Appendix.MCHBG to States Guidance.
(1) Updated OMB Change Request.Appendix.MCHBG to States Guidance.April_11_2017 Nora.docx
Maternal and Child Health Services Block Grant Application/Annual Report Guidance
Appendix.MCHBG to States Guidance.
OMB: 0915-0172

TITLE V MATERNAL AND CHILD HEALTH SERVICES BLOCK GRANT TO STATES PROGRAM
GUIDANCE AND FORMS
FOR THE
TITLE V APPLICATION/ANNUAL REPORT
APPENDIX OF SUPPORTING DOCUMENTS
U.S. Department of Health and Human Services
Health Resources and Services Administration
Maternal and Child Health Bureau
Division of State and Community Health
Room 5C-26
5600 Fishers Lane, Rockville, MD 20857
(Phone 301-443-2204 FAX 301-443-9354)
TABLE of CONTENTS
APPENDIX A: HISTORY AND ADMINISTRATIVE BACKGROUND 2
APPENDIX B: SAMPLE OF FIVE-YEAR STATE ACTION PLAN TABLE 7
APPENDIX C: ASSURANCES AND CERTIFICATIONS 9
APPENDIX D: NEEDS ASSESSMENT − BACKGROUND AND 12
CONCEPTUAL FRAMEWORK
APPENDIX E: PERFORMANCE MEASURE FRAMEWORK 17
APPENDIX F: DETAIL SHEETS FOR THE NATIONAL OUTCOME 29
MEASURES AND NATIONAL PERFORMANCE MEASURES
APPENDIX G: REQUIRED APPLICATION/ANNUAL REPORT COMPONENTS 91 AND TIMELINE
APPENDIX H: GLOSSARY 94
APPENDIX A: HISTORY AND ADMINISTRATIVE BACKGROUND
As one of the largest Federal block grant programs, Title V is a key source of support for promoting and improving the health of all the nation’s mothers and children. When Congress passed the Social Security Act in 1935, it contained the initial key landmark legislation which established Title V. This legislation is the origin of the federal government’s pledge of support to states and their efforts to extend and improve health and welfare services for mothers and children throughout the nation. To date, the Title V federal-state partnership continues to provide a dynamic program to improve the health of all mothers and children, including children with special health care needs (CSHCN.)
The Maternal and Child Health Bureau
The Maternal and Child Health Bureau (MCHB) is the principal focus within Health Resources and Services Administration (HRSA) for all Maternal and Child Health (MCH) activities within the Department of Health and Human Services (HHS). MCHB’s mission is to provide national leadership through working in partnership with states, communities, public/private partners, tribal entities and families to strengthen the MCH infrastructure, and to build knowledge and human resources. Its mission also includes ensuring continued improvement in the health, safety, and well-being of the MCH population. To achieve its mission, MCHB directs resources towards a combination of integrated public health services and coordinated systems of care for the MCH population.
Within the MCHB, the Division of State and Community Health (DSCH) has the administrative responsibility for the Title V MCH Block Grant to States Program. DSCH is committed to being the Bureau’s main line of communication with states and communities, in order to consult and work closely with both of these groups and others who have an interest in and contribute to the provision of a wide range of MCH programs and community-based service systems.
Maternal and Child Health Services Block Grant (Title V)
Under Title V, MCHB administers a Block Grant and competitive Discretionary Grants. The purpose of the Title V MCH Services Block Grant Program is to create federal/state partnerships in all 59 states for developing service systems that address MCH challenges, such as:
• Significantly reducing infant mortality;
• Providing comprehensive care for all women before, during, and after pregnancy and childbirth;
• Providing preventive and primary care services for infants, children, and adolescents;
• Providing comprehensive care for children and adolescents with special health care needs;
• Immunizing all children;
• Reducing adolescent pregnancy;
• Preventing injury and violence;
• Putting into community practice national standards and guidelines for prenatal care, for healthy and safe child care, and for the health supervision of infants, children, and adolescents;
• Assuring access to care for all mothers and children; and
• Meeting the nutritional and developmental needs of mothers, children and families.
Under Title V, MCHB also administers two types of Federal Discretionary Grants, Special Projects of Regional and National Significance (SPRANS) and Community Integrated Service Systems (CISS) grants. SPRANS funds projects (through grants, contracts, and other mechanisms) in research, training, genetic services and newborn screening/follow-up, sickle cell disease, hemophilia, and MCH improvement. CISS projects (through grants, contracts, and other mechanisms) seek to increase the capacity for service delivery at the local level and to foster formation of comprehensive, integrated, community level service systems for mothers and children.
In addition to SPRANS and CISS grants, the MCHB also administers the following categorical programs:
• Emergency Medical Services for Children;
• Traumatic Brain Injury;
• Healthy Start Initiative;
• Universal Newborn Hearing Screening;
• Autism; and
• Home Visiting Program
In recent years, some state Title V programs have begun to utilize the life course model as an organizing framework for addressing identified MCH needs. The life course approach points to broad social, economic, and environmental factors as underlying contributors to health and social outcomes. This approach also focuses on persistent inequalities in the health and well-being of individuals and how the interplay of risk and protective factors at critical points of time can influence an individual’s health across his/her lifespan and potentially across generations.
Maternal and Child Health Block Grant to States Program
Since its original authorization in 1935, Title V of the Social Security Act has been amended several times to reflect the increasing national interest in maternal and child health and well-being. One of the first changes occurred when Title V was converted to a block grant program as part of the Omnibus Budget Reconciliation Act (OBRA) of 1981. This change resulted in the consolidation of seven categorical programs into a single block grant. These programs included:
Maternal and Child Health and Services for Children with Special Health Care Needs (Title V of the Social Security Act);
Supplemental Security Income for children with disabilities (Section 1651(c) of the Social Security Act);
Lead-based paint poisoning prevention programs (Section 316 of the Public Health Service (PHS) Act);
Genetic disease programs (Section 101 of the PHS Act);
Sudden infant death syndrome programs (Section 1121 of the PHS Act);
Hemophilia treatment centers (Section 1131 of the PHS Act); and
Adolescent pregnancy grants (Public Law PL 95-626).
Another significant change in the Title V MCH Block Grant came as a result of the Omnibus Budget Reconciliation Act (OBRA) of 1989, which specified new requirements for accountability. The amendments enacted under OBRA introduced stricter requirements for the use of federal funds and for state planning and reporting. Congress sought to balance the flexibility of the block grant with greater accountability, by requiring State Title V programs to report their progress on key MCH indicators and other program information. Thus, the block grant legislation emphasizes accountability while providing states with appropriate flexibility to respond to state-specific MCH needs and to develop targeted interventions and solutions for addressing them. This theme of assisting states in the design and implementation of MCH programs to meet state and local needs, while at the same time asking them to account for the use of federal/state Title V funds, was embodied in the requirements contained in the Guidance documents for the state MCH Block Grant Applications/Annual Reports.
In 1993 the Government Performance and Results Act (GPRA), Public Law 103-62, required federal agencies to establish measurable goals that could be reported as part of the budgetary process. For the first time, funding decisions were linked directly with performance. Among its purposes, GPRA is intended to “...improve federal program effectiveness and public accountability by promoting a new focus on results, service quality, and customer satisfaction.” GPRA requires each federal agency to develop comprehensive strategic plans, annual performance plans with measurable goals and objectives, and annual reports on actual performance compared to performance goals. The MCHB effort to respond to GPRA requirements coincided with other planned improvements to the MCH Block Grant Guidance. As a result, the MCH Block Grant Application/Annual Report and forms contained in the 1997 edition of the Maternal and Child Health Services Title V Block Grant Program - Guidance and Forms for the Title V Application/Annual Report served to ensure that the states and jurisdictions could clearly, concisely, and accurately tell their MCH “stories.” This Application/Annual Report became the basis by which MCHB met its GPRA reporting requirements for the MCH Block Grant to States Program.
In 1996, the MCHB began a process of programmatic assessments and planning activities aimed at improving the Title V MCH Block Grant Application/Annual Report Guidance document for states. Since that time, the Maternal and Child Health Services Title V Block Grant Program - Guidance and Forms for the Title V Application/Annual Report (Guidance) has been revised, submitted to and approved by the Office of Management and Budget (OMB) six times. Revisions to each subsequent edition were based on changes in MCH priorities, availability of new national data sources and continuing efforts to refine and streamline the Application/Annual Report preparation and submission process for states. The reduced burden that resulted from this latter commitment was largely achieved through efficiencies that were created by the electronic reporting vehicle for the state MCH Block Grant Applications/Annual Reports, specifically the Title V Information System (TVIS.)
Title V Information System
The development of an electronic reporting package in 1996 was a significant milestone for the Title V MCH Block Grant to States Program. Advances in technology allowed for the development of an electronic information system (TVIS) within the next several years. The TVIS is designed to capture the performance data and other program and financial information contained in the state Applications/Annual Reports. While descriptive information is available on state Title V-supported efforts, state MCH partnership efforts and other program-specific initiatives of the state in meeting its MCH needs, TVIS primarily serves as an online, Web-accessible interface for the submission of the 59 state and jurisdictional Title V MCH Block Grant Applications/Annual Reports each year on July 15th. Developed in conjunction with the program requirements outlined in the Title V MCH Block Grant Application/Annual Report Guidance, the TVIS is available to the public on the World Wide Web at: https://mchdata.hrsa.gov/TVISReports/. Over the years, the TVIS has increasingly become recognized as a powerful and useful tool for a number of audiences. The transformational changes to the Title V MCH Block Grant to States Program outlined in this revised Application/Annual Report Guidance mandate the development of a new data collection and web report system for the TVIS. HRSA is providing funding support for a contract to develop, implement and operate this new information system.
Integrated with HRSA’s grants management system (i.e., the HRSA Electronic Handbooks (EHB),) the TVIS makes available to the public through its web reports the key financial, program, performance, and health indicator data reported by states in their yearly MCH Block Grant Applications/Annual Reports. Examples of the data that are collected include information on populations served; budget and expenditure breakdowns by source of funding, service and program; program data, such as individuals served and breakdowns of MCH populations by race/ethnicity, other state data (OSD), and performance and outcome measure data for the national and state measures. Reporting on performance relative to the national measures is used to assess national progress in key MCH priority areas and to facilitate the Bureau’s annual GPRA reporting.
APPENDIX B: SAMPLE OF FIVE-YEAR STATE ACTION PLAN TABLE
States will prepare a Five-year State Action Plan Table in follow-up to the Five-Year Needs Assessment and submit an interim State Action Plan Table as part of the first year Title V MCH Block Grant Application/Annual Report. (Note: States will refine the interim State Action Plan Table in the second year Application/Annual Report by further clarifying the identified objectives and strategies and by adding the Evidence-based or –informed Strategy Measures (ESMs) and the State Performance Measures (SPMs).) The following sample is provided to help guide states in understanding the types of information that they should include in their Five-year Action Plan Table. States can use a different tabular form for presenting similar information in the Five-year State Action Plan Table that they prepare.
The Five-year State Action Plan Table is intended to serve as a working tool for states in developing an Action Plan that addresses the state and national MCH priorities identified through the Five-year Needs Assessment process. While there is no required format for the Five-year State Action Plan Table, the information contained must be clearly presented, organized by population health domain, link the state priority needs to the defined priority needs/strategies and serve to inform the selection/development of the NOMs, NPMs, SPMs and ESMs.
As the organizational framework, states will utilize the Five-year State Action Plan Table in developing a five-year State Action Plan. States should review the Table annually and provide updates, as needed, in preparing each year’s Application/Annual Report. In the narrative State Action Plan (i.e., Application/Annual Report), states will report annually on their planned activities for the coming year and on the activities they implemented in the reporting year; their planned efforts for improving performance and analyses of current performance trends relative to the NOMs, NPMs, SPMs and ESMs; and their progress/achievements in addressing their identified priority needs through the implementation of strategies defined in their Five-year State Action Plan Table.
Five-Year State Action Plan Table – SAMPLE
Domains |
State Priority Needs |
Objectives |
Strategies |
National Outcome Measures* |
National Performance Measures* |
Evidence-Based or –Informed Strategy Measures |
State Performance Measures |
Women/ Maternal Health |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Perinatal/ Infant Health |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Child Health |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CSHCN |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Adolescent Health |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Cross-Cutting or Life Course |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Other
|
|
|
|
|
|
|
|
* Data to be provided by MCHB
APPENDIX C: ASSURANCES AND CERTIFICATIONS


