Crosswalk
Appendix_B_CY 2021 PBP 30-day List of Changes.docx
The Plan Benefit Package (PBP) and Formulary Submission for Advantage (MA) Plans and Prescription Drug Plans (PDPs) (CMS-R-262)
Crosswalk
OMB: 0938-0763
CY
2021 PBP, Formulary, and MTMP List of Changes
CY 2021 PBP Changes
Landing Page
The PBP software landing page will be updated to reflect the CY2021 year change. SOURCE: Internal
PBP SCREEN/CATEGORY: Landing Screen
DOCUMENT: Appendix_C_PBP2021_Screenshots-SectionA-Upload-2019-12-09.pdf PAGE(S): Page 9
CITATION: 42 CFR 422.256
REASON WHY CHANGE IS NEEDED: To update the year references throughout the software. IMPACT ON BURDEN: No impact
Section B
The PBP software will be updated to change service category name B4a from “Emergency Care/Post- Stabilization Care Services” to “Emergency/Post-Stabilization Services.”
SOURCE: CMS Policy
PBP SCREEN/CATEGORY: Section B4a: Emergency/Post-Stabilization Services DOCUMENT: Appendix_C_PBP2021_Screenshots-SectionB-2019-12-09.pdf PAGE(S): Pages 52 and 53
CITATION: 42 CFR 422.256
REASON WHY CHANGE IS NEEDED: To remove the word “care” as it is no longer applicable to the benefit.
IMPACT ON BURDEN: No Impact
The PBP software will be updated to change service category name B7k from “Opioid Treatment Services” to "Opioid Treatment Program Services.”
SOURCE: CMS Policy
PBP SCREEN/CATEGORY: Section B7k: Opioid Treatment Program Services DOCUMENT: Appendix_C_PBP2021_Screenshots-SectionB-2019-12-09.pdf PAGE(S): Pages 95 and 96
CITATION: 42 CFR 422.256
REASON WHY CHANGE IS NEEDED: To more accurately represent the benefit to plans and beneficiaries. IMPACT ON BURDEN: No Impact
The PBP software will be updated to change the benefit name for B14c from “Bathroom Safety Devices” to "Home and Bathroom Safety Devices and Modifications."
SOURCE: CMS Policy
PBP SCREEN/CATEGORY: Section B14c: Other Defined Supplemental Benefits DOCUMENT: Appendix_C_PBP2021_Screenshots-SectionB-2019-12-09.pdf PAGE(S): Pages 188-201
CITATION: 42 CFR 422.256
REASON WHY CHANGE IS NEEDED: To more accurately represent the range of items plans are offering for this supplemental benefit.
IMPACT ON BURDEN: No Impact
The PBP software will be updated to add a question to specify “type of Fitness Benefit offered” underneath “type of benefit” for Fitness Benefit” in Section 14c “Other Defined Supplemental Benefits."
SOURCE: CMS Policy
PBP SCREEN/CATEGORY: Section B14c: Other Defined Supplemental Benefits DOCUMENT: Appendix_C_PBP2021_Screenshots-SectionB-2019-12-09.pdf PAGE(S): Page 188
CITATION: 42 CFR 422.256
REASON WHY CHANGE IS NEEDED: To more precisely capture the type of fitness benefit offered. IMPACT ON BURDEN: Low Impact
The PBP software will be updated to add “Radiation drugs” to “B15 Medicare Part B Chemotherapy drugs”
SOURCE: CMS Policy
PBP SCREEN/CATEGORY: Section B15: Medicare Part B Rx Drugs DOCUMENT: Appendix_C_PBP2021_Screenshots-SectionB-2019-12-09.pdf PAGE(S): Pages 210 and 211
CITATION: 42 CFR 422.256
REASON WHY CHANGE IS NEEDED: To add a new type of benefit to the existing Medicare Part B chemotherapy drugs category
IMPACT ON BURDEN: Low Impact
The PBP software will be updated to add “Radiation drugs” to “B20 Outpatient Drugs” SOURCE: CMS Policy
PBP SCREEN/CATEGORY: Section B20: Outpatient Drugs
DOCUMENT: Appendix_C_PBP2021_Screenshots-SectionB-2019-12-09.pdf PAGE(S): Pages 245 and 246
CITATION: 42 CFR 422.256
REASON WHY CHANGE IS NEEDED: To add a new type of benefit to the existing Medicare Part B chemotherapy drugs category
IMPACT ON BURDEN: Low Impact
The PBP software will be updated 19b/13i name change from "Transitional/Temporary Supports" name to "General Supports for Living.”
