 457.310; 2102(b)(1)(B)(v) |
Children |
Optional |
62 |
Deemed Newborn |
Children born to targeted low-income pregnant women who are deemed eligible for CHIP or Medicaid for one year. |
2112(e) |
Children |
Optional |
63 |
Children Ineligible for Medicaid Due to Loss of Income Disregards |
Children determined to be ineligible for Medicaid as a result of the elimination of income disregards under the MAGI income methodology. |
42 CFR 457.340(d) Section 2101(f) of the ACA |
Children |
Mandatory |
CHIP ADDITIONAL OPTIONS FOR COVERAGE |
|||||
64 |
Coverage from Conception to Birth |
Uninsured children from conception to birth who do not have access to public employee coverage and whose household income is within standards established by the state. |
42 CFR 457.310 2102(b)(1)(B)(v) |
Children |
Option for Coverage |
65 |
Children with Access to Public Employee Coverage |
Uninsured children under age 19 having access to public employee coverage and whose household income is within standards established by the state. |
2110(b)(2)(B) and (b)(6) |
Children |
Option for Coverage |
66 |
Children Eligible for Dental Only Supplemental Coverage |
Children who are otherwise eligible for CHIP but for the fact that they are enrolled in a group health plan or health insurance offered through an employer. Coverage is limited to dental services. |
2110(b)(5) |
Children |
Option for Coverage |
67 |
Targeted Low-Income Pregnant Women |
Uninsured pregnant women who do not have access to public employee coverage and whose household income is within standards established by the state. |
2112 |
Pregnant Women |
Option for Coverage |
68 |
Pregnant Women with Access to Public Employee Coverage |
Uninsured pregnant women having access to public employee coverage and whose household income is within standards established by the state. |
2110(b)(2)(B) and (b)(6) |
Pregnant Women |
Option for Coverage |
1115 EXPANSION ELIGIBILITY GROUPS |
|||||
69 |
Individuals with Mental Health Conditions (expansion group) |
Individuals with mental health conditions who do not qualify for Medicaid due to the severity or duration of their disability or due to other eligibility factors; and/or those who are otherwise eligible but require benefits or services that are not comparable to those provided to other Medicaid beneficiaries. |
1115 expansion |
|
|
70 |
Family Planning Participants (expansion group) |
Individuals of child bearing age who require family planning services and supplies and for which the state does not choose to, or cannot provide, optional eligibility coverage under the Individuals Eligible for Family Planning Services eligibility group (1902(a)(10)(A)(ii)(XXI)). |
1115 expansion |
|
|
71 |
Other expansion group |
Individuals who do not qualify for Medicaid or CHIP under a mandatory eligibility or coverage group and for whom the state chooses to provide eligibility and/or benefits in a manner not permitted by title XIX or XXI of the Social Security Act. |
1115 expansion |
|
|
Appendix G: ISO 639 Language Codes Reference
ISO 639-2 Code |
Language |
ISO 639-2 Code |
Language |
abk |
Abkhazian |
kru |
Kurukh |
ace |
Achinese |
kut |
Kutenai |
ach |
Acoli |
lad |
Ladino |
ada |
Adangme |
lah |
Lahnda |
ady |
Adyghe; Adygei |
lam |
Lamba |
aar |
Afar |
day |
Land Dayak languages |
afh |
Afrihili |
lao |
Lao |
afr |
Afrikaans |
lat |
Latin |
afa |
Afro-Asiatic languages |
lav |
Latvian |
ain |
Ainu |
lez |
Lezghian |
aka |
Akan |
lim |
Limburgan; Limburger; Limburgish |
akk |
Akkadian |
lin |
Lingala |
alb |
Albanian |
lit |
Lithuanian |
alb |
Albanian |
jbo |
Lojban |
ale |
Aleut |
nds |
Low German; Low Saxon; German, Low; Saxon, Low |
alg |
Algonquian languages |
dsb |
Lower Sorbian |
tut |
Altaic languages |
loz |
Lozi |
amh |
Amharic |
lub |
Luba-Katanga |
anp |
Angika |
lua |
Luba-Lulua |
apa |
Apache languages |
lui |
Luiseno |
ara |
Arabic |
smj |
Lule Sami |
arg |
Aragonese |
lun |
Lunda |
arp |
Arapaho |
luo |
Luo (Kenya and Tanzania) |
arw |
Arawak |
lus |
Lushai |
arm |
Armenian |
ltz |
Luxembourgish; Letzeburgesch |
rup |
Aromanian; Arumanian; Macedo-Romanian |
mac |
Macedonian |
art |
Artificial languages |
mad |
Madurese |
asm |
Assamese |
mag |
Magahi |
ast |
Asturian; Bable; Leonese; Asturleonese |
mai |
Maithili |
ath |
Athapascan languages |
mak |
Makasar |
aus |
Australian languages |
mlg |
Malagasy |
map |
Austronesian languages |
may |
Malay |
ava |
Avaric |
mal |
Malayalam |
ave |
Avestan |
mlt |
Maltese |
awa |
Awadhi |
mnc |
Manchu |
aym |
Aymara |
mdr |
Mandar |
aze |
Azerbaijani |
man |
Mandingo |
ban |
Balinese |
mni |
Manipuri |
bat |
Baltic languages |
mno |
Manobo languages |
bal |
Baluchi |
glv |
Manx |
bam |
Bambara |
mao |
Maori |
bai |
Bamileke languages |
arn |
Mapudungun; Mapuche |
bad |
Banda languages |
mar |
Marathi |
bnt |
Bantu languages |
chm |
Mari |
bas |
Basa |
mah |
Marshallese |
bak |
Bashkir |
mwr |
Marwari |
baq |
Basque |
mas |
Masai |
btk |
Batak languages |
myn |
Mayan languages |
bej |
Beja; Bedawiyet |
men |
Mende |
bel |
Belarusian |
mic |
Mi'kmaq; Micmac |
bem |
Bemba |
min |
Minangkabau |
ben |
Bengali |
mwl |
Mirandese |
ber |
Berber languages |
moh |
Mohawk |
bho |
Bhojpuri |
mdf |
Moksha |
bih |
Bihari languages |
lol |
Mongo |
bik |
Bikol |
mon |
Mongolian |
bin |
Bini; Edo |
mkh |
Mon-Khmer languages |
bis |
Bislama |
mos |
Mossi |
byn |
Blin; Bilin |
mul |
Multiple languages |
zbl |
Blissymbols; Blissymbolics; Bliss |
mun |
Munda languages |
nob |
Bokmål, Norwegian; Norwegian Bokmål |
nah |
Nahuatl languages |
bos |
Bosnian |
nau |
Nauru |
bra |
Braj |
nav |
Navajo; Navaho |
bre |
Breton |
nde |
Ndebele, North; North Ndebele |
bug |
Buginese |
nbl |
Ndebele, South; South Ndebele |
bul |
Bulgarian |
ndo |
Ndonga |
bua |
Buriat |
nap |
Neapolitan |
bur |
Burmese |
new |
Nepal Bhasa; Newari |
cad |
Caddo |
nep |
Nepali |
cat |
Catalan; Valencian |
nia |
Nias |
cau |
Caucasian languages |
nic |
Niger-Kordofanian languages |
ceb |
Cebuano |
ssa |
Nilo-Saharan languages |
cel |
Celtic languages |
niu |
Niuean |
cai |
Central American Indian languages |
nqo |
N'Ko |
khm |
Central Khmer |
nog |
Nogai |
chg |
Chagatai |
non |
Norse, Old |
cmc |
Chamic languages |
nai |
North American Indian languages |
cha |
Chamorro |
frr |
Northern Frisian |
che |
Chechen |
sme |
Northern Sami |
chr |
Cherokee |
nor |
Norwegian |
chy |
Cheyenne |
nno |
Norwegian Nynorsk; Nynorsk, Norwegian |
chb |
Chibcha |
nub |
Nubian languages |
nya |
Chichewa; Chewa; Nyanja |
nym |
Nyamwezi |
chi |
Chinese |
nyn |
Nyankole |
chn |
Chinook jargon |
nyo |
Nyoro |
chp |
Chipewyan; Dene Suline |
nzi |
Nzima |
cho |
Choctaw |
oci |
Occitan (post 1500) |
chu |
Church Slavic; Old Slavonic; Church Slavonic; Old Bulgarian; Old Church Slavonic |
arc |
Official Aramaic (700-300 BCE); Imperial Aramaic (700-300 BCE) |
chk |
Chuukese |
oji |
Ojibwa |
chv |
Chuvash |
ori |
Oriya |
nwc |
Classical Newari; Old Newari; Classical Nepal Bhasa |
orm |
Oromo |
syc |
Classical Syriac |
osa |
Osage |
cop |
Coptic |
oss |
Ossetian; Ossetic |
cor |
Cornish |
oto |
Otomian languages |
cos |
Corsican |
pal |
Pahlavi |
cre |
Cree |
pau |
Palauan |
mus |
Creek |
pli |
Pali |
crp |
Creoles and pidgins |
pam |
Pampanga; Kapampangan |
cpe |
Creoles and pidgins, English based |
pag |
Pangasinan |
cpf |
Creoles and pidgins, French-based |
pan |
Panjabi; Punjabi |
cpp |
Creoles and pidgins, Portuguese-based |
pap |
Papiamento |
crh |
Crimean Tatar; Crimean Turkish |
paa |
Papuan languages |
hrv |
Croatian |
nso |
Pedi; Sepedi; Northern Sotho |
cus |
Cushitic languages |
per |
Persian |
cze |
Czech |
peo |
Persian, Old (ca.600-400 B.C.) |
dak |
Dakota |
phi |
Philippine languages |
dan |
Danish |
phn |
Phoenician |
dar |
Dargwa |
pon |
Pohnpeian |
del |
Delaware |
pol |
Polish |
din |
Dinka |
por |
Portuguese |
div |
Divehi; Dhivehi; Maldivian |
pra |
Prakrit languages |
doi |
Dogri |
pro |
Provençal, Old (to 1500);Occitan, Old (to 1500) |
dgr |
Dogrib |
pus |
Pushto; Pashto |
dra |
Dravidian languages |
que |
Quechua |
dua |
Duala |
raj |
Rajasthani |
dum |
Dutch, Middle (ca.1050-1350) |
rap |
Rapanui |
dut |
Dutch; Flemish |
rar |
Rarotongan; Cook Islands Maori |
dyu |
Dyula |
roa |
Romance languages |
dzo |
Dzongkha |
rum |
Romanian; Moldavian; Moldovan |
frs |
Eastern Frisian |
roh |
Romansh |
efi |
Efik |
rom |
Romany |
egy |
Egyptian (Ancient) |
run |
Rundi |
eka |
Ekajuk |
rus |
Russian |
elx |
Elamite |
sal |
Salishan languages |
eng |
English |
sam |
Samaritan Aramaic |
enm |
English, Middle (1100-1500) |
smi |
Sami languages |
ang |
English, Old (ca.450-1100) |
smo |
Samoan |
myv |
Erzya |
sad |
Sandawe |
epo |
Esperanto |
sag |
Sango |
est |
Estonian |
san |
Sanskrit |
ewe |
Ewe |
sat |
Santali |
ewo |
Ewondo |
srd |
Sardinian |
fan |
Fang |
sas |
Sasak |
fat |
Fanti |
sco |
Scots |
fao |
Faroese |
sel |
Selkup |
fij |
Fijian |
sem |
Semitic languages |
fil |
Filipino; Pilipino |
srp |
Serbian |
fin |
Finnish |
srr |
Serer |
fiu |
Finno-Ugrian languages |
shn |
Shan |
fon |
Fon |
sna |
Shona |
fre |
French |
iii |
Sichuan Yi; Nuosu |
frm |
French, Middle (ca.1400-1600) |
scn |
Sicilian |
fro |
French, Old (842-ca.1400) |
sid |
Sidamo |
fur |
Friulian |
sgn |
Sign Languages |
ful |
Fulah |
bla |
Siksika |
gaa |
Ga |
snd |
Sindhi |
gla |
Gaelic; Scottish Gaelic |
sin |
Sinhala; Sinhalese |
car |
Galibi Carib |
sit |
Sino-Tibetan languages |
glg |
Galician |
sio |
Siouan languages |
lug |
Ganda |
sms |
Skolt Sami |
gay |
Gayo |
den |
Slave (Athapascan) |
gba |
Gbaya |
sla |
Slavic languages |
gez |
Geez |
slo |
Slovak |
geo |
Georgian |
slv |
Slovenian |
ger |
German |
sog |
Sogdian |
gmh |
German, Middle High (ca.1050-1500) |
som |
Somali |
goh |
German, Old High (ca.750-1050) |
son |
Songhai languages |
gem |
Germanic languages |
snk |
Soninke |
gil |
Gilbertese |
wen |
Sorbian languages |
gon |
Gondi |
sot |
Sotho, Southern |
gor |
Gorontalo |
sai |
South American Indian languages |
got |
Gothic |
alt |
Southern Altai |
grb |
Grebo |
sma |
Southern Sami |
grc |
Greek, Ancient (to 1453) |
spa |
Spanish; Castilian |
gre |
Greek, Modern (1453-) |
srn |
Sranan Tongo |
grn |
Guarani |
suk |
Sukuma |
guj |
Gujarati |
sux |
Sumerian |
gwi |
Gwich'in |
sun |
Sundanese |
hai |
Haida |
sus |
Susu |
hat |
Haitian; Haitian Creole |
swa |
Swahili |
hau |
Hausa |
ssw |
Swati |
haw |
Hawaiian |
swe |
Swedish |
heb |
Hebrew |
gsw |
Swiss German; Alemannic; Alsatian |
her |
Herero |
syr |
Syriac |
hil |
Hiligaynon |
tgl |
Tagalog |
him |
Himachali languages; Western Pahari languages |
tah |
Tahitian |
hin |
Hindi |
tai |
Tai languages |
hmo |
Hiri Motu |
tgk |
Tajik |
hit |
Hittite |
tmh |
Tamashek |
hmn |
Hmong; Mong |
tam |
Tamil |
hun |
Hungarian |
tat |
Tatar |
hup |
Hupa |
tel |
Telugu |
iba |
Iban |
ter |
Tereno |
ice |
Icelandic |
tet |
Tetum |
ido |
Ido |
tha |
Thai |
ibo |
Igbo |
tib |
Tibetan |
ijo |
Ijo languages |
tig |
Tigre |
ilo |
Iloko |
tir |
Tigrinya |
smn |
Inari Sami |
tem |
Timne |
inc |
Indic languages |
tiv |
Tiv |
ine |
Indo-European languages |
tli |
Tlingit |
ind |
Indonesian |
tpi |
Tok Pisin |
inh |
Ingush |
tkl |
Tokelau |
ina |
Interlingua (International Auxiliary Language Association) |
tog |
Tonga (Nyasa) |
ile |
Interlingue; Occidental |
ton |
Tonga (Tonga Islands) |
iku |
Inuktitut |
tsi |
Tsimshian |
ipk |
Inupiaq |
tso |
Tsonga |
ira |
Iranian languages |
tsn |
Tswana |
gle |
Irish |
tum |
Tumbuka |
mga |
Irish, Middle (900-1200) |
tup |
Tupi languages |
sga |
Irish, Old (to 900) |
tur |
Turkish |
iro |
Iroquoian languages |
ota |
Turkish, Ottoman (1500-1928) |
ita |
Italian |
tuk |
Turkmen |
jpn |
Japanese |
tvl |
Tuvalu |
jav |
Javanese |
tyv |
Tuvinian |
jrb |
Judeo-Arabic |
twi |
Twi |
jpr |
Judeo-Persian |
udm |
Udmurt |
kbd |
Kabardian |
uga |
Ugaritic |
kab |
Kabyle |
uig |
Uighur; Uyghur |
kac |
Kachin; Jingpho |
ukr |
Ukrainian |
kal |
Kalaallisut; Greenlandic |
umb |
Umbundu |
xal |
Kalmyk; Oirat |
mis |
Uncoded languages |
kam |
Kamba |
und |
Undetermined |
kan |
Kannada |
hsb |
Upper Sorbian |
kau |
Kanuri |
urd |
Urdu |
krc |
Karachay-Balkar |
uzb |
Uzbek |
kaa |
Kara-Kalpak |
vai |
Vai |
krl |
Karelian |
ven |
Venda |
kar |
Karen languages |
vie |
Vietnamese |
kas |
Kashmiri |
vol |
Volapük |
csb |
Kashubian |
vot |
Votic |
kaw |
Kawi |
wak |
Wakashan languages |
kaz |
Kazakh |
wln |
Walloon |
kha |
Khasi |
war |
Waray |
khi |
Khoisan languages |
was |
Washo |
kho |
Khotanese; Sakan |
wel |
Welsh |
kik |
Kikuyu; Gikuyu |
fry |
Western Frisian |
kmb |
Kimbundu |
wal |
Wolaitta; Wolaytta |
kin |
Kinyarwanda |
wol |
Wolof |
kir |
Kirghiz; Kyrgyz |
xho |
Xhosa |
tlh |
Klingon; tlhIngan-Hol |
sah |
Yakut |
kom |
Komi |
yao |
Yao |
kon |
Kongo |
yap |
Yapese |
kok |
Konkani |
yid |
Yiddish |
kor |
Korean |
yor |
Yoruba |
kos |
Kosraean |
ypk |
Yupik languages |
kpe |
Kpelle |
znd |
Zande languages |
kro |
Kru languages |
zap |
Zapotec |
kua |
Kuanyama; Kwanyama |
zza |
Zaza; Dimili; Dimli; Kirdki; Kirmanjki; Zazaki |
kum |
Kumyk |
zen |
Zenaga |
kur |
Kurdish |
zha |
Zhuang; Chuang |
|
|
zul |
Zulu |
|
|
zun |
Zuni |
Appendix H: Benefit Types
Code Value |
Benefit |
Short Description |
Category |
Type of Care |
Long Term Care* |
Citations (Act and 42 CFR) |
|
Mandatory Benefits for Categorically Needy (Mandatory and Options for Coverage) Individuals and Optional Benefits for Medically Needy Individuals |
|||||
001 |
Inpatient Hospital Services |
Services furnished in a hospital or institution (licensed or formally approved as a hospital), for the care and treatment of inpatients with disorders other than mental health disease. |
Mandatory |
Institutional |
No |
1905(a)(1), 440.10, 440.189(g) |
002 |
Outpatient Hospital Services |
Preventive, diagnostic, therapeutic, rehabilitative, or palliative services furnished to outpatients by a hospital or institution (licensed or formally approved as a hospital). |
Mandatory |
Ambulatory |
No |
1905(a)(2)(A), 440.20(a) |
003 |
Rural Health Clinics |
Services and supplies provided by a physician within the scope of his/her practice, a physician assistant (if not prohibited by state law), nurse practitioner (if not prohibited by state law) nurse midwife, or other specialized nurse practitioners, intermittent visiting nurse care and related medical supplies (other than drugs and biologicals), and other ambulatory services when furnished in a certified rural health clinic or away from the clinic if an agreement between the physician and clinic for payment of services by the clinic exists. |
Mandatory |
Ambulatory |
No |
1905(a)(2)(B), 440.20(b) and (c), 1910(a) |
004 |
Federally Qualified Health Centers |
Services and related supplies provided by a physician within the scope of his/her practice, physician assistants, nurse practitioners, nurse midwives, clinical psychologists, clinical social workers, and other ambulatory services when furnished in a federally qualified health center. |
Mandatory |
Ambulatory |
No |
1905(a)(2)(C) |
005 |
Other Laboratory and X-Ray Services |
Technical and radiological services ordered and provided by or under direction of a physician or other licensed practitioner in an office or similar facility other than a clinic or hospital outpatient department and furnished by an approved laboratory. |
Mandatory |
Ambulatory |
No |
1905(a)(3), 440.30 |
006 |
Nursing Facility Services for Individuals Age 21 and Older |
Services (other than services in an institution for mental health conditions), furnished to individuals age 21 and older, which are needed on a daily basis and required to be provided in an inpatient basis provided by a Medicaid-approved facility and ordered by and provided under the direction of a physician. |
Mandatory |
Institutional |
Yes |
1905(a)(4)(A), 440.40(a) |
007 |
Early and Periodic Screening, Diagnostic and Treatment Services |
Screening and diagnostic services to determine physical or mental health condition; health care treatment and other measures to correct or ameliorate any chronic conditions discovered in recipients under age 21. |
Mandatory |
Both |
No |
1905(a)(4)(B), 1902(a)(43), 1905(r) |
008 |
Family Planning Services and Supplies |
Family planning services and supplies furnished (directly or under arrangements with others) to individuals of child-bearing age (including minors who can be considered to be sexually active) who desire such services and supplies. |
Mandatory |
Ambulatory |
No |
1905(a)(4)(C), 441 Subpart F |
009 |
Cessation of Tobacco Use by Pregnant Women |
Counseling and pharmacotherapy services for cessation of tobacco use by pregnant women. |
Mandatory |
Ambulatory |
No |
1905(a)(4)(D) |
010 |
Physician Services |
Services furnished by a state-licensed physician within his or her scope of practice of medicine or osteopathy. |
Mandatory |
Ambulatory |
No |
1905(a)(5)(A), 440.50(a) |
011 |
Medical and Surgical Services Furnished by a Dentist |
Medical and surgical services furnished by a doctor of dental medicine or dental surgery, or if permitted by state law, by a physician. |
Mandatory |
Ambulatory |
No |
1905(a)(5)(B), 440.50(b) |
012 |
Nurse Midwife Services |
Services furnished by a licensed nurse midwife within the scope of practice authorized by State law or regulation; Inpatient or outpatient hospital services or clinic services furnished by a licensed nurse midwife under the supervision of, or associated with a physician or other health care provider. |
Mandatory |
Ambulatory |
No |
1905(a)(17), 440.165 |
013 |
Certified Pediatric or Family Nurse Practitioner Services |
Services furnished by a certified pediatric nurse practitioner with a practice limited to providing primary health care to individuals under age 21; or a certified family nurse practitioner with a practice limited to providing primary health care to individuals and families. |
Mandatory |
Ambulatory |
No |
1905(a)(21), 440.166 |
014 |
Free Standing Birth Center Services |
Services furnished to an individual at a freestanding birth center, which include prenatal labor and delivery, or postpartum care and other ambulatory services related to the health and safety of the individual. |
Mandatory |
Institutional |
No |
1905(a)(28) |
015 |
Home Health Services - Intermittent and Part-time Nursing Services Provided by a Home Health Agency |
Nursing service that is provided on a part-time or intermittent basis by a home health agency or in the absence of an agency in the area, by a registered nurse. |
Mandatory |
Ambulatory |
Yes |
1905(a)(7), 440.70(b)(1), 441.15 |
016 |
Home Health Services - Home Health Aide Services Provided by a Home Health Agency |
Home health aide services provided by a home health agency. |
Mandatory |
Ambulatory |
Yes |
1905(a)(7), 440.70(b)(2), 441.15 |
017 |
Home Health Services - Medical Supplies, Equipment and Appliances Suitable for Use in the Home |
Services include medical supplies, equipment and appliances suitable for use in the home. |
Mandatory |
Ambulatory |
Yes |
1905(a)(7), 440.70(b)(3), 441.15 |
|
Optional Benefits for Categorically Needy (Mandatory and Options for Coverage) and Medically Needy Individuals |
|||||
018 |
Medical Care and Any Type of Remedial Care Recognized Under State Law - Podiatrist Services |
Medical or remedial care or services provided by licensed podiatrists within the scope of practice as defined under state law. |
Optional |
Ambulatory |
No |
1905(a)(6), 440.60 |
019 |
Medical Care and Any Type of Remedial Care Recognized Under State Law - Optometrist Services |
Medical or remedial care or services provided by licensed optometrists within the scope of practice as defined under state law |
Optional |
Ambulatory |
No |
1905(a)(6), 440.60 |
020 |
Medical Care and Any Type of Remedial Care Recognized Under State Law - Chiropractors' Services |
Services provided by licensed chiropractors consisting of treatment by means of manual manipulation of the spine within the scope authorized by the state to perform. |
Optional |
Ambulatory |
No |
1905(a)(6), 440.60 |
021 |
Medical Care and Any Type of Remedial Care Recognized Under State Law - Other Licensed Practitioner Services |
Medical or any other remedial care or services provided by a licensed practitioner within the scope of his/her practice as defined by state law. |
Optional |
Ambulatory |
No |
1905(a)(6), 440.60 |
022 |
Home Health Services - Physical Therapy, Occupational Therapy, Speech Pathology, Audiology Provided by a Home Health Agency |
Physical therapy, occupational therapy, or speech pathology and audiology services provided by a home health agency or by a facility licensed by the state to provide medical rehabilitation services. |
Optional |
Ambulatory |
Yes |
1905(a)(7), 440.70(b)(4), 441.15 |
023 |
Private Duty Nursing Services |
Nursing services, provided by RNs or LPNs, in a home, hospital, or skilled nursing facility, to recipients who require more individual and continuous care than is available from a visiting nurse, or routinely provided by hospital or skilled nursing facility staff. |
Optional |
Ambulatory |
Yes |
1905(a)(8), 440.80 |
024 |
Clinic Services |
Preventive, diagnostic, therapeutic, rehabilitative or palliative services furnished by a facility that is not part of a hospital, but is organized and operated to provide medical care; services provided at the clinic or outside the clinic under the direction of a physician or dentist. |
Optional |
Ambulatory |
No |
1905(a)(9), 440.90 |
025 |
Dental Services |
Diagnostic, preventive, or corrective procedures provided by or under the supervision of a licensed dentist; treatment of the teeth and associated structures of the oral cavity; treatment of disease, injury, or impairment that my affect general health of recipient. |
Optional |
Ambulatory |
No |
1905(a)(10), 440.100 |
026 |
Physical Therapy and Related Services- Physical Therapy |
Services prescribed by a physician or other licensed practitioner of the healing arts, and provided to a recipient by or under the direction of a qualified physical therapist; includes supplies and equipment. |
Optional |
Ambulatory |
Yes |
1905(a)(11), 440.110(a) |
027 |
Physical Therapy and Related Services- Occupational Therapy |
Services provided by a qualified occupational therapist, which have been prescribed by a physician or practitioner of the healing arts; includes supplies and equipment. |
Optional |
Ambulatory |
Yes |
1905(a)(11), 440.110(b) |
028 |
Physical Therapy and Related Services - Services for Individuals with Speech, Hearing and Language Disorders |
Diagnostic, screening, preventive or corrective services for individuals with speech, hearing and language disorders; provided by or under the direction of a certified speech pathologist or audiologist or other licensed practitioner of the healing arts; includes supplies and equipment. |
Optional |
Ambulatory |
Yes |
1905(a)(11), 440.110(c ) |
029 |
Prescribed Drugs, Dentures, and Prosthetic Devices; and Eyeglasses - Prescribed Drugs |
Single or compound substances or mixture of substances prescribed by a physician or licensed practitioner, and dispensed by a licensed pharmacist or authorized practitioner, for the cure, mitigation, or prevention of disease or maintenance of health. |
Optional |
Ambulatory |
No |
1905(a)(12), 440.120(a) |
030 |
Prescribed Drugs, Dentures, and Prosthetic Devices; and Eyeglasses - Dentures |
Artificial structures made by or under the direction of a dentist to replace a full or partial set of teeth. |
Optional |
Ambulatory |
No |
1905(a)(12), 440.120(b) |
031 |
Prescribed Drugs, Dentures, and Prosthetic Devices; and Eyeglasses - Prosthetic Devices |
Replacement, corrective or supportive devices prescribed by a physician or licensed practitioner, to artificially replace a missing portion of the body, prevent or correct physical deformity or malfunction, or to support a weak or deformed portion of the body. |
Optional |
Ambulatory |
No |
1905(a)(12), 440.120(c ) |
032 |
Prescribed Drugs, Dentures, and Prosthetic Devices; and Eyeglasses - Eyeglasses |
Lenses, including frames and other aids to vision, prescribed by a physician skilled in eye disease, or an optometrist. |
Optional |
Ambulatory |
No |
1905(a)(12), 440.120(d) |
033 |
Other Diagnostic, Screening, Preventive, and Rehabilitative Services - Diagnostic Services |
Medical procedures or supplies recommended by a physician or licensed practitioner to enable him/her to identify the existence, nature or extent of illness, injury or other health deviation in a recipient. |
Optional |
Ambulatory |
No |
1905(a)(13), 440.130(a) |
034 |
Other Diagnostic, Screening, Preventive, and Rehabilitative Services - Screening Services |
Use of standardized tests given to a designated population, to detect the existence of one or more particular diseases or health deviations or to identify for more definitive studies individuals suspected of having certain diseases. |
Optional |
Ambulatory |
No |
1905(a)(13), 440.130(b) |
035 |
Other Diagnostic, Screening, Preventive, and Rehabilitative Services - Preventive Services |
Services provided by a physician or other licensed practitioner to prevent disease, disability or other health conditions or their progression, to prolong life and to promote physical and mental health efficiency. |
Optional |
Ambulatory |
No |
1905(a)(13), 440.130(c ) |
036 |
Other Diagnostic, Screening, Preventive, and Rehabilitative Services - Rehabilitative Services |
Medical or remedial services recommended by a physician or other licensed practitioner for maximum reduction of physical or mental health condition, and restoration of a recipient to his/her best possible functional level. |
Optional |
Ambulatory |
Yes |
1905(a)(13), 440.130(d) |
037 |
Services for Individuals Age 65 and Over in IMDs - Inpatient Hospital Services |
Services for the care and treatment of recipients, age 65 and older, in an institution for mental health conditions, provided under the direction of a physician. |
Optional |
Institutional |
Yes |
1905(a)(14), 440.140(a) |
038 |
Services for Individuals Age 65 and Over in IMDs - Nursing Facility Services |
Nursing services needed on a daily basis and required to be provided on an inpatient basis to individuals age 65 and older in an institution for mental health conditions. |
Optional |
Institutional |
Yes |
1905(a)(14), 440.140(b) |
039 |
Intermediate Care Facility Services for Individuals with Intellectual Disabilities (ICF-IID) |
Items and health rehabilitative services provided to persons with intellectual disabilities or related conditions, receiving active treatment in a licensed ICF/IID. |
Optional |
Institutional |
Yes |
1905(a)(15), 440.150 |
040 |
Inpatient Psychiatric Services for Individuals Under 21 |
Inpatient psychiatric services provided to individuals under age 21, under the direction of a physician, furnished in an approved and accredited psychiatric hospital or facility. |
Optional |
Institutional |
Yes |
1905(a)(16), 440.160 |
041 |
Hospice Care Services |
Items and services provided to a terminally ill individual, which includes nursing care, physical or occupational therapy, medical social services, homemaker services, medical supplies and appliances, physician services, short-term inpatient care and counseling. |
Optional |
Both |
Yes |
1905(a)(18) |
042 |
Case Management and TB-Related Services - Case Management and Targeted Case Management Services |
Services to assist eligible individuals who reside in a community setting or are transitioning to a community setting, in gaining access to medical, social, educational, and other services. As specified in a state’s plan, may be offered to individuals within targeted groups. |
Optional |
Ambulatory |
Yes |
1905(a)(19), 440.169, 1915(g) |
043 |
Case Management Services and TB-Related Services -Special TB Related Services |
Services for the treatment of infection with tuberculosis consisting of prescribed drugs, physicians’ services, laboratory and x-ray services (including services to confirm the presence of infection), clinic services and federally-qualified health center services, case management services, and services (other than room and board) designed to encourage completion of regimens of prescribed drugs by outpatients, including services to observe directly the intake of prescribed drugs. |
Optional |
Ambulatory |
No |
1905(a)(19) |
044 |
Respiratory Care Services |
Services provided in home, under the direction of a physician, by a respiratory therapist or other health care professional trained in respiratory therapy, to an individual who is medically dependent on a ventilator for life support for 6 hours or more per day, has been dependent on the ventilator for at least 30 consecutive days as an inpatient in a hospital, NF or ICF/IID, has adequate social support, and wishes to be cared for at home. |
Optional |
Ambulatory |
No |
1905(a)(20), 1902(e)(9)(A)-(C ), 440.185 |
045 |
Personal Care Services |
Services, furnished to an individual who is not an inpatient or resident of a hospital, nursing facility, or intermediate facility for individuals with intellectual and or developmental disabilities, or institution for mental health conditions, that are authorized by a physician in accordance with a plan of treatment, and provided by an individual qualified to provide such services, who is not a legally responsible relative. |
Optional |
Ambulatory |
Yes |
1905(a)(24), 440.167 |
046 |
Primary Care Case Management Services (Integrated Care Model) |
Case management related services which include location, coordination, and monitoring of primary health care services and provider under a contract between the State and either a PCCM who is a physician, or at the State’s option, a physician assistant, nurse practitioner, certified nurse midwife, physician group practice, or an entity that employs or arranges with physicians to furnish services. |
Optional |
Ambulatory |
No |
1905(a)(25), 440.168 |
047 |
Special Sickle-Cell Anemia-Related Services |
Primary and secondary medical strategies and treatment and services for individuals who have Sickle Cell Disease. |
Optional |
Ambulatory |
No |
1905(a)(27) |
048 |
Any other medical care and any other type of remedial care recognized under State law, specified by the Secretary - Transportation |
Expenses for transportation and other related travel expenses determined to be necessary by the agency to secure medical examinations and treatment for a beneficiary. |
Optional, but states are required to assure that transportation is available to and from Medicaid services, either as a State Plan benefit, an administrative activity or under a waiver |
Ambulatory |
No |
1905(a)(29), 440.170(a) |
049 |
Any other medical care and any other type of remedial care recognized under State law, specified by the Secretary - Services provided in religious non-medical health care facilities |
Non-medical services and items, furnished in an institution that is defined in the Internal Revenue Code and is exempt from taxes, to patients who choose to rely solely upon a religious method of healing and for whom the acceptance of medical health services would be inconsistent with their religious beliefs. |
Optional |
Institutional |
Yes |
1905(a)(29), 440.170(b) and (c ) |
050 |
Any other medical care and any other type of remedial care recognized under State law, specified by the Secretary - Nursing facility services for individuals under age 21 |
Services (other than services in an Institution for mental health conditions), furnished to individuals under the age of 21, which are needed on a daily basis and required to be provided in an inpatient basis provided by a Medicaid-approved facility and ordered by and provided under the direction of a physician. |
Optional |
Institutional |
Yes |
1905(a)(29), 440.170(d) |
051 |
Any other medical care and any other type of remedial care recognized under State law, specified by the Secretary - Emergency hospital services |
Services that are necessary to prevent death or serious impairment of health of a recipient, and that the threat to life or health necessitates that use of the most accessible hospital available that is equipped to furnish the services, with no regard to conditions of participation under Medicare or definitions of inpatient or outpatient hospital services. |
Optional |
Ambulatory |
No |
1905(a)(29), 440.170(e) |
052 |
Any other medical care and any other type of remedial care recognized under State law, specified by the Secretary - Critical Access Hospitals |
Services that are furnished by a Medicare participating Critical Access Hospital (CAH) provider and are of a type that would be paid for by Medicare when provided to a Medicare recipient, other than nursing facility services by a CAH with a swing-bed approval. |
Optional |
Institutional |
No |
1905(a)(29), 440.170(g) |
053 |
Extended Services for Pregnant Women - Additional Services for Any Other Medical Conditions That May Complicate Pregnancy |
Extended services for pregnant women - Additional Services for any other medical conditions that may complicate pregnancy, except Pregnancy-related and postpartum services for a 60-day period after the pregnancy ends and any remaining days in the month in which the 60th day falls. (These services will fall into valid value # 71.) |
Optional |
Ambulatory |
No |
1902(a)(10)(end)(V) |
054 |
Community First Choice |
Home and community-based attendant services and supports to assist eligible beneficiaries in accomplishing activities of daily living (ADLs), instrumental activities of daily living (IADLs), and health-related tasks through hands-on assistance, supervision or cueing. |
Optional |
Ambulatory |
No |
1915(k) |
055 |
Health Homes |
Comprehensive and timely high-quality services that are provided by a designated provider, a team of health care professionals operating with such a provider, or a health team. Services include care management, care coordination and promotion, comprehensive transitional care, patient and family support, referral to community and social support services, and use of information technology to link services. |
Optional |
Ambulatory |
No |
1945 |
|
Special Benefit Provisions |
|||||
056 |
Limited Pregnancy-Related Services for Pregnant Women with Income Above the Applicable Income Limit |
Potentially limited services for pregnant women with income above a certain limit to pregnancy-related services that are necessary for the health of the pregnant woman and fetus, or have become necessary as a result of the woman having been pregnant, including, but not limited to prenatal care, delivery, postpartum care, and family planning services. |
|
|
No |
1902(a)(10)(end)(VII), 440.210(a)(2), 440.250(p) |
057 |
Ambulatory prenatal care for pregnant women furnished during a presumptive eligibility period |
Ambulatory prenatal care services provided to an eligible pregnant woman during the PE period, which begins on the date a pregnant woman is determined presumptively eligible by a Medicaid qualified provider based on preliminary information, and ends on the day on which a full determination of eligibility is made or at the end of the month following the month in which the PE determination was made if the woman fails to file an application for full benefits. |
|
|
No |
1920, 1902(a)(47) |
058 |
Benefits for Families Receiving Transitional Medical Assistance |
Benefits provided to families who would have lost eligibility because of hours of, or income from employment of the caretaker relative. Benefits may be limited or provided through alternative methods during the second six months of the 12 month period of extended benefits. |
|
|
|
1925, 1902(a)(52) |
059 |
Standards for Coverage of Transplant Services |
Standards which provide that similarly situated individuals are treated alike and any restriction, on the facilities or practitioners which may provide such procedures, is consistent with accessibility to high quality care. |
|
|
|
1903(i)(1), 441.35 |
060 |
School-Based Services Payment Methodologies |
Provision of benefits in a school-based setting or arranged by a school to a child with a disability even if such services are included in the child's individualized education program (IEP), and to an infant or toddler with a disability even if such services are included in the child's individualized family service plan (IFSP). |
|
|
|
1903(c ) |
061 |
Indian Health Services and Tribal Health Facilities |
Allows for reimbursement of state plan covered services when provided by a facility of the Indian Health Service, including a hospital, nursing facility or any other type of facility which provides covered services under the state plan. |
|
|
|
1911, 431.110(b) |
062 |
Methods and Standards to Assure High Quality Care |
The plan must include a description of methods and standards used to assure that services are of high quality and that the care and services are available under the plan at least to the extent that such care and services are available to the general populations in the geographic area. |
|
|
|
1902(a)(30)(A), 440.260 |
|
Coordination of Medicaid with Medicare and Other Insurance |
|||||
063 |
Medicare Premium Payments |
Provisions related to payment of Medicare A, B and C premiums for qualifying Medicaid beneficiaries. |
|
|
|
1902(a)(10(E ), 1905(p), 1905(s), 1933, 431.625 |
064 |
Medicare Coinsurance and Deductibles |
Provisions for Medicaid payment of Medicare coinsurance and deductibles for individuals dually eligible for Medicare and Medicaid. |
|
|
|
1902(a)(10(E ), 1902(n), 1905(p)(3) and (4) |
065 |
Other Medical Insurance Premium Payments |
Payment of insurance premiums, if cost-effective, for eligible individuals; payment of COBRA premiums; and requirement of enrollment in an employer-sponsored insurance with payment of premiums, if cost-effective. |
|
|
|
1906, 1906A, 1902(a)(10)(F), 1902(u)(1) |
|
Special Benefit Programs |
|||||
066 |
Programs for Distribution of Pediatric Vaccines |
The establishment of a pediatric vaccine distribution program, which provides eligible children with qualified pediatric vaccines. |
Mandatory |
|
|
1928 |
|
Home and Community-Based Services |
|||||
067 |
Laboratory and x-ray services |
|
|
|
|
|
068 |
Home Health Services - Home health aide services provided by a home health agency |
|
|
|
|
|
069 |
Private duty nursing services |
|
|
|
|
|
070 |
Physical Therapy and Related Services - Audiology services |
|
|
|
|
|
071 |
Extended services for pregnant women - Additional Pregnancy-related and postpartum services for a 60-day period after the pregnancy ends and any remaining days in the month in which the 60th day falls. |
|
|
|
|
|
072 |
Home and Community Care for Functionally Disabled Elderly individuals as defined and described in the State Plan |
|
|
|
|
|
073 |
Emergency services for certain legalized aliens and undocumented aliens |
An emergency medical condition is a medical condition (including emergency labor and delivery) manifesting itself by acute symptoms of sufficient severity (including severe pain) such that the absence of immediate medical attention could reasonably be expected to result in placing the patient’s health in serious jeopardy, serious impairment to bodily functions, or serious dysfunction of any bodily organ or part. |
|
|
|
|
074 |
Licensed or Otherwise State-Approved Free-Standing Birthing Center and other ambulatory services that are offered by a freestanding birth center |
|
|
|
|
|
075 |
Homemaker |
|
|
|
|
|
076 |
Home Health Aide |
|
|
|
|
|
077 |
Adult Day Health services |
|
|
|
|
|
078 |
Habilitation |
|
|
|
|
|
079 |
Habilitation: Residential Habilitation |
|
|
|
|
|
080 |
Habilitation: Supported Employment |
|
|
|
|
|
081 |
Habilitation: Education (non IDEA available) |
|
|
|
|
|
082 |
Habilitation: Day Habilitation |
|
|
|
|
|
083 |
Habilitation: Pre-Vocational |
|
|
|
|
|
084 |
Habilitation: Other Habilitative Services |
|
|
|
|
|
085 |
Respite |
|
|
|
|
|
086 |
Day Treatment (mental health service) |
|
|
|
|
|
087 |
Psychosocial rehabilitation |
|
|
|
|
|
088 |
Environmental Modifications (Home Accessibility Adaptations) |
|
|
|
|
|
089 |
Vehicle Modifications |
|
|
|
|
|
090 |
Non-Medical Transportation |
|
|
|
|
|
091 |
Special Medical Equipment (minor assistive Devices) |
|
|
|
|
|
092 |
Home Delivered meals |
|
|
|
|
|
093 |
Assistive Technology (i.e., communication devices) |
|
|
|
|
|
094 |
Personal Emergency Response (PERS) |
|
|
|
|
|
095 |
Nursing Services |
|
|
|
|
|
096 |
Community Transition Services |
|
|
|
|
|
097 |
Adult Foster Care |
|
|
|
|
|
098 |
Day Supports (non-habilitative) |
|
|
|
|
|
099 |
Supported Employment |
|
|
|
|
|
100 |
Supported Living Arrangements |
|
|
|
|
|
101 |
Supports for Consumer Direction (Supports Facilitation) |
|
|
|
|
|
102 |
Participant Directed Goods and Services |
|
|
|
|
|
103 |
Senior Companion (Adult Companion Services) |
|
|
|
|
|
104 |
Assisted Living |
|
|
|
|
|
|
Other |
|||||
105 |
Program for All-inclusive Care for the Elderly (PACE) Services |
|
|
|
|
|
106 |
Self-directed Personal Assistance Services under 1915(j) |
|
|
|
|
|
Appendix I: MBES CBES Category of Service Line Definitions for the 64.9 Base Form
Line |
Line - Form Display |
Line - Definition |
1A |
Inpatient Hospital - Reg. Payments |
1A. - Inpatient Hospital Services.-- Regular Payments.--Other than services in an institution for mental health conditions. (See 42 CFR 440.10). These are services that:
NOTE: Inpatient hospital services do not include NF services furnished by a hospital with swing-bed approval. However, include services provided in a psychiatric wing of a general hospital if the psychiatric wing is not administratively separated from the general hospital. |
1B |
Inpatient Hospital - DSH |
1.B. Inpatient Hospital Services -- DSH Adjustment Payment. - Other than services in an institution for mental health conditions. DSH payments are for the express purpose of assisting hospitals that serve a disproportionate share of low-income patients with special needs and are made in accordance with section 1923 of the Act. Report the total payments that were determined to be disproportionate share payments to the hospital by entering the amounts on the pop-up feeder form which in turn will pre-fill the Form CMS-64.9D as well as the appropriate lines on the Forms CMS-64.9, CMS-64.9P, CMS-64.21, CMS-64.21P, CMS-6421U or CMS-64.21UPs. |
1C |
Inpatient Hospital - Sup. Payments |
1C. - Inpatient Hospital Services.- Supplemental Payments.--Other than services in an institution for mental health conditions. (Refer to the definition on Line 1A above). These are payments made in addition to the standard fee schedule or other standard payment for those services. These payments are separate and apart from regular payments and are based on their own payment methodology. Payments may be made to all providers or targeted to specific groups or classes of providers. Groups may be defined by ownership type (state, county or private) and/or by the other characteristics, e.g., caseload, services or costs. The combined standard payment and supplemental payment cannot exceed the upper payment limit described in 42 CFR 447.272. Address supplemental payments for inpatient hospitals associated with (1) state government operated facilities, (2) non-state government operated facilities, and (3) privately operated facilities by entering payments on the pop-up feeder form. |
1D |
Inpatient Hospital - GME Payments |
1D. - Inpatient Hospital Services.—Graduate Medical Education (GME) Payments.-- GME payments include supplemental payments for direct medical education (DME) (i.e. costs of training physicians such as resident and teaching physician salaries/benefits, overhead and other costs directly related to the program) and indirect medical education (IME) costs hospitals incur for operating teaching programs. Report all supplemental payments for DME and IME that are provided for in the State plan. |
2A |
Mental Health Facility Services - Reg. Payments |
2.A. Mental Health Facility Services - Report Institution for Mental Disease (IMD) (or mental health conditions) services for individuals age 65 or older and/or under age 21 (See 42 CFR 440.140 and 440.160.). Report Other Mental Services which are not provided in an inpatient setting in the Other Appropriate Service categories, e.g., Physician Services, Clinic Services. 1. Mental Health Hospital Services for the Aged.--Refers to those inpatient hospital services provided under the direction of a physician for the care and treatment of recipients in an institution for mental health conditions that meets the Conditions of Participation under 42 CFR Part 482. Institution for mental health conditions means an institution that is primarily engaged in providing diagnosis, treatment, or care of individuals with mental health conditions, including medical care, nursing care, and related services. (See 42 CFR 440.140(a)(2).) 2. NF Services for the Aged.--Means those NF services (as defined at 42 CFR 440.40) and those ICF services (as defined at 42 CFR 483, Subpart B) provided in an institution for mental health conditions to recipients determined to be in need of such services. (See 42 CFR 440.140.) 3. Inpatient Psychiatric Facility Services for Individuals Age 21 and Under. (See 42 CFR 441.151) --Means those services that:
|
2B |
Mental Health Facility - DSH |
2.B. Mental Health Facility Services -- DSH Adjustment Payments.- (See 42 CFR 440.140 and 440.160). DSH payments are for the express purpose of assisting hospitals that serve a disproportionate share of low-income patients with special needs and are made in accordance with section 1923 of the Act. Report the total payments that were determined to be disproportionate share payments to the hospital by entering the amounts on the pop-up feeder form which in turn will pre-fill the Form CMS-64.9D as well as the appropriate lines on the Forms CMS-64.9, CMS-64.9P, CMS-64.21, CMS-64.21P, CMS-6421U or CMS-64.21UPs. |
3A |
Nursing Facility Services - Reg. Payments |
3A. - Nursing Facility Services.--Regular Payments.-- (Other than services in an institution for mental health conditions). (See 42 CFR 483.5 and 440.155). These are services provided by an institution (or a distinct part of an institution) which:
|
3B |
Nursing Facility Services - Sup. Payments |
3B. - Nursing Facility Services - Supplemental Payments.-- (Other than services in an institution for mental health conditions). (Refer to the definition on Line 3A above). These are payments made in addition to the standard fee schedule or other standard payment for those services. These payments are separate and apart from regular payments and are based on their own payment methodology. Payments may be made to all providers or targeted to specific groups or classes of providers. Groups may be defined by ownership type (state, county or private) and/or by the other characteristics, e.g., caseload, services or costs. The combined standard payment and supplemental payment cannot exceed the upper payment limit described in 42 CFR 447.272. Address supplemental payments for nursing facility services associated with
|
4A |
Intermediate Care Facility Services – Individuals with Intellectual Disabilities: Public Providers |
4A Intermediate Care Facility Services - Public Providers – Individuals with Intellectual Disabilities (ICF/IID) (See 42 CFR 440.150). These include services provided in an institution for individuals with intellectual disabilities or persons with related conditions if:
NOTE: Line 4 is divided into sections for public providers (Line 4.A.) and private providers (Line 4.B.). Public providers are owned or operated by a State, county, city or other local governmental agency or instrumentality. Increasing adjustments related to private providers are considered current expenditures for the quarter in which the expenditure was made and are matched at the FMAP rate for that quarter. Increasing adjustments related to public providers are considered adjustments to prior period claims and are matched using the FMAP rate in effect at the earlier of the time the expenditure was paid or recorded by any State agency. (See 45 CFR Part 95 and §2560.) |
4B |
Intermediate Care Facility Services - Individuals with Intellectual Disabilities: Private Providers |
4B --Intermediate Care Facility Services - Private Providers - Individuals with Intellectual Disabilities (ICF/IID). (See 42 CFR 440.150). These include services provided in an institution for individuals with intellectual disabilities or persons with related conditions if:
