Workgroup Meeting Summary
Att D- 2020 BSC NAMCS Workgroup Meeting Summary.docx
National Ambulatory Medical Care Survey (NAMCS)
Workgroup Meeting Summary
OMB: 0920-0234
Attachment D- 2020 BSC NAMCS Workgroup Meeting Summary
National Ambulatory Medical Care Survey Workgroup Meeting
National Center for Health Statistics (NCHS) Board of Scientific Counselors (BSC)
Wednesday, May 20, 9:00am-5:00pm ET
Zoom Virtual Meeting
Draft June 17, 2020
T his
meeting summary was prepared by Lucas Smalldon, Rose Li and
Associates, Inc., under contract to the National Center for Health
Statistics (NCHS). The views expressed in this document reflect both
individual and collective opinions of the meeting participants and
not necessarily those of NCHS. Review of earlier versions of this
meeting summary by the following individuals is gratefully
acknowledged: Nancy Tuvesson.
his
meeting summary was prepared by Lucas Smalldon, Rose Li and
Associates, Inc., under contract to the National Center for Health
Statistics (NCHS). The views expressed in this document reflect both
individual and collective opinions of the meeting participants and
not necessarily those of NCHS. Review of earlier versions of this
meeting summary by the following individuals is gratefully
acknowledged: Nancy Tuvesson.
Community Health Centers Scope 4
Panel Presentations on Discussion Themes by Representatives of Non-Federal Stakeholders 5
Kathy Hempstead, Robert Wood Johnson Foundation (RWJF) 5
Lynn Olson, American Academy of Pediatrics (AAP) 6
Christine Pintz, George Washington University (GWU) School of Nursing 6
Ryan White, Rutgers University 6
Workgroup Question and Answer Period 7
Discussion of Presentations with Professional Organization and University Panel 8
Panel Presentations on Discussion Themes by Representatives from Federal Agency Stakeholders 10
Joel Cohen, Agency for Healthcare Research and Quality (AHRQ) 10
Sharon Arnold, Office of the Assistant Secretary for Planning and Evaluation (ASPE) 11
Talisha Searcy, Office of the National Coordinator for Health Information Technology (ONC) 12
Lucie Dalzell, Census Bureau 12
Workgroup Question and Answer Period 12
Discussion of Presentations with Federal Agency Panel 13
Appendix B: Participants List 18
Meeting Summary
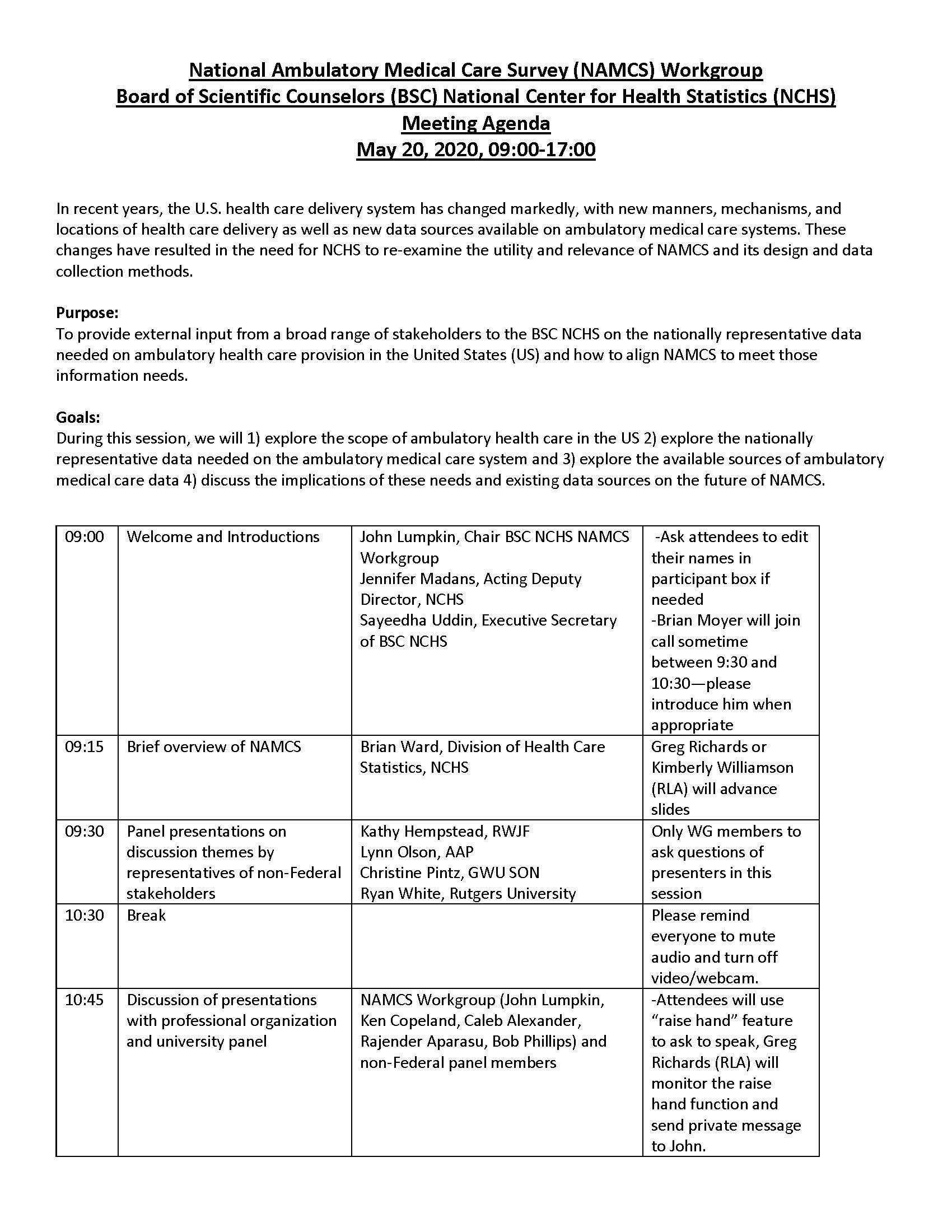
On Wednesday, May 20, 2020, the National Ambulatory Medical Care Survey (NAMCS) Workgroup of the National Center for Health Statistics (NCHS) Board of Scientific Counselors (BSC) convened a virtual meeting of federal and nonfederal stakeholders to discuss the usefulness, relevance, and limitations of NAMCS’ design and of its data collection methods.
Since NAMCS began in 1973, U.S. ambulatory health care has changed markedly, with new manners, mechanisms, and locations of health care delivery, as well as new data sources on ambulatory care systems. Given these changes, NCHS must reexamine NAMCS, consider how it might be redesigned/improved, and assess whether and how it should be continued.
Summary of findings:
Based on stakeholder input gathered during this meeting, the NAMCS Workgroup formulated its conclusions for submission to the BSC at its September 2020 meeting. See Appendix A for the meeting agenda, B for the participants list, C for participant poll results regarding how to define “ambulatory health care,” and D for Zoom chat log. The findings that emerged from the discussions follow:
Redesign NAMCS to optimize its present-day function and status as a “gold standard” data source on the delivery of ambulatory health care in the United States, as well as to serve as a potential reference for validation of other ambulatory health care datasets.
Who gets sampled: Definition of ambulatory care needs to be refined to reflect the current state of health care delivery. Ambulatory care definition should be refined to reflect that care is being provided in more diverse settings by a more diversified workforce.
