2 Assessment
Online Skills Training for PCPs on Substance Abuse (NIDA)
N44DA-9-2214-Attachment5AssessmentForms_March2011
Physicians
OMB: 0925-0632
Attachment 5: Assessment Instrument
Online Skills Training for PCPs on Substance Abuse (NIDA)
January 2011
ASSESSMENT INSTRUMENT
Text of instruments and screenshots follows. The assessment instruments are online at http://www.sbirttraining.com/assessment, with OMB number added appropriately.
OMB # 0925-XXX
Expiration Date xx/xxxx
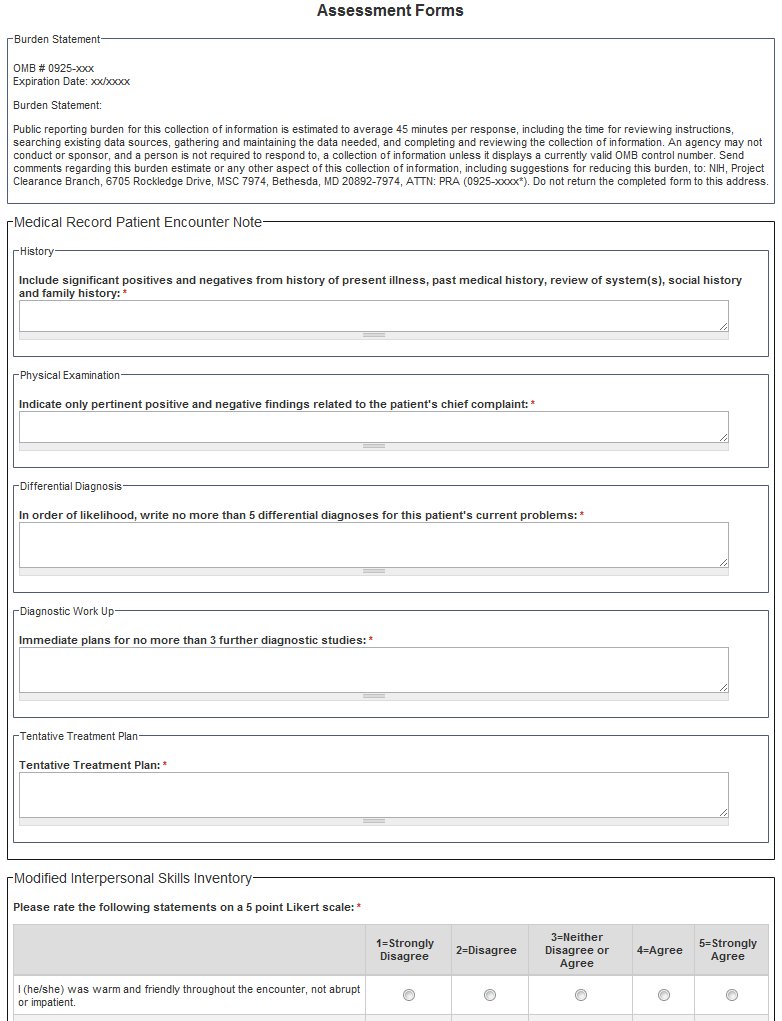
BURDEN STATEMENT
Public reporting burden for this collection of information is estimated to average 45 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not required to respond to, a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden, to: NIH, Project Clearance Branch, 6705 Rockledge Drive, MSC 7974, Bethesda, MD 20892-7974, ATTN: PRA (0925-xxxx*). Do not return the completed form to this address.
Medical Record Patient Encounter Note – SOAP Note: Pre-, Post-, Follow-up
Form will be online at http://www.sbirttraining.com/assessment, with OMB number added appropriately
Medical Record Patient Encounter Note (SOAP note)
History
Include significant positives and negatives from history of present illness, past medical history, review of system(s), social history and family history.
Physical Examination
Indicate only pertinent positive and negative findings related to the patient's chief complaint.
Differential Diagnosis
In order of likelihood, write no more than 5 differential diagnoses for this patient's current problems:
1.
