Form 0920-1282 State/Local/Territorial Freely Associated States Public
[OADPS] The Performance Measures Project: Improving Performance Measurement and Monitoring by CDC Programs
ORR-PHEP TU-24-0137 Data Entry and Reporting Guide
[ORR_PPEO] Performance Measure Specifications and Implementation Guidance: Codebook for Data Entry and Reporting
OMB: 0920-1282
-
Form Approved
OMB Control Number: 0920-1282
Expiration Date: 06/30/2026
Project Title: Public Health Emergency Preparedness Cooperative Agreement
Performance Measure Specifications and Implementation Guidance: Codebook for Data Entry and Reporting
Period of Performance: Fiscal Years 2024–2028
OMB Burden Statement: Public reporting burden of this collection of information is estimated to average 3168 hours per response per year, including the time for reviewing instructions, searching existing data sources, gathering, and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not required to respond to a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden to CDC/ATSDR Reports Clearance Officer; 1600 Clifton Road NE, MS D-74, Atlanta, Georgia 30333; Attn: OMB-PRA (0920-1282).
Contents
Introduction and Purpose of Guidance 5
Evaluation and Performance Measurement Plan 5
Performance Measures by Readiness and Response Framework Strategies 5
All-Hazards Activities (AHA) 6
AHA-A: Complete and submit a risk assessment (RA) and data elements 6
AHA-B: Complete and submit a multiyear integration preparedness plan (MYIPP) and data elements 7
AHA-C: Develop and conduct required exercises 8
AHA-D: Submit exercise and incident response improvement plan (IP) data elements 8
AHA-F: Review and update CHEMPACK plans 9
Public Health Laboratory (LAB) 11
LAB-A: Participate in LRN-C specimen packaging and shipping exercises (SPaSE) 11
LAB-B: Participate in LRN-B challenge panels 11
LAB C: Participate in LRN-C proficiency testing 12
LAB D: Implement specified standards for electronic reporting of LRN-B and LRN-C laboratory data 12
LAB E: Develop surge capacity plans for LRN laboratories 12
LAB F: Maintain LRN program fiscal strategy 12
PAR-A: Include critical response and recovery partners in required plans and exercises 18
REC-A: Incorporate recovery operations into public health multiyear integrated preparedness plans 22
Administrative and Budget Preparedness (ADM) 26
ADM-A: Update administrative preparedness plans using lessons learned from emergency responses 26
ADM-D: Reduce the time PHEP-funded positions at the recipient level remain vacant 27
LOC-B: Provide direct technical assistance and surge support staffing to increase local readiness 32
LOC-C: Include local representation on senior advisory committees (SAC) 32
Appendix A: PHEP Logic Model 36
Appendix B: Roster Answer Choices 39
Appendix D: Exercise Data Elements 53
1. ADM-B: Administrative Preparedness 53
2. BIO100: Biological Incident 100 53
4. RADNUC: Radiological/Nuclear Incident 53
5. RFT: Rural/frontier/tribal coordination 53
8. CAP200: Drill Capstone 200 53
9. CCD: Drill Critical contacts 53
10. IDE: Drill Inventory data exchange 53
11. BIO200: Functional Biological incident 200 53
12. CAP300: Functional Capstone 300 53
13. CAP400: Full-scale exercise Capstone 400 53
Appendix E: One PHEP Community of Practice (CoP) 55
One PHEP CoP baseline survey 55
One PHEP CoP quarterly survey 56
Appendix F: Evaluation of Trainings 58
Appendix G: Monitoring and Technical Assistance 60
Technical Assistance Survey (TAS) 60
Technical Assistance Feedback (TAF) 60
Introduction and Purpose of Guidance
The Centers for Disease Control and Prevention (CDC) is responsible for developing and implementing standardized, relevant, feasible, and useful performance measures and evaluation strategies as part of the Public Health Emergency Preparedness (PHEP) cooperative agreement. The PHEP program provides 62 jurisdictions with funding to enhance the preparedness, response, and recovery capabilities of state, tribal, local, and territorial public health systems through a continuous cycle of planning, training, equipping, exercising, evaluating, and implementing corrective actions.
Evaluation and Performance Measurement Plan
PHEP recipients must submit an evaluation and performance measurement plan once during the five-year period of performance. The evaluation and performance measurement plan must address the overall methods for collecting and monitoring performance data and specify the data management plan for each activity described in the NOFO CDC-RFA-TU-24-0137. Additionally, the evaluation and performance measurement plan will describe the recipients plans for how the data will be generated, protected, operationalized (data standards and documentation), archived, and disseminated.
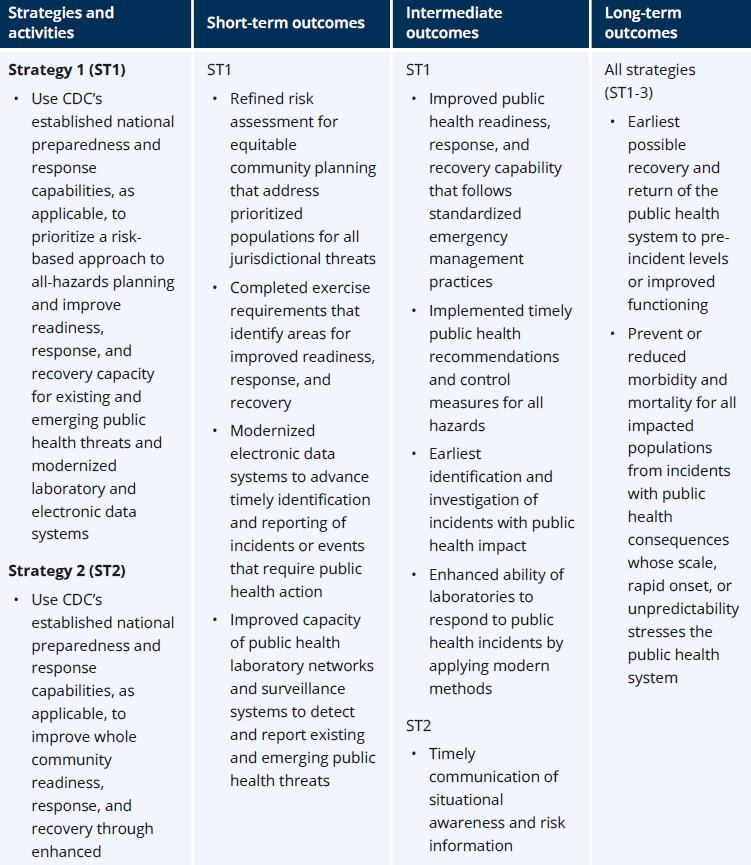
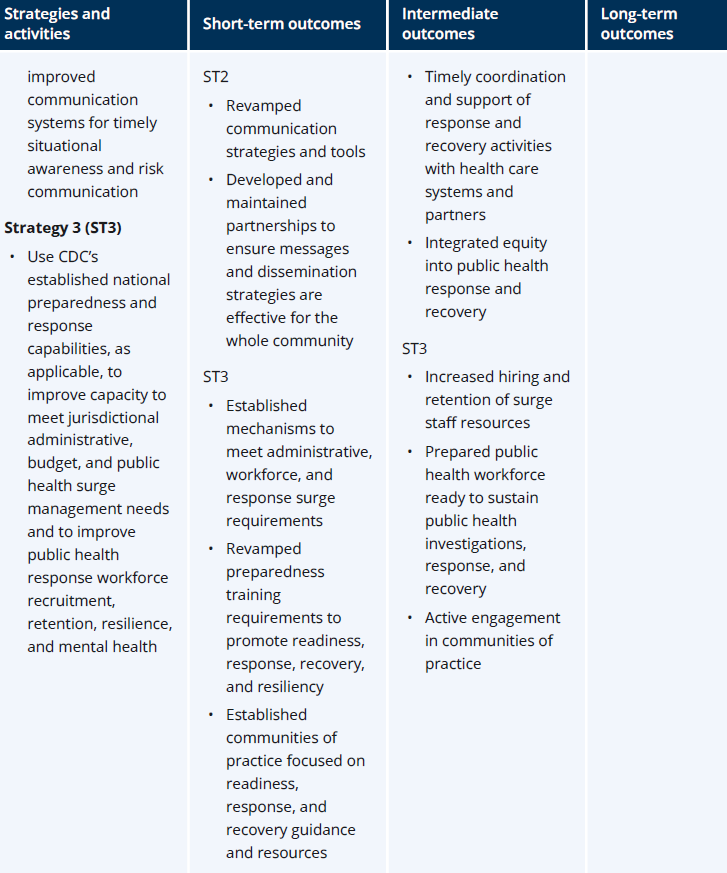
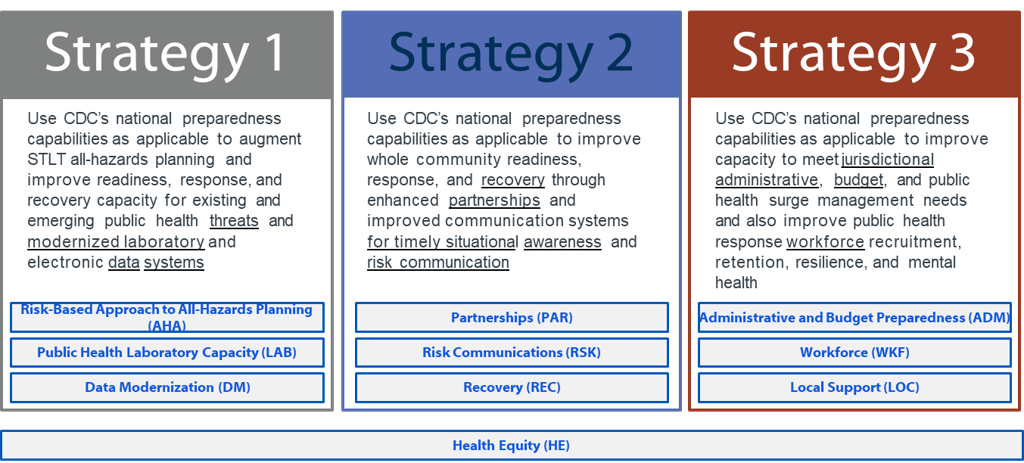
Performance Measures by Readiness and Response Framework Strategies
This section details the specific activities PHEP recipients must complete during the five-year performance period, July 1, 2024–June 30, 2029. Performance measures are based on specific short-, intermediate-, and long-term outcomes in alignment with the PHEP logic model (see Appendix A). Recipients must apply the foundational capabilities that the PHEP program has established and track and report progress on 10 cross-cutting priorities anchored in CDC’s RRF. Additionally, Section 319C-1(g) of the Public Health Service Act requires recipients meet benchmark requirements and report complete and accurate performance data. Activities with benchmarks are indicated in Tables 1–10. The guidance delineates linkage of related activities by indicating where credit of related activities is associated.
