DPRP Standards 2017
Att 3 DPRP Standards 2018.docx
CDC Diabetes Prevention Recognition Program (DPRP)
DPRP Standards 2017
OMB: 0920-0909

Form Approved
OMB No. 0920-0909
Exp. Date: 12/30/2020
CENTER FOR DISEASE CONTROL AND REVENTION
Centers for Disease Control and Prevention Diabetes Prevention Recognition Program
Standards and Operating Procedures
www.cdc.gov/diabetes/prevention/recognition
January 1, 2018
Public reporting burden of this collection of information is estimated to average one hour per responses for the Diabetes Prevention Recognition Program Application Form and one hour per response for the submission of Evaluation Data, including the time for reviewing instructions, searching existing data sources, gathering and maintaining data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not required to respond to a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden to CDC Reports Clearance Officer; 1600 Clifton Road NE, MS D-74, Atlanta, Georgia 30329; ATTN: PRA #0920-0909
II. Standards and Requirements for Recognition 3
B. Safety of Participants and Data Privacy 4
G. Required Curriculum Content 6
H. Requirements for Pending, Preliminary, and Full Recognition 9
III. Applying for Recognition 16
IV. Submitting Evaluation Data to the DPRP 19
VI. Quality Assurance Assessments 27
VII. National Registry of Organizations with CDC Recognition 27
Appendix A. Organizational Capacity Assessment 28
Appendix B. CDC Prediabetes Screening Test 33
Appendix D. Description of the Data Submission and Evaluation Timeline with Examples 41
Appendix E. Using Data for Evaluation 44
Appendix F. DPRP Recommended Procedures for Measuring Weight 47
2018 Centers for Disease Control and Prevention Diabetes Prevention Recognition Program
I. Overview
The Centers for Disease Control and Prevention (CDC) established the CDC Diabetes Prevention Recognition Program (DPRP) (https://www.cdc.gov/diabetes/prevention/lifestyle-program/index.html) as part of the National Diabetes Prevention Program (National DPP) (https://www.cdc.gov/diabetes/prevention/index.html). The DPRP provides information to people at high risk of type 2 diabetes, their health care providers, and health payers about the location and performance of type 2 diabetes prevention programs across organizations with various delivery modes (in-person, online, and combination). The purpose of the DPRP is to recognize organizations that have demonstrated their ability to effectively deliver a proven type 2 diabetes prevention lifestyle change program. The recognition program helps to assure that decisions about individual participation, patient referral, and health insurance benefits are based on accurate, reliable, and trustworthy information. The DPRP is further committed to ensuring health equity by increasing access to type 2 diabetes prevention lifestyle change programs among vulnerable populations, including those living in geographically hard to reach or rural areas, through a variety of modalities.
The DPRP assures the quality of recognized organizations and provides standardized reporting on their performance. The original 2011 DPRP Standards for type 2 diabetes prevention lifestyle change programs and requirements for recognition were based on successful efficacy and effectiveness studies. In one such efficacy study, the U.S. Diabetes Prevention Program research trial (DPP), participants in the lifestyle intervention losing 5-7% of their bodyweight experienced a 58% lower incidence of type 2 diabetes than those who did not receive the lifestyle intervention (see https://www.niddk.nih.gov/about-niddk/research-areas/diabetes/diabetes-prevention-program-dpp/Documents/DPP_508.pdf).The current standards, though still grounded in the earlier research, incorporate innovations from further translational studies, best practices, and expert opinion.
The DPRP has three key objectives:
Assure program quality, fidelity to scientific evidence, and broad use of effective type 2 diabetes prevention lifestyle change programs throughout the United States;
Develop and maintain a registry of organizations that are recognized for their ability to deliver effective type 2 diabetes prevention lifestyle change programs to people at high risk;
Provide technical assistance to organizations to assist staff in effective program delivery and in problem-solving to achieve and maintain recognition status.
This document—CDC Diabetes Prevention Recognition Program Standards and Operating Procedures (or DPRP Standards, for short)—describes in detail the DPRP standards for type 2 diabetes prevention lifestyle change programs and explains how an organization may apply for, earn, and maintain CDC recognition.
II. Standards and Requirements for Recognition
Any organization that has the capacity to deliver an approved type 2 diabetes prevention lifestyle change program may apply for recognition. It is strongly recommended that potential applicants thoroughly read the DPRP Standards (this document) and conduct a capacity assessment (see guidance titled Organizational Capacity Assessment) before submitting an application for recognition.
Recognized organizations will enroll participants according to the following requirements:
All of a program’s participants must be 18 years of age or older and not pregnant at time of enrollment. These programs are intended for adults at high risk for developing type 2 diabetes.
All of a program’s participants must have a body mass index (BMI) of ≥25 kg/m2 (≥23 kg/m2, if Asian American).
All of a program’s participants must be considered eligible based on either:
a recent (within the past year) blood test (may be self-reported for CDC recognition purposes; but, for Medicare DPP suppliers, a self-reported blood test is not permitted) meeting these one of specifications:
Fasting glucose of 100 to 125 mg/dl (CMS eligibility requirement for Medicare DPP suppliers is 110 to 125 mg/dl)
Plasma glucose measured 2 hours after a 75 gm glucose load of 140 to 199 mg/dl
A1c of 5.7 to 6.4
Clinically diagnosed gestational diabetes mellitus (GDM) during a previous pregnancy (may be self-reported; allowed for CDC, but not for Medicare beneficiaries.); or
a positive screening for prediabetes based on the CDC Prediabetes Screening Test (available in the Guidance section of this document or accessible online at https://www.cdc.gov/diabetes/prevention/pdf/prediabetestest.pdf) or a screening result indicating high risk for type 2 diabetes on the hard copy or electronic version of the American Diabetes Association Type 2 Diabetes Risk Test (http://www.diabetes.org/are-you-at-risk/diabetes-risk-test/). .Note: These are not options for eligibility for Medicare beneficiaries.
4. Participants cannot have a previous diagnosis of type 1 or type 2 diabetes prior to enrollment.
5. A health care professional may refer potential participants to the program, but a referral is not required for participation in CDC-recognized programs.
Recognized organizations can retain participants if the following occurs:
1. Participants who develop type 2 diabetes while in the program should be referred to their primary care provider for referrals to ADA-recognized or AADE-accredited diabetes self-management education and support (DSMES) programs and other resources such as Medical Nutrition Therapy (MNT) as appropriate. See Submitting Evaluation Data to the DPRP section for details on how to code these participants.
2. Lifestyle change programs for type 2 diabetes prevention emphasize weight loss and are not appropriate for women who are currently pregnant. Participants who become pregnant may continue at the discretion of their health care provider and the CDC-recognized program delivery organization. See Submitting Evaluation Data to the DPRP section for details on how to code these participants.
Lifestyle change programs for type 2 diabetes prevention typically do not involve physical activity during class time. If physical activity is offered, it is the organization’s responsibility to have procedures in place to assure safety. This may include obtaining a liability waiver from the participant and/or having the participant obtain clearance from his/her primary care provider to participate in physical activity.
Along with the physical safety of the participants, organizations should also be mindful of the need to ensure the privacy and confidentiality of participants’ data. It is the organization’s responsibility to be versed in and to comply with any federal, state, and/or local laws governing individual-level identifiable data, including those laws related to the Health Insurance Portability and Accountability Act (HIPAA), data collection, data storage, data use, and disclosure.
If the lifestyle change program is offered in-person, organizations may use any suitable venue. Organizations should provide private settings in which participants can be weighed or meet individually with Lifestyle Coaches. Some may choose to deliver the lifestyle change program online or via one or more distance learning modalities (e.g., telehealth, remote classroom). Those organizations can obtain weights via digital technology, such as Bluetooth-enabled scales, or accept a self-report from a participant’s own at-home digital scale. (Bluetooth-enabled scales refer to scales that transmit weights securely via wireless or cellular transmission.)
Organizations may offer the program through any or all of the following delivery modes, but are required to submit a single application for each delivery mode being used. This will result in a separate organization code (orgcode) for each delivery mode. Data for each delivery mode will be submitted under the corresponding orgcode during the anniversary month of the effective date for that orgcode.
In-person. Yearlong lifestyle change program delivered 100% in-person for all participants by trained Lifestyle Coaches; meaning, participants are physically present in a classroom or classroom-like setting. Lifestyle Coaches may supplement in-person sessions with handouts, emails, or reminder texts; although none of these may be the sole method of participant communication. Organizations that conduct make-up sessions online, via some other virtual modality, or over the phone are still considered to be delivering the program in-person.
Online. Yearlong lifestyle change program delivered 100% online for all participants; meaning, participants log into course sessions via a computer, laptop, tablet, or smart phone. Participants also must interact with Lifestyle Coaches at various times and by various communication methods, including online classes, emails, phone calls, or texts.
Distance Learning. Yearlong lifestyle change program delivered 100% by trained Lifestyle Coaches via remote classroom or telehealth (i.e., conference call or Skype) where the Lifestyle Coach is present in one location and participants are calling in or video-conferencing from another location is considered Distance Learning.
Combination. Yearlong lifestyle change program delivered as a combination of any of the previously defined delivery modes (1. – 3. above) for all participants by trained Lifestyle Coaches.
Make-up sessions can be provided in any delivery mode, but only one make-up session can be held on the same date as a regularly scheduled session. Furthermore, only one make-up session per participant per week can be held. Make-up sessions must be comparable to regularly scheduled sessions in content and length (approximately one hour). Timeframes for conducting make-up sessions are as follows: 1) missed core sessions must be made up within months 1-6, and 2) missed core maintenance sessions must be made up in months 7-12. Make-up sessions must be offered within these timeframes in order for data to be analyzed. Make-up sessions will be analyzed in the same way as regularly scheduled sessions. See Submitting Evaluation Data to the DPRP section for details on how to code these participants.
The eligibility criteria, skills, knowledge, qualities, and training required of Lifestyle Coaches and Diabetes Prevention Program Coordinators (Program Coordinators) are described in the guidance section of this document titled Guidelines for Staff Eligibility, Roles, Responsibilities, and Sample Job Descriptions.
Recognized organizations are responsible for hiring, training, and supporting their Lifestyle Coaches. Lifestyle Coaches should have the ability to help participants make and sustain positive lifestyle changes. They should also have the understanding and sensitivity to help participants deal with a range of issues and challenges associated with making important lifestyle changes.
Organizations should designate an individual to serve as the Program Coordinator. Program Coordinators should have the ability to serve both as the primary external champions of the program and as the organizational experts for program implementation consistent with the DPRP Standards. Program Coordinators should supervise daily operations of the lifestyle change program, and should provide guidance and support for the Lifestyle Coaches. They should understand the DPRP data collection and submission requirements, including the importance of monitoring program data to ensure quality performance outcomes.
Program Coordinator functions and responsibilities are described in more detail in the position description in the guidance section. When an organization is ready to expand their program, they may require accessing or adding business or leadership support. Leaders and/or business staff may help increase referrals, enrollment, and reimbursement by serving as community spokespersons, by contacting physician offices to encourage referrals, and by working with employers and insurers to increase coverage and benefit uptake for the lifestyle change program.
It is the organization’s responsibility to determine staffing needs for effective implementation. If an organization serves a large number of participants at the same time, it should consider hiring additional Lifestyle Coaches and designating more than one Program Coordinator. Similarly, if an organization serves only a small number of participants at one time, it may consider allowing a single person to serve as both the Lifestyle Coach and the Program Coordinator.
