NACP Year 2 (16-606) and Year 4 (14-1404) _AIRS Performance Measures Spreadsheet Instructions
Att3a1_AIRS PM Reporting Spreadsheet Instructions.docx
Asthma Information Reporting System (AIRS)
NACP Year 2 (16-606) and Year 4 (14-1404) _AIRS Performance Measures Spreadsheet Instructions
OMB: 0920-0853
NACP Year 2 (16-1606) and Year 4 (14-1404)
Combined instructions for completing the templates for the phase I, II, and III performance measures: Updated September 25, 2018
(Important changes or clarifications from previous instructions are highlighted in yellow throughout this set of instructions)
General: These instructions augment the information in the performance measure profiles. Performance measures are not expected to reflect all activities and accomplishments of the grantees. Grantees are encouraged to develop additional state-specific performance measures as needed and to provide additional detail in the narrative part of their annual report. Please submit performance measure spreadsheets and maps to your assigned project officer and to [email protected].
All measures request the state abbreviation in column A and the funding year in column B and have a column for comments. The term “Funding Year” appearing in the reporting spreadsheets refers to the following periods of data collection:
Funding Years for 14-1404 Grantees
Funding Year 1 - 1404 |
Funding Year 2 - 1404 |
Funding Year 3 - 1404 |
Funding Year 4 -1404 |
Funding Year 5 - 1404 |
September 1, 2014 to August 31, 2015 |
September 1, 2015 to August 31, 2016 |
September 1, 2016 to August 31, 2017 |
September 1, 2017 to August 31, 2018 |
September 1, 2018 to August 31, 2019 |
Funding Years for 16-1606 Grantees
|
||||
Funding Year 1 - 1606 |
Funding Year 2 - 1606 |
Funding Year 3 - 1606 |
|
|
September 1, 2016 to August 31, 2017 |
September 1, 2017 to August 31, 2018 |
September 1, 2018 to August 31, 2019 |
|
|
Please do not change the formatting of the spreadsheets (i.e. do not merge cells, add columns or erase the pre-populated cells that are indicated with zeros). The following instructions focus on columns and entries that may not be self-evident and may require additional explanation.
Phase I performance measures A, B, E, F, and J
A. Health Care Reform Opportunities
This should be a short list (4-6) of opportunities that the state asthma program (SAP) identified through an inventory of health care reform activities and projects in the state and that it intends to explore during the following year. It is expected that some of these opportunities may not prove productive while others may.
The list of opportunities should be updated annually in a new row (do not change the previous year’s entry) to reflect the status of program activities as of the end of funding year. PLEASE USE THE UPDATED SPREADSHEET DISTRIBUTED SEPTEMBER 2018, WHICH HAS BEEN REVISED TO LIST YEARLY ENTRIES FOR EACH OPPORTUNITY IN SEQUENTIAL ROWS. THERE IS AN INCOMPLETE ENTRY FOR YEAR 4 FOR YOU TO FILL OUT THAT IS HIGHLIGTED IN YELLOW FOR EASY INDENTIFICATION. PLEASE limit ANY NEW OPPORTUNITIES to the 2 or 3 most promising.
Columns C-D: Opportunity related to: Select the type of organization or activity related to the opportunity (e.g., Federally Qualified Health Centers or State Primary Care Association, State Health Department Committees, Medicaid Managed Care Organizations, etc.) in Column C. If the opportunity is related to multiple organizations from the drop down list, please select “Other” in Column C and identify the organizations in Column D (Description of "Other" type of opportunity).
Columns E-L: Anticipated outcome of the Opportunity: Note, there is a checklist provided for individual anticipated outcome(s) of the opportunity. Please check all that apply. Also, please describe “Other” anticipated outcomes in Column L (Description of “Other” anticipated outcomes of the opportunity.
Column M: Brief description of opportunity. If you add a new opportunity please start the entry with “NEW”. Please add “NEW” opportunities at the bottom of the spreadsheet.
Column N: Status: Select the status (i.e., Exploring, Planning, Implementing, Monitoring, or Discontinued) of the opportunity during the funding year. Priorities may change from year to year but the grantees are asked to track the status of the different opportunities over time. Thus, status for many items might be “exploring” or “planning” during year 1 and may be “discontinued,” “implementing,” or “monitoring” in subsequent years.
Column O: Use this to explain if an opportunity has been discontinued, or to provide other comments.
B. High-level meetings
Starting in funding year 4, all Grantees (14-1404 and 16-1606) may choose not to report this as a performance measure. At this point the reporting emphasis in on outcome measures (Phase II and III measures). Information about important meetings can be reported in the Annual Report.
Column C: High-level decision maker(s) at the meeting: When indicating high-level decision maker(s), please include the title (not name) of main high-level decision maker(s). Those considered high-level decision makers are context relevant but must have the ability to influence multiple settings.
Examples of high-level decision makers include:
State health department medical directors and commissioners
Federally Qualified Health Centers (FQHC) network chief operating officer
Clinical director of state primary care association and state hospital association
State Medicaid director
State and national legislators
Head of school nurses association
Column D: Person(s) representing the State Asthma Program (SAP): Similarly, please specify the title (not name) of who represented the SAP at the meeting. Please note, this may also be a higher level state official, such as the chronic disease program manager if they are representing the asthma program.
Columns E-N: Sector(s) represented by the high-level decision makers: Note, there is a checklist provided for the sectors for ease of aggregation. Please check all that apply. If a particular sector is not provided in the options listed in Columns E-L, please select “Other Sector” in Column M and provide a description of the other sector in Column N (Description of “Other” Sector).