SOURCE: CMS Policy
PBP SCREEN/CATEGORY: Section B19/13i VBID/UF/SSBCI 19B #13i Non-Primarily Health Related Benefits for the Chronically III-Type
DOCUMENT: Appendix_C_PBP2021_Screenshots-SectionB-VBID-UF-SSBCI-2019-12-09.pdf PAGE(S): Page 126-128
CITATION: 42 CFR 422.256
REASON WHY CHANGE IS NEEDED: To expand on the benefit for increased flexibility. IMPACT ON BURDEN: No Impact
9. The PBP software will be updated to include new Part C Rewards and Incentives screens for plans to consolidate mandatory or optional supplemental services by offering them at a reduced cost through debit card and other sources.
SOURCE: CMS Policy
PBP SCREEN/CATEGORY: Section B19 VBID Part C Rewards and Incentives
DOCUMENT: Appendix_C_PBP2021_Screenshots-SectionB-VBID-UF-SSBCI-2019-12-09.pdf
PAGE(S): Page 3-5
CITATION: 42 CFR 422.256
REASON WHY CHANGE IS NEEDED: To allow plans to offer Part C Rewards and Incentives.
IMPACT ON BURDEN: Low impact
Screenshot:
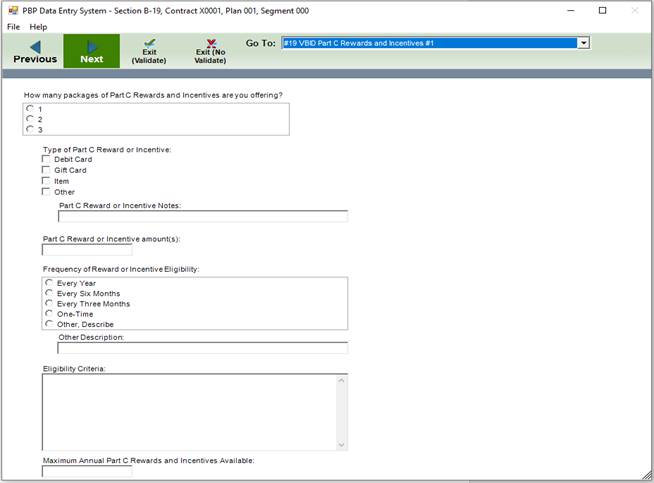
Additional explanation:
The PBP software update includes new screens to offer reduced cost through debit card and other sources in the new Part C Rewards and Incentives screen.
The reason for the Low Impact burden estimate is that there are minimal number of plans that may be affected by the options included with this change and they would have minimal data inputs. The change should not increase the overall burden for the entire industry much if any at all, as it is only a small group that may be using the option included with this change.
The PBP software will be updated to a) separate chronic condition(s) from socioeconomic status on an updated Reduced Cost Sharing Target Population screen b) request information about whether the enrollee needs to have all or combination of disease states to qualify and c) capture estimated enrollees to be targeted and engaged to receive model benefits.
