Attachment 1. Authorizing Legislation
Attachment 1 a-c Leg Auth.doc
Surveillance of HIV/AIDS Related Events Among Persons Not Receiving Care ("Never In Care")
Attachment 1. Authorizing Legislation
OMB: 0920-0748
Attachments to
Justification for OMB Clearance for Paperwork Reduction Act
Surveillance of HIV-Related Events Among Persons Not Receiving HIV Care
"Never In Care Project"
April 11, 2007
Project Officer:
Jeanne Bertolli, PhD
Epidemiologist, Clinical Outcomes Team
National Center for HIV, STD, and TB Prevention
Coordinating Center for Infectious Diseases
Centers for Disease Control and Prevention
1600 Clifton Rd, NE, MS E-46
Atlanta, Georgia 30333
Phone: (404) 639-8500
Fax: (404) 639-8640
E-mail: [email protected]
Table of Contents
Attachment 1a. Section 306 of the Public Health Service Act 3
Attachment 1b. Section 308(d) of the Public Health Service Act 6
Attachment 1c. Section 301 of the Public Health Service Act 8
Attachment 2a. Standard Structured Questionnaire 10
Attachment 2b. Qualitative Interview Guide and Observation Form 39
Attachment 2c. 2007 Non-Response Data Collection Form 50
Attachment 3. 2007 Interview Guide 55
Attachment 4. Cdc IRB Approval 75
Attachment 5a. Template Informed Consent For Standard Structured Interview and Blood Collection 78
Attachment 5b. Template Informed Consent For Standard Structured Interview, Qualitative Interview, and Blood Collection 85
Attachment 6. Agreement to Abide by the Restrictions On Release of Surveillance Data 92
Attachment 7. Assurance of Confidentiality 96
Attachment 8. Contact and Recruitment Procedures and Scripts 99
Attachment 9. Script for Returning CD4 T-Lymphocyte and HIV Viral Load Test Results to Participants 120
Attachment 1a. Section 306 of the Public Health Service Act
TITLE 42 - THE PUBLIC HEALTH AND WELFARE
CHAPTER 6A - PUBLIC HEALTH SERVICE
SUBCHAPTER II - GENERAL POWERS AND DUTIES
Part A - Research and Investigations
Sec. 242k. National Center for Health Statistics
-STATUTE-
(a) Establishment; appointment of Director; statistical and
epidemiological activities
There is established in the Department of Health and Human Services the National Center for Health Statistics (hereinafter in this section referred to as the "Center") which shall be under the direction of a Director who shall be appointed by the Secretary.
The Secretary, acting through the Center, shall conduct and support statistical and epidemiological activities for the purpose of improving the effectiveness, efficiency, and quality of health services in the United States.
(b) Duties
In carrying out subsection (a) of this section, the Secretary, acting through the Center,
(1) shall collect statistics on -
(A) the extent and nature of illness and disability of the population of the United States (or of any groupings of the people included in the population), including life expectancy, the incidence of various acute and chronic illnesses, and infant and maternal morbidity and mortality,
(B) the impact of illness and disability of the population on the economy of the United States and on other aspects of the well-being of its population (or of such groupings),
(C) environmental, social, and other health hazards,
(D) determinants of health,
(E) health resources, including physicians, dentists, nurses, and other health professionals by specialty and type of practice and the supply of services by hospitals, extended care facilities, home health agencies, and other health institutions,
(F) utilization of health care, including utilization of
(i) ambulatory health services
by specialties and types of practice of the health professionals
providing such services, and (ii) services of hospitals, extended
care facilities, home health agencies, and other institutions,
(G) health care costs and financing, including the trends in health care prices and cost, the sources of payments for health care services, and Federal, State, and local governmental expenditures for health care services, and
(H) family formation, growth, and dissolution;
(2) shall undertake and support (by grant or contract) research, demonstrations, and evaluations respecting new or improved methods for obtaining current data on the matters referred to in paragraph (1);
(3) may undertake and support (by grant or contract) epidemiological research, demonstrations, and evaluations on the matters referred to in paragraph (1); and
(4) may collect,
furnish, tabulate, and analyze statistics, and prepare studies, on
matters referred to in paragraph (1) upon request of public and
nonprofit private entities under arrangements under which the
entities will pay the cost of the service provided.
Amounts appropriated to the Secretary from payments made under arrangements made under paragraph (4) shall be available to the Secretary for obligation until expended.
Attachment 1b. Section 308(d) of the Public Health Service Act
TITLE 42 - THE PUBLIC HEALTH AND WELFARE
CHAPTER 6A - PUBLIC HEALTH SERVICE
SUBCHAPTER II - GENERAL POWERS AND DUTIES
Part A - Research and Investigations
Sec. 241. Research and investigations generally
-STATUTE-
(d) Protection of privacy of individuals who are research subjects
The Secretary may authorize persons engaged in biomedical, behavioral, clinical, or other research (including research on mental health, including research on the use and effect of alcohol and other psychoactive drugs) to protect the privacy of individuals who are the subject of such research by withholding from all persons not connected with the conduct of such research the names or other identifying characteristics of such individuals. Persons so authorized to protect the privacy of such individuals may not be compelled in any Federal, State, or local civil, criminal, administrative, legislative, or other proceedings to identify such individuals.
Attachment 1c. Section 301 of the Public Health Service Act
Attachment 2a. Standard Structured Questionnaire For Never In Care Project
form approved
OMB No.___ -___
expiration date: ___/___/_____
Never in Care Project (NIC)
2007 Standard Questionnaire
VERSION 1.3
Public reporting burden of this collection of information is estimated to average 30 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not required to respond to a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden to: CDC, Project Clearance Officer, 1600 Clifton Road, MS D–24, Atlanta, GA 30333, ATTN: PRA (0920–0011). Do not send the completed form to this address.
DEPARTMENT OF HEALTH AND HUMAN SERVICES
P


Centers for Disease Control and Prevention
Atlanta, GA 30333
Preliminary Information
Interviewer instructions: Enter Preliminary Information prior to the interview.
P1. Never In Care ID Number: __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __
Inconsistency check: P1 cannot be greater than 22 digits.
P2. HIV/AIDS Reporting System (HARS) Mode of Exposure: ____
Inconsistency check: P2 cannot be less than 0 or greater than 9.
P3. Interviewer ID: ___ ___
Inconsistency check: P3 cannot be less than 1 or greater than 20.
P4. Date first positive test reported: __ __ /__ __ / __ __ __ __
M M D D Y Y Y Y
Inconsistency check: P4 cannot be earlier than 07/01/2006 and cannot be later than current date.
P5. Interview location: [CHOOSE ONE.]
1 Indiana
2 New Jersey
3 New York City
4 Philadelphia
5 Washington
P6. Interview date: __ __ /__ __ / __ __ __ __
M M D D Y Y Y Y
Inconsistency check: P6 cannot be earlier than 10/01/2007 or later than current date.
P7. Time questionnaire began:
__ __: __ __ AM PM
Eligibility
SAY: “I’d like to thank you for taking part in this interview. Remember that all the information you give me will be private and your name will not be recorded anywhere on this form (computer).
E1. What is your date of birth?
__ __ /__ __ / __ __ __ __
M M D D Y Y Y Y
[Month: 77 = Refused to answer, 88= Don’t know; Day: 77 = Refused to answer, 88= Don’t know
Year: 7777 = Refused to answer, 8888 = Don’t know]
Inconsistency check: E1 cannot be earlier than 01/01/1900.
Interviewer instructions: If “Refused to answer” or “Don’t know,” skip to Say box before E2.
E1a. So, you are ______ [AGE] years old. Is that correct?
No………………………………………..SAY: “Please tell me your date of birth
again.” [RETURN TO E1.]
Yes
7 Refused to answer……………………………Skip to Say box before E2
8 Don’t know…………………………………..Skip to Say box before E2
Interviewer instructions: If respondent is less than 18 years old, go to Say box before E2; otherwise skip to E2
SAY BOX: “We are only interviewing people who are 18 years or older. Thank you very much for your time.” [DISCONTINUE INTERVIEW AND SKIP TO INTERVIEW COMPLETION.]
E2. Do you live in _______________ [USE INTERVIEW LOCATION FROM P5.]?
No
Yes……………………………………………Skip to E2b
7 Refused to answer……………………………Skip to Say box before E3
8 Don’t know…………………………………..Skip to Say box before E3
E2a. In which city and state do you live?
__________________ / _______________________
(City) (State)
7 Refused to answer
8 Don’t know
Interviewer instructions: Skip to Say box before E3.
E2b. What is your zip code?
__ __ __ __ __
777777 Refused to answer
888888 Don’t know
Interviewer note: If respondent does not have a permanent residence, use the zip code where he or she is currently residing.
Inconsistency check: E2b cannot be greater than 5 digits.
Interviewer instructions: Skip to E3.
SAY: “At this time we are only interviewing people who live in ____ [USE INTERVIEW LOCATION FROM P5]. Thank you very much for your time.” [DISCONTINUE INTERVIEW AND SKIP TO INTERVIEW COMPLETION SECTION.]
E3. What month and year did you first test positive for the human immunodeficiency virus ( HIV)? When I say “first test positive,” I mean the very first time you ever had a test result that was positive.
__ __ / __ __ __ __
M M Y Y Y Y
[Month: 77 = Refused to answer, 88= Don’t know;
Year: 7777 = Refused to answer, 8888 = Don’t know]
Interviewer note: If respondent has difficulty remembering the date, suggest key dates and seasons to narrow the time period (i.e. “Was it in the winter or summer?”)
Inconsistency check: E3 cannot be earlier than 03/1985 and cannot be later than current date.
SAY: “The next question is about medical care you may have received for HIV. When I say ‘HIV medical care’, I mean physical exams and lab tests such as HIV viral load and CD4 testing that can tell your doctor how fast the virus is multiplying and how your body is fighting the virus.”
E4. Since you tested positive for HIV, have you seen a doctor, nurse, or other heath care worker for HIV medical care?
No…………………………………………..Skip to Say box before D1
Yes
7 Refused to answer……………………….….Skip to Say box after E7a
8 Don’t know………………………………... Skip to Say box after E7a
E5. What month and year did you first see a doctor, nurse, or other health care worker for HIV medical care?
__ __ / __ __ __ __
M M Y Y Y Y
[Month: 77 = Refused to answer, 88= Don’t know;
Year: 7777 = Refused to answer, 8888 = Don’t know]
Inconsistency check: Confirm response if E5 is earlier than 03/1985. E5 cannot be later than current date.
Interviewer instructions: If E3 (date first tested positive) is later than E5, confirm dates in both E3 and E5. If E3 and E5 are the same date, go to E5a; otherwise, skip to E6.
E5a. You said that you got HIV medical care on the same day that you tested positive for HIV. Did you get any HIV medical care after [INSERT DATE FROM E5]?
0 No…………………………………………..Skip to Say box before D1
1 Yes
7 Refused to answer
8 Don’t know
E6. When you first went for HIV medical care, in what city and state did you get care? Please tell me the country if you received care outside the U.S.
__________________ / _____________________
(City) (State)
___________________________
(Country)
7 Refused to answer
8 Don’t know
Interviewer instructions: If respondent identifies a U.S. city and state, skip to E7.
E6a. Since you tested positive for HIV, have you seen a doctor, nurse, or other heath care worker for HIV medical care in the U.S.?
0 No…………………………………………..Skip to Say box before D1
1 Yes
7 Refused to answer………………………….Skip to Say box after E7a
8 Don’t know………………………………... Skip to Say box after E7a
E6b. When you first went for HIV medical care in the U.S., what city and state did you get care in?
__________________ / _____________________
(City) (State)
7 Refused to answer
8 Don’t know
E7. Since you tested positive for HIV, have you had a CD4 test or viral load test?
0 No
1 Yes
7 Refused to answer
8 Don't know
E7a. Since you tested positive for HIV, have you participated in an HIV clinical trial? When I say “HIV clinical trial,” I mean a study that tests how well new medications or other HIV treatments work in people.
0 No
1 Yes
7 Refused to answer
8 Don’t know
SAY: “At this time, we are only interviewing people who have never received medical care for their HIV infection in the U.S. Thank you very much for your time.” [OFFER INFORMATION AND RESOURCES ACCORDING TO PROTOCOL. DISCONTINUE INTERVIEW AND SKIP TO INTERVIEW COMPLETION SECTION.]
Demographics
SAY: Now I would like to ask you some questions about your background. The answers to some questions may seem obvious to you, but I need to ask you all of the questions.”
D1. In what country or territory were you born? [DON’T READ CHOICES. CHOOSE ONE.]
United States………………………………...Skip to D2
Puerto Rico…………………………………..Skip to D2
Mexico
Other (Specify:____________________________)
Refused to Answer…………………………Skip to D2
8 Don’t Know………………………………..Skip to D2
D1a. How many years have you been living in the United States?
__ __ __ (years)
777 Refused to answer
888 Don’t know
Interviewer instructions: If less than one year, enter “0.”
Inconsistency check: D1a cannot be less than 0 or greater than 106.
D2. What language or languages do you speak with your family and friends? [DON’T READ CHOICES. CHOOSE ALL THAT APPLY.]
1 English
2 Spanish
3 Arabic
4 Chinese
5 French
6 Hindi
7 Korean
8 Polish
9 Russian
10 Tagalog
11 Vietnamese
12 Other (Specify________________________________)
13 Other (Specify________________________________)
77 Refused to answer
88 Don’t know
D3. Do you consider yourself to be Hispanic or Latino/a?
No……………………………………….......Skip to D4
Yes
7 Refused to answer…………………………...Skip to D4
8 Don’t know…………………………………Skip to D4
D3a. What best describes your Hispanic ancestry? [DON’T READ CHOICES. CHOOSE ALL THAT APPLY.]
Mexican
Puerto Rican
Cuban
Dominican
Other (Specify:_________________)
Other (Specify:_________________)
7 Refused to answer
8 Don’t know
Interviewer instructions: If respondent indicates a non-Hispanic ethnicity say, “When I say Hispanic ancestry I mean your origins can be traced to Mexico, Puerto Rico, Cuba, Central or South America, or other Spanish cultures.”
D4. Which racial group or groups do you consider yourself to be in? You may choose more than one. [READ CHOICES. CHOOSE ALL THAT APPLY.]
Asian
Black or African American
American Indian or Alaskan Native
Native Hawaiian or other Pacific Islander
White
6 Other (Specify:_________________)
Other (Specify:_________________)
77 Refused to answer
88 Don’t know
D5. What is the highest level of education you completed? [DON’T READ CHOICES. CHOOSE ONE.]
1 Never attended school
2 Grades 1 through 8
3 Grades 9 through 11
4 Grade 12 or high school diploma equivalency (GED)
5 Some college, associate’s degree, or technical degree
6 Bachelor’s degree
7 Any post-graduate studies
77 Refused to answer
88 Don't Know
D6. What was your sex at birth? [READ CHOICES EXCEPT “INTERSEX/AMBIGUOUS” CHOOSE ONE.]
Male
Female
3 Intersex/ambiguous
7 Refused to answer
D7. Do you consider yourself to be male, female, or transgender? [CHOOSE ONE.]
Male
Female
Transgender
7 Refused to answer
8 Don’t know
D8. Do you think of yourself as? [READ CHOICES EXCEPT “OTHER.” CHOOSE ONE.]
Homosexual, Gay, or Lesbian
Heterosexual or Straight
Bisexual
4 Other (Specify____________________)
7 Refused to answer
8 Don't know
SAY: “Now I am going to ask you some questions about the past 3 months.
Interviewer instructions: Show respondent calendar.
D9. During the past 3 months, have you had any kind of health insurance or health care coverage? This includes Medicaid and Medicare.
0 No……………………………………………Skip to D10
1 Yes
7 Refused to answer……………………………Skip to D10
8 Don’t know…………………………………..Skip to D10
D9a. During the past 3 months, what are all the kinds of health insurance or health care coverage you have had? [DON’T READ CHOICES. CHOOSE ALL THAT APPLY.]
Private health insurance or health maintenance organization (HMO)
Medicaid
Medicare
Tricare or Champus
Veterans Administration or military coverage
Some other health insurance (Specify:____________)
Some other health insurance (Specify:____________)
77 Refused to answer
88 Don't know
Interviewer note: Interviewers should be aware of any local names of government insurance programs.
D9b. During the past 3 months, was there a time that you didn’t have any health insurance or health care coverage?
0 No
1 Yes
7 Refused to answer
8 Don't know
D10.
|
During the past 3 months, have you: |
No |
Yes |
Refused to answer |
Don’t know |
a. |
…lived on the street? |
|
|
|
|
b. |
…lived in a shelter? |
|
|
|
|
c. |
…lived in a Single Room Occupancy (SRO) hotel |
|
|
|
|
d. |
…lived in a car? |
|
|
|
|
e. |
…lived with friends? |
|
|
|
|
D11. During the past 3 months, have you been in jail, detention, or prison for longer than 24 hours?
0 No
1 Yes
7 Refused to answer
8 Don't know
D12 What best describes your current employment status? Are you: [READ CHOICES. CHOOSE ONE.]
1 Unemployed
2 Working occasionally
3 Employed part-time (less than 35 hours per week)
4 Employed full-time (35 or more hours per week)
5 A full-time homemaker
7 Refused to answer
8 Don’t know
D13 Are you currently a student?
0 No
1 Yes
7 Refused to answer
8 Don't know
SAY: “Now I would like to ask you some questions about 2006. That is January 1st, 2006 to December 31st, 2006.”
Interviewer instructions: Show respondent calendar.
D14 In 2006, where did most of your money or financial support come from? [DON’T READ CHOICES. CHOOSE ONE.]
Salary or Wages
Savings or investments
Pension or retirement fund
Social Security Supplemental Income or Disability Insurance (SSI or SSDI)
Public assistance (“welfare”)
Spouse, partner, or family
Friends
Illegal or possibly illegal activities
No income or financial support………………..Skip to Say box before C1a
Other (Specify:________________)
Refused to answer
88 Don’t know
D15 In 2006, what was your household income from all sources before taxes? [DON’T READ CHOICES.]
Interviewer note: Household income refers to the total amount of money from all people living in the household.
Interviewer instructions: Show Response Card A.
SAY: “Please take a look at this card and tell me either your monthly or yearly income.”
Monthly Income Yearly Income
1 $0 to $417 1 $0 to $4,999
2 $418 to $833 2 $5,000 to $9,999
3 $834 to $1250 3 $10,000 to $14,999
4 $1251 to $1667 4 $15,000 to $19,999
5 $1668 to $2500 5 $20,000 to $29,999
6 $2501 to $3333 6 $30,000 to $39,999
7 $3334 to $4167 7 $40,000 to $49,999
8 $4168 to $6250 8 $50,000 to $74,999
9 $6251 or more 9 $75,000 or more
77 Refused to answer 77 Refused to answer
88 Don’t Know 88 Don’t Know
D16 Including you, how many people depended on this income in 2006?
[MUST BE AT LEAST 1.]
___ ___
77 Refused to answer
88 Don’t know
Inconsistency check: D16 cannot be less than 1 or greater than 76.
