Performance Measures Guidance [13NOV2024]
Appendix A_OE22-2203_Performance Measures Guidance (Revision).docx
[OADPS] The Performance Measures Project: Improving Performance Measurement and Monitoring by CDC Programs
Performance Measures Guidance [13NOV2024]
OMB: 0920-1282

 Component
A Recipient Performance Measures Guidance Document
Component
A Recipient Performance Measures Guidance Document
Form approved
OMB Control Number: 0920-1282
Expiration date: 06/30/26
OE22-2203: Strengthening U.S. Public Health Infrastructure, Workforce, and Data Systems Grant
Component A Recipient Performance Measure Guidance Document
Public reporting burden of this collection of information varies from 22 hours to 56 hours per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not required to respond to a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden to CDC/ATSDR Reports Clearance Officer; 1600 Clifton Road NE, MS D-74, Atlanta, Georgia 30333; Attn: OMB-PRA (0920-1282)
Introduction and Purpose of Guidance 3
Summary of Updates to Guidance for Reporting Period 4 8
Reporting Deadlines and Submission Guidance 10
Measure A1.2. Retention: Overall agency staff retention rate 17
Measure A2.1. Hiring Timeliness: Time-to-fill position 22
Measure A2.2. Procurement Timeliness: Procurement cycle time 26
Measure A3.1. Dedicated agency staff to lead and coordinate data modernization efforts 34
Measure A3.4. Demonstrated use of shared services to enhance existing systems or data exchange 39
Measure A3.5. Percent of lab report volume received through electronic laboratory reporting (ELR) 40
Measure A3.8. Systems/programs at the PHL with ETOR interfaces 44
Appendix A: Job Classification Categories and Program Areas 45
Appendix B: Measure A1.1: Hiring – Example Scenario 48
Appendix C: ELC HIS Reporting and PHIVE Acknowledgement Schedule 51
Introduction and Purpose of Guidance
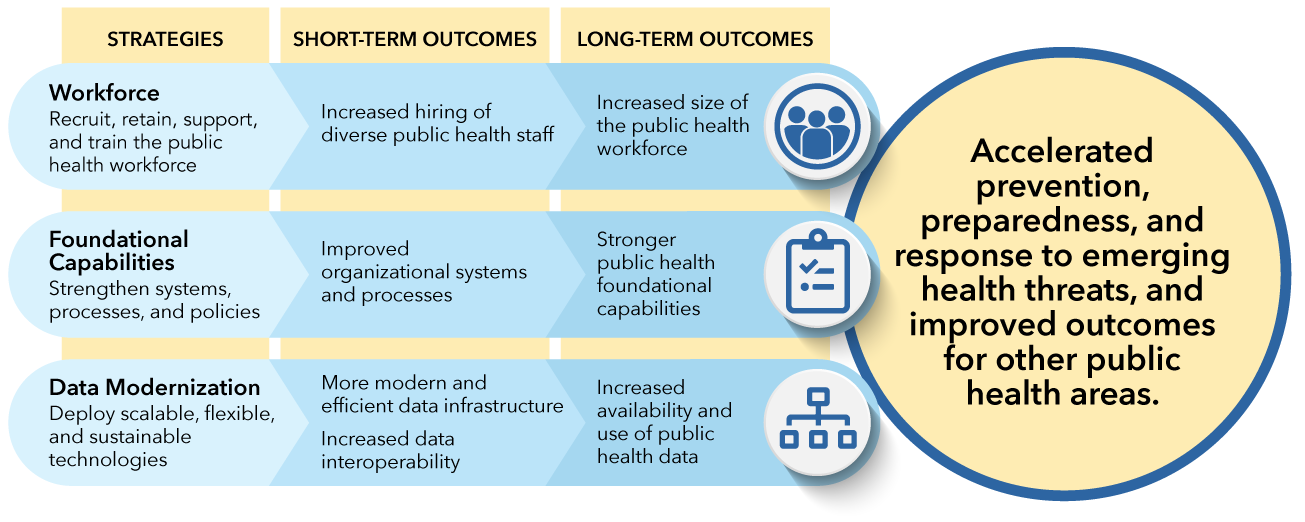
On November 29, 2022, the Centers for Disease Control and Prevention (CDC) awarded $3.2 billion to help state, local, and territorial and freely associated public health agencies across the U.S. strengthen their public health workforce and infrastructure through the Public Health Infrastructure Grant (PHIG). This grant provides 107 jurisdictions (Component A recipients) with disease-agnostic funding to support public health infrastructure needs. The three grant strategies are Strategy A1: Workforce; Strategy A2: Foundational Capabilities; and Strategy A3: Data Modernization. The priority short-term outcomes recipients are expected to achieve by the end of the five (5)-year period of performance include: (1) Increased hiring of diverse public health staff and (2) Improved organizational systems and processes, among other outcomes. In the long term, expected outcomes include: (1) Increased size and capabilities of the public health workforce; (2) Stronger public health foundational capabilities; (3) Increased availability and use of public health data; and (4) Improved sharing of lessons learned.
This document provides detailed information on the performance measures, data elements, and rationale for Component A recipient reporting on grant performance measures. This document should be reviewed before reporting and submitting these data to CDC primarily through the Public Health Infrastructure Virtual Engagement (PHIVE) Platform.
For the purposes of this document, Component A recipients are referred to as “recipient agencies.” Recipient agencies are defined as: the 107 public health departments in all 50 states, Washington D.C., 8 territories/freely associated states, and 48 large localities (cities serving a population of 400,000 or more and counties serving a population of 2,000,000 or more based on the 2020 U.S. Census) that were awarded funding through this grant.
Throughout this document, important updates to the Reporting Period 4 guidance are highlighted in yellow.
If you have any questions about the grant performance measures or need support calculating and reporting on these measures, please submit a programmatic technical assistance (TA) request through PHIVE.
Use of Measures
The grant performance measures are intended to be used by CDC, recipient agencies, and partners—including PHIG national partners (Component B recipients) and the National Evaluation Team—to:
Track and report progress consistently across recipient agencies on priority outcomes,
Inform CDC and PHIG national partners’ TA activities, such as site visits, training opportunities, and peer-to-peer sharing activities, to support recipients with advancing their work through this grant,
Inform CDC and partners on progress and gaps, to ultimately identify actions to improve performance over time, and
Stimulate discussions between Project Officers and recipients (e.g., What are opportunities for improvements? What are you doing well that you want to share with others?), which may inform current and future grant activity planning (e.g., Work Plan and budget development).
CDC recognizes the limitations of using performance measures to evaluate the scope of work being conducted by recipient agencies, especially considering the flexible nature of this grant, and contextual factors. CDC will leverage other methods of collecting information, via NOFO grant reporting requirements (e.g., work plan updates, annual progress reports, progress calls, and focused evaluation projects), to assess progress and performance robustly.
