Attachment 4
MMP Attach 4.doc
Medical Monitoring Project
Attachment 4
OMB: 0920-0740
Attachment 4
Interview Guide
Medical Monitoring Project
(MMP)
2006 Interview Guide
Clinical Outcomes Team
NCHSTP/DHAP-SE/BCSB
TABLE OF CONTENTS
1. MMP Rationale and Objectives 47
3. Basic Interviewer Skills 48
3.1 Establishing and Maintaining Rapport 48
3.3 Responding Empathetically 48
4. Identifying, Addressing, and Resolving Problems 49
4.1 Awareness of Respondent 50
5. Questionnaire Administration: General Guidance 51
5.2 Questionnaire Structure 51
5.3 Standard Administration 51
5.5 Additional Guidance When Using Paper Surveys 54
6. Starting the Interview with the Handheld Computer 55
6.2 Survey Information Section: Handheld Computer 55
6.3 Survey Information Section: Paper Forms 55
6.4 Ending the Survey Prematurely 56
6.5 Entering Data on Handheld Computers 56
7. Eligibility for Interview: Specific Guidance 64
8.1 Incarcerated Populations 65
9. Questionnaire Administration: Specific Guidance 65
9.5 Drug and alcohol use history 99
9.7 Assessment of Prevention Activities 102
10.2 Short Questionnaire: Specific Guidance 106
Overview
This interviewer guide is written for persons involved in the administration or supervising the administration of the questionnaire for the Medical Monitoring Project (MMP). MMP was created to monitor clinical outcomes, behaviors related to the spread of HIV, medical and social service use and needs, and quality of care among HIV-infected persons currently receiving care for HIV. The first section of this document discusses the rationale and objectives of MMP. Understanding the rationale and objectives is important because it may help you justify participation to others and thus motivate persons to join the study or to provide valid and complete information. The second section of this guide is on quality control. In this section, we introduce those areas in which you have control in collecting valid and complete data. The third section of this document is about basic interviewer skills. This section describes the set of key interviewing skills that are necessary to develop rapport with respondents, and the skills necessary to identify and address non-verbal and verbal cues that suggest miscommunication or inconsistent responses. The fourth section is about identifying, addressing, and resolving problem indicators. The fifth section of this document provides general instructions on administering the questionnaire. The sixth section of this document covers issues unique to starting the survey on the handheld computer. The seventh section discusses administering or coding responses to each of the questions in the eligibility screener. The eighth section reviews the procedures for documenting informed consent. The ninth section addresses specific issues in administering or coding responses to questions in the individual modules of the questionnaire. Lastly, the tenth, eleventh, and twelfth sections detail instructions for administering the Short and Proxy questionnaires and the Non-Response Form.
This guidance should be used in conjunction with the protocol for MMP in your area, to help you in your duties as an interviewer or supervisor for this project. The success of this project, to a very large extent, rests on you. The ability to translate data into findings that can assist in improving services for HIV-infected people and in preventing the spread of HIV are only as good as the quality and completeness of data that you collect.
1. MMP Rationale and Objectives
1.1 Rationale
The Medical Monitoring Project (MMP) will provide information about the circumstances of people living with HIV, the types of medical and social services they use and need, and the quality of the medical care they receive. The results of MMP will allow state or city health departments to plan for and improve both programs to prevent the spread of HIV and services for those who have HIV.
Data from MMP will be used, along with other data, by health departments and communities of participating states and cities to describe the needs of HIV-infected clientele when requesting funding from federal agencies and to make decisions about how to spend funding received for HIV prevention and care. At the national level, data from MMP will be useful for tracking the health of HIV-infected persons, to improve provision of treatment and prevention resources, and for measuring progress towards national prevention and treatment goals. National data will be used to document the need for prevention and treatment resources and the impact of these resources on care and treatment for people with HIV infection.
1.2 Objectives
The primary objectives of MMP are to obtain data from a national probability sample of HIV-infected persons receiving care in the U.S. to:
Describe the clinical and virologic status of these patients
Describe HIV care and support services being received and the quality of such services
Describe the prevalence and occurrence of co-morbidities related to HIV disease
Determine the prevalence of ongoing risk behaviors and access to and use of prevention services among persons living with HIV
Identify met and unmet needs for HIV care and prevention services in order to inform community and care planning groups, health care providers and other stakeholders
2. Quality Control
The collection of high-quality interview data is crucial for meeting the MMP objectives. The quality of data obtained from this project is largely dependent on you!
Not everyone can be an effective interviewer. You were selected because you were perceived to have traits that are fundamental for being a good interviewer for this project. These traits include:
Being people-oriented and responsive to others.
Relating easily with a wide variety of people of different demographic and social backgrounds, personalities, and sexual orientations.
Being comfortable with your own sexuality and feelings regarding illegal drug use and HIV/AIDS.
Being detail oriented, organized, and methodical.
Having a desire to contribute to expanding the knowledge of HIV prevention and care at the local and national level.
The following are some important strategies that help interviewers obtain data that is of high quality: (1) establishing and maintaining rapport with respondents; (2) appropriately identifying, addressing, and resolving both verbal and nonverbal problem indicators; (3) administering the questionnaire in a standard way, yet tailoring it to the respondent as instructed; (4) translating the underlying intentions of specific measures, if necessary; and (5) reviewing the questionnaire for errors, and identifying and correcting those errors which can be corrected. Each of these critical quality-control topics is discussed in the following sections.
3. Basic Interviewer Skills
3.1 Establishing and Maintaining Rapport
The more comfortable the respondent is with you, the more likely she/he will provide honest and complete answers. You establish rapport when the respondent perceives you as a nonjudgmental, understanding and caring person. To establish rapport, it is also helpful to have a warm and engaging introduction, a comfortable interview environment, and appropriate use of body language and humor.
To establish rapport, first be aware of your own feelings and the nonverbal and verbal signals you may send to respondents. Before your interviews, take a moment and check in with yourself on the following questions:
1. Are you feeling and looking relaxed?
2. Is your body language open or closed?
3. Are you angry or upset about something or someone? Can your appearance be interpreted as stern, inflexible, or self-righteous?
4. Do you appear as if you enjoy and value your work?
Over the course of a long survey, it is difficult to always be your best when interviewing respondents. After recognizing your feelings and the signals you may give on a particular day or interview, minimize those verbal and non-verbal signals that can be perceived as judgmental, disinterested, or non-caring. If you cannot effectively minimize these signals, please do not administer the questionnaire.
3.2 Introduction
The most important time in which to influence a successful interview may be the time when you first introduce yourself to the respondent. During the introduction, demonstrate interest and appreciation for their participation.
3.3 Responding Empathetically
Some of the questions that you ask during the interview may cause respondents to recall difficult experiences in their lifetimes. Be prepared to respond appropriately to these disclosures and the range of feelings that might accompany them. Allow time for the respondent to work through the disclosure and respond empathetically if appropriate. Being empathic (showing empathy) means understanding and appreciating the respondent’s feelings and personal situation; this is not to be confused with feeling sorry for someone. This is an important foundation on which to build rapport. As much as your personal experience might allow, demonstrate empathy verbally and non-verbally during your interactions. Be aware that even an empathetic statement may undermine rapport if not conveyed sincerely.
3.4 Humor
Humor can bring relief to tense situations and can give a sense of perspective by showing that you don’t take yourself too seriously. Within reason and personal comfort, use humor to help put nervous respondents at ease, and use it to help you cope with your work! However, do not overuse humor as it can be distracting and undermine your purpose. Use your best judgment when applying humor to build rapport.
3.5 Closure
Close the interview with the same attention and commitment to your client as you demonstrated during the introduction. Be gracious for their time and participation. Be sure to attend to their needs, including providing information about follow-up health care or other services, if appropriate, as directed by your supervisor. Remember that even though the respondent may have seen you only once, you might be the only person to whom she/he ever disclosed certain experiences or emotional states that warrant follow-up and possible intervention.
3.6 Staff Conduct
Do not try to be the participant's best friend. By maintaining a professional yet friendly demeanor you will help complete the interview in a timely manner and be a better representative of the project and your agency. Some “small talk” at start and closure are useful rapport builders; but to the greatest extent possible, outside the administration of the interview, you should be mostly listening and not speaking. Do not make inappropriate disclosures that could appear unprofessional. Examples of inappropriate disclosures might include the sharing of personal experiences of a sexual or drug taking nature. Contrast “yes, I know always using a condom can be hard” (OK) with “yes, I haven't used any condoms with my last 2 partners either” (not OK).
Staff working on MMP should abide by their state/local HIV/AIDS surveillance security and confidentiality requirements and guidelines. In addition, the following are guidelines for conduct:
• Do not come to work under the influence of alcohol or drugs
• Do not have sex with participants during the project period (January 2005-December 2005)
• Do not use drugs with, sell drugs to, or buy drugs from participants during the project period (January 2005-December 2005)
• All participant incentives for the project must be accounted for; the interviewer is responsible for the appropriate distribution of incentives and the return of undistributed incentives to the state/local project site
These guidelines apply not only to staff conducting interviews, but to all other staff working on the project. If a staff member believes that these guidelines or state/local guidelines have been breached, this should be reported to their supervisor or principal investigator.
4. Identifying, Addressing, and Resolving Problems
For each interview you must ensure that you interpret the questionnaire accurately and that respondents provide reasonably consistent responses. Therefore, interviewers must be able to identify an indication that there may be a problem (“problem indicator”) then address and resolve problems; this is a critical ongoing priority for obtaining high-quality data. In this context, problem indicators are either non-verbal or verbal cues given by respondents that suggest confusion or misunderstanding, inconsistent or incomplete disclosures, or other problems (stress, fear, impatience, anger, etc.).
Because even simple ordinary speech is frequently misunderstood, and because the language in the questionnaire is frequently technical and may be demanding (e.g., may ask the respondent to recall events), you must always consider the possibility that the respondent may not fully understand a question. In addition, some respondents may be troubled by the content of some questions, and some may withhold information on purpose. To obtain useful data, you must be an attentive observer and listener in order to recognize these problem indicators, and you must “think on your feet” to address them. Falling into a “habit,” and administering the questionnaire in a rote, mechanistic, and non-thinking manner will keep you from picking up and responding to these cues. It is important to stay alert!
4.1 Awareness of Respondent
Be observant about the respondent’s behavior and apparent level of comfort throughout the interview. Stay tuned to their facial expressions, tone and speed of voice and posture, and recognize potentially problematic non-verbal and verbal signals. If a respondent exhibits anxiety or disinterest, temporarily stop the interview and explore her/his reactions. Section breaks within the instrument offer good opportunities to stop and assess these problematic reactions.
Another factor in being aware of the respondent’s signals is that they may not be able to complete the interview and provide high quality data. If a participant appears to be intoxicated or under the influence of drugs, the interviewer should terminate the survey as soon as possible and make a note in the comments that the interviewer determined that the respondent was not able to complete the interview. The respondent should be compensated and thanked for his/her time.
Similarly, if you believe the respondent is not telling the truth about some of the questions, you should make a note to that effect in the interviewer comments. If the respondent consistently gives what you believe are inaccurate or untruthful answers, the interview should be stopped and a note put in the interviewer comments to that effect. The respondent should be compensated and thanked for his/her time.
4.2 Active Listening
To listen actively, periodically paraphrase key respondent responses to ensure accurate communication and to inform respondents that you are attentive. Paraphrasing involves using different words to say what the respondent already said. Responding with "It sounds like..." or "I hear that..." are frequently used active-listening transition statements. After these statements it is good to also ask “Is that right?” or words to that effect, to encourage the respondent to correct your information if needed. For example:
Respondent: “I’m not sure. I have had lots of sex partners; it’s going to be hard to give you an exact number.”
Interviewer: “Ok, it sounds like it may be difficult. Take your time to think about it.”
Although active listening is important to fully understand respondents’ answers, it should not be used as a means to suggest a response or to help a respondent choose a particular answer. Some kinds of questions used in ordinary conversations must be avoided because they suggest answers. For example:
DON’T ASK: “Do you mean A or B?” This is not neutral because it suggests two possible answers and there may be others that do not occur to you as the interviewer but may be appropriate to the respondent if left to choose on his/her own.
DON’T ASK: “Do you mean (such and such)?” because many people tend to say “Yes” to any suggestion, either because it’s easy or because they think it is the “right” answer.
DON’T ASK: “Then you feel (such and such)?” Even though you think you’re summarizing what the respondent has already said, your interpretation may be correct but you may be placing the emphasis in the wrong direction.
4.3 Responding to Problems
When checking in with respondents, acknowledge your observation (e.g., “You seemed hesitant to answer that question..”), explore and clarify concerns (e.g., “Are you concerned about what will happen to your answers?”), and respond appropriately (“We protect your information in many ways....”). Interviewers may find that assuming someone's mood, disposition or attitude may result in anger, alienation, and/or termination of the interview. It places the interviewer in a very precarious position. If this client suffers from an anxiety disorder, the comment may be interpreted as confrontational, no matter how mildly and politely it was intended. Other options for obtaining a subjects response to a question might include “Do you have any concerns about this question” or “Can I help clarify anything?” It might be better to help open the conversation by seeking to understand the client's discomfort. Certainly, verbal and non-verbal problem indicators have many causes over which the interviewer has no control. Evaluate whether the cause might be attributed to the interview process or uncertainty in participating in this surveillance effort. Within reason, try to understand the underlying issues and respond appropriately. When needed, reassure the respondent that:
S/he is a participant in and not just the subject of MMP.
We are interested in learning about her/his experiences, perceptions, and opinions. That is, we believe that her/his experiences are valuable and important for HIV prevention and improving the quality of care: "We hope you can help us understand"..."We want to hear what you think"... etc.
We are also interested in the variety of experiences and opinions s/he has. We do not want to come across as prying. We want to approach the respondent in a way that he/she doesn’t censor his/her own responses.
5. Questionnaire Administration: General Guidance
5.1 Administrative Issues
Prior to administering the interview, complete required activities and cover important administrative issues. These activities and discussions include obtaining consent for the interview, which ensures that the respondent understands the project, and discussing the amount of time required for the interview, confidentiality protections, reimbursement, and other concerns or questions the respondent may have. Remember to make the respondent feel as comfortable as possible and ensure her/his basic needs are met (bathroom, etc.) Explain to the respondent that s/he can ask questions at any time. Remember, these pre-interview discussions are important opportunities to establish rapport and facilitate successful interviews. As you enter these interactions, be aware of your own mood and the mood and manner of your client.
5.2 Questionnaire Structure
The questionnaire is divided into six core modules, each of which cover a particular domain (demographics, access to health care, unmet needs, sexual behavior, drug and alcohol use history, and interview completion) and two optional modules (health and well-being and assessment of prevention activities.) Within each section is a list of questions for that particular module. These section headings are to help guide you through the instrument but are not indicated to the respondent.
Instructions to respondents are written in regular font, typically enclosed in boxes and beginning with the instruction “SAY”; questions are in regular font; and instructions to you (the interviewer) are in bold, italics, and typically enclosed within brackets or boxes. Not all questions are intended to be asked of all respondents. On the paper version, instructions to skip particular questions are positioned either next to responses, at the top of some questions, or at the bottom of the page or question; on the computer, the skips are automatic.
5.3 Standard Administration
Administering the questionnaire in a standard way is critical for collecting high-quality data that can be combined and analyzed from all interviewers and sites. Please follow the instructions below. This is imperative in order to assure that all interviewers administer the questionnaire in the same manner.
1. Ask all applicable questions within each section in numeric sequence. Do not ask questions out of sequence unless you are instructed to do so.
2. Read clearly and exactly as written all respondent-instruction statements (in regular font within boxes) that head sections or are interspersed throughout the questionnaire. Most sections begin with one or two sentences that begin with "SAY: ...." These important sentences are included in the questionnaire to help the respondent make the transition to a different topic. NOTE: While you may have read these instructions numerous times, this is the respondents’ first time hearing them. Therefore, do not rush through these instructions. After reading the instructions, check in with the respondent to ensure they understand what you’ve just read.
3. Read each question completely.
4. Read each question in a comfortable style and at an appropriate speed, maintaining eye-contact. Maintaining eye contact is important so that you can stay connected with the respondent, demonstrate interest and empathy, and evaluate and respond to problem indicators.
5. When instructed in the questionnaire, read the entire set of responses for specific questions. ‘Read required response’ instructions are positioned under specific questions and identify which responses are to be read. Even if a respondent selects a response before all possible choices have been read, take time to read all response options. The only exception is if a respondent “never” engaged in a particular behavior, “didn’t use” a particular substance, or “didn’t go” to a particular place; then the remaining frequency options are not read.
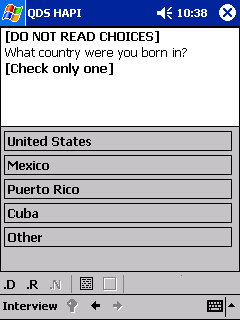
6. Do not read responses unless specifically instructed. When responses are not to be read, instructions are positioned under those specific questions.
7. When instructed, use standard response cards for specific questions. Prior to use, routinely orient all respondents on how to use the response cards. Response cards should be made of sturdy material, preferably laminated, and include the set of responses for only one question (i.e., one response card per question). The set of response cards should be readily available. Be sure to pause in order to give the respondent time to review the response card.
8. When instructed in the questionnaire, assist respondents in recalling specific events. Respondents will have to recall sexual and drug use behaviors in a 12-month period preceding the interview and prevention activities in which they might have been involved in the 12-month period preceding the interview. These different recall periods and particular events place considerable recall demand on respondents. It is very important that you pause and ensure the respondent understands the recall period or particular event in question.
9. If a respondent’s injection of a particular drug during the past 12 months was sporadic (e.g., they had used but stopped several months ago; they had stopped but have recently restarted; on some days/weeks they injected more frequently then others, etc.), have them pick one of the response options they think best characterizes their use.
In some cases, it may be acceptable to use slang or every day language, in addition to or in place of our more technical terms. For example, some local terms about drugs and drug use may be used to help the respondent understand the question better. Also, some sexual behavior vernacular may also be used to help translate our technically-defined behaviors.