Columns O-W: Meeting outcomes: Note, there is a checklist provided for meeting outcome(s). Please check all that apply. For Column T, please describe “Other specific actions identified,” if applicable. If a particular meeting outcome is not provided in the options listed in Columns O-U, please select “Other” in Column V and provide a description of the other meeting outcomes in Column W.
Columns X-AD: Desired outcome(s) of collaboration: Note, there is a checklist provided for desired outcome(s) of the collaboration. Please check all that apply. If a particular desired outcome is not provided in the options listed in Columns X-AB, please select “Other” in Column AC and provide a description of the other desired outcome in Column AD.
Columns AE-AF: Level of proposed outcome: From the dropdown menu in Column AE, select the level of the proposed outcome (i.e., Statewide, County, District, Local, N/A, and Other). If “Other” is selected, please provide a description of “Other” level of proposed outcome in Column AF.
Column AG: Meeting Date: If multiple meetings are conducted with the same high-level decision makers, and have the same meeting outcomes and desired outcome of collaboration, multiple dates can be entered on one line here. Separate dates with a semi-colon (;).
E. Alignment between program activities and burden data
A map is preferred. If a table or chart is used, be sure to include the entire state. Please label maps appropriately: Include an informative title, indicate source and time period for the data, and indicate overlap between program activities and asthma burden. If submitting multiple maps, charts or tables, use a separate line in the reporting spreadsheet for each.
PLEASE UPDATE YOUR MAPS/TABLES TO REFLECT THE STATUS OF PROGRAM ACTIVITIES AS OF THE END OF EACH FUNDING YEAR.
When showing the overlap of areas of need and activities, distinguish currently implemented activities from those in the planning stage. Activities that are carried out and supported independent of the state asthma program may be included but should be identified as such. Please do not include the location of coalition members unless they are actively implementing interventions.
Column C: The actual map, chart, or tool should be submitted to the project officer as well as the [email protected] mailbox. Please indicate if the updated document has already been submitted to the project officer.
Columns D-J: Measure(s) of Asthma Outcome Used: The measure(s) should be based on the asthma burden NOT the asthma program interventions. Please check all that apply. If a particular measure is not provided in the options listed in Columns D-H, please select “Other” in Column I and provide a description of the other measure of asthma outcome used in Column J.
Column L: Rationale for selection of sites for program activities: A brief rationale for selection of sites (or gaps in coverage) should be included.
F. Use of evaluation findings
Performance measure F is an opportunity to document how you have used evaluation findings to make program improvements or arrive at important decisions. To complete measure F, describe the actions taken during the designated reporting period that were based on evaluation findings, regardless of when the evaluation was conducted. Completing this measure requires you to revisit your evaluation action plans or findings, thus ensuring that important information is not overlooked. Some people find it useful to think about this as “backwards” reporting. That is, start with actions taken, not with the evaluation name or design. If no actions have been taken to date as a result of an evaluation, or if an action is planned but not implemented, DO NOT report it here.
Include only those actions or changes that have been implemented and that you believe have had or will have a valuable impact on your program. You may borrow or summarize from your action plan.
Column C: Type of action taken: From the drop down menu, select the action(s) taken. If an evaluation resulted in multiple actions taken, list each action on a separate line. The categories of type of action taken are as follows:
Specific improvements to interventions: Select if the evaluation identified specific changes that were made to enhance the operations of a service or health system intervention.
Sustain intervention: Select if the evaluation confirmed the success of a program, such that it was sustained.
Expand intervention: Select if the evaluation confirmed the success of a program, such that it was expanded to other areas/populations.
Accountability: Select if the evaluation was primarily used to document or justify the program’s investment of resources/funding. An explanation of the entity (ies) needing such information should be described in the Comments section (Column I).
Address policy gap/issues: Select if the evaluation identified areas in need of policy enhancement.
Enhance surveillance systems or reports: Select if the evaluation identified changes to surveillance systems or information products produced and disseminated using surveillance data.
Increase collaboration: Select if the evaluation resulted in changes to coalition operations (e.g., communications) or operating structures (e.g., workgroups, taskforces) that optimized interactive work.
Expand partnerships: Select if the evaluation identified and prompted inclusion of new partners or new areas for partnerships.
Revise program plans: Select if the evaluation prompted revisions to the overall asthma program’s plans (i.e., change priorities, defund interventions).
Change funding: Select if evaluation resulted in reallocation of funds or resources.
Other: Select if the evaluation use does not fit in the above categories. Please describe “Other” type of action taken in the Comments section (Column I).
Column D: Actual programmatic action: Describe all decisions or actions taken that were considered valuable or useful to your program, partners, or stakeholders.
Clearly describe how the evaluation findings contributed to the decision or action.
Include current or completed actions. Note: Do not report anticipated plans or actions (if implementation has not occurred).
To be thorough, revisit recent reports, presentations, or other relevant documents to identify any actions or decisions that may have resulted (directly or indirectly) from the evaluation.
Column E: Recommended programmatic actions based on findings: Clearly describe how the findings logically led to the recommendations or decisions.
Column F: Evaluation finding(s) on which action was taken: Summarize the specific evaluation finding(s) that led to the action(s) taken. Provide enough detail to give context to the “recommendations” described in Column E.
Column G: Main evaluation question(s) that produced findings: Record the main evaluation question(s) addressed by the finding(s) [i.e., the relevant, overarching evaluation question(s), not a specific question(s) on a survey instrument or interview guide].
Column I: Comments: Note that actions may be based on multiple findings or findings from different evaluations (if, an action resulted from multiple recommendations provide additional explanation here).
