CMS-10398. GenIC # Monitoring Report Workbook
[Medicaid] Generic Clearance for Medicaid and CHIP State Plan, Waiver, and Program Submissions (CMS-10398)
5b - Monitoring Report Workbook (2020 version 3).xlsm
GenIC # 59 (Revision) - Medicaid Section 1115 Severe Mental Illness and Children with Serious Emotional Disturbance Demonstrations
OMB: 0938-1148
⚠️ Notice: This form may be outdated. More recent filings and information on OMB 0938-1148 can be found here:
Document [xlsx]
Download: xlsx | pdf
SMI-SED metrics
SMI-SED reporting issues
Avail Assessment instructions
Avail Assessment definitions
Annual Avail Assessment
Overview
PRA Disclosure StatementSMI-SED metrics
SMI-SED reporting issues
Avail Assessment instructions
Avail Assessment definitions
Annual Avail Assessment
Sheet 1: PRA Disclosure Statement
| PRA Disclosure Statement This information is being collected to assist the Centers for Medicare & Medicaid Services in program monitoring of Medicaid Section 1115 Serious Mental Illness and Serious Emotional Disturbance Demonstrations. This mandatory information collection (42 CFR § 431.428) will be used to support more efficient, timely and accurate review of states’ monitoring report submissions of Medicaid Section 1115 Serious Mental Illness and Serious Emotional Disturbance Demonstrations, and also support consistency in monitoring and evaluation, increase in reporting accuracy, and reduction in timeframes required for monitoring and evaluation. Under the Privacy Act of 1974 any personally identifying information obtained will be kept private to the extent of the law. |
| End of worksheet |
| According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is 0938-1148 (CMS-10398 #59). The time required to complete this information collection is estimated to average 29 hours per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. If you have comments concerning the accuracy of the time estimate(s) or suggestions for improving this form, please write to: CMS, 7500 Security Boulevard, Attn: PRA Reports Clearance Officer, Mail Stop C4-26-05, Baltimore, Maryland 21244-1850. |
Sheet 2: SMI-SED metrics
| Medicaid Section 1115 SMI/SED Demonstrations Monitoring Report (Part A) - Metrics (Version 2.0) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| State | [Enter State Name] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Demonstration Name | [Enter Demonstration Name] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| SMI/SED Demonstration Year (DY) (Format: DY1, DY2, DY3, etc.) | [Enter SMI/SED Demonstration Year] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Calendar Dates for SMI/SED DY (Format: MM/DD/YYYY - MM/DD/YYYY) | [Enter Calendar Dates for SMI/SED Demonstration Year] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| SMI/SED Reporting Period (Format: Q1, Q2, Q3, Q4) | [Enter SMI/SED Reporting Period] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Calendar Dates for SMI/SED Reporting Period (Format: MM/DD/YYYY - MM/DD/YYYY) | [Enter Calendar Dates for SMI/SED Reporting Period] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Serious Mental Illness/Serious Emotional Disturbance (SMI/SED) Metricsa | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Demonstration Reporting | Standardized definition of SMI | State-specific definition of SMI | Children (Age <16) | Transition-age youth (Age 16-24) | Adults (Age 25-64) | Older adults (Age 65+) | Dual-eligible (Medicare-Medicaid eligible) | Medicaid only | Eligible for Medicaid on the basis of disability | Not eligible for Medicaid on the basis of disability | Criminally involved | Not criminally involved | Co-occurring SUD | Co-occurring physical conditions | [State-specific subpopulation]d,e | |||||||||||||||||||||||||||||||||||||||||||||
| # | Metric name | Metric description | Milestone or reporting topic | Metric type | Reporting category | Data source | Approved protocol indicates that reporting matches the CMS-provided technical specifications manual (Y/N)b | Deviations from CMS-provided technical specifications manual in approved protocol | Technical specifications manual version | Reporting issue (Y/N) (further describe in SMI-SED reporting issues tab) |
Measurement period (month, quarter, yearc) | Dates covered by measurement period (MM/DD/YYYY-MM/DD/YYYY) | Demonstration Reporting Denominator |
Demonstration Reporting Numerator or count |
Demonstration Reporting Rate/Percentaged |
Standardized definition of SMI Denominator | Standardized definition of SMI Numerator or count |
Standardized definition of SMI Rate/Percentaged | State-specific definition of SMI Denominator |
State-specific definition of SMI Numerator or count | State-specific definition of SMI Rate/Percentaged | Children (Age <16) Denominator | Children (Age <16) Numerator or count | Children (Age <16) Rate/Percentaged | Transition-age youth (Age 16-24) Denominator | Transition-age youth (Age 16-24) Numerator or count | Transition-age youth (Age 16-24) Rate/Percentaged | Adults (Age 25-64) Denominator | Adults (Age 25-64) Numerator or count | Adults (Age 25-64) Rate/Percentaged | Older adults (Age 65+) Denominator | Older adults (Age 65+) Numerator or count | Older adults (Age 65+) Rate/Percentaged | Dual-eligible (Medicare-Medicaid eligible) Denominator | Dual-eligible (Medicare-Medicaid eligible) Numerator or count | Dual-eligible (Medicare-Medicaid eligible) Rate/Percentaged | Medicaid only Denominator | Medicaid only Numerator or count | Medicaid only Rate/Percentaged | Eligible for Medicaid on the basis of disability Denominator | Eligible for Medicaid on the basis of disability Numerator or count | Eligible for Medicaid on the basis of disability Rate/Percentaged | Not eligible for Medicaid on the basis of disability Denominator | Not eligible for Medicaid on the basis of disability Numerator or count | Not eligible for Medicaid on the basis of disability Rate/Percentaged | Criminally involved Denominator | Criminally involved Numerator or count | Criminally involved Rate/Percentaged | Not criminally involved Denominator | Not criminally involved Numerator or count | Not criminally involved Rate/Percentaged | Co-occurring SUD Denominator | Co-occurring SUD Numerator or count | Co-occurring SUD Rate/Percentaged | Co-occurring physical conditions Denominator | Co-occurring physical conditions Numerator or count | Co-occurring physical conditions Rate/Percentaged | [State-specific subpopulation] Denominator | [State-specific subpopulation] Numerator or count | [State-specific subpopulation] Rate/Percentaged |
| EXAMPLE: 24 (Do not delete or edit this row) |
EXAMPLE: Screening for Depression and Follow-Up Plan: Age 18 and Older (CDF-AD) |
EXAMPLE: Percentage of beneficiaries age 18 and older screened for depression on the date of the encounter using an age appropriate standardized depression screening tool, AND if positive, a follow-up plan is documented on the date of the positive screen. |
EXAMPLE: Milestone 4 |
EXAMPLE: Established quality measure |
EXAMPLE: Annual metrics that are an established quality measure |
EXAMPLE: Claims Medical records |
EXAMPLE: N |
EXAMPLE: The Department will use state-defined procedure codes (list specific codes) to calculate this metric. |
EXAMPLE: Version 2.0 |
EXAMPLE: Y |
EXAMPLE: Year |
EXAMPLE: 01/01/2020-12/31/2020 |
EXAMPLE: 200 |
EXAMPLE: 100 |
EXAMPLE: 0.5 |
EXAMPLE: |
EXAMPLE: |
EXAMPLE: |
||||||||||||||||||||||||||||||||||||||||||
| 1 | SUD Screening of Beneficiaries Admitted to Psychiatric Hospitals or Residential Treatment Settings (SUB-2) | SUB-2: Patients who screened positive for unhealthy alcohol use who received or refused a brief intervention during the hospital stay. | Milestone 1 | Established quality measure | Annual metrics that are an established quality measure | Medical record review or claims | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | SUB-2a: Patients who received the brief intervention during the hospital stay. | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| 2 | Use of First-Line Psychosocial Care for Children and Adolescents on Antipsychotics (APP-CH) | Percentage of children and adolescents ages 1 to 17 who had a new prescription for an antipsychotic medication and had documentation of psychosocial care as first-line treatment. | Milestone 1 | Established quality measure | Annual metrics that are an established quality measure | Claims | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 3 | All-Cause Emergency Department Utilization Rate for Medicaid Beneficiaries who may Benefit From Integrated Physical and Behavioral Health Care (PMH-20) | Number of all-cause ED visits per 1,000 beneficiary months among adult Medicaid beneficiaries age 18 and older who meet the eligibility criteria of beneficiaries with SMI. | Milestone 2 | Established quality measure | Annual metrics that are an established quality measure | Claims | Year | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4 | 30-Day All-Cause Unplanned Readmission Following Psychiatric Hospitalization in an Inpatient Psychiatric Facility (IPF) | The rate of unplanned, 30-day, readmission for demonstration beneficiaries with a primary discharge diagnosis of a psychiatric disorder or dementia/Alzheimer’s disease. The measurement period used to identify cases in the measure population is 12 months from January 1 through December 31. | Milestone 2 | Established quality measure | Annual metrics that are an established quality measure | Claims | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 5 | Medication Reconciliation Upon Admission | Percentage of patients for whom a designated prior to admission (PTA) medication list was generated by referencing one or more external sources of PTA medications and for which all PTA medications have a documented reconciliation action by the end of Day 2 of the hospitalization. | Milestone 2 | Established quality measure | Annual metrics that are an established quality measure | Electronic/paper medical records | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 6 | Medication Continuation Following Inpatient Psychiatric Discharge | This measure assesses whether psychiatric patients admitted to an inpatient psychiatric facility (IPF) for major depressive disorder (MDD), schizophrenia, or bipolar disorder filled a prescription for evidence-based medication within 2 days prior to discharge and 30 days post-discharge. | Milestone 2 | Established quality measure | Annual metrics that are an established quality measure | Claims | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 7 | Follow-up After Hospitalization for Mental Illness: Ages 6-17 (FUH-CH) | Percentage of discharges for children ages 6 to 17 who were hospitalized for treatment of selected mental illness or intentional self-harm diagnoses and who had a follow-up visit with a mental health practitioner. Two rates are reported: | Milestone 2 | Established quality measure | Annual metrics that are an established quality measure | Claims | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | Percentage of discharges for which the child received follow-up within 30 days after discharge. | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | Percentage of discharges for which the child received follow-up within 7 days after discharge. | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| 8 | Follow-up After Hospitalization for Mental Illness: Age 18 and Older (FUH-AD) | Percentage of discharges for beneficiaries age 18 years and older who were