Standard Form 4248 (Rev. 7-97) Back
APPENDIX D: |
NEEDS ASSESSMENT − BACKGROUND AND CONCEPTUAL FRAMEWORK
|
Needs Assessment is a systematic process to acquire an accurate, thorough picture of the strengths and weaknesses of a state’s public health system that can be used in response to the preventive and primary care services needs for ALL pregnant women, mothers, infants (up to age one), children including children with special health care needs [Section 505 (a)(1)]. The Needs Assessment process includes the collection and examination of information about the state’s capacity and infrastructure, needs and desired outcomes for the MCH population, and legislative mandates, etc. This information is utilized to determine priority goals, develop a plan of action, and to allocate funds and resources. The Needs Assessment is a collaborative process that should include the HRSA/MCHB, the state Department of Health, families, practitioners, the community, and other agencies and organizations within each state and jurisdiction that have an interest in the wellbeing of the MCH population.
Title V of the Social Security Act requires states to conduct a statewide Needs Assessment every five years. States will report on the next Five-year Needs Assessment in calendar year 2015 as part of the FY 2016 MCH Block Grant Application process. Rather than submitting a comprehensive “stand-alone document, as in previous years, states will submit a Five-year Needs Assessment Summary that concisely describes the process and findings. As the Needs Assessment document may serve multiple purposes, a state may wish to develop a more comprehensive document to meets its broader needs. This document cannot be submitted in place of the required Five-year Needs Assessment Summary, but states may include a URL, if the document is posted online, in the Five-year Needs Assessment Summary or they may submit the document as an attachment to the Application/Annual Report in the electronic application system. Over the five-year reporting period, states are encouraged to continuously revisit the Five-Year Needs Assessment Summary and to provide updates, as needed, in the interim year Applications/Annual Reports. Furthermore, it is expected that states will have ongoing communication with stakeholders and partners throughout the Needs Assessment process and continue to engage with such partners during the interim reporting years.
The following figure illustrates the continuity of the Needs Assessment process and its relationship to the planning and monitoring functions of Title V and the population that it serves. The primary goal of the statewide Needs Assessment is to improve MCH outcomes and to strengthen its state, local and community partnerships for addressing the needs of its MCH population. A brief description of the steps involved in the Needs Assessment process is presented in the following sections.
Engage Stakeholders
As depicted, the starting point for the Needs Assessment process is to engage stakeholders. Engaging stakeholders and strengthening partnerships is a continuous and on-going activity. The state needs strong partnerships with its stakeholders throughout the Needs Assessment process. Effective coalitions can help the state to realistically assess needs and identify desired outcomes and mandates, assess strengths and examine capacity, select priorities, seek resources, set performance objectives, develop an action plan, allocate resources, and monitor progress for impact on targeted outcomes.
State Title V MCH Program Needs Assessment, Planning, Implementation and Monitoring Process
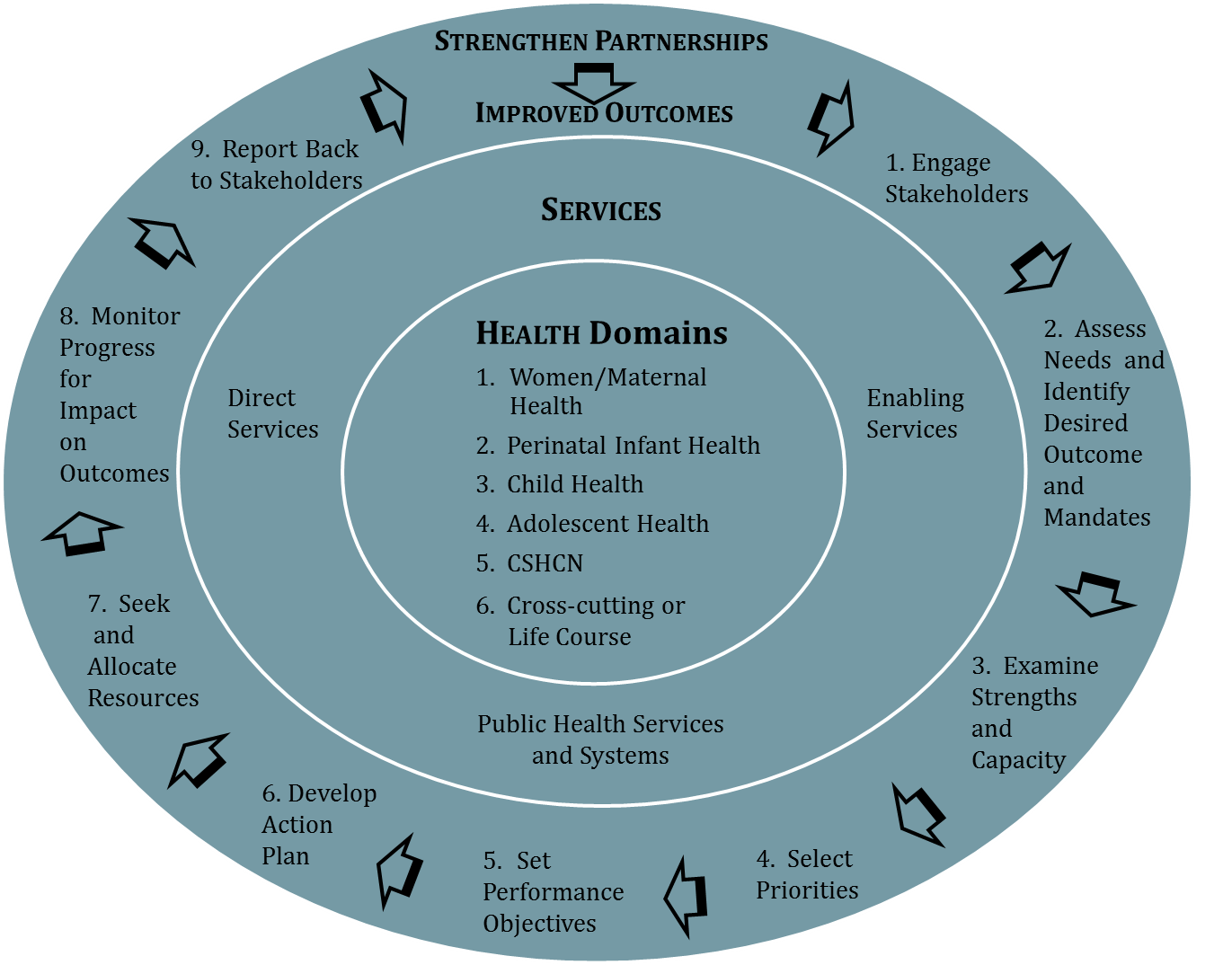
Assess Needs and Identify Desired Outcomes and Mandates
The second stage in the process is to assess needs of the MCH population groups using the Title V National Outcome Measures (NOMs), national, state and strategy performance measures and other available state-level quantitative and qualitative data. States should assess MCH population needs based on the following six population health domains: 1) Women/Maternal Health; 2) Perinatal/Infant Health; 3) Child Health; 4) Adolescent Health; 5) Children with Special Health Care Needs (CSHCN); and 6) Cross-cutting or Life Course. These population health domains fall with the three MCH population groups that are defined in Section 505(a)(1) of the Title V legislation. The anticipated outcome of this assessment is to identify community/system needs and desired outcomes by specific MCH population groups. In addition, the state will need to identify legislative, political, community-driven, financial, and/or other internal and external mandates which may go beyond the findings identified through the Needs Assessment process but are priorities for implementation within the state.
Examine Strengths and Capacity
The third stage in the Needs Assessment process is examining strengths and capacity. This stage involves examining the State’s capacity to engage in various activities, including conducting the statewide Five-year Needs Assessment and collecting/reporting annual performance data based on the six identified MCH population health domains and the types of MCH services provided. The working framework for MCH services is presented in Figure 1 of Part One, Section II of the Title V MCH Block Grant to States Application/Annual Report Guidance.
This stage involves describing and assessing the state’s current resources, activities, and services as well as the state’s ability to continue to provide quality services by each of the three MCH service levels. These levels include 1) Direct Services; 2) Enabling Services; and 3) Public Health Services and Systems. The anticipated outcome is a better understanding of the relationship of the state’s existing program/system capacity to its identified strengths and needs. This examination may reveal strengths and weaknesses in capacity not previously identified.
Select Priorities
In the select priorities stage, each state examines the identified needs and matches them to the desired outcomes, required mandates and level of existing capacity. As a result, states will select seven to ten priority areas for targeted focus in promoting continued improvement and progress. Examples of inputs include: the Needs Assessment process, the opinions of stakeholders, the examination of program capacity and the political priorities within the State. The anticipated outcome is the development of a set of priority needs (between seven and ten), which are unique to the individual state based on its Needs Assessment findings. Priorities identified should address areas in which the state believes there is reasonable opportunity for a focused programmatic effort (e.g., new or enhanced interventions, initiatives, or systems of care) to lead to an improved outcome.
Set Performance Objectives
Setting performance objectives consists of two phases. In the first phase, each state will develop action strategies to address their identified priority needs. Based on the priority needs and program strategies developed, the state will select eight National Performance Measures (NPMs) as part of its interim Five-year Action Plan. States will also give consideration to the potential Evidence-based or –informed Strategy Measures (ESMs) for addressing the selected NPMs and the three to five State Performance Measures (SPMs) that will be developed in Application Year 02. The SPMs should be based on the state’s identified MCH priorities and target those priority needs that are not fully addressed by the selected NPMs and their related ESMs.
Secondly, the state will set five-year targets (i.e., performance objectives) for the eight selected NPMs in Application Year 01. In Application Year 02, the state will develop five-year performance targets for the ESMs and the SPMs. The anticipated results of this stage are the identification of NOMs, NPMs, SPMs and, ultimately, ESMs that directly relate to the State priorities and establish a level of accountability for achieving measureable progress.
Develop an Action Plan
The next stage is to develop an action plan, which involves the planning and identification of specific activities for implementing the program strategies which were developed in Stage 5 to address the identified priority needs and selected national/state measures. In developing an Action Plan, states will create the Five-year State Action Plan Table described in Appendix B. As a planning tool, states will have flexibility in how they format the Table provided that the information is organized around the six identified population health domains. At a minimum, the Five-year State Action Plan Table should include the relevant priority needs, key strategies and measures (i.e., NOMs, NPMs, SPMs and ESMs) for each of the population health domains. Based on the identified priorities, measures and strategies, the state will develop a five-year program plan that includes specific activities for achieving the targeted outcomes and performance specific to each population health domain.
In developing the Action Plan, the state shall complete an interim Five-year State Action Plan Table (see sample in Appendix B) as part of the first year Application/ Annual Report (i.e., FY 2016/FY 2014). This Table is a tool to assist states in aligning their program strategies, NPMs, SPMs and ESMs with the priority needs that were identified in the Five-year Needs Assessment. States will refine the objectives and strategies and add the ESMs for the selected NPMs and the SPMs to the Five-year Action Plan Table in the second year Application/Annual Report (i.e., FY 2017/FY 2015). Updates to the strategies and activities will be provided by the state, as needed, in subsequent interim year Applications/Annual Reports. Figure 3 in Part Two, Section II.F of the Application/Annual Report Guidance depicts the steps involved in the development of, and the annual reporting on, the implementation of the Five-year State Action Plan.
Seek and Allocate Resources
Following the identification of program activities is the allocation of resources stage. In this stage, the focus is on the funding of planned activities to address state priorities. Inputs include the five-year State Action Plan, current budgets, political priorities, and partnerships. The anticipated outcome is the development of a program budget and plan that directs available resources towards the activities identified in Stage Six as the most important for addressing the state's priorities.
Monitor Progress for Impact on Outcomes
In monitoring progress for impact on outcomes, the states examine the results of their efforts to see if there has been improvement. Inputs include NOMs, NPMs, SPMs and ESMs, performance objectives and other quantitative and qualitative information. Potential outcomes may include altered activities and shifting of resource allocations to address current levels of performance and availability of resources. Feedback loops between various stages of the process allow for continuous input and re-evaluation of the outputs.
Report Back to Stakeholders
This final step assures accountability to the stakeholders and partners who have worked with the MCH staff throughout the Needs Assessment process. It also assures the continued involvement of all stakeholders and partners in the ongoing Needs Assessment processes.
APPENDIX E: PERFORMANCE MEASURE FRAMEWORK
Overview of the Framework
The performance measure framework is based on a three-tiered performance measure system: National Outcome Measures (NOMs), National Performance Measures (NPMs), and Evidence-based or -informed Strategy Measures (ESMs).
Measures were considered as NOMs, which are reflective of population health status, if they met one or more of the following criteria: it was mandated by the Title V legislation that the data be collected; it was considered a sentinel health marker for women, infants, or children; it was a major focus of either the Title V legislation or Title V activities; it was considered an important health condition to monitor because the prevalence was increasing, but the reasons for the increase were unclear; or there was a recognized need to move the MCH field forward in this area, even if there was not yet a consensus on how to measure the construct. The latter were considered developmental outcome measures.
Measures were considered as NPMs if they met one or more of the following criteria: there was a large investment of resources as determined by the State narratives; it was considered modifiable through Title V activities; a state could delineate measurable activities to address the performance measures; significant disparities existed among population groups; research had indicated that the condition or activity had large societal costs; or research had indicated that the promotion of certain behaviors, practices or policies had improved outcomes. There also had to be evidence that an NPM was associated with at least one of the NOMs (see Table 2). Fifteen NPMs were identified for the Title V MCH Services Block Grant. Data for NOMs and NPMs will be populated by MCHB from national data sources, as available. NPMs will be stratified by different risk factors, when available. See Table 3 for planned stratifiers.
The ESMs are the key to understanding how a State Title V program tracks programmatic investments designed to impact the NPMs. In the framework, States create ESMs designed to impact the NPMs. These measures would assess the impact of State Title V strategies and activities contained in the State Action Plan. The development of ESMs is guided through an examination of the evidenced-based or evidence-informed practices on what strategies and activities are both practical and measurable. The main criteria for ESMs would be that the activities had to measurable, and there had to be evidence that the activity was related to the NPM chosen. States Can determine the number of ESMs that they will use for addressing the selected NPMs but there is a required minimum of one ESM for each NPM. States may also retire an ESM during the five-year reporting cycle, if it has successfully achieved its objective toward the NPM or new ESMs are introduced measuring new, promising practices.
Fifteen NPMs were identified for the Title V MCH Services Block Grant, covering six population domains: Women/Maternal Health, Perinatal/Infant Health, Child Health, Adolescent Health, Children with Special Health Care Needs, and Cross-cutting or Life Course. In the table below are the 15 national priority areas addressed by the NPMs and the corresponding MCH Population domain(s).
Table 1. NPMs and MCH Population Domains
NPM # |
National Performance Priority Areas |
MCH Population Domains |
1 |
Well-woman visit |
Women/Maternal Health |
2 |
Low-risk cesarean delivery |
Women/Maternal Health |
3 |
Perinatal regionalization |
Perinatal/Infant Health |
4 |
Breastfeeding |
Perinatal/Infant Health |
5 |
Safe sleep |
Perinatal/Infant Health |
6 |
Developmental screening |
Child Health |
7 |
Injury |
Child Health and/or Adolescent Health |
8 |
Physical activity |
Child Health and/or Adolescent Health |
9 |
Bullying |
Adolescent Health |
10 |
Adolescent well-visit |
Adolescent Health |
11 |
Medical home |
Children with Special Health Care Needs |
12 |
Transition |
Children with Special Health Care Needs |
13 |
Oral health |
Cross-cutting/Life course |
14 |
Smoking |
Cross-cutting/Life course |
15 |
Adequate insurance coverage |
Cross-cutting/Life course |
In implementing this framework, states will choose eight (8) out of 15 NPMS for its Title V program to address during the five-year needs assessment cycle. States shall ensure that at least one NPM from each of the six MCH Population domains is selected and that the selected NPMs are based on the findings of the Five-Year Needs Assessment process. There are no mandatory NPMs. For the NPMs on injury and physical activity, they can be selected for either the children’s or the adolescent domains or both because the age ranges span both domains, but the interventions to either reduce injuries or increase physical activity are different, depending on the children’s ages.
Implementation of Measurement
National Outcome Measures
NOMs are for population health assessment which is an important core function of public health. They should be tracked to understand the MCH population’s health, and are important for the development of the needs assessment. Changes in NOM indicators can be discussed in the appropriate population domain section of the narrative but there is not a reporting requirement for this discussion. Data for NOMs will be prepopulated, where possible. States do not provide performance objectives for NOMs.
National Performance Measures
Once NPMs are selected, a state will track the eight NPMs throughout the five-year reporting cycle. States are encouraged not to change the selected NPMs during the five-year reporting cycle. If a state determines that a NPM needs to be changed, clear justification must be provided. In an effort to reduce state burden, annual performance data (indicator/numerator/denominator) for the NOMs and the NPMs will be pre-populated by MCHB from national data sources, as available, and provided to the states for their use in preparing the yearly Title V MCH Block Grant Applications/Annual Reports. If a state selects a NPM for which it is not part of the national data source, the state can develop its own detail sheet and report its data for the measure. However, the definition and data that are collected must match the definition and measure of the national data source.
In the first reporting year of this guidance, a State selects its NPMs and determines performance objectives for FY 2016-2020 for the NPMs. Performance objectives for future years can be changed for individual NPMs based on ongoing needs assessment efforts and performance monitoring.
Other Guidelines for NPMs
Use of Provisional Data: States may, but are not required to, include more timely provisional data if they choose. This will not replace the prepopulated final data provided for the measures.
Lacking a National Data Source: States can choose a measure if they do not have the data source noted on the detail sheet, as long as they provide the indicator, numerator and denominator data as defined on the detail sheet. As for PRAMS, States will be able to submit their PRAMS or PRAMS-like data to TVIS following the same definition for a given measure if CDC cannot furnish it. The same situation may apply to other data sources; for example, not all states with hospital discharge data furnish it to AHRQ. If a state provides its own data from a different source, this should be annotated in a field note.
Integrated Measures: For integrated measures, states can choose a NPM even if they do not have the data from both data sources. Both measures will be reported for these types of measures. Where there are data for both sources, data will be displayed and would need to be discussed for both populations. If only one data source is available, that population will need to be addressed. States will develop an ESM to address each of the strategies developed for the measure.
Evidence-based or -informed Strategy Measures
Developed by the State, Evidence-based or -informed Strategy Measures would assess the impact of State Title V strategies and activities contained in the State Action Plan. It is envisioned that the development of the ESMs will be guided through an examination of the evidenced-based or evidence-informed practices on what strategies and activities are both practical and measurable. The main criteria for the state ESMs would be that the strategies and activities have to be measurable, and there has to be evidence that the activity is related to the performance measure chosen. Most issues in MCH are multifactorial, therefore, while states are strongly encouraged to develop multiple strategies with a related ESM for each strategy to impact a selected NPM, states are required to submit at least one ESM for each of the NPMs selected.
In the second reporting year (FY 2017 Application/FY 2015 Annual Report), states will develop a detail sheet for each ESM, which they will submit as part of the FY 2017 Application/FY 2015 Annual Report. On the detail sheet, states will define the: (1) measures; (2) goal; (3) indicator, numerator, and denominator; (4) data source; and (5) significance. Beginning with the third reporting year (FY 2018 Application/FY 2016 Annual Report), states will track performance for the ESMs that were established for this five-year needs assessment cycle. States will determine performance objectives for each of the ESMs for application years FY 2018-FY 2020. These objectives can be revised, as needed, for future reporting years. Data for the ESMs (i.e., numerator/denominator) will be entered annually by the state. During the five-year reporting cycle, the ESMs may be modified, replaced, or retired, based on analysis of the effectiveness of the strategy or the validity of the measure.
State Performance and Outcome Measures
To address state priorities not addressed by the National Performance Measures, the State Performance Measures (SPMs) will be developed as part of the second reporting year Application/Annual Report (i.e., FY 2017 Application/FY 2015 Annual Report), and states will establish performance objectives for five years FY 2018-FY 2022) for each of the measures. States may revise their SPM objectives in future years’ Applications/Annual Reports. The development of the SPMs coincides with the development of the state ESMs.
States will also develop detail sheets on these measures, which will define the: (1) measure; (2) goal; (3) indicator, numerator, and denominator; (4) data source; and (5) significance. States will track their three to five SPMs throughout the five-year reporting cycle. Data for the SPMs (i.e., indicator/numerator/denominator) will be entered annually by the state. A state can retire a SPM during the five-year reporting cycle and replace it with another SPM based on its MCH priority needs. States are not required to develop ESMs for SPMs.
A state may also develop (but is not required to develop) one or more State Outcome Measures (SOMs) based on its MCH priorities, as determined by the findings of the Five-Year Needs Assessment, provided that none of the NOMs address the same priority area for the state. A SOM should be linked with a performance measure to show the impact of performance on the intended outcome. States will track the SOMs during the five-year reporting cycle and the SOM can be retired if the state chooses. Data for the SOMs (i.e., indicator/numerator/ denominator) will be entered annually by the state.
Table 2. National Outcome Measures - National Performance Measures Linkage
NPM # |
National Performance Measure (NPM) |
National Outcome Measures Associated with National Performance Measure |
1 |
Well-woman visit (Percent of women with a past year preventive medical visit) |
Severe maternal morbidity per 10,000 delivery hospitalizations Maternal mortality rate per 100,000 live births Low birth weight rate (%) Very low birth weight rate (%) Moderately low birth weight rate (%) Preterm birth rate (%) Early preterm birth rate (%) Late preterm birth rate (%) Early term birth rate (%) Infant mortality per 1,000 live births Perinatal mortality per 1,000 live births plus fetal deaths Neonatal mortality per 1,000 live births Postneonatal mortality rate per 1,000 live births Preterm-related mortality per 100,000 live births |
2 |
Low risk cesarean deliveries (Percent of cesarean deliveries among low-risk first births) |
Severe maternal morbidity per 10,000 delivery hospitalizations Maternal mortality rate per 100,000 live births |
3 |
Perinatal regionalization (Percent of very low birth weight (VLBW) infants born in a hospital with a Level III+ Neonatal Intensive Care Unit (NICU)) |
Infant mortality per 1,000 live births Perinatal mortality per 1,000 live births plus fetal deaths Neonatal mortality per 1,000 live births Preterm-related mortality per 100,000 live births |
4 |
Breastfeeding (A. Percent of infants who are ever breastfed and B. Percent of infants breastfed exclusively through 6 months) |
Infant mortality rate per 1,000 live births Postneonatal mortality rate per 1,000 live births Sleep-related SUID per 100,000 live births |
5 |
Safe sleep (Percent of infants placed to sleep on their backs) |
Infant mortality per 1,000 live births Post neonatal mortality per 1,000 live births Sleep-related SUID per 100,000 live births |
6 |
Developmental screening (Percent of children, ages 10 through 71 months, receiving a developmental screening using a parent-completed screening tool) |
Percent of children in excellent or very good health Percent of children meeting the criteria developed for school readiness |
7 |
Child Injury (Rate of hospitalization for non-fatal injury per 100,000 children ages 0 through 9 and adolescents ages 10 through 19 |
Child mortality ages 1 through 9 per 100,000 Adolescent mortality ages 10 through 19 per 100,000 Adolescent motor vehicle mortality ages 15 through 19 per 100,000 Adolescent suicide ages 15 through 19 per 100,000 |
8 |
Physical activity (Percent of children ages 6 through 11 and adolescents ages 12 through 17 who are physically active at least 60 minutes per day) |
Percent of children in excellent or very good health Percent of children and adolescents who are overweight or obese (BMI at or above the 85th percentile) |
9 |
Bullying (Percent of adolescents, 12 through 17, who are bullied or who bully others) |
Adolescent mortality ages 10 through 19 per 100,000 Adolescent suicide ages 15 through 19 per 100,000 |
10 |
Adolescent well-visit (Percent of adolescents, ages 12 through 17, with a preventive medical visit in the past year) |
Percent of children in excellent or very good health Percent of children ages 6 months through 17 years who are vaccinated annually against seasonal influenza Percent of adolescents, ages 13 through 17, who have received at least one dose of the HPV vaccine Percent of adolescents, ages 13 through 17, who have received at least one dose of the Tdap vaccine Percent of adolescents, ages 13 through 17, who have received at least one dose of the meningococcal conjugate vaccine Adolescent mortality ages 10 through 19 per 100,000 Adolescent motor vehicle mortality ages 15 through 19 per 100,000 Adolescent suicide ages 15 through 19 per 100,000 Percent of children with mental/behavioral health condition who receive treatment or counseling Percent of adolescents who are overweight or obese (BMI at or above the 85th percentile) Severe maternal morbidity per 10,000 delivery hospitalizations Maternal mortality rate per 100,000 live births Low birth weight rate (%) Very low birth weight rate (%) Moderately low birth weight rate (%) Preterm birth rate (%) Early preterm birth rate (%) Late preterm birth rate (%) Early term birth rate (%) Infant mortality per 1,000 live births Perinatal mortality per 1,000 live births plus fetal deaths Neonatal mortality per 1,000 live births Postneonatal mortality rate per 1,000 live births Preterm-related mortality per 100,000 live births |
11 |
Medical home (Percent of children with and without special health care needs having a medical home) |
Percent of children with special health care needs (CSHCN) receiving care in a well-functioning system Percent of children in excellent or very good health Percent of children ages 19 through 35 months, who have received the 4:3:1:3(4):3:1 :4 combined series of routine vaccinations Percent of children, ages 6 months through 17 years, who are vaccinated annually against seasonal influenza Percent of adolescents, ages 13 through 17, who have received at least one dose of the HPV vaccine Percent of adolescents, ages 13 through 17, who have received at least one dose of the Tdap vaccine Percent of adolescents, ages 13 through 17, who have received at least one dose of the meningococcal conjugate vaccine |
12 |
Transition (Percent of adolescents with and without special health care needs who received services necessary to make transitions to adult health care) |
Percent of children with special health care needs (CSHCN) receiving care in a well-functioning system Percent of children in excellent or very good health |
13 |
Oral health (A. Percent of women who had a dental visit during pregnancy and B. Percent of children, ages 1 through 17, who had a preventive dental visit in the past year) |
Percent of children in excellent or very good health Percent of children ages 1 through 17 who have decayed teeth or cavities in the past 12 months |
14 |
Smoking during Pregnancy and Household Smoking (A. Percent of women who smoke during pregnancy and B. Percent of children who live in households where someone smokes) |
Severe maternal morbidity per 10,000 delivery hospitalizations Maternal mortality rate per 100,000 live births Low birth weight rate (%) Very low birth weight rate (%) Moderately low birth weight rate (%) Preterm birth rate (%) Early preterm birth rate (%) Late preterm birth rate (%) Early term birth rate (%) Infant mortality per 1,000 live births Perinatal mortality per 1,000 live births plus fetal deaths Neonatal mortality per 1,000 live births Preterm-related mortality per 100,000 live births Post neonatal mortality per 1,000 live births Sleep-related SUID per 100,000 live births Percent of children in excellent or very good health |
15
|
Adequate insurance coverage (Percent of children ages 0 through 17 who are adequately insured) |
Percent of children without health insurance Systems of care for children with special health care needs (Percent of children and youth with special health care needs (CYSHCN) receiving care in a well-functioning system) |
Table 3. Stratifiers for National Performance Measures
No. |
Title |
Planned Stratifiers |
1 |
Percent of women with a past year preventive medical visit |
Age |
2 |
Percent of cesarean deliveries among low-risk first births |
Age |
3 |
Percent of very low birth weight (VLBW) infants born in a hospital with a Level III+ Neonatal Intensive Care Unit (NICU) |
Age |
4 |
A) Percent of infants who are ever breastfed and B) Percent of infants breastfed exclusively through 6 months |
Sex
|
5 |
Percent of infants placed to sleep on their backs |
Age |
6 |
Percent of children, ages 10 through 71 months, receiving a developmental screening using a parent-completed screening tool |
Age |
7 |
Rate of hospitalization for non-fatal injury per 100,000 children ages 0 through 9 and adolescents ages 10 through 19 |
Age |
8 |
Percent of children ages 6 through 11 years and adolescents ages 12 through 17 years who are physically active at least 60 minutes per day |
YRBSS:
|
9 |
Percent of adolescents, ages 12 through 17 years, who are bullied or bully others |
YRBSS: Sex
NSCH: Age |
10 |
Percent of adolescents, ages 12 through 17, with a preventive medical visit in the past year |
Age
|
11 |
Percent of children with and without special health care needs having a medical home |
Age
|
12 |
Percent of adolescents with and without special health care needs who received services necessary to make transitions to adult health care |
Age
|
13 |
A) Percent of women who had a dental visit during pregnancy and B) Percent of children, ages 1 through 17 years, who had a preventive dental visit in the last year |
PRAMS: |
14 |
A) Percent of women who smoke during pregnancy and B) Percent of children who live in households where someone smokes |
Vitals: Age Race/ethnicity Nativity Education Insurance Marital status Quarter of the year Metro/non-metro
NSCH: Age |
15 |
Percent of children 0 through 17 years who are adequately insured |
Age
|
APPENDIX F: |
DETAIL SHEETS FOR THE NATIONAL OUTCOME MEASURES AND NATIONAL PERFORMANCE MEASURES |
National Outcome Measures
National Performance Measures
A.
NOM # |
National Outcome Measure |
1 |
Percent of pregnant women who receive prenatal care beginning in the first trimester |
2 |
Rate of severe maternal morbidity per 10,000 delivery hospitalizations |
3 |
Maternal mortality rate per 100,000 live births |
4.1 |
Percent of low birth weight deliveries (<2,500 grams) |
4.2 |
Percent of very low birth weight deliveries (<1,500 grams) |
4.3 |
Percent of moderately low birth weight deliveries (1,500-2,499 grams) |
5.1 |
Percent of preterm births (<37 weeks gestation) |
5.2 |
Percent of early preterm births (<34 weeks gestation) |
5.3 |
Percent of late preterm births (34-36 weeks gestation) |
6 |
Percent of early term births (37,38 weeks gestation) |
7 |
Percent of non-medically indicated early elective deliveries |
8 |
Perinatal mortality rate per 1,000 live births plus fetal deaths |
9.1 |
Infant mortality rate per 1,000 live births |
9.2 |
Neonatal mortality rate per 1,000 live births |
9.3 |
Postneonatal mortality rate per 1,000 live births |
9.4 |
Preterm-related mortality rate per 100,000 live births |
9.5 |
Sleep-related Sudden Unexpected Infant Death (SUID) rate per 100,000 live births |
10 |
Percent of infants born with fetal alcohol exposure in the last 3 months of pregnancy |
11 |
The rate of infants born with neonatal abstinence syndrome per 1,000 delivery hospitalizations |
12 |
Percent of eligible newborns screened for heritable disorders with on time physician notification for out of range screens who are followed up in a timely manner. (DEVELOPMENTAL) |
13 |
Percent of children meeting the criteria developed for school readiness (DEVELOPMENTAL) |
14 |
Percent of children ages 1 through 17 who have decayed teeth or cavities in the past 12 months |
15 |
Child mortality rate ages 1 through 9 per 100,000 |
16.1 |
Adolescent mortality rate ages 10 through 19 per 100,000 |
16.2 |
Adolescent motor vehicle mortality rate ages 15 through 19 per 100,000 |
16.3 |
Adolescent suicide rate ages 15 through 19 per 100,000 |
17.1 |
Percent of children with special health care needs |
17.2 |
Percent of children with special health care needs (CSHCN) receiving care in a well-functioning system |
17.3 |
Percent of children diagnosed with an autism spectrum disorder |
17.4 |
Percent of children diagnosed with Attention Deficit Disorder/Attention Deficit Hyperactivity Disorder (ADD/ADHD) |
18 |
Percent of children with a mental/behavioral condition who receive treatment or counseling |
19 |
Percent of children in excellent or very good health |
20 |
Percent of children and adolescents who are overweight or obese (BMI at or above the 85th percentile) |
21 |
Percent of children without health insurance |
22.1 |
Percent of children ages 19 through 35 months, who have received the 4:3:1:3(4):3:1 :4 series of routine vaccinations |
22.2 |
Percent of children 6 months through 17 years who are vaccinated annually against seasonal influenza |
22.3 |
Percent of adolescents, ages 13 through 17, who have received at least one dose of the HPV vaccine |
22.4 |
Percent of adolescents, ages 13 through 17, who have received at least one dose of the Tdap vaccine |
22.5 |
Percent of adolescents, ages 13 through 17, who have received at least one dose of the meningococcal conjugate vaccine |
OUTCOME MEASURE 1 |
Percent of pregnant women who receive prenatal care beginning in the first trimester |

