Federal IDR Process for Services relating to Nonparticipating Providers or Nonparticipating Emergency Facilities
No Surprises Act: IDR Process
IDR_Initiation_Webform
Federal IDR Process for Services relating to Nonparticipating Providers or Nonparticipating Emergency Facilities
OMB: 1210-0169
Welcome Page
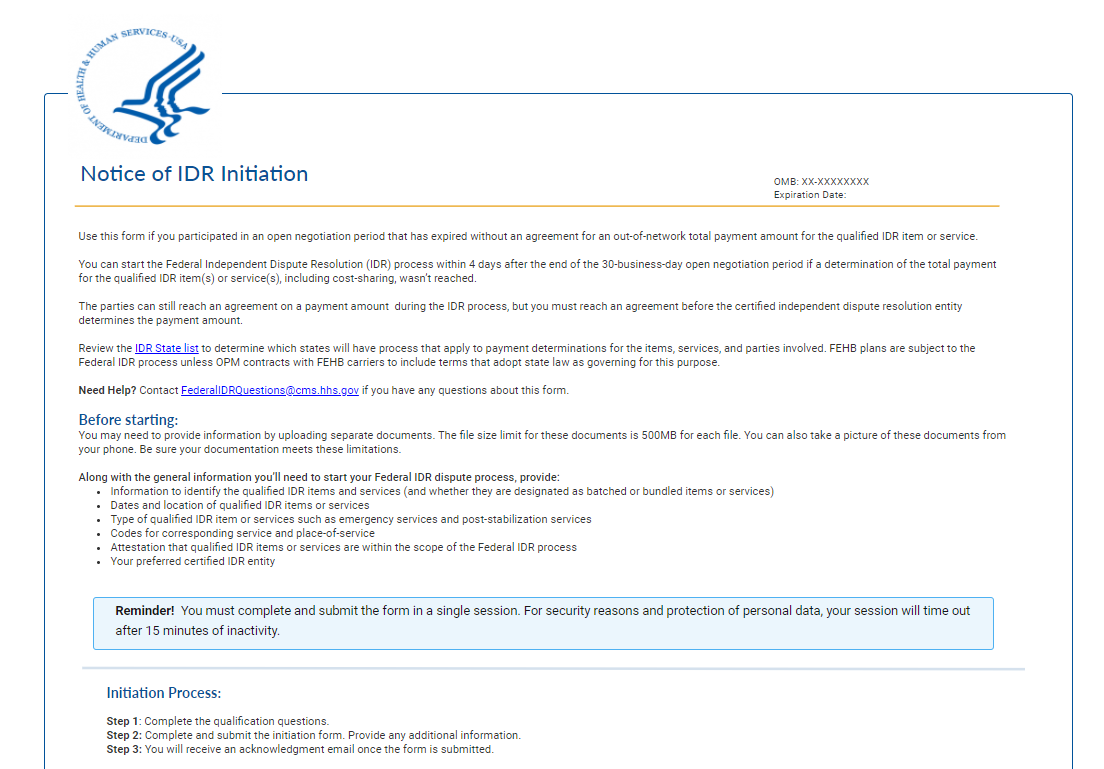
Notice of IDR Initiation
Use this form if you participated in an open negotiation period that has expired without an agreement for an out-of-network total payment amount for the qualified IDR item or service.
You can start the Federal Independent Dispute Resolution (IDR) process within 4 days after the end of the 30-business-day open negotiation period if a determination of the total payment for the qualified IDR item(s) or service(s), including cost-sharing, wasn’t reached.
The parties can still reach an agreement on a payment amount during the IDR process, but you must reach an agreement before the certified independent dispute resolution entity determines the payment amount.
Review the IDR State list to determine which states will have processes that apply to payment determinations for the items, services, and parties involved. FEHB carriers are subject to the Federal IDR process unless OPM contracts with FEHB carriers to include terms that adopt state law as governing for this purpose.
Need help? Contact [email protected] if you have any questions about this form.
Before starting:
You may need to provide information by uploading separate documents. The file size limit for these documents is 500MB for each file. Be sure your files meet these limitations.
Along with the general information you’ll need to start your Federal IDR dispute process, provide:
Information to identify the qualified IDR items or services (and whether they are designated as batched or bundled items or services)
Dates and location of qualified IDR items or services
Type of qualified IDR items or services such as emergency services and post-stabilization services
Codes for corresponding service and place-of-service
Attestation that qualified IDR items or services are within the scope of the Federal IDR process
Your preferred certified IDR entity
Reminder - You must complete and submit the form in a single session. For security reasons and protection of personal data, your session will time out after 15 minutes of inactivity.
Initiation Process:
Step 1: Complete the qualification questions.
Step 2: Complete and submit the initiation form. Provide any additional information.
Step 3: You will receive an acknowledgment email once the form is submitted.
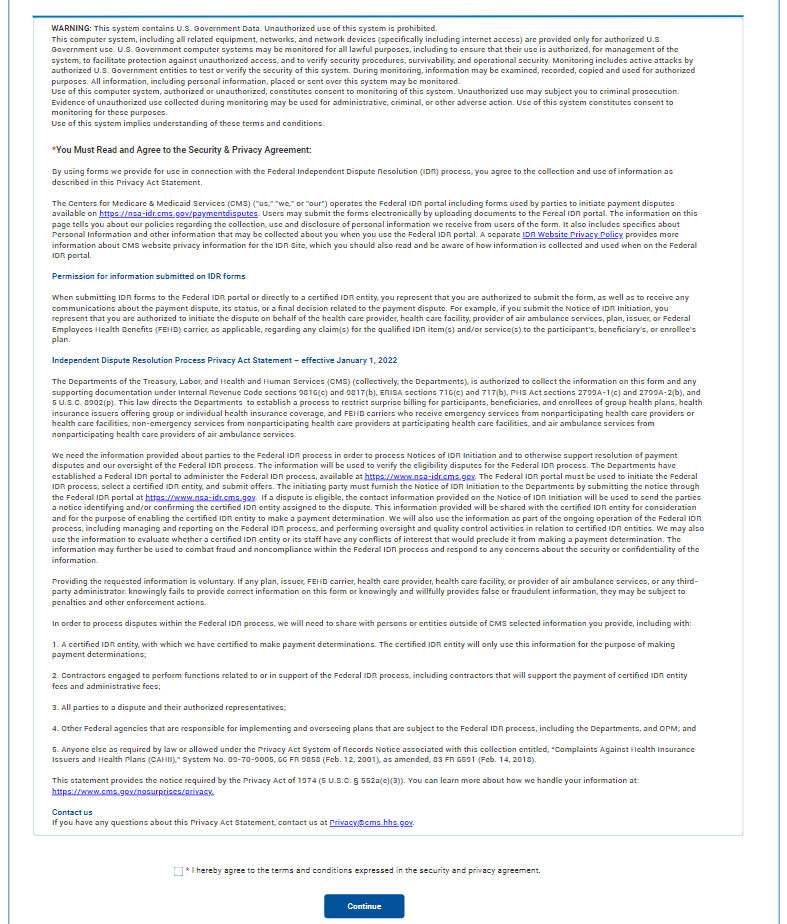
WARNING: This system contains U.S. Government Data. Unauthorized use of this system is prohibited.
This computer system, including all related equipment, networks, and network devices (specifically including internet access) are provided only for authorized U.S. Government use. U.S. Government computer systems may be monitored for all lawful purposes, including to ensure that their use is authorized, for management of the system, to facilitate protection against unauthorized access, and to verify security procedures, survivability, and operational security. Monitoring includes active attacks by authorized U.S. Government entities to test or verify the security of this system. During monitoring, information may be examined, recorded, copied and used for authorized purposes. All information, including personal information, placed or sent over this system may be monitored.