Barriers to HIV Medical Care
SAY: Now I’m going to read you a list of reasons why some people don’t get HIV medical care. Please tell me if the following are reasons why you didn’t get HIV medical care during the past 3 months. Answer yes or no to each question.
|
Was one of the reasons you didn’t get HIV medical care during the past 3 months: |
No |
Yes |
Refused to answer |
Don’t know |
|
|
C1a. |
Because you felt good? |
|
|
|
|
|
|
C1b. |
Because you didn’t believe that you were infected with HIV? |
|
|
|
|
|
|
C1c. |
Because you didn’t want to think about being HIV positive? |
|
|
|
|
|
|
C1d. |
Because you didn’t want to tell anyone that you have HIV? |
|
|
|
|
|
|
C1e. |
Because you didn’t have enough money or health insurance? |
|
|
|
|
|
|
C1f. |
Because of responsibilities such as child care or work? |
|
|
|
|
|
|
C1g. |
Because you were living on the street, in a shelter, in a car, or in a SRO (single room occupancy hotel)? |
|
|
|
|
|
|
C1h. |
Because you felt depressed? |
|
|
|
|
|
|
C1i. |
Because you were drinking or using drugs? |
|
|
|
|
|
|
C1j. |
Because you felt too sick? |
|
|
|
|
|
|
C1k. |
Because there is no cure? |
|
|
|
|
|
|
C1l. |
Because you didn’t believe HIV causes acquired immune deficiency syndrome (AIDS)?
|
|
|
|
|
|
|
C1m. |
Because of religious reasons. |
|
|
|
|
|
|
C1n. |
Because you believed the medicines would do more harm than good or would be unpleasant? |
|
|
|
|
|
|
C1o. |
Because you shared HIV prescription medicines with someone else? |
|
|
|
|
|
|
C1p. |
Because you didn’t like or trust health care workers? |
|
|
|
|
|
|
C1q. |
Because you had trouble getting transportation to a clinic or doctor’s office? |
|
|
|
|
|
|
C1r. |
Because the location of the clinic or doctor’s office was inconvenient? |
|
|
|
|
|
|
C1s. |
Because the clinic hours were inconvenient? |
|
|
|
|
||
|
Was one of the reasons you didn’t get HIV medical care during the past 3 months: |
No |
Yes |
Refused to answer |
Don’t know |
||
C1t. |
Because you couldn’t get an appointment? |
|
|
|
|
||
Interview instructions: If response to D2 is “English,” skip to C2.
C1u. |
Because no one at the clinic or doctor’s office spoke your language? |
|
|
|
|
C2. Are there any other reasons why you didn’t get HIV medical care during the past 3 months?
0 No
1 Yes (Specify_____________________________________)
7 Refused to answer
8 Don't know
C3. Of all the reasons we just talked about, what was the main reason you didn’t get HIV medical care during the past 3 months? [DON’T READ CHOICES. CHOOSE ONLY ONE.]
1 Felt healthy
Denial of status
Avoidance of status
Disclosure issues
Lack of money or health insurance
Other responsibilities
Homelessness
Mental health
Substance use
Felt sick
No cure
Disbelief that HIV causes AIDS
Religious reasons
HIV medicines harmful or unpleasant
Sharing HIV prescription medications
Dislike or lack of trust in health care workers
Transportation problems
Inconvenient clinic hours
Inconvenient clinic location
Appointment not available
Language barrier
Other (Specify_________________________)
Refused to answer
88 Don’t know
C4. How likely is it that you will start HIV medical care within the next 3 months? [READ CHOICES. CHOOSE ONE. SHOW RESPONSE CARD D.]
1 Very unlikely to start care within the next 3 months
2 Fairly unlikely to start care within the next 3 months
3 Fairly likely to start care in within the next 3 months
4 Very likely to start care in within the next 3 months…Skip to Say box before N1
7 Refused to Answer……………………………………Skip to Say box before N1
8 Don’t know……………………………………………Skip to Say box before N1
C4a. What, if anything, would make you more likely to start HIV medical care within the next 3 months? You may give more than one answer. [DON’T READ CHOICES. CHOOSE ALL THAT APPLY.]
1 If respondent felt sick
2 Sufficient money or health insurance
3 Concerns addressed about status being disclosed
4 Other responsibilities covered
5 Stable living situation
6 Sound mental health
7 Substance use recovery
8 Cure for HIV/AIDS discovered
9 HIV medicines that are not harmful or unpleasant
10 Likeable or trustworthy health care workers
11 Transportation available
12 Convenient clinic hours
13 Convenient clinic location
14 Available appointments
15 Services available in respondent’s primary language
16 Nothing would make the respondent more likely to start HIV care
17 Other (Specify_________________________)
Refused to answer
88 Don’t know
Interviewer instructions: If C4a is “Refused to answer,” “Don’t know,” or “Nothing would make the respondent more likely to start HIV care,” skip to Say box before N1. If there is only one response for C4a, skip to Say box before N1.
C4b. Of the answers you just gave, what is the most important one? [DON’T READ CHOICES. CHOOSE ONLY ONE.]
1 If respondent felt sick
2 Sufficient money or health insurance
3 Concerns addressed about status being disclosed
4 Other responsibilities covered
5 Stable living situation
6 Sound mental health
7 Substance use recovery
8 Cure for HIV/AIDS discovered
9 HIV medicines that are not harmful or unpleasant
10 Likeable or trustworthy health care workers
11 Transportation available
12 Convenient clinic hours
13 Convenient clinic location
14 Available appointments
15 Services available in respondent’s primary language
16 Other (Specify_________________________)
77 Refused to answer
88 Don’t know
Unmet Need
SAY: “Now I’m going to ask about services you used or needed during the past 3 months.” [SHOW RESPONDENT CALENDAR]
Interviewer instructions: If response to N1a is “No,” go to N1b; otherwise, skip to N2a. If response to N1b is “Yes,” go to N1c; otherwise, skip to N2a. Follow the same pattern for N1–N18.
|
|
During the past 3 months, did you get: |
IF “NO” IN N1A–N18A, ASK: During the past 3 months, have you needed: |
IF “YES” IN N1B–N18B, ASK: What was the main reason you haven’t been able to get this service during the past 3 months? |
|
|
CODE: No = 0, Yes = 1, Refused to answer= 7, Don’t know = 8 |
CODE: No = 0, Yes = 1, Refused to answer= 7, Don’t know = 8 |
CODE: SEE CODE LIST BELOW FOR RESPONSES. [DON’T READ CHOICES. CHECK ONLY ONE]
|
N1. |
Medical care for any reason
|
a. [______] |
b. [______] |
c. [______] |
N2. |
HIV case management services
|
a. [______] |
b. [______] |
c. [______] |
N3. |
Education or information about HIV
|
a. [______] |
b. [______] |
c. [______] |
N4.
|
HIV peer group support
|
a. [______] |
b. [______] |
c. [______] |
N5. |
Dental care
|
a. [______] |
b. [______] |
c. [______] |
N6. |
Mental health services |
a. [______] |
b. [______] |
c. [______]
|
N7. |
Drug or alcohol counseling or treatment |
a. [______] |
b. [______] |
c. [______]
|
N8. |
Public benefits including Supplemental Security Income (SSI) or Social Security Disability Insurance (SSDI)
|
a. [______] |
b. [______] |
c. [______]
|
N9. |
Transportation assistance
|
a. [______] |
b. [______] |
c. [______] |
N10. |
Domestic violence services |
a. [______] |
b. [______] |
c. [______]
|
N11. |
Shelter or housing services
|
a. [______] |
b. [______] |
c. [______]
|
N12. |
Home health services
|
a. [______] |
b. [______] |
c. [______] |
N13. |
Meal or food services
|
a. [______] |
b. [______] |
c. [______]
|
N14. |
Job placement or training
|
a. [______] |
b. [______] |
c. [______] |
N15. |
Childcare services
|
a. [______] |
b. [______] |
c. [______] |
Interviewer instructions: If response to D2 is “English,” skip to N17.
N16. |
Interpreter services |
a. [______] |
b. [______] |
c. [______]
|
N17. |
Legal assistance |
a. [______] |
b. [______] |
c. [______]
|
N18. |
Other HIV-related services (Specify:____________)
|
a. [______] |
b. [______] |
c. [______]
|
Interviewer instructions: For N1c–N18c: [DON’T READ CHOICES. CHECK ONLY ONE.]
1 Didn’t know where to go or whom to call
2 Didn’t complete application process
3 Waiting list is too long
4 Service isn’t available
5 Not eligible or denied services
6 Service hours are inconvenient
7 Service costs too much/lack of insurance
8 Transportation problems
9 Language barrier
10 Too sick to get service
11 Other (Specify____________________)
77 Refused to answer
88 Don’t know
HIV Testing
SAY: “Now I am going to ask you some questions about getting tested for HIV. To begin, I will ask questions about the first time you tested positive. Earlier you told me that you first tested positive on [INSERT RESPONSE FROM E3]. These next questions refer to that test.”
H1. The first time you tested positive, where were you tested for HIV?
[READ CHOICES. CHOOSE ONE. SHOW RESPONSE CARD E.]
1 HIV counseling and testing site
2 Sexually transmitted disease (STD) clinic
3 HIV/AIDS or infectious disease clinic
4 Tuberculosis (TB) clinic
5 Drug and alcohol treatment clinic
6 Prenatal or family planning clinic
7 Private physician or HMO
8 Community health center
9 Health department
10 Mobile test site (health department van, needle exchange, etc.)
11 Emergency room
12 Inpatient hospital
13 Outpatient hospital
14 Jail, prison, or detention facility
15 Blood bank
16 Homeless shelter
17 Military facility
18 Other (Specify:________________)
77 Refused to answer
88 Don’t know
H1a. In what city and state did you get this test? If the first time you tested positive was outside the U.S., please tell me the country where you were tested.
__________________ / _____________________
(City) (State)
___________________________
(Country)
7 Refused to answer
8 Don’t know
H2. The first time you tested positive, did someone else recommend you get tested, did you decide to get tested yourself, or was the test required? [READ CHOICES. CHOOSE ONE.]
1 Someone else recommended it
2 You decided yourself to get tested…………..Skip to H3
3 The test was required………………………..Skip to H2b
7 Refused to answer………………………….. Skip to H3
8 Don’t know………………………………….Skip to H3
H2a. The first time you tested positive, who recommended you get tested? [DON’T READ CHOICES. CHOOSE ALL THAT APPLY.]
Doctor, nurse, or other health care worker
Sexual partner
Family member or friend
Someone from the health department (partner notification)
Counselor
Peer educator
Other (Specify:___________________________)
Other (Specify:___________________________)
Refused to answer
Don’t know
Interviewer instructions: Skip to H4
H2b. The first time you tested positive, why were you required to get this test? [DON’T READ CHOICES. CHOOSE ONE.]
Insurance
Military
Jail
Hospitalization
Employment
Blood donation
Immigration
Ordered by the court
Other (Specify:____________________________)
Refused to answer
Don’t know
Interviewer instructions: Skip to H4
H3. The first time you tested positive, what was the main reason you decided to get tested? [DON’T READ CHOICES. CHOOSE ONE.]
Was ill
Was an injection drug user (IDU)
Man who had sex with men (MSM)
Had multiple sex partners
Wanted to stop using condoms with partner(s)
Was worried about infecting sex partner(s)
Sex partner was worried I might have HIV
Sex partner was HIV positive
Sex partner was an IDU
Sex partner was a MSM
Sex partner had multiple sex partners
Needle sharing partner was HIV positive
Friends were getting tested
Needle stick follow-up or occupational exposure
Offered as a screening test at a clinic (like STD, family planning, etc.)
Routine check-up or physical exam
Pregnancy
Paid to get tested
Read, saw, or heard something that made the respondent want to get tested
Wanted to know status
Other (Specify:__________________________)
Refused to answer
Don’t know
H4. The first time you tested positive, what type of test did you have? [READ CHOICES. CHOOSE ONE.]
1 An anonymous test, where you didn’t give your name or you used a code
2 A confidential test, where you gave your name for identification
7 Refused to answer
8 Don’t know
H4a. Was this test a rapid test where you got your results the same day?
No
Yes
7 Refused to answer
8 Don’t know
SAY: “Now I would like to ask you some questions about your experience with an HIV counselor.
Interviewer note: Questions H5–H9 refer to HIV post-test counseling. If the respondent has difficulty with the term ‘counselor’, say: “When I say ‘counselor’ I mean someone who may have spoken with you about your infection when you were first told you tested positive for HIV, such as a trained advisor or health care worker.”
H5. When you were first told you tested positive for HIV, did you receive counseling?
No…………………………………………..Skip to Say box before B1
Yes
7 Refused to answer………………………….Skip to Say box before B1
8 Don’t know………………………………...Skip to Say box before B1
H6. Did you feel your counselor spent enough time with you?
0 No
1 Yes
7 Refused to answer
8 Don’t know
H7. When you were first told you tested positive for HIV, were you told where you could go for HIV medical care?
0 No
1 Yes
7 Refused to answer
8 Don’t know
H8. When you were first told you tested positive for HIV, did anyone try to help you get into HIV medical care?
0 No………………………………………….Skip to H9
1 Yes
7 Refused to answer………………………….Skip to H9
8 Don’t know………………………..……….Skip to H9
H8a. Who was that person or persons? [DON’T READ CHOICES. CHOOSE ALL THAT APPLY.]
1 A counselor
2 A social worker
3 A case manager or other professional
4 A family member or friend
5 Other (Specify___________________________)
6 Other (Specify___________________________)
7 Refused to answer
8 Don’t know
Interviewer instructions: Skip to Say box before B1.
H9. Has anyone ever tried to help you get into HIV medical care?
0 No………………………………………….Skip to Say box before B1
1 Yes
7 Refused to answer………………………….Skip to Say box before B1
8 Don’t know………………………..……….Skip to Say box before B1
H9a. Who was that person or persons? [DON’T READ CHOICES. CHOOSE ALL THAT APPLY.]
1 A counselor
2 A social worker
3 A case manager or other professional
4 A family member or friend
5 Other (Specify___________________________)
6 Other (Specify___________________________)
7 Refused to answer
8 Don’t know
Care-Seeking Behavior
SAY: “Now, I’m going to ask you some questions about any health care you may have received in the past.”
B1. Have you ever seen a doctor, nurse, or other health care worker for any medical problem other than HIV?
0 No…………………………………………..Skip to Say box before B6
1 Yes
7 Refused to answer…………………………. Skip to Say box before B6
8 Don’t know………………………………… Skip to Say box before B6
B1a. What month and year did you last see a doctor, nurse, or other health care worker for any medical problem other than HIV?
__ __ / __ __ __ __
M M Y Y Y Y
[Month: 77 = Refused to answer, 88= Don’t know;
Year: 7777 = Refused to answer, 8888 = Don’t know]
Interviewer note: If respondent has difficulty remembering the date, suggest key dates and seasons to narrow the time period (i.e. “Was it in the winter or summer?”)
Inconsistency check: B1a cannot be earlier than the respondent’s date of birth (E1) or later than current date.
B2. Has a doctor, nurse, or other health care worker ever told you that you had hepatitis?
0 No…………………………………………..Skip to Instructions before B3
1 Yes
7 Refused to answer…………………………. Skip to Instructions before B3
8 Don’t know………………………………… Skip to Instructions before B3
B2a. What type or types of hepatitis have you had? [READ CHOICES.]
|
|
No |
Yes |
Refused to answer |
Don’t know |
a. |
Hepatitis A
|
|
|
|
|
b. |
Hepatitis B
|
|
|
|
|
c. |
Hepatitis C
|
|
|
|
|
d. |
Other(Specify:__________)
|
|
|
|
|
e. |
Other(Specify:__________)
|
|
|
|
|
Interviewer instructions: If response to B1a is more than 3 months from date of interview (P6), skip to B5.
SAY: “Now I am going to ask you some questions about the past 3 months.” [SHOW RESPONDENT CALENDAR.]
B3. During the past 3 months, how many times did you go to an emergency room or urgent care center for any care?
___ ___
777 Refused to answer
888 Don’t know
Interviewer note: Urgent care is defined as the delivery of care outside of a hospital emergency department on a walk-in basis. Urgent care centers include private medical centers and facilities intended for episodic treatment of medical conditions and not ongoing care.
Inconsistency check: B3 cannot be less than 0 or greater than 90.
B4. During the past 3 months, how did you pay for your medical costs? [DON’T READ CHOICES. CHOOSE ALL THAT APPLY.]
2 Paid out of pocket
3 Family or friend paid out of pocket
4 Private health insurance or HMO
5 Medicaid
6 Medicare
7 Tricare or Champus
8 Veterans Administration or military coverage
9 Other (Specify:______________________)
10 Other (Specify:______________________)
77 Refused to answer
88 Don't know
B5. Do you have a place where you usually go to see a doctor, nurse, or other health care worker when you are sick?
0 No……………………………………………Skip to Say box before B7
1 Yes
7 Refused to answer……………………………Skip to Say box before B7
8 Don’t know…………………………………..Skip to Say box before B7
B6. Do you have one person you think of as your personal doctor, nurse, or other health care worker?
0 No……………………………………………Skip to Say box before B7
1 Yes
7 Refused to answer……………………………Skip to Say box before B7
8 Don’t know…………………………………..Skip to Say box before B7
B6a. Has this person ever talked to you about HIV?
0 No…………………………………………....Skip to Say box before B7
1 Yes
7 Refused to answer……………………………Skip to Say box before B7
8 Don’t know……………………………..…....Skip to Say box before B7
B6b. Do you trust what this person has told you about HIV?
0 No
1 Yes
7 Refused to answer
8 Don’t know
SAY: “Now I would like to ask you about complementary and alternative medicines. These are products (such as herbs) or practices (such as yoga). Although many people use these therapies, it is uncertain whether they are safe or work for HIV.”
B7. Since you tested positive for HIV, have you taken or used any of the following complementary or alternative therapies specifically for your HIV infection?
|
|
No |
Yes |
Refused to answer |
Don’t know |
a. |
Traditional Chinese medicine including acupressure or acupuncture |
|
|
|
|
b. |
Vitamins, minerals, or herbs |
|
|
|
|
c. |
Yoga or massage |
|
|
|
|
d. |
Chiropractic |
|
|
|
|
e. |
Mind-body techniques including relaxation, hypnosis, visualization |
|
|
|
|
f. |
Spiritual healing by others |
|
|
|
|
g. |
Homeopathy |
|
|
|
|
h. |
Medicines from outside the U.S. |
|
|
|
|
i. |
Marijuana |
|
|
|
|
j. |
Energy healing such as biofeedback, magnets, or electric fields. |
|
|
|
|
k. |
Other (Specify:_______________)
|
|
|
|
|
Social Relationships
SAY: “Now I’d like to ask you some questions about people who might help or support you.”
S1. Do you personally know anyone who has HIV or AIDS, or who died of AIDS?
0 No…………………………………Skip to S2
1 Yes
7 Refused to answer…………………Skip to S2
8 Don’t know ……………………….Skip to S2
S1a. What is your relation to this person or these people? [READ CHOICES. CHOOSE ALL THAT APPLY.]
1 Family member(s)
2 Friend(s)
3 Other person(s)
7 Refused to answer
8 Don’t know
S2. Have you ever told anyone that you are HIV positive?
0 No……………………………………………Skip to S3
1 Yes
7 Refused to answer……………………………Skip to S3
8 Don’t know…………………………………..Skip to S3
S2a. Not including health care workers, how many people have you told that you are HIV positive? [READ CHOICES. CHOOSE ONE. SHOW RESPONSE CARD F.]