GOAL |
To ensure early entrance into prenatal care to enhance pregnancy outcomes. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of live births with reported first prenatal visit during the first trimester (before 13 weeks’ gestation) in the calendar year |
|
|
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) 10.1. Increase the proportion of pregnant women who receive prenatal care beginning in the first trimester. (Baseline: 70.8 % of females delivering a live birth received prenatal care beginning in the first trimester in 2007, Target: 77.9%)
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
Early identification of maternal disease and risks for complications of pregnancy or birth are the primary reason for first trimester entry into prenatal care. This can help ensure that women with complex problems and women with chronic illness or other risks are seen by specialists. Early high-quality prenatal care is critical to improving pregnancy outcomes. |
|
OUTCOME MEASURE 2 |
Rate of severe maternal morbidity per 10,000 delivery hospitalizations |

GOAL |
To reduce life-threatening maternal illness and complications. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of deliveries hospitalizations with an indication of severe morbidity from ICD-10 diagnosis or procedure codes (e.g. heart or kidney failure, stroke, embolism, hemorrhage). |
|
|
|
|
|
Denominator: |
|
|
Number of delivery hospitalizations |
|
|
|
|
|
Units: 10,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) 5. Reduce the rate of maternal mortality. (Baseline:12.7 maternal deaths per 100,000 live births in 2007, Target: 11.4 maternal deaths per 100,000 live births)
Related to Maternal, Infant, and Child Health (MICH) 6. Reduce maternal illness and complications due to pregnancy (complications during hospitalized labor and delivery) . (Baseline: 31.1%, Target: 28%)
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
State Inpatient Database (SID) |
|
|
|
|
SIGNIFICANCE |
Severe maternal morbidity is more than 100 times as common as pregnancy-related mortality—translating to about 52,000 women affected annually—and it is estimated to have increased by 75 percent over the past decade. Rises in chronic conditions, including obesity, diabetes, hypertension, and cardiovascular disease, are likely to have contributed to this increase (Callaghan et al, 2012).
Minority women and particularly non-Hispanic black women have higher rates of severe maternal morbidity. Non-Hispanic Black, Hispanic, Asian/Pacific Islander, and American Indian/Alaska Native women had 2.1, 1.3, 1.2, and 1.7 times, respectively, higher rates of severe morbidity compared with non-Hispanic white women (Creanga et al, 2014). |
|
|
|
|
OUTCOME MEASURE 3 |
Maternal mortality rate per 100,000 live births |

GOAL |
To reduce the maternal mortality rate. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of deaths related to or aggravated by pregnancy and occurring within 42 days of the end of a pregnancy |
|
|
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 100,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Identical to Maternal, Infant, and Child Health (MICH) 5. Reduce the rate of maternal mortality. (Baseline:12.7 maternal deaths per 100,000 live births in 2007, Target: 11.4 maternal deaths per 100,000 live births)
Related to Maternal, Infant, and Child Health (MICH) 6. Reduce maternal illness and complications due to pregnancy (complications during hospitalized labor and delivery) . (Baseline: 31.1%, Target: 28%)
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System-Mortality (NVSS-M), CDC/NCHS; National Vital Statistics System-Natality (NVSS-N), CDC/NCHS |
|
|
|
|
SIGNIFICANCE |
Maternal deaths related to childbirth in the U.S. are nearly at the highest rate in a quarter century, and the U.S. has seen a rise in maternal mortality over the past decade. The rate of death for mothers for every 100,000 live births was18.5 in the U.S. in 2013, a total of almost 800 deaths, showing a rise in pregnancy-related deaths in the U.S. since at least 1987, when the mortality rate was 7.2 per 100,000 births.
There are also significant racial disparities with Black women being three times as likely White women to experience maternal death. |
|
|
|
|
OUTCOME MEASURE 4.1 |
Percent of low birth weight deliveries (<2,500 grams)
|

GOAL |
To reduce the proportion of low birth weight deliveries |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of live births weighing less than 2,500 grams
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 100 |
Text: Percent
|
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Identical to Maternal, Infant, and Child Health (MICH) Objective 8.1: Reduce low birth weight (LBW). (Baseline: 8.2% in 2007, Target 7.8%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
The general category of low birth weight infants includes pre-term infants and infants with intrauterine growth retardation. Many risk factors have been identified for low birth weight babies including: both young and old maternal age, poverty, late prenatal care, smoking, substance abuse, and multiple births. Advanced maternal age and in vitro fertilization has increased the number of multiple births. Multiple births often result in shortened gestation and low or very low birth weight infants. In 2010, 68% of all infant deaths occurred to the 8.2% of low birth weight infants and over half (53%) of all infant deaths occurred to the 1.5% of very low birth weight infants.
Infants born to non-Hispanic Black women have the highest rates of low birth weight, particularly very low birth weight. In 2012, 13.2 percent of non-Hispanic Black infants were born low birthweight and 2.9 percent were born at very low birth weight--these rates are 1.9 and 2.6 times the rates for infants born to non-Hispanic Whites women (7.0 and 1.1 percent, respectively). Infants born to Puerto Rican women also have elevated rates of low and very low birth weight (9.4 and 1.8, respectively). |
|
|
|
|
OUTCOME MEASURE 4.2 |
Percent of very low birth weight deliveries (<1,500 grams) |

GOAL |
To reduce the proportion of low birth weight deliveries |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of live births weighing less than 1,500 grams |
|
|
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Identical to MICH Objective 8.2: Reduce very low birth weight (VLBW). (Baseline: 1.5% in 2007, Target 1.4%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
The general category of low birth weight infants includes pre-term infants and infants with intrauterine growth retardation. Many risk factors have been identified for low birth weight babies including: both young and old maternal age, poverty, late prenatal care, smoking, substance abuse, and multiple births. Advanced maternal age and in vitro fertilization has increased the number of multiple births. Multiple births often result in shortened gestation and low or very low birth weight infants. In 2010, 68% of all infant deaths occurred to the 8.2% of low birth weight infants and over half (53%) of all infant deaths occurred to the 1.5% of very low birth weight infants.
Infants born to non-Hispanic Black women have the highest rates of low birth weight, particularly very low birth weight. In 2012, 13.2 percent of non-Hispanic Black infants were born low birthweight and 2.9 percent were born at very low birth weight--these rates are 1.9 and 2.6 times the rates for infants born to non-Hispanic Whites women (7.0 and 1.1 percent, respectively). Infants born to Puerto Rican women also have elevated rates of low and very low birth weight (9.4 and 1.8, respectively). |
|
|
|
|
OUTCOME MEASURE 4.3 |
Percent of moderately low birth weight deliveries (1,500-2,499 grams)
|

GOAL |
To reduce the proportion of low birth weight deliveries |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of live births weighing between 1,500-2,499 grams |
|
|
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) Objective 8.1: Reduce low birth weight (LBW). (Baseline: 8.2% in 2007, Target 7.8%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
The general category of low birth weight infants includes pre-term infants and infants with intrauterine growth retardation. Many risk factors have been identified for low birth weight babies including: both young and old maternal age, poverty, late prenatal care, smoking, substance abuse, and multiple births. Advanced maternal age and in vitro fertilization has increased the number of multiple births. Multiple births often result in shortened gestation and low or very low birth weight infants. In 2010, 68% of all infant deaths occurred to the 8.2% of low birth weight infants and over half (53%) of all infant deaths occurred to the 1.5% of very low birth weight infants.
Infants born to non-Hispanic Black women have the highest rates of low birth weight, particularly very low birth weight. In 2012, 13.2 percent of non-Hispanic Black infants were born low birthweight and 2.9 percent were born at very low birth weight--these rates are 1.9 and 2.6 times the rates for infants born to non-Hispanic Whites women (7.0 and 1.1 percent, respectively). Infants born to Puerto Rican women also have elevated rates of low and very low birth weight (9.4 and 1.8, respectively). |
|
|
|
|
OUTCOME MEASURE 5.1 |
Percent of preterm births (<37 weeks)
|

GOAL |
To reduce the proportion of all preterm, early term, and early elective deliveries. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of live births before 37 weeks of complete gestation |
|
|
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Identical to Maternal, Infant, and Child Health (MICH) Objective 9.1: Reduce total preterm births (PTB). (Baseline:12.7% in 2007, Target 11.4%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
Babies born preterm, before 37 completed weeks of gestation, are at increased risk of immediate life-threatening health problems, as well as long-term complications and developmental delays. Among preterm infants, complications that can occur during the newborn period include respiratory distress, jaundice, anemia, and infection, while long-term complications can include learning and behavioral problems, cerebral palsy, lung problems, and vision and hearing loss. As a result of these risks, preterm birth is a leading cause of infant death and childhood disability. Although the risk of complications is greatest among those babies who are born the earliest, even those babies born “late preterm” (34 to 36 weeks’ gestation) and "early term" (37, 38 weeks' gestation) are more likely than full-term babies to experience morbidity and mortality.
Infants born to non-Hispanic Black women have the highest rates of preterm birth, particularly early preterm birth. In 2012, 16.5 percent of non-Hispanic Black infants were born preterm and 5.9 percent were born early preterm--these rates are 1.6 and 2.0 times the rates for infants born to non-Hispanic Whites women (10.3 and 2.9 percent, respectively). Infants born to Puerto Rican, Cuban, and American Indian/Alaska Native mothers also had elevated rates of preterm and early preterm birth.
Non-medically indicated early term births (37,38 weeks) present avoidable risks of neonatal morbidity and costly NICU admission (Clark et al, 2009; Tita et al, 2009). Early elective delivery prior to 39 weeks is an endorsed perinatal quality measure by the Joint Commission, National Quality Forum, ACOG/NCQA, Leapfrog Group, and CMS/CHIPRA. |
|
|
|
|
OUTCOME MEASURE 5.2 |
Percent of early preterm births (<34 weeks) |

GOAL |
To reduce the proportion of all preterm, early term, and early elective deliveries. |
||
|
|
||
DEFINITION |
Numerator: |
||
|
Number of live births before 34 weeks of completed gestation. |
||
|
|
||
|
Denominator: |
||
|
Number of live births |
||
|
|
||
|
Units: 100 |
Text: Percent |
|
|
|
||
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) Objective 9.3: Reduce live births at 32-33 weeks. (Baseline: 1.6% in 2007, Target 1.4%)
Related to MICH Objective 9.4: Reduce early preterm or births at less than 32 weeks' gestation. (Baseline: 2.0% in 2007, Target 1.8%) |
||
|
|
||
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
||
|
|
||
SIGNIFICANCE |
Babies born preterm, before 37 completed weeks of gestation, are at increased risk of immediate life-threatening health problems, as well as long-term complications and developmental delays. Among preterm infants, complications that can occur during the newborn period include respiratory distress, jaundice, anemia, and infection, while long-term complications can include learning and behavioral problems, cerebral palsy, lung problems, and vision and hearing loss. As a result of these risks, preterm birth is a leading cause of infant death and childhood disability. Although the risk of complications is greatest among those babies who are born the earliest, even those babies born “late preterm” (34 to 36 weeks’ gestation) and "early term" (37, 38 weeks' gestation) are more likely than full-term babies to experience morbidity and mortality.
Infants born to non-Hispanic Black women have the highest rates of preterm birth, particularly early preterm birth. In 2012, 16.5 percent of non-Hispanic Black infants were born preterm and 5.9 percent were born early preterm--these rates are 1.6 and 2.0 times the rates for infants born to non-Hispanic Whites women (10.3 and 2.9 percent, respectively). Infants born to Puerto Rican, Cuban, and American Indian/Alaska Native mothers also had elevated rates of preterm and early preterm birth.
Non-medically indicated early term births (37,38 weeks) present avoidable risks of neonatal morbidity and costly NICU admission (Clark et al, 2009; Tita et al, 2009). Early elective delivery prior to 39 weeks is an endorsed perinatal quality measure by the Joint Commission, National Quality Forum, ACOG/NCQA, Leapfrog Group, and CMS/CHIPRA. |
||
|
|
||
OUTCOME MEASURE 5.3 |
Percent of late preterm births (34-36 weeks) |
|
|

GOAL |
To reduce the proportion of all preterm, early term, and early elective deliveries. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of live births between 34 and 36 weeks of completed gestation |
|
|
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Identical to MICH Objective 9.2: Reduce late preterm or births at 34-36 weeks' gestation. (Baseline: 9.0% in 2007, Target 8.1%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
Babies born preterm, before 37 completed weeks of gestation, are at increased risk of immediate life-threatening health problems, as well as long-term complications and developmental delays. Among preterm infants, complications that can occur during the newborn period include respiratory distress, jaundice, anemia, and infection, while long-term complications can include learning and behavioral problems, cerebral palsy, lung problems, and vision and hearing loss. As a result of these risks, preterm birth is a leading cause of infant death and childhood disability. Although the risk of complications is greatest among those babies who are born the earliest, even those babies born “late preterm” (34 to 36 weeks’ gestation) and "early term" (37, 38 weeks' gestation) are more likely than full-term babies to experience morbidity and mortality.
Infants born to non-Hispanic Black women have the highest rates of preterm birth, particularly early preterm birth. In 2012, 16.5 percent of non-Hispanic Black infants were born preterm and 5.9 percent were born early preterm--these rates are 1.6 and 2.0 times the rates for infants born to non-Hispanic Whites women (10.3 and 2.9 percent, respectively). Infants born to Puerto Rican, Cuban, and American Indian/Alaska Native mothers also had elevated rates of preterm and early preterm birth.
Non-medically indicated early term births (37,38 weeks) present avoidable risks of neonatal morbidity and costly NICU admission (Clark et al, 2009; Tita et al, 2009). Early elective delivery prior to 39 weeks is an endorsed perinatal quality measure by the Joint Commission, National Quality Forum, ACOG/NCQA, Leapfrog Group, and CMS/CHIPRA. |
|
|
|
|
OUTCOME MEASURE 6 |
Percent of early term births (37,38 weeks) |