Recognized organizations are responsible for ensuring that an adequate and well-trained workforce is available prior to launching a first class (see the Organizational Capacity Assessment). All Lifestyle Coaches must be trained to the specific curriculum being used by the recognized organization before offering their first class. The recommended minimum length of formal training for new Lifestyle Coaches is at least 12 hours or two days. Formal training is defined as training conducted by one of the four methods listed in Section III. Applying for Recognition, Lifestyle Coach Training Entity. Shortly after completing formal training, Lifestyle Coaches should begin facilitating program sessions and, ideally, should receive on-the-job coaching from a Program Coordinator or other trained Lifestyle Coach.
Since Program Coordinators are responsible for overall program implementation, they must also complete formal training as Lifestyle Coaches. This will permit them to mentor Lifestyle Coaches and serve as back-up Coaches if required.
Recognized organizations are responsible for the ongoing support and continued training of Lifestyle Coaches. They are further responsible for ensuring continued success, quality, and adherence of Lifestyle Coaches to the DPRP Standards. They should provide new Lifestyle Coaches with an opportunity to attend CDC-sponsored webinar trainings on specialized topics such as program delivery (“Welcome to the DPRP”), data submission (“Submit for Success”), and any others offered by CDC. Additional new or refresher training for experienced Coaches is highly recommended, since program evaluation findings have demonstrated that well trained and highly motivated Lifestyle Coaches have a significant impact on participant outcomes. All Lifestyle Coaches should receive additional training each time CDC revises the DPRP Standards, and CDC will offer such training at no cost to organizations.
Training entities that provide formal training to a CDC-approved curriculum are listed on CDC’s website at http://www.cdc.gov/diabetes/prevention/lifestyle-program/staffing-training.html. These entities are not officially endorsed by CDC, but they sign a Memorandum of Understanding (MOU) agreeing to train to a CDC-approved curriculum and to provide training nationally or regionally to organizations recognized by CDC. These entities further agree to provide quality training aligned with the DPRP Standards, which should help ensure competent Lifestyle Coaches. In addition to the training entities listed on the CDC website, training may be provided by 1) a private organization with a national network of program sites, 2) a CDC-recognized virtual organization with national reach, or 3) a Master Trainer (has completed at least 12 hours of formal training as a Lifestyle Coach, has successfully offered the National DPP lifestyle change program for at least one year, and has completed a Master Trainer program offered by a training entity listed on the CDC website.). CDC may conduct random quality assurance assessments of any program, organization, or Master Trainer providing formal training for Lifestyle Coaches to ensure that training requirements are being met.
The National DPP lifestyle change program consists of a series of sessions that present information, provide outside-of-class activities, and offer feedback in stages to optimize behavioral change. The program may be presented in-person or by an online or distance learning modality as described in the Delivery Mode section of this document. As demonstrated in the DPP and other diabetes prevention research trials, the lifestyle change program, as well as the behavioral and motivational content, must be geared toward the overarching goal of preventing type 2 diabetes. In addition, the content should emphasize the need to make lasting lifestyle changes.
The participant’s body weight must be recorded at all sessions. Goals for the yearlong program should focus on moderate changes in both diet and physical activity to achieve modest weight loss in the range of 5-7% of baseline body weight. Strategies used to achieve these goals must include a focus on self-monitoring of diet and physical activity, building self-efficacy and social support for maintaining lifestyle changes, and problem solving strategies for overcoming common challenges to sustaining weight loss.
Recognized organizations must emphasize that the lifestyle change program is specifically designed for prevention of type 2 diabetes in persons at high risk for type 2 diabetes. Therefore, rather than focusing solely on weight loss, the lifestyle change program must also emphasize long-term improvements in nutrition and physical activity. To support learning and lifestyle modification, programs should provide appropriate materials for all participants. The format of the materials (e.g., hard copy, electronic, web-based, etc.) is determined by the program.
Although lifestyle change programs may incorporate innovative ideas and expert opinion, these programs should be based on evidence from efficacy and effectiveness trials. The CDC-developed PreventT2 curriculum is freely available for use and can be found at https://www.cdc.gov/diabetes/prevention/lifestyle-program/curriculum.html. However, organizations may also use other curricula that have been approved by CDC as meeting the standards.
Names of corresponding sessions from the 2012 National DPP and PreventT2 curricula are listed below. Organizations developing their own alternate curricula must use similar session titles and evidence-based content supporting their sessions, and must submit their curricula to CDC for review against the session topics below.
Table 1. Curriculum Topics (Months 1-6)
During the first 6 months (weeks 1-26) of the lifestyle change program, all of these curriculum topics must be covered in at least 16 weekly sessions. Organizations may repeat core modules or use core maintenance modules to offer additional sessions in months 1-6 after they have offered the 16 required weekly core sessions. In this case, organizations must code the use of core maintenance modules in months 1-6 as core sessions. Below are the corresponding sessions from the 2012 National DPP and PreventT2 curricula. All alternate curricula should contain similar session titles and content.
2012 National DPP Curriculum |
PreventT2 Curriculum |
Welcome to the National Diabetes Prevention Program |
Program Overview & Introduction to the Program
|
Being Active - A Way of Life |
Get Active to Prevent T2 |
Move Those Muscles |
Track Your Activity |
Be a Fat and Calorie Detective |
Track Your Food |
Three Ways to Eat Less Fat and Fewer Calories |
Eat Well to Prevent T2 |
Jump Start Your Activity Plan |
Get More Active |
Tip the Calorie Balance |
Burn More Calories Than You Take In |
Healthy Eating |
Shop and Cook to Prevent T2 |
You Can Manage Stress |
Manage Stress |
The Slippery Slope of Lifestyle Change |
Find Time for Fitness |
Make Social Cues Work for You & Talk Back to Negative Thoughts |
Cope with Triggers |
Can use Heart Health from months 7-12 |
Keep Your Heart Healthy |
Problem Solving |
Take Charge of Your Thoughts |
Take Charge of What's Around You |
Get Support |
Four Keys to Healthy Eating Out |
Eat Well Away from Home |
Ways to Stay Motivated |
Stay Motivated to Prevent T2 |
Table 2. Curriculum Topics (Months 7-12)
During the last 6 months (weeks 27-52) of the lifestyle change program, organizations must include at least one session delivered in each of the 6 months (for a minimum of 6 sessions). Organizations wishing to deliver more sessions (going beyond the minimum requirement of one session each month) are encouraged to do so, as this may be beneficial to participants needing additional support. An organization may use a core module to offer additional sessions in months 7-12 after they have offered the required 6 core maintenance modules. In this case, the organization must code the use of the core module in months 7-12 as a core maintenance session. Sessions must focus on topics that reinforce and build on the content delivered during the first 6 months of the lifestyle change program.
Lifestyle Coaches will select topics from either curriculum below based on participants’ needs and interests. Lifestyle Coaches must select from the following topics, and may choose the order in which they are presented.
2012 National DPP Curriculum |
Prevent T2 Curriculum |
Welcome to Sessions 7-12 |
N/A |
Balance Your Thoughts for Long-Term Maintenance |
When Weight Loss Stalls |
Staying on Top of Physical Activity |
Take a Fitness Break |
Stepping up to Physical Activity |
Stay Active Away from Home |
A Closer Look at Type 2 Diabetes |
More About T2 |
More Volume, Fewer Calories |
More About Carbs |
Fats - Saturated, Unsaturated, and Trans Fat |
Can repeat Eat Well to Prevent T2 from months 1-6 |
Healthy Eating - Taking it One Meal at a Time & Food Preparation and Recipe Modification |
Have Healthy Food You Enjoy |
Stress and Time Management |
Get Enough Sleep |
Preventing Relapse |
Get Back on Track |
Handling Holidays, Vacations, and Special Events |
Can repeat Eat Well Away from Home from months 1-6 |
Heart Health |
Stay Active to Prevent T2 |
Healthy Eating with Variety and Balance |
Can repeat Shop and Cook to Prevent T2 from months 1-6 |
Looking Back and Looking Forward |
Prevent T2—for Life! |
Medicare DPP suppliers and ongoing maintenance sessions. Organizations that are Medicare DPP suppliers may repeat any curriculum topic from months 1-6 or months 7-12, with the exception of the introductory session, for use in ongoing maintenance sessions. See the Data Submissions section for details on how to code these sessions.
Use of an alternate curriculum. If an organization chooses to use an alternate curriculum (a curriculum not previously approved or developed by CDC), it must send the curriculum to CDC to be reviewed for consistency with the evidence-based curriculum topics listed above. An organization can submit a culturally adapted curriculum in English to CDC for review before translating it into an appropriate language. An organization must submit all final versions (in English) to CDC for final evaluation and feedback. CDC review of alternate curricula takes approximately 4-6 weeks.
Changes made to a current curriculum. If an organization chooses to change its curriculum to another CDC-approved curriculum, an e-mail notification to CDC at [email protected] is required, and no further steps are needed. If an organization chooses to develop its own curriculum during its tenure in the DPRP, it must notify CDC of the new curriculum at [email protected]. CDC will explain next steps for submission and review of the new curriculum. If an organization chooses to change its curriculum to one that is culturally adapted for a specific population, or translated into another language, or to make other changes to its currently approved curriculum, it must notify CDC at [email protected]. CDC will explain next steps for submission and review of the adapted or translated curriculum. Four to 6 weeks should be allowed for review and approval of new or changed curricula.
The DPRP awards three categories of recognition: pending, preliminary, and full recognition. Organizations are required to submit data every 6 months regardless of recognition status achieved.
Pending Recognition
To begin the process, an organization must submit an application to the DPRP. When the DPRP determines that the organization has met requirements 1-4 in Table 3, the DPRP will assign an approval date and award pending recognition. Concurrent with the initial approval date, the organization will also be assigned an effective date. The effective date is the first day of the month following the approval date and is used to determine due dates for required data submissions. An organization may begin offering classes immediately upon approval and is required to start offering classes no later than 6 months after its effective date.
An organization with pending recognition is required to make its first data submission 6 months after its effective date. An organization may remain in pending status for up to 36 months if it continues to submit the required data every 6 months. The 36 month limitation applies regardless of which version of the DPRP Standards was in effect at the time of application. If an organization has not obtained either preliminary or full recognition by that time, it will be withdrawn from the DPRP and will need to wait 6 months before reapplying. Note: In order to have a data submission every 6 months, an organization must start at least one class every 12 months, with no gaps (i.e., each new class must begin in the month after the previous class ends).
Preliminary Recognition
Preliminary or full recognition is required to become a Medicare DPP supplier. Any organization that has Medicare DPP preliminary recognition will automatically move to CDC preliminary recognition on January 1, 2018. All other transitioning organizations will be evaluated for preliminary recognition based on the criteria listed below.
Organizations will be evaluated for preliminary recognition only at the time of required data submissions. To be evaluated for preliminary recognition, organizations must have submitted a full 12 months of data on at least one completed cohort. A completed cohort is a set of participants that entered into a lifestyle change program that has a fixed first and last session and runs for 12 months. An organization can have multiple cohorts running at the same time.
Organizations will be awarded preliminary recognition when they meet the following criteria:
The 12 month data submission includes at least 5 participants who attended at least 3 sessions in the first 6 months and whose time from first session attended to last session of the lifestyle change program was at least 9 months (a statistical package used by the DPRP calculates months lapsed; this is an automated process).
Of the participants eligible for evaluation in #1, at least 60% attended at least 9 sessions in months 1-6, and at least 60% attended at least 3 sessions in months 7-12 (Requirement 5 in Table 3). Note: The attendance benchmark for months 7-12 is assessed only after a full 12 months has passed from the date of the first session.