J. Asthma policies
Add any new policies related to educational or housing agencies that went into effect during the reporting year for which the state asthma program had a clear role. This is defined as “influenced” in the profile (see definition below). Indicate “NEW” in the comments section.
Influenced: Provided data, information, tools, resources, or other assistance
If there has been a change to a policy listed in previous years, update the policy in a new row to reflect the status at the end of the funding year. Indicate “UPDATE” in the comments section. Do not change the previous year’s entry.
Policies not related to educational or housing agencies should not be reported here, but can be reported in state-specific performance measures or in the narrative section of the annual report.
There are drop down menus for:
Column C: Education or housing agency
Column D: Focus of policy (e.g., smoking/tobacco related, increasing access to asthma meds in school, improving knowledge/skills/awareness [KSA] among staff/students/parents, improving indoor or outdoor air quality, etc.). See the table below for the type of policies falling under each category. The table was revised in funding year 2 for 14-1404 Grantees to more clearly define the types of policies falling under each category and is currently applicable to both 14-1404 and 16-1606 Grantees. If a particular policy focus is not provided in the options, please select “Other” and provide a description of the other focus of policy in Column E.
The revised spreadsheet includes “smoking/tobacco” as a separate category.
Column G: Level of policy (i.e., Statewide, County, District, Local, N/A, and Other): If a particular policy level is not provided in the options, please select “Other” and provide a description of the level of policy in Column H.
Column F: Group(s) affected by the policy: Groups might include age groups, schools grades, type of residents (in multiunit housing), etc.
Column I: Name of agency adopting the policy: Consolidate similar policies implemented in different locations to the extent possible by the focus of policy (e.g., smoke-free policies in multi-unit housing). For example, under “Name of agency adopting the policy,” list something like “12 housing districts – list available upon request.”
Column J: Policy name: give the official name if available
Column K: Template or language available to share: Indicate whether there is a template or language of the policy available for sharing. If yes, the link can be included in the comments column (W)
Column L: Brief narrative description of policy for example “Landlord must notify tenant when applying pesticides in rental housing unit” or “Smoking is prohibited in all child day care centers and licensed group day care homes.”
Column M: Policy effective date (enter month/year or only year)
Columns N-S: Role of SAP in influencing agency: Note, there is a checklist provided for the role of the SAP in influencing the agency. Please check all that apply. If a particular role is not provided in the options listed in Columns N-Q, please select “Other” in Column R and provide a description of the other role of the SAP in Column S.
Columns T-V: Status
Column T: Indicate the policy’s status (i.e., In development, Passed or adopted only, Implemented, or Discontinued).
Column U: If the policy was implemented, provide a brief description of the implementation.
Column V: Indicate whether the policy was evaluated. If evaluated, provide a brief description of the evaluation in the Comments section (Column W).
-
Sample Policies and How They Can be Categorized
Note the type of policies in many of the categories has been revised
Category of Policy
Type of policies in this category
1. Improve access to asthma/ allergy medication in school
• Physician's written instructions for medication on file
• Students' rights to self-carry/self-administer asthma/anaphylaxis medication
• Medication policies that provide resources, guidelines, and parameters
2. Improve documentation of student asthma/allergy information in schools
•Identify and maintain records for students with chronic conditions
• Update health records regularly
• Maintain asthma/allergy incident reports
• Maintain a health history form for each student
• Identify/track all students with asthma diagnosis
3. Improve asthma management plans in schools
• Standard emergency protocols for asthma/anaphylaxis
• Explicit asthma/anaphylaxis management programs with policies, procedures, and resources
• Use of an asthma action plan for all students with asthma
4. Increase health services capacity in schools
• Nurse-to-student ratio
• Nurse coverage at schools
• Case management for students with chronic conditions
5. Improve awareness/knowledge among school staff
• Asthma education for school personnel, including emergency response
• State funding for staff training on asthma/allergy programs, policies, and procedures
• Inclusion of asthma/allergy in the health curriculum for all students
6. Improve awareness/knowledge among community members
• Asthma education for community members, including emergency response
• State funding for community members’ training on asthma/allergy programs, policies, and procedures
7. Improve awareness/knowledge among people/students with asthma/parents
• Policies to include asthma education during home visits conducted by other programs
• Asthma education for students, including self-management
8. Improve indoor air quality (excluding smoking/tobacco)
• IAQ management policies (including HVAC; HEPA filters; carpeting; pesticide use; dampness; mold; maintenance and repairs, and cleaning)
• State funding/resources for technical IAQ assistance
• Use of integrated pest management (IPM) techniques/banning of pesticides inside schools when students are present
• Integrated pest management in multi-unit housing
9. Improve outdoor air quality (excluding smoking/tobacco)
• Notification of students with asthma, parents, etc. of upcoming pesticide applications
• Limiting bus idling time; implementing/promoting diesel school bus engine retrofitting program
10. No smoking policy
• No smoking policies in multi-unit housing
• Prohibition of smoking/tobacco in school buildings, buses, and school-related functions and on school grounds
• Tobacco use cessation services
• Health education curriculum includes tobacco use prevention component
11. Other
Table adapted from: Lynn, Oppenheimer, and Zimmer Using public policy to improve outcomes for asthmatic children in schools.
Phase II performance measures C, G, H, I, K, L, N, and R
C. School Enrollment Covered by Formal Agreements
Column C: Name or Brief Description of Formal Agreement: We anticipate responses, such as:
MOU to train school nurses in teaching asthma self-management education
Letter of agreement to refer students without a provider to a partnering FQHC
MOA to provide training for coaches and other school personnel
If the SAP has multiple types of agreements with different schools or districts, list each agreement on a separate row.