GOAL |
To reduce the proportion of all preterm, early term, and early elective deliveries. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of live births born at 37,38 weeks of completed gestation |
|
|
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
Babies born preterm, before 37 completed weeks of gestation, are at increased risk of immediate life-threatening health problems, as well as long-term complications and developmental delays. Among preterm infants, complications that can occur during the newborn period include respiratory distress, jaundice, anemia, and infection, while long-term complications can include learning and behavioral problems, cerebral palsy, lung problems, and vision and hearing loss. As a result of these risks, preterm birth is a leading cause of infant death and childhood disability. Although the risk of complications is greatest among those babies who are born the earliest, even those babies born “late preterm” (34 to 36 weeks’ gestation) and "early term" (37, 38 weeks' gestation) are more likely than full-term babies to experience morbidity and mortality.
Infants born to non-Hispanic Black women have the highest rates of preterm birth, particularly early preterm birth. In 2012, 16.5 percent of non-Hispanic Black infants were born preterm and 5.9 percent were born early preterm--these rates are 1.6 and 2.0 times the rates for infants born to non-Hispanic Whites women (10.3 and 2.9 percent, respectively). Infants born to Puerto Rican, Cuban, and American Indian/Alaska Native mothers also had elevated rates of preterm and early preterm birth.
Non-medically indicated early term births (37,38 weeks) present avoidable risks of neonatal morbidity and costly NICU admission (Clark et al, 2009; Tita et al, 2009). Early elective delivery prior to 39 weeks is an endorsed perinatal quality measure by the Joint Commission, National Quality Forum, ACOG/NCQA, Leapfrog Group, and CMS/CHIPRA. |
|
|
|
|
OUTCOME MEASURE 7 |
Percent of non-medically indicated early elective deliveries |

GOAL |
To reduce the proportion of all preterm, early term, and early elective deliveries. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of inductions or cesareans without labor or spontaneous rupture of membranes among deliveries at 37, 38 weeks' gestation without conditions possibly justifying elective delivery <39 weeks according to The Joint Commission |
|
|
|
|
|
Denominator: |
|
|
Number of deliveries at 37, 38 weeks' gestation without conditions possibly justifying elective delivery <39 weeks according to The Joint Commission |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
CMS Hospital Compare |
|
|
|
|
SIGNIFICANCE |
Babies born preterm, before 37 completed weeks of gestation, are at increased risk of immediate life-threatening health problems, as well as long-term complications and developmental delays. Among preterm infants, complications that can occur during the newborn period include respiratory distress, jaundice, anemia, and infection, while long-term complications can include learning and behavioral problems, cerebral palsy, lung problems, and vision and hearing loss. As a result of these risks, preterm birth is a leading cause of infant death and childhood disability. Although the risk of complications is greatest among those babies who are born the earliest, even those babies born “late preterm” (34 to 36 weeks’ gestation) and "early term" (37, 38 weeks' gestation) are more likely than full-term babies to experience morbidity and mortality.
Infants born to non-Hispanic Black women have the highest rates of preterm birth, particularly early preterm birth. In 2012, 16.5 percent of non-Hispanic Black infants were born preterm and 5.9 percent were born early preterm--these rates are 1.6 and 2.0 times the rates for infants born to non-Hispanic Whites women (10.3 and 2.9 percent, respectively). Infants born to Puerto Rican, Cuban, and American Indian/Alaska Native mothers also had elevated rates of preterm and early preterm birth.
Non-medically indicated early term births (37,38 weeks) present avoidable risks of neonatal morbidity and costly NICU admission (Clark et al, 2009; Tita et al, 2009). Early elective delivery prior to 39 weeks is an endorsed perinatal quality measure by the Joint Commission, National Quality Forum, ACOG/NCQA, Leapfrog Group, and CMS/CHIPRA. |
|
|
|
|
OUTCOME MEASURE 8 |
Perinatal mortality rate per 1,000 live births plus fetal deaths |

GOAL |
To reduce the rate of perinatal deaths. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of fetal deaths 28 weeks or more gestation plus early neonatal deaths occurring under 7 days |
|
|
|
|
|
Denominator: |
|
|
Number of live births plus fetal deaths |
|
|
|
|
|
Units: 1,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) Objective 1.2: Reduce the rate of fetal and infant deaths during the perinatal period (28 weeks of gestation to 7 days after birth). (Baseline: 6.6 fetal and infant deaths per 1,000 live births and fetal deaths occurred during the perinatal period, 28 weeks gestation to 7 days after birth, in 2005; Target: 5.9 perinatal deaths per 1,000 live births and fetal deaths) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
Perinatal mortality is a reflection of the health of the pregnant woman and newborn and reflects the pregnancy environment and early newborn care.
Perinatal mortality is particularly high for non-Hispanic Black women. In 2006, the rate for non-Hispanic black women (11.76) was the highest among the racial and ethnic groups, and was more than twice the rate for non-Hispanic white women. |
|
|
|
|
OUTCOME MEASURE 9.1 |
Infant mortality rate per 1,000 live births |

GOAL |
To reduce the rate of infant death. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of deaths to infants from birth through 364 days of age |
|
|
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 1,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Identical to Maternal, Infant, and Child Health (MICH) Objective 1.3: Reduce the rate of all infant deaths (within 1 year). (Baseline: 6.7 infant deaths per 1,000 live births within the first year of life in 2006, Target: 6.0 infant deaths per 1,000 live births) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
The U.S. infant mortality rate has substantially declined over the last century. Based on preliminary data for 2011, 23,910 infants died before age one year, representing an infant mortality rate of 6.05 deaths per 1,000 live births, which is the lowest infant mortality rate recorded in the U.S. However, significant disparities continue to persist in U.S. infant deaths between racial groups, especially for Blacks and American Indians and Alaskan Natives. The non-Hispanic Black infant mortality rate (12.2 deaths per 1,000 live births in 2010) is nearly two and half times the rate among non-Hispanic Whites and Hispanics. (Child Health USA 2013: Department of Health and Human Services, HRSA). The infant mortality rate in American Indians and Alaskan Natives is more than one and a half times the rate of non-Hispanic Whites. Infant mortality continues to be an extremely complex health issue with many medical, social, and economic determinants, including race/ethnicity, maternal age, education, smoking and health status. |
|
|
|
|
OUTCOME MEASURE 9.2 |
Neonatal mortality rate per 1,000 live births |

GOAL |
To reduce the rate of neonatal deaths. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of deaths to infants under 28 days |
|
|
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 1,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Identical to Maternal, Infant, and Child Health (MICH) Objective 1.4: Reduce the rate of neonatal deaths (within the first 28 days of life). (Baseline: 4.5 neonatal deaths per 1,000 live births occurred within the first 28 days of life in 2006, Target: 4.1 neonatal deaths per 1,000 live births) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
The preliminary U.S. neonatal infant mortality rate was 4.06 deaths per 1,000 live births in 2011, accounting for two-thirds of all infant deaths. Neonatal mortality is related to gestational age, low birth weight, congenital malformations and health problems originating in the perinatal period, such as infections or birth trauma.
A significant disparity exists in neonatal deaths between racial groups, especially for infants born to Black women. Non-Hispanic black women had the highest neonatal mortality rate in 2010 at 7.45, 2.2 times that for non-Hispanic white women (3.35). Neonatal mortality rates were also higher for Puerto Rican (4.82), AIAN (4.28), and Mexican women (3.53) than for non-Hispanic white women. |
|
|
|
|
OUTCOME MEASURE 9.3 |
Post neonatal mortality rate per 1,000 live births |

GOAL |
To reduce the rate of post-neonatal deaths. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of deaths to infants 28 through 364 days of age |
|
|
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 1,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Identical to Maternal, Infant, and Child Health (MICH) Objective 1.5: Reduce the rate of post-neonatal deaths (between 28 days and 1 year). (Baseline: 2.2 post-neonatal deaths per 1,000 live births occurred between 28 days and 1 year of life in 2006, Target: 2.0 post-neonatal deaths per 1,000 live births) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
Postneonatal mortality is generally related to Sudden Unexpected Infant Death (SUID)/Sudden Infant Death Syndrome (SIDS), unintentional injuries and congenital malformations. In 2011, the preliminary U.S. postneonatal mortality rate was 2.01 deaths per 1,000 live births.
Similar to overall infant mortality, infants of non-Hispanic black (4.01) and AIAN (4.00) women had the highest postneonatal mortality rates of any group—more than twice those for non-Hispanic white women (1.82) in 2010. The postneonatal mortality rate was also higher for Puerto Rican women (2.28) than for non-Hispanic white women. |
|
|
|
|
OUTCOME MEASURE 9.4 |
Preterm-related mortality rate per 100,000 live births |

GOAL |
To reduce the rate of preterm-related death. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of deaths due to preterm-related causes. Causes are defined as preterm-related if 75% or more of infants whose deaths were attributed to that cause were born at at less than 37 weeks of gestation, and the cause of death was a direct consequence of preterm birth based on a clinical evaluation and review of the literature. This includes low birth weight, several maternal complications, respiratory distress, bacterial sepsis, etc. To be included as a preterm-related death, the infant must have been born preterm (<37 completed weeks of gestation) with the underlying cause of death assigned to one of the following ICD-10 categories: K550, P000, P010, P011, P015, P020, P021, P027, P070–P073, P102, P220–229, P250–279, P280, P281, P360–369, P520–523, and P77. |
|
|
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 100,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) Objective 1.4: Reduce the rate of neonatal deaths (within the first 28 days of life). (Baseline: 4.5 neonatal deaths per 1,000 live births occurred within the first 28 days of life in 2006, Target: 4.1 neonatal deaths per 1,000 live births)
Related to Maternal, Infant, and Child Health (MICH) Objective 1.3: Reduce the rate of all infant deaths (within 1 year). (Baseline: 6.7 infant deaths per 1,000 live births within the first year of life in 2006, Target: 6.0 infant deaths per 1,000 live births)
Related to Maternal, Infant, and Child Health (MICH) Objective 9.1: Reduce total preterm births (PTB). (Baseline:12.7% in 2007, Target 11.4%)
Related to Maternal, Infant, and Child Health (MICH) 33: Increase the proportion of very low birth weight (VLBW) infants born at Level III hospitals or subspecialty perinatal centers (Baseline: 75% in 2003-2006, Target: 83.7) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
Preterm birth is a leading cause of infant mortality. In 2010, 35% of infant deaths were preterm-related or considered to be a direct consequence of prematurity. There are significant racial/ethnic disparities in preterm-related deaths. The preterm-related infant mortality rate for non-Hispanic black women (4.87 per 1,000) is three times that for non-Hispanic white women. The preterm-related infant mortality rate is 86% higher for Puerto Rican women (2.95 per 1,000), and 10% higher for Mexican women (1.74 per 100,000), than for non-Hispanic white women. |
|
|
|
|
OUTCOME MEASURE 9.5 |
Sleep-related Sudden Unexpected Infant Death (SUID) rate per 100,000 live births |

GOAL |
To reduce the rate sleep-related SUID |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of sleep-related SUID deaths to infants |
|
|
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 100,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Identical to Maternal, Infant, and Child Health (MICH) Objective 1.9: Reduce the rate of infant deaths from sudden unexpected infant deaths (includes SIDS, Unknown Cause, Accidental Suffocation, and Strangulation in Bed). (Baseline: .93 per 1,000 live births in 2006, Target: .84 infant deaths per 1,000 live births)
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
Sleep-related SUIDs are the leading cause of death in infants from one month up to one year (postneonatal deaths) and the third leading cause of all infant deaths. In 2010, there were a total of 3,610 or 0.9 sudden unexpected infant deaths (SUID) per 1,000 live births, accounting for 43 percent of postneonatal deaths and 15 percent of all infant deaths.
SUID rates vary greatly by race and ethnicity. In 2010, SUID rates were highest for infants born to American Indian/Alaska Native and non-Hispanic Black mothers (1.82 and 1.77 per 1,000, respectively); these rates were more than twice the rate among infants born to non-Hispanic Whites (0.87 per 1,000). |
|
|
|
|
OUTCOME MEASURE 10 |
The percent of infants born with fetal alcohol exposure in the last 3 months of pregnancy
|

GOAL |
To reduce the percent of infants born with fetal alcohol exposure
|
|
DEFINITION |
Numerator: |
|
|
Number of women who report drinking alcohol in the last 3 months of pregnancy
|
|
|
Denominator: |
|
|
Number of live births
|
|
|
Units: 100 |
Text: Percent
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) 2.11. Increase abstinence from alcohol among pregnant women. (Baseline: 89.4 percent of pregnant females ages15 to 44 years reported abstaining from alcohol in the past 30 days in 2007–08, Target: 98.3%)
Related to Maternal, Infant, and Child Health (MICH) 25. Reduce the occurrence of fetal alcohol syndrome. (Baseline: 3.6 cases of fetal alcohol syndrome per 10,000 live births in 2006 were suspected or confirmed among children born in 2001–04, Target: Not Applicable)
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
Pregnancy Risk Assessment Monitoring System (PRAMS) |
|
|
|
|
SIGNIFICANCE |
Fetal alcohol spectrum disorders (FASDs), which result in life-long physical and cognitive or behavioral problems, are caused by drinking during pregnancy. Fetal alcohol syndrome (FAS) represents the severe end of FASDs, and is characterized by abnormal facial features (e.g., smooth ridge between nose and upper lip), lower than average height or weight, and central nervous system problems that create deficits in learning, memory, attention, communication, vision, and/or hearing. FASDs are preventable through abstinence from alcohol among pregnant women. Early diagnosis and intervention programs are critical to improve developmental outcomes for children with FAS. |
|
|
|
|
OUTCOME MEASURE 11 |
The rate of infants born with neonatal abstinence syndrome per 1,000 delivery hospitalizations
|

GOAL |
To reduce the rate of infants born with drug dependency.
|
|
DEFINITION |
Numerator: |
|
|
Number of infants born with neonatal abstinence syndrome
|
|
|
Denominator: |
|
|
Number of delivery hospitalizations
|
|
|
Units: 1,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health Objective 11.4. Increase abstinence from illicit drugs among pregnant women. (Baseline: 94.8 percent of pregnant females ages 15 to 44 years reported abstaining from illicit drugs in the past 30 days in 2007–08; Target 100%)
|
|
DATA SOURCES and DATA ISSUES |
HCUP - State Inpatient Database (SID)
|
|
SIGNIFICANCE |
Neonatal drug dependency or withdrawal symptoms, known as neonatal abstinence syndrome (NAS), occur from maternal use of opiates such as heroin, methadone, and prescription pain medications. Symptoms of NAS include fever, diarrhea, irritability, trembling, and increased muscle tone. Along with a rise in prescription drug abuse, the incidence of NAS nearly tripled over the past decade with substantial increases in health care costs (Patrick et al, 2012). Prevention strategies exist along the continuum from preconception, prenatal, postpartum, and infant/childhood stages to help avert substance-exposed pregnancies and improve outcomes for infants born with NAS (ASTHO, 2014; SAMHSA, 2009). |
|
|
|
|
OUTCOME MEASURE 12 |
Percent of eligible newborns screened for heritable disorders with on time physician notification for out of range screens who are followed up in a timely manner. (DEVELOPMENTAL) |

GOAL |
To increase the percent of eligible newborns screened for heritable disorders with on-time physician notification for out of range screens and timely follow up. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of eligible newborns screened for heritable disorders with on time physician notification for out of range screens who are followed up in a timely manner. UNDER DEVELOPMENT. |
|
|
|
|
|
Denominator: |
|
|
Number of live eligible births |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Identical to Maternal, Infant, and Child Health (MICH) Objective 32: Increase appropriate newborn blood-spot screening and follow-up testing (Baseline: 98.3% of screen-positive children received follow-up testing within the recommended time period in 2003–06, Target: 100%). |
|
|
|
|
DATA SOURCES and DATA ISSUES |
The American Public Health Laboratories data set |
|
|
|
|
SIGNIFICANCE |
Newborn screening detects thousands of babies each year with potentially devastating, but treatable disorders. The benefits of newborn screening depend upon timely collection of the newborn blood-spots or administration of a point-of-care test (pulse oximeter for critical congenital heart disease), receipt of the newborn blood spot at the laboratory, testing of the newborn blood spot, and reporting out of all results. Timely detection prevents death, mental retardation, and other significant health complications.
1) The number of eligible infants for screening differs by state so the denominator should reflect the individual state protocol. This will typically be the number of live births minus those who die before screening can occur, or transferred and screened elsewhere, or or whom screening may not be appropriate. 2) The American Public Health Laboratories is a voluntary database so not all states will be represented. 3) The Health People Objective was written before point-of-care testing for CCHD was added to the Recommended Uniform Screening Panel. |
|
|
|
|
OUTCOME MEASURE 13 |
Percent of children meeting the criteria developed for school readiness (DEVELOPMENTAL) |

GOAL |
To increase the proportion of children ready for school. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Under development |
|
|
|
|
|
Denominator: |
|
|
Under development |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Early and Middle Childhood (EMC) 1. (Developmental) Increase the proportion of children who are ready for school in all five domains of healthy development: physical development, social-emotional development, approaches to learning, language, and cognitive development. |
|
|
|
|
DATA SOURCES and DATA ISSUES |
The National Survey of Children's Health (NSCH). |
|
|
|
|
SIGNIFICANCE |
The early years are a critical period where the pathways to a child’s lifetime social, emotional and educational outcomes begin. Although early experiences do not determine children’s ongoing development, the patterns laid down early tend to be very persistent and some have lifelong consequences. Studies have shown that children’s literacy and numeracy skills at age 4–5 are a good predictor of academic achievement in primary school. Social gradients in language and literacy, communication and socioemotional functioning emerge early for children across socioeconomic backgrounds, and these differences persist into the school years. There are also disparities in the US as to who participates in an early childhood program. Further, it is known that children at risk of poor developmental and educational outcomes benefit from attending high-quality education and care programs in the years before school. |
|
|
|
|
OUTCOME MEASURE 14 |
Percent of children ages 1 through 17 who have decayed teeth or cavities in the past 12 months |

GOAL |
To reduce the proportion of children and adolescents who have dental caries or decayed teeth. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children ages 1 through 17 who have decayed teeth or cavities in the past 12 months |
|
|
|
|
|
Denominator: |
|
|
Number of children, ages 1 through 17 |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Oral Health of Children and Adolescents (OH) Objectives 1.1 : Reduce the proportion of children ages 3-5 who have dental caries experience in their primary or permanent teeth, (Baseline: 33.3%, Target: 30.0%) and 1.2: Reduce the proportion of children ages 6-9 who have dental caries experience in their primary or permanent teeth (Baseline: 54.4%, Target: 49.0%)
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Survey of Children's Health (NSCH) |
|
|
|
|
SIGNIFICANCE |
Early childhood caries (ECC), despite being preventable, remains extremely consequential and prevalent (NHANES reports 11% of 2 year olds and 21% of 3 year olds, 34% of 4 year olds, and 44% of 5 year olds are affected). Early childhood is the only life period for which CDC reports increasing prevalence and ECC is the best predictor of future caries risk. ECC is marked by profound income and racial disparities as evidenced by federal NHANES, NHIS, and NSCH data. |
|
|
|
|
|
|
|
OUTCOME MEASURE 15 |
Child mortality rate ages 1 through 9 per 100,000 |
|