Use of this computer system, authorized or unauthorized, constitutes consent to monitoring of this system. Unauthorized use may subject you to criminal prosecution. Evidence of unauthorized use collected during monitoring may be used for administrative, criminal, or other adverse action. Use of this system constitutes consent to monitoring for these purposes.
Use of this system implies understanding of these terms and conditions.
*You must read and agree to the Security & Privacy Agreement:
By using forms we provide for use in connection with the Federal Independent Dispute Resolution (IDR) process, you agree to the collection and use of information as described in this Privacy Act Statement.
The Centers for Medicare & Medicaid Services (CMS) ("us," "we," or "our") operates the Federal IDR portal including forms used by parties to payment disputes available on https://nsa-idr.cms.gov/paymentdisputes. Users may submit the forms electronically by uploading documents to the Federal IDR portal. The information on this page tells you about our policies regarding the collection, use and disclosure of personal information we receive from users of the form. It also includes specifics about Personal Information and other information that may be collected about you when you use the Federal IDR portal. A separate IDR Website Privacy Policy provides more information about CMS website privacy information for the IDR Site, which you should also read and be aware of how information is collected and used when on the Federal IDR portal.
Permission for information submitted on IDR forms
When submitting IDR forms to the Federal IDR portal or directly to a certified IDR entity, you represent that you are authorized to submit the form, as well as to receive any communications about the payment dispute, its status, or a final decision related to the payment dispute. For example, if you submit the Notice of IDR Initiation, you represent that you are authorized to initiate the dispute on behalf of the health care provider, health care facility, provider of air ambulance services, plan, issuer, or Federal Employees Health Benefits (FEHB) carrier, as applicable, regarding any claim(s) for the qualified IDR item(s) and/or service(s) to the participant’s, beneficiary’s, or enrollee’s plan.
Independent Dispute Resolution Process Privacy Act Statement
The Departments of the Treasury, Labor, and Health and Human Services (CMS) (collectively, the Departments), are authorized to collect the information on this form and any supporting documentation under Internal Revenue Code sections 9816(c) and 9817(b), ERISA sections 716(c) and 717(b), PHS Act sections 2799A-1(c) and 2799A-2(b), and 5 U.S.C. 8902(p). This law directs the Departments to establish a process to restrict surprise billing for participants, beneficiaries, and enrollees of group health plans, health insurance issuers offering group or individual health insurance coverage, and FEHB carriers who receive emergency services from nonparticipating health care providers or health care facilities, non-emergency services from nonparticipating health care providers at participating health care facilities, and air ambulance services from nonparticipating health care providers of air ambulance services.
The information will be used to verify the eligibility disputes for the Federal IDR process. The Departments have established a Federal IDR portal to administer the Federal IDR process, available at https://www.nsa-idr.cms.gov. The Federal IDR portal must be used to initiate the Federal IDR process, select a certified IDR entity, and submit offers. The initiating party must furnish the Notice of IDR Initiation to the Departments by submitting the notice through the Federal IDR portal at https://www.nsa-idr.cms.gov. If a dispute is eligible, the contact information provided on the Notice of IDR Initiation will be used to send the parties a notice identifying and/or confirming the certified IDR entity assigned to the dispute. This information provided will be shared with the certified IDR entity for consideration and for the purpose of enabling the certified IDR entity to make a payment determination. We will also use the information as part of the ongoing operation of the Federal IDR process, including managing and reporting on the Federal IDR process, and performing oversight and quality control activities in relation to certified IDR entities. We may also use the information to evaluate whether a certified IDR entity or its staff have any conflicts of interest that would preclude it from making a payment determination. The information may further be used to combat fraud and noncompliance within the Federal IDR process and respond to any concerns about the security or confidentiality of the information.
Providing the requested information is voluntary. If any plan, issuer, FEHB carrier, health care provider, health care facility, provider of air ambulance services, or any third-party administrator knowingly fails to provide correct information on this form or knowingly and willfully provides false or fraudulent information, they may be subject to penalties and other enforcement actions.
In order to process disputes within the Federal IDR process, we will need to share with persons or entities outside of CMS selected information you provide, including with:
1. A certified IDR entity, with which we have certified to make payment determinations. The certified IDR entity will only use this information for the purpose of making payment determinations;
2. Contractors engaged to perform functions related to or in support of the Federal IDR process, including contractors that will support the payment of certified IDR entity fees and administrative fees;
3. All parties to a dispute and their authorized representatives;
4. Other Federal agencies that are responsible for implementing and overseeing plans that are subject to the Federal IDR process, including the Departments, and OPM; and
5. Anyone else as required by law or allowed under the Privacy Act System of Records Notice associated with this collection entitled, “Complaints Against Health Insurance Issuers and Health Plans (CAHII),” System No. 09-70-9005, 66 FR 9858 (Feb. 12, 2001), as amended, 83 FR 6591 (Feb. 14, 2018).
This statement provides the notice required by the Privacy Act of 1974 (5 U.S.C. § 552a(e)(3)). You can learn more about how we handle your information at: https://www.cms.gov/nosurprises/privacy.
Contact us
If you have any questions about this Privacy Act Statement, contact us at [email protected].
Checkbox - * I hereby agree to the terms and conditions expressed in the security and privacy agreement.
Button – Continue
Glossary Info Text (appears on every page after Welcome screen)
Need help with terms? See a glossary of insurance terms and definitions that are commonly used in this form.
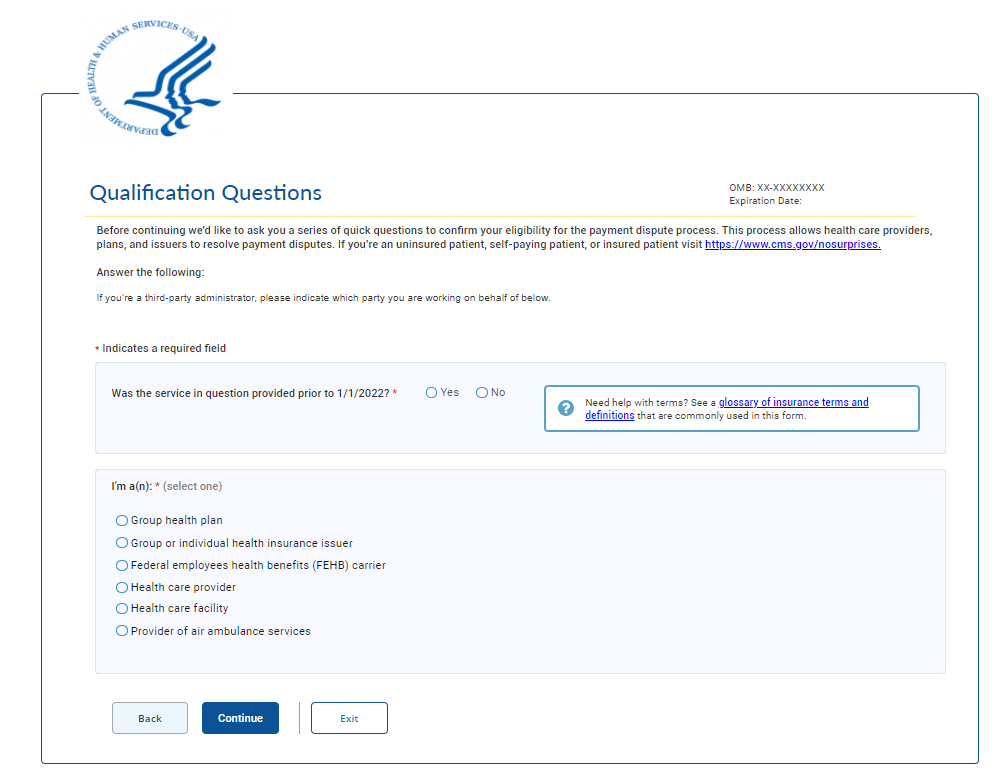
Qualification Questions 1
Before continuing we'd like to ask you a series of quick questions to confirm your eligibility for the payment dispute process. This process allows health care providers, plans, and issuers to resolve payment disputes. If you're an uninsured patient, self-paying patient, or insured patient visit https://www.cms.gov/nosurprises.