NOTE: Line 4 is divided into sections for public providers (Line 4.A.) and private providers (Line 4.B.). Public providers are owned or operated by a State, county, city or other local governmental agency or instrumentality. Increasing adjustments related to private providers are considered current expenditures for the quarter in which the expenditure was made and are matched at the FMAP rate for that quarter. Increasing adjustments related to public providers are considered adjustments to prior period claims and are matched using the FMAP rate in effect at the earlier of the time the expenditure was paid or recorded by any State agency. (See 45 CFR Part 95 and §2560.) |
4C |
Intermediate Care Facility Services – Individuals with Intellectual Disabilities: Supplemental Payments |
Line 4C. Intermediate Care Facility Services (ICF/IID) - Supplemental Payments (Refer to the definition on Line 4A above). These are payments made in addition to the standard fee schedule or other standard payment for those services. These payments are separate and apart from regular payments and are based on their own payment methodology. Payments may be made to all providers or targeted to specific groups or classes of providers. Groups may be defined by ownership type (state, county or private) and/or by the other characteristics, e.g., caseload, services or costs. The combined standard payment and supplemental payment cannot exceed the upper payment limit described in 42 CFR 447.272. Address supplemental payments for ICF/IID services associated with (1) state government operated facilities, (2) non-state government operated facilities, and (3) privately operated facilities by entering payments on the pop-up feeder form. |
5A |
Physician & Surgical Services - Reg. Payments |
5A. - Physician and Surgical Services.--Regular Payments.-- (See 42 CFR 440.50.).--Whether furnished in the office, the recipient's home, a hospital, a NF, or elsewhere, physicians' services are services provided:
NOTE: Exclude all services provided and billed for by a hospital, clinic, or laboratory. Include any services provided and billed by a physician under physician services with the exception of lab and X-ray services. Include such services provided and billed for by a physician under the lab and X-ray services category. In a primary care case management system under a Freedom of Choice waiver, you sometimes use a physician as the case manager. In these situations, the physician is allowed to charge a flat fee for each person. Although this fee is not truly a physician service, report the expenditures for the fee on this line. |
5B |
Physician & Surgical Services - Sup. Payments |
5B. - Physician and Surgical Services.--Supplemental Payments.-- (refer to definition for Line 5A above) Payments for physician and other practitioner services as defined in Line 5A that are made in addition to the standard fee schedule payment for those services. When combined with regular payments, these supplemental payments are equal to or less than the Federal upper payment limit. Address supplemental payments for physicians and practitioners associated with
|
5C |
Physician & Surgical Services - Evaluation and Management |
5C. Physician & Surgical Services - Evaluation and Management -- ACA Section 1202 - Services in the category designated Evaluation and Management in the Healthcare Common Procedure Coding System. 100% Federal Share Matching. |
5D |
Physician & Surgical Services - Vaccine codes |
5D. Physician & Surgical Services - Vaccine codes -- ACA Section 1202 - Services related to immunization administration for vaccines and toxoids for which CPT codes 90465, 90466, 90467, 90468, 90471, 90472, 90473, or 90474 (as subsequently modified) apply under such system. 100% Federal Share Matching Rate |
6A |
Outpatient Hospital Services - Reg. Payments |
6A. - Outpatient Hospital Services.--Regular Payments.-- (See 42 CFR 440.20.).--These are preventive, diagnostic, therapeutic, rehabilitative, or palliative services that:
|
6B |
Outpatient Hospital Services - Sup. Payments |
6B. - Outpatient Hospital Services.--Supplemental Payments.-- (refer to definition for Line 6A above) Payments for outpatient hospital services as defined in line 6A that are made in addition to the base fee schedule or other standard payment for those services. These payments are separate and apart from regular payments and are based on their own payment methodology. The combined standard payment and supplemental payment cannot exceed the Federal upper payment limit. Address outpatient hospital services supplemental payments associated with (1) state owned or operated hospitals, (2) non state government owned or operated hospitals and (3) private hospitals by entering payment information on the pop-up feeder sheet. |
7 |
Prescribed Drugs |
7 - Prescribed Drugs. (See 42 CFR 440.120(a).).--These are simple or compound substances or mixtures of substances prescribed for the cure, mitigation, or prevention of disease, or for health maintenance that are:
|
7A1 |
Drug Rebate Offset - National |
7.A.1. Drug Rebate Offset.--This is a refund from the manufacturer to the State Medical Assistance plan for single source drugs, innovator multiple source drugs, and non-innovator multiple source drugs that are dispensed to Medicaid recipients. Rebates are to take place quarterly. Report these offsets as (1) National Agreement or (2) State Sidebar Agreement. National Agreement refers to rebates manufacturers pay your State pursuant to the manufacturers' agreements with CMS under OBRA 1990 provisions. State Sidebar Agreements refer to rebates manufacturers pay under an agreement directly with your State. These may have been entered into before January 1, 1991, the effective date of the OBRA rebate program. Or they may represent agreements your State entered into with a given manufacturer on or after January 1, 1991, under which the manufacturer pays at least as great a rebate as it would under the National Agreement. All States receive rebates under the National Agreements. A few States receive most of their rebates under the National Agreement, but some States receive other rebates under their State Sidebar Agreement with specific manufacturers. All manufacturer rebates received under CMS's National Agreement are reported on Line 7.A.1, National Agreement. All rebates received under State Sidebar Agreements are reported on Line 7.A.2, State Sidebar Agreement. NOTE: Vaccines are not subject to the rebate agreements. |
7A2 |
Drug Rebate Offset - State Sidebar Agreement |
7A2. Drug Rebate Offset.--This is the rebate collected under a separate State agreement Sidebar Agreement. These are rebates received that do not fall under 7A1 (National Drug Rebate). |
7A3 |
MCO - National Agreement |
7.A.3. National Agreement 7A3. Managed Care Organizations (MCO) – National Agreement: The Affordable Care Act requires manufacturers that participate in the Medicaid Drug Rebate Program to pay rebates for drugs dispensed to individuals enrolled with a Medicaid MCO if the MCO is responsible for coverage of such drugs, effective March 23, 2010. This is a refund from the manufacturer to the State Medical Assistance plan for single source drugs, innovator multiple source drugs, and non-innovator multiple source drugs that are dispensed to Medicaid recipients who are enrolled in a Medicaid MCO. Rebates are to take place quarterly. Report these offsets as MCO National Agreement. National Agreement refers to rebates manufacturers pay your State pursuant to the manufacturers agreements with CMS under OBRA 1990 provisions. All States receive rebates under the National Agreement. For rebates for Medicaid MCO drugs, there will be no rebates under their State Sidebar Agreement with specific manufacturers. All MCO manufacturer rebates received under CMS National Agreement are reported on Line 7.A.3, National Agreement NOTE: Vaccines are not subject to the National agreement. |
7A4 |
MCO - State Sidebar Agreement |
7.A.4. MCO State Sidebar Agreement. This is the rebate collected under a separate State agreement Sidebar Agreement. These are rebates received that do not fall under 7A3 (National Drug Rebate). |
7A5 |
Increased ACA OFFSET - Fee for Service - 100% |
7.A.5. Increased ACA OFFSET - Fee for Service - 100% Section 2501 of the Affordable Care Act increased the amount of rebates that drug manufacturers are required to pay under the Medicaid drug rebate program, with different formulas for single source and innovator multiple source drugs (brand name drugs) and noninnovator multiple source drugs (generic drugs), and drugs that are line extensions of a single source drug or an innovator multiple source drug, effective January 1, 2010. The Affordable Care Act also required that amounts “attributable” to these increased rebates be remitted to the Federal Government. Below is a description of how the offset is calculated: Brand name drugs other than blood clotting factors and drugs approved by the Food and Drug Administration (FDA) exclusively for pediatric indications are subject to a minimum rebate percentage of 23.1 percent of AMP:
Brand name drugs that are blood clotting factors and drugs approved by the FDA exclusively for pediatric indications are subject to a minimum rebate percentage of 17.1 percent of AMP:
For a drug that is a line extension of a brand name drug that is an oral solid dosage form, we plan to apply the same offset calculation as described above to the basic rebate. Further, we plan to offset only the difference in the additional rebate of the reformulated drug based on the calculation methodology of the additional rebate for the drug preceding the requirements of the Affordable Care Act and the calculation of the additional rebate for the reformulated drug, if greater, in accordance with the Affordable Care Act. If there is no difference in the additional rebate amount in accordance with the Affordable Care Act, then we do not plan to take any offset amount. For a noninnovator multiple source drug, we plan to offset an amount equal to two percent of the AMP (the difference between 13 percent of AMP and 11 percent of AMP). |
7A6 |
Increased ACA OFFSET - MCO - 100% |
7.A.6. Increased ACA OFFSET - MCO - 100% 7A6. Increased ACA OFFSET – MCO: Similar to the increased ACA offset for fee-for-service, for covered outpatient drugs that are dispensed to Medicaid MCO enrollees, the Affordable Care Act also required that amounts “attributable” to the increased rebates be remitted to the Federal Government. Below is a description of how the offset is calculated: Brand name drugs other than blood clotting factors and drugs approved by the Food and Drug Administration (FDA) exclusively for pediatric indications are subject to a minimum rebate percentage of 23.1 percent of AMP:
Brand name drugs that are blood clotting factors and drugs approved by the FDA exclusively for pediatric indications are subject to a minimum rebate percentage of 17.1 percent of AMP:
For a drug that is a line extension of a brand name drug that is an oral solid dosage form, we plan to apply the same offset calculation as described above to the basic rebate. Further, we plan to offset only the difference in the additional rebate of the reformulated drug based on the calculation methodology of the additional rebate for the drug preceding the requirements of the Affordable Care Act and the calculation of the additional rebate for the reformulated drug, if greater, in accordance with the Affordable Care Act. If there is no difference in the additional rebate amount in accordance with the Affordable Care Act, then we do not plan to take any offset amount. For a noninnovator multiple source drug, we plan to offset an amount equal to two percent of the AMP (the difference between 13 percent of AMP and 11 percent of AMP). |
8 |
Dental Services |
8. Dental Services (See 42 CFR 440.100.).--These are services that are diagnostic, preventive, or corrective procedures provided by, or under the supervision of, a dentist in the practice of his/her profession including treatment of:
Report all EPSDT dental services on this line. Dentist means an individual licensed to practice dentistry or dental surgery. NOTE: Exclude all such services provided as part of inpatient hospital, outpatient hospital, nondental, clinic or laboratory services and billed for by the hospital, nondental clinic, or laboratory. |
9A |
Other Practitioners Services - Reg. Payments |
9A. - Other Practitioners Services - Regular Payments (see CFR 440.60). Any medical or remedial care or services, other than physicians' services, provided by licensed practitioners with the scope of practice defined under State law. Chiropractors' services may be included here as long as the services that (1) are provided by a chiropractor who is licensed by the State and meets standards issued by the Secretary under section 405.232(b), and (2) consists of treatment by means of manual manipulation of the spine that the chiropractor is legally authorized by the State to perform. |
9B |
Other Practitioners Services - Sup. Payments |
9B. - Other Practitioners Services - Supplemental Payments Payments for other practitioner services as defined in Line 9A that are made in addition to the standard fee schedule payment for those services. When combined with regular payments, these supplemental payments are equal to or less than the Federal upper payment limit. Address supplemental payments for other practitioners associated with (1) governmental hospitals or university medical schools, and (2) private hospitals or university medical schools, and (3) other supplemental payments by entering payment information on the pop-up feeder sheet. |
10 |
Clinic Services |
10. Clinic Services (See 42 CFR 440.90.).--These are preventive, diagnostic, therapeutic, rehabilitative, or palliative items or services that:
NOTE: Place dental clinics under Dental Services. Report any services not included above under Other Care Services. A clinic staff may include practitioners with different specialties. |
11 |
Laboratory/Radiological |
11. Laboratory And Radiological Services (See 42 CFR 440.30.).--These are professional, technical laboratory and radiological services:
NOTE: Report X-rays by dentists under Dental Services, Line 8. |
12 |
Home Health Services |
12, Home Health Services (See 42 CFR 440.70.).--These are services provided at the patient's place of residence in compliance with a physician's written plan of care that is renewed every 60 days and includes the following items and services:
Place of residence is normally interpreted to mean the patient's home, and does not apply to hospitals or NFs. Services received in a NF that are different from those normally provided as part of the institution's care may qualify as Home Health Services. For example, a registered nurse may provide short-term care for a recipient in a NF during an acute illness to avoid the recipient's transfer to another NF. |
13 |
Sterilizations |
13. Sterilizations (See 42 CFR 441, Subpart F.).--These are medical procedures, treatments, or operations for the primary purpose of rendering an individual permanently incapable of reproducing. |
14 |
Other Pregnancy-related Procedures |
14. Other Pregnancy-related Procedures (See 42 CFR 441, Subpart E.).--FFP is available when a physician has certified, in writing, to the Medicaid agency, that on the basis of professional judgment the woman suffers from a physical disorder, physical injury, or physical illness, including a life-endangering physical condition caused by or arising from the pregnancy itself, that would, as certified by a physician, place the woman in danger of death unless a termination is performed. The certification must contain the name and address of the patient. The revision to the Hyde Amendment, P.L. 103-112, Health and Human Services Appropriations Bill, made FFP available for expenditures for other pregnancy-related procedures when the pregnancy is a result of an act of rape or incest. This reimbursement is effective for dates of service October 1, 1993 and thereafter. Provide a breakout of the number of other pregnancy-related procedures and associated expenditures in the following cases:
NOTE 1: Report all other pregnancy-related procedures on this line regardless of the type of provider. For prior period adjustments, only include any entry in number of procedures if, for increasing claims, it is a new pregnancy-related procedure that has not been previously reported, or, for decreasing claims, you want to remove a procedure previously claimed. Make no entry in number of procedures if all you are changing is the dollar amount claimed. NOTE 2: The "morning after pill" (ECP) is not considered a termination as it is a contraceptive to prevent pregnancy. However, the drug Mifepristone (RU486) should be counted as an other pregnancy-related procedure as long as all Hyde amendment and other federal requirements are met. |
15 |
EPSDT Screening |
15. EPSDT Screening Services - Physical and mental assessment given to Medicaid eligibles under age 21 to carry out the screening provisions of the EPSDT program. However, the agency must provide at least the following services through consultation with health experts, determine the specific health evaluation procedures to be used, and the mechanisms needed to carry out the screening program.
The above services may be provided by any qualified Medicaid provider. NOTE: Do not include data for dental, hearing, or vision services here. Report dental examinations and preventative dental services on Line 8, Dental Services. Report hearing services, including hearing aids, on Line 32, Services for Speech, Hearing and Language. Report vision services rendered by professionals (e.g. – examinations, etc.) on Line 9, Other Practitioners' Services. Note that the cost of eyeglasses and other aids to vision is to be reported on Line 33, Prosthetic Devices, Dentures, and Eyeglasses. Report other necessary health care according to the appropriate category. |
16 |
Rural Health |
16. Rural Health Clinic (RHC) Services (See 42 CFR 440.20(b).).--If a State permits the delivery of primary care by a nurse practitioner (NP) or physician's assistant (PA), rural health clinic (RHC) means the following services furnished by a RHC that has been certified in accordance with the conditions of 42 CFR Part 491 (Certification of Certain Health Facilities):
|
17A |
Medicare - Part A |
17A. Part A Premiums--(See §301 P.L. 100-360 and §1902 (a)(10) (E)(ii) of the Act)-- Include Part A premiums paid for Qualified Disabled and Working Individuals (QWDIs) under §1902(a)(10)(E)(ii) of the Act. |
17B |
Medicare - Part B |
17B. Part B Premiums--(See §1902(a). Part B Premiums - Include premiums paid through Medicare buy-in under 1843 for Qualified Medicare Beneficiaries (QMBs) under 1902(a)(10)(E)(i),Specified Low-Income Medicare Beneficiaries (SLMBs) under 1902(a)(10)(E)(iii),and other Medicare/Medicaid dual eligibles covered in 1902(a)(10) of the Act. Do not include part B premiums for line 17C (Qualifying Individuals). This amount is shown on the bottom of each monthly bill sent to you on the summary accounting statement Form CMS-1604. |
17C1 |
120% - 134% Of Poverty |
Line 17C.1. - 120% - 134% of Poverty - Include premiums paid for Medicare Part B under §1902(a)(10)(E)(iv)(I). |
17D |
Coinsurance |
17D. Coinsurance and Deductibles-- Include Medicare deductibles and coinsurance required to be paid for QMBs under §1905 (p)(3). (Do not include any Medicare deductibles and coinsurance for other Medicare/Medicaid dual eligibles. Report expenditures for Medicaid services also covered by Medicare under the appropriate Medicaid service category.) Coinsurance is a joint assumption of risk by the insured and the insurer, whereby each shares on a specific basis, the applicable medical expenses of the insured. The insured's share of coinsurance may be paid on his/her behalf. For example, under part B of Medicare, the beneficiary's coinsurance responsibility is a percent of reasonable and customary expenses greater than the stipulated deductible. A deductible is that portion of applicable medical expenses which must be borne by the insured (or be paid on his/her behalf) before insurance benefits for the calendar year begin. EXCEPTION: REPORT ALL OTHER PREGNANCY-RELATED PROCEDURES ON LINE 14. |
18A |
Medicaid - MCO |
18A. Managed Care Organizations (MCOs)-- (See §1903(m)(1)(A) of the Act revised by BBA §4701(b)). - Include capitated payments made to a Medicaid Managed Care Organization which is defined as follows: A Medicaid Managed Care Organization (MCO) means a health maintenance organization, an eligible organization with a contract under §1876 or a Medicare+ Choice organization with a contract under part C of title XVIII, a provider sponsored organization, which meets the requirements of §1902(w)and -
An organization that is a qualified health maintenance organization ( as defined in §1310(d) of the Public Health Service Act) is deemed to meet the requirements of clauses (i) and (ii). |
18A1 |
Medicaid MCO - Evaluation and Management |
18A1. Medicaid MCO - Evaluation and Management -- ACA Section 1202 - Services in the category designated Evaluation and Management in the Healthcare Common Procedure Coding System. 100% Federal Share Matching. |
18A2 |
Medicaid MCO - Vaccine codes |
18A2. Medicaid MCO - Vaccine codes -- ACA Section 1202 - Services related to immunization administration for vaccines and toxoids for which CPT codes 90465, 90466, 90467, 90468, 90471, 90472, 90473, or 90474 (as subsequently modified) apply under such system. 100% Federal Share matching rate |
18A3 |
Medicaid MCO - Community First Choice |
18A3. Medicaid MCO - Community First Choice -- 6% FMAP rate for Total Computable entered at the FMAP Federal Share rate. ACA Section 2401 - The provision established a new Medicaid State Plan option effective October 1, 2011 to allow States to cover HCBS and supports for individuals with incomes not exceeding 150 percent of the FPL, or, if greater, who have been determined to require an institutional level of care. States are provided an additional 6% increase in the FMAP matching funds for services and supports provided to such individuals. |
18A4 |
Medicaid MCO - Preventive Services Grade A OR B, ACIP Vaccines and their Admin |
18A4. Medicaid MCO - Preventive Services Grade A or B, ACIP Vaccines and their Admin -- 1% FMAP rate for Total Computable entered at the FMAP Federal Share rate. As a result of ACA 4106 Any clinical preventive services that are assigned a grade of A or B by the United States Preventive Services Task Force. States get the 1% additional FMAP upon an approved SPA. Effective January 1, 2013 |
18B1 |
Prepaid Ambulatory Health Plan |
A Prepaid Ambulatory Health Plan (PAHP) means an entity that provides medical services to enrollees under contract with the State agency, and on the basis of prepaid capitation payments, or other payment arrangements that do not use State plan payment rates. A PAHP does not provide or arrange for the provision of any inpatient hospital or institutional services for its enrollees, and does not have a comprehensive risk contract. NOTE: Include dental, mental health, transportation and other plans covering limited services (without inpatient hospital or institutional services) under PAHP. |
18B1a |
MCO PAHP - Evaluation and Management |
18B1a. MCO PAHP - Evaluation and Management -- ACA Section 1202 - Services in the category designated Evaluation and Management in the Healthcare Common Procedure Coding System. 100% Federal Share Matching. |
18B1b |
MCO PAHP - Vaccine codes |
18B1b. MCO PAHP - Vaccine codes -- ACA Section 1202 - Services related to immunization administration for vaccines and toxoids for which CPT codes 90465, 90466, 90467, 90468, 90471, 90472, 90473, or 90474 (as subsequently modified) apply under such system. 100% Federal Share matching rate |
18B1c |
MCO PAHP - Community First Choice |
18B1c. MCO PAHP - Community First Choice -- 6% FMAP rate for Total Computable entered at the FMAP Federal Share rate. ACA Section 2401 - The provision established a new Medicaid State Plan option effective October 1, 2011 to allow States to cover HCBS and supports for individuals with incomes not exceeding 150 percent of the FPL, or, if greater, who have been determined to require an institutional level of care. States are provided an additional 6% increase in the FMAP matching funds for services and supports provided to such individuals. |
18B1d |
MCO PAHP - Preventive Services Grade A OR B, ACIP Vaccines and their Admin |
18B1d. MCO PAHP. Preventive Services Grade A OR B, ACIP Vaccines and their Admin -- 1% FMAP rate for Total Computable entered at the FMAP Federal Share rate. As a result of ACA 4106 Any clinical preventive services that are assigned a grade of A or B by the United States Preventive Services Task Force. States get the 1% additional FMAP upon an approved SPA. Effective January 1, |
18B2 |
Prepaid Inpatient Health Plan |
A Prepaid Inpatient Health Plan (PIHP) means an entity that provides medical services to enrollees under contract with the State agency, and on the basis of prepaid capitation payments, or other payment arrangements that do not use State plan payment rates. A PIHP provides, arranges for, or otherwise has responsibility for the provision of any inpatient hospital or institutional services for its enrollees. A PIHP does not have a comprehensive risk contract. NOTE: Include dental, mental health, transportation and other plans covering limited services (with inpatient hospital or institutional services) under PIHP. |
18B2a |
MCO PIHP - Evaluation and Management |
18B2a. MCO PIHP - Evaluation and Management -- ACA Section 1202 - Services in the category designated Evaluation and Management in the Healthcare Common Procedure Coding System. 100% Federal Share Matching. |
18B2b |
MCO PIHP - Vaccine codes |
18B2b. MCO PIHP - Vaccine codes -- ACA Section 1202 - Services related to immunization administration for vaccines and toxoids for which CPT codes 90465, 90466, 90467, 90468, 90471, 90472, 90473, or 90474 (as subsequently modified) apply under such system. 100% Federal Share matching rate |
18B2c |
MCO PIHP - Community First Choice |
18B2c. MCO PIHP - Community First Choice -- 6% FMAP rate for Total Computable entered at the FMAP Federal Share rate. ACA Section 2401 - The provision establishes a new Medicaid State Plan option effective October 1, 2011 to allow States to cover HCBS and supports for individuals with incomes not exceeding 150 percent of the FPL, or, if greater, who have been determined to require an institutional level of care. States are provided an additional 6% increase in the FMAP matching funds for services and supports provided to such individuals. |
18B2d |
MCO PIHP - Preventive Services Grade A OR B, ACIP Vaccines and their Admin |
18B2d. MCO PIHP. Preventive Services Grade A OR B, ACIP Vaccines and their Admin -- 1% FMAP rate for Total Computable entered at the FMAP Federal Share rate. As a result of ACA 4106 Any clinical preventive services that are assigned a grade of A or B by the United States Preventive Services Task Force. States get the 1% additional FMAP upon an approved SPA. Effective January 1, |
18C |
Medicaid - Group Health |
18C. Group Health Plan Payments-- Include payments for premiums for cost effective employer group health insurance under §1906 of the Act. |
18D |
Medicaid - Coinsurance |
18D. Coinsurance and Deductibles-- Include payments for coinsurance and deductibles for cost employer group health insurance under §1906 of the Act. |
18E |
Medicaid - Other |
18E. Other--Include premiums paid for other insurance for medical or any other type of remedial care in order to maintain a third party resource under §1905(a). (Report expenditures here only if you have elected to pay these premiums in item 3.2(a)(2) on page 29b of your State Plan Preprint.) EXCEPTION: REPORT ALL OTHER PREGNANCY-RELATED PROCEDURES ON LINE 14. |
19A |
Home & Community-Based Services - Reg. Pay. (Waiv) |
19A. Home and Community-Based Services (See 42 CFR 440.180.(a).).--These are services furnished under a 1915(c) waiver approved under the provisions in 42 CFR 441, Subpart G (Home and Community-Based Services; Waiver Requirements). NOTE: Report only approved waiver services as designated in the State's approved waiver applications which are provided to eligible waiver recipients. |
19B |
Home & Community-Based Services - St. Plan 1915(i) Only Pay. |
19B. - Other Practitioners Services - State Plan 1915(i) Only Payment. Only the home and community based services elected and defined in the approved State plan may be claimed on this line and form. Enter cost data on the lines in the pop-up feeder sheet that match the services approved in the State plan. |
19C |
Home & Community-Based Services - St. Plan 1915(j) Only Pay. |
19C Home and Community Based Services – State Plan 1915(j) Only Payment – 42 CFR Part 441 – Self-Directed Personal Assistance Services Program State Plan Option. These are PAS services provided under the self-directed service delivery model authorized by 1915(j) including any approved home and community-based services otherwise available under a 1915(c) waiver. The MBES will automatically enter in row 19C the totals from the pop-up 1915(j) Self-Directed Personal Assistance Services Feeder Form. Expenditures for 1915(c) waiver like services provided under 1915(j) Self Direction are entered on the line 19C Feeder Form rather than on the Line 19A Waiver Form which is reserved for approved waiver expenditures. NOTE: 1915(j) services that are using the self-directed service delivery model for State Plan Personal Care and related services should be claimed separately on Line 23B. |
19D |
Home & Community Based Services State Plan 1915(k) Community First Choice |
19D Home and Community Based Services State Plan 1915(k) Community First Choice ACA Section 2401 - The provision established a new Medicaid State Plan option effective October 1, 2011 to allow States to cover HCBS and supports for individuals with incomes not exceeding 150 percent of the FPL, or, if greater, who have been determined to require an institutional level of care. States are provided an additional 6% increase in the FMAP matching funds for services and supports provided to such individuals. |
22 |
All-Inclusive Care Elderly |
22. Programs of All-Inclusive Care for the Elderly (PACE)(See 42 CFR Part 460).--PACE provides pre-paid, capitated, comprehensive health care services designed to enhance the quality of life and autonomy for frail, older adults. Required services (See 42 CFR 460.92) The PACE benefit package for all participants, must include:
NOTE: This is an option within the Medicaid Program to establish Programs of All-Inclusive Care for the Elderly beginning August 5, 1998. (See §1905(a)(26) and §1934 of the Act.) Do not report payments for PACE programs which continue to operate under §1115 authority on this line. Report payments for PACE programs continuing to operate under §1115 waiver authority on the appropriate waiver forms under the appropriate categories of services. |
23A |
Personal Care Services - Reg. Payments |
23A. - Personal Care Services.--Regular Payment.-- (See 42 CFR 440.167).-- Unless defined differently by a State agency for purposes of a waiver granted under Part 441, subpart G of this chapter Personal care services means services furnished to an individual who is not an inpatient or resident of a hospital, nursing facility, intermediate care facility for individuals with intellectual disabilities, or institution for mental health conditions that are--
|
23B |
Personal Care Services - SDS 1915(j) |
23B. - Personal Care Services.--SDS 1915(j).-- (See 42 CFR Part 441).-- Self-Directed Personal Assistance Services (PAS) State Plan Option. These are PAS provided under the self-directed service delivery model authorized by 1915(j) for State plan personal care and related services. NOTE: 1915(j) PAS that are using the self-directed service delivery model for section 1915(c) home and community-based services should be claimed separately on line 19C. |
24A |
Targeted Case Management Services - Com. Case-Man. |
24A. - Targeted Case Management Services (see section 1915(g)(1) of the Social Security Act) are case management services that are furnished without regard to the requirements of section 1902(a)(1) and section 1902(a)(10)(B) to specific classes of individuals or to individuals who reside in specified areas. Case management services means services which will assist individuals eligible under the plan in gaining access to needed medical, social, educational, and other services (See section 1915(g)(2) of the Act). |
24B |
Case Management - State Wide |
24B. - Case Management.--State Wide.-- (See §1915(g)(2) of the Act.).--These are services that assist individuals eligible under the State plan in gaining access to needed medical, social, educational and other services. The agency must permit individuals to freely choose any qualified Medicaid provider when obtaining case management services in accordance with 42 CFR 431.51. |
25 |
Primary Care Case Management |
25. Primary Care Case Management Services (PCCM) (See §1905(a)(25) and §1905 (t)--These are case-management related services (including locating, coordinating, and monitoring of health care services) provided by a primary care case manager under a primary care case management contract. Currently most PCCM programs pay the primary care case manager a monthly case management fee. Report service costs and/or related fees on this line. Report other service costs and/or related fees on the appropriate type of service line. NOTE: Where the fee includes services beyond case management, report the fees under line 18B. |
26 |
Hospice Benefits |
26 - Hospice Benefits (See Section1905(o)(1)(A) of the Act.).--The care described in section 1861(dd)(1) furnished by a hospice program (as defined in section 1861(dd)(2)) to a terminally ill individual who has voluntarily elected to have payment made for hospice care instead of having payment made for certain benefits described under 1812(d)(2)(A) and for which payment may otherwise be made under Title XVIII and intermediate care facility services under the plan. Hospice care may be provided to an individual while such individual is a resident of a skilled nursing facility or intermediate care facility, but the only payment made under the State plan shall be for the hospice care. NOTE: These are services that are:
|
27 |
Emergency Services for Undocumented Aliens |
27. Emergency Services Undocumented Aliens Pursuant to the Act The Medicaid program pays for emergency medical services provided to certain aliens. Section §1903(v) of the Act sates that "...no payment may be made to a State under this section for medical assistance furnished to an alien who is not lawfully admitted... " The only exception is if such care and services are for
|
28 |
Federally-Qualified Health Center |
28. Federally-Qualified Health Center (FQHC) (See §1905(a)(2) of the Act.) --These are services performed by facilities or programs more commonly known as Community Health Centers, Migrant Health Centers, and Health Care for the Homeless Programs. FQHCs qualify to provide covered services under Medicaid if:
|
29 |
Non-Emergency Medical Transportation |
29. - Non-Emergency Medical Transportation (see 42CFR431.53; 440.170; 440.170(a); 440.170(a)(4))--A ride, or reimbursement for a ride, provided so that a Medicaid beneficiary with no other transportation resources can receive services from a medical provider. (NEMT does not include transportation provided on an emergency basis, such as trips to the emergency room for life-threatening situations. NOTE: Transportation provided via the State is consider an administrative cost and should be reported on the form CMS-64.10. |
30 |
Physical Therapy |
30. - Physical Therapy (See 42CFR440.110(a)(1)).--Services prescribed by a physician or other licensed practitioner of the healing arts within the scope of his or her practice under State law and provided to a recipient by or under the direction of a qualified physical therapist. It includes any necessary supplies and equipment. NOTE: Do not include any costs for physical therapy services provided under the school based environment. Those costs should be reported on the pop-up feeder form for Line 39 below. NOTE: Do not include any costs for physical therapy services provided under the rehabilitative services option. Those costs should be reported on the pop-up feeder form for Line 40 below. |
31 |
Occupational Therapy |
31. - Occupational Therapy (see 42CFR440.110(b))--Occupational therapy means services prescribed by a physician or other licensed practitioner of the healing arts within the scope of his or her practice under State law and provided to a recipient by or under the direction of a qualified occupational therapist. It includes any necessary supplies and equipment. NOTE: Do not include any costs for occupational therapy services provided under the school based environment. Those costs should be reported on the pop-up feeder form for Line 39 below. NOTE: Do not include any costs for occupational therapy services provided under the rehabilitative services option. Those costs should be reported on the pop-up feeder form for Line 40 below. |
32 |
Services for Speech, Hearing & Language |
32. - Services for Speech, Hearing and Language--Services for individuals with speech, hearing, and language disorders (See 42CFR440.110(c)). Services for individuals with speech, hearing, and language disorders means diagnostic, screening, preventive, or correction services provided by or under the direction of a speech pathologist or audiologist, for which a patient is referred by a physician or other licensed practitioner of the healing arts within the scope of his or her practice under State law. It includes any necessary supplies and equipment, including hearing aids. NOTE: Do not include any costs for speech and language services provided under the school based environment. Those costs should be reported on the pop-up feeder form for Line 39 below. NOTE: Do not include any costs for speech / language therapy services provided under the rehabilitative services option. Those costs should be reported on the pop-up feeder form for Line 40 below. . It includes any necessary supplies and equipment. |
33 |
Prosthetic Devices, Dentures, Eyeglasses |
Line 33 - Prosthetic Devices, Dentures, Eyeglasses (See 42 CFR 440.120) Prosthetic devises means replacement, corrective, or supportive devices prescribed by a physician or other licensed practitioner to: 1. Artificially replace a missing portion of the body; 2. Prevent or correct physical deformity or malfunction; 3. Support a weak or deformed portion of the body. Dentures are artificial structures made by or under the direction of a dentist to replace a full or partial set of teeth. Eyeglasses means lenses, including frames, and other aids to vision prescribed by a physician skilled in diseases of the eye or an optometrist. |
34 |
Diagnostic Screening & Preventive Services |
34. - Diagnostic Screening & Preventive Services (see 42CFR440.130)
NOTE: This does not include Rehabilitative services - those services are reported on the pop-up feeder sheet for line 40 below. |
34A |
Preventive Services Grade A OR B, ACIP Vaccines and their Admin |
34A. Preventive Services Grade A OR B, ACIP Vaccines and their Admin -- 1% FMAP rate for Total Computable entered at the FMAP Federal Share rate. As a result of ACA 4106- Any clinical preventive services that are assigned a grade of A or B by the United States Preventive Services Task Force. States get the 1% additional FMAP upon an approved SPA. Effective January 1, 2013 |
35 |
Nurse Mid-Wife |
Line 35 - Nurse Mid-Wife (See 42 CFR 440.165) "Nurse-midwife services" means services that are furnished within the scope or practice authorized by State law or regulation and, in the case of inpatient or outpatient hospital services or clinic services, are furnished by or under the direction of a nurse mid-wife to the extent permitted by the facility. Unless required by required by State law or regulations or a facility, are reimbursed without regard to whether the nurse-midwife is under the supervision of, or associated with, a physician or other health care provider. See 42 CFR 441.21 for provisions on independent provider agreements for nurse-midwives. |
36 |
Emergency Hospital Services |
36. - Emergency Hospital Services (See 42 CFR 440.170) Emergency hospital services means services that:
|
37 |
Critical Access Hospitals |
Line 37 - Critical Access Hospitals (See 42 CFR 440.170) -- Critical access hospital services that are furnished by a provider that meet the requirements for participation in Medicare as a CAH (see subpart F of 42 CFR part 485), and (ii) are of a type that would be paid for by Medicare when furnished to a Medicare beneficiary. Inpatient CAH services do not include nursing facility services furnished by a CAH with a swing-bed approval. |
38 |
Nurse Practitioner Services |
Line 38 - Nurse Practitioner Services (See 42 CFR 440.166) Nurse practitioner services means services that are furnished by a registered professional nurse who meets a State's advanced educational and clinical practice requirements, if any, beyond the 2 to 4 years of basic nursing education required of all registered nurses. See 42 CFR 440.166 for requirements related to certified pediatric nurse practitioner and certified family nurse practitioner. |
39 |
School Based Services |
39. - School Based Services (See section 1903(c) of the Act)--These services include medical assistance for covered services (see section 1905(a)) furnished to a child with a disability because such services are included in the child's individualized educational program established pursuant to Part B of the Individuals with Disabilities Education Act or furnished to an infant or toddler with a disability because such services are included in the child's individualized family service plan. |
40 |
Rehabilitative Services (non-school-based) |
40. - Rehabilitative Services (non-school-based) (see 42CFR440.130(d))--Except as otherwise provided under this subpart, rehabilitative services includes any medical or remedial services recommended by a physician or other licensed practitioner of the healing arts, with the scope of his practice under State law, for maximum reduction of physical or mental health condition and restoration of a recipient to his best possible functional level. NOTE: Do not include any costs for rehabilitative services provided under the school based environment which should be reported on Line 39. |
41 |
Private Duty Nursing |
41. - Private Duty Nursing (see 42CFR440.80)--Nursing services for recipients who require more individual and continuous care than is available from a visiting nurse or routinely provided by the nursing staff of the hospital or skilled nursing facility. These services are provided:
|
42 |
Freestanding Birth Center |
Line 42 - Freestanding Birth Center -- COVERAGE FOR FREESTANDING BIRTH CENTER SERVICES Section 2301 of the Affordable Care Act amended section 1905(a) of the Social Security Act (the Act) to provide coverage for freestanding birth center services, as defined in section 1905(l)(3)(A) of the Act. In that provision, the benefit is defined as services furnished at a freestanding birth center, which is defined in new subparagraph 1905(l)(3)(B) as a health facility:
In addition to payment for freestanding birth center facilities, section 1905(l)(3)(C) of the Act requires separate payment for the services furnished by practitioners providing prenatal, labor and delivery, or postpartum care in a freestanding birth center facility, such as nurse midwives and birth attendants. Payment must be made to these practitioners directly, regardless of whether the individual is under the supervision of, or associated with, a physician or other health care provider. It is important to note that section 2301 of the Affordable Care Act does not require States to license or otherwise recognize freestanding birth centers or practitioners who provide services in these facilities if they do not already do so. Coverage and payment are limited to only those facilities and practitioners licensed or otherwise recognized under State law. Prior to passage of the Affordable Care Act, only nurse midwife services were mandatory services under section 1905(a)(17) of the Act and implementing regulations at 42 CFR 440.165. In addition, States had the option to cover the services of other practitioners who are licensed by the State to provide midwifery services such as Certified Professional Midwives (CPM) under section 1905(a)(6) of the Act and implementing regulations at 42 CFR 440.60. These practitioner services are now mandatory when provided in a freestanding birth center as defined above. Further, other practitioner services, such as those furnished by so-called direct entry or lay midwives or birth attendants, who are not licensed but are recognized under State law to provide these services, are now required to be covered when provided in the freestanding birth center. Submission of State Plan Amendments These provisions became effective with the enactment of the Affordable Care Act, beginning March 23, 2010. To implement these provisions, States will need to submit amendments to their State plans that specify coverage and separate reimbursement of freestanding birth center facility services and professional services. Unless the compliance exception discussed below applies, or the State does not license or otherwise recognize freestanding birth centers or practitioners who provide services in these facilities, States must submit a State plan amendment (SPA) not later than the end of the next calendar quarter that follows the date of this guidance. In accordance with section 2301(c) of the Affordable Care Act, States that require State legislation (other than appropriation legislation) to meet the new requirements related to their Medicaid coverage of freestanding birth center services will not be regarded as out of compliance with the standards governing this coverage option as long as they come into compliance not later than the first day of the first calendar quarter beginning after the close of the first regular session of the State legislature that begins after the date of the enactment of the Affordable Care Act. For example, if the next regular legislative session beginning after March 23, 2010, is from January 1 through April 30, 2011, then the State would have until September 30, 2011, to submit the required SPA with an effective date of July 1, 2011. In the case of the State that has a 2-year legislative session, each year is treated as a separate regular session of the State legislature. For example, if a legislature is in session from January 1, 2010, through December 31, 2012, then the State would have until March 31, 2011, to submit a SPA with an effective date that is no later than January 1, 2011. A State should promptly notify its CMS regional office if this compliance exception is applicable. We encourage any State that has questions about this guidance to contact Ms. Vikki Wachino, Director, Family and Children’s Health Programs Group, who may be reached at 410-786-5647. As always, CMS is available to help in making changes to your State plan. Please contact your servicing CMS regional office should you want to schedule a technical assistance session |
43 |
Health Home for Enrollees w Chronic Conditions |
43. Health Home for Enrollees w Chronic Conditions - Health Home services which includes - Comprehensive care Management - Care Coordination - Health promotion - Comprehensive transitional care (Planning and coordination) - Individual and Family Support - Referral to community/social supports - Use of Health Information Technology to link services as feasible and appropriate |
44 |
Tobacco Cessation for Pregnant Women |
44. Tobacco Cessation for Preg Women - ACA Section 4107 Payments for tobacco cessation counseling services for pregnant women and smoking/tobacco cessation outpatient drugs for pregnant women. |
49 |
Other Care Services |
49 -- Other Care Services --These are any medical or remedial care services recognized under State law and authorized by the approved Medicaid State Plan. Such services do not meet the definition of, and are not classified under, any category of service included on Lines 1 through 41. |