PLEASE NOTE: The DPRP will only evaluate organizations for preliminary recognition at the time of their required data submissions. If a new organization wants to be eligible for an evaluation for preliminary recognition at its first 12-month data submission, it will need to begin offering classes immediately after approval of its application and before the effective date. This is the only way that the organization will have the full 12 months of data required for a preliminary recognition evaluation. Organizations that are not eligible for an evaluation for preliminary recognition at 12 months will need to wait until their next required data submission at 18 months.
Organizations may remain in preliminary recognition status for four consecutive 6-month data submission periods (i.e., two years), provided they continue to meet the requirements for preliminary recognition at the 12 month mark. The 24 month limit in preliminary recognition applies regardless of how many months the organization was in pending status. Organizations that either do not maintain preliminary recognition at 12 months or fail to achieve full recognition at 24 months will lose recognition and will need to wait 6 months before reapplying. Loss of preliminary recognition will preclude an organization from participation as a Medicare DPP supplier until preliminary recognition is reachieved.
Full Recognition
Full recognition is required to remain a Medicare DPP supplier after the 24 months of preliminary recognition expires.
Organizations will be evaluated for full recognition only at the time of required data submissions. To be evaluated for full recognition, organizations must have submitted a full 12 months of data on at least one completed cohort.
Organizations will be awarded full recognition when they meet the following criteria:
The 12 month data submission includes at least 5 participants who attended at least 3 sessions in the first 6 months and whose time from first session to last session of the lifestyle change program was at least 9 months.
They meet the requirements for pending and preliminary recognition.
They meet requirements 6-9 in Table 3.
Organizations may remain in full recognition status for four consecutive 6-month data submission periods (i.e., two years). If organizations do not continue to meet full recognition at 24 months, but do meet the requirements for preliminary recognition, they can remain in full recognition status on a Corrective Action Plan for an additional 12 months. Organizations that do not re-achieve full recognition requirements at the 36 month mark will lose recognition and will need to wait 6 months before reapplying. Loss of full recognition will preclude an organization from participation as a Medicare DPP supplier until preliminary recognition is reachieved.
PLEASE NOTE: Organizations can voluntarily withdraw at any point in their timeline, but regardless of circumstances of the withdrawal, they must wait 6 months prior to reapplying.
Data Submissions
There must be at least one session record per participant in the organization’s submission at 6 months post effective date and at least 6 months of participant data in the organization’s submission at 12 months post effective date. This will allow for timely data analysis and provide opportunities for the organization to receive interim feedback on its progress in meeting recognition requirements.
Data may be submitted at any time during the month of the effective date. Data submissions should include data for all participant cohorts held during the data collection period. Organizations failing to submit complete and acceptable data in the month in which it is due or failing to report attendance in a 6-month period will lose recognition and must wait 6 months before reapplying. The DPRP will offer technical assistance to all organizations to help assess their progress toward achieving preliminary or full recognition.
If, after the first evaluation where an organization has at least one complete 12-month cohort, the organization has not achieved all of the requirements for preliminary or full recognition, it will continue in pending recognition status for an additional 6 months. During this period, the DPRP will offer technical assistance to the organization to help it achieve preliminary or full recognition. The DPRP will conduct evaluations for preliminary and full recognition every 6 months when data are submitted. These evaluations will be based on data from participants who attended their first session at least one year but not more than 18 months before the submission due date. If the organization is not successful in achieving preliminary or full recognition by the 36 month evaluation, it will lose pending recognition and must wait 6 months before reapplying.
The Description of the Data Submission and Evaluation Timeline, with Examples section summarizes the data submission and evaluation plan described above and provides examples.
Requirements for Pending, Preliminary, and Full Recognition Status
1. Application for recognition. Submit completed application at https://nccd.cdc.gov/DDT_DPRP/applicationForm.aspx.
2. Lifestyle curriculum. The lifestyle change program must be based on evidence from efficacy and effectiveness trials on type 2 diabetes prevention. The required curriculum topics can be found in the Required Curriculum Content section of this document and the CDC-approved curricula at http://www.cdc.gov/diabetes/prevention/recognition/curriculum.htm.
If the organization chooses to use an alternate curriculum, it must submit it to the DPRP for review to ensure that it meets all of the key elements of the curriculum used in the DPP research trial.
Intervention duration. The lifestyle change program must have a duration of one year. If organizations choose to continue the intervention for a period longer than one year, only the first 365 days of data from each participant will be analyzed to determine recognition.
Intervention intensity. The lifestyle change program must begin with an initial 6-month phase during which a minimum of 16 weekly sessions are offered over a period lasting at least 16 weeks and not more than 26 weeks. Each session must be of a sufficient duration to convey the session content (approximately one hour).
The initial 6-month phase must be followed by a second 6-month phase consisting of at least one session delivered each month (for a minimum of 6 sessions). Organizations wishing to deliver additional sessions (going beyond the minimum requirement of one session each month) are encouraged to do so, as this may be beneficial to participants needing additional support. Each session must be of a sufficient duration to convey the session content (approximately one hour).
There must be regular opportunities for direct, individual, or group interaction between the Lifestyle Coach and the participants either in-person, online, by phone, or through a combination of these. For sessions delivered in-person, participants should be provided a private opportunity for measurement of body weight. Either participants or Lifestyle Coaches may take body weight measurements. However, only Coaches or other trained on-site facilitators may officially record weights and other evaluation data elements used to determine recognition status (described below in requirements 5-9). For sessions delivered online, weights may be either objectively obtained through the use of digital or Bluetooth-enabled scales or by self-report and must be reported during each session. For online Medicare DPP participants, weights can only be obtained through Bluetooth-enabled scales. For guidance on measuring weights, see the DPRP Recommended Procedures for Measuring Weight section of this document.
If participants miss a session during any phase of the intervention, organizations may offer a make-up session. This make-up session can be held either on a day other than a regular class session day or, for the convenience of the participant, on the same day as a regular class session. Only one make-up session per participant can be held per week. Weight recorded at a make-up session should reflect the weight of the participant on the date the make-up session is attended. Physical activity minutes recorded at a make-up session should reflect the number of physical activity minutes logged by participants for the week preceding the missed session.
5. Session attendance during months 1-6 and 7-12 (requirement for preliminary and full recognition)
Months 1-6: Session attendance in months 1-6 will be considered for participants who attended at least 3 sessions in months 1-6 and whose time from first session to last session is at least 9 months.
Months 7-12: Session attendance in months 7-12 will be considered for participants who attended at least 3 sessions in months 1-6 and whose time from first session to last session is at least 9 months.
At least 5 participants per submission who meet the above criteria are required for evaluation. (See requirement 5 in Table 3.)
A yearlong cohort must have at least 60% of its participants attending at least 9 sessions during months 1-6 and at least 60% of its participants attending at least 3 sessions in months 7-12. Note: The attendance benchmark for months 7-12 is assessed only once a full 12 months has passed from the date of the first session.
6. Documentation of body weight (requirement for full recognition)
A yearlong cohort of participants must have body weight documented during at least 80% of the sessions. Evaluation for this requirement is based on all participants attending at least 3 sessions during months 1-6 and whose time from first session to last session is at least 9 months. At least 5 participants per submission who meet this criterion are required for evaluation.
The DPRP recommended procedures for measuring weights are included in the section titled DPRP Recommended Procedures for Measuring Weight.
7. Documentation of physical activity minutes (requirement for full recognition)
A yearlong cohort of participants must have physical activity (PA) minutes documented during at least 60% of the sessions. Evaluation for this requirement is based on all participants attending at least 3 sessions during months 1-6 and whose time from first session to last session is at least 9 months. At least 5 participants per submission who meet this criterion are required for evaluation. Zero (0) minutes reported will not count as documented PA minutes. It is unlikely that participants are not completing any PA minutes, since the curriculum indicates that even simple activities such as house cleaning and gardening can count as PA minutes.
8. Weight loss achieved at 12 months (requirement for full recognition)
The average weight loss across all participants in the yearlong cohort must be a minimum of 5% of starting body weight. The first and last weights recorded for each participant during months 1-12 will be used to calculate this measure. Evaluation for this requirement is based on all participants attending at least 3 sessions during months 1-6 and whose time from first session to last session is at least 9 months. At least 5 participants per submission who meet this criterion are required for evaluation. Note: While CDC is only analyzing average weight loss at 12 months, individual payers, including Medicare, may require more frequent individual weight loss reporting for reimbursement purposes.
9. Program eligibility requirement (requirement for full recognition)
A minimum of 35% of all participants in a yearlong cohort must be eligible for the lifestyle change program based on either a blood test indicating prediabetes or a history of GDM. The remainder (a maximum of 65% of participants) must be eligible based on the CDC Prediabetes Screening Test or the American Diabetes Association (ADA) Type 2 Diabetes Risk Test. If a participant comes into a program on the basis of a risk test score, organizations are permitted to make a one-time change to the participant’s eligibility status based on a post-enrollment blood test. Evaluation for this requirement is based on all participants attending at least 3 sessions during months 1-6 and whose time from first session to last session is at least 9 months. At least 5 participants per submission who meet this criterion are required for evaluation. If a recognized organization is also a Medicare DPP supplier, all Medicare participants must be eligible based solely on a blood test indicating prediabetes. Refer to the Participant Eligibility section for more information. Note: While CDC is setting an organizational requirement for eligibility, individual payers, including Medicare, may impose higher or lower participant level eligibility requirements for blood testing for reimbursement purposes.
Table 3. Summarizes the requirements for recognition. An example of how CDC’s DPRP evaluates organizational performance is included in the Example of Using Data for Evaluation section of this document. The DPRP will calculate all performance indicators for organizations seeking recognition.
Table 3. Requirements for Recognition
|
Standard |
Requirement |
How Evaluated |
When Evaluated |
Recognition Status |
1 |
Application for recognition |
Must provide the organization’s identifying information to the DPRP |
|
Upon receipt of application |
Pending |
2 |
Lifestyle curriculum |
Must meet requirements for curriculum content described in the Required Curriculum Content section |
—or—
|
Upon receipt of application |
Pending |
3 |
Intervention duration |
1 year duration |
Curriculum review |
Upon receipt of application |
Pending |
4 |
Intervention intensity |
Minimum of 16 sessions delivered approximately once per week during months 1-6, followed by a minimum of 6 sessions delivered approximately once per month during months 7-12 |
Curriculum review |
Upon receipt of application |
Pending |
5 |
Session attendance during months 1-6 and 7-12 |
At least 60% of participants attending at least 9 sessions during months 1-6 and at least 60% of participants attending at least 3 sessions in months 7-12. |
Session attendance in months 1-6 will be considered for participants who attended at least 3 sessions in months 1-6 and whose time from first session to last session is at least 9 months. Session attendance in months 7-12 will be considered for participants who attended at least 3 sessions in months 1-6 and whose time from first session to last session is at least 9 months. At least 5 participants per submission who meet these criteria are required for evaluation. |
Every 6 months beginning at 12 or 18 months from the effective date, depending on when an organization starts delivering classes |
Preliminary and Full |
6 |
Documentation of body weight |
Body weights are recorded at a minimum of 80% of the sessions attended |
A yearlong cohort of participants must have body weight documented during at least 80% of the sessions. Includes all participants attending at least 3 sessions during months 1-6 and whose time from first session to last session is at least 9 months. At least 5 participants per submission who meet these criteria are required for evaluation. |
Every 6 months beginning at 12 or 18 months from the effective date, depending on when an organization starts delivering classes |
Full |
7 |
Documentation of physical activity minutes |
Physical activity minutes are recorded at a minimum of 60% of all sessions attended |
A yearlong cohort of participants must have physical activity minutes documented during at least 60% of the sessions. Includes all participants attending at least 3 sessions during months 1-6 and whose time from first session to last session is at least 9 months. At least 5 participants per submission who meet these criteria are required for evaluation. Zero (0) minutes reported will not count as documented physical activity minutes. |
Every 6 months beginning at 12 or 18 months from the effective date, depending on when an organization starts delivering classes |
Full |
8 |
Weight loss achieved at 12 months |
Average weight loss achieved over the entire 12-month intervention period must be a minimum of 5% of starting body weight |
The average weight loss across all participants in the yearlong cohort must be a minimum of 5% of starting body weight. The first and last weights recorded for each participant during months 1-12 will be used to calculate this measure. Includes all participants attending at least 3 sessions during months 1-6 and whose time from first session to last session is at least 9 months. At least 5 participants per submission who meet these criteria are required for evaluation. |
Every 6 months beginning at 12 or 18 months from the effective date, depending on when an organization starts delivering classes |
Full |
9 |
Program eligibility requirement |
Minimum of 35% of participants must be eligible for the yearlong lifestyle change program based on either a blood test indicating prediabetes or a history of GDM. The remainder (maximum of 65% of participants) must be eligible based on the CDC Prediabetes Screening Test or the ADA Type 2 Diabetes Risk Test. |
The last entry for eligibility is used in determining this outcome. Includes all participants attending at least 3 sessions during months 1-6 and whose time from first session to last session is at least 9 months. At least 5 participants per submission who meet these criteria are required for evaluation.