Answer the following:
If you’re a third-party administrator, please indicate which party you are working on behalf of below.
* Indicates a required field
Was the service in question provided prior to 1/1/2022? * Yes / No
I'm a(n): * (select one)
Group health plan
Group or individual health insurance issuer
Federal employees health benefits (FEHB) carrier
Health care provider
Health care facility
Provider of air ambulance services
Buttons – Back, Continue, Exit
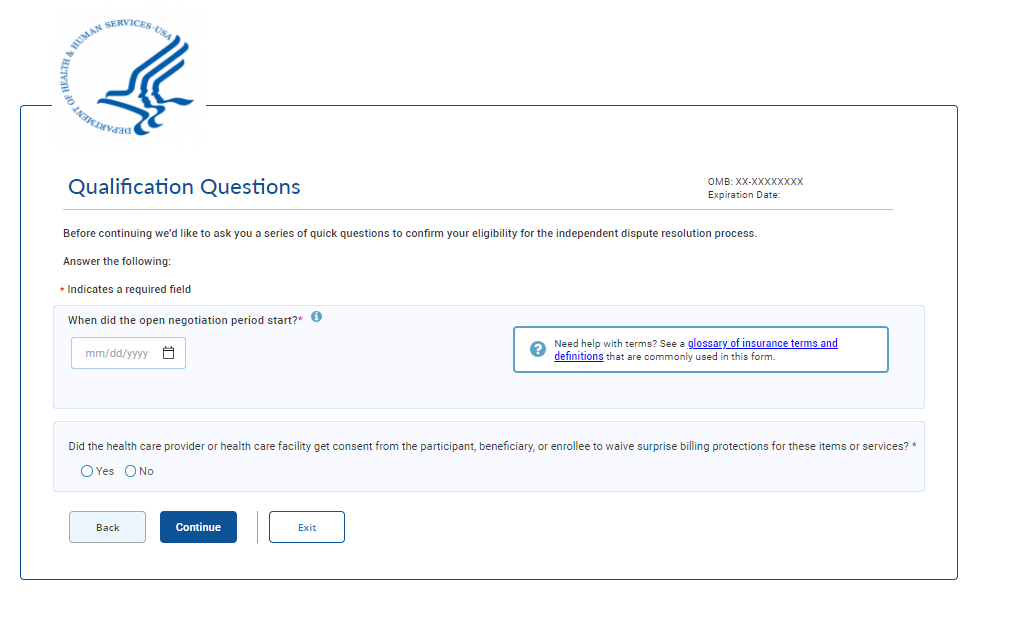
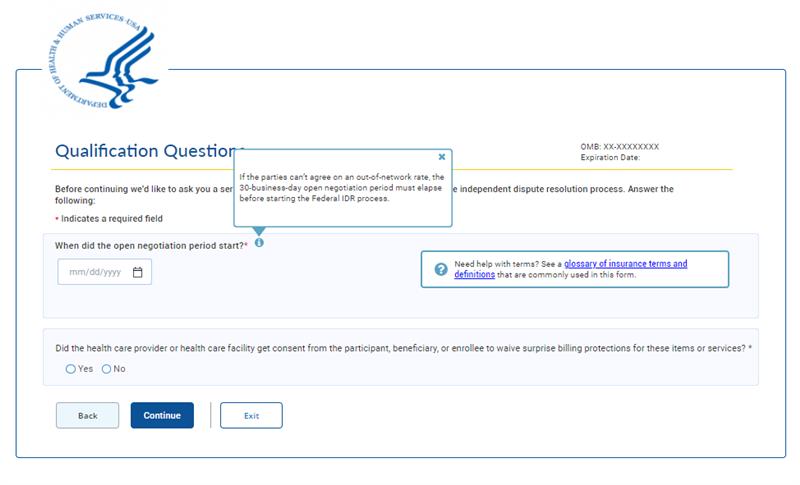
Qualification Questions 2
When did the open negotiation period start? *
Date Picker
Did the health care provider or health care facility get consent from the participant, beneficiary, or enrollee to waive surprise billing protections for these items or services? * Yes/No
Info Bubble: If the parties can’t agree on an out-of-network rate, the 30-business-day open negotiation period must elapse before starting the Federal IDR process.
Buttons – Back, Continue, Exit
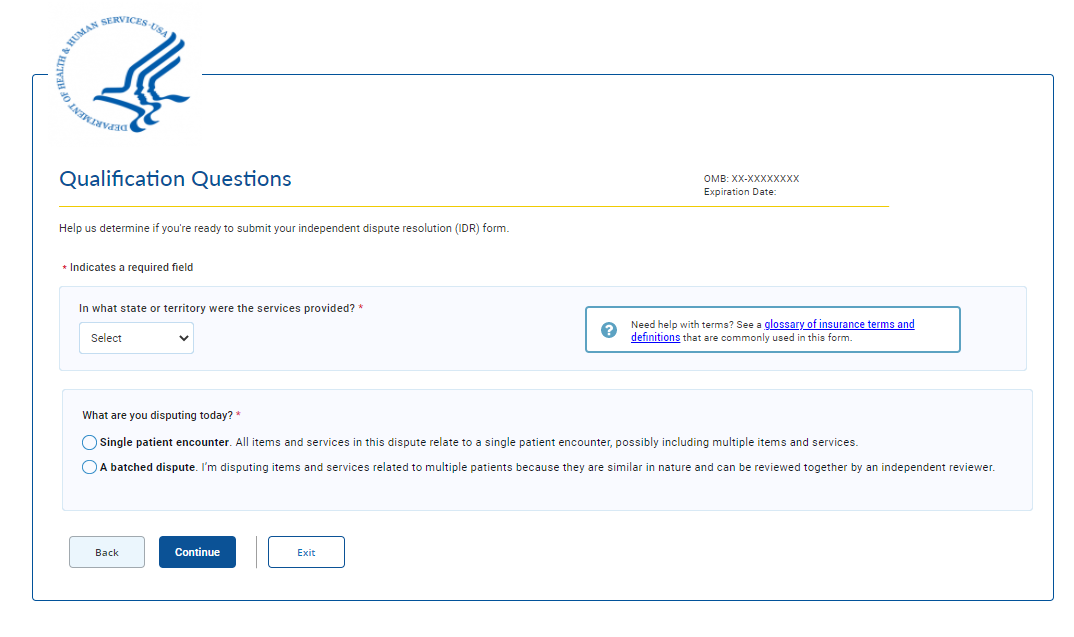
Qualification Questions 3
Help us determine if you're ready to submit your independent dispute resolution (IDR) form
In what state or territory were the items or services provided? * (state picklist)
What are you disputing today?*
Single patient encounter. All items and services in this dispute relate to a single patient encounter, possibly including multiple items and services.
A batched dispute. I’m disputing items and services related to multiple patients because they are similar in nature and can be reviewed together by an independent reviewer.