How sampling occurs: Update NAMCS’ sampling frame (e.g., transitioning from physician encounters to either provider groups or sites, or individual patients), in part to better capture the role of nonphysician ambulatory health care professionals such as nurse practitioners (NPs) and physician assistants (PAs), and to gather data covering the full patient experience. Re-examine eligibility for selection of providers as in-scope e.g. clinicians practicing in outpatient settings owned by hospitals, but not hospital-based. Institute a hybrid data collection approach to leverage both the speed of electronic data capture (e.g., from EHRs) and the depth derived from manual data abstraction, thus balancing the priorities of deep cross-sectional data capture with the unique benefits of longitudinal data capture
Data collection period: Increase the measurement period of data collection to better view real-time changes in dynamic situations (e.g., the Coronavirus Disease 2019 [COVID-19] pandemic). The current methodology (i.e. only 1 week of data collection) results in fluctuations that might be artifact. Consider collection one quarter or 12 months of data. (footnote—while the workgroup considers that real-time reporting may be possible in the near future, we did not believe the technological infrastructure was supportive at this time. However, NCHS should consider this potential development in any system redesign.)
Speed of data release: Consider producing quarterly estimates.
What information is collected: Tailor NAMCS’ original design to better characterize the modern, dynamic “structure and process” of ambulatory health care delivery in the United States to
Account for the increased variation of payers, as well as types and sites of care.
Broaden NAMCS’ data collection strategies to adapt to the emergence of technology-based health care delivery modes such as telehealth, e-visits, and remote monitoring.
Expand the induction interview to better describe the system of ambulatory care delivery.
Increase the value of NAMCS: Restructure NAMCS data collection to maximize the ability to link NAMCS data to external datasets to other sources of health information including Centers for Medicare & Medicaid [CMS] claims data or proprietary electronic health records [EHRs] data).
Welcome and Introductions
John Lumpkin, BSC Member and Workgroup Chair
Jennifer Madans, Acting Deputy Director, NCHS
Sayeedha Uddin, BSC Executive Secretary
NAMCS Workgroup members introduced themselves and declared their conflicts of interest, as well as their special government employee status (wherever relevant). Participant introductions and disclosures are available in the meeting transcript.
Brief Overview of NAMCS
Brian Ward, Division of Health Care Statistics, NCHS
NAMCS was designed to meet the need for objective, reliable information about the provision and use of ambulatory medical care services in the United States. To meet this purpose, NAMCS uses national probability samples to survey and collect patient visit data from office-based physicians and community health centers (CHCs). Since its origins in 1973, NAMCS has become an annual survey that now includes data abstraction and computerized data collection.
All physicians included in the NAMCS sample are classified by the American Medical Association (AMA) or American Osteopathic Association (AOA) as primarily engaged in office-based care. In addition, they are not employed by the U.S. government; are not interns, residents, or fellows; and are not anesthesiologists, radiologists, or pathologists. Captured visits are for medical care.
Community Health Centers Scope
CHC providers include physicians, physician assistants (PAs), nurse practitioners (NPs), and certified nurse midwives (CNMs). To be included in the NAMCS sample, CHCs must meet one of the following criteria:
Receive grant funds from the federal government through Section 330 of the Public Health Service Act
Be a look-alike CHC that meets all the requirements to receive Section 330 grant funding, despite not receiving such a grant
Be an Urban Indian Health Center
NAMCS Sampling
The bullet points below summarize sample parameters for physicians and CHCs.
Physicians
Eligibility criteria are applied to AMA and AOA Masterfile databases
Sample of 3,000 physicians
2,750 MDs and 250 DOs
Approximately 30 visits abstracted from each physician’s records
CHCs
Eligibility criteria are applied to the Health Resources and Services Administration (HRSA) CHC database
Sample of 104 CHCs
1-3 advanced practice providers within CHC selected
Approximately 30 visits abstracted from each CHC provider’s records
NAMCS Strengths
NAMCS is the only nationally representative survey of physicians and CHCs. It collects visit-level data directly from provider sites, including clinical data elements such as patient demographics, diagnoses, procedures, medications, immunizations, laboratory and diagnostic tests, and reasons for visits. Provider characteristics can be analyzed either independently or with visit-level data. NAMCS can also include sponsored content on timely and relevant health topics (e.g., EHR adoption and interoperability).
NAMCS Limitations
Although NAMCS has remained an important data source on the provision of ambulatory care, the ambulatory health care system itself has changed since the survey was first fielded. Settings and providers of ambulatory care now include more PAs and NPs, and physicians’ offices have become more complex with the growth of health care conglomerates and hospital-owned groups. Moreover, much ambulatory care delivery no longer occurs in person. As these changes have proliferated, ambulatory care data have also changed. Providers face increased reporting requirements, and more physicians and CHCs are adopting EHRs. As electronic data become more prevalent, so do concerns about data security and confidentiality.
In addition to these changes to the ambulatory health care data landscape, NAMCS response rates have declined across recent years. During 2018, unweighted physician participation rates were approximately 41 percent, with unweighted response rates of approximately 37 percent.
As a result of these challenges, the NCHS BSC established the NAMCS Workgroup to help chart the future of NAMCS. The Workgroup convened today’s meeting to solicit expert input from a panel of knowledgeable federal, academic, and professional stakeholders.
Panel Presentations on Discussion Themes by Representatives of Non-Federal Stakeholders
Kathy Hempstead, Robert Wood Johnson Foundation (RWJF)
Dr. Hempstead emphasized that ambulatory medical care includes not only traditional visits to physicians’ offices, but also visits to retail clinics and urgent care centers, as well as virtual visits. She suggested that NAMCS should define the scope of ambulatory care using clinically relevant criteria, as opposed to, for example, payer-related criteria. She also suggested that meeting participants consider what types of care to classify as ambulatory (Appendix C contains these poll results); for example, many patients now use technology for self-monitoring, yet it remains unclear how this trend has affected traditional ambulatory care services.
Dr. Hempstead also noted the importance of understanding how patients use different forms of ambulatory care across time, including how encounters or visits are distributed across different types of patients, and how payers as well as barriers to access affect different populations. She noted that the main alternatives to NAMCS for obtaining ambulatory care data are claims (e.g., CMS) and EHR vendors. Although claims data are typically more comprehensive than EHR data, they are also slower to become available. Dr. Hempstead expressed a desire for a national-level all-payer claims database (APCD) to provide reliable, high-quality, and nationally representative EHR and claims data.
Lynn Olson, American Academy of Pediatrics (AAP)
Dr. Olson stated that NAMCS provides unique, valuable data on trends in pediatric care, noting that how and where ambulatory pediatric care is delivered continues to evolve. She highlighted the importance of valid, reliable, and generalizable data to capture these trends, and stressed the need to balance tradeoffs between capturing trends and ensuring validity of measures. She also noted the need for NAMCS to capture multiple measures that can be used for triangulation across survey, clinical, claims, and EHR data. One example of a unique dataset provided for AAP by NAMCS is trends in length of pediatric primary care office visits between 2005 and 2015.
Christine Pintz, George Washington University (GWU) School of Nursing
Dr. Pintz noted that NAMCS is medically oriented and that health care has become more expansive. She suggested that modern modes of ambulatory care could be better captured by adopting a patient-centered perspective, at least for a portion of NAMCS. Such a perspective could more holistically account for care components such as patient engagement, prevention practices, health promotion, lifestyle management, social determinants of health, behavioral health, and alternative health practices. Dr. Pintz also highlighted that ambulatory care is increasingly team-based and not tied to one particular provider, reinforcing the argument that the NAMCS sampling frame should be modified to focus on patients rather than physicians.
Dr. Pintz noted that important gaps currently limit the utility of NAMCS: (1) lack of longitudinal data and external linkages to other surveys and (2) failure to distinguish between different nursing roles (e.g., NP versus nurse midwife, and registered nurse [RN] versus licensed practical nurse [LPN]). She also mentioned various tradeoffs between electronic versus manual data abstraction: although electronic abstraction is fast, seamless, and cost-effective, and can offer larger sample sizes, manual abstraction tends to provide higher-quality data.