2.
3.
4.
5.
Diagnostic Work Up
Immediate plans for no more than 3 further diagnostic studies:
1.
2.
3.
Tentative Treatment Plan
1.
2.
3.
4.
5.
Learner Self-Assessment Modified Interpersonal Skills Inventory: Pre-, Post-, Follow-up
Please rate the following questions on a 5 point Likert Scale:
1=Strongly Disagree, 2=Disagree, 3=Neither Disagree or Agree, 4=Agree, 5=Strongly Agree
I (he/she) was warm and friendly throughout the encounter, not abrupt or impatient.
I (he/she) listened carefully as the patient described the problem and did not interrupt him or her.
I (he/she) encouraged the patient to ask questions.
I (he/she) gave the patient adequate time to ask any questions and to express his or her thoughts and concerns.
I (he/she) used words that the patient could understand when explaining any technical or medical terms.
I (he/she) did not lecture or talk down to the patient.
I (he/she) showed interest in the patient as a person, did not act bored, or ignore what the patient had to say.
I (he/she) expressed empathy for the patient's suffering when appropriate
I (he/she) used an appropriate and polite manner to end the interview.
Overall, I felt (he/she seemed) comfortable in the interview.
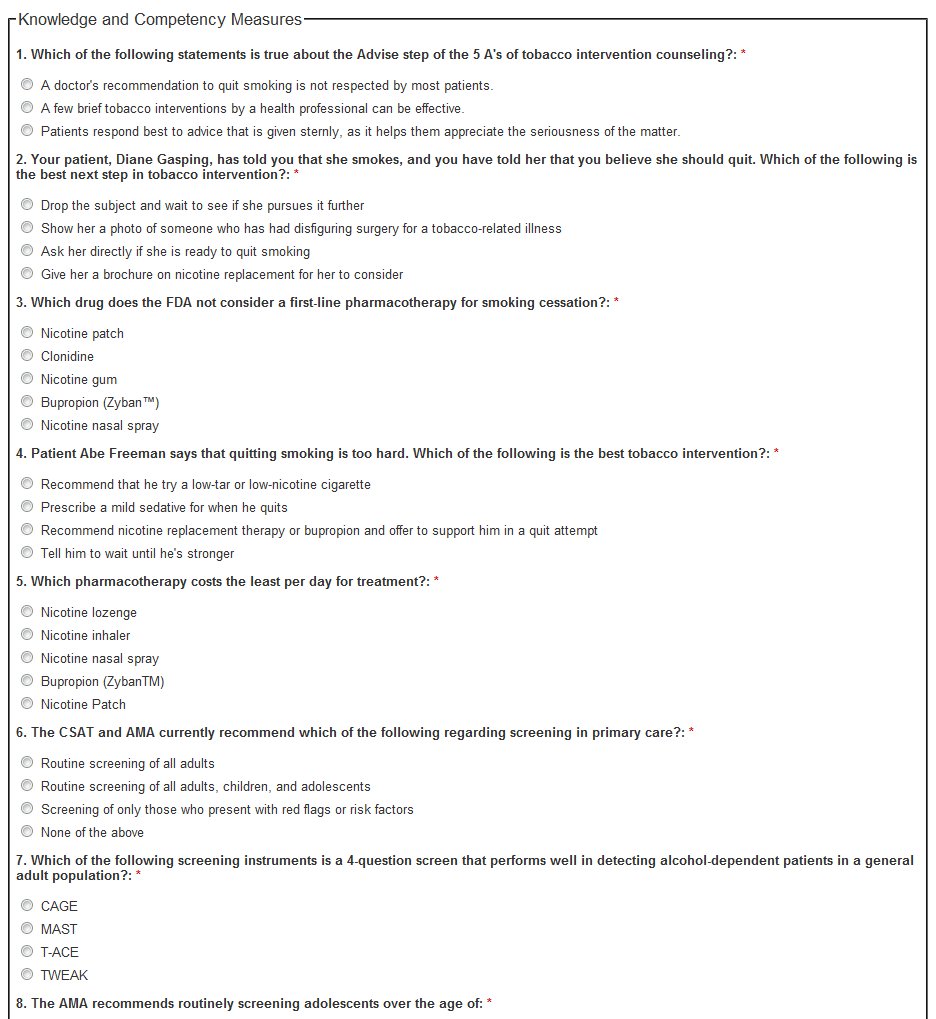
Knowledge and Competency Measure: Pre-, Post- and Follow-up
1. Which of the following
statements is true about the Advise step of the 5 A's of tobacco
intervention counseling?