5.4 Recording Responses
When using the handheld computer, responses are recorded by using the stylus to click on the appropriate response on the handheld screen. In addition, responses to structured questions are formatted in different ways. Thus, you will record responses by either checking designated response boxes or recording answers in defined (e.g., number of partners) or open-ended fields (e.g., reason why respondent didn’t seek HIV care soon after diagnosis). Please familiarize yourself with how responses are coded for particular questions, and please be careful in recording responses. Filling out the questionnaire will become second nature to you, and you will want to make the interview as brief as possible for the respondent. However, rushing through the questionnaire produces careless errors, which will be returned to you for correction. Please follow the guidance below in coding responses.
1. When to code. The only time an interviewer will leave all responses for a question blank is if the question has not been asked (e.g., when it falls under a skip pattern).
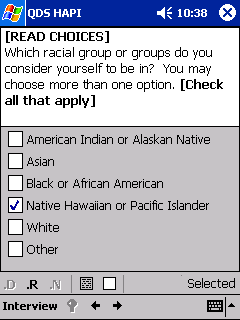
2. Single or multiple responses. Most questions will require you to code only one response; however, several questions will require you to code multiple responses. Single-response questions typically do not have interviewer instructions; however, in some instances you will be instructed to “read choices” and check only one response. Multiple-response questions will have an instruction telling you to “check all that apply.”
3. Other responses. Some questions have an “Other” response option which you can use to record responses that haven’t already been provided. A line is provided next to “Other” for you to clearly record, verbatim, the respondent’s answer. However, check to see if the answer fits a structured response before marking “Other.” Reserve “Other” for responses that are not equivalent to those which are already provided. If you are unsure if a response is equivalent, make appropriate notes in the interviewer notes (computer) or margin (paper) so that your field supervisor can make a determination.
4. Open-ended questions. A few questions are open-ended and do not have structured responses. As with “Other,” clearly record the respondent’s answers verbatim on the space provided. When needed, ask questions that will help the respondent clarify their answer, but be careful not to lead the respondent (see examples in section 4.2). Again, if a respondent’s answer to an open-ended question is not explicit, ask a clarifying question and then clearly record exactly what the respondent said. Code the response that most closely matches the answer from the list provided. If you are using the handheld computer, it will automatically display the open-ended response and instruct you to code the response from the list. Do not read the list of coding options to the respondent.
5. Unknown responses. There may be times when a respondent does not know the answer to a question. Many structured questions include a “Don’t Know” response. Please code these responses only when absolutely necessary. Before coding “Don’t Know,” probe to see if you can code part or all of the answer (e.g., date of most recent HIV test). However, do not lead the respondent to a particular answer. An unknown answer is always better than a contrived answer. All unknown responses are coded as “??” or “.D” in the handheld computer or some combination of a “9” (e.g., “09”, “99”, etc.) on the paper form.
6. Refused responses. Nearly all questions have a “refused response” option. Use your judgment about whether to probe when a respondent refuses to answer a particular question. All refused responses are coded as “.R” when administered using the handheld computer or some combination of a “7" (e.g., “07”, “77”, etc.) on the paper form.
If for some reason you are unable to code a confusing response, record information about the response you received in the interviewer notes (computer) or margin (paper). This information can be used by the coordinator later to help you come to a decision regarding the coding of a confusing response.
5.5 Additional Guidance When Using Paper Surveys
1. When using the paper interview, some questions must be read using responses obtained from previous questions. For example, you will ask about specific behaviors with partners in the last 12 months. When reading these questions, you must recall and use the number of partners reported in a previous question. Be sure to know those responses that you’ll need to memorize and use for subsequent questions.
2. When using the paper interview, familiarize yourself with the designated skip patterns within each section and skip to appropriate questions when instructed. Failing to skip particular questions or inappropriately skipping questions are common but preventable errors. If you accidentally skip a section during an interview, return to that section and administer it.
3. When using the paper version of the questionnaire, be sure to mark a response from the list given for structured questions; only write in responses for open-ended questions, for which no response categories are provided.
4. Unreadable handwriting (e.g., 4’s that look like 9’s) and misplaced checkmarks that overlap response boxes are common errors that undermine the validity of data collected on paper questionnaires. Please record responses such that they are unquestionable.
5. Following the interview, if you missed some questions, do NOT code any response and do NOT code “Don’t Know.” Even if you think a particular response would apply to the respondent, it is critical that you leave all the responses to these missed questions blank.
6. There are several questions in the Sexual Behavior and Drug and Alcohol Use History sections that have a table where the question is worded differently for one partner than for more than one partner. If the respondent only reported one partner, use the alternate wording in the right column for these questions.
PLEASE NOTE: Respondents with multiple sex partners are asked a question in the sex behavior grid about discussing HIV status with their partners before having sex. Respondents with a single sex partner are asked a version of this question later in the section about the most recent sex episode.
7. For the paper survey, two supplemental forms were created to facilitate administration of several questions in the Drug and Alcohol Use History section. Form 1 is used for Q14a-14s responses and Form 2 for Q16a-16h responses.
8. Note that the electronic files for the core interview questionnaire, optional module(s) and local questions are separate. When you must use a paper version of the survey, be sure that you have all documents and that the survey ID is filled out on the top of each of these forms.
6. Starting the Interview with the Handheld Computer
There are several components that can be included in the MMP interview file on the handheld computer:
• MMP interview questionnaire
• Optional module(s)
• Local use questions
All handheld computers will have the MMP interview questionnaire. Project areas using optional modules or local questions will have these included in the file also. Please refer to sections 6.5 through 6.x for specific guidance on data entry using the handheld computer.
6.2 Survey Information Section: Handheld Computer
Before beginning an interview, make sure that you know whether it is for your site or another MMP site, and if it is for another MMP site, that you have the appropriate ID number and Population Definition Period (PDP) start and end dates for that site. Verify that the handheld computer’s date and time is set correctly. When you first launch the survey in the handheld computer, a number of questions will appear that you need to complete. All of the information requested when you first launch the MMP survey in the handheld computer is critical. Pay close attention to the detail requested in this section. Accurately enter the information. A brief description of the items follows:
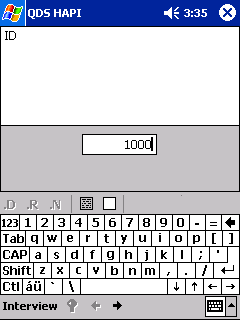
Participant ID: |
The Participant ID consists of 3 parts: a 4-digit Site ID, a 4-digit Facility ID, and a 4-digit Respondent ID. Site ID is the ID number for the MMP Site, or project area, for which the facility and respondent were selected. (Note that occasionally one MMP Site may conduct interviews for another MMP Site [e.g., Illinois conducts an interview for Indiana]. In these cases, the Site ID for interviews that are performed for another MMP Site will be different from those used at your site.)
Facility ID is the ID number for the facility from which the respondent was selected.
Respondent ID is the 4-digit code assigned to the person selected to participate in the interview. Check with your Field Supervisor if you are not sure which ID number to use for the Site, Facility, or Respondent ID components. |
Interviewer ID: |
Refers to the unique 3-digit identification number of the interviewer. The Field Supervisor will assign each interviewer an ID number to use throughout the survey period. |
Population Definition Period START date |
The PDP start date will be the same date for all interviews conducted for a specific Site or project area. (Note that occasionally one MMP Site may conduct interviews for another MMP Site. In these cases, the PDP start date for interviews that are performed for another MMP Site may be different from the date used at your site.) Enter the date provided by your Field Supervisor as the PDP start date. |
Interview Language |
Check the language (English or Spanish) for the interview. |
6.3 Survey Information Section: Paper Forms
Before beginning an interview, make sure that you know whether it is for your site or another MMP site, and if for another site, that you have the appropriate ID number and PDP start and end dates for that site. Note that some of the survey information for paper forms is located at the beginning in the ID Codes and Dates section. Follow the instructions for the fields above. There are several additional fields that must be filled in on the paper forms, which are described below. These are automatically completed by the computer so you won’t need to complete them when using the electronic version of the survey.
Population Definition Period START and END date: |
For paper interviews write the dates provided by your Field Supervisor as the PDP start and end dates. (Note that occasionally one MMP Site may conduct interviews for another MMP Site. In these cases, the PDP start and end dates for interviews that are performed for another MMP Site may be different from the dates used at your site.) |
Date of Interview: |
Write in the month, day and four-digit year for the date you conduct the interview. |
Time began: |
Write the time the interview began. Be sure to check “AM” or “PM.” |
Time ended: |
Write the time the core questionnaire was completed. |
6.4 Ending the Survey Prematurely
Situations may arise where an interviewer must end a survey before the last question in the interview is asked. Such situations may be initiated by the participant or the interviewer. For example, interviewers may end an interview early if they find the participant is “too high” to respond to the questions in the survey.
If an interviewer feels he/she needs to end the interview early, the first step is simply to end the interview verbally with the participant by thanking him/her for their time as you would at the end of the interview. Interviewers should be cautious about telling the participant that the interview is being terminated early or the reason for terminating the interview early because it may frustrate or anger the participant. Participants who begin but do not complete the survey should still be compensated when the interview is terminated.
To end a survey early on the handheld computer, the interviewer should first enter interviewer comments for the open question on the handheld computer. In the comments, the interviewer should explain the reasons the interview was prematurely ended. After entering the interviewer comments, the interviewer would then end the survey. Instructions for entering interviewer comments and ending an interview early are provided in the handheld computer basic training, which is included in the QDS manual. It is important to enter the interviewer comments before ending the survey, because the data manager will need to determine if the interview was valid prior to shipping the data to the Centers for Disease Control and Prevention (CDC).
6.5 Entering Data on Handheld Computers
This section explains the data entry and interviewing process on the handheld computers. It briefly explains the following:
1) Handling interviews on the handheld
2) Entering letters and numbers
3) QDS HAPI program basics
4) Handling the pocket pc device.
Handling interviews on the handheld:
Opening the survey:
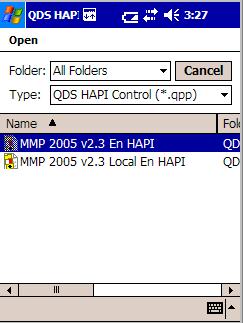
1) Go to Start ► Programs ► QDS HAPI.
2) Tap “Interview” on the lower left section of the handheld device
3) Tap on the “Begin” option here.
4) An open screen shall pop-up.
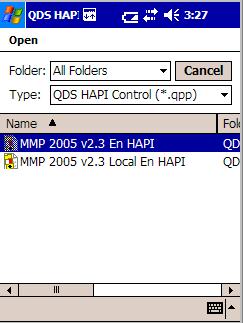
5) On this screen, tap on “MMP 2005 vXXX En HAPI”
Ending the survey:
1) Survey will automatically close at the end of the Interview Completion module.
2) DO NOT tap on the “X” in the upper right. This will not close the survey properly and the data won’t be encrypted.
3) If it is necessary to terminate the interview before it is completed, Tap “Interview” and then tap “End”
Interrupted Interviews:
If respondent needs to take a break, leave the survey open and wait for respondent, you then may need to perform the following:
If the handheld backlight has turned off after 2 minutes:
• Tap the screen to turn it back on.
• Survey will appear where you left off.
If the handheld has turned off completely after 5 minutes:
• Turn handheld on.
• Survey will appear where you left off.
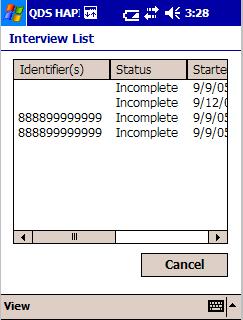
If the interview was terminated before it was completed and needs to be resumed, the following steps need to be followed:
1) Tap “Interview” on the lower left section of the handheld device, then tap “Resume”.
2) Tap on “MMP 2005 vXXX En HAPI” on the open screen that pops up.
3) An “Interview List” screen will pop-up. On this screen, tap on the incomplete interview to be loaded. A pop up box will confirm the interview being loaded.
Entering letters and numbers:
There are several ways text data can be typed into the handheld device. The Windows PocketPC 2003 consists of the following SIP’s (Soft Input Panels)
Block Recognizer
Keyboard
Letter Recognizer
Transcriber
W e
recommend the use of keyboard for entering the text data.
e
recommend the use of keyboard for entering the text data.
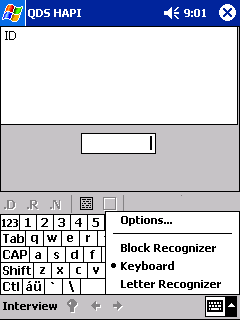
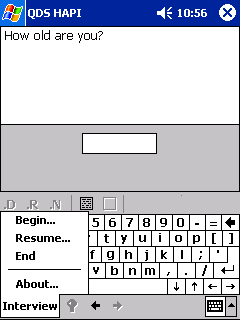
Using the keyboard SIP:
1) Tap the SIP selection area on the right bottom corner of the handheld screen to select the keyboard SIP. A small keyboard icon will appear as a block. To enable the keyboard, tap on the keyboard block. A picture of a keyboard appears on the screen.
2) Enter the letters and numbers by tapping the keyboard.
3 )
Use the Shift
and the Caps options to switch between lower and upper case for text
and between numbers and symbols.
)
Use the Shift
and the Caps options to switch between lower and upper case for text
and between numbers and symbols.
4) For more symbol options, tap the123 key in the upper left corner of the keyboard.
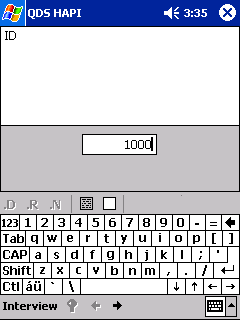
The keyboard SIP will automatically be activated while using the HAPI program when a textbox or text area has been tapped into.
III. HAPI program basics:
Reading Questionnaire Text:
I nterviewer
Instructions are in bold and/or italics and SHOULD
NOT be read to the
respondents.
nterviewer
Instructions are in bold and/or italics and SHOULD
NOT be read to the
respondents.
The interview questions appear in plain font and should be read to the respondents.
Some questions are only for the interviewers and are not meant to be asked to the respondents. These are generally preceded by the instruction “Interviewer:”
References to the show cards and special response sets are made as special instructions to the interviewers.
Moving Between Questions:
The questions and instructions in the HAPI program appear in a linear sequence. The skipping between questions follows a linear pattern and can be done only one question at a time.
• Advance to the next question by tapping the forward arrow at the bottom of the screen.
 • If an answer to
a question is required, the interviewer cannot advance without
entering an answer and the forward arrow will be grayed out.
• If an answer to
a question is required, the interviewer cannot advance without
entering an answer and the forward arrow will be grayed out.
• Go back to previous questions by tapping the back arrow at the bottom of the screen.
• When moving back to the previous questions, the HAPI will skip all instructions to the interviewer.
Entering Special Responses:
The Don’t Know (.D), Refused to Answer (.R) and Not Applicable (.N) are called the special responses for the HAPI.
Tap .D in order to enter the Don’t Know response.
Tap .R in order to enter the Refused to Answer response.
T
 ap
.N in
order to enter the Not Applicable response.
ap
.N in
order to enter the Not Applicable response.
Clearing an entry:
T
 o
clear an entry, tap on the empty box below the question area.
o
clear an entry, tap on the empty box below the question area.
T
 he
interviewer can add comments to each question by tapping on the
filled box below the question.
he
interviewer can add comments to each question by tapping on the
filled box below the question.
After entering interviewer comments, click on “ok” or “X” at the upper right to return to questionnaire.
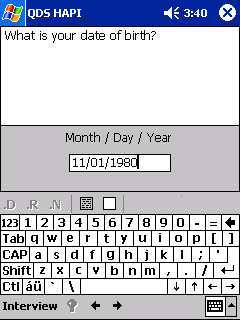
Entering Dates:
Dates always need to be in MM/DD/YYYY or MM/YYYY format.
The interviewer must enter the “/” between the numbers.
Example: November 1, 1980 would be entered as: “11”, “/”, “01”, “/”, “1980”
Most dates in the questionnaire are in a MM/YYYY format (exception: Date of Birth, PDP Start Date.)
When a respondent knows the year but not the month:
Probe to assist respondent in remembering.
If additional probing is not successful, enter the date information in this format:
“??/YYYY”
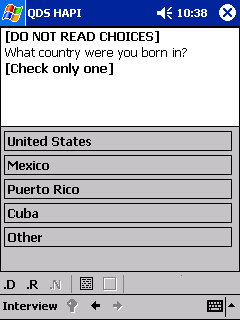
Entering Single Choice Responses:
U
 se
the stylus to tap the box that applies.
se
the stylus to tap the box that applies.
The questionnaire will automatically advance to the next question when an answer is selected.
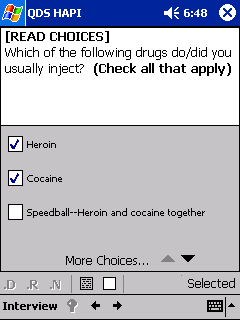
Entering Multiple Choice Responses:
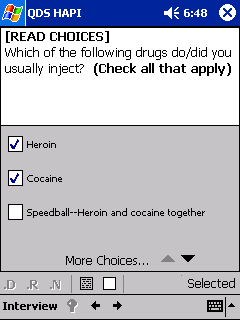
Use the stylus to tap the boxes that apply.
A
 checkmark appears in the checked box or boxes.
checkmark appears in the checked box or boxes.
The questionnaire does not automatically advance.
The interviewer must tap the forward arrow at the bottom of the page.
Some questions have a list of answers which do not fit on one screen (Indicated by the “More Choices” phrase at the bottom of the answer list).
Tap on the down arrow to the right of “More Choices” to see additional answers.
IV. Handling the Handheld Device:
Handheld Battery:
• Keep the battery charged when handheld device is not in use.
• The handhelds will come with a battery expansion pack to provide longer battery life.
• The battery has an estimated life-time of five hours.
If the battery dies you
will lose all data plus the questionnaire program!
Other Care Instructions:
• Only use the stylus with the handheld.
o Don’t use pens, pencils, other sharp objects on screen.
• To clean the handheld use soft, damp cloth moistened with water only.
• Keep the handheld away from temperature extremes and moisture/liquids.
• Do not expose handheld to direct sunlight.