GOAL |
To reduce the death rate of children ages 1 through 9. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of deaths among children ages 1 through 9 years |
|
|
|
|
|
Denominator: |
|
|
Number of children ages 1 through 9 |
|
|
|
|
|
Units: 100,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) Objective 3.1: Reduce the rate of child deaths aged 1 to 4 years. (Baseline: 28.6 deaths among children aged 1 to 4 years per 100,000 population occurred in 2007, Target: 25.7 deaths per 100,000 population)
Related to Objective Maternal, Infant, and Child Health (MICH) 3.2: Reduce the rate of child deaths aged 5 to 9 years. (Baseline: 13.7 deaths among children aged 5 to 9 years per 100,000 population occurred in 2007, Target: 12.3 deaths per 100,000 population)
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
Child death certificates are collected by State vital records/NVSS. Data on total number of children comes from the U.S. Census Bureau. |
|
|
|
|
SIGNIFICANCE |
The overall mortality rate for children 1 to 4 years was 26.5 per 100,000 children in 2010 and 12.9 per 100,000 for children ages 5 to 14 years. Unintentional injury continues to be the leading cause of death in children 1 to 14 years. Mortality rates were higher among males than females in each age group. Also, child death rates reflect racial/ethnic disparities, with non-Hispanic Black children having considerably higher rates of mortality than children of other racial/ethnic groups. (Child Health USA 2012, Department of Health and Human Services, HRSA) |
|
|
|
|
OUTCOME MEASURE 16.1 |
Adolescent mortality rate ages 10 through 19 per 100,000
|

GOAL |
To reduce the death rate of adolescents age 10 through19. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of deaths among adolescents ages 10 through 19 years |
|
|
|
|
|
Denominator: |
|
|
Number of adolescents ages 10 through 19 |
|
|
|
|
|
Units: 100,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Objective Maternal, Infant, and Child Health (MICH) 4.1: Reduce the rate of adolescent deaths aged 10 to 14 years. (Baseline: 16.9 deaths among adolescents aged 10 to 14 years per 100,000 population occurred in 2007, Target: 15.2 deaths per 100,000)
Related to Objective Maternal, Infant, and Child Health (MICH) 4.2: Reduce the rate of adolescent deaths aged 15 to 19 years. (Baseline: 60.3 deaths among adolescents aged 15 to 19 years per 100,000 population occurred in 2007, Target: 54.3 deaths per 100,000) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
The leading causes of illness and death among adolescents and young adults are largely preventable. Health outcomes for adolescents and young adults are grounded in their social environments and are frequently mediated by their behaviors. Behaviors of young people are influenced at the individual, peer, family, school, community, and societal levels. |
|
|
|
|
OUTCOME MEASURE 16.2 |
Adolescent motor vehicle mortality rate ages 15 through 19 per 100,000
|

GOAL |
To reduce the death rate of adolescents age 15 through19 from motor vehicle crashes |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of deaths to children ages 15 through 19 years caused by motor vehicle crashes. This includes all occupant, pedestrian, motorcycle, bicycle, etc. deaths caused by motor vehicles |
|
|
|
|
|
Denominator: |
|
|
Number of children in the State ages 15 through19 years |
|
|
|
|
|
Units: 100,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Objective IVP-13: Reduce motor vehicle crash-related deaths. (Baseline: 13.8 motor vehicle traffic-related deaths per 100,000 population occurred in 2007 , Target: 12.4 deaths per 100,000 population) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
Unintentional injuries are the leading cause of mortality among adolescents, with motor vehicle crashes accounting for 64% of those deaths. |
|
|
|
|
OUTCOME MEASURE 16.3 |
Adolescent suicide rate ages 15 through 19 per 100,000 |

GOAL |
To eliminate self-induced, preventable morbidity and mortality. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of deaths attributed to suicide among youths ages 15 through 19 |
|
|
|
|
|
Denominator: |
|
|
Number of youths ages 15 through 19 |
|
|
|
|
|
Units: 100,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Mental Health and Mental Disorders (MHMD) Objective 1: Reduce the suicide rate. (Baseline: 11.3 suicides per 100,000 in 2007, Target: 10.2 suicides per 100,000)
Related to Mental Health and Mental Disorders (MHMD) Objective 2: Reduce suicide attempts by adolescents. (Baseline: 1.9 suicide attempts per 100 occurred in 2009, Target: 1.7 suicide attempts per 100) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
|
|
|
SIGNIFICANCE |
Suicide is the second leading cause of death for ages 10 through 24, and the third leading cause of death for college age youths and ages 12 through18. In the U.S. each day, there are an average of more than 5,400 suicide attempts by young people grades 7-12. |
|
|
|
|
OUTCOME MEASURE 17.1 |
Percent of children with special health care needs |

GOAL |
To track the percent of children and youth with special health care needs, autism spectrum disorder (ASD), and attention deficit disorder/attent deficit hyperactivity disorder (ADD/ADHD). |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children, ages 0 through17, who met the criteria for having a special health care need based on the CSHCN screener |
|
|
|
|
|
Denominator: |
|
|
Number of children, ages 0 through 17 |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Survey of Children's Health (NSCH). |
|
|
|
|
SIGNIFICANCE |
The percent of children with special health care needs has been increasing since 2001. About 12-18% of all US children are considered to have special health care needs. However, they account for almost half of all health care expenditures for children. |
|
|
|
|
OUTCOME MEASURE 17.2 |
Percent of children with special health care needs (CSHCN) receiving care in a well-functioning system |

GOAL |
To ensure access to needed and continuous systems of care for children and youth with special health care needs. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of CSHCN ages 0 through 17 that received all components of a well-functioning system (family partnership, medical home, early screening, adequate insurance, easy access to services, and preparation for adult transition) |
|
|
|
|
|
Denominator: |
|
|
Number of CSHCN ages 0 through 17 |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) Objectives 30.1 : Increase the proportion of children who have access to a medical home, (Baseline: 57.5%, Target: 63.3%) and 30.2: Increase the proportion of children with special health care needs who have access to a medical home. (Baseline: 49.8%, Target: 54.8%)
Related to Objective Maternal, Infant, and Child Health (MICH) 31: Increase the proportion of children with special health care needs who receive their care in family-centered, comprehensive, coordinated systems. (Baseline: 20.4% for children aged 0-11 Target: 22.4% Baseline: 13.8%, for children aged 12 through 17, Target: 15.2%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
The revised National Survey of Children's Health (NSCH). States can use the 2009-2010 National Survey of Children with Special Health Care Needs as a baseline. |
|
|
|
|
SIGNIFICANCE |
According to the 2009-10 NS-CSHCN, only 17.6% of CSHCN receive services in a well-functioning system of services. The Omnibus Budget Reconciliation Act of 1989 requires Title V to provide and promote family-centered, community-based, coordinated care and facilitate the development of community-based systems of services for children with special health care needs and their families. To address this requirement a minimum of 30 percent of the Title V Block Grant funding is allocated for this purpose, and HP 2020 Objective MICH-31 establishes the goal to increase the proportion of children with special health care needs who receive their care in family-centered, comprehensive, and coordinated systems. |
|
|
|
|
OUTCOME MEASURE 17.3 |
Percent of children diagnosed with an autism spectrum disorder |

GOAL |
To track the percent of children and youth with special health care needs, autism spectrum disorder (ASD), and attention deficit disorder/attent deficit hyperactivity disorder (ADD/ADHD). |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children, ages 3 through 17, reported by their parents to have been diagnosed by a health care provider with ASD |
|
|
|
|
|
Denominator: |
|
|
Number of children, ages 3 through17 |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Survey of Children's Health (NSCH) |
|
|
|
|
SIGNIFICANCE |
The prevalence of autism spectrum disorders has risen sharply over the last two decades. However, the average age at diagnosis for ASD is 4 years old, while the American Academy of Pediatrics recommends screening beginning at nine months. Interventions for ASD are more effective when they're started earlier. |
|
|
|
|
OUTCOME MEASURE 17.4 |
Percent of children diagnosed with Attention Deficit Disorder/Attention Deficit Hyperactivity Disorder (ADD/ADHD) |

GOAL |
To track the percent of children and youth with special health care needs, autism spectrum disorder (ASD), and attention deficit disorder/attent deficit hyperactivity disorder (ADD/ADHD). |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children, ages 3 through17, reported by their parents to have been diagnosed by a health care provider with ADD/ADHD |
|
|
|
|
|
Denominator: |
|
|
Number of children, ages 3 through17 |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Survey of Children's Health (NSCH) |
|
|
|
|
SIGNIFICANCE |
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common neurobehavioral disorders of childhood. The prevalence has been increasing over the last decade for reasons that are not yet clear. It is sometimes referred to as Attention Deficit Disorder (ADD). It is usually first diagnosed in childhood and often lasts into adulthood. Children with ADHD may have trouble paying attention, controlling impulsive behaviors, or be overly active. |
|
|
|
|
OUTCOME MEASURE 18 |
Percent of children with a mental/behavioral condition who receive treatment or counseling |

GOAL |
To increase the percent of children with a mental/behavioral condition who receive treatment or counseling. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children, ages 3 through 17, reported by their parents to have been diagnosed by a health care provider with a mental/behavioral condition (depression, anxiety problems, or behavioral or conduct problems) who received treatment or counseling |
|
|
|
|
|
Denominator: |
|
|
Number of children, ages 3 through 17, reported by their parents to have been diagnosed by a health care provider with a mental/behavioral condition (depression, anxiety problems, or behavioral or conduct problems |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Mental Health and Mental Disorders Objective 6: Increase the proportion of children with mental health problems who receive treatment (Baseline: 68.9% in 2008, Target: 75.0%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Survey of Children's Health (NSCH) |
|
|
|
|
SIGNIFICANCE |
The prevalence of mental/behavioral health conditions has been increasing among children and has been found to vary by geographic and sociodemographic factors. However, a significant portion of children diagnosed with a mental health condition do not receive treatment. Further, the receipt of treatment is generally dependent on sociodemographic and health-related factors. |
|
|
|
|
OUTCOME MEASURE 19 |
Percent of children in excellent or very good health |

GOAL |
To improve the health status of children. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children ages 0 through 17 reported by their parents to be in excellent or very good health |
|
|
|
|
|
Denominator: |
|
|
Number of children ages 0 through 17 |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Survey of Children's Health (NSCH) |
|
|
|
|
SIGNIFICANCE |
Overall health status for children provides a global, summary measure of children’s health and well-being. Children reported to be in excellent or very good health are more likely to thrive in a variety of health dimensions, including physical and mental health. |
|
|
|
|
OUTCOME MEASURE 20 |
Percent of children and adolescents who are overweight or obese (BMI at or above the 85th percentile) |

GOAL |
To reduce the proportion of children and adolescents who are considered overweight or obese. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children aged 2 through 4 and adolescents aged 10 through 17 who are overweight or obese |
|
|
|
|
|
Denominator: |
|
|
Number of children aged 2 through 4 (WIC), adolescents aged 10 through 17 (NSCH), and adolescents in grades 9 through 12 (YRBSS) |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Nutrition and Weigh Status (NWS) 10.4. Reduce the proportion of children and adolescents aged 2 to 19 years who are considered obese. (Baseline: 16.1% in 2005-2008, Target: 14.5%).
Related to NWS 11. (Developmental) Prevent inappropriate weight gain in youth and adults. |
|
|
|
|
DATA SOURCES and DATA ISSUES |
WIC for children 2 through 4 years; NSCH for children 10 through17 years (parent-report); YRBSS for adolescents grades 9 through 12 (adolescent report) |
|
|
|
|
SIGNIFICANCE |
Childhood overweight/obesity is a serious health problem in the United States, and the prevalence of overweight among preschool children has doubled since the 1970s. There have been significant increases in the prevalence of overweight in children younger than 5 years of age across all ethnic groups. Onset of overweight in childhood accounts for 25 percent of adult obesity; but overweight that begins before age 8 and persists into adulthood is associated with an even greater degree of adult obesity. Childhood overweight is associated with a variety of adverse consequences, including an increased risk of cardiovascular disease, type 2 diabetes mellitus, asthma, social stigmatization, and low self-esteem. |
|
|
|
|
OUTCOME MEASURE 21 |
Percent of children without health insurance |

GOAL |
To ensure access to needed and continuous health care services for children. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children ages 0 through 17 who are not covered by any private or public health insurance (Including Medicaid or risk pools) at some time during the reporting year |
|
|
|
|
|
Denominator: |
|
|
Number of children ages 0 through 17 under 18 (estimated by Census Bureau) |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Access to Health Services Objective 1: Increase the proportion of persons with health insurance. (Baseline: 83.2% persons had medical insurance in 2008, Target: 100%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
American Community Survey (ACS) and the revised National Survey of Children's Health (NSCH) |
|
|
|
|
SIGNIFICANCE |
There is a well documented benefit for children in having health insurance. Research has shown that children who acquire health insurance are more likely to have access to a usual source of care, receive well child care and immunizations, to have developmental milestones monitored, and receive prescriptions drugs, appropriate care for asthma and basic dental services. Serious childhood problems are more likely to be identified early in children with insurance, and insured children with special health care needs are more likely to have access to specialists. Insured children not only receive more timely diagnosis of serious health care conditions but experience fewer avoidable hospitalizations, improved asthma outcomes and fewer missed school days. (Institute of Medicine’s report, America’s Uninsured Crisis: Consequences for Health and Health Care, 2009) |
|
|
|
|
OUTCOME MEASURE 22.1 |
Percent of children, ages 19 through 35 months, who have received the 4:3:1:3(4):3:1:4 series of routine vaccinations
|

GOAL |
To increase the number of children and adolescents who have completed recommended vaccines. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children, ages 19 through 35 months, that completed the 4:3:1:3(4):3:1:4 combined series of vaccines |
|
|
|
|
|
Denominator: |
|
|
Number of children, ages 19 through 35 months
|
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Identical to Immunization and Infectious Disease (IID) 8.0: Increase the percentage of children aged 19 to 35 months who receive the recommended doses of DTaP, polio, MMR, Hib, hepatitis B, varicella and pneumococcal conjugate vaccine (PCV) (Baseline in 2009 of 44.3%, Target of 80.0%)
|
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Immunization Survey (NIS) |
|
|
|
|
SIGNIFICANCE |
Vaccination is one of the greatest public health achievements of the 20th century, resulting in dramatic declines in morbidity and mortality for many infectious diseases. Childhood vaccination in particular is considered among the most cost-effective preventive services available, as it averts a potential lifetime lost to death and disability.
Currently, there are 12 different vaccines recommended by the Centers for Disease Control and Prevention from birth through age 18, many of which require multiple doses for effectiveness as well as boosters to sustain immunity. (CDC National Immunization Program; Child Health USA 2012)
|
|
|
|
|
OUTCOME MEASURE 22.2 |
Percent of children 6 months through 17 years who are vaccinated annually against seasonal influenza
|

GOAL |
To increase the number of children and adolescents who have completed recommended vaccines. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children 6 months through 17 years who are vaccinated annually against seasonal influenza |
|
|
|
|
|
Denominator: |
|
|
Number of children, ages 6 months through 17 years |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Identical to Immunization and Infectious Disease (IID) 12.11. Increase the percentage of children aged 6 months through 17 years who are vaccinated annually against seasonal influenza (Baseline of 46.9% in 2010-11 flu season, Target of 70%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Immunization Survey (NIS) |
|
|
|
|
SIGNIFICANCE |
Vaccination is one of the greatest public health achievements of the 20th century, resulting in dramatic declines in morbidity and mortality for many infectious diseases. Childhood vaccination in particular is considered among the most cost-effective preventive services available, as it averts a potential lifetime lost to death and disability.
Currently, there are 12 different vaccines recommended by the Centers for Disease Control and Prevention from birth through age 18, many of which require multiple doses for effectiveness as well as boosters to sustain immunity. (CDC National Immunization Program; Child Health USA 2012)
|
|
|
|
|
OUTCOME MEASURE 22.3 |
Percent of adolescents, ages 13 through 17, who have received at least one dose of the HPV vaccine |

GOAL |
To increase the number of children and adolescents who have completed recommended vaccines. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of adolescents, ages 13 through17, who have received at least one dose of the HPV vaccine |
|
|
|
|
|
Denominator: |
|
|
Number of adolescents, ages 13 through17 years |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Immunization and Infectious Disease (IID) 11.4 Increase the vaccination coverage level of 3 doses of human papillomavirus (HPV) vaccine for females by age 13 to 15 years (Baseline in 2008 of 16.6%, Target of 80%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Immunization Survey (NIS) |
|
|
|
|
SIGNIFICANCE |
Vaccination is one of the greatest public health achievements of the 20th century, resulting in dramatic declines in morbidity and mortality for many infectious diseases. Childhood vaccination in particular is considered among the most cost-effective preventive services available, as it averts a potential lifetime lost to death and disability.
Currently, there are 12 different vaccines recommended by the Centers for Disease Control and Prevention from birth through age 18, many of which require multiple doses for effectiveness as well as boosters to sustain immunity. (CDC National Immunization Program; Child Health USA 2012)
|
|
|
|
|
OUTCOME MEASURE 22.4 |
Percent of adolescents, ages 13 through 17, who have received at least one dose of the Tdap vaccine
|

GOAL |
To increase the number of children and adolescents who have completed recommended vaccines. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of adolescents, ages 13 through17, who have received at least one dose of the Tdap vaccine |
|
|
|
|
|
Denominator: |
|
|
Number of adolescents, ages 13 through17 years
|
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Immunization and Infectious Disease (IID) 11.1. Increase the vaccination coverage level of 1 dose of tetanus-diphtheria-acellular pertussis (Tdap) booster vaccine for adolescents by age 13 to 15 years (Baseline 46.7% in 2008; Target of 80%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Immunization Survey (NIS) |
|
|
|
|
SIGNIFICANCE |
Vaccination is one of the greatest public health achievements of the 20th century, resulting in dramatic declines in morbidity and mortality for many infectious diseases. Childhood vaccination in particular is considered among the most cost-effective preventive services available, as it averts a potential lifetime lost to death and disability.
Currently, there are 12 different vaccines recommended by the Centers for Disease Control and Prevention from birth through age 18, many of which require multiple doses for effectiveness as well as boosters to sustain immunity. (CDC National Immunization Program; Child Health USA 2012)
|
|
|
|
|
OUTCOME MEASURE 22.5 |
Percent of adolescents, ages 13 through 17, who have received at least one dose of the meningococcal conjugate vaccine
|

B.
Title V MCH Services Block Grant National Performance Measures
|
|
No. |
National Performance Measure |
1 |
Percent of women with a past year preventive medical visit |
2 |
Percent of cesarean deliveries among low-risk first births |
3 |
Percent of very low birth weight (VLBW) infants born in a hospital with a Level III+ Neonatal Intensive Care Unit (NICU) |
4 |
A) Percent of infants who are ever breastfed and B) Percent of infants breastfed exclusively through 6 months |
5 |
Percent of infants placed to sleep on their backs |
6 |
Percent of children, ages 10 through 71 months, receiving a developmental screening using a parent-completed screening tool |
7 |
Rate of hospitalization for non-fatal injury per 100,000 children ages 0 through 9 and adolescents ages 10 through 19 |
8 |
Percent of children ages 6 through 11 and adolescents ages 12 through 17 who are physically active at least 60 minutes per day |
9 |
Percent of adolescents, ages 12 through 17, who are bullied or who bully others |
10 |
Percent of adolescents, ages 12 through 17, with a preventive medical visit in the past year |
11 |
Percent of children with and without special health care needs having a medical home |
12 |
Percent of adolescents with and without special health care needs who received services necessary to make transitions to adult health care |
13 |
A) Percent of women who had a dental visit during pregnancy and B) Percent of children, ages 1 through 17, who had a preventive dental visit in the past year |
14 |
A) Percent of women who smoke during pregnancy and B) Percent of children who live in households where someone smokes |
15 |
Percent of children ages 0 through 17 who are adequately insured |
PERFORMANCE MEASURE 1 |
Percent of women with a past year preventive medical visit |