A doctor's recommendation to
quit smoking is not respected by most patients.
A few brief
tobacco interventions by a health professional can be
effective.
Patients respond best to advice that is given
sternly, as it helps them appreciate the seriousness of the matter.
2. Your patient, Diane Gasping,
has told you that she smokes, and you have told her that you believe
she should quit. Which of the following is the best next step in
tobacco intervention?
Drop the subject and wait to see if
she pursues it further
Show her a photo of someone who has had
disfiguring surgery for a tobacco-related illness
Ask her
directly if she is ready to quit smoking
Give her a brochure on
nicotine replacement for her to consider
3. Which drug does the FDA not
consider a first-line pharmacotherapy for smoking
cessation?
Nicotine patch
Clonidine
Nicotine
gum
Bupropion (Zyban™)
Nicotine nasal
spray
4. Patient Abe Freeman says that
quitting smoking is too hard. Which of the following is the best
tobacco intervention?
Recommend that he try a low-tar or
low-nicotine cigarette
Prescribe a mild sedative for when he
quits
Recommend nicotine replacement therapy or bupropion and
offer to support him in a quit attempt
Tell him to wait until
he's stronger
5. Which pharmacotherapy costs
the least per day for treatment?
Nicotine
lozenge
Nicotine inhaler
Nicotine nasal
spray
Bupropion (ZybanTM)
Nicotine Patch
6.
The CSAT and AMA currently recommend which of the following
regarding screening in primary care?
Routine screening of
all adults
Routine screening of all adults, children, and
adolescents
Screening of only those who present with red flags
or risk factors
None of the above
7. Which of the following
screening instruments is a 4-question screen that performs well in
detecting alcohol-dependent patients in a general adult
population?
CAGE
MAST
T-ACE
TWEAK
8. The AMA recommends routinely
screening adolescents over the age of:
10
12
13
14
17
9. Which of the following is a
barrier to screening for alcohol use problems?
Patient
resistance
Discomfort discussing substance abuse
Time
constraints
Lack of insurance coverage
All of the above
10. Which of the following
statements is true about Brief Interventions (BIs)?
BIs
attempt to motivate patients to participate in their own treatment
for alcohol use.
Compared to formal substance abuse treatment,
BIs are often shorter in duration and frequency.
BI uses many
of the same techniques used in addressing chronic health problems
such as obesity and blood pressure management.
All of the
above
None of the above
11. When assessing a patient's
readiness to change, what is the most stage-appropriate assistance
that you can provide to an individual in the contemplation
stage?
Help the patient explore the benefits and
challenges of changing the problem behavior
Provide information
about alcohol use, risk levels, and health consequences
Help
the patient anticipate potential difficulties and apply corrective
action, if needed
Assist the patient in developing realistic
goals and a plan for changing drinking behavior
None of the
above are appropriate
12. Sally has a history of
alcohol use. She has increasingly become concerned about her
drinking habits and has decided that she really wants to change. She
is hoping that you can assist her in her treatment. What treatment
option is the best for her at this point?
Brief
intervention
Motivational
Interviewing
Pharmacotherapy
Referral
13. Zack has arrived at your
office with an alcohol-related injury. You apply the AUDIT screening
instrument in order to determine his level of use and he scores a
28. Based on this score, what can you infer?
Zack has a
drinking issue that may be curtailed by an in-house brief
intervention.
Since he came to your office with an
alcohol-related injury, he might be motivated to change.
Zack's
score is very high and might warrant pharmacological
intervention.
