0920-24EV AppxB-B Performance Measure Guidance
[OADPS] The Performance Measures Project: Improving Performance Measurement and Monitoring by CDC Programs
AppxB-B Performance Measure Guidance
[OADPS] [PMP] A Strategic Approach to Advancing Health Equity for Priority Populations with or at Risk for Diabetes.
OMB: 0920-1282
Appendix B: Component B: OPPE-NCCDPHP-DDT-Component B Performance Measure Guidance-PS23-0020-new-2024-2026-04-15-2024
Form Approved |
OMB Control Number: 0920-1282 |
Expiration Date: 06/30/2026 |
DP23-0020: A Strategic Approach to Advancing Health Equity for Priority Populations with or at Risk for Diabetes (2320)
Centers for Disease Control and Prevention
Component B
Performance Measure Definitions Guidance
February 2024
Public reporting burden of this collection of information is estimated to average 8 hours per response per year, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. An agency may not conduct or sponsor, and a person is not required to respond to a collection of information unless it displays a currently valid OMB control number. Send comments regarding this burden estimate or any other aspect of this collection of information, including suggestions for reducing this burden to CDC/ATSDR Reports Clearance Officer; 1600 Clifton Road NE, MS D-74, Atlanta, Georgia 30333; Attn: OMB-PRA (0920-1282).
Table of Contents
Organization of this Document 5
Selection of Performance Measures 5
Strategies and Performance Measures 5
2320 Performance Measure Reporting 9
0
Measure B. 1.2………………………………………………………………………………………………………………………………….12
Measure B.1.3…………………………………………………………………………………………………………………………………..14
Measure B.1.a………………………………………………………………………………………………………..…………………………16
Measure B.1.b…………………………………………………………………………………………………………………………………..18
Measure B.4.a……………………………………………………………………………………………………………………………………33
Measure B.8.1……………………………………………………………………………………………………………………………………48
Measure 15.1…………………………………………………………………………………………………………………………………….86
Strategy 1 Resources……………………………………………………………………………………………………………………………..89
Purpose of this Document
The purpose of this document is to provide guidance on reporting performance measures for the Centers for Disease Control and Prevention (CDC) Notice of Funding Opportunity (NOFO) DP23-0020. Performance measurement is a critical component of CDC’s strategy for monitoring and evaluating both program and recipient performance. The performance measures monitor progress towards short-term, intermediate, and long-term outcomes as a result of recipient efforts to implement evidence-based diabetes management and type 2 diabetes prevention and risk mitigation strategies. All recipients are required to collect and report on performance measures annually to clarify and describe what is occurring as a result of the implementation of NOFO strategies.
Performance measures in this document are organized by DP23-0020 Component B.
General Guidance
Selection of Performance Measures
All DP23-2320 recipients must document progress for all performance measures associated with DP23-2320 strategies in their workplan. Each performance measure profile in this document lists the related strategies. Component B will report on all short-term, intermediate, and long-term performance measures. CDC will monitor and evaluate the following short-term, intermediate, and long-term performance measures 1.a, 5.1, 5.a, 10.a, 10.b, 14, 15. However, recipients may be required to provide contextual information for these performance measures in the progress and measure notes. Recipients should review the performance measure profiles for additional reporting guidance on what to measure, how to set targets, etc.
Strategies and Performance Measures
Some performance measures may have more than one related strategy listed in the profiles. The AMP system will label the performance measure to help you identify which performance measure to choose depending on the strategy. Use the table below to confirm the appropriate performance measures associated with each strategy.
Component B Strategies and Performance Measures
2320 Performance Measure Reporting
Reporting Period
Unless otherwise indicated in the performance measure profile, the reporting period for performance measures is the DP23-0020 performance period. Recipients will report on performance measures 90 days after the close of each budget period.
Baseline Data Collection
Baseline data are considered the initial data collected at the start of the program. These data serve as a point of reference (comparison) in which program goals can be measured over the course of the 5-year funding period. Recipients are expected to submit baseline data, Year 2 target values, and Year 5 target values on Monday, April 1, 2024, as part of the Evaluation and Performance Measurement Plan (EPMP). For the April 1st EPMP deliverable, baseline data for performance measures that are new and “as a result of work supported by DP23-0020” should be reported as zero. Baseline data can be updated until Year 2, September 30, 2024, of the cooperative agreement. Baseline data can be updated up to Year 2 evaluation reporting period, Monday, September 30, 2024.
Performance Measure Targets
Target values for subsequent years will then be submitted annually as part of the continuation application process. Recipients should work closely with their evaluator and project officer to identify a feasible and achievable target. Recipients are asked to submit their performance measure data 90 days after the end of each performance period in the Annual Performance Report.
Net new and Cumulative Values
Net new performance measure data is defined as the individual’s program year data and should only be reported Year 1, 2, 3, and 4 actuals.
Cumulative performance measure data reflects the cumulative progress over the cooperative agreement years (1-5). This will only be reported for Year 5 target and actual values.
Questions or Technical Assistance Needs
Any questions about the guidance included in this document should be directed to the evaluator and project officer assigned to your state/organization. All questions should be submitted through the AMP system. Communicate any challenges with data collection to CDC. CDC understands that collecting some of this data may be challenging and time-consuming. CDC will make an effort to be flexible and accommodate the specific circumstances of the recipient where appropriate.
2320 Performance Measure Definitions
The purpose of the performance measure definitions is to assist recipients with submitting all required components on the Annual Performance Report. The performance measure definitions operationalize each measure as a tool for planning and reporting. There is a definition for each performance measure that includes a detailed set of required reporting components and additional information and guidance.
The Values to be Reported section comprises the following:
Progress notes;
Numerator definition;
Denominator definition (if applicable);
Proportion definition (if applicable);
Measure elements;
Date data collected;
Measure notes; and
Other attachments (if applicable).
Note that recipients will report information for the areas highlighted in BLUE* in alignment with the annual reporting template. Review the Additional Information and Guidance section for helpful hints, data source recommendations, unit of analysis, result statement(s), definitions of key terms, and resources associated with each measure.
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.1 |
Strengthen self-care practices by improving access, appropriateness, and feasibility of diabetes self-management education and support (DSMES) services for priority populations |
Measure B.1.1 |
Number of new ADA-recognized or ADCES-accredited DSMES services established during the reporting period as a result of the recipient’s work under 2320. |
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress toward increasing access to American Diabetes Association (ADA)-recognized and Association of Diabetes Care and Education Specialists (ADCES)-accredited DSMES services among priority populations with diabetes.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
Number of new ADA-recognized or ADCES-accredited services established during the reporting period as a result of work supported by DP23-0020 |
Denominator Definition* |
Not Applicable. |
Proportion Definition* |
Not Applicable. |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable. |
Additional Information and Guidance |
|
Helpful Hints
|
In the “Measure Notes,” describe any additional information that provides context for the values reported.
How to report this measure:
Note: Recipients can count both new programs and new delivery sites as a result of work supported by DP23-0020. |
Data Source(s) |
Program records: Recipients will track this information and report to CDC. |
Unit of Analysis |
ADA-recognized or ADCES-accredited DSMES programs
|
Result Statement(s) |
In the US, CDC-funded recipients worked to increase the number of new ADA-recognized and ADCES-accredited DSMES programs established from # (baseline) to # (reporting period). This represents an increase of ___% over the funding period. |
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.1 |
Strengthen self-care practices by improving access, appropriateness, and feasibility of diabetes self-management education and support (DSMES) services for priority populations |
Measure B.1.2 |
Number of new diabetes support programs or services established during the reporting period as a result of the recipient's work under 2320 |
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient efforts to increase the number of new diabetes support programs or services in areas of the state with limited or no support programs, including geographical areas with priority populations.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
Number of new diabetes support programs or services established during the reporting period as a result of work supported by DP23-0020 |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints
|
In the “Measure Notes,” describe any additional information that provides context for the values reported and underserved areas in which you are working.
How to report values for this measure:
|
Data Source(s) |
Program records: Recipients will track this information and report to CDC. |
Unit of Analysis |
Diabetes support programs/services |
Result Statement(s) |
In the US, CDC-funded recipients worked to increase the number of new diabetes support programs or services established from # (baseline) to # (reporting period) . This represents an increase of ___% over the funding period. |
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.1 |
Strengthen self-care practices by improving access, appropriateness, and feasibility of diabetes self-management education and support (DSMES) services for priority populations |
Measure B.1.3
|
Number of existing ADA-recognized or ADCES-accredited DSMES services and diabetes support programs that have tailored their programs or recruitment strategies to increase participation of priority populations. |
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress towards increasing participation in existing American Diabetes Association (ADA)-recognized and Association of Diabetes Care and Education Specialists (ADCES)-accredited DSMES services and diabetes support programs that have tailored their programs or recruitment strategies among priority populations with diabetes.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
Number of existing ADA-recognized or ADCES-accredited DSMES services that have tailored their programs or recruitment strategies to increase participation of priority populations for the reporting period as a result of work supported by DP23-0020.
Number of diabetes support programs that have tailored their programs or recruitment strategies to increase participation of priority populations for the reporting period as a result of work supported by DP23-0020. |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints
|
In the “Measure Notes,” describe any additional information that provides context for the values reported.
How to report this measure:
Note: Delivering DSMES services in a pharmacy setting would not meet the definition of “tailoring.” |
Data Source(s) |
Program records: Recipients will track this information and report to CDC. |
Unit of Analysis |
|
Result Statement(s) |
In the US, CDC-funded recipients worked to increase the number of existing ADA-recognized or ADCES-accredited DSMES services that have tailored their programs or recruitment strategies to increase participation of priority populations from # (baseline) to # (reporting period) . This represents an increase of ___% over the funding period.
In the US, CDC-funded recipients worked to increase the number of existing diabetes support programs that have tailored their programs or recruitment strategies to increase participation of priority populations from # (baseline) to # (reporting period). This represents an increase of ___% over the funding period. |
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.1 |
Strengthen self-care practices by improving access, appropriateness, and feasibility of diabetes self-management education and support (DSMES) services for priority populations |
Measure B.1.a |
Number of people with diabetes (total number and number from priority populations) participating in recognized/accredited DSMES services |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress towards increasing access and participation in American Diabetes Association (ADA)-recognized or Association of Diabetes Care and Education Specialists (ADCES)-accredited DSMES programs in areas of high need counties with limited access to DSMES programs, including areas with large priority populations.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
None. Recipients are not required to report data for this measure. This measure will be monitored and reported by CDC. |
CDC-Reported Data (INTERNAL) |
Total number of people with diabetes participating in recognized/accredited DSMES services for the reporting period Number of people with diabetes from priority populations participating in recognized/accredited DSMES services for the reporting period |
Denominator Definition* |
Not Applicable. |
Proportion Definition* |
Not Applicable. |
Measure Elements |
Not Applicable |
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
|
Progress Notes* |
The progress notes should include the following for this measure:
Any additional notes that are applicable to the progress |
Other Attachments* |
Not applicable |
Additional Information and Guidance |
|
Helpful Hints
|
In the “Measure Notes,” describe any additional information that provides context for the values reported.
|
Data Source(s) |
CDC – ADA/ADCES DSMES State Report |
Unit of Analysis |
People with diabetes |
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.1 |
Strengthen self-care practices by improving access, appropriateness, and feasibility of diabetes self-management education and support (DSMES) services for priority populations |
Measure B.1.b |
Number of people with diabetes (total number and number from priority populations) participating in diabetes support programs/services |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress towards increasing participation of people with diabetes in diabetes support programs/services, including areas with priority populations.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
Total number of people with diabetes participating in diabetes support programs/services as a result of work supported by DP23-0020
Number of people with diabetes from priority populations participating in diabetes support programs/services as a result of work supported by DP23-0020
Note: Required to collect and report both values |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* (Narrative) |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not applicable. |
Additional Information and Guidance |
|
Helpful Hints
|
In the “Measure Notes”, describe any additional information that provides context for the values reported.
How to report values for this measure:
|
Data Source(s) |
Program records: Recipients will track this information and report to CDC. |
Unit of Analysis |
People with diabetes |
Result Statement(s) |
In the US, CDC-funded recipients worked to increase the number of people with diabetes participating in diabetes support programs/services from # (baseline) to # (reporting period). This represents an increase of ___% over the funding period.
In the US, CDC-funded recipients worked to increase the number of people with diabetes from priority populations participating in diabetes support programs/services from #(baseline) to # (reporting period). This represents an increase of ___% over the funding period. |
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.2 |
Expand availability of ADA-recognized and ADCES-accredited DSMES services as a covered health benefit for Medicaid beneficiaries and employees with diabetes |
Measure B.2.2 |
Number of employers working to establish new health benefit coverage DSMES or strengthen existing coverage |
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient’s progress towards establishing new or strengthening existing employer coverage of ADA-recognized and ADCES-accredited DSMES services to increase access and availability of these services for people with diabetes.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
|
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes,” describe any additional information that provides context for the values reported and areas in which you are working.
How to report values for this measure:
|
Data Source(s) |
Program records: Recipients will track this information and report to CDC. |
Unit of Analysis |
|
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.2 |
Expand availability of ADA-recognized and ADCES-accredited DSMES services as a covered health benefit for Medicaid beneficiaries and employees with diabetes |
Measure B.2.a |
Number of state Medicaid beneficiaries and/or employees covered |
Measure Type
|
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure
|
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress towards increasing the number of people with diabetes who have DSMES as a covered benefit through Medicaid and/or employers to expand the availability and accessibility of these services.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
|
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes,” describe any additional information that provides context for the values reported and underserved areas in which you are working.
How to report values for this measure:
|
Data Source(s) |
|
Unit of Analysis |
People with diabetes who have DSMES as a covered benefit |
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.3 |
Prevent diabetes complications for priority populations through early detection |
Measure B.3.1 |
Number of health care organizations working with the recipient to a) increase diabetic retinopathy screening and b) improve early detection of chronic kidney disease (CKD) in priority populations with diabetes |
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient efforts to increase the number of health care organizations that are working to screen for diabetic retinopathy (DR) and to improve early detection of chronic kidney disease (CKD) in people with diabetes (PWD) among priority populations.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
i) Number of health care organizations working with the recipient to increase diabetic retinopathy screening in priority populations with diabetes during the reporting period as a result of DP23-0020 work. ii) Number of health care organizations working with the recipient to improve early detection of CKD in priority populations with diabetes during the reporting period as a result of DP23-0020 work. |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes,” describe any additional information that provides context for the values reported.
How to report values for this measure:
Note: These measures were intended to align with the following HEDIS measures:
|
Data Source(s) |
Program records: Recipients will track this information and report to CDC.
|
Unit of Analysis |
Health care organizations |
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.3 |
Prevent diabetes complications for priority populations through early detection |
Measure B.3.a |
Number and percentage of patients with diabetes screened for diabetic retinopathy and chronic kidney disease (CKD) in health care organizations working with the recipient on this strategy |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress towards increasing the number and percentage of patients with diabetes who have been screened for diabetic retinopathy and CKD in the health care organizations identified in measure B.3.1.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
|
Denominator Definition*
|
|
Proportion Definition*
|
i) Number of patients with diabetes who have received diabetic retinopathy screening in the health care organizations identified in B.3.1 divided by the number of adults with diagnosed diabetes with a medical visit during the measurement year ii) Number of patients with diabetes who have received CKD screening in the health care organizations identified in B.3.1. divided by the number of adults with diagnosed diabetes with a medical visit during the measurement year |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes,” describe any additional information that provides context for the values reported.
How to report values for this measure:
Note: These measures were intended to align with the following HEDIS measures:
|
Data Source(s) |
Program records: Recipients will track this information and report to CDC. |
Unit of Analysis |
Patients with diabetes |
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.4 |
Improve acceptability and quality of care for priority populations with diabetes |
Measure B.4.1 |
Number of health care organizations that have adopted or enhanced a) team-based care supported by sustainable payment models and b) clinical systems and care practices to improve health outcomes for people with diabetes |
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress towards increasing the number of health care organizations adopting or enhancing team-based care supported by sustainable payment models and clinical systems and care practices to improve health outcomes for people with diabetes.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
|
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes,” describe any additional information that provides context for the values reported.
How to report values:
Note: Sustainable payment models should align with the intent of the strategy, which is to ensure sustainable financing/payment for services rendered by all members of the diabetes care team—including individuals such as pharmacists, community health workers, and others who may not be reimbursed through traditional claims-based payment mechanisms. The goal is to help ensure the team is able to function long-term. |
Data Source(s) |
Program records: Recipients will track this information and report to CDC. |
Unit of Analysis |
Health care organizations |
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.4 |
Improve acceptability and quality of care for priority populations with diabetes |
Measure B.4.a |
Number of people with diabetes served by health care organizations that have adopted or enhanced a) team-based care supported by sustainable payment models and b) clinical systems and care practices to improve health outcomes for people with diabetes |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress toward increasing the number of people with diabetes served by health care organizations that have adopted or enhanced a) team-based care supported by sustainable payment models and b) clinical systems and care practices to improve their health outcomes.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
|
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes*
|
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints
|
In the “Measure Notes,” describe any additional information that provides context for the values reported and underserved areas in which you are working.
How to report values for this measure:
Note: Sustainable payment models should align with the intent of the strategy, which is to ensure sustainable financing/payment for services rendered by all members of the diabetes care team—including individuals such as pharmacists, community health workers, and others who may not be reimbursed through traditional claims-based payment mechanisms. The goal is to help ensure the team is able to function long-term. |
Data Source(s) |
Program records: Recipients will track this information and report to CDC. |
Unit of Analysis
|
|
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.5 |
Increase enrollment and retention of priority populations in the National Diabetes Prevention Program (National DPP) lifestyle intervention and the Medicare Diabetes Prevention Program (MDPP) by improving access, appropriateness, and feasibility of the programs |
Measure B.5.1 |
Number of participants (total number and number from priority populations) enrolled by CDC-recognized National DPP delivery organizations |
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose
|
The purpose of this performance measure is to monitor recipient’s work towards increasing the number of participants enrolled in CDC-recognized National DPP delivery organization among the priority populations.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
None. Recipients are not required to report data for this measure. This measure will be monitored and reported by CDC. |
CDC-Reported Data (INTERNAL) |
Total number of participants enrolled in CDC-recognized National DPP delivery organizations
Number of participants from priority populations enrolled in CDC-recognized National DPP delivery organizations |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
Not Applicable |
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes*
|
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes*
|
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints
|
In the “Measure Notes,” describe any additional information that provides context for the values reported and underserved areas in which you are working. |
Data Source(s)
|
|
Unit of Analysis
|
|
Result Statement(s)
|
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.5 |
Increase enrollment and retention of priority populations in the National Diabetes Prevention Program (National DPP) lifestyle intervention and the MDPP by improving access, appropriateness, and feasibility of the programs |
Measure B.5.a |
Number of participants (total number and number from priority populations) retained* by CDC-recognized National DPP delivery organizations |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor progress toward increasing the number of participants (in general and from priority populations) retained* in CDC-recognized National DPP delivery organizations.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP.
*Based on CDC’s Diabetes Prevention Recognition Program (DPRP) Standards, participants who are retained in the National DPP lifestyle intervention (i.e., program completers) are defined as those who attended 8+ sessions in the first six months and whose total time in the program is 9 or more full months. |
VALUES TO BE REPORTED |
|
Numerator Definition* |
None. Recipients are not required to report data for this measure. This measure will be monitored and reported by CDC. |
CDC-Reported Data (INTERNAL) |
Total number of participants retained* by CDC-recognized National DPP delivery organizations.