• Store in protective case to keep screen from getting scratched.
• Keep the handheld secure when not in use.
7. Eligibility for Interview: Specific Guidance
The eligibility criteria to be used for all participants are the following:
Has not previously completed an interview for MMP during the survey period
Is age 18 years or older at the start of the PDP
Is able to complete interview in English or Spanish
If the patient is not able to complete the interview in English or Spanish, please note this in the interviewer comments. If possible, also note the language the patient speaks. If a translator was used or a proxy (relative or other person) responded on behalf of the patient, this should also be noted.
8. Consent Procedures
Interviewers should follow local consent protocol before administering the questionnaire to eligible respondents. Informed consent procedures are described in Chapter 9 of this guide and Appendix H of the MMP Protocol.
8.1 Incarcerated Populations
Interviewers should take additional precautions when working with incarcerated persons to prevent possible harm or coercion. Detainees may take notice of a respondent being called out for an interview and either infer the HIV status of the respondent or assume that the respondent is trading secrets for favor within the correctional facility (“snitching”). Interviewers should ensure that the respondent has the option to participate or not participate without repercussions to their care or from the administration of the correction facility, including guards. Interviewers may need to reaffirm the voluntary basis of the project with correctional staff who are assisting with recruitment and escort of prisoners.
9. Questionnaire Administration: Specific Guidance
9.1 Demographics
This section begins the questionnaire. The questionnaire is found in Appendix E of the MMP Protocol.
D1. Prior Participation in MMP
Patients may participate in MMP once during a cycle. If the respondent indicates they have previously been interviewed, even in another project area during the current cycle, they should be thanked for their time and the interview terminated (no incentive will be provided). Interviewers should be clear that the previous interview was during the current calendar year and not a previous year.
D2. Date of Birth
Enter in the respondent’s date of birth. Respondent’s date of birth should never be left blank, as this information is critical in determining eligibility for the study. Respondents who are younger than 18 years old at the start of the PDP are NOT eligible to participate. The handheld computer will calculate the age and inform the interviewer of the patient’s eligibility. Even if someone mentions date of birth that indicates that they are younger than 18, do not stop the screening process. The computer will determine their eligibility.
D2a. Age at beginning of PDP
The computer will use the respondent’s date of birth and the PDP start date to compute the respondent’s age at the beginning of the PDP. If result is less than 18 years confirm date of birth with respondent and, if correct, end the interview.
D3. Highest education
An Associate’s Degree is conferred by junior colleges. “Technical school” refers to technical training received after graduating from high school or obtaining a GED. “Any postgraduate studies” refers to education beyond a bachelor’s degree. The interviewer should interpret the answer given and read the appropriate choice back to the respondent before marking.
Bilingual interviewer: It is important to be aware that in Latin American countries there are different school systems. The labels will vary from country to country. The interviewer must avoid coding errors by probing the respondent and asking them what they mean. Here are some examples; “Bachillerato” is the name for high school level in some countries like Colombia. The term does not have a direct correspondent to the English term: “Bachelor’s degree.” In Mexico “preparatoria” is the name for “high school” and “secundaria” is the name for “junior high.” On the other hand, in some South American countries, the word” “colegio” may be used for high school. “Universidad” is the Spanish term for “College” in most countries (like Mexico, Colombia, or Puerto Rico). Younger Latino respondents may only be familiar with the US school system and the corresponding English terminology.
If the respondent’s level of education is not recorded accurately, the result may be unintended coding errors. Interviewers are encouraged to probe and clarify how many years of schooling the respondent completed beyond primary school.
D4. Ethnicity
This is the same question used on the census for determining Hispanic ethnicity. It is separate from the question about race. According to the Office of Management and Budget (OMB): The term “Hispanic” or “Latino” refers to persons who trace their origin or descent to Mexico, Puerto Rico, Cuba, Central and South America, and other Spanish cultures.
D4a. Hispanic ancestry
The term “ancestry” in this question refers to where the respondent traces his/her Hispanic or Latino origin or descent. Record the response to this question by checking all that apply. If respondent indicates a non-Hispanic ethnicity, provide him/her with a definition of what we mean by Hispanic ethnicity, i.e., origin or descent that can be traced to Mexico, Puerto Rico, Cuba, Central or South America (this includes Brazil), or other Spanish cultures.
If the respondent gives a response other than those listed, record the response in “Other (Specify).”
D5. Race
Read each racial group and check all that apply. If a respondent reports they are of mixed race, be sure each race is recorded. Responses should be read as listed and in order, conforming to OMB requirements for collection of race and ethnicity. Hispanic is NOT a race category. However, if a respondent insists their race is “Hispanic,” check “Other” and code “Hispanic” in the blank after “Other (Specify)”. In general, use the “Other” category sparingly for this question.
According to OMB, Central and South American Indians should be classified as American Indian.
D6. Country of birth
Country of birth is asked of all respondents and helps identify foreign-born respondents.
D6a. Years living in the United States
Respondents who are foreign born (including potentially non-U.S. citizens) may be concerned about this question. Care should be made to reassure the respondent of the confidentiality of their responses.
If the respondent has lived in the U.S. for less than a year, try to determine how many months the respondent has lived in the U.S.
D7. Homelessness
This question is designed to identify whether the respondent had a regular home/residence in the 12 months before the interview. Be sure to read the definition of homeless as part of the question. Homeless status refers to not having a place to stay at night. Rely on the respondent’s interpretation of their housing status.
NOTE: In this survey, “homeless” is defined (Stewart B. McKinney Act, 42 U.S.C. § 11301, et seq.) as a person who lacks a fixed, regular, and adequate night-time residence and…has a steady night time residency that is (A) a supervised publicly or privately operated shelter designed to provide temporary living accommodation…(B) an institution that provides a temporary residence for individuals intended to be institutionalized or (C) a public or private place not designed for, or ordinarily used as, a regular sleeping accommodation for human beings.” (e.g., one’s automobile, under a bridge, etc.)
A single-room occupancy (SRO) is defined as multi-unit housing for low-income persons, generally consisting of a single room and shared bath, and may also include a shared kitchen. These are typically not licensed or regulated by a government agency.
D9. Health insurance
This question serves as a screener to determine if the respondent has health insurance coverage. Interviewers should emphasize that our interest is in whether the respondent had a policy that covers medical expenses or health care services, but not if the respondent had only a single-service policy like dental, vision, or prescription drug coverage. (Prescription drug coverage is asked about in D12)
D9a. Type of health insurance coverage
This question refers to any form of comprehensive medical health insurance (does not refer to dental, life or vision insurance). This coverage can be in the respondent’s own name or they can be listed on another’s policy. For respondent clarity, the insurance of interest is coverage that would allow respondent to see a provider for care, not insurance that only would cover medication. Interviewers should be aware of any local branding (names) of government insurance programs like Medicare and Medicaid, e.g. “MediCal” in California.
D9b. Gaps in insurance coverage
Gaps in insurance coverage can affect access to health care. Gaps can include time between policies, transitions from coverage to non-coverage (or vice versa) or waiting periods for benefits. In the above situations, participants would be considered not to have had insurance coverage.
D10. Prescription drug coverage
Interviewers should be aware of local branding (names) of drug assistance programs.
D11. Income/financial support
Respondents should select the single source of the majority of their income during the past 12 months. This can include income gained from legal and illegal sources.
D12. Public assistance applied for
Emphasis should be made that this question is seeking whether the respondent applied for assistance, even if it was not received. If the application was from more than 12 months ago, “No” should be checked. Interviewers should be aware of any local branding (names) of public assistance programs.
D13. Public assistance receipt
Similar to D12, but asking if public assistance was actually received.
D14. Sex at birth
Read the question no matter how obvious gender may appear to you. This classifies their gender at birth rather than that which may be apparent today. This item is particularly critical to enter correctly as it relates to which sexual behavior questions should be completed later in the interview. Intersex/ambiguous refers to those who may have been born with a combination of male and female physiology (similar to hermaphrodite).
Bilingual interviewer: The term, “hermafrodita,” though not common, may also be used to refer to a person born with the physiology of one gender, but knows/feels to be of the other.
D15. Gender identity
It may feel awkward to read this item. If necessary you can explain to the respondent that you are required to read all questions as written, however obvious the answer might be. The computer will classify persons whose current gender identity and birth sex do not match as transgendered. While some individuals identify themselves solely as “transgender” we are attempting to collect their true gender self identity. (i.e., the male in a female-to-male [FTM] and the female in a male-to-female [MTF]).
Bilingual Interviewer comments: The term commonly used is “transgénero”.
D16. Sexual orientation
We would like to know how the respondent views him or herself in terms of sexual orientation. Sexual orientation may not reflect sexual behavior. For example, some respondents may later report having sex with someone of the same sex, but consider themselves to be heterosexual. In these situations, do not probe. Read the choices. Use the “Other” category sparingly. Only read the first three options.
9.2 Access to Health Care
A1. First positive test
Enter the date when the respondent first tested positive for HIV. Some respondents may have difficulty remembering the date of their first positive HIV test. This date may also not be the same as the most recent HIV test date since some persons with HIV infection may get tested again after their first diagnosis. Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If month is unknown, code “??/YYYY”. If both month and year are unknown code “.D” for a full “Don’t Know” response.
A5. First HIV care
It is important to know how quickly after diagnosis persons with HIV are getting into health care. For this question put the date the respondent entered into care specifically for their HIV infection. This may not necessarily have involved treatment, and might have only included assessment of the stage of their HIV infection.
A6a. Delayed first HIV care
Guidelines for the treatment of HIV infection recommend that all persons who are newly diagnosed with HIV infection be seen by a health care provider within 3 months of their initial diagnosis. The respondent may not consider their entering into care as being delayed; for these individuals explain the 3 months recommendation. Enter all reasons reported by the respondent. Do not read list of reasons.
A6b. Main reason delayed first care
Enter the primary reason from the reasons mentioned in A3a as to why respondent delayed getting into HIV care. If the respondent only reported one reason in A3a, that reason can carry forward to A3b.
A7. Last HIV care visit
When was the respondent’s most recent visit to their health care provider? Depending on when the patient interview occurs, the patient’s last HIV care visit might have occurred after the PDP. Some respondents may have difficulty remembering the date of their last provider visit. Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If month is unknown, code “??/YYYY”. If both month and year are unknown, then code “D” for a full “Don’t Know” response. Probe extensively to at least obtain the year of this visit.
A7a. Last HIV care visit > 3 months
Current guidelines recommend HIV-positive individuals see a medical provider for evaluation of their health status every 3 months. Ask the reason they have not gone to their provider in the last 3 months. Enter all reasons reported by the respondent. Do not read list of reasons.
A7b. Main reason last visit >3 months
Enter the primary reason from the reasons mentioned in A4a as to why respondent has not had a HIV care visit in the past 3 months. If the respondent only reported one reason in A4a, that reason can carry forward to A4b.
A10. CD4 test ever
Respondents may refer to the test either as a T-cell test or CD4 test. Respondents may be confused between this number and their CD4% (number of CD4 cells in proportion to all other white blood cells). The CD4 count is an absolute number ranging from 0 (for someone who has no CD4 cells) to a high of around 1400. A typical range is between 800-1200 in a healthy individual. An HIV antibody test (used to diagnose someone with HIV) is not included in this definition. Usually a CD4 test is done in conjunction with a viral load test.
A10a. First CD4 test
If respondent has difficulty in recalling the date of the first CD4 test, probe for events in their life around that time to attempt to narrow down the date. If month is unknown, code “??/YYYY”. If both month and year are unknown code “.D” for a full “Don’t Know” response. Interviewers should take care not to lead the respondent in their answers, just probe to aid recall.
A10b. First CD4 test value
Use Response Card A to have the respondent indicate the range of their first CD4 test result after learning their HIV status. However, if the patient knows his/her exact CD4 result, enter the appropriate category. Tests done prior to learning their HIV status should be excluded. Again, interviewers should take care not to lead the respondent to an answer, just give them time to remember the count.
A10c. Lowest CD4
Use the Response Card A to have the respondent indicate the range of their lowest CD4 test result after learning their HIV status. If the patient knows the exact count, enter the appropriate category. Tests done prior to learning their HIV status should be excluded. Again, interviewers should take care not to lead the respondent to an answer, preferring to just giving them time to remember the count. Lowest ever CD4 could have been anytime in the patient’s history with HIV, regardless of subsequent CD4 recovery.
A10d. Date of lowest CD4
If respondent has difficulty in recalling the date of the lowest CD4 test, probe for events in their life around that time to attempt to narrow down the date. If year is recalled, but not the month, code “??/YYYY.” If both month and year are unknown code “.D” for a full “Don’t Know” response. Interviewers should take care not to lead the respondent in their answers, just probe to aid recall.
A11. CD4 count in 12 months
Ensure respondent is clear that you are asking for the number of CD4 tests in the one year period prior to the interview date.
A11a. Most recent CD4
Use Response Card A to have the respondent indicate the range of their most recent CD4 test result. Again, interviewers should take care not to lead the respondent to an answer, just give them time to remember the count.
A12. Viral load ever
HIV viral load tests measure the number of virus copies in a square ml of blood. The range of this test can be from undetectable (typically below 50 copies depending on the type of viral load test used) to millions. HIV viral load tests are often used by clinicians to determine the viral burden of a patient and to measure the effect of treatment on virus levels. Viral load tests are typically performed after diagnosis and in regular (every 3 months is recommended) intervals after that point. Some of the tests used to determine viral load are known as a quantitative PCR or a branched chain (b)DNA test or Nucleic Acid Sequenced Based Amplification (NASBA) test.
A12a. First viral load
If respondent has difficulty in recalling the date of the first HIV viral load test, probe for events in their life around that time to attempt to narrow down the date. If month is unknown, code “??/YYYY”. If both month and year are unknown code “D” for a full “Don’t Know” response. Interviewers should take care not to lead the respondent in their answers, just probe to aid recall.
A12b. First viral load value
Use Response Card B to have the respondent indicate the range of their first HIV viral load test result after learning their HIV status. If the person knows the exact value, enter the appropriate category. Tests done prior to learning their HIV status should be excluded. Again, interviewers should take care not to lead the respondent to an answer, just give them time to remember the value.
A12c. Ever undetectable
An undetectable viral load means the quantity of virus in the blood is too small to measure. It is not an indication of not being infectious or being “cured” of HIV. This test only tells the level of free virus within the blood and does not include other HIV bearing fluids such as semen or vaginal secretions. Undetectable can be at different levels depending on the test used, typically below 50 copies/ml for a PCR or below 75 copies/ml for a bDNA.
A12d. Highest viral load
Use the Response Card B to have the respondent indicate the range of their highest HIV viral load test result after learning their HIV status. If the person knows the exact value, enter the appropriate category. Tests done prior to learning their HIV status should be excluded. Again, interviewers should take care not to lead the respondent to an answer, just give them time to remember the value. Note that this is the highest level ever.
A12e. Last date highest viral load
If respondent has difficulty in recalling the date of the last highest HIV viral load test, probe for events in their life around that time to attempt to narrow down the date. If month is unknown, code “??/YYYY”. If both month and year are unknown code “D” for a full “Don’t Know” response. Interviewers should take care not to lead the respondent in their answers, just probe to aid recall.
A13. Viral load tests in 12 months
Ensure respondent is clear that you are asking for the number of viral load tests in the one year period prior to the interview date.
A13a. Most recent viral load
Use Response Card B to have the respondent indicate the range of their most recent HIV viral load. Tests done prior to learning their HIV status should be excluded. Again, interviewers should take care not to lead the respondent to an answer, just give them time to remember the value.
A13b. Undetectable in last 12 months
An undetectable viral load means the quantity of virus in the blood is too small to measure. It is not an indication of not being infectious or being “cured” of HIV. This test only tells the level of free virus within the blood and does not include other HIV bearing fluids such as semen or vaginal secretions. Undetectable can be at different levels depending on the test used, typically below 50 copies/ml for a PCR or below 75 copies/ml for a bDNA.
A14. Source of health care
This question screens for persons who have a primary source of HIV care. Individuals who see several different providers but don’t consider any to be a main source should answer “No” to this question.
A15. Reason no usual source of health care
Respondents may have multiple reasons for not having a primary source of care for their HIV infection. Interviewers should allow time for respondents to offer all reasons for not having a usual source of care and attempt to categorize each of the answers into one of the listed choices. Interviewers should not read the list of reasons, so as not to influence respondents’ answers. Enter all that apply, fitting responses into appropriate categories in the list. If you are unsure what category a response fits into, record it under “Other.”
A16. Name of source of HIV care
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A16a. HIV care during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent received HIV related care from the facility during the PDP a follow-up question will be asked.
A16b. Number of HIV care visits during PDP
It is necessary to determine the number of times a respondent received care from a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A18a. Non-HIV care
This question refers to facilities a respondent may have attended that were the primary source of medical care, not related to HIV. NOTE: this facility could be the same facility the respondent went to for HIV related care, in which case the follow-up questions should be answered the same.
A18b. Name of source of non-HIV care
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A18c. Non-HIV care during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent received non-HIV related care from the facility during the PDP a follow-up question will be asked.
A18d. Number of non-HIV care visits during PDP
It is necessary to determine the number of times a respondent received care from a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A19a. Gynecological care
Be sure to read definition of gynecological care: pelvic exams, Pap smears or treatment for specific female conditions such as vaginal itching, pain or bleeding. Gynecological care also includes pregnancy-related care.
A19b. Gynecological care visit
This question refers to facilities a respondent may have attended that were sources of gynecological care other than the facility where HIV care is received.
A19c. Name of gynecological care
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A19d. Gynecological care during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent received gynecological care from the facility during the PDP a follow-up question will be asked.
A19e. Number of gynecological care visits during PDP
It is necessary to determine the number of times a respondent received care from a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A20. Other HIV care provider
This question attempts to identify any additional sources of HIV care the respondent may have utilized during the past 12 months. These could be occasional sources as opposed to “usual” sources captured in A10.
A20a. Name of other source of HIV care
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A20b. Care at other provider during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent received HIV-related care from the facility during the PDP a follow-up question will be asked.
A20c. Number of visits at other provider during PDP
It is necessary to determine the number of times a respondent received HIV-related care from a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A20d. Other HIV care Yes/No
If there are no other sources of care related to HIV, proceed to next question.