The
Public
Health Emergency Preparedness and Response Capabilities: National
Standards for State, Local, Tribal, and Territorial Public Health,
describe the foundational capabilities used to support advancement
of preparedness, response, and recovery operations for PHEP
recipients.
Performance data are used to inform CDC and partners on recipient progress and areas requiring improvement; facilitate discussions among recipients, key partners, and CDC for opportunities for improvement and sharing of best practices; and inform future PHEP program activities such as work plan and budget plan adjustments during the performance period.
CDC’s new online platform to collect and maintain all data for the PHEP cooperative agreement is called DSLR Ready Camp. DSLR Ready Camp is built on the Salesforce platform. DSLR Ready Camp will be released for use by recipients in Spring 2025. In the meantime, to meet the reporting requirements outlined in the PHEP cooperative agreement as specified in this document, CDC is providing standardized templates that recipients will use to report and submit data to CDC. Data submitted via this interim solution will be incorporated into the DSLR Ready Camp system.
Strategy 1
Use CDC’s established national preparedness and response capabilities, as applicable, to prioritize a risk-based approach to all-hazards planning and improve readiness, response, and recovery capacity for existing and emerging public health threats and modernized laboratory and electronic data systems.
All-Hazards Activities (AHA)
Table 1. Response Readiness Framework: All-Hazards Activities Priorities
All-hazards risk assessment identifies potential hazards, unique vulnerabilities, and community risk factors that could impact the jurisdiction’s public health, medical, and mental/behavioral health infrastructure. Preparedness programs use the identified threats and hazards to strengthen planning and response protocols and capabilities. |
|
Activity |
AHA-A: Complete and submit a risk assessment (RA) and data elements (RADE) reflecting the needs of the whole jurisdiction. *AHA-B: Complete and submit multiyear integrated preparedness plans (MYIPP) and data elements. AHA-C: Develop and conduct required exercises. AHA-D: Submit exercise and incident response improvement plan data elements. AHA-E: Maintain capacity and capability to distribute, dispense, administer medical countermeasures, and manage medical material. AHA-F: Review and update CHEMPACK plans. AHA-G: Complete training to ensure baseline competency and integration with preparedness requirements.
*PHEP Benchmark |
Who must report |
62 recipients |
Rationale |
Risk assessment is an integral part of overall risk management of public health events, and it informs risk mitigation measures and risk communication activities. A systematic all-hazards risk assessment identifies potential hazards, unique vulnerabilities, and community risk factors that could impact the jurisdiction’s public health, medical, and mental/behavioral health infrastructure, and guide defensible decision-making and the foundation for appropriate response measures. |
Data elements |
Each recipient must submit the described data elements to CDC. Data marked with “**” contributes to recipients’ performance evaluation. Additional data are collected to evaluate program impact and address national preparedness, readiness, and response. The technical specification for all data elements is described in the following bullets. Relevant answer choices are found in Appendix B, Appendix C, or as specified. Data will be submitted via DSLR Ready Camp. AHA-A: Complete and submit a risk assessment (RA) and data elements
AHA-B: Complete and submit a multiyear integration preparedness plan (MYIPP) and data elements
AHA-C: Develop and conduct required exercises
AHA-D: Submit exercise and incident response improvement plan (IP) data elements
AHA-E: Maintain capacity and capability to distribute, dispense, administer medical countermeasures (MCMs) and manage medical materiel
AHA-F: Review and update CHEMPACK plans
AHA-G: Complete training to ensure baseline competency and integration with preparedness requirements
|
Additional guidance |
Use CDC’s established national preparedness and response capabilities, as applicable, to prioritize a risk-based approach to all-hazards planning and improve readiness, response, and recovery capacity for existing and emerging public health threats and modernized laboratory and electronic data systems.
The AHA is designed to improve your response and recovery readiness when used with the exercise framework. It offers a cohesive and structured process that includes:
Along with your CRI local planning jurisdictions, you must maintain the capacity and capability to manage, distribute, dispense, and administer MCM according to the Administration for Strategic Preparedness and Response/Strategic National Stockpile (ASPR/SNS) requirements and guidelines. Direct questions to ASPR regarding requirements on validating receipt, stage, and storage (RSS) sites and testing inventory data exchange, along with SNS guidance on developing capacity and capability to receive, distribute, dispense, and administer MCM. See also Hospital Preparedness Program details in the PHEP NOFO CDC-RFA-TU-24-0137 (pages 62-63). |
How will this data be used? |
Preparedness programs use the identified threats and hazards to strengthen planning and response protocols and capabilities. Refined risk assessment for equitable community planning that addresses prioritized populations for all jurisdictional threats informs community preparedness and improves public health readiness, response, and recovery capability. By implementing standardized emergency management practices, jurisdictions will implement timely public health recommendations and control measures for all hazards and be positioned to identify and investigate, at the earliest signals, incidents with public health impact. |
Target (if applicable) |
Each recipient must complete all AHA activities and submit required data.
|
Recommended data source |
Recipients must compile data while conducting the activity. Recipients can store data in any format that is available to them. |
Reporting frequency |
Recipients must report progress on all activities, at a minimum, on a quarterly basis. Following are activities with specific deadlines.
|
Public Health Laboratory (LAB)
Table 2. Response Readiness Framework: Public Health Laboratory Capacity Priorities
Strategy 1: Public health laboratory capacity (LAB) |
Public health laboratory (PHL) testing is the ability to implement and perform methods to detect, characterize, and confirm public health threats. It also includes the ability to report timely data, provide investigative support, and use partnerships to address actual or potential exposure to threat agents in multiple matrices, including clinical specimens, food, water, and other environmental samples. Laboratory services must support the rapid detection of biological samples for the investigation and containment of hazards to the public’s health. |
Activity |
LAB-A: Participate in LRN-C specimen packaging and shipping exercises (SPaSE) *LAB-B: Participate in LRN-B challenge panels *LAB C: Participate in LRN-C proficiency testing LAB D: Implement specified standards for electronic reporting of LRN-B and LRN-C laboratory data LAB E: Develop surge capacity plans for LRN laboratories and incorporate related surge activities in jurisdictional exercises LAB F: Maintain LRN program fiscal strategy *PHEP Benchmark |
Who must report |
|
Rationale |
PHEP funding supports the Laboratory Response Network for Biological Threats Preparedness (LRN-B) and LRN for Chemical Threats Preparedness (LRN-C) laboratories. PHLs must advance capacity and capability to respond to emerging public health threats through initial detection and rapid electronic results sharing. |
Data elements |
Each recipient must submit the described data elements to CDC. Data marked with “**” contributes to recipients’ performance evaluation. CDC collects additional data to evaluate program impact and address national preparedness, readiness, and response. The technical specification for all data elements is described in the following bullets. Relevant answer choices are found in Appendix B, Appendix C, or as specified. Data will be submitted via DSLR Ready Camp. LAB-A: Participate in LRN-C specimen packaging and shipping exercises (SPaSE)
LAB-B: Participate in LRN-B challenge panels
LAB C: Participate in LRN-C proficiency testing
LAB D: Implement specified standards for electronic reporting of LRN-B and LRN-C laboratory data
LAB E: Develop surge capacity plans for LRN laboratories
LAB F: Maintain LRN program fiscal strategy
|
Additional guidance |
Laboratory services must support the rapid detection of biological or chemical samples for the investigation and containment of hazards to the public’s health.