Ryan White, Rutgers University
Dr. White noted that no nationally representative dataset captures the clinical activities of PAs, even as that profession continues to grow rapidly. Approximately 40 percent of PAs report their primary work setting to be office-based private practices, and approximately 26 percent of PAs work in primary care. Further, CHCs employ 2-3 percent of the PA workforce nationwide, and since 2018 have employed PAs, NPs, and certified midwives at higher rates than physicians. Lacking a nationally representative data set on PAs, researchers find it difficult to characterize this workforce and to analyze outcomes associated with their delivery of ambulatory care services.
The lack of a Masterfile challenges researchers’ ability to collect and work with PA data. Although the National Commission on Certification of PAs maintains a database on all certified PAs, it is incomplete, making it difficult for researchers to identify PAs who fall within the sampling frames of NAMCS and other surveys. PAs who do fall within the NAMCS sampling frame may not have the authority to determine whether they participate in the survey. In addition, administrative, billing, or claims data sometimes attribute PA visits to physicians (e.g., if a physician’s National Provider Identifier [NPI] number is used to code for billing)—further complicating study of this workforce.
Dr. White suggested that NAMCS capture PA practice specialty to supplement other data sources and to offer a more comprehensive picture of the PA workforce. NAMCS could also develop a partnership with professional organizations such as the American Academy of PAs to identify those PAs who could participate in a redesigned NAMCS.
Dr. White noted that a redesigned NAMCS should aim to characterize the who, what, when, and where of ambulatory medical services; identify access and outcome disparities; and investigate the quality of ambulatory medical care to help inform health policy decisions. The COVID-19 pandemic may well precipitate certain permanent changes to ambulatory care, and NAMCS could provide a valuable window into the nature of those changes.
Workgroup Question and Answer Period
Discussions during the Question and Answer period focused on adjusting the sampling frame and increasing response rates.
Sampling Frame
Panelists revisited Dr. Pintz’ suggestion to organize the NAMCS sampling frame around patients rather than providers. This reframing would help NAMCS capture all modes of patient interaction with ambulatory health care services, including with nonphysician providers, as well as virtual health care delivery mechanisms such as telehealth and self-monitoring apps. Dr. Copeland recommended combining the provider and patient perspectives, such as how the Medicare Current Beneficiary Survey both interviews Medicare beneficiaries and acquires claims data.
Dr. Hempstead suggested that the sampling frame limitations could also be addressed by modernizing the definition of providers to include both nonphysicians (e.g., NPs and PAs) and physicians who have traditionally been considered out of scope for nonclinical reasons (e.g., affiliated with an academic institution or technically employed by a hospital). Other panelists noted that NAMCS could move toward the framework increasingly adopted by payers, in which ambulatory care is conceptualized in terms of episodes rather than visits—that is, one episode corresponds to all encounters a patient has with health systems in order to address a particular concern or condition.
To inform strategies to better capture the roles of nonphysician providers to outpatient care, Dr. Lumpkin suggested consulting licensing board records. However, Drs. Pintz and White noted that such records may not provide equal value across professional categories (e.g., they provide clinical specialty information on NPs but not on PAs).
Dr. Alexander suggested that modifications to the NAMCS physician induction interview could improve identification of NPs and PAs in ambulatory health care practices, which could then inform adjustments to NAMCS’ sampling frame.
Response Rates
Participants also discussed potential strategies to increase NAMCS response rates, such as changing which providers are asked to participate or providing incentives to participate. Dr. Olson proposed that NCHS test various strategies on NAMCS subsamples before broadly implementing any one strategy. Dr. Hempstead noted that Medical Expenditure Panel Survey (MEPS) researchers modified the MEPS sampling frame to solicit practice-level information from practice managers, which led to increased response rates.
Discussion of Presentations with Professional Organization and University Panel
NAMCS Workgroup and Non-Federal Panel Members
Following nonfederal panelist presentations and NAMCS Workgroup questions, participants addressed five questions about a NAMCS redesign, under the theme “understanding the gap between the ambulatory health care data that are needed versus what data are available.”
Question 1: What is the scope of ambulatory medical care in the United States (i.e., should telemedicine, retail clinics, visits to nonphysicians be included in the scope)? What scope should be included in NAMCS?
Participants
raised telemedicine, home visits, and out-of-scope practices (i.e.,
those in which a physician is employed by a hospital, an urgent care
facility, or a retail clinic, mobile clinic, work-based clinic,
specialty clinic, or perhaps an ambulatory surgical clinic) as
potential directions for expanding the scope of NAMCS. They
reiterated the need to capture contributions of nonphysician
providers, especially PAs, NPs, and certified nurse midwives.
Question 2: What information is needed on the ambulatory health care system in the United States? What is the biggest contribution that NAMCS could make?
Participants
reemphasized earlier sentiments that NAMCS “cannot be
everything to everybody” and therefore must be designed to
fulfill a specific function (i.e., to fill a specific data gap in the
health data landscape). Dr. O’Malley noted that NAMCS’
role in capturing the contents of ambulatory health care
encounters (i.e., patients’ diagnoses, conditions, complaints)
continues to be vitally important, adding that a NAMCS redesign could
also focus on capturing continuity of care (e.g., from primary care
physicians to specialists). Dr. Phillips reinforced Dr. O’Malley’s
desire for continuity-of-care, and they both agreed that this could
be done in a cross-sectional way (e.g., by asking providers or
patients how long they have been in contact). However, Dr. Phillips
also noted that NAMCS’ survey data could be supplemented with
longitudinal EHR data. Dr. Phillips noted that NAMCS should capture
relationships between trends in the provision of ambulatory care and
patient outcomes, and Dr. Copeland stated that the complications of
longitudinal data capture could be mitigated by following a NAMCS
subsample longitudinally.
Dr. Olson recommended that NAMCS strive for maximum generalizability—capturing a limited set of high-validity markers that can be linked to external data sources and used to triangulate answers to a wide range of research questions that no single survey can answer. Dr. Alexander, however, echoed an earlier comment that NAMCS’ most important contribution is its capture of the structure and process (from the Donabedian model of measuring quality of care in terms of structure, process, and outcome) of ambulatory care in the United States. Dr. Aparasu noted that physician induction interviews could be redesigned to capture key elements of the structure of ambulatory health care. He also stressed that NAMCS already excels at capturing the process of care and that its depth as a cross-sectional survey is a vital asset; he cautioned that an attempt to transform NAMCS into a longitudinal survey could thus undermine its key strength.
Dr. Lumpkin suggested that NAMCS capture more granular payment information so that researchers and policymakers can explore, for example, the impacts of high-deductible plans on provision of ambulatory care services, and the differences in health care usage among patients with different payment sources (e.g., Medicare Fee-for-Service versus Medicare Advantage). He also proposed the use of NAMCS data to compare various payment arrangements (i.e., value-based purchasing) to help view the structure of ambulatory care delivery. However, Dr. Alexander commented that MEPS and other data sources (both public and proprietary) are better suited to that aim.
Dr. White proposed that NAMCS capture practice-level information regarding Accountable Care Organization (ACO) participation to help inform users of organizational and structural models of payment, as well as practice-level information regarding timeliness or accessibility of care (e.g., time to next appointment).
Question 3: What sources of ambulatory health care data exist outside of NAMCS?
Participants
acknowledged the following non-NAMCS sources of ambulatory health
care data: EHRs, CMS/claims data (public and proprietary), other
federally sponsored surveys (e.g., MEPS).
Question 4: What are the strengths and limitations of those sources compared to NAMCS?
MEPS
excels at providing granular financial and payer information, whereas
CMS claims data are best for viewing information on procedures and
procedure-specific costs. EHRs enable fast and easy data
extraction—including longitudinal data—but lack the depth
of cross-sectional surveys such as NAMCS. NAMCS captures
provider-level encounter information, which provides better data
richness, but misses longitudinal patterns and neglects ambulatory
health care encounters that do not involve a physician. Dr. Kurtzman
noted that NAMCS also enables sub-sampling of CHCs, which researchers
have used to study differences in quality of care among provider
types. Dr. Copeland noted that NAMCS could benefit from directly
linking diagnosis and medication information, as MEPS and IQVIA
already do. Dr. Stafford identified slow data releases as a major
weakness of NAMCS, and participants highlighted NAMCS’
inability to show local-level information.