hospitalized for treatment of selected mental illness diagnoses or intentional self-harm and who had a follow-up visit with a mental health practitioner. Two rates are reported: | Milestone 2 | Established quality measure | Annual metrics that are an established quality measure | Claims | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | Percentage of discharges for which the beneficiary received follow-up within 30 days after discharge. | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | Percentage of discharges for which the beneficiary received follow-up within 7 days after discharge. | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| 9 | Follow-up After Emergency Department Visit for Alcohol and Other Drug Abuse (FUA-AD) | Percentage of emergency department (ED) visits for beneficiaries age 18 and older with a primary diagnosis of alcohol or other drug (AOD) abuse dependence who had a follow-up visit for AOD abuse or dependence. Two rates are reported: | Milestone 2 | Established quality measure | Annual metrics that are an established quality measure | Claims | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | Percentage of ED visits for AOD abuse or dependence for which the beneficiary received follow-up within 30 days of the ED visit. | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | Percentage of ED visits for AOD abuse or dependence for which the beneficiary received follow-up within 7 days of the ED visit. | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| 10 | Follow-Up After Emergency Department Visit for Mental Illness (FUM-AD) | Percentage of emergency department (ED) visits for beneficiaries age 18 and older with a primary diagnosis of mental illness or intentional self-harm and who had a follow-up visit for mental illness. Two rates are reported: | Milestone 2 | Established quality measure | Annual metrics that are an established quality measure | Claims | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | Percentage of ED visits for mental illness for which the beneficiary received follow-up within 30 days of the ED visit. | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | Percentage of ED visits for mental illness for which the beneficiary received follow-up within 7 days of the ED visit. | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| 11 | Suicide or Overdose Death Within 7 and 30 Days of Discharge From an Inpatient Facility or Residential Treatment for Mental Health Among Beneficiaries With SMI or SED (count) | Number of suicide or overdose deaths among Medicaid beneficiaries with SMI or SED within 7 and 30 days of discharge from an inpatient facility or residential stay for mental health. | Milestone 2 | CMS-constructed | Other annual metrics | State data on cause of death | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | 7 days of discharge from an inpatient facility or residential stay for mental health. | blank | blank | blank | blank | blank | blank | blank | blank | Year | |||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | 30 days of discharge from an inpatient facility or residential stay for mental health. | blank | blank | blank | blank | blank | blank | blank | blank | Year | |||||||||||||||||||||||||||||||||||||||||||||||||
| 12 | Suicide or Overdose Death Within 7 and 30 Days of Discharge From an Inpatient Facility or Residential Treatment for Mental Health Among Beneficiaries With SMI or SED (rate) | Rate of suicide or overdose deaths among Medicaid beneficiaries with SMI or SED within 7 and 30 days of discharge from an inpatient facility or residential stay for mental health. | Milestone 2 | CMS-constructed | Other annual metrics | State data on cause of death | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | 7 days of discharge from an inpatient facility or residential stay for mental health. | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | #DIV/0! | #DIV/0! | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||
| blank | blank | 30 days of discharge from an inpatient facility or residential stay for mental health. | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | #DIV/0! | #DIV/0! | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||
| 13 | Mental Health Services Utilization - Inpatient | Number of beneficiaries in the demonstration population who use inpatient services related to mental health during the measurement period. | Milestone 3 | CMS-constructed | Other monthly and quarterly metrics | Claims | Month 1 | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 2 | |||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 3 | |||||||||||||||||||||||||||||||||||||||||||||||||
| 14 | Mental Health Services Utilization - Intensive Outpatient and Partial Hospitalization | Number of beneficiaries in the demonstration population who used intensive outpatient and/or partial hospitalization services related to mental health during the measurement period. | Milestone 3 | CMS-constructed | Other monthly and quarterly metrics | Claims | Month 1 | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 2 | |||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 3 | |||||||||||||||||||||||||||||||||||||||||||||||||
| 15 | Mental Health Services Utilization - Outpatient | Number of beneficiaries in the demonstration population who used outpatient services related to mental health during the measurement period. | Milestone 3 | CMS-constructed | Other monthly and quarterly metrics | Claims | Month 1 | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 2 | |||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 3 | |||||||||||||||||||||||||||||||||||||||||||||||||
| 16 | Mental Health Services Utilization - ED | Number of beneficiaries in the demonstration population who use emergency department services for mental health during the measurement period. | Milestone 3 | CMS-constructed | Other monthly and quarterly metrics | Claims | Month 1 | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 2 | |||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 3 | |||||||||||||||||||||||||||||||||||||||||||||||||
| 17 | Mental Health Services Utilization - Telehealth | Number of beneficiaries in the demonstration population who used telehealth services related to mental health during the measurement period. | Milestone 3 | CMS-constructed | Other monthly and quarterly metrics | Claims | Month 1 | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 2 | |||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 3 | |||||||||||||||||||||||||||||||||||||||||||||||||
| 18 | Mental Health Services Utilization - Any Services | Number of beneficiaries in the demonstration population who used any services related to mental health during the measurement period. | Milestone 3 | CMS-constructed | Other monthly and quarterly metrics | Claims | Month 1 | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 2 | |||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 3 | |||||||||||||||||||||||||||||||||||||||||||||||||
| 19a | Average Length of Stay in IMDs | Average length of stay (ALOS) for beneficiaries with SMI discharged from an inpatient or residential stay in an IMD. Three rates are reported: | Milestone 3 | CMS-constructed | Other annual metrics | Claims State-specific IMD database |
||||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | ALOS for all IMDs and populations | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | ALOS among short-term stays (less than or equal to 60 days) | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | ALOS among long-term stays (greater than 60 days) | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| 19b | Average Length of Stay in IMDs (IMDs receiving FFP only) | Average length of stay (ALOS) for beneficiaries with SMI discharged from an inpatient or residential stay in an IMD receiving federal financial participation (FFP). Three rates are reported: | Milestone 3 | CMS-constructed | Other annual metrics | Claims State-specific IMD database |
||||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | ALOS for all IMDs and populations | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | ALOS among short-term stays (less than or equal to 60 days) | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | ALOS among long-term stays (greater than 60 days) | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| 20 | Beneficiaries With SMI/SED Treated in an IMD for Mental Health | Number of beneficiaries in the demonstration population who have a claim for inpatient or residential treatment for mental health in an IMD during the reporting year. | Milestone 3 | CMS-constructed | Other annual metrics | Claims | Year | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 21 | Count of Beneficiaries With SMI/SED (monthly) | Number of beneficiaries in the demonstration population during the measurement period and/or in the 11 months before the measurement period. | Milestone 4 | CMS-constructed | Other monthly and quarterly metrics | Claims | Month 1 | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 2 | |||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | blank | Month 3 | |||||||||||||||||||||||||||||||||||||||||||||||||
| 22 | Count of Beneficiaries With SMI/SED (annually) | Number of beneficiaries in the demonstration population during the measurement period and/or in the 12 months before the measurement period. | Milestone 4 | CMS-constructed | Other annual metrics | Claims | Year | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23 | Diabetes Care for Patients with Serious Mental Illness: Hemoglobin A1c (HbA1c) Poor Control (>9.0%) (HPCMI-AD) | Percentage of beneficiaries ages 18 to 75 with a serious mental illness and diabetes (type 1 and type 2) whose most recent Hemoglobin A1c (HbA1c) level during the measurement year is >9.0%. | Milestone 4 | Established quality measure | Annual metrics that are an established quality measure | Claims Medical records |
Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 24 | Screening for Depression and Follow-Up Plan: Age 18 and Older (CDF-AD) | Percentage of beneficiaries age 18 and older screened for depression on the date of the encounter using an age appropriate standardized depression screening tool, AND if positive, a follow-up plan is documented on the date of the positive screen. | Milestone 4 | Established quality measure | Annual metrics that are an established quality measure | Claims Medical records |
Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 25 | Screening for Depression and Follow-Up Plan: Ages 12–17 (CDF-CH) | Percentage of beneficiaries ages 12 to 17 screened for depression on the date of the encounter using an age appropriate standardized depression screening tool, AND if positive, a follow-up plan is documented on the date of the positive screen. | Milestone 4 | Established quality measure | Annual metrics that are an established quality measure | Claims Electronic medical records |
Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 26 | Access to Preventive/Ambulatory Health Services for Medicaid Beneficiaries With SMI | The percentage of Medicaid beneficiaries age 18 years or older with SMI who had an ambulatory or preventive care visit during the measurement period. | Milestone 4 | Established quality measure | Annual metrics that are an established quality measure | Claims | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 27 | Tobacco Use Screening and Follow-up for People with Serious Mental Illness or Alcohol or Other Drug Dependence | The percentage of patients 18 years and older with a serious mental illness or alcohol or other drug dependence who received a screening for tobacco use and follow-up for those identified as a current tobacco user. Two rates are reported: | Milestone 4 | Established quality measure | Annual metrics that are an established quality measure | Claims | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | Percentage of adults with SMI who received a screening for tobacco use and follow-up for those identified as a current tobacco user | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | Percentage of adults with AOD who received a screening for tobacco use and follow-up for those identified as a current tobacco user | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| 28 | Alcohol Screening and Follow-up for People with Serious Mental Illness | The percentage of patients 18 years and older with a serious mental illness, who were screened for unhealthy alcohol use and received brief counseling or other follow-up care if identified as an unhealthy alcohol user. | Milestone 4 | Established quality measure | Annual metrics that are an established quality measure | Claims | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 29 | Metabolic Monitoring for Children and Adolescents on Antipsychotics | The percentage of children and adolescents ages 1 to 17 who had two or more antipsychotic prescriptions and had metabolic testing. Three rates are reported: | Milestone 4 | Established quality measure | Annual metrics that are an established quality measure | Claims | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | Percentage of children and adolescents on antipsychotics who received blood glucose testing | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | Percentage of children and adolescents on antipsychotics who received cholesterol testing | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| blank | blank | Percentage of children and adolescents on antipsychotics who received blood glucose and cholesterol testing | blank | blank | blank | blank | blank | blank | blank | blank | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||
| 30 | Follow-Up Care for Adult Medicaid Beneficiaries Who are Newly Prescribed an Antipsychotic Medication | Percentage of Medicaid beneficiaries age 18 years and older with new antipsychotic prescriptions who have completed a follow-up visit with a provider with prescribing authority within four weeks (28 days) of prescription of an antipsychotic medication. | Milestone 4 | Established quality measure | Annual metrics that are an established quality measure | Claims | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 32 | Total Costs Associated With Mental Health Services Among Beneficiaries With SMI/SED - Not Inpatient or Residential | The sum of all Medicaid spending for mental health services not in inpatient or residential settings during the measurement period. | Other SMI/SED metrics | CMS-constructed | Other annual metrics | Claims | Year | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 33 | Total Costs Associated With Mental Health Services Among Beneficiaries With SMI/SED - Inpatient or Residential | The sum of all Medicaid costs for mental health services in inpatient or residential settings during the measurement period. | Other SMI/SED metrics | CMS-constructed | Other annual metrics | Claims | Year | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 34 | Per Capita Costs Associated With Mental Health Services Among Beneficiaries With SMI/SED - Not Inpatient or Residential | Per capita costs for non-inpatient, non-residential services for mental health, among beneficiaries in the demonstration population during the measurement period. | Other SMI/SED metrics | CMS-constructed | Other annual metrics | Claims | Year | #DIV/0! | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| 35 | Per Capita Costs Associated With Mental Health Services Among Beneficiaries With SMI/SED - Inpatient or Residential | Per capita costs for inpatient or residential services for mental health among beneficiaries in the demonstration population during the measurement period. | Other SMI/SED metrics | CMS-constructed | Other annual metrics | Claims | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 36 | Grievances Related to Services for SMI/SED | Number of grievances filed during the measurement period that are related to services for SMI/SED. | Other SMI/SED metrics | CMS-constructed | Grievances and appeals | Administrative records | Quarter | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 37 | Appeals Related to Services for SMI/SED | Number of appeals filed during the measurement period that are related to services for SMI/SED. | Other SMI/SED metrics | CMS-constructed | Grievances and appeals | Administrative records | Quarter | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 38 | Critical Incidents Related to Services for SMI/SED | Number of critical incidents filed during the measurement period that are related to services for SMI/SED. | Other SMI/SED metrics | CMS-constructed | Grievances and appeals | Administrative records | Quarter | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 39 | Total Costs Associated With Treatment for Mental Health in an IMD Among Beneficiaries With SMI/SED | Total Medicaid costs for beneficiaries in the demonstration population who had claims for inpatient or residential treatment for mental health in an IMD during the reporting year. | Other SMI/SED metrics | CMS-constructed | Other annual metrics | Claims | Year | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| 40 | Per Capita Costs Associated With Treatment for Mental Health in an IMD Among Beneficiaries With SMI/SED | Per capita Medicaid costs for beneficiaries in the demonstration population who had claims for inpatient or residential treatment for mental health in an IMD during the reporting year. | Other SMI/SED metrics | CMS-constructed | Other annual metrics | Claims | Year | #DIV/0! | #DIV/0! | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Q1 | Insert selected metric(s) related to key health IT question 1 | Health IT | State-specific | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Q2 | Insert selected metric(s) related to key health IT question 2 | Health IT | State-specific | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Q3 | Insert selected metric(s) related to key health IT question 3 | Health IT | State-specific | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| State-specific metrics | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Add rows for any additional state-specific metrics | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Note: Licensee and state must prominently display the following notice on any display of Measure rates: The MPT, FUH-CH, FUH-AD, FUA-AD, FUM-AD, AAP, and APM measures (#13, 14, 15, 16, 17, 18, 7, 8, 9, 10, 26, 29) are Healthcare Effectiveness Data and Information Set (HEDIS®) measures that are owned and copyrighted by the National Committee for Quality Assurance (NCQA). HEDIS measures and specifications are not clinical guidelines, do not establish a standard of medical care and have not been tested for all potential applications. The measures and specifications are provided “as is” without warranty of any kind. NCQA makes no representations, warranties or endorsements about the quality of any product, test or protocol identified as numerator compliant or otherwise identified as meeting the requirements of a HEDIS measure or specification. NCQA makes no representations, warranties, or endorsement about the quality of any organization or clinician who uses or reports performance measures and NCQA has no liability to anyone who relies on HEDIS measures or specifications or data reflective of performance under such measures and specifications. The measure specification methodology used by CMS is different from NCQA’s methodology. NCQA has not validated the adjusted measure specifications but has granted CMS permission to adjust. A calculated measure result (a “rate”) from a HEDIS measure that has not been certified via NCQA’s Measure Certification Program, and is based on adjusted HEDIS specifications, may not be called a “HEDIS rate” until it is audited and designated reportable by an NCQA-Certified HEDIS Compliance Auditor. Until such time, such measure rates shall be designated or referred to as “Adjusted, Uncertified, Unaudited HEDIS rates.” |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| a States should create a new metrics report for each reporting quarter. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| b For state-specific metrics, states should attest that they are reporting as specified in their monitoring protocol. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| c Report metrics that are one annual value for a demonstration year only in the report specified in the reporting schedule. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| d If applicable. See CMS-provided technical specifications manual. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| e Enter any state-specific subpopulations that will be reported after column BF; create new columns as needed. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Checks: | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Numerator in #32 is equal to the Numerator in #34 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Numerator in #33 is equal to the Numerator in #35 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Denominator in #34 is equal to the Numerator in #22 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Denominator in #35 is equal to the Numerator in #22 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Denominator in #34 is equal to the Denominator in #35 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Numerator in #40 is equal to the Numerator in #39 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| End of worksheet | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Sheet 3: SMI-SED reporting issues
| Medicaid Section 1115 SMI/SED Demonstrations Monitoring Report (Part A) - Reporting issues (Version 2.0) | ||||||||
| State | [Enter State Name] | |||||||
| Demonstration Name | [Enter Demonstration Name] | |||||||
| SMI/SED Demonstration Year (DY) (Format: DY1, DY2, DY3, etc.) | [Enter SMI/SED Demonstration Year] | |||||||
| Calendar Dates for SMI/SED DY (Format: MM/DD/YYYY - MM/DD/YYYY) | [Enter Calendar Dates for SMI/SED Demonstration Year] | |||||||
| SMI/SED Reporting Period (Format: Q1, Q2, Q3, Q4) | [Enter SMI/SED Reporting Period] | |||||||
| Calendar Dates for SMI/SED Reporting Period (Format: MM/DD/YYYY - MM/DD/YYYY) | [Enter Calendar Dates for SMI/SED Reporting Period] | |||||||
| Serious Mental Illness/Serious Emotional Disturbance (SMI/SED) Metrics Reporting Issues | ||||||||
| # | Metric name | Milestone or reporting topic | Summary of issue | Date and report in which issue was first reported | Remediation plan and timeline for resolution | Status | Update(s) to issue summary, remediation plan, and/or timeline for resolution, if issue previously reported | |
| EXAMPLE: 24 |
EXAMPLE: Screening for Depression and Follow-Up Plan: Age 18 and Older (CDF-AD) |
EXAMPLE: Milestone 4 (Do not delete or edit this row) |
EXAMPLE: Difficulty with collecting data for metric 24. Necessary fields not available in one site’s EHR, so data for the measure cannot be extracted. |
