Form 1 2018 CRUNK-NCI sandpit research call
Conference, Meeting, Workshop, and Poster Session Registration Generic Clearance (OD)
2018 CRUK-NCI_sandpit research call_Final
Sandpit Workshop
OMB: 0925-0740
OMB Number: 0925-0740
Expiration Date: 05/2019
![]()

Implementing
Digital Health Interventions For Cancer Prevention
sandpit
workshop
28-31
October 2018
application
guidelines
Implementing Digital Health Interventions For Cancer Prevention: Sandpit Workshop
CONTENTS
Collection of this information is authorized by The Public Health Services Act, Section 410 (42 U.S.C. § 285 : US Code - Section 285: Purpose of Institute). Rights of applicants are protected by The Privacy Act of 1974. Participation is voluntary, and there are no penalties for not submitting an application or withdrawing an application from consideration at any time. Refusal to participate will not affect your benefits in any way. The information collected will be kept private to the extent provided by law. The information you provide will not be publicly released and will be used by the representatives involved in planning the training workshop to select workshop participants. This workshop application solicitation document is being sent out so that individuals interested in participating in the workshop can submit information that will help the planning committee select the most suitable applicants for the workshop.
Public reporting burden for this collection of information is estimated to average 120 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not required to respond to, a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden to: NIH, Project Clearance Branch, 6705 Rockledge Drive, MSC 7974, Bethesda, MD 20892-7974, ATTN: PRA (0925-0740). Do not return the completed form to this address.
EXECUTIVE SUMMARY
Digital health tools can be used to collect health data, support the exchange of health information between consumers, providers, and systems, and serve as the basis of interventions aimed at enhancing health and reducing disease burden. It is estimated that 40% of cancer incidence are associated with modifiable behaviors such as smoking, diet, physical activity, and alcohol consumption and therefore may be preventable. Digital health interventions hold promise in supporting healthy behavioral choices. Yet limited use of evidence-based interventions within systems such as the home, community and healthcare systems has resulted in missed opportunities for improved population health. Research to increase our understanding of contextual factors (e.g., social, cultural, and organization) that influence the implementation and uptake of digital health interventions for cancer prevention are needed.
To address this issue, the US National Cancer Institute (a component of the National Institutes of Health, which is an agency within the U.S. Department of Health and Human Services) and Cancer Research UK (CRUK) are seeking applications to participate in a "sandpit" (i.e. ideas lab) that will bring together a broad group of participants, from a range of different disciplines, including implementation science, computer science, behavioral science, human-computer interaction, ethnography, anthropology, communication, and systems engineering in order to generate innovative ideas for advancing cancer prevention through the effective implementation of digital health tools. Applicants from a variety of academic, industry, and community sectors are welcome.
The three-day sandpit will take place 28-31 October 2018 in Potomac, MD with participants arriving for an evening briefing on the evening of October 28th. We anticipate that participants will help define challenge areas and generate novel hypotheses and ideas that can be tested experimentally or through analysis of extant data sources. Sandpit participants will be expected to engage constructively with each other, the event facilitators, the director, and the mentors in order to develop collaborative research ideas. We particularly welcome applications from early- and mid-career individuals interested in contributing their expertise and novel thinking to generate transformative hypotheses and project ideas. Participants will have the opportunity to:
Network and form collaborations with researchers outside their typical domain and across organizations
Form new collaborative teams and generate project ideas
Receive NCI and CRUK programmatic guidance
NCI invites prospective participants to apply for participation in the sandpit by 4 June 2018 at 5 PM EDT / 10 PM BST. The sandpit is an intensive, residential workshop, and participants must attend all three days of the event. By submitting an application, you are committing to complete all three days of the workshop.
Digital
Health Tools Any device or
software application that harnesses the transformational power of modern
information and communication technology for improving health and
healthcare (e.g. telehealth platforms, patient portals/electronic
health records, wearable devices, and mobile apps).
Population
health The
health outcomes of a group of individuals, including the
distribution of such outcomes within the group.
Preventable
cancers:
Cancers
that are linked to modifiable behavioral risk factors, such as
smoking, diet, physical activity, and alcohol consumption.
Implementation
The
use of strategies to adopt and integrate evidence-based health
interventions into clinical and community settings in order to
improve patient outcomes and benefit population health.
Context Context is defined
as a set of characteristics and circumstances that surround the
implementation effort. Context includes the outer setting, such as
the social, cultural, economic, political, legal, and physical
environment in which the intervention takes place, as well as the
inner setting, which refers to the structural
characteristics, networks, culture, resources, leadership qualities
and climate of the implementation setting. The characteristics
of individuals involved
in the implementation efforts, such as their knowledge,
self-efficacy and motivations, are also an important component of
context.
Interdisciplinary
research Research
undertaken by scholars from two or more distinct scientific
disciplines that is based on a conceptual model that
links/integrates theoretical frameworks from those disciplines, uses
study design and methodology that is not limited to any one field,
and leverages the perspectives/skills of the involved disciplines
throughout the research process.