50 |
Total |
Line 50 – TOTAL -The MBES automatically enters the total of Columns (a)- (e). |
Appendix J: MBES CBES Category of Service Line Definitions for the 21 Form
Line |
Line - Form Display |
Line - Definition |
1A |
Premiums - Up To 150%: Gross Premiums Paid |
Line 1.A. Gross Premiums Paid.--Report on line 1.A. the amount of expenditures related to premiums paid for children whose family income is up to 150 percent of the Federal poverty level. Use the definition as contained in Part 2 Section 2500.2.E., lines 18.A. -18.E. (Medicaid Health Insurance Payments-Health Maintenance Organizations (HMO), Health Insuring Organization (HIO), Prepaid Health Plans (PHP), Group Health Plan Payments, and Other, respectively) of the State Medicaid Manual. Remember to report the total amount of the premiums. DO NOT NET THE OFFSETS WITH THE PREMIUMS. For example, it costs the State 500 per month per person and there are 100 people under this plan. Assume that the state receives $20 from one of the individuals covered for his share of the cost. Report $50,000 (500 x 100) on Line 1.A. and $20 on Line 1.B. |
1B |
Premiums - Up To 150%: Cost Sharing Offset |
Line 1.B. Cost Sharing Offsets.--Report any cost sharing offset amounts received with respect to the amounts reported on Line 1.A. for children whose family income is up to 150 percent of the Federal poverty level. As indicated above, for line 1.A, the cost sharing offset amounts relate to the expenditures reported on line 1.A. should be reported separately on line 1.B. |
1C |
I Premiums - Over 150%: Gross Premiums Paid |
Line 1.C. Gross Premiums Paid.--For children above 150% of poverty, premiums may be imposed on a sliding scale related to family income. Use the definition as contained in Part 2 Section 2500.2.E., lines 18.A. -.18.E (Medicaid Health Insurance Payments-Health Maintenance Organizations (HMO), Health Insuring Organization (HIO), Prepaid Health Plans (PHP), Group Health Plan Payments, and Other, respectively) of the State Medicaid Manual. DO NOT NET THE OFFSETS WITH THE PREMIUMS For an example see item 1.A. |
1D |
Premiums - Over 150%: Cost Sharing Offset |
Line 1.D. Cost Sharing Offsets.--Report any cost sharing offset amounts received with respect to the amounts reported on line 1.C. for children whose family income is above 150 percent of the Federal poverty level. As indicated above for line 1.A, the cost sharing offset amounts related to the expenditures reported on line 1.A. should be reported separately on line 1.B. NOTE: Line items 1.A. - D. above relate to capitated payments on behalf of CHIP recipients in Managed Care Arrangements. Do not breakout out the amounts reported on lines 1.A.- 1.D. in lines 2 - 26 below, as they relate to expenditures for CHIP recipients in Fee-For-Service Plans. |
2 |
Inpatient Hospital |
Line 2. Inpatient Hospital Services - Regular Payments..--Use the definition as contained in Part 2 Section 2500.2.E., line 1.A. (Inpatient Hospital Services - Regular Payments) of the State Medicaid Manual. |
3 |
Inpatient Mental Health |
Line 3. Inpatient Mental Health Facility Services - Regular Payments..---Use the definition as contained in Part 2 Section 2500.2.E., line 2.A. (Mental Health Facility Services-Regular Payments) of the State Medicaid Manual. |
4 |
Nursing Care Services |
Line 4. Nursing Care Services. - (Other than services in an institution for mental health conditions).---Use the definition as contained in Part 2 Section 2500.2.E., line 29 paragraph g., (Other Care Services- nurse midwife services), of the State Medicaid Manual. |
5 |
Physician/Surgical |
Line 5. Physician and Surgical Services..--Use the definition as contained in Part 2 Section 2500.2.E., line 5. (Physicians’ Services) of the State Medicaid Manual. |
6 |
Outpatient Hospital |
Line 6. Outpatient Hospital Services. .-:-Use the definition as contained in Part 2 Section 2500.2.E., line 6. (Outpatient Hospital Services) of the State Medicaid Manual for services related to non-mental health facilities which are reported on line 7. below. |
7 |
Outpatient Mental Health |
Line 7. Outpatient Mental Health Facility Services. .---Use the definition as contained in Part 2 Section 2500.2.E., line 6 (Outpatient Hospital Services) of the State Medicaid Manual for services related to mental health facilities only. |
8 |
Prescribed Drugs |
Line 8. Prescribed Drugs..--Use the definition as contained in Part 2 Section 2500.2.E., line 7. (Prescribed Drugs) of the State Medicaid Manual. |
8A |
Drug Rebate |
8.A.1. Drug Rebate Offset.--This is a refund from the manufacturer for single source drugs, innovator multiple source drugs, and non-innovator multiple source drugs. |
9 |
Dental Services |
Line 9. Dental Services..--Use the definition as contained in Part 2 Section 2500.2.E., lines 8 (Dental Services) and 29 paragraph e. (Other Care Services-Dentures) of the State Medicaid Manual |
10 |
Vision Services |
Line 10. Vision Services...--Use the definition as contained in Part 2 Section 2500.2.E., line 29. paragraph e., (Other Care Services-eyeglasses) of the State Medicaid Manual. |
11 |
Other Practitioners |
Line 11. Other Practitioners' Services..---Use the definition as contained in Part 2 Section 2500.2.E., lines 9. (Other Practitioners’ Services) and 29 paragraph f. (Other Care Services--diagnostic, screening, rehabilitative, and preventive services) of the State Medicaid Manual. |
12 |
Clinic Services |
Line 12. Clinic Services..--Use the definition as contained in Part 2 Section 2500.2.E., lines 10.(Clinic Services) and 16. (Rural Health Clinic Services) of the State Medicaid Manual. |
13 |
Therapy Services |
Line 13. Therapy Services..---Use the definition as contained in Part 2 Section 2500.2.E., line 29 (Other Care Services) paragraphs b. (Physical Therapy), c. (Occupational Therapy), and d. (Services for individuals with speech, hearing, and language disorders) of the State Medicaid Manual. |
14 |
Laboratory/Radiological |
Line 14. Laboratory And Radiological Services..--Use the definition as contained in Part 2 Section 2500.2.E., line 11. (Laboratory and Radiological Services of the State Medicaid Manual. |
15 |
Medical Equipment |
Line 15. Durable and Disposable Medical Equipment.-Use the definition as contained in Part 2 Section 2500.2.E., line 29. paragraph e. (Other Care Services-prosthetic devices) of the State Medicaid Manual |
16 |
Family Planning |
Line 16.Family Planning..--On the Form HCFA-64.21 series, the reporting on the family planning line 16 is blocked. This is because of the way family planning services are treated with respect to the available FMAP rate and the application of payments against the States’ FY CHIP allotments (refer to SMM §2500.9.I.1. and .2). |
17 |
Other Pregnancy-related Procedures |
Line 17. Other Pregnancy-related Procedures .--Use the definition as contained in Part 2 Section 2500.2.E., line 14. of the State Medicaid Manual. |
18 |
Screening Services |
Line 18. Screening Services..--Use the definition as contained in Part 2 Section 2500.2.E., line 15. (EPSDT Screening Services) of the State Medicaid Manual. |
19 |
Home Health |
Line 19. Home Health Services..---Use the definition as contained in Part 2 Section 2500.2.E., line 12. (Home Health Services) of the State Medicaid Manual. |
20 |
Health Services Initiatives |
Line 20. Health Services Initiatives States may use funds available under their 10 percent administrative cap to fund Health Service Initiatives (HSIs). An HSI is an activity that protects public health, protects the health of individuals, improves or promotes a state's capacity to deliver public health services, or strengthens the human and material resources necessary to accomplish public health goals relating to improving the health of children, including targeted low-income children and other low-income children. States are not limited in the number of different HSIs they may fund, as long as the state ensures that title XXI funding, within the state's 10 percent limit, is sufficient to continue the proper administration of the CHIP program. If such funds become less than sufficient, the state agrees to redirect title XXI funds from the support of HSIs to the administration of the CHIP program. |
21 |
Home and Community |
Line 21. Home and Community-Based Services..---Use the definition as contained in Part 2 Section 2500.2.E., lines 19. (Home and Community-Based Services) and 23. (Personal Care Services) of the State Medicaid Manual. |
22 |
Hospice |
Line 22. Hospice Care Services..--Use the definition as contained in Part 2 Section 2500.2.E., line 26. (Hospice Benefits) of the State Medicaid Manual. |
23 |
Medical Transportation |
Line 23. Medical Transportation Services..--Use the definition as contained in Part 2 Section 2500.2.E., line 29. paragraph a. (Other Care Services-Transportation) of the State Medicaid Manual. |
24 |
Case Management |
Line 24. Case Management Services..--Use the definition as contained in Part 2 Section 2500.2.E., lines 24. (Targeted Case Management Services) and 25 (Primary Care Case Management Services). of the State Medicaid Manual. |
25 |
Translation and Interpretation |
Line 25. Translation and Interpretation (Section 201 CHIPRA) Translation may be allowable as an administrative activity if it is not included and paid for as part of a direct medical service and if it is necessary for the proper and efficient administration of the State plan. However, in order for translation to be claimable as administration, it must be provided either by separate units or separate employees performing solely translation activities and it must facilitate access |
31 |
Other Services |
Line 31. Other Services |
32 |
Outreach |
Outreach Amounts reported on this line should NOT include any amounts reported on Lines 32A or 32B |
32A |
Increased Outreach and Enrollment of Indians |
Line 32.A - Increased Outreach and Enrollment of Indians (Section 202 CHIPRA) )--Enter in Column (a) the total computable amount of expenditures for the Increased Outreach and Enrollment of Indians The MBES will automatically calculate the Federal Share in Columns (b) and (e) at the CHIP rate. These expenditures are NOT applicable to the 10% limit on Outreach and Certain other expenditures. Amounts reported on this line should NOT include any amounts reported on Lines 32 or 32B |
32B |
Increase outreach and enrollment of children through premium subsidies |
Line 32.B - Increase Outreach and Enrollment of children through premium subsidies Amounts reported on this line should NOT include any amounts reported on Lines 32 or 32A |
33 |
Administration |
Line 33. Administration. (section 2105(a)(2)(D) of the Act).--Enter the amount of other reasonable costs incurred by the State to administer the plan. NOTE: All of these administrative activities are subject to the 10 percent limit and must be entered in Column(c). See Section 2115 K above for a discussion of administrative costs and Section 2115 J above for a discussion of the 10 percent limit. |
34 |
PERM Administration |
Line 34 - PERM Administration - (Section 601 CHIPRA) )--Enter in Column (a) the total computable amount of expenditures for the administration of PERM. The MBES will automatically enter in Columns (b) and (e) 90 percent of the amount reported in Column (a). |
35 |
Citizenship Verification Technology CHIPRA |
Line 35. Citizenship Verification Technology- (Section 211 CHIPRA) |
35A |
CVT Development |
Line 35A. CVT Development: (Section 211 CHIPRA)--Enter in Column (a) the total computable amount of expenditures for the design, development, or installation of Citizenship Verification technology. The MBES will automatically enter in Columns (b) and (e) 90 percent of the amount reported in Column (a). |
35B |
CVT Operation |
Line 35B. CVT Operation (Section 211 CHIPRA)--Enter in Column (a) the total computable amount of expenditures for the operation of Citizenship Verification technology. The MBES will automatically enter in Columns (b) and (e) 75 percent of the amount reported in Column (a). |
48 |
Balance |
Line 48 - Balance.--The CBES will generate and enter the subtotal of Lines 1 through 47 for Columns (a)-(e). |
49 |
Less: Collections |
Line 49 - Collections.--Enter the total computable amount of refunds or collections attributable to the CHIP program, e.g., refunds for erroneous payments to providers, tort collections, any cost sharing amounts not included in Lines 1B or 1D, or any other refunds that offset allowable expenditures. |
50 |
Total |
Line 50. Total |
Appendix K: Crosswalk of T-MSIS to MSIS Type of Service Values
Old Code Definitions |
MSIS Old Valid Values |
|
T-MSIS 1.0 Valid Values |
New Code Definitions |
|
T-MSIS 1.1 Valid Values |
New Code Definitions |
Inpatient Hospital |
01 |
|
020 |
Inpatient Hospital Services (General) |
|
001 |
Inpatient hospital services, other than services in an institution for mental diseases |
|
|
|
|
|
|
090 |
Critical access hospital services - IP |
|
|
|
022 |
Inpatient hospital services (physical rehabilitation |
|
|
|
|
|
|
017 |
Anesthesia services |
|
|
|
|
|
|
037 |
Skilled care – hospital residing |
|
091 |
Skilled care – hospital residing |
|
|
|
038 |
Exceptional care – hospital residing |
|
092 |
Exceptional care – hospital residing |
|
|
|
039 |
DD/MI non-acute care – hospital residing |
|
093 |
Non-acute care – hospital residing |
Mental Health Hospital Services for the Aged |
02 |
|
107 |
Mental Health Hospital Services for the Aged |
|
044 |
Inpatient hospital services for individuals age 65 or older in institutions for mental diseases |
|
|
|
|
|
|
045 |
Nursing facility services for individuals age 65 or older in institutions for mental diseases |
Disproportionate Share Hospital (DSH) |
03 |
|
123 |
Disproportionate Share Hospital (DSH) |
|
123 |
Disproportionate Share Hospital (DSH) |
Inpatient Psychiatric Facility Services for Individuals Age 21 Years and Under |
04 |
|
106 |
Inpatient Psychiatric Facility Services for Individuals Age 21 Years and Under |
|
048 |
Inpatient psychiatric services for individuals under age 21 |
ICF Services for Individuals with Mental Health Condition |
05 |
|
105 |
ICF Services for Individuals with Mental Health Condition |
|
046 |
Intermediate care facility (ICF/IIDICF/IID) services |
NF'S - All Other |
07 |
|
108 |
NF'S - All Other |
|
009 |
Nursing facility services for individuals age 21 or older (other than services in an institution for mental disease) |
|
|
|
|
|
|
047 |
Nursing facility services, other than in institutions for mental diseases |
Physicians |
08 |
|
112 |
Physicians |
|
012 |
Physicians’ services |
|
|
|
017 |
Anesthesia services |
|
|
|
Dental |
09 |
|
002 |
Dental Services |
|
029 |
Dental Services |
Other Practitioners |
10 |
|
109 |
Other Practitioners |
|
015 |
Medical or other remedial care or services, other than physicians' services, provided by licensed practitioners within the scope of practice as defined under State law |
Outpatient Hospital |
11 |
|
024 |
Outpatient Services (General) |
|
002 |
Outpatient hospital services |
|
|
|
|
|
|
061 |
Critical access hospital services - OT |
|
|
|
025 |
Outpatient Services (ESRD) |
|
|
|
Clinic |
12 |
|
026 |
General Clinic Services |
|
028 |
Clinic services |
|
|
|
030 |
Healthy Kids Services |
|
041 |
Preventive Services |
|
|
|
027 |
Psychiatric Clinic Services (Type 'A') |
|
|
|
|
|
|
028 |
Psychiatric Clinic Services (Type 'B') |
|
|
|
|
|
|
029 |
Clinic Services (Physical Rehabilitation) |
|
|
|
|
|
|
035 |
Alcohol & Substance Abuse Rehab |
|
014 |
Outpatient Substance Abuse Treatment Services |
Home Health |
13 |
|
124 |
Home Health |
|
016 |
Home health services - Nursing services |
|
|
|
|
|
|
017 |
Home health services - Home health aide services |
|
|
|
|
|
|
018 |
Home health services - Medical supplies, equipment, and appliances suitable for use in the home |
|
|
|
|
|
|
019 |
Home health services - Physical therapy provided by a home health agency or by a facility licensed by the State to provide medical rehabilitation services |
|
|
|
|
|
|
020 |
Home health services - Occupational therapy provided by a home health agency or by a facility licensed by the State to provide medical rehabilitation services |
|
|
|
|
|
|
021 |
Home health services - Speech pathology and audiology services provided by a home health agency or by a facility licensed by the State to provide medical rehabilitation services |
Lab and X-Ray |
15 |
|
043 |
Clinical Laboratory Services |
|
005 |
Professional laboratory services provided by a referral laboratory in an office or similar facility other than a hospital outpatient department or clinic |
|
|
|
|
|
|
006 |
Technical laboratory services provided by a referral laboratory in an office or similar facility other than a hospital outpatient department or clinic |
|
|
|
044 |
Portable X-Ray Services |
|
007 |
Professional radiological services provided by a referral x-ray facility in an office or similar facility other than a hospital outpatient department or clinic |
|
|
|
|
|
|
008 |
Technical radiological services provided by a referral x-ray facility in an office or similar facility other than a hospital outpatient department or clinic |
Prescribed Drugs |
16 |
|
113 |
Prescribed Drugs |
|
033 |
Prescribed drugs |
|
|
|
135 |
Pharmacy OTC |
|
034 |
Over-the-counter medications.
|
|
|
|
041
|
Medical Equipment/Prosthetic devices |
|
036 |
Medical Equipment/Prosthetic devices |
|
|
|
|
|
|
|
|
Other Services |
19 |
|
060 |
Home Care |
|
064 |
HCBS - Home health aide services |
|
|
|
110 |
Other Services |
|
035 |
Dentures |
|
|
|
|
|
|
037 |
Eyeglasses |
|
|
|
|
|
|
062 |
HCBS - Case management services |
|
|
|
|
|
|
063 |
HCBS - Homemaker services |
|
|
|
|
|
|
065 |
HCBS - Personal care services |
|
|
|
|
|
|
066 |
HCBS - Adult day health services |
|
|
|
|
|
|
067 |
HCBS - Habilitation services |
|
|
|
063 |
Respite Care |
|
068 |
HCBS - Respite care services |
|
|
|
|
|
|
069 |
HCBS - Day treatment or other partial hospitalization services, psychosocial rehabilitation services and clinic services (whether or not furnished in a facility) for individuals with chronic mental illness |
|
|
|
|
|
|
073 |
HCBS - Other services requested by the agency and approved by CMS as cost effective and necessary to avoid institutionalization |
|
|
|
|
|
|
074 |
HCBS - Expanded habilitation services - Prevocational services |
|
|
|
|
|
|
075 |
HCBS - Expanded habilitation services - Educational services |
|
|
|
|
|
|
076 |
HCBS - Expanded habilitation services - Supported employment services, which facilitate paid employment |
|
|
|
|
|
|
077 |
HCBS-65-plus - Case management services |
|
|
|
|
|
|
078 |
HCBS-65-plus - Homemaker services |
|
|
|
|
|
|
079 |
HCBS-65-plus - Home health aide services |
|
|
|
|
|
|
080 |
HCBS-65-plus - Personal care services |
|
|
|
|
|
|
081 |
HCBS-65-plus - Adult day health services |
|
|
|
063 |
Respite Care |
|
082 |
HCBS-65-plus - Respite care services |
|
|
|
|
|
|
083 |
HCBS-65-plus - Other medical and social services requested by the Medicaid agency and approved by CMS, which will contribute to the health and well-being of individuals and their ability to reside in a community-based care setting |
Capitated Payment s to HMO, HIO or PACE Plan |
20 |
|
119 |
Capitated Payment s to HMO, HIO or PACE Plan |
|
119 |
Capitated payments to HMOs, HIOs, or PACE plans |
Capitated Payments to Prepaid Health Plans (PHPs) |
21 |
|
122 |
Capitated Payments to Prepaid Health Plans (PHPs) |
|
122 |
Capitated payments to prepaid health plans (PHPs) |
Capitated Payments for Primary Care Case Management (PCCM) |
22 |
|
120 |
Capitated Payments for Primary Care Case Management (PCCM) |
|
120 |
Capitated payments for primary care case management (PCCM) |
Capitated Payments for Private Health Insurance |
23 |
|
121 |
Capitated Payments for Private Health Insurance |
|
121 |
Capitated payments for private health insurance |
Sterilizations |
24 |
|
116 |
Sterilizations |
|
084 |
Sterilizations |
Other Pregnancy-related Procedures |
25 |
|
100 |
Other Pregnancy-related Procedures |
|
086 |
Other Pregnancy-related Procedures |
Transportation Services |
26 |
|
118 |
Transportation Services |
|
056 |
Transportation services |
Personal Care Services |
30 |
|
111 |
Personal Care Services |
|
051 |
Personal care services |
Targeted Case Management |
31 |
|
117 |
Targeted Case Management |
|
053 |
Targeted case management services |
|
|
|
068 |
Targeted Care Management |
|
|
|
Rehabilitation Services |
33 |
|
114 |
Rehabilitation Services |
|
043 |
Rehabilitative services |
PT, OT, Speech, Hearing Language |
34 |
|
011 |
Physical Therapy Services |
|
030 |
Physical therapy services (when not provided under home health services) |
|
|
|
012 |
Occupational Therapy Services |
|
031 |
Occupational therapy services (when not provided under home health services) |
|
|
|
013 |
Speech Therapy/Pathology Services |
|
032 |
Speech, hearing, and language disorders services (when not provided under home health services) |
|
|
|
014 |
Audiology Services |
|
032 |
Speech, hearing, and language disorders services (when not provided under home health services) |
Hospice Benefits |
35 |
|
104 |
Hospice Benefits |
|
087 |
Hospice Benefits |
Nurse Midwife Services |
36 |
|
018 |
Midwife Services |
|
025 |
Nurse-midwife service |
Nurse Practitioner Services |
37 |
|
057 |
Nurse Practitioner Services |
|
026 |
Nurse practitioner services |
|
|
|
010 |
Nursing Services |
|
|
|
Private Duty Nursing |
38 |
|
129 |
Private Duty Nursing |
|
022 |
Private duty nursing services |
Religious Non-Medical Health Care Institutions |
39 |
|
131 |
Religious Non-Medical Health Care Institutions |
|
058 |
Services furnished in a religious nonmedical health care institution |
Supplemental Payment - Inpatient |
40 |
|
132 |
Supplemental Payment - Inpatient |
|
132 |
Supplemental payment – inpatient |
Supplemental Payment - Nursing |
41 |
|
133 |
Supplemental Payment - Nursing |
|
133 |
Supplemental payment – nursing |
Supplemental Payment - Outpatient |
42 |
|
134 |
Supplemental Payment - Outpatient |
|
134 |
Supplemental payment – outpatient |
Durable Medical Equipment and Supplies (including emergency response systems and home modifications) |
51 |
|
103 |
Durable Medical Equipment and Supplies (including emergency response systems and home modifications) |
|
018 |
Home health services - Medical supplies, equipment, and appliances suitable for use in the home |
Residential Care |
52 |
|
115 |
Residential Care |
|
115 |
Residential Care |
Psychiatric services (excluding adult day care) |
53 |
|
130 |
Psychiatric services (excluding adult day care) |
|
048 |
Inpatient psychiatric services for individuals under age 21 |
Adult Day Care |
54 |
|
101 |
Adult Day Care |
|
066 |
HCBS - Adult day health services |
|
|
|
|
|
|
069 |
HCBS - Day treatment or other partial hospitalization services, psychosocial rehabilitation services and clinic services (whether or not furnished in a facility) for individuals with chronic mental illness |
Indian Health Service (IHS) - Family Plan |
60 |
|
127 |
Indian Health Service (IHS) - Family Plan |
|
011 |
Family planning services and supplies for individuals of child-bearing age |
Indian Health Service (IHS) - BCC |
61 |
|
125 |
Indian Health Service (IHS) - BCC |
|
004 |
Other ambulatory services furnished by a rural health clinic |
Indian Health Service (IHS) - BIP |
62 |
|
126 |
Indian Health Service (IHS) - BIP |
|
004 |
Other ambulatory services furnished by a rural health clinic |
Appendix L: Crosswalk of Washington Publishing Company Provider Taxonomy Codes to Provider Facility Type Categories
Source: |
Provider Taxonomy Code |
Provider Taxonomy Description |
Provider Facility Type Code |
Provider Facility Type Description |
193200000X |
Unspecified Multi-Specialty Group |
100000000 |
Individuals or Groups (of Individuals) |
193400000X |
Unspecified Single Specialty Group |
100000000 |
Individuals or Groups (of Individuals) |
207K00000X |
Allergy & Immunology |
100000000 |
Individuals or Groups (of Individuals) |
207KA0200X |
Allergy |
100000000 |
Individuals or Groups (of Individuals) |
207KI0005X |
Clinical & Laboratory Immunology |
100000000 |
Individuals or Groups (of Individuals) |
207L00000X |
Anesthesiology |
100000000 |
Individuals or Groups (of Individuals) |
207LA0401X |
Addiction Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207LC0200X |
Critical Care Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207LH0002X |
Hospice and Palliative Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207LP2900X |
Pain Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207LP3000X |
Pediatric Anesthesiology |
100000000 |
Individuals or Groups (of Individuals) |
208U00000X |
Clinical Pharmacology |
100000000 |
Individuals or Groups (of Individuals) |
208C00000X |
Colon & Rectal Surgery |
100000000 |
Individuals or Groups (of Individuals) |
207N00000X |
Dermatology |
100000000 |
Individuals or Groups (of Individuals) |
207NI0002X |
Clinical & Laboratory Dermatological Immunology |
100000000 |
Individuals or Groups (of Individuals) |
207ND0900X |
Dermatopathology |
100000000 |
Individuals or Groups (of Individuals) |
207ND0101X |
MOHS-Micrographic Surgery |
100000000 |
Individuals or Groups (of Individuals) |
207NP0225X |
Pediatric Dermatology |
100000000 |
Individuals or Groups (of Individuals) |
207NS0135X |
Procedural Dermatology |
100000000 |
Individuals or Groups (of Individuals) |
204R00000X |
Electrodiagnostic Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207P00000X |
Emergency Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207PE0004X |
Emergency Medical Services |
100000000 |
Individuals or Groups (of Individuals) |
207PH0002X |
Hospice and Palliative Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207PT0002X |
Medical Toxicology |
100000000 |
Individuals or Groups (of Individuals) |
207PP0204X |
Pediatric Emergency Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207PS0010X |
Sports Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207PE0005X |
Undersea and Hyperbaric Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207Q00000X |
Family Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207QA0401X |
Addiction Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207QA0000X |
Adolescent Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207QA0505X |
Adult Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207QB0002X |
Bariatric Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207QG0300X |
Geriatric Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207QH0002X |
Hospice and Palliative Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207QS1201X |
Sleep Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207QS0010X |
Sports Medicine |
100000000 |
Individuals or Groups (of Individuals) |
208D00000X |
General Practice |
100000000 |
Individuals or Groups (of Individuals) |
208M00000X |
Hospitalist |
100000000 |
Individuals or Groups (of Individuals) |
202C00000X |
Independent Medical Examiner |
100000000 |
Individuals or Groups (of Individuals) |
207R00000X |
Internal Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207RA0401X |
Addiction Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207RA0000X |
Adolescent Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207RA0201X |
Allergy & Immunology |
100000000 |
Individuals or Groups (of Individuals) |
207RB0002X |
Bariatric Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207RC0000X |
Cardiovascular Disease |
100000000 |
Individuals or Groups (of Individuals) |
207RI0001X |
Clinical & Laboratory Immunology |
100000000 |
Individuals or Groups (of Individuals) |
207RC0001X |
Clinical Cardiac Electrophysiology |
100000000 |
Individuals or Groups (of Individuals) |
207RC0200X |
Critical Care Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207RE0101X |
Endocrinology, Diabetes & Metabolism |
100000000 |
Individuals or Groups (of Individuals) |
207RG0100X |
Gastroenterology |
100000000 |
Individuals or Groups (of Individuals) |
207RG0300X |
Geriatric Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207RH0000X |
Hematology |
100000000 |
Individuals or Groups (of Individuals) |
207RH0003X |
Hematology & Oncology |
100000000 |
Individuals or Groups (of Individuals) |
207RI0008X |
Hepatology |
100000000 |
Individuals or Groups (of Individuals) |
207RH0002X |
Hospice and Palliative Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207RH0005X |
Hypertension Specialist |
100000000 |
Individuals or Groups (of Individuals) |
207RI0200X |
Infectious Disease |
100000000 |
Individuals or Groups (of Individuals) |
207RI0011X |
Interventional Cardiology |
100000000 |
Individuals or Groups (of Individuals) |
207RM1200X |
Magnetic Resonance Imaging (MRI) |
100000000 |
Individuals or Groups (of Individuals) |
207RX0202X |
Medical Oncology |
100000000 |
Individuals or Groups (of Individuals) |
207RN0300X |
Nephrology |
100000000 |
Individuals or Groups (of Individuals) |
207RP1001X |
Pulmonary Disease |
100000000 |
Individuals or Groups (of Individuals) |
207RR0500X |
Rheumatology |
100000000 |
Individuals or Groups (of Individuals) |
207RS0012X |
Sleep Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207RS0010X |
Sports Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207RT0003X |
Transplant Hepatology |
100000000 |
Individuals or Groups (of Individuals) |
209800000X |
Legal Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207SG0202X |
Clinical Biochemical Genetics |
100000000 |
Individuals or Groups (of Individuals) |
207SC0300X |
Clinical Cytogenetic |
100000000 |
Individuals or Groups (of Individuals) |
207SG0201X |
Clinical Genetics (M.D.) |
100000000 |
Individuals or Groups (of Individuals) |
207SG0203X |
Clinical Molecular Genetics |
100000000 |
Individuals or Groups (of Individuals) |
207SM0001X |
Molecular Genetic Pathology |
100000000 |
Individuals or Groups (of Individuals) |
207SG0205X |
Ph.D. Medical Genetics |
100000000 |
Individuals or Groups (of Individuals) |
207T00000X |
Neurological Surgery |
100000000 |
Individuals or Groups (of Individuals) |
207U00000X |
Nuclear Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207UN0903X |
In Vivo & In Vitro Nuclear Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207UN0901X |
Nuclear Cardiology |
100000000 |
Individuals or Groups (of Individuals) |
207UN0902X |
Nuclear Imaging & Therapy |
100000000 |
Individuals or Groups (of Individuals) |
204D00000X |
Neuromusculoskeletal Medicine & OMM |
100000000 |
Individuals or Groups (of Individuals) |
204C00000X |
Neuromusculoskeletal Medicine, Sports Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207V00000X |
Obstetrics & Gynecology |
100000000 |
Individuals or Groups (of Individuals) |
207VB0002X |
Bariatric Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207VC0200X |
Critical Care Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207VF0040X |
Female Pelvic Medicine and Reconstructive Surgery |
100000000 |
Individuals or Groups (of Individuals) |
207VX0201X |
Gynecologic Oncology |
100000000 |
Individuals or Groups (of Individuals) |
207VG0400X |
Gynecology |
100000000 |
Individuals or Groups (of Individuals) |
207VH0002X |
Hospice and Palliative Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207VM0101X |
Maternal & Fetal Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207VX0000X |
Obstetrics |
100000000 |
Individuals or Groups (of Individuals) |
207VE0102X |
Reproductive Endocrinology |
100000000 |
Individuals or Groups (of Individuals) |
207W00000X |
Ophthalmology |
100000000 |
Individuals or Groups (of Individuals) |
204E00000X |
Oral & Maxillofacial Surgery |
100000000 |
Individuals or Groups (of Individuals) |
207X00000X |
Orthopaedic Surgery |
100000000 |
Individuals or Groups (of Individuals) |
207XS0114X |
Adult Reconstructive Orthopaedic Surgery |
100000000 |
Individuals or Groups (of Individuals) |
207XX0004X |
Foot and Ankle Surgery |
100000000 |
Individuals or Groups (of Individuals) |
207XS0106X |
Hand Surgery |
100000000 |
Individuals or Groups (of Individuals) |
207XS0117X |
Orthopaedic Surgery of the Spine |
100000000 |
Individuals or Groups (of Individuals) |
207XX0801X |
Orthopaedic Trauma |
100000000 |
Individuals or Groups (of Individuals) |
207XP3100X |
Pediatric Orthopaedic Surgery |
100000000 |
Individuals or Groups (of Individuals) |
207XX0005X |
Sports Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207Y00000X |
Otolaryngology |
100000000 |
Individuals or Groups (of Individuals) |
207YS0123X |
Facial Plastic Surgery |
100000000 |
Individuals or Groups (of Individuals) |
207YX0602X |
Otolaryngic Allergy |
100000000 |
Individuals or Groups (of Individuals) |
207YX0905X |
Otolaryngology/Facial Plastic Surgery |
100000000 |
Individuals or Groups (of Individuals) |
207YX0901X |
Otology & Neurotology |
100000000 |
Individuals or Groups (of Individuals) |
207YP0228X |
Pediatric Otolaryngology |
100000000 |
Individuals or Groups (of Individuals) |
207YX0007X |
Plastic Surgery within the Head & Neck |
100000000 |
Individuals or Groups (of Individuals) |
207YS0012X |
Sleep Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207ZP0101X |
Anatomic Pathology |
100000000 |
Individuals or Groups (of Individuals) |
207ZP0102X |
Anatomic Pathology & Clinical Pathology |
100000000 |
Individuals or Groups (of Individuals) |
207ZB0001X |
Blood Banking & Transfusion Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207ZP0104X |
Chemical Pathology |
100000000 |
Individuals or Groups (of Individuals) |
207ZC0006X |
Clinical Pathology |
100000000 |
Individuals or Groups (of Individuals) |
207ZP0105X |
Clinical Pathology/Laboratory Medicine |
100000000 |
Individuals or Groups (of Individuals) |
207ZC0500X |
Cytopathology |
100000000 |
Individuals or Groups (of Individuals) |
207ZD0900X |
Dermatopathology |
100000000 |
Individuals or Groups (of Individuals) |
207ZF0201X |
Forensic Pathology |
100000000 |
Individuals or Groups (of Individuals) |
207ZH0000X |
Hematology |
100000000 |
Individuals or Groups (of Individuals) |
207ZI0100X |
Immunopathology |
100000000 |
Individuals or Groups (of Individuals) |
207ZM0300X |
Medical Microbiology |
100000000 |
Individuals or Groups (of Individuals) |
207ZP0007X |
Molecular Genetic Pathology |
100000000 |
Individuals or Groups (of Individuals) |
207ZN0500X |
Neuropathology |
100000000 |
Individuals or Groups (of Individuals) |
207ZP0213X |
Pediatric Pathology |
100000000 |
Individuals or Groups (of Individuals) |
208000000X |
Pediatrics |
100000000 |
Individuals or Groups (of Individuals) |
2080A0000X |
Adolescent Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2080C0008X |
Child Abuse Pediatrics |
100000000 |
Individuals or Groups (of Individuals) |
2080I0007X |
Clinical & Laboratory Immunology |
100000000 |
Individuals or Groups (of Individuals) |
2080P0006X |
Developmental – Behavioral Pediatrics |
100000000 |
Individuals or Groups (of Individuals) |
2080H0002X |
Hospice and Palliative Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2080T0002X |
Medical Toxicology |
100000000 |
Individuals or Groups (of Individuals) |
2080N0001X |
Neonatal-Perinatal Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2080P0008X |
Neurodevelopmental Disabilities |
100000000 |
Individuals or Groups (of Individuals) |
2080P0201X |
Pediatric Allergy/Immunology |
100000000 |
Individuals or Groups (of Individuals) |
2080P0202X |
Pediatric Cardiology |
100000000 |
Individuals or Groups (of Individuals) |
2080P0203X |
Pediatric Critical Care Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2080P0204X |
Pediatric Emergency Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2080P0205X |
Pediatric Endocrinology |
100000000 |
Individuals or Groups (of Individuals) |
2080P0206X |
Pediatric Gastroenterology |
100000000 |
Individuals or Groups (of Individuals) |
2080P0207X |
Pediatric Hematology-Oncology |
100000000 |
Individuals or Groups (of Individuals) |
2080P0208X |
Pediatric Infectious Diseases |
100000000 |
Individuals or Groups (of Individuals) |
2080P0210X |
Pediatric Nephrology |
100000000 |
Individuals or Groups (of Individuals) |
2080P0214X |
Pediatric Pulmonology |
100000000 |
Individuals or Groups (of Individuals) |
2080P0216X |
Pediatric Rheumatology |
100000000 |
Individuals or Groups (of Individuals) |
2080T0004X |
Pediatric Transplant Hepatology |
100000000 |
Individuals or Groups (of Individuals) |
2080S0012X |
Sleep Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2080S0010X |
Sports Medicine |
100000000 |
Individuals or Groups (of Individuals) |
202K00000X |
Phlebology |
100000000 |
Individuals or Groups (of Individuals) |
208100000X |
Physical Medicine & Rehabilitation |
100000000 |
Individuals or Groups (of Individuals) |
2081H0002X |
Hospice and Palliative Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2081N0008X |
Neuromuscular Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2081P2900X |
Pain Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2081P0010X |
Pediatric Rehabilitation Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2081P0004X |
Spinal Cord Injury Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2081S0010X |
Sports Medicine |
100000000 |
Individuals or Groups (of Individuals) |
208200000X |
Plastic Surgery |
100000000 |
Individuals or Groups (of Individuals) |
2082S0099X |
Plastic Surgery Within the Head and Neck |
100000000 |
Individuals or Groups (of Individuals) |
2082S0105X |
Surgery of the Hand |
100000000 |
Individuals or Groups (of Individuals) |
2083A0100X |
Aerospace Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2083T0002X |
Medical Toxicology |
100000000 |
Individuals or Groups (of Individuals) |
2083X0100X |
Occupational Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2083P0500X |
Preventive Medicine/Occupational Environmental Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2083P0901X |
Public Health & General Preventive Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2083S0010X |
Sports Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2083P0011X |
Undersea and Hyperbaric Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2084A0401X |
Addiction Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2084P0802X |
Addiction Psychiatry |
100000000 |
Individuals or Groups (of Individuals) |
2084B0002X |
Bariatric Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2084B0040X |
Behavioral Neurology & Neuropsychiatry |
100000000 |
Individuals or Groups (of Individuals) |
2084P0804X |
Child & Adolescent Psychiatry |
100000000 |
Individuals or Groups (of Individuals) |
2084N0600X |
Clinical Neurophysiology |
100000000 |
Individuals or Groups (of Individuals) |
2084D0003X |
Diagnostic Neuroimaging |
100000000 |
Individuals or Groups (of Individuals) |
2084F0202X |
Forensic Psychiatry |
100000000 |
Individuals or Groups (of Individuals) |
2084P0805X |
Geriatric Psychiatry |
100000000 |
Individuals or Groups (of Individuals) |
2084H0002X |
Hospice and Palliative Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2084P0005X |
Neurodevelopmental Disabilities |
100000000 |
Individuals or Groups (of Individuals) |
2084N0400X |
Neurology |
100000000 |
Individuals or Groups (of Individuals) |
2084N0402X |
Neurology with Special Qualifications in Child Neurology |
100000000 |
Individuals or Groups (of Individuals) |
2084N0008X |
Neuromuscular Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2084P2900X |
Pain Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2084P0800X |
Psychiatry |
100000000 |
Individuals or Groups (of Individuals) |
2084P0015X |
Psychosomatic Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2084S0012X |
Sleep Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2084S0010X |
Sports Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2084V0102X |
Vascular Neurology |
100000000 |
Individuals or Groups (of Individuals) |
208VP0014X |
Interventional Pain Medicine |
100000000 |
Individuals or Groups (of Individuals) |
208VP0000X |
Pain Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2085B0100X |
Body Imaging |
100000000 |
Individuals or Groups (of Individuals) |
2085D0003X |
Diagnostic Neuroimaging |
100000000 |
Individuals or Groups (of Individuals) |
2085R0202X |
Diagnostic Radiology |
100000000 |
Individuals or Groups (of Individuals) |
2085U0001X |
Diagnostic Ultrasound |
100000000 |
Individuals or Groups (of Individuals) |
2085H0002X |
Hospice and Palliative Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2085N0700X |
Neuroradiology |
100000000 |
Individuals or Groups (of Individuals) |
2085N0904X |
Nuclear Radiology |
100000000 |
Individuals or Groups (of Individuals) |
2085P0229X |
Pediatric Radiology |
100000000 |
Individuals or Groups (of Individuals) |
2085R0001X |
Radiation Oncology |
100000000 |
Individuals or Groups (of Individuals) |
2085R0205X |
Radiological Physics |
100000000 |
Individuals or Groups (of Individuals) |
2085R0203X |
Therapeutic Radiology |
100000000 |
Individuals or Groups (of Individuals) |
2085R0204X |
Vascular & Interventional Radiology |
100000000 |
Individuals or Groups (of Individuals) |
208600000X |
Surgery |
100000000 |
Individuals or Groups (of Individuals) |
2086H0002X |
Hospice and Palliative Medicine |
100000000 |
Individuals or Groups (of Individuals) |
2086S0120X |
Pediatric Surgery |
100000000 |
Individuals or Groups (of Individuals) |
2086S0122X |
Plastic and Reconstructive Surgery |
100000000 |
Individuals or Groups (of Individuals) |
2086S0105X |
Surgery of the Hand |
100000000 |
Individuals or Groups (of Individuals) |
2086S0102X |
Surgical Critical Care |
100000000 |
Individuals or Groups (of Individuals) |
2086X0206X |
Surgical Oncology |
100000000 |
Individuals or Groups (of Individuals) |
2086S0127X |
Trauma Surgery |
100000000 |
Individuals or Groups (of Individuals) |
2086S0129X |
Vascular Surgery |
100000000 |
Individuals or Groups (of Individuals) |
208G00000X |
Thoracic Surgery (Cardiothoracic Vascular Surgery) |
100000000 |
Individuals or Groups (of Individuals) |
204F00000X |
Transplant Surgery |
100000000 |
Individuals or Groups (of Individuals) |
208800000X |
Urology |
100000000 |
Individuals or Groups (of Individuals) |
2088F0040X |
Female Pelvic Medicine and Reconstructive Surgery |
100000000 |
Individuals or Groups (of Individuals) |
2088P0231X |
Pediatric Urology |
100000000 |
Individuals or Groups (of Individuals) |
103K00000X |
Behavioral Analyst |
100000000 |
Individuals or Groups (of Individuals) |
103G00000X |
Clinical Neuropsychologist |
100000000 |
Individuals or Groups (of Individuals) |
103GC0700X |
Clinical |
100000000 |
Individuals or Groups (of Individuals) |
101Y00000X |
Counselor |
100000000 |
Individuals or Groups (of Individuals) |
101YA0400X |
Addiction (Substance Use Disorder) |
100000000 |
Individuals or Groups (of Individuals) |
101YM0800X |
Mental Health |
100000000 |
Individuals or Groups (of Individuals) |
101YP1600X |
Pastoral |
100000000 |
Individuals or Groups (of Individuals) |
101YP2500X |
Professional |
100000000 |
Individuals or Groups (of Individuals) |
101YS0200X |
School |
100000000 |
Individuals or Groups (of Individuals) |
106H00000X |
Marriage & Family Therapist |
100000000 |
Individuals or Groups (of Individuals) |
102X00000X |
Poetry Therapist |
100000000 |
Individuals or Groups (of Individuals) |
102L00000X |
Psychoanalyst |
100000000 |
Individuals or Groups (of Individuals) |
103T00000X |
Psychologist |
100000000 |
Individuals or Groups (of Individuals) |
103TA0400X |
Addiction (Substance Use Disorder) |
100000000 |
Individuals or Groups (of Individuals) |
103TA0700X |
Adult Development & Aging |
100000000 |
Individuals or Groups (of Individuals) |
103TC0700X |
Clinical |
100000000 |
Individuals or Groups (of Individuals) |
103TC2200X |
Clinical Child & Adolescent |
100000000 |
Individuals or Groups (of Individuals) |
103TB0200X |
Cognitive & Behavioral |
100000000 |
Individuals or Groups (of Individuals) |
103TC1900X |
Counseling |
100000000 |
Individuals or Groups (of Individuals) |
103TE1000X |
Educational |
100000000 |
Individuals or Groups (of Individuals) |
103TE1100X |
Exercise & Sports |
100000000 |
Individuals or Groups (of Individuals) |
103TF0000X |
Family |
100000000 |
Individuals or Groups (of Individuals) |
103TF0200X |
Forensic |
100000000 |
Individuals or Groups (of Individuals) |
103TP2701X |
Group Psychotherapy |
100000000 |
Individuals or Groups (of Individuals) |
103TH0004X |
Health |
100000000 |
Individuals or Groups (of Individuals) |
103TH0100X |
Health Service |
100000000 |
Individuals or Groups (of Individuals) |
103TM1700X |
Men & Masculinity |
100000000 |
Individuals or Groups (of Individuals) |
103TM1800X |
Mental Retardation & Developmental Disabilities |
100000000 |
Individuals or Groups (of Individuals) |
103TP0016X |
Prescribing (Medical) |
100000000 |
Individuals or Groups (of Individuals) |
103TP0814X |
Psychoanalysis |
100000000 |
Individuals or Groups (of Individuals) |
103TP2700X |
Psychotherapy |
100000000 |
Individuals or Groups (of Individuals) |
103TR0400X |
Rehabilitation |
100000000 |
Individuals or Groups (of Individuals) |
103TS0200X |
School |
100000000 |
Individuals or Groups (of Individuals) |
103TW0100X |
Women |
100000000 |
Individuals or Groups (of Individuals) |
104100000X |
Social Worker |
100000000 |
Individuals or Groups (of Individuals) |
1041C0700X |
Clinical |
100000000 |
Individuals or Groups (of Individuals) |
1041S0200X |
School |
100000000 |
Individuals or Groups (of Individuals) |
111N00000X |
Chiropractor |
100000000 |
Individuals or Groups (of Individuals) |
111NI0013X |
Independent Medical Examiner |
100000000 |
Individuals or Groups (of Individuals) |
111NI0900X |
Internist |
100000000 |
Individuals or Groups (of Individuals) |
111NN0400X |
Neurology |
100000000 |
Individuals or Groups (of Individuals) |
111NN1001X |
Nutrition |
100000000 |
Individuals or Groups (of Individuals) |
111NX0100X |
Occupational Health |
100000000 |
Individuals or Groups (of Individuals) |
111NX0800X |
Orthopedic |
100000000 |
Individuals or Groups (of Individuals) |
111NP0017X |
Pediatric Chiropractor |
100000000 |
Individuals or Groups (of Individuals) |
111NR0200X |
Radiology |
100000000 |
Individuals or Groups (of Individuals) |
111NR0400X |
Rehabilitation |
100000000 |
Individuals or Groups (of Individuals) |
111NS0005X |
Sports Physician |
100000000 |
Individuals or Groups (of Individuals) |
111NT0100X |
Thermography |
100000000 |
Individuals or Groups (of Individuals) |
125K00000X |
Advanced Practice Dental Therapist |
100000000 |
Individuals or Groups (of Individuals) |
126800000X |
Dental Assistant |
100000000 |
Individuals or Groups (of Individuals) |
124Q00000X |
Dental Hygienist |
100000000 |
Individuals or Groups (of Individuals) |
126900000X |
Dental Laboratory Technician |
100000000 |
Individuals or Groups (of Individuals) |
125J00000X |
Dental Therapist |
100000000 |
Individuals or Groups (of Individuals) |
122300000X |
Dentist |
100000000 |
Individuals or Groups (of Individuals) |
1223D0001X |
Dental Public Health |
100000000 |
Individuals or Groups (of Individuals) |
1223D0004X |
Dentist Anesthesiologist |
100000000 |
Individuals or Groups (of Individuals) |
1223E0200X |
Endodontics |
100000000 |
Individuals or Groups (of Individuals) |
1223G0001X |
General Practice |
100000000 |
Individuals or Groups (of Individuals) |
1223P0106X |
Oral and Maxillofacial Pathology |
100000000 |
Individuals or Groups (of Individuals) |
1223X0008X |
Oral and Maxillofacial Radiology |
100000000 |
Individuals or Groups (of Individuals) |
1223S0112X |
Oral and Maxillofacial Surgery |
100000000 |
Individuals or Groups (of Individuals) |
1223X0400X |
Orthodontics and Dentofacial Orthopedics |
100000000 |
Individuals or Groups (of Individuals) |
1223P0221X |
Pediatric Dentistry |
100000000 |
Individuals or Groups (of Individuals) |
1223P0300X |
Periodontics |
100000000 |
Individuals or Groups (of Individuals) |
1223P0700X |
Prosthodontics |
100000000 |
Individuals or Groups (of Individuals) |
122400000X |
Denturist |
100000000 |
Individuals or Groups (of Individuals) |
132700000X |
Dietary Manager |
100000000 |
Individuals or Groups (of Individuals) |
136A00000X |
Dietetic Technician, Registered |
100000000 |
Individuals or Groups (of Individuals) |
133V00000X |
Dietitian, Registered |
100000000 |
Individuals or Groups (of Individuals) |
133VN1006X |
Nutrition, Metabolic |
100000000 |
Individuals or Groups (of Individuals) |
133VN1004X |
Nutrition, Pediatric |
100000000 |
Individuals or Groups (of Individuals) |
133VN1005X |
Nutrition, Renal |
100000000 |