SOURCE: CMS Policy
PBP SCREEN/CATEGORY: #19a Reduced Cost Sharing for VBID/UF/SSBCI – Target Population: VBID DOCUMENT: Appendix_C_PBP2021_Screenshots-SectionB-VBID-UF-SSBCI-2019-12-09.pdf PAGE(S): Page 8
CITATION: 42 CFR 422.256
REASON WHY CHANGE IS NEEDED: Separate chronic condition(s) from socioeconomic status in specifying targeting methodology and gather additional information on disease state requirements as well as estimated enrollees to be targeted and engaged to receive model benefits.
IMPACT ON BURDEN: Low Impact
The PBP software will be updated to a) separate chronic condition(s) from socioeconomic status on an updated Additional Benefits Target Population screen b) request information about whether the enrollee needs to have all or combination of disease states to qualify and c) capture estimated enrollees to be targeted and engaged to receive model benefits.
SOURCE: CMS Policy
PBP SCREEN/CATEGORY: #19b Reduced Cost Sharing Additional Benefits for VBID/UF/SSBCI – Target Population: VBID
DOCUMENT: Appendix_C_PBP2021_Screenshots-SectionB-VBID-UF-SSBCI-2019-12-09.pdf PAGE(S): Page 32
CITATION: 42 CFR 422.256
REASON WHY CHANGE IS NEEDED: Separate chronic condition(s) from socioeconomic status in specifying targeting methodology and gather additional information on disease state requirements as well as estimated enrollees to be targeted and engaged to receive model benefits.
IMPACT ON BURDEN: Low Impact
Section D
12. The PBP software will be updated to include new Part D reductions in cost sharing screens for plans to consolidate mandatory or optional supplemental services by offering them at a reduced cost through debit card and other sources.
SOURCE: CMS Policy
PBP SCREEN/CATEGORY: Section D: Reductions in Cost Sharing
DOCUMENT: Appendix_C_PBP2021-Screenshots-SectionD-2019-12-09.pdf
PAGE(S): Pages 25-30
CITATION: 42 CFR 422.256
REASON WHY CHANGE IS NEEDED: To allow plans to offer reduced cost sharing for Non-Medicare covered benefits via other cost sharing options.
IMPACT ON BURDEN: Low impact
Screenshot:
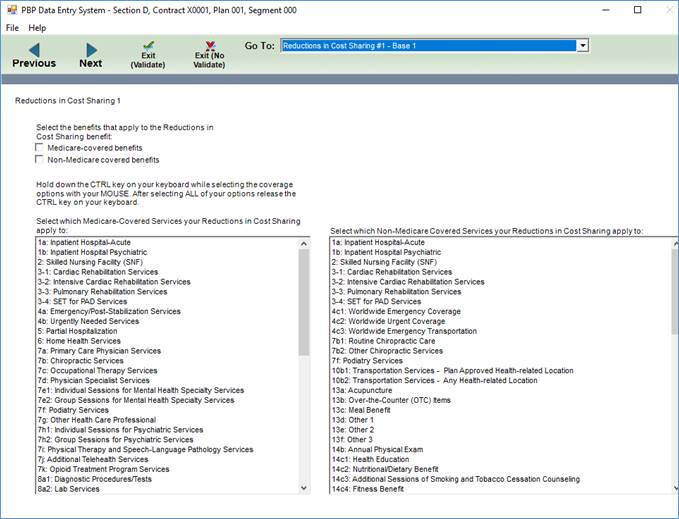
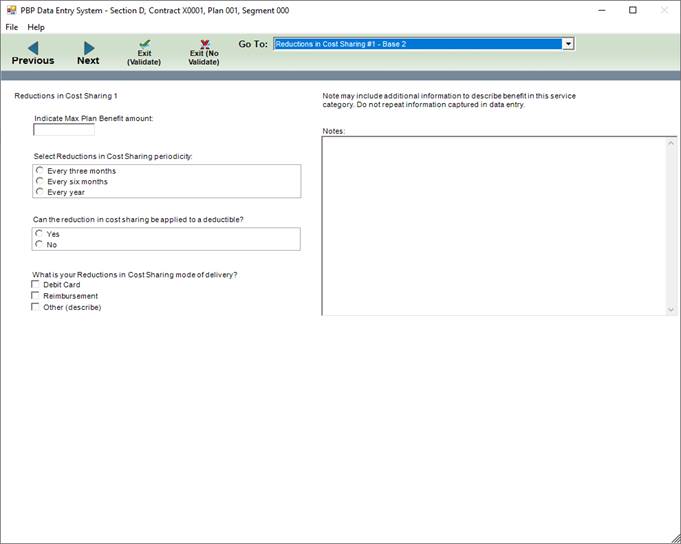
Additional explanation:
The PBP Software update includes new screens to offer reduced cost through debit cards in the new Part D reductions in cost sharing screen.