For CDC-recognized organizations that are also Medicare DPP suppliers: All Medicare participants in the yearlong cohort must be eligible based on a blood test indicating prediabetes. |
Every 6 months beginning at 12 or 18 months from the effective date, depending on when an organization starts delivering classes |
Full |
III. Applying for Recognition
CDC welcomes organizations that offer a yearlong lifestyle change program to prevent or delay type 2 diabetes to apply for recognition through the DPRP. Any organization with the capacity to deliver a lifestyle change program meeting DPRP Standards may apply for recognition.
Before an organization applies, leadership and staff should read the Diabetes Prevention Recognition Program Standards and Operating Procedures contained in this document, which describes the criteria for delivering lifestyle change programs that achieve and sustain CDC recognition. The DPRP Standards also contains a capacity assessment. This is a list of questions designed to help an organization determine its readiness to deliver a CDC-recognized lifestyle change program (see section titled Organizational Capacity Assessment). All organizations are strongly encouraged to complete this assessment.
An organization must be ready to start classes immediately or within 6 months after its effective date (the first day of the month immediately following CDC approval of its application). If an organization is not ready to start classes within 6 months, it should postpone submitting an application.
To apply for recognition, an organization should complete the online application at https://www.cdc.gov/diabetes/prevention/lifestyle-program/apply_recognition.html. The organization must indicate whether it will be using a CDC-approved curriculum, such as the PreventT2 curriculum (https://www.cdc.gov/diabetes/prevention/lifestyle-program/curriculum.html), or submitting an alternate curriculum for review. After submitting the application form, the organization will receive a confirmation email. Organizations using a CDC-approved curriculum will normally be notified of the results of the CDC review within 15 working days. Organizations submitting an alternate curriculum for review will normally be notified of the results of the CDC review within 4-6 weeks.
Any organization in the DPRP and assigned a DPRP organization code that contracts with another
CDC-recognized organization to deliver their lifestyle change program must ensure that the
contracted organization uses a CDC-approved curriculum and follows the requirements set forth herein. Upon approval, DPRP staff will inform the organization of its effective date.
Each organization will be required to complete the following elements in the online application form:
Type of Application. Select Initial if this is the first application being submitted. Select Reapplying if this is a subsequent application due to previous withdrawal or loss of recognition.
Organization Code. This code is assigned by the DPRP. Choose Not applicable if this is an initial application. For re-applicants, enter the previously assigned organization code. Organization codes will be published in the DPRP registry corresponding to the organization name on the CDC website here: https://nccd.cdc.gov/DDT_DPRP/Registry.aspx.
3. Organization Name. Upon application approval, the organization name will be published in the DPRP registry on the CDC website.
4. Delivery Mode. An applicant organization can select one delivery mode per each application submitted (either in-person only, online only, distance learning, or combination). Delivery modes will be published in the DPRP registry on the CDC website. For definitions, see the Standards and Requirements for Recognition, Delivery Mode section.
5. Class Type. Select all applicable class types offered: public (open to anyone who qualifies for the lifestyle change program without further restrictions), employee (open only to employees of the organization or the host organization), member-only (open only to member insureds; membership required) or other (write in target audience served such as American Indians/Alaskan Natives, patients, clients, etc.). Organizations offering classes to the public should provide the physical addresses of the classes, or online link to class offerings, to [email protected]. Upon application approval, the class type as well as public class locations will be published in the DPRP registry on the CDC website. If public classes are added, deleted, or changed, organizations should email updated public class location addresses at least every 6 months to [email protected].
6. Organization Physical Address. Provide the main organization’s business office or headquarters address. Upon application approval, this will be published in the DPRP registry and on the CDC website.
7. Organization Mailing Address. Include if different from the Organization Physical Address. DPRP staff will use this address to communicate by mail with the organization (i.e., mailing the certificate of achievement of full recognition if/when achieved).
8. Organization Web Address or URL. Optional. Upon application approval, this will be published in the DPRP registry and on the CDC website. All web addresses must link directly to a location where participants can find information about the organization’s CDC-recognized lifestyle change program and enroll in the program. CDC will not accept or host any other web addresses.
9. Organization Phone Number. Provide the number that participants, payers, and others should call to obtain information about the program. Organizations should not provide a 1-800 number unless a live operator is available. Upon application approval, this will be published in the DPRP registry on the CDC website.
10. Organization Type. Choose the option that best describes the organization type. This refers to an organization’s main headquarters location or main office: Local or community YMCAs; Universities/Schools; State/Local Health Departments; Hospitals/Healthcare Systems/Medical Groups/Physician Practices; Community-Based Organizations/Community Health Centers/Federally Qualified Health Centers; Pharmacies/Drug Stores/Compounding Pharmacies; Indian Health Service/Tribal/Urban Indian Health Systems; Business Coalitions on Health/Cooperative Extension Sites; Worksites/Employee Wellness Programs; Senior/Aging/Elder Centers; Health Plans/Insurers; Faith-Based Organizations/Churches; For-profit Private Businesses; Other (please specify).
11. Program Coordinator Name. Provide the name of the individual who will be the applicant organization’s Program Coordinator. Provide a salutation [e.g., Mr., Mrs., Dr., Ms., Miss, other (please specify)], last name, first name, middle initial, and academic credentials, if applicable [e.g., MD, RN, MPH, MPA, PhD, other (please specify)]. The Program Coordinator’s information will not be included in the DPRP registry.
12. Program Coordinator Contact Information. Provide an email address, phone number, and fax number (if applicable) of the organization’s Program Coordinator. DPRP staff will use this information to communicate with the organization. All DPRP-related documents, reports, and emails will go to the Program Coordinator.
13. Secondary Contact Name. Provide the name of the individual who will be the applicant organization’s Secondary Contact, if applicable. This person would be contacted in the event an organization’s Program Coordinator cannot be reached for routine communication. Provide a salutation [e.g., Mr., Mrs., Dr., Ms., Miss, other (please specify)], last name, first name, middle initial, and academic credentials, if applicable [e.g., MD, RN, MPH, MPA, PhD, other (please specify)]. The Secondary Contact’s information will not be included in the DPRP registry.
14. Secondary Contact Information. Provide the email address, phone number, and fax number of the organization’s Secondary Contact, if applicable. DPRP staff will use this information to communicate with the organization in the event an organization’s Program Coordinator cannot be reached for routine communication, including data-related communication.
15. Lifestyle Coach Training Entity. Provide the name of the training entity the applicant organization will use or has used to train their main Lifestyle Coaches. Choose from 1) a training entity that has an MOU with CDC and is listed on the CDC website (found here: https://www.cdc.gov/diabetes/prevention/lifestyle program/staffing training.html), 2) a private organization with a national network of program sites, 3) a CDC-recognized virtual organization with national reach, or 4) a Master Trainer (has completed at least 12 hours of formal training as a Lifestyle Coach, has successfully offered the National DPP lifestyle change program for at least one year, and has completed a Master Trainer program offered by a training entity listed on the CDC website).
16. Data Preparer Name. Provide the name of the individual who will be the organization’s Data Preparer. This can be either the Program Coordinator or the Lifestyle Coach if a third person is not designated at this time. Provide a salutation [(e.g., Mr., Mrs., Dr., Ms., Miss, other (please specify)], last name, first name, middle initial, and academic credentials, if applicable [(e.g., MD, RN, MPH, MPA, PhD, other (please specify)]. The Data Preparer’s contact information will not be included in the DPRP registry.
17. Data Preparer Contact Information. Provide the email address, phone number, and fax number of the organization’s Data Preparer. (This can be either the Program Coordinator or Lifestyle Coach if a third person is not designated at this time.) DPRP staff will use this information to communicate with the organization about data submission issues, if required.
18. Curriculum. Select either a CDC-approved curriculum (one that CDC has either developed or previously approved for use by your organization) or ‘Other Curriculum’ if the applicant organization is submitting an alternate curriculum for review and approval. If selecting Other Curriculum, provide the completed yearlong curriculum with any supplemental materials, handouts, or web-based content together with the application.
Certification of Application:
Electronic signature. Submitting the application asserts that the organization has thoroughly reviewed the CDC Diabetes Prevention Recognition Program Standards and Operating Procedures and is voluntarily seeking participation in the CDC recognition program. The organization agrees to comply with all of the recognition criteria contained in DPRP Standards, including the transmission of data to CDC every 6 months from the CDC-assigned effective date, for the purpose of program evaluation, continuing recognition, and technical assistance. (Enter name of authorized representative, title of authorized representative, organization name, and date.)
Once an organization’s application has been reviewed and approved, the DPRP will send an email to the organization’s Program Coordinator indicating that the organization has been awarded pending recognition. This email will include the unique organization code assigned by the DPRP, the organization’s effective date (which determines the date the organization’s evaluation data is due to the DPRP) and instructions for data submission. At the same time, the organization will be listed in the DPRP Registry on the CDC website. This entire process takes approximately 15 days.
If an organization submits an alternate curriculum for review and approval by CDC, an initial email indicating receipt will be sent. Organizations should allow 4-6 weeks for review and approval of the application and assignment of an organization code. If an alternate curriculum is not approved by CDC, the application will not be approved. CDC will delineate the reasons why a curriculum is not approved in writing and allow the organization an opportunity to correct any issues and reapply for recognition once the curriculum is amended. Any questions about an organization’s application or the DPRP should be directed to [email protected].
IV. Submitting Evaluation Data to the DPRP
Each CDC-recognized organization (with pending, preliminary, or full recognition) must submit evaluation data to the DPRP every 6 months. This requirement begins 6 months from the organization’s effective date. Four weeks prior to an organization’s first data submission due date, the DPRP will send an email reminder to the organization’s Program Coordinator and other contacts. A second data submission reminder (if necessary) will be sent to the organization’s Program Coordinator and other contacts, as a courtesy, approximately 2 weeks after the data submission due date. If, after this second reminder, the DPRP still does not receive the first evaluation data submission within an additional 4 weeks, the organization will lose recognition and will be removed from the DPRP Registry.
Each data submission must include one record per participant for each session attended during the preceding 6 months. The first data submission must also include records for any sessions attended between the application approval date and the effective date. Subsequent data submissions should not include participant data previously submitted.