Question 5: What gaps exist between the information needed and information available on the ambulatory medical care system?
Dr.
Radhakrishnan highlighted that NAMCS lacks information on mental and
behavioral health issues (e.g., depression, abuse, comorbidities,
substance misuse/dependence) and the requisite services provided
(e.g., screening, treatment, and counseling).
Participants reiterated earlier comments about NAMCS’ inability to adequately capture patient encounters with NPs, PAs, and other nonphysician providers. Dr. Phillips suggested modification of NAMCS’ starting sampling strategy (i.e., going beyond the AMA and AOA Masterfile) to address this issue and the previously mentioned issue of physicians being designated out of scope. He also hypothesized that such adjustments to NAMCS’ sampling strategy may improve response rates; Dr. Chai suggested that response rates could also be improved by offering a nonmonetary incentive to participate, such as a certification.
Participants noted that revising NAMCS’ sampling strategy may enable capture of telehealth visits, which have become much more common during the COVID-19 pandemic (this change in the process of ambulatory health care delivery may have permanent effects following the pandemic). Moreover, as the pandemic spreads and vertical integrations continue to occur across the health care industry, NAMCS could help to track the composition of the ambulatory health care provider workforce.
Dr. Chai suggested that NAMCS include anesthesiologists who serve in ambulatory pain clinics.
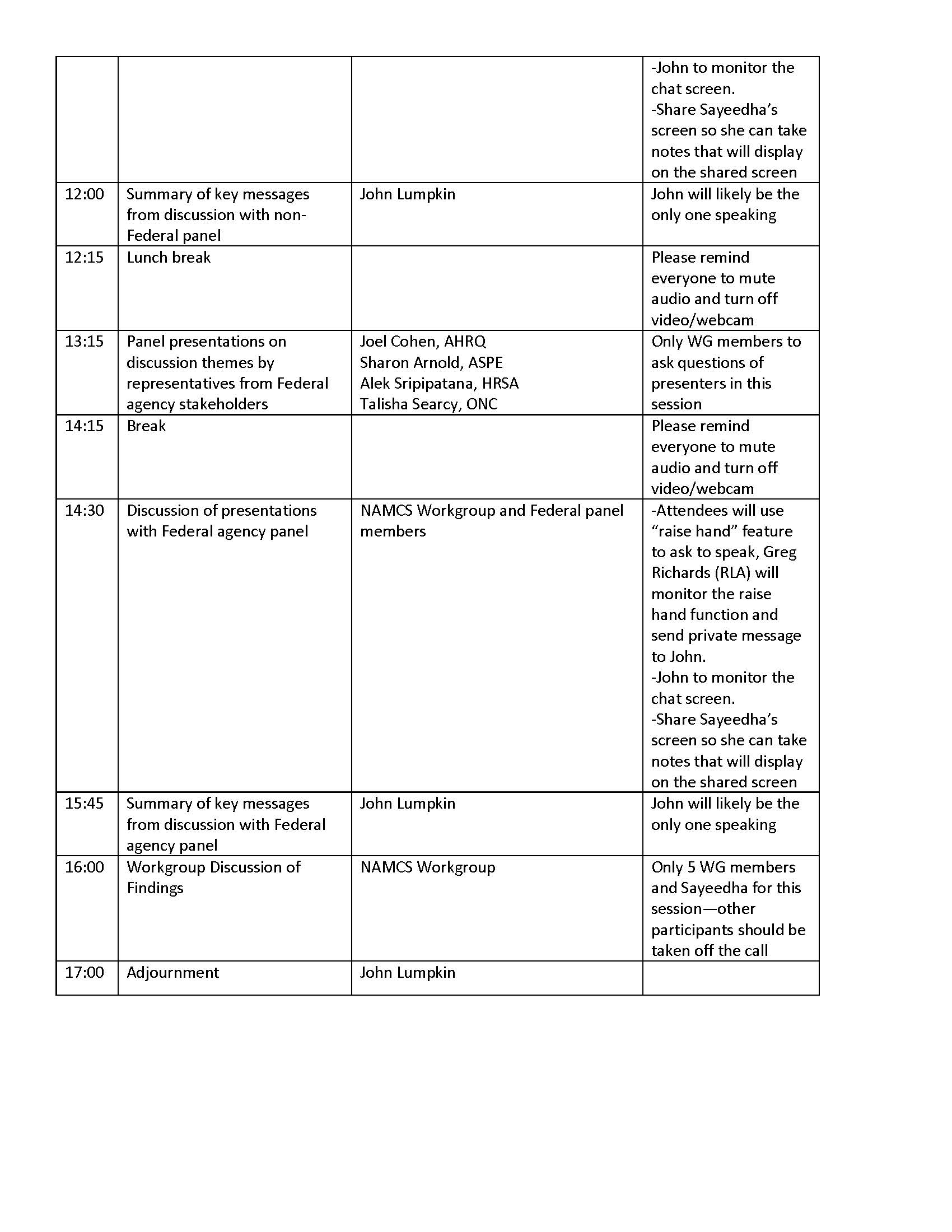
Panel Presentations on Discussion Themes by Representatives from Federal Agency Stakeholders
Joel Cohen, Agency for Healthcare Research and Quality (AHRQ)
Dr. Cohen highlighted the comparative lack of available data on the supply (i.e., provider) side of ambulatory health care delivery relative to the demand (i.e., patient) side. The relative lack of supply-side data stymies efforts to generate and validate predictive models of provider-side ambulatory care. This lack of models, in turn, challenges the health care system in the context of emerging crises, such as the COVID-19 pandemic (e.g., public health experts/policymakers cannot determine whether provider capacity can meet the demand for care, whether prices will rise, or how changing demand may jeopardize the financial security of provider groups).
Dr. Cohen also noted that laboratories providing services associated with ambulatory care are frequently omitted from surveys and other data collection efforts, despite playing a major role in the delivery of such care. He acknowledged the difficulty of capturing the many elements of ambulatory health care in a single survey and stated that the NAMCS team should select which elements of the system to target for data collection—or split its efforts across several surveys. The structure of ambulatory health care is quickly changing as hospitals purchase small physicians’ practices, while others merge. Current data collection efforts neglect these changes.
Dr. Cohen also highlighted the tradeoff between attaining rich data and achieving high response rates. Providers often lack time to complete a dense survey, and although previous efforts to streamline surveys have effectively raised response rates, the resulting data are limited. However, in some cases it may be feasible to ask different types of questions of different respondents, thereby maintaining data richness without increasing respondent burden (e.g., asking providers to provide clinical information while asking practice managers or office managers to provide financial data). In general, NAMCS may benefit from adopting mixed methods for data collection (e.g., electronic EHR data extraction combined with provider surveys).
Finally, Dr. Cohen advocated for increased linkages between NAMCS and other federal surveys, using the example of the National Health Interview Survey’s (NHIS) linkage to MEPS (i.e., MEPS’ sample is selected from NHIS respondents, which facilitates easy and efficient linkage).
Sharon Arnold, Office of the Assistant Secretary for Planning and Evaluation (ASPE)
Dr. Arnold highlighted NAMCS’ role as a gold standard reference to validate other supply-side ambulatory health care datasets. She reinforced Dr. Cohen’s point that many sources exist for demand-side ambulatory care data (e.g., EHRs, surveys, registries, and claims databases). Thus, NAMCS can serve a vital role by providing detailed data on the organizational structure of the ambulatory health care system. Dr. Arnold also echoed earlier comments about increasing the scope of NAMCS to include more types of providers.
Dr. Arnold cautioned the Workgroup against undervaluing NAMCS, because most of the existing data sources on ambulatory health lack representative samples. NAMCS’ representative dataset can serve as a benchmark against which policymakers can gauge the validity of other datasets, which they must consult to inform more urgent policy choices (i.e., because these other sources can release data on a faster timeframe than NAMCS).
