LAN Measurement page
Updates for the 2018 LAN Measurement page.docx
Generic Clearance for the Heath Care Payment Learning and Action Network (CMS-10575)
LAN Measurement page
OMB: 0938-1297
Here is the hyperlink to the 2018 APM measurement webpage that has already been mostly updated. This word version of text is provided in case edits are suggested before the website goes live when the 2018 APM measurement efforts starts in May.
[Landing page]
Nearly one
quarter of all US health care payments are already flowing through
alternative payment models –
Where does your organization
stand?
The Health Care Payment Learning and Action Network (LAN) was launched in 2015 to accelerate the health care system’s transition to alternative payment models by combining the innovation, power, and reach of the private and public sectors. By sharing information about successful models and encouraging private entities to share their best practices, the LAN works to reduce barriers and accelerate adoption of APMs.
The development and adoption of alternative payment models (APMs) is central to revolutionizing health care payment in the United States. APMs can realign treatment and payment incentives with the aim of improving care quality while managing cost.
The Health Care Payment Learning and Action Network (LAN) is measuring nationwide progress toward alternative payment model (APM) adoption as a means to a more effective health care system. As leaders in this space, participating health plans will contribute to that understanding.
PRA Disclosure Statement
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is 0938-1297. The expiration date is 01/31/2019. The time required to complete this information collection is estimated to average 25 hours per calendar year per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. If you have comments concerning the accuracy of the time estimate(s) or suggestions for improving this form, please write to: CMS, 7500 Security Boulevard, Attn: PRA Reports Clearance Officer, Mail Stop C4-26-05, Baltimore, Maryland 21244-1850. Please do not send applications, claims, payments, medical records or any documents containing sensitive information to the PRA Reports Clearance Office. Please note that any correspondence not pertaining to the information collection burden approved under the associated OMB control number listed on this form will not be reviewed, forwarded, or retained. If you have questions or concerns regarding where to submit your documents, please contact Grischa Metlay at [email protected].
[“Why Participation Matters” tab]
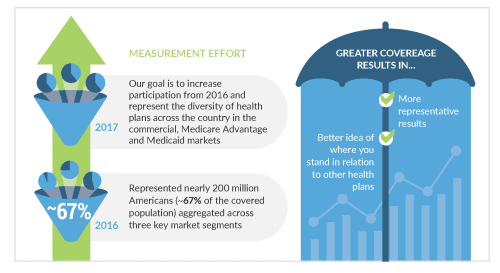
How are health care payments shifting away from traditional fee-for-service arrangements toward alternative payment models (APMs)? Where does the nation stand in APM adoption across the commercial, Medicare Advantage, and Medicaid markets?
Having a common definition of alternative payment is critical to our ability to move forward together. When health plans report payments in alignment with the Health Care Payment Learning and Action Network (LAN) APM Framework, you gain an understanding of your position in the market.
The LAN is currently recruiting health plans to participate in the 2018 APM Measurement Effort. Grab a seat at the table as health plans across the country contribute to our collective understanding of progress in APM adoption. Your participation will inform and bolster our understanding of nationwide progress toward APMs, and thus give you a better idea of where you stand in relation to other health plans.
[“How will we measure?” tab]
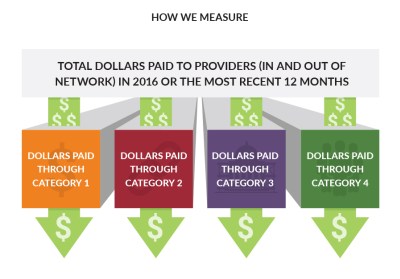
For 2018, participating health plans will report total in- and out-of-network health care spending paid to providers through each of the categories during 2017 or the most recent 12 months in the commercial, Medicaid and Medicare Advantage markets. The LAN works directly with participants to ensure a clear understanding of how to classify payments in the original APM framework. This makes participation as simple and straightforward as possible.
Individual plan data will be kept strictly confidential. It will not be shared with other health plan participants or parties outside of the LAN data collection team. For reporting purposes, individual plan data will be aggregated with data from other health plans.
More detailed information on the 2018 APM Measurement Effort methodology, FAQs, and data collection tool are linked below:
[“How do you define APMs?” tab]
The LAN’s original APM Framework provides standardized definitions and categories of APMs. The original APM framework was first published in January 2016 and was refreshed in 2017, in part based on feedback from LAN Measurement Effort participants. We will use category definitions from the refreshed APM Framework to measure APMs using similar metrics and methodology as were used in 2017.

[“How do you define APMs?” tab]
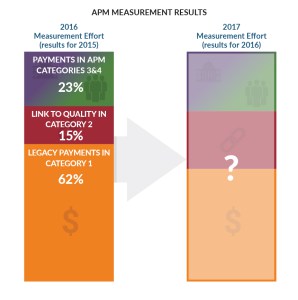
The LAN’s second APM Measurement Effort in 2017, which included data on roughly 245 million Americans (84% of covered lives), revealed that 29% of payments made in 2016 were in APM categories 3 and 4.
The 2018 Measurement Effort will provide information on payments made in 2017, allowing for an indication of the movement toward APM adoption.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | Metlay, Grischa J |
| File Modified | 0000-00-00 |
| File Created | 2021-01-21 |
© 2026 OMB.report | Privacy Policy