Number of participants from priority populations retained* by CDC-recognized National DPP delivery organizations |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
Not Applicable. |
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes*
|
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes,” describe any additional information that provides context for the values reported and underserved areas in which you are working. |
Data Source(s) |
|
Unit of Analysis |
|
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.6 |
Expand availability of the National DPP lifestyle intervention as a covered health benefit for Medicaid beneficiaries and/or employees and covered dependents at high risk for type 2 diabetes |
Measure B.6.2
|
Number of employers working to establish new health benefit coverage for the National DPP lifestyle intervention or strengthen existing coverage |
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient efforts to expand the availability of the National Diabetes Prevention Program (National DPP) lifestyle change program (LCP) as a covered health benefit for Medicaid beneficiaries and/or employees and covered dependents who are at high risk for type 2 diabetes.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
Number of employers (private or public) working to establish new health benefit coverage for the National DPP-LCP or strengthen existing coverage as a result of the work supported by DP23-0020 |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes*
|
The progress notes should include the following for this measure:
|
Other Attachments* |
Not applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes”, describe any additional information that provides context for the values reported and underserved areas in which you are working.
How to report values for this measure:
|
Data Source(s) |
Program records: Recipient will track this information and report to CDC. |
Unit of Analysis |
|
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.6 |
Expand availability of the National Diabetes Prevention Program (National DPP) lifestyle intervention as a covered health benefit for Medicaid beneficiaries and/or employees at high risk for type 2 diabetes |
Measure B.6.a |
Number of Medicaid beneficiaries and/or employees covered |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress towards increasing the number of Medicaid beneficiaries and/or employees with covered benefits at high risk for type 2 diabetes for the National DPP lifestyle change intervention.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP. |
VALUES TO BE REPORTED |
|
Numerator Definition* |
|
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable. |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes”, describe any additional information that provides context for the values reported, Medicaid beneficiaries covered, and employees and dependents covered.
How to report values for this measure:
Note: Capture the number of Medicaid beneficiaries and/or employees who have access to coverage. If eligible dependents are covered, they can be included in the total – Include a note to this effect in the notes section. You can include employees for both public and private employers, but please note the names of the employers in the notes section. |
Data Source(s) |
|
Unit of Analysis |
|
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.7 |
Improve sustainability of CDC-recognized National DPP delivery organizations serving priority populations by establishing or expanding National DPP Umbrella Hub Arrangements |
Measure B.7.1 |
Number of program participants enrolled in CDC-recognized National DPP delivery organizations participating in Umbrella Hub Arrangements |
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of the performance measure is to monitor recipients’ progress toward increasing the number of program participants enrolled in CDC-recognized National Diabetes Prevention Program (National DPP) delivery organizations participating in Umbrella Hub Arrangements as a result of work done under DP23-0020.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
Total number of program participants enrolled in CDC-recognized National DPP delivery organizations participating in Umbrella Hub Arrangements |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: For a list of type of organization see “orgtype” for DPRP
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period.
|
Progress Notes*
|
The progress notes should include the following for this measure:
|
Other Attachments* |
Not applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes”, describe any additional information that provides context for the values reported.
How to report values for this measure:
Note: The type of delivery organization would be the org type based on DPRP options. |
Data Source(s) |
Program records: Recipients will track this information and report to CDC. |
Unit of Analysis |
Participants enrolled |
Result Statement(s) |
In the US, CDC-funded recipients worked to increase the number of program participants enrolled in CDC-recognized National DPP delivery organizations participating in Umbrella Hub Arrangements from # (baseline) to # (reporting period). This represents an increase of ___% over the funding period. |
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.7 |
Improve sustainability of CDC-recognized National DPP delivery organizations serving priority populations by establishing or expanding National DPP Umbrella Hub Arrangements. |
Measure B.7.a |
Number of program participants enrolled by CDC-recognized National DPP delivery organizations participating in Umbrella Hub Arrangements for whom claims are submitted to payers. |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure
Note: PM B.7.1 is the short term measure that is conducive to this measure, A.7.a. Review information to ensure alignment. |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of the performance measure is to monitor recipient progress towards increasing the number of participants enrolled in the National Diabetes Prevention Program (National DPP-LCP).
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP. |
VALUES TO BE REPORTED |
|
Numerator Definition |
Number of program participants enrolled in CDC-recognized National DPP delivery organizations participating in Umbrella Hub Arrangements for whom claims are submitted to payers. |
Denominator Definition |
Not Applicable |
Proportion Definition |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected |
Provide the date these data were collected. |
Measure Notes |
The measure notes should include the following for this measure:
|
Progress Notes |
The progress notes should include the following for this measure:
|
Other Attachments |
Not applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes”, describe any additional information that provides context for the values reported and areas in which you are working.
How to report values for this measure:
|
Data Source(s) |
Program records: Recipients will track this information and report to CDC. |
Unit of Analysis |
Participants enrolled |
Result Statement(s) |
In the US, CDC-funded recipients worked to increase the number of program participants enrolled in CDC-recognized National DPP delivery organizations participating in Umbrella Hub Arrangements for whom claims are submitted to payers from # (baseline) to # (reporting period). This represents an increase of ___% over the funding period. |
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.8 |
Implement, spread, and sustain one of the following evidence-based, family-centered childhood obesity interventions (Family Healthy Weight Programs, FHWPs): |
Measure B.8.1 |
# of sites newly implementing family health weight programs (FHWPs) in the community. |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of measure A.8.1 is to monitor the funded recipient’s efforts to increase the number of new sites where an evidence-based FHWP is being implemented to increase FHWP access and availability for priority populations. Focusing on the number of sites aims to concentrate the strategy on enhancing access and availability of these programs. A family healthy weight program is a comprehensive, family-based lifestyle change program to help children with overweight or obesity make progress toward a healthier weight through positive behavior changes. Several national organizations, including the US Preventive Services Task Force (USPSTF), the American Academy of Pediatrics (AAP), and the American Psychological Association, recommend family healthy weight programs to help treat childhood obesity. For example, AAP’s Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents with Obesity recommends that clinicians refer children 2 to 18 years old with overweight or obesity to family-based multicomponent behavioral interventions with a minimum of 26 contact hours. Despite these recommendations, most US children in need have not been able to access a family healthy weight program due to issues related to low program availability, high costs due to little or no insurance coverage, and the societal or cultural bias and stigma associated with weight. During the community assessment stage, recipients should identify and prioritize the populations in highest need of this intervention. To address the health disparities among priority populations, the purpose of this strategy is to reduce the many structural and psychosocial barriers that impact access to these programs. Barriers to participation include program cost and availability, no insurance coverage, school and work conflicts, transportation, childcare and other family obligations, in addition to the stigma and cultural attitudes attached to health care and weight. Barriers to implementation include cost, and insurance reimbursement, limited qualified staff, low funding, lack of space. In all stages of the intervention, the funding recipient should address the most common barriers impacting access to FHWPs that are relevant to that community setting. |
VALUES TO BE REPORTED |
|
Numerator Definition* |
B.8.1 # of sites newly implementing a FHWP in the community. |
Denominator Definition* |
Not applicable |
Proportion Definition* |
Not applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
The date of scheduled first implementation cohort |
Measure Notes* |
The measure notes should include the following:
|
Progress Notes* |
The progress notes should include the following:
|
Other Attachments* |
Not applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes”, describe any additional information that provides context for the values reported and underserved areas in which you are working. How to report values for this measure:
|
Data Source(s) |
Program records: Information will come from the implementation partner. This information will be summarized for each FHWP site during the reporting period. Funded recipients will obtain summary counts from the implementation partner and report them to CDC. |
Unit of Analysis |
Number of sites newly implementing FHWPs in the community. |
Result Statement(s) |
In the U.S., CDC-funded recipients worked to increase the number sites offering FHWPs to reduce childhood obesity with an increase from # (baseline) to # (reporting period). This represents a __% increase over the funding period. |
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.8
|
Implement, spread, and sustain one of the following evidence-based, family-centered childhood obesity interventions (Family Healthy Weight Programs, FHWPs): |
Measure B.8.2 |
Number of children for whom the family healthy weight program implementing partner received a referral (total number) |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose measure A.8.b is to monitor the recipients and implementing partners efforts related to engagement of priority populations through recruitment and referral strategies, reduce barriers to participation, and where feasible, increase the number of eligible participants who have been reached and referred to the program. A family healthy weight program is a comprehensive, family-based lifestyle change program to help children with overweight or obesity make progress toward a healthier weight through positive behavior changes. Several national organizations, including the US Preventive Services Task Force (USPSTF), the American Academy of Pediatrics (AAP), and the American Psychological Association, recommend family healthy weight programs to help treat childhood obesity. For example, AAP’s Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents with Obesity recommends that clinicians refer children 2 to 18 years old with overweight or obesity to family-based multicomponent behavioral interventions with a minimum of 26 contact hours. Despite these recommendations, most US children in need have not been able to access a family healthy weight program due to issues related to low program availability, high costs due to little or no insurance coverage, and the societal or cultural bias and stigma associated with weight. During the community assessment stage, recipients should identify and prioritize the populations in highest need of this intervention. To address the health disparities among priority populations, the purpose of this strategy is to reduce the many structural and psychosocial barriers that impact access to these programs. Barriers to participation include program cost and availability, no insurance coverage, school and work conflicts, transportation, childcare and other family obligations, in addition to the stigma and cultural attitudes attached to health care and weight. Barriers to implementation include cost, and insurance reimbursement, limited qualified staff, low funding, lack of space. In all stages of the intervention, the funding recipient should address the most common barriers impacting access to FHWPs that are relevant to that community setting. |
VALUES TO BE REPORTED |
|
Numerator Definition |
B.8.2 Number of children for whom the FHWP implementing partner received a referral. |
Denominator Definition |
Not Applicable |
Proportion Definition |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected |
Date(s) of referral receipt by FHWP implementing partner |
Measure Notes |
The measure notes should include the following:
If available, include the following:
|
Progress Notes |
The progress notes should include the following for this measure:
|
Other Attachments |
Not applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes”, describe any additional information that provides context for the values reported and areas in which you are working. How to report values for this measure:
|
Data Source(s) |
Program records: The source of the data is from the implementing partner. Funded recipients will obtain cumulative counts of referrals per site from the implementing partner and report them to CDC. All personal information needs to be aggregated and deidentified. |
Unit of Analysis |
Number of children for whom the FHWP implementing partner received a referral |
Result Statement(s) |
In the U.S., CDC-funded recipients will work to increase the number of children referred to a FHWP from # (baseline) to # (reporting period). This represents a __% increase over the funding period. |
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.9 |
Increase and sustain diabetes self-management education and support (DSMES) and National Diabetes Prevention Program (National DPP) delivery sites within pharmacy networks and chain pharmacies to improve reach to priority populations |
Measure B.9.1 |
Number of pharmacies and pharmacists offering DSMES services to priority populations |
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress towards increasing and sustaining pharmacy based DSMES delivery sites by working with pharmacy networks (e.g., Community Pharmacy Enhanced Services Networks [CPESNs], state pharmacy associations, etc.) and chain pharmacies to improve reach to priority populations as well as increasing the number of pharmacists who offer DSMES services to priority populations.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
Number of pharmacies offering DSMES services to priority populations as a result of DP23-0020 work |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
Number of pharmacies Type of pharmacy (e.g. network, chain) Description of DSMES services
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
If the recipient executed an agreement to implement patient care processes with the pharmacy reported for this measure. Please attach a copy of that agreement. Note: Remember to remove any personal/unique identifiers from the agreement before attaching it to the report. |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes,” describe any additional information that provides context for the values reported and underserved areas in which you are working.
How to report values for this measure:
|
Data Source(s) |
Program Records: Recipients will track this information and report to CDC. |
Unit of Analysis |
Pharmacy Locations and Pharmacists |
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.9 |
Increase and sustain diabetes self-management education and support (DSMES) and National Diabetes Prevention Program (National DPP) delivery sites within pharmacy networks and chain pharmacies to improve reach to priority populations.
|
Measure B.9.2 |
Number of pharmacies delivering the National DPP lifestyle change program (LCP) for priority populations |
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress towards increasing and sustaining pharmacy-based National DPP LCP delivery sites by working with pharmacy networks (e.g., Community Pharmacy Enhanced Services Networks [CPESNs], state pharmacy associations, etc.) and chain pharmacies to improve reach to priority populations.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
Number of pharmacies delivering the National DPP lifestyle intervention to priority populations as a result of work supported by DP23-0020 . |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Any additional information that provides context for the values reported. Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes,” describe any additional information that provides context for the values reported and underserved areas in which you are working.
How to report values for this measure:
|
Data Source(s) |
Program Records: Recipients will track this information and report to CDC. |
Unit of Analysis |
Pharmacy Locations |
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.9 |
Increase and sustain DSMES and National DPP delivery sites within pharmacy networks and chain pharmacies to improve reach to priority populations |
Measure B.9.a |
Number of pharmacy locations offering DSMES services that operate within a billing-capable network |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress towards increasing the number of pharmacies delivering DSMES services that operate within a billing-capable network.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP
Note: A network is 2 or more pharmacies working together to support one another in offering and sustaining DSMES and/or National DPP within their separate pharmacy locations (i.e. sharing billing, reporting, marketing, resources (materials, coaches, etc.)) to improve sustainability and infrastructure. The network is capable of working collaboratively to share resources and pursue reimbursement for diabetes-related services with various payors such as Medicare, Medicaid, and private/commercial payors. The networks are not managed by Medicaid as not all state Medicaid support DSMES and National DPP. |
VALUES TO BE REPORTED |
|
Numerator Definition* |
Number of pharmacy locations offering DSMES services that operate within a billing capable network as a result of DP23-0020 work.
|
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
If the recipient executed an agreement to implement patient care processes with the pharmacy or pharmacist reported for this measure, please attach a copy of that agreement. |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes”, describe any additional information that provides context for the values reported and underserved areas in which you are working.
How to report values for this measure:
Note: A network is 2 or more pharmacies working together to support one another in sustaining DSMES and/or National DPP i.e., sharing billing, reporting, marketing, resources (materials, coaches, etc.) to improve sustainability and infrastructure. The networks are not managed by Medicaid as not all state Medicaid support DSMES and National DPP. Note: Billing-capable means they have become credentialed by the payor to submit eligible claims for reimbursement i.e., approved MDPP supplier organization. |
Data Source(s) |
Program records: Recipients will track this information and report to CDC.
|
Unit of Analysis |
Pharmacy Locations |
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.9 |
Increase and sustain DSMES and National DPP delivery sites within pharmacy networks and chain pharmacies to improve reach to priority populations |
Measure B.9.b
|
Number of pharmacy locations delivering the National DPP lifestyle intervention that operate within a billing-capable network.
|
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient’s progress towards increasing the number of pharmacies that deliver the National DPP lifestyle intervention within a billing-capable network.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
Number of pharmacy locations delivering the National DPP lifestyle intervention operating in a billing-capable network as a result of DP23-0020 work.
|
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
If the recipient executed an agreement to implement patient care processes with the pharmacy or pharmacist reported for this measure, please attach a copy of that agreement. |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes,” describe any additional information that provides context for the values reported and underserved areas in which you are working.
Note: A pharmacy billing-capable network is a group of 2 or more pharmacies that work together to offer and support National DPP and/or DSMES services within their separate pharmacy locations. The network is capable of working collaboratively to share resources and pursue reimbursement for diabetes-related services with various payors such as Medicare, Medicaid, and private/commercial payors Note: The desire is that the “network” will work together to pursue billing opportunities through Medicaid, Medicare, Private, and/or commercial payors for these services.
|
Data Source(s) |
Program records: Recipients will track this information and report to CDC.
|
Unit of Analysis |
Pharmacies
|
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.9 |
Increase and sustain DSMES and National DPP delivery sites within pharmacy networks and chain pharmacies to improve reach to priority populations |
Measure B.9.c
|
Number of pharmacy locations delivering DSMES services that are receiving patient referrals from health care organizations for individuals with or at risk for diabetes through a bi-directional e-referral system |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress towards increasing the number of pharmacies offering DSMES services that are capable of receiving patient referrals from health care organizations for individuals with or at risk for diabetes through a bidirectional e-referral system.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP
|
VALUES TO BE REPORTED |
|
Numerator Definition* |
Number of pharmacy locations delivering DSMES services that are receiving referrals from health care organizations for individuals with diabetes through a at risk for diabetes through a bi-directional e-referral system as a result of DP23-0020 work.
|
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes,” describe any additional information that provides context for the values reported.
How to report values for this measure:
|
Data Source(s) |
Program records
|
Unit of Analysis |
Pharmacy Locations and billing-capable networks |
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
||
Strategy B.9 |
Increase and sustain DSMES and National DPP delivery sites within pharmacy networks and chain pharmacies to improve reach to priority populations |
|
Measure B.9.d
|
Number of pharmacy locations delivering the National DPP lifestyle intervention that are receiving patient referrals from health care organizations for individuals with or at risk for diabetes through a bi-directional e-referral system.
|
|
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
|
AREAS |
DESCRIPTIONS |
|
Purpose |
The purpose of this performance measure is to monitor recipient progress towards increasing the number of pharmacies who deliver the National DPP lifestyle intervention that are receiving referrals from health care organizations for individuals with or at risk for diabetes through a bi-directional e-referral system.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
|
VALUES TO BE REPORTED |
||
Numerator Definition* |
Number of pharmacy locations delivering the National DPP intervention that are receiving referrals from health care organizations for individuals with or at risk for diabetes through a bi-directional e-referral system as a result of DP23-0020 work |
|
Denominator Definition* |
Not Applicable |
|
Proportion Definition* |
Not Applicable |
|
Measure Elements |
The following elements will be submitted as part of the measure:
|
|
Date Data Collected* |
Provide the date these data were collected. |
|
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
|
Progress Notes* |
The progress notes should include the following for this measure:
|
|
Other Attachments* |
Not Applicable |
|
Additional Information and Guidance |
||
Helpful Hints |
In the “Measure Notes,” describe any additional information that provides context for the values reported.