|
How will this data be used? |
CDC will use these data to verify if the laboratory is qualified to test for certain biological and chemical agents and demonstrate ongoing proficiency of testing capabilities. The LRN proficiency testing challenge counts toward the PHEP programmatic benchmark. |
Target (if applicable) |
Each recipient must complete all LAB activities (as applicable). Data is received from LRN.
|
Recommended data source |
Recipients must compile data while conducting the activity. Recipients can store data in any format that is available to them. |
Reporting frequency |
Recipients must report progress on all activities, at a minimum, on a quarterly basis. |
Data Modernization (DM)
Table 3. Response Readiness Framework: Data Modernization Priorities
Strategy 1: Data modernization (DM) |
CDC’s Public Health Data Strategy is a mission-focused and goal-driven two-year plan providing accountability for data, technology, policy and administrative actions necessary to meet public health data goals. Its measurable milestones address challenges in data exchange between healthcare organizations and public health authorities and between state, tribal, local, territorial, and federal public health authorities. Data modernization is essential for protecting health and improving lives during public health emergencies. |
Activity |
DM-A: Incorporate data systems and data source functionality and infrastructure in public health emergency response plans DM-B: Incorporate testing of the functionality and infrastructure of data systems and data sources into jurisdictional exercises |
Who must report |
62 recipients |
Rationale |
An effective plan for information and data sharing increases the capacity of public health agencies to electronically exchange accurate health data and information from a variety of sources. Access to timely, relevant information is critical to accurately assess a situation and take appropriate actions to mitigate adverse public health consequences and promote healthy outcomes. |
Data elements |
Each recipient must submit the described data elements to CDC. Data marked with “**” contributes to recipients’ performance evaluation. CDC collects additional data to evaluate program impact and address national preparedness, readiness, and response. The technical specification for all data elements is described in the following bullets. Relevant answer choices are found in Appendix B, Appendix C, or as specified. Data will be submitted via DSLR Ready Camp. DM-A: Incorporate data systems and data source functionality and infrastructure in Public Health Emergency response plans
DM-B: Incorporate testing of the functionality and infrastructure of data systems and data sources into jurisdictional exercises
|
Additional guidance |
Recipients must modernize data and data systems by demonstrating improvements through exercising at least three core public health data sources or systems prioritized by the jurisdiction or as described in the Public Health Data Strategy. |
How will this data be used? |
Completion of DM activities will ensure that the health departments, hospitals, and laboratories are prepared at the state and local levels to easily exchange information across data collection and other data systems in real-time to respond effectively to public health emergencies. |
Target (if applicable) |
Each recipient must complete all DM activities and submit required data. |
Recommended data source |
Recipients must compile data while conducting the activity. Recipients can store data in any format that is available to them. |
Reporting frequency |
Recipients must report progress on all activities, at a minimum, on a quarterly basis. |
Health Equity (HE)
Table 4a. Response Readiness Framework: Health Equity Priorities
Strategy 1–3: Health equity (HE)
|
Health equity (HE) in public health preparedness and response refers to the principle and practice of ensuring that all communities and people have fair access to the resources, strategies, and interventions necessary to protect health before, during, and after a public health emergency or disaster. This concept recognizes that some populations may be at greater risk for disproportionate outcomes given socioeconomic status, geography, age, disability, race, ethnicity, or other characteristics historically linked to discrimination or exclusion. Note: HE is applicable across all three strategies and is addressed in relevant sections. |
Activity |
*HE-A: Update risk assessment to include people who are disproportionately impacted by public health emergencies *PHEP Benchmark |
Who must report |
62 recipients |
Rationale |
By focusing on HE in public health preparedness and response, recipients aim to minimize the adverse effects of a public health emergency on populations likely to be disproportionality affected or those with access and functional needs while promoting the well-being of all community members regardless of their background or circumstances. |
Data elements |
Each recipient must submit the described data elements to CDC. Data marked with “**” contributes to recipients’ performance evaluation. CDC collects additional data to evaluate program impact and address national preparedness, readiness, and response. The technical specification for all data elements is described in the following bullets. Relevant answer choices are found in Appendix B, Appendix C, or as specified. Data will be submitted via DSLR Ready Camp. HE-A: Update risk assessment to include people who are disproportionately impacted by public health emergencies
|
Additional guidance |
Providing equitable resources, strategies, and interventions must be accounted for during all phases of the preparedness life cycle and include:
Recipients must complete a RA that identifies prioritized populations and those that are potentially disproportionately affected or have access and functional needs, given the identified risks; see AHA-A). |
How will this data be used? |
PHEP aims to improve preparedness and response support for communities facing health disparities by integrating HE practices into preparedness and response plans. Recipients will be assessed based on whether HE is incorporated into the jurisdictions’ preparedness and response plans and exercises. |
Target (if applicable) |
Each recipient must complete all HE activities and submit required data.
|
Recommended data source |
Recipients must compile data while conducting the activity. Recipients can store data in any format that is available to them. |
Reporting frequency |
Recipients must report progress on all activities, at a minimum, on a quarterly basis. |
Strategy 2
Use CDC’s established national preparedness and response capabilities, as applicable, to improve whole community readiness, response, and recovery through enhanced partnerships and improved communication systems for timely situational awareness and risk communication.
Partnerships (PAR)
Table 5. Response Readiness Framework: Partnership Priority
Public health partners for preparedness and response are a diverse set of stakeholders who collaborate to plan for, respond to, and recover from public health emergencies. These partners come from various sectors and possess knowledge, skills, resources, and perspectives that contribute to a comprehensive understanding of the community. |
|
Activity |
*PAR-A: Include critical response and recovery partners in required plans and exercises *PHEP Benchmark |
Who must report |
62 recipients |
Rationale |
Partner inclusion will also increase knowledge and support for community involvement in jurisdictions' preparedness and response efforts. CDC encourages PHEP recipients to effectively partner with local, state, territorial, tribal, and federal governments; private sector organizations, including community and non-governmental organizations, and other entities as appropriate to create opportunities to coordinate, amplify, and support whole community planning, readiness, and response goals. |
Data elements |
Each recipient must submit the described data elements to CDC. Data marked with “**” contributes to recipients’ performance evaluation. CDC collects additional data to evaluate program impact and address national preparedness, readiness, and response. The technical specification for all data elements is described in the following bullets. Relevant answer choices are found in Appendix B, Appendix C, or as specified. Data will be submitted via DSLR Ready Camp. PAR-A: Include critical response and recovery partners in required plans and exercises
|
Additional guidance |
Strong, fully engaged community (jurisdictional) partners are critical for public health preparedness. Public and private partners are often perceived as trusted sources and support preparedness by working with the health department to provide input and mitigate identified health risks for the communities they serve. Partners also help identify community roles and responsibilities and coordinate the delivery of essential health services to strengthen community resilience as early as possible before, during, and after a public health emergency. Jurisdictions can leverage partner insights to develop and disseminate information that address the needs of at-risk populations that may be disproportionately affected by a public health response. See also partner detail in the PHEP NOFO CDC-RFA-TU-24-0137 (page 60).
Engaging community partners that work with at-risk populations is essential for preparedness planning. The 2019 Pandemic and All-Hazards Preparedness and Advancing Innovation Act (PAHPAIA), Public Law No. 116-22 requires the health and medical needs of all individuals, including at-risk populations, be protected. The Americans with Disabilities Act (ADA) also protects people with disabilities and prohibits discrimination. Updated in 2008, the ADA Amendments Act (ADAAA) mandates that individuals with access and functional needs be included in all disaster plans developed for a community under Title II. PAHPAIA defines at-risk individuals as children, pregnant women, older adults, individuals with disabilities, or others who may have access or functional needs in the event of a public health emergency, as determined by the Secretary of Health and Human Services. |
How will this data be used? |
CDC will use this information to verify jurisdictions adopt a whole community planning approach. |
Target (if applicable) |
Each recipient must complete the PAR activity and submit required data.