Individuals or Groups (of Individuals) |
133N00000X |
Nutritionist |
100000000 |
Individuals or Groups (of Individuals) |
133NN1002X |
Nutrition, Education |
100000000 |
Individuals or Groups (of Individuals) |
146N00000X |
Emergency Medical Technician, Basic |
100000000 |
Individuals or Groups (of Individuals) |
146M00000X |
Emergency Medical Technician, Intermediate |
100000000 |
Individuals or Groups (of Individuals) |
146L00000X |
Emergency Medical Technician, Paramedic |
100000000 |
Individuals or Groups (of Individuals) |
146D00000X |
Personal Emergency Response Attendant |
100000000 |
Individuals or Groups (of Individuals) |
152W00000X |
Optometrist |
100000000 |
Individuals or Groups (of Individuals) |
152WC0802X |
Corneal and Contact Management |
100000000 |
Individuals or Groups (of Individuals) |
152WL0500X |
Low Vision Rehabilitation |
100000000 |
Individuals or Groups (of Individuals) |
152WX0102X |
Occupational Vision |
100000000 |
Individuals or Groups (of Individuals) |
152WP0200X |
Pediatrics |
100000000 |
Individuals or Groups (of Individuals) |
152WS0006X |
Sports Vision |
100000000 |
Individuals or Groups (of Individuals) |
152WV0400X |
Vision Therapy |
100000000 |
Individuals or Groups (of Individuals) |
156F00000X |
Technician/Technologist |
100000000 |
Individuals or Groups (of Individuals) |
156FC0800X |
Contact Lens |
100000000 |
Individuals or Groups (of Individuals) |
156FC0801X |
Contact Lens Fitter |
100000000 |
Individuals or Groups (of Individuals) |
156FX1700X |
Ocularist |
100000000 |
Individuals or Groups (of Individuals) |
156FX1100X |
Ophthalmic |
100000000 |
Individuals or Groups (of Individuals) |
156FX1101X |
Ophthalmic Assistant |
100000000 |
Individuals or Groups (of Individuals) |
156FX1800X |
Optician |
100000000 |
Individuals or Groups (of Individuals) |
156FX1201X |
Optometric Assistant |
100000000 |
Individuals or Groups (of Individuals) |
156FX1202X |
Optometric Technician |
100000000 |
Individuals or Groups (of Individuals) |
156FX1900X |
Orthoptist |
100000000 |
Individuals or Groups (of Individuals) |
164W00000X |
Licensed Practical Nurse |
100000000 |
Individuals or Groups (of Individuals) |
167G00000X |
Licensed Psychiatric Technician |
100000000 |
Individuals or Groups (of Individuals) |
164X00000X |
Licensed Vocational Nurse |
100000000 |
Individuals or Groups (of Individuals) |
163W00000X |
Registered Nurse |
100000000 |
Individuals or Groups (of Individuals) |
163WA0400X |
Addiction (Substance Use Disorder) |
100000000 |
Individuals or Groups (of Individuals) |
163WA2000X |
Administrator |
100000000 |
Individuals or Groups (of Individuals) |
163WP2201X |
Ambulatory Care |
100000000 |
Individuals or Groups (of Individuals) |
163WC3500X |
Cardiac Rehabilitation |
100000000 |
Individuals or Groups (of Individuals) |
163WC0400X |
Case Management |
100000000 |
Individuals or Groups (of Individuals) |
163WC1400X |
College Health |
100000000 |
Individuals or Groups (of Individuals) |
163WC1500X |
Community Health |
100000000 |
Individuals or Groups (of Individuals) |
163WC2100X |
Continence Care |
100000000 |
Individuals or Groups (of Individuals) |
163WC1600X |
Continuing Education/Staff Development |
100000000 |
Individuals or Groups (of Individuals) |
163WC0200X |
Critical Care Medicine |
100000000 |
Individuals or Groups (of Individuals) |
163WD0400X |
Diabetes Educator |
100000000 |
Individuals or Groups (of Individuals) |
163WD1100X |
Dialysis, Peritoneal |
100000000 |
Individuals or Groups (of Individuals) |
163WE0003X |
Emergency |
100000000 |
Individuals or Groups (of Individuals) |
163WE0900X |
Enterostomal Therapy |
100000000 |
Individuals or Groups (of Individuals) |
163WF0300X |
Flight |
100000000 |
Individuals or Groups (of Individuals) |
163WG0100X |
Gastroenterology |
100000000 |
Individuals or Groups (of Individuals) |
163WG0000X |
General Practice |
100000000 |
Individuals or Groups (of Individuals) |
163WG0600X |
Gerontology |
100000000 |
Individuals or Groups (of Individuals) |
163WH0500X |
Hemodialysis |
100000000 |
Individuals or Groups (of Individuals) |
163WH0200X |
Home Health |
100000000 |
Individuals or Groups (of Individuals) |
163WH1000X |
Hospice |
100000000 |
Individuals or Groups (of Individuals) |
163WI0600X |
Infection Control |
100000000 |
Individuals or Groups (of Individuals) |
163WI0500X |
Infusion Therapy |
100000000 |
Individuals or Groups (of Individuals) |
163WL0100X |
Lactation Consultant |
100000000 |
Individuals or Groups (of Individuals) |
163WM0102X |
Maternal Newborn |
100000000 |
Individuals or Groups (of Individuals) |
163WM0705X |
Medical-Surgical |
100000000 |
Individuals or Groups (of Individuals) |
163WN0002X |
Neonatal Intensive Care |
100000000 |
Individuals or Groups (of Individuals) |
163WN0003X |
Neonatal, Low-Risk |
100000000 |
Individuals or Groups (of Individuals) |
163WN0300X |
Nephrology |
100000000 |
Individuals or Groups (of Individuals) |
163WN0800X |
Neuroscience |
100000000 |
Individuals or Groups (of Individuals) |
163WM1400X |
Nurse Massage Therapist (NMT) |
100000000 |
Individuals or Groups (of Individuals) |
163WN1003X |
Nutrition Support |
100000000 |
Individuals or Groups (of Individuals) |
163WX0002X |
Obstetric, High-Risk |
100000000 |
Individuals or Groups (of Individuals) |
163WX0003X |
Obstetric, Inpatient |
100000000 |
Individuals or Groups (of Individuals) |
163WX0106X |
Occupational Health |
100000000 |
Individuals or Groups (of Individuals) |
163WX0200X |
Oncology |
100000000 |
Individuals or Groups (of Individuals) |
163WX1100X |
Ophthalmic |
100000000 |
Individuals or Groups (of Individuals) |
163WX0800X |
Orthopedic |
100000000 |
Individuals or Groups (of Individuals) |
163WX1500X |
Ostomy Care |
100000000 |
Individuals or Groups (of Individuals) |
163WX0601X |
Otorhinolaryngology & Head-Neck |
100000000 |
Individuals or Groups (of Individuals) |
163WP0000X |
Pain Management |
100000000 |
Individuals or Groups (of Individuals) |
163WP0218X |
Pediatric Oncology |
100000000 |
Individuals or Groups (of Individuals) |
163WP0200X |
Pediatrics |
100000000 |
Individuals or Groups (of Individuals) |
163WP1700X |
Perinatal |
100000000 |
Individuals or Groups (of Individuals) |
163WS0121X |
Plastic Surgery |
100000000 |
Individuals or Groups (of Individuals) |
163WP0808X |
Psychiatric/Mental Health |
100000000 |
Individuals or Groups (of Individuals) |
163WP0809X |
Psychiatric/Mental Health, Adult |
100000000 |
Individuals or Groups (of Individuals) |
163WP0807X |
Psychiatric/Mental Health, Child & Adolescent |
100000000 |
Individuals or Groups (of Individuals) |
163WR0006X |
Registered Nurse First Assistant |
100000000 |
Individuals or Groups (of Individuals) |
163WR0400X |
Rehabilitation |
100000000 |
Individuals or Groups (of Individuals) |
163WR1000X |
Reproductive Endocrinology/Infertility |
100000000 |
Individuals or Groups (of Individuals) |
163WS0200X |
School |
100000000 |
Individuals or Groups (of Individuals) |
163WU0100X |
Urology |
100000000 |
Individuals or Groups (of Individuals) |
163WW0101X |
Women's Health Care, Ambulatory |
100000000 |
Individuals or Groups (of Individuals) |
163WW0000X |
Wound Care |
100000000 |
Individuals or Groups (of Individuals) |
372600000X |
Adult Companion |
100000000 |
Individuals or Groups (of Individuals) |
372500000X |
Chore Provider |
100000000 |
Individuals or Groups (of Individuals) |
373H00000X |
Day Training/Habilitation Specialist |
100000000 |
Individuals or Groups (of Individuals) |
374J00000X |
Doula |
100000000 |
Individuals or Groups (of Individuals) |
374U00000X |
Home Health Aide |
100000000 |
Individuals or Groups (of Individuals) |
376J00000X |
Homemaker |
100000000 |
Individuals or Groups (of Individuals) |
376K00000X |
Nurse's Aide |
100000000 |
Individuals or Groups (of Individuals) |
376G00000X |
Nursing Home Administrator |
100000000 |
Individuals or Groups (of Individuals) |
374T00000X |
Religious Nonmedical Nursing Personnel |
100000000 |
Individuals or Groups (of Individuals) |
374K00000X |
Religious Nonmedical Practitioner |
100000000 |
Individuals or Groups (of Individuals) |
374700000X |
Technician |
100000000 |
Individuals or Groups (of Individuals) |
3747A0650X |
Attendant Care Provider |
100000000 |
Individuals or Groups (of Individuals) |
3747P1801X |
Personal Care Attendant |
100000000 |
Individuals or Groups (of Individuals) |
171100000X |
Acupuncturist |
100000000 |
Individuals or Groups (of Individuals) |
171M00000X |
Case Manager/Care Coordinator |
100000000 |
Individuals or Groups (of Individuals) |
174V00000X |
Clinical Ethicist |
100000000 |
Individuals or Groups (of Individuals) |
172V00000X |
Community Health Worker |
100000000 |
Individuals or Groups (of Individuals) |
171W00000X |
Contractor |
100000000 |
Individuals or Groups (of Individuals) |
171WH0202X |
Home Modifications |
100000000 |
Individuals or Groups (of Individuals) |
171WV0202X |
Vehicle Modifications |
100000000 |
Individuals or Groups (of Individuals) |
172A00000X |
Driver |
100000000 |
Individuals or Groups (of Individuals) |
176P00000X |
Funeral Director |
100000000 |
Individuals or Groups (of Individuals) |
170300000X |
Genetic Counselor, MS |
100000000 |
Individuals or Groups (of Individuals) |
174H00000X |
Health Educator |
100000000 |
Individuals or Groups (of Individuals) |
175L00000X |
Homeopath |
100000000 |
Individuals or Groups (of Individuals) |
171R00000X |
Interpreter |
100000000 |
Individuals or Groups (of Individuals) |
174N00000X |
Lactation Consultant, Non-RN |
100000000 |
Individuals or Groups (of Individuals) |
173000000X |
Legal Medicine |
100000000 |
Individuals or Groups (of Individuals) |
172M00000X |
Mechanotherapist |
100000000 |
Individuals or Groups (of Individuals) |
170100000X |
Medical Genetics, Ph.D. Medical Genetics |
100000000 |
Individuals or Groups (of Individuals) |
176B00000X |
Midwife |
100000000 |
Individuals or Groups (of Individuals) |
175M00000X |
Midwife, Lay |
100000000 |
Individuals or Groups (of Individuals) |
171000000X |
Military Health Care Provider |
100000000 |
Individuals or Groups (of Individuals) |
1710I1002X |
Independent Duty Corpsman |
100000000 |
Individuals or Groups (of Individuals) |
1710I1003X |
Independent Duty Medical Technicians |
100000000 |
Individuals or Groups (of Individuals) |
172P00000X |
Naprapath |
100000000 |
Individuals or Groups (of Individuals) |
175F00000X |
Naturopath |
100000000 |
Individuals or Groups (of Individuals) |
173C00000X |
Reflexologist |
100000000 |
Individuals or Groups (of Individuals) |
173F00000X |
Sleep Specialist, PhD |
100000000 |
Individuals or Groups (of Individuals) |
174400000X |
Specialist |
100000000 |
Individuals or Groups (of Individuals) |
1744G0900X |
Graphics Designer |
100000000 |
Individuals or Groups (of Individuals) |
1744P3200X |
Prosthetics Case Management |
100000000 |
Individuals or Groups (of Individuals) |
1744R1103X |
Research Data Abstracter/Coder |
100000000 |
Individuals or Groups (of Individuals) |
1744R1102X |
Research Study |
100000000 |
Individuals or Groups (of Individuals) |
174M00000X |
Veterinarian |
100000000 |
Individuals or Groups (of Individuals) |
174MM1900X |
Medical Research |
100000000 |
Individuals or Groups (of Individuals) |
183500000X |
Pharmacist |
100000000 |
Individuals or Groups (of Individuals) |
1835G0000X |
General Practice |
100000000 |
Individuals or Groups (of Individuals) |
1835G0303X |
Geriatric |
100000000 |
Individuals or Groups (of Individuals) |
1835N0905X |
Nuclear |
100000000 |
Individuals or Groups (of Individuals) |
1835N1003X |
Nutrition Support |
100000000 |
Individuals or Groups (of Individuals) |
1835X0200X |
Oncology |
100000000 |
Individuals or Groups (of Individuals) |
1835P0018X |
Pharmacist Clinician (PhC)/ Clinical Pharmacy Specialist |
100000000 |
Individuals or Groups (of Individuals) |
1835P1200X |
Pharmacotherapy |
100000000 |
Individuals or Groups (of Individuals) |
1835P1300X |
Psychiatric |
100000000 |
Individuals or Groups (of Individuals) |
183700000X |
Pharmacy Technician |
100000000 |
Individuals or Groups (of Individuals) |
367A00000X |
Advanced Practice Midwife |
100000000 |
Individuals or Groups (of Individuals) |
367H00000X |
Anesthesiologist Assistant |
100000000 |
Individuals or Groups (of Individuals) |
364S00000X |
Clinical Nurse Specialist |
100000000 |
Individuals or Groups (of Individuals) |
364SA2100X |
Acute Care |
100000000 |
Individuals or Groups (of Individuals) |
364SA2200X |
Adult Health |
100000000 |
Individuals or Groups (of Individuals) |
364SC2300X |
Chronic Care |
100000000 |
Individuals or Groups (of Individuals) |
364SC1501X |
Community Health/Public Health |
100000000 |
Individuals or Groups (of Individuals) |
364SC0200X |
Critical Care Medicine |
100000000 |
Individuals or Groups (of Individuals) |
364SE0003X |
Emergency |
100000000 |
Individuals or Groups (of Individuals) |
364SE1400X |
Ethics |
100000000 |
Individuals or Groups (of Individuals) |
364SF0001X |
Family Health |
100000000 |
Individuals or Groups (of Individuals) |
364SG0600X |
Gerontology |
100000000 |
Individuals or Groups (of Individuals) |
364SH1100X |
Holistic |
100000000 |
Individuals or Groups (of Individuals) |
364SH0200X |
Home Health |
100000000 |
Individuals or Groups (of Individuals) |
364SI0800X |
Informatics |
100000000 |
Individuals or Groups (of Individuals) |
364SL0600X |
Long-Term Care |
100000000 |
Individuals or Groups (of Individuals) |
364SM0705X |
Medical-Surgical |
100000000 |
Individuals or Groups (of Individuals) |
364SN0000X |
Neonatal |
100000000 |
Individuals or Groups (of Individuals) |
364SN0800X |
Neuroscience |
100000000 |
Individuals or Groups (of Individuals) |
364SX0106X |
Occupational Health |
100000000 |
Individuals or Groups (of Individuals) |
364SX0200X |
Oncology |
100000000 |
Individuals or Groups (of Individuals) |
364SX0204X |
Oncology, Pediatrics |
100000000 |
Individuals or Groups (of Individuals) |
364SP0200X |
Pediatrics |
100000000 |
Individuals or Groups (of Individuals) |
364SP1700X |
Perinatal |
100000000 |
Individuals or Groups (of Individuals) |
364SP2800X |
Perioperative |
100000000 |
Individuals or Groups (of Individuals) |
364SP0808X |
Psychiatric/Mental Health |
100000000 |
Individuals or Groups (of Individuals) |
364SP0809X |
Psychiatric/Mental Health, Adult |
100000000 |
Individuals or Groups (of Individuals) |
364SP0807X |
Psychiatric/Mental Health, Child & Adolescent |
100000000 |
Individuals or Groups (of Individuals) |
364SP0810X |
Psychiatric/Mental Health, Child & Family |
100000000 |
Individuals or Groups (of Individuals) |
364SP0811X |
Psychiatric/Mental Health, Chronically Ill |
100000000 |
Individuals or Groups (of Individuals) |
364SP0812X |
Psychiatric/Mental Health, Community |
100000000 |
Individuals or Groups (of Individuals) |
364SP0813X |
Psychiatric/Mental Health, Geropsychiatric |
100000000 |
Individuals or Groups (of Individuals) |
364SR0400X |
Rehabilitation |
100000000 |
Individuals or Groups (of Individuals) |
364SS0200X |
School |
100000000 |
Individuals or Groups (of Individuals) |
364ST0500X |
Transplantation |
100000000 |
Individuals or Groups (of Individuals) |
364SW0102X |
Women's Health |
100000000 |
Individuals or Groups (of Individuals) |
367500000X |
Nurse Anesthetist, Certified Registered |
100000000 |
Individuals or Groups (of Individuals) |
363L00000X |
Nurse Practitioner |
100000000 |
Individuals or Groups (of Individuals) |
363LA2100X |
Acute Care |
100000000 |
Individuals or Groups (of Individuals) |
363LA2200X |
Adult Health |
100000000 |
Individuals or Groups (of Individuals) |
363LC1500X |
Community Health |
100000000 |
Individuals or Groups (of Individuals) |
363LC0200X |
Critical Care Medicine |
100000000 |
Individuals or Groups (of Individuals) |
363LF0000X |
Family |
100000000 |
Individuals or Groups (of Individuals) |
363LG0600X |
Gerontology |
100000000 |
Individuals or Groups (of Individuals) |
363LN0000X |
Neonatal |
100000000 |
Individuals or Groups (of Individuals) |
363LN0005X |
Neonatal, Critical Care |
100000000 |
Individuals or Groups (of Individuals) |
363LX0001X |
Obstetrics & Gynecology |
100000000 |
Individuals or Groups (of Individuals) |
363LX0106X |
Occupational Health |
100000000 |
Individuals or Groups (of Individuals) |
363LP0200X |
Pediatrics |
100000000 |
Individuals or Groups (of Individuals) |
363LP0222X |
Pediatrics, Critical Care |
100000000 |
Individuals or Groups (of Individuals) |
363LP1700X |
Perinatal |
100000000 |
Individuals or Groups (of Individuals) |
363LP2300X |
Primary Care |
100000000 |
Individuals or Groups (of Individuals) |
363LP0808X |
Psychiatric/Mental Health |
100000000 |
Individuals or Groups (of Individuals) |
363LS0200X |
School |
100000000 |
Individuals or Groups (of Individuals) |
363LW0102X |
Women's Health |
100000000 |
Individuals or Groups (of Individuals) |
363A00000X |
Physician Assistant |
100000000 |
Individuals or Groups (of Individuals) |
363AM0700X |
Medical |
100000000 |
Individuals or Groups (of Individuals) |
363AS0400X |
Surgical |
100000000 |
Individuals or Groups (of Individuals) |
211D00000X |
Assistant, Podiatric |
100000000 |
Individuals or Groups (of Individuals) |
213E00000X |
Podiatrist |
100000000 |
Individuals or Groups (of Individuals) |
213ES0103X |
Foot & Ankle Surgery |
100000000 |
Individuals or Groups (of Individuals) |
213ES0131X |
Foot Surgery |
100000000 |
Individuals or Groups (of Individuals) |
213EG0000X |
General Practice |
100000000 |
Individuals or Groups (of Individuals) |
213EP1101X |
Primary Podiatric Medicine |
100000000 |
Individuals or Groups (of Individuals) |
213EP0504X |
Public Medicine |
100000000 |
Individuals or Groups (of Individuals) |
213ER0200X |
Radiology |
100000000 |
Individuals or Groups (of Individuals) |
213ES0000X |
Sports Medicine |
100000000 |
Individuals or Groups (of Individuals) |
229N00000X |
Anaplastologist |
100000000 |
Individuals or Groups (of Individuals) |
221700000X |
Art Therapist |
100000000 |
Individuals or Groups (of Individuals) |
224Y00000X |
Clinical Exercise Physiologist |
100000000 |
Individuals or Groups (of Individuals) |
225600000X |
Dance Therapist |
100000000 |
Individuals or Groups (of Individuals) |
222Q00000X |
Developmental Therapist |
100000000 |
Individuals or Groups (of Individuals) |
226300000X |
Kinesiotherapist |
100000000 |
Individuals or Groups (of Individuals) |
225700000X |
Massage Therapist |
100000000 |
Individuals or Groups (of Individuals) |
224900000X |
Mastectomy Fitter |
100000000 |
Individuals or Groups (of Individuals) |
225A00000X |
Music Therapist |
100000000 |
Individuals or Groups (of Individuals) |
225X00000X |
Occupational Therapist |
100000000 |
Individuals or Groups (of Individuals) |
225XR0403X |
Driving and Community Mobility |
100000000 |
Individuals or Groups (of Individuals) |
225XE0001X |
Environmental Modification |
100000000 |
Individuals or Groups (of Individuals) |
225XE1200X |
Ergonomics |
100000000 |
Individuals or Groups (of Individuals) |
225XF0002X |
Feeding, Eating & Swallowing |
100000000 |
Individuals or Groups (of Individuals) |
225XG0600X |
Gerontology |
100000000 |
Individuals or Groups (of Individuals) |
225XH1200X |
Hand |
100000000 |
Individuals or Groups (of Individuals) |
225XH1300X |
Human Factors |
100000000 |
Individuals or Groups (of Individuals) |
225XL0004X |
Low Vision |
100000000 |
Individuals or Groups (of Individuals) |
225XM0800X |
Mental Health |
100000000 |
Individuals or Groups (of Individuals) |
225XN1300X |
Neurorehabilitation |
100000000 |
Individuals or Groups (of Individuals) |
225XP0200X |
Pediatrics |
100000000 |
Individuals or Groups (of Individuals) |
225XP0019X |
Physical Rehabilitation |
100000000 |
Individuals or Groups (of Individuals) |
224Z00000X |
Occupational Therapy Assistant |
100000000 |
Individuals or Groups (of Individuals) |
224ZR0403X |
Driving and Community Mobility |
100000000 |
Individuals or Groups (of Individuals) |
224ZE0001X |
Environmental Modification |
100000000 |
Individuals or Groups (of Individuals) |
224ZF0002X |
Feeding, Eating & Swallowing |
100000000 |
Individuals or Groups (of Individuals) |
224ZL0004X |
Low Vision |
100000000 |
Individuals or Groups (of Individuals) |
225000000X |
Orthotic Fitter |
100000000 |
Individuals or Groups (of Individuals) |
222Z00000X |
Orthotist |
100000000 |
Individuals or Groups (of Individuals) |
224L00000X |
Pedorthist |
100000000 |
Individuals or Groups (of Individuals) |
225100000X |
Physical Therapist |
100000000 |
Individuals or Groups (of Individuals) |
2251C2600X |
Cardiopulmonary |
100000000 |
Individuals or Groups (of Individuals) |
2251E1300X |
Electrophysiology, Clinical |
100000000 |
Individuals or Groups (of Individuals) |
2251E1200X |
Ergonomics |
100000000 |
Individuals or Groups (of Individuals) |
2251G0304X |
Geriatrics |
100000000 |
Individuals or Groups (of Individuals) |
2251H1200X |
Hand |
100000000 |
Individuals or Groups (of Individuals) |
2251H1300X |
Human Factors |
100000000 |
Individuals or Groups (of Individuals) |
2251N0400X |
Neurology |
100000000 |
Individuals or Groups (of Individuals) |
2251X0800X |
Orthopedic |
100000000 |
Individuals or Groups (of Individuals) |
2251P0200X |
Pediatrics |
100000000 |
Individuals or Groups (of Individuals) |
2251S0007X |
Sports |
100000000 |
Individuals or Groups (of Individuals) |
225200000X |
Physical Therapy Assistant |
100000000 |
Individuals or Groups (of Individuals) |
224P00000X |
Prosthetist |
100000000 |
Individuals or Groups (of Individuals) |
225B00000X |
Pulmonary Function Technologist |
100000000 |
Individuals or Groups (of Individuals) |
225800000X |
Recreation Therapist |
100000000 |
Individuals or Groups (of Individuals) |
225C00000X |
Rehabilitation Counselor |
100000000 |
Individuals or Groups (of Individuals) |
225CA2400X |
Assistive Technology Practitioner |
100000000 |
Individuals or Groups (of Individuals) |
225CA2500X |
Assistive Technology Supplier |
100000000 |
Individuals or Groups (of Individuals) |
225CX0006X |
Orientation and Mobility Training Provider |
100000000 |
Individuals or Groups (of Individuals) |
225400000X |
Rehabilitation Practitioner |
100000000 |
Individuals or Groups (of Individuals) |
227800000X |
Respiratory Therapist, Certified |
100000000 |
Individuals or Groups (of Individuals) |
2278C0205X |
Critical Care |
100000000 |
Individuals or Groups (of Individuals) |
2278E1000X |
Educational |
100000000 |
Individuals or Groups (of Individuals) |
2278E0002X |
Emergency Care |
100000000 |
Individuals or Groups (of Individuals) |
2278G1100X |
General Care |
100000000 |
Individuals or Groups (of Individuals) |
2278G0305X |
Geriatric Care |
100000000 |
Individuals or Groups (of Individuals) |
2278H0200X |
Home Health |
100000000 |
Individuals or Groups (of Individuals) |
2278P3900X |
Neonatal/Pediatrics |
100000000 |
Individuals or Groups (of Individuals) |
2278P3800X |
Palliative/Hospice |
100000000 |
Individuals or Groups (of Individuals) |
2278P4000X |
Patient Transport |
100000000 |
Individuals or Groups (of Individuals) |
2278P1004X |
Pulmonary Diagnostics |
100000000 |
Individuals or Groups (of Individuals) |
2278P1006X |
Pulmonary Function Technologist |
100000000 |
Individuals or Groups (of Individuals) |
2278P1005X |
Pulmonary Rehabilitation |
100000000 |
Individuals or Groups (of Individuals) |
2278S1500X |
SNF/Subacute Care |
100000000 |
Individuals or Groups (of Individuals) |
227900000X |
Respiratory Therapist, Registered |
100000000 |
Individuals or Groups (of Individuals) |
2279C0205X |
Critical Care |
100000000 |
Individuals or Groups (of Individuals) |
2279E1000X |
Educational |
100000000 |
Individuals or Groups (of Individuals) |
2279E0002X |
Emergency Care |
100000000 |
Individuals or Groups (of Individuals) |
2279G1100X |
General Care |
100000000 |
Individuals or Groups (of Individuals) |
2279G0305X |
Geriatric Care |
100000000 |
Individuals or Groups (of Individuals) |
2279H0200X |
Home Health |
100000000 |
Individuals or Groups (of Individuals) |
2279P3900X |
Neonatal/Pediatrics |
100000000 |
Individuals or Groups (of Individuals) |
2279P3800X |
Palliative/Hospice |
100000000 |
Individuals or Groups (of Individuals) |
2279P4000X |
Patient Transport |
100000000 |
Individuals or Groups (of Individuals) |
2279P1004X |
Pulmonary Diagnostics |
100000000 |
Individuals or Groups (of Individuals) |
2279P1006X |
Pulmonary Function Technologist |
100000000 |
Individuals or Groups (of Individuals) |
2279P1005X |
Pulmonary Rehabilitation |
100000000 |
Individuals or Groups (of Individuals) |
2279S1500X |
SNF/Subacute Care |
100000000 |
Individuals or Groups (of Individuals) |
225500000X |
Specialist/Technologist |
100000000 |
Individuals or Groups (of Individuals) |
2255A2300X |
Athletic Trainer |
100000000 |
Individuals or Groups (of Individuals) |
2255R0406X |
Rehabilitation, Blind |
100000000 |
Individuals or Groups (of Individuals) |
231H00000X |
Audiologist |
100000000 |
Individuals or Groups (of Individuals) |
231HA2400X |
Assistive Technology Practitioner |
100000000 |
Individuals or Groups (of Individuals) |
231HA2500X |
Assistive Technology Supplier |
100000000 |
Individuals or Groups (of Individuals) |
237600000X |
Audiologist-Hearing Aid Fitter |
100000000 |
Individuals or Groups (of Individuals) |
237700000X |
Hearing Instrument Specialist |
100000000 |
Individuals or Groups (of Individuals) |
235500000X |
Specialist/Technologist |
100000000 |
Individuals or Groups (of Individuals) |
2355A2700X |
Audiology Assistant |
100000000 |
Individuals or Groups (of Individuals) |
2355S0801X |
Speech-Language Assistant |
100000000 |
Individuals or Groups (of Individuals) |
235Z00000X |
Speech-Language Pathologist |
100000000 |
Individuals or Groups (of Individuals) |
390200000X |
Student in an Organized Health Care Education/Training Program |
100000000 |
Individuals or Groups (of Individuals) |
242T00000X |
Perfusionist |
100000000 |
Individuals or Groups (of Individuals) |
247100000X |
Radiologic Technologist |
100000000 |
Individuals or Groups (of Individuals) |
2471B0102X |
Bone Densitometry |
100000000 |
Individuals or Groups (of Individuals) |
2471C1106X |
Cardiac-Interventional Technology |
100000000 |
Individuals or Groups (of Individuals) |
2471C1101X |
Cardiovascular-Interventional Technology |
100000000 |
Individuals or Groups (of Individuals) |
2471C3401X |
Computed Tomography |
100000000 |
Individuals or Groups (of Individuals) |
2471M1202X |
Magnetic Resonance Imaging |
100000000 |
Individuals or Groups (of Individuals) |
2471M2300X |
Mammography |
100000000 |
Individuals or Groups (of Individuals) |
2471N0900X |
Nuclear Medicine Technology |
100000000 |
Individuals or Groups (of Individuals) |
2471Q0001X |
Quality Management |
100000000 |
Individuals or Groups (of Individuals) |
2471R0002X |
Radiation Therapy |
100000000 |
Individuals or Groups (of Individuals) |
2471C3402X |
Radiography |
100000000 |
Individuals or Groups (of Individuals) |
2471S1302X |
Sonography |
100000000 |
Individuals or Groups (of Individuals) |
2471V0105X |
Vascular Sonography |
100000000 |
Individuals or Groups (of Individuals) |
2471V0106X |
Vascular-Interventional Technology |
100000000 |
Individuals or Groups (of Individuals) |
243U00000X |
Radiology Practitioner Assistant |
100000000 |
Individuals or Groups (of Individuals) |
246X00000X |
Specialist/Technologist Cardiovascular |
100000000 |
Individuals or Groups (of Individuals) |
246XC2901X |
Cardiovascular Invasive Specialist |
100000000 |
Individuals or Groups (of Individuals) |
246XS1301X |
Sonography |
100000000 |
Individuals or Groups (of Individuals) |
246XC2903X |
Vascular Specialist |
100000000 |
Individuals or Groups (of Individuals) |
246Y00000X |
Specialist/Technologist, Health Information |
100000000 |
Individuals or Groups (of Individuals) |
246YC3301X |
Coding Specialist, Hospital Based |
100000000 |
Individuals or Groups (of Individuals) |
246YC3302X |
Coding Specialist, Physician Office Based |
100000000 |
Individuals or Groups (of Individuals) |
246YR1600X |
Registered Record Administrator |
100000000 |
Individuals or Groups (of Individuals) |
246Z00000X |
Specialist/Technologist, Other |
100000000 |
Individuals or Groups (of Individuals) |
246ZA2600X |
Art, Medical |
100000000 |
Individuals or Groups (of Individuals) |
246ZB0500X |
Biochemist |
100000000 |
Individuals or Groups (of Individuals) |
246ZB0301X |
Biomedical Engineering |
100000000 |
Individuals or Groups (of Individuals) |
246ZB0302X |
Biomedical Photographer |
100000000 |
Individuals or Groups (of Individuals) |
246ZB0600X |
Biostatistician |
100000000 |
Individuals or Groups (of Individuals) |
246ZC0007X |
Certified First Assistant |
100000000 |
Individuals or Groups (of Individuals) |
246ZE0500X |
EEG |
100000000 |
Individuals or Groups (of Individuals) |
246ZE0600X |
Electroneurodiagnostic |
100000000 |
Individuals or Groups (of Individuals) |
246ZG1000X |
Geneticist, Medical (PhD) |
100000000 |
Individuals or Groups (of Individuals) |
246ZG0701X |
Graphics Methods |
100000000 |
Individuals or Groups (of Individuals) |
246ZI1000X |
Illustration, Medical |
100000000 |
Individuals or Groups (of Individuals) |
246ZN0300X |
Nephrology |
100000000 |
Individuals or Groups (of Individuals) |
246ZS0400X |
Surgical |
100000000 |
Individuals or Groups (of Individuals) |
246Q00000X |
Specialist/Technologist, Pathology |
100000000 |
Individuals or Groups (of Individuals) |
246QB0000X |
Blood Banking |
100000000 |
Individuals or Groups (of Individuals) |
246QC1000X |
Chemistry |
100000000 |
Individuals or Groups (of Individuals) |
246QC2700X |
Cytotechnology |
100000000 |
Individuals or Groups (of Individuals) |
246QH0401X |
Hemapheresis Practitioner |
100000000 |
Individuals or Groups (of Individuals) |
246QH0000X |
Hematology |
100000000 |
Individuals or Groups (of Individuals) |
246QH0600X |
Histology |
100000000 |
Individuals or Groups (of Individuals) |
246QI0000X |
Immunology |
100000000 |
Individuals or Groups (of Individuals) |
246QL0900X |
Laboratory Management |
100000000 |
Individuals or Groups (of Individuals) |
246QL0901X |
Laboratory Management, Diplomate |
100000000 |
Individuals or Groups (of Individuals) |
246QM0706X |
Medical Technologist |
100000000 |
Individuals or Groups (of Individuals) |
246QM0900X |
Microbiology |
100000000 |
Individuals or Groups (of Individuals) |
246W00000X |
Technician, Cardiology |
100000000 |
Individuals or Groups (of Individuals) |
247000000X |
Technician, Health Information |
100000000 |
Individuals or Groups (of Individuals) |
2470A2800X |
Assistant Record Technician |
100000000 |
Individuals or Groups (of Individuals) |
247200000X |
Technician, Other |
100000000 |
Individuals or Groups (of Individuals) |
2472B0301X |
Biomedical Engineering |
100000000 |
Individuals or Groups (of Individuals) |
2472D0500X |
Darkroom |
100000000 |
Individuals or Groups (of Individuals) |
2472E0500X |
EEG |
100000000 |
Individuals or Groups (of Individuals) |
2472R0900X |
Renal Dialysis |
100000000 |
Individuals or Groups (of Individuals) |
2472V0600X |
Veterinary |
100000000 |
Individuals or Groups (of Individuals) |
246R00000X |
Technician, Pathology |
100000000 |
Individuals or Groups (of Individuals) |
247ZC0005X |
Clinical Laboratory Director, Non-physician |
100000000 |
Individuals or Groups (of Individuals) |
246RH0600X |
Histology |
100000000 |
Individuals or Groups (of Individuals) |
246RM2200X |
Medical Laboratory |
100000000 |
Individuals or Groups (of Individuals) |
246RP1900X |
Phlebotomy |
100000000 |
Individuals or Groups (of Individuals) |
251300000X |
Local Education Agency (LEA) |
250000000 |
Non-Individual - Agencies |
251B00000X |
Case Management |
250000000 |
Non-Individual - Agencies |
251S00000X |
Community/Behavioral Health |
250000000 |
Non-Individual - Agencies |
251C00000X |
Day Training, Developmentally Disabled Services |
250000000 |
Non-Individual - Agencies |
252Y00000X |
Early Intervention Provider Agency |
250000000 |
Non-Individual - Agencies |
253J00000X |
Foster Care Agency |
250000000 |
Non-Individual - Agencies |
251E00000X |
Home Health |
250000000 |
Non-Individual - Agencies |
251F00000X |
Home Infusion |
250000000 |
Non-Individual - Agencies |
251G00000X |
Hospice Care, Community Based |
250000000 |
Non-Individual - Agencies |
253Z00000X |
In Home Supportive Care |
250000000 |
Non-Individual - Agencies |
251J00000X |
Nursing Care |
250000000 |
Non-Individual - Agencies |
251T00000X |
Program of All-Inclusive Care for the Elderly (PACE) Provider Organization |
250000000 |
Non-Individual - Agencies |
251K00000X |
Public Health or Welfare |
250000000 |
Non-Individual - Agencies |
251X00000X |
Supports Brokerage |
250000000 |
Non-Individual - Agencies |
251V00000X |
Voluntary or Charitable |
250000000 |
Non-Individual - Agencies |
261Q00000X |
Clinic/Center |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QM0855X |
Adolescent and Children Mental Health |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QA0600X |
Adult Day Care |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QM0850X |
Adult Mental Health |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QA0005X |
Ambulatory Family Planning Facility |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QA0006X |
Ambulatory Fertility Facility |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QA1903X |
Ambulatory Surgical |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QA0900X |
Amputee |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QA3000X |
Augmentative Communication |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QB0400X |
Birthing |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QC1500X |
Community Health |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QC1800X |
Corporate Health |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QC0050X |
Critical Access Hospital |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QD0000X |
Dental |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QD1600X |
Developmental Disabilities |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QE0002X |
Emergency Care |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QE0800X |
Endoscopy |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QE0700X |
End-Stage Renal Disease (ESRD) Treatment |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QF0050X |
Family Planning, Non-Surgical |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QF0400X |
Federally Qualified Health Center (FQHC) |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QG0250X |
Genetics |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QH0100X |
Health Service |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QH0700X |
Hearing and Speech |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QI0500X |
Infusion Therapy |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QL0400X |
Lithotripsy |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QM1200X |
Magnetic Resonance Imaging (MRI) |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QM2500X |
Medical Specialty |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QM3000X |
Medically Fragile Infants and Children Day Care |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QM0801X |
Mental Health (Including Community Mental Health Center) |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QM2800X |
Methadone |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QM1000X |
Migrant Health |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QM1103X |
Military Ambulatory Procedure Visits Operational (Transportable) |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QM1101X |
Military and U.S. Coast Guard Ambulatory Procedure |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QM1102X |
Military Outpatient Operational (Transportable) Component |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QM1100X |
Military/U.S. Coast Guard Outpatient |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QM1300X |
Multi-Specialty |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QX0100X |
Occupational Medicine |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QX0200X |
Oncology |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QX0203X |
Oncology, Radiation |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QS0132X |
Ophthalmologic Surgery |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QS0112X |
Oral and Maxillofacial Surgery |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QP3300X |
Pain |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QP2000X |
Physical Therapy |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QP1100X |
Podiatric |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QP2300X |
Primary Care |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QP2400X |
Prison Health |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QP0904X |
Public Health, Federal |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QP0905X |
Public Health, State or Local |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QR0200X |
Radiology |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QR0206X |
Radiology, Mammography |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QR0208X |
Radiology, Mobile |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QR0207X |
Radiology, Mobile Mammography |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QR0800X |
Recovery Care |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QR0400X |
Rehabilitation |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QR0404X |
Rehabilitation, Cardiac Facilities |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QR0401X |
Rehabilitation, Comprehensive Outpatient Rehabilitation Facility (CORF) |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QR0405X |
Rehabilitation, Substance Use Disorder |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QR1100X |
Research |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QR1300X |
Rural Health |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QS1200X |
Sleep Disorder Diagnostic |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QS1000X |
Student Health |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QU0200X |
Urgent Care |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
261QV0200X |
VA |
260000000 |
Non-Individual - Ambulatory Health Care Facilities |
273100000X |
Epilepsy Unit |
270000000 |
Non-Individual - Hospital Units |
275N00000X |
Medicare Defined Swing Bed Unit |
270000000 |
Non-Individual - Hospital Units |
273R00000X |
Psychiatric Unit |
270000000 |
Non-Individual - Hospital Units |
273Y00000X |
Rehabilitation Unit |
270000000 |
Non-Individual - Hospital Units |
276400000X |
Rehabilitation, Substance Use Disorder Unit |
270000000 |
Non-Individual - Hospital Units |
287300000X |
Christian Science Sanitorium |
280000000 |
Non-Individual - Hospitals |
281P00000X |
Chronic Disease Hospital |
280000000 |
Non-Individual - Hospitals |
281PC2000X |
Children |
280000000 |
Non-Individual - Hospitals |
282N00000X |
General Acute Care Hospital |
280000000 |
Non-Individual - Hospitals |
282NC2000X |
Children |
280000000 |
Non-Individual - Hospitals |
282NC0060X |
Critical Access |
280000000 |
Non-Individual - Hospitals |
282NR1301X |
Rural |
280000000 |
Non-Individual - Hospitals |
282NW0100X |
Women |
280000000 |
Non-Individual - Hospitals |
282E00000X |
Long Term Care Hospital |
280000000 |
Non-Individual - Hospitals |
286500000X |
Military Hospital |
280000000 |
Non-Individual - Hospitals |
2865C1500X |
Community Health |
280000000 |
Non-Individual - Hospitals |
2865M2000X |
Military General Acute Care Hospital |
280000000 |
Non-Individual - Hospitals |
2865X1600X |
Military General Acute Care Hospital. Operational (Transportable) |
280000000 |
Non-Individual - Hospitals |
283Q00000X |
Psychiatric Hospital |
280000000 |
Non-Individual - Hospitals |
283X00000X |
Rehabilitation Hospital |
280000000 |
Non-Individual - Hospitals |
283XC2000X |
Children |
280000000 |
Non-Individual - Hospitals |
282J00000X |
Religious Nonmedical Health Care Institution |
280000000 |
Non-Individual - Hospitals |
284300000X |
Special Hospital |
280000000 |
Non-Individual - Hospitals |
291U00000X |
Clinical Medical Laboratory |
290000000 |
Non-Individual - Laboratories |
292200000X |
Dental Laboratory |
290000000 |
Non-Individual - Laboratories |
291900000X |
Military Clinical Medical Laboratory |
290000000 |
Non-Individual - Laboratories |
293D00000X |
Physiological Laboratory |
290000000 |
Non-Individual - Laboratories |
302F00000X |
Exclusive Provider Organization |
300000000 |
Non-Individual - Managed Care Organizations |
302R00000X |
Health Maintenance Organization |
300000000 |
Non-Individual - Managed Care Organizations |
305S00000X |
Point of Service |
300000000 |
Non-Individual - Managed Care Organizations |
305R00000X |
Preferred Provider Organization |
300000000 |
Non-Individual - Managed Care Organizations |
311500000X |
Alzheimer Center (Dementia Center) |
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
310400000X |
Assisted Living Facility |
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
3104A0630X |
Assisted Living, Behavioral Disturbances |
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
3104A0625X |
Assisted Living, Mental Illness |
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
317400000X |
Christian Science Facility |
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
311Z00000X |
Custodial Care Facility |
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
311ZA0620X |
Adult Care Home |
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
315D00000X |
Hospice, Inpatient |
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
310500000X |
Intermediate Care Facility, Mental Illness |
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
315P00000X |
Intermediate Care Facility, Mentally Retarded |
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
313M00000X |
Nursing Facility/Intermediate Care Facility |
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
314000000X |
Skilled Nursing Facility |
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
3140N1450X |
Nursing Care, Pediatric |
310000000 |
Non-Individual - Nursing & Custodial Care Facilities |
177F00000X |
Lodging |
170000000 |
Non-Individual - Other Service Providers |
174200000X |
Meals |
170000000 |
Non-Individual - Other Service Providers |
320800000X |
Community Based Residential Treatment Facility, Mental Illness |
320000000 |
Non-Individual - Residential Treatment Facilities |
320900000X |
Community Based Residential Treatment Facility, Mental Retardation and/or Developmental Disabilities |
320000000 |
Non-Individual - Residential Treatment Facilities |
323P00000X |
Psychiatric Residential Treatment Facility |
320000000 |
Non-Individual - Residential Treatment Facilities |
322D00000X |
Residential Treatment Facility, Emotionally Disturbed Children |
320000000 |
Non-Individual - Residential Treatment Facilities |
320600000X |
Residential Treatment Facility, Mental Retardation and/or Developmental Disabilities |
320000000 |
Non-Individual - Residential Treatment Facilities |
320700000X |
Residential Treatment Facility, Physical Disabilities |
320000000 |
Non-Individual - Residential Treatment Facilities |
324500000X |
Substance Abuse Rehabilitation Facility |
320000000 |
Non-Individual - Residential Treatment Facilities |
3245S0500X |
Substance Abuse Treatment, Children |
320000000 |
Non-Individual - Residential Treatment Facilities |
385H00000X |
Respite Care |
380000000 |
Non-Individual - Respite Care Facility |
385HR2050X |
Respite Care Camp |
380000000 |
Non-Individual - Respite Care Facility |
385HR2055X |
Respite Care, Mental Illness, Child |
380000000 |
Non-Individual - Respite Care Facility |
385HR2060X |
Respite Care, Mental Retardation and/or Developmental Disabilities |
380000000 |
Non-Individual - Respite Care Facility |
385HR2065X |
Respite Care, Physical Disabilities, Child |
380000000 |
Non-Individual - Respite Care Facility |
331L00000X |
Blood Bank |
330000000 |
Non-Individual - Suppliers |
332100000X |
Department of Veterans Affairs (VA) Pharmacy |
330000000 |
Non-Individual - Suppliers |
332B00000X |
Durable Medical Equipment & Medical Supplies |
330000000 |
Non-Individual - Suppliers |
332BC3200X |
Customized Equipment |
330000000 |
Non-Individual - Suppliers |
332BD1200X |
Dialysis Equipment & Supplies |
330000000 |
Non-Individual - Suppliers |
332BN1400X |
Nursing Facility Supplies |
330000000 |
Non-Individual - Suppliers |
332BX2000X |
Oxygen Equipment & Supplies |
330000000 |
Non-Individual - Suppliers |
332BP3500X |
Parenteral & Enteral Nutrition |
330000000 |
Non-Individual - Suppliers |
333300000X |
Emergency Response System Companies |
330000000 |
Non-Individual - Suppliers |
332G00000X |
Eye Bank |
330000000 |
Non-Individual - Suppliers |
332H00000X |
Eyewear Supplier (Equipment, not the service) |
330000000 |
Non-Individual - Suppliers |
332S00000X |
Hearing Aid Equipment |
330000000 |
Non-Individual - Suppliers |
332U00000X |
Home Delivered Meals |
330000000 |
Non-Individual - Suppliers |
332800000X |
Indian Health Service/Tribal/Urban Indian Health (I/T/U) Pharmacy |
330000000 |
Non-Individual - Suppliers |
335G00000X |
Medical Foods Supplier |
330000000 |
Non-Individual - Suppliers |
332000000X |
Military/U.S. Coast Guard Pharmacy |
330000000 |
Non-Individual - Suppliers |
332900000X |
Non-Pharmacy Dispensing Site |
330000000 |
Non-Individual - Suppliers |
335U00000X |
Organ Procurement Organization |
330000000 |
Non-Individual - Suppliers |
333600000X |
Pharmacy |
330000000 |
Non-Individual - Suppliers |
3336C0002X |
Clinic Pharmacy |
330000000 |
Non-Individual - Suppliers |
3336C0003X |
Community/Retail Pharmacy |
330000000 |
Non-Individual - Suppliers |
3336C0004X |
Compounding Pharmacy |
330000000 |
Non-Individual - Suppliers |
3336H0001X |
Home Infusion Therapy Pharmacy |
330000000 |
Non-Individual - Suppliers |
3336I0012X |
Institutional Pharmacy |
330000000 |
Non-Individual - Suppliers |
3336L0003X |
Long Term Care Pharmacy |
330000000 |
Non-Individual - Suppliers |
3336M0002X |
Mail Order Pharmacy |
330000000 |
Non-Individual - Suppliers |
3336M0003X |
Managed Care Organization Pharmacy |
330000000 |
Non-Individual - Suppliers |
3336N0007X |
Nuclear Pharmacy |
330000000 |
Non-Individual - Suppliers |
3336S0011X |
Specialty Pharmacy |
330000000 |
Non-Individual - Suppliers |
335V00000X |
Portable X-Ray Supplier |
330000000 |
Non-Individual - Suppliers |
335E00000X |
Prosthetic/Orthotic Supplier |
330000000 |
Non-Individual - Suppliers |
344800000X |
Air Carrier |
340000000 |
Non-Individual - Transportation Services |
341600000X |
Ambulance |
340000000 |
Non-Individual - Transportation Services |
3416A0800X |
Air Transport |
340000000 |
Non-Individual - Transportation Services |
3416L0300X |
Land Transport |
340000000 |
Non-Individual - Transportation Services |
3416S0300X |
Water Transport |
340000000 |
Non-Individual - Transportation Services |
347B00000X |
Bus |
340000000 |
Non-Individual - Transportation Services |
341800000X |
Military/U.S. Coast Guard Transport |
340000000 |
Non-Individual - Transportation Services |
3418M1120X |
Military or U.S. Coast Guard Ambulance, Air Transport |
340000000 |
Non-Individual - Transportation Services |
3418M1110X |
Military or U.S. Coast Guard Ambulance, Ground Transport |
340000000 |
Non-Individual - Transportation Services |
3418M1130X |
Military or U.S. Coast Guard Ambulance, Water Transport |
340000000 |
Non-Individual - Transportation Services |
343900000X |
Non-emergency Medical Transport (VAN) |
340000000 |
Non-Individual - Transportation Services |
347C00000X |
Private Vehicle |
340000000 |
Non-Individual - Transportation Services |
343800000X |
Secured Medical Transport (VAN) |
340000000 |
Non-Individual - Transportation Services |
344600000X |
Taxi |
340000000 |
Non-Individual - Transportation Services |
347D00000X |
Train |
340000000 |
Non-Individual - Transportation Services |
347E00000X |
Transportation Broker |
340000000 |
Non-Individual - Transportation Services |
Appendix M: Crosswalk of T-MSIS, MSIS and MMA Duel Eligible Code
Coding requirement on the DUAL-ELIGIBLE-CODE data element
When populating the DUAL-ELIGIBLE-CODE data element, States should ignore the coding requirement regarding Medicare Modernization Act. ("This field should be populated from the same data that were used to populate the State’s submission of the Medicare Modernization Act (“State MMA File”) monthly file to CMS. In other words, the data values from the State MMA File should match this dual eligible data element.")