Implementation Outcomes
Implementation outcomes can be measured at various levels, for instance - at the individual level (providers or consumers) and organization or setting. Implementation outcomes include (but are not limited to) measures of acceptability, adoption, appropriateness, feasibility, fidelity, implementation cost, penetration, sustainability.
What are the barriers and facilitators to implementing effective digital health interventions at the population level?
How can a better understanding of context and systems (particularly at the population level) lead to improved implementation of digital health interventions?
How do differences between contexts or systems influence the successful implementation of digital health technology? Which specific aspects of a context or specific characteristics of a system are most salient for implementation success?
How can digital tools be leveraged to improve the implementation of interventions within and across different contexts and health systems?
How can contextual factors be used to adapt digital health interventions to increase implementation success?
How can evidence about the implementation of effective digital health interventions directly inform policy and practice?
To express interest in participating, please send: (1) your CV; (2) the names of two professional references; (3) a cover letter that outlines your interests in applying for the sandpit; (4) a visual representation (e.g., diagram or mental model) that illustrates a conceptual schema of your area of interest; and (5) a letter of commitment from your organization or institution.
The cover letter should not exceed 800 words, and it should include: your background, interests, and expertise, particularly as they relate to this sandpit topic; your approach to working in a team; and your experience with or interest in stepping outside your area of expertise and thinking creatively and innovatively to develop novel approaches in partnership with individuals you may not know. Applicants should demonstrate the skills, expertise, and capacity for successful collaboration in this intensive, interactive, and fast-paced event. It is strongly advised that applicants do not merely list their achievements (e.g., publications, research experience, funding track record), but rather use them to demonstrate innovative and collaborative capacity.
The visual representation should depict the components and processes that are central to your area of interest (see example and more information on the last page). Please caption the diagram with a brief description of the area in language that would be accessible to people with expertise in a different area (no more than 300 words). The visual representation may be drawn by hand and scanned or illustrated electronically and submitted in pdf format.
The letter of commitment should include a covering statement from a representative of your organization (e.g., supervisor, manager, or other relevant persons) confirming that, in the event of receiving a seed grant from CRUK, their organization is willing and able to engage in and support a collaborative project. The letter should acknowledge the following: (a) neither indirect funds nor personnel support will be provided; and (b) the participant shall be allowed to spend up to 5% of their time on the Sandpit project if awarded a CRUK seed grant.
SUBMISSION DEADLINE
The submission deadline for completed applications is 4 June 2018, at 5 PM EDT/10 PM BST. Applications should be emailed to [email protected] . Application receipt will be acknowledged via email within two business days. If you do not receive acknowledgement, please send an email inquiry to be certain your application was received. Applications submitted after the deadline will not be considered.
ELIGIBILITY
Participants will be selected for the sandpit workshop via expert review of the application materials. All applications received by the deadline will be reviewed by an expert review committee.
Applications are welcome from academic, industry, and community sectors. The group of people selected will be intentionally diverse, and it is intended that a wide variety of disciplines, including those from private, public and third sector organizations and community groups. If you would like to help transform the future of digital health in the context of cancer prevention, we invite you to apply, regardless of your expertise or background. We are more interested in new ideas, underpinned by radical and innovative thinking. We regret that, on this occasion, PhD students and applicants based outside of the UK and US are not eligible to apply.
The Sandpit is an intensive, residential workshop, and participants must attend all three days of the event as well as a briefing the evening before the event starts. By submitting an application, you are committing to complete all three days of the workshop. Participants will be reimbursed for travel, subsistence and lodging expenses in accordance with NIH policy.
NCI is committed to providing reasonable accommodations for qualified individuals with a disability.
CRUK will provide a grant opportunity for proposals selected at the workshop. It is anticipated that at least four proposals will receive awards of up to £40,000 each. The proposals will be reviewed, funded, and administered independently by CRUK. The Sandpit workshop will include both US and UK participants. CRUK grant proposals require at least one UK-based co-applicant. Funds will be distributed to a UK-based organization and sub-contracts to other organizations in the USA and UK will be established as needed. Following the sandpit, each successful project team will have four weeks to draft a full feasibility study proposal that covers their group’s intended activities as presented at the sandpit. PIs who are not established members of a recognized research organization must be accommodated by a research organization and provided with appropriate facilities to carry out the research as agreed by the Head of the organization in the cover letter. The specific role of each project team member, in terms of their involvement with, and contribution to, the project will be agreed on by the project team (i.e., some members may be named as joint lead investigators or contribute in an advisory capacity, etc.).
Feasibility study proposals will be submitted via CRUK’s electronic Grant Management System (eGMS) by 30 November 2018. Feasibility studies will last up to 12 months in duration, starting in February 2019. All awards are subject to CRUK’s terms and conditions. CRUK will offer support and advice throughout the lifetime of the project, including quarterly teleconferences with project groups. A report of feasibility outputs will be required by CRUK on completion of the project. Additional guidance on the post-award processes will be made available at the sandpit.
