Form #1 Form #1 Separately billing doctors questionnaire
Medical Expenditure Panel Survey Household Component and Medical Provider Component (MEPS-HC and MEPS-MPC)
Attachment 83 MPC SBD Event Form
Separately billing doctors questionnaire
OMB: 0935-0118
Form Approved
OMB No.
0935-0118
Exp. Date 12/31/2015
Attachment 83
Medical expenditure panel survey
medical provider component
event form
FOR
SEPARATELY BILLING DOCTORS
for
reference year 2014
SECTION 1 – omb
OMB HYPERLINK ON FIRST SCREEN
DCS: READ THIS ALOUD ONLY IF REQUESTED BY RESPONDENT.
PRESS NEXT TO CONTINUE IN THIS EVENT FORM
PRESS BREAKOFF TO DISCONTINUE
(Public reporting burden for this collection of information is estimated to average 3 minutes per response, the estimated time required to complete the survey. An agency may not conduct or sponsor, and a person is not required to respond to, a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden, to: AHRQ Reports Clearance Officer Attention: PRA, Paperwork Reduction Project (0935-0118) AHRQ, 540 Gaither Road, Room # 5036, Rockville, MD 20850.)
OMB No. 0935-0118; Exp. Date XX/XX/XXXX
SECTION 2 – INTRODUCTION
[Page 1 – INTRODUCTION (1 of 1)]
Again we are asking about [PATIENT NAME] who received health care services from someone in this practice during [an inpatient stay from BEGIN DATE to END DATE/a long term stay from BEGIN DATE to END DATE/an institutional stay].
Within this stay, when did you have your [first/next] encounter with this patient?
MM/DD/YYYY
Again we are asking about [PATIENT NAME] who received health care services from someone in this practice during [an outpatient visit on DATE/an emergency room visit on DATE/a visit on DATE].
ENTER A DATE IN THIS FORMAT: MM/DD/YYYY
MM/DD/YYYY
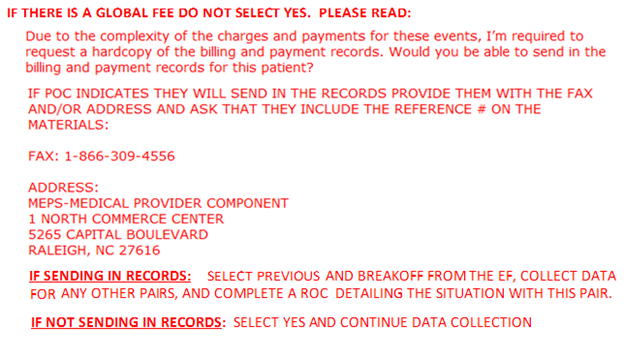
SECTION 3 – GLOBAL FEE
[Page 2 – GLOBAL FEE (1 of 2)]
GLOBAL FEE |
|
||||
B2a. Was the visit on (FILL_VISITDATE ) covered by a global fee, that is, was it included in a charge that covered services received on other dates as well?
EXPLAIN IF NECESSARY: Examples would be a surgeon’s fee covering surgery as well as pre- and post-operative care, or an obstetrician’s fee covering normal delivery as well as pre- and post-natal care.
DK/REF/RETRIEVABLE – GO TO B5a
|
YES=1, NO=2 |
|
|||
[Page 3 – GLOBAL FEE (2 of 2)]
B2b. What other dates of service were covered by this global fee? Please include dates before or after 2014 if they were included in the global fee.
ADMINISTER B2c FOR EACH DATE OF SERVICE COVERED BY THE GLOBAL FEE
|
|
|
|||
B2c. Did (PATIENT NAME) receive the services on GLOBAL FEE DATE in a:
Physician's Office (TYPE=MV); Hospital as an Inpatient (TYPE=SH); Hospital Outpatient Department (TYPE=SO); Hospital Emergency Room (TYPE=SE); or Somewhere else (TYPE=96)?
RECORD RESPONSE UNDER “TYPE”
|
|
|
|||
B2d. Do you expect (PATIENT NAME) will receive any future services that will be covered by this same global fee? |
YES=1, NO=2 |
|
|||
SECTION 4 – SERVICES/CHARGES
[Page 4 – SERVICES/CHARGES (1 of 2)]
B5a. I need to know what services were provided during (this visit/these visits). I would prefer the CPT-4 codes, if they are available.
IF CPT-4 CODES ARE NOT USED, DESCRIBE SERVICES AND PROCEDURES PROVIDED. ENTER UP TO 8 CHARACTERS.
IF CODE BEGINS WITH W, X, Y OR Z, ENTER A DESCRIPTION INSTEAD.
B5b. ASK FOR EACH CPT-4 CODE OR DESCRIPTION: What was the full established charge for this service, before any adjustments or discounts?