|
Recommended data source |
Recipients must compile data while conducting the activity. Recipients can store data in any format that is available to them. |
Reporting frequency |
Recipients must report progress on all activities, at a minimum, on a quarterly basis. |
Risk Communications (RSK)
Table 6. Response Readiness Framework: Risk Communication (RSK) Priorities
Strategy 2: Risk communications (RSK) |
Providing emergency public information and warnings during a public health event is the ability to develop, coordinate, and disseminate information, alerts, warnings, and notifications to the public and incident management personnel. Timely risk communication is necessary during all phases of an incident through multiple methods to a variety of audiences, including communities and incident management partners, to understand the current situation and take appropriate actions. |
Activity |
RSK-A: Develop or update CERC and information dissemination plans *RSK-B: Identify and implement communication surveillance, media relations, and digital communication strategies in exercises RSK-C: Identify and implement specific CERC activities that meet the diverse needs of communities of focus *PHEP Benchmark |
Who must report |
62 recipients |
Rationale |
An effective plan for information and data sharing increases the capacity of public health agencies to electronically exchange accurate health data and information from a variety of sources during incidents. |
Data elements |
Each recipient must submit the described data elements to CDC. Data marked with “**” contributes to recipients’ performance evaluation. CDC collects additional data to evaluate program impact and address national preparedness, readiness, and response. The technical specification for all data elements is described in the following bullets. Relevant answer choices are found in Appendix B, Appendix C, or as specified. Data will be submitted via DSLR Ready Camp. RSK-A: Develop or update crisis and emergency risk communication (CERC) and information dissemination plans
RSK-B: Identify and implement communication surveillance, media relations, and digital communication strategies in exercises
RSK-C: Identify and implement specific CERC activities that meet the diverse needs of communities of focus
|
Additional guidance |
Recipients must engage partners that represent prioritized populations to develop and disseminate culturally appropriate messages for use during public health responses. In addition to clear messaging for the whole community, an effective CERC plan must address the capacity of public health agencies to electronically exchange accurate health data and information from a variety of sources during incidents. Access to timely, relevant information flow is critical to incident partners’ ability to understand the current situation and take appropriate actions. Engage partners and exercise the ability to conduct multijurisdictional and multidisciplinary exchange of health-related information and situational awareness data among federal, state, local, territorial, and tribal levels of government and the private sector. |
How will this data be used? |
CDC will evaluate recipient’s ability to identify and incorporate best practices for strengthening risk communication and reducing mis-/dis-information into plans for communication during public health emergencies. |
Target (if applicable) |
Each recipient must complete all RSK activities and submit required data.
|
Recommended data source |
Recipients must compile data while conducting the activity. Recipients can store data in any format that is available to them. |
Reporting frequency |
Recipients must report progress on all activities, at a minimum, on a quarterly basis. |
Recovery (REC)
Table 7. Response Readiness Framework: Recovery (REC) Priorities
Strategy 2: Recovery activity (REC) |
Community recovery is the ability of communities to identify critical assets, facilities, and other services within public health, emergency management, health care, human services, mental/behavioral health, and environmental health sectors that can guide and prioritize recovery operations. |
Activity |
REC-A: Incorporate recovery operations into public health MYIPP |
Who must report |
62 recipients |
Rationale |
It is important to prioritize community recovery efforts into response and preparedness plans to support health department reconstitution and incorporate lessons learned from responses. |
Data elements |
Each recipient must submit the described data elements to CDC. Data marked with “**” contributes to recipients’ performance evaluation. CDC collects additional data to evaluate program impact and address national preparedness, readiness, and response. The technical specification for all data elements is described in the following bullets. Relevant answer choices are found in Appendix B, Appendix C, or as specified. Data will be submitted via DSLR Ready Camp. REC-A: Incorporate recovery operations into public health multiyear integrated preparedness plans
|
Additional guidance |
Communities should consider collaborating with jurisdictional partners to plan, advocate, facilitate, monitor, and implement the restoration of public health, health care, human services, mental/behavioral health, and environmental health sectors to a level of functioning comparable to pre-incident levels or improved levels where possible.
|
How will this data be used? |
Incorporating recovery into the preparedness life cycle helps ensure the earliest possible recovery and return of the public health system to pre-incident levels or improved functioning post response. During this performance period, recipients must progressively exercise recovery objectives to demonstrate how the jurisdiction’s plans will readily return the community to routine public health function post response. Partners involved in response and recovery should be actively engaged in training and exercises. Lessons learned from exercises should prompt updates to relevant plans and be documented as strengths or areas for improvements in the MYIPP (see AHA-B). |
Target (if applicable) |
Each recipient must complete the REC activity and submit all required data. |
Recommended data source |
Data must be compiled by the recipient while conducting the activity. Data can be stored in any format that is available to the recipient. |
Reporting frequency |
Progress on all activities must be reported, at minimum, on a quarterly basis. Activities with specific deadlines are noted below.
|
Health Equity (HE)
Table 4b. Response Readiness Framework: Health Equity Priorities
Strategy 1–3: Health Equity (HE)
|
Health equity (HE) in public health preparedness and response refers to the principle and practice of ensuring that all communities and people have fair access to the resources, strategies, and interventions necessary to protect health before, during, and after a public health emergency or disaster. This concept recognizes that some populations may be at greater risk for disproportionate outcomes given socioeconomic status, geography, age, disability, race, ethnicity, or other characteristics historically linked to discrimination or exclusion. Note: HE is applicable across all three strategies and is addressed in relevant sections. |
Activity |
HE-B: Engage partners to incorporate HE principles into preparedness plans and exercises |
Who must report |
62 recipients |
Rationale |
By focusing on HE in public health preparedness and response, recipients aim to minimize the adverse effects of a public health emergency on populations likely to be disproportionality affected or those with access and functional needs while promoting the well-being of all community members regardless of their background or circumstances. |
Data elements |
Each recipient must submit the described data elements to CDC. Data marked with “**” contributes to recipients’ performance evaluation. CDC collects additional data to evaluate program impact and address national preparedness, readiness, and response. The technical specification for all data elements is described in the following bullets. Relevant answer choices are found in Appendix B, Appendix C, or as specified. Data will be submitted via DSLR Ready Camp. HE-B: Engage partners to incorporate health equity principles into preparedness plans and exercises
|
Additional guidance |
Providing equitable resources, strategies, and interventions must be accounted for during all phases of the preparedness life cycle and include:
Recipients must complete a risk assessment that identifies prioritized populations, those that are potentially disproportionately affected or have access and functional needs, given the identified risks; see AHA-A). |
How will this data be used? |
PHEP aims to improve preparedness and response support for communities facing health disparities by integrating health equity practices into preparedness and response plans. Recipients will be assessed based on how well health equity is incorporated into the jurisdictions’ preparedness and response plans and exercises. |
Target (if applicable) |
Each recipient must complete the HE activity and submit all required data. |
Recommended data source |
Recipients must compile data while conducting the activity. Recipients can store data in any format that is available to them. |
Reporting frequency |
Recipients must report progress on all activities, at a minimum, on a quarterly basis. |
Strategy 3
Use CDC’s established national preparedness and response capabilities, as applicable, to improve capacity to meet jurisdictional administrative, budget, and public health surge management needs and to improve public health response workforce recruitment, retention, resilience, and mental health.
Administrative and Budget Preparedness (ADM)
Table 8. Response Readiness Framework: Administrative and Budget Preparedness (ADM) Priorities
Strategy 3: Administrative and budget preparedness (ADM)
|
ADM activities intend to improve the overall policies, systems, and mechanisms that support human and financial resource requirements that underpin the agency’s ability to respond rapidly to a new public health threat. Flexible and scalable policies, processes, and systems will improve administrative and budget preparedness and ensure timely access to resources for supporting jurisdictional responses. |
Activity |
ADM-A: Update administrative preparedness plans using lessons learned from emergency responses ADM-B: Integrate administrative and budget preparedness recommendations into training and exercises ADM-C: Improve adherence to guidance related to spending, lapsing of funds, awarding of local contracts, and other administrative and budgetary requirements *ADM-D: Reduce the time PHEP-funded positions at the recipient level remain vacant *ADM-E: Distribute or award funds to local health departments and tribal entities within 90 days after the start of the budget period
*PHEP Benchmark |
Who must report |
62 recipients |
Rationale |
Recipients must comply with federal regulations as stated in the terms and conditions of the funding award for appropriate use of federal funds including restrictions, tracking, and reporting requirements. Recipients must ensure fiscal and programmatic accountability are in place to document authorized, disbursed, and unobligated funds and demonstrate overall annual improvement. |
Data elements |
Each recipient must submit the described data elements to CDC. Data marked with “**” contributes to recipients’ performance evaluation. CDC collects additional data to evaluate program impact and address national preparedness, readiness, and response. The technical specification for all data elements is described in the following bullets. Relevant answer choices are found in Appendix B, Appendix C, or as specified. Data will be submitted via DSLR Ready Camp. ADM-A: Update administrative preparedness plans using lessons learned from emergency responses
ADM-B: Integrate administrative and budget preparedness recommendations into training and exercises
ADM-C: Improve adherence to guidance related to spending, lapsing of funds, awarding of local contracts, and other administrative and budgetary requirements
ADM-D: Reduce the time PHEP-funded positions at the recipient level remain vacant
ADM-E: Distribute or award funds to local health departments and tribal entities within 90 days after the start of the budget period
|
Additional guidance |
ADM-B: Recipients must have PHEP-funded staff complete the jurisdiction's minimum training requirements and participate in exercises as relevant (see AHA-G & WKF-B). |
How will this data be used? |
This measure intends to understand how recipients have improved their overall procurement process by implementing these policies by assessing the timeliness of an agency’s procurement cycle time. This information would further help in identifying the need for continued funding and improvements or opportunities in the public health system’s ability to spend money more efficiently. |
Target (if applicable) |
Each recipient must complete all ADM activities and submit required data.