1 None
2 One person
3 2–5 people
4 6–10 people
5 More than 10 people
7 Refused to answer
8 Don’t know
S2b. Not including health care workers, who have you told that you are HIV positive? [READ CHOICES. CHOOSE ALL THAT APPLY.]
1 Family member(s)
2 Friend(s)
3 Other person(s)
7 Refused to answer
8 Don’t know
S3. SAY: “People sometimes look to others for companionship, assistance, or other types of support. Please tell me how often the following kinds of support are available to you if you need it. Would you say this is available never, rarely, about half the time, most of the time, or always?”
Interviewer instructions: Show Response Card G.
|
|
Never |
Rarely |
About half the time |
Most of the time |
Always |
Refused to answer |
Don’t know |
||
a. |
Someone to give you good advice about a crisis. |
|
|
|
|
|
|
|
||
b. |
Someone to confide in or talk to about yourself or your problems. |
|
|
|
|
|
|
|
||
c. |
Someone who understands your problems. |
|
|
|
|
|
|
|
||
Mode of Infection
SAY: “Now I am going to ask you some questions about how you might have gotten HIV. To begin, I am going to ask you about having sex. For these questions, ‘having sex’ means oral sex (mouth on the vagina or penis), vaginal sex (penis in the vagina), or anal sex (penis in the anus).”
M1.
|
Before you tested positive for HIV, did you: |
No |
Yes |
Refused to answer |
Don’t know |
|
a. |
…have sex with a man without a condom? |
|
|
|
|
|
b. |
…have sex with a woman without a condom? |
|
|
|
|
|
c. |
…have sex without a condom with someone who had HIV? |
|
|
|
|
|
d. |
…receive a blood transfusion or organ transplant? |
|
|
|
|
|
e. |
…have sex without a condom with someone who received a blood transfusion? |
|
|
|
|
|
f. |
…receive blood products for a bleeding disorder? |
|
|
|
|
|
g. |
…have sex without a condom with someone who received blood products for a bleeding disorder? |
|
|
|
|
|
h. |
…work in a health care setting where you may have been exposed to blood? |
|
|
|
|
|
i. |
…shoot up or inject any drugs that weren’t used for medical purposes? |
|
|
|
|
|
j. |
… have sex without a condom with someone who shot up or injected any drugs that weren’t used for medical purposes? |
|
|
|
|
|
|
|
|
|
|
|
|
Interviewer instructions: If M1i is “Yes,” go to M2; otherwise skip to end of interview.
M2. In the past 3 months, have you shot up or injected any drugs that weren’t used for medical purposes?
No
1 Yes
7 Refused to answer
8 Don’t know
Health and Well-Being
SAY: “The next questions ask for your views about your overall health; not just related to HIV. This information will help keep track of how you feel and how well you are able to do your usual activities.”
W1. In general, would you say your health is:
Excellent |
Very good |
Good |
Fair |
Poor |
|
|
|
|
|
1 |
2 |
3 |
4 |
5 |
[7 = Refused to answer]
W2. The following questions are about activities you might do during a typical day. Does your health now limit you in these activities? If so, how much?
-
Yes,
limited
a lot
Yes,
limited
a little
No, not
limited
at all



a Moderate activities, such as moving a table,
pushing a vacuum cleaner, bowling, or
playing golf? 1 2 3
b Climbing several flights of stairs? 1 2 3
[7 = Refused to answer]
W3. During the past 4 weeks, how much of the time have you had any of the following problems with your work or other regular daily activities as a result of your physical health?
-
All of the time
Most of the time
Some of the time
A little of the time
None of the time





a Accomplished less than you would
like? 1 2 3 4 5
b Were limited in the kind of work or
other activities? 1 2 3 4 5
[7 = Refused to answer]
W4. During the past 4 weeks, how much of the time have you had any of the following problems with your work or other regular daily activities as a result of any emotional problems (such as feeling depressed or anxious)?
-
All of the time
Most of the time
Some of the time
A little of the time
None of the time





a Accomplished less than you would like? 1 2 3 4 5
b Did work or other activities less
carefully than usual? 1 2 3 4 5
[7 = Refused to answer]
W5. During the past 4 weeks, how much did pain interfere with your normal work (including both work outside the home and housework)?
Not at all |
A little bit |
Moderately |
Quite a bit |
Extremely |
|
|
|
|
|
1 |
2 |
3 |
4 |
5 |
[7 = Refused to answer]
W6. These questions are about how you feel and how things have been with you during the past 4 weeks. For each question, please give the one answer that comes closest to the way you have been feeling. How much of the time during the past 4 weeks...
-
All of the time
Most of the time
Some of the time
A little of the time
None of the time





a Have you felt calm and peaceful? 1 2 3 4 5
B Did you have a lot of energy? 1 2 3 4 5
C Have you felt downhearted and depressed?1 2 3 4 5
[7 = Refused to answer]
W7. During the past 4 weeks, how much of the time has your physical health or emotional problems interfered with your social activities (like visiting friends, relatives, etc.)?
All of the |
Most of the |
Some of the |
A little of the |
None of the |
|
|
|
|
|
1 |
2 |
3 |
4 |
5 |
[7 = Refused to answer]
Time questionnaire ended:
Time questionnaire ended:
__ __: __ __ AM PM
Interview Completion
SAY: “Thank you again for taking part in this survey. Please remember that all the information you have given me will be kept private. ”
Interviewer instructions:
Ask if the respondent has any questions.
Offer information and resources as indicated in the protocol.
If the interview was discontinued because the respondent is < 18 years old, lives outside the survey area, has received medical care for HIV, or has never been told his/her HIV status, don’t pay the respondent.
If the interview was discontinued because the interview was partially or fully completed, pay the respondent and have him/her sign the receipt.
SAY: “To learn how to make HIV services better and more available to people living with HIV/AIDS in this community, we would like to talk with others in your community. If you know anyone who is HIV infected and has never had medical care for their HIV infection, we ask that you tell them about this project if you are comfortable doing so, and encourage them to call us about taking part in the survey. If a person you have told about the project calls us, we will check to see if he or she is eligible to be interviewed. If you wish, we have written information about this project that we can give you now to give others who might be interested in telling us about their experiences.“
Interviewer Instructions: Give the respondent enough copies of the flyer about NIC to give to others he/she is considering referring to the project.
Interviewer: Please enter the following items after completion of the interview. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Payment Verification
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
________________________________________________________________________________________ |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
________________________________________________________________________________________ |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
________________________________________________________________________________________ |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
________________________________________________________________________________________ |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
________________________________________________________________________________________ |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
________________________________________________________________________________________ |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
________________________________________________________________________________________ |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Attachment 2b. Qualitative Interview Guide and Observation Form
Never in Care Project (NIC)
2007 Qualitative Interview
VERSION 1.3
Public reporting burden of this collection of information is estimated to average 60 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not required to respond to a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden to: CDC, Project Clearance Officer, 1600 Clifton Road, MS D-24, Atlanta, GA 30333, ATTN: PRA (0920-0011). Do not send the completed form to this address.
DEPARTMENT OF HEALTH AND HUMAN SERVICES
Public Health Service
Centers for Disease Control and Prevention
Atlanta, GA 3033


Never in Care (NIC) 2007 Qualitative Interview
Interviewer instructions: Offer the respondent a short break before starting the qualitative interview. During the break, complete the preliminary information.
PRELIMINARY INFORMATION
P1. Interviewer: Check all responses listed in the handheld or laptop device located at the end of the standard questionnaire.
|
Reponses from 2007 NIC standard questionnaire and corresponding question number:
|
Included |
a. |
Health insurance coverage during the past 3 months (D9) |
|
b. |
Gaps in health insurance coverage during the past 3 months (D9b) |
|
c. |
Incarcerated during the past 3 months (D11) |
|
d. |
Currently unemployed (D12) |
|
e. |
Barriers to HIV care and health (C1a, C1j) |
|
f. |
Barriers to HIV care and denial of HIV status (C1b) |
|
g. |
Barriers to HIV care and avoidance of HIV status or disclosure issues (C1c, C1d) |
|
h. |
Barriers to HIV care and economics (C1e) |
|
i. |
Barriers to HIV care and other responsibilities (C1f) |
|
j. |
Barriers to HIV care and homelessness (C1g) |
|
k. |
Barriers to HIV care and substance use (C1i) |
|
l. |
Barriers to HIV care and religious reasons (C1m) |
|
m. |
Barriers to HIV care and mistrust or dislike of HIV medicines (C1n) |
|
n. |
Barriers to HIV care and mistrust or dislike of health care professionals (C1p) |
|
o. |
Barriers to HIV care and health facilities (C1q, C1r, C1s, C1t, C1u) |
|
p. |
Assistance accessing HIV care (H9) |
|
q. |
ER or urgent care visits in the past 3 months (B3) |
|
P2. NIC ID No: __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __ __
P3. Interviewer ID: ___ ___
P4. Interview date: __ __ /__ __ / __ __ __ __
M M D D Y Y Y Y
P5. Time interview began: __ __: __ __ AM PM
SAY: “I’d like to thank you for taking part in this interview. This interview is different from the one we just finished. I’ll ask you some questions and I want you to describe your thoughts and experiences. When we are ready to start, I will turn on a tape recorder to record our voices as we talk. Remember that all the information you give me will be private and your name will not be recorded anywhere. Please let me know if you have any questions [PAUSE FOR QUESTIONS]. I’d like to start the tape recorder now.”
Interviewer instructions: Keep in mind that respondents may not distinguish between the health care system, health professionals, and HIV medical care.
Topic: Health Care System
Q1. Tell me how you feel about medical care in the United States (U.S.)?
PROBE: positive and negative attitudes
EXAMPLE: Describe what is good and bad about medical care in the U.S.
PROBE: previous experiences
EXAMPLE: Tell me about the good and bad experiences you’ve had with medical care in the U.S.
PROBE: influence getting into care
EXAMPLE: How have your experiences with medical care in the U.S. influenced your decision to get HIV medical care?
IF NO EXPERIENCES: word of mouth
EXAMPLE: What have you heard from others about medical care in the U.S.?
Topic: Health Professionals
Q2. Tell me how you feel about health care workers.
PROBE: positive and negative experiences with health care providers
EXAMPLE: Tell me about the good and bad experiences you’ve had with a health care workers.
PROBE: influence getting into care
EXAMPLE: How have your experiences with a health care worker influenced your decision to get HIV medical care?
Interviewer instructions: If P1n is checked, then go to probe 1; otherwise, skip to probe 2.
PROBE 1: mistrust of health professionals
EXAMPLE: Earlier you said you don’t like or trust health care workers. What is it about them that you don’t like or trust?
PROBE 2: attitude about HIV care providers
EXAMPLE: How do you feel about the health care providers who treat people living with HIV?
Topic: HIV Medical Care
Q3. Tell me how you feel about HIV medical care.
PROBE: attitude about HIV medical care
EXAMPLE: Describe what is good and bad about HIV medical care.
PROBE: word of mouth
EXAMPLE: Tell me what you’ve heard about HIV medical care.
PROBE: barrier to care
EXAMPLE: How has this influenced your decision to get HIV medical care?
Q4. In your opinion, what are the advantages or disadvantages of getting into HIV medical care?
PROBE: outlook on getting into care within 3 months of diagnosis date
EXAMPLE: What are the advantages or disadvantages of getting into HIV medical care within 3 months of testing positive?
Topic: HIV Therapy
Q5. What have you heard about the medicines used for HIV?
PROBE: positive or negative outlook about HIV medications
EXAMPLE: Have you heard anything good or bad about the medicines used for HIV?
PROBE: people who use HIV medications
EXAMPLE: Do you know anyone who has used HIV medicines?
IF YES: Have you heard anything good or bad from those who have used HIV medicines?
Q6. What kind of treatment, if any, do you feel you should use for your HIV?
IF NO TREATMENT: rational for no treatment
EXAMPLE: Why do you feel that you shouldn’t use any treatment?
IF TREATMENT: perceived outcome of treatment
EXAMPLE: What do you feel this treatment will do for you?
PROBE: behaviors to minimize HIV infection
Example: Are there other things you do to take care of yourself and keep your HIV infection in check?
Topic: Barriers to Care
Interviewer instructions: If P1h is checked, then go to Q7; otherwise, skip to interviewer instructions before Q8.
Q7. Earlier, you said that you didn’t get into HIV medical care because you didn’t have enough money or health insurance. Tell me more about how this has kept you from getting into HIV care.
Interviewer instructions: If P1a and/or P1b are checked, then go to Q8; otherwise, skip to interviewer instructions before Q9.
Q8. Earlier, you said that in the past 3 months you didn’t have any or enough health insurance. What are the reasons that you didn’t have health insurance?
PROBE: lack of health insurance as a barrier to care
EXAMPLE: Did not having health insurance keep you from getting HIV medical care?
IF YES: How so?
Interviewer instructions: If P1j is checked, then go to Q9; otherwise, skip to interviewer instructions before Q10.
Q9. Earlier, you said that you didn’t get into HIV care because you were living on the street, in a shelter, in a car, or in a SRO (single room occupancy) hotel. Tell me more about this.
PROBE: homelessness as a barrier to care
EXAMPLE: How did your living situation keep you from getting into care?
Interviewer instructions: If P1d is checked, then go to Q10; otherwise, skip to interviewer instructions before Q11.
Q10. Earlier you said that you are currently unemployed. How has your unemployment status affected your HIV?
Interviewer instructions: If P1c is checked, then go to Q11; otherwise, skip to interviewer instructions before Q12.
Q11. Earlier you said that you have been in jail, detention, or prison during the past 3 months. Tell me what it is like to have HIV in jail, detention, or prison?
PROBE: care system in incarcerated settings
EXAMPLE: Tell me about the HIV medical care available in jail, detention, or prison.
PROBE: quality of care
EXAMPLE: What do you think about the quality of care given to people with HIV in jail, detention, or prison?
Interviewer instructions: If P1e is checked, then go to Q12; otherwise, skip to interviewer instructions before Q13.
Q12. Earlier you said that you did not get into HIV medical care because of reasons related to your health. Tell me more about your state of health.
PROBE: health as a barrier to care
EXAMPLE: Tell me how your health has affected getting into HIV medical care.
Interviewer instructions: If P1o is checked, then go to Q13; otherwise, skip to interviewer instructions before Q14.
Q13. Earlier you said that you didn’t get into HIV medical care because of reasons related to a health facility. Tell me about this facility.
PROBE: previous experiences
EXAMPLE: Tell me about any good or bad experiences that you’ve had with this facility.
PROBE: word-of-mouth
EXAMPLE: Tell me what you’ve heard about this facility or other facilities like it that offer HIV medical care.
Interviewer instructions: If P1i is checked, then go to Q14; otherwise, skip to interviewer instructions before Q15.
Q14. Earlier you said that you didn’t get into HIV medical care because of other responsibilities. Tell me more about your other responsibilities.
Topic: Accessing Care
Interviewer instructions: If P1p is checked, then go to Q15; otherwise, skip to interviewer instructions before Q16.
Q15. Earlier you said that someone tried to get you into HIV care. How did you feel when this person tried to get you into care?
Interviewer instructions: If P1q is checked, then go to Q16; otherwise, skip to Q17.
Q16. Earlier you said that you have been to the emergency room or urgent care clinic in the past 3 months. Tell me about those experiences and why you decided to go to the emergency room or urgent care clinic?
Q17. If you wanted HIV medical care, what kinds of things would you need or want in order to get it?
PROBE: physical needs
EXAMPLE: How important to you is HIV medical care compared to other things that you need right now?
Topic: Perceived Etiology of HIV
Interviewer instructions: If P1f is checked, then go to Q18; otherwise, skip to Q19.
Q18. Earlier you said that you didn’t believe you had HIV. Why do you feel that you don’t have HIV?
Interviewer instructions: Skip to next topic.
Q19. How do you think you got HIV?
PROBE: reason for onset
EXAMPLE: Why do you think your HIV started when it did?
Topic: Illness Perceptions
Q20. How did you feel when you first learned you were HIV positive?
PROBE: feelings about status
EXAMPLE: How do you feel now about being HIV positive?
PROBE: barrier to HIV care
EXAMPLE: Has this affected your decision to get into HIV care?
Topic: Stigma
Q21. In your opinion, what do others think about people with HIV?
Q22. What do you think about people with HIV?
Topic: Access to HIV Information
Q23. If you wanted information about HIV, how would you get it?
PROBE: place
EXAMPLE: Where would you go to get information?
PROBE: person
EXAMPLE: Who would you talk with?
Q24. Is there anything else that you can tell me to help me understand why some people don’t get HIV medical care?
SAY: “We’re finished. Thank you very much for talking to me. Remember, everything you told me will be kept private. Do you have any questions about HIV, HIV care, or anything that we’ve discussed here today?”
Time interview ended: __ __: __ __ AM PM
OMB Number:
Expiration Date:
Observation Form for the Qualitative Interview
Never in Care Project (NIC)
Public reporting burden of this collection of information is estimated to average 10 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not required to respond to a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden to: CDC, Project Clearance Officer, 1600 Clifton Road, MS D-24, Atlanta, GA 30333, ATTN: PRA (0920-0011). Do not send the completed form to this address.
DEPARTMENT OF HEALTH AND HUMAN SERVICES
Public Health Service
Centers for Disease Control and Prevention
Atlanta, GA 3033


Observation Form for the Qualitative Interview
Record your observations of the interview setting. This may include information such as a description of the interview location or any external interruptions during the interview.
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
Record your observations and perceptions of the respondent. This may include information about the respondent’s behavior during the interview, resistance to answering the questions, comprehension of the questions, or mental and physical state:
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
Record your observations about the respondent’s rapport with the interviewer. This may include whether the respondent was engaged or distant during the interview.
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
How confident are you of the validity of the respondent’s answers?
________________________________________________________________________
Attachment 2c. 2007 Non-Response Data Collection Form
|
NON-RESPONSE DATA COLLECTION FORM
VERSION 1.3
Public reporting burden of this collection of information is estimated to average 5 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not required to respond to a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden to: CDC, Project Clearance Officer, 1600 Clifton Road, MS D–24, Atlanta, GA 30333, ATTN: PRA (0920–0011). Do not send the completed form to this address.
DEPARTMENT OF HEALTH AND HUMAN SERVICES
P


Centers for Disease Control and Prevention
Atlanta, GA 30333
Collect the following information for all persons selected for NIC who do not participate in the NIC interview. You may obtain this information from the HIV AIDS Reporting System (HARS) or any other surveillance database.