Measures Summary
There are thirteen (13) performance measures, eight (8) of which are shared measures with the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases Cooperative Agreement (ELC). These measures reflect priority outcomes for the grant. These measures were selected to serve as meaningful markers of program outcomes; to inform actions to drive improvements for achieving intended outcomes; to keep recipient reporting burden low; and to contribute to a meaningful set of measures overall for this grant.
There are two (2) measures for Strategy A1: Workforce, three (3) measures for Strategy A2: Foundational Capabilities, and eight (8) shared measures with ELC for Strategy A3: Data Modernization.
Recipients will monitor and report data to CDC through the PHIVE platform for five (5) measures (A1.1. Hiring; A1.2. Retention; A2.1. Hiring Timeliness; A2.2. Procurement Timeliness; and A2.3. Accreditation Involvement and Readiness).
The performance measures for Strategy A3: Data Modernization are aligned with select measures for ELC Project C.
PHIG has partnered with the ELC HIS program to collect the A3 Performance Measures. Within recipient jurisdictions, representatives from both programs should coordinate to submit data on these shared measures.
To reduce reporting burden, recipients will continue to submit data on these measures through the ELC Health Information Systems (HIS) REDCap forms only. Recipients will not report any data on A3 performance measures in PHIVE.
A3 recipient agencies will be required to complete two activities for A3 performance measure reporting: 1) In REDCap, an A3 representative from the jurisdiction should confirm their review of submitted measure data by checking the box under the “ELC & PHIG Coordination Acknowledgement” box. 2) In PHIVE, the same person should acknowledge their intended coordination with their agency’s ELC representatives to report on the A3 performance measures in REDCap. This person should be familiar with the jurisdiction’s A3 activities and objectives.
For expectations on timing of each coordination acknowledgement and performance measure review, see Appendix C.
Please note that A3 performance measures and reporting guidance will be updated to align with ELC NOFO CK24-0002 after August 2024.
CDC will monitor data via the Public Health Workforce Interests and Needs Survey (PH WINS) for two (2) measures (A1.3. Employee Engagement and Satisfaction and A1.4. Diversity of the Public Health Workforce). PH WINS is a periodic survey administered by the de Beaumont Foundation. Recipients will not report these data directly to CDC.
A table summarizing key differences among the A1 and A2 performance measures can be found in Appendix D.
Recipient participation in PH WINS, Public Health Accreditation Board (PHAB) Accreditation, and the Association of State and Territorial Health Officials (ASTHO) Profile or the National Association of County and City Health Officials (NACCHO) Profile Surveys is highly encouraged.
Strategy |
Topic |
Measure |
Reporting Frequency |
Reporting Location |
A1. Workforce |
A1.1. Number of PHI grant-funded positions filled by job classification and program area |
6 months |
PHIVE |
|
A1.2. Overall agency staff retention rate |
12 months |
PHIVE |
||
Employee Engagement and Satisfaction |
A1.3. Employee engagement and satisfaction |
Not Applicable; monitored via PH WINS data |
N/A |
|
Diversity1 of the Public Health Workforce |
A1.4. Diversity of the public health workforce |
Not Applicable; monitored via PH WINS data |
N/A |
|
A2. Foundational Capabilities |
A2.1. Time-to-fill position |
6 months |
PHIVE |
|
A2.2. Procurement cycle time |
6 months |
PHIVE |
||
A2.3. Level of involvement with PHAB accreditation |
12 months |
PHIVE |
||
A3. Data Modernization2 |
A3.1.3 Dedicated agency staff to lead and coordinate data modernization efforts |
3 months |
REDCap |
|
A3.2. Established workforce, data, and health information system capabilities, needs and opportunities |
3 months |
REDCap |
||
A3.3. Enhanced workforce capacities and capabilities to accelerate data and health information system modernization |
3 months |
REDCap |
||
A3.4. Demonstrated use of shared services to enhance existing systems or data exchange |
3 months |
REDCap |
||
A3.5. Percent of lab report volume received through electronic laboratory reporting (ELR) |
12 months |
REDCap |
||
A3.6. Number of hospitals and public health labs with established electronic test ordering and result (ETOR) reporting using HL7 messages or a web-portal |
12 months |
REDCap |
||
A3.7. Proportion of test orders and results processed through ETOR at the public health laboratory (PHL) |
3 months |
REDCap |
||
A3.8. Systems/programs at the PHL with ETOR interfaces |
3 months |
REDCap |
Summary of Updates to Guidance for Reporting Period 4
The Reporting Period 4 guidance includes some updates from Reporting Period 3. The Table below provides a high-level overview of the major changes.
Section |
Updates to Guidance |
Guidance clarifies that:
|
|
Guidance clarifies that:
|
|
Guidance clarifies that:
|
|
Guidance clarifies that:
|
Reporting Deadlines and Submission Guidance
The grant Period of Performance is 12/1/2022 – 12/1/2027. This grant follows a reporting period of six (6) months for three measures (A1.1. Hiring; A2.1. Hiring Timeliness; and A2.2. Procurement Timeliness) and a reporting period of twelve (12) months for two measures (A1.2. Retention and A2.3. Accreditation Involvement and Readiness).
Strategy A3 performance measure reporting should occur on the quarterly ELC HIS reporting schedule4 in REDCap. A3 recipients should coordinate with their agency’s ELC representatives to prepare for reporting of A3 performance measures, including data preparation, verification, and submission. Beginning in Reporting Period 2, acknowledgement of coordination between the two programs should occur in PHIVE every six (6) months on the dates below.
The PHIVE reporting portal will be open for performance data submission two months prior to the submission due date. Recipient agencies will submit all A1 and A2 performance measures data via PHIVE. All data submitted through PHIVE are due within 60 days of close of reporting period, on the dates indicated below. The REDCap reporting portal will open one month prior to the submission due date, which is 30 days following the close of the data collection period. See Appendix C for more detail on ELC HIS reporting timelines.
Year |
Reporting Period |
Dates |
Data Submission^ Due Date |
Year 1
|
1 |
12/1/2022 – 5/31/2023 |
8/1/2023* |
2 |
6/1/2023 – 11/30/2023 |
2/1/2024 |
|
Year 2
|
3 |
12/1/2023 – 5/31/2024 |
8/1/2024* |
4 |
6/1/2024 – 11/30/2024 |
2/1/2025 |
|
Year 3
|
5 |
12/1/2024 – 5/31/2025 |
8/1/2025* |
6 |
6/1/2025 – 11/30/2025 |
2/1/2026 |
|
Year 4
|
7 |
12/1/2025 – 5/31/2026 |
8/1/2026* |
8 |
6/1/2026 – 11/30/2026 |
2/1/2027 |
|
Year 5
|
9 |
12/1/2026 – 5/31/2027 |
8/1/2027* |
10 |
6/1/2027 – 11/30/2027 |
2/1/2028 |
^These dates represent the schedule for actions needed in PHIVE. Strategy A3 performance measure data should be submitted and reviewed on the ELC HIS reporting schedule in REDCap. However, acknowledgement of coordination between the two programs should occur in PHIVE on the dates in this table.