You need to refer him to a substance abuse
specialist because his score is well above what can be handled
in-house.
14. Frank comes to your office
after having relapsed. He is sure that this is a sign he can't stay
sober. What would you say next?
You're right. Erasing a
month's worth of sobriety shows a definite lack of willpower.
I
am very disappointed that you chose to drink.
Come back when
you're committed to getting your drinking under control.
One
failure does not mean you lack the willpower to follow through with
recovery
15. Alex has had repeated
outpatient treatment attempts, but they have not proven successful.
He has increased his alcohol consumption dramatically since the last
treatment attempt and now he is posing a danger to those around him.
What is an appropriate next step in his treatment?
Try
another round of outpatient treatment in hopes that this time it
will prove successful.
Prescribe him pharmacological
treatment in hope that it will curtail his need for alcohol.
Try
to motivate him to change through directed conversations and
repeated office visits.
Refer him to an inpatient
treatment facility which can provide a more intensive treatment
regimen.
16. Which of the following have reimbursement codes for Screening and Brief intervention?
Medicare
Commercial
insurance
Medicaid
All of these
17. A patient is admitted from the ER into the hospital after an automobile accident. Under the proposed Joint Commission standards for SBIRT, this patient should....
Be screened for alcohol, and if
positive receive brief intervention
Be screened for excessive
alcohol use, use of illicit drugs, misuse of prescription drugs, and
tobacco use, receive brief intervention and follow up after
discharge
Be screened if the ER indicated substance use was
suspected or confirmed, and brief intervention provided
Be
screened at the attending physician's discretion and treatment
initiated as necessary for substance use.
Not receive an
intervention - no screening required due to Uniform Policy and
Provision Law (UPPL) concerns
18. For a physician who treats mostly adults in an urban setting, which screening instrument would you choose?
NIAAA
CAGE
DAST
TICS
NIDA-modified
ASSIST
19. Estimating from national statistics, about how many of the patients you see as a primary care provider will have a substance use/abuse problem?
Less than 10%
10%
20%
35%
Over
40%
20. SBIRT is successful with which of the following groups:
Nicotine users
Illicit drug
users
Moderate & heavy alcohol users
Non-dependent
drinkers
Illicit drug users and moderate & heavy alcohol
users only
All of the above
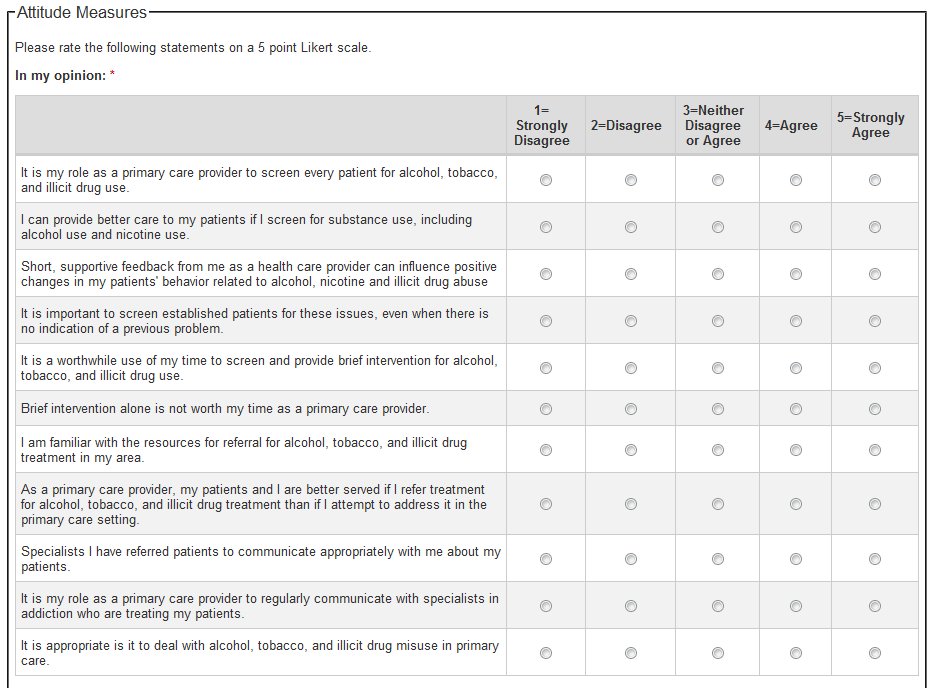
Participant Attitude Measure: Pre-, Post-, and Follow-up
Please rate the
following questions on a 5 point Likert Scale:
1= Strongly
Disagree, 2=Disagree, 3=Neutral, 4=Agree, 5=Strongly Agree
In my opinion:
It is my role as a primary care provider to screen every patient for alcohol, tobacco, and illicit drug use.
