5 Vspe
Web-based Skills Training for SBIRT (Screening Brief Intervention and Referral to Treatment) NIDA
Attachment 10_VSPEs 11 2 11
Primary Care Providers
OMB: 0925-0646
Attachment 10: VIDEO STANDARDIZED PATIENT EVALUATIONS
Web-based Skills Training for SBIRT (Screening Brief Intervention and Referral to Treatment)
November 2011
OMB # 0925-XXX
Expiration Date xx/xxxx
Public reporting burden for this collection of information is estimated to average less than 35 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information and typing your written responses. Each time the assessment is completed, it is expected to be completed in a single sitting. An agency may not conduct or sponsor, and a person is not required to respond to, a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden, to: NIH, Project Clearance Branch, 6705 Rockledge Drive, MSC 7974, Bethesda, MD 20892-7974, ATTN: PRA (0925-xxxx*). Do not return the completed form to this address.
|
Video Standardized Patient Evaluations
Alcohol: James Tinsley, 42 year old African American male
Mr. Tinsley presents with abdominal pain. He has had epigastric pain intermittently for the past several months with increasing frequency and severity over the past month. He describes the pain as gnawing and sometimes sharp. It is worse at night and early in the morning and improves sometimes after meals. He has tried over the counter Mylanta, Rolaids, and Zantac all of which have been helpful but he is concerned that he has had to increase the use of these to a daily basis. He denies vomiting, diarrhea or fever. He has had no melena. He considers himself to be generally healthy and has had no surgery or serious medical problems. He is worried about his pain because his father died of stomach cancer. Further discussion reveals that his father was a heavy drinker for many years.
Physical exam: afebrile, BP: 146/92, Pulse: 88, Resp: 12, Weight: 212 pounds, Height 71 inches
Abdomen: protuberant, positive bowel sounds, no bruits, soft, mild egigastric tenderness without rebound or guarding, no hepatosplenomegaly. The remainder of his exam is unremarkable.
Video Clip--Mr. Tinsley: "Hi Doc. I hope you can help me with my stomach today. Nothing I'm doing seems to work".
1. How would you introduce screening to Mr. Tinsley?
[Open response text box]
Mr. Tinsley's ASSIST and AUDIT-C results are as follows:
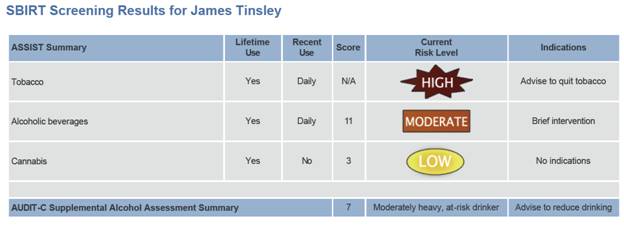
2. Looking over these results and in light of Mr. Tinsley's medical exam, for which substance(s) would you choose to provide brief intervention (BI)?
a. Tobacco
b. Alcohol
c. Cannabis
d. None of the above
3. Briefly describe how you would give feedback.
[text box]
4. How would you begin the process of giving Mr. Tinsley feedback about his substance use?
[text box]
Video Clip--Mr. Tinsley: "Well, of course I know I shouldn't be smoking, so I don't need a lecture about that. And ya know, I don't really think it's affecting my health at all, at least not yet. I'm here about my stomach pain. I don't see what my smoking has to do with that."
5. What would you say to Mr. Tinsley in response to his thoughts about his smoking?
[text box]
6. Despite your best efforts, Mr. Tinsley does not want to talk about smoking. However, he is willing to discuss alcohol consumption. What information would you include in giving Mr. Tinsley feedback about his rate of alcohol use?
[text box]
Video Clip--Mr. Tinsley: "Wow, that's a lot to take in. I didn't see any harm in drinking. So what you're telling me is that alcohol is actually making my stomach worse? And, I'm increasing my risk of stomach cancer by drinking? This is really not what I expected to hear."
7. How would you respond to Mr. Tinsley?
[text box]
8. What specific advice would you give Mr. Tinsley? How would you say it?
[text box]
Video Clip--Mr. Tinsley: "Well, I'm not sure I want to quit drinking completely. My job's pretty demanding, so I like to have a few drinks with my buddies to relax after a hard day. They might think I'm some kind of an alcoholic if I just stopped all of a sudden. (pause)But, ya know, I'm getting tired of dealing with this stomach pain and I don't want it to get worse, guess I'm not sure what to do.”
9. Help Mr. Tinsley figure out his next step.
[text box]
10. How would you end the brief intervention?
[text box]
Dylan Williams, 34 year old Caucasian male
Mr. Williams is a software engineer, married with a 2 y.o. son. He has been complaining of a productive cough and fatigue for 3 weeks. He felt hot and flushed at times when the illness began but has no documented fever. He denies chills, nausea or post-tussive emesis. He has no sore throat or rhinorrhea. He has no ill contacts and no recent travel. He exercises 2-3 times per week on a regular basis, but the fatigue and cough have disrupted this routine. The fatigue is also starting to interfere with his desire to help out at home. He has been smoking off and on since his early 20's, and more recently has cut back smoking to one half pack per day. On examination he is afebrile with normal vital signs, his lungs are clear to auscultation and percussion and the remainder of his physical examination is normal. He has a normal expiratory peak flow and a chest x-ray is normal
Screening results:
· Tobacco: high risk
· Alcohol: ASSIST: low risk, AUDIT-C: low risk
· No other drug use
Video Clip--Mr. Williams "Hi doc. So...did you take a look at my x-ray yet? I hope it isn't serious."
1. How would you present to Mr. Williams the purpose of the drug and alcohol screening?
[Open response text box]
Video Clip--Mr. Williams "(nodding) Yeah, that makes sense – it's good you’re asking about drug use. I don't do any of that."
2. Give Mr. Williams his screening results:
[Open response text box]
Video Clip--Mr. Williams: "You’re not going to give me a lecture are you? I know smoking isn't good for me, and I already cut down to about half a pack a day. I hardly ever drink and I work out every week- smoking a little bit is my only bad habit."
3. What would you say to Mr. Williams in response to his thoughts about smoking?
[text box]
4. What words would you use to advise Mr. Williams to quit smoking?
[Text box]
5. How would you make your advice to Mr. Williams personal to his situation?
[Text box]
Video Clip--Mr. Williams: "I suppose you're right. I know it’s bad for my 2 year old to be around smoke, and I can tell when I run or bike that I’m still short of breath even though I've cut back. But I've tried to quit so many times, and I just can't do it. I always end up miserable and stressed out."
6. How would you respond to Mr. Williams
[Text box]
Video Clip--Mr. Williams: "Alright, (sigh), I've guess been avoiding this for a long time, but I should probably give it another try. (pause) Any ideas for me? Is there anything that can help?
7. Would you consider recommending pharmacotherapy for Mr. Williams? Why or why not?
[text box]
8. What are the four elements of a brief behavioral plan for quitting that you could develop with Mr. Williams in your office?
[text box]
9. What would you say in referring Mr. Williams to the tobacco quitline?
[text box]
| File Type | application/msword |
| Author | Glenda Polwarth |
| Last Modified By | bbarker |
| File Modified | 2011-11-29 |
| File Created | 2011-11-29 |
© 2026 OMB.report | Privacy Policy