How to report values for this measure:
|
|
Data Source(s) |
Program records: Recipient will track this information and report to CDC
|
|
Unit of Analysis |
Pharmacies |
|
Result Statement(s) |
In the U.S., CDC-funded recipients worked to increase the number of pharmacy locations delivering the National DPP lifestyle intervention that are receiving patient referrals from health care organizations for individuals with or at risk for diabetes through a bidirectional e-referral system. There was an increase from # (baseline) to # (reporting period). This represents a __% increase over the funding period.
|
|
|
|
|
DP23-0020 Component B Performance Measure Definitions |
||
Strategy B.10 |
Support the development of multi-directional e-referral systems that support electronic exchange of information between health care and CBOs, including:
|
|
Measure B.10.2
|
Number of health care systems and providers using these multidirectional e-referral system to exchange information with a.) CDC-recognized organizations offering the National DPP lifestyle intervention and/or b.) DSMES or diabetes support services and c.) community programs/services that address SDOH or meet social needs; and the total # of patients served within these health care organizations. Note: Recipients can select to implement a and/or b, but c is required. |
|
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
|
AREAS |
DESCRIPTIONS |
|
Purpose |
The purpose of this performance measure is to monitor recipients’ progress toward increasing the number of health care organizations using multi-directional e-referral systems to exchange information with CDC-recognized organizations offering the National DPP lifestyle intervention and/or DSMES or diabetes support services and community programs/services that address SDOH or meet social needs; and the total number of patients served within these health care organizations.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
|
VALUES TO BE REPORTED |
||
Numerator Definition* |
Number of health care systems using the multi-directional e-referral system to exchange information with a) CDC-recognized organizations offering the National DPP lifestyle intervention and/or b) DSMES or diabetes support services and c) community programs/services that address SDOH or meet social needs
Total number of patients served within these health care organizations
|
|
Denominator Definition*
|
Not Applicable |
|
Proportion Definition* |
Not Applicable |
|
Measure Elements |
The following elements will be submitted as part of the measure:
|
|
Date Data Collected* |
Provide the date these data were collected. |
|
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP 23-0020 during the reporting period. |
|
Progress Notes* |
The progress notes should include the following for this measure:
|
|
Other Attachments* |
Not Applicable |
|
Additional Information and Guidance |
||
Helpful Hints |
In the “Measure Notes,” describe any additional information that provides context for the values reported and underserved areas in which you are working.
How to report values for this measure:
Note: Providers are defined as healthcare providers such as doctors, nurse practitioners, physician assistants, etc. |
|
Data Source(s) |
Program records: Recipients will track this information and report it to CDC. |
|
Unit of Analysis |
|
|
Result Statement(s) |
|
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.10
Strategy B.11
Strategy B.12
Strategy B.13 |
Strategy B.10: Support the development of multi-directional e-referral system that support two-way electronic exchange of information between health care and community-based organizations (CBOs) managing social needs. Strategy B.11: Design and test innovative payment models that bundle the National DPP lifestyle intervention and/or DSMES with other programs and services that address relevant health or social needs of priority populations. Strategy B.12: Improve the sustainability of Community Health Workers (CHWs) by building or strengthening a supportive infrastructure to expand their involvement in evidence-based diabetes prevention and management programs and services. Strategy B.13: Improve the capacity of the diabetes workforce to address factors related to the SDOH that impact health outcomes for priority populations with and at risk for diabetes |
Measure B.10.a |
Number of participants (total number and number from priority populations) enrolled by CDC-recognized National DPP delivery organizations |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor the number of participants (total number and number from priority populations) enrolled by CDC-recognized National DPP delivery organizations as a result of the short-t
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
None. Recipients are not required to report data for this measure. This measure will be monitored and reported by CDC. |
CDC-Reported Data (INTERNAL) |
Total number of participants enrolled in CDC-recognized National DPP delivery organizations.
Number of participants from priority populations enrolled in CDC-recognized National DPP delivery organizations |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
|
Date Data Collected* |
Provide the date these data were collection. |
Measure Notes* |
The measure notes should include the following for this measure:
|
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes”, describe any additional information that provides context for the values reported and underserved areas in which you are working.
How to report values for this measure:
|
Data Source(s) |
CDC DPRP Report |
Unit of Analysis |
Participants/individuals |
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.10
Strategy B.11
Strategy B.12
Strategy B.13 |
Strategy B.10: Support the development of multi-directional e-referral systems that support two-way electronic exchange of information between health care and community-based organizations (CBOs) managing social needs. Strategy B.11: Design and test innovative payment models that bundle the National DPP lifestyle intervention and/or DSMES with other programs and services that address relevant health or social needs of priority populations. Strategy B.12: Improve the sustainability of Community Health Workers (CHWs) by building or strengthening a supportive infrastructure to expand their involvement in evidence-based diabetes prevention and management programs and services Strategy B.13: Improve the capacity of the diabetes workforce to address factors related to the SDOH that impact health outcomes for priority populations with and at risk for diabetes |
Measure B.10.b
|
Number of people with diabetes (total number and number from priority populations) participating in DSMES services offered by an ADA-recognized or ADCES-accredited organization |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress towards increasing the number of people with diabetes (total number and number of priority populations) participating in DSMES services offered by an ADA-recognized or ADCES-accredited organization as a result of DP23-0020.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
None. Recipients are not required to report data for this measure. This measure will be monitored and reported by CDC. |
CDC-Reported Data (Internal) |
Total number of people with diabetes participating in recognized/accredited DSMES services offered by an ADA-recognized or ADCES-accredited organization for the reporting period
Number of people with diabetes from priority populations participating in ADA recognized or ADCES-accredited DSMES services for the reporting period |
Denominator Definition* |
Not Applicable |
Proportion Definition*
|
Not Applicable |
Measure Elements |
|
Date Data Collected* |
Provide the date these data were collection. |
Measure Notes* |
The measure notes should include the following for this measure:
Note: The information/data provided should reflect the work supported by DP23-0020 during the reporting period. |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes”, describe any additional information that provides context for the values reported and underserved areas in which you are working. How to report values for this measure:
|
Data Source(s) |
CDC – ADA/ADCES DSMES State Report |
Unit of Analysis |
Number of participants |
Result Statement(s) |
In the US, CDC-funded recipients worked to increase the number of people with diabetes from priority populations participating in DSMES services offered by an ADA-recognized or ADCES-accredited organization from # (baseline) to # (reporting period). This represents an increase of ___% over the funding period. |
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.10
Strategy B.11
Strategy B.12
Strategy B.13 |
Strategy B.10: Support the development of multi-directional e-referral systems that support two-way electronic exchange of information between health care and community-based organizations (CBOs) managing social needs. Strategy B.11: Design and test innovative payment models that bundle the National DPP lifestyle intervention and/or DSMES with other programs and services that address relevant health or social needs of priority populations. Strategy B.12: Improve the sustainability of Community Health Workers (CHWs) by building or strengthening a supportive infrastructure to expand their involvement in evidence-based diabetes prevention and management programs and services. Strategy B.13: Improve the capacity of the diabetes workforce to address factors related to the SDOH that impact health outcomes for priority populations with and at risk for diabetes |
Measure B.10.c
|
Number of people with diabetes (total and number from priority population) participating in diabetes support programs/ services |
Measure Type |
☐ Short Term Measure ☒ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor the number of participants (total number and number from priority populations) enrolled by CDC-recognized National DPP delivery organizations.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP
|
VALUES TO BE REPORTED |
|
Numerator Definition* |
Total number of people with diabetes participating in diabetes support programs or services for the reporting period
Number of people with diabetes from priority populations participating in diabetes support programs or services for the reporting period |
Denominator Definition* |
Not Applicable |
Proportion Definition*
|
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
|
Measure Notes* |
The measure notes should include the following for this measure:
|
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes”, describe any additional information that provides context for the values reported.
How to report values for this measure:
|
Data Source(s) |
|
Unit of Analysis |
People with diabetes |
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.11 |
Design and test innovative payment models that bundle the National Diabetes Prevention Program (National DPP) lifestyle change program (LCP) and/or diabetes self-management education and support (DSMES) with other programs and services that address relevant health or social needs of priority populations |
Measure B.11.1 |
Number and types of models implemented that bundle the National DPP lifestyle intervention and/or DSMES with other programs and services that address relevant health or social needs of priority population. |
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor the progress increasing the number of models implemented that bundle the National DPP lifestyle intervention and/or DSMES with other programs and services that address relevant health or social needs of priority population.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
Number of people covered by a model that bundle the National DPP lifestyle intervention and/or DSMES with other programs and services that address relevant health or social needs of priority populations |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
|
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes”, describe any additional information that provides context for the values reported and underserved areas in which you are working.
How to report values for this measure:
Note: Include examples of bundled models such as CCHs and contract, etc. with a payer that includes a payment model that isn't a standard model (standard models are MDPP, Medicaid coverage for the National DPP that looks like MDPP, or any private payer model that looks like the MDPP.). Provide additional details of the model in the measure notes. |
Data Source(s) |
The following data sources will be used to collect data for this measure:
|
Unit of Analysis |
Bundle models Priority population |
Result Statement(s) |
In the US, CDC-funded recipients worked to increase the number of models implemented that bundle the National DPP lifestyle intervention and/or DSMES with other programs and services that address relevant health or social needs of priority population from # (baseline) to # (reporting period). This represents an increase of ___percent over the funding period. |
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.12 |
Improve the sustainability of Community Health Workers (CHWs) by building or strengthening a supportive infrastructure to expand their involvement in evidence-based diabetes prevention and management programs and services. |
Measure B.12.1 |
Number of CHWs in the workforce who:
|
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient progress to increase the number of CHWs in the workforce that:
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP The recipient should report only those measures supported by the approved DP23-0020 workplan. |
VALUES TO BE REPORTED |
|
Numerator Definition* |
Number of CHWs in the workforce who:
Note: Recipient should report only on the ones that are a result of the program activities approved and implemented under DP23-0020. *State and local CHW associations and networks should utilize the Community Health Worker Core Consensus (C3) Project definition of the roles and competencies of CHWs as it represents a nationwide approach to achieving consensus around the CHW scope of practice in advancement of the CHW field |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure (as available):
Note: Recipient should report only on the ones that are a result of the program activities approved and implemented under DP23-0020 |
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Please attach any surveys, toolkits, etc. that were used for data collection. |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure
Notes,”
How to report the values for this measure:
Are reimbursed for their services through public and private insurers and employer payment mechanisms Note: State and local CHW associations and networks should utilize the Community Health Worker Core Consensus (C3) Project definition of the roles and competencies of CHWs as it represents a nationwide approach to achieving consensus around the CHW scope of practice in advancement of the CHW field.
*It is recommended that state, regional and local CHW associations formulate their scope of practice based on the recommendations of the Community Health Worker Core Consensus (C3) Project’s definition of the roles and competencies of CHWs as it represents a nationwide approach to achieving consensus around the CHW scope of practice in advancement of the CHW field.
|
Data Source(s) |
|
Unit of Analysis |
Community Health Workers |
Result Statement(s) |
|
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.13 |
Improve the capacity of the diabetes workforce to address factors related to the SDOH that impact health outcomes for priority populations with and at risk for diabetes |
Measure 13.1 |
Number and type of staff trained on SDOH strategies and training type |
Measure Type |
☒ Short Term Measure ☐ Intermediate Measure ☐ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor recipient’s efforts to increase the number and type of staff trained on SDOH strategies.
Note: For more details, please refer to the 2320 Strategy Guide (cdc.gov) in AMP |
VALUES TO BE REPORTED |
|
Numerator Definition* |
Number and type of staff trained on SDOH strategies, to include training type |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
The following elements will be submitted as part of the measure:
|
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
|
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes”, describe any additional information that provides context for the values reported.
How to report the values for this measure:
|
Data Source(s) |
|
Unit of Analysis |
Staff trainings |
Result Statement(s) |
In the US, CDC-funded recipients worked to increase the number of staff trained for SDOH awareness related to recipient needs in CDC-recognized organizations # (baseline) to # (reporting period). This represents an increase of ___% over the funding period. |
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B. 1 Strategy B. 2 Strategy B. 3 Strategy B. 4 Strategy B. 9 Strategy B. 10 Strategy B. 11 Strategy B. 12 Strategy B. 13
|
Strategy B.1: Strengthen self-care practices by improving access, appropriateness, and feasibility of diabetes self-management education and support (DSMES) services for priority populations Strategy B.2: Expand availability of ADA-recognized and ADCES-accredited DSMES services as a covered health benefit for Medicaid beneficiaries and employees with diabetes Strategy B.3: Prevent diabetes complications for priority populations through early detection Strategy B.4: Improve acceptability and quality of care for priority populations with diabetes Strategy B.9: Increase and sustain DSMES and National DPP delivery sites within pharmacy networks and chain pharmacies to improve reach to priority populations Strategy B.10: Support the development of multi-directional e-referral systems that support electronic exchange of information between health care and CBOs Strategy B.11: Design and test innovative payment models that bundle the National DPP lifestyle intervention and/or DSMES with other programs and services that address relevant health or social needs of priority populations Strategy B.12: Improve the sustainability of Community Health Workers (CHWs) by building or strengthening a supportive infrastructure to expand their involvement in evidence-based diabetes prevention and management programs and services Strategy B.13: Improve the capacity of the diabetes workforce to address factors related to the SDOH that impact health outcomes for priority populations with and at risk for diabetes
|
Measure 14.1 |
Proportion of people with diabetes with an A1C > 9% (decrease desired in this measure) |
Measure Type |
☐ Short Term Measure ☐ Intermediate Measure ☒ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose |
The purpose of this performance measure is to monitor and ultimately see a decrease in the proportion of people with diabetes (PWD) with poor glycemic control (A1c > 9%) and at greatest risk of diabetes complications. |
VALUES TO BE REPORTED |
|
Numerator Definition* |
None. Recipients are not required to report data for this measure. This measure will be monitored and reported by CDC. |
CDC-Reported Data (INTERNAL)
|
|
Proportion Definition*
|
Not Applicable |
Measure Elements |
Not Applicable |
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes* |
The measure notes should include the following for this measure:
|
Progress Notes* |
The progress notes should include the following for this measure:
|
Other Attachments* |
Not Applicable |
Additional Information and Guidance |
|
Helpful Hints |
In the “Measure Notes”, describe any additional information that provides context for the values reported and underserved areas in which you are working. |
Data Source(s) |
The following data sources will be used to collect data for this measure:
|
Unit of Analysis |
People with diabetes |
Result Statement(s) |
In the US, the number of people 18-75 years of age whose most recent A1c level is > 9%. This represents a decrease of ___% over the funding period. |
DP23-0020 Component B Performance Measure Definitions |
|
Strategy B.5 Strategy B.6 Strategy B.7 Strategy B.9 Strategy B.10 Strategy B.11 Strategy B.12 Strategy B.13 |
Strategy B.5: Increase enrollment and retention of priority populations in the National Diabetes Prevention Program (National DPP) lifestyle intervention and the MDPP by improving access, appropriateness, and feasibility of the programs Strategy B.6: Expand availability of the National DPP lifestyle intervention as a covered health benefit for Medicaid beneficiaries and/or employees and covered dependents at high risk for type 2 diabetes Strategy B.7: Improve sustainability of CDC-recognized National DPP delivery organizations serving priority populations by establishing or expanding National DPP Umbrella Hub Arrangements Strategy B.9: Increase and sustain DSMES and National DPP delivery sites within pharmacy networks and chain pharmacies to improve reach to priority populations Strategy B.10: Support the development of multi-directional e-referral systems that support electronic exchange of information between health care and CBOs Strategy B.11: Design and test innovative payment models that bundle the National DPP lifestyle intervention and/or DSMES with other programs and services that address relevant health or social needs of priority populations Strategy B.12: Improve the sustainability of Community Health Workers (CHWs) by building or strengthening a supportive infrastructure to expand their involvement in evidence-based diabetes prevention and management programs and services Strategy B.13: Improve the capacity of the diabetes workforce to address factors related to the SDOH that impact health outcomes for priority populations with and at risk for diabetes |
Measure B.15 |
Number of program completers (total # and # from priority populations) in CDC-recognized National DPP delivery organizations who reduce their risk for type 2 diabetes** * Based on CDC’s Diabetes Prevention Recognition Program (DPRP) Standards, participants who are retained in the National DPP lifestyle intervention (i.e., program completers) are defined as those who attended 8+ sessions in the first six months and whose total time in the program is 9 or more full months. |
Measure Type |
☐ Short Term Measure ☐ Intermediate Measure ☒ Long Term Measure |
AREAS |
DESCRIPTIONS |
Purpose
|
The purpose of this performance measure is to monitor change resulting from efforts to increase the number of program completers* served by CDC-recognized National DPP delivery organizations. |
VALUES TO BE REPORTED |
|
Numerator Definition* |
None. Recipients are not required to report data for this measure. This measure will be monitored and reported by CDC. |
CDC-Reported Data (INTERNAL) |
Total number of program completers for the DPP-LCP program in a CDC-recognized National DPP delivery organization Number of program completers from priority populations in the DPP-LCP program in a CDC-recognized National DPP delivery organization. |
Denominator Definition* |
Not Applicable |
Proportion Definition* |
Not Applicable |
Measure Elements |
Not Applicable |
Date Data Collected* |
Provide the date these data were collected. |
Measure Notes*
|
The measure notes should include the following for this measure:
Describe any additional information that provides context for the values reported and underserved areas recipient is working in. |
Progress Notes*
|
The progress notes should include the following for this measure:
|
Other Attachments* |
Not applicable |
Additional Information and Guidance |
|
Helpful Hints
|
In the “Measure Notes”, describe any additional information that provides context for the values reported.
How to report values for this measure:
|
Data Source(s)
|
CDC DPRP State-level Evaluation Report |
Unit of Analysis
|
Program completers |
Result Statement(s)
|
|
Glossary
Strategy 1 Key Terms
Certified diabetes care and education specialist (CDCES): a health care professional with expertise in diabetes care and education who has met eligibility requirements and successfully completed a certification exam.
Diabetes self-management education and support (DSMES): the ongoing process of facilitating the knowledge, skills, and ability necessary for diabetes self-care, as well as activities that assist a person in implementing and sustaining the behaviors needed to manage their condition on an ongoing basis, beyond or outside of formal self-management training (Powers et al., 2020; Davis et al., 2022).
Diabetes self-management support (DSMS): the support that is required for implementing and sustaining coping skills and behaviors needed to self-manage diabetes on an ongoing basis (Powers et al., 2020).
Diabetes self-management training (DSMT): the Centers for Medicare & Medicaid Services (CMS) uses the term “training” (DSMT) instead of “education and support” (DSMES) when defining the reimbursable benefit. This term relates specifically to Medicare billing.
Priority Populations: defined in the DP23-0020 notice of funding opportunity (2320 NOFO) as those who have systematically experienced greater obstacles to health based on their racial or ethnic group, religion, socioeconomic status, gender, age, mental health, cognitive, sensory, or physical disability, sexual orientation or gender identity, geographic location, or other characteristics historically linked to discrimination or exclusion. Priority populations will be determined by the awardee.
Recognition and accreditation: processes that help ensure that DSMES services offer quality education. CMS has authorized two organizations, ADA and ADCES, to grant recognition or accreditation for DSMES. ADA uses the term recognition, while ADCES uses the term accreditation. The two terms involve similar processes to evaluate DSMES services. Both organizations rely on the 2022 National Standards for DSMES (Davis et al., 2022).
Self-care: the seven behaviors that persons with diabetes can use to manage their diabetes. They include healthy coping, healthy eating, being active, taking medicine, monitoring, problem solving, and lowering risks.
Umbrella DSMES ADA-recognized/ADCES-accredited service: a DSMES service where one agency serves as the sponsoring organization to secure ADA-recognition or ADCES-accreditation, managing all the certification requirements, while other agencies serve as multi-sites or branch sites to deliver DSMES services.
Strategy 1 Resources
CDC DSMES Technical Assistance Guide: This tool identifies four key drivers that influence DSMES access and participation: 1) availability of DSMES services, 2) payers and payment mechanisms, 3)
DSMES CDC DSMES Toolkit: The purpose of this toolkit is to increase access to and participation in DSMES services among persons with diabetes. The toolkit provides available resources and tools in one place to assist with the development, promotion, implementation, and sustainability of DSMES services.
To learn more about removing barriers to DSMES services, refer to Increasing Referrals and Overcoming Barriers to Participation.
ADCES Diabetes Education Accreditation Program (DEAP): As one of the certifying organizations for DSMES, ADCES offers an accreditation process based on the 2022 National Standards for DSMES.