If the SAP has the same agreement with multiple schools or districts, please indicate the number of entities involved but DO NOT list each entity here (see example below).
Example: Same agreement with 36 schools – list available upon request
Columns D-J: Topic of Formal Agreement: Note, there is a checklist provided for topic(s) of the formal agreement. Please check all that apply. If a particular topic is not provided in the options listed in Columns D-H, please select “Other” in Column I and provide a description of the other topic of formal agreement in Column J.
Columns K-L: Level of agreement: From the dropdown menu, indicate the level of agreement (i.e., School(s), School District(s), Statewide, or Other). If a particular level is not provided in the options, please select “Other” in Column K and provide a description of the other level of agreement in Column L.
Column M: School/District/Other Entity Name: Again, if the SAP has the same agreement with multiple schools or districts, please indicate the number of entities involved but DO NOT list each entity here (see example above for Column C).
Column O: Total enrollment of students covered by the agreement: This enrollment refers to all enrolled students covered by the agreement, not just students with asthma. If the agreement is with a school-based health center, include all the schools served by that health center when calculating total enrollment.
Column R: Provide a brief description of the racial/ethnic characteristics of the student population if this information is available
Column S: Percent of students receiving free or reduced school lunches: If available, indicate the percentage of students (NOT the number of students) receiving free or reduced school lunches.
Column T: Percent of students with asthma in participating schools: If available, indicate the percent of students (NOT the number of students) with asthma in participating schools.
G. Self-management Education
Please note that performance measures (PMs) G, H, I, K, L, and R are linked together as indicated in the diagram below. EVERY ENTRY IN MEASURE G SHOULD BE CARRIED ACROSS PMS H, I K L AND R even if the information for that particular measure is not unavailable at the time of reporting.
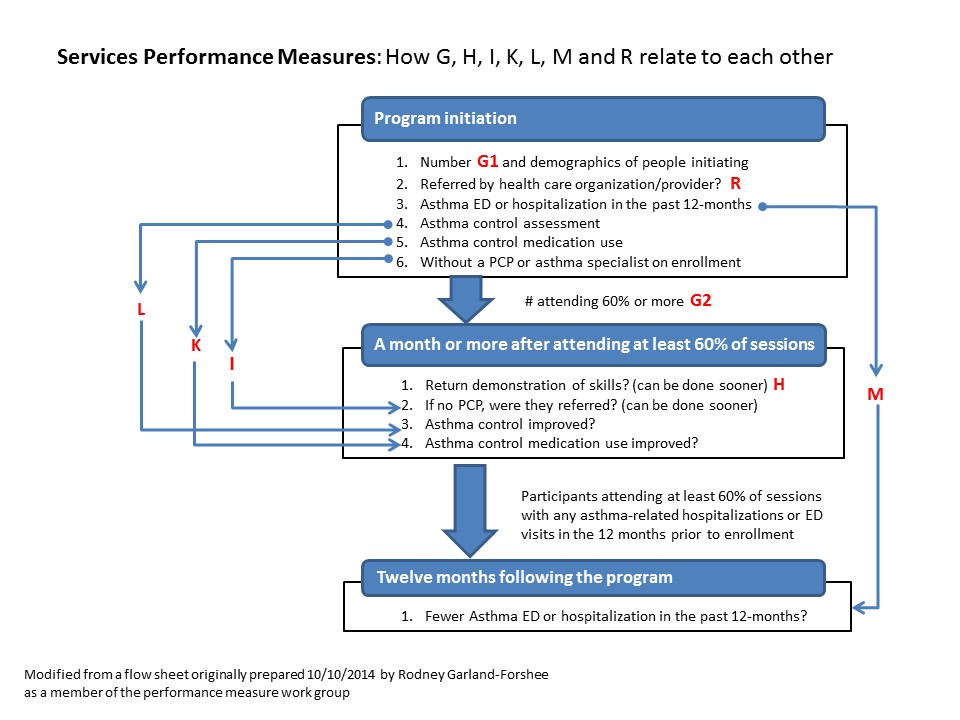
To facilitate your reporting, some information for measures H, I, K, L, and R is pre-populated from measure G. In those cases, columns containing “0” indicate that information will be automatically copied from the previous spreadsheet so PLEASE DO NOT DELETE THE PRE-POPULATED FIELDS AS THIS WILL ALSO DELETE THE FORMATTING. Thus, the responses entered for “Partner delivering intensive asthma self-management education” (Column C) and “SME curriculum name” (Column D) should be identical on PMs G, H, I, K, L, and R. Similarly, the entries for “Number of participants initiating intensive asthma SME,” “Number of participants attending at least 60% of sessions,” and “Number of participants attending 100% of sessions” should be identical across all of these PMs.
Please use the legend below to specify information that is unavailable, not applicable, or “0”:
Unavailable information: Enter “Unavailable” in the respective column(s) and state the reason in the Comments section for each measure
Not applicable: Enter “N/A” in the respective column(s)
0 (zero): Enter “0” only as numerical value, not for missing/unavailable, or not applicable information.
Only interventions that meet the definition of intensive self-management education as stated in the profile for measure G should be included here.
“Intensive asthma-self management education: Includes the key educational messages listed in the NAEPP guidelines (Section 3, Component 2 page 124) and a return demonstration of basic asthma knowledge and skills, and is tailored as much as possible to an individual’s underlying knowledge and beliefs about asthma; it must include two or more in-person sessions. Interactive sessions held by video conference are acceptable.”