All of the data elements listed below must be transmitted to the DPRP. Data must be transmitted as a data file using the comma separated value (CSV) format, which is compatible with the majority of statistical, spreadsheet, and database applications. A CSV template file is provided by CDC. Each row in the data file should represent one session date attended by one participant (i.e., participant will have a new row for each session date). If a participant is absent from a session, no record should be submitted for that participant for that session. Each column in the data file should represent one field containing specific data for the evaluation data elements listed below. There should be no empty fields and no empty cells. When a data value is unknown, the default value should be entered.
Transmitted data must conform to the specifications in the data dictionary included below. The variable names, codes, and values contained in the data dictionary (Table 4.) must be used. Do not make any changes in the spelling. Variables (columns) in the data submission file should have the same names (column headings) and appear in the same order as in the data dictionary.
Organizations should take time to become familiar with all of the data elements and specifications.
No personally identifiable information (PII) from Lifestyle Coaches or participants should be transmitted to the DPRP. All identifiers (except the orgcode, which is provided by CDC) will be assigned and maintained by the organization according to the specifications outlined in the data dictionary.
Evaluation Data Elements (Numbers correspond with Table 4. Data Dictionary: Evaluation Data Elements)
Organization Code. Will be assigned by the DPRP when the organization’s application is approved. Each applicant will have a unique organization code. This code must be included by the applicant organization on all data records submitted.
Participant ID. Will be assigned by the organization to uniquely identify and track participants across sessions. The participant ID must be included on all session attendance records generated for an individual participant. The participant ID should not be based on social security number or other PII. If a participant re-enrolls in a new class, the organization should assign this participant a new participant ID.
Enrollment Source. Will identify the source (person, place, or thing) which led the participant to enroll in the yearlong program (see data dictionary for the appropriate code).
Payer Type. Will identify one, main payment method that participants are using to pay for their participation in the yearlong program (see data dictionary for the appropriate code).
Participant State. The state in which a participant resides should be recorded at enrollment and included on all session attendance records generated for that participant. The two-letter postal abbreviation for the U.S. state or territory should be used. Organizations choosing to deliver the lifestyle program to U.S. citizen participants residing outside of the U.S. or its territories should default to the participant’s U.S. resident state or U.S. Army Post Office (APO) address state.
6- 8) Participant’s Prediabetes Determination. Should be recorded at enrollment and included
on all session attendance records generated for an individual participant. This indicates whether a participant’s prediabetes status was determined by a blood test, a previous diagnosis of GDM, or by screening positive on the CDC Prediabetes Screening Test (see guidance titled CDC Prediabetes Screening Test) or the ADA Type 2 Diabetes Risk Test. Multiple responses are allowed and may be added. For example, if a participant was originally enrolled on the basis of a risk test and then subsequently received a blood test indicating prediabetes, the risk test value remains the same, and the blood test value is changed to a positive.
9) Participant’s Age. Should be recorded at enrollment and the recorded age used throughout all records regardless of a birthday occurring during the yearlong program. If the participant’s age is incorrectly recorded at enrollment (or at the first session), then the age should be corrected on all records. If an organization’s recordkeeping system automatically adjusts the age on a participant’s birthday, then the two recordings of age are okay.
10) Participant’s Ethnicity. Should be recorded at enrollment and included on all session attendance records generated for an individual participant. The participant should self- identify and have the opportunity to choose one of the following: Hispanic/Latino, Not Hispanic/ Latino, or not reported.
11–15) Participant’s Race. Should be recorded at enrollment and included on all session attendance records generated for an individual participant. The participant should self-identify and have the opportunity to choose one or more of the following: American Indian or Alaska Native, Asian or Asian American, Black or African American, Native Hawaiian or Other Pacific Islander, and White. Multiple responses are allowed. This element requires responses for five fields, and each field includes a response for not reported (refer to Table 2, the data dictionary).
16) Participant’s Sex. Should be recorded at enrollment and included on all session attendance records generated for an individual participant. The data record should indicate male, female, or not reported.
17) Participant’s Height. Should be recorded at enrollment and included on all session attendance records generated for an individual participant. Height may be self-reported (i.e., it is not necessary to measure the participant’s height; the participant may simply be asked, “What is your height?” or “How tall are you?”). The participant’s height should be recorded to the nearest whole inch.
18) Education. Will identify the highest grade or year of school the participant completed. This information should be recorded at enrollment and included on all session attendance records generated for an individual participant.
19) Delivery Mode. Will identify the delivery mode, as defined in the Applying for Recognition section, for this specific participant and session (i.e., in-person, online, distance learning).Please note that since this is a session level variable, combination mode does not apply.
20) Session ID. Will identify weekly sessions offered throughout the yearlong program. Session IDs in months 1-6 could be numbered 1 through 26 depending on the frequency of weekly offerings. Session IDs in months 7-12 will all be numbered as 99, and sessions in ongoing maintenance months (for Medicare DPP supplier organizations or other organizations that choose to offer ongoing maintenance sessions) will all be numbered as 88. If a 7-12 month curriculum module (such as one from PreventT2) is used in months 1-6, it should be coded as 1 through 26, since it is being delivered during that timeframe. If a 1-6 month curriculum module is used in months 7-12, it should be coded as 99, since it is being delivered during that timeframe.
21) Session Type. Will identify the session attended within months 1-6 (scheduled core sessions) as “C”, core maintenance sessions attended within months 7-12 as “CM”, or ongoing maintenance sessions as “OM” in the second year (post-yearlong lifestyle change program) for Medicare DPP suppliers or other organizations that choose to offer ongoing maintenance sessions. Medicare DPP suppliers must collect and report data for ongoing maintenance sessions in the same way they do for core and core maintenance sessions, including recording participant weights. CDC will collect these data for Medicare to assist with their continued implementation and assessment of the Medicare DPP expanded model.
Make-up sessions will be identified as “MU” and should be used with the corresponding Session ID that was previously missed by the participant (i.e., the session they are making up). If a 7-12 month curriculum module (such as one from PreventT2) is used in months 1-6, it should be coded as a “C”, since it is being utilized as a core session. If a 1-6 month curriculum module is used in months 7-12, it should be coded as a “CM”, since it is being utilized as a core maintenance session.
22) Session Date. Each time a participant attends a session, the actual date of the session should be recorded. The date should be recorded in mm/dd/yyyy format. A participant should not have more than one record (line of data) for any specific session date, with the exception of make-up sessions. One make-up session per week may be held on the same date as a regularly scheduled session for the convenience of the participant. For online sessions, organizations should record the date each session is completed.
23) Participant’s Weight. Each time a participant attends a session, his or her body weight should be measured and recorded to the nearest whole pound. The weight should be included on the record for that participant and session. For online programs, organizations should record the weight associated with the session completion date.
24) Participant’s Physical Activity Minutes. Once physical activity monitoring has begun in the curriculum, participants will be asked to report the number of minutes of moderate or brisk physical activity completed during the preceding week. This information should be included on the record for that participant and session. If a participant reports doing no activity during the preceding week, then zero (0) minutes should be recorded. Note: Zero (0) minutes reported will not count as documented physical activity minutes.
Table 4. Data Dictionary: Evaluation Data Elements
Data element description |
Variable name |
Coding/valid values |
Comments |
1. Organization Code |
ORGCODE |
Up to 25 alphanumeric characters* |
Required, provided by DPRP |
2. Participant ID |
PARTICIP |
Up to 25 alphanumeric characters* |
Required. Participant ID is uniquely assigned and maintained by the applicant organization and must not contain any PII. |
3. Enrollment Source
|
ENROLL |
1 Non-primary care health professional (e.g., pharmacist, dietitian) 2 Primary care provider/office or specialist (e.g., MD, DO, PA, NP, or other staff at the provider’s office) 3 Community-based organization or community health worker. 4 Self (decided to come on own) 5 Family/friends 6 An employer or employer’s wellness program 7 Insurance company 8 Media (radio, newspaper, billboard, poster/flyer, etc.), national media (TV, Internet ad), and social media (Twitter, Facebook, etc.) 9 Other 10 Not reported |
Required. At enrollment, participants are asked by whom they were referred to this lifestyle change program. If a participant’s referral source is not provided, this variable will be coded as ‘9’. |
4. Payer Type |
PAYER |
1 Medicare 2 Medicaid 3 Private Insurer 4 Self-pay 5 Dual Eligible (Medicare and Medicaid) 6 Grant funding 7 Employer 8 Other 9 Not reported |
Required. At enrollment, participants are asked “Who is the primary payer for your participation in this lifestyle change program?” If a participant’s payer source is not provided, this variable will be coded as ‘9’. |
5. Participant State |
STATE |
Two-letter abbreviation for the U.S. state or territory in which the participant resides |
Required |
6. Participant’s Prediabetes Determination (1 of 3) |
GLUCTEST |
|
Required; acceptable tests include FG, oral glucose tolerance test (OGTT), A1c, or claim code indicating diagnosis of prediabetes. |
7. Participant’s Prediabetes Determination (2 of 3) |
GDM |
|
Required |
8. Participant’s Prediabetes Determination (3 of 3) |
RISKTEST |
|
Required |
9. Participant’s Age |
AGE |
18 to 125 (in years, rounded with no decimals) |
Required |
10. Participant’s Ethnicity |
ETHNIC |
9 Not reported (default) |
Required; if ethnicity is not reported by the participant, this variable will be coded as ‘9’. |
11. Participant’s Race (1 of 5) |
AIAN |
|
Required; if race is not reported by the participant, all of the 5 race variables will be coded as ‘2’. |
12. Participant’s Race (2 of 5) |
ASIAN |
|
Required; if race is not reported by the participant, all of the 5 race variables will be coded as ‘2’. |
13. Participant’s Race (3 of 5) |
BLACK |
|
Required; if race is not reported by the participant, all of the 5 race variables will be coded as ‘2’. |
14. Participant’s Race (4 of 5) |
NHOPI |
|
Required; if race is not reported by the participant, all of the 5 race variables will be coded as ‘2’. |
15. Participant’s Race (5 of 5) |
WHITE |
|
Required; if race is not reported by the participant, all of the 5 race variables will be coded as ‘2’. |
16. Participant’s Sex |
SEX |
9 Not reported |
Required |
17. Participant’s Height |
HEIGHT |
30 to 98 (in inches)
|
Required |
18. Education |
EDU |
1 Less than grade 12 (No high school diploma or GED) 2 Grade 12 or GED (High school graduate) 3 College- 1 year to 3 years (Some college or technical school) 4 College- 4 years or more (College graduate) 9 Not reported (default) |
Required |
19. Delivery Mode |
DMODE |
1 In-person 2 Online 3 Distance learning
|
Required |
20. Session ID |
SESSID |
1 to 26 Core or makeup session —or— 99 Core maintenance or makeup session —or— 88 Ongoing maintenance or makeup session (for Medicare DPP supplier organizations or other organizations that choose to offer ongoing maintenance sessions) |
Required. Core sessions and any core make-up sessions should be numbered 1 through 26. The session ID should correspond to the specific session attended. Core maintenance and any core maintenance make-up sessions should all be coded as ‘99’. Ongoing maintenance and any ongoing maintenance make-up sessions should all be coded as ‘88’. |
21. Session Type |
SESSTYPE |
C Core session CM Core maintenance session OM Ongoing maintenance sessions (for Medicare DPP supplier organizations or other organizations that choose to offer ongoing maintenance sessions) MU Make-up session
|
Required. Any session delivered in months 1-6, even if pulled from months 7-12 of the PreventT2 curriculum content, for example, must be coded as a Core session, C. Any session delivered in months 7-12, even if pulled from months 1-6 of curriculum content, must be coded as a Core Maintenance session, CM. |
22. Session Date |
DATE |
mm/dd/yyyy |
Required. Each data record represents attendance by one participant at one session; must specify actual date of the session. One make-up session per week may be recorded on the same session date as a regularly scheduled session. |
23. Participant’s Weight |
WEIGHT |
70 to 997 (in pounds) —or— 999 Not recorded (default) |
Required. At each session, participants are weighed; weight must be included on the record for that session and participant. Weight may be obtained by the Lifestyle Coach or participant or a Bluetooth-enabled scale. For Medicare DPP suppliers, participants cannot self-report weight. |
24. Participant’s Physical Activity Minutes |
PA |
0 to 997 (in minutes) —or— 999 Not recorded (default) |
Required. At some or all program sessions, participants are asked to report the number of minutes of brisk physical activity they completed in the preceding week. If the number of minutes is greater than or equal to 997, 997 should be used. If a participant reports doing no activity during the preceding week, then zero (0) minutes should be recorded. The default value of 999 should only be used until physical activity monitoring begins in the curriculum.
|
A1c: Hemoglobin A1c test; FG: fasting glucose test; GDM: Gestational Diabetes Mellitus; PII: personally identifiable information (directly or indirectly identifiable); OGTT: oral glucose tolerance test
*All alphanumeric coding values are case sensitive and should not include any spaces or special characters.