CMS has already incorporated the MMA valid values into MSIS and carried them forth into T-MSIS, as can be seen in the crosswalk below.
T-MSIS |
MSIS |
MMA* |
00 Eligible is not a Medicare beneficiary |
00 Eligible is not a Medicare beneficiary
|
00 = Not Medicare enrolled for the month
|
01 Eligible is entitled to Medicare- QMB only |
01 Eligible is entitled to Medicare- QMB only
|
01 = QMB only
|
02 Eligible is entitled to Medicare- QMB AND Medicaid coverage |
02 Eligible is entitled to Medicare- QMB AND Medicaid coverage including RX
|
02 = QMB and Medicaid coverage including RX
|
03 Eligible is entitled to Medicare- SLMB only |
03 Eligible is entitled to Medicare- SLMB only
|
3 = SLMB only
|
04 Eligible is entitled to Medicare- SLMB AND Medicaid coverage |
04 Eligible is entitled to Medicare- SLMB AND Medicaid coverage including RX
|
04 = SLMB and Medicaid coverage including RX
|
05 Eligible is entitled to Medicare- QDWI |
05 Eligible is entitled to Medicare- QDWI
|
05 = QDWI
|
06 Eligible is entitled to Medicare- Qualifying individuals |
06 Eligible is entitled to Medicare- Qualifying individuals
|
06 = Qualifying Individuals
|
08 Eligible is entitled to Medicare- Other Dual Eligibles (Non QMB, SLMB, QDWI or QI) |
08 Eligible is entitled to Medicare- Other Dual Eligibles (Non QMB, SLMB,QWDI or QI) with Medicaid coverage including RX
|
08 = Other Dual Eligibles (Non-QMB, SLMB, QWDI, or QI) w/Medicaid coverage including RX
|
09 Eligible is entitled to Medicare – Other (This code is to be used only with specific CMS approval.) |
09 Eligible is entitled to Medicare – Other Dual Eligibles
|
09 = Other Dual Eligibles but without Medicaid coverage
|
10 Separate CHIP Eligible is entitled to Medicare |
10 Separate CHIP Eligible is entitled to Medicare
|
|
99 Eligible's Medicare status is unknown. |
99 Eligible's Medicare status is unknown.
|
99 – Unknown |
|
|
NA = Non-Medicaid
|
Appendix N: Coding Specific Data Elements for Claim Files
Clarification of the use of the PROCEDURE-CODE, REVENUE-CODE, HCPCS-RATE, BEGINNING-DATE-OF-SERVICE, and ENDING-DATE-OF-SERVICE fields in the CLAIMOT File.
Because the CLAIMOT file is a catch-all file that includes outpatient facility claims, professional claims and financial transactions, states are having confusion over when to populate the PROCEDURE-CODE, REVENUE-CODE, HCPCS-RATE , BEGINNING-DATE-OF-SERVICE, ENDING-DATE-OF-SERVICE, PROCEDURE-CODE-DATE, PROCEDURE-CODE-FLAG, and PROCEDURE-CODE-MOD-1 thru -4 fields. To assist them we have prepared the following guidelines.
For professional claims:
REVENUE-CODE should be 8-filled.
HCPCS-RATE should be 8-filled.
PROCEDURE-CODE-FLAG should be populated with either “01 (CPT-4), “06” (HCPCS), or “10” through “87” (to indicate other coding schemas).
PROCEDURE-CODE should be used to capture the CPT/HCPCS service codes.
PROCEDURE-CODE-MOD-1 thru -4 should be populated as needed.
BEGINNING-DATE-OF-SERVICE should show the 1st DOS associated with the service code in the PROCEDURE-CODE field.
ENDING-DATE-OF-SERVICE should show the last DOS associated with the service code in the PROCEDURE-CODE field.
PROCEDURE-CODE-DATE should be 8-filled (This field is superfluous. Beginning-/Ending-Date-of-Service captures the same information and provides more flexibility if the service is provided repeatedly over a period of time.)
For institutional claims for ambulatory care (reported on CLAIMOT file):
REVENUE-CODE should be used to capture the services provided.
HCPCS-RATE should be used to capture HCPCS details whenever they are needed to support the value in the REVENUE-CODE field. Otherwise, the field should be 8-filled.
PROCEDURE-CODE-FLAG should be 8-filled.
PROCEDURE-CODE field should be 8-filled.
PROCEDURE-CODE-MOD-1 thru -4 should be 8-filled.
BEGINNING-DATE-OF-SERVICE should show the 1st DOS associated with the service code in the REVENUE-CODE field.
ENDING-DATE-OF-SERVICE should show the last DOS associated with the service code in the REVENUE-CODE field.
PROCEDURE-CODE-DATE should be 8-filled (This field is superfluous. Beginning-/Ending-Date-of-Service captures the same information and provides more flexibility if the service is provided repeatedly over a period of time.)
For financial transactions1:
REVENUE-CODE field should be 8-filled.
HCPCS-RATE should be 8-filled.
PROCEDURE-CODE-FLAG should be 8-filled, or populated with “10” through “87” (to indicate other coding schemas if state-specific codes are used).
PROCEDURE-CODE field should be 8-filled unless the State has state-specific codes it uses to provide further detail (e.g., codes to split capitation payments into subcategories).
PROCEDURE-CODE-MOD-1 thru -4 should be 8-filled.
BEGINNING-DATE-OF-SERVICE should show the 1st day of the time period covered by this financial transaction.
ENDING-DATE-OF-SERVICE should show the last day of the time period covered by this financial transaction.
PROCEDURE-CODE-DATE should be 8-filled (This field is superfluous. Beginning-/Ending-Date-of-Service captures the same information and provides more flexibility if the service is provided repeatedly over a period of time.)
Appendix O: TYPE-OF-SERVICE Hierarchy Table
When a claim has multiple claim lines that could be reported in more than one CLAIMS file, in any combination as represented in columns A, B, C, or D, please report all claim lines in the CLAIMS file type represented by the green highlight in the table below, and report the TYPE-OF-SERVICE as follows:
For claim lines that would have been reported in the MSIS the LT, OT, and RX files,
They are now to be reported in
the T-MSIS CLAIMIP file as a complete claim, and
code the TYPE-OF-SERVICE to reflect the type of service that represents the entire facility claim (TYPE OF SERVICE CODE of 001, 060, 084, 086, 090, 091, 092, 093, 058, 123, 132, or 135, whichever is most appropriate for CLAIMIP record being reported).
Example – a multi-line claim that was reported in MSIS by the state as separate IP and OT records for the inpatient care, laboratory services, and emergency room services -is now to be reported in T-MSIS entirely as a single inpatient hospital facility claim with every line containing a TYPE-OF-SERVICE – 001.
2. For claim lines that would have been reported in the MSIS OT and RX files,
They are now to be reported in
the T-MSIS CLAIMLT file as a complete claim,
and code the TYPE-OF-SERVICE to reflect the type of service that represents the entire facility claim (TYPE-OF-SERVICE 009, 044, 045, 046, 047, 048, 050, 059, or 133 whichever is most appropriate for CLAIMLT claim record being reported)
3. For claim lines that would have been reported the RX and OT files in MSIS,
They are now to be reported in
the T-MSIS CLAIMRX file as a complete claim billed by a pharmacy or pharmacist (through a pharmacy point-of-sale system),and
code the TYPE-OF-SERVICE to reflect the type of service that was provided
Hierarchy Table – to be used when determining which file a claim is to be reported in when the TYPE-OF-SERVICE may be reportable in more than one claims file type. |
|||||||
A |
|
B |
|
C |
|
D |
|
IP |
Code TYPE-OF-SERVICE as one of the following for all lines 001, 060, 084, 086, 090, 091, 092, 093, 058, 123, 132, or 135 |
IP |
Code TYPE-OF-SERVICE as one of the following for all lines 001, 058, 123, 132, 135 |
|
|
|
|
LT |
|
|
|
LT |
Code TYPE-OF-SERVICE as one of the following for all lines 009, 044, 045, 046, 047, 048, 050, 059, 133 |
|
|
OT |
|
OT |
|
OT |
|
RX |
Code RX TYPE-OF-SERVICE for the RX line 033, 034 |
RX |
|
RX |
|
RX |
|
OT |
Code OT TYPE-OF-SERVICE as the Specific OT TYPE-OF-SERVICE |
Appendix P: CMS Guidance Library
Appendix P.01: Submitting Adjustment Claims to TMSIS
Brief Issue Description
There are two ways original claims and their subsequent adjustments can be linked into a claim family – either through all adjustments linking back to the original claim or each subsequent adjustment linking back to the prior claim (i.e. “daisy chain”). Identifying the members of a claim family is necessary in order to evaluate the changes to a claim that occur throughout its life.
Background Discussion
Before delving into CMS’ guidance on how to populate the ICN-ORIG and ICN-ADJ fields, some background discussion is needed on terminology and concepts.
What claim transactions should be submitted to T-MSIS?
Every “final adjudicated version of the claim/encounter” should be submitted to T-MSIS.
A “final adjudicated version of the claim/encounter” is a claim that has completed the adjudication process and the paid/denied process. The claim and each claim line will have one of the finalized claim status categories listed in Table 1, below. The actual disposition of the claim can be either “paid” or “denied.”
Table 1: Finalized Claim Status Categories
Code |
Finalized Claim Status Category Description |
F0 |
Finalized-The encounter has completed the adjudication cycle and no more action will be taken. (Used on encounter records) |
F1 |
Finalized/Payment-The claim/line has been paid. |
F2 |
Finalized/Denial-The claim/line has been denied. |
F3 |
Finalized/Revised - Adjudication information has been changed. |
Both original claims (or encounters) and adjusted claims (or encounters) can be a “final adjudicated version of the claim/encounter.” Whenever a claim/encounter flows through the adjudication and payment processes (if applicable) and falls into one of the claim status categories in Table 1, the state should send the claim/encounter to T-MSIS.
If a claim flows through the adjudication and payment processes and falls into one of the finalized claim status categories multiple times within a single T-MSIS reporting period, CMS expects each of these final adjudicated versions of the claim/encounter to be submitted to T-MSIS, not just the one effective on the last day of the reporting period.
If the claim has not been through the final adjudication process or is “pending” (or in “suspense”), the claim should not be sent to T-MSIS until disposition has been settled to one of the finalized claim status categories. Table 2 provides examples and CMS’ expectations.
Table 2: Scenarios for When to Submit Claims
Claim Submission Scenario |
CMS’ Expectation |
Adjudicated and paid in the same reporting month |
CMS expects the claim to be sent to T-MSIS in the reporting month. |
Adjudicated in one reporting period, but paid in another reporting month |
CMS expects the claim to be sent to T-MSIS in the month that the claim was paid. |
Adjudicated and paid in one reporting month, and then re-adjudicated and paid in a subsequent month |
The claim should be reported in the month it is paid, regardless of whether it is an original claim or an adjustment. Therefore, in this scenario, CMS expects the original to be reported in month one and the adjustment to be reported in the subsequent month. |
Adjudicated and paid, and then re-adjudicated and paid in the same reporting month |
In this scenario, if a claim flows through the adjudication and payment processes and falls into one of the claim status categories in Table 1 multiple times within a single T-MSIS reporting period, CMS expects each of these final adjudicated versions of the claim/encounter to be submitted to T-MSIS, not just the one effective on the last day of the reporting period. |
Re-adjudicated and paid multiple times in the same reporting month |
In this scenario, if a claim flows through the adjudication and payment processes and falls into one of the claim status categories in Table 1 multiple times within a single T-MSIS reporting period, CMS expects each of these final adjudicated versions of the claim/encounter to be submitted to T-MSIS, not just the one effective on the last day of the reporting period. |
What is a claim family?
A “claim family” (a.k.a. “adjustment set”)is defined as a set of post-adjudication claim transactions in paid or denied status that relate to the same provider/enrollee/services/dates of service. This grouping of the original claim and all of its subsequent adjustment and/or void claims shows the progression of changes that have occurred since it was first submitted.
How should ADJUSTMENT-IND codes be used?
The table below lists each of the adjustment indicator codes contained in the T-MSIS Data Dictionary version 1.1 and describes when it should be used.
Table 3: Adjustment Indicator Codes and Their Uses
Code |
Description of Use |
0 |
Original Claim/Encounter – Indicates this is the first time this family of claim/encounter records has been through the state’s adjudication and payment processes and is a final adjudicated version of the claim/encounter. |
1 |
Void of a prior submission – Use this code when the state wishes to remove a claim/encounter from T-MSIS and not replace it with an adjusted claim/encounter record. These records must have the same claim key data element values as the claim/encounter being voided. |
2 |
Do not use. |
3 |
Do not use. |
4 |
Debit Adjustment (positive supplemental) – Use whenever the claim is an adjusted claim. |
5 |
Credit Gross Adjustment – Use this code to indicate an aggregate-level recoupment of payments made previously to a provider (e.g., for a set of enrollees, claims, etc.) rather than recoupments made on specific claims. Amounts on these claims should be expressed as negative numbers. |
6 |
Debit Gross Adjustment – Use this code to indicate an aggregate-level additional payment to a provider (e.g., for a set of enrollees, claims, etc.) rather than payment made on a specific claim. Amounts on these claims should be expressed as positive numbers. |
9 |
Unknown |
Are gross adjustments considered claims/encounters?
While the gross adjustment adjudication indicator codes (values “5” and “6” in Table 3) are reported to T-MSIS in the CLAIM-OT file, they are not technically “claims” or “encounters.” Each of these transactions does not relate to a specific service-provider/enrollee episode of care. Instead, these transactions represent payments made by the state for services rendered to multiple enrollees (as in the case of a provider providing screening services for a group of enrollees), DSH payments, or a recoupment of funds previously dispensed in a debit gross adjustment. Therefore, the concept of “claims family” does not apply. Each of these transactions stands on its own, and does not constitute a subsequent transaction being a replacement of the earlier transaction.
What alternatives are there for tying the members of a claim family together?
The Original ICN Approach
Under this approach, the state assigns an ICN to the initial final adjudicated version of the claim/encounter and records this identifier in the ICN-ORIG field. If adjustment claims subsequently are created, the ICN assigned to the initial final adjudicated version of the claim/encounter is carried forward on every subsequent adjustment claim. Table 4 illustrates how the ICN-ORIG and ICN-ADJ values on the members of a claim family are populated when the original ICN approach is used.
Table 4: ICN-ORIG/ICN-ADJ Relationships Under the Original ICN Approach
Event |
ADJUDICATION-DATE |
ICN-ORIG |
ICN-ADJ |
ADJUSTMENT-IND |
On 5/1/2014, the state completes the adjudication process on the initial version of the claim |
5/1/2014 |
1 |
- |
0 |
On 7/15/2014, the state completes a claim re-adjudication / adjustment |
7/15/2014 |
1 |
2 |
4 |
On 8/12/2014, the state completes a 2nd claim re-adjudication / adjustment |
8/12/2014 |
1 |
3 |
4 |
On 9/5/2014, the state completes a 3rd claim re-adjudication / adjustment |
9/5/2014 |
1 |
4 |
4 |
The Daisy-Chain ICN Approach
Under this approach, the state records the ICN of the previous final adjudicated version of the claim/encounter in the ICN-ORIG field of the adjustment claim record. If additional adjustment claims are subsequently created, the ICN-ORIG on the new adjustment claim only points back one generation. Table 5 illustrates how the ICN-ORIG and ICN-ADJ values on the members of a claim family are populated when the daisy-chain ICN approach is used.
Table 5: ICN-ORIG/ICN-ADJ Relationships Under the Daisy-Chain ICN Approach
Event |
ADJUDICATION-DATE |
ICN-ORIG |
ICN-ADJ |
ADJUSTMENT-IND |
On 6/1/2014, the state completes the adjudication process on the initial version of the claim |
6/1/2014 |
11 |
- |
0 |
On 8/15/2014, the state completes a claim re-adjudication/adjustment |
8/15/2014 |
11 |
12 |
4 |
On 9/12/2014, the state completes a 2nd claim re-adjudication/adjustment |
9/12/2014 |
12 |
13 |
4 |
On 10/5/2014, the state completes a 3rd claim re-adjudication/adjustment |
10/5/2014 |
13 |
14 |
4 |
How are ICN-ORIG and ICN-ADJ fields impacted when voids are submitted?
The primary purpose of void transactions (ADJUSTMENT-IND = 1) is to nullify a claim/encounter from T-MSIS when the state does not wish to replace it with an adjusted claim/encounter record. These records must have the same claim key data element values as the claim/encounter being voided. Dollar and quantity fields should be set to zero. The ADJUDICATION-DATE on these records should be set to the date that the state voided the claim. Table 6 illustrates how the ICN-ORIG and ICN-ADJ values on the members of a claim family are populated when the state wishes to void a claim.
Table 6: ICN-ORIG/ICN-ADJ – Impact of Voids
Event |
ADJUDICATION-DATE |
ICN-ORIG |
ICN-ADJ |
ADJUSTMENT-IND |
Dollar Fields |
Quantity Fields |
On 6/1/2014, the state completes the adjudication process on the initial version of the claim |
6/1/2014 |
51 |
- |
0 |
100.00 |
5 |
On 8/15/2014, the state completes a claim re-adjudication/adjustment |
8/15/2014 |
51 |
52 |
4 |
80.00 |
5 |
On 8/19/2014, the claim is voided |
8/19/2014 |
51 |
52 |
1 |
0.00 |
0 |
If a state uses a process to record adjustments whereby they void the previous version of the claim and then follow-up with the creation of a new original transaction, and the state can identify that the void and the new original claim are from the same adjudication set, the state should link them together into one claims family using the ICN-ORIG. CMS recognizes that some states may not be able to link a resubmitted claim after a void to the original claim. Table 7 illustrates how CMS is expecting the states to populate the ICN-ORIG/ICN-ADJ fields when the state processes a void/new original when adjusting claims.
Table 7: ICN-ORIG/ICN-ADJ – Keeping the Claim Family Intact When the “Void/New Original” Scenario Occurs
Event |
ADJUDICATION-DATE |
ICN-ORIG |
ICN-ADJ |
ADJUSTMENT-IND |
Dollar Fields |
Quantity Fields |
On 6/1/2014, the state completes the adjudication process on the initial version of the claim |
6/1/2014 |
51 |
- |
0 |
100.00 |
5 |
On 8/15/2014, the state completes the adjudication process of a void and associated new original |
8/15/2014
|
51 |
- |
1 |
0.00 |
0 |
8/15/2014
|
51 |
52 |
0 |
80.00 |
5 |
|
On 9/20/2014, the state completes the adjudication process of a void and associated new original |
9/20/2014
|
51 |
52 |
1 |
0.00 |
0 |
9/20/2014
|
51 |
53 |
0 |
60.00 |
5 |
How Adjustment Records will be Applied by CMS
There is an inherent limitation in the way that CMS can interpret what to do with two claim transactions having the same ICN-ORIG and ADJUDICATION-DATE when both transactions are received in a single submission file. The processing rules that T-MSIS will follow are outlined below. It is up to each state to assure that claim transactions are processed in the appropriate sequence. If the rules below do not result in the sequence of transactions that the state desires, it is up to the state to submit transactions in separate files so that the desired sequence is attained.
Rules for inserting claim transactions into the T-MSIS database when two or more claim transactions with the same ICN-ORIG and ADJUDICATION-DATE are in the same submission file
If two or more transactions in an incoming claim file have the same ICN-ORIG and ADJUDICATION-DATE values, T-MSIS will evaluate the ADJUSTMENT-IND values and insert the transactions into the T-MSIS database as follows:
If more than two transactions in the incoming claim file have the same ICN-ORIG and ADJUDICATION-DATE values, then T-MSIS will reject all of the incoming transactions;
If the ADJUSTMENT-IND values of both incoming transactions are the same (but not ‘5’ or ‘6’), then T-MSIS will reject both incoming transactions;
If the ADJUSTMENT-IND values of both incoming transactions are some combination of ‘5’ and ‘6’ and if there is no active existing transaction in the T-MSIS DB, then T-MSIS will insert both incoming transactions into the T-MSIS DB (note, since neither transaction supersedes the other, the order in which they are inserted does not matter);
If the ADJUSTMENT-IND values of both incoming transactions are some combination of ‘5’ and ‘6’ and if there is an active existing transaction in the T-MSIS DB with an ADJUSTMENT-IND value of ‘5’ or ‘6’, then T-MSIS will insert both incoming transactions into the T-MSIS DB (note, since neither transaction supersedes the other, the order in which they are inserted does not matter);
If the ADJUSTMENT-IND values of both incoming transactions is a ‘5’ or ‘6’ and if there is an active existing transaction in the T-MSIS DB with an ADJUSTMENT-IND value of ‘0’, ‘1’, or ‘4’, then T-MSIS will reject both the incoming transactions;
If the ADJUSTMENT-IND value of one incoming transaction is a ‘5’ or ‘6’ and the ADJUSTMENT-IND of the other transaction is ‘0’, ‘1’, or ‘4’ and if there is an active existing transaction in the T-MSIS DB with an ADJUSTMENT-IND value of ‘5’ or ‘6’, then T-MSIS will insert the incoming transaction with ADJUDICATION-IND of ‘5’ or ‘6’ and reject the incoming transaction with ADJUSTMENT-IND value ‘0’, ‘1’, or ‘4’;
If the ADJUSTMENT-IND value of one incoming transaction is a ‘5’ or ‘6’ and the ADJUSTMENT-IND of the other transaction is ‘0’, ‘1’, or ‘4’ and there is an active existing transaction in the T-MSIS DB with an ADJUSTMENT-IND value of ‘0’, ‘1’, or ‘4’, then T-MSIS will reject the incoming transaction with ADJUSTMENT-IND value ‘5’ or ‘6’ and evaluate the remaining incoming transaction as follows:
ADJUSTMENT-IND of the remaining incoming transaction is ‘0’ and the ADJUSTMENT-IND of the active existing transaction is ‘0’, then T-MSIS will reject the incoming transaction;
ADJUSTMENT-IND of the remaining incoming transaction is ‘0’ and the ADJUSTMENT-IND of the active existing transaction is ‘1’, then T-MSIS will insert the incoming transaction;
ADJUSTMENT-IND of the remaining incoming transaction is ‘0’ and the ADJUSTMENT-IND of the active existing transaction is ‘4’, then T-MSIS will reject the incoming transaction;
ADJUSTMENT-IND of the remaining incoming transaction is ‘1’ and the ADJUSTMENT-IND of the active existing transaction is ‘0’, then T-MSIS will insert the incoming transaction;
ADJUSTMENT-IND of the remaining incoming transaction is ‘1’ and the ADJUSTMENT-IND of the active existing transaction is ‘1’, then T-MSIS will reject the incoming transaction;
ADJUSTMENT-IND of the remaining incoming transaction is ‘1’ and the ADJUSTMENT-IND of the active existing transaction is ‘4’, then T-MSIS will insert the incoming transaction;
ADJUSTMENT-IND of the remaining incoming transaction is ‘4’ and the ADJUSTMENT-IND of the active existing transaction is ‘0’, then T-MSIS will insert the incoming transaction;
ADJUSTMENT-IND of the remaining incoming transaction is ‘4’ and the ADJUSTMENT-IND of the active existing transaction is ‘1’, then T-MSIS will insert the incoming transaction;
ADJUSTMENT-IND of the remaining incoming transaction is ‘4’ and the ADJUSTMENT-IND of the active existing transaction is ‘4’, then T-MSIS will insert the incoming transaction;
If the ADJUSTMENT-IND value of one incoming transaction is ‘1’ and the ADJUSTMENT-IND of the other transaction is ‘0’ or ‘4’ and the ADJUSTMENT-IND of the active existing transaction in the T-MSIS DB is ‘0’ or ‘4’, then T-MSIS will insert the incoming transaction with ADJUSTMENT-IND = ‘1’ first, and then insert the other transaction;
If the ADJUSTMENT-IND value of one incoming transaction is ‘1’ and the ADJUSTMENT-IND of the other transaction is ‘0’ or ‘4’ and the ADJUSTMENT-IND of the active transaction in the T-MSIS DB is ‘1’, then T-MSIS will insert the incoming transaction with ADJUSTMENT-IND value of ‘0’ or ‘4’ first and then insert the incoming transaction with ADJUSTMENT-IND = ‘1’;
If the ADJUSTMENT-IND value of one incoming transaction is ‘0’ and the ADJUSTMENT-IND value of the other incoming transaction is ‘4’ and there is no active existing transaction in the T-MSIS DB, then T-MSIS will insert the incoming transaction with ADJUSTMENT-IND value of ‘0’ first and then insert the incoming transaction with ADJUSTMENT-IND = ‘4’;
If any other combination of ADJUSTMENT-IND values occurs, then T-MSIS will reject all of the transactions.
CMS Guidance
The state can use either the original ICN approach or the daisy-chain ICN approach to populate the ICN-ORIG field on each member of the claims family. T-MSIS will group claim transactions into claim families as part of the ETL process.
Appendix P.02: Reporting Financial Transactions in T-MSIS - How to populate T-MSIS claim files when reporting non-claim expenditures and recoupments
Brief Issue Description:
The purpose of this guidance document is to clarify the appropriate way to report non-claim expenditure and recoupment transactions, since many of the data elements on the claim records (CLAIMIP, CLAIMLT, CLAIMOT, and CLAIMRX) do not seem appropriate for these types of transactions.
Background Discussion
Definition of a financial transaction:
For purposes of this guidance, CMS defines a financial transaction as an expenditure transaction or a recoupment of a previously made expenditure that does not flow through the usual claim adjudication/adjustment process.
The cause or effect of this may be that these types of transactions do not contain the same level of detail as other types of transactions in the state’s system. For example, a state might not assign a service code to a capitation claim. Payments made in lump sums, such as Disproportionate Share Hospital (DSH) payments, because they cannot be attributed to a single beneficiary would not contain a beneficiary identifier.
For some states, examples of financial transactions might include capitation payments made to managed care organizations, supplemental payments (i.e., payments that are above a capitation fee or for a sum above a negotiated rate, such as an FQHC additional reimbursement), drug rebates, DSH payments, cost settlements (e.g., program cost reconciliations and settlements, year-end reconciliation of risk pools), aggregate-level payments to providers (e.g., for a set of enrollees, claims, etc.) rather than payments made on a specific claim.
Financial Transactions may be reported on CLAIMIP, CLAIMLT, CLAIMOT, or CLAIMRX depending on the type and circumstances of the financial transaction. “Table 1 – Financial Transactions and the appropriate T-MSIS file for reporting them” identifies which T-MSIS files are appropriate for the various types of financial transactions.
Table 1 – Financial transactions and the appropriate T-MSIS file for reporting them
-
At Enrollee Level
For Multiple Enrollees (i.e., a Service Tracking Claim)
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
DSH Pymt
Other Pymt
CLAIMOT
CLAIMOT
CLAIMRX
CLAIMIP
CLAIMLT
CLAIMOT
CLAIMRX
CLAIMIP
CLAIMLT
CLAIMOT
CLAIMRX
CLAIMOT
CLAIMOT
CLAIMRX
CLAIMIP
CLAIMLT
CLAIMOT
CLAIMRX
CLAIMIP
CLAIMLT
CLAIMOT
CLAIMRX
CLAIMIP
CLAIMOT
CLAIMIP
CLAIMLT
CLAIMOT
CLAIMRX
Financial transactions can be contained within the same files as fee-for-service claims and encounter records.
CMS Guidance
When and how to populate data elements for financial transactions:
The data elements listed on the following pages are ones that should be populated on financial transactions. Additional verbiage is provided for those data elements that CMS believes need explicit instructions for building T-MSIS files. States should contact their T-MSIS technical assistant or state liaison if they have questions or concerns. Data elements not specifically listed below can be 8-filled.
CLAIM-HEADER-RECORD data elements
RECORD-ID
SUBMITTING-STATE
RECORD-NUMBER
MSIS-IDENTIFICATION-NUM – Populate with beneficiary’s MSIS ID for any beneficiary-specific financial transactions. Otherwise first character of MSIS-IDENTIFICATION-NUM must be “&” to indicate that any characters that might follow do not represent an individual beneficiary’s identifier.
ICN-ORIG – See the document entitled CMS Guidance: T-MSIS Adjustment Claim Records- Populating ICN-ORG and ICN-ADJ Fields posted on 2/18/2014 to the T-MSIS State Support.
ICN-ADJ – See the document entitled CMS Guidance: T-MSIS Adjustment Claim Records- Populating ICN-ORG and ICN-ADJ Fields posted on 2/18/2014 to the T-MSIS State Support
ADJUDICATION-DATE – Date the transaction's approval and payment processes were completed.
CHECK-EFF-DATE – Populate with the date that Medicaid funds were disbursed. (Note: Even though the TOT-MEDICIAD-PAID-AMT field may be set to zero in some circumstances, Medicaid funds were disbursed – and are captured in the SERVICE-TRACKING-PAYMENT-AMT data element.)
ADMISSION-DATE – Populate with the first day of the time period covered by this financial transaction (CLAIMIP and CLAIMLT).
DISCHARGE-DATE – Populate with the last day of the time period covered by this financial transaction (CLAIMIP and CLAIMLT).
BEGINNING-DATE-OF-SERVICE – Populate with the first day of the time period covered by this financial transaction (CLAIMOT).
ENDING-DATE-OF-SERVICE – Populate with the last day of the time period covered by this financial transaction (CLAIMOT).
DATE-PRESCRIBED – Populate with the first day of the time period covered by this financial transaction (CLAIMRX).
PRESCRIPTION-FILL-DATE – Populate with the last day of the time period covered by this financial transaction (CLAIMRX).
WAIVER-TYPE – Populate if applicable and available
WAIVER-ID – Populate if applicable and available
PLAN-ID-NUMBER – Populate with the managed care plan ID for capitation payments made to managed care plans. 8-fill if transaction does not involve a manage care plan.
BILLING-PROV-NPI-NUM – Populate with the provider or entity that the financial transaction was addressed to. 8-fill if transaction involves a manage care plan.
TOT-MEDICIAD-PAID-AMT – If TYPE-OF-CLAIM is 4, D, or X, then set to zero – service tracking payment amount will be populated instead. Otherwise populate with the amount paid to the provider or health plan.
SERVICE-TRACKING-PAYMENT-AMT – If TYPE-OF-CLAIM is 4, D, or X, then populate this with the amount paid, otherwise 0-fill.
TYPE-OF-CLAIM – valid values appropriate for each type of financial transaction are shown in Table 2. (The descriptions of the TYPE-OF-CLAIM values are shown in Table 3. The values appropriate for financial transactions are highlighted in yellow.)
Table 2 – TYPE-OF-CLAIM values for financial transactions
-
At Enrollee Level
For Multiple Enrollees (i.e., a Service Tracking Claim)
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
DSH Pymt
Other Pymt
2, B, V
5, E, Y
5, E, Y
5, E, Y
4, D, X
4, D, X
4, D, X
4, D, X
4, D, X
4, D, X
Table 3 – Descriptions of TYPE-OF-CLAIM values
-
Type of Claim Code
Description
Purpose
Medicaid or Medicaid Expansion
Separate CHIP (Title XXI)
Other
1
A
U
Fee-For-Service Claim
Used to report services billed & payments made for specific services rendered to a specific enrollee by a specific provider during a specific period of time. Payment is made only for services actually rendered.
2
B
V
Capitation Payment
Used to report periodic payments made in return for a contractual commitment by the recipient to provide a specified set of services to a specified set of enrollees for a specified period of time. The volume of services actually provided to any given individual is not a factor in the amount of the capitation payment.
3
C
W
Encounter Record
Used to report services provided under a capitated payment arrangement.
This includes billing records submitted by providers to non-state entities (e.g., MCOs, health plans) for which the State has no financial liability, since the risk entity has already received a capitated payment from the State.
4
D
X
Service Tracking Claim
Use to report payments made for services rendered to enrollees when the services are not billed and paid at the single enrollee/provider/visit level of detail.
5
E
Y
Supplemental Payment
Used to identify payments that are above a capitation fee or for a sum above a negotiated rate, such as an FQHC additional reimbursement.
SOURCE-LOCATION– valid values appropriate for each type of financial transaction are shown in Table 4.
Table 4 – Descriptions of SOURCE-LOCATION values
-
Code
Description
01
MMIS
02
Non-MMIS CHIP Payment System
03
Pharmacy Benefits Manager (PBM) Vendor
04
Dental Benefits Manager Vendor
05
Transportation Provider System
06
Mental Health Claims Payment System
07
Financial Transaction/Accounting System
08
Other State Agency Claims Payment System
09
County/Local Government Claims Payment System
10
Other Vendor/Other Claims Payment System
20
Managed Care Organization (MCO)
SERVICE-TRACKING-TYPE – The appropriate values for financial transactions are shown in Table 5. (The descriptions of the SERVICE-TRACKING-TYPE values are shown in Table 6.)
Table 5 – SERVICE-TRACKING-TYPE values for financial transactions
-
At Enrollee Level
For Multiple Enrollees (i.e., a Service Tracking Claim)
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
DSH Pymt
Other Pymt
00
00
00
00
03
01
04
05
02
03, 06
Table 6 – Descriptions of SERVICE-TRACKING-TYPE values
-
Code
Description
00
Not a Service Tracking Claim – Use this code when codes 01 through 06 do not apply
01
Drug Rebate
02
DSH Payment
03
Lump Sum Payment (The "lump sum payment" code identifies payments made for specific services rendered to individual patients, when the state accepts a lump sum bill from a provider that covered similar services delivered to more than one patient (e.g., a group screening for EPSDT).