The reason for the Low Impact burden estimate is that there are minimal number of plans that may be affected by the options included with this change and they would have minimal data inputs. The change should not increase the overall burden for the entire industry much, as it is only a small group that may be using the option included with this change.
13. The PBP software will be updated to include new screens for combined mandatory supplemental benefits being offered together. These screens will allow the plan to offer groups of mandatory supplemental benefits together with overlapping cost sharing.
SOURCE: CMS Policy
PBP SCREEN/CATEGORY: Section D: Combined Benefits
DOCUMENT: Appendix_C_PBP2021-Screenshots-SectionD-2019-12-09.pdf
PAGE(S): Pages 31-34
CITATION: 42 CFR 422.256
REASON WHY CHANGE IS NEEDED: To allow plans to combine supplemental mandatory benefits.
IMPACT ON BURDEN: Low impact
Screenshot:
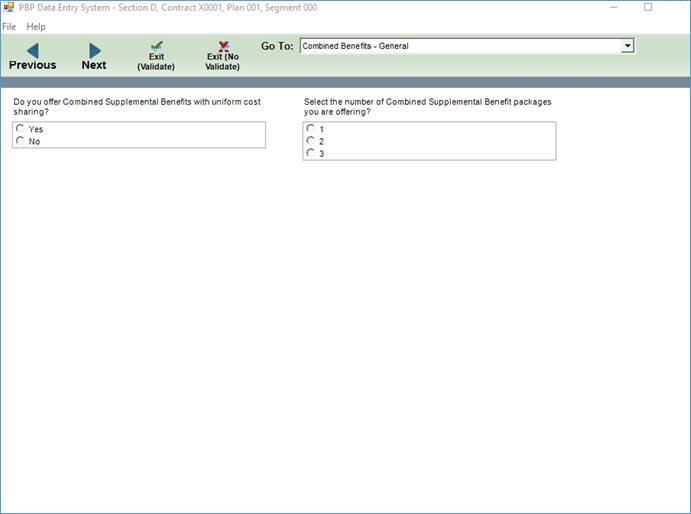
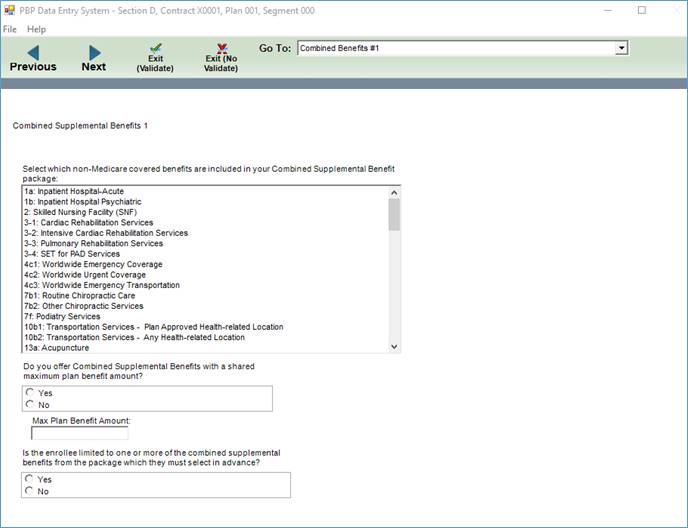
Additional Explanation: The PBP Software includes new screens to allow plans to combine supplemental mandatory benefits for Part D.