EXAMPLE: 08/29/2021; SMI/SED DY3Q1 |
EXAMPLE: Demonstration site in process of updating EHR, to be completed in June 2022. Once completed, will report according to specification. |
EXAMPLE: Ongoing |
EXAMPLE: EHR implementation is preceeding as planned and will be completed by June 2022. |
|
| 1 | SUD Screening of Beneficiaries Admitted to Psychiatric Hospitals or Residential Treatment Settings (SUB-2) | Milestone 1 | ||||||
| 2 | Use of First-Line Psychosocial Care for Children and Adolescents on Antipsychotics (APP-CH) | Milestone 1 | ||||||
| 3 | All-Cause Emergency Department Utilization Rate for Medicaid Beneficiaries who may Benefit From Integrated Physical and Behavioral Health Care (PMH-20) | Milestone 2 | ||||||
| 4 | 30-Day All-Cause Unplanned Readmission Following Psychiatric Hospitalization in an Inpatient Psychiatric Facility (IPF) | Milestone 2 | ||||||
| 5 | Medication Reconciliation Upon Admission | Milestone 2 | ||||||
| 6 | Medication Continuation Following Inpatient Psychiatric Discharge | Milestone 2 | ||||||
| 7 | Follow-up After Hospitalization for Mental Illness: Ages 6-17 (FUH-CH) | Milestone 2 | ||||||
| 8 | Follow-up After Hospitalization for Mental Illness: Age 18 and older (FUH-AD) | Milestone 2 | ||||||
| 9 | Follow-up After Emergency Department Visit for Alcohol and Other Drug Abuse (FUA-AD) | Milestone 2 | ||||||
| 10 | Follow-Up After Emergency Department Visit for Mental Illness (FUM-AD) | Milestone 2 | ||||||
| 11 | Suicide or Overdose Death Within 7 and 30 Days of Discharge From an Inpatient Facility or Residential Treatment for Mental Health Among Beneficiaries With SMI or SED (count) | Milestone 2 | ||||||
| 12 | Suicide or Overdose Death Within 7 and 30 Days of Discharge From an Inpatient Facility or Residential Treatment for Mental Health Among Beneficiaries With SMI or SED (rate) | Milestone 2 | ||||||
| 13 | Mental Health Services Utilization - Inpatient | Milestone 3 | ||||||
| 14 | Mental Health Services Utilization - Intensive Outpatient and Partial Hospitalization | Milestone 3 | ||||||
| 15 | Mental Health Services Utilization - Outpatient | Milestone 3 | ||||||
| 16 | Mental Health Services Utilization - ED | Milestone 3 | ||||||
| 17 | Mental Health Services Utilization - Telehealth | Milestone 3 | ||||||
| 18 | Mental Health Services Utilization - Any Services | Milestone 3 | ||||||
| 19a | Average Length of Stay in IMDs | Milestone 3 | ||||||
| 19b | Average Length of Stay in IMDs (IMDs receiving FFP only) | Milestone 3 | ||||||
| 20 | Beneficiaries With SMI/SED Treated in an IMD for Mental Health | Milestone 3 | ||||||
| 21 | Count of Beneficiaries With SMI/SED (monthly) | Milestone 4 | ||||||
| 22 | Count of Beneficiaries With SMI/SED (annually) | Milestone 4 | ||||||
| 23 | Diabetes Care for Patients with Serious Mental Illness: Hemoglobin A1c (HbA1c) Poor Control (>9.0%) (HPCMI-AD) | Milestone 4 | ||||||
| 24 | Screening for Depression and Follow-Up Plan: Age 18 and Older (CDF-AD) | Milestone 4 | ||||||
| 25 | Screening for Depression and Follow-Up Plan: Ages 12–17 (CDF-CH) | Milestone 4 | ||||||
| 26 | Access to Preventive/Ambulatory Health Services for Medicaid Beneficiaries With SMI | Milestone 4 | ||||||
| 27 | Tobacco Use Screening and Follow-up for People with SMI or Alcohol or Other Drug Dependence | Milestone 4 | ||||||
| 28 | Alcohol Screening and Follow-up for People with SMI | Milestone 4 | ||||||
| 29 | Metabolic Monitoring for Children and Adolescents on Antipsychotics | Milestone 4 | ||||||
| 30 | Follow-Up Care for Adult Medicaid Beneficiaries Who are Newly Prescribed an Antipsychotic Medication | Milestone 4 | ||||||
| 32 | Total Costs Associated With Mental Health Services Among Beneficiaries With SMI/SED - Not Inpatient or Residential | Other SMI/SED metrics | ||||||
| 33 | Total Costs Associated With Mental Health Services Among Beneficiaries With SMI/SED - Inpatient or Residential | Other SMI/SED metrics | ||||||
| 34 | Per Capita Costs Associated With Mental Health Services Among Beneficiaries With SMI/SED - Not Inpatient or Residential | Other SMI/SED metrics | ||||||
| 35 | Per Capita Costs Associated With Mental Health Services Among Beneficiaries With SMI/SED - Inpatient or Residential | Other SMI/SED metrics | ||||||
| 36 | Grievances Related to Services for SMI/SED | Other SMI/SED metrics | ||||||
| 37 | Appeals Related to Services for SMI/SED | Other SMI/SED metrics | ||||||
| 38 | Critical Incidents Related to Services for SMI/SED | Other SMI/SED metrics | ||||||
| 39 | Total Costs Associated With Treatment for Mental Health in an IMD Among Beneficiaries With SMI/SED | Other SMI/SED metrics | ||||||
| 40 | Per Capita Costs Associated With Treatment for Mental Health in an IMD Among Beneficiaries With SMI/SED | Other SMI/SED metrics | ||||||
| Q1 | [Insert selected metric(s) for health IT question 1] | Health IT | ||||||
| Q2 | [Insert selected metric(s) for health IT question 2] | Health IT | ||||||
| Q3 | [Insert selected metric(s) for health IT question 3] | Health IT | ||||||
| Note: Licensee and state must prominently display the following notice on any display of Measure rates: The MPT, FUH-CH, FUH-AD, FUA-AD, FUM-AD, AAP, and APM measures (#13, 14, 15, 16, 17, 18, 7, 8, 9, 10, 26, 29) are Healthcare Effectiveness Data and Information Set (HEDIS®) measures that are owned and copyrighted by the National Committee for Quality Assurance (NCQA). HEDIS measures and specifications are not clinical guidelines, do not establish a standard of medical care and have not been tested for all potential applications. The measures and specifications are provided “as is” without warranty of any kind. NCQA makes no representations, warranties or endorsements about the quality of any product, test or protocol identified as numerator compliant or otherwise identified as meeting the requirements of a HEDIS measure or specification. NCQA makes no representations, warranties, or endorsement about the quality of any organization or clinician who uses or reports performance measures and NCQA has no liability to anyone who relies on HEDIS measures or specifications or data reflective of performance under such measures and specifications. The measure specification methodology used by CMS is different from NCQA’s methodology. NCQA has not validated the adjusted measure specifications but has granted CMS permission to adjust. A calculated measure result (a “rate”) from a HEDIS measure that has not been certified via NCQA’s Measure Certification Program, and is based on adjusted HEDIS specifications, may not be called a “HEDIS rate” until it is audited and designated reportable by an NCQA-Certified HEDIS Compliance Auditor. Until such time, such measure rates shall be designated or referred to as “Adjusted, Uncertified, Unaudited HEDIS rates.” |
||||||||
| End of worksheet | ||||||||
Sheet 4: Avail Assessment instructions
| Medicaid Section 1115 SMI/SED Demonstrations Availability Assessment - Instructions (Version 2.0) | ||
| Instructions for Completing the Assessment of the Availability of Mental Health Services ("Annual Availability Assessment" tab) | ||
| Before you begin: | The state will submit multiple Availability Assessments. The state will submit an Initial Availability Assessment at the time of application and annual assessments thereafter. | |
| In populating its Initial Availability Assessment and each subsequent Annual Availability Assessment, the state should report data as of the same month and day each year. In other words, if the Initial Availability Assessment displays values as of August 1, 2019, subsequent Availability Assessments should display values as of August 1, 2020, August 1, 2021, August 1, 2022, etc. Within each assessment, the state should enter this information into the cell labeled “Time Period Reflected in Assessment (month/day/year)" (found in the "Availability Assessment" tab). It is also important to use the same data sources to populate the Initial and Annual Availability Assessments. The state should enter information on its data sources into the columns labeled “Brief description of data source(s) used to populate this (sub-)section” (found in the “Availability Assessment” tab). |
||
| Enter the state name, data entry date(s), and time period reflected in the Availability Assessment in cells C2-4. | ||
| To hide pop-up instructions as you complete the Availability Assessment, hit "escape." | ||
| Please Note: To add rows for additional geographic designations you must use the "Add Row" button in cell F2 (you may need to click "Enable Content" at the top of the tab if it appears). Please do not add rows manually. | ||
| Column | Instructions | |
| B | In column B, enter each geographic designation starting in cell B10. Add rows using the "Add Row" button as needed to capture all geographic designations. Geographic designation means a state-defined geographic unit for reporting data, such as county, region, or catchment area. The state should consider how it divides its mental health system into smaller units or catchment areas to select geographic designations that will yield meaningful, actionable information. | |
| C | In column C, starting in cell C10, please select whether geographic designation entered in the corresponding cell in column B could be considered urban or rural. If the geographic designation should be categorized as something other than urban or rural, select "Other-please explain" and record an explanation in the notes box in column D. Urban is defined as a Metropolitan Statistical Area or a Metropolitan division (in the case where a Metropolitan Statistical Area is divided into Metropolitan Divisions), as defined by the Executive Office of Management and Budget (42 CFR § 412.64(b)) Rural is defined as any area outside an urban area as defined in 42 CFR § 412.64(b). | |
| D | In column D, beginning in cell D10, please use this space to explain the state's response if the state selects 'Other-please explain' in column C. | |
| E | In column E, starting in cell E10, enter the total number of adult Medicaid beneficiaries ages 18-20 in each geographic designation at the selected point in time. Medicaid beneficiary means a person who has been determined to be eligible to receive Medicaid services as defined at 42 CFR §400.200. Note: this age category is separate in order to avoid double counting beneficiaries in the residential treatment category and to facilitate the calculation of certain ratios in the assessment. See the note in the following cell for additional explanation. | |
| F | In column F, starting in cell F8, enter the number of adult Medicaid beneficiaries ages 18-20 with SMI in each geographic designation at the selected point in time. As defined on page 1 of the State Medicaid Directors Letter, serious mental illness means persons age 18 and over who currently, or at any time during the past year, have had a diagnosable mental, behavioral, or emotional disorder of sufficient duration to meet diagnostic criteria, that has resulted in functional impairment which substantially interferes with or limits one or more major life activities. Note: in the State Medicaid Directors letter (SMDL #18-011), SMI is defined to include individuals age 18 years and older, and SED includes children younger than 18. However, the residential treatment section of the Availability Assessment requests data on PRTFs, and the federal definition for PRTFs includes facilities that serve individuals under the age of 21. In order to avoid double counting beneficiaries in the residential treatment category, the assessment requests data on beneficiaries age 0-17, 18-20, and 21 and older separately. |