For example, interventions that consist of only one session or do not include a return demonstration of basic asthma knowledge and skills (for each participant) should not be reported here but can be reported in state-specific performance measures. We are providing a template for reporting a state-specific measure for asthma self-management education that does meet the definition of “intensive:”
As defined in the Phase II profiles, a participant is a person with asthma. For measures G and H, a caregiver can be counted as a proxy for the person with asthma. A caregiver is a person who is the parent, guardian, or other person responsible for the care of, and who acts as a proxy for, a person with asthma who is unable (because of young age or other condition) to take responsibility for his/her own asthma self-management. If BOTH a person with asthma and a caregiver are trained, this counts as one participant for reporting purposes.
Column C: Partner delivering intensive asthma self-management education:
If the same intensive asthma self-management education curriculum is delivered by multiple partners, list each partner in a separate row.
If the same partner delivers multiple intensive asthma self-management education curricula, list each curriculum and partner in a separate row.
Column D: SME curriculum name: List the name of the SME curriculum used, not the program. For example the “All Good Hospital Asthma Control Program” may have its own asthma program but uses the “You Can Control Asthma Curriculum” to teach about asthma. In that case, please enter “You Can Control Asthma” here.
Column E: Curriculum setting: From the dropdown menu, select the primary curriculum setting (i.e., Home, School, Community, Healthcare setting, or Other). If the curriculum was conducted in multiple settings, select “Other” and provide a description of the other setting in Column F.
Column G: Number of sessions: Note, intensive asthma self-management education should have a minimum of 2 sessions. If only one session was conducted, do not report this information here. It should be reported in the state-specific performance measure.
Column H: Type of instructors: From the dropdown menu, select the type of instructors delivering instruction (i.e., AE-C, CHW, Nurse, Respiratory Therapist, or Other). If multiple instructors were utilized, select “Other” and provide a description of the other setting in Column I.
Column J: Does the SAP provide funding (Y/N)
Column K: Contributions of the SAP other than funding: Examples of contributions of the SAP include, evaluation incentives or assistance, curriculum materials, personnel time, etc.
Column L: Test used to measure asthma control: From the dropdown menu, select the asthma control test used:
ACT: Asthma Control Test
cACT: Childhood Asthma Control Test
ATAQ: Asthma Therapy Assessment Questionnaire
ACQ: Asthma Control Questionnaire
TRACK: Test for Respiratory and Asthma Control in Kids
ITG Child Asthma: Integrated Therapeutics Group Child Asthma Short Form
Other (if another test was used, specify the other test of asthma control in Column M)
Column N: Number of participants initiating intensive asthma SME: Indicate the total number of participants who started intensive asthma SME, even if they did not complete all of the sessions. This number will be carried forward (pre-populated to the other sheets) where appropriate
NOTE: Because the timing of the interventions may have overlapped the reporting periods (e.g. the participant initiated intensive AS-ME in June of 2017 and completed the session in November 2017), the information reported at the end of October 2017 may have been incomplete. Please update the currently available information for participants initiating AS-ME in Year 3 PUTTING ANY CHANGES (UPDATED OR CORRECTED INFORMATION) IN RED FONT.
Column O: Number of participants attending at least 60% of sessions: This includes the number of participants attending 100% of sessions. This number will also be carried forward
Column P: Number of participants attending 100% of sessions: If reported (This number is optional), the number should be a subset of Column O. That is, of the number of participants attending AT LEAST 60% of sessions, how many attended all sessions? For example, if 100 participants enrolled in a 3-session course and 20 attended 1 session, 50 attended only 2 sessions, and 30 attended all three sessions, enter 80 in Column O and 30 in column P.
Columns Q-U: Age of participants (person with asthma) upon enrollment:
Column V: Provide a brief description of the racial/ethnic characteristics of the participants if available
Columns W-X: Asthma control status on enrollment:
Column W: Indicate the number of participants with well-controlled asthma (i.e., having scores on a validated, age-appropriate asthma control questionnaire that fall inside the well-controlled range).
Column X: Indicate the number of participants with poorly-controlled asthma (i.e., having scores on a validated, age-appropriate asthma control questionnaire that fall outside the well-controlled range, in either the “not well controlled” or “very poorly controlled” range).
Column Y: Number of participants (upon enrollment) with any hospitalizations OR ED visits for asthma in the 12 months prior to enrollment. Enter the number of participants, not the number of hospitalizations or ED visits.
H. Demonstration of basic asthma self-management knowledge and skills
Column C: Partner delivering intensive asthma self-management education: This information should be identical to the response provided for PM G Column C.
Column D: SME curriculum name: This information should be identical to the response provided for PM G Column D.
Column E: Number of participants initiating intensive asthma SME: This information should be identical to the response provided for PM G Column N.
Column F: Number of participants attending at least 60% of sessions: This information should be identical to the response provided for PM G Column O.
Column G: Number of participants attending 100% of sessions: This information should be identical to the response provided for PM G Column P.
Column H: Number of participants attending at least 60% of sessions who successfully demonstrate basic knowledge and skills: This number should be a subset of Column F.
Column I: Number of participants attending 100% of sessions who successfully demonstrate basic knowledge and skills: This number should be a subset of Column G.
Column J: Knowledge and skills test/instrument submitted to project officer (Y/N)
Column K: It would be helpful if you would include a description of the knowledge and skills test/instrument that is used in the Comments section.
I. Referral to a primary care or specialty care provider
Participants receiving care for asthma from a primary or specialty care provider (allergist or pulmonologist) at the time of enrollment should not be included in this measure.
Column C: Partner delivering intensive asthma self-management education: This information should be identical to the response provided for PM G Column C.
Column D: SME curriculum name: This information should be identical to the response provided for PM G Column D.
Column E: Number of participants initiating intensive asthma SME: This information should be identical to the response provided for PM G Column N.