A20e. Name other provider
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A20f. Care at other provider during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent received HIV-related care from the facility during the PDP a follow-up question will be asked.
A20g. Number of visits at other provider during PDP
It is necessary to determine the number of times a respondent received HIV-related care from a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A20h. Other HIV care Yes/No
If there are no other sources of care related to HIV, proceed to next question.
A20i. Name other provider
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A20j. Care at other provider during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent received HIV-related care from the facility during the PDP a follow-up question will be asked.
A20k. Number of visits at other provider during PDP
It is necessary to determine the number of times a respondent received care from a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A20l. Other HIV care Yes/No
If there are no other sources of care related to HIV, proceed to next question.
A20m. Name other provider
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A20n. Care at other provider during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent received HIV-related care from the facility during the PDP a follow-up question will be asked.
A20o. Number of visits at other provider during PDP
It is necessary to determine the number of times a respondent received care from a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A21. ER visits in past 12 months
Clarify the 12 month period for respondent as needed. HIV care received though the ER does not include those for accidents or injury. This does not include visits to the ER that resulted in admittance to the hospital (captured in A18).
A22. Urgent care visits in past 12 months
Urgent care is defined as the delivery of ambulatory medical care outside of a hospital emergency department on a walk-in basis without a scheduled appointment. Urgent care centers would include private medical centers and facilities intended for episodic treatment of medical conditions and not ongoing care. Care received should have been for HIV related purposes and not related to accident or injury.
A23. Hospital admissions in past 12 months
This question seeks the total number of admittances for HIV care, not the total number of nights spent in a hospital. Do not include visits that were solely made to the ER. You may need to confirm A16 (ER visits).
A24. Hospital days
This question seeks the total number of days from the past 12 months the respondent was in the hospital for HIV care.
A24a. Hospital name
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A24b. Hospital admission during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent had an HIV-related hospital admission during the PDP a follow-up question will be asked.
A24c. Number of hospital admissions during PDP
It is necessary to determine the number of times a respondent was admitted to a hospital during the PDP in order to determine how many chances the patient had to be selected from that facility.
A24d. Other hospital Yes/No
If there are no other hospital visits related to HIV, proceed to next question.
A24e. Name other hospital
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A24f. Hospital admission during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent was admitted to a hospital for HIV-related care during the PDP a follow-up question will be asked.
A24g. Number of hospital admissions during PDP
It is necessary to determine the number of times a respondent was admitted to a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A24h. Other hospital Yes/No
If there are no other hospital admissions related to HIV, proceed to next question.
A24i. Name other hospital
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A24j. Hospital admissions during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent had an HIV-related hospital admission during the PDP a follow-up question will be asked.
A24k. Number of hospital admissions during PDP
It is necessary to determine the number of times a respondent was admitted to a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A24l. Other hospital Yes/No
If there are no other hospital admissions related to HIV, proceed to next question.
A24m. Name other hospital
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A24n. Hospital admissions during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent had an HIV-related hospital admission during the PDP a follow-up question will be asked.
A24o. Number of hospital admissions during PDP
It is necessary to determine the number of times a respondent was admitted to a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A25. Mental health facility admissions in last 12 months
Review the 12 month period as required with the respondent. Admittance to a facility refers to an inpatient facility, not solely seeing a mental health professional on an outpatient basis.
A25a. Name of mental health facility
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A25b. Mental health facility admissions during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent was admitted to a mental health facility during the PDP a follow-up question will be asked.
A25c. Number of mental health facility admissions during PDP
It is necessary to determine the number of times a respondent received care at a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A25d. Other mental health facility Yes/No
If there are no other mental health facility admissions, proceed to the next question.
A25e. Name of mental health facility
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A25f. Mental health facility admissions during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent was admitted to a mental health facility during the PDP a follow-up question will be asked.
A25g. Number of mental health facility admissions during PDP
It is necessary to determine the number of times a respondent received care at a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A25h. Other mental health facility admissions Yes/No
If there are no other mental health facility admissions related to HIV, proceed to the next question.
A25i. Name of mental health facility
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A25j. Mental health admissions during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent had a mental health admission to a facility during the PDP a follow-up question will be asked.
A25k. Number of mental health facility admissions during PDP
It is necessary to determine the number of times a respondent received care a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A25l. Other mental health facility Yes/No
If there are no other mental health facility admissions related to HIV, proceed to the next question.
A25m. Name of mental health facility
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A25n. Mental health admissions during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent had a mental health admission to a facility during the PDP a follow-up question will be asked.
A25o. Number of mental health facility admissions during PDP
It is necessary to determine the number of times a respondent received care from a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A26. Inpatient drug or alcohol treatment
A drug treatment facility can include residential communities, detoxification centers and other similar facilities. Outpatient treatment should not be included.
A26a. Name of inpatient drug or alcohol treatment facility
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A26b. Inpatient drug or alcohol treatment during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent was admitted as an inpatient to a drug or alcohol treatment facility during the PDP a follow-up question will be asked.
A26c. Number of inpatient drug of alcohol treatment facility admissions during PDP
It is necessary to determine the number of times a respondent received care from a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A26d. Other drug or alcohol treatment facility Yes/No
If there are no other inpatient drug or alcohol treatment admissions, proceed to the next question.
A26e. Name of inpatient drug or alcohol treatment facility
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, and etc.
A26f. Inpatient drug or alcohol treatment during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent was admitted as an inpatient to a drug or alcohol treatment facility during the PDP a follow-up question will be asked.
A26g. Number of inpatient drug of alcohol treatment facility admissions during PDP
It is necessary to determine the number of times a respondent received care from a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A26h. Other drug or alcohol treatment facility Yes/No
If there are no other inpatient drug or alcohol treatment admissions, proceed to the next question.
A26i. Name of inpatient drug or alcohol treatment facility
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A26j. Inpatient drug or alcohol treatment during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent was admitted as an inpatient to a drug or alcohol treatment facility during the PDP a follow-up question will be asked.
A26k. Number of inpatient drug of alcohol treatment facility admissions during PDP
It is necessary to determine the number of times a respondent received care from a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A26l. Other drug or alcohol treatment facility admissions Yes/No
If there are no other inpatient drug or alcohol treatment admissions, proceed to the next question.
A26m. Name of inpatient drug or alcohol treatment facility
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A26n. Inpatient drug or alcohol treatment during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent was admitted as an inpatient to a drug or alcohol treatment facility during the PDP a follow-up question will be asked.
A26o. Number of inpatient drug of alcohol treatment admissions during PDP
It is necessary to determine the number of times a respondent received care from a facility during the PDP in order to determine how many chances the patient had to be selected from that facility.
A27. Antiretrovirals ever
Record antiretrovirals taken for treatment of the respondent’s HIV infection and not for other conditions such as hepatitis (this includes Lamivudine which is prescribed for both conditions) or for the prevention of HIV. For the purposes of this question antiretrovirals include approved medications for the treatment of HIV including nucleoside/nucleotide analogues, non-nucleoside analogues, protease inhibitors, and fusion inhibitors. Naturopathic or eastern medicinal treatments that are not FDA approved for the treatment of HIV infection should not be included. Immune boosting treatments such as Hydroxyurea and IL-2 should not be included.
A27a. Antiretrovirals never
Many individuals choose to delay or avoid treatment of their HIV infection for various reasons. Give time for the respondent to give as many reasons for non-use of ART. Probes should be limited to, “Is there anything else?” so as not to influence respondents’ answers.
A27b. Main reason antiretrovirals never
The handheld computer will present a list of reasons mentioned in A21a. The interviewer should record the one main reason that the respondent has never taken ART.
A28. First ART use
If respondent has difficulty remembering the date of first ART use, probe accordingly to obtain as much information as possible. If month is unknown, code “??/YYYY”. If both month and year are unknown code “D” for a full “Don’t Know” response. NOTE: This question is referring to date of first ART use for treatment and not any potential use of ART in post or pre-exposure prophylaxis or exclusively for prevention of mother-to-child transmission.
A29a. NRTI use ever
The interviewer should present the HIV medication chart showing all FDA approved antiretrovirals to the respondent and orient the respondent to the card. Verify that the respondent is aware of the groupings by class with a separate grouping for NRTIs and for combination pills. It is important to record the exact medications in the formulation that the respondent has taken. For instance, if a respondent has only taken AZT and 3TC in a combination pill as Combivir, only Combivir should be marked (the component drugs should only be marked if taken separately previously). Any drug that is mentioned but not found on the chart should be coded by the interviewer as “Other” and verified following the interview. Again, for these questions we are only interested in drugs being prescribed as antiretrovirals for HIV and are not including immune boosters or Eastern forms of treatment.
A29b. PI use ever
The interviewer should present the HIV medication chart showing all FDA approved antiretrovirals to the respondent and orient the respondent to the card. Verify the respondent is aware of the groupings by class with a separate grouping for protease inhibitors. Any drug that is mentioned but not found on the chart should be coded by the interviewer as “Other” and verified once in the office. Again, for these questions we are only interested in drugs being prescribed as antiretrovirals for HIV and are not including immune boosters or Eastern forms of treatment.
A29c. NNRTI use ever
The interviewer should present the HIV medication chart showing all FDA approved antiretrovirals to the respondent and orient the respondent to the card. Verify the respondent is aware of the groupings by class with a separate grouping for NNRTIs. Any drug that is mentioned but not found on the chart should be coded by the interviewer as “Other” and verified once in the office. Again, for these questions we are only interested in drugs being prescribed as antiretrovirals for HIV and are not including immune boosters or Eastern forms of treatment.
A29d. Combination medication use ever
The interviewer should present the HIV medication chart showing all FDA approved antiretrovirals to the respondent and orient the respondent to the card. Verify the respondent is aware of the groupings by class with a separate grouping for combination pills. It is important to record the exact medications in the formulation that the respondent had taken. For instance, if a respondent has only taken AZT and 3TC in a combination pill as Combivir, only Combivir should be marked (the component drugs should only be marked if taken separately previously). Any drug that is mentioned but not found on the chart should be coded by the interviewer as “Other” and verified following the interview. Again, for these questions we are only interested in drugs being prescribed as antiretrovirals for HIV and are not including immune boosters or Eastern forms of treatment.
A29e. FI use ever
The interviewer should present the HIV medication chart. Verify the respondent is aware of the groupings by class with a separate grouping for fusion inhibitors. There is only one drug in this group that is FDA approved. It is administered by subcutaneous injection. Any drug that is mentioned but not found on the chart should be coded by the interviewer as “Other” and verified once in the office. Again, for these questions we are only interested in drugs being prescribed as antiretrovirals for HIV and are not including immune boosters or Eastern forms of treatment.
A29f. Other ART medications
Some respondents may report being on drugs which are not FDA approved or have been approved too recently to have been included in the drug response card. Also some respondents may mention drugs that are currently in clinical trials. Any drug that is mentioned but not found on the chart should be coded by the interviewer as “Other” and verified once in the office.
A30. Current ART use
Record if the respondent is currently taking any ART to treat HIV. If a respondent is currently taking a “drug holiday” or a Strategic (i.e., structured or planned) Treatment Interruption (STI) with the intention to resume treatment at a later point, this question should be coded as “Yes.”
A30a. Reason not currently on antiretrovirals
Many individuals choose to delay or avoid treatment of their HIV infection for various reasons. Give time for the respondent to give as many reasons for non-use of ART. Fit each response into the appropriate category in the list. If you are unsure which category a response should be assigned to, record under “Other.” Probes should be limited to “is there anything else?” so as not to influence respondent’s answers.
A30b. Main reason not currently on antiretrovirals
The handheld computer will present a list of reasons mentioned for not currently taking ART in A25a. The interviewer should record the one main reason that the respondent is not currently taking ART.
A31. Current ART use and adherence
Respondents should be shown the antiretroviral drug response card and indicate the medications they are currently taking for treatment of their HIV infection. For each drug currently used, indicate the required dosage and frequency of dosing, and how many dose times were missed over the past 2 days. Missed would include not taking a scheduled drug or not taking the appropriate dosing required for effective treatment. For adherence questions a dose refers to a set amount of medications at a point during the day. If a medication requires a pill to be taken 4 times per day, this equals 4 doses. Record the number of missed doses over the past 2 days.
A32. Adherence last weekend
Missed would include not taking a scheduled drug or not taking the appropriate dosing required for effective treatment. For adherence questions a dose refers to a set amount of medications at a point during the day. If a medication requires a pill to be taken 4 times per day, this equals 4 doses. Interviewers should confirm if a respondent indicates never missing doses.
A33. Last missed ART dose
Missed would include not taking a scheduled drug or not taking the appropriate dosing required for effective treatment. For adherence questions a dose refers to a set amount of medications at a point during the day. If a medication requires a pill to be taken 4 times per day, this equals 4 doses. Interviewers should confirm if a respondent indicates never missing doses.
A33a. Reason for missed ART
Only responses the respondent believes were directly responsible for missing of doses should be recorded. Read all choices to the respondent. Probe during any responses of “maybe” or “might be” to see if it indeed was a reason.
A34. Adherence to dosing times
Use Response Card C to indicate how often the respondent properly followed dosing time requirements for their medications. The interviewer should not interpret for the respondent.
A35. Adherence to special instructions
Many medications have special instructions either to maximize absorption of the medication or to minimize the occurrence of side effects.
A36. Followed instructions last two days
Use Response Card C to indicate the frequency that special antiretroviral medication instructions were followed during the past 2 days.
A37. Antiretrovirals in last 12 months
This question is only asked of those who indicated they are not currently taking antiretroviral medications.
A38. Drug holidays
Drug holidays are sometimes used by patients to minimize long term side effects, to escape from treatment rituals and other reasons. For this question we are strictly asking about non-physician sanctioned drug holidays the respondent may have taken. A holiday for this question is 2 or more days in a row without medications. Physician directed plans (also known as Strategic Treatment Interruptions or STIs) are not included.
A38a. Drug holiday reasons
Record all the reasons for the most recent drug holiday from antiretroviral medicines. Do not read choices to the respondent. Fit each response into the appropriate category in the list. If you are unsure which category a response should be assigned to, record under “Other.”
A38b. Drug holiday main reason
Record the one main reason a drug holiday was taken from antiretroviral medicines.
A39. Discussed HIV resistance
HIV is resistant to a drug if it keeps multiplying rapidly while the patient is taking the drug. Changes (mutations) in the virus cause resistance. HIV mutates almost every time a new copy is made, but not every mutation causes resistance. The “wild type” virus is the most common form of HIV. Anything different from the wild type is considered a mutation.
Resistance can develop even in the presence of total compliance to a drug treatment regimen. Interviewers should not attempt to interpret the reasons for resistance or the actions the patient should take because of existing resistance.
A40. HIV resistance test
There are two types of drug resistance testing: genotypic and phenotypic. These tests are laboratory procedures used to determine whether a person’s virus is likely to be suppressed by each anti-HIV drug. Drug resistance testing requires a detectable viral load. If patients are tested while they are off ART, re-emergence of wild type virus may make the mutated virus a significant minority population, which makes it more difficult to test and detect resistant virus.
A41. PPD ever
Explain that the PPD (Mantoux test, TST) is a screening test done by pricking the skin to test for exposure to TB. A positive result is not sufficient to indicate infection with or a diagnosis of TB.
A41a. Most recent PPD
Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If month is unknown, code “??/YYYY”. If both month and year are unknown code “D” for a full “Don’t Know” response.
A41b. Positive PPD Yes/No
A reactive skin test for TB will appear raised and a certain diameter. A health care provider will take the reading within 48-72 hours of the test.
A42. TB clinic
This question seeks to know if the respondent received care from a TB clinic in the last 12 months.
A42a. TB clinic name
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A42b. Other TB clinic Yes/No
If there are no other TB clinics visited, proceed to next question.
A42c. TB clinic name
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A42d. Other TB clinic Yes/No
If there are no other TB clinics visited, proceed to next question.
A42e. TB clinic name
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A42f. Other TB clinic Yes/No
If there are no other TB clinics visited, proceed to next question.
A42g. TB clinic name
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A43. PCP
PCP, Pneumocystis carinii pneumonia or Pneumocystis jiroveci pneumonia, is a common opportunistic infection among HIV-infected persons with compromised immune systems.
A43a. First PCP diagnosis
Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If month is unknown, code “??/YYYY”. If both month and year are unknown code “D” for a full “Don’t Know” response.
A44. PCP medications
Medications could be used either to prevent or treat PCP infection. These medications may be prescribed for conditions other than PCP; the “Yes” response should be used only if the medications were used to prevent or treat PCP infection. HIV-positive patients with CD4 counts <200 should be given PCP prophylaxis in order to prevent the development of PCP. Use Response Card D to show the respondent the names of PCP medications.
A45. MAC
Mycobacterium avium complex (MAC) is an opportunistic infection that can develop in persons with HIV/AIDS. These medications may be prescribed for conditions other than MAC; the “Yes” response should be used only if the medications were used to prevent or treat MAC infection. Prophylaxis to prevent the development of MAC should be given to those with CD4 counts <50 cells/ml. Use Response Card D to show the respondent the names of MAC medications.
A46. Flu vaccine
Flu shots are administered annually to prevent serious influenza illness during the flu season. Persons with HIV are recommended to get a flu shot. Use of the nasal flu vaccine by HIV-positive persons is not recommended.
A46a. Place received flu vaccine
Where was the flu vaccine in the past 12 months received. This is asked because there are many places other than the usual sources of patient care where patients can receive their flu vaccination.
A47. Pneumovax
Pneumococcal vaccine is generally given to prevent serious infections with Streptococcus pneumoniae. This is different than the prophylaxis given to prevent PCP and/or the vaccination to prevent influenza.
A48. Pelvic Exam
Pelvic exams are done to check for signs of illness in the vagina, cervix, uterus, fallopian tubes, ovaries, sometimes the urinary bladder and rarely, the rectum. Procedures typically involve an external examination and a digital examination. Pap smears are often part of the procedure.
A48a. Most recent pelvic exam
Record the date of the most recent pelvic exam. Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If month is unknown, code “??/YYYY”. If both month and year are unknown code “D” for a full “Don’t Know” response.