GOAL |
To increase the number of women who have a preventive medical visit. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of women, ages 18 through 44, who had a preventive medical visit in the past year |
|
|
|
|
|
Denominator: |
|
|
Number of women, ages 18 through 44 |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) Developmental Objective 16.1: Increase the percentage of women delivering a live birth who discussed preconception health with a health care worker prior to pregnancy
Related to Access to Health Services (AHS) Developmental Objective 7.0: Increase the proportion of persons who receive appropriate clinical preventive services |
|
|
|
|
DATA SOURCES and DATA ISSUES |
Behavioral Risk Factor Surveillance System (BRFSS) |
|
MCH POPULATION DOMAIN
|
Women/Maternal Health |
|
SIGNIFICANCE |
A well-woman or preconception visit provides a critical opportunity to receive recommended clinical preventive services, including screening, counseling, and immunizations, which can lead to appropriate identification, treatment, and prevention of disease to optimize the health of women before, between, and beyond potential pregnancies. For example, screening and management of chronic conditions such as diabetes, and counseling to achieve a healthy weight and smoking cessation, can be advanced within a well woman visit to promote women’s health prior to and between pregnancies and improve subsequent maternal and perinatal outcomes. The annual well-woman visit has been endorsed by the American College of Obstetrics and Gynecologists (ACOG) and was also identified among the women’s preventive services required by the Affordable Care Act (ACA) to be covered by private insurance plans without cost-sharing. |
|
|
|
|
PERFORMANCE MEASURE 2 |
Percent of cesarean deliveries among low-risk first births |

GOAL |
To reduce the number of cesarean deliveries among low-risk first births. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of cesarean delivery among term (37+ weeks), singleton, vertex births to nulliparous women |
|
|
|
|
|
Denominator: |
|
|
Number of term (37+ weeks), singleton, vertex births to nulliparous women
|
|
|
Units: 100 |
Text: Percent
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) Objective 7.1. Reduce cesarean births among low-risk women with no prior cesarean (Baseline: 26.5%, Target: 23.9%) |
|
DATA SOURCES and DATA ISSUES |
National Vital Statistics System (NVSS) |
|
MCH POPULATION DOMAIN
|
Women/Maternal Health |
|
SIGNIFICANCE |
Cesarean delivery can be a life-saving procedure for certain medical indications. However, for most low-risk pregnancies, cesarean delivery poses avoidable maternal risks of morbidity and mortality, including hemorrhage, infection, and blood clots—risks that compound with subsequent cesarean deliveries. Much of the temporal increase in cesarean delivery (over 50% in the past decade), and wide variation across states, hospitals, and practitioners, can be attributed to first-birth cesareans. Moreover, cesarean delivery in low-risk first births may be most amenable to intervention through quality improvement efforts. This low-risk cesarean measure, also known as nulliparous term singleton vertex (NTSV) cesarean, is endorsed by the ACOG, The Joint Commission (PC-02), National Quality Forum (#0471), Center for Medicaid and Medicare Services (CMS) – CHIPRA Child Core Set of Maternity Measures, and the American Medical Association-Physician Consortium for Patient Improvement. |
|
|
|
|
PERFORMANCE MEASURE 3 |
Percent of very low birth weight (VLBW) infants born in a hospital with a Level III+ Neonatal Intensive Care Unit (NICU) |

GOAL |
To ensure that higher risk mothers and newborns deliver at appropriate level hospitals.
|
|
DEFINITION |
Numerator: |
|
|
Number of VLBW infants born in a hospital with a level III or higher NICU
|
|
|
Denominator: |
|
|
Number of VLBW infants (< 1500 grams) |
|
|
Units: 100 |
Text: Percent
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) Objective 33: Increase the proportion of VLBW infants born at level III hospitals or subspecialty perinatal centers (Baseline: 75%, Target: 83.7%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
Linked birth certificate and hospital data on NICU levels from American Academy of Pediatrics (AAP) |
|
MCH POPULATION DOMAIN
|
Perinatal/Infant Health |
|
SIGNIFICANCE |
Very low birth weight infants (<1,500 grams or 3.25 pounds) are the most fragile newborns. Although they represented less than 2% of all births in 2010, VLBW infants accounted for 53% of all infant deaths, with a risk of death over 100 times higher than that of normal birth weight infants (≥2,500 grams or 5.5 pounds). VLBW infants are significantly more likely to survive and thrive when born in a facility with a level-III Neonatal Intensive Care Unit (NICU), a subspecialty facility equipped to handle high-risk neonates. In 2012, the AAP provided updated guidelines on the definitions of neonatal levels of care to include Level I (basic care), Level II (specialty care), and Levels III and IV (subspecialty intensive care) based on the availability of appropriate personnel, physical space, equipment, and organization. Given overwhelming evidence of improved outcomes, the AAP recommends that VLBW and/or very preterm infants (<32 weeks’ gestation) be born in only level III or IV facilities. This measure is endorsed by the National Quality Forum (#0477). |
|
|
|
|
PERFORMANCE MEASURE 4 |
|

GOAL |
To increase the proportion of infants who are breastfed and who are breastfed at six months |
|
|
||
|
|
|
|
||
DEFINITION |
Numerator: |
|
|
||
|
|
|
|
||
|
|
|
|
||
|
Denominator: |
|
|
||
|
|
|
|
||
|
|
|
|
||
|
Units: 100 |
Text: Percent |
|
|
|
|
|
|
|
||
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) Objective 21.1: Increase the proportion of children who are ever breastfed (Baseline: 74% in 2006, Target: 81.9%) Related to Maternal, Infant, and Child Health (MICH) Objective 21.5: Increase the proportion of children who are breastfed exclusively at (Baseline: 14.1% in 2006, Target: 25.5%) |
|
|
||
|
|
|
|
||
DATA SOURCES and DATA ISSUES |
A) National Immunization Survey (NIS)
|
|
|
||
MCH POPULATION DOMAIN
|
Perinatal/Infant Health |
|
|
||
SIGNIFICANCE |
Advantages of breastfeeding are indisputable. The American Academy of Pediatrics recommends all infants (including premature and sick newborns) exclusively breastfeed for about six months as human milk supports optimal growth and development by providing all required nutrients during that time. Breastfeeding strengthens the immune system, improves normal immune response to certain vaccines, offers possible protection from allergies, and reduces probability of SIDS. Research demonstrates breastfed children may be less likely to develop juvenile diabetes; and may have a lower risk of developing childhood obesity, and asthma; and tend to have fewer dental cavities throughout life. The bond of a nursing mother and child is stronger than any other human contact. A woman's ability to meet her child’s nutritional needs improves confidence and bonding with the baby and reduces feelings of anxiety and post natal depression. Increased release of oxytocin while breastfeeding, leads to a reduction in post-partum hemorrhage and quicker return to a normal sized uterus over time, mothers who breastfeed may be less likely to develop breast, uterine and ovarian cancer and have a reduced risk of developing osteoporosis. |
|
|
||
|
|
||||
PERFORMANCE MEASURE 5 |
Percent of infants placed to sleep on their backs |
|
|||

GOAL |
To increase the number of infants placed to sleep on their backs |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of mothers reporting that they most often place their baby to sleep on their back only |
|
|
|
|
|
Denominator: |
|
|
Number of live births |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Identical to Maternal, Infant, and Child Health (MICH) Objective 20: Increase the proportion of infants placed to sleep on their backs (Baseline: 69.0%, Target: 75.9%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
Pregnancy Risk Assessment Monitoring System (PRAMS) |
|
MCH POPULATION DOMAIN
|
Perinatal/Infant Health |
|
SIGNIFICANCE |
Sleep-related infant deaths, also called Sudden Unexpected Infant Deaths (SUID), are the leading cause of infant death after the first month of life and the third leading cause of infant death overall. Sleep-related SUIDs include Sudden Infant Death Syndrome (SIDS), unknown cause, and accidental suffocation and strangulation in bed. Due to heightened risk of SIDS when infants are placed to sleep in side (lateral) or stomach (prone) sleep positions, the AAP has long recommended the back (supine) sleep position. However, in 2011, AAP expanded its recommendations to help reduce the risk of all sleep-related deaths through a safe sleep environment that includes use of the back-sleep position, on a separate firm sleep surface (room-sharing without bed sharing), and without loose bedding. Among others, additional higher-level recommendations include breastfeeding and avoiding smoke exposure during pregnancy and after birth. These expanded recommendations have formed the basis of the National Institute of Child Health and Development (NICHD) Safe to Sleep Campaign. |
|
|
|
|
PERFORMANCE MEASURE 6 |
Percent of children, ages 10 through 71 months, receiving a developmental screening using a parent-completed screening tool |

GOAL |
To increase the number of children who receive a developmental screening. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children 10 months through 71 months (5 years) who had a health care visit in the past 12 months and whose parents completed a Standardized Developmental Screening tool in the past 12 months |
|
|
|
|
|
Denominator: |
|
|
Number of children ages 10 through 71 months who had a health care visit in the past 12 months |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) Objective 29-1: Increase the proportion of children (aged 10-35 months) who have been screened for an Autism Spectrum Disorder and other developmental delays. (Baseline: 22.6%, Target: 24.9%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
The National Survey of Children's Health (NSCH). |
|
MCH POPULATION DOMAIN
|
Child Health |
|
SIGNIFICANCE |
Early identification of developmental disorders is critical to the well-being of children and their families. It is an integral function of the primary care medical home. The percent of children with a developmental disorder has been increasing, yet overall screening rates have remained low. The American Academy of Pediatrics recommends screening tests begin at the nine month visit. |
|
|
|
|
PERFORMANCE MEASURE 7 |
Rate of hospitalization for non-fatal injury per 100,000 children ages 0 through 9 and adolescents 10 through 19 |

GOAL |
To decrease the number of hospital admissions for non-fatal injury among children ages 0 through 19. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of hospital admissions with a primary diagnosis of unintentional or intentional injury among children ages 0 through 19. (excludes in-hospital deaths) |
|
|
|
|
|
Denominator: |
|
|
Number of children and adolescents ages 0 through 19 |
|
|
|
|
|
Units: 100,000 |
Text: Rate |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Injury and Violence Prevention (IVP) Objective 1.2: Reduce hospitalizations for nonfatal injuries. (Baseline: 617.6 per 100,000. Target: 555.8 per 100,000.) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
State Inpatient Databases (SID); U.S. Census Bureau |
|
MCH POPULATION DOMAIN
|
Child Health and/or Adolescent Health |
|
SIGNIFICANCE |
Injury is the leading cause of child mortality. For those who suffer non-fatal severe injuries, many will become children with special health care needs. Effective interventions to reduce injury exist but are not fully implemented in systems of care that serve children and their families. Reducing the burden of nonfatal injury can greatly improve the life course trajectory of infants, children, and adolescents resulting in improved quality of life and cost savings. |
|
|
|
|
PERFORMANCE MEASURE 8 |
Percent of children ages 6 through 11 and adolescents ages 12 through 17 who are physically active at least 60 minutes per day |

GOAL |
To increase the number of children and adolescents who are physically active. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children, ages 6 through 11, and adolescents, ages 12 through 17, who are reported by their parents to be physically active at least 60 minutes per day in the past week (NSCH) and adolescents in grades 9 through 12 who report being physically active at least 60 minutes per day in the past week (YRBSS) |
|
|
|
|
|
Denominator: |
|
|
Number of children ages 6 through 11 and adolescents ages 12 through 17 (NSCH) and number of adolescents in grades 9 through 12 (YRBSS) |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Physical Activity (PA) Objective 4.1: Increase the proportion of the Nation’s public and private elementary schools that require daily physical education for all students. (Baseline: 3.8%, Target: 4.2%)
Related to Physical Activity (PA) Objective 3: Increase the proportion of adolescents who meet current Federal physical activity guidelines for aerobic physical activity and for muscle-strengthening activity. (Baseline: 18.4%, Target: 20.2% for adolescents to meet current physical activity guidelines for aerobic physical activity) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Survey of Children's Health (NSCH) and Youth Risk Behavior Surveillance System (YRBSS). The revised NSCH will capture physical activity of at least 60 minutes per day with baseline NSCH data reflecting at least 20 minutes per day. |
|
MCH POPULATION DOMAIN
|
Child Health and/or Adolescent Health |
|
SIGNIFICANCE |
Regular physical activity can improve the health and quality of life of Americans of all ages, regardless of the presence of a chronic disease or disability. Physical activity in children and adolescents reduces the risk of early life risk factors for cardiovascular disease, hypertension, Type II diabetes, and osteoporosis. In addition to aerobic and muscle-strengthening activities, bone-strengthening activities are especially important for children and young adolescents because the majority of peak bone mass is obtained by the end of adolescence. |
|
|
|
|
PERFORMANCE MEASURE 9 |
Percent of adolescents, ages 12 through 17, who are bullied or who bully others |

GOAL |
To reduce the number of adolescents who are bullied or who bully others. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of adolescents in grades 9 through 12 who report that they are bullied on school property or electronically in the past year (YRBSS) and adolescents ages 12 through 17 who are reported by a parent/guardian to bully others in the past month (NSCH) |
|
|
|
|
|
Denominator: |
|
|
Number of adolescents ages 12 through 17 (NSCH) and adolescents in grades 9 through 12 (YRBSS) |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Injury and Violence Prevention (IVP) Objective 35: Reduce bullying among adolescents. (Baseline: 19.9%, Target: 17.9%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
Youth Risk Behavior Surveillance System (YRBSS) and the revised National Survey of Children's Health (NSCH) will also capture bullying victimization |
|
MCH POPULATION DOMAIN
|
Adolescent Health |
|
SIGNIFICANCE |
Bullying, particularly among school-age children, is a major public health problem. Current estimates suggest nearly 30% of American adolescents reported at least moderate bullying experiences as the bully, the victim, or both. Specifically, of a nationally representative sample of adolescents, 13% reported being a bully, 11% reported being a victim of bullying, and 6% reported being both a bully and a victim. Studies indicate bullying experiences are associated with a number of behavioral, emotional, and physical adjustment problems. Adolescents who bully others tend to exhibit other defiant and delinquent behaviors, have poor school performance, be more likely to drop-out of school, and are more likely to bring weapons to school. Victims of bullying tend to report feelings of depression, anxiety, low self-esteem, and isolation; poor school performance; suicidal ideation; and suicide attempts. Evidence further suggests that people who are the victims of bullying and who also perpetrate bullying (i.e., bully-victims) may exhibit the poorest functioning, in comparison with either victims or bullies. Emotional and behavioral problems experienced by victims, bullies, and bully-victims may continue into adulthood and produce long-term negative outcomes, including low self-esteem and self-worth, depression, antisocial behavior, vandalism, drug use and abuse, criminal behavior, gang membership, and suicidal ideation. |
|
|
|
|
PERFORMANCE MEASURE 10 |
Percent of adolescents, ages 12 through 17, with a preventive medical visit in the past year |

GOAL |
To increase the number of adolescents who have a preventive medical visit. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of adolescents, ages 12 through 17, with a preventive medical visit in the past year |
|
|
|
|
|
Denominator: |
|
|
Number of adolescents, ages 12 through 17 |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Adolescent Health (AH) Objective 1: Increase the proportion of adolescents who have had a wellness checkup in the past 12 months. (Baseline: 68.7%, Target: 75.6%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
The National Survey of Children's Health (NSCH) beginning in 2017. States can use data from the 2011-2012 NSCH as a baseline. |
|
MCH POPULATION DOMAIN
|
Adolescent Health |
|
SIGNIFICANCE |
Adolescence is a period of major physical, psychological, and social development. As adolescents move from childhood to adulthood, they assume individual responsibility for health habits, and those who have chronic health problems take on a greater role in managing those conditions. Initiation of risky behaviors is a critical health issue during adolescence, as adolescents try on adult roles and behaviors. Risky behaviors often initiated in adolescence include unsafe sexual activity, unsafe driving, and use of substances, including tobacco, alcohol, and illegal drugs.
Receiving health care services, including annual adolescent preventive well visits, helps adolescents adopt or maintain healthy habits and behaviors, avoid health‐damaging behaviors, manage chronic conditions, and prevent disease. Receipt of services can help prepare adolescents to manage their health and health care as adults.
The Bright Futures guidelines recommends that adolescents have an annual checkup starting at age 11. The visit should cover a comprehensive set of preventive services, such as a physical examination, discussion of health‐related behaviors, and immunizations. It recommends that the annual checkup include discussion of several health‐related topics, including healthy eating, physical activity, substance use, sexual behavior, violence, and motor vehicle safety. |
|
|
|
|
PERFORMANCE MEASURE 11 |
Percent of children with and without special health care needs having a medical home |

GOAL |
To increase the number of children with and without special health care needs who have a medical home |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children with and without special health care needs, ages 0 through 17, who meet the criteria for having a medical home |
|
|
|
|
|
Denominator: |
|
|
Number of children and adolescents, ages 0 through 17 |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Maternal, Infant, and Child Health (MICH) Objectives 30.1: Increase the proportion of children who have access to a medical home, (Baseline: 57.5%, Target: 63.3%) and 30.2: Increase the proportion of children with special health care needs who have access to a medical home. (Baseline: 49.8%, Target: 54.8%)
Related to Objective Maternal, Infant, and Child Health (MICH) Objective 31: Increase the proportion of children with special health care needs who receive their care in family-centered, comprehensive, coordinated systems. (Baseline: 20.4% for children aged 0-11, Target: 22.4%; Baseline: 13.8% for children aged 12 through 17, Target 15.2%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Survey of Children's Health (NSCH) |
|
MCH POPULATION DOMAIN
|
Children with Special Health Care Needs |
|
SIGNIFICANCE |
The American Academy of Pediatrics (AAP) specifies seven qualities essential to medical home care: accessible, family-centered, continuous, comprehensive, coordinated, compassionate and culturally effective. Ideally, medical home care is delivered within the context of a trusting and collaborative relationship between the child’s family and a competent health professional familiar with the child and family and the child’s health history. Providing comprehensive care to children in a medical home is the standard of pediatric practice. Research indicates that children with a stable and continuous source of health care are more likely to receive appropriate preventive care and immunizations, are less likely to be hospitalized for preventable conditions, and are more likely to be diagnosed early for chronic or disabling conditions. The Maternal and Child Health Bureau uses the AAP definition of medical home. |
|
|
|
|
PERFORMANCE MEASURE 12 |
Percent of adolescents with and without special health care needs who received services necessary to make transitions to adult health care |

GOAL |
To increase the percent of adolescents with and without special health care needs who have received the services necessary to make transitions to all aspects of adult life, including adult health care, work, and independence. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of adolescents with and without special health care needs, ages 12 through 17, whose families report that they received the services necessary to transition to adult health care |
|
|
|
|
|
Denominator: |
|
|
Number of adolescents, ages 12 through 17 |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Disability and Health (DH) Objective 5: Increase the proportion of youth with special health care needs whose health care provider has discussed transition planning from pediatric to adult health care. (Baseline: 41.2%, Target: 45.3%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
The revised National Survey of Children's Health (NSCH) beginning in 2017. States can use data from the 2009-2010 NS-CSHCN as a baseline. |
|
MCH POPULATION DOMAIN
|
Children with Special Health Care Needs |
|
SIGNIFICANCE |
The transition of youth to adulthood has become a priority issue nationwide as evidenced by the clinical report and algorithm developed jointly by the AAP, American Academy of Family Physicians and American College of Physicians to improve healthcare transitions for all youth and families. Over 90 percent of children with special health care needs now live to adulthood, but are less likely than their non-disabled peers to complete high school, attend college or to be employed. Health and health care are cited as two of the major barriers to making successful transitions. |
|
|
|
|
PERFORMANCE MEASURE 13 |
A) Percent of women who had a dental visit during pregnancy and B) Percent of children, ages 1 through 17, who had a preventive dental visit in the past year |