Buttons – Back, Continue, Exit
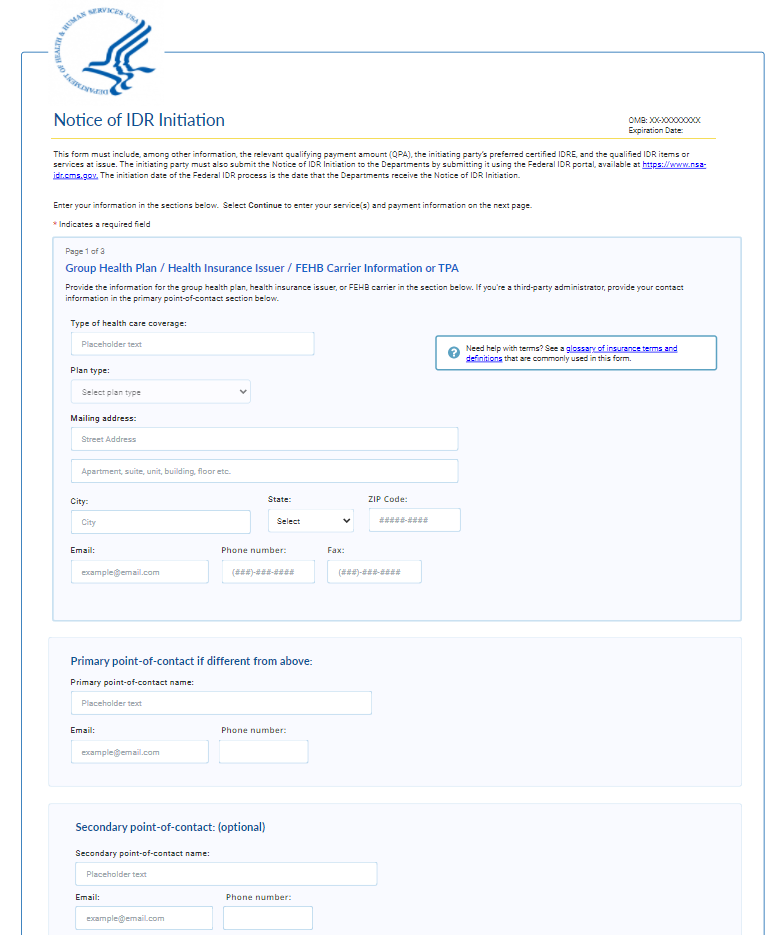
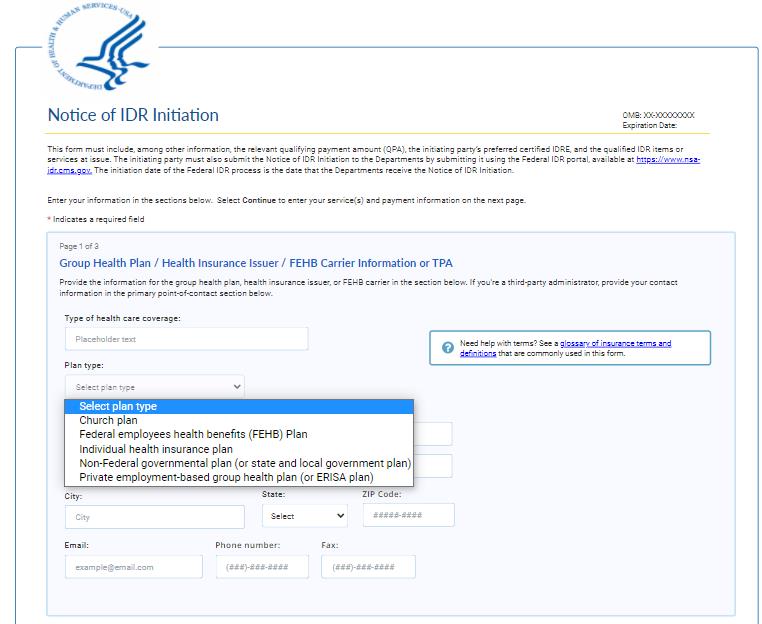
Notice of IDR Initiation
This form must include, among other information, the relevant qualifying payment amount (QPA), the initiating party’s preferred certified IDR entity, and the qualified IDR items or services at issue. The initiating party must also submit the Notice of IDR Initiation to the Departments by submitting it using the Federal IDR portal, available at https://www.nsa-idr.cms.gov. The initiation date of the Federal IDR process is the date that the Departments receive the Notice of IDR Initiation.
Enter your information in the sections below. Select Continue to enter the item(s) or service(s) and payment information on the next page.
* Indicates a required field
Group Health Plan / Health Insurance Issuer / FEHB Carrier Information or TPA
Provide the information for the group health plan, health insurance issuer, or FEHB carrier in the section below. If you’re a third-party administrator, provide your contact information in the primary point-of-contact section below.
Field Inputs:
Type of Health Care Coverage:
Plan type:
Federal employees health benefits (FEHB) plan
Individual health insurance plan
Non-federal governmental plan (or state and local government plan)
Church plan
Private employment-based group health plan (or ERISA plan)
Mailing address
City
State
ZIP code
Email
Phone number
Fax
Primary point-of-contact name:
Email
Phone number
Secondary point-of-contact name:
Email
Phone number
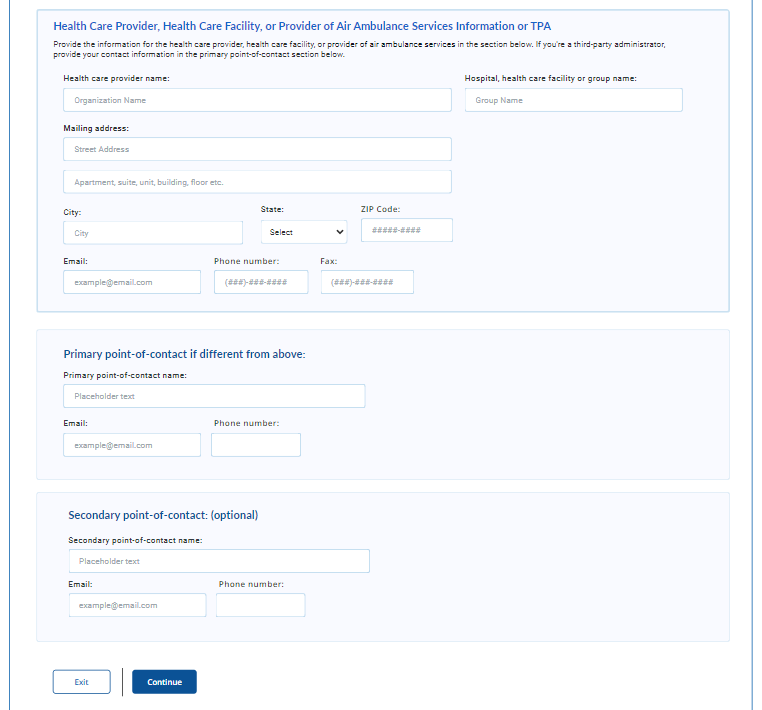
Health Care Provider, Health Care Facility, or Provider of Air Ambulance Services Information or TPA
Provide the information for the health care provider, health care facility, or provider of air ambulance services in the section below. If you’re a third-party administrator, provide your contact information in the primary point-of-contact section below.