*Recipient agencies will report data every twelve (12) months, on dates indicated, for two (2) measures: A1.2. Retention and A2.3 Accreditation Involvement and Readiness.
Recipient agencies will report on the data elements defined in the Guidance section below. For each measure, except for the A3 measures, recipients will also respond to the following questions:
Are the data provided questionable or low/poor quality? (Yes/No)
Select “yes” if you feel that, for any reason, the data for the performance measure are of poor quality, incomplete, or of uncertain validity. Please tell us if you have serious doubts about whether this measure should be interpreted as accurate for your agency, for this reporting period. If you select “yes,” please explain.
Does the data provided adhere to the definitions established by CDC in the performance measures guidance? (Yes/No)
Describe any data limitations, including reasons unable to report, and steps taken to obtain data and/or improve data quality in the future. If you reported on these data using a definition that was different than provided in CDC’s guidance, please describe. (Open-ended, optional)
Does your PHIG workplan include any activities related to this performance measure? (Yes/No)
Provide any additional context or information related to this measure. (Open-ended, optional)
Within this guidance, text in blue underlined font are hyperlinks. To access the hyperlinked section of the document, press CTRL and click + on the text. Bold italic font is used to emphasize select key terms.
Guidance
Measure A1.1. Hiring: Number of PHIG-funded positions filled by job classification and program area
Topic |
Hiring |
Measure |
Number of PHIG-funded positions filled by job classification and program area |
Definition |
Number of PHIG-funded positions filled by job classification and program area at the end of each reporting period, including positions filled since December 2022 with current employees and new hires |
Purpose |
A sufficient public health workforce within governmental public health agencies is needed to accelerate prevention, preparedness, and response to emerging health threats and improve public health outcomes. Increased hiring and retention of diverse public health staff is an intended outcome of this grant. Types of hiring activities recipients may implement include, among others, expanding recruitment efforts, creating new positions, improving hiring incentives, and creating new hiring mechanisms (with Component B partners’ assistance).
The intent of this measure is to understand the number of positions supported by funds from this grant within health departments across all three strategies (A1, A2, and A3). This includes positions supported within health departments that have received direct funding, and it also includes positions supported within local health departments (LHDs) that did not receive direct funding from this grant (i.e., LHDs that were distributed funds from this grant from state health department recipients). However, this excludes positions that received incentives or bonuses paid for with PHIG funding. Recipients will report on the number of positions filled by job classification and program area, so CDC can better understand the gaps these positions are supporting (e.g., program-specific vs. cross-cutting).
|
Terms and Definitions |
Position filled: The terms of employment have been agreed upon and no one else can occupy that position.
Total positions filled by job classification and program area: Total number of positions under this grant filled since the beginning of the grant.
Positions filled with current employees by job classification and program area: Number of positions under this grant filled with staff already employed (including full-time, part-time, contractual, and seasonal) at the agency. This should include any internal transfers supported through this grant. Positions filled with new hires by job classification and program area: Number of positions under this grant filled with new hires.
Year 5 target: This is the target value that recipients aim to achieve for this measure by the end of the project period (11/30/2027). |
Additional Guidance |
Guidance on calculating positions filled:
|
Data Elements to be Reported |
Recipients will enter the following information:
*Recipients previously reported the Year 5 target to CDC. These targets will be pre-populated in PHIVE and used to calculate the percent of positions filled based on intended hiring targets for Year 5. |
Example Scenario |
At of the end of the reporting period, the recipient has filled 6 positions with PHI grant funds; 3 of these positions were filled with new hires and 3 were filled with current employees. The new hires are a Chronic Disease Program Manager, Contracts Specialist, and Community Health Worker (Communicable Disease). The current employees are an Environmental Epidemiologist, Health Equity Communications Specialist, and Health Educator (working on COVID-19 and Influenza 60% and Maternal and Child Heath 40%). The recipient is a state health department, and LHDs funded through the grant have not yet filled any positions, as of this reporting period.
The recipient would report (see Appendix B: Measure A1.1: Hiring – Example Scenario for sample data):
|
Unit of Measurement |
Number of positions |
Reporting Frequency |
6 months |
Considerations |
|
Measure A1.2. Retention: Overall agency staff retention rate
Topic |
Retention |
Measure |
Overall agency staff retention rate |
Definition |
Retention rate, including permanent and temporary/contract staff
|
Purpose |
A sufficient public health workforce within governmental public health agencies is needed to accelerate prevention, preparedness, and response to emerging health threats and improve public health outcomes. Data suggests that strategies to increase retention of the public health workforce must be prioritized, given current trends in actual separations of workforce from the state, local, territorial, and freely associated state governmental public health agencies. Public health agencies have reported challenges with retaining skilled workers, particularly among different sub-groups, such as younger staff.5,6 Increased hiring and retention of diverse public health staff is an intended outcome of this grant. Types of retention activities recipients may implement include, among others, strengthening retention incentives, rewarding creativity and innovation, creating promotional opportunities, improving employee satisfaction and engagement, and transitioning staff from one program NOFO to another one.
The intent of this measure is to assess the stability of the public health workforce within recipient agencies. Following this intent, recipients should include only staff employed within the recipient agency; (if applicable) exclude staff from a larger governmental unit or “super agency.” For example, if you operate within a broader Department of Health and Human Services, only include the Division of Public Health in your calculations. This information will help monitor recipients’ abilities to maintain, make progress, and/or overcome challenges in retaining their public health workforce and maintaining a functional workforce system.
|
Terms and Definitions |
Permanent staff: Permanent staff are part-time and full-time governmental employees. Permanent staff are regular employees, typically eligible for benefits, and do not have a defined duration of employment.
Temporary/contract staff: Temporary/contract staff have a defined duration of employment. Temporary/contract staff are not typically eligible for benefits through the government agency. Includes limited-term employees (LTEs).
A1: Number of staff, including permanent and temporary/contract staff, on last day of reporting period: Count of total number of staff at the recipient agency, including permanent and temporary/contract staff, on the last day of the reporting period (e.g., May 31, 2024).
A2: Number of permanent staff on last day of reporting period: Count of permanent staff at the recipient agency on the last day of the reporting period (e.g., May 31, 2024).