04
Cost Settlement
05
Supplemental (The "supplemental payment" code identifies payments that are above a capitation fee or sum above a negotiated rate (e.g., FQHC additional reimbursement).)
06
Other
FUNDING-CODE – The appropriate values for financial transactions are shown in Table 7. (The descriptions of the FUNDING-CODE values are shown in Table 8.)
Table 7 – FUNDING-CODE values for financial transactions
-
At Enrollee Level
For Multiple Enrollees (i.e., a Service Tracking Claim)
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
DSH Pymt
Other Pymt
A or B as appro-priate
A through E
A through I as appro-priate
A through I as appro-priate
A or B as appro-priate
A through E
A through I as appro-priate
A through I as appro-priate
A through I as appro-priate
A through I as appro-priate
Table 8 – Descriptions of FUNDING-CODE values
-
Code
Description
A
Medicaid Agency
B
CHIP Agency
C
Mental Health Service Agency
D
Education Agency
E
Child and Family Services Agency
F
County
G
City
H
Providers
I
Other
CLAIM-LINE-RECORD data elements
SUBMITTING-STATE
RECORD-NUMBER
MSIS-IDENTIFICATION-NUM
ICN-ORIG
ICN-ADJ
LINE-NUM-ORIG
LINE-NUM-ADJ
ADJUDICATION-DATE – Date the line-level transaction's approval and payment processes were completed
REVENUE-CODE – 8-fill
PROCEDURE-CODE – 8-fill
NATIONAL-DRUG-CODE – 8-fill
MEDICAID-PAID-AMT – Because there is no data element on the claim line record segment specifically designated to capture service tracking payment amounts at the claim line level, states should populate MEDICAID-PAID-AMT with the amount of Medicaid funds disbursed. For service tracking claims, the sum of the claim line MEDICAID-PAID-AMT values on a claim’s claim line record segments should equal the amount reported in the SERVICE-TRACKING-PAYMENT-AMT data element on the claim’s claim header record segment.
TYPE-OF-SERVICE – The appropriate values for financial transactions are shown in Table 9.
Table 9 – TYPE-OF-SERVICE values for financial transactions
-
At Enrollee Level
For Multiple Enrollees (i.e., a Service Tracking Claim)
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
DSH Pymt
Other Pymt
119, 120, 121, 122
131
132, 133, 134, 135
Any TOS except 119, 120, 121, 122, 123, 131, 132, 133, 134, 135
119, 120, 121, 122
131
132, 133, 134, 135
Any TOS except 119, 120, 121, 122, 123, 131, 132, 133, 134, 135
123
Any TOS except 119, 120, 121, 122, 123, 131, 132, 133, 134, 135
CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT – The appropriate values for financial transactions are shown in Table 10.
Table 10 – CMS-64-CATEGORY-FOR-FEDERAL-REIMBURSEMENT values for financial transactions
-
At Enrollee Level
For Multiple Enrollees (i.e., a Service Tracking Claim)
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
DSH Pymt
Other Pymt
If TYPE-OF-CLAIM = 2, then 01
If TYPE-OF-CLAIM = B then 02
If TYPE-OF-CLAIM = V then 03 or 04 as appro-priateIf TYPE-OF-CLAIM = 5, then 01
If TYPE-OF-CLAIM = E then 02
If TYPE-OF-CLAIM = Y then 03 or 04 as appro-priateIf TYPE-OF-CLAIM = 5, then 01
If TYPE-OF-CLAIM = E then 02
If TYPE-OF-CLAIM = Y then 03 or 04 as appro-priateIf TYPE-OF-CLAIM = 5, then 01
If TYPE-OF-CLAIM = E then 02
If TYPE-OF-CLAIM = Y then 03 or 04 as appropriateIf TYPE-OF-CLAIM = 2, then 01
If TYPE-OF-CLAIM = B then 02
If TYPE-OF-CLAIM = V then 03 or 04 as appro-priateIf TYPE-OF-CLAIM = 4, then 01
If TYPE-OF-CLAIM = D then 02
If TYPE-OF-CLAIM = X then 03 or 04 as appro-priateIf TYPE-OF-CLAIM = 4, then 01
If TYPE-OF-CLAIM = D then 02
If TYPE-OF-CLAIM = X then 03 or 04 as appro-priateIf TYPE-OF-CLAIM = 4, then 01
If TYPE-OF-CLAIM = D then 02
If TYPE-OF-CLAIM = X then 03 or 04 as appropriateIf TYPE-OF-CLAIM = 4, then 01
If TYPE-OF-CLAIM = D then 02
If TYPE-OF-CLAIM = X then 03 or 04 as appro-priateIf TYPE-OF-CLAIM = 4, then 01
If TYPE-OF-CLAIM = D then 02
If TYPE-OF-CLAIM = X then 03 or 04 as appropriate
o. XIX-MBESCBES-CATEGORY-OF-SERVICE – The appropriate values for financial transactions are shown in Table 11.
Table 11 – XIX-MBESCBES-CATEGORY-OF-SERVICE values for financial transactions
-
At Enrollee Level
For Multiple Enrollees (i.e., a Service Tracking Claim)
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
DSH Pymt
Other Pymt
17A, 17B, 17C1, 18A, 18B1, 18B2, 18C, 18E, 22
7A1, 7A2, 7A3, 7A4, 7A5, 7A6
Any code
1C, 1D, 3B, 4C, 5B, 6B, 9B
17A, 17B, 17C1, 18A, 18B1, 18B2, 18C, 18E, 22
7A1, 7A2, 7A3, 7A4, 7A5, 7A6
Any code
1C, 1D, 3B, 4C, 5B, 6B, 9B
1B, 2B
Any code except 1B, 1C, 1D, 2B, 3B, 4C, 5B, 6B, 9B, 7A1, 7A2, 7A3, 7A4, 7A5, 7A6, 17A, 17B, 17C1, 18A, 18B1, 18B2 18C, 18E, 22
p. XXI-MBESCBES-CATEGORY-OF-SERVICE – The appropriate values for financial transactions are shown in Table 12.
Table 12 – XXI-MBESCBES-CATEGORY-OF-SERVICE values for financial transactions
-
At Enrollee Level
For Multiple Enrollees (i.e., a Service Tracking Claim)
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
Cap Pymt
Drug Rebate
Cost Stlmnt
Spplmntl Pymt
DSH Pymt
Other Pymt
1A, 1B, 1C, 1D, or 32B
8A
Any code
8-fill
1A, 1B, 1C, 1D, or 32B
8A
Any code
8-fill
8-fill
Any code except 1A, 1B, 1C, 1D, 32B, or 8A
Appendix P.03: Full File Replacement Submissions for Non-Claim T-MSIS File revised
Brief Issue Description
States, CMS Analysts and T-MSIS partners have provided extensive feedback regarding the complexities of submitting only changed records to T-MSIS for non-claim files (TPL, ELIGIBLE, PROVIDER and MNGDCARE). As a result, the technical requirements for submitting non-claim T-MSIS files have been modified.
CMS Guidance
CMS will now require states to submit full-file refreshes for each reporting period for the non-claims files. This supersedes the previous requirement for states to submit only those fully changed or added records that were instituted in the states’ MMIS for the reporting period (referred to as Delta records or Deltas) each month after the initial T-MSIS production submission.
CMS believes this revised approach will be less burdensome to states. If this requirement creates additional concerns for a state, please contact your CMS liaison immediately to discuss.
The following requirements and points of clarification are applicable to the submission of full-file refreshes of non-claims files:
The first T-MSIS production submission for each file type provides a baseline of the State’s active Medicaid records for eligible, claims, providers, third party claims, and managed care data that were processed during the month.
For each subsequent reporting period, states will submit the complete historical data content for each of the non-claims files. States will be required to submit full-file refreshes on a monthly basis, regardless of whether there are changes to submit for the reporting period.
Each monthly Create submission for non-claim files will encompass a full-file refresh. Update submissions will be used to correct record errors in the Create submission that prevent them from being accepted. A Replacement submission replaces all records in the Create submission.
The Replacement file will be rejected for a previous month’s submission if a Create file for the subsequent month has already been processed. An Update file will be accepted for a previous month’s submission even if a Create file for the subsequent month has already been processed.
It is important to note that states are the system of record for the T-MSIS data; therefore, when states submit corrections in Update or Replacement files, the order of their submissions may overlay data that should be correctly stored in T-MSIS. When the state generates an Update file to correct rejected records, T-MSIS will process and apply those records to the data repository and that data will become the current data. It will be up to the states to ensure that Update and Replacement files are submitted in the appropriate sequence.
Each time the full-file refresh is submitted for the non-claims files, T-MSIS will review the content to determine if the data already exists, identify the data that will be added or changed and the content in that full-file refresh that excludes data reported in previous months. CMS expects that, at some point in the future, the state’s MMIS will archive data from the non-claims files and will no longer report those archived records in future T-MSIS submissions.
For those records that are archived in the state’s MMIS, T-MSIS will generate an informational report. T-MSIS will retain these archived records and provide the states with a report of those records after the file submissions. States will submit an Update or Replacement file when there is a need to make correction to those archived records, otherwise the records will remain in T-MSIS.
All child segments must have effective time ranges that fit within the time range of their parent segments. Multiple child segments may exist for a single parent segment or multiple parent segments can exist for a single child segment; however, the time spans of multiple records for a segment should not overlap. Keep in mind that as a general rule, parent segment date spans should not have gaps. Otherwise, the parent/child date span constraint rules will be violated. The diagram below illustrates the concept of a single child segment having multiple parent segments:
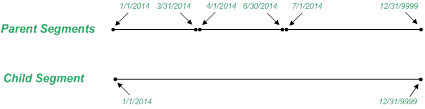
If gaps in the date span of the parent do legitimately exist, its child records should be adjusted accordingly.
Parent and child records can be submitted in any order in the file. States must ensure that the parent and child segments for each record have the correct data elements identified as ‘keys’ for the segments to have the right correlation and no orphan segments exist in the file. For data elements where the state tracks the date spans, the state will submit the effective and end dates as stored in the state’s systems.
Examples of segments expected to include business dates2:
ELIGBILE
HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006
HEALTH-HOME-SPA-PROVIDERS-ELG00007
LOCK-IN-INFORMATION-ELG00009
MFP-INFORMATION-ELG00010
STATE-PLAN-OPTION-PARTICIPATION-ELG00011
WAIVER-PARTICIPATION-ELG00012
LTSS-PARTICIPATION-ELG00013
MANAGED-CARE-PARTICIPATION-ELG00014
1115A-DEMONSTRATION-INFORMATION-ELG00018
ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021
PROVIDER
PROV-LICENSING-INFO-PRV00004
PROV-IDENTIFIERS-PRV00005
PROV-TAXONOMY-CLASSIFICATION-PRV00006
PROV-MEDICAID-ENROLLMENT-PRV00007
PROV-AFFILIATED-GROUPS-PRV00008
PROV-AFFILIATED-PROGRAMS-PRV00009
PROV-BED-TYPE-INFO-PRV00010
TPL
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004
TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005
MNGDCARE
MANAGED-CARE-MAIN-MCR00002
MANAGED-CARE-SERVICE-AREA-MCR00004
MANAGED-CARE-OPERATING-AUTHORITY-MCR00005
MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008
CHPID-SHPID-RELATIONSHIPS-MCR00009
For data elements where the state doesn’t track the beginning and ending dates of the effective period, the state will report the value effective as of the close of the reporting period and the effective time span for these data elements will cover all time. (If the data element value changes at some point, the new value will be applicable to all time and the previous value will be considered irrelevant.)
Examples of segments that are not expected to include business dates
ELIGIBLE
PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002
VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003
ELIGIBILE-CONTACT-INFORMATION-ELG00004
ETHNICITY-INFORMATION-ELG00015
RACE-INFORMATION-ELG00016
PROVIDER
PROV-ATTRIBUTES-MAIN-PRV00002
PROV-LOCATION-AND-CONTACT-INFO-PRV00003
TPL
TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002
TPL-ENTITY-CONTACT-INFORMATION-TPL00006
MNGDCARE
MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003
The Excel workbook entitled T-MSIS Record Segment Effective Date Span Example - 2014-02-07.xlsx illustrates how CMS expects a state to populate the data elements in a record segment when some of the data elements’ values change.
The monthly claims files will continue to encompass those records or transactions that occur within the start and end times of the reporting period. In other words, the full-file replacement option does not apply to claims files (CLAIMIP, CLAIMOT, CLAIMRX and CLAIMLT).
Appendix P.04: Non-Claim Full File Refreshes - Amount of History Required
How to use this guidance document
This guidance document is not intended to slow down or derail existing state development initiatives. The intent is to provide clarification and standardization across the nation in key areas raised by state partners. Should guidance introduce rework in ongoing development, please bring this to the attention of your TA and CMS analyst to direct you to the most appropriate path that minimizes impact to your progress.
Brief Issue Description
In its guidance on the submission of non-claim files to T-MSIS (CMS Guidance: Submission of Full-file Replacement Submissions for Non-Claims Files; released 2/18/2014 and revised 3/19/2014), CMS required states to submit the complete historical data content for each of the non-claims files in each monthly submission. Subsequent to this guidance, states have raised questions about how CMS defines the term “complete historical data content.”
This guidance document provides clarification on what CMS means by “complete historical data content.”
Background Discussion
Definitions
Non-Claim Subject Area – The general focus of the four non-claim T-MSIS files – (1) eligibility/enrollment, (2) providers, (3) managed care entities, and (4) third party liability sources.
Active – The data element values at the time the state creates the T-MSIS file which it believes to be valid and accurate for the time span bounded by the record segment’s effective and end dates.
“Active” segments are not limited only to those which are effective as of the close of the reporting period. For example, an enrollee may have multiple record segments in the current tables of the state’s MMIS for time spans during which the person’s eligibility characteristics changed over time. One or all of these spans could represent “inactive eligibility” (i.e., the span’s end date is some date in the past), but these records would still need to be submitted to T-MSIS since claims with service dates falling into these time spans may exist.
Complete – All data elements on all record segments for all active records in the state’s system. Even if a data element (or even an entire record segment) is not applicable (e.g., the state does not offer a health home program), T-MSIS is still expecting an 8-filled data element, or in the case of a not-applicable record segment, a record segment with all data elements 8-filled except the two or three needed to tie the segment to its parent segment. (For example, SUBMITTING–STATE and MSIS-IDENTIFICATION-NUM is needed to tie the HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 child segment to its parent (i.e., PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002))
Historical – Table 1 (T-MSIS Non-Claim, Full-File Refresh File Content Requirements by Subject Area) outlines CMS’ definition of historical data content for each of the four non-claim subject areas.
Table 1: T-MSIS Non-Claim, Full-File Refresh File Content Requirements by Subject Area
Scenario |
Eligible |
Provider |
Managed Care |
Third Party Liability |
Initial T-MSIS File Submission |
All active records – both those with open-ended active periods and those historical records with effective end dates going back at least to 10/1/2006 (i.e., 7 fiscal years from the 1/1/2014 T-MSIS go-live target date)3 – for all Medicaid or CHIP enrollees who:
Note: MSIS eligibility data will be migrated into the T-MSIS environment. MSIS-sourced data that are overlapped by subsequent T-MSIS submissions will be end-dated so that the overlapping effective period is removed and the MSIS-sourced and T-MSIS-sourced data’s effective periods will be contiguous. |
All active records – both those with open-ended active periods and those historical records with effective end dates going back at least to 10/1/2006 (i.e., 7 fiscal years from the 1/1/2014 T-MSIS go-live target date)1 – for all providers who:
|
All active records – both those with open-ended active periods and those historical records with effective end dates going back at least to 10/1/2006 (i.e., 7 fiscal years from the 1/1/2014 T-MSIS go-live target date)1 – for all managed care entities that:
|
TPL sources (health insurance and other third party sources of funds) that are actively being worked by the state at the time the initial TPL file is created. |
Subsequent Months’ Submissions |
Same as for the initial T-MSIS file submission, except that when the state archives records,4 these records no longer need to be included in subsequent submissions. |
Same as for the initial T-MSIS file submission, except that when the state archives records,2 these records no longer need to be included in subsequent submissions. |
Same as for the initial T-MSIS file submission, except that when the state archives records,2 these records no longer need to be included in subsequent submissions. |
As the state resolves, closes-out, and archives cases, it can stop sending these archived records.2 New TPL sources should be added as the state becomes aware of them. |
CMS Guidance
States should submit the complete, active, historical data content for the subject area in every T-MSIS non-claim, full-file refresh file as defined in Table 1, above.
Appendix P.05: Populating Qualifier Fields and Their Associated Value Fields
Brief Issue Description
The purpose of this guidance document is to when record segments need to be created for all valid values in a qualifier field’s valid value set and when it is appropriate to create a record segment for only one of the valid values.
Background Discussion
Definitions
Simple Qualifier Field – is a data element that contains a code (a.k.a. “flag”) that defines/qualifies the coding schema used when populating a set of corresponding data elements. This is necessary because there are several different schemas that a state could use and it needs to be clear which of the schemas is actually used.
Examples of “simple qualifier fields” are the DIAGNOSIS-CODE-FLAG-1 through -12 on the CLAIM-HEADER-RECORD-IP record segment (CIP00002). The valid value set for these fields is:
ICD-9
ICD-10
Other
The state would indicate which coding schema is being used to populate the corresponding data elements DIAGNOSIS-CODE-1 through -12.
Complex Qualifier Field – is a data element that not only defines/qualifies the contents of its corresponding data elements (similar to a “simple qualifier field”), but also represents a situation where the state needs to create a record segment for each valid value that applies to the record’s subject.
An example of a “complex qualifier field is LICENSE-TYPE on the PROV-LICENSING-INFO record segment (PRV00004). The valid value set for this field is:
State, county, or municipality professional or business license
DEA license
Professional society accreditation
CLIA accreditation
Other
The state would create a PROV-LICENSING-INFO record segment and populate the corresponding data elements for each LICENSE-TYPE valid value that applies to the provider.
Corresponding Data Elements – Are data elements that contain values as defined by the qualifier field.
Fully Populated Record Segment – Means that all data elements in the record segment will be populated, not just the qualifier field and its corresponding data elements. These additional data elements are necessary to enable CMS to tie the record segment to its parent segment. These data elements comprise the segment’s natural key. Generally these data elements are the ones bulleted below, but there could potentially be additional ones, depending on the record segment. See the “Record Keys & Constraints” tab in the T-MSIS Data Dictionary if there are questions concerning a record segment’s natural key.
RECORD-ID
SUBMITTING-STATE
RECORD-NUMBER
MSIS-IDENTIFICATION-NUM / STATE-PLAN-ID-NUM / SUBMITTING-STATE-PROV-ID
Record Subject – This is the individual/entity around which the record segments in a file are built. The Medicaid/CHIP enrollee is the subject of Eligible Files. In Provider Files, the subject is the provider. The managed care entity is the subject of Managed Care Files, and third party payers and their associated beneficiaries are the subjects of TPL Files.
Overview
The complex qualifier fields are included in the T-MSIS record layouts so that a given record segment layout can be used to capture a standard set of data elements (i.e., the corresponding data elements) for a category of data (i.e., the complex qualifier field’s valid values list) when more than one category may be applicable to the record subject.
The complex qualifier fields’ valid values lists are not “select one value from the valid values list and provide the corresponding data element values (which is the case for simple qualifier fields).” A separate record segment should be created and fully populated for every “complex qualifier field” valid value or unique combination of “complex qualifier field” valid value and corresponding data element value (in accordance with the Record Keys & Constraints) that applies to the record subject. Table 1 illustrates what CMS is expecting, using LICENSE-TYPE in the PROV-LICENSING-INFO record segment (PRV00004) as an example.
Example Scenario
The purpose of the PROV-LICENSING-INFO segment is to capture licensing and accreditation information relevant to a provider. The valid value list for the LICENSE-TYPE data element shows the types of information that CMS is interested in collecting in this record segment:
State, county, or municipality professional or business license
DEA license
Professional society accreditation
CLIA accreditation
Other
For our example, assume three of these categories are applicable to provider # P0123: (a) a professional license issued by the state’s Board of Physicians (valid value # 1); (b.1) a board certification from the ABMS (valid value # 3); (b.2) a board certification from the AOA (also valid value # 3); and (c) a DEA number (valid value # 2). Table 1 lists the data elements in the PRV00004 record segment, and shows the contents of each data element in the four PRV00004 segments that would be required by this example.
Table 1: Examples of fully populated record segments supplying “complex qualifier field” corresponding data
|
|
Physician
|
ABMS
Board |
AOA
Board |
DEA
|
|
|
|
|
RECORD-ID |
PRV00004 |
PRV00004 |
PRV00004 |
PRV00004 |
|
While these data elements aren't strictly "corresponding data elements," they are necessary to tie the segments to their parent segment. |
|
|
SUBMITTING-STATE |
24 |
24 |
24 |
24 |
|||
|
RECORD-NUMBER |
4506 |
4507 |
4508 |
4509 |
|||
|
SUBMITTING-STATE-PROV-ID |
P0123 |
P0123 |
P0123 |
P0123 |
|||
|
PROV-LOCATION-ID |
0 |
0 |
0 |
0 |
|||
Corresponding Data Element → |
PROV-LICENSE-EFF-DATE |
19921119 |
20100101 |
20120701 |
20131001 |
|
|
|
Corresponding Data Element → |
PROV-LICENSE-END-DATE |
20150930 |
20191231 |
20150630 |
20160930 |
|
|
|
"Complex Qualifier” Data Element → |
LICENSE-TYPE |
1 |
3 |
3 |
2 |
|
|
|
Corresponding Data Element → |
LICENSE-ISSUING-ENTITY-ID |
24 |
American Board of Medical Specialties |
American Osteopathic Association |
DEA |
|
|
|
Corresponding Data Element → |
LICENSE-OR-ACCREDITATION-NUMBER |
D98765 |
IM012345 |
A5546 |
FD1234563 |
|
|
|
|
STATE-NOTATION |
|
|
|
|
|
|
|
|
FILLER |
|
|
|
|
|
|
|
CMS Guidance
CMS is instructing States to provide information corresponding to each of a complex qualifier field’s valid values to the extent that the valid value is applicable to the record subject. Additionally, States should fully populate the affected record segments.
In its first four columns, Table 2 displays the T-MSIS file name, record segment name, complex qualifier field name and the complex qualifier field’s list of valid values for each of the complex qualifier fields in the T-MSIS data set. The last two columns identify the corresponding data elements (along with the file segments where they reside) that need to be populated for every applicable valid value in the “complex qualifier field’s” valid value list.
Table 2: “Complex Qualifier fields” their valid values, and the corresponding data elements that need to be populated
|
File Name |
"Complex Qualifier Field" Information |
Corresponding Data Elements To Be Populated |
||||
Record Segment |
Data Element Name |
Valid Values |
Record Segment |
Data Element Name |
|||
1 |
ELIGIBLE |
ELIGIBILE-CONTACT-INFORMATION (ELG00004) |
ADDR-TYPE |
01 |
Primary home address and contact information (used for the eligibility determination process) |
ELIGIBILE-CONTACT-INFORMATION-ELG00004 |
ELIGIBLE-ADDR-LN1 |
|
|
|
|
02 |
Primary work address and contact information |
|
ELIGIBLE-ADDR-LN2 |
|
|
|
|
03 |
Secondary residence and contact information |
|
ELIGIBLE-ADDR-LN3 |
|
|
|
|
04 |
Secondary work address and contact information |
|
ELIGIBLE-CITY |
|
|
|
|
05 |
Other category of address and contact information |
|
ELIGIBLE-STATE |
|
|
|
|
06 |
Eligible person’s official mailing address |
|
ELIGIBLE-ZIP-CODE |
|
|
|
|
|
|
|
ELIGIBLE-COUNTY-CODE |
|
|
|
|
|
|
|
ELIGIBLE-PHONE-NUM |
|
|
|
|
|
|
|
TYPE-OF-LIVING-ARRANGEMENT ELIGIBLE-ADDR-EFF-DATE ELIGIBLE-ADDR-END-DATE |
2 |
MNGDCARE |
MANAGED-CARE-MAIN (MCR00002) |
MANAGED-CARE-SERVICE-AREA |
1 |
Statewide – The managed care entity provides services to beneficiaries throughout the entire state. |
MANAGED-CARE-SERVICE-AREA-MCR00004 |
MANAGED-CARE-SERVICE-AREA-NAME
|
|
|
|
|
2 |
County – The managed care entity provides services to beneficiaries in specified counties. |
|
MANAGED-CARE-SERVICE-AREA-EFF-DATE |
|
|
|
|
3 |
City – The managed care entity provides services to beneficiaries in specified cities. |
|
MANAGED-CARE-SERVICE-AREA-END-DATE |
|
|
|
|
4 |
Region – The managed care entity provides services to beneficiaries in specified regions, not defined by individual counties within the state (“region” is state-defined). |
|
|
|
|
|
|
5 |
Zip Code – The managed care entity program provides services to beneficiaries in specified zip codes. |
|
|
|
|
|
|
6 |
Other – The managed care entity provides services to beneficiaries in "other" area(s), not Statewide, County, City, or Region. |
|
|
3 |
MNGDCARE |
MANAGED-CARE-LOCATION-AND-CONTACT-INFO (MCR00003) |
MANAGED-CARE-ADDR-TYPE |
1 |
MCO’s corporate address and contact information |
MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 |
MANAGED-CARE-LOCATION-ID |
|
|
|
|
2 |
MCO’s mailing address |
|
MANAGED-CARE-ADDR-LN1 |
|
|
|
|
3 |
MCO’s service location address |
|
MANAGED-CARE-ADDR-LN2 |
|
|
|
|
4 |
MCO’s Billing address and contact information |
|
MANAGED-CARE-ADDR-LN3 |
|
|
|
|
5 |
CEO’s address and contact information |
|
MANAGED-CARE-CITY |
|
|
|
|
6 |
CFO’s address and contact information |
|
MANAGED-CARE-STATE |
|
|
|
|
7 |
Other |
|
MANAGED-CARE-ZIP-CODE |
|
|
|
|
|
|
|
MANAGED-CARE-COUNTY |
|
|
|
|
|
|
|
MANAGED-CARE-TELEPHONE |
|
|
|
|
|
|
|
MANAGED-CARE-EMAIL |
|
|
|
|
|
|
|
MANAGED-CARE-FAX-NUMBER MANAGED-CARE-LOCATION-AND-CONTACT-INFO-EFF-DATE MANAGED-CARE-LOCATION-AND-CONTACT-INFO-END-DATE |
4 |
MNGDCARE |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO (MCR00008) |
NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE |
1 |
Controlling Health Plan (CHP) ID |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 |
STATE-PLAN-ID-NUM |
|
|
|
|
2 |
Subhealth Plan (SHP) ID |
|
NATIONAL-HEALTH-CARE-ENTITY-ID |
|
|
|
|
3 |
Other Entity Identifier (OEID) |
|
NATIONAL-HEALTH-CARE-ENTITY-NAME NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-END-DATE |
5 |
PROVIDER |
PROV-LOCATION-AND-CONTACT-INFO (PRV00003) |
ADDR-TYPE |
1 |
Billing Provider |
PROV-LOCATION-AND-CONTACT-INFO-PRV00003 |
PROV-LOCATION-ID |
|
|
|
|
2 |
Provider Mailing |
|
ADDR-LN1 |
|
|
|
|
3 |
Provider Practice |
|
ADDR-LN2 |
|
|
|
|
4 |
Provider Service Location |
|
ADDR-LN3 |
|
|
|
|
|
|
|
ADDR-CITY |
|
|
|
|
|
|
|
ADDR-STATE |
|
|
|
|
|
|
|
ADDR-ZIP-CODE |
|
|
|
|
|
|
|
ADDR-TELEPHONE |
|
|
|
|
|
|
|
ADDR-EMAIL |
|
|
|
|
|
|
|
ADDR-FAX-NUM |
|
|
|
|
|
|
|
ADDR-BORDER-STATE-IND |
|
|
|
|
|
|
|
ADDR-COUNTY PROV-LOCATION-AND-CONTACT-INFO-EFF-DATE PROV-LOCATION-AND-CONTACT-INFO-END-DATE |
6 |
PROVIDER |
PROV-LICENSING-INFO (PRV00004) |
LICENSE-TYPE |
1 |
State, county, or municipality professional or business license |
PROV-LICENSING-INFO-PRV00004 |
LICENSE-OR-ACCREDITATION-NUMBER |
|
|
|
|
2 |
DEA license |
|
LICENSE-ISSUING-ENTITY-ID |
|
|
|
|
3 |
Professional society accreditation |
|
PROV-LICENSE-EFF-DATE |
|
|
|
|
4 |
CLIA accreditation |
|
PROV-LICENSE-END-DATE |
|
|
|
|
5 |
Other |
|
|
7 |
PROVIDER |
PROV-IDENTIFIERS (PRV00005) |
PROV-IDENTIFIER-TYPE |
1 |
State-specific Medicaid Provider ID |
PROV-IDENTIFIERS-PRV00005 |
PROV-IDENTIFIER |
|
|
|
|
2 |
NPI |
|
PROV-IDENTIFIER-ISSUING-ENTITY-ID |
|
|
|
|
3 |
Medicare ID |
|
PROV-IDENTIFIER-EFF-DATE
|
|
|
|
|
4 |
NCPDP ID |
|
PROV-IDENTIFIER-END-DATE |
|
|
|
|
5 |
Federal Tax ID |
|
|
|
|
|
|
6 |
State Tax ID |
|
|
|
|
|
|
7 |
SSN |
|
|
|
|
|
|
8 |
Other |
|
|
8 |
PROVIDER |
PROV-TAXONOMY-CLASSIFICATION (PRV00006) |
PROV-CLASSIFICATION-TYPE |
1 |
Taxonomy code |
PROV-TAXONOMY-CLASSIFICATION-PRV00006 |
PROV-CLASSIFICATION-CODE |
|
|
|
|
2 |
Provider specialty code |
|
PROV-TAXONOMY-CLASSIFICATION-EFF-DATE
|
|
|
|
|
3 |
Provider type code |
|
PROV-TAXONOMY-CLASSIFICATION-END-DATE |
|
|
|
|
4 |
Authorized category of service code |
|
|
9 |
PROVIDER |
PROV-AFFILIATED-PROGRAMS |
AFFILIATED-PROGRAM-TYPE |
1 |
Health Plan (NHP-ID) |
PROV-AFFILIATED-PROGRAMS-PRV00009 |
AFFILIATED-PROGRAM-ID |
|
|
PRV00009 |
|
2 |
Health Plan (state-assigned health plan ID) |
|
PROV-AFFILIATED-PROGRAM-EFF-DATE |
|
|
|
|
3 |
Waiver |
|
PROV-AFFILIATED-PROGRAM-END-DATE |
|
|
|
|
4 |
Health Home Entity |
|
|
|
|
|
|
5 |
Other |
|
|
10 |
TPL |
TPL-ENTITY-CONTACT-INFORMATION |
TPL-ENTITY-ADDR-TYPE |
06 |
TPL-Entity Corporate Location |
TPL-ENTITY-CONTACT-INFORMATION-TPL00006 |
INSURANCE-CARRIER-ADDR-LN1 |
|
|
(TPL00006) |
|
07 |
TPL-Entity Mailing |
|
INSURANCE-CARRIER-ADDR-LN2 |
|
|
|
|
08 |
TPL-Entity Satellite Location |
|
INSURANCE-CARRIER-ADDR-LN3 |
|
|
|
|
09 |
TPL-Entity Billing |
|
INSURANCE-CARRIER-CITY |
|
|
|
|
10 |
TPL-Entity Correspondence |
|
INSURANCE-CARRIER-STATE |
|
|
|
|
11 |
TPL-Other |
|
INSURANCE-CARRIER-ZIP-CODE |
|
|
|
|
|
|
|
INSURANCE-CARRIER-PHONE-NUM INSURANCE-CARRIER-NAIC-CODE INSURANCE-CARRIER-NAME NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE NATIONAL-HEALTH-CARE-ENTITY-ID NATIONAL-HEALTH-CARE-ENTITY-NAME TPL-ENTITY-CONTACT-INFO-EFF-DATE TPL-ENTITY-CONTACT-INFO-END-DATE |
Appendix P.06: IIFI (Inter/Intra-File Indices)
How to use this guidance document
This guidance document is intended to provide clarification on previous guidance or clarification to requirement areas that states need to assist in the development and implementation of T-MSIS file submissions.
Brief Issue Description
This document provides information about T-MSIS Inter/Intra-File Indices (IIFI) data elements and an additional set of important data elements; both comprise a subset of the overall T-MSIS
data elements.
Background Discussion
The IIFI data elements are made up of three groups.
Ten Logical Record Keys and eleven File Header Keys. Logical Keys are keys that are used in parent child relationship queries and in the creation of the logical records in the Federal T-MSIS data model. File Header Keys are keys that are required on the T-MSIS File header segments.
Source-to-target matrices submitted by states ideally should report each of these corresponding twenty-one data elements with a Data Source Availability of "Always". We expect that 100 percent of the twenty-one group one IIFI data elements are to be reported as “Always” when CMS compares the files submitted to the State’s Source-to-Target Mapping document. CMS envisions that no problem will exist in compliance to the reporting of group one elements.
Twenty Program Specific Segment keys. Program Specific Segment keys comprise of data elements that are keys used in identifying records uniquely in a Program Specific segment in the T-MSIS files. These are also keys are used for updating the records in the data warehouse for those Program specific segments. Program Specific data refer to whether states are participating in any of five Medicaid/CHIP program areas (1115A waiver, Money-Follows-the-Person (MFP), Lock-In-Providers, Health Home SPAs, and Managed Care participation). There are twenty Program Specific segment keys – applicable to specific programs.
Regarding this second group of Program Specific data elements, the presence or absence of these data elements in the State’s T-MSIS submission, of course, depends on whether the State is participating in one or more of the five Medicaid/CHIP program areas (1115A waiver, Money-Follows-the-Person (MFP), Lock-In-Providers, Health Home SPAs, and Managed Care participation). When States participate in one or more of the ‘Medicaid/CHIP Program areas’, the source-to-target matrices ideally should report each of the corresponding Program Specific data elements with a Data Source Availability of "Always" or “Sometimes”.
When States do not participate in a ‘program area’, their source-to-target matrices ideally should report each of the corresponding Program Specific data elements with a Data Source Availability of "Never".
211 Segment keys. These segment keys only differ from the second group in that they are non-program specific, and are relevant to all states, regardless if they are included in the second group. Segment keys comprise of data elements that are keys used in identifying records uniquely in a segment in the T-MSIS files. These are also keys are used for updating the records in the data warehouse for those segments.
States should follow these guidelines when building records.
States must provide primary keys (as listed below) in all segments irrespective of segment being applicable to the state.
Coding segments which are ‘not applicable’ for all records;
Example – if the State does not operate a HEALTH-HOME, the State must populate one record in the HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 segment with key values for SUBMITTING-STATE and MSIS-IDENTIFICATION-NUM and ‘8-fill’ all other elements in the segment. This should be completed for every enrollee in the file.
-
RECORD-ID
1
SUBMITTING-STATE
11
RECORD-NUMBER
1
MSIS-IDENTIFICATION-NUM
456698821
HEALTH-HOME-SPA-NAME
8-fill
HEALTH-HOME-ENTITY-NAME
8-fill
HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE
8-fill
HEALTH-HOME-SPA-PARTICIPATION-END-DATE
8-fill
HEALTH-HOME-ENTITY-EFF-DATE
8-fill
STATE-NOTATION
8-fill
FILLER
Coding segments which are ‘not applicable’ for some records and ‘applicable’ for other records;
Example - when a state operates a HEALTH-HOME for enrollees who are not enrolled in a HEALTH-HOME - code segments which are ‘not applicable’;
If the State has an approved HEALTH-HOME SPA, the State must populate one record in the HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 segment with key values for SUBMITTING-STATE and MSIS-IDENTIFICATION-NUM and ‘8-fill’ all other elements in the segment. This should be completed for every enrollee in the file that is not enrolled in a HEALTH HOME.
-
RECORD-ID
1
SUBMITTING-STATE
11
RECORD-NUMBER
1
MSIS-IDENTIFICATION-NUM
789550702245
HEALTH-HOME-SPA-NAME
8-fill
HEALTH-HOME-ENTITY-NAME
8-fill
HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE
8-fill
HEALTH-HOME-SPA-PARTICIPATION-END-DATE
8-fill
HEALTH-HOME-ENTITY-EFF-DATE
8-fill
STATE-NOTATION
8-fill
FILLER
Example - when a state operates a HEALTH-HOME for enrollees who are enrolled in a HEALTH-HOME - coding segments which are ‘applicable’;
If the State has an approved HEALTH-HOME SPA, the State must populate one record in the HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 segment with key values for SUBMITTING-STATE and MSIS-IDENTIFICATION-NUM, and code all other fields appropriately with data that are applicable for the situation. This should be completed for every enrollee in the file that is enrolled in a HEALTH HOME
-
RECORD-ID
1
SUBMITTING-STATE
11
RECORD-NUMBER
1
MSIS-IDENTIFICATION-NUM
2335-445-07
HEALTH-HOME-SPA-NAME
Happy-Go-Lucky Inc.
HEALTH-HOME-ENTITY-NAME
Health Homes of DC.
HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE
20140101
HEALTH-HOME-SPA-PARTICIPATION-END-DATE
20140131
HEALTH-HOME-ENTITY-EFF-DATE
20130701
STATE-NOTATION
FILLER
Coding segments when segments are ‘applicable’ but data values are ‘unknown’ at certain points in time.
If the State has an approved HEALTH-HOME SPA, the State must populate one record in the HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 segment with key values for SUBMITTING-STATE and MSIS-IDENTIFICATION-NUM and ‘9-fill’ the elements in the segment . This should be completed for every enroll in the file that is enrolled in a HEALTH HOME
-
RECORD-ID
1
SUBMITTING-STATE
11
RECORD-NUMBER
1
MSIS-IDENTIFICATION-NUM
789550702245
HEALTH-HOME-SPA-NAME
Golden Years HH
HEALTH-HOME-ENTITY-NAME
9-fill
HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE
9-fill
HEALTH-HOME-SPA-PARTICIPATION-END-DATE
9-fill
HEALTH-HOME-ENTITY-EFF-DATE
9-fill
STATE-NOTATION
9-fill
FILLER
Data Elements by File Name
Tables 1-8 below contain 448 IIFI data elements with their data element number. These tables represent a duplicated list of the IIFI data element subset found in groups 1-3. Table 9 is the unduplicated listing of 21 IIFI data elements.
Tables 10 –15 contain data elements with their data element number. This represents the 20 Program Specific data elements found in the 2nd group (Program Specific segment keys subset). Table 16 is the unduplicated list of 20 Program Specific data elements.
The unique data element number (DE No), data element name, file name, and file segment are listed in each chart.
Note that data element names in these tables are duplicated on multiple file segments and multiple files.