ADA Diabetes Support Directory: This directory provides an overview of ADA-approved research-tested and practice-tested diabetes support programs.
ADCES DSMES Directory: Find an ADCES-accredited DSMES program in your area.
ADA DSMES Directory: Find an ADA-recognized DSMES program in your area.
Sample DSMES and diabetes support programs/services successes:
DiabetesSmart: Diabetes Education Recognition Program: North Carolina was the first state to develop a statewide “umbrella” service where the Division of Public Health serves as the sponsoring agency, managing all the ADA recognition requirements, while local health agencies are “multi-sites”, providing DSMES services for people in their communities.
New Mexico: The New Mexico Department of Health implemented Kitchen Creations in local senior centers to teach seniors with diabetes how to plan and cook meals. Participants were able to enroll in the program multiple times.
Colorado: The Colorado Department of Public Health and Environment worked alongside their priority populations to identify opportunities to increase referrals to existing DSMES and National Diabetes Prevention Program (National DPP) programs and launch new programs in high-need areas, through identifying community subject matter experts and conducting interviews with DSMES and National DPP participants.
Diabetes State Burden Toolkit: Use this tool to determine the health, economic, and mortality burden of diabetes in your state.
DSMES Consensus Report: This report describes the benefits of DSMES, defines four critical times to provide and modify DSMES, proposes how to locate DSMES-related resources, and discusses potential solutions to access and utilization barriers.
Refer to the DSMES Algorithm of Care for a full-page version of the algorithm.
2023 Standards of Care in Diabetes: This resource provides current clinical practice recommendations and is intended to provide information for clinicians, patients, researchers, payers, and others on the components of diabetes care, general treatment goals, and tools to evaluate the quality of care.
Approaches to Increase Access to and Participation in DSMES: This report describes the work of three previous CDC cooperative agreement recipients to increase access to and participation in DSMES through targeted outreach, partnership, technical assistance, funding opportunities, and reimbursement initiatives.
CDC Evaluability Assessments and Rapid Evaluations: DSMES Programs in Underserved Populations and Communities: In 2018, CDC conducted rapid evaluations of DSMES services. The goal was to understand implementation processes that may help others wishing to offer DSMES services for underserved populations. Lessons learned from 2 programs are highlighted.
Strategy 2 Key Terms
Covered Benefit: A health service included in the premium of a health insurance policy** paid by or on behalf of the enrolled individual (also called a benefit or covered service). For Medicaid, a covered benefit describes coverage for eligible beneficiaries paid for by state and federal funding. (**Note that including a program/service as a covered health benefit is a more sustainable way to offer preventive services than through a wellness program.)
Diabetes Self-Management Education and Support (DSMES): The ongoing process of facilitating the knowledge, skills, and ability necessary for diabetes self-care, as well as activities that assist a person in implementing and sustaining the behaviors needed to manage their condition on an ongoing basis, beyond or outside of formal self-management training (Powers et al., 2020; Davis et al., 2022).
Diabetes Self-Management Support (DSMS): The support that is required for implementing and sustaining coping skills and behaviors needed to self-manage diabetes on an ongoing basis (Powers et al., 2020).
Diabetes Self-Management Training (DSMT): CMS uses the term “training” (DSMT) instead of “education and support” (DSMES) when defining the reimbursable benefit. This term relates specifically to Medicare billing.
DSMES Recognition and Accreditation: Processes that help ensure that DSMES services adhere to national quality standards. CMS has authorized two organizations, the ADA and ADCES, to grant recognition or accreditation for DSMES. ADA uses the term recognition, while ADCES uses the term accreditation. The two terms involve similar processes to evaluate DSMES services. Both organizations rely on the 2022 National Standards for DSMES (Davis et al., 2022).
Fully insured Employer: An employer that pays a predetermined premium to the insurance carrier. The insurance carrier assumes the financial risk for providing all contracted health care benefits.
Medicaid: A jointly funded state and federal program to provide health care for low-income Americans; requirements for basic services to be delivered are determined by the federal government, while additional services may be added by the states, resulting in every state having a unique Medicaid program.
Medicaid Managed Care Organizations (MCOs): Private organizations that contract with health care providers in a state to deliver specific services to Medicaid beneficiaries under the state’s Medicaid plan. MCOs operate on a capitated basis, meaning they are reimbursed on a per-capita basis per beneficiary. If the costs of providing care to a beneficiary are over the capitation fee, the MCO is responsible for absorbing the overage. If the costs of providing care to a beneficiary are below the capitation fee, the MCO retains the excess as profit. MCOs are also reimbursed for administrative costs and care management in addition to specific health care costs.
Medicaid State Plan and State Plan Amendment (SPA): A Medicaid state plan is an agreement between a state and the Federal government describing how that state administers its Medicaid program. It provides assurance that a state will abide by Federal rules and may claim Federal matching funds for its program activities. The state plan sets out groups of individuals to be covered, services to be provided, methodologies for providers to be reimbursed and the administrative activities that are underway in the state. Every state is required to file a Medicaid State Plan with CMS. If the state wants to make a change to its state Medicaid program by altering the services covered (within federal guidelines), or the populations covered, it must submit a SPA.
Priority Populations: Defined in the DP23-0020 notice of funding opportunity (2320 NOFO) as those who have systematically experienced greater obstacles to health based on their racial or ethnic group, religion, socioeconomic status, gender, age, mental health, cognitive, sensory, or physical disability, sexual orientation or gender identity, geographic location, or other characteristics historically linked to discrimination or exclusion. Priority populations of focus will be determined by each recipient.
Self-insured Employer: An employer that assumes the financial risk for providing health care benefits to its employees. Self-insured employers may still contract with an insurance carrier to handle the administrative aspects of the claims process. (This is also called an Administrative Services Only [ASO] health care plan.) Many medium-to-large employers are self-insured and are the most likely to be participants in regional or state organizations promoting prevention in health benefits. For this reason, it is most productive for 2320 recipients to focus their efforts on self-insured employers.
Umbrella DSMES ADA-Recognized/ADCES-Accredited Service: A DSMES service where one agency, such as a state health department, serves as the sponsoring organization to secure ADA-recognition or ADCES-accreditation, managing all the certification requirements, while other agencies serve as multi-sites or branch sites to deliver DSMES.
1115 Demonstration Waiver: A process instituted by CMS to allow states to institute reforms that go beyond routine medical care and focus on evidence-based interventions that drive better health outcomes and quality of life improvements.
Strategy 2 Resources
National Diabetes Prevention Program Coverage Toolkit: This online toolkit was developed to provide information about the mechanics of covering the National DPP LCP. While the content on this site is focused on National DPP, the methods can be transferred to DSMES employer coverage. The following links are specific resources for Medicaid Coverage and participating public and private employers:
Diabetes State Burden Toolkit: Use this tool to identify the health, economic, and mortality burden of diabetes in your state. This tool is particularly useful to determine what the projected outlook of health and economic costs will be if nothing is done to prevent type 2 diabetes.
Working with Employers and Insurers Guide: This implementation guide will help you learn how to work with employers and insurers to engage, recruit, and enroll people with prediabetes who have health insurance coverage in the National DPP LCP to prevent or delay the onset of type 2 diabetes. While the content in this guide is focused on the National DPP, much of the information can be transferred to DSMES employer coverage.
Employer Path to Adoption (cdc.gov) This resource provides a checklist to guide employers through making the decision to offer the National DPP lifestyle change program as a covered benefit. While the content of this resource is focused on the National DPP, much of the information can be transferred to DSMES employer coverage.
CMS Medicare DSMES Benefit: This resource provides the language used by CMS in defining the requirements for DSMT.
CDC DSMES Toolkit: The toolkit provides available resources and tools in one place to assist with the development, promotion, implementation, and sustainability of DSMES services. The following pages focus on building the business case for DSMES and overcoming barriers to participation:
Healm: Diabetes Prevention For Your Workforce: Healm is a free, online decision-support tool that helps employer benefit plans make informed decisions about providing the National DPP lifestyle change program as a covered benefit for employees. While the content on this site is focused on the National DPP, many of the tools and resources it provides can be transferred to DSMES employer coverage.
Strategy 3 Key Terms
A1C Test: Measures your average blood sugar level over the past 2 or 3 months. An A1C below 5.7% is normal, between 5.7 and 6.4% indicates you have prediabetes, and 6.5% or higher indicates you have diabetes.
Chronic Kidney Disease (CKD): CKD is a chronic condition in which the kidneys are damaged and can’t filter wastes from the bloodstream as well as healthy kidneys. Kidney disease is the ninth leading cause of death in the US. About 38 million people, or 15% of US adults, are estimated to have CKD, yet about 90% are not aware of their condition. In diabetic kidney disease, in addition to cardiovascular disease, individuals are at higher risk of other diabetes-related complications, including retinopathy. Once detected, CKD is typically treated with medications such as angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers to slow disease progression.
CKD Testing: Regardless of cause, CKD is diagnosed by the presence of either of the following two indicators for at least 3 months (Levin et al., 2013):
Markers of kidney damage (one or more):
Albuminuria (albumin excretion rate ≥30 mg/24 hours; albumin-to-creatinine ratio ≥30 mg/g [≥3 mg/mmol])
Urine sediment abnormalities
Electrolyte and other abnormalities due to tubular disorder
Abnormalities detected by histology
Structural abnormalities detected by imaging
History of kidney transplantation
Decreased glomerular filtration rate (eGFR): eGFR <60 ml/min/1.73 m2
Clinical Decision Support (CDS): CDS provides clinicians, staff, patients, and others with knowledge and person-specific information, intelligently filtered, or presented at appropriate times, to enhance health and health care. CDS encompasses a variety of tools to enhance decision-making in the clinical workflow. These tools include computerized alerts and reminders to care providers and patients, clinical guidelines, condition-specific order sets, focused patient data reports and summaries, documentation templates, diagnostic support, and contextually relevant reference information, among other tools. They require computable biomedical knowledge, person-specific data, and a reasoning or inferencing mechanism that combines knowledge and data to generate and present helpful information to clinicians as care is being delivered. This information must be filtered, organized, and presented in a way that supports the current workflow, allowing the user to make an informed decision quickly and act. The majority of CDS applications operate as components of comprehensive EHR systems, although stand-alone CDS systems are also used.
Diabetes Complications: Diabetes can affect many different organ systems in the body, and over time, elevated blood sugar levels can lead to serious complications. Diabetes complications can be classified as microvascular or macrovascular. Microvascular complications include nervous system damage (neuropathy), renal system damage (nephropathy, also known as CKD), and eye damage (retinopathy). Macrovascular complications include cardiovascular disease, stroke, and peripheral vascular disease. Peripheral vascular disease may lead to bruises or injuries that do not heal, gangrene, and ultimately, amputation. Additional information on the prevention of complications can be found at CDC’s Diabetes Complications.
Diabetic Retinopathy (DR): DR is a common microvascular complication of diabetes and the leading cause of incident blindness among working age adults 20-74 years in the US (Harris, 1995). DR affects blood vessels in the retina (the light-sensitive layer of tissue in the back of your eye). The early stages of DR usually don’t have any symptoms. Some people notice changes in their vision, like trouble reading or seeing faraway objects. These changes may come and go. In later stages of the disease, blood vessels in the retina start to bleed into the vitreous (gel-like fluid that fills your eye). If this happens, there may be a presence of dark, floating spots or streaks that look like cobwebs. Sometimes, the spots clear up on their own — but it’s important to get treatment right away. Without treatment, scars can form in the back of the eye. Blood vessels may also start to bleed again, or the bleeding may get worse. The prevalence of DR in the US is high, with an estimated 4.1 million persons aged 40 and older (or 1 in 29 persons) experiencing it (Kempen et al. 2004). Risk for vision loss increases the longer an individual lives with diabetes. DR is nearly three times higher among adults aged 45 and over who had a diagnosis of diabetes for 10 years or more (12.2%) compared with less than 10 years (4.2%). Nearly 9.0% of adults aged 45 and over with diagnosed diabetes have DR (8.6%), and 4.1% have vision loss due to DR (Cha et al., 2019). And people who are Black or Latino are 2 to 3 times more likely to develop DR than their White counterparts (Coney and Adrienne, 2022).
DR Screening: DR is best diagnosed with a comprehensive dilated eye exam, where a doctor would place drops in a patient’s eyes to dilate the pupils and look for abnormalities (“Diabetic Retinopathy”, 2023). DR screening is significant because an 83% increase in diabetes is expected— 24 million in 2009 to 44 million by 2034 (Mansberger et al., 2013). Minority populations, including American Indian/Alaska Natives, are two times more likely to have diabetes than non-Hispanic whites. There is a 78% chance that people with poorly managed diabetes for more than 15 years will develop eye disease. Early diagnosis of DR and timely treatment can reduce the risk of permanent visual impairment and blindness by 90%. Only 62.5% of people with diabetes in the US receive annual DR screenings, and social determinants of health have an important role in DR screening rates (Baccaglini et al., 2021). In many communities, it can be challenging to obtain eye exams from eye care providers due to transportation challenges, lack of health insurance, limited access to eye care providers, and financial burdens such as co-pays or other associated costs of the exam.
Electronic Health Records (EHR): An EHR is an electronic version of a patient’s medical history that is maintained by the provider over time. EHRs may include all key administrative clinical data relevant to an individual’s care under a particular provider, including demographics, progress notes, problems, medications, vital signs, past medical history, immunizations, laboratory data, and radiology reports. The EHR automates access to information and has the potential to streamline the clinician's workflow. The EHR also can support other care-related activities, directly or indirectly, through various interfaces, including evidence-based decision support, quality management, and outcomes reporting.
Health Care Organizations: A center (such as a hospital, skilled nursing facility, home health agency, outpatient clinic, comprehensive rehabilitation facility, physician or non-physician practice, laboratory, etc.) that provides health services such as diagnosis of diseases, education or disease management, surgical operations and treatments, and patient recovery support.
Priority Populations: defined in the DP23-0020 notice of funding opportunity (2320 NOFO) as those who have systematically experienced greater obstacles to health based on their racial or ethnic group, religion, socioeconomic status, gender, age, mental health, cognitive, sensory, or physical disability, sexual orientation or gender identity, geographic location, or other characteristics historically linked to discrimination or exclusion. Priority populations will be determined by the awardee.
Reminders (Alerts): Reminders set within the EHR, and other e-alerts, are notifications triggered by particular parameters (e.g., time and date, high/low threshold, or clinical indication) usually presented as highlighted text or a pop-up that requires action. Reminders serve to cue clinicians that certain events should take place but have not yet done so. Reminders are regularly used in primary care systems, particularly with respect to the management of patients with chronic conditions that require regularly scheduled repetitive tasks.
Telehealth: The exchange of medical information from one site to another through electronic communication to improve a patient’s health. Telehealth technology may be used to increase access to DR screening among priority populations by using a non- mydriatic retinal camera at the screening site connected to a central reading center through telemedicine. Coverage for telehealth in state Medicaid programs varies by state. It is important to understand how a third-party payer reimburses for services using telehealth technologies. The Center for Connected Health Policy publishes the most current telehealth-related policies, laws, and regulations that can be searched by all 50 states and the District of Columbia.
Strategy 3 Resources
CDC’s Vision and Eye Health Toolkit: Provides public health agencies and their partners with information to improve vision and eye health using 4 recommended actions: 1) assess vision and eye health in your community, 2) build effective partnerships, 3) implement interventions to improve vision and eye health, and 4) evaluate the impact of vision-related interventions.
Current State Partnerships for Improving Eye Health: The Vision Health Initiative selected seven state partners for the 2019-2021 funding period to improve eye health.
CKD Change Package: Represents a list of suggested process improvements that ambulatory care can utilize to improve CKD screening, recognition, and management.
Kidney Health Toolkit: Provides resources for patients, providers, health plans, and health systems to employ best practices in promoting kidney health and CKD care.
National Kidney Disease Education Program: Promoted evidence-based interventions to improve understanding, detection, and management of kidney disease, including identification of patients at greatest risk for progression to kidney failure.
National Kidney Foundation Professional Education Resource Center: Provides a catalog of events and courses for professionals committed to improving patient outcomes related to kidney disease.
Voices for Kidney Health: Provides a list of resources to promote awareness, prevention, and treatment of kidney disease in the US.
CKD Initiative | CDC: Provides public health strategies for promoting kidney health.
National Kidney Disease Education Program: Promotes evidence-based interventions to improve understanding, detection, and management of kidney disease, including identification of patients at greatest risk for progression to kidney failure.
National Kidney Foundation Professional Education Resource Center: Designed for professionals committed to continuing their education and improving patient outcomes. Here you will find activities included courses, events, and other engaging content on an array of carefully selected topics given by renowned faculty.
Resources – National Kidney Foundation: These materials will help you learn more about how you can work with public leaders to become a voice for kidney health and advance policy that will help the kidney community.
Strategy 4 Key Terms
Care Practices: The process and delivery of care, in this case for persons with diabetes. Appropriate diabetes-related care practices should align with evidence-based clinical guidelines, such as the ADA Standards of Medical Care in Diabetes.
Chronic Care Model (CCM): Identifies the essential elements of a health care system that encourage high-quality, chronic disease care. These elements include the community, the health system, self-management support, delivery system design, decision support, and clinical information systems. In combination, evidence-based change concepts under each element foster productive interactions between informed patients who take an active part in their care and providers with resources and expertise.
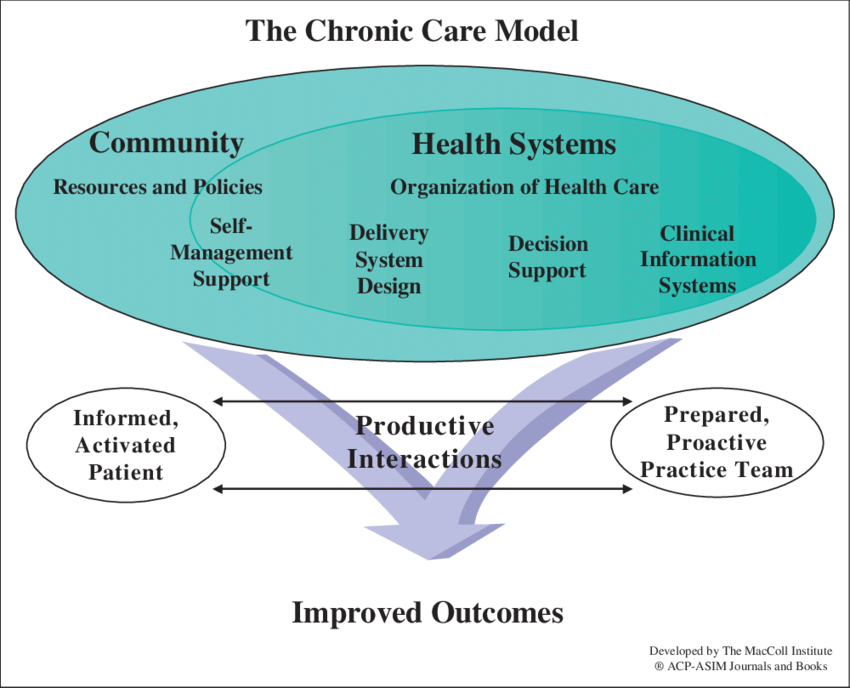
Clinical Decision Support (CDS): CDS provides clinicians, staff, patients, and others with knowledge and person-specific information, intelligently filtered, or presented at appropriate times, to enhance health and health care. CDS encompasses a variety of tools to enhance decision-making in the clinical workflow. These tools include computerized alerts and reminders to care providers and patients, clinical guidelines, condition-specific order sets, focused patient data reports and summaries, documentation templates, diagnostic support, and contextually relevant reference information, among other tools. They require computable biomedical knowledge, person-specific data, and a reasoning or inferencing mechanism that combines knowledge and data to generate and present helpful information to clinicians as care is being delivered. This information must be filtered, organized, and presented in a way that supports the current workflow, allowing the user to make an informed decision quickly and act. The majority of CDS applications operate as components of comprehensive EHR systems, although stand-alone CDS systems are also used.