B1: Number of new hires, including permanent and temporary/contract staff, during reporting period: Count of staff newly hired within the recipient agency, including permanent and temporary/contract staff, during the reporting period (e.g., June 1, 2023, to May 31, 2024).
B2: Number of new hires (permanent staff only) during reporting period: Count of permanent staff newly hired within the recipient agency during the reporting period (e.g., June 1, 2023, to May 31, 2024).
C1: Number of staff, including permanent and temporary/contract staff, on Day 1 of reporting period: Count of staff employed at the recipient agency, including permanent and temporary/contract staff, on Day 1 of the reporting period (e.g., June 1, 2023).
C2: Number of permanent staff on Day 1 of reporting period: Count of permanent staff employed at the recipient agency on Day 1 of the reporting period (e.g., June 1, 2023). Recipient agency: The state, local, territorial, or freely associated state health department or agency awarded funding through this grant. If the health department operates within a larger governmental unit or is part of a “super public health agency” or “umbrella agency,” include only the division or department awarded funding.
Year 5 target: This is the target value that recipients aim to achieve for this measure by the end of the project period (11/30/2027). |
Additional Guidance |
Guidance on types of staff to include:
|
Data Elements to be Reported |
Recipients will enter the following information: A1. Number of staff, including permanent and temporary/contract staff, on last day of reporting period (Number) A2. Number of permanent staff on last day of reporting period (Number) B1. Number of new hires, including permanent and temporary/contract staff, during reporting period (Number) B2. Number of new hires (permanent staff only) during reporting period (Number) C1. Number of staff, including permanent and temporary/contract staff, on Day 1 of reporting period (Number) C2. Number of permanent staff on Day 1 of reporting period (Number) Year 5 target: This value should include target retention rates for both 1) permanent staff only and 2) permanent and temporary/contract staff.
Recipients will enter data for A1, A2, B1, B2, C1, and C2 in PHIVE. The system will calculate two retention rates: one for staff including temporary staff and contractors (A1-B1)/C1) and one for permanent staff only (A2-B2)/C2. |
Example Scenario |
Retention rate for staff, including permanent and temporary/contract staff. The reporting period is from June 1, 2023 to May 31, 2024. The recipient agency employs 100 staff (including staff in temporary/contract positions) on May 31, 2024 (A1). Between June 1, 2023 and May 31, 2024, 10 of those staff were hired, including temporary/contract staff (B1). There were 120 staff (including temporary/contract staff) employed by the agency on June 1 (C1). The retention rate is (A1-B1)/C1*100, or in this example, (100-10)/120: 0.75*100 = 75%. Note: Recipient will not need to calculate the rate. Rates will be calculated automatically in PHIVE.
Retention rate for permanent staff. The reporting period is from June 1, 2023 to May 31, 2024. The recipient agency employs 80 permanent staff on May 31, 2023 (A2). Between June 1, 2023 and May 31, 2024, 5 of those staff were hired (B2). There were 90 permanent staff employed by the agency on June 1 (C2). The retention rate is (A2-B2)/C2*100, or in this example, (80-5)/90: 0.75*100 = 83.3%. Note: Recipient will not need to calculate the rate. Rates will be calculated automatically in PHIVE. |
Unit of Measurement |
Number of staff (rates will be calculated automatically in PHIVE) |
Reporting Frequency |
12 months |
Considerations |
|
Measure A2.1. Hiring Timeliness: Time-to-fill position
Topic |
Hiring Timeliness |
Measure |
Time-to-fill position |
Definition |
Median number of calendar days from the date the job description was posted for hiring to date of first day of work (for all employees that started at the recipient agency during the reporting period). |
Purpose |
Improved organizational systems and processes, through strengthened workforce systems, processes, and/or policy improvements, is an intended outcome of this grant. Specifically, improving the timeliness for filling a position can improve public health agencies’ ability to attract and retain higher quality candidates, improve productivity, and reduce costs. Recipients may be working to improve human resources (HR) processes by upgrading their HR systems (hardware and software); developing policies or tools to improve the management of human resources; and working on improving recruitment and retention strategies, among others.
The intent of this measure is to monitor and understand the ability of recipients to maintain, make progress, and/or overcome challenges in filling job positions in a timely manner.
|
Terms and Definitions |
Job description posted: Date job opening is posted.
First day of work: Date of first day of work for employee.
Median: The middle value in a set of data.
Year 5 target: This is the target value that recipients aim to achieve for this measure by the end of the project period (11/30/2027). |
Additional Guidance |
Guidance on types of job positions to include:
Guidance on job offers to include:
Guidance on calculating the median and minimum number of calendar days:
|
Data Elements to be Reported |
Recipients will enter the following information:
|
Example Scenario |
The agency hired 9 new employees this reporting period. The number of calendar days from the date the job description was posted to the start date for each employee was: 15, 30, 33, 40, 41, 45, 60, 65, 80 days. The time to fill position is 41 days. The recipient will report:
|
Unit of Measurement |
Number of days |
Reporting Frequency |
6 months |
Considerations |
|
Measure A2.2. Procurement Timeliness: Procurement cycle time
Topic |
Procurement Timeliness |
Measure |
Procurement cycle time |
Definition |
Median number of calendar days from date the required documentation/information is received by the unit within the health department responsible for procurement review and approval and the date contract is fully executed (i.e., all parties have signed the contract). |
Purpose |
Improved organizational systems and processes by addressing human resources, financial management, contract, and procurement services is an intended outcome of this grant. This measure focuses on the ability of health departments to have ready and timely access to available resources by examining the timeliness of their procurement process.8 Many recipients are implementing improvements to their procurement services including, but not limited to, streamlining their procurement process; developing and/or updating their practices and policies; conducting trainings; hiring more procurement and financial staff; and upgrading their procurement systems.
Procurement is a vital business function encompassing a range of activities for an organization to obtain goods, services, and works. The purpose of procurement is to obtain competitive prices while delivering the most value. Government procurement, or public procurement, is the formal process by which the government acquires the goods and services it needs by purchasing from businesses.
Procurement of equipment, supplies, and services refers to the policies, procedures, and actions taken by the health department to obtain the necessary equipment, supplies, and services that may be needed to carry out both its regular agency functions and those functions that may be needed during times of emergencies, disasters, or outbreaks. This includes contracting for professional public health services. Timeliness in the approval and execution of procurement actions is a key element of administration.
The intent of this measure is to understand the extent to which recipients have improved their overall procurement process by assessing the timeliness of an agency’s procurement cycle time. Monitoring procurement cycle time can help indicate where there might be improvements or opportunities in the public health system’s ability to spend money more efficiently. It is also an opportunity to show the need for continued funding and investments in public health infrastructure.