|
| G | In column G, starting in cell G8, enter the total number of adult Medicaid beneficiaries age 21 and older in each geographic designation at the selected point in time. | |
| H | In column H, starting in cell H10, enter the number of adult Medicaid beneficiaries age 21 and older with SMI in each geographic designation at the selected point in time. Note: in the SMDL, SMI is defined to include individuals age 18 years and older, and SED includes children younger than 18. However, the residential treatment section of the Availability Assessment requests data on PRTFs, and the federal definition for PRTFs includes facilities that serve individuals under the age of 21. In order to avoid double counting beneficiaries in the residential treatment category, the assessment requests data on beneficiaries age 0-17, 18-20, and 21 and older separately. |
|
| I | In column I, starting in cell I10, the Availability Assessment will automatically calculate the percent of adult Medicaid beneficiaries who have SMI in each geographic designation. The state should not input any values into this column or modify the formulas in this column. | |
| J | In column J, starting in cell J10, enter the total number of Medicaid beneficiaries under the age of 18 in each geographic designation at the selected point in time. | |
| K | In column K, starting in cell K10, enter the number of beneficiaries under the age of 18 with SED in each geographic designation at the selected point in time. As defined on page 2 of the SMDL, individuals with SED are those from birth up to age 18 who currently, or at any time during the past year, have had a diagnosable mental, behavioral, or emotional disorder of sufficient duration to meet diagnostic criteria that resulted in functional impairment which substantially interferes with or limits the child’s role or functioning in family, school, or community activities. Functional impairment” is defined as difficulties that substantially interfere with or limit a child or adolescent from achieving or maintaining one or more developmentally-appropriate social, behavioral, cognitive, communicative, or adaptive skills. | |
| L | In column L starting in cell L10, the Availability Assessment will automatically calculate the percent of beneficiaries under the age of 18 who have SED in each geographic designation. The state should not input any values into this column or modify the formulas in this column. | |
| M | In column M, starting in cell M10, the Availability Assessment will automatically calculate the number of Medicaid beneficiaries (total) in each geographic designation. | |
| N | In column N, starting in cell N10, the Availability Assessment will automatically calculate the percent with Medicaid beneficiaries with SMI or SED (total) in each geographic designation. | |
| O | In column O, starting in cell O10, the Availability Assessment will automatically calculate the percent with SMI or SED (total) in each geographic designation. | |
| P | In column P, beginning in cell P10, please use this space to provide notes about the data source(s) used to populate the section. | |
| Q | In column Q, beginning in cell Q10, please use this space to provide any additional notes regarding the section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| R | In column R, starting in cell R10, enter the number of psychiatrists or other practitioners who are authorized to prescribe psychiatric medications in each geographic designation. A psychiatrist is any psychiatrist licensed to practice in the state under state licensure laws. Other prescribers authorized to prescribe psychiatric medications means the number of mental health practitioners other than psychiatrists who are authorized to prescribe psychiatric medications as defined by state licensure laws. | |
| S | In column S, starting in cell S10, enter the number of Medicaid-enrolled psychiatrists or other practitioners who are authorized to prescribe psychiatric medications in each geographic designation. Medicaid-enrolled means any provider enrolled in Medicaid to obtain Medicaid billing privileges, as defined in 42 CFR §455.410. | |
| T | In column T, starting in cell T10, enter the number of Medicaid-enrolled psychiatrists or other practitioners who are authorized to prescribe psychiatric medications and are accepting new Medicaid patients in each geographic designation. Accepting new Medicaid patients means any provider enrolled in Medicaid to obtain Medicaid billing privileges who will treat new Medicaid-enrolled patients. | |
| U-W | In columns U-W, starting in cell U10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| X | In column X, beginning in cell X10, please use this space to provide details on the specific types of practitioners used to populate this sub-section. | |
| Y | In column Y, beginning in cell Y10, please use this space to provide notes about the data source(s) used to populate the sub-section. | |
| Z | In column Z, beginning in cell Z10, please use this space to provide any additional notes regarding the sub-section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| AA | In column AA, starting in cell AA10, enter the number of other practitioners certified or licensed to independently treat mental illness in each geographic designation. Other types of practitioners certified or licensed to independently treat mental illness means non-psychiatrist mental health providers who are certified or licensed to independently treat mental illness as defined by state licensure laws. This may include, but is not limited to, licensed psychologists, clinical social workers, and professional counselors. | |
| AB | In column AB, starting in cell AB10, enter the number of Medicaid-enrolled other types of practitioners certified and licensed to independently treat mental illness in each geographic designation. | |
| AC | In column AC, starting in cell AC10, enter the number of Medicaid-enrolled other types of practitioners certified and licensed to independently treat mental illness accepting new Medicaid patients in each geographic designation. | |
| AD-AF | In columns AD-AF, starting in cell AD10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| AG | In column AG, beginning in cell AG10, please use this space to provide details on the specific types of practitioners used to populate this sub-section. | |
| AH | In column AH, beginning in cell AH10, please use this space to provide notes about the data source(s) used to populate the sub-section. | |
| AI | In column AI, beginning in cell AI10, please use this space to provide any additional notes regarding the sub-section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| AJ | In column AJ, starting in cell AJ10, enter the number of community mental health centers (CMHCs) in each geographic designation. A community mental health center is an entity that provides outpatient mental health services, 24 hour emergency care services, day treatment, screenings, and consultation and educational services, as defined at 42 CFR §410.2. | |
| AK | In column AK, starting in cell AK10, enter the number of Medicaid-enrolled CMHCs in each geographic designation. | |
| AL | In column AL, starting in cell AL10, enter the number of Medicaid-enrolled CMHCs accepting new Medicaid patients in each geographic designation. | |
| AM-AO | In columns AM-AO, starting in cell AM10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| AP | In column AP, beginning in cell AP10, please use this space to provide notes about the data source(s) used to populate the section. | |
| AQ | In column AQ, beginning in cell AQ10, please use this space to provide any additional notes regarding the section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| AR | In column AR, starting in cell AR10, enter the number of providers offering intensive outpatient services in each geographic designation. Intensive outpatient services are designed to meet the needs of individuals who may be at risk for crisis or requiring a higher level of care, or who are in transition from a higher level of care. Intensive outpatient services may include partial hospitalization programs, day treatment, intensive outpatient programs, assertive community treatment, and other services and settings more intensive than regular outpatient and less intensive than inpatient or residential care. | |
| AS | In column AS, starting in cell AS10, enter the number of Medicaid-enrolled providers offering intensive outpatient services providers in each geographic designation. | |
| AT | In column AT, starting in cell AT10, enter the number of Medicaid-enrolled providers offering intensive outpatient services accepting new Medicaid patients in each geographic designation. | |
| AU-AW | In columns AU-AW, starting in cell AU10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| AX | In column AX, beginning in cell AX10, please use this space to provide details on the specific types of services used to populate this section. | |
| AY | In column AY, beginning in cell AY10, please use this space to provide notes about the data source(s) used to populate the section. | |
| AZ | In column AZ, beginning in cell AZ10, please use this space to provide any additional notes regarding the section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| BA | In column BA, starting in cell BA10, enter the number of residential mental health treatment facilities (adult) in each geographic designation. A residential mental health treatment facilities (adult) is a facility not licensed as a psychiatric hospital, whose primary purpose is to provide individually planned programs of mental health treatment services in a residential care setting for adults as defined for SAMHSA's N-MHSS. Please exclude residential SUD treatment facilities. | |
| BB | In column BB, starting in cell BB10, enter the number of Medicaid-enrolled residential mental health treatment facilities (adult) in each geographic designation. | |
| BC | In column BC, starting in cell BC10, enter the number of Medicaid-enrolled residential mental health treatment facilities (adult) accepting new Medicaid patients in each geographic designation. | |
| BD-BF | In columns BD-BF, starting in cell BD10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| BG | In column BG, starting in cell BG10, enter the total number of residential mental health treatment facility beds (adult) in each geographic designation. | |
| BH | In column BH, starting in cell BH10, enter the total number of Medicaid-enrolled residential mental health treatment beds (adult) in each geographic designation. | |
| BI | In column BI, starting in cell BI10, enter the total number of Medicaid-enrolled residential mental health treatment beds available to adult Medicaid patients in each geographic designation. Available to Medicaid adult Medicaid patients means any facility or bed available to serve Medicaid patients over the age of 110. | |
| BJ-BL | In columns BJ-BL, starting in cell BJ10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| BM | In column BM, beginning in cell BM10, please use this space to provide details on the specific types of facilities used to populate this sub-section. | |
| BN | In column BN, beginning in cell BN10, please use this space to provide notes about the data source(s) used to populate the sub-section. | |