Table |
File Name |
1 |
Eligible |
2 |
TPL |
3 |
Managed Care |
4 |
Provider |
5 |
Claim OT |
6 |
Claim RX |
7 |
Claim LT |
8 |
Claim IP |
Table 1: Eligible IIFI Data Elements (132 IIFIs)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
ELG001 |
RECORD-ID |
ELIGIBLE |
FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 |
ELG002 |
DATA-DICTIONARY-VERSION |
ELIGIBLE |
FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 |
ELG003 |
SUBMISSION-TRANSACTION-TYPE |
ELIGIBLE |
FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 |
ELG004 |
FILE-ENCODING-SPECIFICATION |
ELIGIBLE |
FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 |
ELG005 |
DATA-MAPPING-DOCUMENT-VERSION |
ELIGIBLE |
FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 |
ELG006 |
FILE-NAME |
ELIGIBLE |
FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 |
ELG007 |
SUBMITTING-STATE |
ELIGIBLE |
FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 |
ELG009 |
START-OF-TIME-PERIOD |
ELIGIBLE |
FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 |
ELG010 |
END-OF-TIME-PERIOD |
ELIGIBLE |
FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 |
ELG011 |
FILE-STATUS-INDICATOR |
ELIGIBLE |
FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 |
ELG012 |
SSN-INDICATOR |
ELIGIBLE |
FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 |
ELG013 |
TOT-REC-CNT |
ELIGIBLE |
FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 |
ELG247 |
SEQUENCE-NUMBER |
ELIGIBLE |
FILE-HEADER-RECORD-ELIGIBILITY-ELG00001 |
ELG016 |
RECORD-ID |
ELIGIBLE |
PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 |
ELG017 |
SUBMITTING-STATE |
ELIGIBLE |
PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 |
ELG018 |
RECORD-NUMBER |
ELIGIBLE |
PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 |
ELG019 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 |
ELG026 |
PRIMARY-DEMOGRAPHIC-ELEMENT-EFF-DATE |
ELIGIBLE |
PRIMARY-DEMOGRAPHICS-ELIGIBILITY-ELG00002 |
ELG030 |
RECORD-ID |
ELIGIBLE |
VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 |
ELG031 |
SUBMITTING-STATE |
ELIGIBLE |
VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 |
ELG032 |
RECORD-NUMBER |
ELIGIBLE |
VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 |
ELG033 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 |
ELG057 |
VARIABLE-DEMOGRAPHIC-ELEMENT-EFF-DATE |
ELIGIBLE |
VARIABLE-DEMOGRAPHICS-ELIGIBILITY-ELG00003 |
ELG061 |
RECORD-ID |
ELIGIBLE |
ELIGIBILE-CONTACT-INFORMATION-ELG00004 |
ELG062 |
SUBMITTING-STATE |
ELIGIBLE |
ELIGIBILE-CONTACT-INFORMATION-ELG00004 |
ELG063 |
RECORD-NUMBER |
ELIGIBLE |
ELIGIBILE-CONTACT-INFORMATION-ELG00004 |
ELG064 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
ELIGIBILE-CONTACT-INFORMATION-ELG00004 |
ELG065 |
ADDR-TYPE |
ELIGIBLE |
ELIGIBILE-CONTACT-INFORMATION-ELG00004 |
ELG075 |
ELIGIBLE-ADDR-EFF-DATE |
ELIGIBLE |
ELIGIBILE-CONTACT-INFORMATION-ELG00004 |
ELG079 |
RECORD-ID |
ELIGIBLE |
ELIGIBILITY-DETERMINANTS-ELG00005 |
ELG080 |
SUBMITTING-STATE |
ELIGIBLE |
ELIGIBILITY-DETERMINANTS-ELG00005 |
ELG081 |
RECORD-NUMBER |
ELIGIBLE |
ELIGIBILITY-DETERMINANTS-ELG00005 |
ELG082 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
ELIGIBILITY-DETERMINANTS-ELG00005 |
ELG083 |
MSIS-CASE-NUM |
ELIGIBLE |
ELIGIBILITY-DETERMINANTS-ELG00005 |
ELG099 |
ELIGIBILITY-DETERMINANT-EFF-DATE |
ELIGIBLE |
ELIGIBILITY-DETERMINANTS-ELG00005 |
ELG103 |
RECORD-ID |
ELIGIBLE |
HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 |
ELG104 |
SUBMITTING-STATE |
ELIGIBLE |
HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 |
ELG105 |
RECORD-NUMBER |
ELIGIBLE |
HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 |
ELG106 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 |
ELG233 |
1115A-DEMONSTRATION-IND |
ELIGIBLE |
1115A-DEMONSTRATION-INFORMATION-ELG00018 |
ELG234 |
1115A-EFF-DATE |
ELIGIBLE |
1115A-DEMONSTRATION-INFORMATION-ELG00018 |
ELG132 |
HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE |
ELIGIBLE |
HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 |
ELG114 |
RECORD-ID |
ELIGIBLE |
HEALTH-HOME-SPA-PROVIDERS-ELG00007 |
ELG115 |
SUBMITTING-STATE |
ELIGIBLE |
HEALTH-HOME-SPA-PROVIDERS-ELG00007 |
ELG116 |
RECORD-NUMBER |
ELIGIBLE |
HEALTH-HOME-SPA-PROVIDERS-ELG00007 |
ELG117 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
HEALTH-HOME-SPA-PROVIDERS-ELG00007 |
ELG131 |
HEALTH-HOME-CHRONIC-CONDITION-OTHER-EXPLANATION |
ELIGIBLE |
HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 |
ELG108 |
HEALTH-HOME-ENTITY-NAME |
ELIGIBLE |
HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 |
ELG119 |
HEALTH-HOME-ENTITY-NAME |
ELIGIBLE |
HEALTH-HOME-SPA-PROVIDERS-ELG00007 |
ELG126 |
RECORD-ID |
ELIGIBLE |
HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 |
ELG127 |
SUBMITTING-STATE |
ELIGIBLE |
HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 |
ELG128 |
RECORD-NUMBER |
ELIGIBLE |
HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 |
ELG129 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 |
ELG120 |
HEALTH-HOME-PROV-NUM |
ELIGIBLE |
HEALTH-HOME-SPA-PROVIDERS-ELG00007 |
ELG107 |
HEALTH-HOME-SPA-NAME |
ELIGIBLE |
HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 |
ELG118 |
HEALTH-HOME-SPA-NAME |
ELIGIBLE |
HEALTH-HOME-SPA-PROVIDERS-ELG00007 |
ELG130 |
HEALTH-HOME-CHRONIC-CONDITION |
ELIGIBLE |
HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 |
ELG136 |
RECORD-ID |
ELIGIBLE |
LOCK-IN-INFORMATION-ELG00009 |
ELG137 |
SUBMITTING-STATE |
ELIGIBLE |
LOCK-IN-INFORMATION-ELG00009 |
ELG138 |
RECORD-NUMBER |
ELIGIBLE |
LOCK-IN-INFORMATION-ELG00009 |
ELG139 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
LOCK-IN-INFORMATION-ELG00009 |
ELG109 |
HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE |
ELIGIBLE |
HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 |
ELG121 |
HEALTH-HOME-SPA-PROVIDER-EFF-DATE |
ELIGIBLE |
HEALTH-HOME-SPA-PROVIDERS-ELG00007 |
ELG142 |
LOCKIN-EFF-DATE |
ELIGIBLE |
LOCK-IN-INFORMATION-ELG00009 |
ELG146 |
RECORD-ID |
ELIGIBLE |
MFP-INFORMATION-ELG00010 |
ELG147 |
SUBMITTING-STATE |
ELIGIBLE |
MFP-INFORMATION-ELG00010 |
ELG148 |
RECORD-NUMBER |
ELIGIBLE |
MFP-INFORMATION-ELG00010 |
ELG149 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
MFP-INFORMATION-ELG00010 |
ELG140 |
LOCKIN-PROV-NUM |
ELIGIBLE |
LOCK-IN-INFORMATION-ELG00009 |
ELG159 |
RECORD-ID |
ELIGIBLE |
STATE-PLAN-OPTION-PARTICIPATION-ELG00011 |
ELG160 |
SUBMITTING-STATE |
ELIGIBLE |
STATE-PLAN-OPTION-PARTICIPATION-ELG00011 |
ELG161 |
RECORD-NUMBER |
ELIGIBLE |
STATE-PLAN-OPTION-PARTICIPATION-ELG00011 |
ELG162 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
STATE-PLAN-OPTION-PARTICIPATION-ELG00011 |
ELG163 |
STATE-PLAN-OPTION-TYPE |
ELIGIBLE |
STATE-PLAN-OPTION-PARTICIPATION-ELG00011 |
ELG164 |
STATE-PLAN-OPTION-EFF-DATE |
ELIGIBLE |
STATE-PLAN-OPTION-PARTICIPATION-ELG00011 |
ELG168 |
RECORD-ID |
ELIGIBLE |
WAIVER-PARTICIPATION-ELG00012 |
ELG169 |
SUBMITTING-STATE |
ELIGIBLE |
WAIVER-PARTICIPATION-ELG00012 |
ELG170 |
RECORD-NUMBER |
ELIGIBLE |
WAIVER-PARTICIPATION-ELG00012 |
ELG171 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
WAIVER-PARTICIPATION-ELG00012 |
ELG172 |
WAIVER-ID |
ELIGIBLE |
WAIVER-PARTICIPATION-ELG00012 |
ELG174 |
WAIVER-ENROLLMENT-EFF-DATE |
ELIGIBLE |
WAIVER-PARTICIPATION-ELG00012 |
ELG178 |
RECORD-ID |
ELIGIBLE |
LTSS-PARTICIPATION-ELG00013 |
ELG179 |
SUBMITTING-STATE |
ELIGIBLE |
LTSS-PARTICIPATION-ELG00013 |
ELG180 |
RECORD-NUMBER |
ELIGIBLE |
LTSS-PARTICIPATION-ELG00013 |
ELG181 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
LTSS-PARTICIPATION-ELG00013 |
ELG182 |
LTSS-LEVEL-CARE |
ELIGIBLE |
LTSS-PARTICIPATION-ELG00013 |
ELG183 |
LTSS-PROV-NUM |
ELIGIBLE |
LTSS-PARTICIPATION-ELG00013 |
ELG184 |
LTSS-ELIGIBILITY-EFF-DATE |
ELIGIBLE |
LTSS-PARTICIPATION-ELG00013 |
ELG188 |
RECORD-ID |
ELIGIBLE |
MANAGED-CARE-PARTICIPATION-ELG00014 |
ELG189 |
SUBMITTING-STATE |
ELIGIBLE |
MANAGED-CARE-PARTICIPATION-ELG00014 |
ELG190 |
RECORD-NUMBER |
ELIGIBLE |
MANAGED-CARE-PARTICIPATION-ELG00014 |
ELG191 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
MANAGED-CARE-PARTICIPATION-ELG00014 |
ELG141 |
LOCKIN-PROV-TYPE |
ELIGIBLE |
LOCK-IN-INFORMATION-ELG00009 |
ELG196 |
MANAGED-CARE-PLAN-ENROLLMENT-EFF-DATE |
ELIGIBLE |
MANAGED-CARE-PARTICIPATION-ELG00014 |
ELG192 |
MANAGED-CARE-PLAN-ID |
ELIGIBLE |
MANAGED-CARE-PARTICIPATION-ELG00014 |
ELG155 |
MFP-ENROLLMENT-EFF-DATE |
ELIGIBLE |
MFP-INFORMATION-ELG00010 |
ELG200 |
RECORD-ID |
ELIGIBLE |
ETHNICITY-INFORMATION-ELG00015 |
ELG201 |
SUBMITTING-STATE |
ELIGIBLE |
ETHNICITY-INFORMATION-ELG00015 |
ELG202 |
RECORD-NUMBER |
ELIGIBLE |
ETHNICITY-INFORMATION-ELG00015 |
ELG203 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
ETHNICITY-INFORMATION-ELG00015 |
ELG204 |
ETHNICITY-CODE |
ELIGIBLE |
ETHNICITY-INFORMATION-ELG00015 |
ELG205 |
ETHNICITY-DECLARATION-EFF-DATE |
ELIGIBLE |
ETHNICITY-INFORMATION-ELG00015 |
ELG209 |
RECORD-ID |
ELIGIBLE |
RACE-INFORMATION-ELG00016 |
ELG210 |
SUBMITTING-STATE |
ELIGIBLE |
RACE-INFORMATION-ELG00016 |
ELG211 |
RECORD-NUMBER |
ELIGIBLE |
RACE-INFORMATION-ELG00016 |
ELG212 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
RACE-INFORMATION-ELG00016 |
ELG213 |
RACE |
ELIGIBLE |
RACE-INFORMATION-ELG00016 |
ELG214 |
RACE-OTHER |
ELIGIBLE |
RACE-INFORMATION-ELG00016 |
ELG216 |
RACE-DECLARATION-EFF-DATE |
ELIGIBLE |
RACE-INFORMATION-ELG00016 |
ELG220 |
RECORD-ID |
ELIGIBLE |
DISABILITY-INFORMATION-ELG00017 |
ELG221 |
SUBMITTING-STATE |
ELIGIBLE |
DISABILITY-INFORMATION-ELG00017 |
ELG222 |
RECORD-NUMBER |
ELIGIBLE |
DISABILITY-INFORMATION-ELG00017 |
ELG223 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
DISABILITY-INFORMATION-ELG00017 |
ELG224 |
DISABILITY-TYPE-CODE |
ELIGIBLE |
DISABILITY-INFORMATION-ELG00017 |
ELG225 |
DISABILITY-TYPE-EFF-DATE |
ELIGIBLE |
DISABILITY-INFORMATION-ELG00017 |
ELG229 |
RECORD-ID |
ELIGIBLE |
1115A-DEMONSTRATION-INFORMATION-ELG00018 |
ELG230 |
SUBMITTING-STATE |
ELIGIBLE |
1115A-DEMONSTRATION-INFORMATION-ELG00018 |
ELG231 |
RECORD-NUMBER |
ELIGIBLE |
1115A-DEMONSTRATION-INFORMATION-ELG00018 |
ELG232 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
1115A-DEMONSTRATION-INFORMATION-ELG00018 |
ELG235 |
1115A-END-DATE |
ELIGIBLE |
1115A-DEMONSTRATION-INFORMATION-ELG00018 |
ELG238 |
RECORD-ID |
ELIGIBLE |
HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 |
ELG239 |
SUBMITTING-STATE |
ELIGIBLE |
HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 |
ELG240 |
RECORD-NUMBER |
ELIGIBLE |
HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 |
ELG241 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 |
ELG242 |
HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-CODE |
ELIGIBLE |
HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 |
ELG243 |
HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-EFF-DATE |
ELIGIBLE |
HCBS-CHRONIC-CONDITIONS-NON-HEALTH-HOME-ELG00020 |
ELG248 |
RECORD-ID |
ELIGIBLE |
ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 |
ELG249 |
SUBMITTING-STATE |
ELIGIBLE |
ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 |
ELG250 |
RECORD-NUMBER |
ELIGIBLE |
ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 |
ELG251 |
MSIS-IDENTIFICATION-NUM |
ELIGIBLE |
ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 |
ELG252 |
ENROLLMENT-TYPE |
ELIGIBLE |
ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 |
ELG253 |
ENROLLMENT-EFF-DATE |
ELIGIBLE |
ENROLLMENT-TIME-SPAN-SEGMENT-ELG00021 |
Table 2: TPL IIFI Data Elements (47 IIFIs)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
TPL001 |
RECORD-ID |
TPL |
FILE-HEADER-RECORD-TPL-TPL00001 |
TPL002 |
DATA-DICTIONARY-VERSION |
TPL |
FILE-HEADER-RECORD-TPL-TPL00001 |
TPL003 |
SUBMISSION-TRANSACTION-TYPE |
TPL |
FILE-HEADER-RECORD-TPL-TPL00001 |
TPL004 |
FILE-ENCODING-SPECIFICATION |
TPL |
FILE-HEADER-RECORD-TPL-TPL00001 |
TPL005 |
DATA-MAPPING-DOCUMENT-VERSION |
TPL |
FILE-HEADER-RECORD-TPL-TPL00001 |
TPL006 |
FILE-NAME |
TPL |
FILE-HEADER-RECORD-TPL-TPL00001 |
TPL007 |
SUBMITTING-STATE |
TPL |
FILE-HEADER-RECORD-TPL-TPL00001 |
TPL009 |
START-OF-TIME-PERIOD |
TPL |
FILE-HEADER-RECORD-TPL-TPL00001 |
TPL010 |
END-OF-TIME-PERIOD |
TPL |
FILE-HEADER-RECORD-TPL-TPL00001 |
TPL011 |
FILE-STATUS-INDICATOR |
TPL |
FILE-HEADER-RECORD-TPL-TPL00001 |
TPL012 |
SSN-INDICATOR |
TPL |
FILE-HEADER-RECORD-TPL-TPL00001 |
TPL013 |
TOT-REC-CNT |
TPL |
FILE-HEADER-RECORD-TPL-TPL00001 |
TPL088 |
SEQUENCE-NUMBER |
TPL |
FILE-HEADER-RECORD-TPL-TPL00001 |
TPL016 |
RECORD-ID |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 |
TPL017 |
SUBMITTING-STATE |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 |
TPL018 |
RECORD-NUMBER |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 |
TPL019 |
MSIS-IDENTIFICATION-NUM |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 |
TPL025 |
ELIG-PRSN-MAIN-EFF-DATE |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-MAIN-TPL00002 |
TPL029 |
RECORD-ID |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 |
TPL030 |
SUBMITTING-STATE |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 |
TPL031 |
RECORD-NUMBER |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 |
TPL032 |
MSIS-IDENTIFICATION-NUM |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 |
TPL033 |
INSURANCE-CARRIER-ID-NUM |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 |
TPL034 |
INSURANCE-PLAN-ID |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 |
TPL035 |
GROUP-NUM |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 |
TPL036 |
MEMBER-ID |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 |
TPL089 |
COVERAGE-TYPE |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 |
TPL048 |
INSURANCE-COVERAGE-EFF-DATE |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-INFO-TPL00003 |
TPL052 |
RECORD-ID |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 |
TPL053 |
SUBMITTING-STATE |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 |
TPL054 |
RECORD-NUMBER |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 |
TPL055 |
INSURANCE-CARRIER-ID-NUM |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 |
TPL056 |
INSURANCE-PLAN-ID |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 |
TPL058 |
COVERAGE-TYPE |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 |
TPL059 |
INSURANCE-CATEGORIES-EFF-DATE |
TPL |
TPL-MEDICAID-ELIGIBLE-PERSON-HEALTH-INSURANCE-COVERAGE-CATEGORIES-TPL00004 |
TPL063 |
RECORD-ID |
TPL |
TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 |
TPL064 |
SUBMITTING-STATE |
TPL |
TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 |
TPL065 |
RECORD-NUMBER |
TPL |
TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 |
TPL066 |
MSIS-IDENTIFICATION-NUM |
TPL |
TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 |
TPL067 |
TYPE-OF-OTHER-THIRD-PARTY-LIABILITY |
TPL |
TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 |
TPL068 |
OTHER-TPL-EFF-DATE |
TPL |
TPL-MEDICAID-ELIGIBLE-OTHER-THIRD-PARTY-COVERAGE-INFORMATION-TPL00005 |
TPL072 |
RECORD-ID |
TPL |
TPL-ENTITY-CONTACT-INFORMATION-TPL00006 |
TPL073 |
SUBMITTING-STATE |
TPL |
TPL-ENTITY-CONTACT-INFORMATION-TPL00006 |
TPL074 |
RECORD-NUMBER |
TPL |
TPL-ENTITY-CONTACT-INFORMATION-TPL00006 |
TPL075 |
INSURANCE-CARRIER-ID-NUM |
TPL |
TPL-ENTITY-CONTACT-INFORMATION-TPL00006 |
TPL076 |
TPL-ENTITY-ADDR-TYPE |
TPL |
TPL-ENTITY-CONTACT-INFORMATION-TPL00006 |
TPL084 |
TPL-ENTITY-CONTACT-INFO-EFF-DATE |
TPL |
TPL-ENTITY-CONTACT-INFORMATION-TPL00006 |
Table 3: Managed Care IIFI Data Elements (62 IIFI)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
MCR001 |
RECORD-ID |
MNGDCARE |
FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 |
MCR002 |
DATA-DICTIONARY-VERSION |
MNGDCARE |
FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 |
MCR003 |
SUBMISSION-TRANSACTION-TYPE |
MNGDCARE |
FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 |
MCR004 |
FILE-ENCODING-SPECIFICATION |
MNGDCARE |
FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 |
MCR005 |
DATA-MAPPING-DOCUMENT-VERSION |
MNGDCARE |
FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 |
MCR006 |
FILE-NAME |
MNGDCARE |
FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 |
MCR007 |
SUBMITTING-STATE |
MNGDCARE |
FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 |
MCR009 |
START-OF-TIME-PERIOD |
MNGDCARE |
FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 |
MCR010 |
END-OF-TIME-PERIOD |
MNGDCARE |
FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 |
MCR011 |
FILE-STATUS-INDICATOR |
MNGDCARE |
FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 |
MCR013 |
TOT-REC-CNT |
MNGDCARE |
FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 |
MCR112 |
SEQUENCE-NUMBER |
MNGDCARE |
FILE-HEADER-RECORD-MANAGED-CARE-MCR00001 |
MCR016 |
RECORD-ID |
MNGDCARE |
MANAGED-CARE-MAIN-MCR00002 |
MCR017 |
SUBMITTING-STATE |
MNGDCARE |
MANAGED-CARE-MAIN-MCR00002 |
MCR018 |
RECORD-NUMBER |
MNGDCARE |
MANAGED-CARE-MAIN-MCR00002 |
MCR019 |
STATE-PLAN-ID-NUM |
MNGDCARE |
MANAGED-CARE-MAIN-MCR00002 |
MCR030 |
MANAGED-CARE-MAIN-REC-EFF-DATE |
MNGDCARE |
MANAGED-CARE-MAIN-MCR00002 |
MCR034 |
RECORD-ID |
MNGDCARE |
MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 |
MCR035 |
SUBMITTING-STATE |
MNGDCARE |
MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 |
MCR036 |
RECORD-NUMBER |
MNGDCARE |
MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 |
MCR037 |
STATE-PLAN-ID-NUM |
MNGDCARE |
MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 |
MCR038 |
MANAGED-CARE-LOCATION-ID |
MNGDCARE |
MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 |
MCR039 |
MANAGED-CARE-LOCATION-AND-CONTACT-INFO-EFF-DATE |
MNGDCARE |
MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 |
MCR041 |
MANAGED-CARE-ADDR-TYPE |
MNGDCARE |
MANAGED-CARE-LOCATION-AND-CONTACT-INFO-MCR00003 |
MCR054 |
RECORD-ID |
MNGDCARE |
MANAGED-CARE-SERVICE-AREA-MCR00004 |
MCR055 |
SUBMITTING-STATE |
MNGDCARE |
MANAGED-CARE-SERVICE-AREA-MCR00004 |
MCR056 |
RECORD-NUMBER |
MNGDCARE |
MANAGED-CARE-SERVICE-AREA-MCR00004 |
MCR057 |
STATE-PLAN-ID-NUM |
MNGDCARE |
MANAGED-CARE-SERVICE-AREA-MCR00004 |
MCR058 |
MANAGED-CARE-SERVICE-AREA-NAME |
MNGDCARE |
MANAGED-CARE-SERVICE-AREA-MCR00004 |
MCR059 |
MANAGED-CARE-SERVICE-AREA-EFF-DATE |
MNGDCARE |
MANAGED-CARE-SERVICE-AREA-MCR00004 |
MCR063 |
RECORD-ID |
MNGDCARE |
MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 |
MCR064 |
SUBMITTING-STATE |
MNGDCARE |
MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 |
MCR065 |
RECORD-NUMBER |
MNGDCARE |
MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 |
MCR066 |
STATE-PLAN-ID-NUM |
MNGDCARE |
MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 |
MCR067 |
OPERATING-AUTHORITY |
MNGDCARE |
MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 |
MCR069 |
MANAGED-CARE-OP-AUTHORITY-EFF-DATE |
MNGDCARE |
MANAGED-CARE-OPERATING-AUTHORITY-MCR00005 |
MCR073 |
RECORD-ID |
MNGDCARE |
MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 |
MCR074 |
SUBMITTING-STATE |
MNGDCARE |
MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 |
MCR075 |
RECORD-NUMBER |
MNGDCARE |
MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 |
MCR076 |
STATE-PLAN-ID-NUM |
MNGDCARE |
MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 |
MCR077 |
MANAGED-CARE-PLAN-POP |
MNGDCARE |
MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 |
MCR078 |
MANAGED-CARE-PLAN-POP-EFF-DATE |
MNGDCARE |
MANAGED-CARE-PLAN-POPULATION-ENROLLED-MCR00006 |
MCR082 |
RECORD-ID |
MNGDCARE |
MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 |
MCR083 |
SUBMITTING-STATE |
MNGDCARE |
MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 |
MCR084 |
RECORD-NUMBER |
MNGDCARE |
MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 |
MCR085 |
STATE-PLAN-ID-NUM |
MNGDCARE |
MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 |
MCR086 |
ACCREDITATION-ORGANIZATION |
MNGDCARE |
MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 |
MCR087 |
DATE-ACCREDITATION-ACHIEVED |
MNGDCARE |
MANAGED- CARE-ACCREDITATION-ORGANIZATION-MCR00007 |
MCR091 |
RECORD-ID |
MNGDCARE |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 |
MCR092 |
SUBMITTING-STATE |
MNGDCARE |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 |
MCR093 |
RECORD-NUMBER |
MNGDCARE |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 |
MCR094 |
STATE-PLAN-ID-NUM |
MNGDCARE |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 |
MCR095 |
NATIONAL-HEALTH-CARE-ENTITY-ID |
MNGDCARE |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 |
MCR096 |
NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE |
MNGDCARE |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 |
MCR098 |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE |
MNGDCARE |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 |
MCR102 |
RECORD-ID |
MNGDCARE |
CHPID-SHPID-RELATIONSHIPS-MCR00009 |
MCR103 |
SUBMITTING-STATE |
MNGDCARE |
CHPID-SHPID-RELATIONSHIPS-MCR00009 |
MCR104 |
RECORD-NUMBER |
MNGDCARE |
CHPID-SHPID-RELATIONSHIPS-MCR00009 |
MCR105 |
STATE-PLAN-ID-NUM |
MNGDCARE |
CHPID-SHPID-RELATIONSHIPS-MCR00009 |
MCR106 |
CHPID |
MNGDCARE |
CHPID-SHPID-RELATIONSHIPS-MCR00009 |
MCR107 |
SHPID |
MNGDCARE |
CHPID-SHPID-RELATIONSHIPS-MCR00009 |
MCR108 |
CHPID-SHPID-RELATIONSHIP-EFF-DATE |
MNGDCARE |
CHPID-SHPID-RELATIONSHIPS-MCR00009 |
Table 4: Provider IIFI Data Elements (74 IIFIs)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
PRV001 |
RECORD-ID |
PROVIDER |
FILE-HEADER-RECORD-PROVIDER-PRV00001 |
PRV002 |
DATA-DICTIONARY-VERSION |
PROVIDER |
FILE-HEADER-RECORD-PROVIDER-PRV00001 |
PRV003 |
SUBMISSION-TRANSACTION-TYPE |
PROVIDER |
FILE-HEADER-RECORD-PROVIDER-PRV00001 |
PRV004 |
FILE-ENCODING-SPECIFICATION |
PROVIDER |
FILE-HEADER-RECORD-PROVIDER-PRV00001 |
PRV005 |
DATA-MAPPING-DOCUMENT-VERSION |
PROVIDER |
FILE-HEADER-RECORD-PROVIDER-PRV00001 |
PRV006 |
FILE-NAME |
PROVIDER |
FILE-HEADER-RECORD-PROVIDER-PRV00001 |
PRV007 |
SUBMITTING-STATE |
PROVIDER |
FILE-HEADER-RECORD-PROVIDER-PRV00001 |
PRV009 |
START-OF-TIME-PERIOD |
PROVIDER |
FILE-HEADER-RECORD-PROVIDER-PRV00001 |
PRV010 |
END-OF-TIME-PERIOD |
PROVIDER |
FILE-HEADER-RECORD-PROVIDER-PRV00001 |
PRV011 |
FILE-STATUS-INDICATOR |
PROVIDER |
FILE-HEADER-RECORD-PROVIDER-PRV00001 |
PRV013 |
TOT-REC-CNT |
PROVIDER |
FILE-HEADER-RECORD-PROVIDER-PRV00001 |
PRV138 |
SEQUENCE-NUMBER |
PROVIDER |
FILE-HEADER-RECORD-PROVIDER-PRV00001 |
PRV016 |
RECORD-ID |
PROVIDER |
PROV-ATTRIBUTES-MAIN-PRV00002 |
PRV017 |
SUBMITTING-STATE |
PROVIDER |
PROV-ATTRIBUTES-MAIN-PRV00002 |
PRV018 |
RECORD-NUMBER |
PROVIDER |
PROV-ATTRIBUTES-MAIN-PRV00002 |
PRV019 |
SUBMITTING-STATE-PROV-ID |
PROVIDER |
PROV-ATTRIBUTES-MAIN-PRV00002 |
PRV020 |
PROV-ATTRIBUTES-EFF-DATE |
PROVIDER |
PROV-ATTRIBUTES-MAIN-PRV00002 |
PRV039 |
RECORD-ID |
PROVIDER |
PROV-LOCATION-AND-CONTACT-INFO-PRV00003 |
PRV040 |
SUBMITTING-STATE |
PROVIDER |
PROV-LOCATION-AND-CONTACT-INFO-PRV00003 |
PRV041 |
RECORD-NUMBER |
PROVIDER |
PROV-LOCATION-AND-CONTACT-INFO-PRV00003 |
PRV042 |
SUBMITTING-STATE-PROV-ID |
PROVIDER |
PROV-LOCATION-AND-CONTACT-INFO-PRV00003 |
PRV043 |
PROV-LOCATION-ID |
PROVIDER |
PROV-LOCATION-AND-CONTACT-INFO-PRV00003 |
PRV044 |
PROV-LOCATION-AND-CONTACT-INFO-EFF-DATE |
PROVIDER |
PROV-LOCATION-AND-CONTACT-INFO-PRV00003 |
PRV046 |
ADDR-TYPE |
PROVIDER |
PROV-LOCATION-AND-CONTACT-INFO-PRV00003 |
PRV060 |
RECORD-ID |
PROVIDER |
PROV-LICENSING-INFO-PRV00004 |
PRV061 |
SUBMITTING-STATE |
PROVIDER |
PROV-LICENSING-INFO-PRV00004 |
PRV062 |
RECORD-NUMBER |
PROVIDER |
PROV-LICENSING-INFO-PRV00004 |
PRV063 |
SUBMITTING-STATE-PROV-ID |
PROVIDER |
PROV-LICENSING-INFO-PRV00004 |
PRV064 |
PROV-LOCATION-ID |
PROVIDER |
PROV-LICENSING-INFO-PRV00004 |
PRV065 |
PROV-LICENSE-EFF-DATE |
PROVIDER |
PROV-LICENSING-INFO-PRV00004 |
PRV067 |
LICENSE-TYPE |
PROVIDER |
PROV-LICENSING-INFO-PRV00004 |
PRV068 |
LICENSE-ISSUING-ENTITY-ID |
PROVIDER |
PROV-LICENSING-INFO-PRV00004 |
PRV072 |
RECORD-ID |
PROVIDER |
PROV-IDENTIFIERS-PRV00005 |
PRV073 |
SUBMITTING-STATE |
PROVIDER |
PROV-IDENTIFIERS-PRV00005 |
PRV074 |
RECORD-NUMBER |
PROVIDER |
PROV-IDENTIFIERS-PRV00005 |
PRV075 |
SUBMITTING-STATE-PROV-ID |
PROVIDER |
PROV-IDENTIFIERS-PRV00005 |
PRV076 |
PROV-LOCATION-ID |
PROVIDER |
PROV-IDENTIFIERS-PRV00005 |
PRV077 |
PROV-IDENTIFIER-TYPE |
PROVIDER |
PROV-IDENTIFIERS-PRV00005 |
PRV078 |
PROV-IDENTIFIER-ISSUING-ENTITY-ID |
PROVIDER |
PROV-IDENTIFIERS-PRV00005 |
PRV079 |
PROV-IDENTIFIER-EFF-DATE |
PROVIDER |
PROV-IDENTIFIERS-PRV00005 |
PRV081 |
PROV-IDENTIFIER |
PROVIDER |
PROV-IDENTIFIERS-PRV00005 |
PRV084 |
RECORD-ID |
PROVIDER |
PROV-TAXONOMY-CLASSIFICATION-PRV00006 |
PRV085 |
SUBMITTING-STATE |
PROVIDER |
PROV-TAXONOMY-CLASSIFICATION-PRV00006 |
PRV086 |
RECORD-NUMBER |
PROVIDER |
PROV-TAXONOMY-CLASSIFICATION-PRV00006 |
PRV087 |
SUBMITTING-STATE-PROV-ID |
PROVIDER |
PROV-TAXONOMY-CLASSIFICATION-PRV00006 |
PRV088 |
PROV-CLASSIFICATION-TYPE |
PROVIDER |
PROV-TAXONOMY-CLASSIFICATION-PRV00006 |
PRV089 |
PROV-CLASSIFICATION-CODE |
PROVIDER |
PROV-TAXONOMY-CLASSIFICATION-PRV00006 |
PRV090 |
PROV-TAXONOMY-CLASSIFICATION-EFF-DATE |
PROVIDER |
PROV-TAXONOMY-CLASSIFICATION-PRV00006 |
PRV094 |
RECORD-ID |
PROVIDER |
PROV-MEDICAID-ENROLLMENT-PRV00007 |
PRV095 |
SUBMITTING-STATE |
PROVIDER |
PROV-MEDICAID-ENROLLMENT-PRV00007 |
PRV096 |
RECORD-NUMBER |
PROVIDER |
PROV-MEDICAID-ENROLLMENT-PRV00007 |
PRV097 |
SUBMITTING-STATE-PROV-ID |
PROVIDER |
PROV-MEDICAID-ENROLLMENT-PRV00007 |
PRV098 |
PROV-MEDICAID-EFF-DATE |
PROVIDER |
PROV-MEDICAID-ENROLLMENT-PRV00007 |
PRV100 |
PROV-MEDICAID-ENROLLMENT-STATUS-CODE |
PROVIDER |
PROV-MEDICAID-ENROLLMENT-PRV00007 |
PRV106 |
RECORD-ID |
PROVIDER |
PROV-AFFILIATED-GROUPS-PRV00008 |
PRV107 |
SUBMITTING-STATE |
PROVIDER |
PROV-AFFILIATED-GROUPS-PRV00008 |
PRV108 |
RECORD-NUMBER |
PROVIDER |
PROV-AFFILIATED-GROUPS-PRV00008 |
PRV109 |
SUBMITTING-STATE-PROV-ID |
PROVIDER |
PROV-AFFILIATED-GROUPS-PRV00008 |
PRV110 |
SUBMITTING-STATE-PROV-ID-OF-AFFILIATED-ENTITY |
PROVIDER |
PROV-AFFILIATED-GROUPS-PRV00008 |
PRV111 |
PROV-AFFILIATED-GROUP-EFF-DATE |
PROVIDER |
PROV-AFFILIATED-GROUPS-PRV00008 |
PRV115 |
RECORD-ID |
PROVIDER |
PROV-AFFILIATED-PROGRAMS-PRV00009 |
PRV116 |
SUBMITTING-STATE |
PROVIDER |
PROV-AFFILIATED-PROGRAMS-PRV00009 |
PRV117 |
RECORD-NUMBER |
PROVIDER |
PROV-AFFILIATED-PROGRAMS-PRV00009 |
PRV118 |
SUBMITTING-STATE-PROV-ID |
PROVIDER |
PROV-AFFILIATED-PROGRAMS-PRV00009 |
PRV119 |
AFFILIATED-PROGRAM-TYPE |
PROVIDER |
PROV-AFFILIATED-PROGRAMS-PRV00009 |
PRV120 |
AFFILIATED-PROGRAM-ID |
PROVIDER |
PROV-AFFILIATED-PROGRAMS-PRV00009 |
PRV121 |
PROV-AFFILIATED-PROGRAM-EFF-DATE |
PROVIDER |
PROV-AFFILIATED-PROGRAMS-PRV00009 |
PRV125 |
RECORD-ID |
PROVIDER |
PROV-BED-TYPE-INFO-PRV00010 |
PRV126 |
SUBMITTING-STATE |
PROVIDER |
PROV-BED-TYPE-INFO-PRV00010 |
PRV127 |
RECORD-NUMBER |
PROVIDER |
PROV-BED-TYPE-INFO-PRV00010 |
PRV128 |
SUBMITTING-STATE-PROV-ID |
PROVIDER |
PROV-BED-TYPE-INFO-PRV00010 |
PRV129 |
PROV-LOCATION-ID |
PROVIDER |
PROV-BED-TYPE-INFO-PRV00010 |
PRV130 |
BED-TYPE-EFF-DATE |
PROVIDER |
PROV-BED-TYPE-INFO-PRV00010 |
PRV134 |
BED-TYPE-CODE |
PROVIDER |
PROV-BED-TYPE-INFO-PRV00010 |
Table 5: Claim OT IIFI Data Elements (34 IIFIs)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
COT001 |
RECORD-ID |
CLAIMOT |
FILE-HEADER-RECORD-OT-COT00001 |
COT002 |
DATA-DICTIONARY-VERSION |
CLAIMOT |
FILE-HEADER-RECORD-OT-COT00001 |
COT003 |
SUBMISSION-TRANSACTION-TYPE |
CLAIMOT |
FILE-HEADER-RECORD-OT-COT00001 |
COT004 |
FILE-ENCODING-SPECIFICATION |
CLAIMOT |
FILE-HEADER-RECORD-OT-COT00001 |
COT005 |
DATA-MAPPING-DOCUMENT-VERSION |
CLAIMOT |
FILE-HEADER-RECORD-OT-COT00001 |
COT006 |
FILE-NAME |
CLAIMOT |
FILE-HEADER-RECORD-OT-COT00001 |
COT007 |
SUBMITTING-STATE |
CLAIMOT |
FILE-HEADER-RECORD-OT-COT00001 |
COT009 |
START-OF-TIME-PERIOD |
CLAIMOT |
FILE-HEADER-RECORD-OT-COT00001 |
COT010 |
END-OF-TIME-PERIOD |
CLAIMOT |
FILE-HEADER-RECORD-OT-COT00001 |
COT011 |
FILE-STATUS-INDICATOR |
CLAIMOT |
FILE-HEADER-RECORD-OT-COT00001 |
COT012 |
SSN-INDICATOR |
CLAIMOT |
FILE-HEADER-RECORD-OT-COT00001 |
COT013 |
TOT-REC-CNT |
CLAIMOT |
FILE-HEADER-RECORD-OT-COT00001 |
COT216 |
SEQUENCE-NUMBER |
CLAIMOT |
FILE-HEADER-RECORD-OT-COT00001 |
COT016 |
RECORD-ID |
CLAIMOT |
CLAIM-HEADER-RECORD-OT-COT00002 |
COT017 |
SUBMITTING-STATE |
CLAIMOT |
CLAIM-HEADER-RECORD-OT-COT00002 |
COT018 |
RECORD-NUMBER |
CLAIMOT |
CLAIM-HEADER-RECORD-OT-COT00002 |
COT019 |
ICN-ORIG |
CLAIMOT |
CLAIM-HEADER-RECORD-OT-COT00002 |
COT020 |
ICN-ADJ |
CLAIMOT |
CLAIM-HEADER-RECORD-OT-COT00002 |
COT025 |
ADJUSTMENT-IND |
CLAIMOT |
CLAIM-HEADER-RECORD-OT-COT00002 |
COT033 |
BEGINNING-DATE-OF-SERVICE |
CLAIMOT |
CLAIM-HEADER-RECORD-OT-COT00002 |
COT035 |
ADJUDICATION-DATE |
CLAIMOT |
CLAIM-HEADER-RECORD-OT-COT00002 |
COT040 |
CLAIM-STATUS-CATEGORY |
CLAIMOT |
CLAIM-HEADER-RECORD-OT-COT00002 |
COT112 |
BILLING-PROV-NUM |
CLAIMOT |
CLAIM-HEADER-RECORD-OT-COT00002 |
COT117 |
REFERRING-PROV-NUM |
CLAIMOT |
CLAIM-HEADER-RECORD-OT-COT00002 |
COT154 |
RECORD-ID |
CLAIMOT |
CLAIM-LINE-RECORD-OT-COT00003 |
COT155 |
SUBMITTING-STATE |
CLAIMOT |
CLAIM-LINE-RECORD-OT-COT00003 |
COT156 |
RECORD-NUMBER |
CLAIMOT |
CLAIM-LINE-RECORD-OT-COT00003 |
COT158 |
ICN-ORIG |
CLAIMOT |
CLAIM-LINE-RECORD-OT-COT00003 |
COT159 |
ICN-ADJ |
CLAIMOT |
CLAIM-LINE-RECORD-OT-COT00003 |
COT160 |
LINE-NUM-ORIG |
CLAIMOT |
CLAIM-LINE-RECORD-OT-COT00003 |
COT161 |
LINE-NUM-ADJ |
CLAIMOT |
CLAIM-LINE-RECORD-OT-COT00003 |
COT166 |
BEGINNING-DATE-OF-SERVICE |
CLAIMOT |
CLAIM-LINE-RECORD-OT-COT00003 |
COT189 |
SERVICING-PROV-NUM |
CLAIMOT |
CLAIM-LINE-RECORD-OT-COT00003 |
COT221 |
ADJUDICATION-DATE |
CLAIMOT |
CLAIM-LINE-RECORD-OT-COT00003 |
Table 6: Claim RX IIFI Data Elements (32 IIFIs)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
CRX001 |
RECORD-ID |
CLAIMRX |
FILE-HEADER-RECORD-RX-CRX00001 |
CRX002 |
DATA-DICTIONARY-VERSION |
CLAIMRX |
FILE-HEADER-RECORD-RX-CRX00001 |
CRX003 |
SUBMISSION-TRANSACTION-TYPE |
CLAIMRX |
FILE-HEADER-RECORD-RX-CRX00001 |
CRX004 |
FILE-ENCODING-SPECIFICATION |
CLAIMRX |
FILE-HEADER-RECORD-RX-CRX00001 |
CRX005 |
DATA-MAPPING-DOCUMENT-VERSION |
CLAIMRX |
FILE-HEADER-RECORD-RX-CRX00001 |
CRX006 |
FILE-NAME |
CLAIMRX |
FILE-HEADER-RECORD-RX-CRX00001 |
CRX007 |
SUBMITTING-STATE |
CLAIMRX |
FILE-HEADER-RECORD-RX-CRX00001 |
CRX009 |
START-OF-TIME-PERIOD |
CLAIMRX |
FILE-HEADER-RECORD-RX-CRX00001 |
CRX010 |
END-OF-TIME-PERIOD |
CLAIMRX |
FILE-HEADER-RECORD-RX-CRX00001 |
CRX011 |
FILE-STATUS-INDICATOR |
CLAIMRX |
FILE-HEADER-RECORD-RX-CRX00001 |
CRX012 |
SSN-INDICATOR |
CLAIMRX |
FILE-HEADER-RECORD-RX-CRX00001 |
CRX013 |
TOT-REC-CNT |
CLAIMRX |
FILE-HEADER-RECORD-RX-CRX00001 |
CRX155 |
SEQUENCE-NUMBER |
CLAIMRX |
FILE-HEADER-RECORD-RX-CRX00001 |
CRX016 |
RECORD-ID |
CLAIMRX |
CLAIM-HEADER-RECORD-RX-CRX00002 |
CRX017 |
SUBMITTING-STATE |
CLAIMRX |
CLAIM-HEADER-RECORD-RX-CRX00002 |
CRX018 |
RECORD-NUMBER |
CLAIMRX |
CLAIM-HEADER-RECORD-RX-CRX00002 |
CRX019 |
ICN-ORIG |
CLAIMRX |
CLAIM-HEADER-RECORD-RX-CRX00002 |
CRX020 |
ICN-ADJ |
CLAIMRX |
CLAIM-HEADER-RECORD-RX-CRX00002 |
CRX025 |
ADJUSTMENT-IND |
CLAIMRX |
CLAIM-HEADER-RECORD-RX-CRX00002 |
CRX027 |
ADJUDICATION-DATE |
CLAIMRX |
CLAIM-HEADER-RECORD-RX-CRX00002 |
CRX031 |
CLAIM-STATUS-CATEGORY |
CLAIMRX |
CLAIM-HEADER-RECORD-RX-CRX00002 |
CRX070 |
BILLING-PROV-NUM |
CLAIMRX |
CLAIM-HEADER-RECORD-RX-CRX00002 |
CRX074 |
PRESCRIBING-PROV-NUM |
CLAIMRX |
CLAIM-HEADER-RECORD-RX-CRX00002 |
CRX156 |
DISPENSING-PRESCRIPTION-DRUG-PROV-NUM |
CLAIMRX |
CLAIM-HEADER-RECORD-RX-CRX00002 |
CRX108 |
RECORD-ID |
CLAIMRX |
CLAIM-LINE-RECORD-RX-CRX00003 |
CRX109 |
SUBMITTING-STATE |
CLAIMRX |
CLAIM-LINE-RECORD-RX-CRX00003 |
CRX110 |
RECORD-NUMBER |
CLAIMRX |
CLAIM-LINE-RECORD-RX-CRX00003 |
CRX112 |
ICN-ORIG |
CLAIMRX |
CLAIM-LINE-RECORD-RX-CRX00003 |
CRX113 |
ICN-ADJ |
CLAIMRX |
CLAIM-LINE-RECORD-RX-CRX00003 |
CRX114 |
LINE-NUM-ORIG |
CLAIMRX |
CLAIM-LINE-RECORD-RX-CRX00003 |
CRX115 |
LINE-NUM-ADJ |
CLAIMRX |
CLAIM-LINE-RECORD-RX-CRX00003 |
CRX157 |
ADJUDICATION-DATE |
CLAIMRX |
CLAIM-LINE-RECORD-RX-CRX00003 |
Table 7: Claim LT IIFI Data Elements (34 IIFIs)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
CLT001 |
RECORD-ID |
CLAIMLT |
FILE-HEADER-RECORD-LT-CLT00001 |
CLT002 |
DATA-DICTIONARY-VERSION |
CLAIMLT |
FILE-HEADER-RECORD-LT-CLT00001 |
CLT003 |
SUBMISSION-TRANSACTION-TYPE |
CLAIMLT |
FILE-HEADER-RECORD-LT-CLT00001 |
CLT004 |
FILE-ENCODING-SPECIFICATION |
CLAIMLT |
FILE-HEADER-RECORD-LT-CLT00001 |
CLT005 |
DATA-MAPPING-DOCUMENT-VERSION |
CLAIMLT |
FILE-HEADER-RECORD-LT-CLT00001 |
CLT006 |
FILE-NAME |
CLAIMLT |
FILE-HEADER-RECORD-LT-CLT00001 |
CLT007 |
SUBMITTING-STATE |
CLAIMLT |
FILE-HEADER-RECORD-LT-CLT00001 |
CLT009 |
START-OF-TIME-PERIOD |
CLAIMLT |
FILE-HEADER-RECORD-LT-CLT00001 |
CLT010 |
END-OF-TIME-PERIOD |
CLAIMLT |
FILE-HEADER-RECORD-LT-CLT00001 |
CLT011 |
FILE-STATUS-INDICATOR |
CLAIMLT |
FILE-HEADER-RECORD-LT-CLT00001 |
CLT012 |
SSN-INDICATOR |
CLAIMLT |
FILE-HEADER-RECORD-LT-CLT00001 |
CLT013 |
TOT-REC-CNT |
CLAIMLT |
FILE-HEADER-RECORD-LT-CLT00001 |
CLT227 |
SEQUENCE-NUMBER |
CLAIMLT |
FILE-HEADER-RECORD-LT-CLT00001 |
CLT016 |
RECORD-ID |
CLAIMLT |
CLAIM-HEADER-RECORD-LT-CLT00002 |
CLT017 |
SUBMITTING-STATE |
CLAIMLT |
CLAIM-HEADER-RECORD-LT-CLT00002 |
CLT018 |
RECORD-NUMBER |
CLAIMLT |
CLAIM-HEADER-RECORD-LT-CLT00002 |
CLT019 |
ICN-ORIG |
CLAIMLT |
CLAIM-HEADER-RECORD-LT-CLT00002 |
CLT020 |
ICN-ADJ |
CLAIMLT |
CLAIM-HEADER-RECORD-LT-CLT00002 |
CLT025 |
ADJUSTMENT-IND |
CLAIMLT |
CLAIM-HEADER-RECORD-LT-CLT00002 |
CLT048 |
BEGINNING-DATE-OF-SERVICE |
CLAIMLT |
CLAIM-HEADER-RECORD-LT-CLT00002 |
CLT050 |
ADJUDICATION-DATE |
CLAIMLT |
CLAIM-HEADER-RECORD-LT-CLT00002 |
CLT055 |
CLAIM-STATUS-CATEGORY |
CLAIMLT |
CLAIM-HEADER-RECORD-LT-CLT00002 |
CLT130 |
BILLING-PROV-NUM |
CLAIMLT |
CLAIM-HEADER-RECORD-LT-CLT00002 |
CLT135 |
REFERRING-PROV-NUM |
CLAIMLT |
CLAIM-HEADER-RECORD-LT-CLT00002 |
CLT184 |
RECORD-ID |
CLAIMLT |
CLAIM-LINE-RECORD-LT-CLT00003 |
CLT185 |
SUBMITTING-STATE |
CLAIMLT |
CLAIM-LINE-RECORD-LT-CLT00003 |
CLT186 |
RECORD-NUMBER |
CLAIMLT |
CLAIM-LINE-RECORD-LT-CLT00003 |
CLT188 |
ICN-ORIG |
CLAIMLT |
CLAIM-LINE-RECORD-LT-CLT00003 |
CLT189 |
ICN-ADJ |
CLAIMLT |
CLAIM-LINE-RECORD-LT-CLT00003 |
CLT190 |
LINE-NUM-ORIG |
CLAIMLT |
CLAIM-LINE-RECORD-LT-CLT00003 |
CLT191 |
LINE-NUM-ADJ |
CLAIMLT |
CLAIM-LINE-RECORD-LT-CLT00003 |
CLT196 |
BEGINNING-DATE-OF-SERVICE |
CLAIMLT |
CLAIM-LINE-RECORD-LT-CLT00003 |
CLT212 |
SERVICING-PROV-NUM |
CLAIMLT |
CLAIM-LINE-RECORD-LT-CLT00003 |
CLT233 |
ADJUDICATION-DATE |
CLAIMLT |
CLAIM-LINE-RECORD-LT-CLT00003 |
Table 8: Claim IP IIFI Data Elements (33 IIFIs)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
CIP001 |
RECORD-ID |
CLAIMIP |
FILE-HEADER-RECORD-IP-CIP00001 |
CIP002 |
DATA-DICTIONARY-VERSION |
CLAIMIP |
FILE-HEADER-RECORD-IP-CIP00001 |
CIP003 |
SUBMISSION-TRANSACTION-TYPE |
CLAIMIP |
FILE-HEADER-RECORD-IP-CIP00001 |
CIP004 |
FILE-ENCODING-SPECIFICATION |
CLAIMIP |
FILE-HEADER-RECORD-IP-CIP00001 |
CIP005 |
DATA-MAPPING-DOCUMENT-VERSION |
CLAIMIP |
FILE-HEADER-RECORD-IP-CIP00001 |
CIP006 |
FILE-NAME |
CLAIMIP |
FILE-HEADER-RECORD-IP-CIP00001 |
CIP007 |
SUBMITTING-STATE |
CLAIMIP |
FILE-HEADER-RECORD-IP-CIP00001 |
CIP009 |
START-OF-TIME-PERIOD |
CLAIMIP |
FILE-HEADER-RECORD-IP-CIP00001 |
CIP010 |
END-OF-TIME-PERIOD |
CLAIMIP |
FILE-HEADER-RECORD-IP-CIP00001 |
CIP011 |
FILE-STATUS-INDICATOR |
CLAIMIP |
FILE-HEADER-RECORD-IP-CIP00001 |
CIP012 |
SSN-INDICATOR |
CLAIMIP |
FILE-HEADER-RECORD-IP-CIP00001 |
CIP013 |
TOT-REC-CNT |
CLAIMIP |
FILE-HEADER-RECORD-IP-CIP00001 |
CIP275 |
SEQUENCE-NUMBER |
CLAIMIP |
FILE-HEADER-RECORD-IP-CIP00001 |
CIP016 |
RECORD-ID |
CLAIMIP |
CLAIM-HEADER-RECORD-IP-CIP00002 |
CIP017 |
SUBMITTING-STATE |
CLAIMIP |
CLAIM-HEADER-RECORD-IP-CIP00002 |
CIP018 |
RECORD-NUMBER |
CLAIMIP |
CLAIM-HEADER-RECORD-IP-CIP00002 |
CIP019 |
ICN-ORIG |
CLAIMIP |
CLAIM-HEADER-RECORD-IP-CIP00002 |
CIP020 |
ICN-ADJ |
CLAIMIP |
CLAIM-HEADER-RECORD-IP-CIP00002 |
CIP026 |
ADJUSTMENT-IND |
CLAIMIP |
CLAIM-HEADER-RECORD-IP-CIP00002 |
CIP098 |
ADJUDICATION-DATE |
CLAIMIP |
CLAIM-HEADER-RECORD-IP-CIP00002 |
CIP103 |
CLAIM-STATUS-CATEGORY |
CLAIMIP |
CLAIM-HEADER-RECORD-IP-CIP00002 |
CIP179 |
BILLING-PROV-NUM |
CLAIMIP |
CLAIM-HEADER-RECORD-IP-CIP00002 |
CIP189 |
REFERRING-PROV-NUM |
CLAIMIP |
CLAIM-HEADER-RECORD-IP-CIP00002 |
CIP231 |
RECORD-ID |
CLAIMIP |
CLAIM-LINE-RECORD-IP-CIP00003 |
CIP232 |
SUBMITTING-STATE |
CLAIMIP |
CLAIM-LINE-RECORD-IP-CIP00003 |
CIP233 |
RECORD-NUMBER |
CLAIMIP |
CLAIM-LINE-RECORD-IP-CIP00003 |
CIP235 |
ICN-ORIG |
CLAIMIP |
CLAIM-LINE-RECORD-IP-CIP00003 |
CIP236 |
ICN-ADJ |
CLAIMIP |
CLAIM-LINE-RECORD-IP-CIP00003 |
CIP237 |
LINE-NUM-ORIG |
CLAIMIP |
CLAIM-LINE-RECORD-IP-CIP00003 |
CIP238 |
LINE-NUM-ADJ |
CLAIMIP |
CLAIM-LINE-RECORD-IP-CIP00003 |
CIP243 |
BEGINNING-DATE-OF-SERVICE |
CLAIMIP |
CLAIM-LINE-RECORD-IP-CIP00003 |
CIP260 |
SERVICING-PROV-NUM |
CLAIMIP |
CLAIM-LINE-RECORD-IP-CIP00003 |
CIP286 |
ADJUDICATION-DATE |
CLAIMIP |
CLAIM-LINE-RECORD-IP-CIP00003 |
IIFI Data Element Names
Table 9 contains a listing of unique data element names that represent the IIFI subset. While 448 total IIFI data elements exist, only 122 unique data element names exist. This data element name duplication is due to data element names that are required in each file segment, such as 'Submitting-State' and 'Record-Number'.