Collaborative Practice Agreement (CPA): A formal agreement in which a licensed provider makes a diagnosis, supervises patient care, and refers patients to a pharmacist or other qualified health professional under a protocol that allows them to perform specific patient care functions.
Medication Management: A practice used by doctors, nurses, and pharmacists to ensure that patients are achieving optimal therapeutic outcomes for the prescription medications they may be taking. Medication management is used to cover a broad range of professional activities, such as:
Performing patient assessments or a comprehensive review of prescription medications and their possible interaction or side effects.
Formulating both short- and long-term medication treatment plans.
Monitoring the compliance, safety, and efficacy of all prescription medication plans and working with prescribers to make timely adjustments when needed.
Ensuring directional or instruction-based compliance through patient education.
Ensuring better documentation and communication between health care providers/professionals to maintain a high standard of care.
Pharmacists’ Patient Care Process: A patient-centered approach used by pharmacists, in collaboration with other providers on the health care team, to optimize patient health and medication outcomes. Although the patient care process focuses on the pharmacist’s perspective, the process can be adapted to include other members of the health care team.
Priority Populations: Defined in the DP23-0020 notice of funding opportunity as those who have systematically experienced greater obstacles to health based on their racial or ethnic group, religion, socioeconomic status, gender, age, mental health, cognitive, sensory, or physical disability, sexual orientation or gender identity, geographic location, or other characteristics historically linked to discrimination or exclusion. Priority populations of focus will be determined by each award recipient.
Team-based Care: The provision of health services to individuals, families, and/or communities by at least two health care professionals who work collaboratively with patients and their caregivers, to the extent preferred by each patient, to accomplish shared goals within and across settings to achieve coordinated high-quality care. A team-based care approach distributes work among individuals that is appropriate to their role and allows for more responsive and timely patient care. A health team’s composition can vary across health systems and health conditions. For example, in addition to a primary care physician, a chronic care team for a patient with diabetes could comprise the following:
CHWs/Patient Navigators
Certified Diabetes Care and Education Specialists
Registered Dietitians
Pharmacists
Dentists
Ophthalmologists/Optometrists
Podiatrists
Rehabilitation Specialists
The Community Preventive Services Task Force recommends team-based care to manage diabetes. Evidence shows that team-based care improves patients’ blood glucose, blood pressure, and lipid levels and increases the proportion of patients who reach target blood glucose, blood pressure, and lipid levels.
Strategy 4 Resources
ADA Standards of Medical Care in Diabetes includes all of ADA's current clinical practice recommendations and is intended to provide clinicians, patients, researchers, payers, and others with the components of diabetes care, general treatment goals, and tools to evaluate the quality of care.
American Association of Clinical Endocrinologists Clinical Guidelines includes 34 evidence-based clinical practice recommendations for the diagnosis and management of persons with nonalcoholic fatty liver disease and/or nonalcoholic steatohepatitis and contains 385 citations that inform the evidence base.
The Diabetes self-management education and support (DSMES) Toolkit is a comprehensive resource for achieving success in DSMES.
The CCM identifies the essential elements of a health care system that encourage high-quality chronic disease care. These elements are the community, the health system, self-management support, delivery system design, decision support and clinical information systems.
Community-clinical linkages are defined as connections between community and clinical sectors to improve population health. This Community-Linkages for the Prevention and Control of Chronic Diseases document guides public health practitioners on key strategies to implement community-clinical linkages that focus on adults 18 years or older.
The Transforming Clinical Practice Initiative model was uniquely designed to support clinician practices through nationwide, collaborative, and peer-based learning networks designed to help clinicians and practices to achieve large scale health care transformation, prepare practices to successfully participate in value-based payment arrangements, including Alternative Payment Models, and improve the quality of care.
The National Quality Forum is a not-for-profit, nonpartisan, membership-based organization that works to catalyze improvements in healthcare.
Pharmacy:
The pharmacists’ patient care process described in this document was developed by examining a number of key source documents on pharmaceutical care and medication therapy management. Patient care process components in each of these resources were catalogued and compared to create the following process that encompasses a contemporary and comprehensive approach to patient-centered care that is delivered in collaboration with other members of the health care team.
This knowledge video reviews Pharmacist CPAs which create formal practice relationships between pharmacists and collaborating prescribers leading to improved patient outcomes.
CHWs/ Community Health Representative:
The CHW Toolkit contains resources including online courses, lessons learned, and best practices to help state health departments train and further build capacity for CHWs in their communities, and training and education materials for CHWs to use within their communities.
The CHW Inclusion Checklist presents a general framework for public health practitioners to lead or assist in including CHWs and integrating the CHW scope of practice in health care settings.
CHW interventions have been found to be a promising strategy for improving diabetes outcomes, especially among low-income and racial and ethnic minority populations. This review serves as an update of the literature published since 2011 on CHWs’ role in diabetes care. Community Health Workers in Diabetes
The Indian Health Service Community Health Representative Program is a unique concept for providing health care, health promotion, and disease prevention services.
CPA:
The CPA implementation guide is a resource for pharmacists to use in developing and executing collaborative practice agreements in the spirit of advancing team-based care. It provides a customizable template that can be used as a starting point to developing a CPA.
This resource on CPAs and Pharmacists’ Patient Care Services provides information on strategies for advancing pharmacists’ patient care services with the help of CPAs. Case examples and actionable next steps are also provided.
SDOH:
This webpage provides information on the innovative approaches at CDC’s National Center for Chronic Disease Prevention and Health Promotion to build healthier communities by reducing chronic diseases and related health disparities for population groups affected by health inequities.
Strategy 5 Key Terms
Community Health Workers (CHWs): Frontline public health workers who are trusted members or have a particularly good understanding of the community served. CHWs serve as liaisons between health and social services and the community to facilitate access to services and to improve the quality and cultural competence of service delivery.
Culturally and linguistically appropriate adaptations: Changes made to resources that are "respectful of and responsive to the cultural and linguistic needs" of the priority population(s) served. This can include language adaptations; cultural adaptations, such as using cultural themes or sayings; dietary adaptations to accommodate cultural or local food preferences; and gender adaptations.
National DPP Find a Program Tool: This tool makes finding publicly available National DPP LCP classes easy for potential participants. It's also easy for delivery organizations to change the location of their publicly available classes by using the Public Class Locations section of DPRP Data Submission Portal. This section of the portal is only accessible to CDC-recognized organizations that choose the public class type and offer in-person delivery.
Priority Populations: Defined in the 2320 NOFO as those who have systematically experienced greater obstacles to health based on their racial or ethnic group, religion, socioeconomic status, gender, age, mental health, cognitive, sensory, or physical disability, sexual orientation or gender identity, geographic location, or other characteristics historically linked to discrimination or exclusion. Priority populations of focus will be determined by each award recipient.
Program Champion Strategy: CDC developed the Program Champion Strategy to support participant recruitment and outreach activities. It uses current and past program participants as Program Champions to help recruit new participants.
Social Determinants of Health (SDOH): The nonmedical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies, racism, climate change, and political systems.
Health-related social needs (HRSN) may serve as a barrier to enrolling and retaining participants in the National DPP LCP. An increasing number of CDC-recognized organizations are structuring their programs so that some of these barriers to staying in the program can be overcome, such as allowing for the provision of childcare vouchers and access to healthy food. For examples of how a CDC-recognized organization can address HRSN, see the Connecting SDOH and HRSN to Prediabetes and Type 2 Diabetes page of the National DPP Coverage Toolkit. For more information on SDOH and HRSN as they relate to the National DPP LCP, visit the suite of Health Equity and the National DPP pages on the Coverage Toolkit.
*Additional relevant terms can be found in the 2021 CDC DPRP Standards
Strategy 5 Resources
Lifestyle Coaches:
Continuing Education for Lifestyle Coaches: This link provides resources and information related to continuing education opportunities available for Lifestyle Coaches delivering the National DPP LCP and MDPP.
CSC Newsletter and Training Entities Archive: This site contains Lifestyle Coach training entity quarterly updates.
Diabetes Prevention Toolkit: For health system implementation or partnerships with health systems that do not have a diabetes prevention strategy, the American Medical Association (AMA) has developed this toolkit for clinicians and their care teams to implement a prediabetes screen/test/refer system-wide strategy.
PreventT2 curriculum: This CDC-approved curriculum comes with ready-to-use and adaptable promotional materials that can be easily modified to add an organization logo and contact information.
The links below provide several resources containing lessons learned and keys to success for participant enrollment and retention in the National DPP LCP:
CDC-Recognized Organizations:
Data Reporting for the National DPP Lifestyle Change Program: This section provides resources and guidance on CDC-recognized organizations’ data submission process. This includes information about reporting timelines, steps to complete the data collection spreadsheet, instructions for uploading the file to the CDC's DPRP data submission website and understanding the evaluation report. Each CDC-recognized organization is required to submit evaluation data to the DPRP every six months from the effective date of their application.
DPRP Data Submission Portal: CDC-recognized organizations are expected to update their public class location information regularly through this portal.
"Find A Program”: This Class Locator Platform features National DPP delivery locations offering in-person, publicly available classes. It helps the general public find organizations offering the program in their local area.
Considerations for Purchasing Technology Platforms to Support CDC-Funded Strategies Related to the National DPP, DSMES, and Pharmacists: This document was created to assist CDC-funded recipients (state health departments and national organizations) and other partners in selecting and implementing technology platforms to deliver and/or bill for the National DPP LCP.
National Registry of Recognized Diabetes Prevention Programs: This site lists contact information for all CDC-recognized organizations that deliver the National DPP LCP in communities across the United States.
MDPP Suppliers:
Centers for Medicare & Medicaid Services Innovation Center: This website provides information on the MDPP expanded model.
MDPP Implementation Resources - National DPP Coverage Toolkit: This section of the Coverage Toolkit includes webinars and resources developed by the National Association of Chronic Disease Directors as part of technical assistance for MDPP suppliers, with funding and support from CDC.
Turning Referrals into Enrollment Summary: Developed in follow-up to an informational webinar held on October 4th, 2021, this resource details best practices shared by MDPP suppliers for turning referrals into enrollments as well as possible solutions to enrollment barriers (CDC, 2021).
SDOH and Older Adults:
Keys to Success: How to Enroll and Retain Older Adults in the Medicare Diabetes Prevention Program or the National Diabetes Prevention Program: Inside this tip sheet are insights and lessons learned from programs with a proven record of enrolling and retaining Medicare or Medicare-eligible participants in the MDPP or National DPP LCP.
Supporting Your Older Adult Patients’ Needs through Enabling Services (National Center for Equitable Care for Elders, Harvard University): This issue brief provides information on how to recognize and access support and enabling services for older adults.
Strengthening Social Connection in Older Adults: This guide is intended as a resource for health center providers, educators, and administrators to understand, identify, and address social isolation and loneliness in older patients using best practices for serving this population.
Developing Cross-Sector Partnerships – Social Determinants of Health – Older Adult Participants: This guide provides health center staff with tools and strategies to initiate, develop, and sustain community partnerships to better serve older adult residents of public housing.
Food Insecurity Among Older Adults: This issue brief describes the lasting impacts food insecurity can have on older adults and lists several recommendations and resources on how to address them.
Strategy 6 Key Terms
Beneficiaries with complex social needs: Many Medicaid beneficiaries have unstable housing or are homeless, are un- or under-employed, are victims of domestic or child abuse, have job insecurity, have no means of transportation, have poor or no education, are involved with the criminal justice system, are refugees or immigrants, may not speak English, and/or may have limited or unreliable social networks (Thompson et al., 2019). These factors can contribute to poor health status and can also make this population harder to reach and harder to retain in lifestyle change programs.
Covered benefit: A health service included in the premium of a health insurance policy** paid by or on behalf of the enrolled individual (also called a benefit or covered service). For Medicaid, a covered benefit describes coverage for eligible beneficiaries paid for by state and federal funding. (**Note that including a program/service as a covered health benefit is a more sustainable way to offer preventive services than through a wellness program.)
Expanded Medicaid (under the Affordable Care Act [ACA]): Under the ACA, passed in 2010, states were required to expand Medicaid coverage to all individuals with incomes at or below 133% of poverty; in a later Supreme Court decision, this was made optional for states. Services provided include the full range of medical services; behavioral health; addiction treatment; and long-term care, residential, and community programs for the disabled and the frail elderly.
Fully insured Employer: An employer that pays a predetermined premium to the insurance carrier. The insurance carrier assumes the financial risk for providing all contracted health care benefits.
Medicaid: A jointly funded state and federal program to provide health care for low-income Americans; requirements for basic services to be delivered are determined by the federal government, while additional services may be added by the states, resulting in every state having a unique Medicaid program.
Medicaid-eligible: Individuals who meet their state Medicaid program’s eligibility requirements; not everyone who is Medicaid-eligible is enrolled in Medicaid.
Medicaid beneficiary: An individual who has been determined to be eligible to receive Medicaid benefits and has enrolled in the program. This status can change if a person’s income changes.
Medicaid Managed Care Organizations (MCOs): Private organizations that contract with health care providers in a state to deliver specific services to Medicaid beneficiaries under the state’s Medicaid plan. MCOs operate on a capitated basis, meaning they are reimbursed on a per-capita basis per beneficiary. If the costs of providing care to a beneficiary are over the capitation fee, the MCO is responsible for absorbing the overage. If the costs of providing care to a beneficiary are below the capitation fee, the MCO retains the excess as profit. MCOs are also reimbursed for administrative costs and care management in addition to specific health care costs.
Medicaid State Plan and state plan amendment (SPA): Every state is required to file a Medicaid State Plan with the Centers for Medicare & Medicaid Services (CMS). If the state wants to make a change to its state Medicaid program by altering the services covered (within federal guidelines), or the populations covered, it must submit an SPA.
Original Medicaid: Delivers health care and other services for the populations originally identified as eligible in the Medicaid program: low-income pregnant women; young children; the elderly and the disabled, including the frail elderly in long-term care; the severely mentally ill; and the cognitively, physically, and developmentally disabled. Populations are covered for specific services, including obstetrical services, pediatrics, long-term care, behavioral health and addiction services, and long-term care, residential, and community programs for the disabled and the frail elderly.
Priority Populations: Defined in the DP23-0020 notice of funding opportunity (2320 NOFO) as those who have systematically experienced greater obstacles to health based on their racial or ethnic group, religion, socioeconomic status, gender, age, mental health, cognitive, sensory, or physical disability, sexual orientation or gender identity, geographic location, or other characteristics historically linked to discrimination or exclusion. Priority populations of focus will be determined by each recipient.
Self-insured employer: An employer that assumes the financial risk for providing health care benefits to its employees. Self-insured employers may still contract with an insurance carrier to handle the administrative aspects of the claims process. (This is also called an Administrative Services Only [ASO] health care plan.) Many medium-to-large employers are self-insured and are the most likely to be participants in regional or state organizations promoting prevention in health benefits. For this reason, it is most productive for 2320 recipients to focus their efforts on self-insured employers.
Wellness benefits/wellness programs: Benefits offered by an employer or health plan to improve and promote employee health and fitness. The employer or health plan generally offers premium discounts, cash rewards, gym memberships, and other incentives to encourage employees to participate. Wellness benefits are not part of a health insurance program. For the purpose of this strategy, an employer may offer the National DPP LCP in several ways: 1) by contracting with a CDC-recognized organization to offer the National DPP LCP at the worksite, 2) by subsidizing employee participation in community-based CDC-recognized organizations offering the National DPP LCP, or 3) by applying for CDC recognition to offer the National DPP LCP directly. While employers generally fund wellness programs with discretionary dollars, these programs can help build long-term sustainable support for the National DPP LCP by demonstrating successful outcomes.
1115 Demonstration Waiver: A process instituted by CMS to allow states to institute reforms that go beyond routine medical care and focus on evidence-based interventions that drive better health outcomes and quality of life improvements.
Strategy 6 Resources
National Diabetes Prevention Program Coverage Toolkit: This online toolkit was developed to provide information about the mechanics of covering the National DPP LCP. The following links are specific resources for Medicaid Coverage, participating public and private employers, and commercial payers:
Preventing Type 2 Diabetes: AMA Prevent Diabetes: This webpage provides helpful tools on preventing type 2 diabetes including tools for the team, tools for physicians, and a cost-savings calculator.
Trends in Employer-Sponsored Insurance Offer and Coverage Rates: This article provides information on trends in employer-sponsored insurance offer and coverage rates.
Diabetes Prevention Impact Toolkit: Use this Impact Toolkit to project the health and economic effects of the National DPP LCP program on your population at risk for type 2 diabetes.
Diabetes State Burden Toolkit: Use this tool to identify the health, economic, and mortality burden of diabetes in your state. This tool is particularly useful to determine what the projected outlook of health and economic costs will be if nothing is done to prevent type 2 diabetes.
Working with Employers and Insurers Guide: This implementation guide will help you learn how to work with employers and insurers to engage, recruit, and enroll people with prediabetes who have health insurance coverage in the National DPP LCP to prevent or delay the onset of type 2 diabetes.
Employer Path to Adoption (cdc.gov) This resource provides a checklist to guide employers through making the decision to offer the National DPP lifestyle change program as a covered benefit at your organization.
Covering the National DPP as an Insurance/Wellness Benefit (cdc.gov): This site provides resources for employers and public and private payers that offer the National Diabetes Prevention Program (National DPP) lifestyle change program as a covered benefit for employees, members, or beneficiaries, or are considering doing so.
CDC 6/18 Initiative: Prevent Type 2 Diabetes: This initiative connects health care purchasers, payers, and providers with CDC researchers, economists, and policy analysts to find ways to improve health and control costs with the 6|18 interventions.
Healm: Diabetes Prevention For Your Workforce: This interactive online tool provides comprehensive guidance for employers wishing to design and implement an effective type 2 diabetes prevention program benefit for their employees.
Strategy 7 Key Terms
CDC-recognized National DPP Organization: An organization that is recognized by CDC based to their ability to meet certain standards (e.g., following a CDC-approved curriculum, using trained Lifestyle Coaches, submitting data to CDC every six months) and demonstrate successful delivery of the National DPP LCP.
Medicare Diabetes Prevention Program (MDPP) Supplier: An organization with either preliminary or full (not pending) CDC-recognition that has successfully completed the Centers for Medicare & Medicaid Services (CMS) application to become an MDPP supplier. In UHAs, the UHO is the MDPP supplier. Subsidiary organizations bill CMS for reimbursement through the UHO.
Payer: A health maintenance organization, insurance company, management services organization, or any other entity that pays for or arranges for the payment of any health care or medical service, procedure, or product.