| BO | In column BO, beginning in cell BO10, please use this space to provide any additional notes regarding the sub-section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| BP | In column BP, starting in cell BP10, enter the number of psychiatric residential treatment facilities (PRTF) in each geographic designation. A PRTF is a non-hospital facility with a provider agreement with a state Medicaid agency to provide the inpatient psychiatric services to individuals under age 21 benefit (psych under 21 benefit). The facility must be accredited by the Joint Commission, the Council on Accreditation of Services for Families and Children, the Commission on Accreditation of Rehabilitation Facilities, or any other accrediting organization with comparable standards recognized by the State. PRTFs must also meet the requirements at 42 CFR §441.151 - §441.1102, and 42 CFR §4103.350 – §4103.376. | |
| BQ | In column BQ, starting in cell BQ10, enter the number of Medicaid-enrolled PRTFs in each geographic designation. | |
| BR | In column BR, starting in cell BR10, enter the number of Medicaid-enrolled PRTFs accepting new Medicaid patients in each geographic designation. | |
| BS-BU | In columns BS-BU, starting in cell BS10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| BV | In column BV, starting in cell BV10, enter the total number of PRTF beds in each geographic designation. | |
| BW | In column BW, starting in cell BW10, enter the number of Medicaid-enrolled PRTF beds in each geographic designation. | |
| BX | In column BX, starting in cell BX10, enter the number of Medicaid-enrolled PRTF beds available to Medicaid patients in each geographic designation. Available to Medicaid patients means any facility or bed available to serve Medicaid patients. | |
| BY-CA | In columns BY-CA, starting in cell BY10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| CB | In column CB, beginning in cell CB10, please use this space to provide details on the specific types of facilities used to populate this sub-section. | |
| CC | In column CC, beginning in cell CC10, please use this space to provide notes about the data source(s) used to populate the sub-section. | |
| CD | In column CD, beginning in cell CD10, please use this space to provide any additional notes regarding the sub-section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| CE | In column CE, starting in cell CE10, enter the number of public and private psychiatric hospitals in each geographic designation. A psychiatric hospital is an institution which provides diagnosis and treatment of mentally ill persons, as defined at 42 USC §1395x. | |
| CF | In column CF, starting in cell CF10, enter the number of public and private psychiatric hospitals available to Medicaid patients in each geographic designation. | |
| CG-CH | In columns CG-CH, starting in cell CG10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| CI | In column CI, beginning in cell CI10, please use this space to provide notes about the data source(s) used to populate the sub-section. | |
| CJ | In column CJ, beginning in cell CJ10, please use this space to provide any additional notes regarding the sub-section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| CK | In column CK, starting in cell CK10, enter the number of psychiatric units in acute care hospitals in each geographic designation. A psychiatric unit is a separate inpatient psychiatric unit of a general hospital that provides inpatient mental health services and has specifically allocated staff and space (beds) for the treatment of persons with mental illness, as defined for SAMHSA's N-MHSS. | |
| CL | In column CL, starting in cell CL10, enter the number of psychiatric units in critical access hospitals (CAHs) in each geographic designation. A critical access hospital is a small facility that provides 24-hour emergency care, outpatient services, as well as inpatient services to people in rural areas, as defined in 42 CFR §4105.606. | |
| CM | In column CM, starting in cell CM10, enter the number of Medicaid-enrolled psychiatric units in acute care hospitals in each geographic designation. | |
| CN | In column CN, starting in cell CN10, enter the number of Medicaid-enrolled psychiatric units in CAHs in each geographic designation. | |
| CO | In column CO, starting in cell CO10, enter the number of Medicaid-enrolled psychiatric units in acute care hospitals accepting new Medicaid patients in each geographic designation. | |
| CP | In column CP starting in cell CP10, enter the number of Medicaid-enrolled psychiatric units in CAHs accepting new Medicaid patients in each geographic designation. | |
| CQ-CV | In columns CQ-CV, starting in cell CQ10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| CW | In column CW, beginning in cell CW10, please use this space to provide notes about the data source(s) used to populate the sub-section. | |
| CX | In column CX, beginning in cell CX10, please use this space to provide any additional notes regarding the sub-section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| CY | In column CY, starting in cell CY10, enter the number of licensed psychiatric hospital beds (psychiatric hospital + psychiatric units) in each geographic designation. Please enter the number of licensed psychiatric hospital beds as defined by state licensure requirements. | |
| CZ | In column CZ, starting in cell CZ10, enter the number of licensed psychiatric hospital beds (psychiatric hospital + psychiatric units) available to Medicaid patients in each geographic designation. | |
| DA-DB | In columns DA-DB, starting in cell DA10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| DC | In column DC, beginning in cell DC10, please use this space to provide notes about the data source(s) used to populate the sub-section. | |
| DD | In column DD, beginning in cell DD10, please use this space to provide any additional notes regarding the sub-section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| DE | In column DE, starting in cell DE10, enter the number of residential mental health treatment facilities (adult) that qualify as an institution for mental diseases (IMDs) in each geographic designation. An IMD is a hospital, nursing facility, or other institution of more than 16 beds that is primarily engaged in providing diagnosis, treatment or care of persons with mental diseases, including medical attention, nursing care and related services per section 1905(i) of the Social Security Act. See also 42 CFR §435.1010 and section 4390 of the State Medicaid Manual. | |
| DF | In column DF, starting in cell DF10, enter the number of Medicaid-enrolled residential mental health treatment facilities (adult) that qualify as IMDs in each geographic designation. | |
| DG | In column DG, starting in cell DG10, enter the number of Medicaid-enrolled residential mental health treatment facilities (adult) that qualify as IMDs accepting Medicaid patients in each geographic designation. | |
| DH-DJ | In columns DH-DJ, starting in cell DH10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| DK | In column DK, beginning in cell DK10, please use this space to provide details on the specific types of facilities used to populate this sub-section. | |
| DL | In column DL, beginning in cell DL10, please use this space to provide notes about the data source(s) used to populate the sub-section. | |
| DM | In column DM, beginning in cell DM10, please use this space to provide any additional notes regarding the sub-section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| DN | In column DN, starting in cell DN10, enter the number of psychiatric hospitals that qualify as IMDs in each geographic designation. | |
| DO | In column DO, starting in cell DO10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| DP | In column DP, beginning in cell DP10, please use this space to provide notes about the data source(s) used to populate the sub-section. | |
| DQ | In column DQ, beginning in cell DQ10, please use this space to provide any additional notes regarding the sub-section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| DR | In column DR, starting in cell DR10, enter the number of crisis call centers in each geographic designation. Please enter the number of crisis call centers as defined by the state. | |
| DS | In column DS, starting in cell DS10, enter the number of mobile crisis units in each geographic designation. A mobile crisis unit is a team that intervenes during mental health crises, as defined by the state. | |
| DT | In column DT, starting in cell DT10, enter the number of crisis observation/ assessment centers in each geographic designation. Please enter the number of observation or assessment centers as defined by the state. | |
| DU | In column DU, starting in cell DU10, enter the number of crisis stabilization units in each geographic designation. Crisis stabilization units offer medically monitored short-term crisis stabilization services, as defined by the state. | |
| DV | In column DV, starting in cell DV10, enter the number of coordinated community crisis response teams in each geographic designation. Coordinated community crisis response means a community-based program or entity that manages crisis response across various community entities or programs, as defined by the state. | |
| DW-EA | In columns DW-EA, starting in cell DW10, the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| EB | In column EB, beginning in cell EB10, please use this space to provide details on the specific types of services used to populate this section. | |
| EC | In column EC, beginning in cell EC10, please use this space to provide notes about the data source(s) used to populate the section. | |
| ED | In column ED, beginning in cell ED10, please use this space to provide any additional notes regarding the section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| EE | In column EE, starting in cell EE10, enter the number FQHCs that offer behavioral health services in each geographic designation. Federally qualified health center (FQHC) means an entity that has entered into an agreement with CMS to meet Medicare program requirements under 42 CFR §405.2434 and 42 CFR §405.2401. | |
| EF | In column EF, starting in cell EF10,the Availability Assessment will automatically calculate the ratios in each geographic designation. The state should not input any values into these columns or modify the formulas in these columns. | |
| EG | In column EG, beginning in cell EG10, please use this space to provide notes about the data source(s) used to populate the section. | |
| EH | In column EH, beginning in cell EH10, please use this space to provide any additional notes regarding the section, such as notes on data limitations, explanations for specific values, or information that could assist with data interpretation. | |
| EI | Beginning in column EI, add additional counts and ratios for provider and setting types that the state considers important to its mental health system. The state should not modify any of the previous columns. | |
| End of worksheet | ||
Sheet 5: Avail Assessment definitions
| Medicaid Section 1115 SMI/SED Demonstrations Availability Assessment - Definitions (Version 2.0) | |
| Definitions of terms used in the Availability Assessment | |
| Term | Definition |
| Accepting new Medicaid patients | Accepting new Medicaid patients means any provider enrolled in Medicaid to obtain Medicaid billing privileges who will treat new Medicaid-enrolled patients. |