We learned through our pilot project that many recipients are not currently tracking data related to procurement timeliness. This grant provides an opportunity for jurisdictions to take their first steps toward developing or improving their systematic data collection and reporting processes. We encourage recipients to collaborate across programmatic and administrative areas to improve systems and capacity to capture data. We do not expect perfection, and we encourage grantees to describe their processes—successes and challenges—using the open-ended fields during data submission. |
Terms and Definitions |
Procurement start date: Date the required documentation/information is received by the unit within the health department responsible for procurement review and approval.
Contract execution: The end date for the measure is the date all relevant parties sign the contract, and the contract is finalized.
Median: The middle value in a set of data.
Year 5 target: This is the target value that recipients aim to achieve for this measure by the end of the project period (11/30/2027). |
Additional Guidance |
Guidance on procurements to include:
Guidance on procurements to exclude:
Guidance on including purchase orders:
Guidance on calculating the median number of calendar days:
**A sampling option will be available for this measure beginning in Reporting Period 3. If you are interested in implementing the sampling methodology, submit a TA request in PHIVE for more information.** |
Data Elements to be Reported |
Recipients will share the following information*:
If using the sampling method, report the number of procurements included in your sample.
*An Excel template is included as an optional tool to help sites track and calculate Procurement Timeliness. This is not required, and recipients who use it do not need to submit a copy to CDC. Please submit a PHIVE TA Request to obtain this template. |
Example Scenario |
The agency executed 4 contracts during this reporting period. The number of calendar days from the date of approval to move forward with procurement to the date of execution of the contract was: 88, 129, 150, and 230 days. The procurement cycle time is 139.5 days. Recipient will report:
|
Unit of Measurement |
Number of days |
Reporting Frequency |
6 months |
Considerations |
The scope is limited to federal awards to help minimize burden on recipient reporting, to maximize understanding of barriers and challenges that impact spend down of federal funds, and to help advocate for additional investments to support federal grantees. Additionally, CDC understands there may be bottlenecks during various phases of approval to move forward with procurement and contract execution that are outside of the recipient agency’s purview. CDC is interested in understanding the time between approval to move forward with procurement and execution, including those bottlenecks. CDC understands some of these bottlenecks may be due to the time other entities, outside of the recipient agency (i.e., other offices, bureaus, departments, etc.), spend on activities, such as review and approval. Recipients will have the opportunity to provide additional contextual information. |
Measure A2.3. Accreditation Involvement and Readiness: Level of involvement with Public Health Accreditation Board (PHAB) accreditation
Topic |
Accreditation Involvement and Readiness |
Measure |
Level of involvement with PHAB Accreditation |
Definition |
Accreditation status and involvement in the Public Health Accreditation Board (PHAB) accreditation program. |
Purpose |
Improved health department quality, accountability, and performance based on standards and measures is an intended outcome of this grant. By formally engaging in PHAB accreditation, health departments are assessed against Standards and Measures aligned with the Essential Public Health Services (EPHS) and the Foundational Public Health Services’ (FPHS) eight foundational capabilities for a strong public health infrastructure. One way to measure progress towards implementation of foundational capabilities and delivery of EPHS is to assess the accreditation status of recipient agencies and level of involvement in the PHAB accreditation program.
The intent of this measure is to track recipients’ current involvement in the PHAB accreditation program. CDC will use this information to help understand how recipients are strengthening their foundational capabilities toward a stronger public health infrastructure. CDC will also use this information to monitor changes in accreditation status and involvement in the PHAB accreditation program over the project period of the grant.
|
Terms and Definitions |
Public Health Accreditation Board (PHAB): The independent accrediting body for state, local, and territorial and freely associated health agencies.
Accreditation status: The accreditation status of the recipient agency in the PHAB accreditation program.
Year 5 target: This is the target value that recipients aim to achieve for this measure by the end of the project period (11/30/2027). |
Data Elements to be Reported |
Recipient agencies will answer the following question. Please select the statement that best reflects your agency’s involvement with the Public Health Accreditation Board (PHAB) national accreditation program (select one)
Year 5 target: This value should include the statement that best reflects your agency’s target involvement with the Public Health Accreditation Board (PHAB) national accreditation program (select one).
Additional Guidance:
|
Unit of Measurement |
N/A |
Reporting Frequency |
12 months |
Considerations |
|
Measure A3.1. Dedicated agency staff to lead and coordinate data modernization efforts
Topic |
Data Modernization Leadership |
Measure |
Dedicated agency staff to lead and coordinate data modernization efforts |
Definition |
Presence of Agency Data Modernization Director (i.e., hired, onboarded). |
Purpose |
This measure will help to assess the ways in which recipients are building workforce capacity within the public health agency to support data modernization. Specifically, this measure will indicate the presence of dedicated agency staff to lead and coordinate data modernization efforts. Centralized leadership and cross-agency coordination are components of a strong foundation for data modernization activity planning and implementation. |
Data Elements to be Reported |
|
Unit of Measurement |
Position of DMI Director |
Reporting Frequency |
Quarterly via ELC HIS REDCap. A3.1 is the same as ELC Measure C2.1. |
Considerations |
|
Measure A3.2. Established workforce, data, and health information system capabilities, needs and opportunities
Topic |
Data Modernization Assessment and Planning |
Measure |
Established workforce, data, and health information system capabilities, needs and opportunities |
Definition |
Agency’s completion or update of 1) data modernization assessment, 2) data modernization plan, and 3) data modernization workforce development plan. |
Purpose |
This measure will indicate the extent to which a recipient has undertaken assessment and reporting of the agency’s current capacity, gaps, and opportunities to modernize the public health data infrastructure and workforce. Assessment and planning are critical for prioritizing data modernization activities. |
Terms and Definitions |
Completed: A data modernization is considered “completed” if it has been developed, reviewed, or updated by the agency in the past two years. If an assessment was completed prior to this time and has not been updated or reviewed, please select “No” for Question 1 and answer the follow-up question. |
Data Elements to be Reported |
|
Unit of Measurement |
Completion or update of 1) data modernization assessment, 2) data modernization plan, and 3) data modernization workforce development plan |
Reporting Frequency |
Quarterly via ELC HIS REDCap. A3.2 is the same as ELC Measure C2.2. |
Considerations |
|
Measure A3.3. Enhanced workforce capacities and capabilities to accelerate data and health information system modernization
Topic |
Data Modernization Workforce Capabilities |
Measure |
Enhanced workforce capacities and capabilities to accelerate data and health information system modernization |
Definition |
Details of trainings attended by agency staff or hosted by the agency to address data modernization workforce capabilities.