Dr. Arnold also emphasized that NAMCS could be redesigned to help capture local variations in ambulatory health care delivery. Although granular local-level data are challenging to generate, they can provide crucial context for policymakers.
Alek Sripipatana, HRSA
Dr. Sripipatana praised NAMCS for providing data that HRSA can use to compare care delivery practices across CHCs and other ambulatory care providers (e.g., primary care clinics). NAMCS also allows HRSA to develop strategies for improving CHCs (e.g., by evaluating variability in EHR adoption across sites).
Talisha Searcy, Office of the National Coordinator for Health Information Technology (ONC)
Dr. Searcy echoed earlier comments on the potential for NAMCS to capture the many changes occurring within the organizational structure of ambulatory health care delivery, as well as on the need for greater linkages between NAMCS and other surveys and data sources. She also highlighted efforts such as the Trusted Exchange Framework and Common Agreement, which was spurred by the 21st Century Cures Act, to help foster health information exchange among health information networks. Such efforts could potentially provide a window into site-specific EHR data that have previously been unobtainable.
Lucie Dalzell, Census Bureau
Dr. Dalzell reinforced an earlier comment that it is often the office manager, rather than the physician, who decides whether to participate in NAMCS. The office manager of a physician practice may determine that the time required to complete NAMCS imposes an unnecessary business burden with no measurable benefit in terms of care, and therefore decide not to participate. If NAMCS were marketed as a resource to improve care, in addition to a scientific resource, it could attain higher response rates, a larger user base, and improved data quality. Response rates and data quality may also be improved by increasing job satisfaction of NAMCS’ field representatives.
Dr. Dalzell also addressed the comparative advantages/drawbacks of manual versus automatic data abstraction. The Census Bureau has used both methods, and Dr. Dalzell was surprised that some Census Bureau regional offices were unhappy when abstraction was conducted remotely, whereas others were pleased at the simplified process as long as field representatives remained available to answer questions or provide support. Dr. Dalzell used this example to highlight the fact that different respondents will have different preferences, and that tradeoffs between data collection modes and their effects on response rates should be carefully considered. Finally, she noted that large organizations tend to prefer that data collectors approach them once at the organization level with a list of desired respondents.
Workgroup Question and Answer Period
Dr. Cohen suggested potential strategies for establishing greater NAMCS linkages, for example by surveying physicians and practices that participate in NHIS or MEPS, or by selecting a NAMCS sample based on the sample of another survey to inform next-year nonresponse adjustments. He also suggested linking NAMCS to administrative data (e.g., from CMS or private claims).
Dr. Phillips suggested that HRSA’s sampling of Federally Qualified Health Centers (FQHCs) link to the Uniform Data System (UDS) or to one of the Community Health Applied Research Networks (CHARNs) in order to incorporate more data about the site encountered by the respondent. An EHR linkage could also fulfill this function.
Participants discussed linkage of clinical NAMCS data with financial MEPS data. If one survey attempts to gather both types of data, data richness will likely decrease. Participants stressed the importance of establishing linkages during survey design rather than post hoc.
Dr. Searcy noted that ONC has worked to develop regulatory guidance around protected health information (PHI) to ensure that the Trusted Exchange Framework and Common Agreement is aligned with the Health Insurance Portability and Accountability Act (HIPAA). This guidance provides regulations on patient privacy and consent, and on other health information governed by HIPAA, effectively standardizing the rules of health information exchange. ONC is also developing data standards to facilitate more efficient bulk data abstraction from multiple providers and practices.
Discussion of Presentations with Federal Agency Panel
NAMCS Workgroup and Federal Panel Members
Following federal panelist presentations and NAMCS Workgroup questions, participants discussed five questions about a potential NAMCS redesign, under the theme “aligning NAMCS to meet existing and future needs for data on the U.S. ambulatory health care system.”
Question 1: What is the purpose of NAMCS (e.g., reference versus repository)?
Dr.
Alexander and others shared their view of NAMCS as an authoritative
source of information about the provision of ambulatory care in the
United States (i.e., as a benchmark). Dr. Alexander noted that
validation of other datasets does not seem to be its primary utility
for users. Dr. Chai reiterated NAMCS’ primary value as a
reference standard and cautioned participants against compromising
that value by collecting too many types of data simultaneously or by
transforming NAMCS into a longitudinal dataset. She also noted that
NAMCS could potentially expand its focus on softer data types that
are unavailable through claims databases (i.e., smoking status,
family history).
Question 2: What are the goals, objectives, and added value of a redesigned NAMCS?
Dr.
Aparasu framed the goal of a redesigned NAMCS as better capture of
the breadth as well as the depth of ambulatory health care delivery
in the United States by collecting data that other sources do not
(e.g., in terms of breadth, what proportion of visits were to urgent
care versus CHCs, office-based practices, and hospital outpatient
departments?)—and in such a way that they can then be linked to
those other sources. Dr. Cohen expressed a similar desire to
distinguish among types of ambulatory care sites but cautioned that
these distinctions can be ambiguous (e.g., a patient may classify the
site as a community clinic, although it may be billed as an emergency
department because of its affiliation with a hospital).
Dr. Copeland reemphasized earlier comments on capturing ambulatory care encounters with nonphysician providers such as NPs and PAs—possibly by sampling at the site level—as well as telecare and other virtual ambulatory health encounters (e.g., via self-monitoring apps). He also proposed an increased focus on the collection of ancillary information, such as which providers become involved in caring for a patient after a primary physician’s initial diagnosis.
Dr. Kurtzman stressed that NCHS must determine which features of NAMCS should remain unchanged to maintain its ability to track health care trends from past decades to the future. Dr. O’Malley advocated for maintaining most of NAMCS’ current content as well as its design.
Question 3: What changes are needed for NAMCS to address the gaps in the information needed on the U.S. ambulatory medical care system (possibilities for linkage to other data sets or longitudinal data collection)?
Dr.
Dalzell explained that the NAMCS out-of-scope rate is approximately
40 percent, which impacts the data generated in unknown ways.
Contributing to that high rate are the 2 percent of physicians in the
NAMCS sample who are deceased and another 15 percent who are retired.
Therefore, NAMCS should update the sampling frame and validate that
each individual targeted for the sample is still practicing.
Question 4: How can validity and reliability of a redesigned NAMCS be assessed (i.e., what data sources can be used to validate the sampling frame or a subset of the frame, can EHR data be used to verify or supplement responses to clinical questions)?
Dr.
Phillips reiterated earlier comments about the potential to use EHR
and MEPS data, as well as data from specialist certification boards
and from the American Board of Family Medicine’s (ABFM) annual
cross-sectional census of family physicians, to help validate a
redesigned NAMCS. Dr. Alexander noted the common practice of
assessing data quality/validity by using proprietary visit-based
audits but questioned the value of using claims data given the many
differences in what information is captured. Several Workgroup
members noted that despite the potential value of validating NAMCS
data with EHRs, the level of EHR implementation and the corresponding
richness of data collection varies widely by ambulatory care site.
Question 5: Which data collection methods (e.g., electronic vs. manual abstraction) should be used for NAMCS?
Participants
generally favored a mixed method that leverages both the richness of
data from manual abstraction and the speed of electronic abstraction
of data such as the number and types of prescriptions written by
particular physicians or practices. In addition, electronic
abstraction can help to reduce NAMCS’ respondent burden and
thus improve response rates. Dr. White agreed that a hybrid approach
presents clear benefits but cautioned against heavy reliance on EHR
data, which often masks the contributions of nonphysician providers
to patient care. Dr. Stafford agreed, adding that data integrity
within various EHR systems may not be well-validated.