| Adult | An adult is a person age 18 and over [SMDL]. |
| Available to Medicaid patients | Available to Medicaid patients means any facility or bed available to serve Medicaid patients. |
| Community mental health center (CMHC) | A community mental health center (CMHC) is defined in §410.2 as “an entity that (1) provides outpatient services, including specialized outpatient services for children, the elderly, individuals who are chronically mentally ill, and clients of its mental health service area who have been discharged from inpatient treatment at a mental health facility; (2) provides 24-hour-a-day emergency care services; (3) provides day treatment or other partial hospitalization services, or psychosocial rehabilitation services; (4) provides screening for patients being considered for admission to state mental health facilities to determine the appropriateness of this admission; (5) meets applicable licensing or certification requirements for CMHCs in the state in which it is located; and (6) provides at least 40 percent of its services to individuals who are not eligible for benefits under title XVIII of the Social Security Act. |
| Coordinated community crisis response | Coordinated community crisis response means a community-based program or entity that manages crisis response across various community entities or programs, as defined by the state. |
| Crisis call center | Crisis call centers are defined by the state. |
| Crisis stabilization unit | Crisis stabilization units offer medically monitored short-term crisis stabilization services, as defined by the state. |
| Critical access hospital | A critical access hospital is a small facility that provides 24-hour emergency care, outpatient services, as well as inpatient services to people in rural areas, as defined in 42 CFR §485.606. |
| Federally qualified health center | Federally qualified health center (FQHC) means an entity that meets all the requirements at 1905(l)(2)(B) of the Social Security Act. |
| Geographic designation | Geographic designation means a state-defined geographic unit for reporting data, such as county, region, or catchment area. |
| Institution for mental diseases (IMD) | An institution for mental diseases is a hospital, nursing facility, or other institution of more than 16 beds that is primarily engaged in providing diagnosis, treatment or care of persons with mental diseases, including medical attention, nursing care and related services per section 1905(i) of the Social Security Act. See also 42 CFR §435.1010 and section 4390 of the State Medicaid Manual. |
| Intensive outpatient services | Intensive outpatient services are designed to meet the needs of individuals who may be at risk for crisis or requiring a higher level of care, or who are in transition from a higher level of care. Intensive outpatient services may include partial hospitalization programs, day treatment services, intensive outpatient programs, Assertive Community Treatment, intensive case management, intensive peer supports, written standardized protocols for escalating outpatient services when an individual is experiencing a crisis or increased need, and other services and settings more intensive than regular outpatient and less intensive than inpatient or residential care. |
| Licensed psychiatric hospital bed | Licensed psychiatric hospital bedsare defined by state licensure requirements. |
| Medicaid beneficiary | Medicaid beneficiary means a person who has been determined to be eligible to receive Medicaid services as defined at 42 CFR §400.200. |
| Medicaid-enrolled | Medicaid-enrolled means any provider enrolled in Medicaid to obtain Medicaid billing privileges, as defined in 42 CFR §455.410. |
| Mental health practitioners other than psychiatrists who are certified or licensed by the state to independently treat mental illness | Mental health practitioners other than psychiatrists who are certified or licensed to independently treat mental illness are non-psychiatrist mental health providers who are certified or licensed to independently treat mental illness as defined by state licensure laws. This may include, but is not limited to, licensed psychologists, clinical social workers, and professional counselors. Practitioners who are required to work under the supervision of another practitioner and/or who are required to bill Medicaid under another practitioner should be excluded. |
| Mobile crisis unit | A mobile crisis unit is a team that intervenes during mental health crises, as defined by the state. |
| Observation or assessment centers | Observation or assessment centers are defined by the state. |
| Other practitioners who are authorized to prescribe psychiatric medications | Other practitioners who are authorized to prescribe psychiatric medications are defined by state licensure laws. |
| Psychiatric hospital | A psychiatric hospital is an institution which provides diagnosis and treatment of mentally ill person, as defined at 42 USC §1395x. The state should report on both public and private psychiatric hospitals. |
| Psychiatric residential treatment facility (PRTF) | A psychiatric residential treatment facility is a non-hospital facility with a provider agreement with a state Medicaid agency to provide the inpatient psychiatric services to individuals under age 21 benefit (psych under 21 benefit). The facility must be accredited by the Joint Commission, the Council on Accreditation of Services for Families and Children, the Commission on Accreditation of Rehabilitation Facilities, or any other accrediting organization with comparable standards recognized by the State. PRTFs must also meet the requirements at 42 CFR §441.151 - §441.182, and 42 CFR §483.350 – §483.376. |
| Psychiatric unit | A psychiatric unit is a separate inpatient psychiatric unit of a general hospital that provides inpatient mental health services and has specifically allocated staff and space (beds) for the treatment of persons with mental illness, as defined for SAMHSA's National Mental Health Services Survey (N-MHSS). |
| Psychiatrist | A psychiatrist is any psychiatrist licensed to practice in the state under state licensure laws. |
| Residential mental health treatment facilities (adult) | A residential mental health treatment facilities (adult) is a facility not licensed as a psychiatric hospital, whose primary purpose is to provide individually planned programs of mental health treatment services in a residential care setting for adults as defined for SAMHSA's N-MHSS. Please exclude residential SUD treatment facilities. |
| Rural | Rural means any area outside an urban area as defined in 42 CFR § 412.64(b). |
| Serious emotional disturbance (SED) | Persons with serious emotional disturbance means individuals from birth up to age 18 who currently, or at any time during the past year, have had a diagnosable mental, behavioral, or emotional disorder of sufficient duration to meet diagnostic criteria that resulted in functional impairment which substantially interferes with or limits the child’s role or functioning in family, school, or community activities. Functional impairment” is defined as difficulties that substantially interfere with or limit a child or adolescent from achieving or maintaining one or more developmentally-appropriate social, behavioral, cognitive, communicative, or adaptive skills [SMDL]. |
| Serious mental illness (SMI) | Persons with serious mental illness means individuals, age 18 and over, who currently, or at any time during the past year, have had a diagnosable mental, behavioral, or emotional disorder of sufficient duration to meet diagnostic criteria, that has resulted in functional impairment which substantially interferes with or limits one or more major life activities. [SMDL] Note: in the SMDL, SMI is defined to include individuals age 18 years and older, and SED includes children younger than 18. However, the residential treatment section of the availability assessment requests data on PRTFs, and the federal definition for PRTFs includes facilities that serve individuals under the age of 21. In order to avoid double counting beneficiaries in the residential treatment category, the assessment requests data on beneficiaries age 0-17, 18-20, and 21 and older separately. |
| Urban | Urban means a Metropolitan Statistical Area or a Metropolitan division (in the case where a Metropolitan Statistical Area is divided into Metropolitan Divisions), as defined by the Executive Office of Management and Budget (42 CFR § 412.64(b)). |
| End of worksheet | |
Sheet 6: Annual Avail Assessment
| Medicaid Section 1115 SMI/SED Demonstrations Annual Availability Assessment (Version 2.0) | 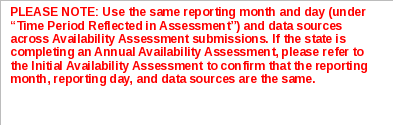
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| State Name | 
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Date of Assessment | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Time Period Reflected in Assessment (month/day/year) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Geographic Designation | Beneficiaries | Providers | Community Mental Health Centers | Intensive Outpatient Services | Residential Mental Health Treatment Facilities | Inpatient | Institutions for Mental Diseases | Crisis Stabilization Services | Federally Qualified Health Centers | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Adult | Children | Total | Psychiatrists or Other Practitioners Who Are Authorized to Prescribe Psychiatric Medications | Other Practitioners Certified and Licensed to Independently Treat Mental Illness | Residential Mental Health Treatment Facilities (Adult) | Psychiatric Residential Treatment Facilities | Public and Private Psychiatric Hospitals | Psychiatric Units | Psychiatric Beds | Residential Treatment Facilities That Qualify As IMDs | Psychiatric Hospitals That Qualify As IMDs | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| . | Geographic designation | Is this geographic designation primarily urban or rural? | Additional notes on this sub-section, including data limitations | Number of adult Medicaid beneficiaries (18 - 20) | Number of adult Medicaid beneficiaries with SMI (18 - 20) |
Number of adult Medicaid beneficiaries (21+) | Number of adult Medicaid beneficiaries with SMI (21+) | Percent with SMI (Adult) | Number of Medicaid beneficiaries (0 - 17) | Number of Medicaid beneficiaries with SED (0 - 17) |