Priority Populations: Defined in the DP23-0020 notice of funding opportunity as those who have systematically experienced greater obstacles to health based on their racial or ethnic group, religion, socioeconomic status, gender, age, mental health, cognitive, sensory, or physical disability, sexual orientation or gender identity, geographic location, or other characteristics historically linked to discrimination or exclusion. Priority populations of focus will be determined by each award recipient.
Social Determinants of Health (SDOH): Non-medical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, as well as the wider set of forces and systems that shape the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies, racism, climate change, and political systems.
Subsidiary Organization: A community-based organization participating in the UHA that delivers the National DPP LCP and receives administrative support from the UHO. Subsidiary organizations may also be referred to as affiliates.
Sustainability: The Center for Public Health Systems Science at the Brown School, Washington University in St. Louis, defines sustainability capacity as the ability to maintain programming and its benefits over time. To improve capacity for sustainability, it suggests that organizations strengthen the structures and processes that exist within their programs to ensure that they can strategically leverage resources to weather the changes and challenges that will come their way (PSAT/CSAT – Program Assessment Sustainability Tool (sustaintool.org).
Umbrella Hub Arrangement (UHA): An overarching term that refers to the entire group, inclusive of the UHO, subsidiaries, and the billing platform. This term is distinct from the term UHO (see below). The UHA may also be referred to as the umbrella arrangement or hub arrangement.
Umbrella Hub Agreements: Contracts, charters, or other business documents. These can include but are not limited to a:
Contract between the UHO and subsidiaries detailing the roles, responsibilities, and expectations of all parties involved, including any financial arrangement between the UHO and subsidiaries.
Charter between the UHO and subsidiaries detailing the UHA’s mission, objectives, and purpose.
Master services agreement between the UHO and billing platform vendor detailing the roles, responsibilities, and expectations of all parties involved.
Business associate agreement and/or data use agreement detailing expectations for private health information and/or expectations for data use. These agreements are often between subsidiaries and the billing platform vendor or between the UHO and billing platform vendor.
Umbrella Hub Organization (UHO): In a UHA, an organization with full or preliminary CDC recognition, agrees to serve as the sponsoring hub for a group of organizations (subsidiaries) that have CDC pending, preliminary, or full recognition. The UHO provides administrative support to subsidiary organizations so those organizations can focus on delivering the National DPP LCP.
UHOs provide administrative support by defining the mission and vision of the UHA, providing support with billing and claims platforms, assisting with financial sustainability, establishing communication and coordination protocols, and identifying and recruiting subsidiaries. Please refer to this guide for further clarification on terminology: UHA Terminology Guide
Strategy 7 Resources
UHAs - National DPP Coverage Toolkit This resource provides information and resources for establishing and sustaining a UHA.
UHA Overview This page provides an overview of a UHA and guidance for organizations interested in becoming a UHO or supporting the operation of a UHA.
UHA Landscape Assessment This tool is intended to serve as a guide for conducting a landscape assessment for UHAs.
Business Model for UHAs This tool describes a business model design for the successful operation of a UHA.
Reimbursement for UHAs This page provides an introduction into the components of the MDPP supplier application followed by information on other payer types.
Sustaining UHAs This page outlines how UHAs can create a sustainable arrangement for the UHO and each subsidiary.
UHA Terminology Guide This guide contains terminology related to UHAs for organizations working towards sustainability of the National DPP LCP. Note that this guide will continue to be updated.
Sample Charter for UHA Participation This document provides an example of a charter and is intended to be educational in nature.
UHA Application This links to the National DPP UHA Guidance and Application for CDC-recognized organizations.
UHA Milestone Chart/UHO Organization Checklist The UHA Milestone Chart illustrates the four phases of UHA development. The UHO Checklist outlines the tasks associated with each phase of the UHA Milestone Chart and is intended to help UHOs create a work plan for the administrative activities that are needed to develop and sustain a UHA.
Strategy 8 Key Terms
Acquire FHWP: Method of procuring a FHWP, which may differ for each FHWP, e.g.,:
funded recipient purchases program curriculum and supporting materials
funded recipient licenses the program or pay a user fee
These could be one-time fees or annual fees
Adaptation/Tailoring: Thoughtful and deliberative process to change the design or delivery of an evidence-based program to improve its fit or effectiveness in a particular context (e.g. language and cultural considerations if delivering to a new population). Care must be taken to retain the core components to preserve fidelity of the intervention. The FHWP service provider will provide guidance on what parts of the FHWP can be adapted freely (e.g., recipes); what adaptations should be approached with caution; and what program components must not be changed. Adaptations can also be related to implementation strategies, which might include referral, recruitment, enrollment, and engagement.
Attendance: presence at a FHWP session. This metric occurs after enrollment. This measure reflects factors about the individual’s ability to participate in the program (e.g. removing barriers or participant readiness).
Barrier: Conditions that prevent successful implementation of the intervention. These can be related to policies (inability to bill insurance for a health service), organizational (lack of leadership support or staffing), or individual (lack of reach to the populations in need and lack of transportation to reach the intervention).
Best Fit FHWP: This is the FHWP that the funded recipient, community partners and relevant stakeholders decide is the most appropriate program for their community’s priority age group and population based on the needs assessment.
Cohort: A group of participants in the FHWP, who enroll in the program at the same time. Or a series of program sessions.
Core components: Also considered the “active ingredients” of the program, these elements are essential for evidence-based programs and practices to produce desired outcomes (e.g., 26 contact hours). Core components must be retained throughout implementation, including when making adaptations.
Engagement: Process of working with and involving partners, stakeholders, and the community in order to implement the FHWP; the degree of engagement of the community will directly impact priority populations awareness of the program.
Enrollment: when a child is registered and assigned to a FHWP session. Enrollment typically follows these steps:
Referral received or family inquiries about program
Staff review the program with family and screen for eligibility
Child is registered for the FHWP and assigned to initial session of the program
Program attendance is the metric after enrollment.
is registered for the FHWP and assigned to initial session of the program
Program attendance is the metric after enrollment.
Family Healthy Weight Program (FHWP): A family healthy weight program is an intensive, family-based lifestyle change treatment program for children aged 2-18 years with overweight and obesity. These programs are for children and their caregivers and deliver a minimum of 26 contact hours over 3 to 12 months. FHWPs have reported benefits, including improvement in health, nutrition, physical activity, and health-related quality of life.
FHWP service provider: The organization that has developed and provides ongoing technical assistance for that specific FHWP.
Fidelity: The degree to which the program is implemented as it was intended. Implementing an effective intervention without compromising the core components is essential for the intervention’s effectiveness.
Funded recipient: The organization that received funding under the cooperative agreement, i.e., HOP or REACH.
Implemented FHWP: A FHWP is considered “implemented” once the implementation partner completes its initial session of its first cohort at a site.
Implementing partner(s): The partner organization that is offering the FHWP. This could be a community or clinical organization depending on which FHWP is selected.
Implementation plan: Steps team should take to have successful implementation. (This should not be confused with the work plan). Specific tasks include those that will improve the adoption, infrastructure (e.g., data systems, staff training) and ongoing improvement of needed practices, programs, or frameworks of the FHWP. This should also include:
Developing plans for hiring staff, training staff, and addressing staff turnover.
Arranging for physical space
Adherence monitoring
Addressing participant context and barriers to maximize engagement
Communication/marketing plan to support reach and referral
Implementation tracking (including measures of adaptation, fidelity, reach, referral, and engagement),
Budgeting
Planning for sustainability
Informal agreement: A written agreement between the funded recipient, implementing partner and the community representative that documents the roles and responsibilities of each entity and how they are involved with the FHWP implementation. A formal MOU or MOA may be necessary depending on the requirements or preferences of the organizations involved.
New FHWP site: A new FHWP will have been implemented when the implementing partner begins its first cohort at a site, this is defined by the date of the initial session of that cohort. A new FHWP site includes expanding implementation of existing FHWP’s to a new site.
Pre-implementation planning: Pre-implementation planning includes the identification of the many elements needed before the program is implemented. Pre-planning is critical for the long-term sustainability of the FHWP. This planning accounts for the features of the community and its preferences, community assets, the cultures of the implementing partners, and their involvement in the implementation process.
Referral (including referred individual and self-referral): the act of directing a family, or self-direction to the FHWP implementing partner to gain further information on the program or be screened for eligibility. Receipt of referral is when the FHWP implementing partner staff receive the name of the child who is potentially appropriate for FHWP enrollment (e.g., self-referral is a parent calling to inquire about the program, a community organization sending the FHWP partner a list of names and contact information for families who are interested in the program).
Setting and Modality: This refers to where and how a FHWP is delivered.
Setting examples: YMCA, Clinic
Mode examples: in-person or virtual
Site: The specific physical location where a FHWP is implemented (e.g. YMCA of Decatur) if virtual, this is the hosting organization (YMCA of Decatur).
Sustainability: After the end of the cooperative agreement, the FHWP will continue to be delivered to support continued individual behavior change and associated benefits. To ensure long-term sustainability, planning for this must begin at the same time as planning the initial FHWP implementation.
Planning
The Childhood Obesity Research Demonstration (CORD): This resource provides information on the background of CORD projects, related publications, and recipients.
Find the Best Intensive Health Behavior and Lifestyle Treatment Program for You: This is a tool to determine recommended programs based on the target age group and implementation plan.
CDC-Recognized Family Healthy Weight Programs webpage: This resource provides an overview of CDC-recognized family healthy weight programs and program screening criteria.
Priority Strategy: Family Healthy Weight Programs webpage: This recourse provides background information, potential activities, and related resources for family healthy weight programs.
The Ready, Set, Change! Tool: a framework for assessing organizational readiness.
Implementing
National Implementation Research Network: Implementation Planning Tool: This tool can be used as a guide to initiate a new program, select a program, and plan for implementation.
The National Implementation Research Hexagon Tool: This tool can be used to assess program indicators and implementing site indicators. It is also used to consider how programs could advance equitable outcomes.
Oregon Social Learning Center’s Stages of Implementation Completion (SIC): This multi-step tool that outlines implementation processes and milestones.
CDC BMI-for-age growth charts: These are tools used by pediatricians, nurses, and parents to track the growth of infants, children, and adolescents.
Evaluating
The National Collaborative on Childhood Obesity Research’s (NCCOR) Toolkit for Evaluating Childhood Healthy Weight Program This toolkit provides an overview and guidance on program evaluation readiness.
The Wilder Collaboration Factors Inventory: This resource includes questionnaires and surveys to assess degree and strength of collaboration with an organization.
American Academy of Pediatrics Institute for Healthy Childhood Weight: Capacity Considerations for Obesity Evaluation and Treat: this can be used to reflect on current capacity related to obesity treatment.
Sustaining
NCCDPHP Knowledge to Action Framework: This framework describes high-level processes necessary to move from discovery into action through translation of evidence-based programs, practices, or policies.
The Program Sustainability Assessment (PSAT): This tool can be used to rate the sustainability capacity of a program.
Health Equity
Racial and Ethnic Approaches to Community Health (REACH). This national CDC program supports culturally appropriate programs to address a wide range of health issues among priority populations.
State Health Equity Toolkit. This toolkit provides public health practitioners with a systematic approach to program planning using a health equity lens.
Promoting Health Equity – A Resource to Help Communities Address Social Determinants of Health. This is a resource for public health practitioners and partners who want to develop initiatives to increase health equity in their communities.
Pathways to Population Health Equity. A framework and toolkit for public health practitioners to address health equity within their communities.
Strategy 9 Key Terms
Diabetes Self-Management Education and Support (DSMES): The ongoing process of facilitating the knowledge, skills, and capabilities necessary for diabetes self-care, as well as activities that assist a person in implementing and sustaining the behaviors needed to manage their condition on an ongoing basis, beyond or outside of formal self-management training (Powers et al., 2020, Davis et al., 2022).
Diabetes Self-Management Training (DSMT): The Centers for Medicare & Medicaid Services (CMS) uses the term “training” (DSMT) instead of “education and support” (DSMES) when defining the reimbursable benefit. This term relates specifically to Medicare billing.
DSMES Recognition and Accreditation: Recognition and accreditation help ensure that DSMES services offer quality education. CMS has authorized 2 organizations, the American Diabetes Association (ADA) and Association of Diabetes Care and Education Specialists (ADCES), to grant recognition or accreditation for DSMES. ADA uses the term recognition, while ADCES uses the term accreditation. The 2 terms involve similar processes to evaluate DSMES services. Both organizations rely on the 2022 National Standards for DSMES (Davis et al., 2022).
Independent Pharmacy: A retail pharmacy that is not directly affiliated with any chain of pharmacies and is not owned (or operated) by a publicly traded company. Independent pharmacies are pharmacist-owned, privately held businesses in varying practice settings.
Medicare Diabetes Prevention Program (MDPP) Supplier: An organization with either preliminary or full (not pending) CDC-recognition that successfully completes the CMS application to become an MDPP supplier. In UHAs, the umbrella hub organization (UHO) will be the MDPP supplier; subsidiary organizations will bill CMS for reimbursement through the UHO.
National Diabetes Prevention Program (National DPP) Lifestyle Change Program (LCP): A structured, evidence-based, year-long lifestyle change program to prevent or delay onset of type 2 diabetes in adults with prediabetes or at risk of developing type 2 diabetes. The program is group-based, facilitated by a trained lifestyle coach, and uses a CDC-approved curriculum. The curriculum supports regular interaction between the lifestyle coach and participants; builds peer support; and focuses on behavior modification through healthy eating, increasing physical activity, and managing stress. The program may be delivered in-person, online, via distance learning, or through a combination of these delivery modes.
Pharmacist: A person who obtains a doctorate degree (B.S. degree in many cases before 2000) and is licensed by the state board of pharmacy within the state that he/she practices pharmacy. The professional curriculum is structured around an integrated approach to drug therapy management. The PharmD program emphasizes an integrated and problem-based approach to disease management as the core of the didactic and laboratory program of study. Many pharmacists will also pursue a 1 to 2-year residency program after formal training.
Pharmacy Chain: A pharmacy is considered a “chain pharmacy” if the organization consists of four or more stores (National Association of Chain Drug Stores, 2018).
Pharmacy Network: A group of pharmacies that have contracted with a health plan or pharmacy benefit manager to provide covered products and services to members. There are many national organizations that fit into this category, such as CPESN, the National Community Pharmacist Association, and the National Association of Chain Drug Stores. However, a “pharmacy network,” for the purpose of this strategy, may also include state pharmacy associations, a group of independent pharmacies, or a franchise of independent community pharmacies.
Pharmacy Technician: A person who is licensed by their state board of pharmacy to perform a wide range of tasks, such as helping pharmacists fill prescriptions, maintaining pharmacies, assisting with administrative work, and offering customer service (National Pharmacy Technician Association, n.d.). Pharmacy technicians can pursue formal training through an education and training program or learn on the job (Accreditation Council for Pharmacy Education, n.d.).
Bi-directional Services e-Referral (BSeR): A system that supports information going from the health care system to a specified community program or resource (e.g., a D-recognized organization offering the National DPP LCP and information returning from that program to the health care system). Ideally, bi-directional referral systems are integrated within the electronic health record (EHR). Bi-directional referrals help “close the loop,” allowing community programs to share information with health care provider(s) on the progress of the individuals they referred using an electronic platform.
Priority Populations: Defined in the 2320 NOFO as those who have systematically experienced greater obstacles to health based on their racial or ethnic group, religion, socioeconomic status, gender, age, mental health, cognitive, sensory, or physical disability, sexual orientation or gender identity, geographic location, or other characteristics historically linked to discrimination or exclusion. Priority populations of focus will be determined by each award recipient.
Subsidiary Organization: A community-based organization (CBO) participating in a UHA that delivers the National DPP LCP and receives administrative support from the UHO. Subsidiary organizations may also be referred to as affiliates.
Umbrella DSMES ADA-recognized/ADCES-accredited service: A DSMES service where an agency serves as the sponsoring organization to secure ADA-recognition or ADCES-accreditation, managing all the certification requirements, while other agencies serve as multi-sites or branch sites to deliver DSMES.
Umbrella Hub Arrangement (UHA): UHAs help connect community-based organizations (CBOs) with health care payment systems to pursue sustainable reimbursement for the National DPP LCP. The overarching term refers to the entire group, inclusive of the UHO, subsidiaries, and billing platform. This term is distinct from the term UHO (see below). The UHA may also be referred to as the umbrella arrangement or hub arrangement.
Umbrella Hub Organization (UHO): In a UHA, this organization, with full or preliminary CDC recognition, agrees to serve as the sponsoring hub for a group of organizations (subsidiaries) that have CDC pending, preliminary, or full recognition. The UHO provides administrative support for subsidiary organizations so those organizations can focus on delivering the National DPP LCP. This includes support with communication and coordination protocols, identification and recruitment of subsidiaries, and billing and claims platforms to help achieve financial sustainability.
National DPP Umbrella Hub Agreements: This term refers to contracts and charters or other business documents. These can include, but are not limited to, the following:
Contract between UHOs and subsidiaries detailing the roles, responsibilities, and expectations of all parties involved, including any financial arrangement between the UHO and subsidiaries.
Charter between the UHO and subsidiaries detailing the UHA’s mission, objectives, and purpose.
Master services agreement between the UHO and billing platform vendor detailing the roles, responsibilities, and expectations of all parties involved.
Business associate agreement and/or data use agreement detailing expectations for private health information and/or expectations for data use. These agreements are often between subsidiaries and the billing platform vendor and between the UHO and billing platform vendor.
Strategy 9 Resources
CDC DSMES Technical Assistance Guide: This tool identifies four key drivers that influence DSMES access and participation: 1) availability of DSMES services, 2) payers and payment mechanisms, 3) referral policies and practices, and 4) willingness of people with diabetes to participate in DSMES services.
CDC DSMES Toolkit: This toolkit is used to increase access to and participation in DSMES services among people with diabetes. The toolkit provides available resources and tools in one place to assist with the development, promotion implementation, and sustainability of DSMES services.
2022 National Standards for DSMES: The Standards define timely, evidence-based, quality DSMES services that meet or exceed the Medicare DSMT regulations and assist those providing or wishing to provide DSMES.
Action Guide for Pharmacists, National DPP: This guide provides information on how the pharmacy workforce can support the National DPP. Provides examples and information on opportunities for pharmacies from promoting awareness all the way to being involved in a UHA.
ADCES DSMES Directory: This directory allows users to search for an ADCES accredited DSMES program in the local area.
ADA DSMES Directory: This directory allows users to search for an ADA-recognized DSMES program in the local area.
Diabetes Management North Carolina: This resource is for pharmacists pertaining to the set up and sustainability of DSMES services.
Engaging Pharmacists - National DPP Coverage Toolkit: This toolkit provides details and examples of how pharmacists can play specific roles and pursue sustainability in their practice setting.
The Pharmacist and Patient-Centered Diabetes Care: The American Pharmacists Association developed the Pharmacist and Patient-Centered Diabetes Care Certificate Training Program. The program provides comprehensive instruction in current diabetes concepts and standards of care and incorporates case studies and hands-on skills training focused on situations likely to be encountered and the services most needed in community and ambulatory care practice settings.
DPRP Registry of All Recognized Organizations: This registry lists contact information for all CDC-recognized organizations that deliver evidence-based type 2 diabetes prevention programs in communities across the US. All of these programs have agreed to use a CDC-approved curriculum that meets the duration, intensity, and reporting requirements described in the DPRP Standards.