Column F: Number of participants attending at least 60% of sessions: This information should be identical to the response provided for PM G Column O.
Column G: Number attending at least 60% of sessions who are without a PCP at enrollment: This information should be a subset of Column F. If this number is 0, enter “0” and proceed to PM K or L.
Column H: Number attending at least 60% of sessions, without a PCP at enrollment, and are provided a referral: This information should be a subset of Column G.
Column I: Number attending at least 60% of sessions, without PCP at enrollment and referred to and access care for asthma: This information should be a subset of Column H.
Column J: Brief description of referral process to PCP or specialty care: Examples include:
Participant is provided a generic list of local providers
Recommendations are customized to participants’ coverage, preference, and geographic area
Appointment scheduled
Column K: Brief description of the mechanism of tracking access to care (For example: follow-up visits or phone calls to participants, providers confirm that the participants was seen, etc.)
Column L-M: Type of provider to which participants are referred: If participants are referred to multiple types of providers, select “Other” in Column L and provide a “Description of ‘Other’ type of provider” in Column M.
K. Use of long-term control medication
Starting in funding year 4, all Grantees (14-1404 and 16-1606) may choose not to report this as a performance measure – it is “optional”.
Column C: Partner delivering intensive asthma self-management education: This information should be identical to the response provided for PM G Column C.
Column D: SME curriculum name: This information should be identical to the response provided for PM G Column D.
Column E: Number of participants attending at least 60% of sessions who had poorly controlled asthma on enrollment: This should be a subset of the response provided for PM G Column O.
Column F (optional): Number of participants attending 100% of sessions who had poorly controlled asthma on enrollment: This should be a subset of the response provided for PM G Column P.
Column G: Number of participants attending at least 60% of sessions who, on enrollment, had poorly controlled asthma and were using long-term control medication less than 7 days per week: This should be a subset of the number provided in column E. If information on medication use is unavailable for some participants, indicate in the Comments section (Column K) that this information is unavailable and specify the number of participants for which these data are missing.
Column H: (optional) Number of participants attending 100% of sessions who, on enrollment, had poorly controlled asthma and were using long-term control medication less than 7 days per week. This should be a subset of the number reported in column F
Column I: Number of participants attending at least 60% of sessions who had poorly controlled asthma on enrollment who self-report better adherence. This should be a subset of the number reported in column G
Column J: (optional) Number of participants attending 100% of sessions who had poorly controlled asthma on enrollment who self-report better adherence. This should be a subset of the number reported in column H
L. Improved asthma control
Column C: Partner delivering intensive asthma self-management education: This information should be identical to the response provided for PM G Column C.
Column D: SME curriculum name: This information should be identical to the response provided for PM G Column D.
Column E: Number of participants attending at least 60% of sessions who had poorly controlled asthma on enrollment: This should be identical to the response provided for PM K Column E.
Column F: (optional) Number of participants attending 100% of sessions who had poorly controlled asthma on enrollment: This should be identical to the response provided for PM K Column F.
Column G: Number of participants with poorly controlled asthma on enrollment who reported well-controlled asthma one month or more after attending at least 60% of sessions: This should be a subset of the number reported in column E, If information on change in asthma control is not available for some participants, indicate in the Comments section (Column I), and specify the number of participants for which these data are missing.
Column H: (optional) Number of participants with poorly controlled asthma on enrollment who reported well-controlled asthma one month or more after attending 100% of sessions. If reported, This should be a subset of the number reported in column F
Column I: Comments. If you have information on the number of participants who reported decreased or no change in their asthma control. Please report here.
N. Quality Improvement (QI) Processes in HC organizations
Include here only health care organizations that have implemented or are currently in the process of implementing QI programs, not those that are considering or in discussion.
A number of important activities (such as, training health care providers or developing EHRs outside of a QI process) meet the requirement of Health Systems Strategy I: Quality Improvement but do not fit under this measure. Please report in the annual report.
We are using the HSRA definition and key principles of quality improvement process which includes ongoing cycle or trial and measurement to achieve improvements: “While each QI program may appear different, a successful program always incorporates the following four key principles:
QI work as systems and processes
Focus on patients
Focus on being part of the team
Focus on use of the data
Columns C-D: Type of HCO: From the dropdown menu, select the type of HCO (i.e., FQHCs, Private practice, ACOs, or Other). If “Other” is selected, describe the other HCO in Column D.
Column E: Brief description of population served by the HCO: This may include, for example, percent Medicaid, percent employer-based coverage, percent health exchange, etc.
Column F: Name/description of QI process (for example ALA’s Enhancing Care for Children with Asthma or the Institute for Healthcare Improvement’s Model for Improvement. If not using a standard QI program briefly describe the process used.
Column G: Asthma-related quality of care (QOC) measures collected: These refers to process measures, such as whether severity and control were documented, whether an AAP or flu shot was provided, whether inhaled corticosteroids were prescribed, and whether asthma education was documented.
Columns H-M: Health outcomes collected: Note, there is a checklist provided for the outcomes. Please check all that apply. These refer to patient level outcomes. For example, was asthma control improved? Were hospitalizations and ED visits reduced? Was satisfaction or quality of care increased? IF THE OUTCOME MEASURED WAS DOCUMENTATION OF ASTHMA CONTROL IN THE CHART OR EHR, THAT SHOULD BE ENTERED IN COLUMN G. IF IT IS CHANGE IN THE PATIENT’S ACTUAL CONTROL STATUS IT SHOULD BE IN COLUMN H. If a particular outcome is not provided in the options listed in Columns H-K, please select “Other” in Column L and provide a description of the other outcome in Column M.