Percent with SED (0-17) | Number of Medicaid beneficiaries (Total) | Number of Medicaid beneficiaries with SMI or SED (Total) | Percent with SMI or SED (Total) | Brief description of data source(s) used to populate this section | Additional notes on this section, including data limitations | Number of Psychiatrists or Other Practitioners Who Are Authorized to Prescribe Psychiatric Medications | Number of Medicaid-Enrolled Psychiatrists or Other Practitioners Who Are Authorized to Prescribe Psychiatric Medications | Number of Medicaid-Enrolled Psychiatrists or Other Practitioners Who Are Authorized to Prescribe Psychiatric Medications Accepting New Medicaid Patients | Ratio of Medicaid beneficiaries with SMI/SED to Medicaid-Enrolled Psychiatrists or Other Prescribers | Ratio of Total Psychiatrists or Other Prescribers to Medicaid-Enrolled Psychiatrists or Other Prescribers | Ratio of Medicaid-Enrolled Psychiatrists or Other Prescribers to Medicaid-Enrolled Psychiatrists or Other Prescribers Accepting New Medicaid Patients | Specific type(s) of practitioners used to populate this sub-section | Brief description of data source(s) used to populate this sub-section | Additional notes on this sub-section, including data limitations | Number of Other Practitioners Certified or Licensed to Independently Treat Mental Illness | Number of Medicaid-Enrolled Other Practitioners Certified or Licensed to Independently Treat Mental Illness | Number of Medicaid-Enrolled Other Practitioners Certified or Licensed to Independently Treat Mental Illness Accepting New Medicaid Patients | Ratio of Medicaid Beneficiaries with SMI/SED to Medicaid-Enrolled Other Practitioners Certified or Licensed to Independently Treat Mental Illness | Ratio of Other Practitioners Certified or Licensed to Independently Treat Mental Illness to Medicaid-Enrolled Other Practitioners Certified or Licensed to Independently Treat Mental Illness | Ratio of Medicaid-Enrolled Other Practitioners Certified and Licensed to Independently Treat Mental Illness to Medicaid-Enrolled Other Practitioners Certified and Licensed to Independently Treat Mental Illness Accepting New Patients | Specific type(s) of practitioners used to populate this sub-section | Brief description of data source(s) used to populate this sub-section | Additional notes on this sub-section, including data limitations | Number of CMHCs | Number of Medicaid- Enrolled CMHCs | Number of Medicaid-Enrolled CMHCs Accepting New Medicaid Patients | Ratio of Medicaid Beneficiaries with SMI/SED to Medicaid- Enrolled CMHCs | Ratio of Total CMHCs to Medicaid- Enrolled CMHCs | Ratio of Medicaid-Enrolled CMHCs to Medicaid-Enrolled CMHCs Accepting New Patients | Brief description of data source(s) used to populate this section | Additional notes on this section, including data limitations | Number of Providers Offering Intensive Outpatient Services | Number of Medicaid-Enrolled Providers Offering Intensive Outpatient Services | Number of Medicaid-Enrolled Providers Offering Intensive Outpatient Services | Ratio of Medicaid Beneficiaries with SMI/SED to Medicaid- Enrolled Providers Offering Intensive Outpatient Services | Ratio of Total Facilities/ Programs Offering Intensive Outpatient Services to Medicaid-Enrolled Providers Offering Intensive Outpatient Services | Ratio of Medicaid-Enrolled Providers Offering Intensive Outpatient Services to Medicaid- Enrolled Providers Offering Intensive Outpatient Services Accepting New Medicaid Patients | Specific type(s) of services used to populate this section | Brief description of data source(s) used to populate this section | Additional notes on this section, including data limitations | Number of Residential Mental Health Treatment Facilities (Adult) | Number of Medicaid- Enrolled Residential Mental Health Treatment Facilities (Adult) | Number of Medicaid-Enrolled Residential Mental Health Treatment Facilities Accepting New Medicaid Patients (Adult) | Ratio of Medicaid Beneficiaries with SMI (Adult) to Medicaid- Enrolled Residential Mental Health Treatment Facilities (Adult) | Ratio of Total Residential Mental Health Treatment Facilities (Adult) to Medicaid-Enrolled Residential Mental Health Treatment Facilities (Adult) | Ratio of Medicaid-Enrolled Residential Mental Health Treatment Facilities (Adult) to Medicaid- Enrolled Residential Mental Health Treatment Facilities (Adult) Accepting New Patients | Total Number of Residential Mental Health Treatment Facility Beds (Adult) | Total Number of Medicaid- Enrolled Residential Mental Health Treatment Beds (Adult) | Total Number of Medicaid-Enrolled Residential Mental Health Treatment Beds Available to Adult Medicaid Patients | Ratio of Medicaid Beneficiaries with SMI (Adult) to Medicaid-Enrolled Residential Mental Health Treatment Beds | Ratio of Total Residential Mental Health Treatment Beds to Medicaid-Enrolled Residential Mental Health Treatment Beds | Ratio of Medicaid-Enrolled Residential Mental Health Treatment Beds to Medicaid- Enrolled Residential Mental Health Treatment Beds Available to Medicaid Patients | Specific type(s) of facilities used to populate this sub-section | Brief description of data source(s) used to populate this sub-section | Additional notes on this sub-section, including data limitations | Number of Psychiatric Residential Treatment Facilities (PRTF) | Number of Medicaid- Enrolled PRTFs | Number of Medicaid-Enrolled PRTFs Accepting New Medicaid Patients | Ratio of Medicaid Beneficiaries with SED to Medicaid-Enrolled PTRFs | Ratio of Total PTRFs to Medicaid- Enrolled PRTFs | Ratio of Medicaid-Enrolled PRTFs to Medicaid-Enrolled PRTFs Accepting New Medicaid Patients | Total Number of PRTF Beds | Number of Medicaid-Enrolled PRTF Beds | Number of Medicaid-Enrolled PRTF Beds Available to Medicaid Patients | Ratio of Medicaid Beneficiaries with SED to Medicaid-Enrolled PRTF Beds Available to Medicaid Patients | Ratio of Total Number of PRTF Beds to Medicaid- Enrolled PRTF Beds | Ratio of Medicaid- Enrolled PRTF Beds to Medicaid- Enrolled PRTFs Available to Medicaid Patients | Specific type(s) of facilities used to populate this sub-section | Brief description of data source(s) used to populate this sub-section | Additional notes on this sub-section, including data limitations | Number of Public and Private Psychiatric Hospitals | Public and Private Psychiatric Hospitals Available to Medicaid Patients | Ratio of Medicaid Beneficiaries with SMI/SED to Public and Private Psychiatric Hospitals Available to Medicaid Patients | Ratio of Public and Private Psychiatric Hospitals to Public and Private Psychiatric Hospitals Available to Medicaid Patients | Brief description of data source(s) used to populate this sub-section | Additional notes on this sub-section, including data limitations | Number of Psychiatric Units in Acute Care Hospitals | Number of Psychiatric Units in Critical Access Hospitals (CAHs) | Number of Medicaid- Enrolled Psychiatric Units in Acute Care Hospitals | Number of Medicaid-Enrolled Psychiatric Units in CAHs | Number of Medicaid-Enrolled Psychiatric Units in Acute Care Hospitals Accepting New Medicaid Patients | Number of Medicaid-Enrolled Psychiatric Units in CAHs Accepting New Medicaid Patients | Ratio of Medicaid Beneficiaries with SMI/SED to Medicaid-Enrolled Psychiatric Units in Acute Care Hospitals | Ratio of Medicaid Beneficiaries with SMI/SED to Medicaid-Enrolled Psychiatric Units in CAHs | Ratio of Psychiatric Units in Acute Care Hospitals to Medicaid-Enrolled Psychiatric Units in Acute Care Hospitals | Ratio of Psychiatric Units in CAHs to Medicaid-Enrolled Psychiatric Units in CAHs | Ratio of Medicaid-Enrolled Psychiatric Units in Acute Care Hospitals to Medicaid-Enrolled Psychiatric Units in Acute Care Hospitals Accepting New Medicaid Patients | Ratio of Medicaid-Enrolled Psychiatric Units in CAHs to Medicaid-Enrolled Psychiatric Units in CAHs Accepting New Medicaid Patients | Brief description of data source(s) used to populate this sub-section | Additional notes on this sub-section, including data limitations | Number of Licensed Psychiatric Hospital Beds (Psychiatric Hospital + Psychiatric Units) | Number of Licensed Psychiatric Hospital Beds (Psychiatric Hospital + Psychiatric Units) Available to Medicaid Patients | Ratio of Medicaid Beneficiaries with SMI/SED to Licensed Psychiatric Hospital Beds Available to Medicaid Patients | Ratio of Licensed Psychiatric Hospital Beds to Licensed Psychiatric Hospital Beds Available to Medicaid Patients | Brief description of data source(s) used to populate this sub-section | Additional notes on this sub-section, including data limitations | Number of Residential Mental Health Treatment Facilities (Adult) that Qualify as IMDs | Number of Medicaid- Enrolled Residential Mental Health Treatment Facilities (Adult) that Qualify as IMDs | Number of Medicaid- Enrolled Residential Mental Health Treatment Facilities (Adult) that Qualify as IMDs Accepting Medicaid Patients | Ratio of Medicaid Beneficiaries with SMI (Adult) to Medicaid- Enrolled Residential Mental Health Treatment Facilities that Qualify as IMDs | Ratio of Total Residential Mental Health Treatment Facilities (Adult) that Qualify as IMDs to Medicaid-Enrolled Residential Mental Health Treatment Facilities (Adult) that Qualify as IMDs | Ratio of Medicaid-Enrolled Residential Mental Health Treatment Facilities (Adult) that Qualify as IMDs to Medicaid- Enrolled Residential Mental Health Treatment Facilities (Adult) that Qualify as IMDs Accepting New Medicaid Patients | Specific type(s) of facilities used to populate this sub-section | Brief description of data source(s) used to populate this sub-section | Additional notes on this sub-section, including data limitations | Number of Psychiatric Hospitals that Qualify as IMDs | Ratio of Medicaid Beneficiaries with SMI/SED to Psychiatric Hospitals that Qualify as IMDs | Brief description of data source(s) used to populate this sub-section | Additional notes on this sub-section, including data limitations | Number of Crisis Call Centers | Number of Mobile Crisis Units | Number of Crisis Observation/ Assessment Centers | Number of Crisis Stabilization Units | Number of Coordinated Community Crisis Response Teams | Ratio of Medicaid Beneficiaries with SMI/SED to Crisis Call Centers | Ratio of Medicaid Beneficiaries with SMI/SED to Mobile Crisis Units | Ratio of Medicaid Beneficiaries with SMI/SED to Crisis Observation/ Assessment Centers | Ratio of Medicaid Beneficiaries with SMI/SED to Crisis Stabilization Units | Ratio of Medicaid Beneficiaries with SMI/SED to Coordinated Community Crisis Response Teams | Specific type(s) of services used to populate this section | Brief description of data source(s) used to populate this section | Additional notes on this section, including data limitations | Number FQHCs that Offer Behavioral Health Services | Ratio of Medicaid Beneficiaries with SMI/SED to FQHCs that Offer Behavioral Health Services | Brief description of data source(s) used to populate this section | Additional notes on this section, including data limitations | |
| 1. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 7. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 16. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 19. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 20. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 21. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 22. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 23. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 24. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 25. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 26. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 27. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 28. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 29. | - | - | 0 | 0 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Total | 0 | 0 | 0 | 0 | - | 0 | 0 | - | 0 | 0 | - | 0 | 0 | 0 | - | - | - | 0 | 0 | 0 | - | - | - | 0 | 0 | 0 | - | - | - | 0 | 0 | 0 | - | - | - | 0 | 0 | 0 | - | - | - | 0 | 0 | 0 | - | - | - | 0 | 0 | 0 | - | - | - | 0 | 0 | 0 | - | - | - | 0 | 0 | - | - | 0 | 0 | 0 | 0 | 0 | 0 | - | - | - | - | - | - | 0 | 0 | - | - | 0 | 0 | 0 | - | - | - | 0 | - | 0 | 0 | 0 | 0 | 0 | - | - | - | - | - | 0 | - | |||||||||||||||||||||||||||||||||||||||
| End of worksheet | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| File Type | application/vnd.openxmlformats-officedocument.spreadsheetml.sheet |
| File Modified | 0000-00-00 |
| File Created | 0000-00-00 |
© 2026 OMB.report | Privacy Policy