Medicare Diabetes Prevention Program (MDPP) Billing and Payment Fact Sheet: This resource provides an overview of the billing process and payment structure for core, core maintenance and ongoing maintenance sessions.
Diabetes Resource Hub - National Center for Farmworker Health: This guide was created to facilitate setup and maintenance in community pharmacies, whether in a health center or independent setting. Provides information on why pharmacies might consider offering these services. This guide will also provide the steps for achieving and maintaining accreditation or recognition and cover additional details such as referrals and billing.
UHAs (National DPP Coverage Toolkit): This toolkit provides information and resources for establishing and sustaining a UHA:
UHA Overview: This page gives an overview of UHAs and presents the case for creating a UHA.
Business Model for UHAs: A sample UHA business model is introduced on this page that is intended to provide a framework for UHOs.
Reimbursement for UHAs: This page provides an introduction into the components of the MDPP supplier application followed by information on other payer types.
Sustaining UHAs: This page gives guidance on avenues to support the sustainability of the UHA in addition to contracting with health care payers.
Strategy 10 Key Terms
Bi-directional Services e-Referral (BSeR): A system that supports information going from the health care system to a specified community program or resource (e.g., a CDC-recognized organization offering the National DPP LCP) and information returning from that program to the health care system. Ideally, bi-directional referral systems are integrated within the electronic health record (EHR). Bi-directional referrals help “close the loop,” allowing community programs to share information back with the health care provider(s) on the progress of the individuals they referred using an electronic platform.
BSeR Fast Health Care Interoperability Resources (FHIR) Implementation Guide (IG): A guide that standardizes how systems should use FHIR to communicate, specifically within the domain of bi-directional e-referrals.
Business Associate: A person or entity, other than an employee of a covered entity, who performs activities on behalf of or provides certain services to a covered entity by accessing protected health information (PHI). A business associate may also be a subcontractor who creates, receives, maintains, or transmits PHI on behalf of another business associate.
Business Associate Contract: A contract that is common in the health care industry that serves to clarify and limit the permissible uses and disclosures of PHI by the business associate, based on the relationship between the parties and the activities or services being performed.
Closed-loop Referral: The ability of health care providers to receive information back from CBOs or social service organizations (or in some cases patients) on the outcomes of their referrals.
Community Information Exchange (CIE): An ecosystem comprised of multidisciplinary network partners that use a shared language, a resource database, and an integrated technology platform to support enhanced community care planning. Care planning tools enable partners to integrate data from multiple sources and make bi-directional referrals to create a shared longitudinal record. By focusing on these core components, a CIE enables communities to shift away from a reactive approach toward proactive, holistic, person-centered care.
Community Resource Platform: A closed-loop system designed to facilitate multi-directional communication, referrals, and coordination across sectors.
Community Readiness: Reflects the existing landscape of needs, assets, initiatives, opportunities, and challenges in the community of focus, including shared interests and capacities.
Community Stewardship: Entails the development of shared rights and responsibilities in the process of co-design, evaluation, and decision-making. The meaning of “community” can vary across contexts, populations, geographies, infrastructures, and arrangements.
Convening Organization: An organization that rallies the community, develops and solidifies relationships among network participants, creates a governance structure, and selects a referral platform.
Data Sharing Agreements: Agreements that set out the legal authority that supports data sharing, establishes and documents the terms of sharing, and delineates responsibility for monitoring and accountability. These formal agreements clearly outline what information each partner will exchange and be able to access.
Dead-end Referrals: Referrals made to organizations that are not currently active in the network, thereby creating a situation where those referrals will not be picked up (i.e., they “hit a dead-end”).
Electronic Health Record (EHR): An electronic version of a patient’s medical history. It is maintained by the provider over time and may include key administrative and clinical data relevant to care under a particular provider, including demographics, progress notes, problems, medications, vital signs, past medical history, immunizations, laboratory data, and radiology reports.
Fast Health Care Interoperability Resources (FHIR): A widely adopted, open-source modern health interoperability standard. FHIR defines two core areas to enable communication between systems:
The way data should be accessed and managed – Reading or searching records, updating records, creating new records, or deleting records.
The structure, or shape, of the data – How parts of a health care record are represented, consistent names of data elements, what everything means, and how it should be used.
Fast Health Care Interoperability Resources (FHIR) Implementation Guides (IGs): Guides that define how FHIR should be used for a specific use case or domain. The FHIR IG process is a collaborative effort between sponsors, developers, subject matter experts (SMEs), and community partners.
Governance: The establishment and oversight of a common set of behaviors, policies, and standards that enable trusted electronic health information exchange among a set of participants. Governance involves decision-making processes and groups at three levels: institutional, administrative, and data governance. Consider the multi-tiered governance framework to help drive decision making. Refer to pages 63-69 in the Social Determinants of Health Information Exchange Toolkit for specific opportunities related to this activity.
Gravity Project: Exists to serve as an open public collaborative to advance health and social data standardization for health equity by building and promulgating consensus driven SDOH data standards for health and social care interoperability and use among multi-stakeholders.
Gravity Project SDOH Standardization: This project seeks to identify coded data elements and associated value sets [possible values or responses for a data element] to represent social determinants of health data documented in EHRs across four clinical activities: screening, diagnosis, planning, and interventions. The project is focused on three specific social risk domains: food insecurity, housing instability and quality, and transportation access. These domains were selected based on existing research linking these factors with health and utilization and on active experiments related to these domains, including in federal, state, or local demonstration projects.
Health Data Utility (HDU): Statewide models or entities with the advanced technical capabilities to combine, enhance, and exchange electronic health data across care and service settings for treatment, care coordination, quality improvement, and public and community health purposes. HDUs enable specific, defined use cases with privacy and security that exceeds federal minimum standards established by the Health Insurance Portability and Accountability Act (HIPAA) and as amended by HITECH to ensure patient privacy and appropriate data use.
Health Equity: The state in which everyone has a fair and just opportunity to attain their fullest health potential and no one is disadvantaged because of social position or other socially determined circumstances.
Health Information Exchange (HIE): Enables the electronic transmission of health -related data among health care facilities. HIEs have traditionally facilitated access to and retrieval of clinical data to provide safer and more timely, efficient, effective, and equitable patient-centered care.
Verb: The electronic sharing of health-related data between two or more organizations facilitated by applied standards for use by a variety of stakeholders to inform health and care.
Noun: Organizations within the United States that provide HIE technology and services at a state, regional, or national level and often work directly with communities to promote secure sharing of health data.
Health Insurance Portability and Accountability Act (HIPPA): A federal law that requires the creation of national standards to protect sensitive PHI from being disclosed without patients’ consent or knowledge.
Health Level 7 (HL7): A standard development organization that develops specifications to structure, encode, and exchange electronic health information. HL7 standards define how information is packaged and communicated from one party to another, setting the language, structure and data types required for seamless integration between systems. These standards support clinical practice and the management, delivery, and evaluation of health services.
HL7 FHIR Connectathons: Events centered on developing HL7 FHIR specifications, including resources, profiles, and implementation guides. For an IG to be published, it must participate in at least one Connectathon and go through a balloting period.
Implementation Services: Inclusive of technical services (e.g., defining requirements, [interoperability] standards specifications, and integration with existing infrastructure) and programmatic services (e.g., defining use cases, workflow design/redesign), as well as support for adoption and utilization by individuals and the community.
Interoperability: Sharing information seamlessly. An interoperable health IT environment makes this possible. EHR interoperability enables better workflows and reduced ambiguity and allows data transfer among EHR systems and health care stakeholders. Ultimately, an interoperable environment improves the delivery of health care by making the right data available at the right time to the right people.
Managed Care Organization (MCO) Contracting: States/counties can integrate language into MCO contracts that encourage collaboration with communities (e.g., social service referrals).
Multi-Stakeholder, Cross-Sector Governance: Public-private partnerships that include state and federal agencies, health care system representatives, consumers, community service organizations, and others depending on implemented use cases. Strategic community and stakeholder engagement in governance informs priorities and increases transparency and accountability. Trust is strengthened with cross-sector input.
Priority Populations: Defined in the 2320 notice of funding opportunity as those who have systematically experienced greater obstacles to health based on their racial or ethnic group, religion, socioeconomic status, gender, age, mental health, cognitive, sensory, or physical disability, sexual orientation or gender identity, geographic location, or other characteristics historically linked to discrimination or exclusion. Priority populations of focus will be determined by each award recipient.
Multi-Directional e-Referral (MDeR): Supports information sharing across multiple systems (health care, CBOs, human (social) service organizations) thereby allowing the different service providers to help “close the loop” in patient care.
Referral: A healthcare system referral is a process whereby a patient is recommended to receive a specific service or program delivered by another entity.
Social Determinants of Health (SDOH): The nonmedical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies, racism, climate change, and political systems.
Social Services: Housing, food, transportation, and other forms of support provided by government and private, for-profit, and nonprofit organizations for the benefit of the community and to promote social well-being.
State Health IT Governance: Enables statewide data exchange across sectors and settings in support of health priorities and multiple agency data needs for data-informed policy, programs, and interventions.
Technical Infrastructure and Data Standards: Alignment of hardware, software, data, processes, and standards to enable scalable and interoperable data and IT systems.
Strategy 10 Resources
Programmatic Infrastructure
MDeR Landscape Assessment: This document provides guided questions for recipients working on MDeR to help them identify existing resources and needs.
Health Data Utility Framework - A Guide to Implementation: This resource is intended to guide states/counties/regions, HIEs, and community partners in the design and implementation of an HDU.
DASH — Data Across Sectors for Health: Data Across Sectors for Health (DASH) is a national initiative that helps communities share data so that every person can reach their full potential for health.
Community Information Exchanges and SDOH Resources
Community-Clinical Linkages for the Prevention and Control of Chronic Diseases: A Practitioner's Guide: Community-clinical linkages (CCLs) are defined as connections between community and clinical sectors to improve population health. This document guides public health practitioners on key strategies to implement community-clinical linkages.
Community-Clinical Linkages: Implementing an Operational Structure with a Health Equity Lens: This guide is for practitioners in public health, community, and clinical sectors. It aims to help practitioners incorporate health equity when organizing a CCL’s structure and supporting its operations.
Social Determinants of Health 201 for Health Care: Plan, Do, Study, Act (PDSA): This discussion paper provides frameworks and approaches to using PDSA cycles to implement SDOH, social risk factors, and HRSNs efforts.
211 Los Angeles County Taxonomy: This site is a support tool which allows licensed subscribers to search and access the 211 LA County Taxonomy in a variety of ways.
211s Nationwide: This website is the main webpage for 211, the 3-digit number designated by the Federal Communications Commission (FCC) for information and referrals to social services and other assistance.
Iowa Healthcare Collaborative SDOH Toolkit: The toolkit is organized around the three stages of SDOH: Prepare, Test, and Spread. It provides tools for each of the 21 concepts discussed, with guidance related to when an organization may want to use each tool or concept.
FHIRed-SHIP: An approach to Health Equity by Design for 21st Century Healthcare: This resource describes Dell Med’s development of a FHIR-enabled Social and Health Information Platform (FHIRed-SHIP).
Community Resource Referral Platforms: A Guide for Health Care Organizations: In this report, SIREN researchers synthesize research findings to offer a guide for safetynet health care providers regarding the current landscape of community resource referral technology platforms.
SDOH Information Exchange Toolkit: This toolkit can support communities working toward achieving health equity through SDOH information exchange and the use of interoperable, standardized data to represent SDOH.
Health Level 7 (HL7) Courses: This website provides information on HL7 and available HL7 training and education.
The Gravity Project: This resource provides information on a collaborative public-private initiative with the goal of developing consensus-driven data standards to support the collection, use, and exchange of data to address SDOH.
SDOH Clinical Care FHIR Implementation Guide Standard: This HL7 Implementation Guide (IG) defines how to exchange SDOH content defined by the Gravity Project using the HL7 FHIR standard.
The Gravity Project Technical Workstream Supplemental Guide: This supplemental guide supports the SDOH Clinical CareIG.
Pilots Workstream Gravity Project - Confluence This page provides information on how to get involved with the Pilot Workstream to drive implementation of Gravity Project terminology and technical standards and evaluate these standards for continuous improvement.
Screening Tools And Tool Kits - NASDOH This page links to 3 SDOH screening tools and toolkits provided by the National Alliance to Impact the SDOH (NASDOH) – the Health Leads Screening Toolkit; Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE); and EveryONE Project Social Needs Screening Tool.
AIRS Standards for Information and Referral Services This website provides information on the Alliance of Information and Referral Systems (AIRS), the professional membership association for community Information and Referral (I&R).
AIRS Standards and Quality Indicators for Professional Information and Referral The AIRS Standards establish reference points that define expected practices within the field of I&R and can be used to measure the compliance of organizations to these requirements.
CDC Public Health Use Case Workgroup- Gravity Project This resource provides information on a cross-sector SDOH Public Health Use Case Workgroup established by CDC to engage public and private sector partners to advance SDOH data exchange for chronic disease prevention and health promotion. This workgroup follows the Gravity Project framework.
National Information
Civitas Annual Conference This webpage provides details on the annual Civitas Networks for Health Conference.
ONC’s SDOH Information Exchange Learning Forum This learning forum, sponsored by the Office of the National Coordinator (ONC), brings together health care providers, community-based organizations, government, payers, HIE networks, IT platform developers, innovators, and other partners to share lessons learned, promising practices, and challenges related to exchanging SDOH data.
Technological Infrastructure
Standardized API for Patient and Population Services | HealthIT.gov This Certification Companion Guide (CCG) is an informative document designed to assist with health IT product development.
Standards Version Advancement Process, Approved Standards for 2020 (healthit.gov) This resource provides information on the Standards Version Advancement Process (SVAP), which permits developers to voluntarily update health IT products certified under the ONC’s Health IT Certification Program to newer versions of adopted standards and implementation specifications.
Data Governance Checklist (PDF) (ed.gov) This checklist is to assist stakeholder organizations with establishing and maintaining a successful data governance program to help ensure the individual privacy and confidentiality of education records.
Federal Data Strategy Data Government Playbook This playbook is intended to help agencies improve their organizational leadership for leveraging data as a strategic asset, including supporting strong data governance and data protection and security.
Data Governance Implementation Checklist This website provides a sample data governance implementation checklist to help remind agencies of what needs to be done and what to avoid when starting the implementation process.
Health Literacy Universal Precautions Toolkit: The PDSA toolkit is a way to test a change that is implemented. This website outlines the four steps for testing and implementing health literacy tools.
Interoperability in Action
Administration for Community Living (ACL) Social Care Referral Challenge: This website provides resources from winners of the ACL Social Care Referral Challenge, competition that sought IT solutions to support health care systems and CBOs in partnering to provide holistic health and social care for older adults and people with disabilities.
ONC Leading Edge Acceleration Projects (LEAP): This resource provides information on the LEAP in Health IT funding opportunity, which addresses well-documented and fast emerging challenges that inhibit the development, use, and/or advancement of well-designed, interoperable health IT.
CMS Accountable Health Communities Guide for Social Needs Screening Tool: This document describes the HRSN Screening Tool from the Accountable Health Communities (AHC) Model and shares promising practices for universal screening.
Strengthening the Technical Advancement & Readiness of Public Health via HIE Program (The STAR HIE Program): This page explains the objectives of the STAR HIE Program, a $5 million cooperative agreement program designed to strengthen and expand the ability of HIEs to support public health agencies in their response to public health emergencies and pandemics such as COVID-19.
Stakeholder Engagement and Collaborative Learning
Social Determinants of Health: This resource outlines the Office of the National Coordinator’s focuses on four key areas for using health IT to advance the interoperability and use of SDOH data.
Public Health IT (PHIT) Workforce Development Program: This resource explains the PHIT Workforce Development Program and its recipients.
StratsHealth Co-Creation Summary: This resource describes the co-creating shared approach to social needs resource referrals in Minnesota.
Standards
ONC Certification Program: This website provides an overview of the ONC’ Health IT Certification Program, which ensures that health IT meets the technological capability, functionality, and security requirements adopted by the US Department of Health and Human Services.
ONC Interoperability Standards Advisory (ISA): This resource provides details about ONC’s ISA process, which is intended to coordinate the identification, assessment, and determination of recognized interoperability standards and implementation specifications for industry to use in fulfilling clinical health IT interoperability needs.
ONC Standards Bulletins This resource provides links to ONC’s Standards Bulletin, a periodically published communication for health care stakeholders that includes updates about ONC health IT standards initiatives.
U.S. Core Data for Interoperability (USCDI) This website links to all versions of the USCDI documents, which are a standardized set of health data classes and constituent data elements for nationwide, interoperable HIE.
Spotlight on HHS Resources
SHARP Function Checklist: Decision Points for CBOs Considering Working with Social Health Access Referral Platforms (SHARP): The guide linked on this website provides information about the issues CBOs should consider when deciding whether to work with a SHARP and can help ensure that CBOs have informed discussions with SHARPs and health care entities to utilize these platforms effectively.
Office of the Assistant Secretary for Planning and Evaluation (ASPE) – Addressing Social Determinants of Health In Federal Programs: This resource includes three documents that: 1) explain why DHHS has identified addressing SDOH as a major priority for the Department; 2) describe DHHS’ strategic approach and specific actions the Department is taking to address SDOH; and 3) link how these actions build on evidence in the field on what works.
Community Care Hub (CCH): a community-focused entity that organizes and supports a network of community-based organizations providing services to address health-related social needs (ACL, 2022). CCHs are supported by a variety of groups including ACL, CMS, and CDC. Note: UHAs are similar to CCHs (see strategy 7), but UHAs, to date, have focused exclusively on offering the LCP.
Health related social needs (HSRN): HRSN are frequently identified as root causes of disparities in health outcomes. The term HRSN is used instead of social determinants of health (SDOH) to emphasize that HRSNs are a proximate cause of poor health outcomes for individual patients as opposed to SDOH, which is a term better suited for describing populations.
Social Determinants of Health (SDOH): SDOH are the nonmedical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies, racism, climate change, and political systems.
Streamlined reimbursement: Streamlined reimbursement, for purposes of this strategy, means developing payment mechanisms for reimbursement of the LCP that do not require claims submission from the LCP (e.g., vouchers or participation in a capitation system where community partners are reimbursed for their share of the capitated payment rate.) For example, the CCH may negotiate a capitated rate in exchange for care management and reimburse for community services on a fee for service basis.
Medicaid Authorities and Options to Address SDOH:
State Plan Authority: Optional state plan services (e.g., peer supports, case management). ACA Health Home option.
Section 1115 Waivers: Federal matching funds to test SDOH-related services and supports alternative payment models (APMs).
Medicaid Managed Care Flexibility: In-lieu of services, value-added services, procurement strategies, contract requirements, state directed payments. o Integrated care models: patient centered medical homes (PCMHs) and accountable care organizations (ACOs)
Integrated care models: Patient centered medical homes (PCMHs) and accountable care organizations (ACOS)
Medicaid In Lieu of Services (ILOS): An innovative option states may consider employing in Medicaid managed care programs to reduce health disparities and address unmet health-related social needs (HRSNs), such as housing instability and nutrition insecurity, through the use of a service or setting that is provided to an enrollee in lieu of a service or setting (ILOS) covered under the state plan.
Social Determinants of Health (SDOH): The nonmedical factors that influence healthoutcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies, racism, climate change, and political systems.