Never In Care (NIC) Identification No: ___ ___ ___ ___
Date Form Completed: ___ ___ / ___ ___ / ___ ___ ___ ____
m m d d y y y y
Data Sources: |
|
|
|
1 |
HARS
|
|
2 |
Other (Specify:_________________) |
Date of Birth: ___ ___ / ___ ___ / ___ ___ ___ ____
m m d d y y y y
First positive HIV antibody test:
Age: ___ ___ Date: ___ ___ / ___ ___ ___ ___
m m y y y y
First AIDS diagnosis:
Age: ___ ___ Date: ___ ___ / ___ ___ ___ ___
m m y y y y
Sex: |
1 |
Male |
|
2 |
Female |
Ethnicity:
(select one) |
1 |
Hispanic/Latino |
|
2 |
Not Hispanic/ Not Latino |
|
8 |
Unknown |
Race: |
1 |
American Indian or Alaska Native |
(select all that apply) |
2 |
Black or African American |
|
3 |
Asian |
|
4 |
Native Hawaiian or Other Pacific Islander |
|
5 |
White |
|
8 |
Unknown
|
Country of Birth: |
1 |
U.S. |
|
2 |
U.S. Dependencies and Possessions (including Puerto Rico) |
|
3 |
Other (Specify): __________________________________ |
|
8 |
Unknown |
Mode of HIV Exposure
|
Yes |
No |
Unknown |
Sex with male…………………………………. |
1 |
0 |
8 |
Sex with female……………………………….. |
1 |
0 |
8 |
Injected nonprescription drugs ……………….. |
1 |
0 |
8 |
Heterosexual intravenous or injection drug user……………………………………………. |
1 |
0 |
8 |
Bisexual male ………………………………… |
1 |
0 |
8 |
Person with hemophilia or coagulation disorder………………………………………... |
1 |
0 |
8 |
Person with AIDS or documented HIV, risk not specified …………………………….…… |
1 |
0 |
8 |
Received transfusion from donor with documented HIV……………………………… |
1 |
0 |
8 |
Received transplant from donor with documented HIV..……………………………. |
1 |
0 |
8 |
Received clotting factor ……………………… |
1 |
0 |
8 |
Received transfusion of blood/blood components (other than clotting factor)………. |
1 |
0 |
8 |
Received transplant of tissue or organs or artificial insemination………………………… |
1 |
0 |
8 |
Worked in a health-care or clinical laboratory setting………………………..………………... |
1 |
0 |
8 |
First CD4 Test:
Count: ___, ___ ___ ___ Date: ___ ___ / ___ ___ ___ ____ Percent: ___ ___
m m y y y y
|
Positive |
Negative |
Indeterminate |
Not tested |
Test Date |
HIV-IEIA |
1 |
2 |
3 |
4 |
__ __ / __ __ __ __ m m y y y y |
HIV-1/HIV-2 Combination EIA |
1 |
2 |
3 |
4 |
__ __ / __ __ __ __ m m y y y y |
HIV-1 WB/IFA |
1 |
2 |
3 |
4 |
__ __ / __ __ __ __ m m y y y y |
Other HIV antibody test |
1 |
2 |
3 |
4 |
__ __ / __ __ __ __ m m y y y y |
Attachment 3. 2007 Interview Guide for Never In Care Project
Never in Care Project
(NIC)
2007 Interview Guide
Overview
This interviewer guide is for those administering and supervising the administration of the questionnaire for the Never in Care Project (NIC). The first section of this document discusses the rationale and objectives of NIC. Understanding the rationale and objectives is important because it may help you justify participation to others and thus motivate persons to join the study or to provide valid and complete information. The second section of this guide is on quality control. In this section, we introduce those areas in which you have control in collecting valid and complete data. The third section of this document is about basic interviewer skills. This section describes the set of key interviewing skills that are necessary to develop rapport with respondents, and the skills necessary to identify and address non-verbal and verbal cues that suggest miscommunication or inconsistent responses. The fourth section is about identifying, addressing, and resolving problem indicators. The fifth section of this document provides general instructions on administering the questionnaire. The sixth section of this document covers issues unique to starting the survey on the handheld computer. The seventh section discusses administering or coding responses to each of the questions in the eligibility screener. The eighth section reviews the procedures for documenting informed consent. Lastly, the ninth section details instructions for administering the Non-Response Form.
Use this guidance in conjunction with the NIC protocol to help you in your duties as an interviewer or supervisor for this project. The success of this project rests on you. The ability to translate data into findings that can assist in improving services for HIV-infected people and in preventing the spread of HIV are only as good as the quality and completeness of data that you collect.
1. NIC Rationale and Objectives
1.1 Rationale
Because of treatment advances, more people with HIV infection are living longer and healthier lives. Persons who know they are infected can benefit from monitoring of their immune status, and, when recommended, treatment with antiretroviral drugs and prophylaxis for opportunistic infections. Additionally, new HIV therapies may reduce the degree of infectiousness by lowering viral load, thereby reducing HIV transmission. However, one cannot achieve these benefits without linkage to care. The Center for Disease Control and Prevention’s (CDC) Strategic Plan for HIV Prevention sets a target of entry to care within 90 days of diagnosis. Capacity to evaluate progress toward this goal is limited in that existing HIV/AIDS surveillance systems provide little information about HIV-infected persons who are not in care, especially those who have never entered care. In addition, an estimate of the size and clinical status of the latter group is critically important for estimating resource needs to support linkage to care. Furthermore, identifying factors related to not being linked to care will be important in designing effective interventions. The NIC Project aims to address these gaps.
Funded jurisdictions and the Department of Health and Human Services (DHHS), Health Resources and Services Administration (HRSA) will use the findings to plan and allocate resources for HIV-related services. CDC will use the findings to measure progress toward the HIV Strategic Plan and Advancing HIV Prevention (AHP) initiative goals. The findings will also be used to develop recommendations to address unmet need and strategies to link HIV-infected persons to care.
1.2 Objectives
The overarching objective is to describe the population of persons who are HIV-infected, are at least 90 days post diagnosis, and have never received HIV care. A secondary objective is to compare this group with HIV-infected persons who have received HIV care within 90 days post diagnosis.
Specific aims:
To identify and describe persons who have been diagnosed with HIV for at least 3 months, but who have never received medical care for their HIV infection;
To ascertain barriers to receiving HIV care associated with never having received care;
To compare the characteristics of HIV-infected persons diagnosed with HIV for at least 3 months, in care and never in care;
To determine the immunologic status of persons who have had a diagnosis of HIV infection for at least 3 months, but who have never received care, to estimate the added resources that would be required when these individuals are linked to care; and
To monitor the impact of interventions to link diagnosed persons to HIV care.
2. Quality Control
The collection of high-quality interview data is crucial for meeting the NIC objectives.
Not everyone can be an effective interviewer. Essential traits needed to be a successful interviewer include:
Being people-oriented and responsive to others
Relating easily with a wide variety of people of different demographic and social backgrounds, personalities, and sexual orientations
Being comfortable with your own sexuality and feelings regarding illegal drug use and HIV/AIDS
Being detail oriented, organized, and methodical
Having a desire to contribute to expanding the knowledge of HIV prevention and care at the local and national level
The following are some important strategies that help interviewers obtain high-quality data: (1) establish and maintain rapport with respondents; (2) appropriately identify, address, and resolve both verbal and nonverbal problem indicators; (3) administer the questionnaire in a standard way, yet tailor it to the respondent as instructed; (4) translate the underlying intentions of specific measures, if necessary; and (5) review the questionnaire for errors, and identify and correct those errors which can be corrected. Each of these critical quality-control topics is discussed in the following sections.
3. Basic Interviewer Skills
3.1 Establishing and Maintaining Rapport
The more comfortable the respondent is with you, the more likely she/he will provide honest and complete answers. You establish rapport when the respondent perceives you as a nonjudgmental, understanding and caring person. To establish rapport, it is also helpful to have a warm and engaging introduction, a comfortable interview environment, and appropriate use of body language and humor.
To establish rapport, first be aware of your own feelings and the nonverbal and verbal signals you may send to respondents. Before your interviews, ask yourself
the following questions:
1. Are you feeling and looking relaxed?
2. Is your body language open or closed?
3. Are you angry or upset about something or someone? Can your appearance be interpreted as stern, inflexible, or self-righteous?
4. Do you appear as if you enjoy and value your work?
During a long survey, it is difficult to always be your best when interviewing respondents. After recognizing your feelings and the signals you may give on a particular day or interview, minimize those verbal and non-verbal signals that can be perceived as judgmental, disinterested, or non-caring. If you cannot effectively minimize these signals, please do not administer the questionnaire.
3.2 Introduction
The most important time in which to influence a successful interview may be the time when you first introduce yourself to the respondent. During the introduction, demonstrate interest and appreciation for their participation.
3.3 Responding Empathetically
Some of the questions that you ask during the interview may cause respondents to recall difficult experiences in their lifetimes. Be prepared to respond appropriately to these disclosures and the range of feelings that might accompany them. Allow time for the respondent to work through the disclosure and respond empathetically if appropriate. Being empathic (showing empathy) means understanding and appreciating the respondent’s feelings and personal situation; this is not to be confused with feeling sorry for someone. This is an important foundation on which to build rapport. As much as your personal experience might allow, demonstrate empathy verbally and non-verbally during your interactions. Be aware that even an empathetic statement may undermine rapport if not conveyed sincerely.
3.4 Humor
Humor can bring relief to tense situations and can give a sense of perspective by showing that you don’t take yourself too seriously. Within reason and personal comfort, use humor to help put nervous respondents at ease, and use it to help you cope with your work! However, do not overuse humor as it can be distracting and undermine your purpose. Use your best judgment when applying humor to build rapport.
3.5 Closure
Close the interview with the same attention and commitment to your client as you demonstrated during the introduction. Be gracious for their time and participation. Be sure to attend to their needs, including providing information about follow-up health care or other services, if appropriate, as directed by your supervisor. Remember that even though the respondent may have seen you only once, you might be the only person to whom she/he ever disclosed certain experiences or emotional states that warrant follow-up and possible intervention.
3.6 Staff Conduct
Do not try to be the participant's best friend. By maintaining a professional yet friendly demeanor you will help complete the interview in a timely manner and be a better representative of the project and your agency. Some “small talk” at start and closure are useful rapport builders; but to the greatest extent possible, outside the administration of the interview, you should be mostly listening and not speaking. Do not make inappropriate disclosures that could appear unprofessional. Examples of inappropriate disclosures might include the sharing of personal experiences of a sexual or drug taking nature. Contrast “yes, I know always using a condom can be hard” (OK) with “yes, I haven't used any condoms with my last 2 partners either” (not OK).
Staff working on NIC should abide by their state/local HIV/AIDS surveillance security and confidentiality requirements and guidelines. In addition, the following are guidelines for conduct:
• Do not come to work under the influence of alcohol or drugs
• Do not have sex with participants during the project period
• Do not use drugs with, sell drugs to, or buy drugs from participants during the project period
• All participant incentives for the project must be accounted for; the interviewer is responsible for the appropriate distribution of incentives and the return of undistributed incentives to the state/local project site
These guidelines apply to both staff conducting interviews, and all other staff working on the project. If you believe a staff member has breached these guidelines or state/local guidelines, report it to your supervisor or principal investigator.
4. Identifying, Addressing, and Resolving Problems
In order to assure that respondents provide reasonably consistent responses, you must be able to identify that there may be a problem (“problem indicator”) then address and resolve problems; this is a critical ongoing priority for obtaining high-quality data. In this context, problem indicators are either non-verbal or verbal cues given by respondents that suggest confusion or misunderstanding, inconsistent or incomplete disclosures, or other problems (stress, fear, impatience, anger, etc.).
Because even simple ordinary speech is frequently misunderstood, and because the language in the questionnaire is frequently technical and may be demanding (e.g., may ask the respondent to recall events), you must always consider the possibility that the respondent may not fully understand a question. In addition, some respondents may be troubled by the content of some questions, and some may withhold information on purpose. To obtain useful data, you must be an attentive observer and listener in order to recognize these problem indicators, and you must “think on your feet” to address them. Falling into a “habit,” and administering the questionnaire in a rote, mechanistic, and non-thinking manner will keep you from picking up and responding to these cues. It is important to stay alert.
4.1 Awareness of Respondent
Be observant about the respondent’s behavior and apparent level of comfort throughout the interview. Stay tuned to their facial expressions, tone and speed of voice and posture, and recognize potentially problematic non-verbal and verbal signals. If a respondent exhibits anxiety or disinterest, temporarily stop the interview and explore her/his reactions. Section breaks within the instrument offer good opportunities to stop and assess these problematic reactions.
Another factor in being aware of the respondent’s signals is that they may not be able to complete the interview and provide high quality data. If a participant appears to be intoxicated or under the influence of drugs, the interviewer should terminate the survey as soon as possible and make a note in the comments that the interviewer determined that the respondent was not able to complete the interview. The respondent should be compensated and thanked for his/her time.
Similarly, if you believe the respondent is not telling the truth about some of the questions, you should make a note to that effect in the interviewer comments. If the respondent consistently gives what you believe are inaccurate or untruthful answers, the interview should be stopped and a note put in the interviewer comments to that effect. The respondent should be compensated and thanked for his/her time.
4.2 Active Listening
To listen actively, periodically paraphrase key respondent responses to ensure accurate communication and to inform respondents that you are attentive. Paraphrasing involves using different words to say what the respondent already said. Responding with "It sounds like..." or "I hear that..." are frequently used active-listening transition statements. After these statements it is good to also ask “Is that right?” or words to that effect, to encourage the respondent to correct your information if needed. For example:
Respondent: “I’m not sure. I have had lots of sex partners; it’s going to be hard to give you an exact number.”
Interviewer: “Ok, it sounds like it may be difficult. Take your time to think about it.”
Although active listening is important to fully understand respondents’ answers, it should not be used as a means to suggest a response or to help a respondent choose a particular answer. Some kinds of questions used in ordinary conversations must be avoided because they suggest answers. For example:
DON’T ASK: “Do you mean A or B?” This is not neutral because it suggests two possible answers and there may be others that do not occur to you as the interviewer, but may be appropriate to the respondent if left to choose on his/her own.
DON’T ASK: “Do you mean (such and such)?” because many people tend to say “Yes” to any suggestion, either because it’s easy or because they think it is the “right” answer.
DON’T ASK: “Then you feel (such and such)?” Even though you think you’re summarizing what the respondent has already said, your interpretation may be correct, but you may be placing the emphasis in the wrong direction.
4.3 Responding to Problems
When checking in with respondents, acknowledge your observation (e.g., “You seemed hesitant to answer that question..”), explore and clarify concerns (e.g., “Are you concerned about what will happen to your answers?”), and respond appropriately (“We protect your information in many ways....”). Interviewers may find that assuming someone's mood, disposition or attitude may result in anger, alienation, and/or termination of the interview. It places the interviewer in a very precarious position. If this client suffers from an anxiety disorder, the comment may be interpreted as confrontational, no matter how mildly and politely it was intended. Other options for obtaining a subjects response to a question might include “Do you have any concerns about this question” or “Can I help clarify anything?” It might be better to help open the conversation by seeking to understand the client's discomfort. Certainly, verbal and non-verbal problem indicators have many causes over which the interviewer has no control. Evaluate whether the cause might be attributed to the interview process or uncertainty in participating in this surveillance effort. Within reason, try to understand the underlying issues and respond appropriately. When needed, reassure the respondent that:
S/he is a participant in and not just the subject of NIC.
We are interested in learning about her/his experiences, perceptions, and opinions. That is, we believe that her/his experiences are valuable and important for HIV prevention and improving the quality of care: "We hope you can help us understand"..."We want to hear what you think"... etc.
We are also interested in the variety of experiences and opinions s/he has. We do not want to come across as prying. We want to approach the respondent in a way that he/she doesn’t censor his/her own responses.
5. Questionnaire Administration: General Guidance
5.1 Administrative Issues
Prior to administering the interview, complete required activities and cover important administrative issues. These activities and discussions include obtaining consent for the interview, which ensures that the respondent understands the project, and discussing the amount of time required for the interview, confidentiality protections, reimbursement, and other concerns or questions the respondent may have. Remember to make the respondent feel as comfortable as possible and ensure her/his basic needs are met (bathroom, etc.) Explain to the respondent that s/he can ask questions at any time. Remember, these pre-interview discussions are important opportunities to establish rapport and facilitate successful interviews. As you enter these interactions, be aware of your own mood and the mood and manner of your client.
5.2 Questionnaire Structure
The questionnaire is divided into modules, each of which cover a particular domain (eligibility, demographics, HIV testing, barriers/facilitators to HIV medical care, therapy, care-seeking behavior, unmet needs, social relationships, risk behavior, and interview completion.) Within each section is a list of questions for that particular module. These section headings are to help guide you through the instrument, but are not indicated to the respondent.
Instructions for you, the interviewer, are enclosed in grey boxes and entitled Interviewer instructions. On occasion, you are instructed to read to the respondent. These instructions are typically in quotations and in regular font. They are enclosed in boxes and begin with the instruction SAY. You may also find instructions embedded in the question. These instructions are in bold, capital letters, italics, and typically enclosed within brackets or boxes.
Not all questions are intended to be asked of all respondents. On the paper version, instructions to skip particular questions are positioned either next to responses, at the top of some questions, or at the bottom of the page or question; on the computer, the skips are automatic.
5.3 Standard Administration
Administering the questionnaire in a standard way is critical for collecting high-quality data that can be combined and analyzed from all interviewers and sites. Please follow the instructions below. This is imperative in order to assure that all interviewers administer the questionnaire in the same manner.
1. Ask all applicable questions within each section in numeric sequence. Do not ask questions out of sequence unless you are instructed to do so.
2. Read clearly and exactly as written all respondent-instruction statements (in regular font within boxes interspersed throughout the questionnaire). Most sections begin with one or two sentences that begin with "SAY: ...." These important sentences are included in the questionnaire to help the respondent make the transition to a different topic. NOTE: While you may have read these instructions numerous times, this is the respondents’ first time hearing them. Therefore, do not rush through these instructions. After reading the instructions, check in with the respondent to ensure they understand what you’ve just read.
3. Read each question completely.
4. Read each question in a comfortable style and at an appropriate speed, maintaining eye-contact. Maintaining eye contact is important so that you can stay connected with the respondent, demonstrate interest and empathy, and evaluate and respond to problem indicators.
5. When instructed in the questionnaire, read the entire set of responses for specific questions. ‘Read required response’ instructions are positioned under specific questions and identify which responses are to be read. Even if a respondent selects a response before all possible choices have been read, take time to read all response options. The only exception is if a respondent “never” engaged in a particular behavior, “didn’t use” a particular substance, or “didn’t go” to a particular place; then the remaining frequency options are not read.
6. Do not read responses unless specifically instructed. When responses are not to be read, instructions are positioned under those specific questions.
7. When instructed, use standard response cards for specific questions. Prior to use, routinely orient all respondents on how to use the response cards. Response cards should be made of sturdy material, preferably laminated, and include the set of responses for only one question (i.e., one response card per question). The set of response cards should be readily available. Be sure to pause in order to give the respondent time to review the response card.
8. When instructed in the questionnaire, assist respondents in recalling specific events. Respondents will have to recall sexual and drug use behaviors since testing positive for HIV and prevention activities in which they might have been involved since testing positive for HIV. These different recall periods place considerable recall demand on respondents. It is very important that you pause and ensure the respondent understands the recall period or particular event in question.
9. In some cases, it may be acceptable to use slang or every day language, in addition to or in place of our more technical terms. For example, some local terms about drugs and drug use may be used to help the respondent understand the question better. Also, some sexual behavior vernacular may also be used to help translate our technically-defined behaviors.