Dr. Copeland proposed a two-stage collection model, wherein NAMCS first collects EHR data via rapid electronic abstraction, then collects more in-depth data via manual abstraction to fill in key gaps. Dr. Aparasu endorsed this hybrid model, noting that it may not only increase the NAMCS sample size, but also accelerate the timeline for release of EHR-derived data—addressing concerns about slow periodicity of data release.
Dr. Dalzell stressed that NCHS’ deliberations about increased electronic data abstraction in NAMCS should consider the importance of maintaining relationships between field representatives and survey respondents.
Workgroup Next Steps
NAMCS Workgroup
Following receipt of this meeting summary, members of the NAMCS Workgroup will use input from nonfederal and federal panelists to help develop a set of recommendations to the BSC for a potential NAMCS redesign.
Adjournment
John Lumpkin, BSC Member and Workgroup Chair
Dr. Lumpkin adjourned the meeting.
Appendix A: Meeting Agenda
Appendix B: Participants List
NAMCS WORKGROUP MEETING MAY 20, 2020 PARTICIPANT LIST
BSC NCHS NAMCS Workgroup Members
John Lumpkin, Workgroup Chair, BSC Member, Blue Cross Blue Shield of North Carolina
Caleb Alexander, Johns Hopkins Bloomberg School of Public Health
Rajender Aparasu, University of Houston, College of Pharmacy
Ken Copeland, BSC Member, NORC
Bob Phillips, American Academy of Family Medicine
Non-federal Participants
Sarah Baizer, National Association of Community Health Centers*
Jean Fuglesten Biniek, Health Care Cost Institute
Elizabeth Hausman, American College of Preventive Medicine
Kathy Hempstead, Robert Wood Johnson Foundation*
Ellen Kurtzman, George Washington University School of Nursing
Lynn Olson, American Academy of Pediatrics*
Ann O’Malley, Mathematica
Darrell Philpot, IQVIA
Christine Pintz, George Washington University School of Nursing*
Randy Stafford, Stanford University
Ryan White, Rutgers University*
Federal Participants
Sharon Arnold, ASPE*
Grace Chai, FDA
Joel Cohen, AHRQ*
Lucinda Dalzell, Census
Eloise Parker, Census
Eric Miller, NIH
Alek Sripipatana, HRSA*
Talisha Searcy, ONC*
NCHS Attendees
Brian Moyer, Director, NCHS
Jennifer Madans, Acting Deputy Director, NCHS
Denys Lau, Director, Division of Health Care Statistics
Carol DeFrances, Deputy Director, Division of Health Care Statistics
Brian Ward, Chief, Ambulatory and Hospital Care Branch, Division of Health Care Statistics
Sayeedha Uddin, Designated Federal Officer, Board of Scientific Counselors, NCHS
*Panelists
Appendix C: Participant Poll Results
Participants were asked to complete an informal poll indicating whether they consider various aspects of health care as falling within the ‘ambulatory care’ category. Results of this poll are summarized below. Note that the poll was not asking whether NAMCS should capture all care modes categorized as ‘ambulatory care’.
|
# Yes |
# No |
% Yes |
% No |
Nurse managed health centers |
22 |
2 |
92% |
8% |
Urgicare centers |
21 |
3 |
88% |
13% |
Ambulatory surgery treatment centers |
15 |
9 |
63% |
38% |
Indian Health Centers |
24 |
0 |
100% |
0% |
Health Departments |
15 |
9 |
63% |
38% |
CHCs |
24 |
0 |
100% |
0% |
Workplace clinics |
12 |
12 |
50% |
50% |
University Clinics |
20 |
4 |
83% |
17% |
FQHCs |
23 |
1 |
96% |
4% |
Home |
12 |
12 |
50% |
50% |
Telemedicine telephone based |
19 |
3 |
86% |
14% |
Mobile Care |
16 |
6 |
73% |
27% |
Telemedicine e mail |
15 |
7 |
68% |
32% |
Urgent care |
20 |
2 |
91% |
9% |
Primary care practice site |
22 |
0 |
100% |
0% |
Specialty care practice site |
21 |
1 |
95% |
5% |
Telemedicine office based |
22 |
0 |
100% |
0% |
Specialty clinic |
21 |
1 |
95% |
5% |
Retail clinic |
19 |
3 |
86% |
14% |
Telemedicine and non-office based |
18 |
4 |
82% |
18% |
Physical Therapy Centers |
11 |
12 |
48% |
52% |
Pharmacy |
11 |
12 |
48% |
52% |
Hospital owned clinics |
23 |
0 |
100% |
0% |
Managed care centers |
22 |
1 |
96% |
4% |
Student Health Centers |
20 |
3 |
87% |
13% |
Hospital outpatient clinics |
22 |
1 |
96% |
4% |
Other clinical sites (Optometry, audiology, spirometry) |
11 |
12 |
48% |
52% |
Dental Offices |
11 |
12 |
48% |
52% |
Dental Clinics |
10 |
13 |
43% |
57% |
Chiropractic Care Sites |
10 |
13 |
43% |
57% |
App-provided care |
14 |
13 |
52% |
48% |
Home based monitoring |
11 |
16 |
41% |
59% |
Complementary and Alternative Care Clinics |
17 |
10 |
63% |
37% |
Community based clinics |
27 |
0 |
100% |
0% |
Behavioral health clinics |
24 |
3 |
89% |
11% |
Appendix D: Zoom Chat Log
00:41:35 Rajender Aparasu - University of Houston: Good Morning All
00:42:21 Sayeedha Uddin--NCHS: Good morning!
00:44:41 John Lumpkin BCBSNC Foundation: Good morning to all, thank you for participating
01:22:42 Sayeedha Uddin--NCHS: Reminder--Please add your name affiliation to your name or phone number in the Zoom participants list. Thanks!
01:24:31 Bob Phillips, ABFM CPV: Small Independent practices remain 36% of practices where family physicians work, and where more than half of family physicians practices. I agree with Dr. Olson that this has been changing, and the pandemic may speed that up
01:28:20 Bob Phillips, ABFM CPV: Given the reliance on NAMCS by researchers like Dr. Olson, I am interested in her reaction to Dr. Dalzell's revelation that In 2018, the physician response rate was 46.2% and the physician out-of-scope rate was 42%. In 2019, the physician response rate was 29.6% and the out-of-scope rate was 41.4%.
01:31:17 Sayeedha Uddin--NCHS: Reminder--Please add your name affiliation to your name or phone number in the Zoom participants list. Thanks!
01:37:18 Bob Phillips, ABFM CPV: Ryan White also raised the issue of sampling and correctly identifying NPs and PAs with the added goals of better understanding of ambulatory care, professional differentiation, better understanding of teams in care, and more correctly identifying their practice specialties. For example the RN Sample Survey NP data from 2018 are not generally available yet, but GWU researchers recently said that it suggests NPs in primary care are less than 30% of the NP workforce. We really can't afford to be so blind to work of health professionals in ambulatory care.
01:44:16 Amy Blum NCHS: Can the PA participation in an encounter be determined by the provider ID #?
01:45:08 Ann O'Malley, Mathematica: If the PA bills under their own NPI yes. But if they work "incident to" a physician, then I don't think so.
01:46:49 Jeannie Fuglesten Biniek, Health Care Cost Institute: This is a limitation of claims data when examining the role and activities of PAs and NPs
01:47:16 Caleb Alexander - Johns Hopkins: Perhaps for Christine: 10. Is there an NP or CNM “Masterfile”, or are the challenges very similar to those of capturing PAs?
01:48:01 Caleb Alexander - Johns Hopkins: General query for panelists: Could induction interview be expanded so as to yield more comprehensive information about important dimensions of care that are currently not well captured (e.g., provision of telehealth, models of team-based care)?