Table 9: Unique IIFI Data Elements (122)
Data Element Name |
1115A-DEMONSTRATION-IND |
1115A-EFF-DATE |
ACCREDITATION-ORGANIZATION |
ADDR-TYPE |
ADJUDICATION-DATE |
ADJUSTMENT-IND |
AFFILIATED-PROGRAM-ID |
AFFILIATED-PROGRAM-TYPE |
BED-TYPE-CODE |
BED-TYPE-EFF-DATE |
BEGINNING-DATE-OF-SERVICE |
BILLING-PROV-NUM |
CHPID |
CHPID-SHPID-RELATIONSHIP-EFF-DATE |
CLAIM-STATUS-CATEGORY |
COVERAGE-TYPE |
DATA-DICTIONARY-VERSION |
DATA-MAPPING-DOCUMENT-VERSION |
DATE-ACCREDITATION-ACHIEVED |
DISABILITY-TYPE-CODE |
DISABILITY-TYPE-EFF-DATE |
DISPENSING-PRESCRIPTION-DRUG-PROV-NUM |
ELIGIBILITY-DETERMINANT-EFF-DATE |
ELIGIBLE-ADDR-EFF-DATE |
ELIG-PRSN-MAIN-EFF-DATE |
END-OF-TIME-PERIOD |
ENROLLMENT-EFF-DATE |
ENROLLMENT-TYPE |
ETHNICITY-CODE |
ETHNICITY-DECLARATION-EFF-DATE |
FILE-ENCODING-SPECIFICATION |
FILE-NAME |
FILE-STATUS-INDICATOR |
GROUP-NUM |
HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-CODE |
HCBS-CHRONIC-CONDITION-NON-HEALTH-HOME-EFF-DATE |
HEALTH-HOME-CHRONIC-CONDITION |
HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE |
HEALTH-HOME-CHRONIC-CONDITION-OTHER-EXPLANATION |
HEALTH-HOME-ENTITY-NAME |
HEALTH-HOME-PROV-NUM |
HEALTH-HOME-SPA-NAME |
HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE |
HEALTH-HOME-SPA-PROVIDER-EFF-DATE |
ICN-ADJ |
ICN-ORIG |
INSURANCE-CARRIER-ID-NUM |
INSURANCE-CATEGORIES-EFF-DATE |
INSURANCE-COVERAGE-EFF-DATE |
INSURANCE-PLAN-ID |
LICENSE-ISSUING-ENTITY-ID |
LICENSE-TYPE |
LINE-NUM-ADJ |
LINE-NUM-ORIG |
LOCKIN-EFF-DATE |
LOCKIN-PROV-NUM |
LOCKIN-PROV-TYPE |
LTSS-ELIGIBILITY-EFF-DATE |
LTSS-LEVEL-CARE |
LTSS-PROV-NUM |
MANAGED-CARE-ADDR-TYPE |
MANAGED-CARE-LOCATION-AND-CONTACT-INFO-EFF-DATE |
MANAGED-CARE-LOCATION-ID |
MANAGED-CARE-MAIN-REC-EFF-DATE |
MANAGED-CARE-OP-AUTHORITY-EFF-DATE |
MANAGED-CARE-PLAN-ENROLLMENT-EFF-DATE |
MANAGED-CARE-PLAN-ID |
MANAGED-CARE-PLAN-POP |
MANAGED-CARE-PLAN-POP-EFF-DATE |
MANAGED-CARE-SERVICE-AREA-EFF-DATE |
MANAGED-CARE-SERVICE-AREA-NAME |
MEMBER-ID |
MFP-ENROLLMENT-EFF-DATE |
MSIS-CASE-NUM |
MSIS-IDENTIFICATION-NUM |
NATIONAL-HEALTH-CARE-ENTITY-ID |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE |
NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE |
OPERATING-AUTHORITY |
OTHER-TPL-EFF-DATE |
PRESCRIBING-PROV-NUM |
PRIMARY-DEMOGRAPHIC-ELEMENT-EFF-DATE |
PROV-AFFILIATED-GROUP-EFF-DATE |
PROV-AFFILIATED-PROGRAM-EFF-DATE |
PROV-ATTRIBUTES-EFF-DATE |
PROV-CLASSIFICATION-CODE |
PROV-CLASSIFICATION-TYPE |
PROV-IDENTIFIER |
PROV-IDENTIFIER-EFF-DATE |
PROV-IDENTIFIER-ISSUING-ENTITY-ID |
PROV-IDENTIFIER-TYPE |
PROV-LICENSE-EFF-DATE |
PROV-LOCATION-AND-CONTACT-INFO-EFF-DATE |
PROV-LOCATION-ID |
PROV-MEDICAID-EFF-DATE |
PROV-MEDICAID-ENROLLMENT-STATUS-CODE |
PROV-TAXONOMY-CLASSIFICATION-EFF-DATE |
RACE |
RACE-DECLARATION-EFF-DATE |
RACE-OTHER |
RECORD-ID |
RECORD-NUMBER |
REFERRING-PROV-NUM |
SEQUENCE-NUMBER |
SERVICING-PROV-NUM |
SHPID |
SSN-INDICATOR |
START-OF-TIME-PERIOD |
STATE-PLAN-ID-NUM |
STATE-PLAN-OPTION-EFF-DATE |
STATE-PLAN-OPTION-TYPE |
SUBMISSION-TRANSACTION-TYPE |
SUBMITTING-STATE |
SUBMITTING-STATE-PROV-ID |
SUBMITTING-STATE-PROV-ID-OF-AFFILIATED-ENTITY |
TOT-REC-CNT |
TPL-ENTITY-ADDR-TYPE |
TPL-ENTITY-CONTACT-INFO-EFF-DATE |
TYPE-OF-OTHER-THIRD-PARTY-LIABILITY |
VARIABLE-DEMOGRAPHIC-ELEMENT-EFF-DATE |
WAIVER-ENROLLMENT-EFF-DATE |
WAIVER-ID |
Program Specific Data Elements
Table 10: Eligible – 1115 Demonstration – (2 Program Specific Data Elements)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
ELG233 |
1115A-DEMONSTRATION-IND |
ELIGIBLE |
1115A-DEMONSTRATION-INFORMATION-ELG00018 |
ELG234 |
1115A-EFF-DATE |
ELIGIBLE |
1115A-DEMONSTRATION-INFORMATION-ELG00018 |
Table 11: Eligible – Health Home – (9 Program Specific Data Elements)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
ELG132 |
HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE |
ELIGIBLE |
HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 |
ELG131 |
HEALTH-HOME-CHRONIC-CONDITION-OTHER-EXPLANATION |
ELIGIBLE |
HEALTH-HOME-CHRONIC-CONDITIONS-ELG00008 |
ELG108 |
HEALTH-HOME-ENTITY-NAME |
ELIGIBLE |
HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 |
ELG107 |
HEALTH-HOME-SPA-NAME |
ELIGIBLE |
HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 |
ELG109 |
HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE |
ELIGIBLE |
HEALTH-HOME-SPA-PARTICIPATION-INFORMATION-ELG00006 |
ELG119 |
HEALTH-HOME-ENTITY-NAME |
ELIGIBLE |
HEALTH-HOME-SPA-PROVIDERS-ELG00007 |
ELG120 |
HEALTH-HOME-PROV-NUM |
ELIGIBLE |
HEALTH-HOME-SPA-PROVIDERS-ELG00007 |
ELG118 |
HEALTH-HOME-SPA-NAME |
ELIGIBLE |
HEALTH-HOME-SPA-PROVIDERS-ELG00007 |
ELG121 |
HEALTH-HOME-SPA-PROVIDER-EFF-DATE |
ELIGIBLE |
HEALTH-HOME-SPA-PROVIDERS-ELG00007 |
Table 12: Eligible – Lock-In Provider – (3 Program Specific Data Elements)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
ELG142 |
LOCKIN-EFF-DATE |
ELIGIBLE |
LOCK-IN-INFORMATION-ELG00009 |
ELG140 |
LOCKIN-PROV-NUM |
ELIGIBLE |
LOCK-IN-INFORMATION-ELG00009 |
ELG141 |
LOCKIN-PROV-TYPE |
ELIGIBLE |
LOCK-IN-INFORMATION-ELG00009 |
Table 13: Eligible – Managed-Care-Participation – (2 Program Specific Data Elements)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
ELG196 |
MANAGED-CARE-PLAN-ENROLLMENT-EFF-DATE |
ELIGIBLE |
MANAGED-CARE-PARTICIPATION-ELG00014 |
ELG192 |
MANAGED-CARE-PLAN-ID |
ELIGIBLE |
MANAGED-CARE-PARTICIPATION-ELG00014 |
Table 14: Eligible – Money Follows the Person – (1 Program Specific Data Element)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
ELG155 |
MFP-ENROLLMENT-EFF-DATE |
ELIGIBLE |
MFP-INFORMATION-ELG00010 |
Table 15: Managed Care – (3 Program Specific Data Elements)
DE No |
Data Element Name |
FILE NAME |
File Segment (with Record-ID) |
MCR095 |
NATIONAL-HEALTH-CARE-ENTITY-ID |
MNGDCARE |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 |
MCR096 |
NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE |
MNGDCARE |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 |
MCR098 |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE |
MNGDCARE |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-MCR00008 |
Program Specific Data Element Names
The following table contains a listing of 20 unique data element names that represent the Program Specific data element subset.
Table 16: Unique Program Specific Data Elements (20)
Data Element Name |
1115A-DEMONSTRATION-IND |
1115A-EFF-DATE |
HEALTH-HOME-CHRONIC-CONDITION-EFF-DATE |
HEALTH-HOME-CHRONIC-CONDITION-OTHER-EXPLANATION |
HEALTH-HOME-ENTITY-NAME |
HEALTH-HOME-ENTITY-NAME |
HEALTH-HOME-PROV-NUM |
HEALTH-HOME-SPA-NAME |
HEALTH-HOME-SPA-NAME |
HEALTH-HOME-SPA-PARTICIPATION-EFF-DATE |
HEALTH-HOME-SPA-PROVIDER-EFF-DATE |
LOCKIN-EFF-DATE |
LOCKIN-PROV-NUM |
LOCKIN-PROV-TYPE |
MANAGED-CARE-PLAN-ENROLLMENT-EFF-DATE |
MANAGED-CARE-PLAN-ID |
MFP-ENROLLMENT-EFF-DATE |
NATIONAL-HEALTH-CARE-ENTITY-ID |
NATIONAL-HEALTH-CARE-ENTITY-ID-TYPE |
NATIONAL-HEALTH-CARE-ENTITY-ID-INFO-EFF-DATE |
CMS Guidance
Since the IIFI and Program Specific data elements are of such fundamental importance to file integrity and data analysis, the state will be asked to review how IIFI and Program Specific data elements marked with “never” or “sometimes” availability can be upgraded to “always”(when applicable). Therefore, states should review each IIFI and Program Specific (when applicable) data element and reevaluate its ability to provide these data elements in its final consolidated 8 file submission.
Appendix P.07: Finding Provider Roles on STD Transactions
How to use this guidance document
This guidance document is not intended to slow down or derail existing state development initiatives. The intent is to provide clarification and standardization across the nation in key areas raised by state partners. Should guidance introduce rework in ongoing development, please bring this to the attention of your TA and CMS analyst to direct you to the most appropriate path that minimizes impact to your progress.
Brief Issue Description
Some States have requested assistance with identifying where to find in the X-12 claim transaction sets the NPIs and taxonomy codes of providers who performed various roles associated with the claim/encounter.
Background Discussion
Definitions
Provider role – The function that a specific provider performed for a particular patient on specified dates of service, and which are contained on fee-for-service claims or reported on encounter records. The particular roles that CMS would like to track on T-MSIS claims are:
Admitting (attending) provider
Billing provider
Dispensing provider
Operating provider
Prescribing provider
Referring provider
Servicing (rendering) provider
Under supervision of provider
Provider role information needed for the T-MSIS claim files can be extracted from the standard X-12 transactions. The five tables in the “CMS Guidance” section of this document provide T-MSIS-toX-12 crosswalks for each provider role. The five tables are:
Table A: Provider roles on T-MSIS CLAIMIP files and their corresponding locations on the X-12 transactions
Table B: Provider roles on T-MSIS CLAIMLT files and their corresponding locations on the X-12 transactions
Table C: Provider roles on T-MSIS CLAIMOT (facility claims) files and their corresponding locations on the X-12 transactions
Table D: Provider roles on T-MSIS CLAIMOT (professional claims) files and their corresponding locations on the X-12 transactions
Table E: Provider roles on T-MSIS CLAIMOT (dental claims) files and their corresponding locations on the X-12 transactions
Table F: Provider roles on T-MSIS CLAIMRX files and their corresponding locations on the X-12 transactions
In each table, the first column identifies the provider role. The second and third columns identify the specific T-MSIS record segments and data elements used to capture the NPI and taxonomy of the provider performing the specified role. The fourth, fifth, sixth, and seventh columns in tables “A” through “E” provide the X-12 transaction name, data element identifier, data element description and loop id that map to the T-MSIS data element. The fourth, fifth, sixth, and seventh columns in table “F” provide the segment name, field identifier, field name and definition of the applicable NCPDP D.0 data set fields.
CMS Guidance
Use tables “A” through “F” to map the provider roles that are contained in the T-MSIS claim record layouts to their corresponding X-12 standard transaction data elements.
If the T-MSIS data element does not exist in the X-12 transaction set (shown as “N/A” in the tables below), 8-fill the T-MSIS data element when building T-MSIS claim files.
Table A: Provider roles on T-MSIS CLAIMIP files and their corresponding locations on the X-12 transactions
Provider Role |
IP – T-MSIS Data element & Record Segment |
X-12 Transaction Information |
|||||
Data Element |
Record Segment |
Transaction |
Element Identifier |
Description |
Loop |
Conditional Rules |
|
Admitting (Attending)
|
ADMITTING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-IP-CIP00002 |
5010 A2 837-I Institutional Claim |
NM109 |
Attending Provider Identifier |
2310A |
|
ADMITTING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-IP-CIP00002 |
5010 A2 837-I Institutional Claim |
PRV03 |
Provider Taxonomy Code |
2310A |
|
|
Billing
|
BILLING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-IP-CIP00002 |
5010 A2 837-I Institutional Claim |
NM109 |
Billing Provider Identifier |
2010AA |
|
BILLING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-IP-CIP00002 |
5010 A2 837-I Institutional Claim |
PRV03 |
Provider Taxonomy Code |
2000A |
|
|
Operating
|
OPERATING-PROV-NPI-NUM |
CLAIM-LINE-RECORD-IP-CIP00003 |
5010 A2 837-I Institutional Claim |
NM109 |
Operating Physician Identifier |
2310B or 2420A |
The identifier in the 837i loop 2310B could be applied to each line in T-MSIS except for lines where there is a different identifier in loop 2420A at the line level of the 837i. If there is a different identifier in 837i loop 2420A then the identifier from loop 2420A should be reported as the operating provider identifier. |
OPERATING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-IP-CIP00002 |
N/A |
N/A |
N/A |
N/A |
|
|
Referring
|
REFERRING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-IP-CIP00002 |
5010 A2 837-I Institutional Claim |
NM109 |
Referring Provider Identifier |
2310F or 2420D |
The identifier in the 837i loop 2310F could be applied to each line in T-MSIS except for lines where there is a different identifier in 2420D at the line level of the 837i. If there is a different identifier in 837i loop 2420D then the identifier from 2420D should be reported as the referring provider identifier. |
REFERRING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-IP-CIP00002 |
N/A |
N/A |
N/A |
N/A |
|
|
Servicing (Rendering)
|
SERVICING-PROV-NPI-NUM |
CLAIM-LINE-RECORD-IP-CIP00003 |
5010 A2 837-I Institutional Claim |
NM109 |
Rendering Provider Identifier |
2310D or 2420C |
The identifier in the 837i loop 2310D could be applied to each line in T-MSIS except for lines where there is a different identifier in 2420C at the line level of the 837i. If there is a different identifier in 837i loop 2420C then the identifier from loop 2420C should be reported as the servicing/rendering provider identifier. |
SERVICING-PROV-TAXONOMY |
CLAIM-LINE-RECORD-IP-CIP00003 |
N/A |
N/A |
N/A |
N/A |
|
|
Under-Direction-of
|
UNDER-DIRECTION-OF-PROV-NPI |
CLAIM-HEADER-RECORD-IP-CIP00002 |
N/A |
N/A |
N/A |
N/A |
|
UNDER-DIRECTION-OF-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-IP-CIP00002 |
N/A |
N/A |
N/A |
N/A |
|
|
Under-Supervision-of
|
UNDER-SUPERVISION-OF-PROV-NPI |
CLAIM-HEADER-RECORD-IP-CIP00002 |
N/A |
N/A |
N/A |
N/A |
|
UNDER-SUPERVISION-OF-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-IP-CIP00002 |
N/A |
N/A |
N/A |
N/A |
|
|
Table B: Provider roles on T-MSIS CLAIMLT files and their corresponding locations on the X-12 transactions
Provider Role |
LT – T-MSIS Data element & Record Segment |
X-12 Transaction Information |
|||||
Data Element |
Record Segment |
Transaction |
Element Identifier |
Description |
Loop |
Conditional Rules |
|
Admitting (Attending) |
ADMITTING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-LT-CLT00002 |
5010 A2 837-I Institutional Claim |
NM109 |
Attending Provider Identifier |
2310A |
|
|
ADMITTING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-LT-CLT00002 |
|
PRV03 |
Provider Taxonomy Code |
2310A |
|
Billing |
BILLING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-LT-CLT00002 |
5010 A2 837-I Institutional Claim |
NM109 |
Billing Provider Identifier |
2010AA |
|
|
BILLING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-LT-CLT00002 |
|
PRV03 |
Provider Taxonomy Code |
2000A |
|
Referring |
REFERRING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-LT-CLT00002 |
5010 A2 837-I Institutional Claim |
NM109 |
Referring Provider Identifier |
2310F or 2420D |
The identifier in the 837i loop 2310F could be applied to each line in T-MSIS except for lines where there is a different identifier in 2420D at the line level of the 837i. If there is a different identifier in 837i loop 2420D then the identifier from 2420D should be reported as the referring provider identifier. |
|
REFERRING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-LT-CLT00002 |
N/A |
N/A |
N/A |
N/A |
|
Servicing (Rendering) |
SERVICING-PROV-NPI-NUM |
CLAIM-LINE-RECORD-LT-CLT00003 |
5010 A2 837-I Institutional Claim |
NM109 |
Rendering Provider Identifier |
2310D or 2420C |
The identifier in the 837i loop 2310D could be applied to each line in T-MSIS except for lines where there is a different identifier in loop 2420C at the line level of the 837i. If there is a different identifier in 837i loop 2420C then the identifier from loop 2420C should be reported as the servicing/rendering provider identifier. |
|
SERVICING-PROV-TAXONOMY |
CLAIM-LINE-RECORD-LT-CLT00003 |
N/A |
N/A |
N/A |
N/A |
|
Under-Direction-of |
UNDER-DIRECTION-OF-PROV-NPI |
CLAIM-HEADER-RECORD-LT-CLT00002 |
N/A |
N/A |
N/A |
N/A |
|
|
UNDER-DIRECTION-OF-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-LT-CLT00002 |
N/A |
N/A |
N/A |
N/A |
|
Under-Supervision-of |
UNDER-SUPERVISION-OF-PROV-NPI |
CLAIM-HEADER-RECORD-LT-CLT00002 |
N/A |
N/A |
N/A |
N/A |
|
|
UNDER-SUPERVISION-OF-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-LT-CLT00002 |
N/A |
N/A |
N/A |
N/A |
|
Table C: Provider roles on T-MSIS CLAIMOT (facility claims) files and their corresponding locations on the X-12 transactions
Provider Role |
OT (facility) – T-MSIS Data element & Record Segment |
X-12 Transaction Information |
|||||
Data Element |
Record Segment |
Transaction |
Element Identifier |
Description |
Loop |
Conditional Rules |
|
Billing |
BILLING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-OT-COT00002 |
5010 A2 837-I Institutional Claim |
NM109 |
Billing Provider Identifier |
2010AA |
|
|
BILLING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-OT-COT00002 |
5010 A2 837-I Institutional Claim |
PRV03 |
Provider Taxonomy Code |
2000A |
|
Referring |
REFERRING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-OT-COT00002 |
5010 A2 837-I Institutional Claim |
NM109 |
Referring Provider Identifier |
2310F or 2420D |
The identifier in the 837i loop 2310F could be applied to each line in T-MSIS except for lines where there is a different identifier in 2420D at the line level of the 837i. If there is a different identifier in 837i loop 2420D then the identifier from 2420D should be reported as the referring provider identifier. |
|
REFERRING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-OT-COT00002 |
N/A |
N/A |
N/A |
N/A |
|
Servicing (Rendering) |
SERVICING-PROV-NPI-NUM |
CLAIM-LINE-RECORD-OT-COT00003 |
5010 A2 837-I Institutional Claim |
NM109 |
Rendering Provider Identifier |
2310D or 2420C |
The identifier in the 837i loop 2310D could be applied to each line in T-MSIS except for lines where there is a different identifier in 2420C at the line level of the 837i. If there is a different identifier in 837i loop 2420C then the identifier from loop 2420C should be reported as the servicing/rendering provider identifier. |
|
SERVICING-PROV-TAXONOMY |
CLAIM-LINE-RECORD-OT-COT00003 |
N/A |
N/A |
N/A |
N/A |
|
Under-Direction-of |
UNDER-DIRECTION-OF-PROV-NPI |
CLAIM-HEADER-RECORD-OT-COT00002 |
N/A |
N/A |
N/A |
N/A |
|
|
UNDER-DIRECTION-OF-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-OT-COT00002 |
N/A |
N/A |
N/A |
N/A |
|
Under-Supervision-of |
UNDER-SUPERVISION-OF-PROV-NPI |
CLAIM-HEADER-RECORD-OT-COT00002 |
N/A |
N/A |
N/A |
N/A |
|
|
UNDER-SUPERVISION-OF-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-OT-COT00002 |
N/A |
N/A |
N/A |
N/A |
|
Table D: Provider roles on T-MSIS CLAIMOT (professional claims) files and their corresponding locations on the X-12 transactions
Provider Role |
OT (professional) – T-MSIS Data element & Record Segment |
X-12 Transaction Information |
|||||
Data Element |
Record Segment |
Transaction |
Element Identifier |
Description |
Loop |
Conditional Rules |
|
Billing |
BILLING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-OT-COT00002 |
5010 A1 837-P Professional Claim
|
NM109 |
Billing Provider Identifier |
2010AA |
|
|
BILLING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-OT-COT00002 |
5010 A1 837-P Professional Claim
|
PRV03 |
Provider Taxonomy Code |
2000A |
|
Referring |
REFERRING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-OT-COT00002 |
5010 A1 837-P Professional Claim
|
NM109 |
Referring Provider Identifier |
2310A or 2420F |
The identifier in the 837p loop 2310A could be applied to each line in T-MSIS except for lines where there is a different identifier in 2420F at the line level of the 837p. If there is a different identifier in 837p loop 2420F then the identifier from 2420F should be reported as the referring provider identifier. |
|
REFERRING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-OT-COT00002 |
N/A |
N/A |
N/A |
N/A |
|
Servicing (Rendering) |
SERVICING-PROV-NPI-NUM |
CLAIM-LINE-RECORD-OT-COT00003 |
5010 A1 837-P Professional Claim
|
NM109 |
Rendering Provider Identifier |
2310B or 2420A |
The identifier in the 837p loop 2310B could be applied to each line in T-MSIS except for lines where there is a different identifier in 2420A at the line level of the 837p. If there is a different identifier in 837p loop 2420A then the identifier from 2420A should be reported as the servicing/rendering provider identifier. |
|
SERVICING-PROV-TAXONOMY |
CLAIM-LINE-RECORD-OT-COT00003 |
5010 A1 837-P Professional Claim
|
PRV03 |
Provider Taxonomy Code |
2310B or 2420A |
The taxonomy in the 837p loop 2310B could be applied to each line in T-MSIS except for lines where there is a different taxonomy in 2420A at the line level of the 837p. If there is a different taxonomy in 837p loop 2420A then the taxonomy from 2420A should be reported as the servicing/rendering provider taxonomy. |
Under-Direction-of |
UNDER-DIRECTION-OF-PROV-NPI |
CLAIM-HEADER-RECORD-OT-COT00002 |
N/A |
N/A |
N/A |
N/A |
|
|
UNDER-DIRECTION-OF-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-OT-COT00002 |
N/A |
N/A |
N/A |
N/A |
|
Under-Supervision-of |
UNDER-SUPERVISION-OF-PROV-NPI |
CLAIM-HEADER-RECORD-OT-COT00002 |
5010 A1 837-P Professional Claim |
NM109 |
Supervising Provider Identifier |
2310D or 2420D |
The identifier in the 837p loop 2310D could be applied to each line in T-MSIS except for lines where there is a different identifier in loop 2420D at the line level of the 837p. If there is a different identifier in loop 2420D then the identifier from loop 2420D should be reported as the under-supervision-of provider identifier. |
|
UNDER-SUPERVISION-OF-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-OT-COT00002 |
N/A |
N/A |
N/A |
N/A |
|
Table E: Provider roles on T-MSIS CLAIMOT (dental claims) files and their corresponding locations on the X-12 transactions
Provider Role |
OT (dental) – T-MSIS Data element & Record Segment |
X-12 Transaction Information |
|||||
Data Element |
Record Segment |
Transaction |
Element Identifier |
Description |
Loop |
Conditional Rules |
|
Billing |
BILLING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-OT-COT00002 |
5010 A1 837-D Dental Claim |
NM109 |
Billing Provider Identifier |
2010AA |
|
|
BILLING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-OT-COT00002 |
5010 A1 837-D Dental Claim |
PRV03 |
Provider Taxonomy Code |
2000A |
|
Referring |
REFERRING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-OT-COT00002 |
5010 A1 837-D Dental Claim |
NM109 |
Referring Provider Identifier |
2310A |
|
|
REFERRING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-OT-COT00002 |
N/A |
N/A |
N/A |
N/A |
|
Servicing (Rendering) |
SERVICING-PROV-NPI-NUM |
CLAIM-LINE-RECORD-OT-COT00003 |
5010 A1 837-D Dental Claim |
NM109 |
Rendering Provider Identifier |
2310B or 2420A |
The identifier in 837d loop 2310B could be applied to each line in T-MSIS except for lines where there is a different identifier in 2420A at the line level of the 837d. If there is a different identifier in 837d) loop 2420A then the identifier from 2420A should be reported as the servicing/rendering provider identifier. |
|
SERVICING-PROV-TAXONOMY |
CLAIM-LINE-RECORD-OT-COT00003 |
5010 A1 837-D Dental Claim |
PRV03 |
Provider Taxonomy Code |
2310B or 2420A |
The taxonomy in the 837d loop 2310B could be applied to each line in T-MSIS except for lines where there is a different taxonomy in 2420A at the line level of the 837p. If there is a different taxonomy in 837p loop 2420A then the taxonomy from 2420A should be reported as the servicing/rendering provider taxonomy. |
Under-Direction-of |
UNDER-DIRECTION-OF-PROV-NPI |
CLAIM-HEADER-RECORD-OT-COT00002 |
N/A |
N/A |
N/A |
N/A |
|
|
UNDER-DIRECTION-OF-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-OT-COT00002 |
N/A |
N/A |
N/A |
N/A |
|
Under-Supervision-of |
UNDER-SUPERVISION-OF-PROV-NPI |
CLAIM-HEADER-RECORD-OT-COT00002 |
5010 A1 837-D Dental Claim |
NM109 |
Supervising Provider Identifier |
2310E or 2420C |
The identifier in the 837d loop 2310E could be applied to each line in T-MSIS except for lines where there is a different identifier in loop 2420C at the line level of the 837d. If there is a different identifier in loop 2420C then the identifier from loop 2420C should be reported as the under-supervision-of provider identifier. |
|
UNDER-SUPERVISION-OF-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-OT-COT00002 |
N/A |
N/A |
N/A |
N/A |
|
Table F: Provider roles on T-MSIS CLAIMRX (prescription drug) files and their corresponding locations on the X-12 transactions
Provider Role |
Rx – T-MSIS Data element & Record Segment |
X-12 Transaction Information |
||||
Data Element |
Record Segment |
Segment |
Field |
Field Name |
Definition |
|
Billing |
BILLING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-RX-CRX00002 |
NCPDP D.0 - Transaction Header Segment |
201-B1 |
Service Provider ID |
ID assigned to a pharmacy or provider |
|
BILLING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-RX-CRX00002 |
N/A |
N/A |
N/A |
N/A |
Dispensing |
DISPENSING-PRESCRIPTION-DRUG-PROV-NPI |
CLAIM-HEADER-RECORD-RX-CRX00002 |
NCPDP D.0 - Pharmacy Provider Segment |
444-E9 |
Provider ID |
ID assigned to a pharmacy or provider individual responsible for dispensing the prescription |
|
DISPENSING-PRESCRIPTION-DRUG-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-RX-CRX00002 |
N/A |
N/A |
N/A |
N/A |
Prescribing |
PRESCRIBING-PROV-NPI-NUM |
CLAIM-HEADER-RECORD-RX-CRX00002 |
NCPDP D.0 - Prescriber Segment |
411-DB |
Prescriber ID |
ID assigned to the prescriber |
|
PRESCRIBING-PROV-TAXONOMY |
CLAIM-HEADER-RECORD-RX-CRX00002 |
N/A |
N/A |
N/A |
N/A |
Appendix Q: Terms and Abbreviations
Acronym/Abbreviation Description
AAAHC Accreditation Association for Ambulatory Health Care, Inc.
ABD Aged, Blind and Disabled
ACA Affordable Care Act
ADA American Dental Association
ADDR Address
AFDC Aid to Families with Dependent Children
AIDS Acquired Immunodeficiency Syndrome
AMT Amount
ANSI American National Standards Institute
APC Ambulatory payment classifications
APPL Application
ARNP Advanced Registered Nurse Practitioner
ASC Ambulatory Surgical Center
ASCII American Standard Code for Information Interchange
ATP Ability-To-Pay
BIP Balancing Incentive Program
BMI Body Mass Index
BOE Basis of Eligibility
CBSA Core Based Statistical Area
CD Code
CDIB Certificate of Degree of Indian or Alaska Native Blood
CEO Chief Executive Officer
CFO Chief Financial Officer
CFR Code of Federal Regulations
CHIP Children’s Health Insurance Program
CHIPRA Children’s Health Insurance Program Reauthorization Act
CHPID Controlling Health Plan Identifiers
CLIA Clinical Laboratory Improvement Amendment
CMCS Center for Medicaid, CHIP and Surveys and Certifications
CMHC Community Mental Health Center
CMMI Center for Medicare and Medicaid Innovation
CMS Centers for Medicare & Medicaid Services
COBOL Common Business Oriented Language
COBRA Consolidated Omnibus Budget Reconciliation Act of 1986
COLA Cost-of-Living Adjustment
CORF Comprehensive Outpatient Rehabilitation Facility
COV Covered
CPE Certified Public Expenditures
CPT Current Procedural Terminology
CRNA Certified Registered Nurse Anesthetists
CRVS California Relative Value Study
CWF Common Working File
DBA Doing Business As
DEA Drug Enforcement Agency
DED Deductible
DME Durable Medical Equipment
DO Doctor of osteopathy
DRG Diagnosis Related Group
DSH Disproportionate Share Hospital
DSN Data Set Name
DTL Detail
DUR Drug Utilization Review
EBCDIC Extended Binary-Coded-Decimal Interchange Code
EDI Electronic Data Interchange
EFF Effective
EFT Electronic Funds Transfer; or Electronic File Transfer
EPSDT Early and Periodic Screening, Diagnosis, and Treatment
ESI Employer Sponsored Insurance
ESRD End Stage Renal Disease
FFP Federal Financial Participation
FFS Fee-for-Service
FFY Federal Fiscal Year
FFYQ Federal Fiscal Year Quarter
FI Fiscal Intermediary
FL Form Locator
FLF Fixed Length Format
FPL Federal Poverty Level
FQHC Federally Qualified Health Center
GME Graduate Medical Education
HCBS Home and Community-Based Services
HCC RA Hierarchical Condition Category Risk Assessment
HCFA Health Care Financing Administration
HCPCS Health Care Procedural Coding System
HETS HIPAA Eligibility Transaction System
HHA Home Health Agency
HHPPS Home Health Prospective Payment System
Hib Haemophilus influenza type b
HIC Health Insurance Claim
HICN Health Insurance Claim Number
HIFA Health Insurance and Flexibility and Accountability
HIO Health Insurance Organization
HIPAA Health Insurance Portability and Accountably Act of 1996
HIV Human immunodeficiency virus
HMO Health Maintenance Organization
HPV Human Papillomavirus
IBM International Business Machines, Inc.
ICD International Classification of Diseases
ICD-10-CM The 10th revision of the ICD
ICD-9-CM The 9th revision of the ICD
ICF Intermediate Care Facility
ICF-IID Intermediate Care Facility for Individuals with Intellectual Disabilities
ICN Item Control Number
IGT Intergovernmental Transfers
IHS Indian Health Service
IHS-BCC IHS-B
IHS-BIP IHS-B
IMD Institution for Mental Disease
INA Immigration and Nationality Act
IND Indicator
IP Inpatient
IPFPPS Inpatient Psychiatric Facility Prospective Payment System
IPPS Acute Inpatient Prospective Payment System
IRFPPS Inpatient Rehabilitation Facility Prospective Payment System
LN Line
LPN Licensed Practical Nurse
LPR Lawful permanent residents
LT Long Term
LTC Long Term Care
LTCHPPS Long Term Care Hospital Prospective Payment System
LTCLA Long Term Care Living Arrangement
LTSS Long Term Services and Support
MACPro Medicaid and CHIP Program Data System
MAGI Modified Adjusted Gross Income
MAS Maintenance Assistance Status
MBI Medicare Beneficiary Identifier
M-CHIP Medicaid Expansion CHIP
MCO Managed Care Organization
MCR Managed Care Record
MD Medical Doctor
MFP Money Follows the Person
MH Mental Health
MMA Medicare Modernization Act
MMIS Medicaid Management Information System
MOD Modifiers
MRI Magnetic resonance imaging
MS-DRG Medicare Severity – Diagnosis Related Group
MSIS Medicaid Statistical Information System
MSP Medicare Secondary Payer
NAIC National Association of Insurance Commissioners
NCPDP National Council for Prescription Drug Programs
NDC National Drug Code
NF Nursing Facility
NHP-ID National Health Plan Identifier
NPI National Provider ID
OASDI Old-Age, Survivors, and Disability Insurance
OEID Other Entity Identifier
OIG Office of Inspector General
OIS Office of Information Services
OMB Office of Management and Budget
OPPS Outpatient Prospective Payment System
ORF Other Rehabilitation Facility
OS Operating System
OT Other Type [of claim]
OTC Over the counter
PACE Program for All-Inclusive Care for the Elderly
PAHP Prepaid Ambulatory Health Plan
PBM Pharmacy Benefits Manager
PCCM Primary Care Case Management
PERS Personal Emergency Response System
PHP Prepaid Health Plan
PHS Public Health Service Act
PIHP Prepaid Inpatient Health Plan
PL Public Law
POA Present on Admission
POP Population
PPS Prospective Payment System
PROV Provider
PRTF Psychiatric Residential Treatment Facilities Demonstration Grant Program
PRWORA Personal Responsibility and Work Opportunity Reconciliation Act of 1996
PT/OT/ST Physical Therapy/Occupational Therapy/Speech Therapy
QDWI Qualified Disabled Working Individuals
QI Qualified Individual
QIO Quality Improvement Organization
QMB Qualified Medicare Beneficiaries
RA Remittance Advice
RBRVS Resource-based relative value scale
REC Record
RHC Rural health clinic
RN Registered Nurse
RRB Railroad Retirement Board
RX Prescription
SCHIP State Children’s Health Insurance Program
SHPID Sub-Health Plan Identifiers
SLMB Specified Low-Income Medicare Beneficiaries
SNF Skilled Nursing Facility
SNFPPS Skilled Nursing Facility Prospective Payment System
SPA State Plan Amendment
SSA Social Security Administration
SSDI Social Security Disability Insurance
SSI Supplemental Security Income
SSP State Supplemental Program
SSN Social Security Number
SUD Substance Use Disorders
T-18 SNF Title 18 Skilled Nursing Facility
TANF Temporary Assistance for Needy Families
TB Tuberculosis
TEFRA Tax Equity and Fiscal Responsibility Act of 1982
TIN Tax Identifier Number
T-MSIS Transformed Medicaid Statistical Information System
TOT Total
TPL Third Party Liability
TWWIIA Ticket to Work and Work Incentives Improvement Act
UB Uniform Billing
URAC Utilization Review Accreditation Commission
USC United States Code
VA Veterans Administration
[1][1] CMS will provide direction at a later date concerning resubmission of records that states are unable to correct.
[1][1] CMS will provide direction at a later date concerning resubmission of records that states are unable to correct.
[1][1] CMS will provide direction at a later date concerning resubmission of records that states are unable to correct.
[1][1] CMS will provide direction at a later date concerning resubmission of records that states are unable to correct.
[1][1] CMS will provide direction at a later date concerning resubmission of records that states are unable to correct.
1 CMS Guidance – Reporting Financial Transactions in T-MSIS – 2014-04-23
2 Business dates represent the date stored in a state’s systems that reflects when a data element value changed. Some states do not store business dates for certain data elements, sometimes because the dates would not affect claim adjudication. For example, if a beneficiary’s enrollment data were updated to correct their sex, the claims processing system will assume that this change should be applied to all claims, regardless of date of service or date of submission.
3 Seven fiscal years of history was selected so that T-MSIS will contain a minimum standard number of years of history across all states. (Note that the 7 years of history – from 1/1/2014 back to 10/1/2006 – is irrespective of the actual date when the state submits its first T-MSIS production file.) If a state has reliable data that go back into history farther than 10/1/2006 and would be willing to submit them, CMS will welcome them.
4 Archived records are those whose data element values are active but which the state considers to be permanently static. (Oftentimes, these records are no longer actively used in the state’s system and are moved to a separate data storage area for long-term retention.) For example, it is very unlikely that a state will receive a claim for a beneficiary that died more than seven years ago. The state might decide to “archive” that beneficiary’s record so that it is not part of the MMIS operational database anymore. After the record is archived, it would no longer be reported in the state’s T-MSIS file, but the record will be maintained in the underlying T-MSIS database.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| File Modified | 0000-00-00 |
| File Created | 0000-00-00 |
© 2026 OMB.report | Privacy Policy