I can provide better care to my patients if I screen for substance use, including alcohol use and nicotine use.
Short, supportive feedback from me as a health care provider can influence positive changes in my patients' behavior related to alcohol, nicotine and illicit drug abuse
It is important to screen established patients for these issues, even when there is no indication of a previous problem.
It is a worthwhile use of my time to screen and provide brief intervention for alcohol, tobacco, and illicit drug use.
Brief intervention alone is not worth my time as a primary care provider.
I am familiar with the resources for referral for alcohol, tobacco, and illicit drug treatment in my area.
As a primary care provider, my patients and I are better served if I refer treatment for alcohol, tobacco, and illicit drug treatment than if I attempt to address it in the primary care setting.
Specialists I have referred patients to communicate appropriately with me about my patients.
It is my role as a primary care provider to regularly communicate with specialists in addiction who are treating my patients.
It is appropriate is it to deal with alcohol, tobacco, and illicit drug misuse in primary care.
Please choose Yes or No for each option:
These are the most significant barriers to implementing SBIRT in my practice...
|
This barrier currently exists |
This training program helped me address this barrier |
My lack of time w/my patients |
Yes / No |
Yes / No |
Patient resistance to discussing these topics |
Yes / No |
Yes / No |
My lack of training in treating these areas |
Yes / No |
Yes / No |
I am not comfortable discussing these areas. |
Yes / No |
Yes / No |
Primary care is not the right setting. |
Yes / No |
Yes / No |
Patients are unlikely to want me to intervene on these topics. |
Yes / No |
Yes / No |
Intervention in the primary care setting is not likely to be successful with these problems. |
Yes / No |
Yes / No |
Difficult to get reimbursed for these services |
Yes / No |
Yes / No |
Distracts from the real reason the patient came in to my office |
Yes / No |
Yes / No |
This is not my role as a physician. |
Yes / No |
Yes / No |
My physician colleagues do not believe in doing this. |
Yes / No |
Yes / No |
My staff is not able to handle additional work |
Yes / No |
Yes / No |
Practice Changes Measure: Pre-, Post- and Follow-up
Please choose Yes or No for each option:
Potential Practice Changes |
This change would make sense in my current practice setting. |
This is a change I WILL MAKE in the next 2 months. |
Increasing screening for alcohol use problems |
Yes / No |
Yes / No |
Increasing screening for tobacco use problems |
Yes / No |
Yes / No |
Increasing screening for illicit drug use |
Yes / No |
Yes / No |
Increasing brief intervention for alcohol use problems |
Yes / No |
Yes / No |
Increasing brief intervention for tobacco use problems |
Yes / No |
Yes / No |
Increasing brief intervention for illicit drug use |
Yes / No |
Yes / No |
Increasing referrals for alcohol use problems |
Yes / No |
Yes / No |
Increasing referrals for tobacco use problems |
Yes / No |
Yes / No |
Increasing referrals for illicit drug use |
Yes / No |
Yes / No |
Other? Please describe... |
Yes / No |
Yes / No |
| File Type | application/msword |
| File Title | Attachment 5: Assessment Instrument |
| Author | rossie |
| Last Modified By | dealmeig |
| File Modified | 2011-01-12 |
| File Created | 2010-07-13 |
© 2026 OMB.report | Privacy Policy