01:49:35 Caleb Alexander - Johns Hopkins: I think we’ll be hearing from colleagues from the Census later about some considerations regarding sampling groups rather than providers - which is quite relevant to issue of capturing advanced practice providers
01:54:26 Ryan White - Rutgers University: To support what's been said by others, PAs can bill under their own NPI for many payers, but not all. In addition, if incident-to billing is used, the PA would be "hidden" in the claims data. I think this emphasizes the importance of seeking methods to capture outcomes associated with teams rather than individual providers.
01:55:18 Ellen Kurtzman: Greetings! A quick note regarding a NP/midwife masterfile -- the state Boards of Nursing maintain license information. So, collectively, they would have a census of all licensed APRNs including NPs and midwives.
01:56:21 Christine Pintz - George Washington University: Nurse practitioners are being encouraged by national NP organizations to bill under their own NPI and not incident to. However, this is often the decision by the practice and not the individual NP.
01:57:54 Christine Pintz - George Washington University: The American Association of Nurse Practitioners (AANP) has approximately 180,000 members which is about half of all NPs in this country. A combination of state boards of nursing and AANP may help identify those NPs.
01:58:47 Caleb Alexander - Johns Hopkins: Is it fair to say that three strategies to increase capture of care delivered by non-physician providers (while preserving general NAMCS design) are to sample them; expand their capture on induction form; and/or expand their capture on visit form?
01:59:27 Bob Phillips, ABFM CPV: Christine, since NPPES now captures more than 90% of NPs, could it be a viable sampling mechanism if NCHS doesn't move to practice sampling. I know NPPES has challenges, but it could get around incident-to limitations of using claims data. Your experience would be valuable in understanding the limitations
02:01:53 Christine Pintz - George Washington University: It could be - there are some issues with individual questions but it could be helpful. At NONPF, we are trying to look into creating a minimum data set for NPs.
02:02:06 Ryan White - Rutgers University: Caleb, I agree with these strategies. Even beyond PAs and NPs, I think about visits that may have involved a mental health professional who is co-located in the same practice. Perhaps the induction form could be amended to capture other members of the team who participated in the encounter or the proximate care of that patient.
02:02:13 Amy Blum NCHS: A modifier to the CPT code indicating a NP or PA was the provider could be an option.
02:07:05 Randall Stafford: I think that attempts to capture different professional groups misses the point. We need to capture the whole patient experience, not the individual slices provided by different types of providers.
02:08:20 Christine Pintz - George Washington University: Caleb - I also agree and agree with Ryan about other types of providers. With the movement to Patient Centered Medical Homes, there are other providers that are important to patient care - PTs, pharmacists, social workers, nurse care coordinators.
02:37:56 Caleb Alexander - Johns Hopkins: If not [a modified] NAMCS, what ARE the currently available federally supported surveys/studies that are most optimal to assess team-based care?
03:06:04 Bob Phillips, ABFM CPV: UDS Data have been helpful for understanding team constructs and outcomes for FQHCs, but NAMCS should be the source for broader settings. The American Board of Family Medicine has modelled a lot of its cross-sectional annual census of family physicians (~12,000/year) to model NAMCS questions about teams, practice ownership, EHR functionality and have been using that as a lens on the settings and systems where they work.
03:21:10 Randall Stafford, MD, PhD, Stanford University: There is a great need to capture the nuances of "telehealth." No one has fully delved into the different types of communications that are implied by this broad term. Different types of video, telephone, messaging, email, app contact.
03:24:20 Bob Phillips, ABFM CPV: EHR and claims data would potentially capture telehealth since it is typically captured in the course of care in the EHR for billing purposes and submitted with that E&M code or modifier
03:27:59 Caleb Alexander - Johns Hopkins: Here are notes on potential changes for NAMCS to address gaps:
03:28:03 Caleb Alexander - Johns Hopkins: (1) Could induction interview be expanded so as to yield more comprehensive information about important dimensions of care that are currently not well captured (e.g., provision of telehealth, models of team-based care)? (2) Could sample frame be expanded so as to separately sample PAs and NPs? (3) Could definition of visits be broadened so as to allow for capture of telehealth visits that occur for sampled providers during sampled weeks? (4) Could additional modules be planned and anticipated – now – that would occur periodically during the coming decade or two to address some of the shortcomings of the current NAMCS? (5) Can visit form be modified so as to better capture team-based care? (6) Recommendations from our group may be channeled laterally to other federal surveys (MCBS, NCHS, MEPS) (7) Link NAMCS visits to longitudinal patient-level information derived from claims or EMR or both for all or at least a subset of NAMCS participants
03:31:25 Bob Phillips, ABFM CPV: This is the area where I have a conflict in that I run a national primary care registry, but there are multiple Qualified Clinical Data Registries that are typically specialty-specific that pull, clean, and structure data from EHRs for more than 100 million people. They can be an effective bridge to structured EHR data and have additional information about practice size, location, patient demographics, payer mix that would help sampling and data quality.
03:31:33 Caleb Alexander - Johns Hopkins: Great point Ellen re: longevity of NAMCS!
03:35:12 Caleb Alexander - Johns Hopkins: Bob - this could be a great resource - and is one of many sources of real world evidence (RWE) that could potentially be used to enhance the NAMCS - i think the key question is whether the primary sampling approach remains the same, or is modified based on these types of registries
03:41:20 Randall Stafford, MD, PhD, Stanford University: Change the dictionary!
03:42:24 Bob Phillips, ABFM CPV: Caleb, good point, thanks. the sampling could change. I also agree with your notion that cross-validation should be fit for purpose. We may be able to identify a handful of NAMCS items that can be checked in other data that give a sense of NAMCS representativeness vs. drift
03:47:10 Lynn Olson: EHR data has many promises, but overall has proved often challenging to turn into research data. What specific lessons were learned with the use of EHR data for the NAMCS in the 2016-17?
03:50:29 Ellen Kurtzman, former NCHS/AH HP Fellow & GW School of Nursing: urgent care, retail clinics, specialty clinics (e.g., dialysis), telehealth, mobile care, freestanding EDs, and work-based clinics
03:50:32 John Lumpkin BCBSNC Foundation: telemedicine
03:51:25 Ellen Kurtzman, former NCHS/AH HP Fellow & GW School of Nursing: And of course (my earlier pitch) health centers (FQHCs, CHCs, Indian Health)
03:51:35 Brian Ward - NCHS: CHCs or FQHCs have also been mentioned in the comments
03:51:41 Caleb Alexander - Johns Hopkins: Homes!!!
03:51:56 Ann O'Malley, Mathematica: regular old primary care and specialty care offices
03:51:59 Caleb Alexander - Johns Hopkins: Might relabel “Freestanding emergency departments” to “Urgicare Centers” or something like that
03:52:07 Christine Pintz - George Washington University: Health Departments
03:52:29 Ellen Kurtzman, former NCHS/AH HP Fellow & GW School of Nursing: nurse managed health centers
03:52:53 Rajender Aparasu - University of Houston: University Clinics
03:53:02 Christine Pintz - George Washington University: Managed Care Centers
03:53:03 Ellen Kurtzman, former NCHS/AH HP Fellow & GW School of Nursing: student health centers?
03:53:15 Caleb Alexander - Johns Hopkins: I thought the mention at one point of synchronous vs. asynchronous might be helpful to revisit or note - it is not a site, but rather, an important feature regarding mode
03:53:20 Rajender Aparasu - University of Houston: yes
03:53:22 Kennon Copeland: NORC at the University of Chicago: Pharmacy
03:54:13 Christine Pintz - George Washington University: Telephone based Tele-health (for patients who don't have the ability to use computer or phone-based - seniors, those with no internet)
03:55:12 Ryan White - Rutgers University: community-based clinics (i.e. free clinics located in community centers, places of worship, schools)
03:56:13 Randall Stafford, MD, PhD, Stanford University: app-provided care (real person messaging and AI driven care)
03:56:51 Randall Stafford, MD, PhD, Stanford University: home-based monitoring (BP, INR, ECG)
04:01:42 Ellen Kurtzman, former NCHS/AH HP Fellow & GW School of Nursing: Chiropractic care???