Field Inputs:
Health care provider name
Hospital, health care facility or group name
Organization name
Mailing address
City
State
ZIP Code
Email
Phone
Fax
Primary point-of-contact name:
Email
Phone number
Secondary point-of-contact name:
Email
Phone number
Buttons – Exit, Continue
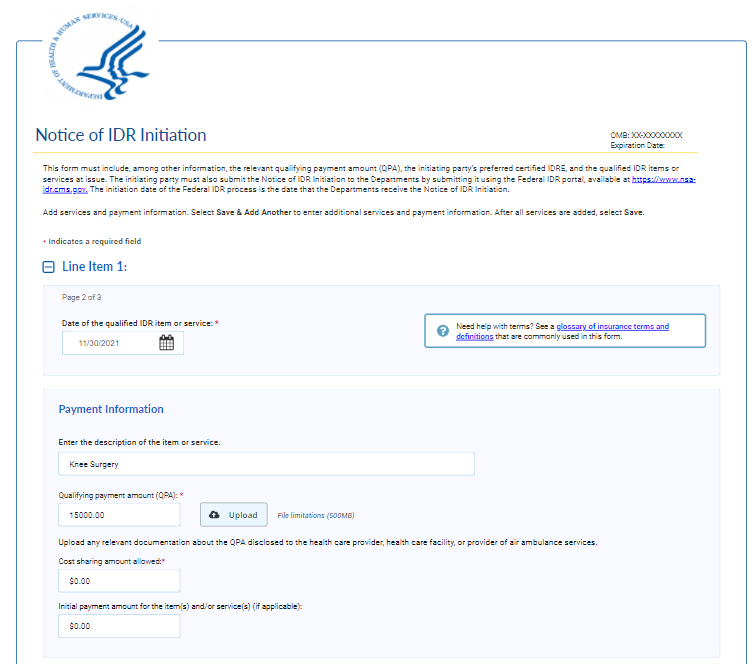
Notice of IDR Initiation
This form must include, among other information, the relevant QPA for each item or service, the initiating party’s preferred certified IDR entity, and the qualified IDR items or services at issue. The initiating party must also furnish the Notice of IDR Initiation to the Departments by submitting notice using the Federal IDR portal, available at https://www.nsa-idr.cms.gov. The initiation date of the Federal IDR process is the date that the Departments receive the Notice of IDR Initiation.
Date of qualified IDR item or service:
Upload any relevant documentation about the QPA disclosed to the health care provider, health care facility, or provider of air ambulance services.
Initial payment amount for the item(s) and/or service(s) (if applicable):
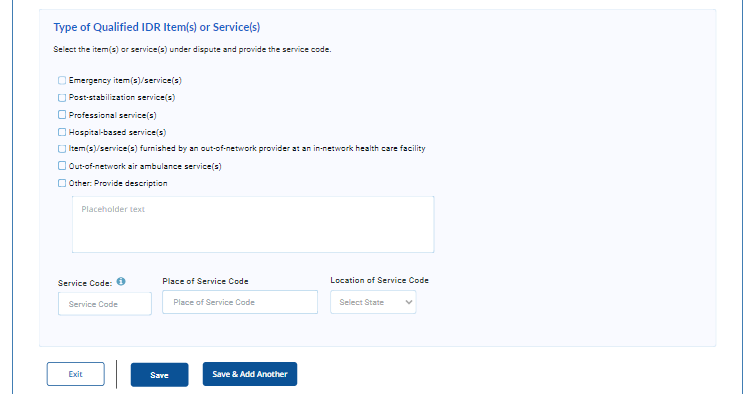
Type of Qualified IDR Item(s) or Service(s)
Select the item(s) or service(s) under dispute and provide the service code.
Emergency item(s)/service(s)
Post-stabilization service(s)
Professional service(s)
Hospital-based service(s)
Item(s)/service(s) furnished by a non-participating provider at a participating health care facility
Non-participating air ambulance service(s)
Other: Provide description
Service code
Place of service code
Buttons – Exit, Save, Save & Add another
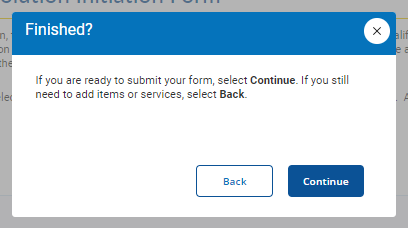
Save Modal
If you are ready to submit your form, select Continue. If you still need to add items or services, select Back.
Buttons: Back, Continue
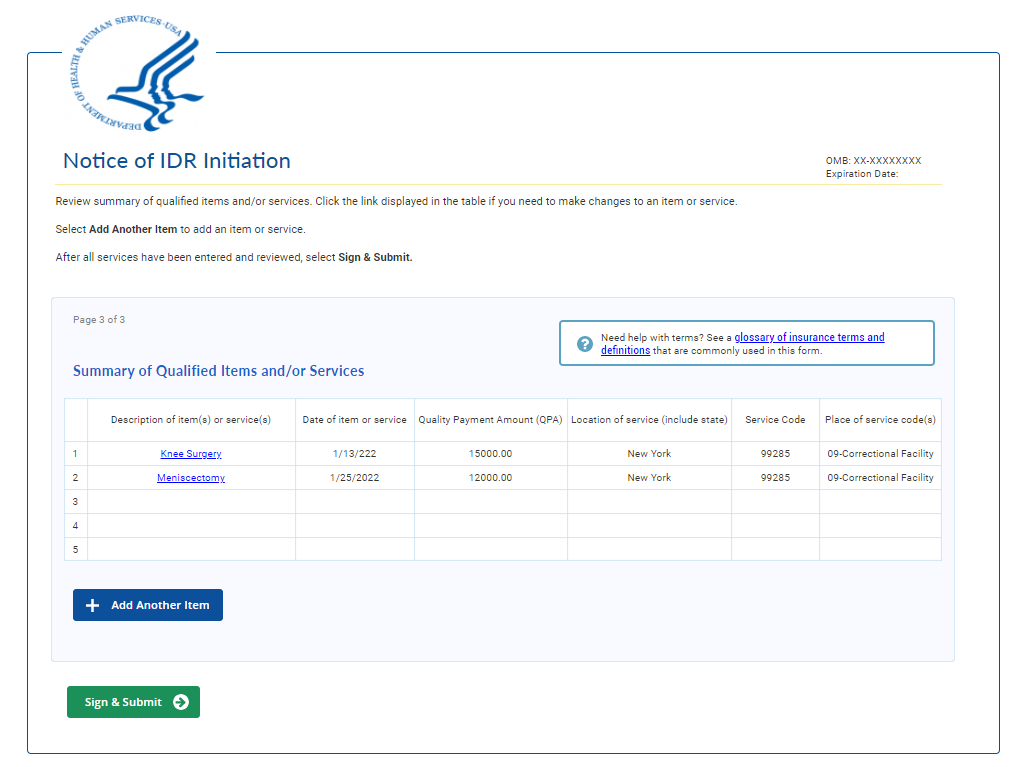
Form Table
Review summary of qualified items and/or services. Click the link displayed in the table if you need to make changes to an item or service.
Select Add Another to add an item or service.
After all services have been entered and reviewed, select Sign & Submit.
