Form CMS-10398 #79 CMS-10398 #79 COVID-19 Risk Corridor Reconciliation Reporting Template
[Medicaid] Generic Clearance for Medicaid and CHIP State Plan, Waiver, and Program Submissions (CMS-10398)
COVID-19 Risk Corridor Reconciliation Reporting Template.xlsm
#79 (New): COVID-19 Risk Corridor Reconciliation Reporting Template
OMB: 0938-1148
⚠️ Notice: This form may be outdated. More recent filings and information on OMB 0938-1148 can be found here:
Document [xlsx]
Download: xlsx | pdf
I_State, program, and plan info
Overview
InstructionsI_State, program, and plan info
Sheet 1: Instructions
| Column A is blank. All information begins in column B, row 1. | Reporting Template for COVID-19 Risk Corridor Reconciliation | ||||||||||||||
| Instructions | |||||||||||||||
| Overview | |||||||||||||||
| Regulations at 42 C.F.R. § 438.6 outline provisions related to payments to Medicaid Managed Care Organizations (MCOs), Prepaid Inpatient Health Plans (PIHPs), and Prepaid Ambulatory Health Plans (PAHPs)—collectively referred to as “managed care plans.” The purpose of this template is to collect and analyze reconciliations for one and two-sided risk corridors that states implemented to reduce uncertainty associated with the COVID-19 Public Health Emergency. To submit this information to the Centers for Medicare & Medicaid Services (CMS), states should complete one (1) template with information for all applicable plans within a program during a particular rating period. States are not expected to report risk corridor reconciliation results in this document for rating periods that end after December 31, 2021. If states have multiple programs that used different COVID-19-related risk corridors or have completed multiple reconciliations, they should submit one (1) template per reconciliation. Consistent with the Managed Care Program Annual Report (MCPAR) required by 42 C.F.R. § 438.66(e), this template defines a program as a group of plans that have a specified set of benefits, eligibility criteria, and capitation rate cells that are articulated in a contract between the state and managed care plans. Information that states submit in this template will assist CMS in helping oversee the performance of state Medicaid managed care plans. Questions regarding the completion of this template should be sent to: [email protected]. |
|||||||||||||||
| Organization | |||||||||||||||
| This template is dynamic and contains formulas to help states submit the information to CMS efficiently and accurately. It includes three tabs (Tabs I, II, and III), which states should fill out in succession. When opening a new file, states will only see this current "Instructions" tab and Tab I. States will use macro-enabled buttons to unhide tabs II and III as they proceed through the reporting process (see “Inputting Information”). In Tab I ("State, program, and plan information"), states should provide general information about the program, the managed care plans (up to 40 plans) and the COVID-19 related risk corridors that have been implemented. Information entered here will determine the layout of the subsequent Tabs II and III. In Tab II ("Risk corridor reconciliation information"), states should provide details on the risk corridor structure and report on plan-level revenue and expenses that are eligible for reconciliations according to the risk corridor. Information entered here will feed into the imbedded formulas that will calculate the final reconciliation amounts. In Tab III ("Detailed plan revenue and expenses"), states should provide detailed breakdowns on plan-level revenue and expenses by month or quarter; states also have the option of reporting specific revenue/expense sources eligible for reconciliations. |
|||||||||||||||
|
|||||||||||||||
| Inputting information | 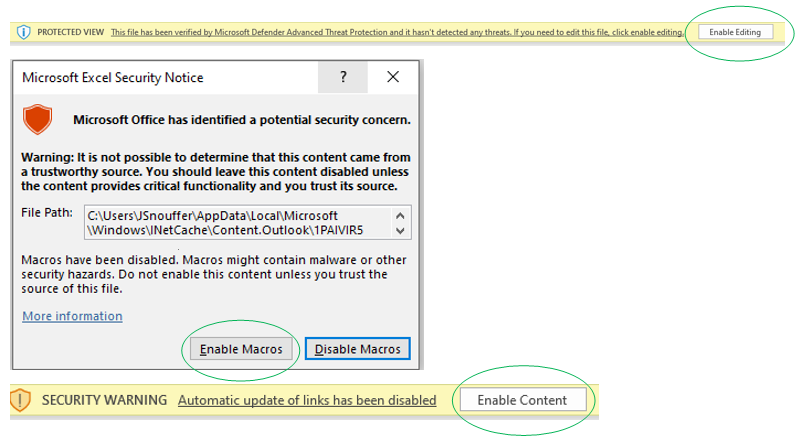
|
||||||||||||||
| A description of how to input information is provided below. Subsequent sections/tabs provide further instructions on how each item should be reported in the “Item Instructions” column. The types of data to be entered (for example, free text, numerical or drop-down list of set values) are specified in the “Data Format” columns. Cells are color coded based on their contents, as follows: | |||||||||||||||
| BEIGE: Cell is a required data entry item. States must follow instructions and input the type of data as specified. | |||||||||||||||
| BLUE: Cell is an optional data entry item. States may follow instructions and input the type of data as specified. These items will also have "(Optional)" in the description. | |||||||||||||||
| GREY: Cell contains a formula and is automatically filled once input data is entered. Grey cells are locked for data entry; states should not attempt to change anything. | |||||||||||||||
| GREEN: Cell contains example data, for reference only. States can refer to the example before they complete the relevant items. | |||||||||||||||
| WHITE: Cell contains instructions, for reference only. States should not attempt to change anything. | |||||||||||||||