A48b. Place received pelvic exam
Many patients receive pelvic exams from a provider other than the one they see for their regular HIV or non-HIV care. Read choices and check only one response.
A48c. Pap smear
Pap smears (used to check for cervical cancer) involve taking a swab to take cell samples from the cervix. It is recommended that HIV-infected women have an annual Pap smear. Clarify what a Pap smear is if the respondent is unsure.
A49. Pap smear ever
Pap smears (used to check for cervical cancer) involve taking a swab to take cell samples from the cervix. It is recommended that HIV-infected women have an annual Pap smear. Clarify again what a Pap smear is if the respondent is unsure.
A49a. Most recent Pap smear
Record the date of the most recent Pap smear. Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If month is unknown, code “??/YYYY”. If both month and year are unknown code “D” for a full “Don’t Know” response.
A50. Abnormal Pap smear ever
Abnormal Pap smears may indicate infection of the cervix (including yeast, HPV or HSV) or signs of precancerous lesions or cancer.
A50a. Follow-up for abnormal Pap smear
Check “Yes” is the patient had a follow-up exam, further testing, biopsy or treatment for their abnormal Pap smear.
A53. Hepatitis test
This question refers to a screening test for hepatitis. These test the blood for the presence of antibodies against hepatitis, components of the hepatitis virus or antigens indicating active hepatitis infection and/or infectious state.
A53a. Hepatitis test type
Clarify the hepatitis strains of interest if necessary. Hepatitis A is typically contracted through ingestion of infected fecal material. This could be from eating food prepared by someone with hepatitis A infection or else through oral-anal sexual contact. Hepatitis B is typically contracted through contact with blood or through sexual contact. Hepatitis C is most commonly contracted through injection drug use or blood transfusion. In rare cases, hepatitis C has been reported to be transmitted though sexual contact.
A54. Hepatitis diagnosed
Hepatitis infection could either have been active at the time of diagnosis or else resolved (just showed antibody markers of past infection).
A54a. Type of hepatitis diagnosed
Clarify the types of hepatitis if necessary.
A55. Hepatitis vaccinations
Vaccinations are available for Hepatitis A and B infection. For this question do not include short term preventative treatments such as gamma globulin.
A56. Type of hepatitis vaccination
Respondents often have difficulty remembering which vaccinations for hepatitis they may have gotten. Interviewers can probe by enquiring about the reason for vaccination or the number of shots received. The hepatitis A vaccine consists of 2 shots, 6 months apart. Note that the combination A & B vaccination is also a three shot series similar to the hepatitis B vaccine alone.
A56a. Reasons for no hepatitis vaccination
Respondents may have multiple reasons for not receiving hepatitis vaccinations. Allow time for respondent to give all their reasons without leading them to a specific response. Interviewers should not read options. Fit responses into appropriate categories in the list. If you are unsure what category a response fits into, record it under “Other.”
A57-58. STD tests
Provide clarification of the various sexually transmitted disease (STD) types as required and also use slang terminology for the names of the STDs as needed. Syphilis tests (such as RPR or VDRL) are blood tests.
A59. STD clinic Yes/No
We are interested in learning which STD clinics the respondent may have seen in the past 12 months. Reinforce the confidentiality of the project as needed to reassure the respondent.
A59a. STD clinic name
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A59b. Additional STD clinic
If no other STD clinics were visited, continue to Unmet Needs section.
A59c. STD clinic name
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A59d. Additional STD clinic
If no other STD clinics were visited, continue to Unmet Needs module.
A59e. STD clinic name
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
A59f. Additional STD clinic
If no other STD clinics were visited, continue to Unmet Needs module.
A59g. STD clinic name
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
9.3 Unmet Needs
These questions are designed to assess what services persons with HIV may need and what barriers may have kept them from accessing these services. Note that these questions refer to need during the past 12 months only. For each type of service, indicate whether the respondent needed the service in the past 12 months, was able to access the service in the past 12 months, and for services needed but not able to access, the main reason why. Do not read the response categories for reason not able to get this service.
N1. HIV case management
HIV case management services are a means to coordinate various aspects of care needed by persons living with HIV. These include insurance, health care, mental health, drug treatment, housing, etc.
N2. Mental heath counseling
Mental health counseling includes psychologists, social workers, counselors, therapists or psychiatric services.
N3. Social services
Credit counseling, assistance getting insurance, etc.
N4. Finding medical service
Assistance in finding a medical provider for ongoing (not urgent) care.
N5. Finding dental service
Assistance in finding a dentist. Examples could be with expertise with HIV-positive patients or accepting certain coverage.
N6. Adherence support
Includes direct therapy observation or techniques to take the prescribed dose of medicines on schedule.
N7. Home health
Home health services could be any form of home nursing, physical therapy or health care providers who provide services within a patients’ home.
N8. Chore or homemaker
Chore and homemaker services may provide cleaning, organizational and other assistance for persons unable to maintain their own home. Often these services are provided by a community-based organization.
N9. Finding shelter/housing
Services to get housing or assistance in finding temporary or long-term housing.
N10. Finding meals/food
Assistance including meal delivery, food delivery or other nutritional support.
N11. Transportation
Providing rides to medical appointments, shopping, case management or other appointments.
N12. Childcare
Day care, babysitting, nanny or other childcare services.
N13. HIV education or risk reduction
Services designed to educate on avoidance of transmission of HIV, living with HIV or mediating risks within ones life.
N14. Other
Any other services not specifically mentioned above.
9.4 Sexual Behavior
The sexual behavior section examines what kind of HIV-related sexual risks respondents are taking. As you read the questions, at times it may be helpful to use some slang words to describe sexual acts. Try not to stray from the questions as written and use interpretation only when necessary. Do your best to maintain a neutral tone throughout this section and do not show any reactions to any answers a respondent might give. NOTE: if a respondent appears confused by the terminology for oral, vaginal or anal sex, it is appropriate to further describe or substitute terms that the person understands. Interviewers and field supervisors should decide together on appropriate alternate terminology. Since some respondents may be offended by the definitions of various sex acts in the sexual behavior section, explain that not everyone uses the same language to describe the ways they have sex.
Bilingual interviewer: Be aware that some respondents may not know the terms, “oral” or “anal.” If necessary, include names of body parts in Spanish that clarify these terms: “Boca”/ “labios” ~ for oral; “Ano”/”Culo” ~ for anal. Also, if the expression “tenido sexo” needs to be clarified, use the following alternate phrases: “relaciones sexuales íntimas;” “contacto sexual.”
Male Respondent – Female Partners
S1. Female partners in last 12 months
This question begins the section for men only, and asks the respondent to indicate the total number of women with whom he has had oral, anal or vaginal sex in the 12 months preceding the interview. When necessary, help the respondent estimate the number of partners, using estimates by month or week.
S2a. Vaginal sex
This question separates the total number of female partners with whom the respondent had vaginal sex from the total number of female partners in the previous 12 months.
S2b. Unprotected vaginal sex
This question, asking about unprotected vaginal sex, is an important measure for estimating the number of partners with whom potential HIV transmission could occur. S2b should always be < S1 and S2a.
Bilingual interviewer: In addition to the term “condom,” the term “barrera” may be used when asking respondents about having sex without protection.
S2c. Anal sex
This question separates the total number of female partners with whom the respondent had anal sex from the total number of female partners in the previous 12 months.
S2d. Unprotected anal sex
This question provides information on the number of partners with whom the respondent may have had unprotected anal sex. S2d should always be ≤ S1 and S2c.
S2e. HIV status
This question specifies mutual disclosure of HIV status before initial sexual activity. Disclosures that may have occurred after first sexual contact are not counted here. If only one of the people disclosed (respondent or his partner) then the answer should be “No.”
S2f. Exchange sex
This means sexual relations or acts in exchange for money, drugs, transportation, shelter, etc. Clarify question and reassure the respondent of confidentiality as needed.
S2g. Who exchanged sex
Record the direction of exchange for all the exchange partners in the last 12 months.
S2h. Sex with most recent female partner
This question begins a series referring to the most recent episode of sex with a female partner. Make sure the respondent has time to identify the most recent sexual episode with the partner. Enter the month and year of the most recent sexual contact with that partner. If the respondent reports a date more than 12 months prior to the interview, clarify that you are asking about the past 12 months; you may need to go back to S1 (number of female sexual partners in last 12 months) if the respondent had the time period wrong and re-administer questions.
S2i. Main or casual partner
If respondent is unclear of definition of main and casual partner, reread description and clarify as needed.
S2j. Recent vaginal sex
This question determines whether the respondent engaged in vaginal sex during the most recent episode of sex.
S2k. Condom use recent vaginal sex
This question assesses the completeness of condom use during vaginal sex during the most recent sexual episode with the most recent partner. If a condom was not used at any time for vaginal sex during the most recent sexual episode, code the response as “00” (none of the time you were having sex). However, if a condom was used some of the time, or if a condom was used but broke or slipped off, code the response as “01” (part of the time). Finally, if a condom was used during the entirety of the sexual episode, code the response as “02” (the whole time). Keep in mind that female condoms meet the definition for condom use.
S2l. Recent anal sex
This question determines whether the respondent engaged in anal sex during the most recent episode of sex.
S2m. Condom use recent anal sex
This question assesses the completeness of condom use during anal sex during the most recent sexual episode with the most recent partner. If a condom was not used at any time for anal sex during the most recent sexual episode, code the response as “00” (none of the time you were having sex). However, if a condom was used some of the time, or if a condom was used but broke or slipped off, code the response as “01” (part of the time). Finally, if a condom was used during the entirety of the sexual episode, code the response as “02” (the whole time). Keep in mind that female condoms meet the definition for condom use.
S2n. Alcohol/drug use
Were drugs (not prescribed for the respondent), alcohol or both used by the respondent at the last sexual encounter? You may need to clarify that this refers to the last encounter with the most recent partner. Be sure the respondent understands we are asking whether he was using alcohol or drugs, not his partner.
S2o. Know partner’s HIV status
This question refers to the last time the respondent had sex, and asks whether the partner’s HIV status was known at the time they had sex. Do not include assumptions. Do not include status learned after the last sexual encounter. Suspicion of a partner’s serostatus or being informed about a partner’s serostatus from a third party (e.g., friend) does not count!
Bilingual Interviewer: Since there is no direct translation for “HIV status” this question asks about knowing the partner’s “HIV test results.”
S2p. Partner’s HIV status
Mark the partner’s HIV status. Do not read answer choices. Mark indeterminate if the partner’s most recent test was inconclusive.
S2q. Discussed HIV status
This question determines if HIV serostatus was discussed before the first sexual episode between the respondent and his most recent sex partner. Note that S2o asks about knowledge of partner’s status at last sex and this question refers to the first time they had sex. If HIV test results were discussed only at a time after the first sexual episode, code the response as “00” (No).
Male Respondent – Male Partners
Many questions in this section follow the pattern of the questions asked of female partners. Remember, however, that this section addresses male partners instead of female partners, so changes in question wording about partner gender should be addressed accordingly.
S3. Male partners
This question asks the respondent to indicate the total number of men with whom he has had oral or anal sex in the 12 months preceding the interview. When necessary, help the respondent estimate the number of partners, using estimates by month or week.
S4a. Anal sex
This question separates the total number of male partners with whom the respondent had anal sex from the total number of male partners in the previous 12 months.
S4b. Unprotected anal sex
This question, asking about unprotected anal sex, is an important measure for estimating the number of partners with whom potential HIV transmission could occur. S3b should always be < S3 and S4a.
S4c. HIV status
This question specifies mutual disclosure of HIV status before initial sexual activity. Disclosures that may have occurred after first sexual contact are not counted here. If only one of the people disclosed (respondent or his partner) then the answer should be “No.”
S4d. Insertive or receptive anal sex
For all the partners in the past 12 months with whom anal sex occurred, what roles were held by the respondent. Clarify using slang terminology if respondent is unclear after reading the question.
S4e. Exchange sex
This means sexual relations or acts in exchange for money, drugs, transportation, shelter, etc. Clarify question and reassure the respondent of confidentiality as needed.
S4f. Who exchanged sex
Record the direction of exchange for all the exchange partners in the last 12 months.
S4g. Sex with most recent male partner
This question begins a series referring to the most recent episode of sex with a male partner. Make sure the respondent has time to identify the most recent sexual episode with the partner. Enter the month and year of the most recent sexual contact with that partner. If the respondent reports a date more than 12 months prior to the interview, clarify that you are asking about the past 12 months; you may need to go back to S3 (number of male sexual partners in last 12 months) if the respondent had the time period wrong and re-administer questions.
S4h. Main or casual partner
If respondent is unclear of definition of main and casual partner, reread description and clarify as needed.
S4i. Recent receptive anal sex
This question begins a breakout of the type of anal sex the respondent had with his most recent sex partner on his last encounter. Verify the respondent understands by receptive in this question is as opposed to insertive anal sex. Colloquially this is known as being the “bottom.”
S4j. Condom use, recent receptive anal sex
This question assesses the completeness of condom use during anal sex during the most recent sexual episode with the most recent partner. If a condom was not used at any time for anal sex during the most recent sexual episode, code the response as “00” (none of the time you were having sex). However, if a condom was used some of the time, or if a condom was used but broke or slipped off, code the response as “01” (part of the time). Finally, if a condom was used during the entirety of the sexual episode, code the response as “02” (the whole time).
S4k. Recent insertive anal sex
This question begins a breakout of the type of anal sex the respondent had with his most recent sex partner on his last encounter. Verify the respondent understands by insertive in this question is as opposed to receptive anal sex. Colloquially this is known as being the “top.”
S4l. Condom use, recent insertive anal sex
This question assesses the completeness of condom use during anal sex during the most recent sexual episode with the most recent partner. If a condom was not used at any time for anal sex during the most recent sexual episode, code the response as “00” (none of the time you were having sex). However, if a condom was used some of the time, or if a condom was used but broke or slipped off, code the response as “01” (part of the time). Finally, if a condom was used during the entirety of the sexual episode, code the response as “02” (the whole time).
S4m. Alcohol/drug use
Were drugs (not prescribed for the respondent), alcohol or both used by the respondent at the last sexual encounter. You may need to clarify that this refers to the last encounter with the most recent partner. Be sure the respondent understands we are asking whether he was using alcohol or drugs, not his partner.
S4n. Know partner’s HIV status
This question asks about the last time the respondent had sex, and whether the partner’s HIV status was known at the time they had sex. Do not include assumptions. Do not include status learned after the last sexual encounter. Suspicion of a partner’s serostatus or being informed about a partner’s serostatus from a third party (e.g., friend) does not count!
S4o. Partner’s HIV status
Mark the partner’s HIV status. Do not read answer choices. Mark indeterminate if the partner’s most recent test was inconclusive.
S4p. Discussed HIV status
This question determines if HIV serostatus was discussed before the first sexual episode between the respondent and his most recent sex partner. Note that S2o asks about knowledge of partner’s status at last sex and this question refers to the first time they had sex. If HIV test results were discussed only at a time after the first sexual episode, code the response as “00” (No).
S5. Disclosure of same sex behavior
Non-disclosure of same sex sexual behavior may affect prevention messages a patient may receive, including from a health care provider. Interviewers should not question the respondent’s perception of their sexual orientation based on behavior.
Female Respondent – Male Partners
S6. Male partners in last 12 months
This question begins the section for women who have male partners, and asks the respondent to indicate the total number of males with whom she has had oral, anal or vaginal sex in the 12 months preceding the interview. When necessary, help the respondent estimate the number of partners by month or week.
S6a. Vaginal sex
This question separates the total number of male partners with whom the respondent had vaginal sex from the total number of male partners in the previous 12 months.
S6b. Unprotected vaginal sex
This question, asking about unprotected vaginal sex, is an important measure for estimating the number of partners with whom potential HIV transmission could occur. S6b should always be < S6 and S6a.
Bilingual interviewer: In addition to the term “condom,” the term “barrera” may be used when asking respondents about having sex without protection.
S6c. Anal sex
This question separates the total number of male partners with whom the respondent had anal sex from the total number of male partners in the previous 12 months.
S6d. Unprotected anal sex
This question provides information on the number of partners with whom the respondent may have had unprotected anal sex. S6d should always be ≤ S6 and S6c.
S6e. HIV status
This question specifies mutual disclosure of HIV status before initial sexual activity. Disclosures that may have occurred after first sexual contact are not counted here. If only one of the people disclosed (respondent or her partner) then the answer should be “No.”
S6f. Exchange sex
This means sexual relations or acts in exchange for money, drugs, transportation, shelter, etc. Clarify question and reassure the respondent of confidentiality as needed.
S6g. Who exchanged sex
Record the direction of exchange for all the exchange partners in the last 12 months.
S6h. Sex with most recent male partner
This question begins a series referring to the most recent episode of sex with a partner. Make sure the respondent has time to identify the most recent sexual episode with the partner. Enter the month and year of the most recent sexual contact with that partner. If the respondent reports a date more than 12 months prior to the interview, clarify that you are asking about the past 12 months; you may need to go back to S6 (number of male sexual partners in last 12 months) if the respondent had the time period wrong and re-administer questions.
S6i. Main or casual partner
If respondent is unclear of definition of main and casual partner, reread description and clarify as needed.
S6j. Recent vaginal sex
This question determines whether the respondent engaged in vaginal sex during the most recent episode of sex.
S6k. Condom use recent vaginal sex
This question assesses the completeness of condom use during vaginal sex during the most recent sexual episode with the most recent partner. If a condom was not used at any time for vaginal sex during the most recent sexual episode, code the response as “00” (none of the time you were having sex). However, if a condom was used some of the time, or if a condom was used but broke or slipped off, code the response as “01” (part of the time). Finally, if a condom was used during the entirety of the sexual episode, code the response as “02” (the whole time). Keep in mind that female condoms meet the definition for condom use.
S6l. Recent anal sex
This question determines whether the respondent engaged in anal sex during the most recent episode of sex.
S6m. Condom use recent anal sex
This question assesses the completeness of condom use during anal sex during the most recent sexual episode with the most recent partner. If a condom was not used at any time for anal sex during the most recent sexual episode, code the response as “00” (none of the time you were having sex). However, if a condom was used some of the time, or if a condom was used but broke or slipped off, code the response as “01” (part of the time). Finally, if a condom was used during the entirety of the sexual episode, code the response as “02” (the whole time). Keep in mind that female condoms meet the definition for condom use.