Data modernization competencies addressed by non-training workforce activities. |
Purpose |
This measure will help to assess the ways in which recipients are building workforce capacity within the public health agency to support data modernization. Specifically, this measure will indicate the non-recruitment workforce activities undertaken to build the competencies and skills of agency staff in data modernization. |
Data Elements to be Reported |
|
Unit of Measurement |
Trainings attended or hosted; competencies addressed |
Reporting Frequency |
Quarterly via ELC HIS REDCap. A3.3 is the same as ELC Measure C2.3. |
Considerations |
This measure applies to all A3 recipients. Data collection and submission should be coordinated with ELC representatives. |
Measure A3.4. Demonstrated use of shared services to enhance existing systems or data exchange
Topic |
Use of Shared Services |
Measure |
Demonstrated use of shared services to enhance existing systems or data exchange |
Definition |
The shared services utilized by the recipient agency for data exchange or information system functionality. |
Purpose |
Leveraging shared services can optimize efficiency and accelerate data modernization. This measure will assess the extent to which recipients have enhanced their capabilities and capacity for data science and health information systems using shared services. |
Data Elements to be Reported |
|
Unit of Measurement |
Shared services utilized for data exchange or information system functionality |
Reporting Frequency |
Quarterly via ELC HIS REDCap. A3.4 is the same as ELC Measure C2.4. |
Considerations |
This measure applies to all A3 recipients. Data collection and submission should be coordinated with ELC representatives. |
Measure A3.5. Percent of lab report volume received through electronic laboratory reporting (ELR)
Topic |
Electronic Laboratory Reporting (ELR) Volume |
Measure |
Percent of lab report volume received through ELR |
Definition |
Of all lab reports received, the percent received through ELR. |
Purpose |
This measure will help the program understand the extent to which the states are making progress with increasing ELR volume in their jurisdictions. Monitoring their progress closely will help the program identify challenges and barriers with program implementation and/or the functionality of the system. The program will provide technical assistance and programmatic interventions based on the information gathered from this measure. |
Data Elements to be Reported |
|
Unit of Measurement |
Number of received lab reports |
Reporting Frequency |
Annually via ELC HIS REDCap. A3.5 is the same as ELC Measure C1.1. |
Considerations |
|
Measure A3.6. Number of hospitals and public health labs with established electronic test ordering and result (ETOR) reporting using HL7 messages or a web-portal
Topic |
Electronic Test Order and Result (ETOR) Capacity |
Measure |
Number of hospitals and public health labs with established electronic test ordering and result (ETOR) reporting using HL7 messages or a web-portal |
Definition |
Number of hospitals with established ETOR using HL7 or a web-portal. Number of public health labs with established ETOR using HL7 or a web portal. |
Purpose |
The capacity for requesting, sending, and receiving electronic test orders and results (ETOR) enables public health laboratories (PHLs) to do their work more efficiently as data is reported faster. This measure will help the program understand the extent to which the jurisdictions have the capacity to request, send, or receive ETOR feeds for various conditions and pathogens using HL7 messages or a web-interface. This information will inform programmatic strategies and technical assistance efforts as the program works to improve PHL’s capacity for data exchange. |
Data Elements to be Reported |
|
Unit of Measurement |
Number of hospitals; number of public health labs |
Reporting Frequency |
Annually via ELC HIS REDCap. A3.6 is the same as ELC Measure C1.2. |
Considerations |
|
Measure A3.7. Proportion of test orders and results processed through ETOR at the public health laboratory (PHL)
Topic |
ETOR Volume |
Measure |
Proportion of test orders and results processed through Electronic Test Orders and Result Reporting (ETOR) at the PHL |
Definition |
Of all test orders received by the PHL, the proportion received through ETOR. Of all test results sent by the PHL, proportion sent through ETOR. |
Purpose |
The percentage of test orders received and results sent through ETOR may provide an understanding of the ETOR capabilities of the laboratory. Volume growth over time is a metric of increased adoption of ETOR. Because ETOR for orders and results may occur independently, collecting the measures separately is needed. |
Terms and Definitions |
|
Data Elements to be Reported |
|
Unit of Measurement |
Test orders received; test results sent |
Reporting Frequency |
Quarterly via ELC HIS REDCap. A3.7 is the same as ELC Measure E.15. |
Considerations |
|
Measure A3.8. Systems/programs at the PHL with ETOR interfaces
Topic |
ETOR Implementation |
Measure |
Systems/programs at the PHL with ETOR interfaces |
Definition |
The public health laboratory’s systems and/or programs actively using ETOR with any healthcare provider. |
Purpose |
The number of different laboratory programs/systems connected electronically with healthcare providers indicates the amount of process automation within the laboratory and the complexity of the ETOR systems within the laboratory. |
Terms and Definitions |
|
Data Elements to be Reported |
|
Unit of Measurement |
Public health laboratory systems and/or programs |
Reporting Frequency |
Quarterly via ELC HIS REDCap. A3.8 is the same as ELC Measure E.16. |
Considerations |
|
Appendix A: Job Classification Categories and Program Areas
The information provided below is relevant to Measure A1.1: Hiring (Number of PHIG-funded positions filled by job classification and program area). Job classification and program area categories are derived from categories from the Foundational Public Health Services, and the NACCHO Profile and PH WINS survey instruments.
Job Classification Categories:
Agency leadership and management: Department/Bureau Director, Deputy Director, Public Health Agency Director, Program Director, Health Officer.
Program manager: Public Health Program Manager.
Business, improvement, and financial operations staff: Attorney or Legal Counsel, Business Support – Accountant/Fiscal, Business Support Services – Administrator, Business Support Services – Coordinator, Grants or Contracts Specialist, Human Resources Personnel, Other Business Support Services, Community Health Planner, Quality Improvement Worker, Training Developer/Manager, Workforce Development Staff. May include positions focused on accreditation and performance improvement.
Office and administrative support staff: Clerical Personnel -Administrative Assistant, Clerical Personnel -Secretary, Customer Service/Support Professional, Custodian, Other Facilities or Operations Worker, Implementation Specialist, Medical/Vital Records Staff.
Information technology and data system staff: Information Systems Manager/Information Technology Specialist, IT Support Staff, Public Health Informatics Specialist, Informatics staff, Web Developer/Computer Programmer.
Public information, communications, and policy staff: Public Information Specialist, Policy Analyst, Communications specialist, Web Content Writer/Content Developer.
Laboratory workers: Laboratory Technician, Laboratory Quality Control Worker, Laboratory Scientist/Medical Technologist, Laboratory Aide or Assistant.
Epidemiologists, statisticians, data scientists, other data analysts: Epidemiologist, Population Health Specialist, Statistician, Economist, Data or Research Analyst, Data Scientist, Program Evaluator.