Questions about the evaluation data elements or their transmission should be addressed to [email protected].
V. Technical Assistance
Technical assistance is currently available to all recognized organizations through a variety of mechanisms.
Monthly informational webinars to review the standards and data submission requirements;
Additional webinars as needed;
Detailed progress and evaluation reports that include organization-specific summaries and recommendations provided with each report;
Technical assistance calls available to organizations as needed;
Direct access through [email protected] to ask questions/seek clarification, request information, update contact information, or request a technical assistance call;
Downloadable tools and resources on CDC’s National DPP website at http://www.cdc.gov/diabetes/prevention/lifestyle-program/resources/index.html;
Additional resources as available;
Customer Support Center.
VI. Quality Assurance Assessments
Quality assurance assessments and site visits will be conducted to assure that organizations are implementing quality programs aligned with the evidence-based standards, collecting and reporting data properly, and addressing all of the DPRP requirements for CDC-recognized organizations. Technical assistance will be provided as needed during the assessment process.
VII. National Registry of Organizations with CDC Recognition
A list of CDC-recognized organizations with pending, preliminary, and full recognition will be published on the CDC website at https://nccd.cdc.gov/DDT_DPRP/Registry.aspx. Other data fields listed on the CDC website include: organization name, code, main address, state, zip code, phone number, public website (where available and provided to CDC), class type, and who can participate (e.g., public, members only, employees, etc.).
VIII. Guidance Documents
Appendix A. Organizational Capacity Assessment
Introduction
The CDC Diabetes Prevention Recognition Program (DPRP) is a voluntary program for organizations interested in establishing local evidence-based lifestyle change programs for people at high risk for type 2 diabetes. Organizations interested in applying to become a CDC-recognized diabetes prevention program are strongly advised to read the CDC DPRP Standards and Operating Procedures and complete this Capacity Assessment prior to applying for recognition.
Benefits of Completing the Capacity Assessment
Assessing your organization’s capacity will identify areas that may need to be enhanced, prior to applying for CDC recognition, to ensure the organization is able to deliver the yearlong lifestyle change program with quality and fidelity to the evidence-based DPRP Standards and sustain the program long term. Sustainable lifestyle change programs are those that have the capacity to implement the lifestyle change program without federal, state, or local government or other non-governmental grant dollars long-term. In addition, it is necessary for the organization to have appropriate staff with the knowledge, skills, and abilities listed in the Guidelines for Staff Eligibility, Skills and Roles, and Sample Job Descriptions in the CDC DPRP Standards and Operating Procedures document.
Directions for Completing the Capacity Assessment
Refer to the CDC DPRP Standards and Operating Procedures document, available at https://www.cdc.gov/diabetes/prevention/lifestyle-program/apply_recognition.html, when completing this questionnaire.
DPRP Standards Reference - indicates the location of the relevant information in the CDC DPRP Standards and Operating Procedures document.
Organizational capacity assessment questions - read the question and check one box: “yes”, “no”, “unsure”, or “Not Applicable (N/A)”. The “N/A” might apply to online/virtual organizations.
Total the number of “yes”, “no”, “unsure”, and “N/A” responses at the bottom of the questionnaire. If the total number of “no” and “unsure” responses outnumber the “yes” responses, then consider applying at a later date when your organization is ready.
5. For each Capacity Assessment topic with a “no” or “unsure” response, consider working with your organization’s leadership to enhance your readiness before applying for recognition. Partnering with an existing CDC-recognized organization in your community or contacting CDC’s DPRP for technical assistance through [email protected] may be helpful.

Organizational Capacity Assessment for Applicant Organizations to the Centers for Disease Control and Prevention’s (CDC’s) Diabetes Prevention Recognition Program (DPRP)
Capacity Topic |
DPRP Standards Reference |
Organizational Capacity Assessment Questions |
Yes |
No |
Unsure |
N/A |
DPRP Standards |
CDC DPRP Standards and Operating Procedures- https://www.cdc.gov/diabetes/prevention/pdf/dprp-standards.pdf
|
A. Have the following people from your organization read the CDC DPRP Standards and Operating Procedures (DPRP Standards)? |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
||
Leadership and Staff Support |
|
B. Do the following people from your organization support submission of this application for CDC recognition? |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
||
Staff |
Guidelines for Staff Eligibility, Skills and Roles, and Sample Job Descriptions |
C. Does your organization have or plan to hire the following staff (at minimum) with the knowledge, skills, and abilities listed in Guidelines for Staff Eligibility, Skills and Roles, and Sample Job Descriptions of the DPRP Standards? |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
||
Staff Training |
|
D. Does your organization have a plan for Program Coordinator(s) and Lifestyle Coach(es) to offer or attend the following? |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
||
DPRP Evaluation Data Collection and Submission |
Submitting Evaluation Data to the DPRP |
E. Does your organization have staff with the knowledge, skills, and tools needed to collect, enter, and submit the required DPRP evaluation data elements using a comma separated value (CSV) format to the CDC DPRP every 6 months? |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
||
Organization Infrastructure: in-person only |
Location and Delivery Mode |
F. For organizations offering in-person only programs: |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
||
Organization Infrastructure: online only, distance learning, or combination programs |
Location and Delivery Mode |
G. For organizations offering online only, distance learning, or combination programs: |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
||
Eligible Participants |
Participant Eligibility |
H. Does your organization have access to a large number of individuals at high risk for type 2 diabetes that meet the eligibility requirements listed with the DPRP Standards? |
|
|
|
|
Recruitment and Enrollment |
Participant Eligibility |
|
|
|
|
|
Sustainability |
|
J. Does your organization have a plan to sustain the yearlong lifestyle change program long-term without federal, state, or local government or other nongovernmental grant funds? |
|
|
|
|
Tools and Resources |
|
K. Has your organization reviewed the following downloadable tools and resources on CDC’s National Diabetes Prevention Program web site available at https://www.cdc.gov/diabetes/prevention/lifestyle-program/resources/index.html? |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
||
|
|
|
|
|
||
|
|
Total number of boxes check for each column |
|
|
|
|
Appendix B. CDC Prediabetes Screening Test
Prediabetes: You Could Be at Risk
Prediabetes means blood glucose (sugar) levels are higher than normal but not high enough to be diagnostic for type 2 diabetes. Diabetes is a serious disease that can cause heart attack, stroke, blindness, kidney failure, or loss of toes, feet, or legs. Type 2 diabetes can be delayed or prevented in people with prediabetes through effective lifestyle change programs. It is important for people to take the first step by identifying their risk for type 2 diabetes.1
An online link to the CDC’s sponsored screening test can be found at https://www.cdc.gov/diabetes/prevention/pdf/prediabetestest.pdf. The screening test can be given on paper using the document on the following page.
An American Diabetes Association (ADA) screening test is also acceptable and can be found here http://www.diabetes.org/are-you-at-risk/diabetes-risk-test/.
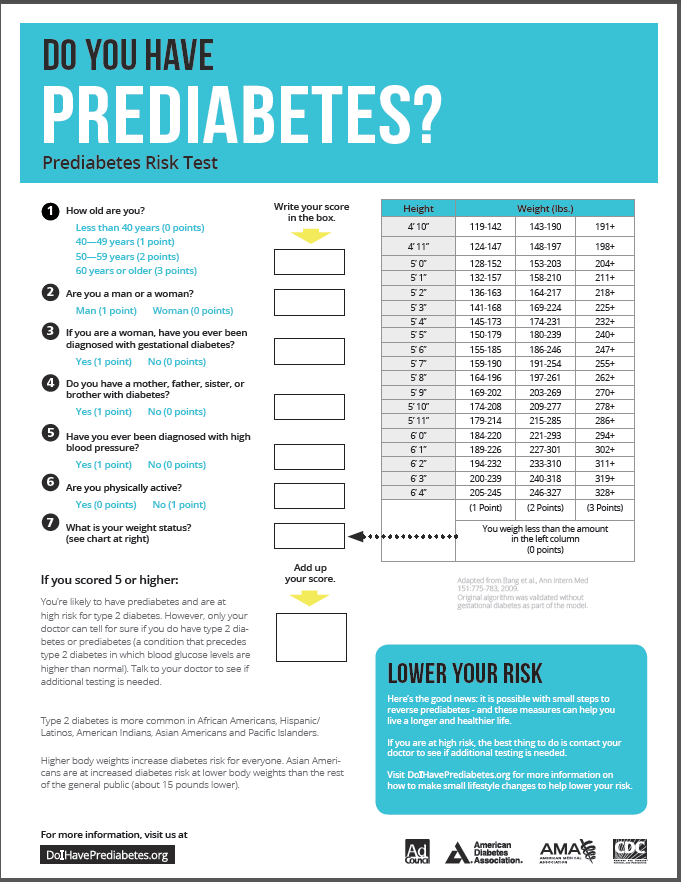
Appendix C. Guidelines for Staff Eligibility, Roles, and Responsibilities; and Sample Position Descriptions
Use of Lifestyle Coaches, Training, and Eligibility
CDC-recognized organizations are responsible for ensuring that an adequate and well-trained workforce is available prior to launching the first class of their type 2 diabetes prevention lifestyle change programs. People who are eligible to be Lifestyle Coaches must have been formally trained to a CDC-approved curriculum for a minimum of 12 hours, or approximately two days, by one of the following: 1) a training entity listed on the CDC website, 2) a private organization with a national network of CDC-recognized program sites, 3) a CDC-recognized virtual organization with national reach, or 4) a Master Trainer, as designated by the CDC-recognized program, who has delivered the lifestyle change program for at least one year and has completed a Master Trainer program offered by a training entity on the CDC website.
Additional training on group facilitation, motivational interviewing, and data collection and interpretation are also essential to effectively carry out Lifestyle Coach responsibilities. While Lifestyle Coaches may have credentials (e.g., RD, RN), credentials are not required. Community Health Workers and lay people can be effective coaches as well.
Recognized organizations are responsible for the ongoing support and continued training of Lifestyle Coaches. Organizations should provide new Lifestyle Coaches with an opportunity to attend CDC-sponsored webinar trainings on specialized topics such as program delivery and data submission. Additional refresher or new skill training for experienced Coaches is not required but is highly recommended and has been shown to have a positive impact on participant outcomes.
Recognized organizations should allocate sufficient time for Lifestyle Coaches to effectively carry out their core responsibilities for delivery of the lifestyle change program. A minimum of 3-5 hours of staff time should be allocated to deliver a one-hour class session. Decisions about the number of Lifestyle Coaches hired and time allocations for program delivery will vary based on the delivery modality (i.e. in-person, online, or combination), the experience of the Lifestyle Coaches, the number of classes and locations served at one time, and whether the organization is in a start-up or expansion phase of program delivery.