S6n. Alcohol/drug use
Were drugs (not prescribed for the respondent), alcohol or both used by the respondent at the last sexual encounter. You may need to clarify that this refers to the last encounter with the most recent partner. Be sure the respondent understands we are asking whether she was using alcohol or drugs, not her partner.
S6o. Know partner’s HIV status
This question asks about the last time the respondent had sex, and whether the partner’s HIV status was known at the time they had sex. Do not include assumptions. Do not include status learned after the last sexual encounter. Suspicion of a partner’s serostatus or being informed about a partner’s serostatus from a third party (e.g., friend) does not count!
Bilingual Interviewer: Since there is no direct translation for “HIV status” this question asks about knowing the partner’s “HIV test results.”
S6p. Partner’s HIV status
Mark the partner’s HIV status. Do not read answer choices. Mark indeterminate if the partner’s most recent test was inconclusive.
S6q. Discussed HIV status
This question determines if HIV serostatus was discussed before the first sexual episode between the respondent and her most recent sex partner. Note that S6o asks about knowledge of partner’s status at last sex and this question refers to the first time they had sex. If HIV test results were discussed only at a time after the first sexual episode, code the response as “00” (No).
Female Respondent – Female Partners
S7. Sex with female partner
This question attempts to determine if the respondent ever has had sex with another woman. Record the number of female partners from the past year. Note that types of sex are not specified. Should a respondent enquire about the lack of questions, interviewers can respond that female-female sex questions are currently under development.
S8. Disclosure of same sex behavior
Non-disclosure of same sex sexual behavior may affect prevention messages a patient may receive, including from a health care provider. Interviewers should not question the respondent’s perception of their sexual orientation based on behavior.
Transgender Respondent
This section begins a separate series of sexual behavior questions that are asked of transgender respondents. These questions ask about male partners and female partners. Note that the option of “not applicable” is found for most questions about specific types of sex; respondents should let you know when to use that response option (see the SAY box at the beginning of this section).
An assumption is made that the male partners are sex partners that have a penis; female partners are those with a vagina. Although it may seem easier to ask the respondent whether his/her sex partners had a penis or a vagina, consultation with transgender groups suggest that transgender respondents may find directly asking about body parts offensive. Therefore, the survey attempts to assess this status by asking the respondent specifically about the number of partners who are a given sex by categorizing the sexual partners into one of the following 3 groups: 1) persons who are not transgender (e.g., males who are not transgender); 2) persons who have had an operation to create the functional sexual parts of the given sex (e.g., post-operative transgender men [FTM]), or 3) persons who were born with the sexual parts associated with the sex and have not had an operation to alter the sexual parts to their desired gender (e.g., pre- or non-operative transgender women [MTF]).
For male and female respondents, the distinction between gender and sex of their sexual partners is not made because doing so would confuse most respondents. This distinction is only made for transgender respondents.
Transgender Respondent – Male Partners
S9. Male partners
This question begins a series of questions about sexual behavior with male partners for transgender respondents. This question asks for the total number of sex partners who were non-transgender men.
S10. FTM partners
This question seeks a total of post-operative transgender men (Female to Male, or FTM) the respondent had sex with in the past 12 months.
S11. MTF partners
This question seeks a total of pre- or non-operative transgender women (Male to Female, or MTF) the respondent had sex with in the past 12 months.
S12a. Vaginal sex
This question separates the total number of male partners with whom the respondent had vaginal sex from the total number of male partners in the previous 12 months.
S12b. Unprotected vaginal sex
This question, asking about unprotected vaginal sex, is an important measure for estimating the number of partners with whom potential HIV transmission could occur. S12b should always be < S12a.
Bilingual interviewer: In addition to the term “condom,” the term “barrera” may be used when asking respondents about having sex without protection.
S12c. Anal sex
This question separates the total number of male partners with whom the respondent had anal sex from the total number of male partners in the previous 12 months.
S12d. Unprotected anal sex
This question provides information on the number of partners with whom the respondent may have had unprotected anal sex. This question, asking about unprotected anal sex, is an important measure for estimating the number of partners with whom potential HIV transmission could occur. S12d should always be < S12c.
S12e. HIV status
This question specifies mutual disclosure of HIV status before initial sexual activity. Disclosures that may have occurred after first sexual contact are not counted here. If only one of the people disclosed (respondent or their partner) then the answer should be “No.”
S12f. Exchange sex
This means sexual relations or acts in exchange for money, drugs, transportation, shelter, etc. Clarify question and reassure the respondent of confidentiality as needed.
S12g. Who exchanged sex
Record the response that reflects the direction of overall with exchange partners in the last 12 months.
S12h. Sex with most recent male partner
This question begins a series referring to the most recent episode of sex with a partner. Make sure the respondent has time to identify the most recent sexual episode with the partner. Enter the month and year of the most recent sexual contact with that partner. If the respondent reports a date more than 12 months prior to the interview, clarify that you are asking about the past 12 months; you may need to go back to S9-11 (number of male sexual partners in last 12 months) if the respondent had the time period wrong and re-administer questions.
S12i. Main or casual partner
If respondent is unclear of definition of main and casual partner, reread description and clarify as needed.
S12j. Recent vaginal sex
This question determines whether the respondent engaged in vaginal sex during the most recent episode of sex.
S12k. Condom use recent vaginal sex
This question assesses the completeness of condom use during vaginal sex during the most recent sexual episode with the most recent partner. If a condom was not used at any time for vaginal sex during the most recent sexual episode, code the response as “00” (none of the time you were having sex). However, if a condom was used some of the time, or if a condom was used but broke or slipped off, code the response as “01” (part of the time). Finally, if a condom was used during the entirety of the sexual episode, code the response as “02” (the whole time). Keep in mind that female condoms meet the definition for condom use.
S12l. Recent anal sex
This question determines whether the respondent engaged in anal sex during the most recent episode of sex.
S12m. Condom use recent anal sex
This question assesses the completeness of condom use during anal sex during the most recent sexual episode with the most recent partner. If a condom was not used at any time for anal sex during the most recent sexual episode, code the response as “00” (none of the time you were having sex). However, if a condom was used some of the time, or if a condom was used but broke or slipped off, code the response as “01” (part of the time). Finally, if a condom was used during the entirety of the sexual episode, code the response as “02” (the whole time).
S12n. Alcohol/drug use
Were drugs (not prescribed for the respondent), alcohol or both used by the respondent at the last sexual encounter. You may need to clarify that this refers to the last encounter with the most recent partner. Be sure the respondent understands we are asking whether the respondent was using alcohol or drugs, not their partner.
S12o. Transgender partner
Was the respondent’s most recent male partner also transgender.
S12p. Partner MTF/FTM
Was the partner MTF or FTM.
S12q. Know partner’s HIV status
This question asks about the last time the respondent has sex and whether the partner’s HIV status was known at the time they had sex. Do not include assumptions. Do not include status learned after the last sexual encounter. Suspicion of a partner’s serostatus or being informed about a partner’s serostatus from a third party (e.g., friend) does not count!
Bilingual Interviewer: Since there is no direct translation for “HIV status” this question asks about knowing the partner’s “HIV test results.”
S12r. Partner’s HIV status
Mark the partner’s HIV status. Do not read answer choices. Mark indeterminate if the partner’s most recent test was inconclusive.
S12s. Discussed HIV status
This question determines if HIV serostatus was discussed before the first sexual episode between the respondent and their most recent sex partner. Note that S12q asks about knowledge of partner’s status at last sex and this question refers to the first time they had sex. If HIV test results were discussed only at a time after the first sexual episode, code the response as “0” (No).
Transgender Respondent – Female Partners
S13. Female partners
This question begins a series of questions about sexual behavior with female partners for transgender respondents. This question asks for the total number of sex partners who were non-transgender women.
S14. MTF partners
This question seeks a total of post-operative transgender women (Male to Female, or MTF) the respondent had sex with in the past 12 months.
S15. FTM partners
This question seeks a total of pre- or non-operative transgender men (Female to Male, or FTM) the respondent had sex with in the past 12 months.
S16a. Vaginal sex
This question separates the total number of female partners with whom the respondent had vaginal sex from the total number of female partners in the previous 12 months.
S16b. Unprotected vaginal sex
This question, asking about unprotected vaginal sex, is an important measure for estimating the number of partners with whom potential HIV transmission could occur. S16b should always be < S16a.
Bilingual interviewer: In addition to the term “condom,” the term “barrera” may be used when asking respondents about having sex without protection.
S16c. Anal sex
This question separates the total number of female partners with whom the respondent had anal sex from the total number of female partners in the previous 12 months.
S16d. Unprotected anal sex
This question provides information on the number of partners with whom the respondent may have had unprotected anal sex. S16d should always be ≤ S16c.
S16e. HIV status
This question specifies mutual disclosure of HIV status before initial sexual activity. Disclosures that may have occurred after first sexual contact are not counted here. If only one of the people disclosed (respondent or her partner) then the answer should be “No.”
S16f. Exchange sex
This means sexual relations or acts in exchange for money, drugs, transportation, shelter, etc. Clarify question and reassure the respondent of confidentiality as needed.
S16g. Who exchanged sex
Record the direction of exchange for all the exchange partners in the last 12 months.
S16h. Sex with most recent male partner
This question begins a series referring to the most recent episode of sex with a partner. Make sure the respondent has time to identify the most recent sexual episode with the partner. Enter the month and year of the most recent sexual contact with that partner. If the respondent reports a date more than 12 months prior to the interview, clarify that you are asking about the past 12 months; you may need to go back to S9-11 (number of male sexual partners in last 12 months if the respondent had the time period wrong and re-administer questions.
S16i. Main or casual partner
If respondent is unclear of definition of main and casual partner, reread description and clarify as needed.
S16j. Recent vaginal sex
This question determines whether the respondent engaged in vaginal sex during the most recent episode of sex.
S16k. Condom use recent vaginal sex
This question assesses the completeness of condom use during vaginal sex during the most recent sexual episode with the most recent partner. If a condom was not used at any time for vaginal sex during the most recent sexual episode, code the response as “00” (none of the time you were having sex). However, if a condom was used some of the time, or if a condom was used but broke or slipped off, code the response as “01” (part of the time). Finally, if a condom was used during the entirety of the sexual episode, code the response as “02” (the whole time). Keep in mind that female condoms meet the definition for condom use.
S16l. Recent anal sex
This question determines whether the respondent engaged in anal sex during the most recent episode of sex.
S16m. Condom use recent anal sex
This question assesses the completeness of condom use during anal sex during the most recent sexual episode with the most recent partner. If a condom was not used at any time for anal sex during the most recent sexual episode, code the response as “00” (none of the time you were having sex). However, if a condom was used some of the time, or if a condom was used but broke or slipped off, code the response as “01” (part of the time). Finally, if a condom was used during the entirety of the sexual episode, code the response as “02” (the whole time).
S16n. Alcohol/drug use
Were drugs (not prescribed for the respondent), alcohol or both used by the respondent at the last sexual encounter. You may need to clarify that this refers to the last encounter with the most recent partner. Be sure the respondent understands we are asking whether the respondent was using alcohol or drugs, not their partner.
S16o. Transgender partner
Was the respondent’s most recent female partner also transgender.
S16p. Partner MTF/FTM
Was the partner MTF or FTM.
S16q. Know partner’s HIV status
This question asks about the last time the respondent had sex and whether the partner’s HIV status was known at the time they had sex. Do not include assumptions. Do not include status learned after the last sexual encounter. Suspicion of a partner’s serostatus or being informed about a partner’s serostatus from a third party (e.g., friend) does not count!
Bilingual Interviewer: Since there is no direct translation for “HIV status” this question asks about knowing the partner’s “HIV test results.”
S16r. Partner’s HIV status
Mark the partner’s HIV status. Do not read answer choices. Mark indeterminate if the partner’s most recent test was inconclusive.
S16s. Discussed HIV status
This question determines if HIV serostatus was discussed before the first sexual episode between the respondent and their most recent sex partner. Note that Q16q asks about knowledge of partner’s status at last sex and this question refers to the first time they had sex. If HIV test results were discussed only at a time after the first sexual episode, code the response as “0” (No).
9.5 Drug and alcohol use history
U1. Injection drug use
This question serves as a screener for the injection drug questions. Make sure respondent understands the injections we are interested in are those not prescribed by a doctor. Probing may be required to determine the respondents’ perception of “medical purpose.” Injection could have been done by the respondent (self injection) or to the respondent (friend or “hit doctor”).
Drug use and injection terms vary by region. Be familiar with the local terminology for injection. For this question we are interested in any injection use, either into the vein directly or through injection just under the skin or in the muscle. We are interested in drugs the respondent used that were not prescribed for him/her.
Bilingual interviewer. Interviewers also should be aware of local Spanish terms for drug use and injection terms that have been gathered through formative assessment activities. For example, in the Southwestern United States, alternate expressions are used for track marks (“piquetes”), injection or “pincharse” (skin pop), or “pincharse las venas” to refer to mainlining where as “sonar las venas” is the expression used for shooting up.
U2. Date of last injection
As with previous questions, probe as needed to narrow down date of last injection if respondent is unclear of last use. Respondents whose last injection was more than 1 year prior to interview will be skipped to the non-injection drug use section.
U3. Drugs injected
This question asks about all the substances the respondent has injected in the past 12 months. Remind respondent that we are asking about injected drugs only. We will ask about non-injecting drugs later in the interview. If necessary, remind the respondent of the 12 month period. Again, this question refers to all injecting behavior, including “mainlining,” “skin popping,” or “muscling.” Although not specified, we only want to know about drugs that were not prescribed for the respondent. Use the provided Response Card G to indicate frequency.
The interviewer must ask respondent about each drug. If respondent previously indicated he/she only used a single drug (e.g., “I’ve only injected heroin”), explain that you have to ask about each drug.
If a respondent’s injection of a particular drug during the past 12 months was sporadic (e.g., they had used but stopped several months ago; they had stopped but have recently restarted; on some days/weeks they injected more frequently then others, etc.), have them pick one of the response options they think best characterizes their use.
Bilingual interviewer: Some Spanish terms included in the questionnaire are direct translations of the English terms (“piedra” or “roca” for rock or ready-rock) or the English terms themselves (speedball). Other terms have become accepted and are used in English such as crystal/cris, terms adapted from crystal meth.
U4. New sterile needle
This question measures the frequency that new sterile needles have been used by the respondent. This could include a needle that was later given to someone else as long as the needle was new when it was first used by the respondent. Use Response Card C to indicate frequency.
U5. Shared needles or rigs
This question assesses frequency of sharing behavior with needles or rigs. For our purposes needle sharing could have the respondent either using a needle either before or after someone else. Use Response Card C to indicate frequency.
U6. Shared equipment of drugs
This question does not refer to needles, but to other drug equipment, such as cookers, cotton, water used for rinsing needles or preparing drugs. Use the Response Card C to indicate frequency that these “works” were shared by the respondent with other persons.
Bilingual interviewer: Cooker may be called by a variety of terms in Spanish, such as “cocinita,” “herbidor,” “estufita,” “chapa,” “tapita,” “caso,” “cocedor,” “sarten,” and “cuchara.” “Algodón” (cotton) is the material used to strain the drug after it is prepared.
U7. Divide drugs with used syringe
Dividing up drugs typically involves the transfer of drugs from the syringe of one person into the syringe of another. This transfer can occur before or after a person has already used the needle/syringe. Use Response Card C to indicate frequency of this behavior. If a respondent indicates the frequency of this behavior was sporadic over the past 12 months, (e.g., they had engaged in it, but stopped several months ago; they had stopped but have recently restarted; some days/weeks they do it more frequently then others, etc.), have them pick one of the response options they think best characterizes the frequency of that behavior.
Non-Injection Drug Use
U8. Alcohol or non-injection drug use
Note that this question includes alcohol use. Non-injection drugs do not include drugs that were prescribed to the respondent by a physician or ones they may have only injected. However, this could include prescription-type drugs (e.g., painkillers) that were received by the respondent from someone other than a health care provider. The question asks for any use in the past 12 months.
U9. Days had a drink
This question begins a series on alcohol use. Those who have not drank at least one drink in the past 30 days will be skipped to the non-injection drug questions (Q13). Be sure the respondent is counting number of days, not number of drinks.
Bilingual interviewer. For this question, “1 cerveza” should be read aloud as “una cerveza.”
U10. Drinks per day
Have the respondent average the number of drinks they have had on a typical day that they drank during the past 30 days.
U11. 5 or more drinks
U12. Binge drinking assessment question
Binge drinking is defined as 5 drinks at one sitting by a male (or MTF transgender) or 4 drinks at a sitting by a female or FTM transgender).
U13a- Frequency of alcohol or non-injection drug use
U13o Use Response Card G to indicate the frequency of non-injection drug and alcohol use within the past 12 months, not including those that were exclusively injected. Interviewers should be familiar with local names for various drugs.
If a respondent’s use of a particular drug during the past 12 months was sporadic (e.g., they had used but stopped several months ago; they had stopped but have recently restarted; some days/weeks they injected more frequently then others, etc.), have them pick one of the response options they think best characterizes their use.
Bilingual interviewer: Interviewer should be aware of local Spanish terms for drug types that have been gathered through formative assessment activities.
U13p- Frequency of other non-injection drug use
U13r If the respondent has used any non-injection drugs not asked about in U13a-U13o, indicate the drug used in U13q and use Response Card G to indicate the frequency of use.
U14a- Drug use during sex
U14h Ask for each drug mentioned in U3a-d, U13a-d and U13i-k, and/or U13n, whether the respondent used it before or during sex in the past 12 months.
U15. Erectile dysfunction (ED) drug use during last 12 months
Was Viagra, Cialis or Levitra or another ED drug used by the respondent during the past 12 months? These drugs are used to enhance potency or erections in males.
U16a-h Drug use with ED drug
Ask for each drug whether an erectile dysfunction drug was used in combination with it in the past 12 months? Erectile dysfunction drugs are often used to counter the inability to achieve an erection while on such drugs as crystal meth.