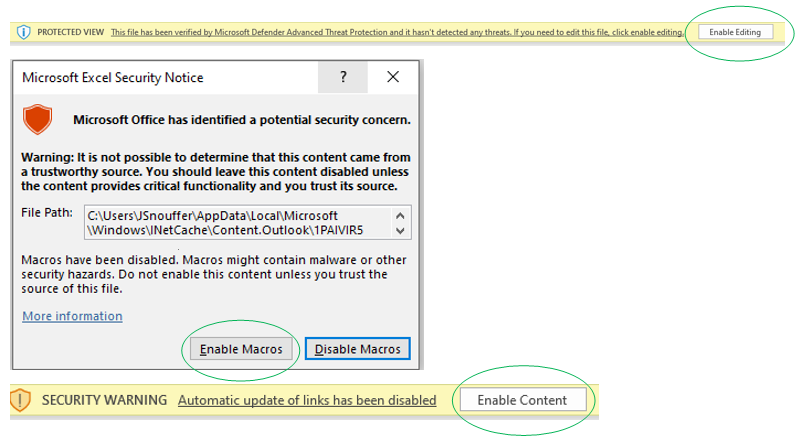
| NOTE: This template requires the use of macros. You may not use this file in "read-only" mode but must save this file. If you have not already enabled content on this file, please do so now. The image on the right shows prompts you may receive and circles the items that a user must select to enable full functionality. NOTE: The template is dynamic and all information in the first tab “I_State, program, and plan info” must be completed before entering data in subsequent tabs. |
|||||||||||||||
| Tab I. State, Program, and Plan Information | |||||||||||||||
| I.A. State and Program Information States should use this section to report their contact information, date of report submission, program information, and other related information. All items are required. I.B Plan Information States should use this section to report information of applicable plans (up to 40 plans) for the risk corridor. All items are required. I.C Risk Corridor Information States must enter all information in this section to determine the layout of the subsequent Tabs II and III. Only information on programs with risk corridors that are specific to the COVID-19 Public Health Emergency should be provided in this template. I.D Covered Providers - Optional If the risk corridor covers a specific program, states may use this section to report the types of provider covered under the program. States can enter "N/A" if the risk corridor is "state-based", meaning the risk corridor applies uniformly to all managed care programs within the state. After completing Tab 1, please click the "Proceed to Tab II" button. This will allow the layout of Tabs II and III to match information provided in Tab I. |
|||||||||||||||
| Tab II. Risk Corridor Reconciliation Information | |||||||||||||||
| II.A. Risk Corridor Features States should use this section to describe key features of the risk corridor being reported on, such as number of bands and target methodology. After completing this section, please click the "Continue Tab II" button to complete the remaining Tab II items. This will allow the layout of the subsequent sections to match features described in Section II.A. II.B. Risk Corridor Band Boundaries States should use this section to specify the risk corridor band boundaries as well as the risk sharing percentages in line with the state’s design of the risk corridor. An example is provided to illustrate how states should complete this section to ensure that the formula-driven reconciliation amounts are calculated correctly. II.C. Eligible Revenue and Expenses for Determining Reconciliations States should use Items II.C.1 and II.C.2 in this section to report the risk corridor target and actuals in terms of the eligible revenue and expense for determining reconciliation amounts for each plan in the risk corridor. After completing Items II.C.1 and II.C.2, please proceed to review item II.C.3, sections II.D through II.G and item II.H.1, which have been pre-populated with formulas to automatically calculate the reconciliation amount according to the risk corridor being reported on. No data entry is allowed with these items. II.H. Federal Share of Reconciliation After confirming the reconciliation amounts as calculated, states should use items II.H.2 through II.H.4 to report the federal and non-federal shares of the gross reconciliation payment. If the state has not established the final federal share amount, please provide an estimate. Please contact [email protected], if the total reconciliation amounts shown in items II.G.1 and II.H.1 is not as expected. Click the "Proceed to Tab III" button. This will allow the layout of Tab III to match information provided in Tab II. |
|||||||||||||||
| Tab III. Detailed Plan Revenue and Expenses | |||||||||||||||
| III.A Monthly/Quarterly Plan Revenue and Expenses States should use this section to report a monthly or quarterly (per item I.C.3) breakdown of plan revenue and expenses that are eligible for the risk corridor reconciliation. For quality assurance, the template automatically compares annual revenue and expenses as reported in Tab II. This is the last required item in this template. III.B Revenue Sources by Plan (Annual) - Optional States may report annual breakdown by revenue sources (per item II.A.5). This section is optional, but states are highly encouraged to provide additional detail that will assist in the CMS review of the reconciliation results. III.C Expense Sources by Plan (Annual) - Optional States may report annual breakdown by expense sources (per item II.A.6). This section is optional, but states are highly encouraged to provide additional detail that will assist in the CMS review of the reconciliation results. |
|||||||||||||||
| End of worksheet | |||||||||||||||
|
|||||||||||||||
Sheet 2: I_State, program, and plan info
| Column A is blank. All information begins in column B, row 2. | ||||||||||||||||||||||||||||||||||||||||||||
| I. State, program, and plan information | ||||||||||||||||||||||||||||||||||||||||||||