Additional time outside of class is typically needed for:
planning and reviewing class session content;
reviewing food and physical activity trackers and providing feedback to individual participants;
arranging and adapting session plans to meet unique participant needs such as language, cultural or dietary restrictions, or hearing or sight impairments;
preparing and monitoring data to support quality improvement; and
interacting with participants between classes to support retention (such as using social media, sending phone call, e-mail, or text reminders, or engaging in online communities).
Position Description- Lifestyle Coach
Role of the Lifestyle Coach: Lifestyle Coaches implement a CDC-approved curriculum designed for effective lifestyle change for preventing or delaying type 2 diabetes, and provide support and guidance to participants in the program.
Responsibilities of the Lifestyle Coach:
Delivering the lifestyle change program and adhering to a CDC-approved curriculum with the required intensity and duration (per the Diabetes Prevention Recognition Program Standards and Operating Procedures, i.e., DPRP Standards) to class participants in an effective, meaningful, and compelling way
Encouraging group or individual participation and interaction through the use of open-ended questions and facilitating commitment to activities for effective lifestyle change
Motivating participants and creating a friendly and interactive environment for group discussion or interactive learning, whether in-person or online
Making learning a shared objective and encouraging peer-to-peer learning
Preparing for each class by reviewing the lesson plan and class content, reviewing data, making reminder calls or sending text messages to participants, and reviewing participants’ food and activity trackers
Being accessible to participants both before and after sessions to answer questions
In collaboration with the Program Coordinator and/or Data Preparer, recording, entering, and submitting session data elements for each participant as noted in Table 2 within the DPRP Standards (i.e., attendance, body weight, total weekly minutes of physical activity, etc.)
When make-up sessions are needed, following up with participants outside of class if they were unable to attend a session that week (during months 1-6) or month (during months 7-12) to offer a make-up session (make-up sessions should consist of a one hour, in-person discussion or can be delivered via phone, video conference, or virtual session)
Supporting and encouraging goal setting and problem solving
Collaborating with the Program Coordinator and others involved in data preparation to regularly monitor participant progress and address any issues to improve participant outcomes
Complying with all applicable laws and regulations, including those governing participant privacy and data security (e.g., the Health Insurance Portability and Accountability Act [HIPAA])
Completing the required organizational trainings, refresher or new skills trainings, and trainings offered by CDC, such as DPRP-related webinars
For organizations seeking reimbursement for delivery to Medicare beneficiaries, Lifestyle Coaches will need to obtain a National Provider Identifier (NPI) number from the Centers for Medicare & Medicaid Services. (Not all Lifestyle Coaches need NPI numbers, only those who teach classes with Medicare beneficiaries in which Medicare is the payer.)
Use of a Program Coordinator, Training, and Eligibility
An organization seeking CDC recognition by participating in the DPRP must designate an individual to serve in the role of Program Coordinator at the time its application is submitted. Because of the important role the Program Coordinator plays in hiring, guiding, and supervising Lifestyle Coaches, it is highly recommended that a Program Coordinator have at least one year of experience working as a Lifestyle Coach. Like Lifestyle Coaches, it is recommended that Program Coordinators have at least 12 hours, or approximately two days, of Lifestyle Coach training aligned to a CDC-approved curriculum.
A Program Coordinator is also responsible for data submission to CDC and receives all programmatic and data-related correspondence from CDC regarding the organization’s recognition status. They are CDC’s point of contact. When an organization has a Program Coordinator staffing change, CDC must be notified of the new point of contact immediately via an email to [email protected]. If a CDC-recognized organization serves a large number of participants at any one time, multiple Program Coordinators may be required. Similarly, if a CDC-recognized organization serves a small number of participants at any one time, it may be appropriate for a Program Coordinator to serve simultaneously in the role of the Lifestyle Coach, provided the proper Lifestyle Coach training has been completed.
Position Description- Program Coordinator
Roles of the Program Coordinator:
Program Coordinators serve as the institutional experts for implementing the lifestyle change program consistent with Diabetes Prevention Recognition Program Standards and Operating Procedures, i.e., DPRP Standards.
They supervise daily operations related to the lifestyle change program and provide guidance and support to Lifestyle Coaches.
Program Coordinators understand program data submitted to CDC’s DPRP and facilitate actions to monitor data and support or mentor Lifestyle Coaches toward quality performance outcomes.
They disseminate information sent from CDC’s DPRP to others in the organization pertaining to training, technical assistance, and an organization’s performance and CDC recognition status.
Program Coordinators may engage in other key functions such as publicity and marketing of the lifestyle change program, which may require assistance from senior leadership in the DPRP organization.
Responsibilities of the Program Coordinator:
Responsibilities to CDC include:
Serving as the direct link between their organization and the CDC and as the lead for distributing DPRP information to relevant staff (i.e., Lifestyle Coaches and data preparers, if applicable)
Participating in technical assistance opportunities offered by CDC’s DPRP and in quality assurance assessments offered by CDC
Notifying the DPRP of changes to organizational information listed on the CDC website in the “Registry of Recognized Organizations” available at https://nccd.cdc.gov/DDT_DPRP/Registry.aspx and class locator “Find a Program Near You” map available at https://nccd.cdc.gov/DDT_DPRP/Programs.aspx
Notifying CDC’s DPRP of any changes to the CDC-approved curriculum used by the organization following the initial application for recognition
Responsibilities to the CDC-recognized organization include:
Hiring and supervising Lifestyle Coaches
Organizing Lifestyle Coach training to a CDC-approved curriculum and ongoing training and skill-building opportunities
Supporting Lifestyle Coaches in implementing the lifestyle change program
Monitoring and evaluating the quality of support that Lifestyle Coaches provide to lifestyle change program participants
Recruiting, screening, and registering eligible participants for the lifestyle change program
Organizing a master schedule of the lifestyle change program classes offered by the CDC-recognized organization
Ensuring adequate publicity for and marketing of the lifestyle change program (Some Program Coordinators have additional responsibility for establishing community partnerships that drive enrollment, referrals, and reimbursement.)
Engaging with payers to bill for program participation, as appropriate
Assisting Lifestyle Coaches with launching each yearlong class (i.e., a set of participants that entered the lifestyle change program with the same start date) and evaluating the cohort based on the goals of the lifestyle change program, realigning program delivery where needed
Assisting in ensuring commitment and retention of lifestyle change program participants
Facilitating a review of program data with Lifestyle Coaches and other relevant staff, including a data preparer as needed, to regularly monitor and strategize how to improve participant performance
Providing class coverage in the absence of a Lifestyle Coach
Complying with all applicable laws and regulations, including those governing participant privacy and data security (e.g., HIPAA)
Completing the required organizational trainings, refresher or new skills trainings, and trainings offered by CDC (e.g., DPRP webinars), and facilitating completion of these trainings by Lifestyle Coaches
For organizations seeking reimbursement for delivery to Medicare beneficiaries, Program Coordinators filling in as Lifestyle Coaches will need to obtain a National Provider Identifier (NPI) number from the Centers for Medicare & Medicaid Services through their CDC-recognized organization. (Not all Lifestyle Coaches need NPI numbers, only those who teach classes with Medicare beneficiaries in which Medicare is the payer.)
Skills, Knowledge, and Abilities of the Lifestyle Coach and Program Coordinator:
-
Skills, Knowledge, and Abilities
Lifestyle Coach
Program Coordinator
Ability to deliver the yearlong lifestyle change program with adherence to a CDC-approved curriculum and DPRP Standards
√
√
Ability to facilitate groups to optimize social interaction, shared learning, and group cohesion appropriate for in–person and/or virtual delivery modes
√
√
Strong interpersonal and communication skills
√
√
Knowledge of the principles of behavior change, including motivational interviewing techniques
√
√
Attention to detail and strong computer (i.e., word processing, working with Excel spreadsheets) and data skills (i.e., data collection, entry, reporting, and interpretation)
√
√
Ability to understand and oversee participant safety-related issues with respect to program delivery and ensuring participant privacy and confidentiality
√
√
Ability to guide behavior change efforts in others without prescribing personal actions or solutions, so that participants increase their self-confidence and capacity to make and sustain positive lifestyle changes
√
√
Ability to communicate empathically to participants, who will likely experience difficulty and frustration at times when trying to adopt and sustain healthy lifestyle behavior changes
√
√
Ability to build strong relationships with individuals and build community within a group, including virtual groups where applicable
√
√
Knowledge of the basic health, nutrition, healthy lifestyle, and fitness principles contained in the CDC-approved curriculum
√
√
Ability to work with people from different backgrounds and cultures; cultural competency related to participants served
√
√
Ability to administer all aspects of delivering the lifestyle change program, provide quality assurance for program delivery, and build a network of referral partners
√
Ability to supervise and evaluate Lifestyle Coaches’ performance according to the CDC DPRP Standards and mentor and provide opportunities for ongoing improvement
√
Ability to work collaboratively and flexibly and serve as a liaison and advocate for the lifestyle change program with internal and external stakeholders (participants, organizational leaders, physicians/health care providers, public health communities, and public and private employers and insurers and other payers that purchase benefits for people with prediabetes)
√
Ability to act as a resource for Lifestyle Coaches by answering questions and providing evidence-based information in a timely manner
√
Ability to ensure adequate publicity for and marketing of the lifestyle change program
√
Ability to engage with payers to bill for program participation, as appropriate. For Medicare programs, ability to navigate Centers for Medicare & Medicaid Services systems and data requirements that are in addition to CDC’s DPRP Standards requirements.
√
Appendix D. Description of the Data Submission and Evaluation Timeline with Examples
Data submission and evaluation for organizations applying on or after January 1, 2018. Please note that for transitioning organizations, there will be a 6-month grace period.
When an application for recognition is approved, the organization will have pending recognition status and may begin offering classes on or after the application approval date. CDC will also assign an “effective date” for the purposes of data submission and evaluation. The effective date will be the first day of the month following approval.
For example, if the application is received on February 20, 2018 and approved by CDC on March 7, 2018, the effective date will be April 1, 2018. The organization will have pending recognition status beginning on the approval date, March 7, 2018.
Classes and data collection may begin on or after the approval date and must begin within 6 months following the effective date.
For example, if the approval date is March 7, 2018 and the effective date is April 1, 2018, the first class session must take place during the period of March 7, 2018 through September 30, 2018. If the applicant will not be able to start classes within 6 months, the organization should defer submitting an application until it is better prepared to begin offering classes.
Data are to be submitted to CDC every 6 months starting at 6 months after the effective date.
For example, if the effective date is April 1, 2018, the first data submission to CDC must occur during October 2018.
The 6 month data submission must include one record for each session attended by each participant during the preceding 6 months. The first data submission must also include records for any sessions attended between the approval date and the effective date.
For example, if the approval date is March 7, 2018 and the effective date is April 1, 2018, the first data submission must include all sessions attended during the period of March 7, 2018 through September 30, 2018, and must be submitted to CDC in October 2018. The second data submission must include all sessions attended during the period October 1, 2018 through March 31, 2019, and must be submitted to CDC in April, 2019.
After the first 6 month data submission, CDC will provide the organization with an interim Progress Report (PR). The organization will continue in pending recognition status.
Once a full 12 months of data are available, CDC will prepare the first Evaluation Report (ER) that assesses whether the organization has met the requirements for preliminary or full recognition. The evaluation will be based on data from participants who attended their first session at least one year but not more than 18 months before the submission due date.