EXPLAIN IF NECESSARY: The full established charge is the charge maintained in the physician’s billing system for billing insurance carriers and Medicare or Medicaid. It is the “list price” for the service, before consideration of any discounts or adjustments resulting from contractual arrangements or agreements with insurance plans.
IF NO CHARGE: Some practices that don't charge for each individual service do associate dollar amounts with services for purposes of budgeting or cost analysis. This is sometimes called a "charge equivalent." Could you give me the charge equivalent(s) for (this/these) procedure(s)?
VERIFY: (Is this/Are these) the full established charge(s) or “list price” for (this/these) service(s)? IF NOT, RECORD FULL ESTABLISHED CHARGES
IF PROVIDER APPLIED THE CHARGE FOR THIS SERVICE TO SOME OTHER SERVICE ON THIS DATE, ENTER -4. NOTE: WE NEVER ENTER $0 FOR A CHARGE
C2. [I show the total charges as _________ / I show the payment as undetermined. / I show the payment as _______, although one or more payments are missing ] Is that correct? IF INCORRECT, CORRECT ENTRIES SHOWN ABOVE AS NEEDED. |
CPT-4 CODE DESCRIPTION
a. MCPT# MCPTDS#
b. MCPT# MCPTDS#
c. MCPT# MCPTDS#
d. MCPT# MCPTDS#
e. MCPT# MCPTDS#
f. MCPT# MCPTDS#
g. MCPT# MCPTDS#
h. MCPT# MCPTDS#
i. MCPT# MCPTDS#
j. MCPT# MCPTDS#
k. MCPT# MCPTDS#
TOTAL CHARGES
|
What was the full established charge, or charge equivalent, for this service?
$MCPTCH#
$
$
$
$
$
$
$
$
$
$
$ |
|
SECTION 5 – REIMBURSEMENT TYPE
[Page 5 – REIMBURSEMENT TYPE (1 of 1)]
C3. Was the practice reimbursed for (this visit/these visits) on a fee-for-service basis or a capitated basis?
EXPLAIN IF NECESSARY: Fee-for-service means that the practice was reimbursed on the basis of the services provided.
Capitated basis means that the patient was enrolled in a prepaid managed care plan where reimbursement is not tied to specific visits.
IF IN DOUBT, CODE FEE-FOR-SERVICE.
|
Fee-for-service basis =1 Capitated basis =2
|
SECTION 6 – SOURCES OF PAYMENT
[Page 6 – SOURCES OF PAYMENT (1 of 1)]
C4. From which of the following sources has the practice received payment for (this visit/these visits) and how much was paid by each source? Please include all payments that have taken place between (FILL DATE) and now for this (stay/visit).
[DCS ONLY] IF NAME OF INSURER, PUBLIC, OR HMO, PROBE: And is that Medicare, Medicaid, or private insurance?
[DCS ONLY] IF PROVIDER VOLUNTEERS THAT PATIENT PAYS A MONTHLY PREMIUM, VERIFY: So, you receive a monthly payment rather than payment for the specific service? IF YES: GO BACK TO C3 AND CODE AS CAPITATED BASIS.
RECORD PAYMENTS FROM ALL APPLICABLE PAYERS
IF ANY OF THE PAYMENTS IS A LUMP SUM THAT IS NOT YET ALLOCATED, ENTER F8 IN THE APPROPRIATE FIELD(S).
C5. [I show the total payment as _____ / I show the payment as undetermined. / I show the payment as _____, although one or more payments are missing] Is that correct?
IF NO, CORRECT ENTRIES ABOVE AS NEEDED.
|
SOURCE
a. Patient or Patient’s Family;
b. Medicare;
c. Medicaid;
d. Private Insurance;
e. VA/Champva;
f. Tricare;
g. Worker’s Comp; or
h. Something else? (IF SOMETHING ELSE: What was that?)
|
PAYMENT AMOUNT
$
$
$
$
$
$
$
$
$
|
SECTION 7 – VERIFICATION OF PAYMENT
[Page 7 – VERIFICATION OF PAYMENT (1 of 1)]
C5a. I recorded that the payment(s) you received equal YES, FINAL PAYMENTS RECORDED IN C4 AND C5 =1
the charge(s). I would like to make sure that I have NO =2
this recorded correctly. I recorded that the total
payment is [SYSTEM WILL DISPLAY TOTAL
PAYMENT FROM C5]. Does this total payment
include any other amounts such as adjustments or
discounts, or is this the final payment?
IF NECESSARY, READ BACK AMOUNT(S)
RECORDED IN C4.
.
PLC1. It appears that the total payments were less than the total charge. Is that because …
a. There were adjustments or discounts YES=1 NO=2
b. You are expecting additional payment YES=1 NO=2
c. This was charity care or sliding scale YES=1 NO=2
d. This was bad debt YES=1 NO=2
ELIGVET2.
It appears that the total payments were less than the total charges. Is that because the person is an eligible veteran?