Health Related Social Needs (HRSN)***: An individual’s unmet, adverse social conditions that contribute to poor health. These needs – including food insecurity, housing instability, unemployment, and/or lack of reliable transportation – can drive health disparities across demographic groups. An individual’s HRSN are a result of their community’s underlying SDOH (CMS, 2021).
Streamlined reimbursement: Streamlined reimbursement, for purposes of this strategy, means developing payment mechanisms for reimbursement of the National DPP LCP that do not require claims submission from the CDC-recognized program delivery organization (e.g., vouchers or participation in a capitation system where community partners are reimbursed for their share of the capitated payment rate). For example, the CCH may negotiate a capitated rate in exchange for care management and reimburse for community services on a fee-for-service basis.
Section 1115 Waiver Watch: Approvals to Address Health-Related Social Needs: This issue brief provides an overview of how Section 1115 waivers have been used to help address social needs, including a summary of these recent approvals.
Improving Health and Well-Being Through Community Care Hubs: This article from Health Affairs describes the roles and responsibilities of Community Care Hubs, provides examples of these organizations, and explores policy opportunities to maximize their role.
ACL Community Care Hub National Learning Community: ACL, in partnership with CDC, announces the selection of 58 organizations for participation in the Community Care Hub National Learning Community (NLC). These organizations will engage in one of two learning tracks to bring together organizations serving as Community Care Hubs that are either in development or interested in expansion.
Community Care Hubs: Making Social Care Happen: The resource is intended to offer a high-level overview of CCHs, identify existing operational CCHs among several well-known organizational models, and identify research that demonstrates the value proposition for health care entities to work with CCHs in pursuing opportunities to align health care and social care systems.
Moving Massachusetts Upstream (MassUP) Initiative: The MassUp initiative helps the government, health care systems, and communities collaborate to improve community health, lower costs, and reduce health inequities across populations in Massachusetts.
How are Payment Reforms Addressing SDOH? Policy Implications and Next Steps: This issue brief summarizes the current landscape of payment reform initiatives addressing SDOH, drawing on results from a systematic review of peer-reviewed and gray literature supplemented with scans of state health policies and proposed payment reform models.
Medicaid Authorities and Options to Address SDOH: This brief from the Kaiser Family Foundation describes options that federal Medicaid authorities may use to address enrollees’ SDOH and provides state examples, including initiatives launched in response to the COVID19 pandemic.
SDOH and Medicaid Payments: This article from Deloitte Insights describes steps states can take to factor SDOH into Medicaid payment policies.
Section 1115 Waivers | Addressing Health-Related Social Needs: This RTI article explains Section 1115 waivers and recent developments to promote coverage, access to and quality of care, improve health outcomes, reduce health disparities, and create long-term, more cost effective alternatives or supplements to traditional medical services.
Health-Related Social Needs: This webpage from the Centers for Medicare & Medicaid Services (CMS) encourages states to utilize authority under section 1115 of the Social Security Act to test a variety of options to more effectively address enrollees’ unmet HRSN and the downstream health impacts.
Health Care Payment Leaning & Action Network (HCPLAN): This organization is an active group of public and private health care leaders dedicated to providing thought leadership, strategic direction, and ongoing support to accelerate adoption of alternative payment models.
HCPLAN Overview: This PDF provides an overview of HCPLAN, its mission statement, and how the network has worked to accelerate the shift of value-based care in order to achieve better outcomes at lower cost.
Ensuring Access to Medicaid Services (CMS 2442-P) Notice of Proposed Rulemaking: This proposed rule by CMS is intended to increase transparency and accountability, standardize data and monitoring, and create opportunities for states to promote active beneficiary engagement in their Medicaid programs. A substantive component of these requirements focus on improving access to, and the quality of home and community-based services.
Incorporating Community-Based Organizations in Medicaid Efforts to Address Health-Related Social Needs: Key State Considerations - Center for Health Care Strategies (chcs.org)
Mechanisms: Broadly, this refers to the means by which CHW services are financially reimbursed. Examples include:
A 2014 update to the regulatory definition of Medicaid preventive services by the Centers for Medicare & Medicaid Services (CMS) allows coverage for preventive services provided by non-licensed providers, including CHWs, when those services are recommended by a physician or other licensed provider (42 CFR 440.130).
CHW services can also be covered under other benefits, such as the outpatient hospital services benefit (42 CFR 440.20), and through programs authorized under the Medicaid health homes state plan option created under Section 2703 of the Patient Protection and Affordable Care Act (ACA, P.L. 111- 148). This team-based care model allows states to establish health homes to coordinate and manage care for people who have chronic conditions. Several states have specified in their state plan amendments that health home teams can or must include a CHW.
Some states cover CHW services using Section 1115 Medicaid demonstration waivers by allowing CHWs to provide services to beneficiaries, providing incentive payments for activities related to CHWs, or by providing funding for CHW infrastructure (Medicaid and CHIP Payment and Access Commission [MACPAC], 2022).
CHW Scope of Practice: It is central to CHWs’ scope of practice to serve as a link between health/social services and the community to facilitate access to services and improve the quality and cultural competence of service delivery (American Public Health Association, 2020). A CHW also builds individual and community capacity by increasing health knowledge and self-sufficiency through a range of activities such as outreach, community education, informal counseling, social support, and advocacy. The roles and tasks of individual CHWs will vary based on their organizations and the needs of the populations served. A list of CHW competencies, with example activities, is provided below:
Cultural Mediation among Individuals, Communities, and Health and Social Service Systems
Educate individuals and communities about how to use health and social service systems (including understanding how systems operate).
Educate systems about community perspectives and cultural norms (including supporting implementation of Culturally and Linguistically Appropriate Services [CLAS] standards).
Build health literacy and cross-cultural communication.
Care Coordination, Case Management, and System Navigation
Participate in care coordination and/or case management.
Make referrals and provide follow-up.
Facilitate transportation to services and help address other barriers to access.
Document and track individual and population level data.
Inform people and systems about community assets and challenges.
Providing Coaching and Social Support
Provide individual support and coaching (e.g., CHWs can be trained as National DPP lifestyle coaches).
Motivate and encourage people to obtain care and other services.
Support self-management of disease prevention and management of health conditions (e.g., CHWs can serve as part of a team providing DSMES services).
Plan and/or lead support groups.
Advocating for Individuals and Communities
Advocate for the needs and perspectives of communities.
Connect to resources (e.g. food and housing).
Building Individual and Community Capacity
Train and build individual capacity with CHW peers and among groups of CHWs.
Implementing Individual and Community Assessments
Participate in design, implementation, and interpretation of individual-level assessments (e.g., home environmental assessment).
Participate in design, implementation, and interpretation of community-level assessments (e.g., windshield survey of community assets and challenges, community asset mapping).
Conducting Outreach
Engage in case-finding/recruitment of individuals, families, and community groups to services and systems.
Follow-up on health and social service encounters with individuals, families, and community groups; conduct home visits to provide education, assessment, and social support.
Present at local agencies and community events.
CHW Sectors: Medical (hospital, health centers, primary care, oral health), public health (local and state health departments and non-profits), education (k-12, parent supports and colleges), housing, food systems (pantries, soup kitchens, and nutrition centers), chronic disease management (diabetes, heart disease and stroke, HIV/AIDS, cancer), mental health (family counseling, support groups, residential facilities, substance use treatment), advocacy (immigration, civil rights, voting rights), health plans (insurance enrollment, care coordination). Examples of CHW job titles can be found here (CDC, 2018). The type of CHW service delivery can be categorized into “covered” or “enabling,” depending on the operation of the organization and how the CHW functions.
CHW Qualities: CHW qualities help inform who is or becomes a CHW. Skills are something a person is capable of doing because they have learned, whereas qualities are personal characteristics or traits that can be enhanced but not taught. When CHWs are recruited, agreement on CHW qualities can help inform a job description and employer decisions. CHW qualities can also establish important parameters for the field and inform CHW training and educational decisions. For more information, visit the CHW Core Consensus Project (The Community Health Worker Core Consensus Project, 2016).
Covered Services: Services ordered by a licensed provider that are to be provided by a CHW. These services frequently include conducting intake assessments, social needs assessments, and providing health education to individuals and groups in conjunction with a health care team. Services can occur face-to-face with recipients in an outpatient clinic, hospital, client’s home, or other community settings. It is also important to ensure that the health education services being provided can be modified to meet clinical needs, cultural norms, and health literacy levels. Reimbursement of covered services may vary from state to state pending state plans and Medicaid coverage. Examples of CHW-covered services can be found in the policy brief developed by CDC’s Division for Heart Disease and Stroke Prevention, Addressing Chronic Disease through Community Health Workers, and in the technical assistance guide, States Implementing CHW Strategies. These and other resources can be found in the CHW Toolkit (CDC, 2011; CDC, 2014; CDC, 2019).
Enabling Services: Non‐clinical services that support the delivery of basic health services and facilitate access to comprehensive patient care as well as social services. They include case management, benefit counseling or eligibility assistance, health education and supportive counseling, interpretation, outreach, transportation, and education of patients and the community regarding the availability and appropriate use of health services. CHWs can be engaged to deliver these enabling services and to serve as advocates and health guides for clients with diabetes or prediabetes.
Priority Populations: Defined in the 2320 NOFO as those who have systematically experienced greater obstacles to health based on their racial or ethnic group, religion, socioeconomic status, gender, age, mental health, cognitive, sensory, or physical disability, sexual orientation or gender identity, geographic location, or other characteristics historically linked to discrimination or exclusion. Priority populations of focus will be determined by each award recipient.
A CHW Scope of Practice (SoP): Describes the roles that CHWs perform including cultural mediation, outreach, health education, social support, advocacy, capacity building, care coordination, provision of direct services, and research, evaluation, and assessment (https://www.cdc.gov/dhdsp/pubs/docs/CHW-PEAR.pdf). Central to CHWs’ scope of practice, is to serve as a link between health/social services and the community to facilitate access to services and improve the quality and cultural competence of service delivery (American Public Health Association, 2020).
Recipients should also refer to the Community Health Worker Core Consensus (C3) Project definition of the roles and competencies of CHWs, the Community Health Workers : Occupational Outlook Handbook: : U.S. Bureau of Labor Statistics (bls.gov) and the ADCES Practice Competencies for Diabetes Community Care Coordinators and Health Care Professionals.
Social Determinants of Health: Nonmedical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies, racism, climate change, and political systems.
Sustainability: The ability to maintain programs or services and their benefits over time. To improve capacity for sustainability, it suggested that organizations strengthen the structures and processes that exist within their programs to ensure that they can strategically leverage resources to weather the changes and challenges that will come their way. Relative to CHWs, sustainable financing refers to systems of budgeting for CHW positions without program or project grants or contracts. Funding may be sustained through continuous revenue streams that explicitly provide for or “cover” CHW services or within an employer’s overall revenue picture without a specific revenue source being dedicated to CHW services (Rush et al., 2020). The Rural Health Information Hub, supported by the Health Resources and Services Administration, suggests that there are three critical issues linked to the sustainability of CHW programs: 1) evaluation, 2) financing, and 3) credentialing (RHIhub, 2019).
Strategy 12 Resources
CMS/Medicaid Resources:
Medicaid Coverage of CHW Services: This issue brief discusses Medicaid coverage of CHW services.
Health Care Innovation Awards (HCIA) Meta-Analysis and Evaluators Collaborative: Annual Report Year 3: This document is the third annual report summarizing findings from work funded under the CMS HCIA program.
Integrating CHWs into Care Teams: This resource discusses how CHWs can be involved in care teams.
Diffusion of CHWs Within Medicaid Managed Care: A Strategy to Address Social Determinants of Health: This article discusses how CHWs can address SDOH for Medicaid managed care.
Center for Medicaid and CHIP Services Informational Bulletin: This memo summarizes CMS’ revised definition of “preventive care services” as stated in final rule CMS-2334-F: Medicaid and Children's Health Insurance Programs: Essential Health Benefits in Alternative Benefit Plans, Eligibility Notices, Fair Hearing and Appeal Processes, and Premiums and Cost Sharing; Exchanges: Eligibility and Enrollment.
Financing Approaches to Address SDOH via Medicaid Managed Care: A 12-State Review: This document from the Association for Community Affiliated Plans reviews ways to address SDOH through Medicaid managed care organizations in a sustainable way.
Additional Guidance on Use of In Lieu of Services (ILOS) and Settings in Medicaid Managed Care: This is a 2023 letter from CMS to State Medicaid Directors that reviews guidance on billing for ILOS and settings within Medicaid managed care.
On the Front Lines of Health Equity: CHWs: This CMS report discusses the benefits of CHW programs and how they can make positive impacts in the communities they serve.
Examples of CHW Models:
National Academy for State Health Policy - State CHW Models: This map summarizes information from a 50-state survey on states’ approaches to integrating CHWs into health care systems in key areas such as financing; education and training; and certification and provides information on CHW roles and scope of practice by state.
University of New Mexico Health Sciences Center Pathways to a Healthy Bernalillo County: This document describes the roles of community health navigators as care coordinators who connect at-risk residents to resources and follow their progress toward improved health outcomes.
Visión y Compromiso Key Workforce Priorities for the Community Transformation Model: This report focuses on the importance of workforce development for promotoras and others involved in supporting the community transformation model in communities throughout California.
Module 2: CHW Program Models – RHI hub Toolkit: This toolkit identifies six models for implementing CHW programs in rural areas.
An Emerging Model for CHW – Based Chronic Care Management for Patients with High Health Care Costs in Rural Appalachia: This CHW-based care model is focused on improving outcomes and lowering costs for high-risk individuals with diabetes in rural Appalachia.
A non-profit CHW model: CHWs/Promotores Training Center – El Sol Neighborhood Educational Center: This group provides technical assistance in the development and implementation of CHW and promotora training and interventions, including identifying and targeting community health priorities.
Expanding the Use of IMPaCT: A CHW Program: This CHW program improved quality of care and reduced hospital stays among people living in low-income neighborhoods using tailored support based on individuals’ needs and preferences.
CHW Certification and Financing:
CHW Return on Investment Study Final Report: Center for Program Evaluation, School of Community Health Sciences, University of Nevada, Reno: This study from the University of Nevada discusses the return-on-investment CHWs and CHW programs provide.
Minnesota Department of Human Services: Minnesota Health Care Programs Provider Manual: This resource provides examples of covered and noncovered CHW services as well as billing information for the state of Minnesota.
Financing Strategies to Support the CHW Workforce: Association of State and Territorial Health Officials Presentation: This presentation walks through different methods for budgeting for and financing CHWs and the benefits they provide to the communities they serve.
National Association of CHWs: Sustainable Financing of CHW Employment: This brief from the National Association of CHWs discusses how to employ CHWs in financially sustainable ways.
Other CHW Resources:
National Association of Chronic Disease Directors: Community Programs Linked to Clinical Services Resources for Diabetes and Hypertension: This site provides resources for reimbursement advocacy for CHWs.
Addressing Chronic Disease through CHWs: A Policy and Systems-Level Approach: This document provides guidance and resources for implementing recommendations to integrate CHWs into community-based efforts to prevent chronic disease.
A CHW Training Resource: This guide is an evidence-based, plain-language training resource and reference for CHWs as well as a curriculum that health educators, nurses, and other instructors can use to train CHWs.
The Community Guide: CHWs: This site provides recommendations from the Community Preventive Services Task Force on the evidence base for involving CHWs in various interventions, including diabetes management and type 2 diabetes prevention.
Diabetes Prevention: Interventions Engaging CHWs: This study reviews interventions that engage CHWs for diabetes prevention to improve glycemic (blood sugar) control and weight-related outcomes among people at increased risk for type 2 diabetes.
Center for Public Health Systems Science, George Warren Brown School of Social Work, Washington University in St. Louis: Program Sustainability Assessment Tool: This tool can be used to rate the sustainability capacity of programs or clinical practices.
APHA: CHWs: This site reviews general information regarding CHWs and their roles in the communities they serve.
Support for CHW Leadership in Determining Workforce Standards for Training and Credentialing: This study discusses the importance of CHW involvement in developing training and credentialing standards for the CHW profession.
CHW Forum: Engaging CHWs in the Development of a Statewide Infrastructure for Sustainability: The 2018 CHW Forum was led by the Division of Diabetes Translation to gather CHWs, CHW allies, and state health department representatives to explore issues related to developing a statewide infrastructure to promote long-term sustainability and financing of CHWs.
Body Mass Index (BMI): BMI is calculated by dividing a person’s weight in kilograms (or pounds) by the square of height in meters (or feet). BMI percentile for children is age- and sex-specific and is often referred to as BMI-for-age. Because children and teens are growing, the ranges of height, weight, and BMI vary by age and sex. As a result, BMI values need to be expressed as a percentile, which is relative to other children of the same sex and age.
Childhood Obesity: Using the CDC BMI-for-age growth charts, childhood obesity is defined as BMI at or above 95th percentile for age and sex.
Childhood Overweight: Using the CDC BMI-for-age growth charts, overweight is defined as a BMI from the 85th percentile to 94th percentile for age and sex.
Continuous Quality Improvement (CQI): A quality management process that encourages all health care team members to review the program implementation and continuously ask the questions, “How are we doing?” and “Can we do it better?”
Family Healthy Weight Programs (FHWP) & Benefits: FHWPs are evidence-based, family-centered childhood obesity interventions that aim to help children with overweight and obesity make progress towards a healthier weight and improved quality of life through positive behavior changes. FHWPs have reported benefits including improvement in nutrition, physical activity, and health-related quality of life (e.g., self-esteem); metabolic markers (e.g., blood pressure, lipids, insulin sensitivity); parental stress, self-efficacy, and quality of life; a child’s BMI, or weight stabilization; and parent or caregiver BMI.
Priority Populations: Defined in the 2320 notice of funding opportunity as those who have systematically experienced greater obstacles to health based on their racial or ethnic group, religion, socioeconomic status, gender, age, mental health, cognitive, sensory, or physical disability, sexual orientation or gender identity, geographic location, or other characteristics historically linked to discrimination or exclusion. Priority populations of focus will be determined by each award recipient.
Social Determinants of Health (SDOH): Social determinants of health are the nonmedical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies, racism, climate change, and political systems.
2017 National Standards for Diabetes Self-Management Education and Support: This article by the 2017 Standards Revision Task Force introduces the 2017 edition of the National Standards.
DSMES Toolkit: https://www.cdc.gov/diabetes/dsmes-toolkit/index.html
Balamurugan, A et al. Barriers to Diabetes Self-Management Education Programs in Underserved Rural Arkansas: Implications for Program Evaluation. Prev Chronic Dis 2006;3(1):1-8. (http://www.ncbi.nlm.nih.gov/pubmed/16356368)
Duncan I, Birkemeyer C, Coughlin S, Li QE, Sherr D, Boren S. Assessing the value of diabetes education. Diabetes Educ. 2009 Sep-Oct;35(5):752-60. (http://www.ncbi.nlm.nih.gov/pubmed/19783766)
Powers M, et al. Diabetes Self-management Education and Support in Type 2 Diabetes: A Joint Position Statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. J Acad Nutr Diet. 2015 Aug;115(8):1323-34. (https://www.ncbi.nlm.nih.gov/pubmed/26054423?report=abstract)
Page
| File Type | application/vnd.openxmlformats-officedocument.wordprocessingml.document |
| Author | Alexander, Dayna |
| File Modified | 0000-00-00 |
| File Created | 2024-11-14 |
© 2026 OMB.report | Privacy Policy