5.4 Recording Responses
When using the handheld computer, responses are recorded by using the stylus to click on the appropriate response on the handheld screen. In addition, responses to structured questions are formatted in different ways. Thus, you will record responses by either checking designated response boxes or recording answers in defined (e.g., number of partners) or open-ended fields (e.g., reason why respondent didn’t seek HIV care soon after diagnosis). Please familiarize yourself with how responses are coded for particular questions, and please be careful in recording responses. Filling out the questionnaire will become second nature to you, and you will want to make the interview as brief as possible for the respondent. However, rushing through the questionnaire produces careless errors, which will be returned to you for correction. Please follow the guidance below in coding responses.
1. When to code. The only time an interviewer will leave all responses for a question blank is if the question has not been asked (e.g., when it falls under a skip pattern).
2. Single or multiple responses. Most questions will require you to code only one response; however, several questions will require you to code multiple responses. Single-response questions typically do not have interviewer instructions; however, in some instances you will be instructed to “read choices” and check only one response. Multiple-response questions will have an instruction telling you to “check all that apply.”
3. Other responses. Some questions have an “Other” response option which you can use to record responses that haven’t already been provided. A line is provided next to “Other” for you to clearly record, verbatim, the respondent’s answer. However, check to see if the answer fits a structured response before marking “Other.” Reserve “Other” for responses that are not equivalent to those which are already provided. If you are unsure if a response is equivalent, make appropriate notes in the interviewer notes (computer) or margin (paper) so that your field supervisor can make a determination.
4. Open-ended questions. A few questions are open-ended and do not have structured responses. As with “Other,” clearly record the respondent’s answers verbatim on the space provided. When needed, ask questions that will help the respondent clarify their answer, but be careful not to lead the respondent (see examples in section 4.2). Again, if a respondent’s answer to an open-ended question is not explicit, ask a clarifying question and then clearly record exactly what the respondent said. Code the response that most closely matches the answer from the list provided. If you are using the handheld computer, it will automatically display the open-ended response and instruct you to code the response from the list. Do not read the list of coding options to the respondent.
5. Unknown responses. There may be times when a respondent does not know the answer to a question. Many structured questions include a “Don’t Know” response. Please code these responses only when absolutely necessary. Before coding “Don’t Know,” probe to see if you can code part or all of the answer (e.g., date of most recent HIV test). However, do not lead the respondent to a particular answer. An unknown answer is always better than a contrived answer. All unknown responses are coded as “??” or “.D” in the handheld computer or some combination of a “9” (e.g., “09”, “99”, etc.) on the paper form.
6. Refused responses. Nearly all questions have a “refused response” option. Use your judgment about whether to probe when a respondent refuses to answer a particular question. All refused responses are coded as “.R” when administered using the handheld computer or some combination of a “7" (e.g., “07”, “77”, etc.) on the paper form.
If for some reason you are unable to code a confusing response, record information about the response you received in the interviewer notes (computer) or margin (paper). This information can be used by the coordinator later to help you come to a decision regarding the coding of a confusing response.
5.5 Additional Guidance When Using Paper Surveys
1. When using the paper interview, familiarize yourself with the designated skip patterns within each section and skip to appropriate questions when instructed. Failing to skip particular questions or inappropriately skipping questions are common, but preventable errors. If you accidentally skip a section during an interview, return to that section and administer it.
2. When using the paper version of the questionnaire, be sure to mark a response from the list given for structured questions; only write in responses for open-ended questions, for which no response categories are provided.
3. Unreadable handwriting (e.g., 4’s that look like 9’s) and misplaced checkmarks that overlap response boxes are common errors that undermine the validity of data collected on paper questionnaires. Please record responses such that they are unquestionable.
4. Following the interview, if you missed some questions do NOT code any response and do NOT code “Don’t Know.” Even if you think a particular response would apply to the respondent, it is critical that you leave all the responses to these missed questions blank.
5. When you must use a paper version of the survey, be sure that you have all documents and that the NIC respondent identification number is filled out on the top of each of these forms.
6. Starting the Interview with the Handheld Computer
6.1 Survey Information Section: Handheld Computer
Before beginning an interview, verify that the handheld computer’s date and time is set correctly. When you first launch the survey in the handheld computer, a number of questions will appear that you need to complete. All of the information requested when you first launch the NIC survey in the handheld computer is critical. Pay close attention to the detail requested in this section. Accurately enter the information. A brief description of the items follows:
-
NIC Respondent ID:
Respondent ID is the 22-digit code assigned to the person selected to participate in the interview.
Interviewer ID:
Refers to the unique 3-digit identification number of the interviewer. The Field Supervisor will assign each interviewer an ID number to use throughout the survey period.
6.2 Survey Information Section: Paper Forms
There are several additional fields that must be filled in on the paper forms, which are described below. These are automatically completed by the computer so you won’t need to complete them when using the electronic version of the survey.
-
Date of Interview:
Write in the month, day and four-digit year for the date you conduct the interview.
Time began:
Write the time the interview began. Be sure to check “AM” or “PM.”
Time ended:
Write the time the questionnaire was completed.
6.3 Ending the Survey Prematurely
Situations may arise where an interviewer must end a survey before the last question in the interview is asked. Such situations may be initiated by the participant or the interviewer. For example, interviewers may end an interview early if they find the participant is “too high” to respond to the questions in the survey.
If an interviewer feels he/she needs to end the interview early, the first step is simply to end the interview verbally with the participant by thanking him/her for their time as you would at the end of the interview. Interviewers should be cautious about telling the participant that the interview is being terminated early or the reason for terminating the interview early because it may frustrate or anger the participant. Participants who begin but do not complete the survey should still be compensated when the interview is terminated.
To end a survey early on the handheld computer, the interviewer should first enter interviewer comments for the open question on the handheld computer. In the comments, the interviewer should explain the reasons the interview was prematurely ended. After entering the interviewer comments, the interviewer would then end the survey. Instructions for entering interviewer comments and ending an interview early are provided in the handheld computer basic training, which is included in the QDS manual. It is important to enter the interviewer comments before ending the survey, because the data manager will need to determine if the interview was valid prior to shipping the data to the Centers for Disease Control and Prevention (CDC).
6.4 Entering Data on Handheld Computers
This section explains the data entry and interviewing process on the handheld computers. It briefly explains the following:
1) Handling interviews on the handheld
2) Entering letters and numbers
3) QDS HAPI program basics
4) Handling the pocket pc device.
Handling interviews on the handheld:
Opening the survey:
1) Go to Start ► Programs ► QDS HAPI.
2) Tap “Interview” on the lower left section of the handheld device
3) Tap on the “Begin” option here.
4) An open screen shall pop-up.
5) On this screen, tap on “NIC 2006 vXXX En HAPI”
Ending the survey:
1) Survey will automatically close at the end of the Interview Completion module.
2) DO NOT tap on the “X” in the upper right. This will not close the survey properly and the
data won’t be encrypted.
3) If it is necessary to terminate the interview before it is completed, Tap “Interview” and then tap
“End”
Interrupted Interviews:
If respondent needs to take a break, leave the survey open and wait for respondent, you then may need to perform the following:
If the handheld backlight has turned off after 2 minutes:
• Tap the screen to turn it back on.
• Survey will appear where you left off.
If the handheld has turned off completely after 5 minutes:
• Turn handheld on.
• Survey will appear where you left off.
If the interview was terminated before it was completed and needs to be resumed, the following steps need to be followed:
1) Tap “Interview” on the lower left section of the handheld device, and then tap “Resume”.
2) Tap on “NIC 2006 vXXX En HAPI” on the open screen that pops up.
3) An “Interview List” screen will pop-up. On this screen, tap on the incomplete interview. A pop up box will confirm the interview being loaded.
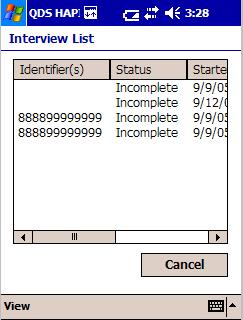
Entering letters and numbers:
There are several ways text data can be typed into the handheld device. The Windows PocketPC 2003 consists of the following SIP’s (Soft Input Panels)
Block Recognizer
Keyboard
Letter Recognizer
Transcriber
W e
recommend the use of keyboard for entering the text data.
e
recommend the use of keyboard for entering the text data.
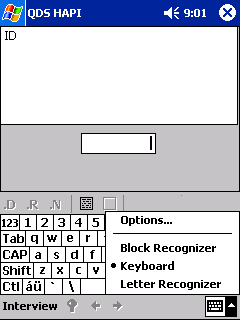
Using the keyboard SIP:
1) Tap the SIP selection area on the right bottom corner of the handheld screen to select the keyboard SIP. A small keyboard icon will appear as a block. To enable the keyboard, tap on the keyboard block. A picture of a keyboard appears on the screen.
2) Enter the letters and numbers by tapping the keyboard.
3) Use the Shift and the Caps options to switch between lower and upper case for text and between numbers and symbols.
4) For more symbol options, tap the123 key in the upper left corner of the keyboard.
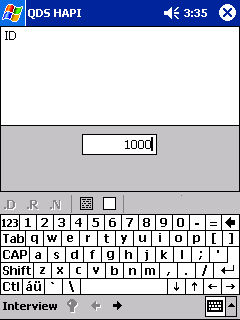
The keyboard SIP will automatically be activated while using the HAPI program when a textbox or text area has been tapped.
III. HAPI program basics:
Reading Questionnaire Text:
I nterviewer
Instructions are in bold and/or italics and SHOULD
NOT be read to the
respondents.
nterviewer
Instructions are in bold and/or italics and SHOULD
NOT be read to the
respondents.

The interview questions appear in plain font and should be read to the respondents.
Some questions are only for the interviewers and are not meant to be asked to the respondents. These are generally preceded by the instruction “Interviewer instructions:”
References to the show cards and special response sets are made as special instructions to the interviewers.
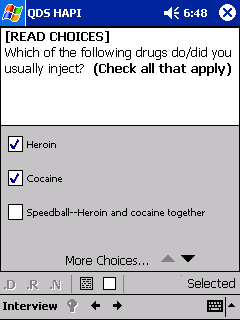
Moving Between Questions:
The questions and instructions in the HAPI program appear in a linear sequence. The skipping between questions follows a linear pattern and can be done only one question at a time.
• Advance to the next question by tapping the forward arrow at the bottom of the screen.
• If an answer to a question is required, the interviewer cannot advance without entering an answer and the forward arrow will be grayed out.
• Go back to previous questions by tapping the back arrow at the bottom of the screen.
• When moving back to the previous questions, the HAPI will skip all instructions to the interviewer.
Entering Special Responses:
The Don’t Know (.D) and Refused to Answer (.R) are called the special responses for the HAPI.
Tap .D in order to enter the Don’t Know response.
Tap .R in order to enter the Refused to answer response.

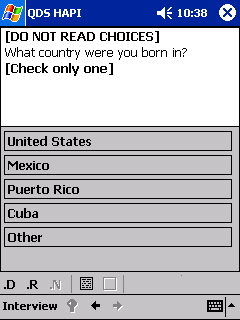
Clearing an entry:
To clear an entry, tap on the empty box below the question area.
T
 he
interviewer can add comments to each question by tapping on the
filled box below the question.
he
interviewer can add comments to each question by tapping on the
filled box below the question.
After entering interviewer comments, click on “ok” or “X” at the upper right to return to questionnaire.
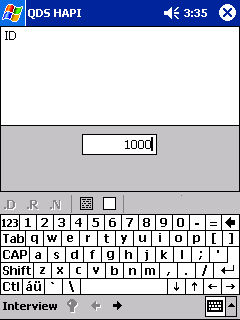
Entering Dates:
Dates always need to be in MM/DD/YYYY or MM/YYYY format.
The interviewer must enter the “/” between the numbers.
Example: November 1, 1980 would be entered as: “11”, “/”, “01”, “/”, “1980”
Most dates in the questionnaire are in a MM/YYYY format (exception: Date of Birth, PDP Start Date.)
When a respondent knows the year but not the month:
Probe to assist respondent in remembering.
If additional probing is not successful, enter the date information in this format:
“??/YYYY”

Entering Single Choice Responses:
Use the stylus to tap the box that applies.
The questionnaire will automatically advance to the next question when an answer is selected.
Entering Multiple Choice Responses:
Use the stylus to tap the boxes that apply.
A checkmark appears in the checked box or boxes.
The questionnaire does not automatically advance.
The interviewer must tap the forward arrow at the bottom of the page.
Some questions have a list of answers which do not fit on one screen (Indicated by the “More Choices” phrase at the bottom of the answer list).
Tap on the down arrow to the right of “More Choices” to see additional answers.
IV. Handling the Handheld Device:
Handheld Battery:
• Keep the battery charged when handheld device is not in use.
• The handhelds will come with a battery expansion pack to provide longer battery life.
• The battery has an estimated life-time of five hours.
If the battery dies
you will lose all data plus the questionnaire program!
Other Care Instructions:
• Only use the stylus with the handheld.
o•Don’t use pens, pencils, other sharp objects on screen.
• To clean the handheld use soft, damp cloth moistened with water only.
• Keep the handheld away from temperature extremes and moisture/liquids.
• Do not expose handheld to direct sunlight.
• Store in protective case to keep screen from getting scratched.
• Keep the handheld secure when not in use.
7. Eligibility for Interview: Specific Guidance
The eligibility criteria to be used for all participants are the following:
Has not previously completed an interview for NIC during the survey period
Is a resident of one of the participating sites
Is age 18 years or older at the start of the interview
Is able to complete interview in English
Is aware of her/his HIV status
Has never been in HIV medical care
If the participant is not able to complete the interview in English, please note this in the interviewer comments. If possible, also note the language the participant speaks. If a translator was used or a proxy (relative or other person) responded on behalf of the participant, this should also be noted.
8. Consent Procedures
Interviewers should follow local consent protocol before administering the questionnaire to eligible respondents. You may find the informed consent procedures in the NIC Protocol.
8.1 Incarcerated Populations
Interviewers should take additional precautions when working with incarcerated persons to prevent possible harm or coercion. Detainees may take notice of a respondent being called out for an interview and either infer the HIV status of the respondent or assume that the respondent is trading secrets for favor within the correctional facility (“snitching”). Interviewers should ensure that the respondent has the option to participate or not participate without repercussions to their care or from the administration of the correction facility, including guards. Interviewers may need to reaffirm the voluntary basis of the project with correctional staff who are assisting with recruitment and escort of prisoners.
9. Non-Response Form
The Non-Response Form collects a minimal amount of basic HIV surveillance information. You may extract this data directly from the HIV/AIDS Reporting System (HARS) or other HIV data sources. Only use the Non-Response Form for selected persons who decline to participate in the interview.
Attachment 4. CDC IRB Approval for Never In Care Project
From: McCleary, Jennifer (CDC/OD/OCSO)
Sent: Monday, November 13, 2006 3:55 PM
To: Bertolli, Jeanne (CDC/CCID/NCHHSTP)
Cc: NCHSTP Human Subjects (CDC); Milton, Micah (CDC/CCHP/NCBDDD); Jones, James F. (CDC/CCID/NCZVED)
Subject: 4923: Site Restricted - IRB Approval of New Protocol (Convened Board - C)
DATE: 11/13/2006
FROM: IRB Administrator
Human Research Protection Office
Office of Scientific Regulatory Services
Office of the Chief Science Officer, OD/CDC
SUBJECT: Site Restricted - IRB Approval of Protocol #4923, "Surveillance of HIV-Related Events Among Persons Not Receiving HIV Care" (Convened Board - C)
TO: Jeanne Bertolli
NCHSTP/DHAP
New protocol #4923 has been approved by CDC IRB "C" for the maximum allowable period of one year and it will expire on 10/18/2007. The IRB has determined that the study involves not greater than minimal risk to subjects.
In accordance with 45 CFR 46, Subpart C, the IRB has determined that this study presents a permissible category of research involving prisoners and qualifies for the waiver of the applicability of 45 CFR 46.305(a)(1) and 46.306(a)(2), by virtue of the criteria established by the Secretary of the Department of Health and Human Services. The regulations require CDC, and all other institutions which will involve prisoners in this research, to certify to the Secretary of Health and Human Services that the IRB fulfilled its duties with regard to the additional protections for prisoners, specified in Subpart C. The Human Research Protection Office will submit this certification to the Office of Human Research Protections (OHRP). Research involving prisoners may not begin until OHRP has indicated its concurrence with the IRB's determination.
Collaborator Note:
Indiana State Department of Health
New Jersey Department of Health and Senior Services
Philadelphia Department of Public Health
Washington State Department of Health
Seattle-King County Department of Public Health
1) Current IRB Approval Documentation: Study activities may not begin with the above collaborators/sites until documentation indicating current IRB approval has been received by CDC and is on file with this office.
2) Confidentiality statements from each of the study collaborators listed above will be forwarded to CDC. Study activities may not begin until the requested documentation has been received by CDC and is on file with this office.
3) Please note that all site specific changes made to study documents not previously approved by the CDC IRB, are required to be submitted and approved by the CDC IRB before being utilized at the sites (i.e. consent forms, scripts, recruitment flyers).
If other institutions involved in this protocol are being awarded CDC funds through the CDC Procurement and Grants Office (PGO), you are required to send a copy of this IRB approval to the CDC PGO award specialist handling the award. You are also required to verify with the award specialist that the awardee has provided PGO with the required documentation and has approval to begin or continue research involving human subjects as described in this protocol.
As a reminder, the IRB must review and approve all human subjects research protocols at intervals appropriate to the degree of risk, but not less than once per year. There is no grace period beyond one year from the last IRB approval date. It is ultimately your responsibility to submit your research protocol for continuation review and approval by the IRB. Please keep this approval in your protocol file as proof of IRB approval and as a reminder of the expiration date. To avoid lapses in approval of your research and the possible suspension of subject enrollment and/or termination of the protocol, please submit your continuation request at least six weeks before the protocol's expiration date of 10/18/2007.
Any problems of a serious nature should be brought to the immediate attention of the IRB, and any proposed changes to the protocol should be submitted as an amendment to the protocol for IRB approval before they are implemented.
If you have any questions, please contact the Human Research Protection Office at (404) 639-4721 or e-mail: [email protected].
Jennifer McCleary
cc:
James F. Jones
Micah Milton
NCHSTP Human Subjects
Attachment 5a. Template Informed Consent for Standard Structured Interview and Blood Collection for Never In Care Project
Template Statement of Informed Consent
Surveillance of HIV/AIDS related events among persons not in care
(Never In Care Project)
CDC Protocol #4923
Flesch-Kincaid grade level 7.4
The _____________________ Department of Health and the Centers for Disease Control and Prevention (CDC) support the Never in Care project. We want to learn about people living with HIV/AIDS who have never been in medical care for HIV. We would like you to join this research project. We invite you to take part in this project because you tested positive for HIV and have never been in medical care for your HIV. The information on this form can help you decide if you want to take part in the research project.
Why we are doing this project
We hope to learn why some people living with HIV/AIDS do not use medical care. We want to know what kind of services people living with HIV/AIDS need to stay healthy. We also hope to learn about ways HIV is being spread. This information will help us improve our programs, improve services for those who have HIV, help people who may have trouble getting HIV services, and prevent other people from getting HIV.
What we will need from you
If you agree to take part in the project, we will ask you to do the following:
Answer some questions:
This will take about 30 minutes. A trained interviewer will ask you questions about HIV testing, medical and social services you have used or needed, and reasons you have never been in medical care for HIV. The interviewer will also ask questions about your social support, drug use and sex practices. Some of the questions are personal and may be difficult to discuss. You don’t have to answer any question if you don’t want to, and you may end the interview at any time.