|
Recommended data source |
Recipients must compile data while conducting the activity. Recipients can store data in any format that is available to them. |
Reporting frequency |
Recipients must report progress on all activities, at a minimum, on a quarterly basis. Following are activities with specific deadlines. |
Workforce (WKF)
Table 9. Response Readiness Framework: Workforce (WKF) Priorities
Strategy 3: Workforce (WKF) |
A sufficient public health workforce is needed to accelerate prevention, preparedness, and response to emerging health threats and improve public health outcomes. Increased hiring and retention of diverse public health staff is an intended outcome during this period of performance. Types of hiring activities include, but are not limited to, expanding recruitment efforts, creating new positions, improving hiring incentives, and streamlining new hiring mechanisms. |
Activity |
*WKF-A: Develop plans, processes, and procedures to recruit, hire, train, and retain a highly qualified and diverse workforce WKF-B: Provide guidance, direction, and training to maintain a ready responder workforce across the entire health department WKF-C: Actively engage in at least one community of practice that identifies problems, solutions, and best practices in workforce recruitment, hiring, training, retention, or resiliency *PHEP Benchmark |
Who must report |
|
Rationale |
Maintaining a workforce development plan that address a coordinated approach to training staff and implementing procedural improvements for a well-qualified, response-ready workforce is essential for administering and promoting public health practices. The intent of this measure is to understand the number of positions supported by PHEP funds within health departments. This includes positions supported within health departments that have received direct funding, and positions supported within local health departments from funds distributed from state health department recipients. |
Data elements |
Each recipient must submit the described data elements to CDC. Data marked with “**” contributes to recipients’ performance evaluation. CDC collects additional data to evaluate program impact and address national preparedness, readiness, and response. The technical specification for all data elements is described in the following bullets. Relevant answer choices are found in Appendix B, Appendix C, or as specified. Data will be submitted via DSLR Ready Camp. WKF-A: Develop plans, processes, and procedures to recruit, hire, train, and retain a highly qualified and diverse workforce
WKF-B: Provide guidance, direction, and training to maintain a ready responder workforce across the entire health department
WKF-C: Actively engage in at least one community of practice (CoP) that identifies problems, solutions, and best practices in workforce recruitment, hiring, training, retention, or resiliency
|
Additional guidance |
Throughout the performance period, monitor and mitigate existing or anticipated staff vacancies and develop strategies for surge staff to support a range of emergency responses.
Include health department preparedness staff and surge staff outside the preparedness program who fill key incident command roles in preparedness training and periodic exercises. Primary response staff must participate in exercises on a rotational basis as determined by the health department. PHEP staff and surge jurisdictional staff must participate in full-scale exercises involving federal agencies.
Actively engage in a CoP that discusses gaps, strengths, barriers and improves PHEP workforce capacity and resiliency. See also Appendix E, CDC One PHEP CoP. |
How will this data be used? |
Workforce activities will improve capacity to meet routine and surge needs by increasing support, retention, and resiliency of a well-qualified, diverse, and response ready public health staff. |
Target (if applicable) |
Each recipient must complete all WKF activities and submit required data.
WKF-A: Recipients must reduce workforce vacancy rates funded by PHEP. The benchmark is dependent on the jurisdiction’s vacancy rate at the start of the five-year performance period.
|
Recommended data source |
Recipients must compile data while conducting the activity. Recipients can store data in any format that is available to them. |
Reporting frequency |
Recipients must report progress on all activities, at a minimum, on a quarterly basis. |
Local Support (LOC)
Table 10. Response Readiness Framework: Local support (LOC) Priorities
Strategy 3: Local support (LOC) |
States must support local readiness efforts and ensure local planning jurisdictions are prepared to respond and recover from public health emergencies. The local support activities pertain to all local planning jurisdictions, tribal entities, rural partners, and other subrecipients within recipients’ geographic boundaries. |
Activity |
LOC-A: Engage local jurisdictions, including rural, frontier, and tribal entities, in public health preparedness planning and exercises LOC-B: Provide direct technical assistance and surge support staffing to increase local readiness LOC-C: Include local representation on senior advisory committees (SAC) |
Who must report |
50 state recipients |
Rationale |
Local planning jurisdictions are critical to advancing readiness and mitigating the impacts of morbidity and mortality prior to or during a public health emergency. |
Data elements |
Each recipient must submit the described data elements to CDC. Data marked with “**” contributes to recipients’ performance evaluation. CDC collects additional data to evaluate program impact and address national preparedness, readiness, and response. The technical specification for all data elements is described in the following bullets. Relevant answer choices are found in Appendix B, Appendix C, or as specified. Data will be submitted via DSLR Ready Camp. LOC-A: Engage local jurisdictions, including rural, frontier, and tribal entities, in public health preparedness planning and exercises
LOC-B: Provide direct technical assistance and surge support staffing to increase local readiness
LOC-C: Include local representation on senior advisory committees (SAC)
|
Additional guidance |
States must assure local planning jurisdictions have or have access to resources that support all preparedness, response, and recovery activities.
|
How will this data be used? |
These data verify how recipients assure local planning jurisdictions are involved in developing and implementing capacity-building activities that support local readiness and response for plans, exercises, and surge needs. |
Target (if applicable) |
Each recipient must complete LOC activities and submit all required data. |
Recommended data source |
Recipients must compile data while conducting the activity. Recipients can store data in any format that is available to them. |
Reporting frequency |
Recipients must report progress on all activities, at a minimum, on a quarterly basis. |
Health Equity (HE)
Table 4c. Response Readiness Framework: Health Equity Priorities
Strategy 1–3: Health Equity (HE)
|
Health equity (HE) in public health preparedness and response refers to the principle and practice of ensuring that all communities and people have fair access to the resources, strategies, and interventions necessary to protect health before, during, and after a public health emergency or disaster. This concept recognizes that some populations may be at greater risk for disproportionate outcomes given socioeconomic status, geography, age, disability, race, ethnicity, or other characteristics historically linked to discrimination or exclusion. Note: HE is applicable across all three strategies and is addressed in relevant sections. |
Activity |
HE-C: Include HE representatives on senior advisory committees (SAC) to increase advocacy for communities of focus. |
Who must report |
62 recipients |
Rationale |
By focusing on HE in public health preparedness and response, recipients aim to minimize the adverse effects of a public health emergency on populations likely to be disproportionality affected or those with access and functional needs while promoting the well-being of all community members regardless of their background or circumstances. |
Data elements |
Each recipient must submit the described data elements to CDC. Data marked with “**” contributes to recipients’ performance evaluation. CDC collects additional data to evaluate program impact and address national preparedness, readiness, and response. The technical specification for all data elements is described in the following bullets. Relevant answer choices are found in Appendix B, Appendix C, or as specified. Data will be submitted via DSLR Ready Camp. HE-C: Include health equity representatives on senior advisory committees (SAC) to increase advocacy for communities of focus
|
Additional guidance |
Providing equitable resources, strategies, and interventions must be accounted for during all phases of the preparedness life cycle and include:
Recipients must complete a RA that identifies prioritized populations and those that are potentially disproportionately affected or have access and functional needs, given the identified risks; see AHA-A). |
How will this data be used? |
PHEP aims to improve preparedness and response support for communities facing health disparities by integrating HE practices into preparedness and response plans. CDC will assess recipients based on how well HE is incorporated into the jurisdictions’ preparedness and response plans and exercises. |
Target (if applicable) |
Each recipient must complete the HE activity and submit all required data. |
Recommended data source |
Recipients must compile data while conducting the activity. Recipients can store data in any format that is available to them. |
Reporting frequency |
Recipients must report progress on all activities, at a minimum, on a quarterly basis. |
Appendix A: PHEP Logic Model
The logic model shows the strategies and activities of the program along with the outcomes we expect over time. You must achieve and report on the outcomes for the five-year performance period.
Appendix B: Roster Answer Choices
Data Elements |
Data Type |
Answer Choices |
ROSTER-NAME: Partner Organization Name |
Text |
|
ROSTER-PRIM-CAT: Primary Partner Category |
Select |
1.