GOAL |
A) To increase the number of pregnant women who have a dental visit during pregnancy and B) To increase the number of children, ages 1 through 17, who had a preventive dental visit in the past year. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
A) Number of women who had a dental visit during pregnancy B) Number of infant or child, ages 1 through 17, who had a preventive dental visit in the past year |
|
|
|
|
|
Denominator: |
|
|
A) Number of live births B) Number of infants and children, ages 1 through 17 |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Oral Health (OH) Objective 7. Increase the proportion of children, adolescents, and adults who used the oral health care system in the past year. (Baseline: 44.5%, Target: 49.0%)
Related to Oral Health (OH) Objective 8. Increase the proportion of low-income children and adolescents who receive any preventive dental service during the past year. (Baseline: 30.2%, Target: 33.2%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
This is an integrated measure with two data sources: A) Pregnancy Risk Assessment Monitoring System (PRAMS); B) National Survey of Children's Health (NSCH)
If a state has access to both PRAMS and the NSCH, the state needs to address both parts (A & B) of the measure. If a state does not have access to PRAMS, the state will need to address part B of the measure. |
|
MCH POPULATION DOMAIN
|
Cross-cutting/Life course |
|
SIGNIFICANCE |
Oral health is a vital component of overall health. Access to oral health care, good oral hygiene, and adequate nutrition are essential component of oral health to help ensure that children, adolescents, and adults achieve and maintain oral health. People with limited access to preventive oral health services are at greater risk for oral diseases.
Oral health care remains the greatest unmet health need for children. Insufficient access to oral health care and effective preventive services affects children’s health, education, and ability to prosper. Early dental visits teach children that oral health is important. Children who receive oral health care early in life are more likely to have a good attitude about oral health professionals and dental visits. Pregnant women who receive oral health care are more likely to take their children to get oral health care.
State Title V Maternal Child Health programs have long recognized the importance of improving the availability and quality of services to improve oral health for children and pregnant women. States monitor and guide service delivery to assure that all children have access to preventive oral health services. Strategies for promoting oral health include providing preventive interventions, such as dental sealants and use of fluoride, increasing the capacity of State oral health programs to provide preventive services, evaluating and improving methods of monitoring oral diseases and conditions, and increasing the number of community health centers with an oral health component.
|
|
|
|
|
PERFORMANCE MEASURE 14 |
A) Percent of women who smoke during pregnancy and B) Percent of children who live in households where someone smokes |

GOAL |
A) To decrease the number of women who smoke during pregnancy and B) To decrease the number of households where someone smokes. |
|
|
|
|
DEFINITION |
Numerator: |
|
|
A) Number of women who report smoking during pregnancy B) Number of children who live in households where there is household member who smokes |
|
|
|
|
|
Denominator: |
|
|
A) Number of live births B) Number of children, ages 0 through 17 |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Tobacco Use (TU) Objective 6: Increase smoking cessation during pregnancy (Target: 30.0%) and related to Tobacco Use (TU) Objective 11.1: Reduce the proportion of children aged 3 to 11 years exposed to secondhand smoke. (Baseline: 52.2% , Target 47%)
Related to Respiratory Diseases (RD) Objective 7.5: Increase the proportion of persons with current asthma who have been advised by a health professional to change things in their home, school, and work environments to reduce exposure to irritants or allergens to which they are sensitive according to National Asthma Education and prevention Program guidelines. (Baseline: 50.8%, Target: 54.5%) |
|
|
|
|
DATA SOURCES and DATA ISSUES |
This is an integrated measure with the following data sources: A) National Vital Statistics System (NVSS) for smoking during pregnancy and B) National Survey of Children's Health (NSCH)
If selected, the state needs to address both parts (A & B) of the measure. |
|
MCH POPULATION DOMAIN
|
Cross-cutting/Life course |
|
SIGNIFICANCE |
Women who smoke during pregnancy are more likely to experience a fetal death or deliver a low birth weight baby. Further, secondhand smoke (SHS) is a mixture of mainstream smoke (exhaled by smoker) and the more toxic side stream smoke (from lit end of nicotine product) which is classified as a “known human carcinogen” by the US Environmental Protection Agency, the US National Toxicology Program, and the International Agency for Research on Cancer. Adverse effects of parental smoking on children have been a clinical and public health concern for decades and were documented in the 1986 U.S. Surgeon General Report. The only way to fully protect non-smokers from indoor exposure to SHS is to prevent all smoking in the space; separating smokers from non-smokers, cleaning the air, and ventilating buildings do not eliminate exposure. Unfortunately, millions (more than 60%) of children are exposed to SHS in their homes. These children have an increased frequency of ear infections; acute respiratory illnesses and related hospital admissions during infancy; severe asthma and asthma-related problems; lower respiratory tract infections leading to 7,500 to 15,000 hospitalizations annually in children under 18 months; and sudden infant death syndrome (SIDS). Higher intensity medical services are also required by children of parents who smoke including an increased need for intensive care unit services when admitted for flu, longer hospital stays; and more frequent use of breathing tubes during admissions. |
|
|
|
|
PERFORMANCE MEASURE 15 |
Percent of children ages 0 through 17 who are adequately insured |