• 4 June, 2018, at 5 PM EDT/10 PM BST - Deadline for submission of application materials
• July 2017 - Applicants notified of outcome
• 29-31 October 2018 - Sandpit held (Potomac, MD)
• 30 November 2018 - Deadline for submission of CRUK Innovation grant proposals
• February 2019 - Feasibility studies commence
FURTHER INFORMATION
US
applicants
please
contact:
Dr.
Kara L. Hall
Email:
[email protected]
Phone:
(240) 276-6831
UK applicants
please contact:
Dr. Gillian
Rosenberg Email:
[email protected]
Phone: 020 3469
5250 

Additional information pertaining to the visual representation
Applications should include a “mental model” or diagrammatic illustration of one’s area expertise. Although there are many ways to approach this kind of visualization, simple models often include an arrangement of concepts linked by arrows to illustrate relationships among key components of a problem space.
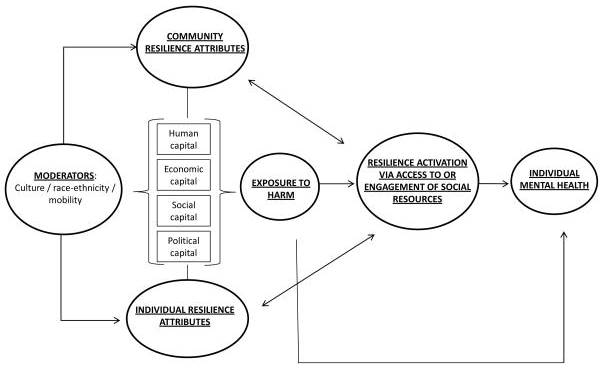
Abramson, D. M., Grattan, L. M., Mayer, B., Colten, C. E., Arosemena, F. A., Bedimo-Rung, A., & Lichtveld, M. (2015). The resilience activation framework: a conceptual model of how access to social resources promotes adaptation and rapid recovery in post-disaster settings. The journal of behavioral health services & research, 42(1), 42-57.
1 Burke, L. E., Ma, J., Azar, K. M., Bennett, G. G., Peterson, E. D., Zheng, Y., ... & Turan, T. N. (2015). Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation, 132(12), 1157-1213.
2 Patrick, K., Hekler, E. B., Estrin, D., Mohr, D. C., Riper, M. M., Crane, D., ... Riley, W. T. (2016). The pace of technologic change: Implications for digital health behavior intervention Research. American Journal of Preventive Medicine, 51(5), 816-824.
3 Yardley, L., Morrison, L., Bradbury, K., & Muller, I. (2015). The person-based approach to intervention development: application to digital health-related behavior change interventions. Journal of medical Internet research, 17(1).
4 Parkin, D. M. (2011). 1. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. British journal of cancer, 105(S2), S2.
5 Islami, F., Goding Sauer, A., Miller, K. D., Siegel, R. L., Fedewa, S. A., Jacobs, E. J., ... & Flanders, W. D. (2018). Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA: a cancer journal for clinicians, 68(1), 31-54.
6 Burke, L. E., Ma, J., Azar, K. M., Bennett, G. G., Peterson, E. D., Zheng, Y., ... & Turan, T. N. (2015). Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation, 132(12), 1157-1213.
7 Krumeich, A., Weijts, W., Reddy, P., & Meijer-Weitz, A. (2001). The benefits of anthropological approaches for health promotion research and practice. Health Education Research, 16(2), 121-130.
8 O’Connor, S., Hanlon, P., O’Donnell, C. A., Garcia, S., Glanville, J., & Mair, F. S. (2016). Understanding factors affecting patient and public engagement and recruitment to digital health interventions: a systematic review of qualitative studies. BMC medical informatics and decision making, 16(1), 120.
9 May, C. R., Johnson, M., & Finch, T. (2016). Implementation, context and complexity. Implementation Science, 11(1), 141.
10 Edwards, N., & Barker, P. M. (2014). The importance of context in implementation research. JAIDS Journal of Acquired Immune Deficiency Syndromes, 67, S157-S162.
11 Pfadenhauer, L. M., Mozygemba, K., Gerhardus, A., Hofmann, B., Booth, A., Lysdahl, K. B., ... & Rehfuess, E. A. (2015). Context and implementation: a concept analysis towards conceptual maturity. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen, 109(2), 103-114.
12 Perski, O., Blandford, A., West, R., & Michie, S. (2016). Conceptualising engagement with digital behaviour change interventions: a systematic review using principles from critical interpretive synthesis. Translational behavioral medicine, 7(2), 254-267.
13 Edwards, N., & Barker, P. M. (2014). The importance of context in implementation research. JAIDS Journal of Acquired Immune Deficiency Syndromes, 67, S157-S162.
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | Hall, Kara (NIH/NCI) [E] |
| File Modified | 0000-00-00 |
| File Created | 2021-01-21 |
© 2026 OMB.report | Privacy Policy