Administration for Strategic Preparedness and Response (ASPR) |
ROSTER-SUB-CAT: Subcategory |
Select |
See table below for detail |
ROSTER-AFN-POPS: AFN populations partners serve or represent
|
Multiselect |
•Children
and youth |
ROSTER-RRF: Partner involvement
|
Multiselect |
•Exercising |
ROSTER-RRF-ACTIVITY: Activity involving partner |
Multiselect |
|
ROSTER-IMPACT: Describe the partner action that resulted from participating in the activity |
text |
Optional narrative |
Primary Partner Category |
|
Subcategory |
|
Multiselect |
• HHS
Coordination Operations and Response Element (HCORE) • Other, specify |
|
Multiselect |
• Aviation
services |
|
Multiselect |
• Audiovisual
Production Specialist |
|
Multiselect |
• Accountant |
|
Multiselect |
• Colleges/Universities |
|
Multiselect |
• Association
of Public Health Laboratories (APHL) |
|
Multiselect |
• Administration
for Children and Families (ACF) |
|
Multiselect |
Jurisdictional risk list |
|
Multiselect |
• Army |
|
Multiselect |
• Community-based
Organizations (CBOs); |
|
Multiselect |
• Emergency
Management |
|
Multiselect |
Federal tribe list |
|
Text |
Optional narrative |
Appendix C: Answer Choices
Data Elements |
Data Type |
Answer Choices |
AHA-A-RADE-NUMBER |
Number |
Enter number of risk assessments for the jurisdiction |
AHA-A-RADE-DATE |
Date |
MM/DD/YYYY |
AHA-A-RADE-ROSTER |
Multiselect |
See Appendix B: Roster |
AHA-A-RADE-RISK1-5 |
Multiselect (5) |
•Bold indicates primary category. Use the jurisdictional risk assessment to select the top 5 ranked risks or hazards
•Biological = agricultural disease outbreak, Anthrax, foodborne disease, food insecurity, or famine, infectious diseases (Ebola, smallpox, novel diseases, etc.), non-infectious diseases, pandemic COVID, pandemic influenza, respiratory viruses (SARS, etc.), vector-borne diseases, or zoonotic diseases •Community resources or utility failures = electrical outage, fuel shortage, generator shortage, sewer failure, supply chain disruption (water, food, pharmaceuticals, etc.), or utilities disruption •Environmental = chemical attack, spill, or release; hazardous materials incident or release; nuclear facility failure; radiological dispersal; or water sanitation, supply contamination, or shortage •Mass gathering = large public events; mass care services; mass sheltering; medical resource shortages; special or VIP events; or volunteer or staffing shortages •Natural disaster = asteroids or meteorites; avalanches; droughts; dust storms; earthquakes; expansive soils; extreme cold; extreme heat; floods; fogs, hailstorms, hurricanes, tropical storms, or cyclones; ice storms; landslides; lightning; mudflows; sinkholes or subsidence; snowstorms or blizzards; soil erosion; solar flare; storm surge; thunderstorms; tornadoes; tsunamis; volcanoes; wildfires; or windstorms •Occupational safety or industrial hygiene = agricultural infestation; arboviral response; factory incident; mining incident; power plants; refinery incident; or safety standard issues • Structural failure = dam failure; infrastructure collapse (bridges, buildings, etc.); levee failure •Technological (failures or disruptions); communication network disruptions or failures; cyber-attacks; or information systems disruptions or failures •Terrorism or violence threats (including explosives) = agro-terrorism or food supply contamination; CBRNE attack (chemical, biological, radiological, nuclear and explosive); hate crimes; hostage situations; kidnapping; mass shootings or active shooter; riots; weapons of mass destruction; or workplace violence •Transportation = aviation; highways; maritime; or railroads •Other, specify |
AHA-A-REASON1-5 |
Multiselect |
Access to medications; chemical exposure; chronic disease management; communication challenges (mis/dis-information); displacement or homelessness; environmental health concerns; first responder health; food and waterborne disease; healthcare system surge needs; infectious disease; injuries and trauma; mental health / psychological distress; radiation exposure; respiratory problems; social disruption; other, specify |
AHA-A-RADE-EXPERTS |
Multiselect |
• Accountant |
AHA-RADE-AFN |
Multiselect |
•Children
and youth |
AHA-A-RADE-SVI |
Select |
Yes; No |
AHA-A-RADE-PLACES |
Select |
Yes; No |
AHA-A-RADE-emPOWER |
Select |
Yes; No |
AHA-B-MYIPP-SUBMIT |
Select |
Not started; in progress; complete; deferred |
AHA-B-MYIPP-DATE |
Date |
MM/DD/YYYY |
AHA-B-MYIPP-IPPW-DATE |
Date |
MM/DD/YYYY |
AHA-B-MYIPP-ROSTER |
Multiselect |
See Appendix B: Roster |
AHA-B-MYIPP-YEARS |
Number |
Enter number |
AHA-B-MYIPP-RRF |
Multiselect |
Administrative and budget preparedness activities (ADM); all-hazards activities (AHA); data modernization activities (DM); health equity activity (HE); local support activities (LOC); partnerships activity (PAR); public health laboratory capacity activities (LAB); recovery activity (REC); risk communications activities (RSK); workforce activities (WKF) |
AHA-B-MYIPP-CAPS |
Multiselect |
Capability 1:Community Preparedness; Capability 2: Community Recovery; Capability 3: Emergency Operations Coordination; Capability 4: Emergency Public Information and Warning; Capability 5: Fatality Management; Capability 6: Information Sharing; Capability 7: Mass Care; Capability 8: Medical Countermeasure Dispensing and Administration; Capability 9: Medical Materiel Management and Distribution; Capability 10: Medical Surge; Capability 11: Nonpharmaceutical Interventions; Capability 12: Public Health Laboratory Testing; Capability 13: Public Health Surveillance and Epidemiological Investigation; Capability 14: Responder Safety and Health; Capability 15: Volunteer Management |
AHA-B-MYIPP-EX |
Multiselect |
see Appendix D |
AHA-B-MYIPP-EXSTRENGTH |
Text/Multiselect |
Open-ended; as exercise data is entered it will populate a dropdown menu to facilitate future data entry |
AHA-B-MYIPP-STRENGTH |
Text/Multiselect |
Open-ended; as exercise data is entered it will populate a dropdown menu to facilitate future data entry |
AHA-B-MYIPP-EXAOI |
Text/Multiselect |
Open-ended; as exercise data is entered it will populate a dropdown menu to facilitate future data entry |
AHA-B-MYIPP-AOI |
Text/Multiselect |
Open-ended; as exercise data is entered it will populate a dropdown menu to facilitate future data entry |
AHA-B-MYIPP-PANFLU |
Date |
MM/DD/YYYY |
AHA-B-MYIPP-AHA |
Date |
MM/DD/YYYY |
AHA-B-MYIPP-ID |
Date |
MM/DD/YYYY |
AHA-B-MYIPP-MCM |
Date |
MM/DD/YYYY |
AHA-B-MYIPP-COOP |
Date |
MM/DD/YYYY |
AHA-B-MYIPP-VOL |
Date |
MM/DD/YYYY |
AHA-B-MYIPP-CERC |
Date |
MM/DD/YYYY |
AHA-B-MYIPP-HC |
Date |
MM/DD/YYYY |
AHA-C-Exercises |
Select |
Not started; in progress; complete; deferred; see exercise requirements (see Appendix D). |
AHA-D-RESPONSE-NAME |
Text |
Open-ended |
AHA-D-RESPONSE-START-DATE |
Date |
MM/DD/YYYY |
AHA-D-RESPONSE-END-DATE |
Date |
MM/DD/YYYY |
AHA-D-RESPONSE-CATEGORY |
Select One |
•Bold indicates primary category. Once selected, subset options display.