9.6 Health and Well-Being
Q1- Q7 These questions taken as a whole represent a scale used to measure general health and well being. Interviewers should ensure that the questions are answered about the health of the respondent in general and not solely relating to how HIV has affected their lives. Because this is a validated psychological measure interviewers should avoid interpreting individual measures and allow respondents to interpret question themselves.
9.7 Assessment of Prevention Activities
P1. Receipt of free condoms in last 12 months
Prevention organizations may distribute condoms through active prevention such as using outreach workers or having staff hand them out or through a passive method such as condoms in a jar for people to take as needed.
P1a. Name of organization providing condoms
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P1b. Additional condom sources
Prevention agencies may distribute condoms through active prevention such as using outreach workers or having staff hand them out or through a passive method such as condoms in a jar for people to take as needed.
P1c. Name of organization providing condoms
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P1d. Additional condom sources
Prevention agencies may distribute condoms through active prevention such as using outreach workers or having staff hand them out or through a passive method such as condoms in a jar for people to take as needed.
P1e. Name of organization providing condoms
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P1f. Additional condom sources
Prevention agencies may distribute condoms through active prevention such as using outreach workers or having staff hand them out or through a passive method such as condoms in a jar for people to take as needed.
P1g. Name of organization providing condoms
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P1h. Use of free condoms
Were any of the condoms received in the last 12 months used by the respondent.
P1i. Increased condom usage because of free condoms
Did the availability of free condoms increase the likelihood that condoms would be used. If a respondent would use condoms regardless of whether they had to pay for them or if they were provided for free, the response should be marked, “No.”
P2. Receipt of free new sterile needles in last 12 months
Needle exchange programs operate on a harm reduction model of attempting to reduce risk of infection while attempting to address addiction issues. Typical needle exchange programs operate on a 1:1 exchange basis; one clean needle in exchange for one used needle. Exchange programs may also exist on an underground basis in those areas where needle exchanges are not legal.
P2a. Name of organization providing needles
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P2b. Additional needle sources
Needle exchange programs operate on a harm reduction model of attempting to reduce risk of infection while attempting to address addiction issues. Typical needle exchange programs operate on a 1:1 exchange basis; one clean needle in exchange for one used needle. Exchange programs may also exist on an underground basis in those areas where needle exchanges are not legal.
P2c. Name of organization providing needles
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P2d. Additional needle sources
Needle exchange programs operate on a harm reduction model of attempting to reduce risk of infection while attempting to address addiction issues. Typical needle exchange programs operate on a 1:1 exchange basis; one clean needle in exchange for one used needle. Exchange programs may also exist on an underground basis in those areas where needle exchanges are not legal.
P2e. Name of organization providing needles
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P2f. Additional needle sources
Needle exchange programs operate on a harm reduction model of attempting to reduce risk of infection while attempting to address addiction issues. Typical needle exchange programs operate on a 1:1 exchange basis; one clean needle in exchange for one used needle. Exchange programs may also exist on an underground basis in those areas where needle exchanges are not legal.
P2g. Name of organization providing needles
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area..
P2h. Use of received new sterile needles
Were any of the new sterile needles received by the respondent used for injection drug use?
P2i. Use of clean needles because of availability of free needles
Did the availability of free needles increase the likelihood that new sterile needles would be used. If a respondent would use clean needles regardless of whether they had to pay for them or if they were provided for free, the response should be marked, “No”.
P3. Receipt of safe injection kits
Safe injection kits include such items as new sterile cookers (used to prepare the drug for injection), cotton (used to filter the drug for injection) and water (used to clean the needles for injection, often in conjunction with bleach).
P3a. Name of organization providing kits
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P3b. Other organization providing kits
Safe injection kits include such items as new sterile cookers (used to prepare the drug for injection), cotton (used to filter the drug for injection) and water (used to clean the needles for injection, often in conjunction with bleach).
P3c. Name of organization providing kits
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P3d. Other organization providing kits
Safe injection kits include such items as new sterile cookers (used to prepare the drug for injection), cotton (used to filter the drug for injection) and water (used to clean the needles for injection, often in conjunction with bleach).
P3e. Name of organization providing kits
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P3f. Other organization providing kits
Safe injection kits include such items as new sterile cookers (used to prepare the drug for injection), cotton (used to filter the drug for injection) and water (used to clean the needles for injection, often in conjunction with bleach).
P3g. Name of organization providing kits
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P3h. Use of free kits
Did the respondent use any of the safe injecting kits they received.
P3i. Increased safe injection practiced because of free kits
Did the availability of free kits increase the likelihood that clean works would be used. If a respondent would use clean works regardless of whether they had to pay for them or if they were provided for free, the response should be marked, “No.”
P4. HIV education and risk reduction
Did the respondent attend any one-on-one sessions with a prevention worker or counselor designed to educate and reduce HIV-related risks. Topics could include condom negotiation, how to practice safer sexual behavior or injection or talking to partners. Do not include sessions which were part of HIV testing and counseling encounters.
P4a. Name of organization providing counseling services
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P4b. Other organizations providing counseling
Did the respondent attend any one-on-one sessions with a prevention worker or counselor designed to educate and reduce HIV-related risks. Topics could include condom negotiation, how to practice safer sexual behavior or injection or talking to partners. Do not include sessions which were part of HIV testing and counseling encounters.
P4c. Name of organization providing counseling services
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P4d. Other organizations providing counseling
Did the respondent attend any one-on-one sessions with a prevention worker or counselor designed to educate and reduce HIV-related risks. Topics could include condom negotiation, how to practice safer sexual behavior or injection or talking to partners. Do not include sessions which were part of HIV testing and counseling encounters.
P4e. Name of organization providing counseling services
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P4f. Other organizations providing counseling
Did the respondent attend any one-on-one sessions with a prevention worker or counselor designed to educate and reduce HIV-related risks. Topics could include condom negotiation, how to practice safer sexual behavior or injection or talking to partners. Do not include sessions which were part of HIV testing and counseling encounters.
P4g. Name of organization providing counseling services
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P4h. Specific topics covered by one on one counseling
Record all topics addressed during the one-on-one counseling sessions.
P4i. Use of skills with sex partners
Record if the respondent believes they talk to their sexual partners differently as a result of the one on one counseling sessions they received.
P4j. Use of skills with injection drug partners
Record if the respondent believes they talk to their injection drug partners differently as a result of the one-on-one counseling sessions they received.
P5. Attendance in HIV prevention group sessions
Group sessions on HIV prevention may bring a group together with a counselor or prevention worker to discuss particular topics regarding prevention of HIV, such as sharing skills for risk reduction and how to talk to partners.
P5a. Name of organization organizing group session
Interviewer should record the name of the organization and classify tit into one of the organization types. Some may fall into more than one possible category, in those cases the list should be used with priority given to options higher in the list. Sites should devise a consistent spelling and classification for sites in their area.
P5b. Specific topics covered by group sessions
Read each question and record all topics addressed during the group sessions for HIV prevention.
P5c. Use of skills with sex partners
Record if the respondent believes they talk to their sexual partners differently as a result of the group sessions they attended.
P5d. Use of skills with injection drug partners
Record if the respondent believes they talk to their injection drug partners differently as a result of the group sessions they attended.
10. Short Questionnaire
10.1 Description
The Short Questionnaire is a condensed version of the standard questionnaire. Interviewers should use the Short Questionnaire only when it is not feasible to administer the standard questionnaire. The Short Questionnaire may be used if it is the only method by which interview responses can be collected from a patient. For example, use of the Short Questionnaire is allowed if a patient is ill or requires a translator, and cannot complete the standard questionnaire by scheduling several interview sessions.
10.2 Short Questionnaire: Specific Guidance
Q1. Prior Participation in MMP
Patients may participate in MMP once during a cycle. If the respondent indicates they have previously been interviewed, even in another project area during the current cycle, they should be thanked for their time and the interview terminated (no incentive will be provided). Interviewers should be clear whether the previous interview was during the current calendar year or a previous calendar year.
Q2. Date of Birth
Enter in the respondent’s date of birth. Respondent’s date of birth should never be left blank, as this information is critical in determining eligibility for the study. Respondents who are younger than 18 years old at the start of the PDP are NOT eligible to participate.
Q3. Sex at birth
Read the question no matter how obvious gender may appear to you. This classifies their gender at birth rather than that which may be apparent today. This item is particularly critical to enter correctly as it relates to which sexual behavior questions should be completed later in the interview. Intersex/ambiguous refers to those who may have been born with a combination of male and female physiology (similar to hermaphrodite).
Bilingual interviewer: The term, “hermafrodita,” though not common, may also be used to refer to a person born with the physiology of one gender, but knows/feels to be of the other.
Q3a. Gender identity
It may feel awkward to read this item. If necessary you can explain to the respondent that you are required to read all questions as written, however obvious the answer might be. The computer will classify persons whose current gender identity and birth sex do not match as transgendered. While some individuals identify themselves solely as “transgender” we are attempting to collect their true gender self identity. (i.e., the male in a female-to-male [FTM] and the female in a male-to-female [MTF]).
Bilingual Interviewer comments: The term commonly used is “transgénero”.
Q4. Highest education
An Associate’s Degree is conferred by junior colleges. “Technical school” refers to technical training received after graduating from high school or obtaining a GED. “Any postgraduate studies” refers to education beyond a bachelor’s degree. The interviewer should interpret the answer given and read the appropriate choice back to the respondent before marking.
Bilingual interviewer: It is important to be aware that in Latin American countries there are different school systems. The labels will vary from country to country. The interviewer must avoid coding errors by probing the respondent and asking them what they mean. Here are some examples; “Bachillerato” is the name for high school level in some countries like Colombia. The term does not have a direct correspondent to the English term: “Bachelor’s degree.” In Mexico “preparatoria” is the name for “high school” and “secundaria” is the name for “junior high.” On the other hand, in some South American countries, the word” “colegio” may be used for high school. “Universidad” is the Spanish term for “College” in most countries (like Mexico, Colombia, or Puerto Rico). Younger Latino respondents may only be familiar with the US school system and the corresponding English terminology.
If the respondent’s level of education is not recorded accurately, the result may be unintended coding errors. Interviewers are encouraged to probe and clarify how many years of schooling the respondent completed beyond primary school.
Q5. Ethnicity
This is the same question used on the census for determining Hispanic ethnicity. It is separate from the question about race. According to the Office of Management and Budget (OMB): The term “Hispanic” or “Latino” refers to persons who trace their origin or descent to Mexico, Puerto Rico, Cuba, Central and South America, and other Spanish cultures.
Q5a. Hispanic ancestry
The term “ancestry” in this question refers to where the respondent traces his/her Hispanic or Latino origin or descent. Record the response to this question by checking all that apply. If respondent indicates a non-Hispanic ethnicity, provide him/her with a definition of what we mean by Hispanic ethnicity, i.e., origin or descent that can be traced to Mexico, Puerto Rico, Cuba, Central or South America (this includes Brazil), or other Spanish cultures.
If the respondent gives a response other than those listed, record the response in “Other (Specify).”
Q6. Race
Read each racial group and check all that apply. If a respondent reports they are of mixed race, be sure each race is recorded. Responses should be read as listed and in order, conforming to OMB requirements for collection of race and ethnicity. Hispanic is NOT a race category. However, if a respondent insists their race is “Hispanic,” check “Other” and code “Hispanic” in the blank after “Other (Specify)”. In general, use the “Other” category sparingly for this question.
According to OMB, Central and South American Indians should be classified as American Indian.
Q7. Homelessness
This question is designed to identify whether the respondent had a regular home/residence in the 12 months before the interview. Be sure to read the definition of homeless as part of the question. Homeless status refers to not having a place to stay at night. Rely on the respondent’s interpretation of their housing status.
NOTE: In this survey, “homeless” is defined (Stewart B. McKinney Act, 42 U.S.C. § 11301, et seq.) as a person who lacks a fixed, regular, and adequate night-time residence and…has a steady night time residency that is (A) a supervised publicly or privately operated shelter designed to provide temporary living accommodation…(B) an institution that provides a temporary residence for individuals intended to be institutionalized or (C) a public or private place not designed for, or ordinarily used as, a regular sleeping accommodation for human beings.” (e.g., one’s automobile, under a bridge, etc.)
A single room occupancy (SRO) is defined as multi-unit housing for low-income persons, generally consisting of a single room and shared bath, and may also include a shared kitchen. These are typically not licensed or regulated by a government agency.
Q8. Health insurance
This question serves as a screener to determine if the respondent has health insurance coverage. Interviewers should emphasize that our interest is in whether the respondent had a policy that covers medical expenses or health care services, but not if the respondent had only a single-service policy like dental, vision, or prescription drug coverage.
Q8a. Gaps in insurance coverage
Gaps in insurance coverage can affect access to health care. Gaps can include time between policies, transitions from coverage to non-coverage (or vice versa) or waiting periods for benefits. In the above situations, participants would be considered not to have had insurance coverage.
Q9. Prescription drug coverage
Interviewers should be aware of local branding (names) of drug assistance programs.
Q11. First positive test
Enter the date when the respondent first tested positive for HIV. Some respondents may have difficulty remembering the date of their first positive HIV test. This date may also not be the same as the most recent HIV test date since some persons with HIV infection may get tested again after their first diagnosis. Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If month is unknown, code “??/YYYY”. If both month and year are unknown code “.99” for a full “Don’t Know” response.
Q12. First HIV care
It is important to know how quickly after diagnosis persons with HIV are getting into health care. For this question put the date the respondent entered into care specifically for their HIV infection. This may not necessarily have involved treatment, and might have only included assessment of the stage of their HIV infection.
Q13. Delayed first HIV care
Guidelines for the treatment of HIV infection recommend that all persons who are newly diagnosed with HIV infection be seen by a health care provider within 3 months of their initial diagnosis. The respondent may not consider their entering into care as being delayed; for these individuals explain the 3 months recommendation. Enter all reasons reported by the respondent. Do not read list of reasons.
Q14. Last HIV care visit
When was the respondent’s most recent visit to their health care provider? Depending on when the patient interview occurs, the patient’s last HIV care visit might have occurred after the PDP. Some respondents may have difficulty remembering the date of their last provider visit. Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If month is unknown, code “??/YYYY”. If both month and year are unknown, then code “.99” for a full “Don’t Know” response. Probe extensively to at least obtain the year of this visit.
Q14a. Last HIV care visit > 3 months
Current guidelines recommend HIV-positive individuals see a medical provider for evaluation of their health status every 3 months. Ask the reason they have not gone to their provider in the last 3 months. Enter all reasons reported by the respondent. Do not read list of reasons.
Q15. Source of health care
This question screens for persons who have a primary source of HIV care. Individuals who see several different providers but don’t consider any to be a main source should answer “No” to this question.
Q15a. Reason no usual source of health care
Respondents may have multiple reasons for not having a primary source of care for their HIV infection. Interviewers should allow time for respondents to offer all reasons for not having a usual source of care and attempt to categorize each of the answers into one of the listed choices. Interviewers should not read the list of reasons, so as not to influence respondents’ answers. Enter all that apply, fitting responses into appropriate categories in the list. If you are unsure what category a response fits into, record it under “Other.”
Q15b. Name of source of HIV care
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
Q15c. HIV care during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent received HIV related care from the facility during the PDP a follow-up question will be asked.
Q16. Non-HIV care
This question refers to facilities a respondent may have attended that were the primary source of medical care, not related to HIV. NOTE: this facility could be the same facility the respondent went to for HIV related care, in which case the follow-up questions should be answered the same.
Q16a. Name of source of non-HIV care
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
Q16b. Non-HIV care during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent received non-HIV related care from the facility during the PDP a follow-up question will be asked.
Q17. ER visits in past 12 months
Clarify the 12 month period for respondent as needed. HIV care received though the ER does not include those for accidents or injury. This does not include visits to the ER that resulted in admittance to the hospital (captured in A18).
Q18. Urgent care visits in past 12 months
Urgent care is defined as the delivery of ambulatory medical care outside of a hospital emergency department on a walk-in basis without a scheduled appointment. Urgent care centers would include private medical centers and facilities intended for episodic treatment of medical conditions and not ongoing care. Care received should have been for HIV related purposes and not related to accident or injury.
Q19. Hospital admissions in past 12 months
This question seeks the total number of admittances for HIV care, not the total number of nights spent in a hospital. Do not include visits that were solely made to the ER. You may need to confirm A16 (ER visits).
Q19a. Hospital name
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
Q19b. Hospital admission during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent had an HIV-related hospital admission during the PDP a follow-up question will be asked.
Q20. Antiretrovirals ever
Record antiretrovirals taken for treatment of the respondent’s HIV infection and not for other conditions such as hepatitis (this includes Lamivudine which is prescribed for both conditions) or for the prevention of HIV. For the purposes of this question antiretrovirals include approved medications for the treatment of HIV including nucleoside/nucleotide analogues, non-nucleoside analogues, protease inhibitors, and fusion inhibitors. Naturopathic or eastern medicinal treatments that are not FDA approved for the treatment of HIV infection should not be included. Immune boosting treatments such as Hydroxyurea and IL-2 should not be included.
Q20a. Antiretrovirals never
Many individuals choose to delay or avoid treatment of their HIV infection for various reasons. Give time for the respondent to give as many reasons for non-use of ART. Probes should be limited to, “Is there anything else?” so as not to influence respondents’ answers.
Q21. Current ART use
Record if the respondent is currently taking any ART to treat HIV. If a respondent is currently taking a “drug holiday” or a Strategic (i.e., structured or planned) Treatment Interruption (STI) with the intention to resume treatment at a later point, this question should be coded as “Yes.”
Q21a. Reason not currently on antiretrovirals
Many individuals choose to delay or avoid treatment of their HIV infection for various reasons. Give time for the respondent to give as many reasons for non-use of ART. Fit each response into the appropriate category in the list. If you are unsure which category a response should be assigned to, record under “Other.” Probes should be limited to “is there anything else?” so as not to influence respondent’s answers.
Q22. Antiretrovirals in last 12 months
This question is only asked of those who indicated they are not currently taking antiretroviral medications.