We will write down your answers or type them into the computer, but we will not write down your name on the paper (or type it into the computer). All the information that you give us will be kept private in a locked file. Only the staff of this project will be able to open the file. We will send information from your questionnaire to the CDC, but we will not send your name or any information that would identify you
If you know the person who is reading this form to you, you may ask for another interviewer so that your privacy will be fully protected.
Give some blood from your finger for blood tests:
If you agree, we will prick your finger with a lancet. The lancet has a sharp tip similar to a needle. We will then collect 10 drops of blood from your finger. Taking blood from your finger will take less than 5 minutes. These tests will help us to learn how fast the virus is multiplying and how your body is fighting the.
We will not put your name on the blood sample. The result from your blood test will be kept private. Your blood sample will not be used for any testing except the testing just described. Your blood sample will be destroyed after this testing is completed.
The tests on your blood are to help us learn more about HIV-infected people who are not getting medical care. The test to learn how fast the virus is multiplying is for research only and is not approved to be used by health care providers for your medical care. We will use the information from the tests to plan for medical care for all the people who are not getting care yet, but who might decide to get medical care soon. If you would like to know the results of these tests on your blood, please call the number below after ___________(date) anytime between ___ and ___ (hours) on these days of the week: ________________.
_____________________________________ at ____________________________.
(Contact at the Health Department) (local telephone number)
If you would like us to send the results of these tests on your blood to your health care provider, please provide the name and address below. Although your health care provider cannot use the test to learn how fast the virus is multiplying for your medical care, he or she can do other tests to measure the amount of virus in your blood.
______________________
(Name)
______________________
(Clinic or Hospital)
______________________
Street
Address
______________________
(City, State, Zip Code)
______________________
(Telephone number)
The results will be sent to the health care provider with a code number rather than your name. To follow up with the health care provider whose name you have given us, please use the code number below:
_____________________________
(Study Identification Number)
If you wish, we can help you get medical care, and the health care provider can do tests on your blood that can be used to make decisions about your medical care.
Things to consider
There are minimal risks from being in this project:
Some of the questions we ask may make you feel uncomfortable. You may feel the questions are too personal. These might include questions on income, drug use, or sex. If you do not wish to answer any questions, you do not have to do so.
If you agree to have your finger pricked, there may be some discomfort or bruising. You will feel a slight sting (like a pin prick). The lancet we use to prick your finger is clean, so it will not harm you. Also, the amount of blood we take will not harm you at all.
The area where we stick your finger may become infected, but this is uncommon. If the site of the finger prick gets red and sore, you would need to go to a clinic. To prevent any infection, we will clean your finger with alcohol before we prick it.
The benefits to taking part in this project include:
You can help your community understand why some people living with HIV/AIDS do not use medical care for HIV.
You can help us improve services for people living with HIV/AIDS, and help people who may have trouble getting these services .
If you wish, your interviewer can give you information about how to avoid spreading HIV. If you decide not to take part in this project, you can still get this information.
If you wish, your interviewer can give you information about medical and social services in your area or connect you with someone who can help you get them. If you decide not to take part in this project, you can still get this information.
Privacy
All answers give will be kept private. [To be added if Confidentiality Certificate is approved: This is so because this study has been given a Certificate of Confidentiality. This means anything you tell us will not have to be given out to anyone, even if a court orders us to do so, unless you say it’s okay. But under the law, we must report suspected cases of child abuse or if you tell us you are planning to cause serious harm to yourself or others.] To protect your privacy, we will group your answers together with answers from other persons, so that no one will know how you answered the questions. We will send information from this project to the CDC, but will not send CDC your name or any information that could identify you. Federal law protects the confidentiality of information kept at the CDC.
Voluntary Participation
Taking part in this project is your decision. Your choice to join the project will not affect your right to health care or other services. If you choose to take part in the project, you may stop the interview at any time. You may choose to participate in the interview only, and decide not to take the blood tests. We will ask for your consent for the interview and blood tests separately.
Payment
You will receive:
$25 as payment for your time and effort if you agree to be interviewed.
Another $25 if you agree to have your finger pricked to give a small amount of blood.
Questions
If you have any questions about this project, please ask the interviewer, or call:
_____________________________________ at ____________________________.
(Local principal investigator) (phone number)
If you have questions about your rights as a participant in this project, please contact:
1) The local institutional review board (IRB):
_________________________________ at ____________________________.
(Local IRB contact) (phone number)
2) The office of CDC’s Deputy Associate Director for Science at 1-800-584-8814.
This is a toll free call. Please leave a brief message including your phone number. Say that you are calling in reference to CDC protocol #4923. Someone will return your call as soon as possible.
Questionnaire Statement of Consent
I have read the explanation of this study, I have been given a copy of this form, the chance to discuss any questions that I might have, and the right to refuse to take part or end the interview at any time. I understand that one of the persons listed above will answer any future questions I may have about the interview and my rights as a participant. I understand that my participation in this interview is voluntary. I agree to be interviewed.
_________________________________ ___________________
Signature of Participant Date
_________________________________ ___________________
Signature of Interviewer Date
Finger Stick Statement of Consent
I have read the explanation about the drawing of drops of blood from a finger so tests on the blood can be done, including a research test to learn how fast the virus is multiplying. I have had a chance to discuss any questions that I might have about having my finger stuck to draw some drops of blood and my right to refuse to give blood for testing. I have also had a chance to discuss any questions I might have about the tests that will be done on my blood if I agree to have my finger stuck, and how to get the results of these tests. I understand that if I would like to know the results of these tests on my blood, I can call the number below after ___________(date) anytime between ___ and ___ (hours) on: ________________ (days of the week).
_____________________________________ at ____________________________.
(Contact at the Health Department) (local telephone number)
I also understand that I can ask to have the results of the tests on my blood sent to my health care provider if I provide the name and address and sign a release form. I understand that one of the persons listed above will answer any future questions I may have about the blood tests and my rights as a participant. I understand that my participation in these blood tests is voluntary. I agree to take part by giving some drops of blood from my finger for testing.
____________________________________ __________________
Signature of Participant Date
____________________________________ ___________________
Signature of person collecting blood specimen Date
Attachment 5b. Template Informed Consent for Standard Structured Interview, Qualitative Interview, and Blood Collection For Never In Care Project
Template Statement of Informed Consent
Surveillance of HIV/AIDS related events among persons not in care
(Never In Care Project)
CDC Protocol #4923
Flesch-Kincaid grade level 7.7
The _____________________ Department of Health and the Centers for Disease Control and Prevention (CDC) support the Never in Care project. We want to learn about people living with HIV/AIDS who have never been in medical care for HIV. We would like you to join this research project. We invite you to take part in this project because you tested positive for HIV and have never been in medical care for your HIV. The information on this form can help you decide if you want to take part in the research project.
Why we are doing this project
We hope to learn why some people living with HIV/AIDS do not use medical care. We want to know what kind of services people living with HIV/AIDS need to stay healthy. We also hope to learn about ways HIV is being spread. This information will help us improve our programs, improve services for those who have HIV, help people who may have trouble getting HIV services,and prevent other people from getting HIV.
What we will need from you
If you agree to take part in the project, we will ask you to do the following:
1) Answer some questions:
This will take about 30 minutes. A trained interviewer will ask you questions about HIV testing, medical and social services you have used or needed, and reasons you have never been in medical care for HIV. The interviewer will also ask questions about your social support, drug use and sex practices. Some of the questions are personal and may be difficult to discuss. You don’t have to answer any question if you don’t want to, and you may end the questionnaire at any time.
We will write down your answers or type them into the computer, but we will not write down your name on the paper (or type it into the computer). All the information that you give us will be kept private in a locked file. Only the staff of this project will be able to open the file. We will send information from your questionnaire to the CDC, but we will not send your name or any information that would identify you.
If you know the person who is reading this form to you, you may ask for another interviewer so that your privacy will be fully protected.
2) Tell us your thoughts and experiences:
The interviewer will ask you another set of questions that will take about 60 minutes more to answer. A trained interviewer will ask you to talk in more detail about reasons you have never been in medical care for HIV. The interviewer may also ask you to talk about medical and social services you have used or needed. You may end the discussion at any time.
During the second interview, we will record your voice with a digital recorder. We will not write down or record your name. The interviewer will also write down your responses on paper or type them into a computer. We will keep all the information that you give us in a locked file. Only the staff of this project will be able to open the file. We will send information from your discussion to the CDC, but we will not send your name or any information that would identify you. All the information that you give us will be kept private. The information you give us will be used only to improve programs and services for those who have HIV, and to prevent other people from getting HIV.
Give some blood from your finger for blood tests:
If you agree, we will prick your finger with a lancet. The lancet has a sharp tip similar to a needle. We will then collect 10 drops of blood from your finger. Taking blood from your finger will take less than 5 minutes. These tests will help us to learn how fast the virus is multiplying, and how your body is fighting the virus.
We will not put your name on the blood sample. The results from your blood tests will be kept private. Your blood sample will not be used for any testing except the testing just described. Your blood sample will be destroyed after this testing is completed.
The tests on your blood are to help us learn more about HIV-infected people who are not getting medical care. The test to learn how fast the virus is multiplying is for research only and is not approved to be used by health care providers for your medical care. We will use the information from the tests to plan for medical care for all the people who are not getting care yet, but who might decide to get medical care soon.
If you would like to know the results of these tests on your blood, please call the number below after ___________(date) anytime between ___ and ___ (hours) on these days of the week: ________________.
_____________________________________ at ____________________________.
(Contact at the Health Department) (local telephone number)
If you would like us to send the results of these tests on your blood to your health care provider, please provide the name and address below. Although your health care provider cannot use the test to learn how fast the virus is multiplying for your medical care, he or she can do other tests to measure the amount of virus in your blood.
______________________
(Name)
______________________
(Clinic or Hospital)
______________________
Street
Address
______________________
(City, State, Zip Code)
______________________
(Telephone number)
The results will be sent to the health care provider with a code number rather than your name. To follow up with the health care provider whose name you have given us, please use the code number below:
_____________________________
(Study Identification Number)
If you wish, we can help you get medical care, and the health care provider can do tests on your blood that can be used to make decisions about your medical care.
Things to consider
There are minimal risks from being in this project:
1) Some of the questions we ask may make you feel uncomfortable. You may feel the questions are too personal. These might include questions on income, drug use, or sex. If you do not wish to answer any questions, you do not have to do so.
2) If you agree to have your finger pricked, there may be some discomfort or bruising. You will feel a slight sting (like a pin prick). The lancet we use to prick your finger is clean, so it will not harm you. Also, the amount of blood we take will not harm you at all.
3) The area where we stick your finger may become infected, but this is uncommon. If the site of the finger prick gets red and sore, you would need to go to a clinic. To prevent any infection, we will clean your finger with alcohol before we prick it.
The benefits to taking part in this project include:
1) You can help your community understand why some people living with HIV/AIDS do not use medical care for HIV.
2) You can help us improve services for those living with HIV/AIDS and help people who may have trouble getting these services.
.
3) If you wish, your interviewer can give you information about how to avoid spreading HIV. If you decide not to take part in this project, you can still get this information.
4) If you wish, your interviewer can give you information about medical and social services in your area or connect you with someone who can help you get them. If you decide not to take part in this project, you can still get this information.
Privacy
All answers you give will be kept private. [To be added if Confidentiality Certificate is approved: This is so because this study has been given a Certificate of Confidentiality. This means anything you tell us will not have to be given out to anyone, even if a court orders us to do so, unless you say it’s okay. But under the law, we must report suspected cases of child abuse or if you tell us you are planning to cause serious harm to yourself or others.] To protect your privacy, we will group your answers together with answers from other persons, so that no one will know how you answered the questions. We will send information from this project to the CDC, but will not send CDC your name or any information that could identify you. Federal law protects the confidentiality of information kept at the CDC.
Voluntary Participation
Taking part in this project is your decision. Your choice to join the project will not affect your right to health care or other services. If you choose to take part in the project, you may stop the questionnaire or discussion at any time. You may choose to participate in the questionnaire only, and decide not to participate in the discussion or take the blood test. We will ask for your consent for the questionnaire, discussion, and blood test separately.
Payment
You will receive:
$25 as payment for your time and effort if you agree to be interviewed.
Another $25 if you agree to a discussion about reasons you have never been in care for HIV.
Another $25 if you agree to have your finger pricked to give a small amount of blood.
Questions
If you have any questions about this project, please ask the interviewer, or call:
_____________________________________ at ____________________________.
(Local principal investigator) (phone number)
If you have questions about your rights as a participant in this project, please contact:
1) The local institutional review board (IRB):
_________________________________ at ____________________________.
(Local IRB contact) (phone number)
2) The office of CDC’s Deputy Associate Director for Science at 1-800-584-8814.
This is a toll free call. Please leave a brief message including your phone number. Say that you are calling in reference to CDC protocol #4923. Someone will return your call as soon as possible.
Questionnaire Statement of Consent
I have read the explanation of this study, I have been given a copy of this form, the chance to discuss any questions that I might have, and the right to refuse to take part or end the interview at any time. I understand that one of the persons listed above will answer any future questions I may have about the interview and my rights as a participant. I understand that my participation in this interview is voluntary. I agree to be interviewed.
_________________________________ ___________________
Signature of Participant Date
_________________________________ ___________________
Signature of Interviewer Date
Discussion Statement of Consent
I agree to take part in this discussion. I understand that I can refuse to answer any question or end the interview at any time. I have read this consent form and all my questions have been answered. I understand that one of the persons listed above will answer any future questions I may have about the discussion and my rights as a participant. I understand that my participation in this discussion is voluntary. I agree to take part in the discussion.
_________________________________ ___________________
Signature of Participant Date
_________________________________ ___________________
Signature of Interviewer Date
Finger Stick Statement of Consent
I have read the explanation about the drawing of drops of blood from a finger so that tests on the blood can be done, including a research test to learn how fast the virus is multiplying. I have had a chance to discuss any questions that I might have about having my finger stuck to draw some drops of blood and my right to refuse to give blood for testing. I have also had a chance to discuss any questions I might have about the tests that will be done on my blood if I agree to have my finger stuck, and how to get the results of these tests. I understand that if I would like to know the results of these tests on my blood, I can call the number below after ___________(date) anytime between ___ and ___ (hours) on: ________________ (days of the week).
_____________________________________ at ____________________________.
(Contact at the Health Department) (local telephone number)
I also understand that I can ask to have the results of the tests on my blood sent to my health care provider if I provide the name and address and sign a release form. I understand that one of the persons listed above will answer any future questions I may have about the blood tests and my rights as a participant. I understand that one of the persons listed above will answer any future questions I may have about the blood test and my rights as a participant. I understand that my participation in this blood test is voluntary. I agree to take part by giving some drops of blood from my finger for testing.
____________________________________ __________________
Signature of Participant Date
____________________________________ ___________________
Signature of person collecting blood specimen Date
Attachment 6. Agreement to Abide by the Restrictions on Release of Surveillance Data
Agreement to abide by restrictions on release of surveillance data collected and maintained by the Division of HIV/AIDS Prevention - Surveillance and Epidemiology
I, ___________________________, understand that data collected by CDC through the HIV/AIDS surveillance system and related surveillance activities, projects, and case investigations under Section 306 of the Public Health Service Act (42 U.S.C. 242k) is protected at the national level by an Assurance of Confidentiality (Section 308(d) of the Public Health Service Act, 42 U.S.C. 242m(d)), which prohibits disclosure of any information that could be used to directly or indirectly identify any individual on whom a record is maintained by CDC. This prohibition has led to the formulation of the following guidelines for release of HIV/AIDS case reports and supplemental data collected on such persons to which, in accepting access to data not considered public-use, I agree to adhere. These guidelines represent a balance between potential for inadvertent disclosure and the need for the CDC/DHAP-SE to be responsive to information requests having legitimate public health application. In particular, variables that identify geographic units or facilities have the potential to indirectly identify individuals.
Therefore, I will not release, either inside or outside CDC, State/Territorial, MSA, city or county specific data in any format (e.g., publications, presentations, slides, interviews) without the consent of the appropriate State or local agency, except as consistent with the format described below and presented in detail in the written documentation for the AIDS Public Information Data Set (AIDS PIDS). Specifically, in accordance with the terms of written agreements between CDC, the Council of State and Territorial Epidemiologists (CSTE), and individual State/Territorial health departments AND in accordance with the principles of the Assurance of Confidentiality for HIV/AIDS surveillance and related data authorized under Section 308d of the U.S. Public Health Service Act:
I am permitted to release national and regional tabulations, from the HIV/AIDS surveillance database in either narrative or tabular format.
For cases in adults/adolescents > 13 years of age, for MSA’s with greater than 500,000 population, I may release multiple-way cross tabulations of 14 variables using the categories and conditions listed in the current AIDS PIDS for the rectangular data file.
For any State, the District of Columbia, or MSA with greater than 500,000 population, I may release 2-way cross tabulations of 8 variables using the categories listed in the current AIDS PIDS if cell sizes are all greater than 3. If cells containing information on 3 or fewer cases are produced, I agree to either delete those cells and all summaries using those cells from the table, or insert in any cell of 3 or less, the notation “less than or equal to 3."
For any MSA with greater than 100,000 population in selected States designated in the current AIDS PIDS, I may release 2-way cross tabulations of 8 variables using the categories and conditions listed in the current AIDS PIDS if cell sizes are all greater than 3. If cells containing information on 3 or fewer cases are produced, I agree to either delete those cells and all summaries using those cells from the table, or insert in any cell of 3 or less, the notation “less than or equal to 3."
For individual counties or health districts in selected States designated in the current AIDS PIDS, I may release one-way frequencies of 3 variables ( age, race/ethnicity, and sex) subject to the small cell size restriction described above.
I understand that release of data not specifically permitted by this agreement is prohibited unless written permission is first obtained from the appropriate Branch Chief (HICSB or BCSB), Division of HIV/AIDS Prevention - Surveillance and Epidemiology.
When presenting or publishing state, city, county, or MSA-specific data in accordance with the restrictions outlined above, I will inform the appropriate state and local health departments in advance of the release of state or local data, so as to afford them the opportunity to anticipate local queries and prepare their response.
When presenting or publishing data from surveillance-related studies, investigations, or evaluations, I will adhere to the principles and guidelines outlined in this agreement.
I also agree to the following:
I will not give my access password to any person.
I will treat all data at my desk site confidentially and maintain records that could directly or indirectly identify any individual on whom CDC maintains a record in a locked file cabinet. Sensitive identifying information from special case investigations will only be maintained in a locked file cabinet in a locked room which has restricted access.
I will keep all hard copies of data runs containing small cells locked in a file cabinet when not in use, shredding them when they are no longer necessary to my analysis.
I will not produce a “back-up” data file of HIV/AIDS case surveillance data or related databases maintained by DHAP-SE.
I will not remove electronic files, records or databases from the worksite.
I will not remove hard copies of case reports, survey instruments, laboratory reports, confidential communications, or any records containing sensitive data and information or the like from the worksite.
I will not remove from the worksite tabulations or data in any format that could directly or indirectly identify any individual.
I will maintain confidentiality of records on individuals in all discussions, communications, e-mails, tabulations, presentations, and publications (and the like) by using only the minimum information necessary to describe the individual case.