•Biological = agricultural disease outbreak, Anthrax, foodborne disease, food insecurity, or famine, infectious diseases (Ebola, smallpox, novel diseases, etc.), non-infectious diseases, pandemic COVID, pandemic influenza, respiratory viruses (SARS, etc.), vector-borne diseases, or zoonotic diseases •Community resources or utility failures = electrical outage, fuel shortage, generator shortage, sewer failure, supply chain disruption (water, food, pharmaceuticals, etc.), or utilities disruption •Environmental = chemical attack, spill, or release; hazardous materials incident or release; nuclear facility failure; radiological dispersal; or water sanitation, supply contamination, or shortage •Mass gathering = large public events; mass care services; mass sheltering; medical resource shortages; special or VIP events; or volunteer or staffing shortages •Natural disaster = asteroids or meteorites; avalanches; droughts; dust storms; earthquakes; expansive soils; extreme cold; extreme heat; floods; fogs, hailstorms, hurricanes, tropical storms, or cyclones; ice storms; landslides; lightning; mudflows; sinkholes or subsidence; snowstorms or blizzards; soil erosion; solar flare; storm surge; thunderstorms; tornadoes; tsunamis; volcanoes; wildfires; or windstorms •Occupational safety or industrial hygiene = agricultural infestation; arboviral response; factory incident; mining incident; power plants; refinery incident; or safety standard issues • Structural failure = dam failure; infrastructure collapse (bridges, buildings, etc.); levee failure •Technological (failures or disruptions); communication network disruptions or failures; cyber-attacks; or information systems disruptions or failures •Terrorism or violence threats (including explosives) = agro-terrorism or food supply contamination; CBRNE attack (chemical, biological, radiological, nuclear and explosive); hate crimes; hostage situations; kidnapping; mass shootings or active shooter; riots; weapons of mass destruction; or workplace violence •Transportation = aviation; highways; maritime; or railroads •Other, specify |
AHA-D-RESPONSE-ROSTER |
Multiselect |
See Appendix B: Roster |
AHA-D-RESPONSE-OBJECTIVES |
Multiselect |
Multiselect or specify the objectives of the response |
AHA-D-RESPONSE-STRENGTH |
Text |
Open-ended |
AHA-D-RESPONSE-AOI |
Text |
Open-ended |
AHA-D-RESPONSE-CA |
Text |
Open-ended |
AHA-D-RESPONSE-IP |
Text |
Open-ended |
AHA-E |
Date |
MM/DD/YYYY |
AHA-F |
Date |
MM/DD/YYYY |
AHA-G |
Number |
Numerator = number of staff that completed training per plan; denominator = total number of staff included in training plan. Credit for AHA-G is associated with LOC-C and WKF-B. See also Appendix F, Evaluation of Trainings and Appendix G, Monitoring and Technical Assistance. |
LAB-A-SPaSE |
Not Applicable |
Data received directly from LRN-C |
LAB-B-CHALLENGE |
Not Applicable |
Data received directly from LRN-B |
LAB-C-PROFICIENCY |
Not Applicable |
Data received directly from LRN-C |
LAB-D |
|
No data entry is required. Successfully implementing specified standards for electronic reporting of LRN-B and LRN-C laboratory data is demonstrated by completing LAB A-C (as applicable). |
LAB-E |
Date |
MM/DD/YYYY |
LAB-F |
Date |
MM/DD/YYYY |
DM-A |
Date |
MM/DD/YYYY |
DM-B-CORE |
Select One |
•Case data •Emergency department data •Health care capacity and utilization data •Immunization data •Laboratory data •Vital statistics data •Wastewater surveillance data •Other, specify
|
DM-B-BASELINE |
Text |
Open-ended |
DM-B |
Date |
MM/DD/YYYY |
DM-B-AOI |
Text |
Open-ended |
DM-B-CA |
Text |
Open-ended |
AHA-A-HE-A-RADE-ROSTER |
Multiselect |
See Appendix B: Roster |
PAR-A |
Multiselect |
See Appendix B: Roster |
RSK-A-DATE |
Date |
MM/DD/YYYY |
RSK-B |
Multiselect/Text |
Multiselect or specify the communication objectives |
RSK-C |
Not Applicable |
Credit for RSK-C is associated with WKF-C and exercise requirements (see Appendix D) |
REC-A |
Date |
MM/DD/YYYY |
HE-B |
Multiselect |
See Appendix B: Roster |
ADM-A-Date |
Date |
MM/DD/YYYY |
ADM-B |
Not Applicable |
Credit for ADM-B is associated with AHA-C (see Appendix D), AHA-G, and WKF-B; no additional data entry required. |
ADM-C-MON |
Not Applicable |
Recipients must comply with federal financial reporting |
ADM-D1-RECIPIENT |
Number |
Total number of staff on the last day of the quarter |
ADM-D2-RECIPIENT |
Number |
Number of new hires in the quarter |
ADM-D3-RECIPIENT |
Number |
Number of staff at the start of the quarter |
ADM-D1-LOCAL |
Number |
Total number of staff on the last day of the quarter |
ADM-D2-LOCAL |
Number |
Number of new hires in the quarter |
ADM-D3-LOCAL |
Number |
Number of staff at the start of the quarter |
ADM-E |
Date |
MM/DD/YYYY |
ADM-E-PROCUREMENT-DATE |
Date |
MM/DD/YYYY |
ADM-E-SUBCONTRACT-DATE |
Date |
MM/DD/YYYY |
ADM-E-90MET |
Select One |
Performed without challenges; performed with challenges; unable to perform; not applicable |
ADM-E-90BARRIERS |
Multiselect |
|
WKF-A-VACANT |
Number |
Job Classification Categories 1. Agency leadership and management: department/bureau director, deputy director, public health agency director, program director, health officer. 2. Program manager: public health program manager. 3. Business, improvement, and operations staff: attorney or legal counsel, business support: accountant/fiscal, business support services: administrator, business support services: coordinator, grants or contracts specialist, human resources personnel, other business support services, community health planner, quality improvement worker, training developer/manager, workforce development staff. May include positions focused on accreditation and performance improvement. 4. Office and administrative support staff: clerical personnel/administrative assistant; clerical personnel -secretary; customer service/support professional; custodian, other facilities or operations worker; implementation specialist, medical/vital Records staff. 5. Information technology and data system staff: information systems manager/information technology specialist, IT support staff, public health informatics specialist, informatics staff, web developer/computer programmer. 6. Public information, communications, and policy staff: public information specialist, policy analyst, communications specialist, web content writer/content developer. 7. Laboratory workers: laboratory technician, laboratory quality control worker, laboratory scientist/medical technologist, laboratory aide or assistant. 8. Epidemiologists, statisticians, data scientists, other data analysts: epidemiologist, population health specialist, statistician, economist, data or research analyst, data scientist, program evaluator. 9. Behavioral health and social services staff: behavioral health professional, disease intervention specialist/contact tracer, peer counselor, health navigator, social worker/social services professional. 10. Community health workers and health educators: health educator, community health worker. 11. Public health physician, nurse and other clinicians or healthcare providers: nursing and home health aide, nutritionist or dietitian, other oral health professional, other nurse -clinical services, physician assistant, public health dentist, health/preventive medicine physician, registered nurse: public health or community health nurse, registered nurse: unspecified, pharmacist, licensed practical or vocational nurse, nurse practitioner emergency medical technician/advanced emergency medical, technician/paramedic, emergency medical services worker, other health professional/clinical support staff, physical/occupational/rehabilitation therapist, public health veterinarian. 12. Preparedness staff: emergency preparedness/management worker. 13. Environmental health workers: environmental health worker, environmental health technician, environmental health physicist, environmental health scientist, environmental engineer. 14. Animal control and compliance/inspection staff: licensure/regulation/enforcement worker, sanitarian or inspector, animal control worker, disability claims/benefits examiner or adjudicator 15. Other, specify |
WKF-A-ADM-D |
Not Applicable |
No additional data entry required. |
WKF-B-AHA-G-DATE-PREPSTAFF |
Date |
MM/DD/YYYY |
WKF-B-DATE-SURGE |
Date |
MM/DD/YYYY |
WKF-B-LOC-B-TOTAL |
Number |
Total number of surge staff |
WKF-B- LOC-B-ROLES |
Multiselect |
See Appendix B: Roster |
WKF-C-COP |
Multiselect |
One PHEP CoP; recipient CoP; regional centers, other, specify |
WKF-C-BP |
Multiselect |
BP1: July 2024–June 2025; BP2: July 2025–June 2026; BP3: July 2026–June 2027; BP4: July 2027–June 2028; BP5: July 2028–June 2029 |
WKF-C-TOPICS |
Multiselect/Text |
HE-C: Health equity principles; LOC-A: Local planning jurisdiction support and technical assistance; RSK-C: Crisis and emergency risk communication related to preparedness, response, and recovery; WKF-C: Workforce recruitment, hiring, training, retention, or resiliency; other, specify |
WKF-C-AOI |
Text |
Open-ended |
WKF-C-CA |
Text |
Open-ended |
WKF-C-BEST-PRACTICE |
Text |
Open-ended |
LOC-A-PLANS |
Multiselect |
Local planning jurisdiction list |
LOC-A-RURAL |
Multiselect |
Local planning jurisdiction list |
LOC-A-TRIBE |
Multiselect |
Federal tribe list |
LOC-B |
Date |
MM/DD/YYYY |
LOC-C-HE-C-ROSTER |
Multiselect |
See Appendix B: Roster |
LOC-C-BP |
Select |
BP1: July 2024–June 2025; BP2: July 2025–June 2026; BP3: July 2026–June 2027; BP4: July 2027–June 2028; BP5: July 2028–June 2029 |
LOC-C-TOPICS |
Multiselect/Text |
HE-C: Health equity principles; LOC-A: Local planning jurisdiction support and technical assistance; RSK-C: Crisis and emergency risk communication related to preparedness, response, and recovery; WKF-C: Workforce recruitment, hiring, training, retention, or resiliency; other, specify |
LOC-C-AOI |
Text |
Open-ended |
LOC-C-CA |
Text |
Open-ended |
LOC-C-BEST-PRACTICE |
Text |
Open-ended |
HE-C-LOC-C-ROSTER |
Multiselect |
See Appendix B: Roster |
Appendix D: Exercise Data Elements
AHA-C: Discussion- and Operations-based Exercises |
The exercise framework aims to improve and support the need for public health agencies to exercise plans based on the jurisdiction’s prioritized risks and threats through a series of discussion- and operations-based exercises over the five-year period of performance. |
Activity |
|
Who must report |
All 62 recipients are required to conduct the exercises unless exempt as noted below.
|
Rationale |
The exercise framework is designed to promote use of common terminology, current standards of practice, and improve collaboration with emergency management, health care coalitions, other government sectors, and private industry within jurisdictional exercise programs. |
Data elements |
Each recipient must provide the following data to CDC. Data marked with “**” contributes to recipients’ performance evaluation. Additional data are collected to evaluate program impact and address national preparedness, readiness, and response. The data elements are the same for all discussion- and operations-based activities and will be linked to the corresponding exercise as listed in the activity section above.