04:02:17 Ellen Kurtzman, former NCHS/AH HP Fellow & GW School of Nursing: behavioral health?
04:03:40 Ellen Kurtzman, former NCHS/AH HP Fellow & GW School of Nursing: breast feeding centers??
05:28:43 Caleb Alexander - Johns Hopkins: What was the precise change in MEPS that the RWJF funding enabled?
05:36:27 Caleb Alexander - Johns Hopkins: Joel, you mentioned, analogous to MEPS building upon NCHS, “maybe NAMCS could link to other data” [to increase efficiency or value] - can you please elaborate a bit on what specific data resources you are thinking of, and how such linkage might take place?
05:39:07 Caleb Alexander - Johns Hopkins: Sharon - thank you for your comments. You suggested possibly moving to more locally informative data - do you have thoughts as to how this might be done?
05:52:59 Caleb Alexander - Johns Hopkins: We should discuss bartering to increase participation
06:02:55 Bob Phillips, ABFM CPV: Joel, AHRQ has been brilliant about capturing more and better data for MEPS than its charge would otherwise produce. Very clever about helping make it so useful.
06:05:31 Alek Sripipatana (HRSA): Great idea Bob. Thanks!
06:07:15 Bob Phillips, ABFM CPV: Alek HRSA's data (or CHARN/PCORNet) could also help on the front end with sampling frame so that NAMCS is more nationally representative.
06:09:48 Alek Sripipatana (HRSA): Great point Bob. I think partnering with the HCCNs is also another opportunity to engage a broad spectrum of health centers that are nationally representative of health centers
06:09:52 Caleb Alexander - Johns Hopkins: Telehealth and care by non-physician providers seem to be two of the largest and most manageable pivots for a retooled NAMCS to make
06:10:46 Caleb Alexander - Johns Hopkins: Can someone define what “trust networks” are?
06:15:10 Talisha Searcy, ONC: Trusted Exchange Framework and Common Agreement (TEFCA), outlines a common set of principles, terms, and conditions to support the development of a Common Agreement that would help enable nationwide exchange of electronic health information (EHI) across disparate health information networks (HINs).
06:16:37 Bob Phillips, ABFM CPV: I appreciate Talisha's point and the interoperability goals of ONC, but that is anticipated to be 3-4 years out at best. The American College of Emergency Medicine CEDR registry routinely draws EHR data from more than 1000 emergency rooms, ~28 million visits annually. They have a standardized data model that could feed to NAMCS, produce analyses to guide sample selection, be a supplementary source, offer a check on representativeness. That capacity is available now.
06:16:46 Talisha Searcy, ONC: Currently, about 57% of hospitals share information on a HiN.
06:19:20 Bob Phillips, ABFM CPV: but ERs are often separate from hospital EHR systems. and I don't think CEDR feeds HINs. Other outpatient QCDRs an be a source now of outpatient standardized data, in fact that is why CMS created them.
06:32:22 Ann O'Malley, Mathematica: seems like the survey results that we did at 1:20PM answers the first question
06:33:30 Lucie Dalzell--Census Bureau: Just to note from something said earlier--NHAMCS stopped collecting outpatient departments and ambulatory surgical locations in 2018; it now only includes emergency departments
06:35:38 Bob Phillips, ABFM CPV: Lucy where do hospital outpatient department and amb surg center data get captured? NAMCS?
06:37:25 Lucie Dalzell--Census Bureau: They are not included in NAMCS. OPDs are included in the Hospital Care Survey that NCHS conducts (Census is not involved with that). Not sure about amb surgery
06:37:36 Lucie Dalzell--Census Bureau: and thanks : )
06:43:28 Ann O'Malley, Mathematica: Seems to me that some of the "softer data" is already available from NHIS, CAHPS and BRFSS
06:44:55 Brian Ward - NCHS: There is a CE course related to NAMCS that participants (and anyone interested) can take to get an hour credit towards their certification.
06:44:58 Lucie Dalzell--Census Bureau: Grace--thanks for the great suggestions! We do have certificates of appreciation and they are popular!
06:45:12 Lucie Dalzell--Census Bureau: yes and the CE course is extremely popular!
06:50:37 Carol DeFrances - NCHS: NCHS has developed an HL7 CDA Implementation Guide for the National Health Care Surveys which includes NAMCS. Epic, Cerner, Allscripts and a number of other EHR vendors have developed interfaces in their system to extract NAMCS data. We also working on a FHIR IG.
06:54:52 Eric Miller, NIH: There may be some work the cancer registries (SEER specifically) are doing with abstracting data from EHRs, pharmacy records, and natural language processing from path reports that could be useful/informative for NAMCS
06:55:12 Caleb Alexander - Johns Hopkins: Thanks Eric - that looks like a great lead
07:07:31 Caleb Alexander - Johns Hopkins: Here is a great example of work by Randy Stafford and a colleague examining off-label use through a direct linkage of drugs and diagnoses: https://pubmed.ncbi.nlm.nih.gov/16682577/
07:09:23 Caleb Alexander - Johns Hopkins: Strengths: Comprehensive and clear documentation, ability to look year over year
07:09:55 Ellen Kurtzman, former NCHS/AH HP Fellow & GW School of Nursing: •Number of years and regularity of NAMCS data collection
• Inclusion of patient and provider variables
• Comprehensiveness of the data/variables collected per visit
07:11:36 Ellen Kurtzman, former NCHS/AH HP Fellow & GW School of Nursing: Did the ability to produce state-level estimates get on the short list?
07:13:30 Ryan White - Rutgers University: To echo Ellen's question, state-level estimates are important for policy and workforce analyses.
07:27:38 John Lumpkin BCBSNC Foundation: account for changes in office based care
07:27:50 Ellen Kurtzman, former NCHS/AH HP Fellow & GW School of Nursing: Would hope the redesigned NAMCS could address issues related to the cost, quality, population health, utilization of ambulatory care and its workforce
07:28:32 John Lumpkin BCBSNC Foundation: more operational efficiency-understand reasons for visits - understand characteristics of team base care - s
07:28:53 Ellen Kurtzman, former NCHS/AH HP Fellow & GW School of Nursing: Wondering about social determinants of health ?
07:34:04 Bob Phillips, ABFM CPV: You could use neighborhood social determinants, like ADI, SDI or Massachusett's NSS (being used to adjust Medicaid Payments)--all are shown to be associated with poorer outcomes when high. They could be assigned to the practice service area
07:34:34 Bob Phillips, ABFM CPV: as an estimate of practice patient panel risk
07:35:55 Ellen Kurtzman, former NCHS/AH HP Fellow & GW School of Nursing: Do we care about the capacity and/or composition of the practices/settings surveyed -- for example, # or type of administrative staff or range of services?
07:40:31 Eric Miller, NIH: A little late but just to add to Randy's comments on measuring effective care and chronic disease management. It's very difficult to know the "why" someone isn't receiving effective care. It seems like this could at least be an opportunity to find what care/treatment is recommended or offered from the practice side and the compliance of it from the patient side. There aren't many datasets that have that opportunity
07:42:28 Ann O'Malley, Mathematica: Thank you!
07:42:34 Christine Pintz - George Washington University: Thank you!
07:42:40 Ellen Kurtzman, former NCHS/AH HP Fellow & GW School of Nursing: Thank you very much for the opportunity to participate. Health and safety to everyone!
07:42:52 Sayeedha Uddin--NCHS: Thank you everyone for your participation and engagement!!
07:42:54 Ryan White - Rutgers University: Thank you all very much
07:43:30 Kathy Hempstead: Thank you for including me. It was a very interesting conversation and I look forward to seeing the report.
07:45:32 Brian Ward - NCHS: Thank you everyone - have a good evening!
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | Lucas Smalldon |
| File Modified | 0000-00-00 |
| File Created | 2021-06-02 |
© 2026 OMB.report | Privacy Policy