YES=1,
NO=2
DCS: IF THE POC IS CONFUSED BY THE QUESTION, ANSWER THE QUESTION “NO”
SECTION 8 – DIFFERENCE BETWEEN PAYMENTS AND CHARGES
[Page 8–DIFFERENCE BETWEEN PAYMENTS AND CHARGES (1 of 1)]
Are you expecting additional payment from:
It appears that the total payments were more than the total charges. Is that correct?
YES=1, NO=2
DCS: IF THE ANSWER IS “NO” PLEASE GO BACK TO C5 (VERIFY TOTAL PAYMENTS) TO RECONFIRM CHARGES AND PAYMENTS AS NEEDED.
|
Expecting additional payment i. Patient or Patient’s Family? YES=1, NO=2 j. Medicare? YES=1, NO=2 k. Medicaid? YES=1, NO=2 l. Private Insurance? YES=1, NO=2 m. VA/Champva? YES=1, NO=2 n. Tricare? YES=1, NO=2 o. Worker’s Comp? YES=1, NO=2 p. Something else? YES=1, NO=2 (IF SOMETHING ELSE: What was that?)
|
SECTION 9 – CAPITATED BASIS
[Page 9–CAPITATED BASIS (1 of 4)] |
|
C7a. What kind of insurance plan covered the patient for (this visit/these visits)? Was it:
[DCS ONLY] IF NAME OF INSURER, PUBLIC, OR HMO, PROBE: And is that Medicare, Medicaid, or private insurance?
C7a(g) – “Other Specify” menu Auto or Accident Insurance CHDP/CHIP Indian Health Service State Public Mental Plan State/County/Local Program Other
|
a. Medicare; YES=1, NO=2 b. Medicaid; YES=1, NO=2 c. Private Insurance; YES=1, NO=2 d. VA/Champva; YES=1, NO=2 e. Tricare; YES=1, NO=2 f. Worker’s Comp; or YES=1, NO=2 g. Something else? YES=1, NO=2 (IF SOMETHING ELSE: What was that?)
|
C7b. Was there a co-payment for (this visit/these visits)?
|
YES=1, NO=2
|
|
|
[Page 10–CAPITATED BASIS (2 of 4)]
C7c. How much was the co-payment? |
$
|
C7d. Who paid the co-payment? Was it:
[DCS ONLY] IF NAME OF INSURER, PUBLIC, OR HMO, PROBE: And is that Medicare, Medicaid, or private insurance?
C7d(e) – Include the following options in a drop down menu for the “Other Specify”; Auto or Accident Insurance CHDP/CHIP Indian Health Service State Public Mental Plan State/County/Local Program Other
[Page 11–CAPITATED BASIS (3 of 4)]
C7e. Do your records show any other payments for (this visit/these visits)?
|
a. Patient or Patient’s Family; YES=1, NO=2 b. Medicare; YES=1, NO=2 c. Medicaid; YES=1, NO=2 d. Private Insurance; or YES=1, NO=2 e. Something else? YES=1, NO=2 (IF SOMETHING ELSE: What was that?)
YES=1, NO=2
|
[Page 12–CAPITATED BASIS (4 of 4)]
C7f. From which of the following other sources has the practice received payment for (this visit/these visits) and how much was paid by each source? Please include all payments that have taken place between (FILL_VISITDATE ) and now for this (stay/visit).
RECORD PAYMENTS FROM ALL APPLICABLE PAYERS
[DCS ONLY] IF NAME OF INSURER, PUBLIC, OR HMO, PROBE: And is that Medicare, Medicaid, or private insurance?
. (h) – “Other Specify” menu Auto or Accident Insurance CHDP/CHIP Indian Health Service State Public Mental Plan State/County/Local Program Other
|
SOURCE a. Patient or Patient’s Family; b. Medicare; c. Medicaid; d. Private Insurance; e. VA/Champva; f. Tricare; g. Worker’s Comp; or h. Something else? (IF SOMETHING ELSE: What was that?)
|
PAYMENT AMOUNT $ $ $ $ $ $ $
$
|
SECTION 10 – LUMP SUM PAYMENTS
[Page 13 – LUMP SUM PAYMENT (1 of 1)]
CHECK WAS ANY LUMP SUM ASSOCIATED WITH THE SOURCES OF PAYMENT?
YES
NO
SECTION 11 – ENCOUNTER
[Page 14 – ENCOUNTER (1 of 1)]
Were any other services provided to (PATIENT NAME) during the inpatient stay of (DATE)
that we have not recorded?
1 YES
2 NO
SECTION 12 – FINISH SCREEN
[Page 15 – FINISH SCREEN (1 of 1)]
PRESS VALIDATE TO COMPLETE THIS EVENT FORM.
SBD_Event_Form Page
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| File Title | MEDICAL EVENT FORM |
| Author | Lori Houck |
| File Modified | 0000-00-00 |
| File Created | 2021-01-21 |
© 2026 OMB.report | Privacy Policy