| A. State and program information | ||||||||||||||||||||||||||||||||||||||||||||
| States should use this section to report their contact information, date of report submission, program information, and other related information. (All items in this section require input.) | Input state/program-level data in this column | |||||||||||||||||||||||||||||||||||||||||||
| # | Item | Item Instructions | Data Format | [State] | ||||||||||||||||||||||||||||||||||||||||
| I.A.1 | Contact name | Enter the name of the individual(s) filling out this document. | Free text | |||||||||||||||||||||||||||||||||||||||||
| I.A.2 | Contact email address | Enter the email address(es) of the individual(s) filling out this document. | Free text | |||||||||||||||||||||||||||||||||||||||||
| I.A.3 | State or territory | Enter the state or territory represented in this document. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.A.4 | State-based or program-based risk corridor | Indicate if the COVID-19 risk corridor that the state is reporting on applies to all programs and plans in the state or is limited to one program and the plans under that program. If the state is reporting on a single risk corridor state-wide across all programs, choose "State". If the state is reporting on a risk corridor that applies to one program, choose “Program”. We do not expect risk corridors structures (i.e., the number of risk corridor bands or risk sharing percentages for plans and states) to vary for a particular risk corridor, although the state may set different risk corridor targets (for example, different Medical Loss Ratio (MLR) targets) for each plan. The state can enter specific targets for plans in the “II_Reconciliation” tab. |
Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.A.5 | Risk corridor title | If the risk corridor that the state is reporting on has a title, indicate the name of the risk corridor. | Free text | |||||||||||||||||||||||||||||||||||||||||
| I.A.6 | Program name(s) for a state-based risk corridor | If the state selected “State” in item I.A.4, indicate the program name(s) that the risk corridor applies to. | Free text | |||||||||||||||||||||||||||||||||||||||||
| I.A.7 | Program name for a program-based risk corridor | If the state selected “Program” in item I.A.4, indicate the program name that the risk corridor applies to. | Free text | |||||||||||||||||||||||||||||||||||||||||
| I.A.8 | Program start date | If the state selected “Program” in item I.A.4, indicate what year the state implemented the program. | Free text | |||||||||||||||||||||||||||||||||||||||||
| I.A.9 | Plan type | Indicate the managed care plan type (MCO, PIHP, or PAHP) that contracts with the state for the risk corridor that the state is reporting on. | Drop down list of set values or free text (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.A.10 | Rating period start date | Enter the rating period start date for the risk corridor reconciliation results that the state is reporting on in this document. | Date (MM/DD/YYYY) | |||||||||||||||||||||||||||||||||||||||||
| I.A.11 | Rating period end date | Enter the rating period end date for the risk corridor reconciliation results that the state is reporting on in this document. States are not expected to report risk corridor reconciliation results in this document for rating periods that end after December 31, 2021. | Date (MM/DD/YYYY) | |||||||||||||||||||||||||||||||||||||||||
| I.A.12 | Date of report submission | Enter the date on which the state is submitting this document to CMS. | Date (MM/DD/YYYY) | |||||||||||||||||||||||||||||||||||||||||
| B. Plan information | ||||||||||||||||||||||||||||||||||||||||||||
| States should use this section to report plan names for the program specified above in I.A.4. (All items in this section require input.) | Input plan-level data in beige cells in these columns >> | |||||||||||||||||||||||||||||||||||||||||||
| # | Item | Item Instructions | Data Format | Plan 1 | Plan 2 | Plan 3 | Plan 4 | Plan 5 | Plan 6 | Plan 7 | Plan 8 | Plan 9 | Plan 10 | Plan 11 | Plan 12 | Plan 13 | Plan 14 | Plan 15 | Plan 16 | Plan 17 | Plan 18 | Plan 19 | Plan 20 | Plan 21 | Plan 22 | Plan 23 | Plan 24 | Plan 25 | Plan 26 | Plan 27 | Plan 28 | Plan 29 | Plan 30 | Plan 31 | Plan 32 | Plan 33 | Plan 34 | Plan 35 | Plan 36 | Plan 37 | Plan 38 | Plan 39 | Plan 40 | |
| I.B.1 | Plan names | Enter the names of the plans that contract with the state for the risk corridor that the state is reporting on. Leave any remaining fields blank. This response will affect the layout of Tab 2 and Tab 3. |
Free text | |||||||||||||||||||||||||||||||||||||||||
| I.B.2 | Plan parent company | For each plan entered for item I.B.1, enter the plan's parent company name. Leave any remaining fields blank. If your plan parent company name is the same as the plan name, please enter it here. | Free text | |||||||||||||||||||||||||||||||||||||||||