The reason for the Low Impact burden estimate is that there are minimal number of plans that may be affected by the options included with this change and they would have minimal data inputs. The change should not increase the overall burden for the entire industry much, as it is only a small group that may be using the option included with this change.
CY 2021 Formulary Changes
CMS will be removing the request to upload responses for what comprehensive strategies an organization is using to combat the opioid crisis. This upload was begun for the 2019 submissions.
SOURCE: Internal DOCUMENT: N/A PAGE(S): N/A
CITATION: 42 CFR 423.120
REASON WHY CHANGE IS NEEDED: CMS collected Opioid Strategy documents from Part D sponsors for CY 2019 and 2020. CMS continues to analyze these submissions to identify best practices and potential areas that could be adopted by CMS in its effort to reduce opioid overutilization. We appreciate Part D sponsors’ submissions to date and we will not collect additional documentation at this time.
IMPACT ON BURDEN: Reduces impact
CMS will be updated the layout for the PA/ST Criteria Change Request file. Some fields were removed to streamline the submission process.
SOURCE: Internal
Formulary Screen/Category: PA/ST Criteria Change Request Record Layout
DOCUMENT: Appendix_C_CY2021_Formulary_PAST_Criteria_Change_Request_Record_Layout.pdf PAGE(S): 1
CITATION: 42 CFR 423.120
REASON WHY CHANGE IS NEEDED: The change is being made to make the PA/ST update process more efficient for plans.
IMPACT ON BURDEN: Reduces Impact
CMS has created a new PA/ST Response record layout. This submission will streamline the submission and review of PA/ST changes for both the annual and monthly formulary submission.
SOURCE: Internal
Formulary Screen/Category: PA/ST Response Submission Layout
DOCUMENT Document: Appendix_C_CY2021_Formulary_PAST_Response_Record_Layout.pdf PAGE(S): 1
CITATION: 42 CFR 423.120
REASON WHY CHANGE IS NEEDED: The change is being made to make the PA/ST update process more efficient for plans, and to allow plans to see their PA/ST approval status in HPMS.
IMPACT ON BURDEN: Low impact
CY 2021 MTMP Changes
There is a requirement to add ‘MTM Vendor Long Term Care consultant pharmacist’ as an additional selection option under ’Qualified Provider of Interactive, Person to Person CMR with written summaries’ section
SOURCE: CMS, Internal
MTMP SCREEN/CATEGORY: CY 2021 MTMP - Enter/Edit Verify Submission Resources Page DOCUMENT: Appendix_C_MTMP CY2021 Enhancements Mockups.docx
PAGE(S): 1
CITATION: Lessons Learned
REASON WHY CHANGE IS NEEDED: To meet the Business needs and provide further identification of source of an MTM Service.
IMPACT BURDEN: No impact
There is a requirement to Add to Specific Beneficiary ‘Interventions’ (TMRs) Page, a selection option for ‘Cost saving opportunities’
SOURCE: CMS, Internal
MTMP SCREEN/CATEGORY: CY 2021 MTMP - Enter/Edit Verify Submission Interventions Page DOCUMENT: Appendix_C_MTMP CY2021 Enhancements Mockups.docx
PAGE(S): 1
CITATION: Lessons Learned
REASON WHY CHANGE IS NEEDED: To meet the Business need and identify a cost saving opportunity IMPACT BURDEN: No impact
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| File Title | CY 2021 PBP, Formulary, and MTMP List of Changes |
| Author | Madhuri Kavuru |
| File Modified | 0000-00-00 |
| File Created | 2021-01-11 |
© 2026 OMB.report | Privacy Policy