Columns N-O: Role of SAP in influencing organization: From the dropdown menu, select the role of the SAP in influencing organization (i.e., Provided sample QI process, Provided comments or plans or results, Funding to assist with development of QI process, Other). If a particular role is not provided in the options listed, please select “Other” in Column N and provide a description of the other role of the SAP in Column O.
R. Referrals from HC organizations
Starting in funding year 4, all Grantees (14-1404 and 16-1606) may choose not to report this as a performance measure.
Information for this measure should be collected on the intake sheet unless there is a sole source of referrals.
Column C: Partner delivering intensive asthma self-management education: This information should be identical to the response provided for PM G Column C.
Column D: SME curriculum name: This information should be identical to the response provided for PM G Column D.
Column E: Number of participants initiating intensive asthma SME: This information should be identical to the response provided for PM G Column N.
Column F: Number of participants referred from HCOs or providers:
If all participants are referred directly from a HCO or the intervention is delivered by a HCO or provider, the number in Column F should equal the number in Column E.
If referral sources are mixed, the number in Column F will probably be less than the number in Column E. Column F is a subset of Column E. That is, of the total number of participants initiating intensive asthma SME (Column E), how many of those participants were referred from HCO or providers (Column F)? The number in Column F should be either the same or less than the number in Column E.
In most school-based programs, the referrals are internal (i.e., teachers, parents, or school nurses). In these cases, the acceptable number in Column F would likely be 0 (zero).
Phase III performance measures M, O, P, Q, and S
Note: Information from the phase II spreadsheets is not transferred to these spreadsheets (not pre-populated)
M. Reduction in hospitalizations and ED visits
This is a supplemental measure and is encouraged but not required.
For this measure, we are asking how many participants had a decrease in the combined total of hospitalizations and ED visits. You may also report changes in hospitalizations (Column K) and changes in ED visits (Column L) separately. Include in this measure anyone for whom 12-month follow up was collected in the funding year. If your reporting period was other than 12 months, please explain in column O
Column B: Indicate the funding year during which the 12-month follow-up was completed which will likely be the reporting year.
Column C: List the partner (or partners) delivering intensive asthma self-management education.
If the same intensive asthma self-management education curriculum is delivered by multiple partners, list each partner in a separate row.
If the same partner delivers multiple intensive asthma self-management education curricula, list each curriculum and partner in a separate row.
Column E: Enter the number of participants attending at least 60% of sessions. This number should be the same as the number reported in Column O in the spreadsheet for performance measure G.
Column F: Number of participants attending at least 60% of sessions with any asthma-related hospitalizations or ED visits in the 12 months prior to enrollment. Because it only includes participants who attended at least 60% of sessions, this number should be a subset of (equal to or less than) the number in column Y of the spreadsheet for performance measure G
Column G: Indicate the “Number of participants attending at least 60% of sessions with any asthma-related hospitalizations or ED visits in the 12 months prior to enrollment for whom 12 month follow up is available.” This should be a subset of (equal to or less than) the number in column F
Columns H- L: These columns refer only to participants for whom 12-month follow-up is available unless otherwise explained in column O.
Column H: Indicate the “Number of participants attending at least 60% of sessions who had any asthma-related hospitalizations or ED visits in the 12 months prior to enrollment who report a reduction in these events 12 months following the program. “
Columns I and J are for the number having no change or an increase in these events respectively
Column K: If available, indicate the “Number attending at least 60% of sessions who had any asthma-related hospitalizations in the 12 months prior to enrollment who report a reduction in hospitalizations 12 months after the program.”
Note: This column refers to a reduction in hospitalizations only.
Column L: If available, indicate the “Number attending at least 60% of sessions who had any asthma-related ED visits in the 12 months prior to enrollment who report a reduction in ED visits 12 months after the program” here.
Note: This column refers to a reduction in ED visits only.
Column M: Select from the drop down menu to indicate the source of information
Column O: Comments. If your reporting period was other than 12 months, please explain here.
Measures O, P, Q, and S (together with measures N and R reported in Phase II) correspond to the Health Systems Strategies. Programs funded through 14-1404 and 16-1606 must implement at least two of the health system strategies during the first two years of funding and are encouraged to implement at least three by the end of the funding cycle. Reporting of PMs O and Q are now optional, but activities related to advancing team-based care and institutionalization of referral systems should be included in the annual report.
O. Team-based approach in health care organizations
Starting in funding year 4, all Grantees (14-1404 and 16-1606) may choose not to report this as a performance measure – it is “optional”.
For this measure, only include health care organizations that have implemented or improved team-based care during this FOA and for which the state asthma program provided data, information, tools, resources, or assistance that were critical to the partner taking action (i.e., the action would likely not have occurred absent state support). Do not include team-based care that is in the planning or development phase.
Column C: Select the type of HCO from the drop-down menu. If not listed select “other” and describe in column D
Column E: List the name of the HCO.
Column F: Provide a brief description of the population served by the HCO.
This can include racial/ethnic characteristics, percent of population covered by Medicaid, etc.
Column G: Describe the composition of teams and roles of team members.
Physician, RN, pharmacist, CHW, and care coordinator are examples of the composition of teams. Examples of the role of each team member may include diagnose and treat, provide self-management education, assess asthma control, coordinate care, conduct home visit, etc.
Column H: Describe the method of sharing information among team members.
For example, regular meetings, documentation in charts, faxed reports, telephone conversations, dedicated electronic platform, etc.
Column I: Describe the role of state asthma program in influencing the organization.
This could include providing data, information, tools, resources, or assistance that were critical to the partner taking action. If the state had no influence in the decision to implement a team-based approach, do not include in this measure.