Behavioral health and social services staff: Behavioral Health Professional, Disease Intervention Specialist/Contact Tracer, Peer Counselor, Health Navigator, Social Worker/Social Services Professional.
Community health workers and health educators: Health Educator, Community Health Worker.
Public health physician, nurse and other clinicians or healthcare providers: Nursing and Home Health Aide, Nutritionist or Dietitian, Other Oral Health Professional, Other Nurse -Clinical Services, Physician Assistant, Public Health Dentist, Public Health/Preventive Medicine Physician, Registered Nurse -Public Health or Community Health Nurse, Registered Nurse -Unspecified, Pharmacist, Licensed practical or vocational nurse, Nurse Practitioner Emergency Medical Technician/Advanced Emergency Medical, Technician/Paramedic, Emergency Medical Services Worker, Other Health Professional/Clinical Support Staff, Physical/Occupational/Rehabilitation Therapist, Public Health Veterinarian.
Preparedness staff: Emergency Preparedness/Management Worker.
Environmental health workers: Environmental Health Worker, Environmental Health Technician, Environmental Health Physicist, Environmental Health Scientist, Environmental Engineer.
Animal control and compliance/inspection staff: Licensure/Regulation/Enforcement Worker, Sanitarian or Inspector, Animal Control Worker, Disability claims/benefits examiner or adjudicator, Medical Examiner.
Other: Student, Professional or Scientific, Interns, Fellows, Other (not categorized)
If positions have crossover categories or operate within several of the job classification categories, select the category that this position will work on most (>50%) of the time. Do not double-count staff if they are working in more than one category.
Job Program Areas (Aligned with the Foundational Public Health Services)
Access to and Linkage with Clinical Care: Clinical Services (excluding TB, STD, family planning), Emergency Medical Services, Immunizations - clinical, Immunizations - non-clinical, Mental Health, Oral Health/Clinical Dental Services, School Health, Substance Abuse, including tobacco control programs
Accountability and Performance Management: Accreditation coordinators, QI staff, performance management leads
Assessment and Surveillance: Community Health Assessment/Planning, Disability services, including disability determinations, Enforcement/Inspection/Licensing/Certification of Facilities, Epidemiology Surveillance, Informatics, Medical Examiner, Public Health Genetics, Public Health Laboratory, Vital Records
Chronic Disease and Injury Prevention: Non-Communicable Disease/Chronic Disease, Health Promotion/Wellness, Injury/Violence Prevention
Communicable Disease Control: COVID-19 Response, Communicable Disease - HIV, Communicable Disease - Influenza, Communicable Disease - STD, Communicable Disease - Tuberculosis, Communicable Disease - Viral Hepatitis, Other Communicable Disease
Communications
Community Partnership Development: Community Health Assessment/Planning
Emergency Preparedness and Response: All Hazards
Environmental Public Health: Environmental Health, Animal Control
Equity
Maternal, Child and Family Health: Children and Youth with Special Health Care Needs, Maternal and Child Health - Family Planning, Maternal and Child Health - WIC
Organizational Competencies: Leadership & Governance; Information Technology Services; Workforce Development & Human Resources; Financial Management, Contract, & Procurement Services, including Facilities and Operations; Legal Services & Analysis
Policy Development and Support
If positions have crossover categories or operate within several of the program areas, select the category that this position will work on most (>50%) of the time. Do not double-count staff if they are working in more than one category.
Appendix B: Measure A1.1: Hiring – Example Scenario
At of the end of this reporting period, the recipient has filled 6 positions with PHIG funds; 3 of these positions were filled with new hires and 3 were filled with current employees. The new hires are a Chronic Disease Program Manager, Contracts Specialist, and Community Health Worker (Communicable Disease). The current employees are an Environmental Epidemiologist, Health Equity Communications Specialist, and Health Educator (working on COVID-19 and Influenza 60% and Maternal and Child Heath 40%). The recipient is a state health department, but LHDs funded through the grant have not yet filled any positions, as of this reporting period.
The tables below provide examples of the data a recipient would report for this measure. These tables are not how data will be entered in PHIVE but could serve as an approach for tracking this information by recipients.
Job Classification Categories – Example Scenario
|
1. Total number of PHIG-funded positions filled (as of 5/31/2024) |
2. Number of positions filled with current employees |
3. Number of positions filled with new hires |
|||
|
Recipient agency |
LHDs funded by state recipient |
Recipient agency |
LHDs funded by state recipient |
Recipient agency |
|
1. Agency leadership and management |
0 |
0 |
0 |
0 |
0 |
0 |
2. Program manager |
1 |
0 |
0 |
0 |
1 |
0 |
3. Business, improvement, and financial operations staff |
1 |
0 |
0 |
0 |
1 |
0 |
4. Office and administrative support staff |
0 |
0 |
0 |
0 |
0 |
0 |
5. Information technology and data system staff |
0 |
0 |
0 |
0 |
0 |
0 |
6. Public information and public policy staff |
1 |
0 |
1 |
0 |
0 |
0 |
7. Laboratory workers |
0 |
0 |
0 |
0 |
0 |
0 |
8. Epidemiologists, statisticians, data scientists, and other data analysts |
0 |
0 |
0 |
0 |
0 |
0 |
9. Behavioral health and social services staff |
0 |
0 |
0 |
0 |
0 |
0 |
10. Community health workers and health educators |
2 |
0 |
1 |
0 |
1 |
0 |
11. Public health physician, nurse, and other health care providers |
0 |
0 |
0 |
0 |
0 |
0 |
12. Preparedness staff |
0 |
0 |
0 |
0 |
0 |
0 |
13. Environmental health workers |
1 |
0 |
1 |
0 |
0 |
0 |
14. Animal control and compliance/inspection staff |
0 |
0 |
0 |
0 |
0 |
0 |
15. Other |
0 |
0 |
0 |
0 |
0 |
0 |
Total |
6 |
0 |
3 |
0 |
3 |
0 |
Job Program Areas
|
1. Total number of PHIG-funded positions filled (as of 5/31/2024) |
2. Number of positions filled with current employees |
3. Number of positions filled with new hires |
|||
|
Recipient agency |
LHDs funded by state recipient |
Recipient agency |
LHDs funded by state recipient |
Recipient agency |
LHDs funded by state recipient |
1. Access to and Linkage with Clinical Care |
0 |
0 |
0 |
0 |
0 |
0 |
2. Emergency Preparedness and Response |
0 |
0 |
0 |
0 |
0 |
0 |
3. Accountability and Performance Management |
0 |
0 |
0 |
0 |
0 |
0 |
4. Assessment and Surveillance |
0 |
0 |
0 |
0 |
0 |
0 |
5. Chronic Disease and Injury Prevention |
1 |
0 |
0 |
0 |
1 |
0 |
6. Communicable Disease Control |
2 |
0 |
1 |
0 |
1 |
0 |
7. Communications |
1 |
0 |
1 |
0 |
0 |
0 |
8. Community Partnership Development |
0 |
0 |
0 |
0 |
0 |
0 |
9. Environmental Public Health |
1 |
0 |
1 |
0 |
0 |
0 |
10. Equity |
0 |
0 |
0 |
0 |
0 |
0 |
11. Maternal, Child, and Family Health |
0 |
0 |
0 |
0 |
0 |
0 |
12. Organizational Competencies |
1 |
0 |
0 |
0 |
1 |
0 |
13. Policy Development and Support |
0 |
0 |
0 |
0 |
0 |
0 |
14. Other |
0 |
0 |
0 |
0 |
0 |
0 |
Total |
6 |
0 |
3 |
0 |
3 |
0 |
Appendix C: ELC HIS Reporting and PHIVE Acknowledgement Schedule
The performance measures for Strategy A3: Data Modernization are aligned with select measures for the Epidemiology and Laboratory Capacity (ELC) Project C.