Button – Add Another Item, Sign & Submit
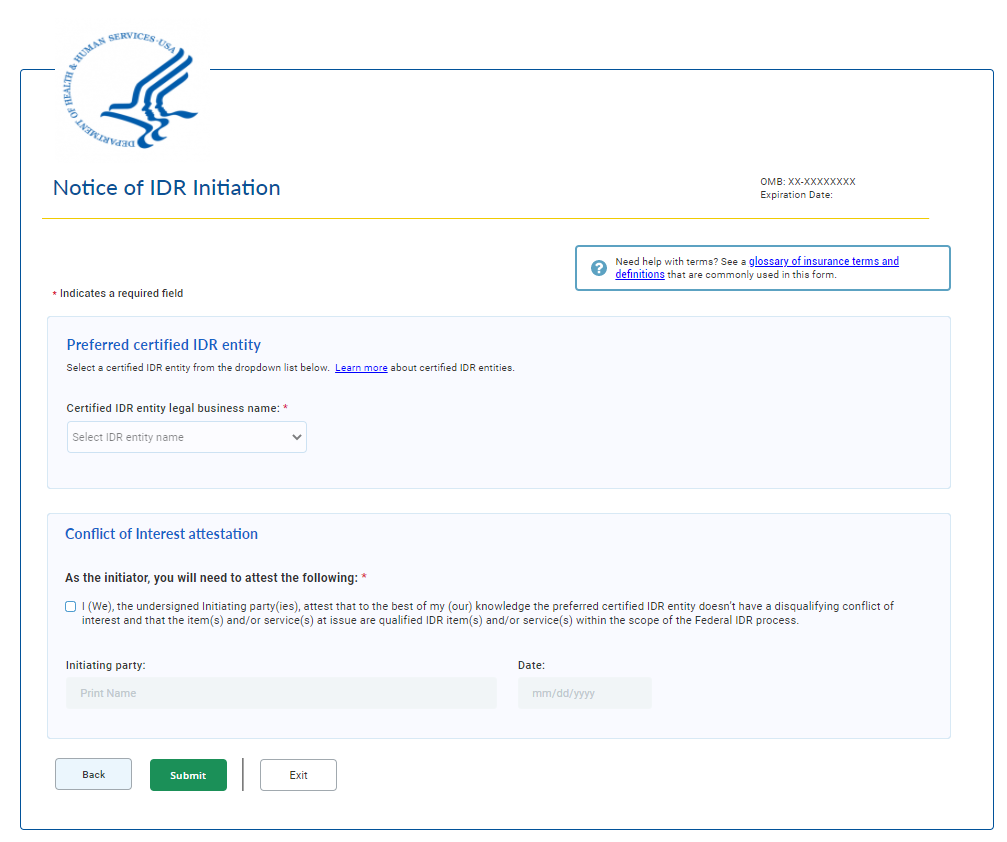
Sign and Submit
Preferred certified IDR entity
Select a certified IDR entity from the dropdown list below. Learn more about certified IDR entities.
IDRE legal business name: *(dropdown)
Conflict of Interest attestation
* As the initiator, you will need to attest the following: *
I (We), the undersigned initiating party(ies), attest that to the best of my (our) knowledge the preferred certified IDR entity doesn’t have a disqualifying conflict of interest and that the item(s) and/or service(s) at issue are qualified IDR item(s) and/or service(s) within the scope of the Federal IDR process.
Buttons: Back, Submit, Exit
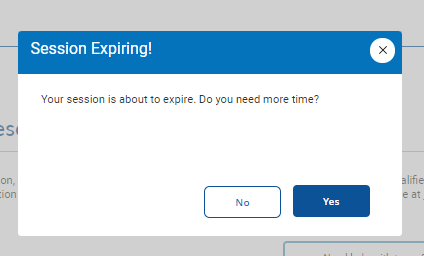
Session Time Out
Session expiring!
Your session is about to expire. Do you need more time?
Buttons – No, Yes
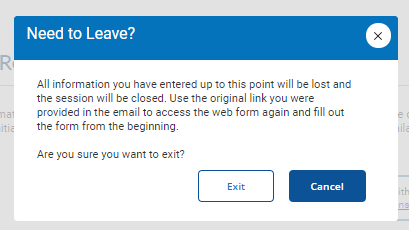
Exit Modal
Need to Leave?
All information you have entered up to this point will be lost and the session will be closed. Use the original link you were provided in the email to access the web form again and fill out the form from the beginning.
Are you sure you want to exit?
Buttons – Exit, Cancel
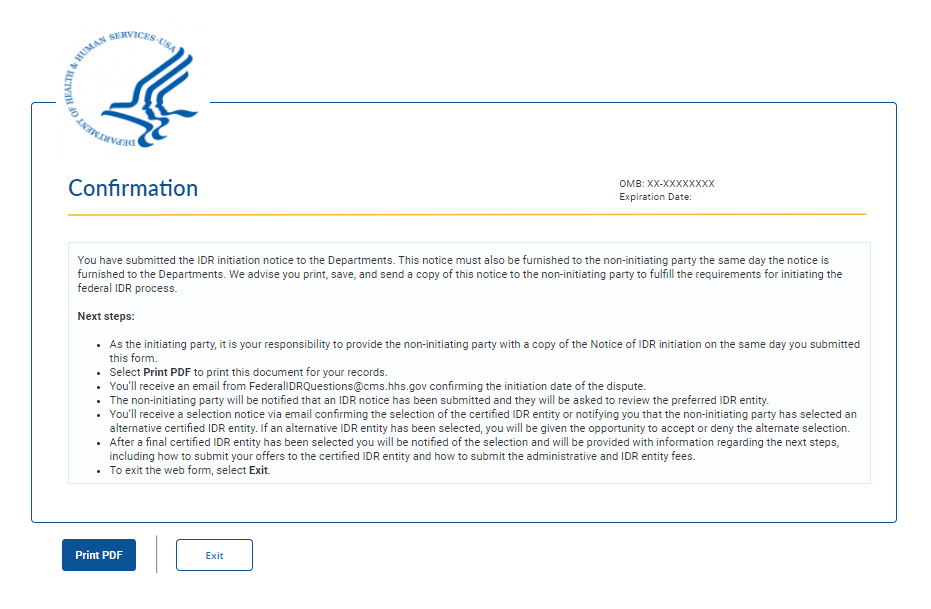
Confirmation
You have submitted the IDR initiation notice to the Departments. This notice must also be furnished to the non-initiating party the same day the notice is furnished to the Departments. We advise you print, save, and send a copy of this notice to the non-initiating party to fulfill the requirements for initiating the federal IDR process.
Next steps:
As the initiating party, it is your responsibility to provide the non-initiating party with a copy of the Notice of IDR initiation on the same day you submitted this form.
Select Print PDF to print this document for your records.
You’ll receive an email from [email protected] confirming the initiation date of the dispute.
The non-initiating party will be notified that an IDR notice has been submitted and they will be asked to review the preferred IDR entity.
You’ll receive a selection notice via email confirming the selection of the certified IDR entity or notifying you that the non-initiating party has selected an alternative certified IDR entity. If an alternative IDR entity has been selected, you will be given the opportunity to accept or deny the alternate selection.
After a final certified IDR entity has been selected you will be notified of the selection and will be provided with information regarding the next steps, including how to submit your offers to the certified IDR entity and how to submit the administrative and IDR entity fees.
To exit the web form, select Exit.