| I.B.3 | Member months covered by the plan | For each plan entered for item I.B.1, indicate how many member months the plan covered for the rating period entered in I.A.12 and I.A.13. | Numeric | |||||||||||||||||||||||||||||||||||||||||
| C. Risk corridor targets and monthly/quarterly expenditure and revenue data | ||||||||||||||||||||||||||||||||||||||||||||
| States should enter information in this section to obtain instructions on which tabs to use in completing this template. After entering the information below, the template will return a list of tabs to complete based on the responses provided. (All items in this section require input.) | Input state/program-level data in this column | |||||||||||||||||||||||||||||||||||||||||||
| # | Item | Item Instructions | Data Format | Input state/program-level data in this column | ||||||||||||||||||||||||||||||||||||||||
| 1.C.1 | If the risk corridor is implemented at the state level, does the risk corridor target differ by plan? | Indicate whether the state-based risk corridor that the state is reporting on has risk corridor targets that vary by plan. For example, this could include unique MLR targets for each plan based on enrollment of beneficiaries from different rate cells. Enter N/A if the state is reporting on a program-based risk corridor per item I.A.4. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.C.2 | If the risk corridor is implemented at the program level, does the risk corridor target differ by plan? | Indicate whether the program-based risk corridor that the state is reporting on has risk corridor targets that vary by plan. For example, this could include unique MLR targets for each plan based on enrollment of beneficiaries from different rate cells. Enter N/A if the state is reporting on a state-based risk corridor per item I.A.4. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.C.3 | Does your state use monthly or quarterly expenditure and revenue data? | Indicate whether the state uses monthly or quarterly expenditure and revenue data for the risk corridor it is reporting on. This response will affect the layout of Tab 3. |
Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| D. Covered providers (Optional) | ||||||||||||||||||||||||||||||||||||||||||||
| If the risk corridor covers a specific program per item I.A.4, complete items I.D.1 - I.D.12. Indicate whether the program specified in I.A.8 covers each 42 C.F.R. § 438.68 provider type specified. The state can reference its model contract for the program for this information. These questions also appear in the Network Adequacy and Access Assurances Report (NAAAR) template that is available on Medicaid.gov. If the state is reporting on a state-based risk corridor per item I.A.4, enter N/A for these items. (This section is optional.) | Input state/program-level data in this column | |||||||||||||||||||||||||||||||||||||||||||
| # | Item | Item Instructions | Data Format | Input state/program-level data in this column | ||||||||||||||||||||||||||||||||||||||||
| I.D.1 | Adult primary care | Indicate whether the program covers adult primary care providers. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.D.2 | Pediatric primary care | Indicate whether the program covers pediatric primary care providers. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.D.3 | OB/GYN | Indicate whether the program covers Ob/Gyn providers. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.D.4 | Adult behavioral health | Indicate whether the program covers adult behavioral health providers. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.D.5 | Pediatric behavioral health | Indicate whether the program covers pediatric behavioral health providers. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.D.6 | Adult specialist | Indicate whether the program covers adult specialist providers. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.D.7 | Pediatric specialist | Indicate whether the program covers pediatric specialist providers. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.D.8 | Hospital | Indicate whether the program covers hospital providers. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.D.9 | Pharmacy | Indicate whether the program covers pharmacy providers. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.D.10 | Pediatric dental | Indicate whether the program covers pediatric dental providers. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.D.11 | LTSS | Indicate whether the program covers long-term services and supports (LTSS) providers. | Drop down list of set values (select one) | |||||||||||||||||||||||||||||||||||||||||
| I.D.12 | Other | Provide (1) any notes for items I.D.1 - 11 and/or (2) other provider types covered under the program not listed in items I.D.1 - 11, such as adult dental services. | Free text | |||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
| File Type | application/vnd.openxmlformats-officedocument.spreadsheetml.sheet |
| File Modified | 0000-00-00 |
| File Created | 0000-00-00 |
© 2026 OMB.report | Privacy Policy