|
Additional guidance |
See Exercise Framework Supplemental Guidance for additional detail to support planning and implementing of all exercise activities. Five central RRF program priorities must be included in all exercises:
|
How will this data be used? |
Each exercise activity is associated with a PHEP program requirement, and every exercise requirement must include at least one associated area identified for improvement. Effective improvement planning serves as an important tool throughout the integrated preparedness cycle (HSEEP 2020). Actions identified during improvement planning help strengthen a jurisdiction’s capability to plan, equip, train and exercise (HSEEP 2020). The MYIPP (see AHA-B) documents a progressive exercise approach that must be adjusted annually to reflect changes in preparedness priorities given exercises or real-world experiences. |
Target (if applicable) |
Each recipient must complete all exercises and submit required data. |
Recommended data source |
Recipients must compile data while conducting the exercise. Recipients can store data in any format that is available to them. |
Reporting frequency |
Recipients must report progress on all activities, at a minimum, on a quarterly basis. Each exercise must be completed one time during the performance period. Following are noted exceptions.
|
Appendix E: One PHEP Community of Practice (CoP)
WKF-C: ONE PHEP |
CDC will facilitate the One PHEP CoP to help meet the WKF-C activity requirement to participate in a CoP. One PHEP CoP will foster a collaborative environment for professionals and advance collective expertise in the expansive fields of public health response readiness. The objectives of the One PHEP CoP are to address gaps and common challenges in public health readiness and response by:
|
Activity |
WKF-C-ONE-PHEP-CoP: Actively engage in at least one CoP that identifies problems, solutions, and best practices in workforce recruitment, hiring, training, retention, or resiliency |
Who must report |
All recipients must participate in a community of practice and respond to annual monitoring questions. Additionally, recipients participating in the One PHEP CoP will provide information specific to One PHEP participation in baseline, quarterly, and annual surveys. |
Rationale |
Peer-to-peer learning and sharing support the capacity-building components of this cooperative agreement and help support implementation of program activities and requirements. The One PHEP CoP monitoring and evaluation will assess the degree to which the One PHEP CoP meets intended goals and objectives, including: addressing identified gaps, supporting knowledge transfer, and encouraging replication, scalability, or adaption of strategies and resources to bolster capabilities and outcomes. Additionally, this information will provide data to inform decision making for future CoP activities and capacity building initiatives. The One PHEP CoP will use an interactive platform to support a collaborative environment for participants to advance collective expertise through peer-to-peer knowledge transfer, learning, and sharing of resources and best practices. In addition to collecting survey data, information from the platform, including but not limited to participant registration, workgroup participation, and observation. Notes from work group meetings, engagements with chats, discussions, and shared information and resources will also inform the overall evaluation. |
Data elements |
Each recipient must provide the following data to CDC. Data marked with “**” contributes to recipients’ performance evaluation. Additional data are collected to evaluate program impact and address national preparedness, readiness, and response. One PHEP CoP baseline survey
One PHEP CoP quarterly survey
|
Additional guidance |
See also Training and Compliance detail in the PHEP NOFO CDC-RFA-TU-24-0137 (pages 63-64). |
How will this data be used? |
This One PHEP monitoring and evaluation plan provides a framework to monitor and evaluate the utility and feasibility of the evaluation results by:
|
Target (if applicable) |
Each recipient participating in One PHEP must submit required data requirements. |
Recommended data source |
Data should be compiled by the recipient while conducting the activity. Data can be stored in any format that is available to the recipient. |
Reporting frequency |
Progress on all activities must be reported, at minimum, on a quarterly basis. Activities with specific deadlines are noted below.
|
Appendix F: Evaluation of Trainings
AHA-G-TRAIN |
Trainings Surveys |
Activity |
AHA-G: Evaluation of trainings |
Who must report |
Participants in trainings |
Rationale |
Trainings and technical assistance are important capacity-building components of the PHEP cooperative agreement and support implementation of program activities and requirements. Evaluation of trainings will measure how well the trainings are conducted and support the advancement of readiness and response related to reporting and monitoring, implementing the RRF activities, program requirements, and addressing knowledge acquisition and transfer.
|
Data elements |
CDC collects additional data to evaluate program impact and address national preparedness, readiness, and response. CDC will send training participants a voluntary survey to measure the value of provided trainings. Responses are optional for all questions.
Training Surveys The following survey questions are applicable for instructor-led, webinar-based, and asynchronous trainings.
The following survey questions are additional for instructor-led or webinar-based trainings.
The following survey questions are applicable for asynchronous trainings.
|
Additional guidance |
Trainings are an important component of workforce development and program implementation. Evaluating and providing feedback on PHEP trainings, whether instructor-led, webinars, or asynchronous learning, help CDC ensure that training activities are focused on gaps and needs of PHEP recipients. See also Training and Compliance detail in the PHEP NOFO CDC-RFA-TU-24-0137 (pages 63-64). |
How will this data be used? |
CDC will use data to identify training gaps and needs, understand how trainings are supporting program reporting and monitoring, activity implementation, knowledge transfer and preparedness and response readiness. |
Target (if applicable) |
75% of trainees |
Recommended data source |
Data should be compiled by the recipient while conducting the activity. Data can be stored in any format that is available to the recipient. |
Reporting frequency |
Training participants will receive an initial evaluation survey following an offered training. CDC will send an additional survey to trainees who volunteer to provide feedback one to four months after an initial training. Training survey responses are voluntary. |
Appendix G: Monitoring and Technical Assistance
Strategy 1–3: Monitoring and Technical Assistance |
Technical assistance (TA) aims to support recipient’s implementation of program activities and requirements. PHEP TA resources are made available to recipients or recipients can directly requests specific TA. |
Activity |
TAS: Technical Assistance Survey TAF: Technical Assistance Feedback |
Who must report |
Recipients requesting technical assistance from CDC or recipients using CDC technical assistance tools. TAS and TAF responses are voluntary. |
Rationale |
TA and training are important capacity-building components of this cooperative agreement and supports implementation of program activities and requirements. The TAS and TAF survey and feedback tools provide a mechanism to evaluate process and the degree to which recipients are receiving timely, useful, and clear TA to implement program activities and requirements. |
Data elements |
CDC collects data to evaluate program impact and address national preparedness, readiness, and response. TAS and TAF responses are voluntary.Technical Assistance Survey (TAS)CDC will send TA recipients a voluntary survey to measure value of provided TA. Responses are optional for all questions.
Technical Assistance Feedback (TAF) CDC will send TA recipients using CDC resources will be sent a voluntary survey about the resources. Responses are optional for all questions.
|
Additional guidance |
TA is an important component of workforce development and program implementation. Evaluating and providing feedback on TA resources help CDC ensure that TA resources and activities are focused on gaps and needs of PHEP recipients and are useful for improving preparedness and response capabilities and support implementing PHEP cooperative agreement activities. CDC requests that those who use using CDC-developed TA resources provide feedback on the resources and their use. See also Training and Compliance detail in the PHEP NOFO CDC-RFA-TU-24-0137 (pages 63-64). |
How will this data be used? |
CDC will use data to assess the satisfaction, timeliness, and provision of TA to PHEP recipients by surveying two areas, the technical request process, and the specific resources. CDC will use the data to help identify gaps and improve knowledge transfer to support response readiness. TAS will assess if CDC met the needs of the requestor and identify if further TA is needed to support the request. TAF will assess how well certain tools are meeting the needs of recipients to implement PHEP activities and meet PHEP reporting and monitoring requirements. Additionally, CDC will combine this information with other data to identify gaps in PHEP resources and improvement to TA processes and resources. |
Target (if applicable) |
60% of CDC TA resource users |
Recommended data source |
Recipients should compile data while conducting the activity. Recipients can store data in any format that is available to them. |
Reporting frequency |
Recipients will receive a survey after technical assistance is delivered or a technical assistance resource is used. Additionally, CDC will ask recipients if they are willing to participate in a voluntary focus group to further clarify responses to survey and help clarify potential improvements for TA resources. Responses are voluntary. |
Appendix H: Key Terms
Acknowledgements
This document was developed by the Centers for Disease Control and Prevention (CDC), Office of Readiness and Response (ORR), Division of State and Local Readiness (DSLR). The RRF was informed by 10 work groups representing more than 100 subject matter experts from CDC, state and local jurisdictions, and national partners who identified state and local preparedness evaluation priorities and proposed new evaluation content.
Rachel Nonkin Avchen, MS, PhD Associate Director for Evaluation, DSLR
Paramjit K. Sandhu, MD, MPH Senior Advisor, Division of Readiness and Response Science
Project Team
Suzette Brown, MS
Hansol Hyon, BS
Nevin Krishna, MPH
Jessica Tomov, MPH, PhD
Other Contributors
Jennifer Buzzell, MS
Kristin C. Delea, MPH, REHS
Christine Kosmos, RN, BSN, MS
Kate Corvese Noelte, MPH
Christopher Reinold, PhD
CDC Centers, Institutes, and Offices subject matter experts
Special Thanks
Association of Public Health Laboratories
Association of State and Territorial Health Officials
Federal Emergency Management Agency
PHEP recipients and state and local preparedness subject matter experts
Public Health Accreditation Board
National Association of County and City Health Officials
U.S. Department of Health and Human Services, Office of the Assistant Secretary for Preparedness and Response
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | Sandhu, Paramjit (CDC/IOD/ORR/DRRS) |
| File Modified | 0000-00-00 |
| File Created | 2024-12-24 |
© 2026 OMB.report | Privacy Policy