Column J: If available, describe the measures taken by the HCO to ensure cultural appropriateness of care.
We were asked for clarification about how we define “team-based care” and offer the following:
What is your definition of “team-based care?”
Provision of comprehensive asthma control services (CACS) by multiple providers who have defined roles and work collaboratively with individuals and families.
What’s the scope of the “team” (to be considered team-based)?
We have been very broad in the scope of the team. It is NOT just about the standard assignment of traditional tasks (the medical assistant takes vital signs and documents meds) but about information sharing and collaboration around individual patients or families. A team may be internal to a practice (MA identified patients with asthma and assure patient flow; nurse or educator teaches asthma education, confirms appropriate inhaler technique, and comprehension of the AAP, and communicates that back to the PCP; front desk tracks referrals and follow-up or it can involve individuals external to the practice (home visitor or pharmacist).
How many different professional groups need to be included?
At a minimum 2, usually more. However, the key point is not number, but coordination and collaboration.
Does it need to be independently coordinated (from the asthma program)?
No. There are a number of ways the asthma program can encourage practices and health systems to develop team-based care, including providing “data, information, tools, resources or assistance that were critical to the partner taking action (i.e., the action would likely not have occurred absent state support).”
Should we include QI processes and home visiting programs as “team-based care”?
If the QI process promoted or funded by the state asthma program leads to the adoption of team-based care by the health care organizations, it can be reported here, as well as in measure N. If a health care practice or organization begins working collaboratively with home visitors around individual patients and families (not just a one-way referral) that can also be reported here.
P. Plans reimburse for AS-ME and home visits
For this measure, only include health plans that have begun covering or reimbursing for intensive asthma-self management education and/or home visits during this cooperative agreement.
Column C: List the name of the health plan.
Column D: Select the type of plan from the drop-down menu.
Column F: Indicate the services covered or reimbursed by selecting from the drop-down menu.
Column G: Provide a detailed description of the services and who provides them.
For example, curriculum used, type of provider, number of visits, supplies, and materials provided, etc.
Column H-I: Indicate eligibility for services in Column H by selecting from the drop-down menu.
If multiple eligibility criteria are used, select the “Other” option in Column H and describe the eligibility criteria in Column I.
Column J: If services are contracted, indicate the amount of reimbursement.
This can include a dollar amount or percent reimbursement.
Column K: Describe the role of state asthma program in influencing the health plan.
This could include providing data, information, tools, resources or assistance that were critical to the partner taking action. If the state had no influence in the decision to cover or reimburse, do not include in this measure.
Column L: Please include links to publications, waiver language or other resources related to the reimbursement policy or decision
Q. HC organizations implement or improve referral systems
Starting in funding year 4, all Grantees (14-1404 and 16-1606) may choose not to report this as a performance measure – it is “optional”.
For this measure, only include health care organizations that have implemented or improved referral systems to home, schools, or community asthma services during this cooperative agreement and for which the state asthma program provided data, information, tools, resources or assistance that were critical to the partner taking action (i.e., the action would likely not have occurred absent state support). Do NOT include referral systems that are in the planning or development phase. Do NOT include one-time activities (as part of a project or study, but systems that have been institutionalized and are sustained.
Column C: Select the type of HCO from the drop-down menu.
Column E: List the name of the HCO.
Column F: Describe the referral process and services.
Examples of the referral process can include dedicated electronic platform, automatic scheduling, care coordinator, etc.
Referral services can include intensive asthma self-management education, home-based trigger reduction services, or both.
Column G: If available, describe the process for assessing the timeliness and completion of referrals.
Column H: Provide a brief description of population served by the HCO.
This can include racial/ethnic characteristics, percent of population covered by Medicaid, etc.
Column I: Describe the role of state asthma program in influencing the organization.
This could include providing data, information, tools, resources or assistance that were critical to the partner taking action. If the state had no influence in the decision to implement or improve the referral system, do not include in this measure.
S. Partnering health care organizations and health plans implementing comprehensive asthma control services and sharing information on health care utilization
This is a supplemental measure and is encouraged but not required.
For this measure please include all health care organizations or plans that implement step-wise comprehensive asthma control services, and share outcome and utilization data during the current FOA cycle with you, EVEN IF THE STATE ASTHMA PROGRAM HAD NO DIRECT INFLUENCE. This differs from measure M in that the outcome and utilization data should be at the PLAN or POPULATION level and not at the level of individuals enrolled in specific interventions or components of comprehensive asthma control services.
Column C: Select the type of HCO or health plan from the drop-down menu.
Column E: List the name of the HCO or health plan.
Column F: Describe the comprehensive asthma control services (CACS) provided (e.g., care coordination or intensive asthma self-management education by an AE-C or nurse, home visits by CHWs, etc.).
Column G: Indicate if state asthma program had some influence on the HCO's or health plan's approach to asthma care by selecting from the drop-down menu.
Column H: If “yes” is indicated in Column G, describe state asthma program's influence on the HCO's or health plan's approach to asthma care here.
For example, this could include providing data, information, tools, resources or assistance that were critical to the partner taking action.
Column I: Describe the actual changes in asthma-related hospitalizations and/or ED visits reported. Include all results, whether showing decrease, increase, or no change.
Column J: Describe other outcomes (if any) tracked by HCOs or health plans that are implementing CACS.
For example, asthma control, school absenteeism, medication adherence, etc.
Column K: Comments. Indicate here if there are reports or publications related to this.
September 25, 2018
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| File Modified | 0000-00-00 |
| File Created | 0000-00-00 |
© 2026 OMB.report | Privacy Policy