To reduce reporting burden, recipients will continue to submit data on these measures through the ELC Health Information Systems (HIS) REDCap forms on the quarterly ELC HIS reporting schedule in REDCap. All measure data should be reported in the REDCap project titled “ELC Health Information Systems Monitoring 2023-2024 (C1, C2).”
A3 recipient agencies will be required to 1) confirm their review of submitted measures in REDCap and 2) acknowledge their coordination with their agency’s ELC representatives to report on the A3 performance measures in REDCap. Beginning in Reporting Period 2, this acknowledgement should be completed in PHIVE every six (6) months along with the submission of performance measure data for Strategies A1 and A2.
Please note that A3 performance measures and reporting guidance will be updated to align with ELC NOFO CK24-0002 after August 2024.
The table below details the ELC HIS reporting schedule and the corresponding dates for acknowledgement of coordination in PHIVE for Reporting Periods 2 and 3.
PHIVE Acknowledgement |
ELC HIS Performance Measure Submission Deadline (REDCap) |
February 1, 2024 |
November 30, 2023 (Dates of work covered: August 1, 2023 - October 31, 2023) |
February 28, 2024 (Dates of work covered: November 1, 2023 - January 31, 2024) |
|
August 1, 2024 |
May 31, 2024 (Dates of work covered: February 1, 2024 - April 30, 2024) |
August 31, 2024 (Dates of work covered: May 1, 2024 - July 31, 2024) |
Appendix D: A1/A2 Performance Measures Summary Table
Measure |
Time Frame |
PHIG only or agency-wide? |
Type of Staff and/or Data Included and Excluded (if applicable) |
A1.1 Number of PHIG-funded positions filled by current (i.e., internal to agency before PHIG) and new (i.e., external to agency at any point during PHIG) staff |
Current status (i.e., position count) at end of reporting period |
PHIG only (filled by job classification and program area) |
Include: Full-time, part-time, contractual, seasonal, and internal transfer staff, LHD positions funded by state PHIG recipients
Do not include: In-kind staff, those who only received an incentive/retention bonus but are not funded by PHIG |
A1.2 Overall agency staff retention rate |
Only specific reporting period (RP4: 6/1/2023-11/30/2024) |
Agency-wide (if recipient is part of a super agency, only include data for the health department) |
Include: Permanent only (full- or part-time) and all staff (including temporary/contract)
Do not include: Volunteers, interns, federal assignees, Direct Assistance or seasonal staff, LHD positions funded by state PHIG recipients |
A2.1 Time-to-fill position |
Only specific reporting period (RP3: 6/1/2023-11/30/2024) |
Agency-wide (if recipient is part of a super agency, only include data for the health department) |
Include: Permanent (full- or part-time) and temporary/contract staff
Do not include: LHD positions funded by state PHIG recipients |
A2.2 Procurement cycle time |
Only specific reporting period (RP3: 6/1/2023-11/30/2024) |
Agency-wide (if recipient is part of a super agency, only include data for the health department) |
Include: All procurements agency-wide, including purchase orders if normally included
Do not include: Procurements related to IT, under $10,000, or from LHDs funded by state PHIG recipients (e.g., grants, subawards) |
A2.3 Level of involvement with PHAB accreditation |
Current status at end of reporting period |
Agency-wide |
N/A |
1 A workforce could be diverse as it relates to, for example, race/ethnicity, culture, language, age, gender, specific geographic area of the health department’s jurisdiction, or skillset. The health department may seek to recruit and hire a workforce that reflects the characteristics and demographics of the population using health department services. (PHAB Standards & Measures for Initial Accreditation, v 2022)
2 A3 measures are aligned with ELC HIS performance measures and should be reported via ELC REDCap. Acknowledgment of PHIG-ELC coordination should occur every 6 months in PHIVE on the PHIG reporting schedule.
3 Note updated numbering schema for A3 measures from 2023 A3 Supplemental Guidance.
4 See Appendix C: ELC HIS Reporting and PHIVE Acknowledgement Schedule for more detail on ELC REDCap reporting requirements. A3 reporting requirements are subject to change following Reporting Period 2.
5 Sellers, K., Leider, J. P., Lamprecht, L., Liss-Levinson, R., & Castrucci, B. C. (2020). Using Public Health Workforce Surveillance Data to Prioritize Retention Efforts for Younger Staff. American journal of preventive medicine, 59(4), 562–569. https://doi.org/10.1016/j.amepre.2020.03.017
6 Leider, Jonathon P., Brian C. Castrucci, Moriah Robins, Rachel Hare Bork, Michael R. Fraser, Elena Savoia, Rachael Piltch-Loeb, and Howard K. Koh. “The Exodus Of State And Local Public Health Employees: Separations Started Before And Continued Throughout COVID-19.” Health Affairs 42, no. 3 (March 2023): 338–48. https://doi.org/10.1377/hlthaff.2022.01251.
7 CDC acknowledges that recipients may have postings that are continuously open. Please include these postings in this data element if possible and feel free to include additional context around the reported number of days. CDC and partners are considering the context of continuously open postings when reviewing the range of days.
8 Procurement of equipment, supplies, and services refers to the policies, procedures, and actions taken by the health department to obtain the necessary equipment and supplies that may be needed to carry out both its regular agency functions and those functions that may be needed during times of emergencies, disasters, or outbreaks. This area includes contracting for public health services.

| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | Chung, Christina L. (CDC/DDPHSS/CSELS/DSEPD) |
| File Modified | 0000-00-00 |
| File Created | 2024-11-14 |
© 2026 OMB.report | Privacy Policy