Buttons – Print PDF, Exit
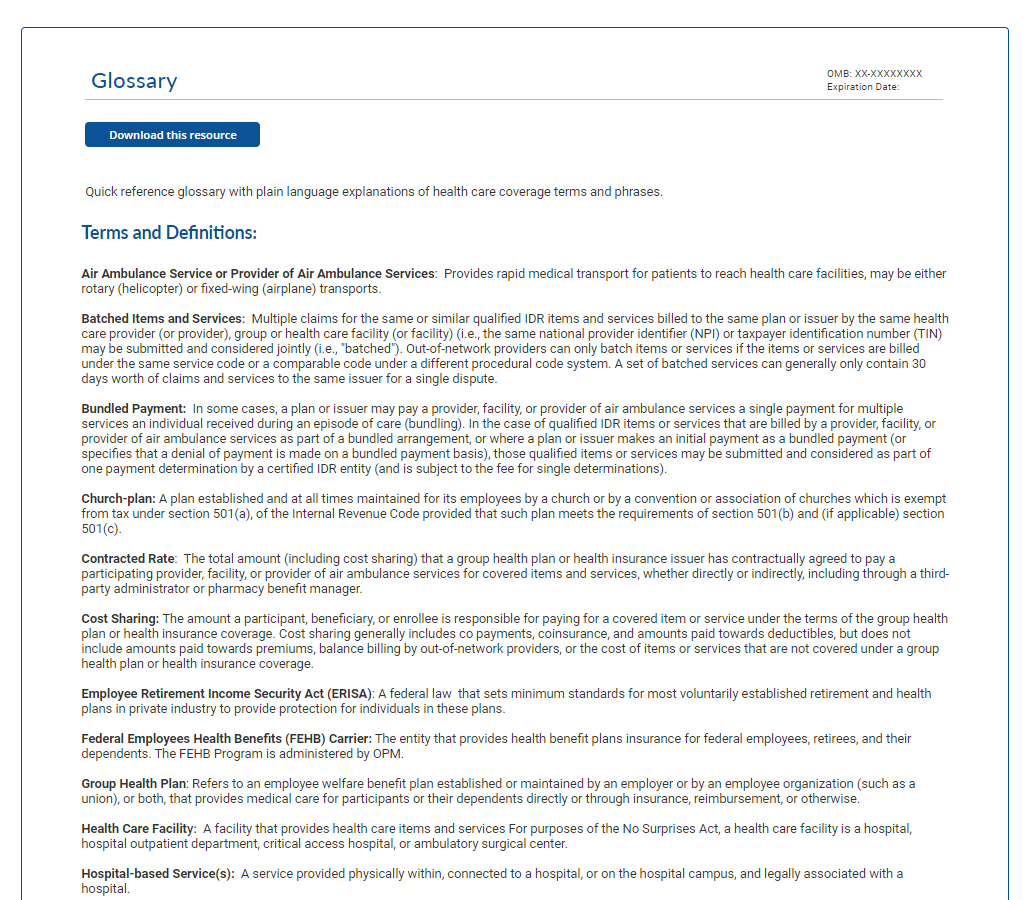
Glossary
Quick reference glossary with plain language explanations of health care coverage terms and phrases.
Terms and Definitions:
Air Ambulance Service or Provider of Air Ambulance Services: Provides rapid medical transport for patients to reach health care facilities, may be either rotary (helicopter) or fixed-wing (airplane) transports.
Batched Items and Services: Multiple claims for the same or similar qualified IDR items and services billed to the same plan or issuer by the same health care provider (or provider), group or health care facility (or facility) (i.e., the same national provider identifier (NPI) or taxpayer identification number (TIN)) may be submitted and considered jointly (i.e., "batched"). Out-of-network providers can only batch items or services if the items or services are billed under the same service code or a comparable code under a different procedural code system. A set of batched services can generally only contain 30 days worth of claims and services to the same issuer for a single dispute.
Bundled payment: In some cases, a plan or issuer may pay a provider, facility, or provider of air ambulance services a single payment for multiple services an individual received during an episode of care (bundling). In the case of qualified IDR items or services that are billed by a provider, facility, or provider of air ambulance services as part of a bundled arrangement, or where a plan or issuer makes an initial payment as a bundled payment (or specifies that a denial of payment is made on a bundled payment basis), those qualified items or services may be submitted and considered as part of one payment determination by a certified IDR entity (and is subject to the fee for single determinations).
Church Plan: A plan established and at all times maintained for its employees by a church or by a convention or association of churches which is exempt from tax under section 501(a), of the Internal Revenue Code provided that such plan meets the requirements of section 501(b) and (if applicable) section 501(c).
Contracted Rate: The total amount (including cost sharing) that a group health plan or health insurance issuer has contractually agreed to pay a participating provider, facility, or provider of air ambulance services for covered items and services, whether directly or indirectly, including through a third-party administrator or pharmacy benefit manager.
Cost Sharing: The amount a participant, beneficiary, or enrollee is responsible for paying for a covered item or service under the terms of the group health plan or health insurance coverage. Cost sharing generally includes copayments, coinsurance, and amounts paid towards deductibles, but does not include amounts paid towards premiums, balance billing by out-of-network providers, or the cost of items or services that are not covered under a group health plan or health insurance coverage.
Employee Retirement Income Security Act (ERISA): A federal law that sets minimum standards for most voluntarily established retirement and health plans in private industry to provide protection for individuals in these plans.
Federal Employees Health Benefits (FEHB) Carrier: The entity that providers health benefit plans insurance for federal employees, retirees, and their dependents. The FEHB Program is administered by OPM.
Group Health Plan: Refers to an employee welfare benefit plan established or maintained by an employer or by an employee organization (such as a union), or both, that provides medical care for participants or their dependents directly or through insurance, reimbursement, or otherwise.
Health Care Facility: A facility that provides health care items and services for purposes of the No Surprises Act, a health care facility is a hospital, hospital outpatient department, critical access hospital, or ambulatory surgical center.
Hospital-based Service(s): A service provided physically within, connected to a hospital, or on the hospital campus, and legally associated with a hospital.
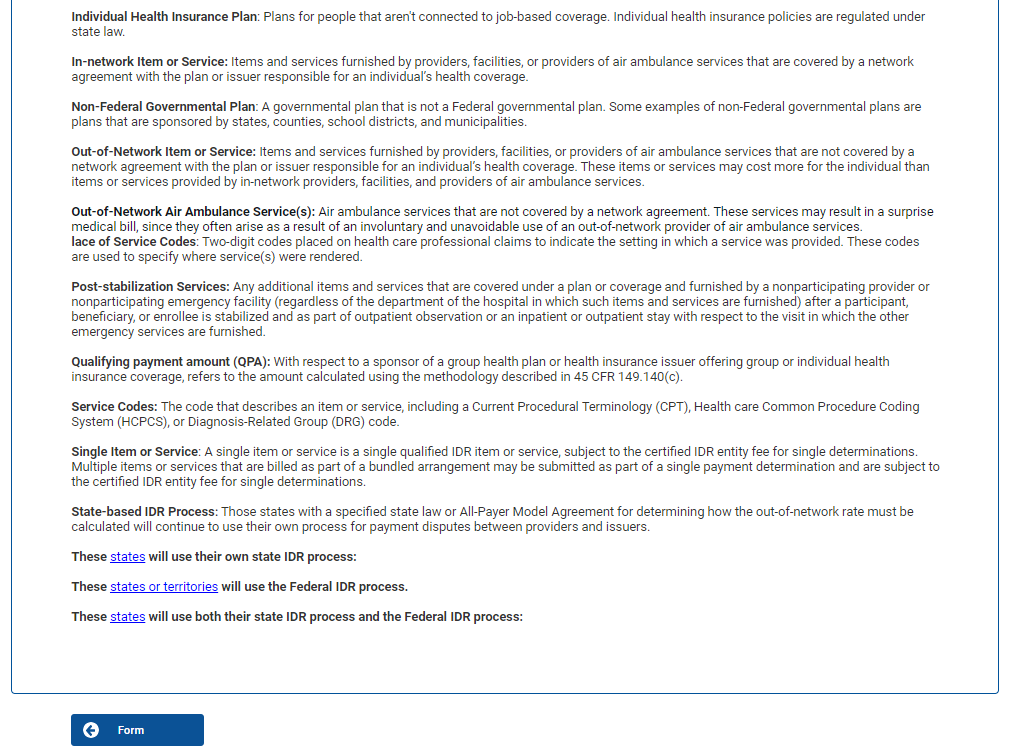
Individual Health Insurance Plan: Plans for people that aren't connected to job-based coverage. Individual health insurance policies are regulated under state law.