GOAL |
To increase the number of children who are adequately insured |
|
|
|
|
DEFINITION |
Numerator: |
|
|
Number of children, ages 0 through 17, who were reported to be adequately insured, based on 3 criteria: whether their children’s insurance covers needed services and providers, and reasonably covers costs. If a parent answered “always” or “usually” to all three dimensions of adequacy, then the child was considered to have adequate insurance coverage. (No out-of-pocket costs were considered to be “always” reasonable.) |
|
|
|
|
|
Denominator: |
|
|
Number of children, ages 0 through 17 |
|
|
|
|
|
Units: 100 |
Text: Percent |
|
|
|
HEALTHY PEOPLE 2020 OBJECTIVE |
Related to Access to Health Services (AHS) Objective 1: Increase the proportion of persons with health insurance
Related to Access to Health Services (AHS) Objective 6: Reduce the proportion of persons who are unable to obtain or delay in obtaining necessary medical care, dental care, or prescription medicines |
|
|
|
|
DATA SOURCES and DATA ISSUES |
National Survey of Children's Health (NSCH) |
|
MCH POPULATION DOMAIN
|
Cross-cutting/Life course |
|
SIGNIFICANCE |
Almost one-quarter of American children with continuous insurance coverage are not adequately insured. Inadequately insured children are more likely to have delayed or forgone care, lack a medical home, be less likely to receive needed referrals and care coordination, and receive family-centered care. The American Academy of Pediatrics highlighted the importance of this issue with a policy statement. The major problems cited were cost-sharing requirements that are too high, benefit limitations, and inadequate coverage of needed services. |
|
APPENDIX G: |
REQUIRED APPLICATION/ANNUAL REPORT COMPONENTS AND TIMELINE
|
Submission Date |
Application Year |
Annual Report Year |
July 15, 2015 |
Fiscal Year (FY) 2016 (First Application Year of New Five-year Reporting Cycle.)
|
FY 2014 (Interim Year 04 of Previous Reporting Cycle)
|
July 15, 2016 |
FY 2017 (Second Year Application, or Interim Year 01, of Five-year Reporting Cycle)
FY 2017 (Continued)
|
FY 2015 (Last Annual Report Year, or Interim Year 05, of Previous Five-year Reporting Cycle)
FY 2015 (Continued)
|
July 15, 2017 |
FY 2018 (Interim Year 03 Application)
FY 2018 (Continued)
|
FY 2016 (First Annual Report of New Five-year Reporting Cycle)
FY 2016 (Continued)
|
APPENDIX H: GLOSSARY
A comprehensive glossary of terms relevant to maternal and child health (MCH) practice, including services for children with special health care needs (CSHCN), is available on the MCH Navigator site. To access the Glossary, click on: http://www.mchnavigator.org. This project is administered by Georgetown University through funding provided by the Health Resources and Services Administration’s (HRSA) Maternal and Child Health Bureau (MCHB.) The MCH Navigator is a learning portal for MCH professionals, students, and others working to improve the health and well-being of women, children, adolescents, and families.
Definitions included in this Glossary are intended to supplement the broader set of terms that are included in the MCH Navigator Glossary. The following list of terms and their definitions have specific relevance to the State Title V MCH Block Grant programs.
MCH Working Framework: MCH Pyramid of Services
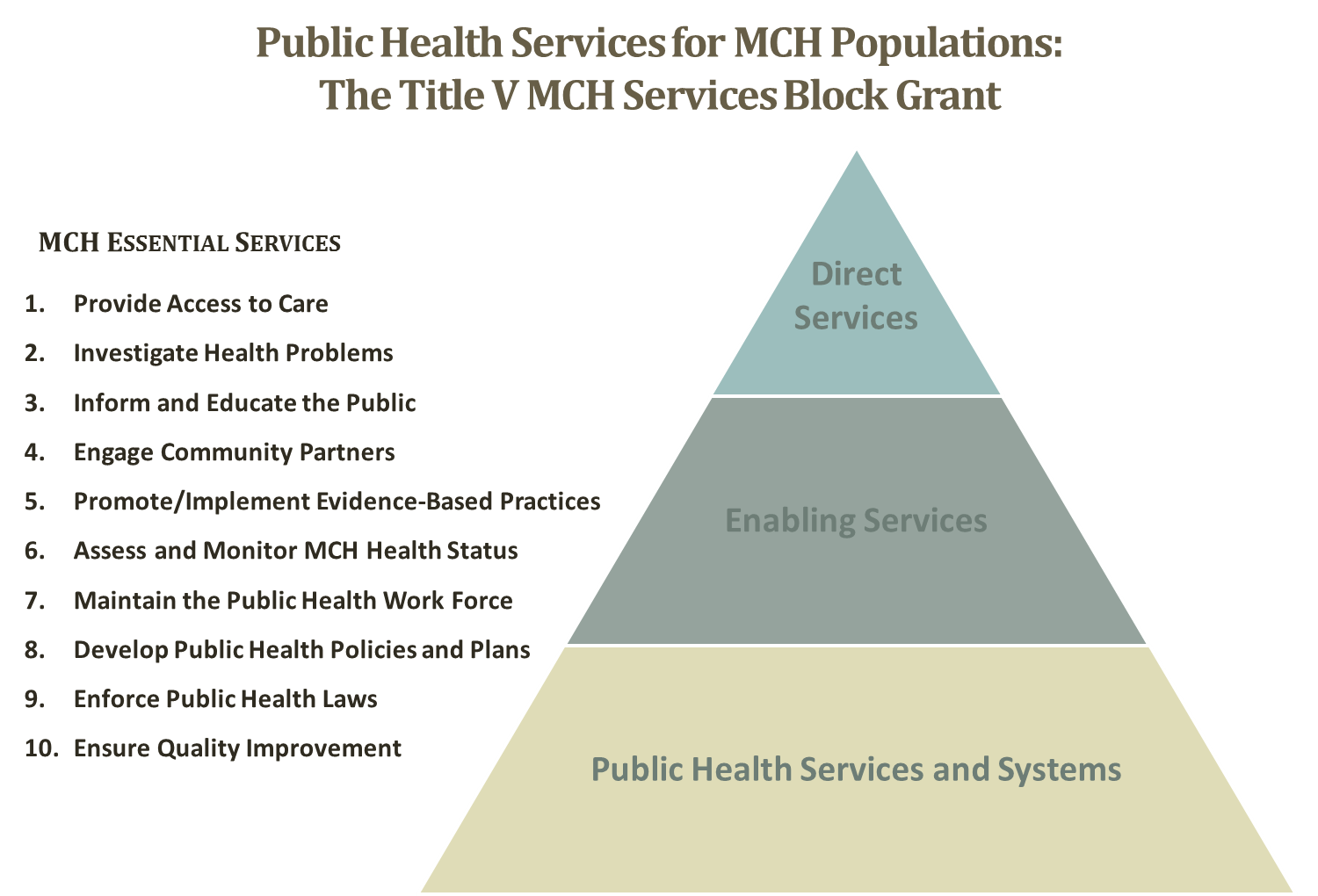
As depicted on the Revised MCH Pyramid, the working framework for the Title V MCH Block Grant to States Program aligns with the 10 MCH Essential Services and consists of three levels. Definitions are provided on the next page for each level of service.
In developing systems of care, States should assure that they are family centered, community based and culturally competent.
Direct Services – Direct services are preventive, primary, or specialty clinical services to pregnant women and children, including children with special health care needs, where MCH Services Block Grant funds are used to reimburse or fund providers for these services through a formal process similar to paying a medical billing claim or managed care contracts. State reporting on direct services should not include the costs of clinical services which are delivered with Title V dollars but reimbursed by Medicaid, CHIP or other public or private payers. Examples include, but are not limited to, preventive, primary or specialty care visits, emergency department visits, inpatient services, outpatient and inpatient mental and behavioral health services, prescription drugs, occupational and physical therapy, speech therapy, durable medical equipment and medical supplies, medical foods, dental care, and vision care.
Enabling Services – Enabling services are non-clinical services (i.e., not included as direct or public health services) that enable individuals to access health care and improve health outcomes where MCH Services Block Grant funds are used to finance these services. Enabling services include, but are not limited to: case management, care coordination, referrals, translation/interpretation, transportation, eligibility assistance, health education for individuals or families, environmental health risk reduction, health literacy, and outreach. State reporting on enabling services should not include the costs for enabling services that are reimbursed by Medicaid, CHIP, or other public and private payers. This category may include salary and operational support to a clinic or program that enable individuals to access health care or improve health outcomes. Examples include the salary of a public health nurse who provides prenatal care in a local clinic or compensation provided to a specialist pediatrician who provides services for children with special health care needs.
Public Health Services and Systems – Public health services and systems are activities and infrastructure to carry out the core public health functions of assessment, assurance, and policy development, and the 10 essential public health services. Examples include the development of standards and guidelines, needs assessment, program planning, implementation, and evaluation, policy development, quality assurance and improvement, workforce development, and population-based disease prevention and health promotion campaigns for services such as newborn screening, immunization, injury prevention, safe-sleep education and anti-smoking. State reporting on public health services and systems should not include costs for direct clinical preventive services, such as immunization, newborn screening tests, or smoking cessation.
Title V Program Administration
Administrative Title V Funds - The amount of funds the State uses for the management of the Title V allocation. This amount is limited by statute to 10 percent of the Federal Title V allotment.
Capacity – Program capacity includes delivery systems, workforce, policies, and support systems (e.g., training, research, technical assistance, and information systems) and other infrastructure needed to maintain service delivery and policy making activities. Program capacity results measure the strength of the human and material resources necessary to meet public health obligations. As program capacity sets the stage for other activities, program capacity results are closely related to the results for process, health outcome, and risk factors. Program capacity results should answer the question, “What does the State need to achieve the results we want?”
Children – A child from his/her first birthday through the 21st year, who is not otherwise included in any other class of individuals (e.g., counted as a pregnant woman.)
Data Systems Development – Development of data management systems (electronic or other) or linking of existing databases to support States’ ability to collect, tabulate, analyze, and report data accurately. (See Systems Development.)
Early Neonatal Period – The early neonatal period begins at birth and lasts through the 6th day of life.
Federal Allocation – The funding provided to the States under the Federal Title V Block Grant in any given fiscal year; applies specifically to the Application Face Sheet
(SF-424) and Form 2.
Government Performance and Results Act (GPRA) – Federal legislation enacted in 1993 that requires Federal agencies to develop strategic plans, prepare annual plans setting performance goals, and report annually on actual performance.
Infants – Children less than one year of age that are not included in any other class of individuals.
Jurisdictions – The following jurisdictions receive Title V Maternal and Child Health Block Grant Program funding: the District of Columbia, the Republic of the Marshall Islands, the Federated States of Micronesia, the Republic of Palau and the U.S. territories of the Commonwealth of Puerto Rico, the Virgin Islands, Guam, American Samoa, and the Commonwealth of the Northern Mariana Islands.
Life Course Theory (LCT) – A conceptual framework that helps explain health and disease patterns – particularly health disparities – across populations and over time. Instead of focusing on differences in health patterns based on one disease or condition at a time, LCT points to broad social, economic and environmental factors as underlying causes of persistent inequalities in health for a wide range of diseases and conditions across population groups. LCT is population focused, and firmly rooted in social determinants and social equity models. Though not often explicitly state, LCT is also community (or “place”) focused, since social, economic and environmental patterns are closely linked to community and neighborhood settings.1
Local – Funds derived from local jurisdictions within the State, which are used for MCH program activities and reported on the Application Face Sheet (SF 424) and Form 2.
Low Income – An individual or family with an income that is determined to be below the income official federal poverty line, as defined by the Office of Management and Budget and revised annually in accordance with section 673(2) of the Omnibus Budget Reconciliation Act of 1981. [Title V, Sec. 501 (b)(2)]
Needs Assessment – A process to understand the strengths and needs of the health service system within a community or population. For maternal and child health purposes, needs assessment efforts consider the following components: 1) health status, 2) health service utilization, 3) health systems capacity, and 4) population/ community characteristics and contextual characteristics.
Neonatal Period – The neonatal period begins at birth and lasts through the 28th day following birth.
Newborn – A human infant from the time of birth through the 28th day of life.
Other Federal Funds – Federal funds other than the Title V Block Grant that are under the control of the person responsible for administration of the Title V program and reported on the Application Face Sheet (SF 424) and Form 2. These funds may include, but are not limited to: WIC, EMSC, Healthy Start, SPRANS, HIV/AIDs monies, CISS funds, MCH targeted funds from CDC, MCH Education funds and Medicaid Federal Medical Assistance Percentage (FMAP).
Others (Class of Individuals) – Women of childbearing age, over age 21, and any others defined by the State who are not otherwise included in any of the other listed classes of individuals. (Form 3a and Form 5a)
Perinatal – The period of gestation between 28 weeks or more to 7 days or less after birth.
Post-neonatal Period – The period between the end of the first month to a year after birth.
Pregnant Woman – A female from the time that she conceives to 60 days after birth, delivery, or expulsion of fetus.
Prenatal – Occurring or existing before birth, referring to both the care of the woman during pregnancy and the growth and development of the fetus.
Program Income – Funds collected by State MCH agencies from sources generated by the State’s MCH program to include insurance payments, Medicaid reimbursements, HMO payments, etc., as reported on the Application Face Sheet [SF 424] and Form 2.
State – Terminology used in this Guidance to reference the 50 States and the nine jurisdictions. (See also “Jurisdictions”)
State Funds – The State’s required matching funds (including overmatch) in any given year, as reported on the Application Face Sheet [SF 424] and Form 2.
Technical Assistance (TA) – The process of providing advice, assistance, and training by an expert with specific technical/content knowledge to address an identified need. Technical Assistance relationships are program-focused, and may use an interactive, on-site/hands-on approach as well as telephone or email assistance. Technical Assistance delivery is short in duration, customized to meet the needs of the client, and offers prescriptive solutions to a specific issue. [Concordia University, 2007www.mnsmart.org]
Title V of the Social Security Act – The authorizing legislation for the Maternal and Child Health Services Block Grant to States Program.
Title V Reporting Form 6, Deliveries to Pregnant Women – Unduplicated number of deliveries to pregnant women who were provided prenatal, delivery, or post-partum services through the Title V program during the reporting period.
Title V Reporting Form 6, Infants Served by Title V – The unduplicated count of infants provided a direct service by the State’s Title V program during the reporting period.
Title XIX of the Social Security Act – The authorizing legislation for the Medicaid program.
Title XIX Reporting on Form 6, Pregnant Women Eligible for Title XIX – The number of pregnant women who delivered during the reporting period and were eligible for the State’s Title XIX (Medicaid) program.
Title XIX Reporting on Form 6, Infants Eligible for Title XIX – The number of infants eligible for the State’s Title XIX (Medicaid) program.
Title XXI – Children’s Health Insurance Program (CHIP) financed via the Centers for Medicare and Medicaid Services (CMS). The purpose of this title is to provide funds to States to enable them to initiate and expand the provision of child health assistance to uninsured, low-income children in an effective and efficient manner that is coordinated with other sources of health benefits coverage for children.
(Sec. 2101. [42 U.S.C. 1397aa])
Total MCH Funding – All of the MCH funds administered by a State MCH program. Included in this sum total are: 1) the Federal Title V Block grant allocation; 2) the Applicant’s funds, which consists of the unobligated balance from the previous year’s MCH Block Grant allocation, the State’s total matching funds for the Title V allocation (match and overmatch); 3) the Local funds, which are the total amount of MCH dedicated funds from local government within the State); 4) Other Federal funds (monies other than the Title V Block Grant that are under the control of the person responsible for administration of the Title V program), and 5) Program Income (funds collected by State MCH agencies from insurance payments, Medicaid, HMO’s, private grants, etc.)
Unobligated Balance – The amount of unexpended funds from the previous year’s Title V MCH Block Grant, as reported as Applicant funds on the Application Face Sheet [SF 424] and as Unobligated Balance on Form 2.
Performance Measurement
Objectives – The yardsticks by which an agency can measure its efforts to accomplish a goal. (See also Performance Objectives)
Outcome Measure – The ultimate focus and desired result of any set of public health program activities and interventions is an improved health and well-being outcome. Health and well-being outcomes are usually longer term and tied to the ultimate program goal. Morbidity and mortality statistics are indicators of achievement of health outcomes. Other outcomes reflect commonly accepted indicators of a highly functioning system of care for children with special health care needs and their families, positive outcomes, outcomes which are legislatively mandated or are a legislative focus, outcomes where the prevalence is increasing, and developmental outcomes where a fully functioning data system does not exist.
Performance Indicator – The statistical or quantitative value that expresses the result of a performance objective.
Performance Measure – A narrative statement that describes a specific maternal and child health need or requirement that, when successfully addressed, will lead to or will assist in leading to a specific health outcome within a community or jurisdiction and generally within a specified time frame. (Example: “The rate of women in [State] who receive early prenatal care in 20__.” This performance measure will assist in leading to [the health outcome measure of] reducing the rate of infant mortality in the State).
Performance Measurement – The collection of data on, recording of, or tabulation of results or achievements, usually for comparison to a benchmark.
Performance Objectives – A statement of intention with which actual achievement and results can be measured and compared. Performance objective statements clearly describe what is to be achieved, when it is to be achieved, the extent of the achievement, and the target populations.
Evidence-based or –Informed Strategy Measure (ESM) –Developed by the State, ESMs would assess the impact of State Title V strategies and activities contained in the State Action Plan. It is envisioned that the development of the ESMs will be guided through an examination of the evidenced-based or evidence-informed practices on what strategies and activities are both practical and measurable. The main criteria for the ESM would be that the activities had to be measurable, and there had to be evidence that the activity was related to the performance measure chosen.
Evidence-based or –Informed Strategy Measure (ESM) Objectives – The objectives for activities and interventions that drive the achievement of higher-level objectives by the State Title V program.
Risk Factors – Public health activities and programs that focus on reduction of scientifically established direct causes of, and contributors to, morbidity and mortality (i.e., risk factors) are essential steps toward achieving desired health outcomes. Changes in behavior or physiological conditions are the indicators of achievement of risk factor results. Results focused on risk factors tend to be intermediate term. Risk factor results should answer the question, “Why should the State address this risk factor (i.e., what health outcome will this result support)?”
Risk Factor Objectives – Objectives that describe an improvement in risk factors (usually behavioral or physiological) that are associated with morbidity and mortality.
Targets – An aspired outcome that is explicitly stated, e.g. achieve 90% of timeliness of reporting, 100% completeness of reporting, etc. In this Guidance, “Targets” is often used interchangeably with “Objectives.”
Collaborative Learning, Innovation and Quality Improvement
Aim Statement – A written measureable description of desired outcomes used in a quality improvement initiative. A strong AIM statement outlines what is to be accomplished, quantifies the changes that are to be achieved and sets a date by which the goals will be reached.
Blueprint for Change – A tool to help define action steps for a team’s strategic priorities.
CoIIN versus COIN – The Collaborative Improvement and Innovation Network (CoIIN) initiative extends the Collaboration Innovation Network (COIN) model to include the concept of improvement in recognition of the need to strengthen existing investments in maternal and infant health as well as to develop innovative, new approaches.
Collaborative Innovation Network (COIN) – A cyberteam of self-motivated people with a collective vision, enabled by the Web to collaborate in achieving a common goal by sharing ideas, information and work.2
Collaborative Learning – Projects using this model enable learners of different abilities and interests to work jointly in small groups to complete a project or solve a problem.
Collective Impact – A concept that provides a framework for bringing diverse people and organizations together in a structured way to achieve social change.3
Driver Diagram – A logic chart that organizes the different aspects of an improvement project so key interventions and relationships between these interventions may be clearly understood by all involved.
Infant Mortality CoIIN Framework – A framework that presents a theory of the relationships between (1) key domains of influence (e.g., engaged leadership or innovation), (2) the periods of engagement, and (3) the strategies priorities that will be employed to reduce infant mortality rates in the U.S.
Learning Collaborative – A group of individuals or organizations that come together for a defined period of time to work together to improve process relevant to a specific topic. Members of a learning collaborative generally agree upon a shared set of data to measure and meet regularly to learn from each other and project experts.
Learning Sessions – Members of learning collaboratives generally agree to a regular schedule of multi-day meetings throughout the collaborative. These meetings may be in person or virtual. The learning sessions allow Collaborative faculty and partners to share latest research or important information on the topic of the collaborative, and they allow participants to share their work and to learn from each other.
Perinatal Periods of Risk (PPOR) – Both a community approach and an analytic framework for investigating and addressing high infant mortality rates in urban settings. The overall intent of the PPOR approach is to develop a simple method that can be used by communities to mobilize and prioritize prevention efforts. PPOR brings community stakeholders together to build consensus, support and partnership around infant mortality rates.4
Primary Drivers – Found in the CoIIN framework and driver diagrams, drivers are system components, factors or broad improvement areas that contribute directly to achieving the stated outcome. For example, if the outcome is reducing infant mortality, a strategic priority/primary driver might be to improve access to and quality of prenatal care for women. (See Strategic Priorities)
Potential Action/Change Concept – Actionable steps for change targeted at improving specific processes, often originating from brainstorming sessions with the team and evidence-based best practices.
Quality Improvement in Public Health – The use of a deliberate and defined improvement process, which is focused on activities that are responsive to community needs and improving population health. This effort is continuous and ongoing to achieve measureable improvements in the efficiency, effectiveness, performance, accountability, outcomes and other indicators of quality in services or processes, which achieve equity and improve the health of the community.5
Strategic Priorities – Found in the CoIIN framework and driver diagrams, these priorities are system components, factors or broad improvement areas that contribute directly to achieving the stated outcome. For example, if the outcome is reducing infant mortality, a strategic priority/primary driver might be to improve access to and quality of prenatal care for women.
Family/Consumer Engagement
Cultural Competence – A set of values, behaviors, attitudes, and practices within a system, organization, program or among individuals and which enables them to work effectively cross culturally. Further, cultural competence refers to the ability to honor and respect the beliefs, language, inter-personal styles and behaviors of individuals and families receiving services, as well as staff who are providing such services. At a systems, organizational, or program level, cultural competence requires a comprehensive and coordinated plan that includes interventions at all the levels from policy-making to the individual, and is a dynamic, ongoing, process that requires a long-term commitment. A component of cultural competence is linguistic competence, the capacity of an organization and its personnel to communicate effectively, and convey information in a manner that is easily understood by diverse audiences including persons of limited English proficiency, those who are not literate or who have low literacy skills and individuals with disabilities.
Regarding the principles of cultural competence, an organization should value diversity in families, staff, providers and communities; have the capacity for cultural self-assessment; be conscious of the dynamics inherent when cultures interact, e.g. families and providers; institutionalize cultural knowledge; and develop adaptations to service delivery and partnership building which reflects an understanding of cultural diversity. An individual should examine one’s own attitude and values; acquire the values, knowledge, and skills for working in cross cultural situations; and remember that everyone has a culture.6
Culturally Sensitive – The recognition and understanding that different cultures may have different concepts and practices with regard to health care; the respect of those differences and the development of approaches to health care with those differences in mind.
Family-Centered Care – Approach that assures the health and well-being of children and their families through a respectful family-professional partnership. It honors the strengths, cultures, traditions and expertise that everyone brings to this relationship. Family-centered care is the standard of practice which results in high quality services.
Family Consumer Partnership – The intentional practice of working with families for the ultimate goal of positive outcomes in all areas through the life course. Family engagement reflects a belief in the value of the family leadership at all levels from an individual, community and policy level.7 Examples of family/consumer partnership for Title V organizations can be found on the Family Voices website at: http://www.familyvoices.org/work/title_v?id=0012
Children with Special Health Care Needs
Care Coordination Services – Services that promote the effective and efficient organization and utilization of resources to assure access to necessary comprehensive services for children with special health care needs and their families.
[Title V Sec. 501(b)(3)] This category sometimes overlaps with services identified as case management.
Case Management Services – Services that assure access to quality prenatal, delivery and postpartum care for pregnant women; Services that assure access to quality preventive and primary care services for infants up to age one. [Title V Sec. 501(b)(4)]
Children With Special Health Care Needs (CSHCN) – Children who have health problems that require more than routine and basic care, which includes children with or at risk of disabilities; chronic illnesses and conditions; and health-related education and behavioral problems. For budgetary purposes, CSHCN are infants or children from birth through the 21st year who have special health care needs and for whom the State has elected to provide with services that are funded through Title V. For planning and systems development, CSHCN are children who have or are at increased risk for a chronic physical, developmental, behavioral, or emotional condition and who also require health and related services of a type or amount that goes beyond that which is required by children generally.
Constructs of a Service System for CSHCN:
State Program Collaboration with Other State Agencies and Private Organizations
States establish and maintain ongoing interagency collaborative processes for the assessment of needs with respect to the development of community-based systems of services for CSHCN. State programs collaborate with other agencies and organizations in the formulation of coordinated policies, standards, data collection and analysis, financing of services, and program monitoring to assure comprehensive, coordinated services for CSHCN and their families.
State Support for Communities
State programs emphasize the development of community-based programs by establishing and maintaining a process for facilitating community systems building through mechanisms, such as technical assistance and consultation, education and training, common data protocols, and financial resources for communities engaged in systems development to assure that the unique needs of CSHCN are met.
Coordination of Health Components of Community-Based Systems
A mechanism exists in communities across the State for coordination of health services with one another. This mechanism includes coordination among providers of primary care, habilitative and rehabilitative services, other specialty medical treatment services, mental health services and home health care.
4. Coordination of Health Services with Other Services at the Community Level
A mechanism exists in communities across the State for coordination and service integration among programs serving CSHCN, which includes early intervention and special education, social services and family support services.
Additional MCH Terms
Acquired Brain Injury – Injury to the brain which is not hereditary, congenital, degenerative, or induced by birth trauma. Traumatic brain injury is a type of acquired brain injury.
Bullying – Unwanted, aggressive behavior among school aged children that involves a real or perceived power imbalance. The behavior is repeated, or has the potential to be repeated, over time. Additional guidance on bullying surveillance is available at: http://www.cdc.gov/violenceprevention/pdf/bullying-definitions-final-a.pdf.
Clinical Genetics – Clinical and laboratory services for individuals and families with, or at risk for, health problems with a heritable component. The application of the principles of inheritance and our knowledge of human genes to diagnose, prevent and treat disease and improve health.
Community – A group of individuals living as a smaller social unit within the confines of a larger one due to common geographic boundaries, cultural identity, a common work environment, common interests and other uniting factors.
Community-based Care – Services provided within the context of a defined community
Community-based Service System – An organized network of services that are grounded in a plan that is developed by a community and based on an assessment of needs.
Genetic Counseling: The process of helping people to understand and adapt to the medical, psychological, and familial implications of genetic contributions to disease. This process integrates: interpretation of family and medical history to assess the chance of disease occurrence or recurrence; education about inheritance, testing, management, prevention, resources and research; counseling to promote informed choices; and adaptation to the risk or condition.
Health Care System – The entirety of the agencies, services, and providers involved or potentially involved in the health care of community members and the interactions among those agencies, services and providers.
(Human) Genetics: The science of genes, heredity and variation in human organisms
Health Care Transition – The process of changing from a pediatric to an adult model of health care. The goal of health care transition (HCT) is to optimize health and assist youth in reaching their full potential. To reach that goal, there’s an active process over time that addresses many aspects of a youth’s life, including medical, psychosocial, educational, and vocational needs and ensures continuity of developmental and age appropriate health care services. Successful transition involves the engagement and participation of the pediatric and adult medical home team, the family and other care givers, and the individual youth collaborating in a positive and mutually respectful relationship.
Medical Home – An approach to providing health care that is accessible, family-centered, continuous, comprehensive, coordinated, compassionate, and culturally effective. Care occurs in an environment of trust and mutual responsibility between the family, patient, and primary care provider. The principle of family-centered care defines the care to be received in a medical home while a team-based approach is central to delivering care in the medical home. Within the medical home, care coordination addresses interrelated medical, dental, mental and behavioral, social, educational, and financial needs to achieve optimal health and wellness outcomes.
Morbidity – A general term for any health condition that encompasses diseases, injuries, and impairments in a population or group.
Mortality – A general term for the incidence of deaths in a population or group. The number of deaths may be reported by age, sex, race/ethnicity, geographic area, and cause of death.
Mortality Rate – The number of deaths occurring in a particular population during a specific time period, as calculated by the number of deaths in that group (numerator) divided by the total population (denominator) and expressed as per 1,000 live births (infant mortality rate only) or per 100,000 population, generally at mid-year.
National Improvement Partnership Network (NIPN) – A network of States who have an Improvement Partnership (IP), which is a durable collaborative of public and private partners that use the science of quality improvement and a systems approach to improve healthcare infrastructure and practice. Established in 2009, NIPN is led by the Vermont Child Health Improvement Program (VCHIP).
National Survey of Children’s Health (NSCH) – Sponsored by the Maternal and Child Health Bureau of the Health Resources and Services Administration, the NSCH examines the physical and emotional health of children ages 0-17 years of age. Special emphasis is placed on factors that may relate to well-being of children, including medical homes, family interactions, parental health, school and after-school experiences, and safe neighborhoods. The NSCH has been fielded three times, in 2003, 2007 and 2011-2012, yielding both State- and nationally-representative data. The NSCH is currently being redesigned, with the first public release of data scheduled for spring 2017.
National Survey of Children with Special Health Care Needs (NS-CSHCN) – This survey was sponsored by the Maternal and Child Health Bureau of the Health Resources and Services Administration. The NS-CSHCN was conducted three times, in 2001, 2005-2006 and 2009-2010, and yielded State- and nationally-representative data on the health care experiences of CSHCN and their families. The NS-CSHCN is currently being combined with the NSCH to provide one unified survey.
Newborn Screening (NBS) – The process of testing newborn babies for some serious, but treatable, conditions. NBS can include a heel stick, hearing screen, and pulse oximetry. The conditions that newborn babies are screened for varies by state. When a newborn screening result is positive, further diagnostic testing is usually required to confirm or specify the results.
Newborn Screening Long-term Follow-up – Comprises the assurance and provision of quality chronic disease management, condition-specific treatment, and age-appropriate preventive care throughout the lifespan of individuals identified with a condition included in newborn screening. Integral to assuring appropriate long-term follow-up are activities related to improving care delivery, including engagement of affected individuals and their families as effective partners in care management, continuous quality improvement through the medical home, research into pathophysiology and treatment options, and active surveillance and evaluation of data related to care and outcomes.
Newborn Screening Short-term Follow-up – The process of ensuring that all newborns are screened, that an appropriate follow-up caregiver is informed of results, that confirmatory testing has been completed, and that the infant has received a diagnosis and, if necessary, treatment.
Preventive Services – Activities aimed at reducing the incidence of health problems or disease prevalence in the community, or the personal risk factors for such diseases or conditions.
Preventive Oral Health Services – Activities that aim to improve and maintain good oral health and function by reducing the onset and/or development of oral diseases or deformities and the occurrence of oro-facial injuries. Examples of preventive oral health services include, but are not limited to, oral hygiene instructions, fluoride treatment, and Dental Sealants.
Primary Care/Primary Care Services – The provision of comprehensive personal health services that include health maintenance and preventive services, initial assessment of health problems, treatment of uncomplicated and diagnosed chronic health problems, and the overall management of an individual’s or family’s health care services.
Recommended Uniform Screening Panel (RUSP) – The RUSP is a list of disorders that are screened at birth and recommended by the Secretary of the Department of Health and Human Services (HHS) for States to screen as part of their State universal newborn screening (NBS) programs. Disorders on the RUSP are chosen based on evidence that supports the potential net benefit of screening, the ability of states to screen for the disorder, and the availability of effective treatments. It is recommended that every newborn be screened for all disorders on the RUSP. Most States screen for the majority of disorders on the RUSP; newer conditions are still in process of adoption. Some states also screen for additional disorders. Although States ultimately determine what disorders their NBS program will screen for, the RUSP establishes a standardized list of disorders that have been supported by the Discretionary Advisory Committee on Heritable Disorders in Newborns and Children (DACHDNC) and the Secretary of HHS.
Safe Infant Sleep Environment – Infant is placed to sleep on its back, in its own crib without blankets or soft items or bed-sharing. Reference: http://pediatrics.aappublications.org/content/early/2011/10/12/peds.2011-2284
Sudden Unexpected Infant Deaths (SUID) - Deaths in infants less than one year of age that occur suddenly and unexpectedly, and in whom the cause of death is not immediately obvious prior to investigation.
Sudden Infant Death Syndrome (SIDS) – The sudden death of an infant less than one year of age that cannot be explained after a thorough investigation is conducted, including a complete autopsy, examination of the death scene, and review of the clinical history.
Systems Development – Activities involving the creation or enhancement of organizational infrastructures at the community level for the delivery of health services and other needed ancillary services to individuals in the community by improving the service capacity of health care service providers.
Traumatic Brain Injury – An alteration in brain function, or other evidence of brain pathology caused by an external force.
2 Gloor, Peter A. “Swarm Creativity.” Competitive Advantage through Collaborative Innovation Networks. (2006)
6 Maternal and Child Health Bureau (MCHB), Guidance and Performance Measures for Discretionary Grants, Health Resources and Services Administration, U.S. Department of Health and Human Services, Denboba and Goode, 1999 and 2004; Cross, Bazron, Dennis and Isaacs, Towards a Culturally Competent System of Care, 1989; Goode and Jones, Definition of Linguistic Competence, National Center for Cultural Competence, Revised 2004; and Denboba, “Federal Viewpoint,” Special Additions Newsletter for Children with Special Health Care Needs, Spring/Summer 2005.
7 Definition provided by the Family and Youth Leadership Committee of AMCHP.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | mlawler |
| File Modified | 0000-00-00 |
| File Created | 2021-01-22 |
© 2026 OMB.report | Privacy Policy