I will not release data to the press or media without pre-screening of the request by the Office of Communications, NCHSTP.
I am responsible for obtaining IRB review of projects when appropriate.
User ID: __________________
Purpose of investigation (provide a brief statement):
Database(s) to be accessed:
Estimated time needed for data access/analysis:
I have read this document, “Agreement to abide by restrictions on release of data...” and the attached document “Release of CDC HIV/AIDS Surveillance and Related Data,” and I agree to abide by them. Failure to comply with this agreement may result in disciplinary action, including possible termination of employment.
Signed: __________________________________ Date: ______________________
(Requestor)
CIO, Division, Branch _______________________________
Approved: ________________________________ Date: ______________________
Chief, (HICSB/BCSB), DHAP-SE, NCHSTP or designee
Revised December, 2003
Attachment 7. Assurance of Confidentiality
ASSURANCE OF CONFIDENTIALITY FOR SURVEILLANCE OF ACQUIRED IMMUNODEFICIENCY SYNDROME (AIDS) AND INFECTION WITH HUMAN IMMUNODEFICIENCY VIRUS (HIV) AND SURVEILLANCE-RELATED DATA (INCLUDING SURVEILLANCE INFORMATION, CASE INVESTIGATIONS AND SUPPLEMENTAL SURVEILLANCE PROJECTS, RESEARCH ACTIVITIES, AND EVALUATIONS)
The national surveillance program for HIV/AIDS is being coordinated by the HIV Incidence and Case Surveillance Branch (HICSB) and the Behavioral and Clinical Surveillance Branch (BCSB) of the Division of HIV/AIDS Prevention - Surveillance and Epidemiology (DHAP - SE), the National Center for HIV/STD/TB Prevention, a component of the Centers for Disease Control and Prevention (CDC), an agency of the United States Department of Health and Human Services. The surveillance information requested by CDC consists of reports of persons with suspected or confirmed AIDS or HIV infection, including children born to mothers infected with HIV, and reports of persons enrolled in studies designed to evaluate the surveillance program. The information collected by CDC is abstracted from laboratory, clinical, and other medical or public health records of suspected or confirmed HIV/AIDS cases; and from surveys that interview persons in recognized HIV risk groups or known to have a diagnosis of HIV/AIDS.
Surveillance data collection is conducted by State and Territorial health departments which forward information to CDC after deleting patient and physician names and other identifying or locating information. Records maintained by CDC are identified by computer-generated codes, patient date of birth, and a state/city assigned patient identification number. The data are used for statistical summaries and research by CDC scientists and cooperating state and local health officials to understand and control the spread of HIV/AIDS. In rare instances, expert CDC staff, at the invitation of state or local health departments, may participate in research or case investigations of unusual transmission circumstances or cases of potential threat to the public health. In these instances, CDC staff may collect and maintain information that could directly identify individuals.
Information collected by CDC under Section 306 of the Public Health Service Act (42 U.S.C. 242k) as part of the HIV/AIDS surveillance system that would permit direct or indirect identification of any individual or institution on whom a record is maintained, and any identifiable information collected during the course of an investigation on either persons supplying the information or persons described in it, is collected with a guarantee that it will be held in confidence, will be used only for the purposes stated in this Assurance, and will not otherwise be disclosed or released without the consent of the individual or institution in accordance with Section 308 (d) of the Public Health Service Act (42 U.S.C. 242m(d)). This protection lasts forever, even after death.
Information that could be used to identify any individual or institution on whom a record is maintained by CDC will be kept confidential. Full names, addresses, social security numbers, and telephone numbers will not be reported to this national HIV/AIDS surveillance system. Medical, personal, and lifestyle information about the individual, and a computer-generated patient code will be collected.
Surveillance information reported to CDC will be used without identifiers primarily for statistical and analytic summaries and for evaluations of the surveillance program in which no individual or institution on whom a record is maintained can be identified, and secondarily, for special research investigations of the characteristics of populations suspected or confirmed to be at increased risk for infection with HIV and of the natural history and epidemiology of HIV/AIDS. When necessary for confirming surveillance information or in the interest of public health and disease prevention, CDC may confirm information contained in case reports or may notify other medical personnel or health officials of such information; in each instance, only the minimum information necessary will be disclosed.
No CDC HIV/AIDS surveillance or research information that could be used to identify any individual or institution on whom a record is maintained, either directly or indirectly, will be made available to anyone for non-public health purposes. In particular, such information will not be disclosed to the public; to family members; to parties involved in civil, criminal, or administrative litigation, or for commercial purposes; to agencies of the federal, state, or local government. Data will only be released to the public, to other components of CDC, or to agencies of the federal, state, or local government for public health purposes in accordance with the policies for data release established by the Council of State and Territorial Epidemiologists.
Information in this surveillance system will be kept confidential. Only authorized employees of DHAP - SE in HICSB, BCSB, and in the Statistics and Data Management Branch (SDMB), their contractors, guest researchers, fellows, visiting scientists, research interns and graduate students who participate in activities jointly approved by CDC and the sponsoring academic institution, and the like, will have access to the information. Authorized individuals are required to handle the information in accordance with procedures outlined in the Confidentiality Security Statement for Surveillance of Acquired Immunodeficiency Syndrome (AIDS) and Infection with Human Immunodeficiency Virus (HIV) and Surveillance-Related Data (Including Surveillance Information, Case Investigations and Supplemental Surveillance Projects, Research Activities, and Evaluations.
Attachment 8. Contact and Recruitment Procedures and Scripts
NIC Contact and Recruitment Procedures and Scripts
There are two ways in which NIC staff may come into contact with potential participants: 1) NIC staff will attempt to contact persons selected for participation in NIC, with the permission of the health care provider who diagnosed their HIV infection, if required, to recruit them to participate; or 2) Self-referral or referral by peers or partner agencies: NIC staff will speak potential participants who call the dedicated project phone line after being referred by peers who have already participated in NIC. (The participants who recruit others will not be asked to refer specific individuals but rather will decide themselves whom to refer based on the NIC eligibility criteria. Referred persons who call NIC study staff will only be recruited if they are on the list of those selected to participate.) Both direct contact and contact through peer referrals are covered in this document.
Direct Contact
. For direct contact, information will be obtained from the facility of diagnosis and/or Health Department contacts (such as through partner counseling and referral services). A physical description and/or information about the person's receptiveness to being contacted by the Health Department (from previous contacts) may be available in Health Department records, and will be useful for approaching people for participation in NIC. NIC staff members should be aware that when contacting potential participants, maintaining confidentiality is essential. The NIC Project Coordinator should review, on a weekly basis, attempts by NIC staff to contact potential participants. Only persons who have been notified of their positive HIV status should be contacted. If there is any doubt that a person has been notified, the interview should be arranged at a Health Department facility where post-test counseling services are available. NIC staff should be prepared to provide linkage to post-test counseling should they contact a potential participant who turns out not to have been notified of his/her HIV status. The NIC staff member should offer to go with the person contacted to post-test counseling.
Contacting Potential Participants for Whom a Telephone Number is Available
If possible, the NIC staff should first attempt to contact the potential participant by telephone,.
1) Contacting the Potential Respondent Directly
To avoid breaching confidentiality, the words “HIV” and “AIDS” must never be spoken during the telephone conversation.
The initial call allows the NIC staff member to identify him/herself, to discreetly establish the nature of the call, and to arrange an appointment for an interview.
Below is an example of a recruitment call:
(NS=NIC Staff Member)
NS: Hello, may I speak with John Doe?
If asked “Who is calling?” respond that you are conducting a survey about health care. If the respondent indicates he is John Doe, or John Doe comes to the phone, say:
NS: I am calling about something for John Doe, and I need to make sure that I am talking to the right person (keep in mind that there could be a Jr and Sr with the same name.) In what year were you born?
If the year of birth matches that of the person you are seeking, this represents preliminary evidence that you have reached the correct person. Say:
NS: My name is Mike Smith and I am from the XXX Health Services. You’ve been selected to help us assess how people are able or not able to get medical care by participating in a survey. This assessment is important and I will pay you for your time. I also have some important information to share with you about health care services. If you agree to participate, you’d be helping your community learn more about gaps in health care services (AND you’d earn something for your time). Because the information I need to speak with you about is personal, I would like to meet you in person to ask you some questions and give you some important information about health care services. Everything we would talk about would be confidential.
NS: The whole visit would take less than 1 hour [1.5 hours for selected participants in Indiana and Washington].
NS: When can we meet?
NS: Would you be able to meet me at [suggest a place] where we can speak privately? [If another place is suggested, say:
Would that place be OK for a private conversation?
If the he/she agrees to a meeting, ask him/her to bring some personal identification.
If the year of birth does not match that of the person you are seeking to interview, say:
NS: My name is Mike Smith and I am from XXX Health Services. John Doe was chosen to take part in a health survey and I need to make sure I am speaking to the right person. The year of birth I have for John Doe is different, what's your name?
If the person confirms that he is John Doe, emphasize the importance of a face-to-face meeting to confirm one another’s identity and to conduct the interview, and ask him if he is willing to meet. Say:
NS: Because the information I need to speak with you about is personal, I would like to meet you in person to ask you some questions face-to-face and to give you some important information about health care services. Everything we would talk about would be confidential. The whole visit would take less than 1 hour [1.5 hours for selected participants in Indiana and Washington].
NS: When can we meet?
NS: Would you be able to meet me at [suggest a place] where we can speak privately?" If another place is suggested, say:
Would that place be OK for a private conversation?
If he/she agrees to the meeting, ask him/her to bring personal identification.
The potential participant may demand additional information before he/she agrees to a meeting. NIC staff may remind the person of the monetary incentive and promise to provide information about health care services to motivate him/her to make an appointment. NIC staff may also use the statement:
NS: I have information about health care for you that I think you will want. When would be a good time to meet?
If transportation is an issue, offer to travel to meet the person at a place of his/her choosing [as long as it meets the auditory privacy conditions necessary for an interview].
If the person says he is not John Doe, say:
NS: "I need to talk with John-- where is he right now? What number can I reach him at?" [If no other number, say:]
NS: What other way can I reach him now? (cell phone, work location, lunch place, regular hangout, pager, email)?
Communicating with a Third Party Over the Telephone
Third Party at Home
Telephone calls to the home of the potential respondent can be challenging, particularly when a related third party answers the call. Precautions must be taken to protect confidentiality.
Conversations with someone other than the person eligible for NIC should be brief, and the information presented in a matter-of-fact fashion.
Example Telephone Conversation
TP = Third Party
NS= NIC Staff Member
TP: Hello
NS: Hello, may I speak with John?
TP: John isn’t here, Who is this?
NS: This is Bill. When will John be home?
TP: After nine. May I help you? What is this about?
NS: John’s been selected to participate in a survey. He will be paid for his time Here is my number—do you have a pen? The number is XXX-XXX-XXXX. He can call collect if he likes. (Make sure that those who answer this phone number don't say the words "HIV/AIDS" or "Health Department" and that the voicemail message and caller ID for the phone number do not indicate it is a phone line for an HIV/AIDS-related program. It may also be necessary to give a time for John to call back when the staff member will be in the office, or a cell phone number).
NS: What other way can I reach John now, such as a cell phone number, different work location, lunch place, regular hangout, pager, email?
TP: Yes, John's cell phone number is XXX-XXX-XXXX.
NS: Thank you.
Third Party at Work
Encountering a third party when calling the workplace is an extremely sensitive and delicate situation. The NIC staff member must attempt to make contact with the potential participant without arousing suspicion or bringing unnecessary attention either to him/herself or to the potential respondent. The best approach in this situation is to ask to speak to the potential respondent while simply identifying yourself by name. If the person asks about the purpose of the call, politely but assertively state that you need John's help. If the potential respondent is unavailable, try to ascertain a time that would be appropriate to make contact and leave your name and telephone number to have the person call you back.
Example Telephone Conversation
TP = Third Party
NS= NIC Staff Member
NS: Hello, may I speak with John Doe?
TP: John is not able to receive calls at this time. Can I take a message?
NS: Yes, I would like to leave my name and number. My name is Mike Smith. I can be reached at XXX-XXX-XXXX. He can call collect if he likes. (It may also be necessary to give a time for John to call back when the staff member will be in the office, or a cell phone number).). When will he get this message?
TP: He takes his break at 3:00 PM. He will be able to get his message then.
NS: What other way can I reach him now (such as a cell phone number, different work location, lunch place, hangout, pager, email…)?
TP: I don't have another number for John.
NS: I will call back at 3 PM, then. Thank you.
Contacting a Potential Respondent Without a Telephone Number
a) Contact by Email
If the only information you have for a person is an email address, you may send an email using the following format.
Example Email #1:
My name is Mike Smith, and I am a working with the XXX health services. You’ve been selected to help us assess how people are able or not able to get medical care by participating in a survey. This assessment is important and I will pay you for your time I also have some important information to share with you about health care services. If you agree to participate, you’d be helping your community learn more about possible gaps in health care services (AND you’d earn something for your time). You can call me at XXX-XXX-XXXX (call collect if you wish), Monday through Friday, 8am to 5pm or XXX-XXX-XXXX (cell). If I am not available, you can leave your name and number on this CONFIDENTIAL line and I or person on the staff will return your call as soon as possible. This is NOT spam!
Thank you for your cooperation.
Mike Smith, public health advisor
XXX Health Services
XXX-XXX-XXXX
Example email #2-
Hello, my name is Mike Smith, and I'm working with XXX Health Services. This is the second time I’ve tried to contact you, I last sent an email on XX/XX/XX. Please call me as soon as possible. You’ve been selected to help us assess assess how people are able or not able to get medical care by participating in a survey. This assessment is important and I will pay you for your time. I also have some important information to share with you about health care services. If you agree to participate, you’d be helping your community learn more about possible gaps in health care services (AND you’d earn something for your time). My only means of contacting you is through this email address. You can call me at XXX-XXX-XXXX (call collect if you wish), Monday through Friday, 8am to 5pm or XXX-XXX-XXXX (cell). If I am not available, you can leave your number on this CONFIDENTIAL line and either I or another person on the staff will return your call as soon as possible.”
Mike Smith, public health advisor
XXX Health Services
XXX-XXX-XXXX
Example email #3-
My name is Mike Smith and I'm working with the XXX Health Services. This is the third time I have tried to contact you regarding your participation in a survey to assess gaps in medical care needs. This assessment is important and I will pay you for your time I also have some important information to share with you about health care services. If you agree to participate, you’d be helping your community learn more about possible gaps in health care services (AND you’d earn something for your time). Please call me as soon as possible at XXX-XXX-XXXX (call collect if you wish), Monday through Friday, 8am to 5pm or XXX-XXX-XXXX (cell). If I am not available, you can leave your number on this CONFIDENTIAL line and either I or another member of the staff will return your call as soon as possible. To assist you in confirming my identity, I’m also including the name and phone number of my supervisor, George Hill XXX-XXX-XXXX.
Please do not delay in contacting one of us. Thank you.
Mike Smith, public health advisor
XXX Health Services
XXX-XXX-XXXX
George Hill, supervisor
XXX Health Services
XXX-XXX-XXXX
If no response to email is received, and a street address is available, NIC staff should attempt a visit to reach the person.
If a telephone number or email address is unavailable, the NIC staff member will try to obtain one. If still unable to obtain a telephone number or email address, but there is a street address for the potential respondent, the NIC staff member will send a letter.
b) Contact by Mailed Letter
The
envelope should contain no street address (a post office box number
is okay) and should be marked:
Potential respondent’s name and address
To be opened by addressee only; and
Confidential.
Example Letter
Dear John Doe,
You’ve been selected to help us assess gaps in medical care needs by participating in a survey. This assessment is important and I will pay you for your time. I also have some important information to share with you about health care services. If you agree to participate, you’d be helping your community learn more about possible gaps in health care services (AND you’d earn something for your time). Please call me, Mike Smith, a public health advisor at the XXX Health Services, as soon as possible. You can call me at XXX-XXX-XXXX (call collect if you wish), Monday through Friday, 8am to 5pm or XXX-XXX-XXXX (cell). If I am not available, you can leave your name and number on this CONFIDENTIAL line and I or another public health advisor will return your call as soon as possible.
Thank you for your cooperation.
Mike Smith, public health advisor
XXX Health Services
XXX-XXX-XXXX
If the potential respondent doesn't call within one week, NIC staff should make a field visit.
c) Making a Field Visit
To recruit a person eligible for NIC without a telephone number or email address, or if the person does not respond to to telephone or email messages or mailed letters, can be time consuming since the NIC staff member does not have the option of scheduling appointments in advance. Several field visits (at different times of day/evening and days of the week) may be necessary before the NIC staff member has the opportunity to reach and meet with the potential respondent.
i) Leaving a Note When the Potential Respondent is Not Available
It is important that a blank sealed envelope, containing the NIC staff member’s contact information, be prepared prior to conducting the field visit, in case the person sought is not available. The outside of the envelope must be addressed in the following manner:
Potential respondent’s name and address;
To be opened by addressee only; and
Confidential.
The note inside will state that the person has been selected to participate in a health survey to assess how people are able or not able to get medical care, to be paid for participating, and to receive important information about health care services. The note will also request that the addressee contact the NIC staff member. When the potential respondent is not available, the NIC staff member will leave this note at the person’s address or with a third party. If the potential respondent doesn't call within one week, NIC staff should make another field visit. If this visit does not result in contact with the potential respondent, the next step should be discussed with the NIC Project Coordinator.
ii) Encountering Third Parties During a Field Visit
Some people may be highly suspicious of any questions asked concerning how to locate someone. It is important that the NIC staff member be prepared for these suspicions in the event that he/she must interact with a third party. The most important technique in this situation is to use open-ended questions, i.e., a question worded in such a way that prevents a “yes” or “no” response and engages the third party to provide additional information. For example: The NIC staff member should ask: “When will Mary be available?” instead of, “Do you know when Mary will be available?”
The following are examples of approaches that should be used in communicating with third parties.
Example 1: Third Party at Work
TP = Third Party
NS= NIC Staff Member
NS: Hello, I am here to see John Doe.
TP: John is not able to receive visits at this time. Can I help you?
NS: I have important information I would like to share with John and I need his assistance. Where is he today?
TP = Just a minute, I’ll get him
When you meet the respondent, verify identity and continue with the recruitment script (section C below).
OR
TP: He isn’t here.
NS: At what time can I see him?
TP: You can see him at 3 pm.
NS: What other way can I reach John now, such as a cell phone number, different work location, lunch place, pager, email?
TP: Your best bet is to catch him here at 3 pm.
NS: Ok, I will be back then. I'd also like to leave my number in case I miss him. Here is my number—do you have a pen? The number is XXX-XXX-XXXX (he can call collect if he wishes). (It may also be necessary to give a time for John to call back when the staff member will be in the office, or a cell phone number).
NS: Thank you.
IF TP says John is not available that day:
NS: Here’s a note for him… When can you give it to him?
TP: This afternoon at 3PM.
NS: Ok, I’ll try and stop back then. Thank you for your assistance.
OR
NS: What's the best way to get him this message?
TP: I would suggest leaving it with his secretary.
NS: Thanks for your assistance.
Example 2: Third Party at Home
If the person who answers the door matches the general description you have of the respondent (e.g., same age, race, sex), then you should greet the person by saying “John?” This open ended greeting facilitates the conversation with “John” if he comes to the door.
TP: Hello
NS: John?