In-network Item or Service: Items and services furnished by providers, facilities, or providers of air ambulance services that are covered by a network agreement with the plan or issuer responsible for an individual’s health coverage.
Non-Federal Governmental Plan: A governmental plan that is not a Federal governmental plan. Some examples of non-Federal governmental plans are plans that are sponsored by states, counties, school districts, and municipalities
Out-of-network Item or Service: Items and services furnished by providers, facilities, or providers of air ambulance services that are not covered by a network agreement with the plan or issuer responsible for an individual’s health coverage. These items or services may cost more for the individual than items or services provided by in-network providers, facilities, and providers of air ambulance services.
Out-of-network air ambulance service(s): Air ambulance services that are not covered by a network agreement. These services may result in a surprise medical bill, since they often arise as a result of an involuntary and unavoidable use of an out-of-network provider of air ambulance services.
Place of Service Codes: Two-digit codes placed on health care professional claims to indicate the setting in which a service was provided. These codes are used to specify where service(s) were rendered.
Post-stabilization Services: Services related to an emergency medical condition that are provided after a patient is stabilized to maintain the stabilized condition, or, under certain circumstances, to improve or resolve the patient’s condition, until the patient consents to be treated by a nonparticipating provider or nonparticipating emergency facility.
Qualifying payment amount (QPA): With respect to a sponsor of a group health plan or health insurance issuer offering group or individual health insurance coverage, refers to the amount calculated using the methodology described in 45 CFR 149.140(c)
Service Codes: the code that describes an item or service, including a Current Procedural Terminology (CPT), Healthcare Common Procedure Coding System (HCPCS), or Diagnosis-Related Group (DRG) code.
Single Item or Service: A single item or service is a single qualified IDR item or service, subject to the certified IDR entity fee for single determinations. Multiple items or services that are billed as part of a bundled arrangement may be submitted as part of a single payment determination and are subject to the certified IDR entity fee for single determinations.
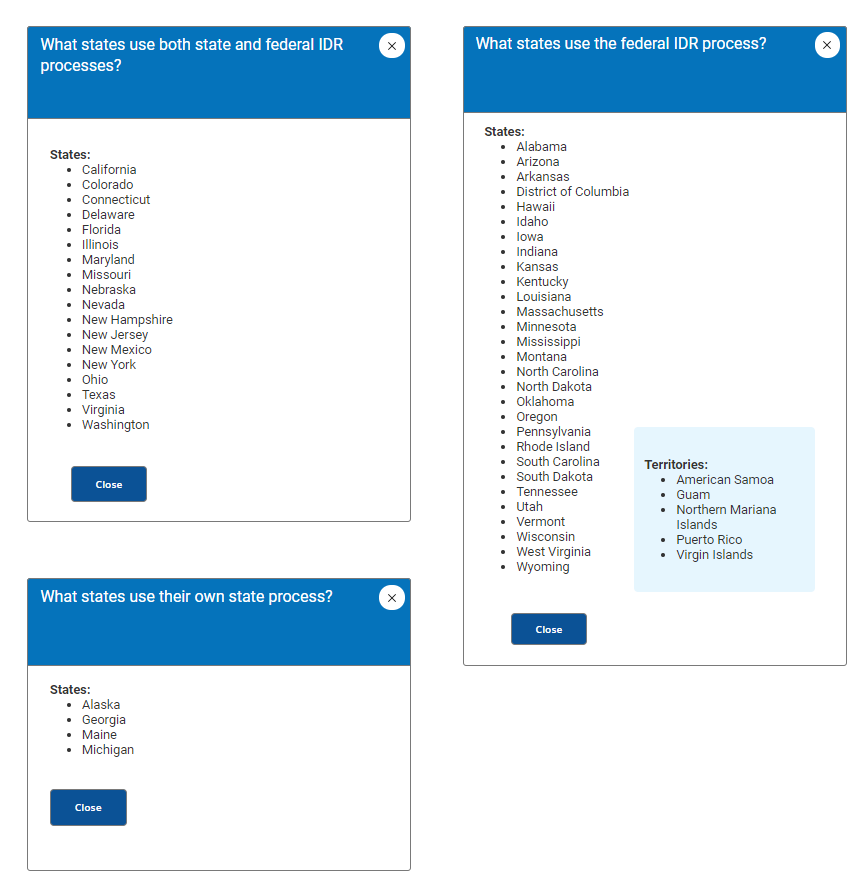
State-based IDR Process: Those states with a specified state law or All-Payer Model Agreement for determining how the out-of-network rate must be calculated will continue to use their own process for payment disputes between providers and issuers.
These states will use their own state IDR process:
Alaska
Georgia
Maine
Michigan
These states or territories will use the Federal IDR process.
States:
Alabama
Arizona
Arkansas
District of Columbia
Hawaii
Idaho
Iowa
Indiana
Kansas
Kentucky
Louisiana
Massachusetts
Minnesota
Mississippi
Montana
North Carolina
North Dakota
Oklahoma
Oregon
Pennsylvania
Rhode Island
South Carolina
South Dakota
Tennessee
Utah
Vermont
Wisconsin
West Virginia
Wyoming
Territories:
American Samoa
Guam
Northern Mariana Islands
Puerto Rico
Virgin Islands
• These states will use both their state IDR process and the Federal IDR process.
California
Colorado
Connecticut
Delaware
Florida
Illinois
Maryland
Missouri
Nebraska
Nevada
New Hampshire
New Jersey
New Mexico
New York
Ohio
Texas
Virginia
Washington
Button – Back to Form
Button - Close
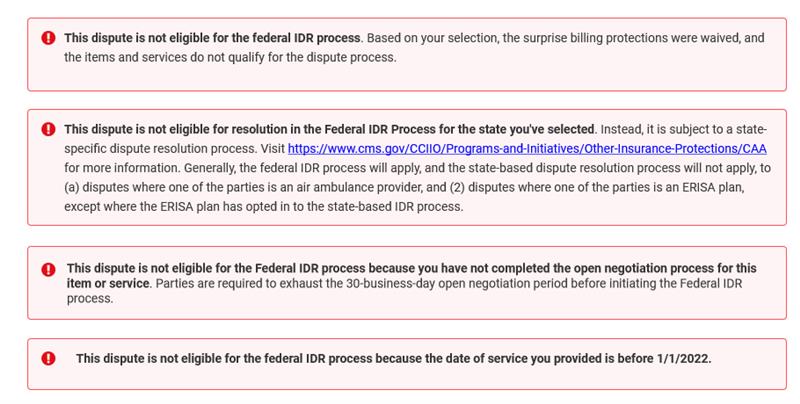
Error Messages
This dispute is not eligible for the federal IDR process. Based on your selection, the surprise billing protections were waived, and the items and services do not qualify for the dispute process.
This dispute is not eligible for resolution in the Federal IDR Process for the state you've selected. Instead, it is subject to a state-specific dispute resolution process. Visit https://www.cms.gov/CCIIO/Programs-and-Initiatives/Other-Insurance-Protections/CAA for more information. Generally, the federal IDR process will apply, and the state-based dispute resolution process will not apply, to (a) disputes where one of the parties is an air ambulance provider, and (2) disputes where one of the parties is an ERISA plan, except where the ERISA plan has opted in to the state-based IDR process.
This dispute is not eligible for the Federal IDR process because you have not completed the open negotiation process for this item or service. Parties are required to exhaust the 30-business-day open negotiation period before initiating the Federal IDR process.
This dispute is not eligible for the federal IDR process because the date of service you provided is before 1/1/2022.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | Charyszyn, Lisa |
| File Modified | 0000-00-00 |
| File Created | 2023-08-30 |
© 2026 OMB.report | Privacy Policy