Q23.-36. Unmet Need
The following questions are designed to assess what services persons with HIV may need and what barriers may have kept them from accessing these services. Note that these questions refer to need during the past 12 months only. For each type of service, indicate whether the respondent needed the service in the past 12 months, was able to access the service in the past 12 months, and for services needed but not able to access, the main reason why. Do not read the response categories for reason not able to get this service.
Q23. HIV case management
HIV case management services are a means to coordinate various aspects of care needed by persons living with HIV. These include insurance, health care, mental health, drug treatment, housing, etc.
Q24. Mental heath counseling
Mental health counseling includes psychologists, social workers, counselors, therapists or psychiatric services.
Q25. Social services
Credit counseling, assistance getting insurance, etc.
Q26. Finding medical service
Assistance in finding a medical provider for ongoing (not urgent) care.
Q27. Finding dental service
Assistance in finding a dentist. Examples could be with expertise with HIV-positive patients or accepting certain coverage.
Q28. Adherence support
Includes direct therapy observation or techniques to take the prescribed dose of medicines on schedule.
Q29. Home health
Home health services could be any form of home nursing, physical therapy or health care providers who provide services within a patients’ home.
Q30. Chore or homemaker
Chore and homemaker services may provide cleaning, organizational and other assistance for persons unable to maintain their own home. Often these services are provided by a community-based organization.
Q31. Finding shelter/housing
Services to get housing or assistance in finding temporary or long-term housing.
Q32. Finding meals/food
Assistance including meal delivery, food delivery or other nutritional support.
Q33. Transportation
Providing rides to medical appointments, shopping, case management or other appointments.
Q34. Childcare
Day care, babysitting, nanny or other childcare services.
Q35. HIV education or risk reduction
Services designed to educate on avoidance of transmission of HIV, living with HIV or mediating risks within ones life.
Q36. Other
Any other services not specifically mentioned above.
11. Proxy Questionnaire
11.1 Description
The Proxy Questionnaire is a condensed version of the standard questionnaire. Interviewers should only administer the Proxy Questionnaire when the selected patient is not available for an interview, and will not be available for interview during the entire annual MMP data collection cycle. For example, the Proxy Questionnaire may be used if a patient has died after recruitment selection.
11.2 Proxy Questionnaire: Specific Guidance
For all questions in the proxy questionnaire, insert “he” or “she” as appropriate.
Q1. Prior Participation in MMP
Patients may participate in MMP once during a cycle. If the respondent indicates they have previously been interviewed, even in another project area during the current cycle, they should be thanked for their time and the interview terminated (no incentive will be provided). Interviewers should be clear whether the previous interview was during the current calendar year or a previous calendar year.
Q2. Patient Living/Deceased
If the patient is deceased, then use the past tense when formulating questions.
Q2b. Relationship to Patient
Do not read the list of responses. Mark the response that corresponds to the proxy’s relationship to the patient. For example, if the person serving as a proxy is the patient’s mother, you enter “parent” as the response.
Q3. Respondent’s Date of Birth
Enter in the respondent’s date of birth. Respondent’s date of birth should never be left blank, as this information is critical in determining eligibility for the study. Respondents who are younger than 18 years old are NOT eligible to participate.
Q3a. Patient’s Date of Birth
Enter in the respondent’s date of birth. Respondent’s date of birth should never be left blank, as this information is critical in determining eligibility for the study. Respondents who are younger than 18 years old at the start of the PDP are NOT eligible to participate.
Q4. Sex at birth
Read the question no matter how obvious gender may appear to you. This classifies their gender at birth rather than that which may be apparent today. This item is particularly critical to enter correctly as it relates to which sexual behavior questions should be completed later in the interview. Intersex/ambiguous refers to those who may have been born with a combination of male and female physiology (similar to hermaphrodite).
Bilingual interviewer: The term, “hermafrodita,” though not common, may also be used to refer to a person born with the physiology of one gender, but knows/feels to be of the other.
Q4a. Gender identity
It may feel awkward to read this item. If necessary you can explain to the respondent that you are required to read all questions as written, however obvious the answer might be. The computer will classify persons whose current gender identity and birth sex do not match as transgendered. While some individuals identify themselves solely as “transgender” we are attempting to collect their true gender self identity. (i.e., the male in a female-to-male [FTM] and the female in a male-to-female [MTF]).
Bilingual Interviewer comments: The term commonly used is “transgénero”.
Q5. Highest education
An Associate’s Degree is conferred by junior colleges. “Technical school” refers to technical training received after graduating from high school or obtaining a GED. “Any postgraduate studies” refers to education beyond a bachelor’s degree. The interviewer should interpret the answer given and read the appropriate choice back to the respondent before marking.
Bilingual interviewer: It is important to be aware that in Latin American countries there are different school systems. The labels will vary from country to country. The interviewer must avoid coding errors by probing the respondent and asking them what they mean. Here are some examples; “Bachillerato” is the name for high school level in some countries like Colombia. The term does not have a direct correspondent to the English term: “Bachelor’s degree.” In Mexico “preparatoria” is the name for “high school” and “secundaria” is the name for “junior high.” On the other hand, in some South American countries, the word” “colegio” may be used for high school. “Universidad” is the Spanish term for “College” in most countries (like Mexico, Colombia, or Puerto Rico). Younger Latino respondents may only be familiar with the US school system and the corresponding English terminology.
If the respondent’s level of education is not recorded accurately, the result may be unintended coding errors. Interviewers are encouraged to probe and clarify how many years of schooling the respondent completed beyond primary school.
Q6. Ethnicity
This is the same question used on the census for determining Hispanic ethnicity. It is separate from the question about race. According to the Office of Management and Budget (OMB): The term “Hispanic” or “Latino” refers to persons who trace their origin or descent to Mexico, Puerto Rico, Cuba, Central and South America, and other Spanish cultures.
Q6a. Hispanic ancestry
The term “ancestry” in this question refers to where the respondent traces his/her Hispanic or Latino origin or descent. Record the response to this question by checking all that apply. If respondent indicates a non-Hispanic ethnicity, provide him/her with a definition of what we mean by Hispanic ethnicity, i.e., origin or descent that can be traced to Mexico, Puerto Rico, Cuba, Central or South America (this includes Brazil), or other Spanish cultures.
If the respondent gives a response other than those listed, record the response in “Other (Specify).”
Q7. Race
Read each racial group and check all that apply. If a respondent reports they are of mixed race, be sure each race is recorded. Responses should be read as listed and in order, conforming to OMB requirements for collection of race and ethnicity. Hispanic is NOT a race category. However, if a respondent insists their race is “Hispanic,” check “Other” and code “Hispanic” in the blank after “Other (Specify)”. In general, use the “Other” category sparingly for this question.
According to OMB, Central and South American Indians should be classified as American Indian.
Q8. Homelessness
This question is designed to identify whether the respondent had a regular home/residence in the 12 months before the interview. Be sure to read the definition of homeless as part of the question. Homeless status refers to not having a place to stay at night. Rely on the respondent’s interpretation of their housing status.
NOTE: In this survey, “homeless” is defined (Stewart B. McKinney Act, 42 U.S.C. § 11301, et seq.) as a person who lacks a fixed, regular, and adequate night-time residence and…has a steady night time residency that is (A) a supervised publicly or privately operated shelter designed to provide temporary living accommodation…(B) an institution that provides a temporary residence for individuals intended to be institutionalized or (C) a public or private place not designed for, or ordinarily used as, a regular sleeping accommodation for human beings.” (e.g., one’s automobile, under a bridge, etc.)
A single room occupancy (SRO) is defined as multi-unit housing for low-income persons, generally consisting of a single room and shared bath, and may also include a shared kitchen. These are typically not licensed or regulated by a government agency.
Q9. Health insurance
This question serves as a screener to determine if the respondent has health insurance coverage. Interviewers should emphasize that our interest is in whether the respondent had a policy that covers medical expenses or health care services, but not if the respondent had only a single-service policy like dental, vision, or prescription drug coverage.
Q9a. Gaps in insurance coverage
Gaps in insurance coverage can affect access to health care. Gaps can include time between policies, transitions from coverage to non-coverage (or vice versa) or waiting periods for benefits. In the above situations, participants would be considered not to have had insurance coverage.
Q10. Prescription drug coverage
Interviewers should be aware of local branding (names) of drug assistance programs.
Q12. First positive test
Enter the date when the respondent first tested positive for HIV. Some respondents may have difficulty remembering the date of their first positive HIV test. This date may also not be the same as the most recent HIV test date since some persons with HIV infection may get tested again after their first diagnosis. Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If month is unknown, code “??/YYYY”. If both month and year are unknown code “D” for a full “Don’t Know” response.
Q12. First HIV care
It is important to know how quickly after diagnosis persons with HIV are getting into health care. For this question put the date the respondent entered into care specifically for their HIV infection. This may not necessarily have involved treatment, and might have only included assessment of the stage of their HIV infection.
Q13. Last HIV care visit
When was the respondent’s most recent visit to their health care provider? Depending on when the patient interview occurs, the patient’s last HIV care visit might have occurred after the PDP. Some respondents may have difficulty remembering the date of their last provider visit. Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If month is unknown, code “??/YYYY”. If both month and year are unknown, then code “D” for a full “Don’t Know” response. Probe extensively to at least obtain the year of this visit.
Q14 Last HIV care visit > 3 months
Current guidelines recommend HIV-positive individuals see a medical provider for evaluation of their health status every 3 months. Ask the reason they have not gone to their provider in the last 3 months. Enter all reasons reported by the respondent. Do not read list of reasons.
Q15. Source of health care
This question screens for persons who have a primary source of HIV care. Individuals who see several different providers but don’t consider any to be a main source should answer “No” to this question.
Q15a. Reason no usual source of health care
Respondents may have multiple reasons for not having a primary source of care for their HIV infection. Interviewers should allow time for respondents to offer all reasons for not having a usual source of care and attempt to categorize each of the answers into one of the listed choices. Interviewers should not read the list of reasons, so as not to influence respondents’ answers. Enter all that apply, fitting responses into appropriate categories in the list. If you are unsure what category a response fits into, record it under “Other.”
Q15b. Name of source of HIV care
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
Q15c. HIV care during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent received HIV related care from the facility during the PDP a follow-up question will be asked.
Q16. Non-HIV care
This question refers to facilities a respondent may have attended that were the primary source of medical care, not related to HIV. NOTE: this facility could be the same facility the respondent went to for HIV related care, in which case the follow-up questions should be answered the same.
Q16a. Name of source of non-HIV care
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
Q16b. Non-HIV care during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent received non-HIV related care from the facility during the PDP a follow-up question will be asked.
Q17. ER visits in past 12 months
Clarify the 12 month period for respondent as needed. HIV care received though the ER does not include those for accidents or injury. This does not include visits to the ER that resulted in admittance to the hospital (captured in A18).
Q18. Urgent care visits in past 12 months
Urgent care is defined as the delivery of ambulatory medical care outside of a hospital emergency department on a walk-in basis without a scheduled appointment. Urgent care centers would include private medical centers and facilities intended for episodic treatment of medical conditions and not ongoing care. Care received should have been for HIV related purposes and not related to accident or injury.
Q19. Hospital admissions in past 12 months
This question seeks the total number of admittances for HIV care, not the total number of nights spent in a hospital. Do not include visits that were solely made to the ER. You may need to confirm A16 (ER visits).
Q19a. Hospital name
Respondents may have difficulty remembering details for facilities they have attended for care. Use whatever probes are necessary to obtain enough information to locate the facility for abstraction of patient records. If you are familiar with the facility, record only the facility name and provider information on the facility visits log and fill in the rest of the information (address, type of facility, etc.) after the interview is completed. If the respondent doesn’t remember the facility name, write down as much information as possible about the location, name of provider, etc.
Q19b. Hospital admission during PDP
The PDP will be set for each site for each cycle of recruitment. If a respondent had an HIV-related hospital admission during the PDP a follow-up question will be asked.
Q20. Antiretrovirals ever
Record antiretrovirals taken for treatment of the respondent’s HIV infection and not for other conditions such as hepatitis (this includes Lamivudine which is prescribed for both conditions) or for the prevention of HIV. For the purposes of this question antiretrovirals include approved medications for the treatment of HIV including nucleoside/nucleotide analogues, non-nucleoside analogues, protease inhibitors, and fusion inhibitors. Naturopathic or eastern medicinal treatments that are not FDA approved for the treatment of HIV infection should not be included. Immune boosting treatments such as Hydroxyurea and IL-2 should not be included.
Q20a. Antiretrovirals never
Many individuals choose to delay or avoid treatment of their HIV infection for various reasons. Give time for the respondent to give as many reasons for non-use of ART. Probes should be limited to, “Is there anything else?” so as not to influence respondents’ answers.
Q21. Antiretrovirals in last 12 months
This question is only asked of those who indicated they are not currently taking antiretroviral medications.
Q22.-Q35. Unmet Need
The following questions are designed to assess what services persons with HIV may need and what barriers may have kept them from accessing these services. Note that these questions refer to need during the past 12 months only. For each type of service, indicate whether the respondent needed the service in the past 12 months, was able to access the service in the past 12 months, and for services needed but not able to access, the main reason why. Do not read the response categories for reason not able to get this service.
Q22. HIV case management
HIV case management services are a means to coordinate various aspects of care needed by persons living with HIV. These include insurance, health care, mental health, drug treatment, housing, etc.
Q23. Mental heath counseling
Mental health counseling includes psychologists, social workers, counselors, therapists or psychiatric services.
Q24. Social services
Credit counseling, assistance getting insurance, etc.
Q25. Finding medical service
Assistance in finding a medical provider for ongoing (not urgent) care.
Q26. Finding dental service
Assistance in finding a dentist. Examples could be with expertise with HIV-positive patients or accepting certain coverage.
Q27. Adherence support
Includes direct therapy observation or techniques to take the prescribed dose of medicines on schedule.
Q28. Home health
Home health services could be any form of home nursing, physical therapy or health care providers who provide services within a patients’ home.
Q29. Chore or homemaker
Chore and homemaker services may provide cleaning, organizational and other assistance for persons unable to maintain their own home. Often these services are provided by a community-based organization.
Q30. Finding shelter/housing
Services to get housing or assistance in finding temporary or long-term housing.
Q31. Finding meals/food
Assistance including meal delivery, food delivery or other nutritional support.
Q32. Transportation
Providing rides to medical appointments, shopping, case management or other appointments.
Q33. Childcare
Day care, babysitting, nanny or other childcare services.
Q34. HIV education or risk reduction
Services designed to educate on avoidance of transmission of HIV, living with HIV or mediating risks within ones life.
Q35. Other
Any other services not specifically mentioned above.
12. Non-Response Form
The Non-Response Form collects a minimal amount of basic HIV surveillance information. This information may be acquired by several methods: requesting the information from facilities as part of the PDP patient lists, which are obtained prior to patient sampling; extracting the data directly from the HIV/AIDS Reporting System (HARS) or other HIV data sources; and administering the Non-Response Form at the time a selected patient declines to participate in the interview.
Only use the Non-Response Form for selected patients who decline to participate in the interview. It is recommended that this information be collected, if possible, directly from the selected patient, even if the data were also obtained from the facility or from another data source. This is because other data may be incomplete or may differ from the response provided by the patient.
The Non-Response Form should be administered at the time of patient recruitment, after a firm refusal has been provided by the patient. Although the patient has declined to participate in the standard interview, wording to request the patient to provide non-response information such as “May I ask you a few basic questions? We will only use this information to understand how our participants differ from those who do not choose to participate” should be used. If the patient declines to provide non-response information, and the facility has not provided this information with the PDP patient list but will allow it to be obtained from the patient’s medical record, the form should be completed using this information.
12.2 Non-Response Form: Specific Guidance
Date Form Completed
Enter the month, day, and four-digit year for the date you complete the Non-Response Form.
Data Sources
Select any data source used to complete the form.
Date of Birth
Enter in the patient’s date of birth.
First HIV Diagnosis
Enter the patient’s age at the time s/he first tested positive for HIV, or enter the date of the first positive HIV test. Some respondents may have difficulty remembering the date of their first positive HIV test. This date may also not be the same as the most recent HIV test date since some persons with HIV infection may get tested again after their first diagnosis. Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If the month is unknown, code “99/YYYY”. If both the month and year are unknown, code “D” for a full “Don’t Know” response.
First AIDS Diagnosis
Enter the patient’s age at the time s/he first was diagnosed with AIDS, or enter the date of the first AIDS diagnosis. Some respondents may have difficulty remembering the date of their first AIDS diagnosis. Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If month is unknown, code “99/YYYY”. If both month and year are unknown code “D” for a full “Don’t Know” response.
Sex
Choose the patient’s apparent gender, or gender as it appears in the selected facility’s records.
Ethnicity
According to the Office of Management and Budget (OMB): The term “Hispanic” or “Latino” refers to persons who trace their origin or descent to Mexico, Puerto Rico, Cuba, Central and South America, and other Spanish cultures.
Race
Read each racial group and check all that apply. If a respondent reports they are of mixed race, be sure each race is recorded. According to OMB, Central and South American Indians should be classified as American Indian.
Country of Birth
Enter the appropriate response.
Mode of HIV Exposure
Enter the appropriate response (Yes, No, Unknown) for each exposure category.
First CD4 Test Count
Enter the count value and the date of the patient’s first CD4 test. Some respondents may have difficulty remembering the date of their first CD4 test. This date may also not be the same as the most recent CD4 test date since many patients with HIV infection may get tested repeatedly. Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If month is unknown, code “99/YYYY”. If both month and year are unknown code “D” for a full “Don’t Know” response.
First CD4 Test Percent
Enter the percent value and the date of the patient’s first CD4 test. Some respondents may have difficulty remembering the date of their first CD4 test. This date may also not be the same as the most recent CD4 test date since many patients with HIV infection may get tested repeatedly. Work with the respondent using key dates and seasons to narrow the time period (“Was it in the winter, summer, etc?”). If month is unknown, code “99/YYYY”. If both month and year are unknown code “D” for a full “Don’t Know” response.
Insurance
Enter the primary method by which the patient’s HIV medical treatment is financed.
| File Type | application/msword |
| File Title | Attachment 4 |
| Author | evu0 |
| Last Modified By | euo5 |
| File Modified | 2006-06-21 |
| File Created | 2006-06-21 |
© 2026 OMB.report | Privacy Policy