TP: John isn’t here. Who are you and what is this about?
NS: I am Bill. When will John be home?
TP: He will be here after 9 pm. I am his father. How may I help you?
NS: Nice to meet you! John’s been selected to participate in our survey—it should be interesting for him and he will be paid for his time. He’d also be helping to assess needs in this community
NS: What other way can I reach him now, such as by cell phone, pager, email, or at another location?
NS: He's down the street at the Starbuck's.
TP: (If you don't have a physical description, ask for one.) Thanks for your assistance.
OR
If a number is given, write it down, thank the person and say that you will be calling John OR if no other number, explain that you will call back after 9 pm, and then say:
NS: When can you give him this note? It will help explain the survey.
TP: [Sees outside of envelope with "confidential" stamp.]
But I am his mother, I have the right to know what this is about.
NS: I understand, and I don’t like being mysterious but there are guidelines I have to follow as part of doing this survey He is the one that I must speak with first. John is not in any trouble—just the opposite. I need his help
TP: I will give the envelope to John tonight.
NS: Thank you for your assistance and understanding.
C. Meeting Face-to-Face
Confirming the Potential participant’s Identity
During a face-to-face meeting, the NIC staff member confirms the identity of the potential respondent. If the physical description and date of birth match with the information the NIC staff member has, proceed to recruitment using the script below. If the physical description and or other identifying information available do not match that of the potential respondent, request a driver’s license or other identifying documentation. In the event that no identification can be provided, the NIC staff member will reschedule the field visit to a time that the potential respondent can produce proper identification. In the meantime, NIC staff should also attempt to verify the physical description.
Recruitment
NS: Hello, my name is Mike Smith and I’m working with XXX health services. (Show the individual your work identification).
You’ve been selected to help us assess how people are able or not able to get medical care by participating in a survey. This assessment is important and I will pay you for your time. I also have some important information to share with you about health care services. If you agree to participate, you’d be helping your community learn more about gaps in health care services (AND you’d earn something for your time). How old are you? Where do you live?
Respondent must be at least 18, live in the project area, and speak English or Spanish. If the person does not meet these eligibility criteria, terminate the interview by saying,
NS: For this survey, we want to talk with people 18 or older who live in [project area) and speak English or Spanish. Thank you for your time."
If the person is over 18 and meets the residence requirements, say,
NS: I would like to tell you more about the survey so you can decide if you want to participate. Everything we talk about will remain confidential. Do you recall having had a medical test at [name of facility] or from [name of provider].
If the person does not recall having been tested: give him/her some other information, such as the date the test was administered.
If the person remembers, then say:
NS: I would like to talk to you about the medical test that you had—I’m referring to an HIV test.
NS: When did you receive the results of this HIV test?
If respondent can’t answer or says that he or she didn’t receive the test, terminate the interview, and provide an immediate referral for post-test counseling. (Note: The interviewer should provide assistance with obtaining post-test counseling services and transportation, if necessary, and offer to accompany the person to the post-test counseling location).
If the person doesn’t remember the test even after the date is given: terminate the interview and provide a referral for post-test counseling. (Note: The interviewer should provide assistance with obtaining post-test counseling services and transportation, if necessary, and offer to accompany the person to the post-test counseling location.)
If the person remembers the test: confirm that he/she received the test results, then say :
NS: The health department has selected you to be confidentially interviewed because our records indicate that you have HIV infection but may not have received medical care for your HIV infection. Before I go on, I would like to check on whether this is correct. Have you received medical care for your HIV infection?
IF YES: Ask where and when, document this information, terminate the interview and thank the person for their time.
If the person confirms he/she has not received care, say,
NS: The health department is trying to learn how to help people with HIV infection get medical care. I'm going to read you a description of what is involved in participating in this survey.” Ready to get started? If yes, read consent....
If consent is not given: Terminate the interview, thank the person for their time, and provide referrals for HIV-related medical and other services.
Contact Through Referral
Each person who agrees to participate in NIC (with the exception of prisoners) will be asked at the end of the interview to share information about the NIC Project with others whom they know who are HIV-infected and have never been in care. Specifically, they will be asked to give the flyer below to others whom they believe to be eligible to participate in the Project. Partner agencies (e.g., community-based agencies offering HIV-related services, substance abuse counseling and treatment agencies, case-management services) will also be asked to refer eligible persons to the NIC project. Finally, flyers will be posted in suitable locations, which may generate self-referrals.
Help [ name of health department] Help the Community and Receive $$$ for Your Time
You may be eligible to participate in an interview and receive $25-$75 for your time. The [ ] health department wants to know how it can better serve the community in [geographic area]. The health department is specifically interested in what it can do to improve HIV services and make them more available. Please call if:
♦You found out your HIV status at least 3 months ago
♦Besides getting an HIV test, you have never been to a doctor, nurse, or other health care worker for HIV care
♦You are 18 years of age or older
♦You speak English or Spanish
If interested call: [phone number].
When you call, you will be asked some questions to determine if you are eligible to take part in the Project. Some eligible people may not be selected. If selected, you will be asked to meet a Project staff member in person. Your responses to interview questions will be kept strictly confidential.
[ ] Health Department
[address, phone number]
When an individual who has been referred (or self-referred calls the NIC Project dedicated phone line, the NIC staff member will identify the reason for the call and then say:
Name of Health Department] has started a project in your area to learn about why some people who have HIV infection don't get HIV medical care, what they need to get care, and what can be done to meet these needs. The Health Department is interviewing people in your community for this project. The interview is completely confidential and those who take part will not be contacted again after it takes place. The interview contains some questions that may be uncomfortable for some people. No one will be pushed to answer questions that they don’t want to answer.
How did you hear about the project / get this phone number?
□ Flyer posted on a wall
□ Flyer given by a friend
□ Partner Agency
□ NIC Staff Member
Then the staff member will say:
I would like to ask you some questions to see if you are eligible to take part in the Project. If you are eligible, then I will set up an appointment to meet you in person for the interview. I will ask you to bring personal identification to the meeting so I can be sure I am talking to the right person.
The caller will be asked his or her name and birth date, so it can be checked against the list of those selected for participation.
What is your name? ___________________
What is your date of birth?_______________
Even if the caller is not on the list of persons selected to participate, ask the questions below:
1. Are you 18 years old or older? [also check available records]
-
Yes
1
[CONTINUE to 2.]
No
2
[Say “For this project, we are interested in talking with people who are 18 years old or older.” THANK AND ASSIST WITH ACCESSING MEDICAL CARE / SOCIAL SERVICES]
Closing Script:
I would like to answer any questions you may have and help you get any medical and social services that you may need. Do you have any questions? Do you need help getting medical or dental services, mental health counseling, drug or alcohol abuse counseling, peer counseling or support, financial counseling or benefits assistance, shelter or housing services, meal or food services, home health services, or education or information about HIV?
If yes, provide information and/or referral to a case manager.
Thank you very much for calling today and for your interest in our project. Goodbye.
2. Did you have your first positive test for HIV at least 3 months ago? [also check available records]
-
Yes
1
[CONTINUE to 3.]
No
2
[Say “For this project we are interested in talking with people who had their first positive HIV test at least 3 months ago.” THANK AND ASSIST WITH ACCESSING NEEDED MEDICAL CARE / SOCIAL SERVICES]
Closing Script:
I would like to answer any questions you may have and help you get any medical and social services that you may need. Do you have any questions? Do you need help getting medical or dental services, mental health counseling, drug or alcohol abuse counseling, peer counseling or support, financial counseling or benefits assistance, shelter or housing services, meal or food services, home health services, or education or information about HIV?
If yes, provide information and/or referral to a case manager.
Thank you very much for calling today and for your interest in our project. Goodbye.
3. Have you ever received HIV medical care (by "HIV medical care" I mean physical exams and laboratory tests such as HIV viral load and CD4 testing that can tell your doctor how fast the virus is multiplying and how your body is fighting the virus.)
-
Yes
1
[Say “For this project we are interested in talking with people who have never received medical care for their HIV infection.” THANK AND ASSIST WITH ACCESSING NEEDED SERVICES]
No
2
[CONTINUE to 4.]
Closing Script:
I would like to answer any questions you may have and help you get any medical and social services that you may need. Do you have any questions? Do you need help getting medical or dental services, mental health counseling, drug or alcohol abuse counseling, peer counseling or support, financial counseling or benefits assistance, shelter or housing services, meal or food services, home health services, or education or information about HIV?
If yes, provide information and/or referral to a case manager.
Thank you very much for calling today and for your interest in our project. Goodbye.
4. You have not been selected to take part in the project at this time; however, you may be selected in the future. Would it be Ok to contact you if you are selected?
-
Yes
1
[COLLECT CONTACT INFORMATION USING FORM BELOW, THEN THANK AND ASSIST WITH ACCESSING MEDICAL CARE/SOCIAL SERVICES]
No
2
[THANK AND ASSIST WITH ACCESSING MEDICAL CARE / SOCIAL SERVICES]
Closing Script:
I would like to answer any questions you may have and help you get any medical and social services that you may need. Do you have any questions? Do you need help getting medical or dental services, mental health counseling, drug or alcohol abuse counseling, peer counseling or support, financial counseling or benefits assistance, shelter or housing services, meal or food services, home health services, or education or information about HIV?
If yes, provide information and/or referral to a case manager.
Thank you very much for calling today and for your interest in our project. Goodbye.
If the caller is on the list of persons selected to participate, ask the screening questions below.
II. Screening Questions & Permission to Contact
Are you 18 years old or older? [also check available records]
-
Yes
1
[CONTINUE]
No
2
[THANK AND ASSIST WITH ACCESSING MEDICAL CARE / SOCIAL SERVICES]
Did you have your first positive test for HIV at least 3 months ago? [also check available records]
-
Yes
1
[CONTINUE]
No
2
[THANK AND ASSIST WITH ACCESSING NEEDED MEDICAL CARE / SOCIAL SERVICES]
Have you ever received HIV medical care (by "HIV medical care" I mean physical exams and laboratory tests such as HIV viral load and CD4 testing that can tell your doctor how fast the virus is multiplying and how your body is fighting the virus.)
-
Yes
1
[THANK AND ASSIST WITH ACCESSING NEEDED SERVICES]
No
2
[CONTINUE]
If you decide to participate, we will need to set up an appointment to meet you in person for the interview, and we will ask you to bring personal identification with you, such as a driver’s license or other ID card with a photograph on it. If you take part in the project you will be given $25-$50 (or $25-75). You will receive $25 for a 30 minute interview [for those selected for the qualitative interview say:and another $25 if you agree to second interview, which would last an hour], plus $25 if you give a some drops of blood from your finger.
Are you interested in participating?
-
Yes
1
Great! [CONTINUE].
No
2
[THANK AND ASSIST WITH ACCESSING NEEDED MEDICAL CARE / SOCIAL SERVICES
To interview you, I will need to set up an appointment to meet you in person. When are you available to meet? [make appointment]
Where shall we meet? [SET LOCATION ]
Confirm date and location.
Do you want a reminder?
-
Yes
1
[CONTINUE].
No
2
[THANK AND ASSIST WITH ACCESSING NEEDED MEDICAL CARE/ SOCIAL SERVICES]
Please remember to bring official identification (including a photo) with you to the appointment.
STEP 1. Collecting Contact Information
Potential participants who want to be reminded of the interview appointment should be asked to give as much contact information as they feel comfortable giving (on a voluntary basis) so that NIC study staff can reach them to confirm their participation and remind them of the date, time and location of their appointment to be interviewed. Participants should be reminded that this information will not be kept with or recorded on any other study materials (consent form or responses to interview) and that the information will be destroyed once the interview has taken place or one year after their call, whichever comes first.
Participants may decline to provide any or all information requested on the contact information form. They may also choose to share information but with specific stipulations that should be honored by study staff and should be recorded on the contact information sheet (e.g. only call at night, don’t use the study name when calling, only talk to participant, don’t leave messages.) If a participant refuses to provide any contact information, record this on the Contact Information Form and be sure to give them the details on the interview and encourage them to show up to participate.
Every effort should be made to obtain a phone number for contact since this method will be the most useful for reaching participants.
Give the contact information to the NIC study staff, following their instructions for protection of sensitive data.
STEP 2.
Explain to the participant that if a NIC staff member calls, he or she will ask for a password which will help to assure that they are actually speaking with them and not someone posing as them. Ask the participant to choose a password that is easily remembered and that no one else will think of.
III. Contact Information Form
The staff of the Never In Care Project need some way of contacting you to confirm your participation in the interview. I am going to ask you now to give me your name, address and phone number, or the name, address and phone number of a person or persons who would know how to reach you to remind you of your appointment. You should know that with your permission now, we will be using this information to contact you and if we are unable to get in contact with you we may contact the people you tell us about on this form. If we do contact the other people on this form, we won’t tell them why we are calling. We will only say that we need to speak with you and leave our phone number. The information you give us now will not be kept with or written on any record of your answers to interview questions. This form will be destroyed the day of the interview or one year after their call, whichever comes first. You can decide not to give us any of this information and this will not change your invitation to participate in the interview.
Date of Call: ______________Interviewer ID: _______
Name __________________________
Nickname __________________________
Date
of Birth___________________________
Address __________________________ OK to mail? _____Yes ____No
Street ___________________
Apt number, c/o______________________________________________
City State Zip_________________________________________________
Telephone (____)______________(h) OK to call? _____Yes ____No
(____)______________(w) OK to call? _____Yes ____No
(____)______________( c) OK to call? _____Yes ____No
Pager ____________________ OK to page? ____Yes ____No
Email ______________@____________ OK to Email? ____Yes ____No
Other specific contact instructions:_____________________________________
Contact # 1 (Person you have known for more than one year and whom you are in steady contact with)
Name __________________________ Relationship ______________
Telephone _________________(h) OK to call? _____Yes ____No
_________________________(w) OK to call? _____Yes ____No
______________________(c ) OK to call? _____Yes ____No
Pager ____________________ OK to page? ____Yes ____
Email ___________@_________ OK to Email? ____Yes ____No
Other specific contact instructions:_____________________________________
Contact # 2 (Person you have known for more than one year and whom you are in steady contact with)
Name __________________________ Relationship ______________
Telephone _________________(h) OK to call? _____Yes ____No
_________________________(w) OK to call? _____Yes ____No
______________________(c ) OK to call? _____Yes ____No
Pager ____________________ OK to page? ____Yes ____
Email ___________@_________ OK to Email? ____Yes ____No
Other specific contact instructions:_____________________________________
Closing Script:
I would like to answer any questions you may have and help you get any medical and social services that you may need. Do you have any questions? Do you need help getting medical or dental services, mental health counseling, drug or alcohol abuse counseling, peer counseling or support, financial counseling or benefits assistance, shelter or housing services, meal or food services, home health services, or education or information about HIV?
If yes, provide information and/or referral to a case manager.
Thank you very much for calling today and for your interest in our project. Goodbye.
Or if a meeting has been arranged, say:
Thank you for agreeing to take part in our project and we look forward to talking with you on [date, time] at [location]
[Follow guidelines for meeting potential participants, specifically, the section beginning on page 257, “Meeting Face to Face.” ]
Attachment 9. Script for Returning CD4 T-Lymphocyte and HIV Viral Load Test Results to Participants
Scripts for Providing CD4 and Viral Load Results
NOTE TO STAFF: This script is for providing results of CD4 and viral load tests. It is consistent with intervention messages (e.g., be active in your relationship with your provider and ask questions if there is anything about your care that you don't understand) and differentiates the Never In Care (NIC) staff from clinical care providers. The script should explain the limitations of the test results.
In an emergency situation in which a person becomes extremely distraught
when they hear their results, notify your project coordinator. They can get in touch with a
clinician on site or by phone who can talk to that person about the test results, or at least
set up a time when the participant might talk to the site’s clinical back up.
"I'm going to give you the results of the blood tests we did a few weeks ago.
Remember, we were testing your CD4 (T-cell) count and your HIV viral load.”
“Now I'm going to tell you what we found and a little bit about what these tests
are looking at. But I want to remind you that I'm not an HIV care provider, and I don't
know about the care you've been receiving from your doctor and other HIV care
providers, if you have one. So I'm not going to be able to answer detailed questions
about these results. You can still feel free to ask me questions, but if I can't answer them,
I'll probably suggest that you ask an HIV provider. Also, remember, if you signed the release form, or if you want to sign it now, we can send these results to your doctor or care provider. If you don't have an HIV care provider, we can refer you to one nearby. We think that everyone who is HIV-positive should be seen by an HIV care provider."
"OK, now your results. First your CD4 (T-cell) count is ___ . Your CD4 (T-
cell) count is the number that gives your doctor an idea of your overall health and how far
your HIV infection has gone. CD4 counts can change a lot between tests. The results can
also be different depending on which lab does the test, whether you’ve been sick recently
and many other reasons. Only a provider who sees you over time can tell you if these results really are significant for your health. HIV attacks the CD4 (t-cell) cells which are important for fighting off infections. For CD4 count, a higher number generally is better. The more that your CD4 counts drop from your normal level, the harder it is for your body to fight infections. If your CD4 count drops below 500, your HIV provider may want to monitor you more closely or discuss the use of HIV treatments with you. People with results below 200 are generally monitored more frequently as they are more likely to develop an illness related to their HIV (an opportunistic infection). Opportunistic infections are diseases that your body would fight off easily if your immune system was healthy. If your immune system is not healthy, opportunistic infections can be very serious for your health."
"Now to move on to viral load; your viral load is ______. Viral load is a newer
test. It measures the amount of HIV, or the number of copies of HIV, in your blood at a
particular time. For the results of the viral load test, a lower number of copies of HIV is
better. People’s viral load test results can be anywhere between what we call
"undetectable," which means the amount of virus in the blood was too low for the test to
measure accurately, to over a million copies of the virus in the blood. For the test we
used in this study, the lowest possible number is 50 copies. So if you have less than 50
copies of the virus, with the test we use, we can only tell you that you have less than 50
copies, we cannot give you an exact number. Generally, if the level is over 10,000
copies, your doctor or HIV care provider would generally consider monitoring you more
closely and might discuss starting you on or changing your medications. The goal of
treatment with medications for HIV is to reduce the viral load, preferably to undetectable
levels. Undetectable does not mean that there is no virus. It means that we cannot detect
the small amount of virus in the person’s blood with our current lab tests, but we know
that a small amount is there because the person is HIV positive. Even if your viral load is
undetectable, you still can transmit HIV to other people. No matter what your test results
are, remember it is important to continue practicing safer sex and safer drug use
behaviors."
WRAP UP
"Remember, we think that everyone who is HIV-positive should be seen by an
HIV care provider. If you don't have an HIV care provider, we can refer you to one
nearby. It is very important for all people with HIV to see their care providers regularly.
Only they can help you make health care decisions based on the status of your immune
system, the amount of virus in your blood, and other medical information that they have."
Attachment 10. Sample Size by Project Area for Never In Care Project
Project Area |
Sample Size for 12-month Data Collection |
Indiana |
100 |
New Jersey |
100 |
New York City |
100 |
Philadelphia |
100 |
Washington |
100 |
| File Type | application/msword |
| File Title | Never In Care Project |
| Author | DTBE User |
| Last Modified By | arp5 |
| File Modified | 2007-05-18 |
| File Created | 2007-05-18 |
© 2026 OMB.report | Privacy Policy