For example, if the approval date is March 7, 2018 and the effective date is April 1, 2018, the first ER (in October 2019) will be based on data from participants who attended their first sessions during the period of March 7, 2018 through September 30, 2018.
If the organization does not meet the requirements for preliminary or full recognition after the first ER, it will remain in pending status and be reevaluated every 6 months. If, at the end of the third year (after 36 months) of pending recognition, the organization still does not meet the requirements for preliminary or full recognition, it will receive notice of Loss of Recognition (LOR) and must wait 6 months before reapplying for pending recognition.
All organizations, including those that have achieved full recognition, are required to submit data every 6 months. An organization must start at least one 12-month class per year in order to have a data submission every 6 months. After each data submission, CDC will prepare a PR or ER (depending on whether data on a full 12-month participant cohort have been submitted at the time of evaluation) and assess whether the organization has met or maintained the requirements for preliminary or full recognition.
Once an organization has achieved preliminary recognition, it may remain in preliminary recognition status for four consecutive 6-month data submission periods (i.e., two years), provided it continues to meet the requirement for preliminary recognition at the 12 month mark. Organizations that do not maintain preliminary recognition at 12 months, or fail to achieve full recognition at the 24 month mark, will lose recognition and will need to wait 6 months before reapplying. Loss of preliminary recognition will preclude an organization from participation as a Medicare DPP supplier until preliminary recognition is reachieved.
If an organization has achieved full recognition, it may remain in full recognition status for four consecutive 6-month data submission periods (i.e., two years). If the organization does not continue to meet full recognition at 24 months, but does meet the requirements for preliminary recognition, it can stay in full recognition on a Corrective Action Plan for an additional 12 months. Organizations that do not re-achieve full recognition at 36 months will lose recognition and will need to wait 6 months before reapplying. Loss of full recognition will preclude an organization from participation as a Medicare DPP supplier until either preliminary or full recognition is reachieved.
If an organization does not submit complete and acceptable data within the month that it is due, the organization will receive notice of LOR and will be required to wait 6 months before reapplying for recognition.
Data submission and evaluation for organizations already in the DPRP by January 1, 2018
Data are to be submitted to CDC every 6 months starting 6 months after the last submission prior to January 1, 2018.
For example, if the last submission was made in October 2017, then the next 6 month submission will be in April 2018.
The first evaluation after January 1, 2018 will be based on data from participants who attended their first session at least one year but not more than 18 months before the submission due date.
c. See items g. – k. in the Data Submission and Evaluation for Organizations Applying on or after January 1, 2018 section above for remaining procedures.
Appendix E. Using Data for Evaluation
Organization requirements for evaluation of data.
In order to have data evaluated, the organization must meet the following criteria:
The organization must have been delivering the program for 12 months, and
The organization must have 5+ participants who have completed 9+ full months in the program and 3+ sessions in months 1-6.
Participant requirements for inclusion in the calculation of outcome measures for Requirements 5-9 found in Table XX “Requirements for Recognition”.
In order to be included in the analysis, participants must meet the following criteria:
All participants included in the analysis must be eligible based on a blood test history of GDM, or a risk test;
All participants included in the analysis must have attended 3+ sessions in months 1-6; and
All participants must have completed 9+ full months in the program.
Sample data for a recognized organization with 6 participants.
Participant |
Prediabetes Determination
|
Number of days in the program
|
Number of sessions attended during months 1-6 |
Number of sessions attended during months 7-12 |
First recorded weight (lbs.) during months 1-12 |
Last recorded weight (lbs.) during months 1-12 |
Percentage weight loss at the last recorded weight
|
1 |
Blood test |
275 |
9 |
3 |
200 |
182 |
9% |
2* |
Ineligible |
180 |
7 |
0 |
175 |
166 |
not used in calculations* |
3 |
Risk test |
330 |
12 |
5 |
305 |
288 |
5.6% |
4 |
Blood test |
360 |
13 |
6 |
181 |
175 |
3.3% |
5 |
History of GDM |
300 |
16 |
4 |
250 |
231 |
7.6% |
6 |
Blood test |
275 |
8 |
3 |
150 |
145 |
3.3% |
7** |
Risk test |
150 |
4 |
0 |
200 |
190 |
not used in calculations** |
* Participant 2 is not included in the analysis, because he/she was deemed ineligible based on Prediabetes Determination.
** Participant 7 is not included in the analysis, because he/she was not in the program for 9+ months.
Calculation of recognition requirements using example table above:
Organization requirements for evaluation of data:
The organization in this example has been delivering the program for 12+ months, and
This organization has 5+ participants who have completed 9+ full months in the program and 3+ sessions in months 1-6.
Participant requirements for inclusion in the analysis:
Of the 7 participants for whom data were submitted, 6 were eligible based on a blood test, history of GDM, or a risk test.
All of the eligible participants attended 3+ sessions in months 1-6, and
Of the 6 eligible participants, 5 completed 9+ full months in the program.
Requirement 5 (Requirement for Preliminary Recognition):
The percent of participants who attend 9+ sessions in months 1-6 must be at least 60% and the percent of participants who attend 3+ sessions in months 7-12 must be at least 60%.
This requirement has two parts. The first part (the percent of eligible participants who attend 9+ sessions in months 1-6 must be at least 60%) is based on participants who had been in the program 9+ months. The second part (the percent of participants who attend 3+ sessions in months 7-12 must be at least 60%) is based on participants who had been in the program 9+ months.
Percent of participants who attend 9+ sessions in months 1-6
= Number of evaluated participants who attended 9+ sessions in months 1-6
Number eligible to be evaluated
= 4/5
= 80%
> 60% (Meets the first part of the requirement)
Percent of participants who attend 3+ sessions in months 7-12
= Number of evaluated participants who attended 3+ sessions in months 7-12
Number eligible to be evaluated
= 5/5
= 100%
> 60% (Meets the second part of the requirement)
Organization achieves Preliminary Recognition
Requirement 8 (Requirement for Full Recognition):
The average weight loss (mean percentage weight loss) achieved over the entire intervention period must be a minimum of 5% of starting body weight.
Average per-participant percentage weight loss at the end of month 12
= Average per-participant percentage weight loss at the end of month 12 among participants eligible to be evaluated
= [ Sum (1-(last weight/first weight)) ] / Number of evaluated participants
= [(1 - (182/200)) + (1 - (288/305)) + (1 - (175/181)) + (1-(231/250)) + (1 – (145/150))] / 5
= 5.8%
> 5% (Meets the requirement)
Organization achieves weight loss requirement for Full Recognition
Appendix F. DPRP Recommended Procedures for Measuring Weight
Place scale on a firm, flat surface.
Make sure the participant removes any coats, heavy sweaters, shoes, keys, or heavy pocket contents. Participants should be advised to wear light clothing.
Each participant should stand in the middle of the scale’s platform with his/her body weight equally distributed on both feet, placing hands at sides, looking straight ahead prior to reading weight.
Weight should be reported to the nearest pound (0.5-0.9 rounds up to the nearest pound, 0.1-0.4 rounds down to the nearest pound).
The same scale should be used to measure weights at each session.
Weights should be measured under similar circumstances at each session and in the same way the initial measurement was taken (e.g., participants wearing similar clothing, measurements taken at the same time of day).
Weight may be measured by the Lifestyle Coach at sessions conducted in-person or by the participant at sessions conducted in-person or virtually.
Organizations using Bluetooth-enabled scales should record only one weight per session date. The closest weight to the recorded session date is the one to be used for each participant. The lowest weight taken during the weekly or monthly session can also be used as long as only one weight is recorded per session date. Bluetooth-enabled refers to scales that transmit weights securely via wireless or cellular transmission.
For participants attending in-person classes who weigh more than once a week, the closest weight to the recorded session date is the one to be used.
Appendix G. Key Terms and Definitions
Application approval date = The date CDC approves an organization’s application for participation in the CDC DPRP. An organization may begin offering classes immediately after receiving its application approval date.
Applicant organization (organization) = An organization that offers the National DPP lifestyle change program and is in the process of applying for pending recognition from the CDC DPRP.
CDC-recognized organization (recognized organization) = An organization that offers the National DPP lifestyle change program and has received pending, preliminary, or full recognition from the CDC DPRP.
Cohort = A completed cohort is a set of participants that entered into a lifestyle change program that has a fixed first and last session and runs for 12 months. An organization can have multiple cohorts running at the same time.
DPP Lifestyle Intervention (lifestyle intervention) = The intervention used during the 2002 DPP research study or replicated during further efficacy and implementation studies.
Data collection period = For the first data submission, the data collection period would include data from sessions held between the application approval date and the data submission due date 6 months later. For subsequent submissions, the data collection period would include data from sessions between the previous due date and the data submission due date 6 months later.
Diabetes Prevention Program (DPP) = The original research study, led by the National Institutes of Health, which showed that making modest behavior changes helped participants lose 5% to 7% of their body weight and reduced the risk of developing type 2 diabetes by 58% in adults with prediabetes (71% for people over 60 years old).
Effective date = The first day of the month following an organization’s application approval date.
Full recognition = The CDC recognition status that, like preliminary (see below), allows organizations to become Medicare DPP suppliers and to begin billing Medicare. Full recognition is required to remain a Medicare DPP supplier after the 24 months of preliminary recognition expires. Organizations will be awarded full recognition when they meet the following criteria:
1. The 12 month data submission includes at least 5 participants who attended at least 3 sessions in the first 6 months and whose time from first session to last session of the lifestyle change program was at least 9 months.
2. They meet the requirements for pending and preliminary recognition.
3. They meet all requirements for documentation of body weight, documentation of physical activity minutes, weight loss achieved at 12 months, and the program eligibility requirement as defined in the DPRP Standards and Operating Procedures.
National Diabetes Prevention Program (National DPP) = A partnership of public and private organizations working collectively to establish, scale, and sustain an evidence-based lifestyle change program for people with prediabetes to prevent or delay onset of type 2 diabetes.
Pending Recognition = The CDC recognition status granted to all applicant organizations once an initial application is approved.
Preliminary Recognition = The CDC recognition status that allows organizations to become Medicare DPP suppliers and to begin billing Medicare. Organizations will be awarded preliminary recognition when they meet the following criteria:
1. The 12 month data submission includes at least 5 participants who attended at least 3 sessions in the first 6 months and whose time from first session attended to last session of the lifestyle change program was at least 9 months.
2. Of the participants eligible for evaluation in #1, at least 60% attended at least 9 sessions in months 1-6, and at least 60% attended at least 3 sessions in months 7-12.
The CDC Diabetes Prevention Recognition Program (DPRP) = The quality assurance arm of the National DPP charged with evaluating organizations’ performance in effectively delivering the lifestyle change program with quality and fidelity. The DPRP awards CDC recognition to organizations that are following a CDC-approved curriculum and achieving meaningful results with participants based on established evidence-based national standards.
The National DPP lifestyle change program (lifestyle change program) = the translated adaptation of the DPP lifestyle intervention which:
• is a yearlong structured program (in-person, online, combination, or other as defined in the DPRP Standards and Operating Procedures) consisting of:
– an initial 6-month phase offering at least 16 sessions over 16–26 weeks and
– a second 6-month phase offering at least one session a month (at least 6 sessions).
• is facilitated by a trained Lifestyle Coach.
• uses a CDC-approved curriculum.
• includes regular opportunities for direct interaction between the Lifestyle Coach and participants.
focuses on behavior modification, managing stress, and social support.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| File Title | DPRP Standards and Operating Procedures |
| Subject | Standards and Operating Procedures |
| Author | Diabetes Prevention Recognition Workgroup |
| File Modified | 0000-00-00 |
| File Created | 2021-01-21 |
© 2026 OMB.report | Privacy Policy